Abstract
Fever in ill travelers returning home from developing nations is common. Most travelers present with undifferentiated febrile syndromes. Regional proportionate morbidity rates and patients’ travel histories are essential in narrowing the differential diagnosis. Most patients in whom a diagnosis is confirmed have malaria, dengue fever, enteric fever, or rickettsial disease. Empiric treatment based on the clinical presentation is required in many cases, because acquisition of confirmatory laboratory data is often delayed. The focus of this article is travel-related illness that falls within the spectrum of the acute febrile syndrome.
Keywords: Fever, International travel, Imported infectious disease, Tropical disease
Key points
-
•
Fever in ill travelers returning home from developing nations is common.
-
•
Most travelers present with undifferentiated febrile syndromes. Regional proportionate morbidity rates and the patient’s travel history are essential in narrowing the differential diagnosis.
-
•
Most patients in whom a diagnosis is confirmed have malaria, dengue, enteric fever, or rickettsial disease.
-
•
Empiric treatment based on the clinical presentation is required in many cases because acquisition of confirmatory laboratory data is often delayed.
Introduction
Worldwide, more than 940 million international journeys were undertaken in 2010.1 Global travel on such a scale exposes individuals to a range of health risks and poses a challenge to clinicians caring for patients who return home ill from international travel. Of the more than 80 million people who travel from industrialized to developing nations, between 20% and 70% report some illness associated with their travel.2, 3, 4 A small proportion, between 5% and 19%, of those who develop a travel-associated illness seek medical attention either during or immediately after travel.3, 4, 5, 6, 7 Mortality in this population is low (1 per 100,000) but the associated morbidity is significant, with high rates of hospitalization and missed work for what is largely a preventable spectrum of disease.
Much of the current epidemiologic understanding of travel-associated illness in developed nations is based on data acquired through surveillance systems such as GeoSentinel (a system of the International Society of Travel Medicine and the Centers for Disease Control and Prevention [CDC]) and TropNet Europe (the European Network on Imported Infectious Disease Surveillance). GeoSentinel sites are located on 6 continents and collect clinician-based surveillance data on travel-associated disease from more than 30 locations. TropNet Europe has 68 member sites, which contribute surveillance data for travel-associated illness in Europe. A case definition for travel-associated illness is a patient has who crossed an international border within the past 10 years and presents for a presumed travel-related illness.5 This definition encompasses a very broad set of clinical conditions, including dermatologic disease, injury, tuberculosis, and chronic diarrhea. The focus of this article is on travel-related illness that falls within the spectrum of the acute febrile syndrome.
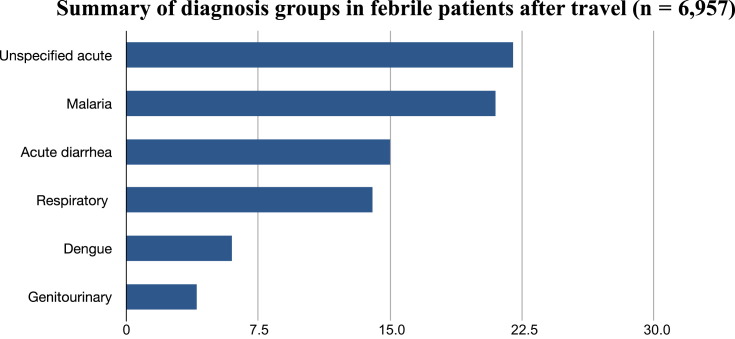
Fever was the chief complaint of 6957 (28%) of the 24,920 ill travelers who were treated in GeoSentinel sites between 1997 and 2006.8 These patients visited clinics in Europe (53%), North America (25%), Israel (9%), Australia/New Zealand (8%), Asia (5%), and other sites (1%), and one-fourth of them were hospitalized.8 Their characteristics are summarized in Table 1 . Most patients in this group were middle-aged men, and most people in the study group had traveled for tourism, on business, or to visit friends and relatives. These individuals (those visiting friends and relatives) constitute a high-risk group because they are much less likely than tourist travelers to receive prophylaxis, and tend to use fewer preventive measures. Consequently they are almost 9 times more likely than other groups to require inpatient treatment when they return with febrile complications of travel.9 Most individuals with fever after travel present within 1 to 3 weeks after returning home. These presentations, considered acute and subacute, are within the direct purview of the emergency medicine specialist. Among those in whom a definitive diagnosis is reached the majority have malaria, acute diarrheal disease, acute respiratory tract infections, or dengue fever (Fig. 1 ).8 More than 35% of patients presenting with a febrile syndrome after travel do not receive a definitive diagnosis, even in the hands of trained experts, which highlights the importance of a structured diagnostic approach.
Table 1.
Characteristics of returned ill travelers with fever: GeoSentinel Surveillance Network
| Characteristic | Number (%) |
|---|---|
| Age (y) | |
| <20 | 429 (6) |
| 20–64 | 6230 (89) |
| ≥65 | 244 (4) |
| Sex | |
| Male | 3995 (57) |
| Female | 2891 (43) |
| Reason for Travel | |
| Tourism | 3802 (55) |
| Business | 1036 (15) |
| Research/education | 283 (4) |
| Missionary/volunteer | 384 (6) |
| Visiting friends and relatives | 1431 (21) |
| Duration of Travel (d) | |
| ≤30 | 4134 (59) |
| ≥31 | 2597 (41) |
| Interval from Travel to Presentation (wk) | |
| <1 | 2789 (40) |
| 1–6 | 2437 (36) |
| >6 | 1551 (22) |
| Total | 6957 |
Data from Wilson ME, Weld LH, Boggild A, et al. Fever in returned travelers: results from the GeoSentinel Surveillance Network. Clin Infect Dis 2007;44(12):1560–8.
Fig. 1.
Summary of diagnosis groups in returned ill travelers with fever (N = 6957). GeoSentinel Surveillance Network.
(Data from Wilson ME, Weld LH, Boggild A, et al. Fever in returned travelers: results from the GeoSentinel Surveillance Network. Clin Infect Dis 2007;44(12):1560–8.)
One of the key principles in approaching the presentation of fever in the returning traveler is a thorough understanding of epidemiology as it applies to the individual’s circumstances. Most patients present with undifferentiated and nonlocalizing systemic febrile syndromes, so the clinical decision-making process and the diagnostic algorithm should reflect the likelihood of acquiring a specific disease based on regional morbidity, host-pathogen interaction, and the clinical assessment. Accordingly, the following 3 key areas are discussed in the next section of this review:
-
1.
Destination-specific variations in proportionate morbidity. What are the most common/likely infections that someone can bring home from a given region?
-
2.
Assessment of travel history, with emphasis on exposure, incubation period, and vaccination/chemoprophylaxis. What did the patient do/not do that might put him or her at risk for a certain infection? Does the course of illness fit with the expected incubation period for that infection?
-
3.
Clinical presentation. What patterns of the fever and other signs/symptoms point toward or rule out a diagnosis?
