Abstract
Searches of the literature or Internet using the term “medical tourism” produce two sets of articles: travel for the purpose of delivering health care or travel for the purpose of seeking health care. The first usage primarily appears in the medical literature and is beyond the scope of this article, which focuses on travel to seek health care. Still, there are some aspects these two topics have in common: both are affected by ease and speed of international travel and communication associated with globalization, and both raise questions about continuity of care as well as issues related to cultural, language, and legal differences; both also raise questions about ethics. This article describes some of the motivating factors, contributing elements, and challenges in elucidating trends, as well as implications for clinicians who provide pretravel advice and those who care for ill returning travelers.
Keywords: Travel, Health seeking traveler, Medical tourism, Transplant tourism, Reproductive tourism
Searches of the literature or Internet using the term “medical tourism” produce two sets of articles: travel for the purpose of delivering health care or travel for the purpose of seeking health care. The first usage primarily appears in the medical literature.1, 2 Articles addressing the latter definition are beginning to appear in the medical literature but have become a common topic in the business sector,3 on the Internet,4, 5 and in the lay media.6, 7, 8 A full discussion of both aspects of medical tourism is beyond the scope of this article, which focuses on travel to seek health care, but there are some aspects in common: both are affected by ease and speed of international travel and communication associated with globalization, and both raise questions about continuity of care as well as issues related to cultural, language, and legal differences; both also raise questions about ethics.
Travel for the purpose of seeking health care is not new. There is a long history of travel to be near friends or family who can provide support during care and convalescence, or to seek more sophisticated or specialized care not available locally, often in a more developed area. “Medical tourism” refers primarily to a new phenomenon of travelers leaving family and friends to seek care abroad, often in less developed countries, along with the organizations that support or offer incentives for such travel. This article describes some of the motivating factors, contributing elements, and challenges in elucidating trends, as well as implications for clinicians who provide pretravel advice and those who care for ill returning travelers.
Globalization
International Travel
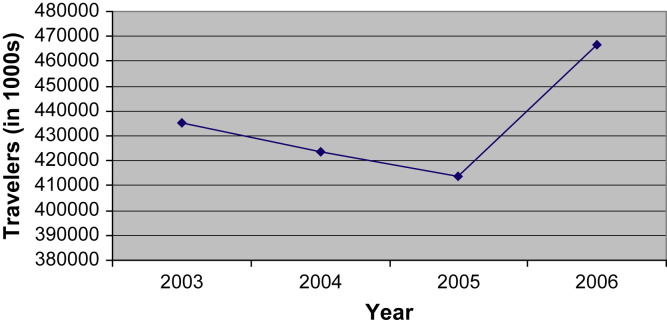
Exact measures of numbers of travelers involved in medical tourism are difficult to obtain. Data from the US Department of Commerce in-flight survey between 2003 and 2006 shows an overall increase in the number of trips taken, for which at least one purpose was health care (Fig. 1 ). In 2006 there were approximately half a million international trips in which health treatment was one purpose of the trip.9, 10, 11, 12
Fig. 1.
United States airline travelers to overseas and Mexico who report health treatment as one purpose of the trip, 2003–2006.
India has a specific category of nonimmigrant medical visa for visitors seeking health care;13, 14 however, figures for entrants in this category are not readily available and it is thought that medical tourists do not routinely use it, nor is it required. This visa category is available via the High Commission of India, London Web site15 but not from the Embassy of India in Washington D.C.16 The Confederation of Indian Industry (CII), in collaboration with international marketing consultants McKinsey and Company, produced a study on the country's medical tourism sector in 2002. Based on data from organization member hospitals, CII estimates that 150,000 medical tourists came to India in 2005, accounting for $22.2 billion in United States funds (USD) or 5.2% of the gross domestic product of India. This sector is anticipated to account for between $40 billion USD and $60 billion USD for India by 2012.5, 13 On its Web site homepage, Bumrumgrad Hospital in Bangkok, Thailand, reports treating 400,000 international patients annually.17
In 2004, United States citizens born in the United States made up 56% of all overseas air travelers outbound from the United States, but contributed a much smaller proportion (17%) of travelers who listed health treatment as the main purpose of the trip. The majority of health-seeking travelers that year were current United States citizens born outside the United States (46%), followed by non-United States citizens (36%).10 Residents born outside the United States have stated that health care needs, such as dentistry, are often included in visits home because of familiarity with care in the country of origin, the high cost of health care in the United States, and lack of insurance coverage.3, 18
Official estimates of the number of United States patients receiving care abroad are not available, as this type of care until recently has been paid for by the person. The introduction of insurance coverage may provide some data in the future. Media reports quote sources at individual facilities as opposed to official records and use different formats to report number of US patients. Estimates of the number of Americans seen at Bumrungrad in Bangkok range from 55,000 to 64,000 in 2006,8, 19 an 11% to 30% increase over 2005, and 83% of visits were for noncosmetic treatments.19 Approximately 850 United States patients were reportedly operated on in 2007 at two Wockhardt hospitals in Bangalore and Bombay, twice as many as in 2006.6 Another source estimates that 50,000 Americans travel each year for major noncosmetic surgery, such as joint replacement, coronary artery bypass, new or repaired heart valves, and back repair.20 As these are nonemergent, elective procedures it is not yet possible to determine if the recent fluctuations noted here and in Fig. 1 reflect true trends or events in the airline and travel industries. For example, following the severe acute respiratory syndrome (SARS) epidemic, travel to Asia was reduced in 2004 and travel may have been postponed, with a subsequent rebound of the accumulated number of trips in 2005 and 2006.
