Abstract
Refugees share a common experience of displacement from their country of origin, migration, and resettlement in an unfamiliar country. More than 17 million people have fled their home countries due to war, generalized violence, and persecution. US primary care physicians must care for their immediate and long-term medical needs. Challenges include (1) language and cultural barriers, (2) high rates of mental health disorders, (3) higher prevalence of latent infections, and (4) different explanatory models for chronic diseases. This article discusses management strategies for common challenges that arise in the primary care of refugees.
Keywords: Refugee, Immigrant, Asylee, Primary care, Mental health, Chronic disease, Cross-cultural medicine, Language
Key points
-
•
Refugees make up a subset of immigrants who have been forcibly displaced from their homes by persecution, generalized violence, rape, and human rights abuses.
-
•
Use of a professional medical interpreter is essential for patients with limited English proficiency.
-
•
Primary care providers should be vigilant for latent infectious conditions such as tuberculosis and hepatitis B virus infection.
-
•
Mental health conditions such as depression, anxiety, and posttraumatic stress disorder are very common in traumatized populations. Screening for these is necessary.
-
•
Multiple barriers to managing chronic conditions in refugee patients exist, including transportation, language, challenges in navigating pharmacies, and insurance. Providers should recognize competing agendas or explanatory models related to their patients’ conditions.
Introduction
Fleeing from generalized violence, rape, and torture, more than 17 million people worldwide are unable to return to their home countries. Civil conflicts and systematic persecutions, some of which have persisted for years, have forced millions into a state of protracted exile in neighboring countries. Many live and wait in overcrowded refugee camps hoping for restoration of political stability, acceptance, and safety in their home countries. The goal of the United Nations High Commissioner for Refugees (UNHCR) is to work toward long-term solutions of either voluntary repatriation or local integration into their host country. However, in some cases, the UNHCR has no other option than to permanently resettle refugees to a third country such as the United States, Australia, or Canada.1
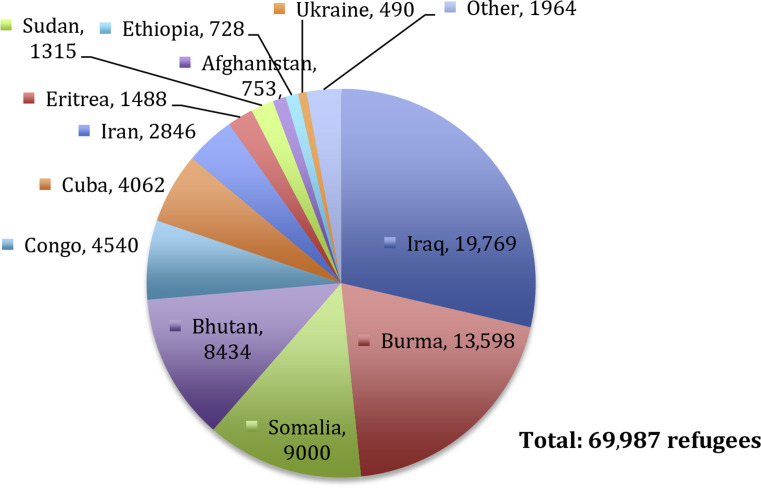
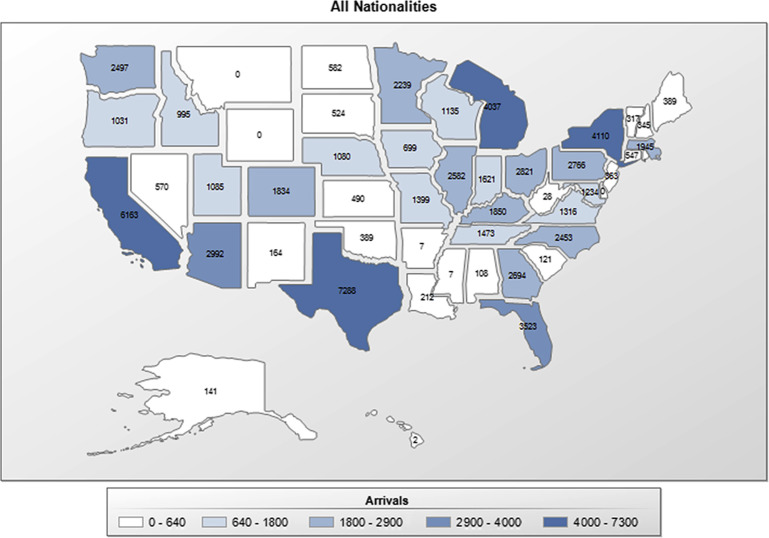
The United States uses a legal definition of a refugee that is similar to the 1951 United Nations’ Convention: a person outside of the United States who demonstrates a history of “persecution or fear of persecution due to race, religion, nationality, political opinion, or membership in a particular social group.2” In 2014, the United States admitted almost 70,000 refugees, with the largest numbers originating from Iraq, Burma (Myanmar), Somalia, and Bhutan (Fig. 1 ). As a subset of the total immigrant population, refugees have been resettled in all but 2 states, with a large proportion going to Texas, California, New York, and Michigan (Fig. 2 ).3 In addition to the refugees who are accepted for admission before their departure from overseas, asylum seekers make up an important group of potential immigrants who apply for asylum after arrival to the United States. To receive asylum, an immigration court must determine whether the asylum seeker meets the same legal definition as a refugee. In 2013, the US Citizenship and Immigration Services granted asylum to 25,199 individuals with the largest proportion being from the People’s Republic of China (34%).4
Fig. 1.
Countries of origin of refugees resettled to the United States during fiscal year 2014.
(Data from Refugee Processing Center. Reports. Available at: http://www.wrapsnet.org/Reports/AdmissionsArrivals/tabid/211/Default.aspx. Accessed October 29, 2014.)
Fig. 2.
Numbers of refugees accepted by state during the fiscal year 2014.
(From Refugee Processing Center. Reports. Available at: http://www.wrapsnet.org/Reports/AdmissionsArrivals/tabid/211/Default.aspx. Accessed October 29, 2014; with permission.)
The legal status of refugee or asylee is important because, in addition to receiving asylum, it confers several short-term government assistance programs, not available to other immigrants. Refugees receive 8 months of medical coverage, representing a window period to complete an initial health evaluation and obtain subspecialty consultation if necessary. They are also eligible to apply for health insurance through the Affordable Care Act; other immigrants must wait 5 years. The government has partnered with private voluntary agencies to assists refugees in their resettlement process with services such as orientation, food and clothing, initial housing, and sponsor programs. Voluntary agencies may also provide case management, English language classes, and vocational training. Also, in contrast to other immigrants, refugees and asylees are entitled to an accelerated path to citizenship. They can apply for a green card after the first year and for citizenship at 5 years.
Whereas much of the published literature on refugees and asylees has addressed the medical care during first year after resettlement, this article primarily focuses on the long-term management of adults in primary care. The first section briefly covers the overseas and domestic evaluation, which is an opportunity to detect and treat latent infectious conditions before they emerge later with dire consequences. Additionally, mental health issues are prevalent in refugee and asylee populations and need to be recognized and managed in a culturally appropriate manner. The final section focuses on chronic disease management in this vulnerable population.
