Abstract
Purpose
The study aimed to examine query strategies that would provide an exhaustive search method to retrieve the most referenced articles within specific categories of critical care.
Material and Methods
A comprehensive list of the most cited critical care medicine articles was generated by searching the Science Citation Index Expanded data set using general critical care terms keywords such as “critical care,” critical care journal titles, and keywords for subsubjects of critical care.
Results
The final database included 1187 articles published between 1905 and 2006. The most cited article was referenced 4909 times. The most productive search term was intensive care. However, this term only retrieved 25% of the top 100 articles. Furthermore, 662 of the top 1000 articles could not be found using any of the basic critical care search terms. Sepsis, acute lung injury, and mechanical ventilation were the most common areas of focus for the articles retrieved.
Conclusion
Retrieving frequently cited, influential articles in critical care requires using multiple search terms and manuscript sources. Periodic compilations of most cited articles may be useful for critical care practitioners and researches to keep abreast of important information.
Keywords: Critical care, ICU, Citation classics, Landmark articles
1. Introduction
Modern methods to search for important medial literature have recently flourished with the dissemination and near ubiquity of Internet-based search engines (eg, PubMed, MEDLINE, OVID). Articles that have been cited most often, referred to as “citation classics,” are frequently important sources of both detailed information that has changed clinical/research practices as well as of useful connectors to other relevant literature that cites these articles. Finding landmarks or classic articles still requires an understanding of the literature and how articles are referenced. Different databases may categorize disciplines and journals from the same clinical areas under different terms and yield different results when using the same search term.
These referencing differences as well as other conceptual arguments have led to some debate regarding attributing the number of times an article is cited to its quality [1], [2], [3], [4] However, there is general agreement that the number of times an article is cited does reflect the “impact of that article on the scientific market” [5].
Garfield [6] first published citation classics of the Journal of the American Medical Association in 1987. Similar studies (citations classic or impact factors) have been published with respect to various clinical specialties [7], [8], [9], [10], [11], [12], [13], [14], [15]. In 2004, Baltussen and Kindler [16] published citation classics of the critical care literature and enumerated the 71 top-cited articles in critical care journals and the 45 top-cited critical care articles in non–critical care journals. This article was somewhat limited by the number of citations referenced as well as the absence of specific critical care topic citations groups. The first and primary aim of this study was to expand on Baltussen's earlier work and provide an updated and more comprehensive catalogue of the most influential articles pertaining to critical care medicine and within specific categories of critical care, something not done in previous studies of this type. We also examined the methods used to retrieve articles to provide an exhaustive search method that future researchers may use in modern electronic databases to find frequently cited critical care articles.
2. Methods
2.1. Creation of master comprehensive list
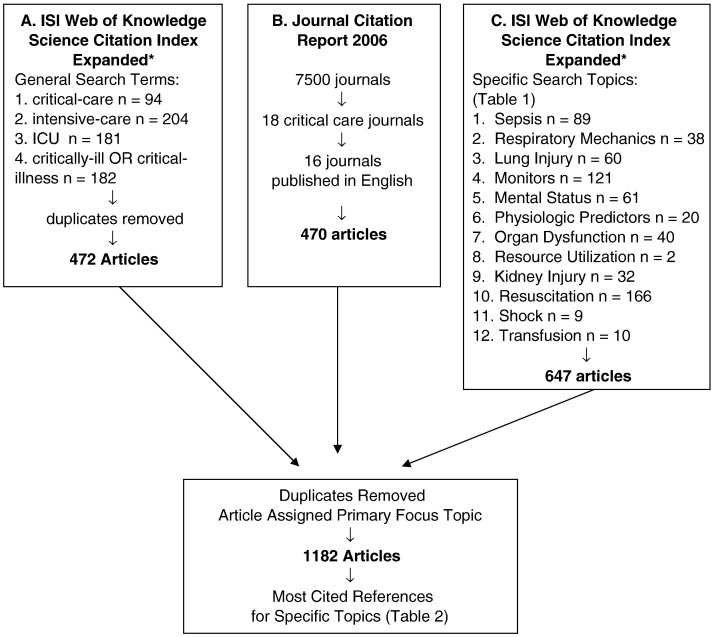
To develop the most comprehensive master list of most often cited critical care medicine–related articles, we first focused on querying the ISI Web of Knowledge (2008 Thompson Corporation) using the Science Citation Index Expanded (SCI Expanded) data set. The SCI Expanded is a database that provides bibliographic information, abstracts, references, and citations counts for more than 6650 scholarly science and technology journals. The SCI Expanded search was limited to articles published from 1900 to December 31, 2007. To find any article among the broadest selection of scientific journals related to critical care, we searched for any article that contained the keywords “critical-care,” “intensive-care,” “ICU,” or “critically-ill OR critical-illness” and that had been cited more than 100 times. A total of 472 articles were retrieved with this technique after duplicates were removed (see Fig. 1A).
Fig. 1.
Methods.
Because many critical care articles found in the SCI Expanded were not tagged by the general keywords noted above, we also searched within critical care journals. To do this, we used the Journal Citation Report (JCR) 2006 to identify journals specializing in critical care medicine from more than 7500 scholarly journals. We first reduced the target list to 16 English-language journals of 18 critical care journals identified by the JCR. We reviewed any article that had been cited more than 100 times and saved articles pertaining to critical care medicine (Fig. 1B). This search resulted in 470 hits; however, we removed 159 duplicate articles that were already found by keyword searches to bring the total database to 783 articles (Fig. 1).
2.2. Creation of disease/condition-specific lists
A representative list of most cited articles for each of the specific critical care topics was created from the existing database and by searching each topic individually using the terms in Table 1 . Using these search terms, articles pertinent to critical care and referenced more than 100 times were added to the database. These searches by specific disease or conditions added 404 articles to the master database as 194 articles were already in the database from either the initial search or from the journal search. From this master database of 1187 articles, we then generated a list of all articles cited more than 150 times (Table 2 ). We organized this table by topics particularly relevant to critical care. Within each category we listed both the most cited articles within that topic as well as that article's ranking within the top 200 most cited articles. Finally, we also listed the absolute number of citations for each article.
Table 1.
Specific critical care subjects
| Subject area | Search terms |
|---|---|
| Sepsis and infectious disease | “sepsis” “septic*” “nosocomial” “blood stream” |
| Mechanical ventilation and lung injury | “ventilation” “respiratory failure” “pulmonary failure” “weaning” “extubation” “ventilator” “PEEP” “positive end expiratory pressure” “noninvasive” “ARDS” “respiratory-distress” “lung injury” |
| Monitors | “hemodynamic-monitor” “CVC” “physiologic-monitor” “noninvasive-monitor” “catheter*” “central venous” “pulmonary-artery-catheter” “Swan-Ganz” “ultrasound” “Doppler” “pressure variation” |
| Mental status | “coma” “brain-damage” “brain-injury” “ICU AND delirium” “ICU AND sedation” |
| Physiologic predictors | “physiology score” “severity of illness” “severity of disease” “mortality-predict” “severity-score” |
| Organ dysfunction | “organ-failure” “organ-dysfunction” “MODS” “MSOF” |
| Resource utilization | “intensivist” “leap frog” “ICU-administration” “critical care management” “ICU management” |
| Kidney injury | “kidney-injury” “renal-failure” “dialysis” “renal-replacement-therapy” “CVVH*” “CRRT” |
| Resuscitation | “life-support” “cardiac-arrest” “cpr” “resuscitation” “cardiac massage” “cardiac-life-support” “fluid” “saline” “lactated” “albumin” “colloid” “crystalloid” |
| Shock (excluding infectious causes) | “shock” “hypoperfusion” “CHF” “heart-failure” |
| Transfusions | “transfusion” “fluid-therapy” |
⁎Denotes any form of the word preceding the symbol, i.e., septic shock, septic.
Table 2.
