Abstract
Results of a clinical study using intravenous (IV) ribavirin for treating Department of Defense personnel with hemorrhagic fever with renal syndrome (HFRS) acquired in Korea from 1987 to 2005 were reviewed to determine the clinical course of HFRS treated with IV ribavirin. A total of 38 individuals enrolled in the study had subsequent serological confirmation of HFRS. Four of the 38 individuals received three or fewer doses of ribavirin and were excluded from treatment analysis. Of the remaining 34 individuals, oliguria was present in one individual at treatment initiation; none of the remaining 33 subjects developed oliguria or required dialysis. The mean peak serum creatinine was 3.46 mg/dl and occurred on day 2 of ribavirin therapy. Both the peak serum creatinine and the onset of polyuria occurred on mean day 6.8 of illness. Reversible hemolytic anemia was the main adverse event of ribavirin, with a ≥25% decrease in hematocrit observed in 26/34 (76.5%) individuals. While inability to adjust for all baseline variables prevents comparison to historical cohorts in Korea where oliguria has been reported in 39–69% cases and dialysis required in approximately 40% HFRS cases caused by Hantaan virus, the occurrence of 3% oliguria and 0% dialysis requirement in the treatment cohort is supportive of a previous placebo-controlled HFRS trial in China where IV ribavirin given early resulted in decreased occurrence of oliguria and decreased severity of renal insufficiency.
Keywords: Ribavirin, Hantavirus, Hantaan, Treatment, HFRS, Korea
1. Introduction
Hemorrhagic fever with renal syndrome (HFRS) is caused by hantaviruses of the family Bunyaviridae. HFRS in Korea, China, and areas of Asia east of the Ural Mountains is caused primarily by two hantaviruses, Hantaan virus and Seoul virus (Lee, 1999). Hantaan virus, carried by the striped field mouse (Apodemus agrarius), is seen primarily in rural areas and associated with a more severe form of disease, with a mortality rate ranging from 1.5% to 12% in Korea (Lee, 1991, Bruno et al., 1990, Kim et al., 2006). Seoul virus, carried by domestic rats (Rattus norvegicus and Rattus rattus), is responsible for urban cases of HFRS. Seoul virus is generally associated with a less severe form of disease, with a mortality rate of less than 1%.
HFRS disease is characterized by fever, headache, abdominal and/or back pain, renal insufficiency, and mild manifestations of hemorrhage. Disease may manifest as five clinical phases of illness: febrile, hypotensive, oliguric, polyuric, and convalescent phases (Lee, 1991, Bruno et al., 1990, Kim et al., 2006). Nearly all individuals present with a febrile illness, 11–40% persons develop hypotension and 40–60% develop oliguria (urine output less than 400 ml per day, generally lasting 3–7 days). Individuals are at greatest risk for hypertension, pulmonary edema, and complications of renal insufficiency during the oliguric phase, resulting in dialysis in approximately 40% of HFRS cases due to Hantaan and 20% cases due to Seoul virus. Causes of death are mainly due to complications of renal insufficiency, shock, or hemorrhage.
Treatment consists of supportive care with careful management of fluids, control of blood pressure, and dialysis, if required. IV ribavirin is an investigational nucleoside analogue, demonstrated to have in vitro activity against hantaviruses (Huggins, 1989). A randomized, double-blind, placebo-controlled trial in China conducted from 1985 to 1987, demonstrated that treatment with IV ribavirin early in disease is associated with a decrease in morbidity and mortality from HFRS (Huggins et al., 1991). In 1987, intravenous (IV) ribavirin was made available on protocol as an investigational drug for treating HFRS in Department of Defense (DoD) medical treatment facilities (control group was not deemed ethical based on decreased mortality reported in the China study). The clinical experience with IV ribavirin for treating HFRS acquired in Korea from 1987 to 2005 was reviewed to assess (1) the clinical course of HFRS treated with IV ribavirin and (2) the safety profile of ribavirin for treating HFRS.
2. Methods
2.1. Study design
The study was conducted at the 121st General Hospital in Seoul, Korea (1987–2005) and at the U.S. Naval Medical Center in Okinawa, Japan (1987–1998). Individuals 18 years old or older were eligible for enrollment, provided they had onset of fever within the past 7 days and either (1) met specific inclusion criteria for a probable case of HFRS or (2) had a clinical syndrome consistent with HFRS meeting most of the criteria (with epidemiological history of possible exposure to hantavirus). A probable case of HFRS was defined as (1) a fever ≥100.5 °F; (2) at least two of the following symptoms: headache; pain in the abdomen, back, or flank; and nausea or vomiting; (3) one physical exam finding suggesting vascular instability or vascular fragility (facial flushing, facial or perioribital edema, conjunctival injection, or petechiae); and (4) and at least one of the following laboratory findings of thrombocytopenia, proteinuria, or elevated serum creatinine. A known severe reaction from ribavirin was the only exclusion criterion.
2.2. Drug formulation and treatment
IV Ribavirin, 1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxiamide (Valeant Pharmaceuticals, Costa Mesa, CA; Manufactured by GensiaSicor Pharmaceuticals Inc., Irvine, CA), was given as a 7-day course, with an initial IV loading dose of 33 mg/kg (maximal dose of 2.64 g), followed by a dose of 16 mg/kg every 6 h for a total of 15 doses (maximum dose of 1.28 g q6 h) for the initial 4 days of therapy, and then 8 mg/kg every 8 h for a total of 9 doses (maximum dose of 0.64 g q8 h) for the next 3 days. The drug was administered in 50–100 ml of normal saline and infused over 30–40 min.
2.3. Clinical and laboratory evaluation
History and physical exams were performed at baseline and daily throughout the 7-day treatment course. A baseline pregnancy test was obtained in women. Baseline and daily laboratory tests included complete blood count, serum electrolytes, renal and liver function tests, serum albumin, total serum protein, prothrombin time, activated partial thromboplastin time, and urinalysis. Individuals were discharged from the hospital after completing the 7-day IV ribavirin course, if clinically stable, with mandatory follow-up and laboratory tests at day 28 and as clinically indicated. In 1999, daily electrocardiogram or cardiac monitoring was required during treatment, after the occurrence of junctional bradycardia temporally related to ribavirin in one subject. Daily pancreatic enzymes were obtained beginning in 1999, and serum magnesium, calcium, and uric acid levels beginning in 2003.
2.4. Serological testing
An investigational serological test, an antibody-specific IgM ELISA for Hantaan virus, was used to confirm HFRS diagnosis. Serological tests were obtained at baseline and the subsequent 2 days. Tests were performed at the 121st General Hospital in Seoul and confirmed at USAMRIID. The procedures for the antibody-specific IgM ELISA are described in a previous publication (LeDuc et al., 1990).
2.5. Data analysis
Subjects with serological confirmed HFRS were included in the analysis of epidemiology and clinical presentation; only subjects who received at least four doses of IV ribavirin were included in analysis of the clinical course of disease and safety. Clinical course analysis assessed occurrence of oliguria, number of subjects requiring dialysis, mean peak serum creatinine; mean day of occurrence of peak serum creatinine and onset of polyuria, hemorrhagic manifestations, nadir platelet count, and death.
3. Results
3.1. Epidemiology (38 cases)
A total of 38 persons with serologically confirmed HFRS acquired in Korea were enrolled in the study from 1987 to 2005 (37 at the 121st General Hospital in Korea; one at U.S. Navy Medical Center Okinawa). The 38 individuals were predominantly male, with a mean age of 26.7 years (Table 1 ). A history of field duty in Korea within the previous 30 days was determined in 31 of 38 (82%) of cases, suggesting Hantaan virus (due to exposure to excreta of field mice) as the cause of the HFRS. The number of cases ranged from zero to seven cases per year. While disease was observed throughout the year, HFRS was seasonal with 79% cases occurring from October through December.
