Abstract
Clostridial abomasitis and enteritis are important alimentary diseases observed in all domestic ruminant species. These diseases most commonly result from overgrowth of Clostridium perfringens types A, B, C, D, and E with the associated release of bacterial exotoxins that result in necrosis of the abomasal or intestinal mucosa. Clostridium difficile may also be associated with enteritis in calves but is much less common than disease caused by C perfringens. This article reviews the causes, pathophysiology, clinical signs, diagnosis, treatment, and prevention of clostridial gastrointestinal diseases in ruminants. Particular emphasis is given to describing the various forms of disease and treatment of individual cases.
Keywords: Clostridium perfringens, Clostridium difficile, Abomasitis, Enteritis, Enterotoxemia, Ruminant
Key points
-
•
Clostridial abomasitis and enteritis are characterized by necrosis of the abomasal or intestinal mucosa caused by exotoxins produced by Clostridium perfringens or Clostridium difficile in the lumen of the gastrointestinal tract.
-
•
C perfringens types A, B, C, D, and E can cause enteric disease in all species of domestic ruminants. The 5 genotypes are identified by the presence of the genes for the lethal exotoxins alpha, beta, epsilon, and iota.
-
•
Multiplex polymerase chain reaction is used diagnostically to identify C perfringens genotypes from anaerobic culture of samples.
-
•
Proliferation of C perfringens in the ruminant gastrointestinal tract is associated with a combination of increased availability of carbohydrate or protein, and alteration in gastrointestinal motility.
-
•
Treatment of abomasitis and enteritis caused by C perfringens should focus on 6 goals: relief of abdominal distention, systemic fluid support, prevention of C perfringens proliferation, decreasing or preventing exotoxin production, restoration of normal gastrointestinal flora, and providing pain management as needed.
Introduction
Clostridial diseases affecting the gastrointestinal tract are common in ruminant livestock; however, their classification can be confusing because of the varied nomenclature of the disease conditions.1, 2, 3, 4 Described diseases have included hemorrhagic enterocolitis, enterotoxemia, pulpy kidney disease, overeating disease, braxy, bradsot, struck, lamb dysentery, enterotoxemic jaundice, yellow lamb disease, clostridial abomasitis, and clostridial enteritis. Other than braxy (bradsot) of sheep, which is caused by Clostridium septicum, these diseases are all caused by different subtypes of Clostridium perfringens. C perfringens type A can also cause gangrenous mastitis and may be present in high numbers in spoiled milk.
Clinical disease is associated with rapid bacterial overgrowth within the gastrointestinal tract and subsequent exotoxin release. Although limited tissue invasion by C perfringens does occur, most local and systemic lesions result from the effects of potent exotoxins produced by certain genotypes of these bacteria. C perfringens is a large, gram-positive, anaerobic bacillus that exists ubiquitously in the environment and in the gastrointestinal tract of most mammals.3, 5, 6, 7, 8 There are 5 defined types, or genotypes, of C perfringens: A, B, C, D, and E (Table 1 ). These genotypes are identified based on the lethal toxins that they produce: C perfringens alpha (CPA), C perfringens beta (CPB), epsilon (ETX), and C perfringens iota (CPI).7, 8, 9, 10 The alpha toxin gene (plc) is present on the chromosome of all C perfringens isolates.7, 8 All genotypes produce alpha toxin, although isolates differ significantly in the amount of alpha toxin produced.11, 12 The other lethal toxins, CPB (cpb gene), ETX (etx gene), and CPI (iap/ibp genes) are contained on transferrable plasmids.7, 8
Table 1.
Toxins, gene, genetic location, and toxin action expressed by different Clostridium perfringens toxinotypes (genotypes)
| Toxin |
C perfringens Type |
Gene | Gene Location | Toxin Action | ||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | ||||
| Alpha (CPA) | + | + | + | + | + | plc | Chromosome | Phospholipase |
| Beta (CPB) | — | + | + | — | — | cpb | Plasmid | Pore formation |
| Epsilon (ETX) | — | + | — | + | — | etx | Plasmid | Pore formation |
| Iota (CPI) | — | — | — | — | + | Iap/ibp | Plasmid | Cytoskeleton disruption |
Two other toxins, enterotoxin (C perfringens enterotoxin [CPE], cpe gene) and the beta-2 toxin (CPB2, cpb2 gene), are also carried on transferable plasmids in livestock isolates. Enterotoxin can be expressed by any of the subtypes if the plasmid containing this gene (cpe) is present, but it is not required for pathogenicity. Enterotoxin is not released by vegetative bacteria but only in sporulating C perfringens cells during lysis of the vegetative cell.7 Thus, the toxin may not be present in intestinal contents of animals with C perfringens enteritis unless sporulation is occurring. The beta-2 toxin may be produced by type A as well as by some isolates of types B, C, and E.13 Strains of C perfringens that carry the beta-2 toxin gene have been isolated from a variety of species of domestic animals, including horses, camelids, cattle, and swine.13, 14
The genotype, and thus the specific subtype of C perfringens, can be determined by a multiplex polymerase chain reaction (mPCR) that detects the specific toxin genes carried by an individual isolate. Because the clinical and pathologic presentations of diseases caused by C perfringens types are not always distinct, anaerobic culture and polymerase chain reaction (PCR) genotyping of the isolates can be instrumental in determining the subtype involved and can help identify specific control measures. Each of the subtypes of C perfringens is associated with specific disease syndromes that are directly or indirectly related to the toxins they produce. The term enterotoxemia is often loosely used to describe enteric or systemic disease caused by any of the C perfringens toxinotypes. The term enterotoxemia refers to systemic disease caused by absorption of a toxin from the intestine. Clostridial abomasitis and enteritis does not require absorption of the toxins. The term enterotoxemia is best reserved for cases in which systemic disease is associated with absorption of bacterial exotoxins, including hemolytic diseases in lambs with C perfringens type A, and systemic disorders caused by the epsilon toxin of C perfringens types B and D. Some of the disease conditions described for C perfringens are listed in Table 2 .
Table 2.
Diseases caused by different subtypes of Clostridium perfringens
| Organism | Disease | Notes |
|---|---|---|
| C perfringens type A |
|
|
|
|
|
|
|
|
| C perfringens type B |
|
|
| C perfringens type C |
|
|
|
|
|
| C perfringens type D |
|
|
| C perfringens type E |
|
|
Recent studies have suggested an association of hemorrhagic bowel syndrome (HBS) in cattle with C perfringens type A.17, 18, 19, 20 Although C perfringens is isolated from the intestinal tract and from lesions of animals with HBS, a causal link has not been established. It is possible that the heavy growth of C perfringens from animals with HBS is caused by an appropriate environment for growth that is associated with gastrointestinal (GI) hemorrhage and stasis. Studies trying to induce HBS by inoculation with C perfringens type A have not been able to reproduce the disease.21
Clostridium perfringens exotoxins
The C perfringens exotoxins are all polypeptides that generally act by phospholipase damage to the plasma membrane or by forming pores or channels in the plasma membrane of host cells.8 This process results in cellular membrane disruption and cell leakage of electrolytes or water. The alpha toxin gene is expressed from the chromosome of all C perfringens subtypes.7, 8 The genes encoding the other toxins are carried on large plasmids.7, 8 The enterotoxin gene can be either chromosomal or plasmid determined. In animal isolates, it is generally carried on a plasmid. However, it is chromosomally located on most (∼70%) isolates from human cases of C perfringens food poisoning.22 All of the toxins except CPE are secreted by vegetative bacteria. Enterotoxin is released after sporulation and bacterial cell lysis.7, 8, 22
Alpha Toxin
Alpha toxin is produced by all subtypes of C perfringens; however, the amount of toxin secreted varies by both isolate and type.7 The alpha toxin gene (plc) is located on the bacterial chromosome. Alpha toxin is a phospholipase C sphingomyelinase (lecithinase) enzyme that binds to cell membranes and causes disruption of the lipid bilayer.7, 8, 23 The toxin is hemolytic and dermonecrotic. Hydrolysis of lecithin by alpha -toxin produces diacylglycerol, which leads to stimulation of eukaryotic cell phospholipases and the arachidonic acid cascade.8, 23 This process can result in alterations in vascular permeability, platelet aggregation, and vasoconstriction. Alpha toxin has been shown to cause alterations in fluid transport within ileal and colonic loops in sheep.24 Alpha toxin likely acts in concert with additional virulence factors, resulting in intestinal mucosal damage and, in particular, the C perfringens toxin perfringolysin (theta toxin) seems to work synergistically with alpha toxin in calves.25, 26
Beta Toxin
Beta toxin is produced by type B and C strains of C perfringens. The beta toxin gene (cpb) is encoded on a large plasmid and codes for a small polypeptide protoxin. The protoxin is secreted from the vegetative bacteria and cleaved by proteases to produce the active toxin.7 Beta toxin is classified as a pore-forming cytolysin, and is similar to other toxins, including Staphylococcus aureus alpha toxin. The channels formed by the beta toxin pores are selective for monovalent cations such as sodium and potassium.27 Beta toxin is rapidly destroyed by trypsin.3, 7 Because of this, disease caused by types B and C tend to occur in young neonates less than 10 to 21 days of age because of the presence of trypsin inhibitors in colostrum and early milk. Disease may also occur later if bacterial or plant-derived trypsin inhibitors are present in the feed.
Epsilon Toxin
The epsilon toxin gene (etx) is carried by type B and D strains of C perfringens. The gene is encoded on a large plasmid.7, 8 The gene encodes a small polypeptide protoxin that is cleaved to the active toxin by intestinal proteases, including trypsin and chymotrypsin.28, 29 C perfringens epsilon toxin is the third most potent bacterial toxin following botulinum toxin and tetanus toxins.28 The toxin is lethal and dermonecrotic. Studies in lambs, goats, and calves show increased vascular permeability associated with exposure to epsilon toxin.30, 31, 32, 33, 34 The toxin binds the plasma membrane of sensitive cells, including endothelial cells, and forms a complex with a particular membrane protein, resulting in altered membrane permeability by an unknown mechanism,8, 28, 29 and this is the primary extent of disease observed in the intestine caused by epsilon toxin.
C perfringens epsilon toxin also results in systemic disorders in ruminant species (enterotoxemia). Toxin-induced damage to the intestinal mucosa allows absorption and systemic dissemination of the toxin. Disruption of endothelial cells causes vascular lesions and edema observed in the heart, lungs, and brain, resulting in pericardial effusion, pleural effusion, pulmonary edema, and perivascular cerebral edema.28 Endothelial cell damage in the brain disrupts the blood-brain barrier, providing the toxin access to cerebral neurons and parenchymal cells. Epsilon toxin causes damage and necrosis to neurons, astrocytes, and oligodendrocytes, producing the characteristic lesion of focal symmetric encephalomalacia.29 Pore formation disrupts transmembrane K+, Cl−, Na+, and Ca++ transport in affected cells. There is also an overexpression of the membrane channel protein aquaporin-4, resulting in a disruption of intracellular water balance. Sublethal intracerebroventricular injections of epsilon toxin into mice and rats produced neuronal degeneration in the cerebral cortex, hippocampus, striatum, and hypothalamus, resulting in permanent behavioral changes.35 Dexamethasone was able to reduce the effects of epsilon toxin in these studies.