Most cited articles in critical care medicine by subject
| Overall Citation Rank |
|---|
| A. Sepsis/systemic inflammatory response syndrome (no. of times cited) |
| 1. (#6) Tracey, KJ et al. Anti-cachectin TNF monoclonal-antibodies prevent septic shock during lethal bacteremia. Nature 1987. (1983) |
| 2. (#7) Bone, RC et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992. (1838) |
| 3. (#8) Bernard, GR et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001. (1827) |
| 4. (#10) Bone, RC et al. American-College of Chest Physicians Society of Critical Care Medicine Consensus Conference—definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992. (1724) |
| 5. (#12) Van den Berghe, G et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001. (1608) |
| 6. (#19) Ziegler, EJ et al. Treatment of gram-negative bacteremia and septic shock with HA-1a human monoclonal-antibody against endotoxin—a randomized, double-blind, placebo-controlled trial. N Engl J Med 1991. (1072) |
| 7. (#22) Angus, DC et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001. (1016) |
| 8. (#25) Bone, RC. The pathogenesis of sepsis. Ann Intern Med 1991. (982) |
| 9. (#28) Waage, A et al. The complex pattern of cytokines in serum from patients with meningococcal septic shock—association between interleukin-6, interleukin-1, and fatal outcome. J Exp Med 1989. (892) |
| 10. (#31) Wichterman, KA et al. Sepsis and septic shock—a review of laboratory models and a proposal. J Surg Res 1980. (846) |
| 11. (#34) Bone, RC et al. A controlled clinical-trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med 1987. (791) |
| 12. (#37) Parrillo, JE. Mechanisms of disease—pathogenetic mechanisms of septic shock. N Engl J Med 1993. (756) |
| 13. (#41) Annane, D et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002. (712) |
| 14. (#43) Petros, A et al. Effect of nitric-oxide synthase inhibitors on hypotension in patients with septic shock. Lancet 1991. (705) |
| 15. (#52) Cannon, JG et al. Circulating interleukin-1 and tumor necrosis factor in septic shock and experimental endotoxin fever. J Infect Dis 1990. (642) |
| 16. (#55) Casey, LC et al. Plasma cytokine and endotoxin levels correlate with survival in patients with the sepsis syndrome. Ann Intern Med 1993. (624) |
| 17. (#56) Vanzee, KJ et al. Tumor-necrosis-factor soluble receptors circulate during experimental and clinical inflammation and can protect against excessive tumor-necrosis-factor–alpha in vitro and in vivo. Proc Nat Acad Sci USA 1992. (600) |
| 18. (#59) Hack, CE et al. Increased plasma-levels of interleukin-6 in sepsis. Blood 1989. (589) |
| 19. (#62) Moore, FA et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications—the results of a metaanalysis. Ann Surg 1992. (578) |
| 20. (#64) Lowenstein, CJ et al. Nitric-oxide—a physiological messenger. Ann Intern Med 1994. (574) |
| 21. (#69) Fry, DE et al. Multiple system organ failure—role of uncontrolled infection. Arch Surg 1980. (549) |
| 22. (#70) Parker, MM et al. Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med 1984. (548) |
| 23. (#72) Kudsk, KA et al. Enteral versus parenteral-feeding—effects on septic morbidity after blunt and penetrating abdominal-trauma. Ann Surg 1992. (543) |
| 24. (#75) Fisher, CJ et al. Treatment of septic shock with the tumor necrosis factor receptor:Fc fusion protein. N Engl J Med 1996. (540) |
| 25. (#77) Hotchkiss, RS et al. Medical progress: the pathophysiology and treatment of sepsis. N Engl J Med 2003. (538) |
| 26. (#78) Greenman, RL et al. A controlled clinical-trial of E5 murine monoclonal IgM antibody to endotoxin in the treatment of gram-negative sepsis. JAMA 1991. (536) |
| 27. (#81) Martin, GS et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003. (529) |
| 28. (#83) Glauser, MP et al. Septic shock—pathogenesis. Lancet 1991. (522) |
| 29. (#89) Dellinger, RP et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004. (513) |
| 30. (#94) Bone, RC et al. Sepsis syndrome—a valid clinical entity. Crit Care Med 1989. (506) |
| 31. (#96) Fisher, CJ et al. Recombinant human interleukin-1 receptor antagonist in the treatment of patients with sepsis syndrome—results from a randomized, double-blind, placebo-controlled trial. JAMA 1994. (499) |
| 32. (#97) Parrillo, JE et al. Septic shock in humans—advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med 1990. (499) |
| 33. (#105) Assicot, M et al. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993. (481) |
| 34. (#109) Ochoa, JB et al. Nitrogen-oxide levels in patients after trauma and during sepsis. Ann Surg 1991. (464) |
| 35. (#114) Moore, FA et al. TEN versus TPN following major abdominal-trauma–reduced septic morbidity. J Trauma 1997. (435) |
| 36. (#120) Abraham, E et al. Efficacy and safety of monoclonal-antibody to human tumor necrosis-factor–alpha in patients with sepsis syndrome—a randomized, controlled, double-blind, multicenter clinical-trial. JAMA 1995. (425) |
| 37. (#121) Meakins, JL et al. Delayed-hypersensitivity—indicator of acquired failure of host defenses in sepsis and trauma. Ann Surg 1977. (425) |
| 38. (#122) Pinsky, MR et al. Serum cytokine levels in human septic shock—relation to multiple system organ failure and mortality. Chest 1993. (422) |
| 39. (#131) Danner, RL et al. Endotoxemia in human septic shock. Chest 1991. (409) |
| 40. (#132) Eickhoff, TC et al. Neonatal sepsis + other infections due to group b beta-hemolytic streptococci. N Engl J Med 1964. (408) |
| 41. (#134) Wheeler, AP et al. Treating patients with severe sepsis. N Engl J Med 1999. (405) |
| 42. (#151) Sprung, CL et al. The effects of high-dose corticosteroids in patients with septic shock—a prospective, controlled-study. N Engl J Med 1984. (386) |
| 43. (#153) Damas, P et al. Cytokine serum level during severe sepsis in human il-6 as a marker of severity. Ann Surg 1992. (382) |
| 44. (#157) Askanazi, J et al. Influence of total parenteral-nutrition on fuel utilization in injury and sepsis. Ann Surg 1980. (377) |
| 45. (#162) Docke, WD et al. Monocyte deactivation in septic patients: restoration by IFN-gamma treatment. Nature Med 1997. (372) |
| 46. (#168) Petros, A et al. Effects of a nitric-oxide synthase inhibitor in humans with septic shock. Cardiovasc Res 1994. (366) |
| 47. (#173) BrunBuisson, C et al. Incidence, risk-factors, and outcome of severe sepsis and septic shock in adults—a multicenter prospective-study in intensive-care units. JAMA 1995. (361) |
| 48. (#174) Nava, E et al. Inhibition of nitric-oxide synthesis in septic shock—how much is beneficial. Lancet 1991. (361) |
| 49. (#178) Szabo, C. The pathophysiological role of peroxynitrite in shock, inflammation, and ischemia-reperfusion injury. Shock 1996. (350) |
| 50. (#180) Warren, BL et al. High-dose a randomized antithrombin III in severe sepsis—a randomized controlled trial. JAMA 2001. (348) |
| 51. (#181) Bone, RC. Sir Isaac Newton, Sepsis, SIRS, and cars. Crit Care Med 1996. (348) |
| 52. (#182) Schumer, W. Steroids in treatment of clinical septic shock. Ann Surg 1976. (348) |
| 53. (#183) Damas, P et al. Tumor necrosis factor and interleukin-1 serum levels during severe sepsis in humans. Crit Care Med 1989. (346) |
| 54. (#185) Cohen, J et al. The immunopathogenesis of sepsis. Nature 2002. (345) |
| 55. (#187) Rush, BF et al. Endotoxemia and bacteremia during hemorrhagic-shock—the link between trauma and sepsis. Ann Surg 1988. (341) |
| 56. (#190) Fourrier, F et al. Septic shock, multiple organ failure, and disseminated intravascular coagulation—compared patterns of antithrombin-III, protein-C, and protein-S deficiencies. Chest 1992. (339) |
| 57. (#192) Munoz, C et al. Dysregulation of in vitro cytokine production by monocytes during sepsis. J Clin Invest 1991. (336) |
| B. Outcome/benchmarking/prediction model articles (no. of times cited) |
|---|
| 1. (#1) Knaus, WA et al. APACHE-II—a severity of disease classification-system. Crit Care Med 1985. (4909) |
| 2. (#4) Baker, SP et al. Injury severity score—method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974. (2637) |
| 3. (#13) Legall, JR et al. A new simplified acute physiology score (SAPS-II) based on a European North-American multicenter study. JAMA 1993. (1402) |
| 4. (#14) Knaus, WA et al. The APACHE-III prognostic system—risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991. (1357) |
| 5. (#21) Knaus, WA et al. A controlled trial to improve care for seriously ill hospitalized-patients—the study to understand prognoses and preferences for outcomes and risks of treatments (support). JAMA 1995. (1056) |