Role of the Internet
The Internet plays a major role in the growth of medical tourism as an industry, as it is the portal for exchange of information across continents between the prospective patients and providers.21 Enter a procedure name in a search engine and international options appear among local options. Enter a procedure name with the addition of the term “abroad” and 100,000 or more citations appear, offering direct connections to services in individual countries from Europe to Asia or entities that will offer assistance with every detail of travel.5, 22
Healthcare Trip (www.healthcaretrip.org), a United States-based 501 (c) (3) nonprofit service of health care Tourism International, reports it has assumed accreditation responsibility for all the major groups involved in the health tourism industry from hotels to recovery facilities, medical tourism booking agencies, and other resources, for nonclinical aspects of health tourism, such as language issues, business practices, and advertising. However, this site differs from other accrediting agency Web sites listed below in that advertisements for medical tourism providers appear in a box driven by the search engine. Registration is required to review the specific criteria and materials used.
Marketplace Issues
Outsourcing of medical treatment has been seen as an option by patients to bypass or reduce waiting time in Canada, Britain, and other countries in the European Union.5, 23, 24, 25 However, in the United States, cost is the primary motivating factor.5 The cost of individual procedures have been estimated to be 20% to 80% lower in less developed countries than in a private hospital in the United States; a hip replacement might be less than $10,000, compared with $40,000 to $50,000 in the United States.6, 7, 8 Patients with limited or no health insurance are attracted by the opportunity to conserve limited financial resources and protect the equity in their homes.19 In 2006, 47 million people, representing 15.6 % of the United States population, did not have health insurance. The proportion without insurance is even higher among the working population aged 18 to 64 at 20.2%, and also varies by nativity: 13.2% for native born citizens, 16.4% for naturalized citizens, and 45% for foreign-born noncitizens.18 Only 50% of Americans have dental insurance.26
Employers, particularly those that are self-insured, unions that manage their own health care resources, insurers, and even governments have also taken note and begun to investigate or provide outsourced medical care.7, 19 Their actions may take the form of including international facilities as preferred providers on low-premium mini-medical plans, which are increasingly popular with contract and hourly workers who are often uninsured, to traditional plans that will make all arrangements, allow a companion to accompany the patient, and include a recuperative stay in a hotel along with a rebate of the savings.7 The West Virginia legislature considered a bill that would offer similar incentives for public employees, and the United States Senate held hearings in June 2006 to examine whether medical tourism can reduce health care costs.7, 19, 27, 28 Some insurers have reportedly begun selling policies that include overseas care5 or are actively forming alliances with facilities in Thailand, Singapore, Ireland, Turkey, and Costa Rica, all accredited by the Joint Commission International (see below).29 Other carriers report cautious investigation, such as tailoring plans to include overseas options at the specific request of an employer.30, 31 The field is rapidly changing. The employer-based rebate plan,7 which formed the basis of the West Virginia proposal, was reportedly discontinued by the next year because of displeasure voiced by the employee union.30 The Internal Revenue Service has also taken note: amounts paid by a group health plan for medical procedures are not taxable to employees, but the issues are less clear around provision of lodging, transportation, and even the cash rebates in self-insured or fully-insured situations.30
Few consumers in a recent poll would elect surgery abroad for incentives below $1,000. Above that, 45% of persons without insurance or who are underinsured and 19% of persons with insurance and an ill family member would travel; those numbers jump to 61% and 40%, respectively, above $5,000.7 It has been suggested that, to balance patient safety and cost savings, nonurgent, short-duration procedures costing more than $15,000 to $20,000, for conditions that are not exacerbated by air travel, be the threshold for outsourcing. This would primarily include major cardiac and orthopedic conditions, which currently account for only about 2% of United States noncosmetic health care (excluding those who live on the United States-Mexico border).19
Types of Care
Distinctions are frequently made between reproductive care, dental care, cosmetic versus noncosmetic surgery, and transplantation.19, 32 Executive check-ups are also becoming popular.8
Reproductive tourism encompasses travel for pregnancy termination and fertility treatment.21 Both are heavily regulated globally, but the lack of regulation in some aspects of infertility treatments (ie, they are generally not covered by public or private health plans) may allow the costs to vary so widely.33, 34 It is a constantly changing arena, and when airfares to and from the United States were lower, “medical cartographers” set out to map which places were “best” (in terms of cost, effectiveness and timeliness), for what procedures and for whom.35 The desperation of many infertile couples and the developing market for donated eggs raise issues similar to that of transplantation tourism on safety for the recipient, in terms of infections, and protection of donors or surrogates from exploitation.36 Adverse events associated with medical tourism for any purpose are primarily anecdotal media accounts; for infertility treatment, these reports concern lack of viable pregnancy, exhaustion of resources, and speculation regarding the health of the donor or surrogate.37
Poland, Hungary, other countries in Eastern Europe, and the Caribbean, Central and South America are mentioned in regard to dental procedures. Costs in developed areas may range from $1,000 for a root canal to 50 times that for multiple crowns.8, 26 As this type of dental care is usually not emergent, it can be bundled into a vacation or a trip home for many immigrants.3, 38, 39 Advertising for care, particularly dental and cosmetic, in immigrant communities reportedly appears in the local native language media, such as newspapers and radio, to a greater extent than the Internet (M. Vega, personal communication, March 8, 2004).40
Dentistry also crosses over into the area of cosmetic procedures and provides a useful example of the two main categories of outsourced care and how they differ. Root canals, just as joint replacements and cardiac by-passes, are therapeutic procedures recommended by clinicians to treat a specific problem based on a diagnostic evaluation that must either be shared with the treating clinician or repeated at the destination. Esthetic procedures are primarily patient driven. For patients who travel abroad for therapeutic procedures, quality is an equal concern with cost. There are issues related to whether a local physician at the patient's home will be comfortable or not providing immediate postprocedure follow-up, but that would also be true if a the patient traveled to another part of the United States. Patients seek cosmetic procedures for issues with appearance; results are subjective and may not be final until healing is complete.41, 42, 43, 44, 45 It is in the cosmetic surgery literature that the majority of adverse events have been noted.