Table 1.
Demographics of 38 individuals with positive antibody-specific IgM ELISA for Hantaan virus.
| Sex | Race | Age (years) | |||
|---|---|---|---|---|---|
| Male | 35 | Caucasian | 21 | Mean | 26.7 |
| Female | 3 | Hispanic | 6 | Range | 19–51 |
| Afro American | 5 | ||||
| Asian | 5 | ||||
| Unknown | 1 | ||||
3.2. Clinical and laboratory presentation (38 cases)
Antibody-specific IgM ELISA for Hantaan virus was positive in 36 of 38 (95%) patients on the first specimen obtained. The initial titers were obtained on mean day 4 of illness (range days 1–7 of fever; range days 1–10 of illness).
A history of fever was obtained from all 38 subjects before initiating IV ribavirin (Table 2 ). The day of onset of fever and day of onset of illness coincided in 32 persons, but fever developed later in six persons (range of 1–4 days after onset of illness). Thrombocytopenia and proteinuria were present in most subjects (36/38 [95%]) but elevated serum creatinine in only 24/38 (63%) persons before initiation of ribavirin.
Table 2.
HFRS presentation: clinical history, examination, and laboratory test findings between the time of illness onset and before initiation of IV ribavirin (N = 38).
| Type | Event | N (%) |
|---|---|---|
| General | Fever (≥100.5 °F.) | 38/38 (100%) |
| Headache | 27/33 (82%) | |
| Hypotension or shock | 4/38 (11%) | |
| Hypertension | 3/38 (8%) | |
| Oliguria (<400 ml/24 h) | 2/38 (5%)a | |
| Polyuria (>4000 ml/24 h) | 2/38 (5%) | |
| Vascular instability or fragility | Conjunctival injection | 24/38 (63%) |
| Periorbital edema or facial flushing | 22/38 (58%) | |
| Facial flushing | 18/38 (47%) | |
| Periorbital edema | 11/35 (31%) | |
| Petechiae | 7/38 (18%) | |
| Ecchymoses | 2/38 (5%) | |
| Bleeding | 1/38 (3%)b | |
| Severe hemorrhage | 0/38 (0%) | |
| Gastrointestinal | Nausea and vomiting | 32/38 (84%) |
| Abdominal, back or flank pain | 32/38 (84%) | |
| Back or flank pain | 26/38 (68%) | |
| Diarrhea | 21/33 (64%) | |
| Abdominal pain | 19/35 (54%) | |
| Laboratory tests | Thrombocytopenia (≤140,000 mm−3) | 36/38 (95%) |
| Proteinuria (plus one or greater) | 36/38 (95%) | |
| Elevated serum creatinine (≥1.3 mg/dl) | 24/38 (63%) | |
Both individuals oliguric on day 0 of IV ribavirin (one oliguric individual only received three doses of ribavirin due to transfer to another hospital for dialysis and was not included in the treatment analysis). No data available to determine if oliguria was present in two severely ill individuals who died within 24 h of receiving the first dose of IV ribavirin (received one or two doses of ribavirin and not included in the treatment analysis).
Epistaxis.
The case definition of a probable HFRS was met by most subjects. All 38 subjects had fevers of ≥100.5 °F and an abnormal laboratory finding of either thrombocytopenia, proteinuria, or an elevated serum creatinine. A history of two of the following symptoms of headache, pain (abdomen, back, or flank), or nausea/vomiting was observed in 32/38 (84%) and findings of vascular fragility or instability in 30/38 (79%) individuals.
3.3. IV Ribavirin initiation and exclusion from analysis (four cases)
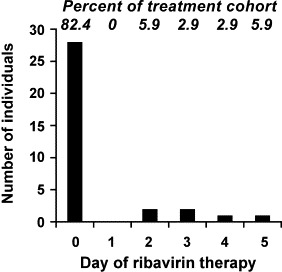
IV Ribavirin was initiated on days 1–7 of fever (days 1–10 illness), with the mean day of ribavirin initiation on day 4 of fever or illness (Fig. 1 ). Four individuals received only one to three doses of IV ribavirin and were excluded from analysis of the clinical course (two subjects had severe disease mimicking septic shock and died within 24 h of ribavirin initiation; two subjects were transferred to another hospital for renal insufficiency with dialysis required in one individual who presented with oliguria and a serum creatinine of 7.3 mg/ml) (Table 3 ).
Fig. 1.
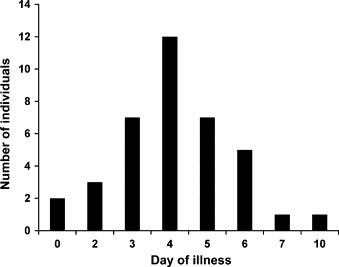
Day of illness of IV ribavirin initiation in 38 individuals with serological confirmation of HFRS.
Table 3.
Number of doses IV ribavirin received in 38 individuals and reasons for early discontinuation of IV ribavirin.
| Number of doses | N (%) | Reason for discontinuation |
|---|---|---|
| 23–25 | 26 (76.5%) | Completion of therapy |
| 22 | 1 | Rash |
| 20 | 1 | Pancreatitisa |
| 19 | 2 | Junctional bradycardiaa |
| Death (respiratory failure) | ||
| 18 | 1 | Sinus bradycardiaa |
| 15 | 1 | Deviation (only 4 days drug ordered) |
| 13 | 1 | Hyperamylasemia/pancreatitisa |
| 10 | 1 | Sinus bradycardiaa |
| 3 | 1 | Transferb |
| 2 | 2 | Transferb |
| Deathb,c | ||
| 1 | 1 | Deathb,c |
Condition may occur from HFRS and unknown if condition is potentiated by ribavirin.
Individuals not included in safety analysis (received < four doses IV ribavirin).
Death occurred within 24 h of IV ribavirin initiation in individuals with severe sepsis-like presentation at the time of drug initiation.
3.4. Treatment analysis (34 cases)
Clinical symptoms and laboratory tests of the 34 persons in the treatment analysis cohort at the time of IV ribavirin initiation (mean day 4 of illness) are listed in Table 4, Table 5 . Most individuals (26/34 [76.5%]) completed a full 7-day course of IV ribavirin therapy, with 91% (31/34) of individuals receiving ≥16 doses of ribavirin. Reasons for early discontinuation of ribavirin in the eight individuals are listed in Table 3.
Table 4.