The importance of using a trained interpreter
The impact of language barriers on health care is well documented in the literature. When compared with fluent English speakers, communication problems contribute to adverse events at a higher rate for patients with limited English proficiency.5 These patients have lower rates of preventive screening and services and higher rates of hospitalization and drug complications.6 Additionally, language barriers are associated with lower patient satisfaction and a lower rate of adherence to medication regimens.7, 8, 9 Given the high stakes of medical interpretation and its inherent difficulties of accurately conveying meaning across language and culture, using a trained interpreter is essential. One study compared trained interpreters to ad hoc interpreters (ie, family members, hospital staff, untrained volunteers, and friends) and found significant higher error rates among ad hoc interpreters.10 In particular, using family members is problematic when it comes to discussing sensitive topics. Moreover, Title VI of the Civil Rights Act of 1964 and the Department of Health and Human Services mandate the provision of competent interpreters in all health care settings.11 Having a face-to-face interpreter is ideal but medical telephonic services are widely available, cheaper, and easier to coordinate without scheduling ahead of time.
A brief description of the overseas evaluation
Before their departure, all immigrants bound for United States, both refugees and nonrefugee immigrants, are required to have a medical evaluation in accordance with guidelines from the Centers for Disease Control and Prevention (CDC). One of the primary purposes of the evaluation is to “prevent the importation of infectious diseases and other conditions of public health significance.2” Screening for infectious tuberculosis (TB) is the major focus and, if found, the immigrant must be adequately treated with directly observed therapy before a waiver to fly is granted. Other inadmissible conditions include gonorrhea, Hansen disease, syphilis, chancroid, granuloma inguinale, and lymphogranuloma venereum. More recently, severe acute respiratory syndrome, viral hemorrhagic fever, and avian influenza, and Ebola, among others, have been added to the list of quarantinable conditions. In reality, very few refugees have been denied entry due to a medical condition (0.4%) and, of those, almost all had untreated infectious TB (93%).12 Importantly, as of 2010, human immunodeficiency virus (HIV) testing is no longer performed as part of the overseas evaluation and the HIV status is often unknown at the time of arrival.13
In most cases, refugees are exposed to harsh living conditions with inadequate health care, sanitation, and access to safe water. Due to their increased risk, the CDC recommends presumptive treatment of parasitic infections for many groups. For example, sub-Saharan Africans living in endemic countries receive artemisinin-based combination therapy directed at Plasmodium falciparum malaria before departure.14 Many refugees also are administered presumptive antihelminthic agents directed at Strongyloides stercoralis and Schistosoma species, both of which can persist subclinically for years after immigration and lead to complications.15
Age-appropriate vaccinations, such as measles-mumps-rubella, tetanus, and pertussis, are required of refugees, the same as for persons born in the United States. There is an effort overseas to provide as many of the vaccines that are available, even though refugees are technically not required to have any before their departure.16 However, in order to apply for a green card at 1 year after arrival, refugees must complete all vaccination series (except human papillomavirus vaccine, zoster vaccine, and the new 13-valent pneumococcal conjugate vaccine). In the cases of hepatitis A and varicella, demonstrating serologic evidence of immunity before vaccination is cost-effective.16 Hepatitis B virus (HBV) testing should also be done before vaccinating to identify those with current infection.
The domestic evaluation of adults
All refugees are recommended to have a domestic medical evaluation. Ideally, this should occur soon after arrival and includes rescreening for TB, mental health screening, and testing for HBV, anemia, and sexually transmitted infections such as HIV, syphilis, chlamydia, and gonorrhea. It should also confirm, either through the overseas documentation or testing, that the appropriate presumptive anthelminthic therapies were administered. Finally, this evaluation is meant to identify chronic diseases such as diabetes and hypertension and update vaccinations. In many regions of the United States, the local health departments have assumed the responsibility for following-up newly arrived persons with TB within 30 days. However, for non-TB conditions, there is a wide range of models at the state and county levels, and many parts of the country rely on primary care physicians to perform the domestic evaluation. In reality, it is likely that a large proportion of refugees do not receive the recommended evaluation.17 Even for TB, the actual rates of follow-up after arrival ranged from zero (Montana) to 100% (Delaware) with a median rate of 75% in 2009.12
Unless there is clear documentation of prior screening and treatment, primary care providers may consider a conservative approach and not assume that any part of the domestic evaluation was previously performed. In the authors’ experience, relying on the patient’s memory of prior treatments can be fraught with recall errors and the authors tend to err on the side of retesting, even years after immigration. The following discussion is a brief overview of infections with a long latency period that may be less familiar to North American providers: TB, parasites, and HBV. More detailed instructions of diagnosis and treatment can found at the CDC website: http://www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/domestic-guidelines.html.
Tuberculosis
In 2013, there were almost 10,000 new cases of active TB in the United States with 64% occurring in foreign-born persons.18 It is recommended that all immigrants from regions where TB is endemic be screened. The evaluation starts with eliciting symptoms of active TB, such as a cough, fever, hemoptysis, weight loss, and night sweats, usually of several weeks or months duration. If negative, the clinician should proceed to screen for latent TB infection with a tuberculin skin test or interferon-gamma release assay followed by a 2-view chest radiograph. All patients diagnosed with TB must have their HIV status evaluated. The decision to offer treatment of latent TB infection is based on weighing the risks of reactivation with the risks of treatment. Estimates of these risks can be found using an online calculator, such as www.tstin3d.com from McGill University. Ample time for a clear discussion of the risks and benefits of treatment is important, as well as a 1-month follow-up appointment to check for medication side effects and to confirm an understanding of the pharmacy refill process.
Chronic Parasitic Worm Infections
Refugees may have been exposed to a multitude of helminthes, depending on the region and living conditions before emigration. However, when in North America without a means to complete its life cycle, most worms (eg, ascaris, Trichuris, hookworm) will gradually decrease in number and be excreted uneventfully from their adult host within a year or 2. There are, however, 2 important exceptions: S stercoralis and Schistosoma species.
Strongyloides is a soil-transmitted round worm that can complete its life-cycle entirely within a human host. This unique property of autoinfection allows Strongyloides to persist indefinitely in the human carrier even in the absence of recurrent exposure. The dreaded complication is hyperinfection, which is a process of massive dissemination of Strongyloides larvae and presents dramatically with gram-negative sepsis and carries a high mortality rate. Those who become immunosuppressed (eg, high-dose corticosteroid therapy) are at the greatest risk even many years after leaving the endemic area. Standard stool examination is insensitive for detection (<50% sensitivity).19 Therefore, all refugees and immigrants from endemic areas should either receive empiric treatment or be screened with serology.
