Abstract
We sought to describe the implementation of the Hospital Emergency Incident Command System (HEICS) at National Cheng Kung University Hospital (NCKUH) in Taiwan, ROC during the outbreak of severe acute respiratory syndrome (SARS) in early 2003. We administered a 14-question survey via structured interviews to individuals occupying activated HEICS leadership positions at NCKUH to identify the organization, structure, and function of the HEICS units and subunits they led and the job actions they performed from 25 March to 16 June 2003 Thirty-three of 38 persons (87%) occupying 39 of 44 (89%) activated HEICS leadership positions directly participated in the survey. The participants collectively reported: 1) the creation of four new HEICS unit leader positions and corresponding units during the outbreak, including the infection control officer (administrative section) and SARS assessment, isolation, and critical care unit leaders (operations section); 2) the creation of six new HEICS subunits, including functional areas for fever screening, SARS assessment, and resuscitation outside the hospital, and SARS patient care, SARS critical care, and employee isolation inside the hospital; and 3) the performance of new job actions related to infection control by all HEICS unit leaders. HEICS provides a flexible framework that seems to have assisted NCKUH in the organization of its emergency response to the SARS outbreak in Taiwan, ROC.
Keywords: emergency management, hospital emergency incident command system, infection control, severe acute respiratory syndrome, Taiwan
Introduction
On 14 March 2003, an outbreak of severe acute respiratory syndrome (SARS) was recognized in Taiwan, Republic of China, an island nation located 130 kilometers east of mainland China, when the first two probable cases of SARS were diagnosed in a recent traveler to Guangdong Province and his wife (1, 2). By 22 April, Taiwan experienced only 29 probable SARS cases, four of which resulted from secondary transmission from the index case (one physician and three family contacts) (1, 3, 4). However, by 22 May, the nosocomial spread of SARS in at least nine hospitals catapulted the number of probable cases to 583, including 60 deaths (1, 5). When the last probable case of SARS was reported on 15 June, 671 probable cases of SARS had occurred, with 83 deaths, seven of which were in health-care workers (4, 6, 7).
Although various aspects of the operational response and clinical management of SARS have been reported from hospitals in several countries, little has been reported about overall hospital emergency management during a SARS outbreak (8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21). Furthermore, despite the growing popularity of the Hospital Emergency Incident Command System (HEICS) as an organizational tool for hospital emergency management in the United States and elsewhere, little has been reported about the application of HEICS to actual hospital emergencies of any type (22, 23, 24). Accordingly, we sought to characterize the implementation of HEICS at a tertiary level hospital during the SARS outbreak in Taiwan, ROC.
Materials and methods
Study design
We performed a cross-sectional survey of individuals occupying activated HEICS leadership positions at National Cheng Kung University (NCKUH) during the SARS outbreak. This study was approved by the IRB at NCKUH on 3 May 2003.
Study setting
The study setting was NCKUH, one of 15 tertiary care medical centers in Taiwan, ROC (population 23 million). Located in the southwestern city of Tainan, NCKUH serves a population of 1.7 million and has a catchment area of approximately 2200 km2. NCKUH has 1173 beds, 83 ICU beds, and 60 emergency department (ED) beds; offers the full complement of medical specialties, including emergency medicine, infectious disease, pulmonary medicine, and hospital epidemiology; and has an affiliated medical school. The annual ED census is 62,602 with 13,545 admissions per year. After the JiJi earthquake in 1999, the hospital adopted the Hospital Emergency Incident Command System (HEICS) as its organizational system for hospital emergency management.
Study period
We defined the study period as the duration of the SARS outbreak at NCKUH, beginning on 25 March and ending on 16 June 2003. We designated 25 March as the first day of our study, because on the evening of 24 March, NCKUH activated its hospital emergency plan and HEICS in response to the growing SARS outbreak. On 26 March, NCKUH received its first suspected case of SARS. We selected 16 June as the last day of the study, because the following day the World Health Organization (WHO) removed its travel advisory for Taiwan (25).
Definitions
We used the definitions of suspected and probable SARS recommended by WHO and implemented in Taiwan on 17 March (26). Diarrhea was also used as a criterion for suspected SARS in Taiwan, because diarrhea had been reported as a prominent early symptom in Hong Kong and Taipei (1, 16). No attempt was made to classify probable patient-cases of SARS in Taiwan into a “confirmed” patient-case category, because no international consensus existed for the case definition of “confirmed SARS” during the study period. These definitions remained unchanged throughout the study period except for the identity of areas with local transmission of SARS, which changed throughout the study. We also used the term “possible SARS” to describe those patients undergoing evaluation for suspected or probable SARS.
We used standard HEICS nomenclature to define HEICS leadership positions (23). We defined a HEICS “subunit” as a separate functional area under the command and control of a single HEICS unit leader.
Selection of participants
We selected persons occupying activated HEICS leadership positions during the SARS outbreak as potential survey participants. These persons were identified by the Emergency Operations Committee (EOC) at NCKUH as occupying HEICS leadership positions that were either activated from the baseline HEICS plan at NCKUH or newly created during the SARS outbreak (the EOC was comprised of all HEICS administrative positions and section chiefs). We excluded persons occupying leadership positions in the baseline HEICS plan that were not activated during the outbreak. The baseline HEICS plan at NCKUH has three fewer positions than the standard 49-position version used in the United States (i.e., a medical staff director, ancillary services director, and cardiopulmonary unit leader are absent) (23, 24).