Baseline symptoms, examination, and laboratory tests on the day of IV ribavirin initiation (day 0 ribavirin) in the 34 individuals in the treatment analysis cohort.
| Type | Clinical symptom or laboratory test | N (%) |
|---|---|---|
| General | Fever (≥100.5 °F.) | 26/33 (79%) |
| Headache | 18/25 (72%) | |
| Hypertension (diastolic >90 mmHg) | 6/34 (18%) | |
| Hypotension (systolic BP < 90 mm) | 2/34 (6%) | |
| Polyuria (>3 l/24 h) | 2/13 (6%) | |
| Oliguria (<400 cm3/24 h) | 1/34 (3%) | |
| Vascular instability or fragility | Conjunctival injection | 21/34 (62%) |
| Facial edema or flushing | 16/34 (47%) | |
| Petechiae | 6/34 (18%) | |
| Ecchymoses | 1/33 (3%) | |
| Bleeding | 1/33 (3%)a | |
| Severe hemorrhage (systolic BP <90 mm) | 0/33 (0%) | |
| Gastrointestinal | Pain in abdomen, back, or flank | 30/34 (88%) |
| Nausea and vomiting | 20/34 (59%) | |
| Diarrhea | 21/34 (62%) | |
| Laboratory | Increased AST (>46 U/ml) | 25/25 (100%) |
| Hypoalbuminemia (<3.9 g/dl) | 26/26 (100%) | |
| Thrombocytopenia (≤140,000 mm−3) | 32/34 (94%) | |
| Proteinuria (trace or greater) | 31/33 (94%) | |
| Decreased corrected calcium | 15/17 (88%) | |
| Increased ALT (>42 U/ml) | 21/25 (84%) | |
| Decreased total protein (<6.6 g/dl) | 18/20 (80%) | |
| Urine red blood cells | 23/32 (72%) | |
| Leukocytosis (>10,800 cells/mm3) | 21/34 (62%) | |
| PTT (>31.9 s) | 9/15 (60%) | |
| Increased creatinine (≥1.3 gm/dl) | 19/34 (56%) | |
| Decreased magnesium (<1.6 mmol/ml) | 4/9 (44%) | |
| Elevated uric acid (>7.2 mg/dl) | 4/15 (27%) | |
| Prothrombin time (>14.1 s) | 4/15 (27%) | |
| Increased lipase (>205 U/ml) | 3/14 (21%) | |
| Increased amylase (>88 U/ml) | 3/20 (15%) | |
| Increased total bilirubin (>1.3 mg/dl) | 3/30 (10%) | |
| Decreased hematocrit (<33%) | 2/34 (6%) | |
| Decreased WBC (<3500 cells/mm3) | 1/34 (3%) | |
BP = blood pressure; AST = aspartate aminotransferase; ALT = alanine aminotransferase; PTT = partial thromboplastin time; WBC = white blood cell count.
Epistaxis.
Table 5.
Mean baseline laboratory values in the 34 individuals included in the treatment cohort on the day of IV ribavirin initiation (Day 0 ribavirin).
| Laboratory test | Na | Mean | Range | S.D. |
|---|---|---|---|---|
| WBC | 34 | 12 868 cells/mm3 | (1600–37 000) | 7021 |
| Hematocrit | 34 | 44.58% | (31.2–54.8) | 5.47 |
| Platelet count | 34 | 59,529 mm−3 | (17 000–204 000) | 38 343 |
| Creatinine | 34 | 2.02 mg/dl | (0.6–6.2) | 1.35 |
| Albumin | 26 | 2.9 g/dl | (2–3.8) | 0.48 |
| Total protein | 20 | 5.8 g/dl | (4.5–7.0) | 0.63 |
| ALT | 25 | 91 U/l | (14–365) | 74.1 |
| AST | 25 | 171 U/l | (44–855) | 193.7 |
| Total bilirubin | 30 | 0.74 mg/dl | (0.1–2.0) | 0.41 |
| Uric acid | 15 | 5.9 mg/dl | (2.3–10) | 2.49 |
| Calcium | 17 | 8.39 mmol/ml | (7.4–9.42) | 0.57 |
| Magnesium | 9 | 1.67 mmol/ml | (1.1–2.3) | 0.35 |
| Amylase | 20 | 81.6 U/ml | (26–611) | 81.6 |
| Lipase | 14 | 320.2 U/ml | (14–2298) | 620.4 |
| Phosphate | 17 | 2.7 mmol/ml | (1.5–4.8) | 1.0 |
N = number individuals with laboratory test result on day of ribavirin initiation.
WBC = white blood cell; ALT = alanine aminotransferase; AST = aspartate aminotransferase.
Oliguria was present in one individual on initiation of ribavirin; none of the remaining 33 individuals developed oliguria or required dialysis. While 15/34 (44%) persons had a normal pretreatment serum creatinine (mean baseline serum creatinine 2.0 mg/dl (range 0.6–6.2 mg/dl), the creatinine remained normal throughout the course of illness in only 4/34 (12%) individuals (Table 6 ). The mean peak serum creatinine of 3.46 mg/dl (range of 0.6–7.8 mg/dl) occurred on day 2 of IV ribavirin therapy (Fig. 2 ). The mean time of occurrence of both the peak serum creatinine and the onset of polyuria was at day 6.79 ± 1.88 of illness (range daya 2–11 illness for peak serum creatinine and days 4–12 of illness for the onset of polyuria), with the polyuria lasting a mean duration of 5.58 ± 3.03 days (range 1–14 days) (Fig. 3 ).
Table 6.
Baseline serum creatinine and maximal serum creatinine levels during treatment of 34 individuals with IV ribavirin.
| Grade toxicity | Day 0 ribavirin, N (%) | Treatment course, N (%) |
|---|---|---|
| 0 (≤1.3 mg/dl) | 15 (44%) | 4 (12%) |
| 1 (1.3 to ≤1.95 mg/dl) | 4 (12%) | 3 (9%) |
| 2 (1.95 to ≤3.9 mg/dl) | 13 (38%) | 18 (53%) |
| 3 (3.9 to ≤7.8 mg/dl) | 2 (6%) | 9 (26%) |
Fig. 2.
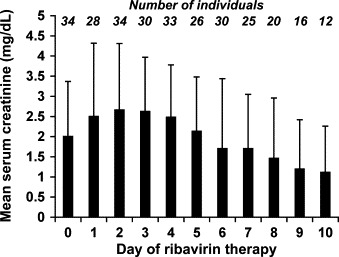
Mean serum creatinine (by day of IV ribavirin therapy) in the IV ribavirin treatment analysis cohort of 34 individuals.
Fig. 3.
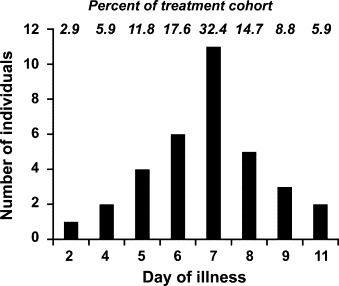
Day of illness on which the peak serum creatinine occurred in the 34 individuals in the IV ribavirin treatment analysis cohort.
Hypotension (defined as systolic blood pressure less than 90 mm of mercury), present in two individuals when IV ribavirin was initiated, was managed with fluids and vasopressors, and resolved within 24 h. A hypotensive phase was not observed in the remaining 32 individuals.
An increase in the platelet count was observed the day after ribavirin initiation in 82% (28/34) individuals (Fig. 4 ). The mean time of the nadir platelet count was on day 0.56 of ribavirin therapy (range 0–5 days) and at day 4.6 of illness (range 0–11 days) (Fig. 5 ). A platelet count less than 50 000 mm−3 was noted in 56% (19/34) of patients, with only 15% (5/34) of patients having a platelet count less than 25 000 mm−3.
Fig. 4.
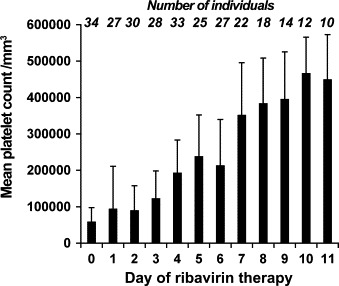
Time of occurrence of the nadir platelet count (by day of IV ribavirin therapy) in the IV ribavirin treatment analysis cohort of 34 individuals.
Fig. 5.
