Abstract
A polysaccharide microarray platform was prepared by immobilizing Burkholderia pseudomallei and Burkholderia mallei polysaccharides. This polysaccharide array was tested with success for detecting B. pseudomallei and B. mallei serum (human and animal) antibodies. The advantages of this microarray technology over the current serodiagnosis of the above bacterial infections were discussed.
Keywords: Polysaccharide microarrays, Burkholderia pseudomallei, Burkholderia mallei, Glanders, Melioidosis
1. Introduction
There has been a great deal of emphasis on the development of DNA and protein microarrays recently (Dietrich, 2003, Schweiter et al., 2003). However, DNA and protein microarrays fail to address glycosylation, which is a posttranslational modification. Many Gram-negative bacteria contain structurally unique polysaccharides, namely, capsular polysaccharide and lipopolysaccharide (LPS) O-antigen, that are often pathogen specific (Raetz and Whitfield, 2002). In other words, these polysaccharides are “signature polysaccharides” of their respective bacteria. It is possible to immobilize microbial polysaccharides on glass slides for use as microarrays. Sera from infected or immunized animals or humans could be used to bind to the arrays. Polysaccharide microarray technology can be used as a novel approach for the diagnosis of bacterial infections (Feizi et al., 2003, Hirabayashi, 2002, Feizi and Mulloy, 2003, Love and Seeberger, 2004, Thirumalpura et al., 2005, Blixt et al., 2004, Willats et al., 2002). Indeed, the employment of carbohydrate microarrays using immobilized microbial polysaccharides (from Klebsiella—type 7, K11, K13, K21), Pneumococcus (type C-type VII, type XIV), meningococcus group B, Haemophilus influenzae type A, and Escherichia coli K92 has been demonstrated recently to diagnose microbial infections (Wang et al., 2002). The application of glycan arrays for the identification of immunologic targets for the viral pathogen severe acute respiratory syndrome coronavirus was also reported (Wang and Lu, 2004). Therefore, carbohydrate and polysaccharide microarrays are emerging technologies that are promising alternatives to DNA and protein microarrays.
In the present study, we generated polysaccharide microarrays by surface immobilization onto glass slides using the polysaccharides derived from Burkholderia pseudomallei and Burkholderia mallei and then probing with antisera containing antibodies specific for a capsular polysaccharide common to both pathogens. B. pseudomallei and B. mallei infections are known as melioidosis and glanders, respectively (Cheng and Currie, 2005, Waag and DeShazer, 2004, Woods et al., 1999). Melioidosis is endemic primarily in Southeast Asia and Northern Australia. Glanders is naturally found in equines, which occasionally transmit the infection to humans. Both B. mallei and B. pseudomallei are Centers for Disease Control and Prevention (CDC) category B biothreat agents (Rotz et al., 2002). The polysaccharide microarray described in this study was successfully used to detect anticapsule antibodies in the serum of a rabbit immunized with purified B. pseudomallei capsular polysaccharide and in the convalescent serum from a human infected with B. mallei (Srinivasan et al., 2001). The application of this array technology could be extended to the diagnosis of other Gram-negative bacterial infections.
1.1. Bacterial strains and growth conditions
The bacterial strains used in this study were B. pseudomallei 1026b (DeShazer et al., 1997), B. pseudomallei 576 (Atkins et al., 2002a), B. pseudomallei SRM117 (DeShazer et al., 1998), B. mallei ATCC 23344. All strains produce a common capsular polysaccharide, but B. pseudomallei 576 produces an atypical LPS O-antigen (Atkins et al., 2002b), and B. pseudomallei SRM117 is an LPS O-antigen mutant. B. pseudomallei strains were grown at 37 °C on Luria–Bertani (LB) agar (Lennox, St. Louis, MO) or in LB broth (Lennox), and B. mallei strain was grown at 37 °C on LB agar or in LB broth containing 4% glycerol. Under these culture conditions, both B. pseudomallei and B. mallei had been shown (Burtnick et al., 2002) to produce capsular polysaccharide and LPS.