Methods of measurement
We administered a survey to the participants, consisting of 14 open-ended questions (Table 1). These questions were aimed at identifying the participant’s pre-existing job title at NCKUH, confirming the participant’s occupation of a HEICS leadership position during the SARS outbreak, and characterizing the organization, structure, and function of the HEICS units and subunits the participant led and the job actions performed during the SARS outbreak. We based our survey on published recommendations for evaluating hospital disaster response and on previous studies that used structured interview methodology to characterize disaster response (27, 28, 29, 30).
Table 1.
Survey Questions
| Questions* | Question Type |
|---|---|
| 1. What is your name? 2. What is your job title at NCKUH? | Identifying information |
| 3. Are you leading an activated HEICS unit at NCKUH during the SARS outbreak? | Inclusion criteria |
| 4. What is the name of each activated HEICS unit under your leadership at NCKUH during the SARS outbreak? | HEICS unit organization |
| 5. What is the name of each activated HEICS subunit under your leadership at NCKUH during the SARS outbreak? | |
| 6. What is the organizational position of each activated HEICS unit and subunit under your leadership within the HEICS organizational structure at NCKUH during the SARS outbreak? | |
| 7. Which of these activated HEICS units and subunits were newly created and added to the HEICS organizational structure at NCKUH during the SARS outbreak? | |
| 8. What is the physical location within the hospital campus of each activated HEICS unit or subunit under your leadership during the SARS outbreak? | |
| 9. What types of facilities have been used or are being used by each activated HEICS unit and subunit under your leadership at NCKUH during the SARS outbreak, including quantity if possible? | |
| 10. What types of equipment and supplies have been used or are being used by each activated HEICS unit and subunit under your leadership at NCKUH during the SARS outbreak, including quantity if possible? | HEICS unit structure |
| 11. What types of personnel have worked or are working in each activated HEICS unit and subunit under your leadership at NCKUH during the SARS outbreak? | |
| 12. What types of functions have been performed or are being performed by each activated HEICS unit and subunit under your leadership during the SARS outbreak, including infection control measures (isolation, personal protective equipment use, decontamination, hand-washing, and fever screening), SARS-related medical care, and routine medical care? | HEICS unit functions |
| 13. What types of job actions have you performed or are performing during the SARS outbreak, including specific policy recommendation, policy implementation, supervision of activities, performance of activities, and communication of information? | HEICS leader job actions |
| 14. Which of these job actions were newly created and added to your HEICS job action list during the SARS outbreak? |
Translated from Chinese into English language.
Data collection and processing
Four trained research assistants under the supervision of the first author surveyed the study participants via structured interviews from 20 to 27 May. Participants were provided our written survey tool and the research assistant recorded their verbal responses. The first author supplemented these primary surveys with periodic secondary surveys of the HEICS administrative and section leaders at the conclusion of daily EOC meetings during the remainder of the outbreak. The first author also attempted to clarify ambiguous or contradictory responses through secondary surveys and structured interviews. Any information remaining ambiguous or contradictory was adjudicated by the consensus agreement of the authors. All participants provided their informed consent to participate in the interviews. When persons occupying activated HEICS leadership positions declined or were unable to participate in the survey, then relevant data were collected from their designated proxies or from their superiors in the activated HEICS organization. Data were entered into spreadsheets using Windows XP Excel software (Microsoft Corporation, Redmond, WA).
Primary data analysis
We combined the survey responses across all participants to produce an organizational chart showing the actual activation of HEICS at NCKUH during the SARS outbreak. We confirmed the identities of HEICS units and subunits that were reported as being newly created and identified HEICS units that did not open by comparison with the HEICS organizational chart in existence at NCKUH before the outbreak. We combined the participants’ descriptions of the structures and functions of HEICS units and subunits that were newly created or substantially modified (i.e., given a new major function)—the infection control office, fever screening subunit, triage unit, SARS assessment unit, SARS isolation unit, and SARS critical care unit.
We combined the survey responses to correlate each activated HEICS leadership position, the pre-existing job title of each individual executing that position, and new SARS-related job actions (not specified in the baseline hospital emergency plan) performed by that leader during the outbreak.
Data presentation
We present our data describing the HEICS organizational structure at NCKUH during the SARS outbreak as a chart (Figure 1) for convenient comparison with the standard HEICS organizational chart. We tabulated other descriptive information according to HEICS unit or subunit.
Figure 1.
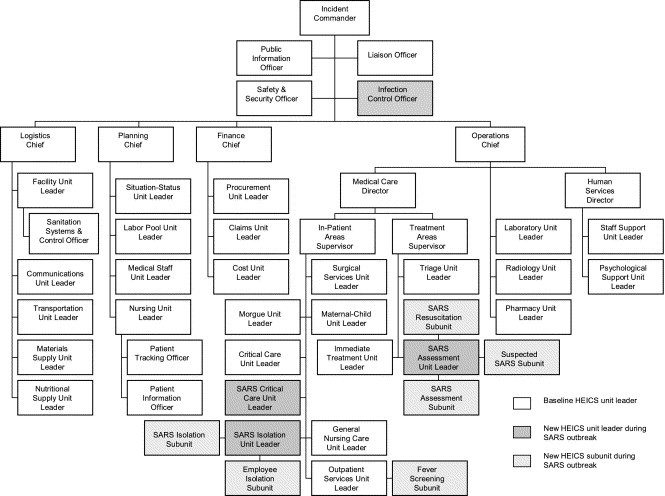
Activated HEICS positions at NCKUH during the SARS outbreak.