Destination-specific variations in proportionate morbidity
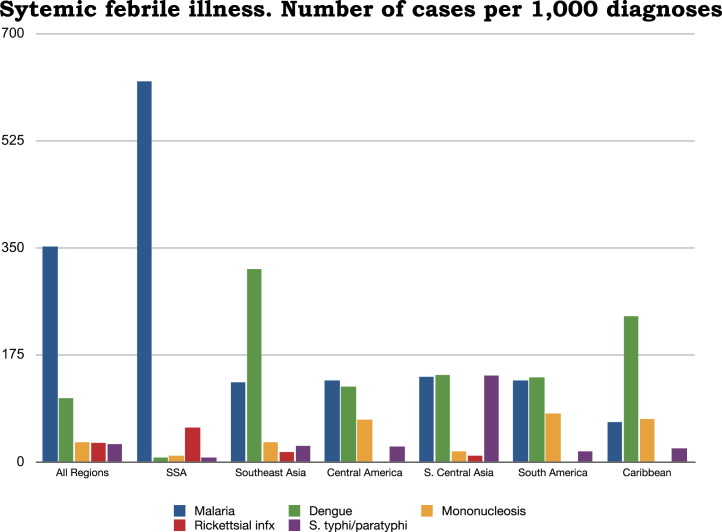
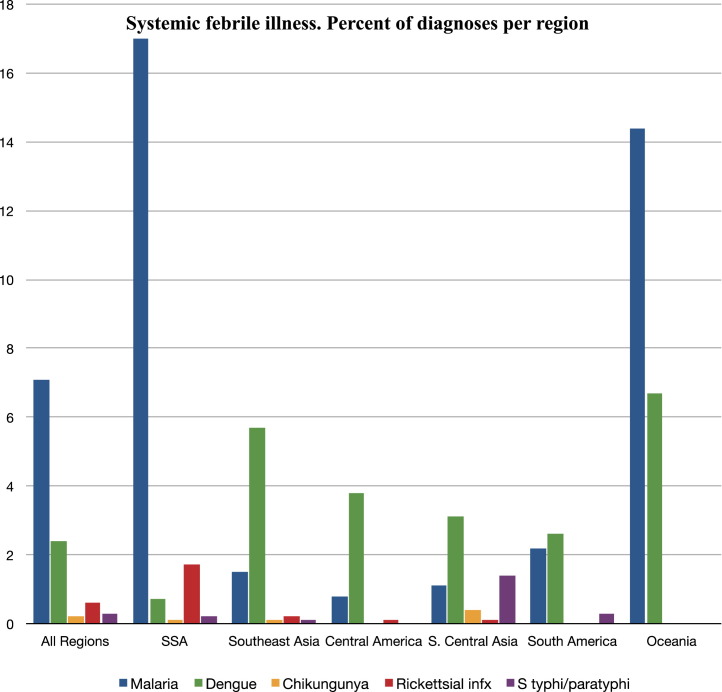
Arguably the most important feature to consider in the initial assessment is the region of travel. Several diagnoses, and their empiric therapies, can be guided by an understanding of regional risk.10 GeoSentinel data, collected from 17,353 patients who traveled to 230 countries between June 1996 and August 2004, demonstrate significant regional differences in proportionate morbidity for 16 of 21 broad syndromic categories, including systemic febrile syndrome.5 In the context of systemic febrile illness, destination-specific variations in proportionate morbidity are stark (Fig. 2 ). Proportionate morbidity rates for malaria and enteric fever are regionally disparate, whereas dengue fever has a fairly broad global distribution. EuroTravelNet data from 17,228 patients show similar patterns of distribution (Fig. 3 ).11 Data from 1842 febrile returned travelers in Belgium demonstrated that 91% of all imported malaria cases were from sub-Saharan Africa, all cases of enteric fever were from Asia, and dengue was nearly evenly split between Asia and the Americas.12 Data from Australia found 6-fold higher rates of malaria in itineraries that included Africa, 13-fold increases in dengue for itineraries that included Asia, and high rates of malaria among visitors to Oceania.13, 14 Although a thorough understanding of destination-specific proportionate morbidity rates is important, other considerations must be incorporated into the assessment process. Generally speaking, geographic trends correlate with the diagnosis in roughly one-third of febrile patients returning from developing nations; the other two-thirds have undifferentiated fever and other diagnoses.
Fig. 2.
Infectious cases of malaria, dengue, mononucleosis, rickettsial disease, and enteric fever per 1000 diagnoses by region. GeoSentinel Surveillance Network. SSA, sub-Saharan Africa.
(Adapted from Freedman DO, Weld LH, Kozarsky PE, et al. Spectrum of disease and relation to place of exposure among ill returned travelers. N Engl J Med 2006;354(2):119–30; with permission.)
Fig. 3.
Infectious cases of malaria, dengue, Chikungunya, rickettsial disease, and enteric fever percentage per region. EuroTravelNet. SSA, sub-Saharan Africa.
(Adapted from Gautret P, Schlagenhauf P, Gaudart J, et al. Multicenter EuroTravNet/GeoSentinel study of travel-related infectious diseases in Europe. Emerg Infect Dis 2009;15(11):1783–90.)
Assessment of travel history
The importance of obtaining a detailed travel history cannot be overstated in the evaluation of the febrile traveler. Determination of possible infectious exposures and their associated incubation periods can be particularly helpful in ruling out causes of fever. For example, a fever that began more than 3 weeks after a traveler returned home is very unlikely to be caused by dengue, rickettsial disease, or viral hemorrhagic fever; it is much more likely to be caused by malaria (particularly the forms caused by Plasmodium vivax or Plasmodium ovale) if the infection was acquired abroad. Careful attention to the exposure history, immunization status, and use of malarial chemoprophylaxis can be very helpful in establishing a diagnosis. In a series of 2071 fever episodes from 1962 patients in Europe, the majority (78%) presented within 1 month after return from travel.15 GeoSentinel data for 6957 patients presenting with fever found that after malaria, the most common specific infections causing systemic febrile illness were dengue, enteric fever, and rickettsioses, all of which have short to medium incubation periods (<21 days).8 Incubation periods for common infectious agents are presented in Table 2 . Whereas most infections in travelers have incubation periods of less than 21 days, several can manifest more than 30 days after return (eg, malaria, tuberculosis, hepatitis, filariasis). Furthermore, patients might spend several weeks to months overseas and then present within a short time after returning home with infections that were acquired months earlier. The most common infection presenting more than 30 days after exposure is P vivax malaria (25% of patients with this infection in the United States present after 30 days).16
Table 2.
Incubation periods for common and severe infections acquired during travel
| Short (<10 d) | Medium (11–21 d) | Long (>30 d) |
|---|---|---|
| Typhoid | Malaria | Reactivation malaria |
| Dengue | Typhoid | Tuberculosis |
| Rickettsial | Hepatitis A | Leishmaniasis |
| Meningitis/encephalitis | Schistosomiasis | Filariasis |
| Chikungunya | Amebic liver abscess | Schistosomiasis |
| Salmonellosis | Leptospirosis | Rabies |
| Shigellosis | Q-fever | African trypanosomiasis |
| VHF | African trypanosomiasis | Enteric protozoal |
| Influenza | Brucellosis | Enteric helminthic |
| Legionella | VHF | |
| Mononucleosis | Rickettsial | |
| HIV Seroconversion |
Abbreviations: HIV, human immunodeficiency virus; VHF, viral hemorrhagic fever.