Quality of care
The American Medical Association developed guiding principles for employers, insurance companies, and other entities that facilitate or offer incentives for care outside the United States. These principles that were recently adopted at the June 17, 2008, annual session. The principles stipulate that international care must be voluntary and provided by accredited institutions; financial incentives should not inappropriately limit or restrict patient options; there should be continuity of care, including coverage of costs upon return; patients should be informed of their rights and legal recourse before travel; patients should have access to licensing, outcome, and accrediting information when seeking care; medical record transfers should comply with Health Insurance Portability and Accountability Act guidelines; and patients should be informed of potential risks of combining surgical procedures with long flights and vacation activities.4, 46
On, June 18, 2008, the American College of Surgeons (ACS), which already had a public section of its Web site devoted to information for patients about choosing a surgeon, qualifications, and second opinions, also took note of the phenomenon. A 14-bullet report summarizing available information and Internet resources was posted on its new Nora Institute for Surgical Patient Safety Web site, supplemented with a list of the 17 country Web sites that promote and the 20 United States-based companies that specialize in medical tourism, along with a cost comparison.32
The American Society for Plastic Surgery Web site has posted information on medical tourism since early April 2005, with a briefing paper that emphasizes plastic surgery is “real” surgery and outlines the issues every patient undergoing surgery should consider, whether at home or abroad, particularly when combined with travel.47 The International Society of Plastic Surgery also certifies approximately 1,500 surgeons in 73 countries who meet United States standards (www.isaps.org). The American Dental Association covers travel, dental care, and “dental tourism” on its Web site and provides a link to “A traveler's guide to dental care,” which is available through the Global Dental Safety Organization for Safety and Asepsis Procedures (www.osap.org).48
Accreditation
In October 2004, the World Health Organization (WHO) launched the World Alliance for Patient Safety in response to a World Health Assembly Resolution (2002) urging WHO and Member States to pay the closest possible attention to the problem of patient safety (who.int/patientsafety/en). Countries have or are in the process of developing national programs to survey facilities for performance on a range of quality-of-care indicators. In India, 35 hospitals had applied for accreditation to the Ministry of Health by March 2007, and 30 of 120 had been certified under the CII system, which has an ethical code but self-regulates by establishing a system for its own members. As of July 2008, nine Indian facilities and facilities in 31 other countries have also voluntarily applied for and been accredited by an external organization, the Joint Commission International (JCI) (www.jointcommissioninternational.org), the international arm of the Joint Commission that accredits United States facilities. The International Society for Quality in Health Care (www.isqua.org) is an umbrella organization that accredits JCI and similar organizations that have also developed international components in the last few years in response to increasing global interest, such as the Trent International Accreditation Scheme (www.trentaccreditationscheme.org), which recently expanded from the United Kingdom to include private hospitals in Hong Kong; the Australian Council for Healthcare Standards International (www.achs.org.au/ACHSI/); and the Canadian Council on Health Services (www.cchsa.ca). The Society for International Healthcare Accreditation (www.sofiha.co.uk/index.htm), “devoted towards the development and promulgation of high-quality accreditation of hospitals and healthcare facilities across international borders,” was also formed recently in response to the increase in medical tourism, and is open to both the public and health care providers interested in international accreditation.
Individuals researching accreditation status should note that, although facilities may be part of a chain, they are surveyed and accredited individually. They should also check the duration of the accreditation and validate that the information is current by consulting the public portion of the appropriate accrediting agency Web site.
Facilities and Staff
The first private hospital opened in India in 1983. As of 2008 it was part of a chain with 41 hospitals in two countries and claimed 10 million patients from 55 countries.49 Such facilities may have allowed local physicians to return home and practice medicine, as they had been trained in developed areas such as North America and Europe. For India it has been postulated that the quality of the local medical schools, a low cost of living, family preferences, and the barriers to foreign accreditation may mean that Indian doctors may prefer to work in India rather than elsewhere, allowing this growth in patient-care capacity.3 The fact that English is commonly spoken and that many of the clinicians trained in institutions familiar to their North American patients are both factors in site selection by United States-born patients, who may have never traveled internationally before.3, 7, 8
Ethics
The lower costs in developing countries are thought to be the result of a lower cost of living, lower wages paid to physicians and other health care workers, low administrative costs and medico-legal expenses, and cheaper prices offered by global suppliers of medical devices.5, 19 The Indian government has offered financial incentives by defining medical care for tourists as an “export,” giving it special tax status along with other related projects, such as building airports and promoting health infrastructure.23 However, World Bank support for building a private hospital in India recently raised concerns that it was diverting resources from government run health services in a country where, according to the 2005 Reproductive and Child Health Facility Survey, fewer than 50% of the primary health centers have a labor room or a laboratory, only one in five have a telephone connection, and fewer than one in three stock essential drugs.13 There is concern that privatization is diverting resources away from the local poor.23 Widening access, improving quality across all strata, and ensuring nonexploitive prices have been identified as measures to ensure that citizens of developing countries will also benefit from developments of a private health care structure beyond the 10% in pro bono care such institutions may provide; whether the public sectors are sufficient to the task is currently a subject of debate. The short waiting time for procedures in these densely populated countries implies that the costs of the services, though correlated with the nations per capita gross domestic product, may still be above the means of the majority of the local population.5, 50
Organ Transplantation