Iota Toxin
The iota toxin is a binary cytotoxin consisting of 2 subunits: Ia and Ib.7, 8, 36 The genes coding for the toxin (iap and iab) are located on an extrachromosomal plasmid. Both subunits are required for toxicity. The Ib subunit constitutes the binding component and the Ia subunit is the enzymatic component. The Ib precursor protein is cleaved by trypsin and binds to the cell membrane, forming a heptameric complex. Ia subunits bind to this complex and enter the cell by receptor-mediated endocytosis. The Ib heptamer forms a pore within the endosome, allowing translocation of the Ia subunits to the cytoplasm. The Ia subunit has ADP-ribosylation activity resulting in the depolymerization of actin and inhibition of cell functions that are dependent on actin.
Enterotoxin
C perfringens enterotoxin is a primary toxin associated with food poisoning in humans, but its relationship to enteric disease in animals is not fully established. The CPE gene (cpe) can be located either on the bacterial chromosome or on an extrachromosomal plasmid.7, 8, 9, 22 The cpe gene is chromosomally determined in C perfringens isolates that cause food poisoning in humans. However, the cpe gene is plasmid determined in isolates from animals. The cpe gene is carried by less than 6% of C perfringens isolates. The enterotoxin gene is most commonly found in type A isolates but is also present in some type C, D, and E isolates.22 Although the gene is expressed in A, C, and D isolates, it is silent in the type E isolates that have been identified. Enterotoxin is only expressed during the process of bacterial sporulation and then released when the vegetative C perfringens cells undergo lysis.7, 22 Expression is regulated at the transcriptional level. The toxin binds claudins in the cell membrane of enterocytes forming a large transmembrane pore complex that allows for calcium influx and cell death by either apoptosis or necrosis.22 The CPE-claudin complex also causes destabilization of intercellular tight junctions and leakage between cells.
Beta-2 Toxin
The beta-2 toxin gene (cpb2) is located on an extrachromosomal plasmid and can be found in all subtypes of C perfringens. Although genetically distinct, the beta-2 toxin shows cytotoxic activity similar to that of C perfringens beta toxin (CPB; also designated beta-1 toxin).8, 37 The significance of the beta-2 toxin as related to disease caused by C perfringens has not been fully determined.14, 37, 38, 39 The toxin is likely a cofactor in the pathogenesis of abomasitis and enteritis when present but is not required for intestinal mucosal necrosis.
Novel Pore-forming Toxins
NetF toxin, a pore-forming toxin produced by a subset of C perfringens type A strains and related to the leukocidin/hemolysin superfamily, was recently associated with necrotizing enteritis in neonatal foals and with canine hemorrhagic gastroenteritis.40, 41 Similarly, NetB toxin (necrotic enteritis toxin B type) produced by some strains of C perfringens type A has been shown to be essential in causing necrotic enteritis in chickens.42 These toxins form pores that result in disruption of the phospholipid membrane bilayer of cells and cause an ion influx that can lead to osmotic cell lysis.43 Although it was previously thought that alpha toxin was the major toxin responsible for avian necrotic enteritis, Keyburn and colleagues44 showed that alpha toxin null mutants were still virulent in an avian necrotic enteritis disease model. These novel toxins have not yet been shown to play a role in clostridial enteric diseases in ruminants.45, 46
Clinical disease
This article focuses on abomasitis and enteritis associated with C perfringens with clarification of the distinctions from true enterotoxemia. Enterotoxemia is a loosely used term for disease caused by C perfringens and is often used in reference to all clinical forms of C perfringens, including abomasitis and enteritis observed in cattle and other ruminants. This loose terminology can cause confusion when discussing the disease because it does not designate the specific genotype and clinical manifestations of C perfringens syndromes seen in cattle and other ruminants. The term enterotoxemia is best reserved for C perfringens diseases that include absorption and systemic spread of toxins with disorders in other organs beyond the intestinal tract. Clinical forms of the wide array of C perfringens disease syndromes are reviewed in Table 2.
Clostridial Abomasitis
All genotypes of C perfringens can cause abomasitis or enteritis in some or all domestic ruminant species. C perfringens type A is an increasingly common isolate associated with clostridial abomasitis in ruminants.4, 15, 30, 45, 47, 48, 49 Type E has also been isolated in cases of abomasitis but seems to be rare.47, 49, 50 Clostridial abomasitis has been reproduced experimentally by intraruminal inoculation of C perfringens type A in calves.51 Clostridial abomasitis may be present by itself or combined with enteritis.
Type A abomasitis is most commonly observed in neonatal and juvenile animals but can also be observed in adult ruminants. C perfringens abomasitis is a sporadic disorder of neonatal to weanling calves, lambs, and kids.15, 45, 47, 49, 52 The condition is common in both dairy and beef calves and seems to be less common in lambs and kid goats. Clinical signs include decreased nursing, lethargy, fluid distension of the abomasum, abdominal tympany, colic, and bruxism.49 Animals generally have a normal temperature unless complications of systemic sepsis or peritonitis have developed, in which case their temperature can be decreased or increased. Mucous membranes may be pale with a prolonged capillary refill time indicating systemic shock. Hydration status is often normal in acute cases but dehydration can develop in animals that are not treated soon. Abdominal distension with a succussion splash is a predominant and consistent clinical sign (Fig. 1 ). The ability of C perfringens to produce gas contributes to gastric dilatation and intramural emphysema evident in affected animals. Abomasal tympany and the associated abdominal distension also causes respiratory difficulty because of pressure placed on the diaphragm. Abomasal distension can also result in hemodynamic effects that can lead to shock. The case fatality rate of clostridial abomasitis seems to be high when rapid treatment is not instituted (75%–100%).15, 45, 47, 48, 49, 51
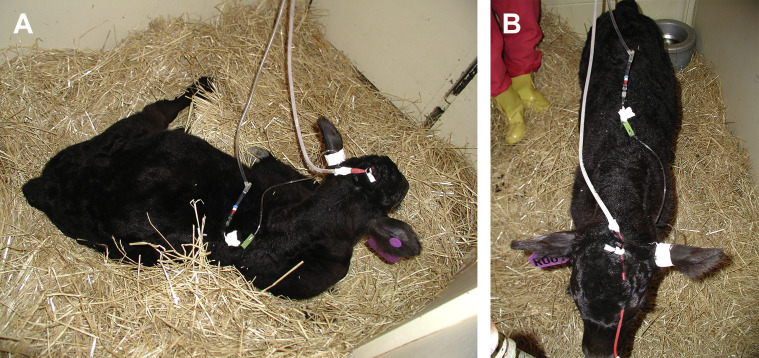
Fig. 1.
A 3-week-old calf with abdominal distension caused by C perfringens type A abomasitis and enteritis.
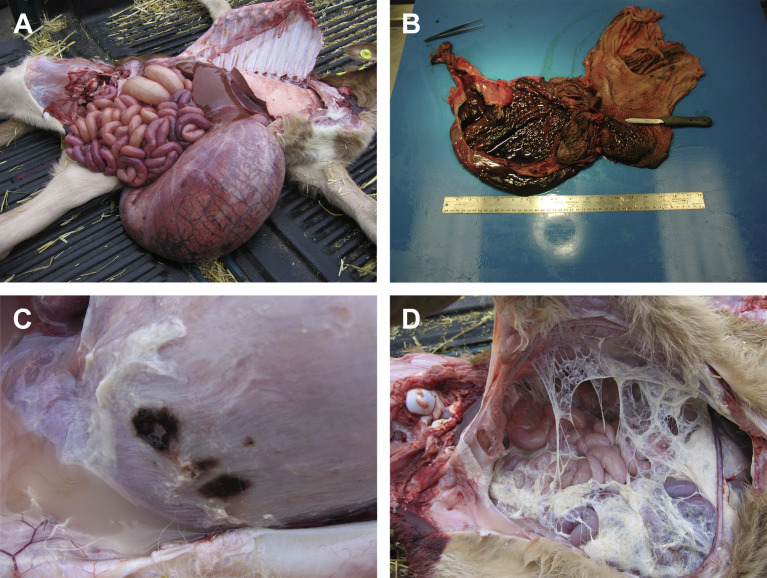
At necropsy, the abomasum is grossly distended and filled with hemorrhagic fluid and gas (Fig. 2A). Gross pathology is characterized by diffuse, hemorrhagic to necrotizing inflammation of the abomasal mucosa, frequently involving the deeper layers of the abomasal wall in severe or chronic cases (Fig. 2B). Abomasal ulceration (Fig. 2C) and perforation with peritonitis (Fig. 2D) may occur in a subset of affected animals. Intramural emphysema and edema of the abomasal wall may be present.
Fig. 2.
Necropsy findings that may be observed in neonates with clostridial abomasitis. Common findings include grossly distended abomasum containing fluid and gas (A); diffuse, hemorrhagic to necrotizing inflammation of the abomasal mucosa (B); abomasal ulceration (C) with or without perforation resulting in fibrinous peritonitis (D).
Other differential causes of abomasitis and abomasal tympany in ruminants include Sarcina spp,47, 53, 54, 55 Salmonella,56, 57, 58 coccidiosis,59 fungal infection,60 immunosuppression, pica, trauma from coarse feed, trichobezoars, gastric ulcers, and vitamin or mineral deficiencies.61 Sarcina spp are implicated as a cause of abomasitis and abomasal tympany in calves, sheep, and goats.47, 53, 54, 55 Abomasal coccidiosis is described in an 11-month-old female sheep with proliferative abomasitis.59 Salmonella typhimurium DT104 was isolated from the abomasal wall of Midwestern veal calves with abomasitis.56, 57 S typhimurium was also isolated from an outbreak in ewes and lambs in which the primary clinical finding was abomasitis.58 Copper deficiency has been associated with abomasitis and abomasal ulcers in beef calves.61, 62, 63 However, Roeder and colleagues51 showed that abomasitis can occur spontaneously and be induced experimentally in the absence of copper deficiency. Thus, although copper deficiency may act as a contributory factor for abomasitis and enteric disease of calves, it does not seem to be a requisite factor for either condition.
Clostridial Enteritis
Clostridial enteritis (inflammation of the small intestine) may be seen in concert with abomasitis or on its own. The condition is most commonly observed in young animals but may also occur in adult ruminants. Clostridial enteritis can be caused by all toxinotypes of C perfringens, although there are important differences. C perfringens type A is the most common cause of clostridial enteritis currently observed in ruminants in the United States, which may in part be caused by the routine use of clostridial C and D toxoids in ruminants in the United States resulting in antibodies to beta and epsilon toxins and providing effective protection against enteritis caused by C perfringens types B, C, and D. It may also be caused by geographic differences in the environmental and host distribution of toxinotypes B, C, D, and E.