| 6. (#26) Fine, MJ et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997. (965) |
| 7. (#33) Deitch, EA. Multiple organ failure—pathophysiology and potential future therapy. Ann Surg 1992. (793) |
| 8. (#36) Knaus, WA et al. APACHE-acute physiology and chronic health evaluation—a physiologically based classification-system. Crit Care Med 1981. (758) |
| 9. (#38) Vincent, JL et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intens Care Med 1996. (735) |
| 10. (#40) Knaus, WA et al. An evaluation of outcome from intensive-care in major medical centers. Ann Intern Med 1986. (715) |
| 11. (#47) Legall, JR et al. A simplified acute physiology score for ICU patients. Crit Care Med 1984. (667) |
| 12. (#49) Boyd, CR et al. Evaluating trauma care—the TRISS method. J Trauma 2001. (658) |
| 13. (#58) Marshall, JC et al. Multiple organ dysfunction score—a reliable descriptor of a complex clinical outcome. Crit Care Med 1995. (592) |
| 14. (#63) Carrico, CJ et al. Multiple-organ-failure syndrome. Arch Surg 1986. (575) |
| 15. (#80) Baker, SP et al. Injury severity score—update. J Trauma 1997. (532) |
| 16. (#87) Champion, HR et al. A revision of the trauma score. J Trauma 1997. (516) |
| 17. (#98) Pollack, MM et al. Pediatric risk of mortality (prism) score. Crit Care Med 1988. (498) |
| 18. (#103) Champion, HR et al. Trauma score. Crit Care Med 1981. (486) |
| 19. (#112) Keene, AR et al. Therapeutic intervention scoring system—update 1983. Crit Care Med 1983. (444) |
| 20. (#115) Higgins, TL et al. Stratification of morbidity and mortality outcome by preoperative risk-factors in coronary-artery bypass patients—a clinical severity score. JAMA 1992. (435) |
| 21. (#149) Lemeshow, S et al. Mortality probability-models (MPM-II) based on an international cohort of intensive-care unit patients. JAMA 1993. (388) |
| 22. (#150) Champion, HR et al. The major trauma outcome study—establishing national norms for trauma care. J Trauma 1996. (386) |
| 23. (#169) Takala, J et al. Increased mortality associated with growth hormone treatment in critically ill adults. N Engl J Med 1999. (365) |
| 24. (#184) Vincent, JL et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med 1998. (346) |
| 25. (#197) Faist, E et al. Multiple organ failure in polytrauma patients. J Trauma 1995. (332) |
| 26. Moore, EE et al. Organ injury scaling—spleen, liver, and kidney. J Trauma 1995. (317) |
| 27. Cockburn, F et al. The CRIB (clinical risk index for babies) score—a tool for assessing initial neonatal risk and comparing performance of neonatal intensive-care units. Lancet 1993. (273) |
| 28. Greenspan, L et al. Abbreviated injury scale and injury severity score—a scoring chart. J Trauma 1993. (267) |
| 29. Ware, JE et al. Comparison of methods for the scoring and statistical-analysis of SF-36 health profile and summary measures—summary of results from the medical outcomes study. Med Care 1995. (259) |
| 30. Richardson, DK et al. Score for neonatal acute physiology—a physiological severity index for neonatal intensive-care. Pediatrics 1993. (252) |
| 31. Moore, EE et al. Organ injury scaling—spleen and liver [1994 revision]. J Trauma 1993. (233) |
| 32. Copes, WS et al. The injury severity score revisited. J Trauma 1988. (217) |
| 33. Pollack, MM et al. PRISM III: an updated pediatric risk of mortality score. Crit Care Med 1996. (212) |
| C. Mechanical and positive pressure ventilation/airway articles (no. of times cited) |
|---|
| 1. (#9) Brower, RG et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000. (1750) |
| 2. (#27) Amato, MBP et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998. (911) |
| 3. (#42) Gregory, GA et al. Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med 1971. (708) |
| 4. (#44) Suter, PM et al. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 1975. (698) |
| 5. (#53) Dreyfuss, D et al. Ventilator-induced lung injury—lessons from experimental studies. Am J Resp Crit Care 1992. (641) |
| 6. (#65) Brochard, L et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary-disease. N Engl J Med 1995. (561) |
| 7. (#85) Stauffer, JL et al. Complications and consequences of endotracheal intubation and tracheotomy—a prospective-study of 150 critically ill adult patients. Am J Med 1981. (517) |
| 8. (#93) Ranieri, VM et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome—a randomized controlled trial. JAMA 1999. (508) |
| 9. (#106) Nash, G et al. Pulmonary lesions associated with oxygen therapy and artificial ventilation. N Engl J Med 1967. (478) |
| 10. (#108) Bendixen, HH et al. Impaired oxygenation in surgical patients during general anesthesia with controlled ventilation—a concept of atelectasis. N Engl J Med 1963. (465) |
| 11. (#111) Webb, HH et al. Experimental pulmonary-edema due to intermittent positive pressure ventilation with high inflation pressures. protection by positive end-expiratory pressure. Amer Rev Resp Dis 1974. (445) |
| 12. (#113) Boyd, O et al. A randomized clinical-trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA 1993. (439) |
| 13. (#129) Muscedere, JG et al. Tidal ventilation at low airway pressures can augment lung injury. Am J Resp Crit Care 1994. (412) |
| 14. (#135) Kumar, A et al. Continuous positive-pressure ventilation in acute respiratory failure—effects on hemodynamics and lung function. N Engl J Med 1970. (403) |
| 15. (#138) Hickling, KG et al. Low mortality associated with low-volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory-distress syndrome. Intens Care Med 1990. (402) |
| 16. (#139) Aroroa, NS et al. Respiratory muscle strength and maximal voluntary ventilation in undernourished patients. Amer Rev Resp Dis 1982. (402) |
| 17. (#142) Kolobow, T et al. Severe impairment in lung-function induced by high peak airway pressure during mechanical ventilation—an experimental-study. Amer Rev Resp Dis 1987. (398) |
| 18. (#147) Haldine, JS et al. The regulation of the lung-ventilation. J Physiol-London 1905. (390) |
| 19. (#154) Ashbaugh, DG et al. Continuous positive-pressure breathing (CPPB) in adult respiratory distress syndrome. J Thorac Cardiov Surg 1969. (382) |
| 20. (#196) Bott, J et al. Randomized controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet 1993. (333) |
| 21. Falke, KJ et al. Ventilation with end-expiratory pressure in acute lung-disease. J Clin Invest 1972. (325) |
| 22. Kramer, N et al. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory-failure. Am J Resp Crit Care 1995. (323) |
| 23. Stewart, TE et al. Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. N Engl J Med 1998. (322) |
| 24. Yang, KL et al. A prospective-study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991. (322) |
| 25. Gattinoni, L et al. Low-frequency positive-pressure ventilation with extracorporeal CO2 removal in severe acute respiratory-failure. JAMA 1986. (321) |
| D. Acute lung injury/adult respiratory distress syndrome articles (no. of times cited) |
|---|
| 1. (#11) Bernard, GR et al. The American-European Consensus Conference on ARDS—definitions, mechanisms, relevant outcomes, and clinical-trial coordination. Am J Resp Crit Care 1994. (1627) |
| 2. (#16) Ashbaugh, DG et al. Acute respiratory distress in adults. Lancet 1967. (1283) |
| 3. (#17) Murray, JF et al. An expanded definition of the adult respiratory-distress syndrome. Amer Rev Resp Dis 1988. (1133) |
| 4. (#18) Rossaint, R et al. Inhaled nitric-oxide for the adult respiratory-distress syndrome. N Engl J Med 1993. (1083) |
| 5. (#32) Ware, LB et al. Medical progress—the acute respiratory distress syndrome. N Engl J Med 2000. (794) |
| 6. (#46) Tate, RM et al. Neutrophils and the adult respiratory-distress syndrome. Amer Rev Resp Dis 1983. (668) |
| 7. (#48) Montgomery, AB et al. Causes of mortality in patients with the adult respiratory-distress syndrome. Amer Rev Resp Dis 1985. (663) |
| 8. (#51) Brigham, KL et al. Endotoxin and lung injury. Amer Rev Resp Dis 1986. (650) |
| 9. (#57) Rinaldo, JE et al. Adult respiratory-distress syndrome—changing concepts of lung injury and repair. N Engl J Med 1982. (599) |
| 10. (#68) Weiland, JE et al. Lung neutrophils in the adult respiratory-distress syndrome—clinical and pathophysiologic significance. Amer Rev Resp Dis 1986. (551) |
| 11. (#77) Fowler, AA et al. Adult respiratory-distress syndrome—risk with common predispositions. Ann Intern Med 1983. (540) |