1.2. Polysaccharide isolation
Polysaccharides (capsular polysaccharide and LPS) were extracted from the bacterial cell pellet by hot phenol extraction method and purified after digestion with DNase, RNase, and proteinase K digestion essentially by the methods described previously (Burtnick et al., 2002, Brett and Woods, 1996). The isolated polysaccharides were hydrolyzed (2% acetic acid, 100 °C, 2 h) to release the lipid A moiety, which was removed by centrifugal filtration (Amicon centrifugal device MW cutoff 5K).
1.3. Polyclonal antibody and human serum
The polyclonal rabbit antibody raised against B. pseudomallei capsular polysaccharide–flagellin protein conjugate was kindly provided by D.E. Woods, Calgary, Alberta, Canada. The details of the preparation and specificity of this antibody were previously published (Reckseidler et al., 2001). Human convalescent serum was collected from an individual after an accidental laboratory exposure to B. mallei and presented with clinical symptoms of glanders infection (Srinivasan et al., 2001). Normal preinfection serum was also collected. The time of collection of serum after exposure is approximately 2 months. A minimal risk protocol to collect the blood sample was approved by the institutional review board at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) (Human Use Committee HP 06-02). The donor was provided with informed consent and met the eligibility criteria.
1.4. Polysaccharide microarray
The polysaccharides were converted to glycosylamines in the presence of ammonium acetate by reductive amination (Spiro and Spiro, 1992). Briefly, to the dry polysaccharides in Reacti-Vials (Pierce, Rockford, IL), 50 μL of 0.3 mol/L sodium cyanoborohydride in 2 mol/L ammonium acetate, pH 6.0, was added, and capped vials were incubated at 105 °C for 4 h. Distilled deionized water (100 μL) and 40 μL of 6 mol/L formic acid were added, and the contents were dried in the Speed Vac at 45 °C. Ammonium acetate in the reaction mixture was removed by addition of methanol (0.5 mL) 3 times followed by repeated drying in the Speed Vac at 45 °C. The glycosylamine derivatives of the polysaccharides were reconstituted in 1.0 mL distilled deionized water. The neutral sugar contents of the polysaccharides were estimated by phenol–sulfuric acid method in microplate format (Masuko et al., 2005) using l-rhamnose as the standard. Glycosylamine polysaccharides were printed on glass slides (Super Epoxy in 16-wells, NUNC, Rochester, NY) using a robotic microarrayer (VIRTEK,Chip Writer Pro, Bio-Rad, Hercules, CA). Custom printing was carried out by Kam Tek, Gaithersburg, MD. The polysaccharides were reconstituted in Tris-buffered saline (TBS) (25 mmol/L Tris, 0.15 mol/L NaCl, pH 7.2) and arrayed at 6 different dilutions in triplicates. The original concentrations of polysaccharides from ATCC 23344, SRM117, 1026b, and 576 (micromoles of rhamnose equivalents per milliliter) were 3.6, 16.0, 3.6, and 3.5, respectively. We also used inulin (Sigma) as a negative control (2.8 μmol glucose equivalents per milliliter). The slides were blocked with 200 μL of 2% (wt/vol) bovine serum albumin (Sigma, St. Louis, MO) in TBS for 1 h at room temperature. After 1 h of incubation at room temperature, with 100 μL of a 1:1000 dilution of rabbit polyclonal serum (specific for B. pseudomallei capsular polysaccharide) in TBS, the slides were washed 3 times with TBS containing 0.1% Tween 20 at 5 min intervals. Serum from a case of human glanders was also used, but at a dilution of 1:5000 in TBS. Cy3- and Cy5-labeled antirabbit IgG (H + L) secondary antibodies were purchased from Amersham Biosciences (Piscataway, NJ). Antihuman IgG (H + L) (KPL, Gaithersburg, MD) secondary antibody was labeled with Cy3 and Cy5 bifunctional NHS (N-hydroxysuccinimide) ester dyes using Amersham Biosciences kit. The secondary antibodies were used at a 1:1000 dilution in TBS. After washing, the slides were scanned for fluorescence at 635 nm (Cy3) and at 532 nm (Cy5) with a Gene Pix 4000B Axon Scanner, using the software Gene Pix Pro 5.1.
