Abstract
An outbreak of respiratory illness proved to be infected by a 2019 novel coronavirus, officially named Coronavirus Disease 2019 (COVID-19), was notified first in Wuhan, China, and has spread rapidly in China and to other parts of the world. Herein, we reported the first confirmed case of novel coronavirus pneumonia (NCP) imported from China in Taiwan. This case report revealed a natural course of NCP with self-recovery, which may be a good example in comparison with medical treatments.
Keywords: COVID-19, First case, Pneumonia, Taiwan
Introduction
On December 31, 2019, an outbreak of respiratory illness later proved to be caused by a novel coronavirus, officially named Coronavirus Disease 2019 (COVID-19), was notified first in Wuhan, a city of Hubei province, People's Republic of China (PRC). COVID-19 rapidly spreads in China and to other parts of the world. Currently more than 70,000 laboratory-confirmed cases in China have been reported, and the case count has been rising daily. Some travelers-related transmission were also identified in many countries, including Taiwan, Singapore, Vietnam, Republic of Korea, Malaysia, Thailand, Japan, Germany, France, United States (U.S.), Australia, etc. through an international conveyance, and raised a global health emergency.1 As of February 18, 2020, there were 22 confirmed cases in Taiwan. Herein we presented the first case identified in Taiwan on January 21, 2020.
Case report
On January 20, 2020, a 55-year-old woman who worked in Wuhan, China, arrived at Taiwan Taoyuan International Airport and presented to quarantine officials immediately, with a history of sore throat, dry cough, fatigue, and low-grade subjective fever since January 11, 2020. Owing to the outbreak of COVID-19 in Wuhan city and the announcement of related symptoms, she was immediately placed in quarantine ward and underwent examination. Although the patient denied spending time at the Huanan Seafood Wholesale Market and reported no known contact with ill people during her stay in Wuhan, specimens including oropharyngeal swab and sputum were collected for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) real-time reverse-transcriptase-polymerase-chain-reaction (rRT-PCR) in accordance with the Taiwan Centers for Disease Control (TCDC) guidance.
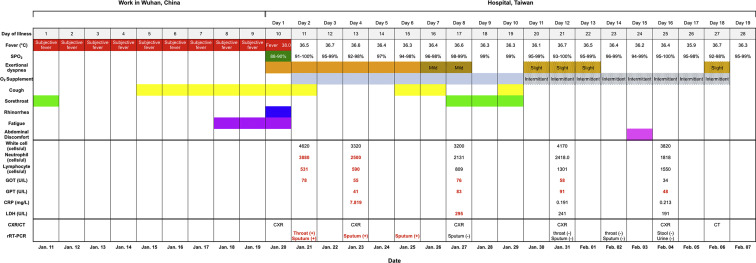
Apart from a history of hypothyroidism with regular medical follow-up, she had no other underlying disease before this onset. According to the records of quarantine officials, the vital sign of the patient showed body temperature (BT) of 38.0 °C and oxygen saturation (SPO2) of 88–90% under ambient air. Before seeking medical treatment in Taiwan, she bought over-the-counter medicine to release the symptoms. After admission to our hospital, her vital signs remained stable, apart from the exertional dyspnea, intermittent dry cough and sore throat (Fig. 1 ). The initial physical examination revealed a BT of 36.4 °C, blood pressure of 93/53 mm Hg, pulse of 87 bpm, respiratory rate of 20 breath/min, and SPO2 of 91% while the patient was breathing supplement oxygen by nasal cannula at 3 L/min. The breathing sound was normal initially. The laboratory results reflected lymphopenia (531 cells/ul), and elevated aspartate aminotransferase (AST, 78 U/L), alanine aminotransferase (ALT, 41 U/L), C-reactive protein (CRP, 7.8 mg/L), and lactate dehydrogenase (LDH, 295 U/L) (Fig. 1). A rapid screening test for influenza A and B showed negative. The chest X-ray revealed bilateral perihilar infiltration and ill-defined patchy opacities. On January 21, 2020, the TCDC confirmed that the patient's oropharyngeal swab and sputum tested positive for SARS-CoV-2 by rRT-PCR assay.
Figure 1.
Vital sign, symptoms, and examination by the day of illness and day of hospitalization, January 11 to February 07, 2020.