Type A
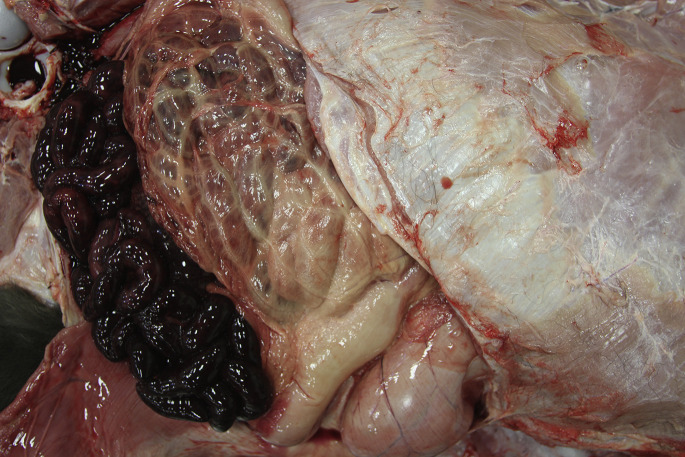
Enteritis caused by C perfringens type A is observed in calves, lambs, and kid goats.1, 3, 10, 25, 30, 47, 50, 64, 65 Enteritis is generally acute and develops over a period of hours. Appetite is significantly decreased. In most cases, diarrhea is not present in the acute stages. The animals generally have a normal temperature and may not show physical or clinicopathologic signs of sepsis or systemic inflammation unless the disease has progressed and generalized sepsis is present. At necropsy, the small intestine is hemorrhagic and distended with hemorrhagic contents (Fig. 3 ). The intestinal wall may be thickened with edema or, if intestinal distension is severe, may appear thin. Ultrasonography examination of affected patients often shows local or generalized areas of distended small intestine. The motility pattern of the affected segments is decreased, or seems to have a lack of coordinated progressive peristalsis. Gross pathology is characterized by segmental to diffuse, hemorrhagic or necrotizing inflammation of small intestinal mucosa. In some cases, mucosal damage can also affect the cecum or spiral colon.
Fig. 3.
Necropsy of a 3-day-old beef calf with C perfringens type A hemorrhagic enteritis. The cause was confirmed with anaerobic culture and mPCR genotyping.
C perfringens type A is also associated with nonobstructive hemorrhagic enteritis in adult ruminants, particularly cattle. This condition in adult ruminants is poorly described in the literature. Type A hemorrhagic enteritis is less common in adults than in young animals. Clinical signs include acute onset of decreased appetite with right side or bilateral ventral abdominal distension (Fig. 4A). The animals may have a fever or be afebrile. Inflammatory changes to the complete blood count (CBC) are often absent but may be present because of translocation of enteric Gram-negative bacteria and secondary septicemia. Hemorrhagic diarrhea may not be apparent at the time of presentation (Fig. 4B) but may be apparent later in the course of the disease (Fig. 4D). Abdominal ultrasonography often reveals multiple loops of fluid-distended small intestine up to 5 cm in diameter (Fig. 4C). Intestinal motility is often decreased or lacks coordinated peristalsis. Scant feces may be noted upon rectal examination in early cases. The clinical signs are often difficult to discriminate from intestinal obstruction caused by intussusception, entrapment, or obstructing HBS. C perfringens type A can be cultured from affected small intestine and these animals often respond to treatment directed toward intraluminal clostridial infection. At this time, it is unclear whether this is an enteritis condition distinct from HBS or part of a continuum of enteric disease caused by C perfringens type A that includes HBS.
Fig. 4.
Hemorrhagic C perfringens enteritis in an adult dairy cow. Note the right ventral abdominal distension caused by distension of the small intestine (A). Transabdominal ultrasonography shows dilated loops of small intestine up to 5 cm in diameter (B). A right flank exploratory laparotomy was performed and confirmed diffuse hemorrhagic enteritis (C). The cow received intraluminal procaine penicillin G in surgery. The following morning the cow had profuse hemorrhagic diarrhea (D), returned to eating, and recovered.
Type A enterotoxemia of sheep (yellow lamb disease) is an apparently rare but highly fatal disorder that manifests as an acute hemolytic disease. Hemolysis is thought to be caused by either alpha toxin or perfringolysin (theta toxin) following absorption into the circulation secondary to damaged intestinal mucosa.
Type B
C perfringens type B causes acute hemorrhagic enterocolitis in neonatal ruminants. Type B enteritis is uncommon in North America but more common in the United Kingdom and Europe. In lambs, the condition is called lamb dysentery. Type B enteritis is also observed in calves and foals. The main contributing toxin is the beta toxin. The disease is restricted to young animals; generally, lambs less than 21 days of age and calves less than 10 days. The main factor responsible for this age restriction is the susceptibility of the beta toxin to destruction by trypsin (discussed further for C perfringens type C). Infection results in a severe acute hemorrhagic enterocolitis with high mortality similar to type C. Type C isolates also express epsilon toxin and can cause clinical signs of enterotoxemia because of systemic absorption and the action of the epsilon toxin.
Type C
Hemorrhagic enterocolitis caused by C perfringens type C is a commonly fatal disease that occurs in calves and lambs and is suspected to occur on rare occasions in goats.5, 65, 66 The hallmark of this disease is acute profuse hemorrhagic diarrhea. Neonates are most commonly affected, although disease losses in older calves and lambs can be significant. Intake of large quantities of soluble carbohydrate and/or protein is considered a risk factor for the development of type C enterotoxemia.5, 65 Neonates nursing heavily lactating dams seem to be at higher risk. Heavy grain feeding, foraging on grain crops, sudden access to high-quality forage, or overfeeding following a period of hunger are also considered risks.
The beta toxin is thought to be responsible for the acute necrohemorrhagic enterocolitis. The disease is generally restricted to neonatal ruminants because of the susceptibility of the beta toxin to proteolytic destruction by trypsin.3, 7 Beta toxin is active in young neonates because of the presence of trypsin inhibitors in colostrum and early postpartum milk. Trypsin inhibitors are present in milk for up to the first 10 to 21 days after parturition and place neonates that nurse postpartum dams at risk. The risk is less for neonates fed pooled milk, including milk from later lactation animals or milk replacer. Disease can occur in older ruminants if bacterial or plant-derived trypsin inhibitors are present in the feed.
Affected animals are acutely listless and reluctant to nurse. Ataxia, colic, bloody diarrhea, depression, and recumbency soon follow. Extensor rigidity and opisthotonus may be seen terminally, and death usually occurs within hours of the onset of signs. Severe hemorrhagic enterocolitis is the primary gross lesion at necropsy. This lesion tends to be most pronounced and is consistently found in the distal jejunum and ileum, although occasionally the entire small intestine or colon is involved.5, 67 Fibrin clots, casts of necrotic mucosa, and red-brown blood may be present within the intestinal lumen. An increased amount of clear, straw-colored, or serosanguinous fluid may be found within the peritoneal, pleural, and pericardial cavities.
Type D
Enteritis is not the predominant clinical feature of enteric infection with C perfringens type D. Clinical enteritis is rare in calves and lambs. Goats more consistently show clinical signs of GI dysfunction with type D infection, including gross and histologic lesions of enteritis.33, 68, 69, 70, 71 In the peracute form of this disease, affected goats may be found dead or may have colic. Abdominal distension, vocalizing, dyspnea, tachypnea, and watery diarrhea containing fibrin, mucus, or strands of blood may occur. Recumbency, respiratory distress, and convulsions associated with true enterotoxemia usually follow, and death typically occurs within hours of the onset of signs.
C perfringens type D is responsible for true enterotoxemia in small ruminants of all ages.5, 65 Type D enterotoxemia in calves is rare.72 Enteritis is not a consistent clinical finding with enterotoxemia except in goats. C perfringens type D is not considered to be a common inhabitant of the GI tract of normal ruminants, although it can be carried sporadically by healthy animals.65 As with type C enterotoxemia, passage of soluble carbohydrates or protein into the small intestine is thought to induce rapid replication and elaboration of epsilon toxin from this organism.66 Unlike beta toxin, however, epsilon toxin is activated by intestinal and pancreatic proteases.5, 7, 8 Once absorbed into the bloodstream, epsilon toxin causes loss of endothelial integrity, increased capillary permeability, and edema formation in multiple tissues.73 Epsilon toxin also causes damage and necrosis to neurons, astrocytes, and oligodendrocytes, producing the characteristic lesion of focal symmetric encephalomalacia and is responsible for the neurologic signs observed with this disease.29
Type D enterotoxemia in sheep is typically a peracute illness, with many cases simply being found dead. If a live ovine case is detected, neurologic signs predominate. Lethargy and ataxia are evident early, with collapse, hyperesthesia, lateral recumbency, convulsive paddling, and opisthotonus following within hours. Diarrhea is inconsistently seen. Glucosuria is frequently present in sheep.74
At necropsy examination, the effusion is typically observed in the peritoneal, pleural, or pericardial spaces with variable volumes of straw-colored or red fluid that may contain fibrin clots. Petechial hemorrhages are often visible on the visceral surfaces. Pulmonary and mesenteric edema may be evident. Gross lesions of the intestinal tract are frequently absent in affected sheep. Dipstick analysis of urine collected from the bladder frequently reveals the presence of glucose in sheep. The renal cortex may be softened (hence the term pulpy kidney), although this is a nonspecific autolytic change seen on occasion in small ruminant cadavers. The classic pathologic lesion is focal symmetric encephalomalacia. Occasionally, no gross lesions are seen in ovine cases of type D enterotoxemia.66
Unlike sheep, goats affected by type D enterotoxemia more consistently show signs of GI dysfunction, and gross and histologic lesions are more consistently found in the GI tract.33, 68, 69, 70, 71 In the peracute form of this disease, affected goats may be found dead or may have colic. Abdominal distension, vocalizing, dyspnea, tachypnea, and watery diarrhea containing fibrin, mucus, or strands of blood may occur. Recumbency, respiratory distress, and convulsions usually follow, and death typically occurs within hours of the onset of signs. Glucosuria is not consistently detected in goats with enterotoxemia.69
The clinical signs of the acute form of type D enterotoxemia in goats are similar to those of the peracute form, but the progression of the disease occurs over 2 to 4 days. Intermittent or protracted diarrhea, weight loss, and reduced milk production are evident in the chronic form of enterotoxemia in goats. In this form of the disease, clinical signs may persist for several days or occur intermittently over weeks or months. Chronic enterotoxemia may be difficult to diagnose unless prior peracute or acute cases are known to have occurred in the herd. GI parasitism, salmonellosis, Johne disease, and rumen acidosis are important differential diagnoses.
The most prominent gross postmortem lesion in goats with peracute or acute type D enterotoxemia is fibrinohemorrhagic colitis, which is usually most severe in the spiral colon.33 Luminal casts of fibrin, blood, and mucus may be present, and a pseudomembrane may form in affected colonic segments. The colonic serosa may be hyperemic or edematous, with edema evident in the colonic mesentery and mesenteric lymph nodes. Pulmonary edema, fluid, and fibrin in the thoracic and abdominal cavities and pericardium, and scattered ecchymotic hemorrhages on serosal surfaces may be present. Occasionally caprine cases of peracute type D enterotoxemia show no gross lesions. Chronic cases may show scant body fat reserves and ulcerated colonic mucosa. Glucosuria is inconsistently found.69
Type E
Enteritis caused by C perfringens type E is rare but has been reported in goats, calves, and adult cattle.50, 75, 76 Clinical signs range from mild diarrhea to severe hemorrhagic enteritis. Type E isolates are not considered to be a common cause of abomasitis or enteritis in cattle. However, their presence makes appropriate diagnostic differentiation important when evaluating cases of clostridial abomasitis or enteritis in ruminants.
Predisposing factors
The underlying factors that allow overgrowth and toxin expression of C perfringens in ruminants are considered multifactorial. Three key components seem to be involved in clostridial abomasitis and enteritis:
-
1.
The presence of C perfringens within the GI tract
-
2.
Sufficient carbohydrate or protein nutrients to support bacterial growth
-
3.
Decreased GI motility that allows segmental overgrowth of the bacteria within the GI tract
C perfringens type A is ubiquitous in the livestock environment and is considered normal flora at low levels in the healthy ruminant.7, 8, 45, 47, 77 Fecal shedding maintains persistence in the environment. Other toxinotypes are not found as consistently in the environment or from fecal samples of ruminants.