The emergency physician who is evaluating a traveler with a febrile illness should inquire about the following topics:
-
•
Details of itinerary/travel dates/seasonality
-
•
Countries and destinations (rural/urban locations) visited
-
•
Exposure to bites/vectors/animals
-
•
Types of food and water that were consumed
-
•
Vaccination and chemoprophylaxis history
-
•
Unprotected intercourse and partners
-
•
Timing and sequence of illness/symptoms
Once an appropriate travel history is obtained, this information, in conjunction with a destination-specific assessment of risk, can be used to formulate a fairly narrow differential diagnosis, which can then be applied to the clinical presentation. Of importance is that although exotic infectious agents are often the focus of interest, nonexotic infectious processes, such as pneumonia, urinary tract infection, and unspecified viral syndromes, are more common than exotic ones and must remain high on the differential diagnosis.17
Clinical presentation
Because the vast majority (close to 80%) of travelers with fever seeks medical care within 1 month after return, this discussion focuses primarily on presentations that are likely to be seen within this time frame.15 In nearly 20% of patients fever is the only symptom, and more than 50% of patients have noncontributory findings on physical examination.15 When associated symptoms are present, they are often nonlocalizing and tend to represent manifestations of systemic disease (eg, headache, fatigue, myalgia). Fever associated with genitourinary, respiratory, and gastrointestinal symptoms should focus on the diagnostic pathway; these combinations rarely pose a major diagnostic challenge. The following sections focus on recognizable fever with concomitant complexes of signs and symptoms, and their associated diagnostic considerations, in patients returning from the tropics.
Fever and Rash
Fever and rash should prompt an urgent and cautionary assessment, as several rare but potentially life-threatening diagnoses are possible. Patients with this combination should undergo respiratory and droplet-isolation precautions until a diagnosis is confirmed. A list of rash characteristics and their associated diagnoses are presented in Table 3 . This list is by no means comprehensive, but does highlight the more common and relevant syndromes presenting with fever and rash in returned travelers. Several nonemergent tropical infections can present with dermatologic manifestations; the absence of an associated acute systemic febrile syndrome usually suggests an indolent process. The majority of patients with fever and rash after travel to the tropics should be admitted to hospital for observation and confirmatory diagnosis of causes, which often take time to isolate via culture or serology.
Table 3.
Infectious causes of fever and rash based on rash type
| Rash | Infection |
|---|---|
| Purpuric | Dengue hemorrhagic syndrome |
| Meningococcal infection | |
| Viral hemorrhagic fever | |
| Rickettsial infection, severe | |
| Leptospirosis | |
| Maculopapular | Arboviral infection |
| Rickettsial infection | |
| VHF | |
| HIV seroconversion | |
| Typhoid | |
| Dengue fever | |
| Leptospirosis | |
| Brucellosis | |
| Vesicular | Herpes simplex virus |
| Varicella | |
| Ulcerative | Chancre: trypanosomiasis |
| Eschar: anthrax, African tick typhus | |
| Ulcer: leishmaniasis, syphilis, tropical ulcer |
Fever and Jaundice
The association of the systemic febrile syndrome and jaundice is rare after travel. Its presentation should prompt a cautious investigation that targets common domestic causes such as cholangitis, hepatitis, and severe sepsis. In the context of pathogens that could have been acquired abroad, the viral hepatitides (A–E) rarely present concurrently with fever and jaundice.10
Common infectious causes of fever and jaundice acquired abroad are malaria with hemolysis, leptospirosis (Weil disease), the hemolytic-uremic syndrome (associated with Escherichia coli), enteric fever, and the viral hemorrhagic fevers. Close attention to regional risk and the incubation period is essential, and can help to rule out several of the aforementioned conditions. Patients with fever and jaundice should be admitted to hospital with appropriate contact precautions, pending diagnostic confirmation, for observation and appropriate therapy.
Fever and Central Nervous System Involvement
Neurologic presentations are seen in 15 of 1000 ill travelers. When they are associated with a febrile syndrome, urgent treatment and diagnosis are necessary.5 The most common treatable causes are malaria and meningitis, and these must be ruled out or treated promptly in most cases. All common domestic causes of meningitis should be considered, and treatment should be initiated before confirmatory diagnosis if there is a high index of suspicion for cerebral malaria or bacterial meningitis. Patients traveling within the meningitis belt and pilgrims traveling with the Hajj to Mecca should be treated promptly for meningococcal disease, which carries a 5% to 10% case-fatality rate, even with antibiotic treatment.18 Nonbacterial encephalitis has a broad differential diagnosis, which includes common arboviral infections native to the Americas and Asia, and often requires reference laboratory analysis for confirmation. Other considerations include tuberculosis, opportunistic disease associated with human immunodeficiency virus (HIV) infection, leptospirosis, rabies, and alcohol withdrawal. Lastly, there have been several reports of tourists who acquired trypanosomal infections (African sleeping sickness) transmitted through bites of the tsetse fly in game parks in east and central Africa.19, 20 Central nervous system (CNS) disease is a late presentation of these infections, although fulminant cases of rapidly progressive Trypanosoma gambiense have been described. Suspected trypanosomal disease should prompt expert consultation for diagnosis and treatment.
Fever and Eosinophilia
Peripheral eosinophilia is generally a result of acute allergic reaction, malignancy, or parasitic infection.21 In the context of fever and eosinophilia in the returned traveler, a high index of suspicion for helminthic infections, in which worms migrate or dwell in tissues, should be considered. Whereas mild elevation in the peripheral eosinophil count (351–1500 cells/mL) can be nonspecific, moderate (1500–5000 cells/mL) to severe (>5000 cells/mL) elevations in individuals traveling to nonindustrialized regions are highly suggestive of invasive helminthic infection.21 Diagnoses to be considered in febrile travelers with eosinophilia include the following:
-
•
Schistosomiasis (Katayama fever)
-
•
Strongyloides hyperinfestation
-
•
Lymphatic filariasis
-
•
Invasive hookworm disease
-
•
Migratory Ascaris lumbricoides
Initial workup should include stool analysis for ova and parasites, serology for strongyloidiasis, and examination of blood smears and skin snips to detect microfilariae, depending on the clinical picture and the area of travel.22, 23
Undifferentiated Fever
Febrile patients without localizing symptoms, presenting after travel to nonindustrialized nations, accounted for 23% to 35% of GeoSentinel cases, with similar proportions reported in smaller European and Australian series.5, 8, 15, 24, 25 In returning travelers with undifferentiated fever, malaria (all species) was the cause of disease in 14% to 35% of patients, accounting for the largest proportion of diagnoses.5, 12, 13, 15, 24, 26, 27, 28 When destination-specific morbidity is considered, the proportion of undifferentiated fever diagnosed as malaria in travelers returning from sub-Saharan Africa is 32% to 62%. Therefore, all patients with fever after returning from the tropics, particularly sub-Saharan Africa, should be considered as having malaria until proven otherwise.5, 8, 12, 13, 15 Following malaria, the most common imported communicable diseases causing undifferentiated fever are dengue, enteric fever, and rickettsial disease.