Mean platelet count (by day of IV ribavirin therapy) in the IV ribavirin treatment analysis cohort of 34 individuals.
Petechiae were present in 35% of individuals (present in seven individuals before ribavirin initiation; only five individuals developed petechiae after initiation of ribavirin). Two individuals developed ecchymoses, and five individuals experienced mild bleeding (four individuals had mild epistaxis; one individual had mild bleeding from an appendectomy and venipuncture site). Severe hemorrhage (resulting in a systolic blood pressure less than 90 mm or hemorrhagic shock) was not observed. However, one death due to respiratory failure of unclear etiology (moderately severe respiratory failure present when IV ribavirin was initiated) was associated with a sudden decrease in hemoglobin over the previous 24 h but without overt evidence of bleeding. The individual died on day 5 of IV ribavirin therapy due to sudden deterioration of respiratory symptoms over 10 min (required intubation and subsequent cardiopulmonary resuscitation). This was the only death in the treatment cohort of 34 persons.
3.5. Safety analysis (34 cases)
3.5.1. Hemolytic anemia
The main adverse event observed from IV ribavirin was a reversible hemolytic anemia. Anemia (hematocrit ≤33%) was observed in 27/34 (79.4%) individuals, with 26 persons (76.5%) having a 25% or greater decrease in the hematocrit. Two of the four cases with World Health Organization (WHO) grade 4 anemia toxicity were not attributed to be secondary to IV ribavirin (Fig. 6 ).
Fig. 6.
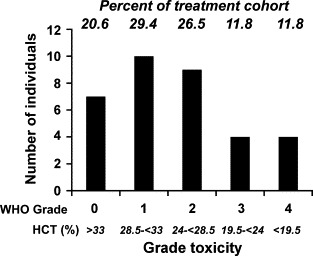
Severity of anemia by World Health Organization (WHO) adverse event classification in the IV ribavirin treatment analysis cohort of 34 individuals.
3.5.2. Rash
A rash on the neck and upper chest was observed in one individual after infusion of dose 21 of ribavirin, which resolved within 24 h after administration of diphenhydramine (Benadryl) 50 mg intramuscularly. The rash recurred during the infusion of dose 22 (premedicated with diphenhydramine), and ribavirin was discontinued (Table 3).
3.5.3. Bradycardia
Asymptomatic bradyarrhythmias were observed in three cases (Table 3). The first case occurred in 1998 when an individual developed an asymptomatic bradycardia (40 beats/min) on day 3 of IV ribavirin, which progressed to an asymptomatic junctional bradycardia (30 beats/min) on day 4 of therapy. The ribavirin was discontinued (total of 19 doses received), and the bradyarrhythmia resolved within 36 h. The protocol subsequently required cardiac monitoring and/or daily EKGs while on therapy. In 2005, two individuals developed intermittent, asymptomatic periods (1–2 h) of sinus bradycardia (as low as 29 and 30 beats/min), beginning on day 3 of ribavirin therapy. After discontinuation of the ribavirin (received 18 doses and 10 doses, respectively), the bradycardia resolved in both individuals within 24–36 h. The “possible” temporal relationship of the bradyarrhythmias with IV ribavirin raised a concern of potentiation of bradyarrhythmias from IV ribavirin. None of the three individuals had severe renal insufficiency (peak serum creatinine ranged from 1.5 to 2.5 mg/dl) to suggest the presence of higher ribavirin levels.
3.5.4. Elevation of pancreatic enzymes, hyperuricemia, hypocalcemia, and hypomagnesemia
Abnormal baseline amylase was noted in 3/20 (15%) persons who had baseline amylase levels performed. Elevation of serum amylase was subsequently observed in 11 of the remaining 17 persons (65%), occurring on mean day 3.7 (range days 2–9) of ribavirin therapy. Five persons exhibited WHO grade-3 toxicity (amylase 177–440 U/ml). Only two individuals had ribavirin discontinued prematurely because of elevated pancreatic enzymes (Table 3). One individual had elevated pancreatic enzymes and abdominal pain before initiation of IV ribavirin, with the amylase decreasing on days 3 and 4 of ribavirin therapy (received 20 doses); the other subject had also received high-dose intravenous methylprednisolone.
Elevation of uric acid was observed in all 14 individuals who had serum uric acid tests performed during the course of ribavirin, with 11 individuals having a peak uric acid greater than 10 mg/dl. The mean peak uric acid level was 13.4 mg/dl (range 7.4–27.1 mg/dl) and occurred on day 4 of ribavirin. All individuals were asymptomatic from the hyperuricemia. Hypocalcemia (corrected for low albumin) and hypomagnesaemia were observed commonly before initiation of IV ribavirin (15/17 (88%) and 4/9 (44.4%) individuals, respectively). Supplemental calcium and magnesium were administered to 6/24 (25%) and 18/29 (62%) individuals, respectively.
4. Discussion
4.1. HFRS clinical presentation and course of illness
The pathogenesis of HFRS is unknown, but most likely immune mediated, as IgM antibody to Hantaan virus and circulating T lymphoblasts are present at the onset of symptoms (Peters et al., 1999, Kanerva et al., 1998, Lewis et al., 1990). Renal insufficiency is most likely caused by proinflammatory mediators generated by the host's immune response against the virus (Takala et al., 2000, Kanerva et al., 1998, Cosgriff, 1991, Peters et al., 1999, Mustonen et al., 1994b). Severity of disease may be dependant upon the species of hantavirus, virulence of the hantavirus strain, exposure dose, and major histocompatibility complex of the host (Huggins et al., 1991, Kompanets et al., 2007, Peters et al., 1999, Mustonen et al., 1996, Mustonen et al., 1998). Lower death rates (range 1.5–7%) have been reported when disease was managed by health-care providers experienced in treating HFRS and/or with dialysis availability (Smadel, 1951, Kim et al., 2006).
IV Ribavirin was demonstrated to decrease severity of disease from HFRS in animals, where disease severity has correlated with viral burden (Kanerva et al., 1998, Zhang et al., 1987, Zhang et al., 1993). Suckling mice infected with Hantaan virus and then treated with ribavirin (either at the onset of viremia on day 6 or at the appearance of viral antigen in tissues on day 10) had decreased severity of illness and increased survival (Huggins et al., 1986). By days 18–20, viral titers in organs of treated animals were a 100-fold lower than those in control animals. Ribavirin-treated mice also had lower levels of viremia.
In a randomized, double-blinded, placebo-controlled clinical trial in China (1985–1987), IV ribavirin given within 7 days of fever onset was associated with a decreased occurrence of oliguria, decreased severity of renal insufficiency, earlier onset of the peak serum creatinine and polyuria, and decreased hemorrhagic manifestation of disease compared to non-ribavirin treated controls (Huggins et al., 1991). A decrease in mortality was observed in ribavirin-treated subjects [2.5% (3/125) versus 8.5% (10/117) in non-ribavirin treated controls], which was a sevenfold decrease in mortality when adjusted for baseline variables (dialysis not available in this study). The mechanism by which ribavirin prevented death was most likely due to prevention of oliguria, as 12 of the 13 deaths were associated with prolonged oliguria. While the antiviral activity of IV ribavirin may be due to multiple mechanisms, recent data suggest ribavirin may exert its primary activity against Hantaan virus by serving as a RNA virus mutagen resulting in an “extinction catastrophe” error, as a result of incorporation in the viral RNA genome (Huggins, 1989, Chung et al., 2007).