All forms of enteric disease caused by C perfringens seem to be associated with increased intake of feeds rich in soluble carbohydrate, protein, or both. Heavy grain feeding, foraging on grain crops, sudden access to high-quality forage, or overfeeding following a period of hunger are also considered risks. Consumption of large volumes of milk at individual feedings also seems to increase risk in nursing ruminants.
Clostridial abomasitis and enteritis in neonatal beef calves is associated with management practices that cause delays in regular nursing patterns (eg, calf separation at branding) or changes in environment that interrupt normal nursing patterns (eg, winter storms).62 In dairy calves, poor milk hygiene, intermittent feeding of large volumes of milk, and milk replacers with higher carbohydrate or protein concentrations are thought to be contributory factors.
There are many factors that can decrease intestinal motility. Abomasal emptying in nursing calves can be delayed by feeding large volumes in single feedings, feeding with an esophageal tube, high caloric content, and high osmolality of the milk.78 Enteric pathogens can alter intestinal motility, including rotavirus, coronavirus, cryptosporidia, and coccidia. Cases of C perfringens enteritis have been associated with concurrent coccidiosis in cattle and New World camelids.79, 80, 81 Other factors, such as abomasal ulcers, coarse feed, foreign bodies, hairballs, and mineral deficiencies, may be associated with abomasal tympany and increase the risk of C perfringens overgrowth in the abomasum.61
Clinical pathology
Because the pathogenesis of the disease is primarily an enterotoxemia, signs of systemic inflammation are often not observed. A CBC may show a neutrophilia without a left shift and normal fibrinogen, suggestive of a physiologic response or a stress response. An inflammatory leukogram is rarely seen unless there is sufficient mucosal compromise to allow for Gram-negative bacterial translocation and/or systemic endotoxin absorption. Most parameters on the serum chemistry are normal. The creatinine and/or blood urea nitrogen level may be increased if systemic shock has resulted in decreased renal perfusion. Sheep and sometimes goats with type D enterotoxemia may be hyperglycemic and glucosuric. Total protein level is usually not increased because systemic dehydration is often not present in peracute or acute cases. The serum chloride may be decreased because of intestinal ileus and delayed abomasal emptying, and metabolic alkalosis may be present in early cases. Metabolic acidosis and increased lactate levels are common in later stages of the disease.
Diagnosis
Definitive diagnosis of C perfringens abomasitis or enteritis has challenges and must rely on clinical signs, gross and microscopic pathology, and appropriate microbiological tests to show the presence of the organism.10 mPCR is currently used to categorize this diverse species into distinct types, or genotypes. Genotyping is based on detection of gene sequences for alpha, beta, beta-2, epsilon, and iota toxins and enterotoxin.13, 14, 82, 83 The presence of the gene for a particular toxin reflects the potential to produce that toxin. It is critical to note that expression of major lethal toxins is not consistent across clinical isolates within a particular genotype. Thus, the potential pathogenicity of isolates within each genotype is suspected to be variable.
Interpretation of positive culture results for C perfringens from the intestinal lumen of a ruminant is a complicated matter. C perfringens type A inhabits the intestine of normal animals and can overgrow in the gut lumen postmortem.5, 65 Thus, its isolation should be considered significant only from a fresh cadaver with compatible history, clinical signs, and lesions. The organism is easily grown in vitro; C perfringens type A grows rapidly in anaerobic culture and may overgrow other potential pathogens.65 Although quantitative culture is considered helpful in discriminating normal flora from overgrowth, a recent study in veal calves showed no difference in bacterial counts between normal veal calves and veal calves with clostridial enteritis.84 Diagnosis of clostridial abomasitis or enteritis therefore requires a combination of observations that may include:
-
•
Observation of abdominal distension with colic.
-
•
The presence of hemorrhagic abomasitis or enteritis (see Figs. 2B and 3). Abomasitis or enteritis may additionally be suggested by ultrasonographic findings.
-
•
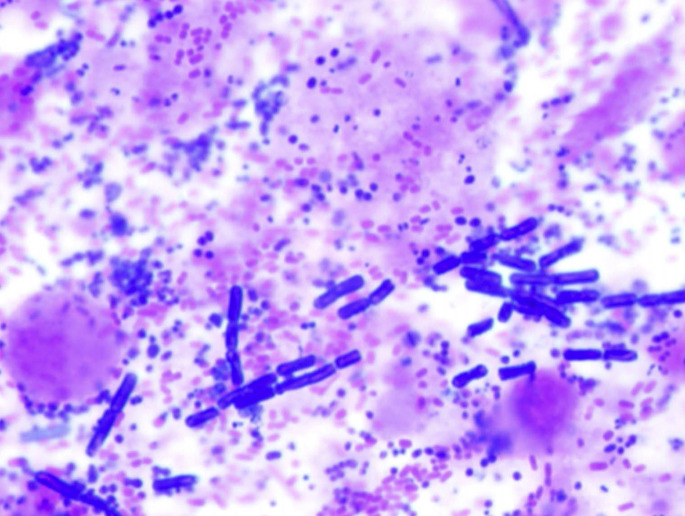
Cytologic evidence of high numbers of gram-positive rods in abomasal or intestinal contents, feces, or on the mucosal surface of tissues (Fig. 5 ).
-
•
Culture of C perfringens in high numbers from abomasal or intestinal contents, feces, or tissue samples.
-
•
Demonstration of the presence of alpha, beta, or epsilon toxin by mouse neutralization test or enzyme-linked immunosorbent assay (ELISA). However, toxin assays for the lethal toxins are not readily available from commercial diagnostic laboratories in the United States. Toxin detection test kits are available from BioX in Belgium (http://www.biox.com).
Fig. 5.
Gram stain of feces from a calf with clostridial enteritis (original magnification, ×1000). Note the group of large Gram positive rods within the background of other bacterial flora. Cytologic evidence of high numbers of large Gram-positive rods in ingesta or feces is suggestive of, but not definitive for, clostridial abomasitis and/or enteritis. The presence of white blood cells, red blood cells, and sloughed mucosal epithelium indicates inflammation with mucosal necrosis and hemorrhage. In early cases of abomasitis or enteritis, changes in fecal flora may not initially be observed.
Recommended samples for diagnostic testing include2, 10:
-
•
Abomasal or intestinal contents or feces for cytologic evaluation.
-
•
Impression smear of the mucosal surface of the affected GI tract for cytology including Gram stain.
-
•
Intestinal contents, tissues, or feces for anaerobic culture and PCR identification of genotype. Samples should be collected antemortem and/or immediately postmortem to avoid normal postmortem clostridial overgrowth.
-
•
Abomasum, small intestine, and colon in 10% buffered formalin for histopathology.
-
•
Brain in 10% formalin for histopathology if neurologic signs are observed and C perfringens type D (or B) is suspected.
-
•
Intestinal contents, refrigerated or frozen for toxin detection.
Treatment
There is very limited information on the efficacy of treatment methods for abomasitis and enteritis caused by C perfringens. The following information is based on treatment protocols at the contributing authors’ institution that seem to be effective in treating animals with clinical signs consistent with clostridial abomasitis or enteritis. Treatment of abomasal or enteric clostridial disease should focus on 6 goals:
-
1.
Relief of abdominal distension, particularly if respiration is compromised because of abdominal pressure on the diaphragm.
-
2.
Systemic and nutritional support with intravenous (IV) fluids if indicated.
-
3.
Preventing ongoing bacterial proliferation.
-
4.
Decreasing or preventing production of and neutralizing clostridial exotoxins.
-
5.
Restore normal GI flora.
-
6.
Pain management as needed.
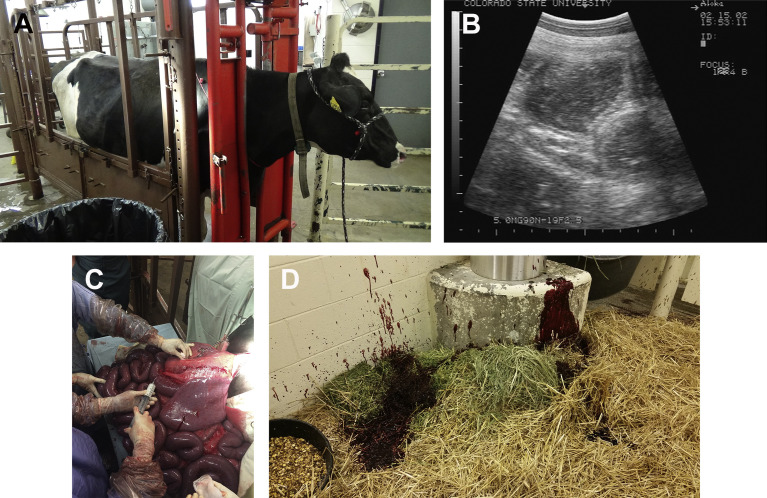
The abdominal distension in cases of clostridial abomasitis and enteritis is caused by gas and fluid distension of the abomasum and/or small intestine. The gaseous distension is a result of a combination of ileus and bacterial gas production. In most cases, passage of an orogastric tube does not provide significant relief. If the distension is severe enough that it is compromising respiration, then percutaneous decompression of the abomasum can be performed. This decompression is best done with the animal in dorsal or left lateral recumbency (Fig. 6 ).85 The area of tympany is localized and quickly clipped and prepared for an aseptic procedure. A percutaneous abomasocentesis can then be performed using a 16-gauge to 20-gauge, 38-mm (1.5-inch) needle inserted directly through the skin into the abomasum. An extension set can be attached to the needle. Allow the gas to freely escape while placing slight pressure on the abdomen. Fluid that drains from the needle can be collected for anaerobic culture, PCR typing, or toxin assays. Before removing the needle, antimicrobials and C perfringens type C and D antitoxin can be administered directly into the abomasum (these syringes should be prepared and ready before starting the abomasocentesis).
Fig. 6.
Abomasocentesis performed in a 3-week-old Holstein calf in order to decompress a tightly distended abomasum. This procedure is best done with the calf in dorsal or left lateral recumbency. Following decompression, fluid samples can be obtained for culture and genotyping as well as cytology. Antibiotics and antitoxin can also be administered directly into the abomasum.
Systemic support generally involves administration of IV fluids. Because the animals typically have ileus and abdominal distension, oral fluids, including milk, are not indicated until the distension is resolved (generally 12–24 hours). IV fluids provide systemic support in treatment of the hypovolemic or maldistributive shock that is often observed in these patients. Some animals with clostridial enteritis do not show significant clinical dehydration, most likely because of the rapid effects of the toxins. Shock fluid rates are 80 mL/kg, and can be divided into one-quarter doses given to effect at intervals of 15 to 30 minutes. Once the shock has been addressed, the fluid rate can be decreased to a maintenance rate of 3 mL/kg/h. Dextrose (5%) can also be provided in the maintenance fluids, because milk is likely to be withheld for 12 to 24 hours. Many animals with clostridial enteritis show mild to moderate hypochloremic metabolic alkalosis caused by the intestinal ileus and delayed abomasal emptying. Thus, isotonic sodium chloride is a suitable initial fluid type to resolve the hypochloremic alkalosis if present. Animals in later stages of the disease may show metabolic acidosis and require the addition of sodium bicarbonate to fluids. IV fluids can be changed to a balanced electrolyte solution after resolution of the shock, or within the first 12 hours.