Results
Thirty-three of 38 persons (87%) occupying 39 of 44 (89%) leadership positions in the activated version of HEICS at NCKUH directly participated in the survey, including the four persons occupying the four leadership positions newly created during the outbreak (Table 2, Table 3, Table 4, Table 5). One individual was represented in the survey by a proxy that he appointed, whereas four others, who declined or were unable to participate, were represented by their superiors in the HEICS structure (Table 2, Table 3, Table 5).
Table 2.
Position, Title, and New Job Actions in HEICS Administrative Section During the SARS Outbreak
| Position (Title) | New Job Actions |
|---|---|
| Incident commander (Superintendent) | Authorized creation of new HEICS units and subunits, conversion of hospital areas to SARS-related functions, new infection control policy, and new job actions for HEICS unit leaders |
| Represented hospital in regional SARS emergency network* | |
| Liaison officer (Secretary of medical affairs) | Reported hospital surveillance results to city health bureau and Taiwan Center for Disease Control (TCDC) |
| Public information officer (Secretary general) | None |
| Infection control officer (Chair of infection control committee) | Recommended infection control policy to EOC |
| Prepared all infection control policy for personnel, patients, employees, and visitors | |
| Prepared policy designating SARS assessment, isolation, and critical care units as hot zones | |
| Prepared policy restricting hospital access by non-essential persons (visitors, vendors, media), allowing only one family member per hospital patient | |
| Prepared policy separating all hospital personnel into three rotating 8-hour shifts and all personnel in SARS hot zone areas into 4-h shifts | |
| Prepared decontamination policy for personnel leaving SARS hot zones | |
| Prepared policy restricting transport of non-essential equipment or materials out of SARS hot zones and requiring decontamination of essential equipment and materials leaving SARS hot zones | |
| Prepared policy designating transport routes for SARS-related patients, specimens, decedents, and possibly contaminated equipment or materials | |
| Prepared policy restricting aerosol-generating interventions in hospital (i.e., nebulized medications, suctioning, non-invasive ventilation, bronchoscopy) | |
| Prepared policy regarding isolation of SARS-related specimens in double plastic bags, laundry or waste in double plastic bags, and decedents in double body bags | |
| Prepared policy designating transport routes for SARS-related patients, specimens, materials, or decedents | |
| Prepared policy requiring fever screening of all persons entering hospital and all personnel twice per 8-h shift, including workers not employed by hospital (i..e., personal attendants, laundry workers, and delivery persons) | |
| Prepared policy requiring employees isolated at home to report their body temperature twice per day | |
| Prepared policy closing hospital restaurant and cafeteria and prohibiting unauthorized food delivery to hospital and requiring individualization of all meals in disposable box-style packages | |
| Supervised collection of body temperature data from all personnel on duty or isolated at home | |
| Supervised collection of health status data from entire hospital patient population and all isolated personnel | |
| Reported surveillance results to EOC | |
| Supervised release of information about health status of isolated persons to families | |
| Supervised acquisition of updated information and policy recommendations about infection control measures from external sources—TCDC, other hospitals in Taiwan, other countries | |
| Safety and security officer (Captain of hospital security)** | Enforced closure of all hospital entrances/exits except outpatient and ED entrances |
| Enforced traffic control in fever screening subunit and triage unit, and perimeter control in SARS assessment, isolation and critical care units | |
| Supervised demarcation of designated traffic routes into, out of, and within hospital, and off-limits areas with yellow tape barriers | |
| Enforced restriction of vendor deliveries to 5:00 a.m. at hospital basement entrance |
Regional SARS Emergency Network was comprised of the Tainan city health bureau and five hospitals in the city.
Appointed deputy safety and security officer to participate in survey.
Table 3.