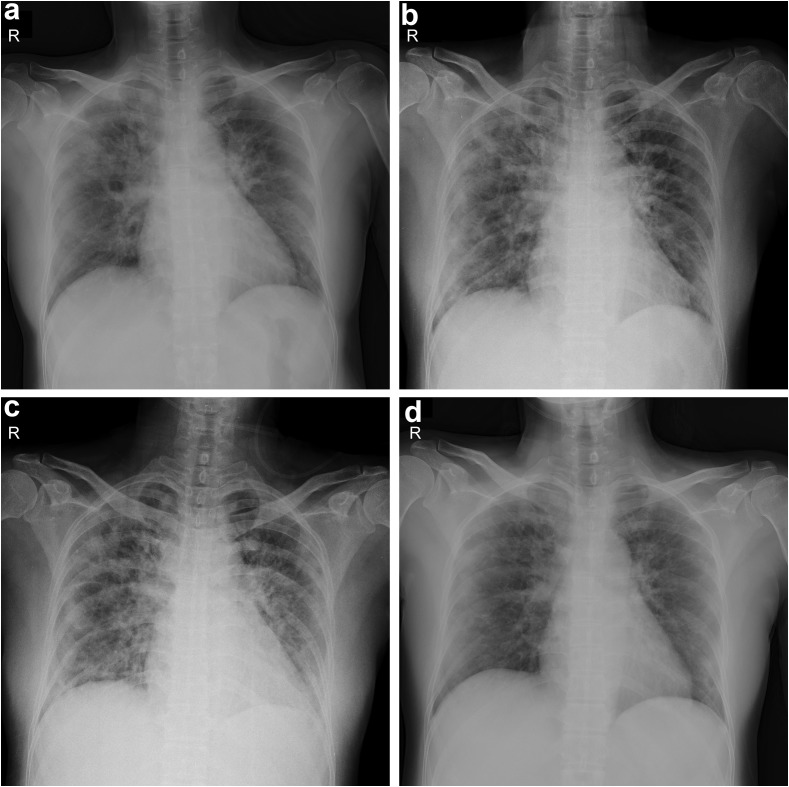
The results of serial chest X-rays performed on illness day 10 (hospital day 1), 13, 17, and 25 coincided with the changes in SPO2 and revealed slowing remission of worsening patches infiltrating at first (Fig. 2 ). These radiographic findings and a subsequent chest computed tomography (CT) indicated the tenacious COVID-19 pneumonia and sequelae (Fig. 3 ). Antitussive agent, O2 supplement, careful saline infusion and empiric antibiotic with ceftriaxone (2 gm loading and 2 gm everyday intravenously) were administered at first. Subsequently, antibiotics were replaced by oral amoxicillin/clavulanate 875/125 mg every 12 h on illness day 17 for another 1 week. Her urine culture showed Streptococcus gallolyticus spp pasteurianus, which was susceptible to above antibiotics. Other cultures showed non-significance.
Figure 2.
Chest X-ray showed progression of prominent bilateral perihilar infiltration and ill-defined patchy opacities at bilateral lungs, which slowly resolved on the follow-up image. (a: January 20; b: Jan. 23; c: Jan. 27; d: February 04).
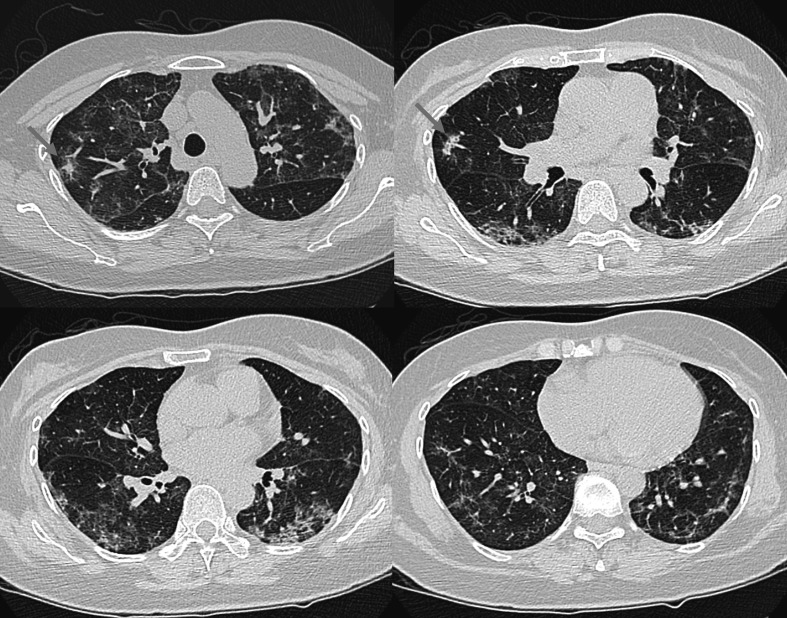
Figure 3.