| 12. (#88) Hammerschmidt, DE et al. Association of complement activation and elevated plasma-C5a with adult respiratory-distress syndrome—pathophysiological relevance and possible prognostic value. Lancet 1980. (515) |
| 13. (#99) Lee, CT et al. Elastolytic activity in pulmonary lavage fluid from patients with adult respiratory-distress syndrome. N Engl J Med 1981. (497) |
| 14. (#100) Bell, RC et al. Multiple organ system failure and infection in adult respiratory-distress syndrome. Ann Intern Med 1983. (495) |
| 15. (#107) Poutanen, SM et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med 2003. (468) |
| 16. (#116) Pepe, PE et al. Clinical predictors of the adult respiratory-distress syndrome. Am J Surg 1982. (432) |
| 17. (#128) Donnelly, SC et al. Interleukin-8 and development of adult respiratory-distress syndrome in at-risk patient groups. Lancet 1993. (413) |
| 18. (#137) Clements, JA et al. Assessment of risk of respiratory-distress syndrome by a rapid test for surfactant in amniotic-fluid. N Engl J Med 1972. (403) |
| 19. (#140) Suter, PM et al. High bronchoalveolar levels of tumor-necrosis-factor and its inhibitors, interleukin-1, interferon, and elastase, in patients with adult respiratory-distress syndrome after trauma, shock, or sepsis. Amer Rev Resp Dis 1992. (402) |
| 20. (#144) Petty, TL et al. Adult respiratory distress syndrome—clinical features, factors influencing prognosis and principles of management. Chest 1971. (393) |
| 21. (#146) Gregory, TJ et al. Surfactant chemical-composition and biophysical activity in acute respiratory-distress syndrome. J Clin Invest 1991. (392) |
| 22. (#165) Milberg, JA et al. Improved survival of patients with acute respiratory-distress-syndrome (ARDS)—1983-1993. JAMA 1995. (370) |
| 23. (#170) Bernard, GR et al. High-dose corticosteroids in patients with the adult respiratory-distress syndrome. N Engl J Med 1987. (365) |
| 24. (#186) Lewis, JF et al. Surfactant and the adult respiratory-distress syndrome. Amer Rev Resp Dis 1993. (342) |
| 25. (#191) Danek, SJ et al. The dependence of oxygen-uptake on oxygen delivery in the adult respiratory-distress syndrome. Amer Rev Resp Dis 1980. (337) |
| 26. Weaver, TE et al. Function and regulation of expression of pulmonary surfactant-associated proteins. Arch Surg 1991. (336) |
| E. Infection disease articles (nonsepsis) (no. of times cited) |
|---|
| 1. (#5) Garner, JS et al. CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988. (2356) |
| 2. (#23) Vincent, JL et al. The prevalence of nosocomial infection in intensive-care units in Europe—results of the European prevalence of infection in intensive-care (EPIC) study. JAMA 1995. (993) |
| 3. (#35) Neiderman, MS et al. Guidelines for the management of adults with community-acquired pneumonia—diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Resp Crit Care 2001. (772) |
| 4. (#50) Niedermann, MS et al. Guidelines for the initial management of adults with community-acquired pneumonia—diagnosis, assessment of severity, and initial antimicrobial therapy. Amer Rev Resp Dis 1993. (655) |
| 5. (#61) Fagon, JY et al. Nosocomial pneumonia in ventilated patients—a cohort study evaluating attributable mortality and hospital stay. Am J Med 1993. (580) |
| 6. (#73) Edmond MB et al. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis 1999. (542) |
| 7. (#79) Pittet, D et al. Nosocomial blood-stream infection in critically ill patients—excess length of stay, extra costs, and attributable mortality. JAMA 1994. (535) |
| 8. (#82) McFarland, LV et al. Nosocomial acquisition of Clostridium difficile infection. N Engl J Med 1989. (524) |
| 9. (#90) Driks, MR et al. Nosocomial pneumonia in intubated patients given sucralfate as compared with antacids or histamine type-2 blockers—the role of gastric colonization. N Engl J Med 1987. (511) |
| 10. (#92) Craven, DE et al. Risk-factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Amer Rev Resp Dis 1986. (510) |
| 11. (#102) Fagon, JY et al. Nosocomial pneumonia in patients receiving continuous mechanical ventilation—prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Amer Rev Resp Dis 1989. (489) |
| 12. (#104) Torres, A et al. Incidence, risk, and prognosis factors of nosocomial pneumonia in mechanically ventilated patients. Amer Rev Resp Dis 1990. (483) |
| 13. (#110) Richards, MJ et al. Nosocomial infections in medical intensive care units in the United States. Crit Care Med 1999. (446) |
| 14. (#117) Evans, RS et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med 1998. (430) |
| 15. (#124) BergogneBerezin, E et al. Acinetobacter spp. as nosocomial pathogens: microbiological, clinical, and epidemiological features. Clin Microbiol Rev 1996. (415) |
| 16. (#125) Kollef, MH et al. Inadequate antimicrobial treatment of infections—a risk factor for hospital mortality among critically ill patients. Chest 1999. (415) |
| 17. (#126) Bradford, PA et al. Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 2001. (413) |
| 18. (#130) Goldmann, DA et al. Strategies to prevent and control the emergence and spread of antimicrobial-resistant microorganisms in hospitals—a challenge to hospital leadership. JAMA 1996. (412) |
| 19. (#141) Celis, R et al. Nosocomial pneumonia—a multivariate-analysis of risk and prognosis. Chest 1988. (399) |
| 20. (#155) Mulligan, ME et al. Methicillin-resistant Staphylococcus aureus—a consensus review of the microbiology, pathogenesis, and epidemiology with implications for prevention and management. Am J Med 1993. (381) |
| 21. (#158) Curry, CR et al. Fungal septicemia in patients receiving parenteral hyperalimentation. N Engl J Med 1971. (376) |
| 22. (#164) Stoutenbeek, CP et al. The effect of selective decontamination of the digestive-tract on colonization and infection-rate in multiple trauma patients. Intens Care Med 1984. (370) |
| 23. (#175) Cosgrove, SE et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003. (359) |
| 24. (#177) Chastre, J et al. Ventilator-associated pneumonia. Am J Resp Crit Care 2002. (355) |
| 25. (#188) Ibrahim, EH et al. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 2000. (341) |
| 26. (#189) Becksague, C et al. Hospital outbreak of multidrug-resistant Mycobacterium tuberculosis infections—factors in transmission to staff and HIV-infected patients. JAMA 1992. (341) |
| 27. Gerberding, J et al. National nosocomial infections surveillance (NNIS) system report, data summary from January 1990-May 1999, issued June 1999. Am J Infect Control 1999. (327) |
| 28. Luna, CM et al. Impact of BAL data on the therapy and outcome of ventilator-associated pneumonia. Chest 1997. (327) |
| 29. Andrew, CP et al. Diagnosis of nosocomial bacterial pneumonia in acute, diffuse lung injury. Chest 1981. (326) |
| 30. Kollef, MH. Ventilator-associated pneumonia—a multivariate-analysis. JAMA 1993. (325) |
| 31. Cardo, D et al. National nosocomial infections surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004. (324) |
| 32. Maki, DG et al. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter—a randomized, controlled trial. Ann Intern Med 1997. (323) |
| 33. Livornese, LL et al. Hospital-acquired infection with vancomycin-resistant Enterococcus faecium transmitted by electronic thermometers. Ann Intern Med 1992. (319) |
| 34. Darouiche, RO et al. A comparison of two antimicrobial-impregnated central venous catheters. N Engl J Med 1999. (312) |
| 35. Maki, DG et al. Prospective randomized trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet 1991. (309) |
| 36. Mermel, LA. Prevention of intravascular catheter-related infections. Ann Intern Med 2000. (267) |
| 37. Raad, I et al. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections—a randomized, double-blind trial. Ann Intern Med 1997. (255) |
| 38. Pearson, ML. Guideline for prevention of intravascular-device–related infections. Infect Control Hosp Epidemiol 1996. (225) |
| 39. Cobb, DK et al. A controlled trial of scheduled replacement of central venous and pulmonary-artery catheters. N Engl J Med 1992. (179) |
| F. Hemodynamic monitoring/oxygen delivery articles (no. of times cited) |
|---|
| 1. (#15) Swan, HJC et al. Catheterization of heart in man with use of flow-directed balloon-tipped catheter. N Engl J Med 1970. (1297) |
| 2. (#20) Rivers, E et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001. (1058) |
| 3. (#29) Connors, AF et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 1996. (890) |
| 4. (#66) Wei, K et al. Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation 1998. (561) |
| 5. (#84) Hayes, MA et al. Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med 1994. (522) |