Positions, Titles, and New Job Actions in HEICS Operations Section During the SARS Outbreak
| Position (Title) | New Job Actions |
|---|---|
| Operations chief (Chair of infection control committee) | Organized education and training on infection control measures and SARS-related medical care for section |
| Supervised implementation of infection control measures | |
| Medical care director (Chief of internal medicine department) | Organized physician education on SARS-related medical care |
| Chaired daily SARS case conference | |
| Supervised conversion of 50-bed pulmonary medicine ward to SARS isolation subunit and SARS critical care unit and adjacent 50-bed psychiatry ward to Employee isolation subunit | |
| Supervised implementation of infection control policy in patient care areas—hand-washing after every patient contact, restricted use of aerosol-producing interventions, etc. | |
| Assigned physicians to SARS-related units to match service loads | |
| Treatment areas supervisor (Chief of emergency medicine department) | Supervised infection control measures and SARS-related medical care in EMS |
| Suspended ED observation functions | |
| Triage unit leader (Head nurse of emergency medicine department) | Supervised fever screening of all persons entering ED entrance |
| Supervised identification of afebrile persons via colored stickers on outer clothing | |
| Supervised provision of respiratory personal protective equipment (PPE) to all afebrile persons entering ED – surgical masks for visitors, N95 or surgical masks for others depending on risk/preference | |
| Supervised diversion of febrile persons to SARS assessment unit | |
| Supervised provision of N95 masks to febrile persons | |
| Immediate treatment unit leader (Designated emergency physician) | Closed ED to EMS when adequate infection control threatened by patient volume |
| SARS assessment unit leader (Head of non-trauma division of emergency department) | Supervised screening of persons with fever for possible SARS |
| Supervised full evaluation of patients with possible SARS for suspected or probable SARS | |
| Supervised medical care of patients undergoing evaluation for suspected or probable SARS | |
| Supervised resuscitation of critically ill or injured patients with fever or possible SARS | |
| Supervised use of powered air purifying respirator with hood for personnel performing endotracheal intubation or airway suctioning | |
| Supervised isolation of persons with fever until possible SARS ruled out | |
| Supervised isolation of patients with suspected or probable SARS outside hospital until bed available in SARS isolation unit | |
| Supervised use of N95 masks by patients | |
| Supervised restriction of transport of non-essential equipment and materials out of area | |
| Supervised decontamination of essential equipment and materials leaving area with 5% bleach | |
| Inpatient areas supervisor (Chief of general medicine) | Coordinated patient disposition to SARS isolation subunit |
| Supervised relocation of patients in pulmonary ward to other inpatient wards at onset of SARS outbreak | |
| Supervised transfer of one patient with pulmonary tuberculosis (TB) requiring negative pressure isolation (NPI) bed to local TB hospital at onset of SARS outbreak | |
| SARS isolation unit leader (Pulmonary medicine attending and infectious disease attending physicians alternating every other day) | Supervised use of powered air purifying respirator with hood for personnel performing endotracheal intubation or airway suctioning |
| Supervised medical care in SARS isolation subunit | |
| Supervised isolation of patients with suspected or probable SARS in SARS isolation subunit | |
| Supervised isolation of febrile personnel in Employee isolation subunit | |
| Supervised use of N95 masks by patients and isolated employees | |
| Supervised decontamination of all personnel leaving unit via shower (with soap and water) and clothing change (hospital scrubs) | |
| Surgical services unit leader (Chief of surgery department)* | Cancelled elective surgery after Surgical Intensive Care Unit (SICU) closed |
| Maternal-child unit leader (Chief of pediatrics department)* | Assigned pediatricians to SARS assessment unit to help evaluate children with fever |
| Supervised planning and preparedness for pediatric SARS isolation unit if needed | |
| Critical care unit leader (Chief of critical care medicine department)* | Supervised conversion of SICU to SARS critical care unit |
| Supervised relocation of SICU patients to burn unit | |
| Supervised conversion of burn unit to new SICU | |
| Supervised planning for SARS-related medical care in two negative pressure isolation-Medical Intensive Care Unit (NPI-MICU) beds if needed | |
| SARS critical care unit leader (chief of internal medicine department) | Supervised use of powered air purifying respirator with hood for personnel performing endotracheal intubation or airway suctioning |
| Supervised medical care in both SARS critical care areas (12th floor and SICU) | |
| Supervised isolation of critically ill patients with suspected or probable SARS | |
| Supervised use of N95 masks by patients | |
| Supervised decontamination of all personnel leaving unit via shower (soap and water) and clothing change (hospital scrubs) | |
| Supervised installation of in-line HEPA filters in ventilator circuits | |
| Supervised planning for medical care in four NPI-MICU beds if needed | |
| General nursing care unit leader (Deputy director of nursing department) | Supervised nursing care in SARS isolation and critical care units |
| Supervised fever screening of personal attendants twice per 8-h shift | |
| Outpatient services unit leader (Chief of family medicine department) | Supervised fever screening of all persons entering outpatient entrance from 7:30 a.m.–9:30 p.m. daily |
| Supervised identification of afebrile persons via colored stickers on outer clothing | |
| Supervised provision of respiratory PPE to all afebrile persons entering hospital—surgical masks for visitors, N95 or surgical masks for others depending on risk/preference | |
| Supervised diversion of febrile persons to SARS assessment unit | |
| Supervised provision of N95 masks to febrile persons | |
| Supervised mailing of prescription refills to outpatient clinic patients | |
| Morgue unit leader (General manager) | Supervised decontamination, storage, and transport of SARS-related decedents for cremation |
| Supervised isolation of SARS-related decedents in two layers of body bags | |
| Supervised transport of SARS-related decedents using designated transport routes | |
| Established transport route from hospital to cremation site | |
| Laboratory unit leader (Chief of clinical pathology department) | Supervised isolation of SARS-related specimens in two plastic bags during transport and handling |
| Supervised identification of SARS-related specimens via colored stickers on containers | |
| Supervised transport of SARS-related specimens, including use of designated transport routes | |
| Organized transport of SARS-related specimens for reverse transcriptase polymerase chain reaction (RT-PCR) testing to TCDC in Taipei before May 1 | |
| Supervised laboratory upgrade to biosafety level 3 | |
| Supervised RT-PCR testing of SARS-related specimens from NCKUH and other hospitals in region after May 1 | |
| Radiology unit leader (Chief of radiology department) | Supervised deployment of portable x-ray machines and radiology technicians to SARS assessment, isolation and critical care units |
| Pharmacy unit leader (Chief of pharmacy department) | Supervised acquisition and distribution of ribavirin to SARS isolation and critical care units |
| Human services director (Chief of personnel department) | Assigned administrative employees to fever screening subunit |
| Supervised distribution of information regarding infection control policy to all personnel | |
| Supervised distribution of advisories to all personnel regarding possible isolation in Employee isolation subunit or home isolation | |
| Staff support unit leader (Chief of labor safety and health department) | Supervised production of intranet database for recording body temperatures of personnel |
| Supervised separation of personnel meal and rest areas from patient care areas | |
| Psychological support unit leader (Chief of psychiatry department) | Supervised counseling for patients and employees isolated in SARS isolation and critical care units |
| Supervised critical incident stress debriefing (CISD) for personnel working in SARS isolation and critical care units | |
| All units | Supervised monitoring of personnel twice per shift |
| Supervised education of personnel regarding infection control policy and measures | |
| Supervised use of N95 masks and universal precautions by personnel or patients in high risk areas—Fever screening subunit, Triage unit, Immediate treatment unit, Laboratory unit, Morgue unit, SARS-related units | |
| Supervised use of N95 or surgical masks by personnel or patients in low-risk areas | |
| Supervised restriction of transport of non-essential equipment or materials out of SARS-related units | |
| Supervised decontamination of essential equipment or materials leaving SARS-related units with 5% bleach |
Did not participate in survey, data obtained from Medical care director and Inpatient areas supervisor.