The general scheme of approach of polysaccharide microarray is outlined in Fig. 1 . A mixture of capsular polysaccharides and O-antigen saccharides was isolated from different bacterial strains including ATCC 23344, 1026b, and 576. SRM117 is an LPS mutant that produces capsular polysaccharide but not O-antigen saccharides. The presence of capsular polysaccharide in these polysaccharide preparations was confirmed by Western blotting (diagram not shown) using a polyclonal antibody specific for the capsular polysaccharide (Burtnick et al. 2002). The polysaccharides were converted to glycosylamines by reductive amination with sodium cyanoborohydride in the presence of ammonium acetate. To investigate whether immobilized polysaccharide macromolecules preserve their antigenic determinants, we printed polysaccharide (capsular polysaccharide and LPS O-antigens) preparations from different strains of B. mallei and B. pseudomallei on glass slides. The slides were probed with a polyclonal antibody specific to capsular polysaccharide. Both B. mallei and B. pseudomallei are encapsulated with a polysaccharide of the same structure. The capsular polysaccharide is a homopolymer of 1,3-linked 2-O-acetyl-6-deoxy-β-d manno-heptopyranose-(1 (Perry et al., 1995, Knirel et al., 1992). All the strains used in the study had been shown to contain this capsular polysaccharide (Atkins et al., 2002a, DeShazer et al., 2001, Reckseidler et al., 2001, DeShazer et al., 1998). It is apparent that the immunoreactivity of this polysaccharide is preserved even after surface immobilization, as evidenced by their recognition and reactivity to the antibody specific for the capsular polysaccharide (Fig. 2 ). It is not clear why this antibody gave weaker signal against the polysaccharide derived from 576 as compared with the other strains. As expected, the rabbit antiserum did not react with inulin, the polysaccharide used as a negative control.
Fig. 1.
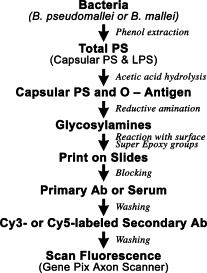
Flow chart of the generation of Burkholderia polysaccharide microarray.
Fig. 2.
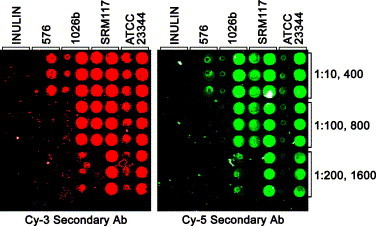
Immunoreactivity of Burkholderia polysaccharide microarray with polyclonal rabbit antiserum raised against purified B. pseudomallei capsular polysaccharide. The concentrations of polysaccharides were in decreasing order in triplicates: 1:10, 1:100, and 1:200 (right lanes); 1:400, 1:800, and 1:1600 (left lanes). Cy3- and Cy5-labeled secondary antibodies were reacted with the microarrays as described in the text. No positive spots were seen (diagram not shown) on probing with normal serum.
Furthermore, using this microarray, we are able to detect capsular polysaccharide antibodies in the serum of a human patient (Srinivasan et al., 2001) exposed to B. mallei infection. Although these antibodies were present in the convalescent serum, they were absent in preinfection serum from the same patient (Fig. 3 ). Possibly, the glanders patient serum also contains antibodies against LPS O-antigens, but this requires further investigation.
Fig. 3.