Antimicrobials are used to slow or stop clostridial proliferation in the GI tract. The challenge is that the bacteria reside within the lumen so antimicrobial treatment must be selected such that an appropriate antimicrobial is delivered to the lumen of the abomasum and small intestine. Many antimicrobials are effective against C perfringens. Penicillin is one of the most effective antibiotics at killing C perfringens; however, penicillin does not immediately kill the bacteria. During the initial phase, the bacteria may continue to produce and release lethal exotoxins.86 Further, systemically administered penicillin is excreted via the renal system and is minimally excreted or secreted into the GI tract. Thus, oral procaine penicillin G (22,000 IU/kg, by mouth, every 24 hours for 3–5 days) may be recommended for treatment and has been used by the authors. Most C perfringens isolates are susceptible to oxytetracycline. Oxytetracycline is a bacteriostatic agent that inhibits protein synthesis. Oxytetracycline reduces C perfringens toxin production in vitro more rapidly than penicillin.86 Systemically administered oxytetracycline is partially excreted through the liver and biliary system and enters the lumen of the GI tract through the common bile duct. Both oral penicillin and systemic or oral oxytetracycline, alone or in combination, have been found to be clinically effective in treating acute cases of clostridial enteritis at Colorado State University (authors’ personal experience). Metronidazole, although effective against C perfringens, is a substituted benzimidazole and is illegal in all food animals including cattle, sheep, goats, and swine.
One study with a food safety focus has suggested that use of egg yolk antibody from hens immunized against C perfringens could significantly inhibit the growth and sporulation of C perfringens in vitro.87 An oral product intended for calves that contains egg-derived antibodies from hens immunized against C perfringens types A, C, and D is commercially available (EPIC Calf Scour Formula, Tomlyn), but its use in treatment or prevention of clinical cases of C perfringens has not been described.
In addition to administering an appropriate antimicrobial, bacterial proliferation may be decreased by withholding milk feedings for a period of 12 to 24 hours. In cases in which medical treatment is successful, the calves generally want to nurse within 12 to 24 hours. It is critical that, after this time, milk feeding is reinstituted slowly in small volumes (500 mL [1 pint]) at more frequent intervals (every 4 to 6 hours). Overfeeding can result in a relapse of C perfringens overgrowth.
Attempts to restore normal GI flora may also be beneficial once oral intake resumes. Oral administration of fresh rumen fluid may help restore normal GI flora in affected animals. Alternatively, commercially available probiotics can be administered. Placement of an indwelling nasogastric tube greatly facilitates frequent administration of oral medications and transfaunation in patients that do not quickly regain nursing activity.
There is limited information on effective treatments for neutralizing C perfringens toxins. In the case of clostridial toxins that work directly on the GI mucosa, neutralization must occur within the GI lumen to be most effective. C perfringens type C and D antitoxin contains antibodies against the beta and epsilon toxins and may provide efficacy against enteritis caused by C perfringens types B, C, and D. Systemically administered antitoxin may not reach effective concentrations within the GI tract. However, it is highly effective at neutralizing systemically absorbed epsilon toxin (C perfringens types D and B) associated with neurologic signs of enterotoxemia. When treating enteric clostridiosis, the authors recommend a combination of both systemic and oral C and D antitoxin at the labeled amounts.
Di-tri-octahedral smectite (Bio-Sponge, Platinum Performance) has been shown to bind C perfringens alpha, beta, and beta-2 toxins, and enterotoxin.88, 89 Kaolin-pectin and bismuth subsalicylate have also been used to bind C perfringens toxins; however, there are limited data showing efficacy. Both kaolin-pectin and bismuth subsalicylate could have clinical benefit in treating the damaged mucosal epithelium. Kaolin in Kaopectate is a potent activator of the extrinsic clotting cascade and may help decrease intestinal blood loss in cases with hemorrhagic gastroenteritis. Use of proton pump inhibitors in an attempt to limit mucosal ulceration in clostridial abomasitis cases should likely be discouraged, because there is evidence that these are a risk factor for the development of some types of clostridial GI infections in humans.90
Pain management should be used on an as-needed basis in these cases. Nonsteroidal antiinflammatories should be used judiciously, because severe shock and decreased renal perfusion may be present. In addition, GI ulceration can occur from the primary disease process, and this could be exacerbated by use or overuse of nonsteroidal antiinflammatory drugs such as flunixin meglumine or meloxicam. A low dose of flunixin meglumine, as is used to treat the effects of Gram-negative sepsis (0.25 mg/kg IV every 6 hours or 0.3 mg/kg IV every 8 hours) may be preferable to using the labeled cattle dose (up to 2.2 mg/kg IV every 24 hours). Opioids are an alternative selection for pain control but can decrease GI motility and should therefore be used cautiously in cases of suspected clostridial gastroenteritis. However, use of butorphanol intramuscularly (0.02–0.1 mg/kg every 6–8 hours) or as a constant rate infusion (CRI) (13 μg/kg/h) in horses with anterior enteritis is reported to have minimal effects on GI motility.91 As with all drugs used extralabel in food-producing species, the Food Animal Residue Avoidance Databank (www.farad.org) should be consulted for a meat and/or milk withdrawal time before the administration of any of these agents.
Early medical treatment of C perfringens type A abomasitis and enteritis cases can often have dramatic success (Fig. 7 ). Calves are often standing and eager to nurse within 12 to 24 hours when treatment is initiated early. It is important to initially limit milk intake to smaller frequent quantities and gradually return to a normal feeding over 5 to 10 days. Differentiation of C perfringens type A hemorrhagic enteritis in adult cattle may be difficult to distinguish from intestinal obstruction. In these cases, an exploratory laparotomy may be performed. Distended hemorrhagic small intestine without intraluminal obstruction is observed (see Fig. 4C). During surgery, intestinal samples can be obtained at surgery for bacterial culture, genotyping, and cytology if indicated. Treatment can be initiated intraoperatively with intraluminal injections of penicillin. In our experience, exploratory laparotomy in these cases has not seemed to be detrimental and greatly aids confirmation of a diagnosis and initial treatment.
Fig. 7.
Beef calf with suspected C perfringens abomasitis. The calf showed marked abdominal distension and abomasal tympany at presentation (A). The calf was treated medically and the abdominal distension resolved within 24 hours (B).
Prevention
Vaccination
Vaccination is considered to be the cornerstone of preventive programs for clostridial diseases in livestock.72, 92 Conventional commercial C perfringens C and D or 7-way or 8-way toxoid vaccines are very effective at preventing disease caused by C perfringens types B, C, and D in young animals. Type B disease, however, is very rare in the United States. In the following review of the literature, summaries to facilitate evidence-based decisions are presented. It is critical to understand that the conclusions reached in these studies should be related to the specific vaccine products tested in each trial.
In sheep in North America, immunization against the major toxins of C perfringens types C and D is warranted. Tetanus is also considered an essential component of a flock immunization program.93, 94 In a 1962 study in sheep, Sterne and colleagues95 showed that a multivalent, alum-adjuvanted, formalin-inactivated clostridial bacterin-toxoid administered to sheep in 2 doses induced titers deemed protective against the beta and epsilon toxins of C perfringens. In another study, antibody titers to epsilon toxin of C perfringens type D were induced in sheep immunized with a 2-dose series of a multivalent (8-way) clostridial vaccine.96 Immunization of ewes 3 weeks before lambing has been shown to induce colostral antibody titers against epsilon toxin that were adequate to impart protection of lambs for up to 12 weeks of age.97 In that study, adding a 2-dose immunization of the lambs at either days 1 and 21 of age or days 21 and 42 of age did not significantly change the titer of passively protected lambs. Immunization of lambs from vaccinated ewes (that do not have failure or suspected failure of passive transfer) with a C perfringens C and D and tetanus toxoid is recommended at 8 to 12 weeks of age and again 3 to 4 weeks later.94 Feeder lambs (and ideally replacement ewe lambs) can also receive a booster before entering the feedlot or being placed on a high-grain ration.94
In goats, most enterotoxemia cases in North America seem to be caused by C perfringens type D.66 Administration of multivalent ovine enterotoxemia vaccines twice annually to goats has been shown to be ineffective in protecting goats against fatal type D enterotoxemia.70 Goats do respond, albeit variably, to the epsilon toxin component of C perfringens type D vaccines labeled for sheep.68 The disparity in protection among the two species may reflect disparate mechanisms of disease. In sheep, most pathologic lesions seem to be the result of translocation of epsilon toxin from the gut to remote organs; for example, the brain. Circulating antitoxin antibodies against epsilon toxin seem to be critical in protecting sheep. In goats, however, the more localized disease process (enterocolitis) does not seem to be effectively or consistently curtailed by anti–epsilon toxin antibodies in the bloodstream.33, 68, 69 However, in a 1998 study, immunization with an epsilon toxoid combined with Freund incomplete adjuvant did protect goats against intraduodenal challenge with purified epsilon toxin, whereas a commercial, aluminum hydroxide–adjuvanted product did not.33 Existing C perfringens C and D toxoids may need to be administered to goats more than twice per year to confer adequate (albeit partial) protection.70
Administration of C perfringens type C and D to cattle has been shown to induce protective titers against both the beta toxin98 and epsilon toxin99 in recipients. Neonates and young, growing animals in stocker operations and feedlots are considered to be at higher risk for clostridial diseases relative to adults, but the risk seems to vary among herds.72, 92 For the former group, immunization of pregnant cows and heifers has been shown to produce antitoxin titers considered adequate for protection against type C and D infections in colostrum-fed calves.99 Many ranchers immunize calves with multivalent clostridial vaccines before weaning, but, in many cases, repeat immunization of calves to provoke an anamnestic titer is not consistently performed during the preweaning period. Troxel and colleagues99 determined that vaccination of colostrum-fed calves (from immunized dams) with a multivalent clostridial vaccine at 50 to 53 days of age and again at weaning at ∼170 days produced titers to beta and epsilon toxin that were not considered protective for calves during the preweaning period. The investigators concluded that this 4-month gap between the first and second immunizations may not be optimal for herds in which clostridial diseases occur in preweaned calves, and alterations in management and/or vaccination schedule would be warranted in such cases. In another study, immunization of colostrum-fed calves (from immunized dams) at 3 weeks of age with a single-dose clostridial bacterin-toxoid did not significantly affect type C or D antitoxin titers over the first 4 months of life; however, significant differences in antitoxin titers among different vaccines were apparent.100
In a 2000 survey of feedlot operators, more than 90% of operators overseeing lots with a capacity more than 8000 head used at least 1 type of clostridial vaccine in their cattle.101 In a prospective feedlot study involving nearly 19,000 animals, death losses were compared among calves immunized against clostridial diseases and those that were not.102 Treated calves were administered a 7-way clostridial vaccine at arrival and 30 days later. Reduction in death loss in the vaccinated calves, weighed against purchase price and vaccine cost, provided an additional net profit of more than $10 per vaccinate.102 More recently, DeGroot and colleagues103 found no detectable effect of booster vaccination with a multivalent clostridial vaccine on sudden death syndrome mortality in feedlot cattle.