| 6. (#86) Gutierrez, G et al. Gastric intramucosal pH as a therapeutic index of tissue oxygenation in critically ill patients. Lancet 1992. (516) |
| 7. (#101) Gattinoni, L et al. A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med 1995. (489) |
| 8. (#159) Bihari, D et al. The effects of vasodilation with prostacyclin on oxygen delivery and uptake in critically ill patients. N Engl J Med 1987. (375) |
| 9. Maynard, N et al. Assessment of splanchnic oxygenation by gastric tonometry in patients with acute circulatory failure. JAMA 1993. (259) |
| 10. Sandham, JD et al. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients? N Engl J Med 2003. (247) |
| 11. Bernstein, DP. A new stroke volume equation for thoracic electrical bioimpedance—theory and rationale. Crit Care Med 1986. (223) |
| 12. Connors, AF et al. Evaluation of right-heart catheterization in the critically ill patient without acute myocardial-infarction. N Engl J Med 1983. (219) |
| 13. Mitchell, JP et al. Improved outcome based on fluid management in critically ill patients requiring pulmonary-artery catheterization. Amer Rev Resp Dis 1992. (217) |
| 14. Dalen, JE et al. Is it time to pull the pulmonary artery catheter? JAMA 1996. (208) |
| 15. Marik, PE. Gastric intramucosal pH—a better predictor of multiorgan dysfunction syndrome and death than oxygen-derived variables in patients with sepsis. Chest 1993. (202) |
| 16. Gore, JM et al. A community-wide assessment of the use of pulmonary-artery catheters in patients with acute myocardial-infarction. Chest 1987. (202) |
| 17. Iberti, TJ et al. A multicenter study of physicians knowledge of the pulmonary-artery catheter. JAMA 1990. (198) |
| 18. Tremper, KK et al. Trans-cutaneous oxygen monitoring of critically ill adults, with and without low flow shock. Crit Care Med 1981. (196) |
| 19. Garcia, MJ et al. An index of early left ventricular filling that combined with pulsed Doppler peak E velocity may estimate capillary wedge pressure. J Amer Coll Cardiol 1997. (195) |
| 20. Elliott, CG et al. Complications of pulmonary-artery catheterization in the care of critically ill patients—prospective-study. Chest 1979. (187) |
| 21. Yu, MH et al. Effect of maximizing oxygen delivery on morbidity and mortality-rates in critically ill patients—a prospective, randomized, controlled-study. Crit Care Med 1993. (182) |
| 22. Robin, ED. The cult of the Swan-Ganz catheter—overuse and abuse of pulmonary flow catheters. Ann Intern Med 1985. (181) |
| 23. McCormick, PW et al. Noninvasive cerebral optical spectroscopy for monitoring cerebral oxygen delivery and hemodynamics. Crit Care Med 1991. (174) |
| 24. Eisenberg, PR et al. Clinical-evaluation compared to pulmonary-artery catheterization in the hemodynamic assessment of critically ill patients. Crit Care Med 1984. (170) |
| 25. Shah, KB et al. A review of pulmonary-artery catheterization in 6,245 patients. Anesthesiology 1984. (169) |
| 26. Bernstein, DP. Continuous noninvasive real-time monitoring of stroke volume and cardiac-output by thoracic electrical bioimpedance. Crit Care Med 1986. (162) |
| 27. Michard, F et al. Relationship between changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Resp Crit Care 2000. (159) |
| G. Neurologic and sedation articles (no. of times cited) |
|---|
| 1. (#2) Teasdale, G et al. Assessment of coma and impaired consciousness—practical scale. Lancet 1974. (3749) |
| 2. (#3) Jennett, B et al. Assessment of outcome after severe brain-damage—practical scale. Lancet 1975. (2825) |
| 3. (#71) Chesnut, RM et al. The role of secondary brain injury in determining outcome from severe head-injury. J Trauma 1993. (546) |
| 4. (#95) Chan PH. Role of oxidants in ischemic brain damage. Stroke 1996. (500) |
| 5. (#127) Jennett, B. Persistent vegetative state after brain-damage—syndrome in search of a name. Lancet 1972. (413) |
| 6. (#148) Muizelaar, JP et al. Adverse-effects of prolonged hyperventilation in patients with severe head-injury—a randomized clinical-trial. J Neurosurg 1991. (390) |
| 7. (#152) Kress, JP et al. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000. (383) |
| 8. (#161) Cohen, WJ et al. Lithium-carbonate, haloperidol, and irreversible brain-damage. JAMA 1974. (373) |
| 9. (#167) Rosner, MJ et al. Cerebral perfusion-pressure—management protocol and clinical results. J Neurosurg 1995. (368) |
| 10. (#179) Hossmann, KA et al. Reversibility of ischemic brain-damage. Arch Neurol 1973. (350) |
| 11. Broderick, JP et al. Volume of intracerebral hemorrhage—a powerful and easy-to-use predictor of 30-day mortality. Stroke 1993. (294) |
| 12. Siesjo, BK. Mechanisms of ischemic brain-damage. Crit Care Med 1988. (291) |
| 13. Levy, DE et al. Predicting outcome from hypoxic-ischemic coma. JAMA 1985. (282) |
| 14. Smith, I et al. Propofol—an update on its clinical use. Anesthesiology 1994. (276) |
| 15. Segredo, V et al. Persistent paralysis in critically ill patients after long-term administration of vecuronium. N Engl J Med 1992. (270) |
| 16. Clifton, GL et al. A phase-II study of moderate hypothermia in severe brain injury. J Neurotraum 1993. (254) |
| 17. Jacobi, J et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002. (242) |
| 18. Lewen, A et al. Free radical pathways in CNS injury. J Neurotraum 2000. (238) |
| 19. Levy, DE et al. Prognosis in non-traumatic coma. Ann Intern Med 1981. (235) |
| 20. Ledingham, IM et al. Influence of sedation on mortality in critically ill multiple trauma patients. Lancet 1983. (227) |
| 21. Schwab, S et al. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke 1998. (226) |
| 22. Brott, T et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke 1997. (225) |
| 23. Teasdale, G et al. Assessment and prognosis of coma after head-injury. Acta Neurochir 1976. (223) |
| 24. Rosner, MJ et al. Cerebral perfusion-pressure management in head-injury. J Trauma 1991. (212) |
| H. ICU management/resource utilization articles (no. of times cited) |
|---|
| 1. (#148) Leape, LL et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA 1999. (331) |
| 2. Needleman, J et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 2002. (312) |
| 3. Danis, M et al. A prospective-study of advance directives for life-sustaining care. N Engl J Med 1991. (308) |
| 4. Smedira, NG et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med 1990. (292) |
| 5. Albert, RK et al. Hand-washing patterns in medical intensive-care units. N Engl J Med 1981. (281) |
| 6. Shortell, SM et al. The performance of intensive-care units—does good management make a difference. Med Care 1994. (256) |
| 7. Aiken, LH et al. Lower Medicare mortality among a set of hospitals known for good nursing-care. Med Care 1994. (244) |
| 8. Cullen, DJ et al. Survival, hospitalization charges and follow-up results in critically ill patients. N Engl J Med 1976. (234) |
| 9. Thibault, GE et al. Medical intensive-care—indications, interventions, and outcomes. N Engl J Med 1980. (229) |
| 10. Prendergast, TJ et al. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Resp Crit Care 1997. (220) |
| 11. Pronovost, PJ et al. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA 1999. (210) |
| 12. Angus, DC et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease—can we meet the requirements of an aging population? JAMA 2000. (209) |
| 13. Pronovost, PJ et al. Physician staffing patterns and clinical outcomes in critically ill patients—a systematic review. JAMA 2002. (204) |
| 14. Landrigan, CP et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med 2004. (200) |
| 15. McQuillan, P et al. Confidential inquiry into quality of care before admission to intensive care. Brit Med J 1998. (193) |
| 16. Cook, DJ et al. Determinants in Canadian health-care workers of the decision to withdraw life-support from the critically ill. JAMA 1995. (193) |
| 17. Donchin, Y et al. A look into the nature and causes of human errors in the intensive-care unit. Crit Care Med 1995. (165) |
| 18. Asch, DA et al. Decisions to limit or continue life-sustaining treatment by critical care physicians in the United States—conflicts between physicians practices and patients wishes. Am J Resp Crit Care 1995. (141) |
| 19. Reynolds, HN et al. Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive-care unit. JAMA 1988. (135) |
| 20. Carson, SS et al. Effects of organizational change in the medical intensive care unit of a teaching hospital—a comparison of “open” and “closed” formats. JAMA 1996. (134) |