In the United States, there is a single system for organ procurement and transplantation coordinated under congressional mandate by the United Network for Organ Sharing, a nonprofit, scientific, and educational organization. As of July 18, 2008, there were 9,029 transplants between January and April from 4,578 donors with 99,393 candidates on the waiting list (www.optn.org). The need for transplantable organs far exceeds the available supply and travel to a country with less rigorous methods of distribution has been termed “transplant tourism” or “organ trafficking.”51 The 2007 United States Annual Report includes a study by Marion and colleagues, that has been published separately,52 on transplant tourism. It examines transplants in foreign countries among patients removed from the United States waiting list from 1986 to 2006. Patients are removed from the US waiting list when they receive a transplant in the United States, die before receiving a transplant, or they can self-elect to remove their name from the list to seek care outside the United States. The majority (89.3%) of the 373 foreign transplants were kidney. Between 2001 and 2006 the annual number of waiting-list removals increased. Recipients of foreign transplants were significantly more likely to be male, college educated, nonresident or resident alien, and 10 times more likely to be Asian and self-funded. Forty-two percent of the transplants occurred in East Asia and the Pacific, with three countries accounting for one half of all foreign transplants: China (26%), Philippines (12%), and India (10%). The report states “…it is possible and indeed probable that instances of organ buying, selling, and/or trafficking outside the U.S. occurred. On the other hand, bona fide emotionally and/or biologically related living donor transplants were likely done. For example, U.S. citizens as well as resident and non-resident aliens may have friends or relatives in their country of origin who are unable to come to the U.S. to donate because of restrictive policies governing the issuance of travel visas.” Conversely, an analysis of kidney and liver transplants to nonresident aliens in the United States, although small in number, shows that these liver candidates had shorter times to transplant and the self paying had the shortest time.53 In an accompanying commentary entitled “‘Transplant Tourism’ in the United States?” the author makes the point that foreign nationals are paying for access to organs, which should cause inward reflection on condemnation of other transplant enterprises. It also demonstrates that the developed world has the opportunity to measure and report on the extent of the behavior and provide outcome results. The author also notes that the National Task Force on Transplantation that developed the United States system in 1986 stated that deceased donor organs were a “national resource,” but did not envision the globalization that has transpired in the interim. Shortages are a universal problem and reliance on deceased organs, even in a well-developed program such as Spain's, can only meet 50% of the demand. Thus, other models involving living donors, which could be regulated, prevent organ vending, and protect the donor, have been proposed for discussion in a series of recent articles.54, 55, 56 Transparency, where there is so much potential to exploit, is key.56, 57, 58
Adverse events
Little is known about the outcomes of medical care abroad.
Infectious Complications
The coordination of the United States transplant network lends itself to identification of patients who undergo transplantation outside the system, as noted above. One United States center identified 10 patients who underwent transplantation outside the United States during the period September 16, 2002 to June 30, 2006, and returned to the same center for care. Three patients had indicated they intended to seek transplantation abroad. Two patients were seen in the emergency room on the day of arrival in the United States. Complications were primarily infectious, with six infections in four patients: severe wound infection with acinetobacter (one); sepsis (three); cytomegalovirus (CMV) (one); and central nervous system aspergillus (one). Nine of the 10 grafts survived, as did 9 of the 10 patients, which is consistent with results obtained for patients transplanted in the United States and from a much larger series of patients, who had also traveled for the purpose of transplantation, reported on from Malaysia (n = 515) at about the same time.59, 60 However, an Australian series of 16 patients who had traveled overseas for commercial transplantation had survival rates at 1 and 5 years that were lower when compared with Australian living-donor transplants.61 Two of the 16 contracted Hepatitis B virus (HBV) abroad, three were hospitalized for acute CMV infection shortly after return home, and one had aspergillus infection of the graft and multiresistant Pseudomona aeruginosa of the surgical wounds. In the Malaysian study there were significant rates of infection, but they did not differ between the living related donor (n = 258) transplanted in Malaysia, the commercial living donor (n = 389), or commercial cadaveric donor (n = 126) transplanted abroad. The infection rates were: bacterial <=35%; viral <=26%; HCV <=17%; HBV <=12%; fungal <=7%; Mycobacterium tuberculosis, CMV and malaria <5%. There were no HIV infections. Case reports such as this are affected by survivorship bias related to those patients who did not return for unknown reasons, and differences of endemic rates of infection in the population with such agents as HBV. One must be careful to examine the year of study when comparing rates of infection with HIV, as prior studies may include patients transplanted in early time periods.61
There are also individual reports of HBV acquired during elective procedures performed overseas; denominator data are difficult to derive and the ability to identify the precise source of infection is also limited. However, Harling and colleagues62 reported an outbreak of HBV in the United Kingdom linked to a patient who had acquired his infection during a renal transplant in India. During the investigation, two additional hospitals identified three other sporadic cases of HBV that had also apparently been acquired during hemodialysis in South Asia. The prevalence of chronic HBV infection in India is less than 2% to 7% and in Malaysia, China, and most of Asia it is greater than 8%.63
Recognition of an outbreak or common source exposure is difficult as patients are seen in a variety of localities upon return. However, posting of unusual cases or questions via electronic listserves has resulted in recognition of links between cases of non-tuberculosis wound infections in 20 United States patients undergoing cosmetic surgery procedures, ranging from abdominoplasty, liposuction, breast lift, and breast reduction to breast implant in the Dominican Republic.64, 65, 66, 67 In a 2005 electronic survey of infectious disease specialists in North America, 6% of the 425 respondents indicated that they or their colleagues encountered infectious complications of cosmetic surgery performed outside the United States in the previous year.68 Systematic data on the rates of infection after cosmetic surgery with M. abscessus in the United States are not available for comparison with other countries. Outbreaks of fast growing mycobacterial species have been reported in the United States;69, 70 however, a review of the records at New York Presbyterian Hospital Columbia University Medical Center for the period 2000 to 2005 found only eight infections with M. abscessus, all in patients who had undergone cosmetic surgery in the Dominican Republic. For the same time period, there were no other postsurgical wound infections at two of the sites where patients were seen among the more than 230,000 surgical procedures at Columbia or the fewer than 60,000 at Baystate Medical Center. Possible sources of infection, stated in the report, would be environmental contamination of water sources, surgical instruments, Gentian violet, injectable medications, and antiseptic solutions. At least one patient in this series had been instructed to use tap water for irrigation.