Schistosomiasis is extremely prevalent with an estimated 200 million infected persons worldwide.20 Chronic disease is caused by the host’s immune response to migration and entrapment of eggs through tissues, thereby causing inflammation and fibrosis.21 Infection with S mansoni, S japonicum, and S mekongi typically results in egg deposition in microvasculature of the liver or intestines, causing hepatomegaly, portal hypertension, and polyposis of the small and large bowels. The classic manifestation of S haematobium is within the genitourinary tract and is a major risk factor for renal disease and bladder carcinoma. Diagnostic screening is indicated for individuals from endemic regions, even in the absence of symptoms. Screening tools include serology and stool studies. Hematuria found on urinalysis without other explanation may warrant an evaluation for S haemotobium.22
Hepatitis B Infection
Almost all chronic HBV infections are acquired at birth or early childhood. Chronic infection substantially increases the risk of cirrhosis, fulminant hepatitis, liver transplant, and liver cancer. Whereas the overall prevalence is relatively low in United States (0.4%), refugees have a significantly high rate of infection ranging from 5% to 14%.23, 24 The highest rates were observed in refugees from sub-Saharan Africa (10.5%) and East Asia (13%).25 The CDC recommends routine screening with serologic testing of immigrants from endemic areas.26 HBV surface antigen is the marker of on-going viral replication and warrants further evaluation to determine whether treatment is needed. Even for inactive carrier state, life-long serial monitoring for liver function and screening for hepatocellular carcinoma (HCC) are necessary. HBV infection is distinct from other hepatitides such as hepatitis C virus infection in that it can lead to the development of HCC in the absence of cirrhosis. Therefore, experts recommend that patients receive a screening liver ultrasound or non–maternal alpha fetoprotein test every 6 to 12 months.27 Box 1 shows the recommended age to begin HCC screening. It is also recommended that patients be counseled regarding transmission (eg, sexual contact and sharing razors and toothbrushes). Household contacts who are not already infected and nonimmune should be vaccinated.27
Box 1. Surveillance ultrasound every 6 to 12 months for HCC screening is recommended for the following groups of patients.
Asian men older than 40 years
Asian women older greater than 50 years
All cirrhotic HBV carriers
Family history of HCC
Africans older than 20 years
Any carrier older than 40 years with alanine aminotransferase elevation and/or HBV DNA greater than 2000 IU/mL
Data from Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology 2009;50:661–2.
Mental health
Being from all regions of the world, refugees, and asylees are diverse, representing a multitude of language groups, levels of education, socioeconomic backgrounds, and belief systems. However, they share a life-changing experience of having been violently displaced from their home and either personally experienced or witnessed significant trauma. During their migration, they often experience a transitional period in an intermediate country or refugee camp, where they are often exposed to more violence, deprivation, and uncertainty about the future. Though meant to be temporary, many live in refugee camps for years and even decades while awaiting permanent resettlement.
After their arrival to the United States, the postmigration stresses of rebuilding a new life without the benefit of social capital, credentials, or money are underestimated. For most who lack English proficiency on arrival, the difficulty of communicating and navigating through complex systems such as hospitals, banks, and schools is a constant reminder of their loss of power. Many accept minimal wage jobs and, from what little earnings they receive, are expected to send a proportion to family members abroad. The stress of day-to-day survival is compounded because many continue to bear the chronic pains of past physical and psychological injuries. They remember friends and family members who were killed, tortured, injured, or left behind. Often, not knowing the whereabouts of their love ones is most distressing and inhibits the healing process (Table 1 ).
Table 1.
The “triple trauma” of common stressors affecting refugees across the major periods of migration
| Premigration | Migration and Refugee Camp | Postmigration and Resettlement |
|---|---|---|
| Persecution Violence Torture Loss of possessions Loss of loved ones |
Violence Deprivation Uncertainty about future Separation from loved ones |
Discrimination Social isolation Financial problems Housing Employment Transportation Language barrier Generational acculturation Loss of social status |
Given the stresses before, during, and after migration, refugees have high rates of posttraumatic stress disorder (PTSD), depression, anxiety, and somatization.28 One systematic review and meta-analysis estimated a prevalence of PTSD of 30.6% and depression of 30.8% among 81,866 refugees and conflict-affected populations.29 However, rates vary widely based on the country of origin, with prevalence ranging from 3% to 86% for PTSD and 3% to 80% for major depression.30 Many also meet criteria for more than one mental health disorder: 86% of those with major depression met criteria for PTSD.31 Risk factors for PTSD and depression included cumulative exposure to potentially traumatic events, time since conflict, and a history of torture.29 In terms of disability and mortality, the exact toll is unknown but a recent report of newly resettled Bhutanese refugees between 2009 and 2012 estimated the annual suicide rate at 24.4 per 100,000 persons, almost twice that of the overall US population. In the same report, a survey of adult Bhutanese refugees found that 3% of participants had contemplated suicide at some point.32
Detection and Treatment
Various screening tools for mental health disorders exist but differ in terms of language availability, domain of interest (depression, anxiety, and PTSD), and feasibility. Commonly used tools that have been validated in multiple languages include the Harvard Trauma Questionnaire (HTQ) for PTSD and the Hopkins Symptom Checklist (HSCL-25) for depression.33, 34 Developed more recently, the Refugee Health Screener-15 (RHS-15) is a relatively short instrument used to detect depression, PTSD, and anxiety. Validated in new arrivals from Iraq, Bhutan, and Burma (Myanmar), the RHS-15 is open-access and can be found through the Pathways to Wellness program at www.lcsnw.org/pathways/.35
Barriers to discussing psychiatric disorders are several. On the part of the provider, there may be a discomfort with dealing with mental health issues, lack of time, and scarcity of mental health resources to refer patients. Patients’ views of mental illness vary widely based on previous experience and one’s medical and cultural beliefs. Although some may readily accept and openly talk about their depression, others may strongly resist any mention of a psychiatric diagnosis. Providers should be sensitive to the fact that mental health disorders are highly stigmatized in many countries (more so than our own) and the label of “being crazy” can lead to severe marginalization or detention.
Some patients may prefer to discuss symptoms such as fatigue, abdominal pain, headaches, and dizziness rather than diagnoses. In the authors’ experience, inquiring about sleep can be a nonthreatening way to broach the topic and may open the door to further questions about nightmares, worries, and sadness. Clinicians can also look for opportunities to acknowledge and validate patients’ on-going daily struggles, including concerns about unsafe neighborhoods, worries about their children, finances, and physical ailments, as a lead-in to discussing mental health. Communication can be tricky at times when an unintended linguistic nuance can lead to a misunderstanding, even with a professional interpreter. Providers should also accept that encounters with non-English speaking refugees require more time and it may take multiple visits to fully discuss a topic as complex as mental health. A patient-centered approach, as stated by Rhema and colleagues,36 can help to overcome barriers, “the refugee experience is one of disempowerment. Refugees are best served when provided with education about procedures and services that include opportunities of choice… explanations and instructions that allow refugees to have control over choices are more effective.” In the rush of seeing patients, it is easy to forget that supportive listening can be therapeutic and build trust.
Ideally, treatment should be multidisciplinary and involve the efforts of primary care providers, social workers, psychiatrists, psychologists, and community organizations. However, it may be the case that a patient will view their problem outside of the realm of what western medicine can offer and seek a solution through their church or mosque, friends and family, or traditional healers.37 Several studies have shown improvement with psychological interventions, including cognitive behavioral therapy and narrative exposure therapy (extinction conditioning) and, if available, these should be offered.38, 39 The prescribing of medicines, such as an antidepressant or α-adrenergic antagonist (eg, prazosin) for PTSD, may be met with resistance and often requires extensive education. Patients, familiar with immediate-acting medications such as antibiotics, may agree to start an antidepressant but discontinue it after a few days due to lack of effect. The authors have found that the willingness to take a medication increases with anticipatory guidance about potential side effects, onset of action, and treatment duration.