Dengue virus infection is confirmed serologically in 3% to 10% of travelers with undifferentiated fever on return from the tropics.5, 8, 12, 13, 15, 24, 26 In patients returning from Central or South America, dengue virus is the causative agent in 8% to 14%, and in those returning from southeast Asia dengue is responsible for 13% to 32% of cases of undifferentiated fever.5, 8, 13 For enteric fever, pooled data demonstrate Salmonella typhi/paratyphi in 1% to 4% of cases of undifferentiated fever.5, 8, 12, 13, 15, 24, 26 Enteric fever should be considered strongly in travelers returning from south Asia, particularly the Indian subcontinent; travel to pockets of sub-Saharan Africa can also pose a risk. When the diagnosis of malaria has been excluded or if the patient has a rash, a heightened index of suspicion for rickettsial infection should be maintained, particularly in patients returning from sub-Saharan Africa. In this group, up to 5% of patients with undifferentiated fever have been found to harbor rickettsial infection (namely, African tick typhus).15
Although the evaluation and workup of patients with undifferentiated fever after travel can be complex and intimidating, there is room for simplification and an evidence-based approach. Because a large proportion of diagnoses will remain in the scope of “cosmopolitan infections,” a practical approach to the workup of patients with imported disease is warranted. Initial assessment should include evaluation for common local causes of fever. Given that no source will be identified in one-third of patients and that a cosmopolitan cause will be identified also in about one-third of patients, it is the remaining third that is the focus of the imported disease workup. The vast majority of patients (>95%) in whom a causative agent is identified will have malaria, dengue, enteric fever, or rickettsial disease.5, 8, 12, 15, 17 Therefore, a detailed clinical discussion focuses on these 4 essential disease entities and their recognition, diagnosis, and treatment.
Pediatric considerations
Most travel-related morbidity data for children stem from limited single-center studies.29, 30 Analysis of data from 1849 pediatric patients from GeoSentinel surveillance found that children can be grouped into 4 general categories of illness after travel: diarrheal syndrome (28%), dermatologic disorders (25%), systemic febrile illness (23%), and respiratory disorders (11%).31 Children were more likely to require hospitalization, were less likely to receive pretravel advice, and generally presented earlier than adults.31 Of those children with systemic febrile syndromes, the majority (35%) was diagnosed with malaria; the remaining diagnoses were viral syndrome (28%), dengue fever (7%), enteric fever (6%), and unspecified febrile illness (24%).31 For children presenting with undifferentiated fever after travel, a high index of suspicion should be maintained for both cosmopolitan and imported causes. The same geographic considerations as for adults hold true. All evaluations for fever in children returning from the tropics should include consideration of malaria, dengue, and enteric fever. A low threshold for admitting pediatric patients with undifferentiated fever after travel should be maintained.
Malaria
In 2010, the CDC received notification of 1691 cases of malaria, 1688 (99.8%) of which were classified as imported, representing a 14% increase from the 1484 recorded in 2009.32 P falciparum and P vivax represented the majority of infections and were identified in 74% and 18% of cases, respectively.32 These infections occurred primarily in United States nationals (75%), and probably underestimate the total disease burden. Of the 828 patients (76%) who reported a purpose for their travel, the largest proportion (71%) were visiting friends or relatives. At least 56% of all patients were hospitalized and 9 of them died (all cases of severe P falciparum).32 Imported cases of malaria in Europe and the United Kingdom number close to 11,000 per annum, making this one of the principal imported tropical infections.33
In patients returning from travel to malaria-endemic regions, the diagnosis must be excluded in those with a history of fever, regardless of travel duration or use of chemoprophylaxis. Of the several species of Plasmodium that cause disease in humans, 4 are of clinical relevance: P falciparum, P vivax, P ovale, and P malariae. Of these, P falciparum poses the highest risk for severe disease and complications while P vivax constitutes the bulk of chronic and recrudescent disease. Transmission occurs through the bite of the female Anopheles mosquito, with multiple species responsible for transmission. Life cycles involve both hepatic and hematologic stages; the intraerythrocytic stages account for the clinical spectrum of disease. The minimum incubation period for P falciparum is 6 days, with most clinical symptoms developing between 9 and 14 days after exposure (median 12) days.34 Incubation periods for P vivax and P ovale are significantly longer, ranging from 8 days to several months. The majority of cases of P vivax infection present within 2 months after exposure; however, cases of P vivax and P ovale have presented several years after exposure, which likely constitutes disease recrudescence.
No specific signs and symptoms are pathognomonic for malaria. Most patients present with a constellation of fever, myalgia, arthralgia, and headache. Patients present occasionally with concomitant abdominal pain, diarrhea, cough, and dyspnea. Rash and lymphadenopathy are rarely present and are clues to an alternative diagnosis. Roughly 10% to 40% of patients with malaria are afebrile on presentation, and, although textbooks frequently describe tertian and quaternary cyclical fevers, they are rarely seen in practice.35, 36 Adults with severe cases of P falciparum infection may present with renal failure, jaundice, and respiratory failure, including acute respiratory distress syndrome. Children with severe disease typically present with severe anemia, acidosis, and respiratory distress. Both adults and children with severe disease can present with CNS involvement, which carries a 15% to 20% mortality rate and can lead to neurologic sequelae in survivors.34 Patients who present with fever and neurologic findings after returning from the tropics should be evaluated for malaria and meningitis, and treated promptly as warranted.
Laboratory diagnosis of malaria is classically made by examination of Giemsa-stained blood films. Thick peripheral blood films have an advantage of allowing more red blood cells to be examined per high-powered field, and therefore have increased sensitivity in comparison with thin films, which are used primarily for parasite speciation. The sensitivity of individual thick smears is variable, and depends on smear preparation and the technical experience of laboratory personnel. In recent years, malarial rapid diagnostic tests (RDTs) have been introduced into clinical practice for antigen detection. Similar to other point-of-care tests, RDTs are fairly simple to use and numerous brands are available worldwide. In the United States, only one RDT has been approved by the US Food and Drug Administration, namely the BinaxNOW Malaria Test kit, which is 97% sensitive for all species of malaria and 100% sensitive for P falciparum.37 Many laboratories find this test to be superior to microscopic diagnosis, particularly when smears are performed infrequently. Other rarely used diagnostic strategies include the quantitative buffy coat technique, which allows centrifugation and separation of parasitized from unparasitized cells to facilitate parasite detection, and polymerase chain reaction (PCR) tests to detect parasite DNA. Regardless of the diagnostic strategy used, it is important that diagnosis should never supersede empiric treatment when severe P falciparum infection is suspected.
Two major classes of drugs are available for the parenteral treatment of severe malaria: the cinchona alkaloids (quinine and quinidine) and the artemisinin derivatives (artesunate and artemether). A meta-analysis of randomized controlled trials that compared mortality rates among patients with severe malaria treated with parenteral artesunate or quinine demonstrated a clear advantage for artemisinin-based compounds (odds ratio [OR] for death, 0.69; 95% confidence interval [CI] 0.57–0.84; P<.00001) in favor of artesunate, with no significant increase in adverse effects.38, 39 Artemisinin derivatives also clear parasitemia more rapidly and are effective against a broader range of parasite stages.40 Despite these advantages, no parenteral formulations of artemisinin-based compounds are available in the United States, and only one oral artemisinin-based combination (artemether/lumefantrine) is approved but is not widely available. As it stands, the CDC recommends parenteral quinidine for severe malaria. Quinidine remains available and effective, and should be considered first-line until parenteral artemisinin therapy is made available.41 Therapy with quinidine should be combined with doxycycline or clindamycin, and a 7-day course should be completed. For cases of uncomplicated malaria, 3 options exist in the United States. Most patients with uncomplicated disease should receive either atovaquone-proguanil (Malarone), artemether-lumefantrine (Coartem) or oral quinidine plus doxycycline. The CDC maintains a 24-hour hotline and updated online treatment guidelines, which should be referenced when treating patients with imported malaria. All nonimmune patients with P falciparum should be admitted to hospital, and infectious disease consultation should be obtained.