Although the former study has sometimes been used as justification for use of clostridial vaccines in feedlot calves,92 additional research has investigated the potential detrimental effects of this use. Because ownership is not always retained for groups of cattle moving from ranch to feedlot, the immunization history of incoming cattle at a feedlot is not always known. As a result, some animals may receive multiple (predicted as many as 6) clostridial vaccinations before marketing, potentially compounding problems with injection site reactions in carcasses.104 When administered subcutaneously twice to feedlot calves, a 7-way clostridial vaccine induced significant reduction in feed intake after the second immunization and larger injection site lesions than did a C perfringens type C and D toxoid.104
C perfringens type C and D toxoid vaccines are not designed to specifically stimulate an immune response against alpha toxin. Thus, these vaccines are generally not considered to be effective at preventing abomasitis or enteritis caused by type A strains. One commercial type A toxoid vaccine is available (Clostridium Perfringens Type A Toxoid, Elanco) and has been shown to be safe and stimulate an antibody response against alpha toxin. However, because of the difficulty in developing a satisfactory experimental challenge model, efficacy has not yet been shown in order to have a preventive label. Autogenous C perfringens type A vaccines can also be used. The efficacy of these vaccines for C perfringens is still not established. A recent study has shown that although formaldehyde inactivated alpha toxin vaccines stimulated antibody production similar to native alpha toxin vaccines, only antibodies produced from the native toxin vaccines provided protection in an intestinal loop assay.105 Recombinant vaccines may offer advantages compared with conventional toxoid vaccines in the future.106
C perfringens vaccination strategies based on species, age, and animal use are provided in Table 3 .
Table 3.
Summary of current best-practice Clostridium perfringens toxoid vaccine recommendations for disease prevention, based on review of the literature
| Species and Age Group | Type of Vaccine | Timing and Frequency of Vaccination | Reasoning and Type of Immunity Induced |
|---|---|---|---|
| Bred heifers and adult cows, both beef and dairy |
|
|
|
|
|
|
|
| Feedlot cattle |
|
|
|
| Beef and dairy calves (particularly from herds with previous C perfringens type C or D outbreaks) |
|
|
|
| Adult sheep |
|
|
|
| Bred ewes |
|
|
|
| Lambs from vaccinated dams |
|
|
|
| Lambs from unvaccinated dams or with suspected FPT |
|
|
|
| Adult goats and kids |
|
|
|
| Bred does |
|
|
— |
Abbreviation: FPT, failure of passive transfer.
Feeding and Environmental Management
Presentation of excessive amounts of starch, sugar, or soluble protein into the stomach and/or intestines is considered pivotal in the development of these diseases; thus, all potential influences on this crucial event must be considered when formulating a preventive plan. Evaluation of ration net energy, fiber content and forage length, bunk space, animal hierarchy within a pen, feeding frequency, the rate and magnitude of changes in ration between successive production groups, and feed mixing practices is essential to identify and correct problems with carbohydrate overload and/or so-called slug feeding. For pasture-fed animals, turnout onto a new, particularly lush pasture should be very gradual (eg, day 1, 15 minutes of grazing; day 2, 30 minutes; day 3, 1 hour; day 4, 2 hours; and so forth).
Prevention of enterotoxemia in nursing animals requires consideration of environmental or management factors that may trigger changes in milk composition or volume for lactating dams. Intermittent provision of high-energy supplements to range animals may trigger changes in milk production. Similarly, management practices that cause prolonged interruption of suckling (eg, cow processing for pregnancy examination) must be made time-efficient in order to limit engorgement of the udder and subsequent ingestion by the neonate of a larger-than-normal milk meal. Sudden and severe changes in weather may cause dams and their offspring to seek shelter or remain recumbent for prolonged periods of time; provision of multiple locales for shelter and bedding, or simply encouraging dams to eat by providing hay (weather permitting) may encourage more frequent nursing than if the animals were left to “sit the storm out.”
In dairy calves, variable or improper mixing of milk replacers may increase the incidence of clostridial GI disease. Milk replacers should be mixed at the appropriate concentration and temperature. Some milk replacers are prone to settling out and can result in variable concentrations between what is fed from the start to the finish of a single batch. Milk replacers high in protein and carbohydrate may also promote clostridial overgrowth in the GI tract.
Clostridium difficile
Clostridium difficile is another potential cause of enteritis, but the relationship between C difficile infection (CDI) and GI disease in ruminants is unclear because the bacterium may be present in the feces of clinically normal animals. A high prevalence of C difficile shedding has been described in otherwise healthy young calves; in one study, 14.9% of calves without clinical disease were shedding the organism.108 In otherwise healthy veal calves, CDI has been reported to be as high as 51%.109 C difficile shedding has also been detected in dairy cows,110 feedlot cattle,111 sheep,112 and goats.113
Hammitt and colleagues114 found C difficile and its toxins (toxin A and toxin B) in 25.3% and 22.9%, respectively, of calves with diarrhea. Diarrheic calves were twice as likely to be culture positive compared with those without diarrhea.114 Nondiarrheic calves, however, more commonly had toxin-positive stools.114 This team of researchers concluded that these findings lent credence to the idea that CDI may manifest as diarrhea in young cattle.114
C difficile–associated diarrhea (CDAD) was also suspected in a neonatal elk calf, based on finding a toxigenic C difficile fecal isolate in the absence of other more common enteropathogens.115 Similarly, the authors have tentatively diagnosed 3 alpaca crias with CDAD based on fecal ELISAs positive for C difficile toxins A and/or B, in combination with exclusion of other common infectious causes of camelid diarrhea and a history of prior antimicrobial administration (authors’ personal experience). It is possible that CDAD in livestock occurs more frequently than reported, but it remains underdiagnosed because attempted identification of C difficile and its toxins is not routinely performed in most diarrheic ruminants.
Summary
Clostridial abomasitis and enteritis remain common clinical diseases in livestock, particularly in young ruminants. C perfringens types A, B, C, and D are the most common causes, although enteritis caused by C difficile is also reported. Commercial C perfringens C and D vaccines are effective at preventing disease caused by type B, C, and D strains but do not provide adequate protection for type A strains. When clinical cases are identified early, treatment can be successful if provided promptly.
Footnotes
Disclosure: The authors have nothing to disclose.
References
- 1.Lebrun M., Mainil J.G., Linden A. Cattle enterotoxaemia and Clostridium perfringens: description, diagnosis and prophylaxis. Vet Rec. 2010;167(1):13–22. doi: 10.1136/vr.167.1.12. [DOI] [PubMed] [Google Scholar]
- 2.Uzal F.A., Songer J.G. Diagnosis of Clostridium perfringens intestinal infections in sheep and goats. J Vet Diagn Invest. 2008;20(3):253–265. doi: 10.1177/104063870802000301. [DOI] [PubMed] [Google Scholar]
- 3.Songer J.G. Clostridial enteric diseases of domestic animals. Clin Microbiol Rev. 1996;9(2):216–234. doi: 10.1128/cmr.9.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis C.J. Control of important clostridial diseases of sheep. Vet Clin North Am Food Anim Pract. 2011;27(1):121–126. doi: 10.1016/j.cvfa.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Borriello S.P., Carman R.J., editors. Clostridia in gastrointestinal disease. CRC Press; Boca Raton (FL): 1992. pp. 195–221. [Google Scholar]
- 6.Vance H.N. A survey of the alimentary tract of cattle for Clostridium perfringens. Can J Comp Med Vet Sci. 1967;31(10):260–264. [PMC free article] [PubMed] [Google Scholar]
- 7.Rood J.I. Virulence genes of Clostridium perfringens. Annu Rev Microbiol. 1998;52:333–360. doi: 10.1146/annurev.micro.52.1.333. [DOI] [PubMed] [Google Scholar]
- 8.Petit L., Gibert M., Popoff M.R. Clostridium perfringens: toxinotype and genotype. Trends Microbiol. 1999;7(3):104–110. doi: 10.1016/s0966-842x(98)01430-9. [DOI] [PubMed] [Google Scholar]
- 9.Stiles B.G., Barth G., Barth H. Clostridium perfringens epsilon toxin: a malevolent molecule for animals and man? Toxins (Basel) 2013;5(11):2138–2160. doi: 10.3390/toxins5112138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deprez P. Clostridium perfringens infections - a diagnostic challenge. Vet Rec. 2015;177(15):388–389. doi: 10.1136/vr.h5428. [DOI] [PubMed] [Google Scholar]
- 11.Hofshagen M., Stenwig H. Toxin production by Clostridium perfringens isolated from broiler chickens and capercaillies (Tetrao urogallus) with and without necrotizing enteritis. Avian Dis. 1992;36(4):837–843. [PubMed] [Google Scholar]
- 12.Katayama S., Matsushita O., Minami J. Comparison of the alpha-toxin genes of Clostridium perfringens type A and C strains: evidence for extragenic regulation of transcription. Infect Immun. 1993;61(2):457–463. doi: 10.1128/iai.61.2.457-463.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bueschel D.M., Jost B.H., Billington S.J. Prevalence of cpb2, encoding beta2 toxin, in Clostridium perfringens field isolates: correlation of genotype with phenotype. Vet Microbiol. 2003;94(2):121–129. doi: 10.1016/s0378-1135(03)00081-6. [DOI] [PubMed] [Google Scholar]
- 14.Garmory H.S., Chanter N., French N.P. Occurrence of Clostridium perfringens beta2-toxin amongst animals, determined using genotyping and subtyping PCR assays. Epidemiol Infect. 2000;124(1):61–67. doi: 10.1017/s0950268899003295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Songer J.G., Miskimins D.W. Clostridial abomasitis in calves: case report and review of the literature. Anaerobe. 2005;11(5):290–294. doi: 10.1016/j.anaerobe.2004.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Songer J.G., Uzal F.A. Clostridial enteric infections in pigs. J Vet Diagn Invest. 2005;17(6):528–536. doi: 10.1177/104063870501700602. [DOI] [PubMed] [Google Scholar]
- 17.Dennison A.C., Van Metre D.C., Morley P.S. Comparison of the odds of isolation, genotypes, and in vivo production of major toxins by Clostridium perfringens obtained from the gastrointestinal tract of dairy cows with hemorrhagic bowel syndrome or left-displaced abomasum. J Am Vet Med Assoc. 2005;227(1):132–138. doi: 10.2460/javma.2005.227.132. [DOI] [PubMed] [Google Scholar]
- 18.Dennison A.C., VanMetre D.C., Callan R.J. Hemorrhagic bowel syndrome in dairy cattle: 22 cases (1997-2000) J Am Vet Med Assoc. 2002;221(5):686–689. doi: 10.2460/javma.2002.221.686. [DOI] [PubMed] [Google Scholar]