Survivors of Torture
Despite international declarations and conventions prohibiting its practice, torture is common worldwide. Broadly defined, torture is an act of inflicting psychological or physical pain on another person with the intention of coercing information or action, or as punishment, or purely for sadistic purposes. In many cases the objective behind torture is political and meant to terrorize a population and “stifle dissent, intimidate opposition, and strengthen the forces of tyranny.”40 For the individual, it serves to humiliate the person and destroy their faith in themselves. Examples include rape, beatings, amputations, suspension, confinement, asphyxiation, and mock executions. Witnessing and forcing one to perpetrate the torture of others are also common41 (Table 2 ).
Table 2.
Common methods of torture
| Physical Methods | Psychological Methods |
|---|---|
| Blunt trauma eg, beatings all over; falanga, beating the soles of the feet; telefono, striking the ears |
Humiliation eg, mocking, sexual humiliation, forced breaking of religious taboos |
| Penetrating trauma eg, cutting, amputations |
Threats |
| Crushing trauma | Mock executions |
| Positional torture eg, suspension, confinement in small spaces, fixation by ropes or chains |
Deprivation of: Light and sound Food and drink Access to toilet facilities Sleep Company Access to medicine and medical care |
| Shaking | Witnessing or perpetrating the torture of others |
| Asphyxiation | — |
| Chemical torture | — |
| Burns eg, electrical, acid, cigarettes |
— |
| Pharmacologic or microbiologic torture eg, forced ingestion of medications, inoculation of pathogens such as HIV |
— |
| Sexual torture | — |
Adapted from Wenzel T, Kastrup MC, Eisenman DP. Survivors of torture: a hidden population. In: Walker PF, Barnett ED, editors. Immigrant medicine. China: Saunders-Elsevier; 2007. p. 657; with permission.
As of 2000, it was estimated that approximately 400,000 torture survivors lived in the United States42 and the number is certainly much higher now. The Amnesty International Report of 2012 found torture and ill treatment in 112 countries, including most countries from which the United States receives refugees.43 Prevalence of torture varies widely by the population studied; however, a meta-analysis including 42,626 refugees and other conflict-affected groups showed an overall prevalence of 21%.29 A study of 1134 Somali and Oromo refugees living in the United States showed a prevalence of 44%.28 Another report found that 56% of Iraqi refugees had been tortured.44
The psychological and physical impact of torture can be long lasting. Mental health disorders occur frequently in survivors of torture, with rates as high as 81.1% with clinically significant anxiety, 84.5% with clinically significant depression, and 45.7% with symptoms of PTSD.45 Chronic pain is extremely common. One study reported that 78% reported persistent multiple pains, mainly in the head and low back.46 Falanga, or beating the soles of the feet, can result in subcutaneous fibrosis or compartment syndrome in the feet, as well as severe pain lasting for years. Sexual dysfunction and chronic pain are common sequelae of genital torture and female genital cutting. Head trauma can result in traumatic brain injury with effects on memory, attention, and behavior.47
Clinicians should have a high degree of suspicion for a history of torture in refugees, particularly those with symptoms of depression, anxiety, PTSD, or those with chronic physical complaints. The topic should be broached gently to prevent patients from feeling interrogated. Often, a history of torture is revealed over several visits, sometimes over the course of years, as a patient becomes comfortable with their physician. Awareness of a torture history can help prevent traumatization because tests such as phlebotomy, electrocardiograms, gynecologic examinations, and imaging studies may have the unintended effect of triggering negative memories from the past. Asking about a patient’s history of torture is also important so that providers can support their process of self-healing. Moreover, it serves as a reminder for us as health providers to remain patient and compassionate while providing necessary medical care.
Somatization and Chronic Pain
Somatization is described as “a tendency to experience and communicate somatic distress in response to psychosocial stress to seek medical help for it.”48 Somatic symptoms vary and take on different expressions based on cultural syndromes, such as those described in Asian populations. For example, the palpitations produced by anxiety can be thought of as a weak heart in China and the resulting fear of cardiac arrest or infarction can predispose the sufferer to be hypervigilant of any cardiac symptom. Among Cambodian patients, symptoms of anxiety and PTSD can present as a sore neck and fear of death due to rupture of the neck vessels can lead patients report any symptom involving the head and neck, including headache, dizziness, and tinnitus.49
Although chronic pain is often attributed to somatization, organic causes such as osteoarthritis, rheumatologic disorders, and osteomalacia must not be overlooked. When compared with other immigrants, refugees are more likely to have arthritis and activity-limitation due to pain.50 Treatment of chronic pain and somatization should include evaluation for coexisting mental health disorders and a history of trauma, including torture (Video 1; available online at http://www.medical.theclinics.com/). Current social stressors can be a contributor to somatization and should be addressed.51 Explaining the limitations of allopathic medicine can help in negotiating what constitutes an appropriate workup of pain complaints, such as in the patients who request multiple tests or procedures. Treatment modalities include acupuncture, trigger point injection, therapeutic massage, antidepressant medications, cognitive behavioral therapy, and relaxation techniques. Providers and patients are encouraged to openly discuss the use of traditional treatments.52, 53, 54
Chronic noncommunicable diseases
The healthy migrant bias argues that first-generation migrants are often healthier than those in the host population because they are self-selecting for the process of migration.55, 56 However, this advantage may be temporary because refugees are at high risk of developing chronic disease through the process of acculturation.57, 58 Therefore, whereas the burden of chronic noncommunicable disease may differ among refugees on arrival to the United States, age-appropriate guidelines for screening of chronic disease still applies.59
Many factors can affect a patient’s ability to manage their chronic medical conditions. Proactive management of chronic disease is similar to other preventive health services in that it requires an element of forward thinking and purpose in life.60 Often an improvement in finances or housing, or stabilization of a mental health condition, can provide the motivation to engage in the management of chronic disease. Rather than discuss the treatment guidelines for these chronic diseases, management principles in refugees are highlighted.
Hypertension
Hypertension is prevalent and sometimes challenging to manage in refugees. Of those adult refugees and asylees, who arrived in Massachusetts from 2001 to 2005, 22% had hypertension.61 This ranged from 9% (East and Southeast Asia) to 32% (Europe and Central Asia).61 Although some refugees from urban areas may be familiar with chronic disease, others may have limited experience with the idea of an asymptomatic disease, which has a waxing and waning course and is incurable.
Making patients aware of their diagnosis is often a prerequisite to medication adherence and behavioral modifications. One study found that foreign-born participants were less likely to be aware of their hypertension and overweight status than participants born in the United States.62 Having awareness of a diagnosis allows patients to make meaning of their new illness, thereby providing motivation for behavioral change.