Dengue fever
Dengue fever is caused by a family of 4 arboviruses that are endemic in most tropical and subtropical regions and represent the most common causes of arboviral disease.42 The viruses are transmitted primarily by the Aedes aegypti mosquito, which is day-biting and has an affinity for small containers and pools of water in urban environments. Approximately one-third of the world’s population lives in dengue-endemic countries, with the highest prevalence in Southeast Asia, Oceania, the Caribbean, and Latin America.43, 44 Close to 100 million cases of dengue fever occur per annum, including 250,000 cases of dengue hemorrhagic fever (DHF), accounting for 25,000 deaths per year.45 The proportion of febrile illness attributed to dengue in returning travelers has increased greatly, from 2% in the 1990s to 16% in 2005. Dengue is currently more than twice as common as malaria in febrile travelers returning from Southeast Asia.46 For United States travelers, the number of confirmed or probable cases rose from 33.5 cases per year in 1990 to 2005 to 244 cases per year in 2006 to 2008.47 At present, no effective vaccine exists for the virus.
Dengue virus has an incubation period of 4 to 8 days. Classic dengue fever is characterized by a clinical syndrome of fever (typically lasting 5–7 days), retro-orbital pain, myalgia, arthralgia (“break-bone fever”), and rash. The rash often begins with an erythrodermic pattern and progresses to a petechial appearance, with desquamation in the convalescent phase. The petechiae are usually seen during the early febrile phase and appear as discrete fine purpura on the face, soft palate, extremities, and axilla.
Dengue infection presents in a spectrum of disease ranging from mild febrile illness (dengue fever) to DHF and dengue shock syndrome (DSS). The more severe syndromes were thought to be rare in returning travelers, as they are associated with repeated infection; however, up to 16% of cases reported to the CDC between 2006 and 2008 were classified as DHF/DSS.47
Progression to the more serious spectrum of DHF/DSS is marked by coagulopathy and increased vascular permeability.48 Hemorrhagic manifestations include easy bruising, bleeding at venipuncture sites, and a positive tourniquet test. On the third to seventh day of illness, often as the fever subsides, changes in vascular permeability may lead to edema, effusions, and the circulatory collapse that marks DSS. Risk factors for developing more severe disease are poorly understood; however, individuals with a history of dengue infection are more likely to develop DHF/DSS (OR 5.1, 95% CI 1.4–17.7).49 Low platelet counts correlate with increased bleeding (OR 3.1, 95% CI 0.95–10.7), and an elevated aminotransferase concentration is associated with progression to DHF (OR 3.5, 95% CI 1.2–10.0).50
The initial diagnosis of dengue fever is clinical, typified by fever and constitutional symptoms in individuals returning from endemic areas. Laboratory features suggestive of dengue infection include thrombocytopenia, leukopenia, and elevated levels of liver enzymes. DHF (mortality rate 10%–20%) is defined as the triad of:
-
•
Thrombocytopenia (<100,000 platelets)
-
•
Hemorrhagic manifestations
-
•
Objective evidence of plasma leakage (hematocrit increase >20%, hypoproteinemia, or evidence of effusions)
DSS (with a mortality rate of up to 40%) is characterized by hypotension (systolic blood pressure <90%) or a narrow pulse pressure (<20 mm Hg). Patients with DHF/DSS warrant admission to a high level of care, as profound hemodynamic shock may rapidly ensue. Leukopenia (<5000 cells/mL) coupled with thrombocytopenia also warrants admission of patients with suspected dengue infection. Serologic diagnosis relies on acute and convalescent serum titers, with convalescent samples drawn 3 weeks after infection. During the acute stage of early infection, a PCR can be used identify dengue viremia.
Mild or classic dengue fever can be treated conservatively with antipyretics, oral fluids, and bed rest. Outpatients should be followed with daily monitoring of the complete blood count for 7 days.50 The day of defervescence (usually between days 4 and 7 of illness) is a common period when capillary leakage and more severe disease can develop. If DHF/DSS is suspected, aggressive fluid replacement with normal saline or lactated Ringer solution is appropriate, and has been shown to decrease the mortality rate.51 In patients with DHF/DSS the hypotension is often profound, although the clinical course is short. Patients with DSS typically either recover rapidly after fluid administration or die within 12 to 24 hours, with an overall mortality rate of 40%.45
Enteric fever (typhoid and paratyphoid)
Typhoid fever is caused by 2 serotypes of the gram-negative bacillus Salmonella enterica: serovar typhi and serovar paratyphi. When these disseminate to cause systemic illness, they are collectively called enteric fever. Infection typically occurs via an oral-fecal route and comes from contaminated food and water, most commonly where standards of personal and environmental hygiene are low. In 2000, enteric fever affected 21.6 million people and claimed 216,500 lives.52 The burden of disease is highest in south central Asia, Southeast Asia, and sub-Saharan Africa (>100 cases/100,000 people per year), and moderately high in the rest of Asia, Africa, Latin America, and Oceania (10–100 cases/100,000 people per year).53 Enteric fever accounts for 2.9% of diagnosed causes of fever in returned travelers, and 14.1% among travelers returning from the Indian subcontinent.5 Two typhoid vaccines are available: the single-dose Vi vaccine (55%–72% effective) and the 3-dose Ty21a vaccine (33%–96% effective).53
Typhoid fever has an incubation period of 7 to 18 days. Affected individuals invariably present with fever. The bacteria initially invade the intestinal mucosa and then pass from the lymphatics to the bloodstream, where they replicate and cause systemic illness. The fever often starts as low grade and then proceeds “stepwise” to become persistent and high grade by the second week. Headache (typically dull and frontal), abdominal pain, constipation or diarrhea, and cough are common symptoms, and can be confused with malaria. Classically, “rose spots” (2–3-mm blanching, pink-red macules) appear early in the course of the disease, but they appear only briefly and are often difficult to detect except in light-skinned persons.17 The Faget sign (relative bradycardia during high fever) has been described in association with typhoid fever, but is rarely seen in clinical practice.
Complications such as disseminated intravascular coagulation, intestinal perforation, gastrointestinal bleeding, and meningitis/encephalitis occur in 10% to 15% of patients, most commonly as delayed manifestations. Peyer patches within the intestinal mucosa are the focus for gastrointestinal hemorrhage and perforation. Intestinal perforation occurs in 1% to 3% of patients and is associated with male sex (OR 4.39, 95% CI 1.37–14.09), leukopenia (OR 3.88, 95% CI 1.46–10.33), and delayed treatment (OR 4.58, 95% CI 1.14–18.35).54 The case-fatality rate for typhoid is less than 1% in the setting of adequate antibiotic treatment and supportive therapy, but can approach 30% to 50% among patients with severe illness in low-resource settings.
