Abstract
(1) Seroepidemiological analysis of influenza pandemics (1986–2003) in Shizuoka Prefecture and all Japan revealed differences in geographical, annual, seasonal, and age distributions. (2) For 17 years, the pandemics generally began at the 50th week every year showing over 1.0 patient/clinic, reached the peak at 5th week the following year, and ended over 10–15th week. Two big A/H3N2 pandemics were seen in 1989/1990 and 1997/1998 seasons, claiming over 1 million patients in Japan. (3) As herald strains, A/H3N2 strains (A/Sydney-like) were found in October 1999, and B strains (B/Victoria- and B/Yamagata-like) were detected in July and November 1998 and, in August and December 2000 in Shizuoka. B/Shizuoka/1/98 strain was registered internationally as a vaccine-recommended strain. (4) A/H3N2 and B viruses were detected in 55–78% of flu patients (almost under 10 years) with encephalopathy in 1999/2000 and 78–91% in 2000/2001 by MDCK and reverse transcription polymerase chain reaction (RT-PCR) methods. (5) High hemagglutination inhibition (HI) titers over 40 in 250 persons were shown against A/Sydney/5/97 (H3N2), A/Yokohama/8/98 (H3N2), A/Panama/2007/99 (H3N2) and A/Moscow/10/99 (H1N1) strains, while low titers showed against A/Beijing/262/95 (H1N1) and A/New Caledonia/20/99 (H1N1), and B/Beijing/243/97, B/Shangdong/7/97 and B/Yamanashi/106/98 strains in 1998–2000. (6) In anti-HA titers against A/H3N2, A/H1N1 and B subtypes, clear generation gaps were observed between children (0–19 years), adults (20–59 years) and old men (over 60 years). (7) The pandemics are dependent on host immunity (acquired and vaccinated) and climatic conditions (low temperature, low humidity and limited rainfall), considering highly pathogenic avian influenza (HPAI) viruses (A/H5N1, A/H7N7) like severe acute respiratory syndrome (SARS) corona virus in 2002–2003.
Keywords: Active dynamic surveillance, Herald strain, Vaccine-recommended strain, Influenza-associated encephalopathy, Highly pathogenic avian influenza
Abbreviations: ILI, influenza-like illness; HPAI, highly pathogenic avian influenza; RT-PCR, reverse transcription polymerase chain reaction; HI, hemagglutination inhibition; SARS, severe acute respiratory syndrome; CoV, coronavirus; NIID, National Institute of Infectious Disease (JAPAN); CDC, Center for Disease Control and Prevention (USA); WHO, World Health Organization
1. Introduction
Statistical and epidemiological analyses in weekly data of active dynamic surveillance of influenza and influenza-like illness (ILI) were carried out in Shizuoka Prefecture and all Japan for the last 17 years (1986–2003).
Furthermore, virological, serological and genetic analyses were done with regard to (1) pathogen's information —mainly the viral subtypes (vaccine, herald and pandemic/endemic strains) and (2) patient's information—mainly percentage (%) of hemagglutination inhibition (HI) antibody titers of Shizuoka Prefectural people in order to serve the prediction of usual and new (avian) types of influenza pandemics–interpandemics in the near future in all Japan.
2. Materials, patients and methods
-
(1)
The weekly data were utilized from national and prefectural, active dynamic surveillance of influenza and ILI in 1986–2003, reported due to the new raw of infectious disease control reestablished in 1999 and 2003.
-
(2)
Several kinds of test samples from gurgled waters, pharyngeal wipes, sera and liquor derived from babies, young and school children, adults and old men in clinical institutions in Shuizuoka Prefecture were stocked at 4 °C.
-
(3)
HI antibody titers of human sera from 250 persons (over 0–60 years old, nine classes of every 5-year stage) in two Shizuoka Prefectural Hospitals were examined.
-
(4)
Viral isolation and identification were done for vaccinated, herald and pandemic/endemic virus strains, by using MDCK cell culture and egg inoculation methods.
-
(5)
Rapid diagnostic tests were applied to viral antigens and genomes, using Directigen Flu A (Becton-Dickinson), Influenza OIA (Bio Star) and reverse transcription polymerase chain reaction (RT-PCR) methods.
-
(6)
National and prefectural survey of viral subtypes and encephalopathy, encephalitis and death associated with influenza was done in Jan–Mar in 1999–2003.
3. Results
-
(A)
From statistical and epidemiological analyses in weekly data of active dynamic surveillance of ILI in Shizuoka Prefecture and all Japan for the last 17 years (1986–2003), differences were found in geographical (prefectural), annual and seasonal (winter and others) and age (generation) distributions [1], [2], [3].
During the past 17 years, with the exception of a few seasons, the influenza pandemics usually started at about week 50 every year, showing the incidences over 1.0 patient per clinical institution, reached the peak at about week 5 of the next year, and ended over 10–15th week in Shizuoka Prefecture as well as all Japan [1], [2], [3].
Two biggest pandemics due to A/H3N2 subtype were seen in the 1989/1990 and 1997/1998 seasons, showing over 1 million (10×105) patients with ILI in all Japan. Three bigger pandemics of A/H3N2 subtype were also seen in the 1992/1993, 1994/1995 and 1998/1999 seasons, showing over 8×105 patients [1], [2], [3].