A patient-centered approach to managing hypertension includes eliciting the patient’s explanatory model of disease.63 Understanding the patient’s beliefs around the causes, course of illness, and treatment of hypertension will guide their management. Although the literature is limited in refugees, a recent article provided examples of how explanatory models can lead to certain self-management behaviors, outlined in Table 3 .64
Table 3.
Explanatory models and corresponding hypertension self-management behaviors
| Explanatory Model | Hypertension Self-management Behavior |
|---|---|
| Cause | |
| Stress as primary cause | Stays calm, avoids stressful situations; takes antidepressant as treatment |
| Exercise causes increased BP | Avoids exercise to keep BP low |
| Pain causes increased BP | Managing pain, taking pain medications will control hypertension |
| Course of illness | |
| Hypertension comes and goes | Takes medications when BP goes up |
| BP cannot be controlled | Will not exercise and forgets medications |
| Little concern about hypertension; it does not affect my life | Avoids going to the doctor; forgets medications |
| Own definition of what is considered high | Only takes medication when BP is >190/100 mm Hg |
| Symptoms | |
| I can tell when my BP is high; I get headaches and dizziness | Takes medications only when symptoms occur |
| I have no symptoms of high BP, therefore it is not a problem | Does not take medications |
| Eating bacon does not make me feel bad, so it does not affect my BP | Eats bacon as desired |
| Treatment | |
| Only exercise can help me control my high BP | Exercises and, therefore, allows himself to smoke, drink, and not take medication |
| Garlic and vinegar can help me control my high BP | Focuses on these remedies while not taking medications or altering diet or sodium intake |
Abbreviation: BP, blood pressure.
Data from Bokhour BG, Cohn ES, Cortes DE, et al. The role of patients' explanatory models and daily-lived experience in hypertension self-management. J Gen Intern Med 2012;27:1626–34.
Finally, it is worthwhile to consider the patient’s motivation for disease management. The desire to control hypertension will likely be met with some obstacles, whether it is other health conditions, financial issues, or competing life stressors. This will be balanced by respect for the provider and the belief that controlled blood pressure will be of benefit. The role of hypertension in cardiovascular disease and the notion of risk-factor modification are often unfamiliar to refugees and deserve explicit explanation. Table 4 provides recommendations for common areas of miscommunication around medications.
Table 4.
Common areas of miscommunication around medications
| Interpreters | Always use an interpreter during every visit but particularly when making medication changes |
| Adherence | Ask patients to bring in all medications to each visit (including inhalers and glucometer) Use objective evidence to assess adherence (date of last refill, number of pills left) Remind patients that it is unsafe for you to increase medications if they are not taking them, so it is better if they are transparent |
| Timeline | Give patients a sense of the timeline for which to expect results so they do not discontinue a medication after a few doses |
| Refills | Often the pharmacy refill system is not well understood Remind patients that it is preferable to use one pharmacy and that they do not need to wait until an appointment to get medications refills |
| Side effects | Stating expected side effects can help warn the patient but if a patient associates a medication with a certain side effect it is unlikely that they will continue to take it (even if think it is unlikely to be the cause) |
| Daily vs as-needed | Be clear about which medications are daily despite symptoms and which are used for symptoms (inhalers, as-needed pain medications). |
| Tools | Identify barriers to compliance and use tools when appropriate Pill organizers are great to help organize but will not remind a patient to take medications |
| Sharing | Explicitly remind patients not to share their medications or to use medications prescribed for others |
| Teach back | Ask them to tell you how they take the medications |
| Team-based | Clinical pharmacists are a great resource for medication reconciliation and inhaler teaching |
| Traditional medicine | Ask about traditional or herbal medications |
Adapted from Avery K. Medication non-adherence issues with refugee and immigrant patients. EthnoMed. Available at: https://ethnomed.org/clinical/pharmacy/medication-non-adherence-issues-with-refugee-and-immigrant-patients. Accessed May 11, 2015.
Diabetes
Refugees from Bhutan, Iraq, and Burma make up greater than 60% of all incoming refugees to the United States.65 Estimates of diabetes in Bhutanese refugees ranges from 11% to 14% and data on Iraqi refugees revealed that 35% had at least 1 of 3 chronic medical conditions, including hypertension, diabetes, or obesity.66, 67, 68 One study looking at Hmong refugees put the blame for diabetes on the refugee movement itself, placing the individual with little control over their ill health.69 In addition to understanding explanatory models of disease, the management of diabetes often requires an understanding of traditional foods, history of food deprivation, and religious fasting.
Food and diet are inherently tied up in culture and religion. The discussion of nutrition and diet is much more relevant if it includes traditional foods. Culturally appropriate meal planning handouts are available in many languages (http://www.kingcounty.gov/healthservices/health/chronic/reach/diabetes.aspx). Furthermore, patients who have had a history of food deprivation or starvation should be approached with sensitivity. One study noted a relationship in Cambodian refugee women with a past experience of food deprivation and current overweight or obesity70 (Box 2 for patient case).
Box 2. Case example of negotiating the management of diabetes in a Cambodian woman.
Case example
A 67-year-old Cambodian woman with poorly controlled diabetes and obesity returned to clinic to review her laboratory results. The hemoglobin A1c was 14%. Her primary care provider was frustrated because during the past year, she tried multiple times to engage the patient to reduce her portion size and lose weight.
However, at an appointment with a nutritionist, the patient revealed that she lost several children to starvation during the Pol Pot era. She herself nearly starved and she recalled her desperate attempts to find food. Even now, feelings of hunger invariably bring back these painful memories.
After learning this, her primary care physician and nutritionist were able to adjust their counseling approach, putting more emphasis on exercise and eating nonstarchy vegetables rather than on limiting portion sizes. During the next 2 years, the patient eventually reduced her body mass index from 30 to 28 and decreased her hemoglobin A1c to 7.8%.
Many of the world’s religions practice fasting. Much of the research on fasting and diabetes management focuses on fasting during the holy month of Ramadan. The Epidemiology of Diabetes and Ramadan (EPIDIAR) study found that 79% of patients with type 2 diabetes reported fasting during Ramadan.71 Another study showed that patients in a Ramadan education program had a decrease in hypoglycemic events whereas a comparison group had a 4-fold increase in hypoglycemic events compared with their baseline.72 Interventions included in the study are summarized in Table 5 . The American Diabetes Association recommends individual management plans and close follow-up around Ramadan. Table 6 summarizes recommendations for adjusting medications for type 2 diabetes during Ramadan.73 Many patients forego clinic appointments during the month of Ramadan and, therefore, these conversations should ideally occur in advance.
Table 5.
Educational interventions for patients with diabetes during Ramadan
| Risk Assessment | Advise patients to seek medical advice from a physician before Ramadan to assess their risk of fasting and make recommendations. |
| Advise patient | Consider discussing the option of not fasting if appropriate but be prepared to hear “no.” |
| Exercise | Avoid rigorous exercise. |
| Diet | Encourage slow energy release foods (wheat, beans), not food high in fat. Iftar food is, by nature, fried. Limit dates, which are used to break fast. Limit sugar in tea. Avoid eating sweet dessert nightly; save it for Eid. |
| Hydration | Increase fluids, specifically water. Water is healthier than soda, juice, or sugary tea. Remember to drink water throughout the night. |
| Glucose monitoring | Advise patient that checking blood glucose does not constitute breaking fast. |
| When to break fast | Remind patients that they need to break fast if hypoglycemia does occur. |
Data from Bravis V, Hui E, Salih S, et al. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with Type 2 diabetes who fast during Ramadan. Diabet Med 2010;27:327–31.