The gold standard for diagnosis of enteric fever is blood culture, although stool cultures, urine cultures, bone marrow biopsy, and serology can play a role. During the first week of illness blood cultures have their highest yield, but their diagnostic sensitivity is only 40% to 80%, which underscores the importance of serial cultures.55, 56 Bone marrow biopsies, though rarely indicated, can have a higher yield.57 Serologic testing using the Widal test is not recommended because of its poor sensitivity (47%–77%) and specificity (50%–92%). Newer serologic tests (Typhidot-M, Tubex) are available and may have some utility.57 Because culture data and serology take time to be obtained, presumptive diagnosis and empiric treatment based on clinical diagnosis are required in suspected cases.
Prompt diagnosis coupled with early administration of appropriate antibiotics, supportive care, and correction of fluid losses should be the primary goals of care. Patients suspected of having enteric fever (S typhi or S paratyphi bacteremia) warrant admission for diagnostic and therapeutic considerations. Previous guidelines recommended treatment with fluoroquinolones; however, recent data have demonstrated up to 70% resistance of strains acquired by United Kingdom travelers in Asia.58 Because fluoroquinolone-resistant strains are all sensitive to ceftriaxone, third-generation cephalosporins are considered first-line therapy. In patients with abdominal tenderness, a low index of suspicion should be maintained for complications, including gastrointestinal bleeding and perforation. Imaging and early surgical consultation are warranted in patients with peritonitis.
Rickettsial infection
Rickettsial diseases are a host of zoonotic infections caused by obligate intracellular, gram-negative bacteria of the order Rickettsiales. The vectors are typically arthropods, encompassing ticks, fleas, lice, and mites. More than 280 diagnoses of rickettsial disease were reported in GeoSentinel Surveillance data from 1996 to 2008, with the majority (82.5%) being spotted fever rickettsiosis.59 Surveillance data from returned travelers with undifferentiated fever show rickettsial disease to account for almost 2% of all fevers and 5.6% of fevers in travelers returning from sub-Saharan Africa, making it the second most common identifiable cause of imported fever in that region behind malaria.5
Rickettsial diseases typically have an incubation period of 1 to 2 weeks following a bite from an infected arthropod vector. Although myriad bacteria, vectors, and hosts are intermixed in complex pathways, all rickettsial diseases share clinical features, diagnostic challenges, and treatment recommendations.
Classic rickettsial disease features short (5–7-day) incubation periods, primary lesions (eschars) at the bite site, fever lasting for a few days up to 2 weeks, lymphadenitis, and a maculopapular rash that develops 3 to 5 days after onset of symptoms.60 Of note, less than 50% of patients exhibit the classic triad of eschar, lymphadenitis, and rash.61 In addition to these symptoms, patients often experience headache, myalgia, arthralgia, and malaise, with up to one-third experiencing diarrhea.17 On physical examination, an eschar at the site of a tick or louse bite, which the patient describes as lasting for 1 or 2 weeks, is found more than 80% of the time, but its absence does not rule out the disease. Less than 20% of patients remember the culprit bite.60 Lymphadenitis is the next most common examination finding. Of note, the clinical presentation of rickettsial disease is similar to that of other diagnoses presenting with undifferentiated fever after travel.
Definitive microbiological diagnosis is available via PCR, culture, and serologic analysis. PCR is sensitive, specific, and rapid. Serologic studies are used more commonly but offer only retrospective diagnosis.
Because this diagnosis is difficult to make and is frequently delayed, clinical suspicion and presumptive diagnosis are required to initiate prompt and appropriate treatment in the absence of confirmatory data. Tetracyclines remain the mainstay of treatment, with doxycycline (100 mg twice daily for 3–14 days, depending on the clinical scenario) being the preferred regimen. Patients should improve within the first 48 hours. Failure to do so should prompt the treating physician to revisit the original diagnosis. Mediterranean spotted fever and murine typhus carry higher mortality rates, and scrub typhus, if left untreated, carries significant morbidity.62, 63 Nonetheless, complications are exceedingly rare and prognosis is usually good, with outpatient treatment being appropriate.
Protection of contacts and staff
Until potentially hazardous diseases are excluded, routine infectious precautions, with source isolation and respiratory/droplet confinement, should be implemented for all patients with undifferentiated fever after travel to the tropics. Local hospital guidelines should be followed. The following suspected or confirmed infections require special consideration10: anthrax, diphtheria, encephalitis, enteric fever, hepatitis (acute), novel influenza, measles, meningitis, mumps, pertussis, plague, poliomyelitis, rabies, and tuberculosis; travelers with respiratory illness and rash, varicella and herpes zoster, and viral hemorrhagic fever.
Several infections pose a risk of infection to laboratory staff from improper sample handling and processing. Laboratory staff should therefore be informed if any of the following infections are being considered: enteric fever, brucellosis, Q-fever, melioidosis, and, in particular, the viral hemorrhagic fevers.
The CDC maintains statutory requirements for notification of certain infectious diseases via the National Notifiable Disease Surveillance System. Current guidelines and case definitions can be accessed online at wwwn.cdc.gov/nndss/document/2012_Case%20Definitions.pdf.
Notifiable infections include suspected or confirmed cases of the following: anthrax, arboviral disease, babesiosis, botulism, brucellosis, chancroid, Chlamydia trachomatis, cholera, coccidioidomycosis, cryptosporidiosis, cyclosporiasis, dengue fever, diphtheria, ehrlichiosis, giardiasis, gonorrhea, Haemophilus influenzae, Hansen disease, hantavirus, hemolytic-uremic syndrome, hepatitis, HIV, legionellosis, listeriosis, Lyme disease, malaria, measles, meningococcal disease, mumps, novel influenza, pertussis, plague, polio, psittacosis, Q-fever, rabies, rubella, salmonellosis, severe acute respiratory syndrome, Shiga toxigenic E coli, shigellosis, smallpox, spotted fever, streptococcal toxic shock, syphilis, tetanus, trichinellosis, tularemia, typhoid, vibriosis, viral hemorrhagic fever, and yellow fever.
The most important facet of public health surveillance begins at local, state, and regional levels. Each state has laws that mandate reporting of certain diseases. Clinicians working with patients who return ill from travel should be familiar with state and national requirements as they relate to these infections. Reporting and surveillance are within the scope of practice for health care providers, and are essential for proper surveillance and disease control.
Summary
Fever in ill travelers returning home from developing nations is common. Most travelers present with undifferentiated febrile syndromes. Regional proportionate morbidity rates and the patient’s travel history are essential in narrowing the differential diagnosis. Most patients in whom a diagnosis is confirmed have malaria, dengue, enteric fever, or rickettsial disease. Emergency clinicians should have a high index of suspicion for these diagnoses. Empiric treatment based on the clinical presentation is required in many cases because acquisition of confirmatory laboratory data is often delayed.
Footnotes
Disclosures: No financial disclosures.
Conflicts of Interest: None.
References
- 1.World Health Organization. International travel and health. 2012. Available at: www.who.int/ith/en. Accessed March 6, 2013.