Table 4.
Positions, Titles, and New Job Actions by HEICS Position in Logistics Section During the SARS Outbreak
| Position (Title) | New Job Actions |
|---|---|
| Logistics chief (Deputy superintendent of administration) | Established designated transport routes for SARS-related patients and specimens, including designated elevator |
| Supervised deployment of SARS-related equipment and supplies | |
| Supervised monitoring of SARS-related supply stockpiles | |
| Facility unit leader (Chief of engineering and maintenance department) | Supervised erection of DRASH© units in fever screening subunit and SARS assessment unit, and large umbrella in triage unit |
| Supervised installation of power and lighting in outdoor units, O2 supply in SARS assessment unit and resuscitation area, and portable suction in SARS resuscitation area | |
| Supervised deployment of furnishings to fever screening subunit, triage unit and SARS assessment unit | |
| Supervised remodeling in SARS isolation unit, including installation of internal physical barriers (e.g., plastic curtain at nurse’s station in SARS isolation unit) | |
| Supervised conversion of elevators to use with special access cards only | |
| Supervised architectural plans for construction of permanent triage unit and SARS assessment unit outside ED if outbreak continued | |
| Sanitation systems officer (General manager) | Supervised installation of 80 portable hand-washing units throughout hospital |
| Supervised installation of portable toilets in fever screening subunit, triage unit, and SARS assessment unit | |
| Supervised decontamination of toilets with 30 cc of 5% hypochlorite by users after each flush | |
| Supervised housekeeping activities in SARS-related areas | |
| Supervised isolation of SARS-related laundry in two layers of plastic bags for transport to designated laundry machines for SARS-related laundry | |
| Supervised washing of SARS-related laundry in designated laundry machines | |
| Supervised fever monitoring of contract laundry workers twice per 8-h shift | |
| Communications unit leader (Chief of medical information department) | Supervised installation of telephones in fever screening subunit, triage unit, SARS assessment unit, security guard stations |
| Supervised distribution of radiophones to personnel in ED, SARS assessment, isolation, and critical care units | |
| Supervised installation of computers with Internet access in triage unit, SARS isolation and critical care units | |
| Supervised implementation of automatic electronic cross-checking system between NCKUH patient registration system and National Health Insurance Bureau database | |
| Transportation unit leader (General manager) | Supervised transport of SARS-related patients via designated routes |
| Materials supply unit leader (Chief of material supply department) | Supervised acquisition and delivery of all SARS-related equipment and supplies to SARS-related areas |
| Supervised fever monitoring of delivery personnel at time of delivery | |
| Nutritional supply unit leader (Chief of nutritional service department) | Supervised individualization of all meals—patients and employees—into disposable box-style packages |
| Supervised scheduled food deliveries to isolated persons | |
| All unit leaders | Supervised fever monitoring of personnel twice per shift |
| Supervised education of personnel regarding infection control policy and measures | |
| Supervised use of N95 or surgical masks by personnel |
Table 5.
Positions, Titles, and New Job Actions by HEICS Position in Planning and Finance Sections During the SARS Outbreak
| Position (Title) | New Job Actions |
|---|---|
| Planning chief (Chief of development and planning department) | Supervised distribution of SARS-related information to hospital employees via hospital intranet (or FAX) |
| Situation-status unit leader (Secretary general) | Supervised preparation of SARS-related policy statements, guidelines, and reports |
| Labor pool unit leader (Chief of social work department) | Supervised suspension of all volunteer activities except in fever screening subunit |
| Supervised isolation of febrile hospital employees at home or in employee isolation unit for 3 days | |
| Supervised separation of all non-medical and non-nursing personnel into 3 teams to work in 8-h shifts to limit nosocomial spread | |
| Medical staff pool unit leader (Secretary of medical affairs) | Allocated additional physician staffing to ED |
| Supervised isolation of febrile physicians at home or in employee isolation unit for 3 days | |
| Supervised separation of all physicians and medical students into 3 teams to work in 8-h shifts to limit nosocomial spread | |
| Nursing unit leader (Director of nursing department) | Supervised staffing of nurses in SARS-related units |
| Supervised isolation of febrile nurses at home or in employee isolation unit for 3 days | |
| Supervised separation of all nurses into 3 teams to work in 8-h shifts to limit nosocomial spread | |
| Patient tracking officer (Infection control nurse) | Supervised tracking of location of all patients with suspected or probable SARS at all times within the hospital system |
| Patient information officer (Chief of medical affairs department) | Supervised the establishment of automated patient information retrieval system from national insurance database to establish epidemiologic risk of SARS |
| Finance chief (Chief of accounting department) | None |
| Procurement unit leader (Chief of purchasing section) | Supervised procurement of personal protective equipment, portable hand-washing units, and SARS-related medications from local vendors |
| Supervised contract with local vendor to upgrade laboratory to biosafety level 3 | |
| Supervised procurement of portable outdoor toilets from Tainan city | |
| Claims unit leader (Chief of cashier section) | Supervised submission of claims to government for reimbursement for SARS-related expenses |
| Cost unit leader (Chief of cost analysis section)* | Supervised tracking of cost of isolation measures and SARS-related medical care |
| All unit leaders | Supervised fever monitoring of personnel twice per shift |
| Supervised education of personnel regarding infection control policy and measures | |
| Supervised use of N95 or surgical masks by personnel |
Did not participate in survey, data obtained from Finance chief.