Comparison of this IV ribavirin-treated cohort to historical non-ribavirin treated HFRS controls in Korea has limitations, as adjustments cannot be made for all variables that may influence disease severity (i.e., demographics of subjects, hantavirus strains, exposure dose that may be influenced by yearly infected rodent population, treatment variability, vaccination status). However, in a cohort comprised of Republic of Korea (ROK) military troops (mainly young adult males) hospitalized on mean day 4 of illness with HFRS at a medical referral center with dialysis capability and experienced clinicians between 2000 and 2004, oliguria was observed in 24/61 (39%) and dialysis was required in 23/61 (38%) individuals (Kim et al., 2006) (Table 7 ). The time of onset of symptoms to admission was similar in the oliguric and non-oliguric groups. Most individuals who developed oliguria (21/24 (87.5%)) subsequently required dialysis: only 2 of 37 (5.4%) non-oliguric persons required dialysis. The mean peak serum creatinine in the 24 oliguric patients was 10.8 mg/dl, and did not occur until mean day 9.3 of illness (range days 6–13). The onset of oliguria occurred on mean day 5.5 of illness (range days 3–8) and lasted a mean duration of 4.9 days (range 1–11 days). The 37 non-oliguric patients had a mean peak serum creatinine of 4.7 mg/dl occurring on mean day 7.6 of illness (range days 5–12). While 40% of HFRS cases had received a hantavirus vaccine, a protective effect of the vaccine on preventing oliguria was not observed.
Table 7.
Review of occurrence of oliguria, dialysis requirement, mean time of peak serum creatinine, severity of renal failure, and death in the IV ribavirin-treated HFRS cohort vs. historical non-ribavirin-treated HFRS controls in Korea.
| Cohort | Oliguria, N (%) | Dialysis, N (%) | Mean day, peak Cr | Mean, peak Cr (mg/dl) | Death, N (%) | |
|---|---|---|---|---|---|---|
| Ribavirin | Rusnak (N = 34)a | 1/34 (3%)b | 0/34 (3%) | 6.8 | 3.46 | 1/34 (3%) |
| Rusnak (N = 38)c | 2/38 (5%)d | 1/38 (3%) | ND | 3.56 | 3/38 (8%) | |
| Non-ribavirin treated | Kim, 2006e | 24/61 (39%) | 23/61 (38%) | 9.3f | 10.8f | 1/68 |
| 7.6g | 4.7g | |||||
| Lee (1999)h | 60% | 40% | 7–12 | ND | 2–7% | |
| Lee (1999)i | 20/40 (50%) | 8/40 (20%) | ND | ND | 0/40 (0%) | |
| Bruno et al. (1990)j | 18/26 (69%) | 4/26 (16%) | ND | ND | 3/26( 12%) |
Cr = serum creatinine; ND = no data.
Treatment cohort of 34 individuals (excludes four individuals who received ≤three doses of IV ribavirin).
Individual was oliguric before IV ribavirin initiation.
Total cohort of 38 individuals (includes four individuals who received ≤three doses of IV ribavirin).
Both individuals oliguric on day 0 ribavirin (one individual received only three doses of IV ribavirin due to transfer to another hospital for dialysis and is not included in the treatment cohort),
ROK troops hospitalized for HFRS.
Patients who developed oliguria.
Patients who did not develop oliguria.
HFRS from Hantaan virus.
HFRS from Seoul virus.
US military troops who acquired HFRS in Korea.
The experience of this ROK cohort reported by Kim was similar to an earlier unvaccinated HFRS cohort (comprised of 124 patients admitted to Central Army Hospital in 1979 and 104 patients to Seoul National University Hospital in 1988), with oliguria reported in 60% of HFRS cases due to Hantaan virus and dialysis required in 40% of cases (creatinine values were greater than 10 mg/dl in 42% cases) (Lee, 1991) (Table 7). The onset of oliguria in HFRS from Hantaan virus generally occurred on days 6–8 of illness, and lasted 3–5 days (range 1–16 days). The peak serum creatinine generally was not observed until days 7–12 of illness, with the onset of polyuria late in the second week of illness (days 9–14 of illness). In this same publication, HFRS due to Seoul virus was associated with oliguria in 50% of patients, with dialysis required in 20% cases (serum creatinine greater than 10 mg/dl in 17% cases).
The experience in a U.S. DoD cohort with HFRS acquired in Korea (1984–1987) before use of IV ribavirin (mainly young adult males treated at U.S. DoD medical facilities with dialysis availability) was similar to the Korean HFRS cohorts, with oliguria occurring in 18/26 (69%) HFRS cases (Bruno et al., 1990) (Table 7). Oliguria lasted a mean duration of 8 days (range 3–17 days), with onset of polyuria generally not occurring until later in the second week of illness. Dialysis was required in 16% cases.
While comparison of the ribavirin-treated HFRS cohort to historical control cohorts cannot be made due to limitations in adjusting for differences in baseline demographics and other variables that may influence disease progression, oliguria in only one (3%) subject (present before initiation of ribavirin) and dialysis requirement in none of 34 subjects in this treatment cohort was lower than the 39–69% oliguria and 16–40% dialysis requirement observed in non-ribavirin-treated HFRS cohorts from Korea (Lee, 1991, Bruno et al., 1990, Kim et al., 2006). Over this similar time period, the dialysis requirement in the two Korean cohorts remained unchanged. Additionally, the mean peak serum creatinine was lower (3.46 mg/dl; maximum creatinine 7.8 mg/dl) and the peak serum creatinine and onset of polyuria (mean day 6.8 illness) occurred earlier, than historically reported. Similar to the ribavirin-treated cohort, the three non-ribavirin treated cohorts were also comprised mainly of young adult males. The ribavirin-treated cohort was managed in a hospital with dialysis referral capability.
The clinical experience in this ribavirin-treated cohort is suggestive that IV ribavirin may be associated with a decrease in oliguria occurrence and renal disease severity (as reported in the IV ribavirin HFRS treatment trial performed in China), and provides support for the need of a second placebo-controlled study for the goal of FDA approval of the drug (Huggins et al., 1991). The concern of a higher death rate in non-ribavirin treated HFRS control group making a control group unethical may not apply in populations with dialysis capability, as the death rate of 1/34 (2.9%) in the ribavirin treatment cohort was similar to death rates (1.5–7%) reported in non-ribavirin HFRS cohorts in Korea with dialysis availability (Lee, 1991, Kim et al., 2006) (Table 7).
The severity of thrombocytopenia (attributed primarily to increased platelet consumption and disseminated intravascular coagulopathy) as well as defects in the platelet function may contribute to problems with hemostasis in HFRS (Guang et al., 1989, Kanerva et al., 1998, Cosgriff, 1991). A trend toward an increased platelet count and a decrease in hemorrhagic manifestations of disease was observed in ribavirin-treated HFRS patients compared to non-ribavirin treated controls (Huggins et al., 1991). Thrombocytosis attributed to ribavirin was observed in rhesus macaques with Argentine hemorrhagic fever (AHF) treated with IV ribavirin (McKee et al., 1988). Studies suggest the mechanism for the increased platelet count was stimulation of platelet production, based on the increase in megakaroctyes and ploidy observed in ribavirin-treated macaques. As aggregation studies suggested platelet function was normal, an increase in normal-functioning platelets could result in a potential hemostasis benefit in HFRS.