Table 6.
Recommended changes to treatment regimen in patients with Type 2 diabetes who fast during Ramadan
| Before Ramadan | During Ramadan |
|---|---|
| Patients on diet and exercise control | Consider modifying the time and intensity of physical activity. |
| Patients on oral metformin | Consider adjusting timing of dose (ie, metformin 500 mg tid; during Ramadan change to metformin 1000 mg at sunset meal and 500 mg at predawn meal). |
| Patients on sulfonylureas | If once per day, adjust dose based on risk of hypoglycemia and give at sunset meal. If twice per day, use half the usual morning dose at the predawn meal and usual dose at the sunset meal. |
| Patients on premixed or intermediate acting insulin twice daily | Take usual dose at sunset meal and half usual dose at predawn meal. Also consider changing to long-acting in the evening and short-acting with meals. |
| Patients on long-acting insulin in the evening and short-acting with meals | Consider adjusting if at high risk of hypoglycemia or hyperglycemia, or continue with careful monitoring of blood glucose and adjust as necessary. |
Adapted from Al-Arouj M, Assaad-Khalil S, Buse J, et al. Recommendations for management of diabetes during Ramadan: update 2010. Diabetes Care 2010;33:1901.
Finally, there is an increase in awareness of the genetic variability in the pharmacokinetic and pharmacodynamics effects between different ethnic groups. When prescribing medications for a heterogeneous group of patients, a one-size-fits-all approach may not be the best approach. For example, studies have demonstrated that Asians (East Asian, Malay, and Indian) can achieve the same therapeutic effects using a lower dose of a statin (HMG-coenzyme A reductase inhibitor) compared with patients of European descent. As more knowledge is gained, providers may consider a lower starting dose in their Asian immigrant patients.74, 75
Summary
More than 3 million refugees have been admitted to the United States since the 1970s and almost all have become citizens, raised families, and work as productive members of society.76 On the surface, their story seems typical, resembling that of any other American immigrant. However, deeper down, refugee patients carry the scars of a violent past, which can continue to affect their health even years later. Although many are resilient and are able to heal themselves, others continue to struggle with depression, anxiety, and PTSD, which can flare up with emotional stress or physical pain. Primary care providers can forge a strong, therapeutic partnership with their refugee patients but it requires patience, compassion, and willingness to educate them about their health. By knowing aspects of their histories, clinicians can better support them through their healing process while managing chronic conditions, palliating pain, and offering preventive services.
Acknowledgments
The authors would like to thank Dr Carey Jackson for his help and support with this article, as well as Rozie Erlewine and Yetta Levine, who filmed and edited the video clip.
Footnotes
Disclosures: We have no commercial or financial conflicts of interest, or any funding sources.
Supplementary data related to this article can be found online at http://dx.doi.org/10.1016/j.mcna.2015.05.006.
Supplementary data
This 82-year-old man from an ethnic minority group in Vietnam received care by multiple physicians for many years for leg pain of unknown cause. Only later, when asked directly about the source of his pain, did he reveal a remote history of imprisonment and torture in Vietnam. In this video, he describes how his history of torture relates to his present symptoms.
References
- 1.United Nations High Commissioner for Refugee. UNHCR: Global Trends 2013: United Nations; 2014 June 20, 2014. Available online at: http://www.unhcr.org/5399a14f9.html. Accessed November 1, 2014.
- 2.United States Citizenship and Immigration Services (USCIS), Department of Homeland Security. Available online at: http://www.uscis.gov/humanitarian/refugees-asylum/refugees. Accessed June 12, 2015.
- 3.Summary of Refugee Admissions. 2014. Available at: http://www.wrapsnet.org. Accessed November 1, 2014.
- 4.Martin D.C., Yankay J.E. Homeland Security OIS; 2014. Annual flow report: Refugees and Asylees: 2013.http://www.dhs.gov/sites/default/files/publications/ois_rfa_fr_2013.pdf Available online at: [Google Scholar]
- 5.Divi C., Koss R.G., Schmaltz S.P. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19:60–67. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- 6.Jackson J.C., Nguyen D., Hu N. Alterations in medical interpretation during routine primary care. J Gen Intern Med. 2011;26:259–264. doi: 10.1007/s11606-010-1519-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carmona R.H. Improving language access: a personal and national agenda. J Gen Intern Med. 2007;22(Suppl 2):277–278. doi: 10.1007/s11606-007-0376-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.David R.A., Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. Mt Sinai J Med. 1998;65:393–397. [PubMed] [Google Scholar]
- 9.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 10.Flores G., Laws M.B., Mayo S.J. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 11.Department of Health and Human Services. Guidance to federal financial assistance recipients regarding title VI prohibition. Against national origin discrimination affecting limited English proficient persons: Policy guidance document. Available online at: http://www.hhs.gov/ocr/civilrights/resources/specialtopics/lep/hhslepguidancepdf.pdf. Accessed November 26, 2014.
- 12.Lee D., Philen R., Wang Z. Disease surveillance among newly arriving refugees and immigrants—Electronic Disease Notification System, United States, 2009. MMWR Surveill Summ. 2013;62:1–20. [PubMed] [Google Scholar]
- 13.Division of Global Migration and Quarantine, Technical Instructions for Panel Physicians. 2014. Available at: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/technical-instructions-panel-physicians.html. Accessed November 12, 2014.
- 14.Division of Global Migration and Quarantine, Center for Disease Control and Prevention. Guidelines for Pre-departure Presumptive Treatment and Directed Treatment for Malaria for all Refugees from Sub Saharan Africa. Available online at: http://www.cdc.gov/immigrantrefugeehealth/pdf/malaria-overseas.pdf. Accessed November 12, 2014.
- 15.Division of Global Migration and Quarantine, Centers for Disease Control and Prevention. Guidelines for overseas presumptive treatment of strongyloidiasis, schistosomiasis, and soil-transmitted helminth infections. 2012. Available online at: http://www.cdc.gov/immigrantrefugeehealth/guidelines/overseas/intestinal-parasites-overseas.html. Accessed November 12, 2014.
- 16.Division of Global Migration and Quarantine, Evaluating and Updating Immunizations during the Domestic Medical Examination for Newly Arrived Refugees. 2012. Available at: http://www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/immunizations-guidelines.html. Accessed November 12, 2014.