| I. Acute kidney injury articles (no. of times cited) |
|---|
| 1. (#91) Thadhani, R et al. Medical progress—acute renal failure. N Engl J Med 1996. (510) |
| 2. (#146) Ronco, C et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 2000. (391) |
| 3. (#160) Brivet, FG et al. Acute renal failure in intensive care units—causes, outcome, and prognostic factors of hospital mortality: a prospective, multicenter study. Crit Care Med 1996. (374) |
| 4. (#171) Levy, EM et al. The effect of acute renal failure on mortality—a cohort analysis. JAMA 1996. (364) |
| 5. Bonventre, JV. Mechanisms of ischemic acute-renal-failure. Kidney Int 1993. (286) |
| 6. Anderson, RJ et al. Non-oliguric acute renal-failure. N Engl J Med 1977. (283) |
| 7. Hakim, RM et al. Effect of the dialysis membrane in the treatment of patients with acute-renal-failure. N Engl J Med 1994. (282) |
| 8. Mangano, CM et al. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. Ann Intern Med 1998. (259) |
| 9. Koffler, A et al. Acute renal-failure due to nontraumatic rhabdomyolysis. Ann Intern Med 1976. (251) |
| 10. Tomita, K et al. Plasma endothelin levels in patients with acute renal-failure. N Engl J Med 1989. (248) |
| 11. Byrd, L et al. Radio contrast-induced acute renal-failure—clinical and pathophysiologic review. Medicine 1979. (244) |
| 12. Miller, TR et al. Urinary diagnostic indexes in acute renal-failure. Ann Intern Med 1978. (243) |
| 13. Better, OS et al. Early management of shock and prophylaxis of acute-renal-failure in traumatic rhabdomyolysis. N Engl J Med 1990. (242) |
| 14. Liano, F et al. Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Kidney Int 1996. (239) |
| 15. Schiffl, H et al. Biocompatible membranes in acute-renal-failure—prospective case-controlled study. Lancet 1994. (234) |
| 16. Firth, JD et al. Endothelin—an important factor in acute renal-failure. Lancet 1988. (226) |
| 17. Stein, JH et al. Current concepts on pathophysiology of acute renal-failure. Am J Physiol 1978. (218) |
| 18. Zager, RA. Rhabdomyolysis and myohemoglobinuric acute renal failure. Kidney Int 1996. (205) |
| 19. Schiffl, H et al. Daily hemodialysis and the outcome of acute renal failure. N Engl J Med 2002. (195) |
| 20. Star, RA. Treatment of acute renal failure. Kidney Int 1998. (195) |
| 21. Thurau, K et al. Acute renal success—unexpected logic of oliguria in acute renal-failure. Am J Med 1976. (193) |
| 22. Bellomo, R et al. Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Lancet 2000. (192) |
| 23. Shusterman, N et al. Risk-factors and outcome of hospital-acquired acute-renal-failure—clinical epidemiologic-study. Am J Med 1987. (191) |
| 24. Lauer, A et al. Continuous arteriovenous hemofiltration in the critically ill patient—clinical use and operational characteristics. Ann Intern Med 1983. (191) |
| 25. Bellomo, R et al. Continuous venovenous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med 1993. (187) |
| J. Resuscitation and cardiac arrest articles (no. of times cited) |
|---|
| 1. (#24) Kouwenhoven, WB et al. Closed-chest cardiac massage. JAMA 1960. (987) |
| 2. (#39) Holzer, M et al. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002. (716) |
| 3. (#45) Bernard, SA et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002. (668) |
| 4. (#60) Ruskin, JN et al. Out-of-hospital cardiac-arrest—electrophysiologic observations and selection of long-term anti-arrhythmic therapy. N Engl J Med 1980. (586) |
| 5. (#67) Bedell, SE et al. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med 1983. (558) |
| 6. (#118) Zoll, PM et al. Resuscitation of the heart in ventricular standstill by external electric stimulation. N Engl J Med 1952. (427) |
| 7. (#133) Eisenberg, MS et al. Cardiac-arrest and resuscitation—a tale of 29 cities. Ann Emerg Med 1990. (407) |
| 8. (#136) Cummins, RO et al. Improving survival from sudden cardiac-arrest—the chain of survival concept—a statement for health-professionals from the Advanced Cardiac Life-Support Subcommittee and the Emergency Cardiac Care Committee, American-Heart-Association. Circulation 1991. (403) |
| 9. (#143) Wilber, DJ et al. Out-of-hospital cardiac-arrest—use of electrophysiologic testing in the prediction of long-term outcome. N Engl J Med 1988. (396) |
| 10. (#156) Melrose, DG et al. Elective cardiac arrest. Lancet 1955. (379) |
| 11. (#176) Clifton, GL et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med 2001. (356) |
| 12. (#193) Baum, RS et al. Survival after resuscitation from out-of-hospital ventricular-fibrillation. Circulation 1974. (336) |
| 13. (#195) Siscovick, DS et al. The incidence of primary cardiac-arrest during vigorous exercise. N Engl J Med 1984. (335) |
| 14. Kuck, KH et al. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest—the Cardiac Arrest Study Hamburg (CASH). Circulation 2000. (321) |
| 15. Valenzuela, TD et al. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med 2000. (317) |
| 16. Becker, LB et al. Outcome of CPR in a large metropolitan-area—where are the survivors. Ann Emerg Med 1991. (295) |
| 17. Cummins, RO et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac-arrest—the Utstein style—a statement for health-professionals from a task-force of the American-Heart-Association, the European-Resuscitation-Council, the Heart-and-Stroke-Foundation-of-Canada, and the Australian-Resuscitation-Council. Circulation 1991. (289) |
| 18. Weil, MH et al. Difference in acid-base state between venous and arterial blood during cardiopulmonary-resuscitation. N Engl J Med 1986. (281) |
| 19. Murphy, DJ et al. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Intern Med 1989. (267) |
| 20. Luu, M et al. Diverse mechanisms of unexpected cardiac-arrest in advanced heart-failure. Circulation 1989. (266) |
| 21. Rudikoff, MT et al. Mechanisms of blood-flow during cardiopulmonary resuscitation. Circulation 1980. (263) |
| 22. Murphy, DJ et al. The influence of the probability of survival on patients preferences regarding cardiopulmonary-resuscitation. N Engl J Med 1994. (258) |
| 23. Myerburg, RJ et al. Clinical, electrophysiologic and hemodynamic profile of patients resuscitated from prehospital cardiac-arrest. Am J Med 1980. (257) |
| 24. Taffet, GE et al. In-hospital cardiopulmonary resuscitation. JAMA 1988. (253) |
| 25. Blackhall, LJ. Must we always use CPR. N Engl J Med 1987. (247) |
| K. Resuscitation and fluid therapy articles (no. of times cited) |
| 1. (#74) Bickell, WH et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994. (541) |
| 2. (#119) Roberts, I. Human albumin administration in critically ill patients: systematic review of randomised controlled trials. Brit Med J 1998. (426) |
| 3. (#123) Ring, J et al. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet 1977. (422) |
| 4. Finfer, S et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004. (279) |
| 5. Sort, P et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 1999. (279) |
| 6. Mattox, KL et al. Prehospital hypertonic saline dextran infusion for posttraumatic hypotension—the USA multicenter trial. Ann Surg 1991. (240) |
| 7. Shierhout, G et al. Fluid resuscitation with colloid or crystalloid solutions in critically ill patients: a systematic review of randomised trials. Brit Med J 1998. (235) |
| 8. Virgilio, RW et al. Crystalloid vs colloid resuscitation—is one better—randomized clinical-study. Surgery 1979. (235) |
| 9. Finfer, S et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004. (223) |
| 10. Kramer, GC et al. Small-volume resuscitation with hypertonic saline dextran solution. Surgery 1986. (222) |
| 11. Nakayama, S et al. Small-volume resuscitation with hypertonic saline (2,400 mosm/liter) during hemorrhagic-shock. Circ Shock 1984. (203) |
| 12. Holcroft, JW et al. 3-percent NaCl and 7.5-percent NaCl/dextran 70 in the resuscitation of severely injured patients. Ann Surg 1987. (201) |
| 13. Choi, PTL et al. Crystalloids vs. colloids in fluid resuscitation: a systematic review. Crit Care Med 1999. (182) |
| 14. Vassar, MJ et al. A multicenter trial for resuscitation of injured patients with 7.5-percent sodium-chloride—the effect of added dextran-70. Arch Surg 1993. (151) |
| 15. Hauser, CJ et al. Oxygen-transport responses to colloids and crystalloids in critically ill surgical patients. Surg Gynecol Obstet 1980. (145) |
| 16. Wiedemann, HP et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 1998. (139) |
| 17. Wikes, MM et al. Patient survival after human albumin administration—a meta-analysis of randomized, controlled trials. Ann Intern Med 2001. (138) |