Chest CT in convalescent stage showed persistent multifocal GGOs with or without superimposed reticulation and mild fibrotic change at bilateral lungs, including peripheral subpleural regions of both lower lobes. Two small irregular opacities at the RUL and RML were probably partially resolved consolidations (arrows).
On illness day 17, her sputum turned undetectable for SARS-CoV-2 by rRT-PCR assay. The results of subsequent rRT-PCR of oropharyngeal swabs and sputum on illness day 21 and 23, respectively, were repeatedly negative. Supplemental oxygen was discontinued on illness day 27, and her SPO2 improved to 92%–98% under ambient air. The patient's clinical condition improved, apart from intermittent exertional dyspnea. Furthermore, the final results of rRT-PCR of stool and urine tests, which were not sent for tests in the beginning, were negative on illness day 25. She was then discharged on illness day 28 (February 07, 2020).
Discussion
We reported the first confirmed case of novel coronavirus pneumonia (NCP) in Taiwan. In accordance with the first report from China, the major symptoms of COVID-19 infection were mainly cough, fever and dyspnea.2 Our case presented with mild fever, dyspnea and mild hypoxemia on day 10 of initial illness. At the same time, the chest X-ray showed bilateral infiltrating pneumonia, which progressed diffusely later. The progression of symptoms in this case also coincided with the first confirmed COVID-19 case in the U.S., with fever on day 5 of illness, dyspnea with mild hypoxemia and radiographical pneumonia on day 9 of illness.3 Furthermore, reports from China showed all patients had bilateral pneumonia on high resolution CT with different severity even in mild cases.2 , 4 These findings suggested that lower respiratory tract seems to be an important location for the replication of SARS-CoV-2. Our case turned afebrile since admission (illness day 10), even without antiviral treatment. Despite pneumonia on chest X-rays worsen in the following seven days, respiratory failure did not occur eventually. Even though ceftriaxone was used, the evidence of negative culture and the worsening chest X-ray findings under antibiotic treatment were not compatible with the clinical picture of bacterial pneumonia. The effective medical treatment against COVID-19 remains unknown. In spite of the first-reported case in the U.S. showing promptly-subsided fever after Remdesivir used on day 12 of illness, with well-improved clinical symptoms later, the effectiveness of Remdesivir was still questioned.3 The randomized-controlled trial of treating Middle East respiratory syndrome coronavirus by the combination of lopinavir/ritonavir/interferon-beta-1b is ongoing, more evidence-based data are needed.5
Some laboratory abnormalities in our case, such as elevated CRP, LDH, ALT and AST, were also observed in influenza virus pandemic.6 Lymphopenia has been considered as a poor prognostic factor for severe hospitalized influenza (H1N1) pandemic 2009,7 as well as severe acute respiratory syndrome (SARS).8 These findings may explain common biomarker presentation in viral pneumonia, including COVID-19. The quarantine period for potentially COVID-19 infected individuals was challenging by our case's laboratory results, her sputum specimens remained positive for SARS-CoV-2 on day 15 and turned negative on day 17 of illness.