Figure 1 shows the actual activation of HEICS during the SARS outbreak at NCKUH. Four HEICS positions (and corresponding units) and six subunits were created during the SARS outbreak. Six HEICS units not activated during the SARS outbreak included the damage assessment and control, time, delayed treatment, minor treatment, discharge, and dependent care units.
The structure and function of newly created HEICS units and subunits (and the modified Triage unit) are summarized in Table 6. Table 2 shows each activated leadership position in the HEICS administrative section at NCKUH, the job title of each position holder, and new job actions during the event that were not anticipated in the baseline hospital emergency plan. Table 3, Table 4, Table 5 show similar information for the HEICS operations, logistics, planning, and finance sections.
Table 6.
Structure and Function of New HEICS Units and Subunits During the SARS Outbreak
| Unit | Subunit | Location | Structure | Function |
|---|---|---|---|---|
| Infection control office | - | 2nd floor of hospital | Office | Development and implementation of infection control policy Monitoring and reporting of health status of patients, personnel, and visitors |
| Outpatient services | Fever screening | Outside hospital—outpatient entrance | Small DRASH© unit** | Screening of persons entering outpatient entrance for fever 7:30 a.m.–9:30 p.m. Diversion of persons with fever to SARS assessment unit |
| Triage* | - | Outside ED—next to SARS assessment unit | Desk in open space with umbrella | Screening of persons entering ED entrance for fever† Triage of ED patients Diversion of persons with fever to SARS assessment unit |
| SARS assessment | Outside ED—next to triage unit | 8-bed DRASH© unit with radiology area and nurse’s station‡ | Screening of persons with fever for possible SARS Evaluation of patients with possible SARS for suspected or probable SARS Isolation and medical care of patients with possible SARS while undergoing evaluation for suspected or probable SARS | |
| SARS assessment | SARS resuscitation | Outside ED—decontamination room | 1-bed unit power column, oxygen supply, suction device, and TV monitor | Isolation and resuscitation of critically ill patients with fever or possible SARS while undergoing evaluation for suspected or probable SARS |
| Suspected SARS | Outside ED—15 meters from triage unit | 2-bed DRASH© unit for suspected SARS 1-bed DRASH© unit for probable SARS | Isolation and medical care of patients with suspected or probable SARS awaiting bed in SARS isolation unit | |
| SARS isolation | 12th floor of hospital | 22 single negative pressure isolation (NPI) rooms in former pulmonary medicine ward | Isolation and medical care of patients with suspected or probable SARS | |
| SARS isolation | Employee isolation | 12th floor of hospital | 25 single isolation rooms in former psychiatric ward | Isolation and medical care of personnel with fever of indeterminate origin for 3 days |
| SARS critical care | - | 12th floor of hospital | 6 single NPI-critical care rooms in former pulmonary medicine ward | Isolation and medical care of critically ill patients with suspected or probable SARS |
| 3rd floor of hospital | 4 single NPI-critical care rooms in Surgical Intensive Care Unit |
- = Not applicable.
Triage unit included here because fever screening function was new.
DRASH© = deployable rapid assembly shelter.
Patients, visitors, and personnel from 9:30 p.m. to 7:30 a.m..
Equipped with O2 supply, pulse oximetry, and cardiac monitors.
Discussion
The implementation of HEICS at NCKUH during this SARS outbreak illustrates several features of HEICS that seem to have assisted the organization of hospital emergency response at NCKUH (23, 24).
First, HEICS provided a flexible organizational structure that facilitated the creation of new units and subunits and new functions of hospital emergency response as the evolving crisis demanded. This organizational flexibility was imperative because a rapidly evolving infectious disease emergency involving a highly contagious agent had never been encountered before. A major critical adaptation at NCKUH was the establishment of the infection control officer within the HEICS administrative section. Because infection control plays a key role in contagious infectious disease emergencies, it is paramount that the infection control officer has an overall perspective of the entire hospital, a close advisory relationship with the incident commander, and direct communication links with other HEICS managers and section chiefs. The importance of infection control in the emergency response to SARS cannot be overstated, because no prophylactic or therapeutic interventions were known to be effective against SARS at the time. Another critical adaptation was the establishment of a new SARS assessment unit leader and corresponding unit in temporary shelters outside the ED. This unit not only provided several new SARS-related functions in its three subunits, but its outdoor configuration enabled the expansion of ED isolation surge capacity without having to modify the existing ED structure or reduce patient care capacity in the already overcrowded ED. Another key adaptation was the creation of a new fever-screening subunit to screen for fever all persons entering the outpatient entrance of the hospital and the expansion of the triage unit’s function to screen for fever all persons entering the ED entrance of the hospital. Because these services were based in temporary areas outside the hospital, no changes were required in the hospital structure. Paralleling these efforts outside the hospital were the creation of the SARS isolation and critical care units inside the hospital for the management of patients with suspected and probable SARS and the isolation of febrile employees. The creation of these units within functionally overlapping areas enabled the production of in-hospital isolation surge capacity without a major disruption of patient care services.