The risk of nosocomial infections in intensive care is estimated to be 25% in developed areas but twice that, between 25% and 40%, in developing countries. In a study by the WHO reported in 2008, it was estimated that 37% to 70% of injections worldwide were given with reused syringes without sterilization, putting patients at risk for blood-borne infections, 70% of medications in developing countries did not meet standards, and 22% of blood donations were not screened for HIV infection. Counterfeit medications accounted for 10% of the global medicines market worldwide and up to 30% of medicines consumed in developing countries.71
Noninfectious Complications
The Australian Society of Plastic Surgeons conducted a national survey in April 2007 regarding women returning from Asia after holiday and requiring treatment for medical complications from surgery, during the previous three years. Of the 68 surgeons surveyed, 40 (59%) reported seeing patients with complications or poor results and 15 (22%) reported treating more than one patient. Most women seeking treatment had undergone breast enlargements or reductions or facelifts. The majority of procedures were reportedly performed in Thailand (66), followed by Malaysia (17).72
The issue of who should bear the costs of complications was raised in a report from Australia of Mycobacterium fortuitum infection of a total knee arthroplasty, performed in India.73 The patient had been advised to pursue a course of symptomatic treatment for osteoarthritis but elected to pay $8,600 for the surgical option over concerns of waiting time in the public sector, cost in the private sector, and desire for early return to work. Treatment for the septic joint, with an organism not commonly encountered in Australia, involved four separate surgeries and antimycobacterial therapy, resulting in a cost of $140,000. The procedure had been done in a hospital accredited by the JCI, rates of infection in the procedure worldwide are known to be 1% to 2%, and it was acknowledged that even if 1 patient in 20 develops an infection, having the operation overseas is an economically viable option. However, the case illustrates many of the issues in medical tourism: exposure to infections of different types or higher prevalence than at home, the lack of ability to address the root source of adverse events and effect change, the wisdom of undertaking major surgery away from one's home environment (especially when long-haul air travel before major surgery significantly increases the risk of perioperative venous thromboembolism74), and in the event a complication does occur, the fairness of using resources that could fund procedures for multiple patients to treat one who had disregarded medical advice. Patients in this situation have little legal recourse75 and may also encounter a radically different cultural framework of reference, based in part on the local perception of an individual's decision to seek care away from home. The president of the Society of Plastic and Reconstructive Surgeons of Thailand is quoted as saying that all plastic surgery is “improvement not perfection,” and patients must realize there are drawbacks to traveling to another country for medical care. “How can a doctor look after patients if they go back to their country? You have to accept there are disadvantages if something goes wrong.”76
Summary
This rapidly evolving area is full of nuances, contradictions and contrasts; few general statements can be made and there is a general dearth of data. For example, many of the same countries profiled as top destinations for medical tourists seeking care are also profiled on the American College of Surgeons Web site link (www.operationgivingback.facs.org), where health care professionals at all stages of their surgical career can search for opportunities to volunteer as the other type of medical tourist, the health care worker who travels to provide medical care. New Orleans is also on the list of destinations, and as the Web site is open source, international surgeons could consider volunteer opportunities in the United States best suited to their expertise and interests here. However, regardless of their level of skill, physicians and surgeons interested in providing medical care in other countries may face legal barriers regarding licensing, structures that have been put in place to establish standards with the goal of protecting patients. Health care that involves invasive procedures is not without risk even in developed countries. The recent investigation of hepatitis C at an endoscopy clinic in Las Vegas has demonstrated how standards are necessary but not sufficient, even in developed areas.77 Recognition of the common source and subsequent gaps in basic infection-control practices were possible because, as a result of vaccination, rates of hepatitis in the United States have declined to the point where individual cases can be investigated.78 These public health and legal checks and balances provide valuable insight but also add to health care costs,79 and although outbreaks receive wide attention, the majority of cases of hepatitis in the United States are now imported by travelers from developing parts of the world.78
It has been said we live in a global village. Medical tourism demonstrates how dynamic the boundaries of the village seem to be and how transit between countries, particularly between country of birth and country of residence, affects health in both areas. The patient having a check-up before visiting a child studying abroad may also plan to have major dental procedures and be of an age to have missed both natural exposure and vaccination programs for hepatitis A or B, be unaware of prevalence rate and vaccination practices at the destination, and be convinced that he or she can tell whether the facility is safe just “by looking,” particularly when significant cost savings are at stake. The field is changing constantly; some international sites now describe care not just for adults but children, particularly for what are perceived as cosmetic procedures, such as orthodontics.22 Physicians should either be familiar with up-to-date sources of information (eg, www.cdc.gov/travel) or referral options, and inquire whether or what role travel plays in their patient's life.
Acknowledgments
The author is indebted to Harvey Lipman for statistical support with the analysis of the US Department of Commerce data.
Footnotes
The opinions expressed by the author do not necessarily reflect the opinions of the Centers for Disease Control and Prevention, 1600 Clifton Road, MS E-04, Atlanta, GA 30333, USA.
References
- 1.Bishop R., Litch J.A. Medical tourism can do harm. BMJ. 2000;320(7240):1017. doi: 10.1136/bmj.320.7240.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morgan M.A. Another view of “humanitarian ventures” and “fistula tourism”. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(6):705–707. doi: 10.1007/s00192-007-0309-9. [DOI] [PubMed] [Google Scholar]
- 3.Lagace M. The rise of medical tourism Harvard Business School Working Knowledge. Available at: http://hbswk.hbs.edu/item/5814.html. Accessed July 14, 2008.