-
(B)The following results [1], [2], [3] were clarified from viral and serological analyses of influenza pandemics in Japan:
-
(1)By viral and genetic analyses of pandemic subtypes of influenza in Shizuoka Prefecture and all Japan in three recent years (1998–2000), A/H3N2 and B subtype strains were isolated as one peak with shoulder in 1998/1999 season, however A/H1N1 and A/H3N2 subtype strains were isolated at the same time as a single peak, namely without viral interference, in 1999/2000 season [1], [2], [3].
-
(2)As herald strains in interpandemic periods, A/H3N2 strain (A/Sydney-like) was found in October 1999, and B strains (B/Victoria- and B/Yamagata-like) were detected in July and November 1998 and in August and December 2000 in different cities of Shizuoka Prefecture. One herald strain of them, B/Shizuoka/1/98 was internationally registered by National Institute of Infectious Disease (NIID, Japan), Center for Disease Control and Prevention (CDC, USA) and World Health Organization (WHO) as a vaccine-recommended strain [1], [2], [3].
-
(3)A/H3N2 subtype strains which were isolated from patients with influenza-associated encephalopathy were detected in 78% (7/9) of the suspected patients in 1998/1999 season, and 55% (6/11) of those patients in 1999/2000 season in Shizuoka Prefecture, by using MDCK cell culture and RT-PCR methods, and rapid viral diagnostic kits (Directigen Flu A and Influenza OIA) [1], [2], [3].Furthermore, it has been reported by national survey of influenza-associated encephalopathy in January–March, 1998–2000 that A/H3N2 and B subtype viruses were also highly detected in 90% (217/238) of the suspected patients in 1998/1999 season, and 77% (109/142) of those patients in 1999/2000 season in all Japan [1], [2], [3].
-
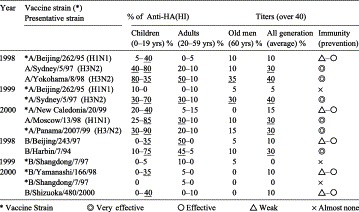
(4)By seroepidemiological analyses of anti-HA antibody titers against influenza subtype strains in 250 persons in Shizuoka Prefecture, high antibody (HI) titers over 40 (meaning protective potency) were shown against A/Sydney/5/97 (H3N2), A/Yokohama/8/98 (H3N2), A/Panama/2007/99 (H3N2) and A/Moscow/10/99 (H1N2) strains, and B/Harbin/09/94 strains (Table 1) [1], [2], [3].
-
(5)By comparison with the percentage (%) of humoral anti-HA antibody (HI) titers against A/H3N2, A/H1N1 and B subtype strains among nine classes of every 5-year stage, clear generation gaps were observed between children (0–19 years), adults (20–59 years) and old men (over 60 years), suggesting the infectious scale of the pandemics in the near future (Table 1) [1], [2], [3].
-
(1)
Table 1.
Percentage (%) of antibody (HI) titers against influenza A and B strains in Shizouka Prefecture (1998–2000)
4. Discussion
-
(1)
The early detection of herald strains like B/Shizuoka/1/98 strain in interpandemic periods every year is very important for vaccine-candidated strains and those productive supply in the following seasons [1], [2], [3].
-
(2)
Low anti-HA antibody (HI) titers under 10 in massive prevention suggest that the next pandemics due to new avian subtypes, e.g., H5N1 in Hong Kong, H7N7 in the Netherlands and other highly pathogenic avian influenza (HPAI) also could be predicted for a world-scale outbreak in the near future among unvaccinated population [1], [2], [3].
-
(3)
On the other hand, influenza pandemics also seem to be dependent on environmental or climatic conditions—low atmospheric temperature (under 10 °C), low humidity (under 40%) and limited rainfall and snow (under 100 ml) [1], [2], [3].
-
(4)
Finally, active dynamic surveillance of new types of influenza pandemics and those predictions by host sensitivity survey should be continued from the viewpoint of health crisis control in the world, considering (1) the rapid and effective collaboration of clinical patient's information (antibody titration) and basic pathogen information (viral isolation/identification) and (2) early detection of herald and new subtype strains of HPAI, and determination of vaccine strains for the following seasons, through the learning of the international outbreak of a new emerging coronavirus of severe acute respiratory syndrome (SARS CoV) in 2002–2003 [1], [2], [3].
References
- 1.Miyamoto H, Sahara K, Sugieda M. Intern. Conf. on “Options for the Control of Influenza V”, Okinawa, Japan, Oct. 7–11. 2003. Sero-epidemilogical analysis of influenza pandemics in Shizuoka Prefecture and all Japan; p. 83. Abstract W01P-79. [Google Scholar]
- 2.Miyamoto H. Ann. Rep. of Natl. Proj. Res. on “Functional Empowerment of Examination in Regional Health Inst. by Scientific EBM”. 2001. Study on the analysis of active dynamic surveillance of influenza and the pandemic prediction; pp. 18–27. in Japanese. [Google Scholar]
- 3.Miyamoto H. Analysis of active dynamic surveillance of influenza and the pandemic prediction. Jpn. J. Public Health. 2003;50(10):815. (in Japanese) [Google Scholar]