The occurrence of the nadir platelet count on mean day 0.56 of ribavirin and an increase in the platelet count in 82% individuals the day after ribavirin initiation in this cohort suggests a possible temporal relation of the platelet increase to ribavirin. The nadir platelet count on mean day 4.6 of illness in this ribavirin-treated cohort is similar to the ROK non-ribavirin treated military cohort (mean day 5.4 in oliguric patients and mean day 4.8 in non-oliguric patients) (Kim et al., 2006), but earlier than reported two non-ribavirin treated HFRS cohorts (day 6 to early in the second week of illness) (Lee, 1991, Bruno et al., 1990). Petechiae have been observed in 32–95% cases, and ecchymoses in 18–37% cases of HFRS acquired in Korea (Lee, 1991, Bruno et al., 1990). While the percentage of individuals with hemorrhagic manifestations of HFRS in this ribavirin-treated cohort (35% petechiae, 6% ecchymoses, 15% mild bleeding, and 0% severe hemorrhage) is lower than historically reported, a decrease in the risk of hemorrhage due to ribavirin cannot be assessed without a control group.
4.2. Adverse events
4.2.1. Anemia
A reversible hemolytic anemia is a common and well-known side effect of ribavirin, and was the most common adverse event observed. The occurrence of a 25% or greater reduction of the hematocrit in 75% individuals in this cohort was higher than observed in the China ribavirin-treated cohort (observed in only one-third of HFRS subjects receiving IV ribavirin) (Huggins et al., 1991), but similar to cohorts receiving IV ribvirin for hantapulmonary syndrome (HPS) and severe acute respiratory syndrome (SARS) (Chapman et al., 1999, Chapman et al., 2002, Chiou et al., 2005, Knowles et al., 2003, Muller et al., 2007, Koren et al., 2003, McEvoy et al., 2004). The anemia was well tolerated in this HFRS cohort comprised of mainly young healthy adults. However, ribavirin should be used with caution in individuals with medical conditions such as coronary artery disease or congestive heart failure (CHF), where anemia may not be tolerated.
4.2.2. Bradyarrhythmias
The three bradyarrhythmias seen in this cohort were most likely from HFRS and not from IV ribavirin. Bradycardia in HFRS has been reported in numerous publications, occurring in 19–73% of individuals with HFRS from the four hantaviruses causing HFRS and most commonly during the oliguric and polyuric phases (between days 9–13 of illness) (Amitina, 1962, Pimenov et al., 2002, Puljiz et al., 2005, Katetanovic et al., 1992). Other cardiac abnormalities reported with HFRS include nonspecific cardiac conduction abnormalities, atrial fibrillation, junctional bradycardia, first and second degree atrioventricular (AV) block, premature atrial and ventricular contractions, sinus tachycardia, depressed left ventricular function, and myocarditis (Markotic et al., 2002, Puljiz et al., 2005, Chun and Godfrey, 1984, Pal et al., 2005, Basin et al., 1992, Liu et al., 2002, Katetanovic et al., 1992, Pimenov et al., 2002). While EKG abnormalities have been reported in 30/79 (38%) cases of HFRS acquired in Croatia (either from Dobrava or Puumala viruses), electrolyte and metabolic disturbances were not found to be statistically different in patients with abnormal EKGs (Puljiz et al., 2005). Autopsy reports demonstrating cardiac findings of hemorrhage and edema (mainly in the right atrium) and mononuclear cell infiltrates (mainly in the left atrium but throughout the heart) (Lukes, 1954, Hullinghorst and Steer, 1953, Kessler, 1953) suggest cardiac abnormalities may be a direct effect of the hantavirus.
The temporal resolution of bradyarrhythmias within 24–36 h of ribavirin cessation in this cohort may reflect the nature of the bradyarrhythmias in HFRS, which are generally self-limiting and occur mainly during the oliguria phase. Higher drug levels were not felt to have been present in the three cases of bradyarrhythmias, as the serum creatinine levels were only mildly elevated. Ribavirin was not associated with cardiotoxicity or cardiac effects in preclinical animal trials involving dogs, monkeys, or rats (myocarditis was observed in an initial study but not in the four subsequent studies in rats) (ribavirin investigator brochure, 1989). However, a recent retrospective analysis of SARS patients showed treatment with IV ribavirin was associated with an increased risk of bradycardia (heart rate < 55 beats/min) (Muller et al., 2007). The possibility that ribavirin may potentiate bradycardia cannot be assessed without a placebo-control study.
4.2.3. Hyperamylasemia/pancreatitis, hyperuricemia, hypocalcemia, and hypomagnesemia
While other nucleoside analogues have been associated with pancreatitis, it is not possible to determine if ribavirin may have caused or potentiated pancreatitis or hyperamylasemia without a placebo-controlled study, as pancreatitis is a known complication of HFRS (present in one third of HFRS autopsies during the Korean conflict) (Hullinghorst and Steer, 1953). Patients with SARS receiving IV ribavirin were not at increased risk for pancreatitis or elevated pancreatic enzymes on a multivariate analysis, although elevated amylase levels (not pancreatitis) occurred more frequently in a univariate analysis (Muller et al., 2007). Hyperamylasemia and pancreatitis were observed in both seronegative and seropositive individuals given IV ribavirin for possible HPS, suggesting either enrollment bias or a drug induced etiology (Chapman et al., 1999, Chiou et al., 2005). Pancreatic enzymes should be followed in individuals with HFRS, and discontinuation of ribavirin may be considered in persons who develop pancreatitis.
As hyperuricemia has been reported in 85% of cases and hypocalcemia and hypomagnesemia in as high as 89% of cases of HFRS not treated with ribavirin, no determination can be made in this study concerning potentiation of these laboratory abnormalities by IV ribavirin (Lee, 1991, Mustonen et al., 1994a). Mild hyperuricemia has been associated with ribavirin, possibly reflecting metabolism of ribavirin to urates (Investigator Brochure, 2004). While uric acid levels in this cohort were commonly ≥10 mg/dl and as high as 27 mg/dl, no subject developed symptoms from hyperuricemia. Retrospective analysis of cohorts of SARS showed patients receiving IV ribavirin were statistically more likely to develop hypomagnesemia, and possibly hypocalcemia, suggesting IV ribavirin may perhaps potentiate hypomagnesemia and hypocalcemia (Muller et al., 2007, McEvoy et al., 2004).
5. Conclusions
While direct comparison of this cohort to historical non-ribavirin treated HFRS controls is not possible due to the inability to adjust for all baseline demographics and variables that may influence disease severity, the clinical experience observed with IV ribavirin for treatment of HFRS in this U.S. DoD cohort in Korea (only 3% oliguria and no dialysis requirement in the treatment cohort) is suggestive that administration of IV ribavirin early in HFRS may decrease renal complications of HFRS, as reported in the initial IV ribavirin trial in China. The ethical concerns for performing a second placebo-controlled trial may also be addressed by this study, as death rates in this cohort were similar to non-ribavirin treated HFRS cohorts in Korea with dialysis availability, suggesting dialysis may prevent deaths related to severe renal insufficiency that were possibly prevented by IV ribavirin in the China study. The main adverse event from IV ribavirin was reversible hemolytic anemia, which is common and may be severe. The association of ribavirin with adverse events of hypocalcemia, hypomagnesemia, hyperuricemia, pancreatitis, and bradycardia is unclear, as these abnormalities are also complications of HFRS. This study supports the need for a randomized, placebo-controlled study to assess IV ribavirin in treating HFRS and to support FDA approval of the drug.