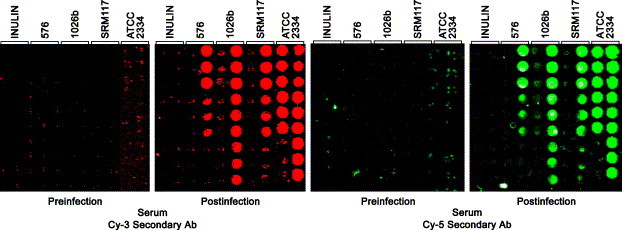
Typical Immunoreactivity of Burkholderia polysaccharide microarray with the serum of a human glanders patient. The microarrays were reacted with preinfection and postinfection sera from a human glanders patient at 1:5000 dilution. Cy3- and Cy5-labeled secondary antibody was reacted with the microarrays as described in the text. Immunoreactivity was also seen at 1:10.000 and 1:40 000 dilutions as well (diagram not shown).
In the present study, we are able to demonstrate the usefulness of polysaccharide microarray technology for the detection of serum antibodies against B. mallei and B. pseudomallei. An indirect hemagglutination and a complement fixation (CF) test had been the routine procedure for the serologic diagnosis of human melioidosis caused by B. pseudomallei infection (Alexander et al., 1970, Wuthiekanun et al., 2006). B. mallei infections (glanders) in horses had been serologically diagnosed employing CF test (Marek and Manninger, 1945). Both indirect hemagglutination and CF tests are based on crude whole-cell preparation or extracts of the bacteria, and therefore, the potential for false-positive serodiagnosis cannot be ruled out (Marek and Manninger, 1945, Wernery et al., 2004, Wernery et al., 2005). Neubauer et al. (2005) suggested the importance of serologic tests using well-characterized antigens in the place of crude bacterial preparations to avoid the diagnosis of false positives. In the present study, we used well-characterized antigens (capsular polysaccharide and O-antigen saccharides) in the microarray, and this should circumvent the problems of false positives in future serodiagnosis of B. mallei and B. pseudomallei infections.
Acknowledgments
We thank R. Barrais for technical assistance. The research described herein was sponsored by the U.S. Army Medical Research and Materiel Command under Project 05-4-2P-002. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
References
- Alexander A.D., Huxsoll D.L., Warner A.R., Shelper V., Dorsey A. Serological diagnosis of human melioidosis with indirect hemagglutination and complement fixation tests. Appl. Microbiol. 1970;20:825–833. doi: 10.1128/am.20.5.825-833.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins T., Prior R., Mack K., Russell P., Nelson M., Prior J., Ellis J., Oyston P.C., Dougan G., Titball R.W. Characterization of an acapsular mutant of Burkholderia pseudomallei identified by signature tagged mutagenesis. J. Med. Microbiol. 2002;51:539–547. doi: 10.1099/0022-1317-51-7-539. [DOI] [PubMed] [Google Scholar]
- Atkins T., Prior R.G., Mack K., Russell P., Nelson M., Oyston P.C., Dougan G., Titball R.W. A mutant of Burkholderia pseudomallei, auxotrophic in the branched chain amino acid biosynthetic pathway, is attenuated and protective in a murine model of melioidosis. Infect. Immun. 2002;70:5290–5294. doi: 10.1128/IAI.70.9.5290-5294.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blixt O., Head S., Mondala T., Scanlan C., Huflejt M.E., Alvarez R., Bryan M.C., Fazio F., Calarese D., Stevens J., Razi N., Stevens D.J., Skehel J.J., van Die I., Burton D.R., Wilson I.A., Cummings R., Bovin N., Wong C.H., Paulson J.C. Printed covalent glycan array for ligand profiling of diverse gleeman binding proteins. Proc. Natl. Acad. Sci. U. S. A. 2004;101:17033–17038. doi: 10.1073/pnas.0407902101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett P.J., Woods D.E. Structural and immunological characterization of Burkholderia pseudomallei O-polysaccharide-flagellin protein conjugates. Infect. Immun. 1996;64:2824–2828. doi: 10.1128/iai.64.7.2824-2828.