| 18. Baxter, CR et al. Physiological response to crystalloid resuscitation of severe burns. Ann NY Acad Sci 1968. (138) |
| 19. Vassar, MJ et al. 7.5-percent sodium-chloride dextran for resuscitation of trauma patients undergoing helicopter transport. Arch Surg 1991. (136) |
| 20. Mazzoni, MC et al. Dynamic fluid redistribution in hyperosmotic resuscitation of hypovolemic hemorrhage. Am J Physiol 1988. (129) |
| 21. Shortgen, F et al. Effects of hydroxyethylstarch and gelatin on renal function in severe sepsis: a multicentre randomised study. Lancet 2001. (120) |
| 22. Velanovich, V et al. Crystalloid versus colloid fluid resuscitation—a meta-analysis of mortality. Surgery 1989. (119) |
| 23. Gross, D et al. Is hypertonic saline resuscitation safe in uncontrolled hemorrhagic-shock. J Trauma 1988. (119) |
| 24. Treib, J et al. An international view of hydroxyethyl starches. Intens Care Med 1999. (116) |
| 25. Wade, CE et al. Efficacy of hypertonic 7.5% saline and 6% dextran-70 in treating trauma: a meta-analysis of controlled clinical studies. Surgery 1997. (110) |
| 26. Simma, B et al. A prospective, randomized, and controlled study of fluid management in children with severe head injury: lactated ringer's solution versus hypertonic saline. Crit Care Med 1998. (107) |
| L. Transfusion medicine/hematology/bleeding articles (no. of times cited) |
|---|
| 1. (#30) Hebert, PC et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999. (867) |
| 2. (#54) Besarab, A et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 1998. (637) |
| 3. (#163) Samama, MM et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. N Engl J Med 1999. (372) |
| 4. (#166) Hastings, SPR et al. Antacid titration in prevention of acute gastrointestinal bleeding-controlled randomized trial in 100 critically ill patients. N Engl J Med, 1978. (369) |
| 5. (#172) Priebe, JH et al. Antacid versus cimetidine in preventing acute gastrointestinal-bleeding-randomized trial in 75 critically ill patients. N Engl J Med 1980. (364) |
| 6. Marik, PE et al. Effect of stored-blood transfusion on oxygen delivery in patients with sepsis. JAMA 1993. (302) |
| 7. Vincent, JL et al. Anemia and blood transfusion in critically ill patients. JAMA 2002. (245) |
| 8. Wu, WC, et al. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med 2001. (235) |
| 9. van de Watering, LMG. Beneficial effects of leukocyte depletion of transfused blood on postoperative complications in patients undergoing cardiac surgery—a randomized clinical trial. Circulation 1998. (234) |
| 10. Rohrer, MJ et al. Effect of hypothermia on the coagulation cascade. Crit Care Med 1992. (213) |
| 11. Horwich, TB et al. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Amer Coll Cardiol 2002. (206) |
| 12. Hebert, PC et al. Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases? Crit Care Med 2001. (161) |
| 13. Moore, FA et al. Blood transfusion—an independent risk factor for postinjury multiple organ failure. Arch Surg 1997. (158) |
| 14. Corwin, HL et al. The CRIT study: anemia and blood transfusion in the critically ill—current clinical practice in the United States. Crit Care Med 2004. (150) |
| 15. Corwin, HL et al. Efficacy of recombinant human erythropoietin in critically ill patients—a randomized controlled trial. JAMA 2002. (147) |
| 16. Ferrara, A et al. Hypothermia and acidosis worsen coagulopathy in the patient requiring massive transfusion. Am J Surg 1990. (144) |
| 17. Rao, SV et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004. (139) |
| 18. Corwin, HL et al. Efficacy of recombinant human erythropoietin in the critically ill patient: a randomized, double-blind, placebo-controlled trial. Crit Care Med 1999. (137) |
| 19. Boffard, KD et al. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma 1984. (129) |
| 20. Hebert, PC et al. Does transfusion practice affect mortality in critically ill patients? Am J Resp Crit Care 1997. (125) |
| 21. Cosgriff, N et al. Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. J Trauma 1997. (118) |
| 22. Corwin, HL et al. RBC transfusion in the ICU—is there a reason. Chest 1995. (118) |
| 23. Fitzgerald, RD et al. Transfusing red blood cells stored in citrate phosphate dextrose adenine-1 for 28 days fails to improve tissue oxygenation in rats. Crit Care Med 1997. (100) |
Article's rankings listed by subgroup then by its position within the overall top 200 citations.
3. Results
The final database included 1187 articles (Fig. 1). The articles collated in this study came from almost 100 different journals with publication years ranging from 1905 (#149) to 2006 (average publication year = 1991). Surprisingly, of the top 1000 most cited critical care articles, 662 were not found using any of the basic critical care search terms—critical care, intensive care, ICU, or critically ill/critical illness. These articles were discovered only after searching within a specific critical care journal (n = 227) or by specific critical care topics (Table 1) (n = 373). In fact, only 4 of the top 1000 articles could be found using any 1 of the 4 basic critical care terms listed above. Of these search terms, the most productive was “intensive care” (25 of top 100 articles), then “critically ill” or “critical illness” (19/100), “ICU” (11/100), and finally “critical care” (5/100). Sepsis/systemic inflammatory response syndrome was the most common topic (193 articles), followed by acute lung injury and mechanical ventilation (177 articles). Overall, 41% of the most cited articles came from critical care journals as designated by the JCR. The most articles were from Critical Care Medicine (23%) followed by American Journal of Respiratory and Critical Care (7%), Journal of Trauma (5%), Intensive Care Medicine (4%), and Shock (1%). Among the non–critical care journals, the New England Journal of Medicine (11%) followed by JAMA (9%) provided the most articles.
4. Discussion
One method to quickly retrieve scholarly articles related to critical care medicine is by using readily available, Internet-based, bibliographic database search tools supported by most medical libraries. We have found, however, that commonly used basic search terms retrieve under only 50% of the most cited and therefore arguably most influential articles in critical care. Therefore, although searches may have become much faster and easier, they may not be sufficient to retrieve a comprehensive list of articles.
We found that there is no single term that exhaustively retrieves all critical care medicine articles. The best generic search term, “intensive care,” only retrieved 25% of what one would consider the 100 of the most influential articles in critical care. Furthermore, the search term “critical care” was linked to only 5 of the top 100 articles, although it is a common keyword used by many search engines. Not to mention the fact that it is in the title of 8 of the 18 “critical care” journals.
One goal of this study was to determine the most efficient search terms for future literature searches. The capriciousness of how efficient a search term is perhaps no better illustrated than with our experience retrieving articles on ICU mortality prediction models. That not one of the basic critical care search terms in the Science Citation Index was tagged to these most influential articles highlights some of the difficulties in finding the most cited studies in critical care. It is clear that even for other types of articles, the best yield of only 25% indicates the need for a comprehensive search strategy such as the one used in this study.
Although this is a problem for those looking for research articles, it can also be an issue for the way published research becomes cited by others. For example, articles without abstracts or very brief abstracts were often found only after using exact topic words found in the article's title or by starting a search from within a specific critical care journal itself. Our experience has been previously demonstrated where the choice of keywords and abstract construction significantly impacts the likelihood that an article will be found using modern electronic searches [17].
This study does highlight the importance of sepsis and infectious disease as well as respiratory physiology in critical care with more than half the articles falling into 1 of these 2 broad categories. On the other hand, the most cited article was related to physiologic predictors of morbidity and mortality and the next 3 articles were related to mental status.