Second, HEICS provided a predictable modular framework that helped NCKUH to logically determine where these new units and subunits were to be placed within the overall organization, enabling their rapid assimilation into the greater whole.
Third, the organizational flexibility of HEICS enabled NCKUH to keep six irrelevant units of response closed. Although these inactivated units may have been helpful during an earthquake or typhoon, they were unnecessary during the SARS outbreak, which did not cause structural damage to the hospital, generate large numbers of victims, produce victims with minor injuries, produce injuries that could be managed in a delayed manner, or displace dependents of hospital personnel.
Fourth, HEICS provided a hierarchical command and control structure that helped infection control policy at NCKUH rapidly evolve as the situation unfolded. Almost daily during the outbreak, the Taiwanese Center for Disease Control recommended new infection control policy to the infection control officer at NCKUH (2). In other cases, the infection control officer communicated directly with hospitals in Taipei, Hong Kong, and Singapore or accessed the Internet to learn from other’s experience with SARS (19). The infection control officer then used this information to make frequent policy recommendations for infection control at NCKUH to the EOC. The EOC considered these recommendations at their daily meetings and the incident commander made any final policy decisions. New or updated infection control policy was then promptly disseminated to relevant HEICS sections and units through the hospital intranet.
Fifth, HEICS provided a flexible mechanism that enabled NCKUH to customize the assignment of individuals to leadership positions based on the requirements of the event and the availability of personnel. For example, the chairman of the infection control committee not only assumed the role of infection control officer, but also that of operations chief, because the deputy superintendent, who would normally occupy this position, was absent from NCKUH during the entire outbreak (altogether, five individuals occupied more than one HEICS position each).
Sixth, HEICS provided a logical framework that assisted NCKUH in assigning and organizing job actions not anticipated in the baseline hospital emergency plan. During the SARS outbreak at NCKUH, every HEICS position was reported as having new job actions related to infection control (Table 2, Table 3, Table 4, Table 5). At a minimum, every HEICS unit leader had the responsibility to educate the unit members about infection control measures, ensure the use of adequate personal protective equipment (PPE), and monitor the unit personnel for fever (body temperature was checked twice per 8-h shift). Overall, many new job actions related to infection control were required, including activities related to patient isolation, traffic and perimeter control, decontamination, hand-washing, and fever screening.
Finally, HEICS provided a convenient mechanism for capturing key hospital emergency response activities according to the job actions of each HEICS position. Knowledge of job actions at NCKUH during the SARS outbreak may assist other hospitals seeking to use HEICS (Table 2, Table 3, Table 4, Table 5). In addition, this SARS outbreak demonstrated many of the features suggestive of a bioterrorist attack, including the aerosol spread of infection, predominate pulmonary pattern of disease, multiple patients with similar signs and symptoms, simultaneous presentation, multiple simultaneous outbreaks, and lack of an identified natural vector. Accordingly, an understanding of the implementation of HEICS at NCKUH may help emergency preparedness not only for future outbreaks of SARS, but also for intentional releases of contagious biological agents in susceptible populations (e.g., smallpox, pneumonic plague).
This study is also subject to several limitations. Our selection of potential survey participants as occupants of HEICS leadership positions may have led to omissions of information about critical actions performed by non-management personnel. Our structured interview methodology may have encouraged some participants to self-report more favorable versions of actions than were actually performed (recall bias). Our analysis of the descriptive data may be biased, because three of the authors also participated in the NCKUH emergency response. Our inability to directly survey five persons occupying HEICS leadership positions may have led to an incomplete description of the structure and function of HEICS during the outbreak. Moreover, we did not evaluate the perceived adequacy or success of HEICS by the participants at NCKUH. Finally, we did not evaluate the effectiveness of HEICS at NCKUH during the outbreak or compare HEICS with other systems of hospital emergency management. On one hand, only 38 patients were hospitalized with suspected or probable SARS during the outbreak at NCKUH, three of whom died, suggesting a low burden of disease. On the other hand, no cases of nosocomial transmission occurred at NCKUH, suggesting that the disease was successfully contained.
In conclusion, HEICS provides a flexible, predictable framework that seems to have facilitated the organization of hospital emergency response at NCKUH during the SARS outbreak in Taiwan, including the creation of new units and subunits of emergency response, the development of new infection control policies in response to the rapidly changing situation, and the implementation of new infection control measures throughout the hospital.
Footnotes
Selected Topics: Disaster Medicine is coordinated by Irving “Jake” Jacoby, md, of the University of California San Diego Medical Center, San Diego, California.
References
- 1.Centers for Disease Control Severe acute respiratory syndrome—Taiwan, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:461–466. [PubMed] [Google Scholar]
- 2.Twu SJ, Chen TJ, Chen CJ, et al. Control measures for severe acute respiratory syndrome (SARS) in Taiwan. Available at: www.cdc.gov/ncidod/EID. Accessed July 15, 2003. [DOI] [PMC free article] [PubMed]
- 3.World Health Organization. Cumulative number of reported probable cases of severe acute respiratory syndrome (SARS) from 1 November 2002 to 22 April 2003. Available at: www.who.int/csr/sarscountry. Accessed July 15, 2003.