- 19.Ceci L., Paradies P., Sasanelli M. Haemorrhagic bowel syndrome in dairy cattle: possible role of Clostridium perfringens type A in the disease complex. J Vet Med A Physiol Pathol Clin Med. 2006;53(10):518–523. doi: 10.1111/j.1439-0442.2006.00884.x. [DOI] [PubMed] [Google Scholar]
- 20.Abutarbush S.M., Radostits O.M. Jejunal hemorrhage syndrome in dairy and beef cattle: 11 cases (2001 to 2003) Can Vet J. 2005;46(8):711–715. [PMC free article] [PubMed] [Google Scholar]
- 21.Ewoldt J.M., Anderson D.E. Determination of the effect of single abomasal or jejunal inoculation of Clostridium perfringens type A in dairy cows. Can Vet J. 2005;46(9):821–824. [PMC free article] [PubMed] [Google Scholar]
- 22.Freedman J.C., Shrestha A., McClane B.A. Clostridium perfringens enterotoxin: action, genetics, and translational applications. Toxins (Basel) 2016;8(3) doi: 10.3390/toxins8030073. [pii:E73] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakurai J., Nagahama M., Oda M. Clostridium perfringens alpha-toxin: characterization and mode of action. J Biochem. 2004;136(5):569–574. doi: 10.1093/jb/mvh161. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez Miyakawa M.E., Uzal F.A. Morphologic and physiologic changes induced by Clostridium perfringens type A alpha toxin in the intestine of sheep. Am J Vet Res. 2005;66(2):251–255. doi: 10.2460/ajvr.2005.66.251. [DOI] [PubMed] [Google Scholar]
- 25.Goossens E., Valgaeren B.R., Pardon B. Rethinking the role of alpha toxin in Clostridium perfringens-associated enteric diseases: a review on bovine necro-haemorrhagic enteritis. Vet Res. 2017;48(1):9. doi: 10.1186/s13567-017-0413-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verherstraeten S., Goossens E., Valgaeren B. The synergistic necrohemorrhagic action of Clostridium perfringens perfringolysin and alpha toxin in the bovine intestine and against bovine endothelial cells. Vet Res. 2013;44:45. doi: 10.1186/1297-9716-44-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tweten R.K. Clostridium perfringens beta toxin and Clostridium septicum alpha toxin: their mechanisms and possible role in pathogenesis. Vet Microbiol. 2001;82(1):1–9. doi: 10.1016/s0378-1135(01)00372-8. [DOI] [PubMed] [Google Scholar]
- 28.Alves G.G., Machado de Avila R.A., Chavez-Olortegui C.D. Clostridium perfringens epsilon toxin: the third most potent bacterial toxin known. Anaerobe. 2014;30:102–107. doi: 10.1016/j.anaerobe.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 29.Freedman J.C., McClane B.A., Uzal F.A. New insights into Clostridium perfringens epsilon toxin activation and action on the brain during enterotoxemia. Anaerobe. 2016;41:27–31. doi: 10.1016/j.anaerobe.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Greco G., Madio A., Buonavoglia D. Clostridium perfringens toxin-types in lambs and kids affected with gastroenteric pathologies in Italy. Vet J. 2005;170(3):346–350. doi: 10.1016/j.tvjl.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 31.Finnie J.W. Pathogenesis of brain damage produced in sheep by Clostridium perfringens type D epsilon toxin: a review. Aust Vet J. 2003;81(4):219–221. doi: 10.1111/j.1751-0813.2003.tb11474.x. [DOI] [PubMed] [Google Scholar]
- 32.Uzal F.A., Kelly W.R., Morris W.E. Effects of intravenous injection of Clostridium perfringens type D epsilon toxin in calves. J Comp Pathol. 2002;126(1):71–75. doi: 10.1053/jcpa.2001.0514. [DOI] [PubMed] [Google Scholar]
- 33.Uzal F.A., Kelly W.R. Experimental Clostridium perfringens type D enterotoxemia in goats. Vet Pathol. 1998;35(2):132–140. doi: 10.1177/030098589803500207. [DOI] [PubMed] [Google Scholar]
- 34.Uzal F.A., Kelly W.R. Effects of the intravenous administration of Clostridium perfringens type D epsilon toxin on young goats and lambs. J Comp Pathol. 1997;116(1):63–71. doi: 10.1016/s0021-9975(97)80044-8. [DOI] [PubMed] [Google Scholar]
- 35.Morris W.E., Goldstein J., Redondo L.M. Clostridium perfringens epsilon toxin induces permanent neuronal degeneration and behavioral changes. Toxicon. 2017;130:19–28. doi: 10.1016/j.toxicon.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 36.Barth H., Aktories K., Popoff M.R. Binary bacterial toxins: biochemistry, biology, and applications of common Clostridium and Bacillus proteins. Microbiol Mol Biol Rev. 2004;68(3):373–402. doi: 10.1128/MMBR.68.3.373-402.2004. Table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schotte U., Truyen U., Neubauer H. Significance of beta 2-toxigenic Clostridium perfringens infections in animals and their predisposing factors–a review. J Vet Med B Infect Dis Vet Public Health. 2004;51(10):423–426. doi: 10.1111/j.1439-0450.2004.00802.x. [DOI] [PubMed] [Google Scholar]
- 38.Gkiourtzidis K., Frey J., Bourtzi-Hatzopoulou E. PCR detection and prevalence of alpha-, beta-, beta 2-, epsilon-, iota- and enterotoxin genes in Clostridium perfringens isolated from lambs with clostridial dysentery. Vet Microbiol. 2001;82(1):39–43. doi: 10.1016/s0378-1135(01)00327-3. [DOI] [PubMed] [Google Scholar]
- 39.Manteca C., Daube G., Jauniaux T. A role for the Clostridium perfringens beta2 toxin in bovine enterotoxaemia? Vet Microbiol. 2002;86(3):191–202. doi: 10.1016/S0378-1135(02)00008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehdizadeh I., Parreira V., Prescott J. 2015 ACVIM proceedings: a novel pore-forming toxin in type A Clostridium perfringens associated with fatal canine hemorrhagic gastroenteritis and neonatal foal necrotizing enterocolitis. J Vet Intern Med. 2015;29:1205. doi: 10.1371/journal.pone.0122684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gohari I.M., Parreira V.R., Timoney J.F. NetF-positive Clostridium perfringens in neonatal foal necrotising enteritis in Kentucky. Vet Rec. 2016;178(9):216. doi: 10.1136/vr.103606. [DOI] [PubMed] [Google Scholar]
- 42.Keyburn A.L., Boyce J.D., Vaz P. NetB, a new toxin that is associated with avian necrotic enteritis caused by Clostridium perfringens. PLoS Pathog. 2008;4(2):e26. doi: 10.1371/journal.ppat.0040026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keyburn A.L., Yan X.X., Bannam T.L. Association between avian necrotic enteritis and Clostridium perfringens strains expressing NetB toxin. Vet Res. 2010;41(2):21. doi: 10.1051/vetres/2009069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keyburn A.L., Sheedy S.A., Ford M.E. Alpha-toxin of Clostridium perfringens is not an essential virulence factor in necrotic enteritis in chickens. Infect Immun. 2006;74(11):6496–6500. doi: 10.1128/IAI.00806-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schlegel B.J., Nowell V.J., Parreira V.R. Toxin-associated and other genes in Clostridium perfringens type A isolates from bovine clostridial abomasitis (BCA) and jejunal hemorrhage syndrome (JHS) Can J Vet Res. 2012;76(4):248–254. [PMC free article] [PubMed] [Google Scholar]
- 46.Valgaeren B., Pardon B., Goossens E. lesion development in a new intestinal loop model indicates the involvement of a shared Clostridium perfringens virulence factor in haemorrhagic enteritis in calves. J Comp Pathol. 2013;149(1):103–112. doi: 10.1016/j.jcpa.2012.11.237. [DOI] [PubMed] [Google Scholar]
- 47.Van Kruiningen H.J., Nyaoke C.A., Sidor I.F. Clostridial abomasal disease in Connecticut dairy calves. Can Vet J. 2009;50(8):857–860. [PMC free article] [PubMed] [Google Scholar]
- 48.Manteca C., Jauniaux T., Daube G. Isolation of Clostridium perfringens from three calves with hemorrhagic abomasitis. Revue de Médecine Vétérinaire. 2001;152:637–639. [Google Scholar]
- 49.Roeder B.L., Chengappa M.M., Nagaraja T.G. Isolation of Clostridium perfringens from neonatal calves with ruminal and abomasal tympany, abomasitis, and abomasal ulceration. J Am Vet Med Assoc. 1987;190(12):1550–1555. [PubMed] [Google Scholar]
- 50.Songer J.G., Miskimmins D.W. Clostridium perfringens type E enteritis in calves: two cases and a brief review of the literature. Anaerobe. 2004;10(4):239–242. doi: 10.1016/j.anaerobe.2004.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roeder B.L., Chengappa M.M., Nagaraja T.G. Experimental induction of abdominal tympany, abomasitis, and abomasal ulceration by intraruminal inoculation of Clostridium perfringens type A in neonatal calves. Am J Vet Res. 1988;49(2):201–207. [PubMed] [Google Scholar]
- 52.Russell W.C. Type A enterotoxemia in captive wild goats. J Am Vet Med Assoc. 1970;157(5):643–646. [PubMed] [Google Scholar]
- 53.Leite Filho R.V., Bianchi M.V., Fredo G. Emphysematous abomasitis in a lamb by bacteria of the Sarcina genus in Southern Brazil. Ciência Rural. 2016;46(2):300–303. [Google Scholar]
- 54.Edwards G.T., Woodger N.G., Barlow A.M. Sarcina-like bacteria associated with bloat in young lambs and calves. Vet Rec. 2008;163(13):391–393. doi: 10.1136/vr.163.13.391. [DOI] [PubMed] [Google Scholar]
- 55.DeBey B.M., Blanchard P.C., Durfee P.T. Abomasal bloat associated with Sarcina-like bacteria in goat kids. J Am Vet Med Assoc. 1996;209(8):1468–1469. [PubMed] [Google Scholar]
- 56.Carlson S.A., Stoffregen W.C., Bolin S.R. Abomasitis associated with multiple antibiotic resistant Salmonella enterica serotype Typhimurium phagetype DT104. Vet Microbiol. 2002;85(3):233–240. doi: 10.1016/s0378-1135(01)00508-9. [DOI] [PubMed] [Google Scholar]
- 57.Carlson S.A., Meyerholz D.K., Stabel T.J. Secretion of a putative cytotoxin in multiple antibiotic resistant Salmonella enterica serotype Typhimurium phagetype DT104. Microb Pathog. 2001;31(4):201–204. doi: 10.1006/mpat.2001.0461. [DOI] [PubMed] [Google Scholar]
- 58.Hunter A.G., Mathieson A.O., Scott J.A. An outbreak of S typhimurium in sheep and its consequences. Vet Rec. 1976;98(7):126–130. doi: 10.1136/vr.98.7.126. [DOI] [PubMed] [Google Scholar]
- 59.Maratea K.A., Miller M.A. Abomasal coccidiosis associated with proliferative abomasitis in a sheep. J Vet Diagn Invest. 2007;19(1):118–121. doi: 10.1177/104063870701900122. [DOI] [PubMed] [Google Scholar]
- 60.Morin M., Lariviere S., Lallier R. Pathological and microbiological observations made on spontaneous cases of acute neonatal calf diarrhea. Can J Comp Med. 1976;40(3):228–240. [PMC free article] [PubMed] [Google Scholar]
- 61.Marshall T.S. Abomasal ulceration and tympany of calves. Vet Clin North Am Food Anim Pract. 2009;25(1):209–220. doi: 10.1016/j.cvfa.2008.10.010. viii. [DOI] [PubMed] [Google Scholar]
- 62.Lilley C.W., Hamar D.W., Gerlach M. Linking copper deficiency with abomasal ulcers in beef calves. Vet Med. 1985;(80):85–88. [Google Scholar]
- 63.Mills K.W., Johnson J.L., Jensen R.L. Laboratory findings associated with abomasal ulcers/tympany in range calves. J Vet Diagn Invest. 1990;2(3):208–212. doi: 10.1177/104063879000200310. [DOI] [PubMed] [Google Scholar]
- 64.Goossens E., Verherstraeten S., Timbermont L. Clostridium perfringens strains from bovine enterotoxemia cases are not superior in in vitro production of alpha toxin, perfringolysin O and proteolytic enzymes. BMC Vet Res. 2014;10:32. doi: 10.1186/1746-6148-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Niilo L. Clostridium perfringens in animal disease: a review of current knowledge. Can Vet J. 1980;21(5):141–148. [PMC free article] [PubMed] [Google Scholar]
- 66.Guss SB. Enterotoxemia. Paper presented at: symposium on health and disease of sheep and goats, American Association of Sheep and Goat Practitioners. Salt Lake City, 1979.