Acknowledgements
We thank all the healthcare and regulatory personnel for their contributions during the 18 years of the protocol (1987–2005), with special appreciation to contributions by the following clinical investigators and clinical coordinators: Michael J. Abele, James Arthur, Steven P. Bennett, Bong Sup Choi, Timothy Endy, Ronald H. Fields, Mark M. Fukuda, Kevin Glass, Patricia B. Gurczak, Yoon Haro, Janet Hays, Duane R. Hospenthal, Nancy E. Huth, Bong Sup Kim, Hoon Kim, Paul B. Kim, James LeDuc, Carl Lindquist, Rodrigo A. Mariono, Mammem P. Mammem, Jr, James W. Martin, James Meegan, William L. Melcher, Viet-Nhan H. Nguyen, Daniel Randall, Rossane Ressner, David Sachar, Joseph Smith, Jeffrey Strong, Glen E. Tompkins, Richard L Urban, and Thomas M. Wiley.
Footnotes
Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the U.S. Army. This article was co-written by an officer or employee of the U.S. Government as part of their official duties and therefore is not subject to U.S. copyrights. Research on human subjects was conducted in compliance with DoD, federal, and state statutes and regulations relating to the protection of human subjects, and adheres to the principles identified in the Belmont Report (1979). All data and human subjects research were gathered and conducted for this publication under IRB approved protocols.
References
- Amitina R.Z. On the sinus bradycardia in hemorrhagic nephroso-nephritis. Terapevticheskii. Arkhiv. 1962;34:92–95. [PubMed] [Google Scholar]
- Basin B., Piperaud R., Guilbaud J.C., Moussinga N. Bloc auriculo-ventriculaire chez deux patients atteints de fievre hemorragique avec syndrome renal (Nephropathies a Hantaan-Virus) Rev. Med. Intern. 1992;13:244–245. doi: 10.1016/s0248-8663(05)81338-4. [DOI] [PubMed] [Google Scholar]
- Bruno P., Hassell L.H., Brown J., Tanner W., Lau A. The protean manifestations of hemorrhagic fever with renal syndrome: a retrospective review of 26 cases from Korea. Ann. Int. Med. 1990;113:385–391. doi: 10.7326/0003-4819-113-5-385. [DOI] [PubMed] [Google Scholar]
- Chapman L.E., Mertz G.J., Peters C.J., Jolson H.M., Khan A.S., Ksiazek T.G., Koster F.T., Baum K.F., Rollin P.E., Pavia A.T., Holman R.C., Christenson J.C., Rubin P.J., Behrman R.E., Bell L.J., Simpson G.L., Sadek R.F., Ribavirin Study Group Intravenous ribavirin for hantavirus pulmonary syndrome: safety and tolerance during one year of open label experience. Antivir. Ther. 1999;4:211–219. doi: 10.1177/135965359900400404. [DOI] [PubMed] [Google Scholar]
- Chapman L.E., Ellis B.A., Koster F.T., Sotir M., Ksiazek T.G., Mertz G.J., Rollin P.E., Baum K.F., Pavia A.T., Christenson J.C., Rubin P.J., Jolson H.M., Behrman R.E., Khan A.S., Bell L.J., Simpson G.L., Hawk J., Holman R.C., Peters C.J., Ribavirin Study Group Discriminators between Hantavirus-infected and–uninfected persons enrolled in a trial of intravenous ribavirin for presumptive hantavirus pulmonary syndrome. Clin. Infect. Dis. 2002;34:293–304. doi: 10.1086/324619. [DOI] [PubMed] [Google Scholar]
- Chiou H.E., Liu C.L., Buttrey M.J., Kuo H.P., Liu H.W., Kuo H.T., Lu Y.T. Adverse effects of ribavirin and outcome in severe acute respiratory syndrome: experience in two medical centers. Chest. 2005;128:263–272. doi: 10.1378/chest.128.1.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun P.K., Godfrey L.J. Unique selective right atrial hemorrhage with epidemic (Korean) hemorrhagic fever. Am. Heart J. 1984;108:410–412. doi: 10.1016/0002-8703(84)90634-3. [DOI] [PubMed] [Google Scholar]
- Chung, D., Sun, Y., Parker, W., Arterburn, J., Johnson, C.B., 2007. Ribavirin inhibits Hantaan virus via an extinction catastrophe rather than an error catastrophe mechanism. VII International Conference on HFRS, HPS, and Hantaviruses. Abstract 107, Buenos Aries, Argentina. June 15, 2007, p. 204.
- Cosgriff T.M. Mechanisms of disease in hantavirus infection: pathophysiology of HFRS. Rev. Infect. Dis. 1991;13:97–107. doi: 10.1093/clinids/13.1.97. [DOI] [PubMed] [Google Scholar]
- Guang M.Y., Liu G.Z., Cosgriff T.M. Hemorrhage in hemorrhagic fever with renal syndrome in China. Rev. Infect. Dis. 1989;11(S4):S884–S890. doi: 10.1093/clinids/11.supplement_4.s844. [DOI] [PubMed] [Google Scholar]
- Huggins J.W., Kim G.R., Brand O.M., McKee K.T. Ribavirin therapy for Hantaan virus infection in suckling mice. J. Infect. Dis. 1986;153:489–497. doi: 10.1093/infdis/153.3.489. [DOI] [PubMed] [Google Scholar]
- Huggins J.W. Prospects for treatment of viral hemorrhagic fevers with ribavirin, a broad-spectrum antiviral drug. Rev. Infect. Dis. 1989;11(S4):S750–S761. doi: 10.1093/clinids/11.supplement_4.s750. [DOI] [PubMed] [Google Scholar]
- Huggins J.W., Hsiang C.M., Cosgriff T.M., Guang M.Y., Smith J.I., Wu Z.O., LeDuc J.W., Zheng Z.M., Meegan J.M., Wang Q.N., Oland D.D., Gui X.E., Gibbs P.H., Yuan H.Y., Zhang T.M. Prospective, double-blind, concurrent, placebo-controlled clinical trial of intravenous ribavirin therapy of hemorrhagic fever with renal syndrome. J. Infect. Dis. 1991;64:1119–1127. doi: 10.1093/infdis/164.6.1119. [DOI] [PubMed] [Google Scholar]
- Hullinghorst R.L., Steer A. Pathology of epidemic hemorrhagic fever. Ann. Intern. Med. 1953;38:77–101. doi: 10.7326/0003-4819-38-1-77. [DOI] [PubMed] [Google Scholar]
- Investigator's Brochure. Ribavirin, 1989. Viratek Inc., Costa Mesa, CA. FDA: Amendment-062 revised August 11, 1989.
- Investigational Drug Brochure, 2004. Virazole (Ribavirin, USP) injection, 100 mg/mL. IND 9076. Fourth edition. Valeant Pharmaceuticals International, Costa Mes, CA.
- Kanerva M., Mustonen J., Vaheri A. Pathogenesis of Puumala and other hantavirus infections. Rev. Med. Virol. 1998;8:67–86. doi: 10.1002/(sici)1099-1654(199804/06)8:2<67::aid-rmv217>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Katetanovic B., Ridanovic Z., Petrovic O., Arslanagic A. ECG in patients with haemorrhagic fever. Medicinski. Arhiv. 1992;46:64–65. [PubMed] [Google Scholar]
- Kessler W.H. Gross anatomic features found in 27 autopsies of epidemic hemorrhagic fever. Ann. Intern. Med. 1953;38:73–76. doi: 10.7326/0003-4819-38-1-73. [DOI] [PubMed] [Google Scholar]
- Kim Y.K., Lee S.C., Kim C.S., Heo S.T., Choi C.M., Kim J.M. Clinical characteristics and predictors of acute oliguric renal failure in hemorrhagic fever with renal syndrome. Korean J. Med. 2006;70:190–195. [Google Scholar]
- Knowles S.R., Phillips E.J., Dresser L., Matukas L. Common adverse events associated with the use of ribavirin for severe acute respiratory syndrome in Canada. Clin. Infect. Dis. 2003;37:1139–1142. doi: 10.1086/378304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kompanets, G., Slonova, R., Lunikhina, O., 2007. Influence of the conditions of airborne mode of hantavirus transmission on the severity of HFRS. VII International Conference on HFRS, HPS, and Hantaviruses. Abstract 6. Buenos Aries, Argentina. June 15, 2007, p. 94.