- 4.World Health Organization. Probable cases of SARS by date of onset Taiwan, China, 1 February–10 July 2003 (n = 671). Available at: www.who.int/csr/sars/epicurve/epiindex/en/index5.html. Accessed July 15, 2003.
- 5.World Health Organization. Cumulative number of reported probable cases of severe acute respiratory syndrome (SARS) from 1 November 2002 to 23 May 2003. Available at: www.who.int/csr/sarscountry. Accessed July 15, 2003.
- 6.World Health Organization. Cumulative number of reported probable cases of severe acute respiratory syndrome (SARS) from 1 November 2002 to 16 June 2003. Available at: www.who.int/csr/sarscountry. Accessed July 15, 2003.
- 7.Pan D. WHO invites Taiwan to SARS conference. Available at: www.etaiwannews.com/Taiwan/2003/06/14/1055555732.htm Accessed July 8, 2003.
- 8.Cameron P.A., Ranier T.H. Update on emerging infections: news from the Centers for Disease Control and Infection. Ann Emerg Med. 2003;42:110–116. [PubMed] [Google Scholar]
- 9.Centers for Disease Control Cluster of severe acute respiratory syndrome cases among protected health-care workers—Toronto, Canada, April 2003. MMWR Morb Mortal Wkly Rep. 2003;52:433–436. [PubMed] [Google Scholar]
- 10.Centers for Disease Control Severe Acute Respiratory Syndrome—Singapore, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:405–411. [PubMed] [Google Scholar]
- 11.Centers for Disease Control Update: outbreak of severe acute respiratory syndrome—worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:226–228. [Google Scholar]
- 12.Centers for Disease Control Update: outbreak of severe acute respiratory syndrome—worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:241–248. [PubMed] [Google Scholar]
- 13.Centers for Disease Control Update: outbreak of severe acute respiratory syndrome—worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:269–272. [PubMed] [Google Scholar]
- 14.Lee N., Hui D., Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 15.Poutanen S.M., Low D.E., Henry B. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348:1995–2005. doi: 10.1056/NEJMoa030634. [DOI] [PubMed] [Google Scholar]
- 16.Tomlinson B., Cockram C. SARS: experience at Prince of Wales Hospital, Hong Kong. Lancet. 2003;361:1486–1487. doi: 10.1016/S0140-6736(03)13218-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ho W. Guideline on management of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1313–1315. doi: 10.1016/S0140-6736(03)13085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lapinsky SE, Hawryluck L. ICU management of severe acute respiratory syndrome. Available at: www.sars.medtau.org/article.htm Accessed June 1, 2003. [DOI] [PMC free article] [PubMed]
- 19.Li T.S.T., Buckley T.A., Yap F.H.Y., Sung J.J.Y., Joynt G.M. Severe acute respiratory syndrome (SARS): infection control. Lancet. 2003;361:1386. doi: 10.1016/S0140-6736(03)13052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.So L.K.Y., Lau A.C.W., Yam L.Y.C. Development of a standard treatment protocol for severe acute respiratory syndrome. Lancet. 2003;361:1615–1617. doi: 10.1016/S0140-6736(03)13265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seto W.H., Tsang D., Yung R.W.H. Effectiveness of precautions against droplets and contact of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnold J., O’Brien D., Walsh D. The perceived usefulness of the Hospital Emergency Incident Command System and an assessment tool for hospital disaster response capabilities and needs in hospital disaster planning in Turkey (abstract) Prehospital Disaster Med. 2001;16:s12. [Google Scholar]
- 23.EMS Authority of California. Available at: www.emsa.cahwnet.gov/heics3.htm. Accessed August 26, 2000.
- 24.Keim M. Key topics for emergency health education in the Pacific. Pac Health Dialog. 2002;9:104–108. [PubMed] [Google Scholar]
- 25.World Health Organization. World Health Organization changes travel recommendation for Taiwan province, China. Available at: www.who.int/mediacentre/notes/2003/np17/en/print.html. Accessed June 18, 2003.
- 26.World Health Organization. Case definitions for surveillance of severe acute respiratory syndrome (SARS). Available at: www.who.int/csr/sars/casedefinition/en. Accessed May 18, 2003.
- 27.Anderson P.B. A comparative analysis of the emergency medical services and rescue responses to eight airliner crashes in the United States, 1987–1991. Prehospital Disaster Med. 1995;10:142–153. doi: 10.1017/s1049023x00041923. [DOI] [PubMed] [Google Scholar]
- 28.Bissell R.A., Pretto E., Angus D.C. Post-preparedness medical disaster response in Costa Rica. Prehospital Disaster Med. 1994;9:96–106. doi: 10.1017/s1049023x00040991. [DOI] [PubMed] [Google Scholar]
- 29.Pretto E.A., Angus D.C., Abrams J.I. An analysis of prehospital mortality in an earthquake. Disaster Reanimatology Study Group. Prehospital Disaster Med. 1994;9:107–117. doi: 10.1017/s1049023x00041005. [DOI] [PubMed] [Google Scholar]
- 30.Ricci E., Pretto E. Assessment of prehospital and hospital response in disaster. Crit Care Clin. 1991;7:471–484. [PubMed] [Google Scholar]