- 2.Ryan E.T., Kain K.C. Health advice and immunizations for travelers. N Engl J Med. 2000;342(23):1716–1725. doi: 10.1056/NEJM200006083422306. [DOI] [PubMed] [Google Scholar]
- 3.Steffen R., deBernardis C., Banos A. Travel epidemiology—a global perspective. Int J Antimicrob Agents. 2003;21(2):89–95. doi: 10.1016/s0924-8579(02)00293-5. [DOI] [PubMed] [Google Scholar]
- 4.Steffen R., Rickenbach M., Wilhelm U. Health problems after travel to developing countries. J Infect Dis. 1987;156(1):84–91. doi: 10.1093/infdis/156.1.84. [DOI] [PubMed] [Google Scholar]
- 5.Freedman D.O., Weld L.H., Kozarsky P.E. Spectrum of disease and relation to place of exposure among ill returned travelers. N Engl J Med. 2006;354(2):119–130. doi: 10.1056/NEJMoa051331. [DOI] [PubMed] [Google Scholar]
- 6.Bruni M., Steffen R. Impact of travel-related health impairments. J Travel Med. 1997;4(2):61–64. doi: 10.1111/j.1708-8305.1997.tb00781.x. [DOI] [PubMed] [Google Scholar]
- 7.Hill D.R. Health problems in a large cohort of Americans traveling to developing countries. J Travel Med. 2000;7(5):259–266. doi: 10.2310/7060.2000.00075. [DOI] [PubMed] [Google Scholar]
- 8.Wilson M.E., Weld L.H., Boggild A. Fever in returned travelers: results from the GeoSentinel Surveillance Network. Clin Infect Dis. 2007;44(12):1560–1568. doi: 10.1086/518173. [DOI] [PubMed] [Google Scholar]
- 9.Leder K., Tong S., Weld L. Illness in travelers visiting friends and relatives: a review of the GeoSentinel Surveillance Network. Clin Infect Dis. 2006;43(9):1185–1193. doi: 10.1086/507893. [DOI] [PubMed] [Google Scholar]
- 10.Johnston V., Stockley J.M., Dockrell D. Fever in returned travellers presenting in the United Kingdom: recommendations for investigation and initial management. J Infect. 2009;59(1):1–18. doi: 10.1016/j.jinf.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Gautret P., Schlagenhauf P., Gaudart J. Multicenter EuroTravNet/GeoSentinel study of travel-related infectious diseases in Europe. Emerg Infect Dis. 2009;15(11):1783–1790. doi: 10.3201/eid1511.091147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bottieau E., Clerinx J., Schrooten W. Etiology and outcome of fever after a stay in the tropics. Arch Intern Med. 2006;166(15):1642–1648. doi: 10.1001/archinte.166.15.1642. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien D., Tobin S., Brown G.V. Fever in returned travelers: review of hospital admissions for a 3-year period. Clin Infect Dis. 2001;33(5):603–609. doi: 10.1086/322602. [DOI] [PubMed] [Google Scholar]
- 14.O'Brien D.P., Leder K., Matchett E. Illness in returned travelers and immigrants/refugees: the 6-year experience of two Australian infectious diseases units. J Travel Med. 2006;13(3):145–152. doi: 10.1111/j.1708-8305.2006.00033.x. [DOI] [PubMed] [Google Scholar]
- 15.Bottieau E., Clerinx J., Van den Enden E. Fever after a stay in the tropics: diagnostic predictors of the leading tropical conditions. Medicine (Baltimore) 2007;86(1):18–25. doi: 10.1097/MD.0b013e3180305c48. [DOI] [PubMed] [Google Scholar]
- 16.Mali S., Tan K.R., Arguin P.M. Malaria surveillance—United States, 2009. MMWR Surveill Summ. 2011;60(3):1–15. [PubMed] [Google Scholar]
- 17.Spira A.M. Assessment of travellers who return home ill. Lancet. 2003;361(9367):1459–1469. doi: 10.1016/S0140-6736(03)13141-8. [DOI] [PubMed] [Google Scholar]
- 18.Memish Z.A. Meningococcal disease and travel. Clin Infect Dis. 2002;34(1):84–90. doi: 10.1086/323403. [DOI] [PubMed] [Google Scholar]
- 19.Jelinek T., Bisoffi Z., Bonazzi L. Cluster of African trypanosomiasis in travelers to Tanzanian national parks. Emerg Infect Dis. 2002;8(6):634–635. doi: 10.3201/eid0806.010432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore A.C., Ryan E.T., Waldron M.A. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 20-2002. A 37-year-old man with fever, hepatosplenomegaly, and a cutaneous foot lesion after a trip to Africa. N Engl J Med. 2002;346(26):2069–2076. doi: 10.1056/NEJMcpc010056. [DOI] [PubMed] [Google Scholar]
- 21.Rothenberg M.E. Eosinophilia. N Engl J Med. 1998;338(22):1592–1600. doi: 10.1056/NEJM199805283382206. [DOI] [PubMed] [Google Scholar]
- 22.Doherty J.F., Moody A.H., Wright S.G. Katayama fever: an acute manifestation of schistosomiasis. BMJ. 1996;313(7064):1071–1072. doi: 10.1136/bmj.313.7064.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulte C., Krebs B., Jelinek T. Diagnostic significance of blood eosinophilia in returning travelers. Clin Infect Dis. 2002;34(3):407–411. doi: 10.1086/338026. [DOI] [PubMed] [Google Scholar]
- 24.Antinori S., Galimberti L., Gianelli E. Prospective observational study of fever in hospitalized returning travelers and migrants from tropical areas, 1997-2001. J Travel Med. 2004;11(3):135–142. doi: 10.2310/7060.2004.18557. [DOI] [PubMed] [Google Scholar]
- 25.Parola P., Soula G., Gazin P. Fever in travelers returning from tropical areas: prospective observational study of 613 cases hospitalised in Marseilles, France, 1999-2003. Travel Med Infect Dis. 2006;4(2):61–70. doi: 10.1016/j.tmaid.2005.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ansart S., Perez L., Vergely O. Illnesses in travelers returning from the tropics: a prospective study of 622 patients. J Travel Med. 2005;12(6):312–318. doi: 10.2310/7060.2005.12603. [DOI] [PubMed] [Google Scholar]
- 27.Casalino E., Le Bras J., Chaussin F. Predictive factors of malaria in travelers to areas where malaria is endemic. Arch Intern Med. 2002;162(14):1625–1630. doi: 10.1001/archinte.162.14.1625. [DOI] [PubMed] [Google Scholar]
- 28.West N.S., Riordan F.A. Fever in returned travellers: a prospective review of hospital admissions for a 2(1/2) year period. Arch Dis Child. 2003;88(5):432–434. doi: 10.1136/adc.88.5.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herbinger K.H., Drerup L., Alberer M. Spectrum of imported infectious diseases among children and adolescents returning from the tropics and subtropics. J Travel Med. 2012;19(3):150–157. doi: 10.1111/j.1708-8305.2011.00589.x. [DOI] [PubMed] [Google Scholar]
- 30.Naudin J., Blonde R., Alberti C. Aetiology and epidemiology of fever in children presenting to the emergency department of a French paediatric tertiary care centre after international travel. Arch Dis Child. 2012;97(2):107–111. doi: 10.1136/archdischild-2011-300175. [DOI] [PubMed] [Google Scholar]
- 31.Hagmann S., Neugebauer R., Schwartz E. Illness in children after international travel: analysis from the GeoSentinel Surveillance Network. Pediatrics. 2010;125(5):e1072–e1080. doi: 10.1542/peds.2009-1951. [DOI] [PubMed] [Google Scholar]