Similar to viral pneumonia due to other etiologies, ground-glass opacities (GGOs) are the main CT findings of the patients with COVID-19.9, 10, 11, 12 Reticular and/or interlobular septal thickening, and consolidation are common associated findings.9 Crazy-paving pattern was also detected in some cases.10 , 13 Pure consolidation without GGO is less common.10 These lesions usually involve bilateral lungs.9 , 10 Peripheral distribution of disease was noted in 33% and 85% of patients, respectively.9 , 10 However, normal scan at the early stage of COVID-19 can be found in a few patients when the disease is diagnosed.10
As the NCP progresses, increasing size and density of these GGOs or crazy paving pattern were reported.9 , 10 , 13 , 15 On the contrary, the GGOs will decrease in size and the consolidations, if present, will decrease in density when patients gradually recover.9 , 15 , 16 Fibrotic change may be left as a sequela after recovery as was seen in patients recovering from SARS.14 , 15
Our case demonstrated a typical NCP without progression to ARDS. The worst status of her pneumonia was on illness day 17 (Fig. 2c) and then gradually resolved. Given the negative rRT-PCR of SARS-CoV-2 on illness day 21 and 23, there were persistent milder bilateral lung opacities on the chest radiograph on illness day 25 (Fig. 2d) which were corresponding to bilateral ill-defined GGO patches with or without reticulation, and mild fibrotic change on CT two days later (Fig. 3). Chest CT might be a tool to assist diagnosis accompanying with symptoms and traveling history, because the chest radiograph could be normal in those patients with mild or no symptoms.3
In summary, our case revealed a natural course of NCP with self-recovery. Rapid diagnostic assays, effective treatment and wide use of chest CT will be crucial to contain the worldwide outbreak of COVID-19 in the future.
Conflict of Interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
The authors thank the dedicated medical team, Hsiu-Hsueh Tseng, PhD and Shu-Hsing Cheng, MD for manuscript preparation, professor Yeun-Chung Chang and professor Shan-Chwen Chang for expert opinions.
Contributor Information
Chia-Husn Huang, Email: 4719@mail.tygh.gov.tw.
Yuan-Nian Hsu, Email: kingjen@mail.tygh.gov.tw.
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2020. Novel coronavirus situation report -28.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200217-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2 [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;S0140–6736(20):30183–30185. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Englera J Med. 2020:1–9. doi: 10.1056/NEJMoa2001191. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J Am Med Assoc. 2020:E1–E9. doi: 10.1001/jama.2020.1585. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arabi Y.M., Alothman A., Balkhy H.H., Al-Dawood A., AlJohani S., Al Harbi S. Treatment of Middle East respiratory syndrome with a combination of lopinavir-ritonavir and interferon-beta1b (MIRACLE trial): study protocol for a randomized controlled trial. Trials. 2018;19:81–93. doi: 10.1186/s13063-017-2427-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song J.Y., Cheong H.J., Heo J.Y., Noh J.Y., Yong H.S., Kim Y.K. Clinical, laboratory and radiologic characteristics of 2009 pandemic influenza A/H1N1 pneumonia: primary influenza pneumonia versus concomitant/secondary bacterial pneumonia. Influenza Other Respir Viruses. 2011;5:e535–e543. doi: 10.1111/j.1750-2659.2011.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F., Li H., Gu L., Liu M., Xue C.X., Cao B. Risk factors for nosocomial infection among hospitalised severe influenza A(H1N1) pandemic 2009 patients. Respir Med. 2018;134:86–91. doi: 10.1016/j.rmed.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 8.Leung G.M., Hedley A.J., Ho L.M., Chau P., Wong I.O., Thach T.Q. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann Intern Med. 2004;141:662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- 9.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H. Emerging coronavirus 2019-nCoV pneumonia. Radiology. 2020:200274. https://doi: 10.1148/radiol.2020200274 [Google Scholar]
- 10.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020:200230. doi: 10.1148/radiol.2020200230. https://doi: 10.1148/radiol.2020200230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lei J., Li J., Li X., Qi X. CT Imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020:200236. doi: 10.1148/radiol.2020200236. https://doi: 10.1148/radiol.2020200236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu P., Tan X.Z. 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020:200257. doi: 10.1148/radiol.2020200257. https://doi: 10.1148/radiol.2020200257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fang Y., Zhang H., Xu Y., Xie J., Pang P., Ji W. CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020:200280. doi: 10.1148/radiol.2020200280. https://doi: 10.1148/radiol.2020200280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang Y.C., Yu C.J., Chang S.C., Galvin J.R., Liu H.M., Hsiao C.H. Pulmonary sequelae in convalescent patients after severe acute respiratory syndrome: evaluation with thin-section CT. Radiology. 2005;236:1067–1075. doi: 10.1148/radiol.2363040958. [DOI] [PubMed] [Google Scholar]
- 15.Pan Y., Guan H. Imaging changes in patients with 2019-nCov. Eur Radiol. 2020 doi: 10.1007/s00330-020-06713-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi H., Han X., Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology. 2020:200269. doi: 10.1148/radiol.2020200269. https://doi: 10.1148/radiol.2020200269 [DOI] [PMC free article] [PubMed] [Google Scholar]