- 17.Waldorf B., Gill C., Crosby S.S. Assessing adherence to accepted national guidelines for immigrant and refugee screening and vaccines in an urban primary care practice: a retrospective chart review. J Immigr Minor Health. 2014;16:839–845. doi: 10.1007/s10903-013-9808-6. [DOI] [PubMed] [Google Scholar]
- 18.Alami N.N., Yuen C.M., Miramontes R. Trends in tuberculosis - United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:229–233. [PMC free article] [PubMed] [Google Scholar]
- 19.Boulware D.R., Stauffer W.M., 3rd, Walker P.F. Hypereosinophilic syndrome and mepolizumab. N Engl J Med. 2008;358:2839. [author reply: 2839–40] [PMC free article] [PubMed] [Google Scholar]
- 20.King C.H., Dickman K., Tisch D.J. Reassessment of the cost of chronic helmintic infection: a meta-analysis of disability-related outcomes in endemic schistosomiasis. Lancet. 2005;365:1561–1569. doi: 10.1016/S0140-6736(05)66457-4. [DOI] [PubMed] [Google Scholar]
- 21.Gryseels B., Polman K., Clerinx J. Human schistosomiasis. Lancet. 2006;368:1106–1118. doi: 10.1016/S0140-6736(06)69440-3. [DOI] [PubMed] [Google Scholar]
- 22.Strickland G.T., Ramirez B.L. Schistosomiasis. In: Strickland G.T., editor. Hunter's tropical medicine and emerging infectious diseases. 8th edition. W.B. Saunders Company; Philadelphia: 2000. pp. 802–832. [Google Scholar]
- 23.Pottie K., Janakiram P., Topp P. Prevalence of selected preventable and treatable diseases among government-assisted refugees: implications for primary care providers. Can Fam Physician. 2007;53:1928–1934. [PMC free article] [PubMed] [Google Scholar]
- 24.Lifson A.R., Thai D., O'Fallon A. Prevalence of tuberculosis, hepatitis B virus, and intestinal parasitic infections among refugees to Minnesota. Public Health Rep. 2002;117:69–77. doi: 10.1016/S0033-3549(04)50110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossi C., Shrier I., Marshall L. Seroprevalence of chronic hepatitis B virus infection and prior immunity in immigrants and refugees: a systematic review and meta-analysis. PLoS One. 2012;7:e44611. doi: 10.1371/journal.pone.0044611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weinbaum C.M., Williams I., Mast E.E. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57:1–20. [PubMed] [Google Scholar]
- 27.Lok A.S., McMahon B.J. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 28.Jaranson J.M., Butcher J., Halcon L. Somali and Oromo refugees: correlates of torture and trauma history. Am J Public Health. 2004;94:591–598. doi: 10.2105/ajph.94.4.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steel Z., Chey T., Silove D. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302:537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- 30.Fazel M., Wheeler J., Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365:1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 31.Marshall G.N., Schell T.L., Elliott M.N. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005;294:571–579. doi: 10.1001/jama.294.5.571. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Suicide and suicidal ideation among Bhutanese refugees–United States, 2009-2012. MMWR Morb Mortal Wkly Rep. 2013;62:533–536. [PMC free article] [PubMed] [Google Scholar]
- 33.Mollica R.F., Caspi-Yavin Y., Bollini P. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180:111–116. [PubMed] [Google Scholar]
- 34.Derogatis L.R., Lipman R.S., Rickels K. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 35.Hollifield M., Verbillis-Kolp S., Farmer B. The Refugee Health Screener-15 (RHS-15): development and validation of an instrument for anxiety, depression, and PTSD in refugees. Gen Hosp Psychiatry. 2013;35:202–209. doi: 10.1016/j.genhosppsych.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 36.Rhema S.H., Gray A., Verbillis-Kolp S. Mental health screening. In: Annamalai A., editor. Refugee health care. Springer; New York: 2014. p. 166. [Google Scholar]
- 37.Piwowarczyk L., Bishop H., Yusuf A. Congolese and Somali beliefs about mental health services. J Nerv Ment Dis. 2014;202:209–216. doi: 10.1097/NMD.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 38.McFarlane C.A., Kaplan I. Evidence-based psychological interventions for adult survivors of torture and trauma: a 30-year review. Transcult Psychiatry. 2012;49:539–567. doi: 10.1177/1363461512447608. [DOI] [PubMed] [Google Scholar]
- 39.Stenmark H., Catani C., Neuner F. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav Res Ther. 2013;51:641–647. doi: 10.1016/j.brat.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Gorman R. Refugee survivors of torture: trauma and treatment. Prof Psychol Res Pract. 2011;32:443–451. [Google Scholar]
- 41.Wenzel T., Kastrup M.C., Eisenman D.P. Survivors of torture: a hidden population. In: Walker P.F., Barnett E.D., editors. Immigrant medicine. Saunders-Elsevier; Beijing (china): 2007. p. 657. [Google Scholar]
- 42.Dross P. U.S. Department of Justice OfVoC; Washington, DC: 2000. Survivors of politically motivated torture: a large, growing, and invisible population of crime victims. [Google Scholar]
- 43.Amnesty International Annual Report 2011: The State of the World's Human Rights. 2011. Available at: http://files.amnesty.org/air11/air_2011_full_en.pdf. Accessed October 16, 2014.
- 44.Willard C.L., Rabin M., Lawless M. The prevalence of torture and associated symptoms in United States iraqi refugees. J Immigr Minor Health. 2014;16:1069–1076. doi: 10.1007/s10903-013-9817-5. [DOI] [PubMed] [Google Scholar]
- 45.Keller A., Lhewa D., Rosenfeld B. Traumatic experiences and psychological distress in an urban refugee population seeking treatment services. J Nerv Ment Dis. 2006;194:188–194. doi: 10.1097/01.nmd.0000202494.75723.83. [DOI] [PubMed] [Google Scholar]
- 46.Williams A.C., Pena C.R., Rice A.S. Persistent pain in survivors of torture: a cohort study. J Pain Symptom Manage. 2010;40:715–722. doi: 10.1016/j.jpainsymman.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 47.Healing the Hurt. Available at: http://www.cvt.org/resources/publications. Accessed November 8, 2014.