- 32.Mali S., Kachur S.P., Arguin P.M. Malaria surveillance—United States, 2010. MMWR Surveill Summ. 2012;61(2):1–17. [PubMed] [Google Scholar]
- 33.Smith A.D., Bradley D.J., Smith V. Imported malaria and high risk groups: observational study using UK surveillance data 1987-2006. BMJ. 2008;337:a120. doi: 10.1136/bmj.a120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Severe falciparum malaria. World Health Organization, communicable diseases cluster. Trans R Soc Trop Med Hyg. 2000;94(Suppl 1):S1–S90. [PubMed] [Google Scholar]
- 35.Dorsey G., Gandhi M., Oyugi J.H. Difficulties in the prevention, diagnosis, and treatment of imported malaria. Arch Intern Med. 2000;160(16):2505–2510. doi: 10.1001/archinte.160.16.2505. [DOI] [PubMed] [Google Scholar]
- 36.Nic Fhogartaigh C., Hughes H., Armstrong M. Falciparum malaria as a cause of fever in adult travellers returning to the United Kingdom: observational study of risk by geographical area. QJM. 2008;101(8):649–656. doi: 10.1093/qjmed/hcn072. [DOI] [PubMed] [Google Scholar]
- 37.Stauffer W.M., Cartwright C.P., Olson D.A. Diagnostic performance of rapid diagnostic tests versus blood smears for malaria in US clinical practice. Clin Infect Dis. 2009;49(6):908–913. doi: 10.1086/605436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dondorp A., Nosten F., Stepniewska K. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet. 2005;366(9487):717–725. doi: 10.1016/S0140-6736(05)67176-0. [DOI] [PubMed] [Google Scholar]
- 39.Dondorp A.M., Fanello C.I., Hendriksen I.C. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet. 2010;376(9753):1647–1657. doi: 10.1016/S0140-6736(10)61924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosenthal P.J. Artesunate for the treatment of severe falciparum malaria. N Engl J Med. 2008;358(17):1829–1836. doi: 10.1056/NEJMct0709050. [DOI] [PubMed] [Google Scholar]
- 41.Treatment with quinidine gluconate of persons with severe Plasmodium falciparum infection: discontinuation of parenteral quinine from CDC Drug Service. MMWR Recomm Rep. 1991;40(RR-4):21–23. [PubMed] [Google Scholar]
- 42.Wilder-Smith A., Schwartz E. Dengue in travelers. N Engl J Med. 2005;353(9):924–932. doi: 10.1056/NEJMra041927. [DOI] [PubMed] [Google Scholar]
- 43.Gubler D.J., Clark G.G. Dengue/dengue hemorrhagic fever: the emergence of a global health problem. Emerg Infect Dis. 1995;1(2):55–57. doi: 10.3201/eid0102.952004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mohammed H.P., Ramos M.M., Rivera A. Travel-associated dengue infections in the United States, 1996 to 2005. J Travel Med. 2010;17(1):8–14. doi: 10.1111/j.1708-8305.2009.00374.x. [DOI] [PubMed] [Google Scholar]
- 45.Gibbons R.V., Vaughn D.W. Dengue: an escalating problem. BMJ. 2002;324(7353):1563–1566. doi: 10.1136/bmj.324.7353.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wilder-Smith A., Renhorn K.E., Tissera H. DengueTools: innovative tools and strategies for the surveillance and control of dengue. Glob Health Action. 2012;5:17274. doi: 10.3402/gha.v5i0.17273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) Travel-associated Dengue surveillance—United States, 2006-2008. MMWR Morb Mortal Wkly Rep. 2010;59(23):715–719. [PubMed] [Google Scholar]
- 48.Halstead S.B. Dengue. Lancet. 2007;370(9599):1644–1652. doi: 10.1016/S0140-6736(07)61687-0. [DOI] [PubMed] [Google Scholar]
- 49.Guzman M.G., Kouri G. Dengue: an update. Lancet Infect Dis. 2002;2(1):33–42. doi: 10.1016/s1473-3099(01)00171-2. [DOI] [PubMed] [Google Scholar]
- 50.Wichmann O., Gascon J., Schunk M. Severe dengue virus infection in travelers: risk factors and laboratory indicators. J Infect Dis. 2007;195(8):1089–1096. doi: 10.1086/512680. [DOI] [PubMed] [Google Scholar]
- 51.Dung N.M., Day N.P., Tam D.T. Fluid replacement in dengue shock syndrome: a randomized, double-blind comparison of four intravenous-fluid regimens. Clin Infect Dis. 1999;29(4):787–794. doi: 10.1086/520435. [DOI] [PubMed] [Google Scholar]
- 52.Crump J.A., Luby S.P., Mintz E.D. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346–353. [PMC free article] [PubMed] [Google Scholar]
- 53.Bhan M.K., Bahl R., Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005;366(9487):749–762. doi: 10.1016/S0140-6736(05)67181-4. [DOI] [PubMed] [Google Scholar]
- 54.Hosoglu S., Aldemir M., Akalin S. Risk factors for enteric perforation in patients with typhoid Fever. Am J Epidemiol. 2004;160(1):46–50. doi: 10.1093/aje/kwh172. [DOI] [PubMed] [Google Scholar]
- 55.Vallenas C., Hernandez H., Kay B. Efficacy of bone marrow, blood, stool and duodenal contents cultures for bacteriologic confirmation of typhoid fever in children. Pediatr Infect Dis. 1985;4(5):496–498. doi: 10.1097/00006454-198509000-00011. [DOI] [PubMed] [Google Scholar]
- 56.World Health Organization. Background document: the diagnosis, treatment and prevention of typhoid fever. World Health Organization; Geneva (Switzerland): 2003. [Google Scholar]
- 57.Bhutta Z.A. Current concepts in the diagnosis and treatment of typhoid fever. BMJ. 2006;333(7558):78–82. doi: 10.1136/bmj.333.7558.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Threlfall E.J., de Pinna E., Day M. Alternatives to ciprofloxacin use for enteric fever, United kingdom. Emerg Infect Dis. 2008;14(5):860–861. doi: 10.3201/eid1405.071184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jensenius M., Davis X., von Sonnenburg F. Multicenter GeoSentinel analysis of rickettsial diseases in international travelers, 1996-2008. Emerg Infect Dis. 2009;15(11):1791–1798. doi: 10.3201/eid1511.090677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jelinek T., Loscher T. Clinical features and epidemiology of tick typhus in travelers. J Travel Med. 2001;8(2):57–59. doi: 10.2310/7060.2001.24485. [DOI] [PubMed] [Google Scholar]
- 61.Jensenius M., Fournier P.E., Vene S. African tick bite fever in travelers to rural sub-Equatorial Africa. Clin Infect Dis. 2003;36(11):1411–1417. doi: 10.1086/375083. [DOI] [PubMed] [Google Scholar]
- 62.Raoult D., Zuchelli P., Weiller P.J. Incidence, clinical observations and risk factors in the severe form of Mediterranean spotted fever among patients admitted to hospital in Marseilles 1983-1984. J Infect. 1986;12(2):111–116. doi: 10.1016/s0163-4453(86)93508-5. [DOI] [PubMed] [Google Scholar]
- 63.Dumler J.S., Taylor J.P., Walker D.H. Clinical and laboratory features of murine typhus in south Texas, 1980 through 1987. JAMA. 1991;266(10):1365–1370. [PubMed] [Google Scholar]