- 4.American Medical Association. AMA provides first ever guidance on medical tourism. http://www.ama-assn.org/ama/pub/category/18678.html Available at: Accessed July 15, 2008.
- 5.Horowitz M.D., Rosensweig J.A., Jones C.A. Medical tourism: globalization of the healthcare marketplace. MedGenMed. 2007;9(4):33. [PMC free article] [PubMed] [Google Scholar]
- 6.Comarow A. Under the knife in Bangalore. US News World Rep. 2008;144(13) 42,45,47–50. [PubMed] [Google Scholar]
- 7.Kher U. Outsourcing your heart. Time. 2006;167(22):44–47. [PubMed] [Google Scholar]
- 8.Mecir A., Greider K. Traveling for treatment. AARP Bulletin. 2007;48(8):12–16. [Google Scholar]
- 9.US Department of Commerce. Office of Travel and Tourism Industries survey of international air travelers US to overseas and Mexico 2006 report, 2006 January–December. 2007.
- 10.US Department of Commerce. Office of Travel and Tourism Industries survey of international air travelers US to overseas and Mexico by birth and citizenship 2004 report, 2004 January–December. 2005.
- 11.US Department of Commerce. Office of Travel and Tourism Industries survey of international air travelers US to overseas and Mexico 2005 report, 2005 January–December. 2006.
- 12.US Department of Commerce. Office of Travel and Tourism Industries survey of international air travelers US to overseas and Mexico by birth and citizenship. 2003 report, 2003 January–December. 2005.
- 13.Chinai R., Goswami R. Medical visas mark growth of Indian medical tourism. Bull World Health Organ. 2007;85(3):164–165. doi: 10.2471/BLT.07.010307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Travel India Company Medical tourism in India. 2006. http://www.indian-medical-tourism.com/medical-visa-india-tourism.html Available at: Accessed July 6, 2008.
- 15.High Commission of India L. Visa application center in the United Kingdom. Available at: http://in.vfsglobal.co.uk/visacategory.aspx. 2008. Accessed July 22, 2008.
- 16.Embassy of India WDC. India Visa Center. Available at: https://indiavisa.travisaoutsourcing.com/requirements/gather?apply=bymail. 2008. Accessed July 22, 2008.
- 17.Bumrungrad International Hospital Overseas Medical Care. 2008. http://www.bumrungrad.com/Overseas-Medical-Care/Bumrungrad-International.aspx Available at: Accessed July 15, 2008.
- 18.US Census Bureau. Income, Poverty, and Health Insurance Coverage in the United States: 2006. In: DeNavas-Walt C, Proctor B, Smith J, editors. Current Population Reports. Available at: http://www.census.gov/prod/2007pubs/p60-233.pdfP60-233 Accessed July 22, 2008.
- 19.Milstein A., Smith M. America's new refugees—seeking affordable surgery offshore. N Engl J Med. 2006;355(16):1637–1640. doi: 10.1056/NEJMp068190. [DOI] [PubMed] [Google Scholar]
- 20.Woodman J. Patients without borders. http://www.patientsbeyondborders.com/ Available at: Accessed July 22, 2008.
- 21.Reed CM. The Health-Seeking Traveler. In: Keystone JS, Kozarsky P, Conner B, et al, editors. Travel Medicine. 2nd edition. Philadelphia: Elsevier Ltd.; 2008. p. 343–50.
- 22.Health Travel Guides. 2007. http://www.healthtravelguides.com/_Content/HTG/Default.aspx Available at: Accessed July 22, 2008.
- 23.Oxford Analytica North America: ‘Medical tourism’ industry grows rapidly. 2006. http://www.oxan.com/display.aspx?ItemID=DB129920 Available at: Accessed February 15, 2008.
- 24.Stargardt T. Health service costs in Europe: cost and reimbursement of primary hip replacement in nine countries. Health Econ. 2008;17(1 Suppl):S9–S20. doi: 10.1002/hec.1328. [DOI] [PubMed] [Google Scholar]
- 25.Beecham L. British patients willing to travel abroad for treatment. BMJ. 2002;325(7354):10. doi: 10.1136/bmj.325.7354.10/c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colliver C. Dental work too expensive? Go overseas. 2006. http://www.sfgate.com/cgi-bin/article.cgi?file=/c/a/2006/04/05/MNGHSI3N671.DTL Available at: San Francisco Chronicle. Accessed July 22, 2008.
- 27.US Senate 109th Congress. The globalization of health care: can medical tourism reduce health care costs? Available at: http://www.gpoaccess.gov/chearings/109scat1.html. 109–26. 2006. Special Committee on Aging. Accessed July 22, 2008.
- 28.Schadler E., Martin T., Ellem C. West Virginia Public Employees Insurance Act. 2007. http://www.legis.state.wv.us/Bill_Text_HTML/2007_SESSIONS/RS/BILLS/hb2841%20intr.htm Available at: HB 2841. Accessed July 22, 2008.
- 29.Einhorn B. Medical travel is going to be part of the solution. Business Week. 2008 Available at: http://www.businessweek.com/globalbiz/content/mar2008/gb20080312_835774.htm. Accessed March 13, 2008. [Google Scholar]
- 30.Higgins L.A. Medical tourism takes off, but not without debate. Manag Care. 2007;16(4):45–47. [PubMed] [Google Scholar]
- 31.Carroll J. Aetna and Hannaford make a Singapore connection. Manag Care. 2008;17(3):44–47. [PubMed] [Google Scholar]
- 32.Unti J. Medical Tourism Report to the American College of Surgeons Patient Safety and Quality Improvement Committee. Nora Institute for Surgical Patient Safety, editor. 2008. Available at: http://www.surgicalpatientsafety.facs.org/news/medicaltourism.html. Accessed July 22, 2008.