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burtnick M.N., Brett P.J., Woods D.E. Molecular and physical characterization of Burkholderia mallei O-antigens. J. Bacteriol. 2002;184:849–852. doi: 10.1128/JB.184.3.849-852.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng A.C., Currie B.J. Melioidosis: epidemiology, pathophysiology, and management. Clin. Microbiol. Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeShazer D., Brett P.J., Carlyon R., Woods D.E. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J. Bacteriol. 1997;179:2116–2125. doi: 10.1128/jb.179.7.2116-2125.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeShazer D., Brett P.J., Woods D.E. The type II O-antigenic polysaccharide moiety of Burkholderia pseudomallei lipopolysaccharide is required for serum resistance and virulence. Mol. Microbiol. 1998;30:1081–1100. doi: 10.1046/j.1365-2958.1998.01139.x. [DOI] [PubMed] [Google Scholar]
- DeShazer D., Waag D.M., Fritz D.L., Woods D.E. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 2001;30:253–269. doi: 10.1006/mpat.2000.0430. [DOI] [PubMed] [Google Scholar]
- Dietrich G. DNA microarrays in vaccine research. Curr. Opin. Mol. Ther. 2003;5:575–583. [PubMed] [Google Scholar]
- Feizi T., Mulloy B. Carbohydrates and glycoconjugates. Glycomics: the new era of carbohydrate biology. Curr. Opin. Struct. Biol. 2003;13:601–604. doi: 10.1016/j.sbi.2003.09.001. [DOI] [PubMed] [Google Scholar]
- Feizi T., Fazio F., Chai W., Wong C.H. Carbohydrate microarrays—a new set of technologies at the frontiers of glycomics. Curr. Opin. Struct. Biol. 2003;13:637–645. doi: 10.1016/j.sbi.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Hirabayashi J. Oligosaccharide microarrays for glycomics. Trends Biotechnol. 2002;21:141–143. doi: 10.1016/S0167-7799(03)00002-7. [DOI] [PubMed] [Google Scholar]
- Knirel Y.A., Paramonov N.A., Shashkov A.S., Kochetkov N.K., Yarullin R.G., Farber S.M., Efremenko V.I. Structure of the polysaccharide chains of Pseudomonas pseudomallei lipopolysaccharides. Carbohydr. Res. 1992;233:185–193. doi: 10.1016/s0008-6215(00)90930-3. [DOI] [PubMed] [Google Scholar]
- Love K.R., Seeberger P.H. Carbohydrate arrays as tools for glycomics. Angew. Chem. Int. Ed. Engl. 2004;19:3583–3586. doi: 10.1002/1521-3773(20021004)41:19<3583::AID-ANIE3583>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Marek J., Manninger R. Spezielle Pathologie und Therapie der Haustiere. 9th ed. Gustav Fischer; Jena (Germany): 1945. Rotzkrankheit: malleus; pp. 591–627. [Google Scholar]
- Masuko T., Minami A., Iwasaki N., Majima T., Nishimura S.-I., Lee Y.C. Carbohydrate analysis by a phenol–sulfuric acid method in a microplate format. Anal. Biochem. 2005;339:69–72. doi: 10.1016/j.ab.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Neubauer H., Sprague L.D., Zachria R., Tomaso H., Dahouk S.A., Werney R., Werney U., Scholz H.C. Serodiagnosis of Burkholderia mallei infections in horses: state-of-the-art and perspectives. J. Vet. Med., Ser. B. 2005;52:201–205. doi: 10.1111/j.1439-0450.2005.00855.x. [DOI] [PubMed] [Google Scholar]