- Koren G., King S., Knowles S., Phillips E. Ribavirin in the treatment of SARS: a new trick for an old drug? Canadian Med. Assn. J. 2003;168:1289–1292. [PMC free article] [PubMed] [Google Scholar]
- LeDuc J.W., Ksiazek T.B., Rossi C.A., Dalrymple J.M. A retrospective analysis of sera collected by the hemorrhagic fever commission during the Korean Conflict. J. Infect. Dis. 1990;162:1182–1184. doi: 10.1093/infdis/162.5.1182. [DOI] [PubMed] [Google Scholar]
- Lee H.W. Epidemiology and epizoology. In: Lee H.W., Calisher C., Schmaljohn C., editors. Manual of Hemorrhagic Fever With Renal Syndrome and Hantavirus Pulmonary Syndrome. WHO Collaborating Center for Virus Reference and Research (Hantaviruses), Asan Institute for Life Sciences; Seoul: 1999. pp. 40–48. [Google Scholar]
- Lee J.S. Clinical features of hemorrhagic fever with renal syndrome in Korea. Kidney Int. 1991;40:S88–S93. [PubMed] [Google Scholar]
- Lewis R.M., Lee H.W., See A.F., Parrish D.B., Moon J.S., Kim D.J., Cosgriff T.M. Changes in population of immune effector cells during the course of HFRS. Trans. R. Soc. Trop. Med. Hyg. 1990;85:282–286. doi: 10.1016/0035-9203(91)90058-7. [DOI] [PubMed] [Google Scholar]
- Liu Y.H., Huang J.H., Hsueh P.R., Luh K.T. Hantavirus infection with marked sinus bradycardia, Taiwan [Letter to the editor] Emerg. Infect. Dis. 2002;8:644. doi: 10.3201/eid0806.010340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukes R.J. The pathology of thirty-nine fatal cases of epidemic hemorrhagic fever. Am. J. Med. 1954;16:639–650. doi: 10.1016/0002-9343(54)90270-3. [DOI] [PubMed] [Google Scholar]
- Markotic A., Nichol S.T., Kuzman I., Sanchez A.J., Ksiazek T.G., Gagro A., Rabatic S., Zgorelec R., Avsic-Zupanc T., Beus I., Dekaris D. Characteristics of Puumala and Dobrava infections in Croatia. J. Med. Virol. 2002;66:542–551. doi: 10.1002/jmv.2179. [DOI] [PubMed] [Google Scholar]
- McEvoy G.K., Miller J., Litvak K. American Society of Health-System Pharmacists Inc.; Bethesda, MD: 2004. AHFS Drug Information; 2004. [Google Scholar]
- McKee K.T., Huggins J.W., Trahan C.J., Mahlandt B.G. Ribavirin prophylaxis and therapy for experimental argentine fever. Antimicrob. Agents Chemother. 1988;32:1304–1309. doi: 10.1128/aac.32.9.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller M.P., Dresser L., Raboud J., McGeer A., Rea E., Richardson S.E., Mazzulli T., Loeb M., Louie M. Adverse events associated with high-dose ribavirin: evidence from Toronto outbreak of severe acute respiratory syndrome. Pharmocotherapy. 2007;27:494–502. doi: 10.1592/phco.27.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustonen J., Brummer-Korvenkontio M., Hedman K., Pasternack A., Pietila K., Vaheri A. Nephropathia epidemica in Finland: a retrospective study of 126 cases. Scand. J. Infect. Dis. 1994;26:7–13. doi: 10.3109/00365549409008583. [DOI] [PubMed] [Google Scholar]
- Mustonen J., Helin H., Pietila K., Brummer-Korvenkontio M., Hedman K., Vaheri A., Pasternack A. Renal biopsy findings and clinicopathologic correlations in nephropathica epidemica. Clin. Nephrol. 1994;41:121–126. [PubMed] [Google Scholar]
- Mustonen J., Partanen J., Kanerva M., Pietila K., Vapalahiti O., Pasternack A., Vaheri A. Genetic susceptibility to severe course of nephropathia epidemica caused by Puumala hantavirus. Kidney Int. 1996;49:217–221. doi: 10.1038/ki.1996.29. [DOI] [PubMed] [Google Scholar]
- Mustonen J., Partanen J., Kanerva M., Pietila K., Vapalahti O., Pasternack A., Vaheri A. Association of HLA B27 with benign clinical course of nephropathia epidemica caused by Puumala hantavirus. Scand. J. Immunol. 1998;47:277–279. doi: 10.1046/j.1365-3083.1998.00302.x. [DOI] [PubMed] [Google Scholar]
- Pal E., Strle F., Avsic-Zupanc T. Hemorrhagic fever with renal syndrome in the Pomurje region of Slovenia- an 18-year survey. Wien. Klin. Wochenschr. 2005;117:398–405. doi: 10.1007/s00508-005-0359-2. [DOI] [PubMed] [Google Scholar]
- Peters C.J., Simpson G.L., Levy H. Spectrum of hantavirus infection: hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. Ann. Rev. Med. 1999;50:531–545. doi: 10.1146/annurev.med.50.1.531. [DOI] [PubMed] [Google Scholar]
- Pimenov L.T., Dudarev M.V., Eshmakov S.V. Clinicofunctional characteristics of the heart in haemorrhagic fever with renal syndrome. Klin. Med. 2002;80:28–31. [PubMed] [Google Scholar]
- Puljiz I., Kuzman I., Markotic A., Turcinov D., Matic M., Makek N. Electrocardiographic changes in patients with haemorrhagic fever with renal syndrome. Scand. J. Infect. Dis. 2005;37:594–598. doi: 10.1080/00365540510036606. [DOI] [PubMed] [Google Scholar]
- Smadel J.E. Epidemic haemorrhagic fever. Am. J. Publ. Health. 1951;43:1327–1330. doi: 10.2105/ajph.43.10.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takala A., Lahdevirta J., Jansson S., Vapalahti O., Orpana A., Karonen S., Repo H. Systemic inflammation in hemorrhagic fever with renal syndrome correlates with hypotension and thrombocytopenia but not with renal injury. J. Infect. Dis. 2000;181:1964–1970. doi: 10.1086/315522. [DOI] [PubMed] [Google Scholar]
- Zhang X.L., Wong X.H., Liu C.Z., Jin W.E., Xiong K.J., Luo D.D. Detection of viral antigens in various organs in 14 fatal cases of epidemic hemorrhagic fever. J. Intern. Med. 1987;26:461–463. [PubMed] [Google Scholar]
- Zhang T.M., Yang Z.Q., Zhong M.Y., Hu Z.J., Hiang J.M., Huggins J.W., Cosgriff T.M., Smith J.I. Early analysis of viremia and clinical tests in patients with epidemic hemorrhagic fever. Chin. Med. J. 1993;106:608–610. [PubMed] [Google Scholar]