- 33.Spar D. Reproductive tourism and the regulatory map. N Engl J Med. 2005;352(6):531–533. doi: 10.1056/NEJMp048295. [DOI] [PubMed] [Google Scholar]
- 34.Spar D.L. Where babies come from: supply and demand in an infant marketplace. Harv Bus Rev. 2006;84(2) 133–140, 142–3, 166. [PubMed] [Google Scholar]
- 35.Jones C.A., Keith L.G. Medical tourism and reproductive outsourcing: the dawning of a new paradigm for healthcare. Int J Fertil Womens Med. 2006;51(6):251–255. [PubMed] [Google Scholar]
- 36.Reuters. Experts say reproductive tourism a growing worry. Available at: http://uk.reuters.com/article/UKNews1/idUKL2492408820080724. 2008. Accessed July 24, 2008.
- 37.Leigh S. Reproductive ‘tourism’. http://www.usatoday.com/news/health/2005-05-02-reproductive-tourism_x.htm Available at: Accessed July 22, 2008.
- 38.Marklein M. The inciDENTAL tourist. Available at: http://www.usatoday.com/travel/news/2005-07-28-dental-tourism_x.htm. 2005. USA Today. Accessed July 22, 2008
- 39.Schlecht N. Face lift, luxury safari—bargain price. 2008. http://www.cnn.com/2008/LIVING/wayoflife/01/03/lipo.tourism/index.html?iref=newssearch Available at: Accessed July 22, 2008.
- 40.Bienvenidos Ortho Oral 2007. http://www.orthooral.com/ Available at: Accessed July 22, 2008.
- 41.Goddard J.C., Vickery R.M., Terry T.R. Development of feminizing genitoplasty for gender dysphoria. J Sex Med. 2007;4(4 Pt 1):981–989. doi: 10.1111/j.1743-6109.2007.00480.x. [DOI] [PubMed] [Google Scholar]
- 42.Grossbart T.A., Sarwer D.B. Psychosocial issues and their relevance to the cosmetic surgery patient. Semin Cutan Med Surg. 2003;22(2):136–147. doi: 10.1053/sder.2003.50013. [DOI] [PubMed] [Google Scholar]
- 43.Liao L.M., Creighton S.M. Requests for cosmetic genitoplasty: how should healthcare providers respond? BMJ. 2007;334(7603):1090–1092. doi: 10.1136/bmj.39206.422269.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Most S.P., Alsarraf R., Larrabee W.F., Jr. Outcomes of facial cosmetic procedures. Facial Plast Surg. 2002;18(2):119–124. doi: 10.1055/s-2002-32202. [DOI] [PubMed] [Google Scholar]
- 45.Sarwer D.B. The psychological aspects of cosmetic breast augmentation. Plast Reconstr Surg. 2007;120(7 Suppl 1):110S–117S. doi: 10.1097/01.prs.0000286591.05612.72. [DOI] [PubMed] [Google Scholar]
- 46.Wapner J. American Medical Association provides guidance on medical tourism. Available at: http://elib2.cdc.gov:2138/cgi/content/full/337/jun30_1/a575. Accessed October 16, 2008. [DOI] [PubMed]
- 47.American Society of Plastic Surgeons Medical Tourism. 2005. http://www.plasticsurgery.org/patients_consumers/patient_safety/Medical-Tourism.cfm Available at: Accessed July 22, 2008.
- 48.American Dental Association Dental care away from home. 2008. http://www.ada.org/public/manage/care/index.asp Available at: Accessed July 27, 2008.
- 49.Apollo Hospitals home page 2008. http://www.apollohospitals.com/ Available at: Accessed July 21, 2008.
- 50.Zwi A.B., Brugha R., Smith E. Private health care in developing countries. BMJ. 2001;323(7311):463–464. doi: 10.1136/bmj.323.7311.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Health Resources and Services Administration. 2007 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1997–2006. 2007. Rockville, MD, Healthcare Systems Bureau, Division of Transplantation. Available at: http://www.optn.org. Accessed July 22, 2008.
- 52.Merion R.M., Barnes A.D., Lin M. Transplants in foreign countries among patients removed from the US Transplant Waiting List. Am J Transplant. 2008;8(4 Pt 2):988–996. doi: 10.1111/j.1600-6143.2008.02176.x. [DOI] [PubMed] [Google Scholar]
- 53.Schold J.D., Meier-Kriesche H.U., Duncan R.P. Deceased donor kidney and liver transplantation to nonresident aliens in the United States. Transplantation. 2007;84(12):1548–1556. doi: 10.1097/01.tp.0000296289.69158.a7. [DOI] [PubMed] [Google Scholar]
- 54.Barsoum R.S. Trends in unrelated-donor kidney transplantation in the developing world. Pediatr Nephrol. 2008;23(11):1925–1929. doi: 10.1007/s00467-008-0858-2. [DOI] [PubMed] [Google Scholar]
- 55.Ghods A.J., Nasrollahzadeh D. Transplant tourism and the Iranian model of renal transplantation program: ethical considerations. Exp Clin Transplant. 2005;3(2):351–354. [PubMed] [Google Scholar]
- 56.Oleksyn V. Top transplant surgeons involved in organ trafficking, expert says. Available at: http://www.bookrags.com/news/top-transplant-surgeons-involved-in-moc/. Accessed July 22, 2008.