- Perry M.B., MacLean L.L., Schollardt T., Bryan L.E., Ho M. Structural characterization of the lipopolysaccharide O-antigens of Burkholderia pseudomallei. Infect. Immun. 1995;63:3348–3352. doi: 10.1128/iai.63.9.3348-3352.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raetz C.R., Whitfield C. Lipopolysaccharide endotoxins. Annu. Rev. Biochem. 2002;71:635–700. doi: 10.1146/annurev.biochem.71.110601.135414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckseidler L.D., DeShazer D., Sokol P.A., Woods D.E. Detection of bacterial virulence genes by subtractive hybridization: identification of capsular polysaccharide of Burkholderia pseudomallei as a major virulence determinant. Infect. Immun. 2001;69:34–44. doi: 10.1128/IAI.69.1.34-44.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotz L.D., Khan A.S., Lillibridge S.R., Ostroff S.M., Hughes J.M. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 2002;8:225–230. doi: 10.3201/eid0802.010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweiter B., Predki P., Snyder M. Microarrays to characterize protein interactions on a whole-proteome scale. Proteomics. 2003;3:2190–2199. doi: 10.1002/pmic.200300610. [DOI] [PubMed] [Google Scholar]
- Spiro M.J., Spiro R.G. Monosaccharide determination of glycoconjugates by reverse-phase high-performance liquid chromatography of their phenylthiocarbamyl derivatives. Anal. Biochem. 1992;204:152–157. doi: 10.1016/0003-2697(92)90155-z. [DOI] [PubMed] [Google Scholar]
- Srinivasan A., Kraus C.N., DeShazer D., Becker P.M., Dick J.D., Spacek L., Bartlett J.G., Byrne W.R., Thomas D.L. Glanders in a military research microbiologist. N. Engl. J. Med. 2001;345:256–258. doi: 10.1056/NEJM200107263450404. [DOI] [PubMed] [Google Scholar]
- Thirumalpura N.R., Mortan R.J., Ramachandran A., Malayer J.R. Lipopolysaccharide microarrays for detection of antibodies. J. Immunol. Methods. 2005;298:73–81. doi: 10.1016/j.jim.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Waag D.M., DeShazer D. Glanders: new insights into an old disease. In: Linder L.E., Lebeda F.J., Korch G., editors. Biological Weapons Defense: Infectious Diseases and Counterbioterrorism. Humana Press Inc; Totowa (NJ): 2004. pp. 209–237. [Google Scholar]
- Wang D., Lu J. Glycan arrays lead to the discovery of autoimmunogenic activity of SARS-CoV. Physiol. Genomics. 2004;18:245–248. doi: 10.1152/physiolgenomics.00102.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Liu S., Trummer B.J., Deng C., Wang A. Carbohydrate microarrays for the recognition of cross-reactive molecular markers of microbes and host cells. Nat. Biotechnol. 2002;20:275–281. doi: 10.1038/nbt0302-275. [DOI] [PubMed] [Google Scholar]
- Wernery U., Kinne J., Morton T. Central Veterinary Research Laboratory; Dubai (United Arab Emirates): 2004. Pictorial guide to the diagnosis of equine glanders. CVRI Brocure 2004. [Google Scholar]
- Wernery U., Zacharia R., Wernery R., Joseph S., Valsini L. Proceedings of the 15th International Conference of Racing Analysis and Veterinarians, Dubai, United Arab Emirates. 2005. Ten years of freedom from notifiable equine diseases in the United Arab Emirates; pp. 1–4. [Google Scholar]
- Willats W.G.T., Rasmussen S.E., Kristensen T., Mikkeisen J.G., Knox J.P. Sugar-coated microarrays: a novel slide surface for high-throughput analysis of glycans. Proteomics. 2002;2:1666–1771. doi: 10.1002/1615-9861(200212)2:12<1666::AID-PROT1666>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Woods D.E., DeShazer D., Moore R.A., Brett P.J., Burtnick M.N., Reckseidler S.L., Senkiw M.D. Current studies on the pathogenesis of melioidosis. Microbes. Infect. 1999;2:157–162. doi: 10.1016/s1286-4579(99)80007-0. [DOI] [PubMed] [Google Scholar]
- Wuthiekanun W., Chierakul W., Rattanalertnavee J., Langa S., Sirodom D., Wattanawaitunechi C., Winothai W., White N.J., Day N., Peacock S.J. Serological evidence for increased human exposure to Burkholderia pseudomallei following the Tsunami in Southern Thailand. J. Clin. Microbiol. 2006;44:239–240. doi: 10.1128/JCM.44.1.239-240.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]