- 48.Lipowski Z.J. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145:1358–1368. doi: 10.1176/ajp.145.11.1358. [DOI] [PubMed] [Google Scholar]
- 49.Hinton D.E., Park L., Hsia C. Anxiety disorder presentations in Asian populations: a review. CNS Neurosci Ther. 2009;15:295–303. doi: 10.1111/j.1755-5949.2009.00095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yun K., Fuentes-Afflick E., Desai M.M. Prevalence of chronic disease and insurance coverage among refugees in the United States. J Immigr Minor Health. 2012;14:933–940. doi: 10.1007/s10903-012-9618-2. [DOI] [PubMed] [Google Scholar]
- 51.Schweitzer R.D., Brough M., Vromans L. Mental health of newly arrived Burmese refugees in Australia: contributions of pre-migration and post-migration experience. Aust N Z J Psychiatry. 2011;45:299–307. doi: 10.3109/00048674.2010.543412. [DOI] [PubMed] [Google Scholar]
- 52.Annamalai A. 2014 North American Refugee Health Conference; Rochester (NY): 2014. Somatization in refugees: an overview. [Google Scholar]
- 53.Kroenke K. Patients presenting with somatic complaints: epidemiology, psychiatric comorbidity and management. Int J Methods Psychiatr Res. 2003;12:34–43. doi: 10.1002/mpr.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Allen L.A., Woolfolk R.L., Escobar J.I. Cognitive-behavioral therapy for somatization disorder: a randomized controlled trial. Arch Intern Med. 2006;166:1512–1518. doi: 10.1001/archinte.166.14.1512. [DOI] [PubMed] [Google Scholar]
- 55.Thomas S.L., Thomas S.D. Displacement and health. Br Med Bull. 2004;69:115–127. doi: 10.1093/bmb/ldh009. [DOI] [PubMed] [Google Scholar]
- 56.Buja A., Gini R., Visca M. Prevalence of chronic diseases by immigrant status and disparities in chronic disease management in immigrants: a population-based cohort study, Valore Project. BMC Public Health. 2013;13:504. doi: 10.1186/1471-2458-13-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palinkas L.A., Pickwell S.M. Acculturation as a risk factor for chronic disease among Cambodian refugees in the United States. Soc Sci Med. 1995;40:1643–1653. doi: 10.1016/0277-9536(94)00344-s. [DOI] [PubMed] [Google Scholar]
- 58.Huh J., Prause J.A., Dooley C.D. The impact of nativity on chronic diseases, self-rated health and comorbidity status of Asian and Hispanic immigrants. J Immigr Minor Health. 2008;10:103–118. doi: 10.1007/s10903-007-9065-7. [DOI] [PubMed] [Google Scholar]
- 59.Amara A.H., Aljunid S.M. Noncommunicable diseases among urban refugees and asylum-seekers in developing countries: a neglected health care need. Global Health. 2014;10:24. doi: 10.1186/1744-8603-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim E.S., Strecher V.J., Ryff C.D. Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A. 2014;111:16331–16336. doi: 10.1073/pnas.1414826111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Geltman P.L., Dookeran N.M., Battaglia T. Chronic disease and its risk factors among refugees and asylees in Massachusetts, 2001-2005. Prev Chronic Dis. 2010;7:A51. [PMC free article] [PubMed] [Google Scholar]
- 62.Langellier B.A., Garza J.R., Glik D. Immigration disparities in cardiovascular disease risk factor awareness. J Immigr Minor Health. 2012;14:918–925. doi: 10.1007/s10903-011-9566-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kleinman A., Eisenberg L., Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 64.Bokhour B.G., Cohn E.S., Cortes D.E. The role of patients' explanatory models and daily-lived experience in hypertension self-management. J Gen Intern Med. 2012;27:1626–1634. doi: 10.1007/s11606-012-2141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Office of Admissions, Refugee Processing Center. Summary of Refugee Admissions. Series Editor: Department of State, Bureau of Population, Refugees, and Migration. Available at: http://www.wrapsnet.org/Reports/AdmissionsArrivals/tabid/211/Default.aspx. Accessed November 8, 2014.
- 66.Bhatta M.P., Shakya S., Assad L. Chronic disease burden among Bhutanese refugee women aged 18-65 years resettled in Northeast Ohio, United States, 2008-2011. J Immigr Minor Health. 2014 doi: 10.1007/s10903-014-0040-9. http://link.springer.com/article/10.1007/s10903-014-0040-9 Available online at: [DOI] [PubMed] [Google Scholar]
- 67.Kumar G.S., Varma S., Saenger M.S. Noninfectious disease among the Bhutanese refugee population at a United States urban clinic. J Immigr Minor Health. 2014;16:922–925. doi: 10.1007/s10903-013-9800-1. [DOI] [PubMed] [Google Scholar]
- 68.Yanni E.A., Naoum M., Odeh N. The health profile and chronic diseases comorbidities of US-bound Iraqi refugees screened by the International Organization for Migration in Jordan: 2007-2009. J Immigr Minor Health. 2013;15:1–9. doi: 10.1007/s10903-012-9578-6. [DOI] [PubMed] [Google Scholar]
- 69.Culhane-Pera K.A., Her C., Her B. “We are out of balance here”: a Hmong cultural model of diabetes. J Immigr Minor Health. 2007;9:179–190. doi: 10.1007/s10903-006-9029-3. [DOI] [PubMed] [Google Scholar]
- 70.Peterman J.N., Wilde P.E., Liang S. Relationship between past food deprivation and current dietary practices and weight status among Cambodian refugee women in Lowell, MA. Am J Public Health. 2010;100:1930–1937. doi: 10.2105/AJPH.2009.175869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Salti I., Benard E., Detournay B. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–2311. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 72.Bravis V., Hui E., Salih S. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with Type 2 diabetes who fast during Ramadan. Diabet Med. 2010;27:327–331. doi: 10.1111/j.1464-5491.2010.02948.x. [DOI] [PubMed] [Google Scholar]
- 73.Al-Arouj M., Assaad-Khalil S., Buse J. Recommendations for management of diabetes during Ramadan: update 2010. Diabetes Care. 2010;33:1895–1902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee E., Ryan S., Birmingham B. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin Pharmacol Ther. 2005;78:330–341. doi: 10.1016/j.clpt.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 75.Liao J.K. Safety and efficacy of statins in Asians. Am J Cardiol. 2007;99:410–414. doi: 10.1016/j.amjcard.2006.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Office of Refugee Resettlement, history. 2014. Available at: http://www.acf.hhs.gov/programs/orr/about/history. Accessed November 14, 2014.
Further readings
General Medical Care for the Refugee Patient
- Annamalai A., editor. Refugee health care: an essential medical guide. Springer; New York: 2014. [Google Scholar]
- Walker P., Barnett E., editors. Immigrant medicine. Saunders-Elsevier; 2007. [Google Scholar]
- HealthReach: Health Information in Many Languages. From the U.S. National Libray of Medicine. Available online at: https://healthreach.nlm.nih.gov.
Cross-Culture Medicine
- Ethnomed website. Available at: http://ethnomed.org.
Overseas and Domestic Evaluation for US Refugees
- CDC website. Available at: http://www.cdc.gov/immigrantrefugeehealth/.
Management of Latent Tuberculosis
- Curry Tuberculosis Center website. Available at: http://www.currytbcenter.ucsf.edu/.
- McGill University’s TST-in-3D website. Available at: http://www.tstin3d.com.
Female Genital Cutting
- Hearst A.A., Molnar A.M. Female genital cutting: an evidence-based approach to clinical management for the primary care physician. Mayo Clin Proc. 2013;88:618–629. doi: 10.1016/j.mayocp.2013.04.004. [DOI] [PubMed] [Google Scholar]
Survivors of Torture
- Healing invisible wounds: paths to hope and recovery in a violent world by Richard Mollica. Vanderbilt University Press; Nashville (TN): 2006. [Google Scholar]
- Refuge: Caring for survivors of torture. Available from Refuge Media Project. 47 Halifax Street Jamaica Plain, MA 02130. Email: refuge@refugemediaproject.org.
- The Center for Victims of Torture website. Available at: http://www.cvt.org.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This 82-year-old man from an ethnic minority group in Vietnam received care by multiple physicians for many years for leg pain of unknown cause. Only later, when asked directly about the source of his pain, did he reveal a remote history of imprisonment and torture in Vietnam. In this video, he describes how his history of torture relates to his present symptoms.