- 57.Freeman R.B. “Transplant tourism” in the United States? Transplantation. 2007;84(12):1559–1560. doi: 10.1097/01.tp.0000296818.13150.aa. [DOI] [PubMed] [Google Scholar]
- 58.Shimazono Y. The state of the international organ trade: a provisional picture based on integration of available information. Bull World Health Organ. 2007;85(12):901–980. doi: 10.2471/BLT.06.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Canales M.T., Kasiske B.L., Rosenberg M.E. Transplant tourism: outcomes of United States residents who undergo kidney transplantation overseas. Transplantation. 2006;82(12):1658–1661. doi: 10.1097/01.tp.0000250763.52186.df. [DOI] [PubMed] [Google Scholar]
- 60.Morad Z., Lim T.O. Outcome of overseas kidney transplantation in Malaysia. Transplant Proc. 2000;32(7):1485–1486. doi: 10.1016/s0041-1345(00)01300-2. [DOI] [PubMed] [Google Scholar]
- 61.Kennedy S.E., Shen Y., Charlesworth J.A. Outcome of overseas commercial kidney transplantation: an Australian perspective. Med J Aust. 2005;182(5):224–227. [PubMed] [Google Scholar]
- 62.Harling R., Turbitt D., Millar M. Passage from India: an outbreak of hepatitis B linked to a patient who acquired infection from health care overseas. Public Health. 2007;121(10):734–741. doi: 10.1016/j.puhe.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 63.Fiore A, Bell B. Hepatitis, viral, type B. In: Arguin P, Kozarsky P, Reed C, editors. Health information for international travel 2008. Atlanta (GA): US Department of Health and Human Services, Public Health Services; 2007. p. 165.
- 64.CDC Nontuberculous mycobacterial infections after cosmetic surgery—Santo Domingo, Dominican Republic, 2003–2004. MMWR Morb Mortal Wkly Rep. 2004;53(23):509. [PubMed] [Google Scholar]
- 65.Newman M.I., Camberos A.E., Ascherman J. Mycobacteria abscessus outbreak in US patients linked to offshore surgicenter. Ann Plast Surg. 2005;55(1):107–110. doi: 10.1097/01.sap.0000168030.87804.93. [DOI] [PubMed] [Google Scholar]
- 66.Newman M.I., Camberos A.E., Clynes N.D. Outbreak of atypical mycobacteria infections in U.S. Patients traveling abroad for cosmetic surgery. Plast Reconstr Surg. 2005;115(3):964–965. doi: 10.1097/01.prs.0000153818.99552.cc. [DOI] [PubMed] [Google Scholar]
- 67.Furuya E.Y., Paez A., Srinivasan A. Outbreak of Mycobacterium abscessus wound infections among “lipotourists” from the United States who underwent abdominoplasty in the Dominican Republic. Clin Infect Dis. 2008;46(8):1181–1188. doi: 10.1086/529191. [DOI] [PubMed] [Google Scholar]
- 68.Sunenshine RH. Complications of lipotourism: infectious complications of cosmetic procedures and lipotourism—experience of infectious disease consultants [abstract 145]. In: Program and abstracts of the 16th Annual Scientific Meeting of The Society for Healthcare Epidemiology of America (Chicago). Arlington, VA: The Society for Healthcare Epidemiology of America, 2006:106. 2008.
- 69.Meyers H., Brown-Elliott B.A., Moore D. An outbreak of Mycobacterium chelonae infection following liposuction. Clin Infect Dis. 2002;34(11):1500–1507. doi: 10.1086/340399. [DOI] [PubMed] [Google Scholar]
- 70.Safranek T.J., Jarvis W.R., Carson L.A. Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentian violet skin-marking solution. N Engl J Med. 1987;317(4):197–201. doi: 10.1056/NEJM198707233170403. [DOI] [PubMed] [Google Scholar]
- 71.WHO Summary of the evidence on patient safety: implications for research. http://www.who.int/patientsafety/information_centre/20080523_Summary_of_the_evidence_on_patient_safety.pdf Available at: Accessed July 22, 2008.
- 72.Metlikovec J. Warning on cheap “holiday” surgeries. 2007. http://www.news.com.au/travel/story/0,00.html, 26058 Available at: Accessed July 22, 2008.
- 73.Cheung I.K., Wilson A. Arthroplasty tourism. Med J Aust. 2007;187(11–12):666–667. doi: 10.5694/j.1326-5377.2007.tb01467.x. [DOI] [PubMed] [Google Scholar]
- 74.Gajic O., Warner D.O., Decker P.A. Long-haul air travel before major surgery: a prescription for thromboembolism? Mayo Clin Proc. 2005;80(6):728–731. doi: 10.1016/S0025-6196(11)61525-5. [DOI] [PubMed] [Google Scholar]
- 75.Turner L. Medical tourism: family medicine and international health-related travel. Can Fam Physician. 2007;53(10) 1639–41, 1646–8. [PMC free article] [PubMed] [Google Scholar]
- 76.Duff E., Hall L. The ugly facts behind beauty tourism. 2007. http://www.theage.com.au/news/beauty/the-ugly-facts-behind-beauty-tourism/2007/09/29/1191090984137.html Available at: Accessed July 22, 2008.
- 77.Labus B., Sands L., Rowley P. Acute Hepatitis C Virus infections attributed to unsafe injection practices at an endoscopy clinic—Nevada, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(19):513–517. [PubMed] [Google Scholar]
- 78.Wasley A., Grytdal S., Gallagher K. Surveillance for acute viral hepatitis—United States, 2006. MMWR Surveill Summ. 2008;57(2):1–24. [PubMed] [Google Scholar]
- 79.Dayan G.H., Ortega-Sanchez I.R., Lebaron C.W. The cost of containing one case of measles: the economic impact on the public health infrastructure—Iowa, 2004. Pediatrics. 2005;116(1):e1–e4. doi: 10.1542/peds.2004-2512. [DOI] [PubMed] [Google Scholar]