4.1. Limitations
This study, like previous ones focusing on citations, has several limitations. Perhaps the most relevant is the debate as to what constitutes the most influential articles within a professional discipline [1], [4], [18]. Citation data found in all bibliographic databases rely not only on correctly acquiring cited references but also on the assumption that a primary study cites other references that are most relevant to the published article. It is likely that this study captured many of the classic articles in critical care as each article in our list of the top 200 articles was cited at least 300 times. Considering that 46% of articles published in medicine are never even cited, this is a remarkable observation [19]. Certainly, these articles deserve attention and must have made an indelible impact. However, this is not always the case. Authors may preferentially cite their or their colleagues' previous works both because of familiarity or to increase the citation of that article. Recent scholarship on social networks, especially in the age of accelerated knowledge transmission, suggests that there may be an enhanced level of “connectedness” related to these networks [20], [21]. It is not known whether, or how, this connectedness may be influencing the dissemination and therefore the pattern of references within the critical care community or among specific critical care topics. However, it is possible that the pattern of some citations may reflect the influence of an individual, as some have referred to as the “ceremonial citation,” rather than the specific findings within an article [16], [22], [23]. In addition, authors are more likely to cite articles of their own language [8], [24] or articles that come from a highly cited journal. Not surprisingly, Baltussen found that among the most cited 45 articles, most of them came from non–critical care-focused journals [16]. Nevertheless, using citations as a proxy for influence and importance has both face validity and is supported by empiric data demonstrating that citation analyses correlate with articles with the highest quality hierarchies of evidence and research design [25].
Most importantly, the use of citations is also confounded by the effect of time from the year of publication [26] with peak of citations differing for different journals and areas of research. Once citations do peak, they eventually become part of common knowledge and are no longer cited. Previous studies suggest that articles peak 7 to 10 years after publication [15], [26]. It has been suggested that “classic” articles are relevant to only a few decades and many important articles are lost to the passage of time [15]. These findings may be supported by the fact that among the top 200 articles in this study, 158 were published during or after 2000. It is probably too early to tell how electronic databases will change the epidemiology of citation classics because it is easier to retrieve and perhaps cite influential articles than before the age of the Internet.
In conclusion, although Web-based search engines can produce lists of references within seconds to minutes, the utility of these searches can be quite limited as a complete end effective literature search remains an art. Periodic reviews of the literature may prove helpful to trainees mastering the most influential literature of our field as well as more established professionals searching for starting points for new investigations.
Footnotes
This study was funded entirely by the Department of Anesthesiology, University of Michigan, Ann Arbor, Mich.
References
- 1.Moed H.F. The impact-factors debate: the ISI's uses and limits. Nature. 2002;415:731–732. doi: 10.1038/415731a. [DOI] [PubMed] [Google Scholar]
- 2.Seglen P.O. Citation rates and journal impact factors are not suitable for evaluation of research. Acta Orthop Scand. 1998;69:224–229. doi: 10.3109/17453679809000920. [DOI] [PubMed] [Google Scholar]
- 3.Moed H.F., van Leeuwen T.N. Impact factors can mislead. Nature. 1996;381:186. doi: 10.1038/381186a0. [DOI] [PubMed] [Google Scholar]
- 4.Tobin M.J. The role of a journal in a scientific controversy. Am J Respir Crit Care Med. 2003;168:511. doi: 10.1164/rccm.2307001. [DOI] [PubMed] [Google Scholar]
- 5.Gisvold S.E. Citation analysis and journal impact factors—is the tail wagging the dog? Acta Anaesthesiol Scand. 1999;43:971–973. doi: 10.1034/j.1399-6576.1999.431001.x. [DOI] [PubMed] [Google Scholar]
- 6.Garfield E. 100 citation classics from the Journal of the American Medical Association. JAMA. 1987;257:52–59. [PubMed] [Google Scholar]
- 7.Loonen M.P., Hage J.J., Kon M. Plastic surgery classics: characteristics of 50 top-cited articles in four plastic surgery journals since 1946. Plast Reconstr Surg. 2008;121s:320e–327e. doi: 10.1097/PRS.0b013e31816b13a9. [DOI] [PubMed] [Google Scholar]
- 8.Paladugu R., Schein M., Gardezi S., Wise L. One hundred citation classics in general surgical journals. World J Surg. 2002;26:1099–1105. doi: 10.1007/s00268-002-6376-7. [DOI] [PubMed] [Google Scholar]
- 9.Fenton J.E., Roy D., Hughes J.P., Jones A.S. A century of citation classics in otolaryngology-head and neck surgery journals. J Laryngol Otol. 2002;116:494–498. doi: 10.1258/002221502760132557. [DOI] [PubMed] [Google Scholar]
- 10.Picknett T., Davis K. The 100 most-cited articles from JMB. J Mol Biol. 1999;293:171–176. doi: 10.1006/jmbi.1999.3148. [DOI] [PubMed] [Google Scholar]
- 11.Hall G.M. BJA citation classics 1945-1992. Br J Anaesth. 1998;80:4–6. doi: 10.1093/bja/80.1.4. [DOI] [PubMed] [Google Scholar]
- 12.Strassels S.A., Carr D.B., Meldrum M., Cousins M.J. Toward a canon of the pain and analgesia literature: a citation analysis. Anesth Analg. 1999;89:1528–1533. doi: 10.1097/00000539-199912000-00040. [DOI] [PubMed] [Google Scholar]
- 13.Terajima K., Aneman A. Citation classics in anaesthesia and pain journals: a literature review in the era of the internet. Acta Anaesthesiol Scand. 2003;47:655–663. doi: 10.1034/j.1399-6576.2003.00137.x. [DOI] [PubMed] [Google Scholar]
- 14.Baltussen A., Kindler C.H. Citation classics in anesthetic journals. Anesth Analg. 2004;98:443–451. doi: 10.1213/01.ANE.0000096185.13474.0A. [table of contents] [DOI] [PubMed] [Google Scholar]
- 15.Aylward B.S., Roberts M.C., Colombo J., Steele R.G. Identifying the classics: an examination of articles published in the journal of pediatric psychology from 1976-2006. J Pediatr Psychol. 2008;33:576–589. doi: 10.1093/jpepsy/jsm122. [DOI] [PubMed] [Google Scholar]
- 16.Baltussen A., Kindler C.H. Citation classics in critical care medicine. Intensive Care Med. 2004;30:902–910. doi: 10.1007/s00134-004-2195-7. [DOI] [PubMed] [Google Scholar]
- 17.Sieck G.C. The “impact factor”: what it means to the impact of applied physiology. J Appl Physiol. 2000;89:865–866. doi: 10.1152/jappl.2000.89.3.865. [DOI] [PubMed] [Google Scholar]
- 18.Seglen P.O. Why the impact factor of journals should not be used for evaluating research. BMJ. 1997;314:498–502. doi: 10.1136/bmj.314.7079.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams A.B., Simonson D. Publication, citations, and impact factors of leading investigators in critical care medicine. Respir Care. 2004;49:276–281. [PubMed] [Google Scholar]
- 20.Wasserman S., Faust K. vol. ed. Cambridge University Press; Cambridge (Mass): 1994. Social network analysis: methods and applications. [Google Scholar]
- 21.Backstrom L., Huttenlocher D., Kleinberg J., Lan X. Proceedings of 12th International Conference on Knowledge Discovery in Data Mining; New York: ACM Press; 2006. [Google Scholar]
- 22.MacRoberts M.H., MacRoberts B.R. Citation analysis and the science policy arena. Trends Biochem Sci. 1989;14:8–12. [Google Scholar]
- 23.Cole S. Citations and the evaluation of individual scientists. Trends Biochem Sci. 1989;14:9–13. [Google Scholar]
- 24.Bhandari M., Busse J., Devereaux P.J., Montori V.M., Swiontkowski M., Tornetta P., III Factors associated with citation rates in the orthopedic literature. Can J Surg. 2007;50:119–123. [PMC free article] [PubMed] [Google Scholar]
- 25.Patsopoulos N.A., Analatos A.A., Ioannidis J.P. Relative citation impact of various study designs in the health sciences. JAMA. 2005;293:2362–2366. doi: 10.1001/jama.293.19.2362. [DOI] [PubMed] [Google Scholar]
- 26.Marx W., Schier H., Wanitschek M. Citation analysis using online databases: feasibilities and shortcomings. Scientometrics. 2001;52:59–82. [Google Scholar]