- 67.Niilo L. Clostridium perfringens type C enterotoxemia. Can Vet J. 1988;29(8):658–664. [PMC free article] [PubMed] [Google Scholar]
- 68.Uzal F.A., Kelly W.R. Enterotoxaemia in goats. Vet Res Commun. 1996;20(6):481–492. doi: 10.1007/BF00396291. [DOI] [PubMed] [Google Scholar]
- 69.Blackwell T.E., Butler D.G., Prescott J.F. Differences in signs and lesions in sheep and goats with enterotoxemia induced by intraduodenal infusion of Clostridium perfringens type D. Am J Vet Res. 1991;52(7):1147–1152. [PubMed] [Google Scholar]
- 70.Blackwell T.E., Butler D.G. Clinical signs, treatment, and postmortem lesions in dairy goats with enterotoxemia: 13 cases (1979-1982) J Am Vet Med Assoc. 1992;200(2):214–217. [PubMed] [Google Scholar]
- 71.Blackwell T.E. Enteritis and diarrhea. Vet Clin North Am Large Anim Pract. 1983;5(3):557–570. doi: 10.1016/s0196-9846(17)30063-0. [DOI] [PubMed] [Google Scholar]
- 72.Songer J.G. Clostridial vaccines. In: Smith B.P., editor. Large animal internal medicine. 3rd edition. Mosby; St Louis (MO): 2002. pp. 1430–1432. [Google Scholar]
- 73.Gardner D.E. Pathology of Clostridium welchii type D enterotoxaemia. II. Structural and ultrastructural alterations in the tissues of lambs and mice. J Comp Pathol. 1973;83(4):509–524. doi: 10.1016/0021-9975(73)90009-1. [DOI] [PubMed] [Google Scholar]
- 74.Bullen J.J., Battey I. Enterotoxaemia of sheep. Vet Rec. 1957;69:1268–1276. [Google Scholar]
- 75.Kim H.Y., Byun J.W., Roh I.S. First isolation of Clostridium perfringens type E from a goat with diarrhea. Anaerobe. 2013;22:141–143. doi: 10.1016/j.anaerobe.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Redondo L.M., Farber M., Venzano A. Sudden death syndrome in adult cows associated with Clostridium perfringens type E. Anaerobe. 2013;20:1–4. doi: 10.1016/j.anaerobe.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 77.Fohler S., Klein G., Hoedemaker M. Diversity of Clostridium perfringens toxin-genotypes from dairy farms. BMC Microbiol. 2016;16(1):199. doi: 10.1186/s12866-016-0812-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Burgstaller J., Wittek T., Smith G.W. Invited review: abomasal emptying in calves and its potential influence on gastrointestinal disease. J Dairy Sci. 2017;100(1):17–35. doi: 10.3168/jds.2016-10949. [DOI] [PubMed] [Google Scholar]
- 79.Rosadio R., Londone P., Perez D. Eimeria macusaniensis associated lesions in neonate alpacas dying from enterotoxemia. Vet Parasitol. 2010;168(1–2):116–120. doi: 10.1016/j.vetpar.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 80.Rojas M., Manchego A., Rocha C.B. Outbreak of diarrhea among preweaning alpacas (Vicugna pacos) in the southern Peruvian highland. J Infect Dev Ctries. 2016;10(3):269–274. doi: 10.3855/jidc.7398. [DOI] [PubMed] [Google Scholar]
- 81.Kirino Y., Tanida M., Hasunuma H. Increase of Clostridium perfringens in association with Eimeria in haemorrhagic enteritis in Japanese beef cattle. Vet Rec. 2015;177(8):202. doi: 10.1136/vr.103237. [DOI] [PubMed] [Google Scholar]
- 82.Meer R.R., Songer J.G. Multiplex polymerase chain reaction assay for genotyping Clostridium perfringens. Am J Vet Res. 1997;58(7):702–705. [PubMed] [Google Scholar]
- 83.Daube G., Simon P., Limbourg B. Hybridization of 2,659 Clostridium perfringens isolates with gene probes for seven toxins (alpha, beta, epsilon, iota, theta, mu, and enterotoxin) and for sialidase. Am J Vet Res. 1996;57(4):496–501. [PubMed] [Google Scholar]
- 84.Valgaeren B.R., Pardon B., Verherstraeten S. Intestinal clostridial counts have no diagnostic value in the diagnosis of enterotoxaemia in veal calves. Vet Rec. 2013;172(9):237. doi: 10.1136/vr.101236. [DOI] [PubMed] [Google Scholar]
- 85.Kümper H. A new treatment for abomasal bloat in calves. Bovine Practitioner. 1995;(29):80–82. [Google Scholar]
- 86.Stevens D.L., Maier K.A., Mitten J.E. Effect of antibiotics on toxin production and viability of Clostridium perfringens. Antimicrob Agents Chemother. 1987;31(2):213–218. doi: 10.1128/aac.31.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Song M.S., Kim C.J., Cho W.I. Growth inhibition of Clostridium perfringens vegetative cells and spores using chicken immunoglobulin Y. J Food Saf. 2009;29(4):511–520. [Google Scholar]
- 88.Weese J.S., Cote N.M., de Gannes R.V. Evaluation of in vitro properties of di-tri-octahedral smectite on clostridial toxins and growth. Equine Vet J. 2003;35(7):638–641. doi: 10.2746/042516403775696384. [DOI] [PubMed] [Google Scholar]
- 89.Lawler J.B., Hassel D.M., Magnuson R.J. Adsorptive effects of di-tri-octahedral smectite on Clostridium perfringens alpha, beta, and beta-2 exotoxins and equine colostral antibodies. Am J Vet Res. 2008;69(2):233–239. doi: 10.2460/ajvr.69.2.233. [DOI] [PubMed] [Google Scholar]
- 90.Furuya-Kanamori L., Stone J.C., Clark J. Comorbidities, exposure to medications, and the risk of community-acquired Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36(2):132–141. doi: 10.1017/ice.2014.39. [DOI] [PubMed] [Google Scholar]
- 91.Javsicas L.H. Duodenitis-proximal jejunitis. In: Reed S.M., Bayly W.M., Sellon D.C., editors. Equine internal medicine. 3rd edition. Saunders; St Louis (MO): 2010. pp. 848–849. [Google Scholar]
- 92.Radostits O.M., Gay C.C., Blood D.C. WB Saunders; London: 2000. Veterinary medicine. [Google Scholar]
- 93.System NAHM. Reference of 1996 US sheep health management practices. In: USDA: APHIS:VS, ed. Fort Collins (CO): 1996.
- 94.Krueder A.J., Plummer P.J. Ovine and caprine vaccination programs. In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier; St. Louis (MO): 2015. pp. 1461–1462. [Google Scholar]
- 95.Sterne M., Batty I., Thomson A. Immunization of sheep with multi-component clostridial vaccines. Vet Rec. 1962;74:909–913. [Google Scholar]
- 96.Kerry J.B., Craig G.R. Field studies in sheep with multicomponent clostridial vaccines. Vet Rec. 1979;105(24):551–554. [PubMed] [Google Scholar]
- 97.de la Rosa C., Hogue D.E., Thonney M.L. Vaccination schedules to raise antibody concentrations against epsilon-toxin of Clostridium perfringens in ewes and their triplet lambs. J Anim Sci. 1997;75(9):2328–2334. doi: 10.2527/1997.7592328x. [DOI] [PubMed] [Google Scholar]
- 98.Kennedy K.K., Norris S.J., Beckenhauer W.H. Antitoxin response in cattle vaccinated with Clostridium perfringens type C toxoid. Vet Med Small Anim Clin. 1977;72(7):1213–1215. [PubMed] [Google Scholar]
- 99.Troxel T.R., Burke G.L., Wallace W.T. Clostridial vaccination efficacy on stimulating and maintaining an immune response in beef cows and calves. J Anim Sci. 1997;75(1):19–25. doi: 10.2527/1997.75119x. [DOI] [PubMed] [Google Scholar]
- 100.Troxel T.R., Gadberry M.S., Wallace W.T. Clostridial antibody response from injection-site lesions in beef cattle, long-term response to single or multiple doses, and response in newborn beef calves. J Anim Sci. 2001;79(10):2558–2564. doi: 10.2527/2001.79102558x. [DOI] [PubMed] [Google Scholar]
- 101.NAHMS . Part II: Baseline reference of feedlot health and management, 1999. In: USDA: APHIS:VS, editor. National Animal Health Monitoring System; Fort Collins (CO): 2000. [Google Scholar]
- 102.Knott G.K.L., Erwin B.G., Classick L.G. Benefits of a clostridial vaccination program in feedlot cattle. Vet Med. 1985;80:95–97. [Google Scholar]
- 103.De Groot B., Dewey C.E., Griffin D.D. Effect of booster vaccination with a multivalent clostridial bacterin-toxoid on sudden death syndrome mortality rate among feedlot cattle. J Am Vet Med Assoc. 1997;211(6):749–753. [PubMed] [Google Scholar]
- 104.Stokka G.L., Edwards A.J., Spire M.F. Inflammatory response to clostridial vaccines in feedlot cattle. J Am Vet Med Assoc. 1994;204(3):415–419. [PubMed] [Google Scholar]
- 105.Goossens E., Verherstraeten S., Valgaeren B.R. Toxin-neutralizing antibodies protect against Clostridium perfringens-induced necrosis in an intestinal loop model for bovine necrohemorrhagic enteritis. BMC Vet Res. 2016;12(1):101. doi: 10.1186/s12917-016-0730-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ferreira M.R., Moreira G.M., Cunha C.E. Recombinant alpha, beta, and epsilon toxins of Clostridium perfringens: production strategies and applications as veterinary vaccines. Toxins (Basel) 2016;8(11) doi: 10.3390/toxins8110340. [pii:E340] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Songer J.G. Clostridial vaccines. In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier; St. Louis (MO): 2015. pp. 1488–1490. [Google Scholar]
- 108.Rodriguez-Palacios A., Stampfli H.R., Duffield T. Clostridium difficile PCR ribotypes in calves, Canada. Emerg Infect Dis. 2006;12(11):1730–1736. doi: 10.3201/eid1211.051581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Costa M.C., Stampfli H.R., Arroyo L.G. Epidemiology of Clostridium difficile on a veal farm: prevalence, molecular characterization and tetracycline resistance. Vet Microbiol. 2011;152(3–4):379–384. doi: 10.1016/j.vetmic.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 110.Bandelj P., Blagus R., Briski F. Identification of risk factors influencing Clostridium difficile prevalence in middle-size dairy farms. Vet Res. 2016;47:41. doi: 10.1186/s13567-016-0326-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Costa M.C., Reid-Smith R., Gow S. Prevalence and molecular characterization of Clostridium difficile isolated from feedlot beef cattle upon arrival and mid-feeding period. BMC Vet Res. 2012;8:38. doi: 10.1186/1746-6148-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Koene M.G., Mevius D., Wagenaar J.A. Clostridium difficile in Dutch animals: their presence, characteristics and similarities with human isolates. Clin Microbiol Infect. 2012;18(8):778–784. doi: 10.1111/j.1469-0691.2011.03651.x. [DOI] [PubMed] [Google Scholar]
- 113.Avbersek J., Pirs T., Pate M. Clostridium difficile in goats and sheep in Slovenia: characterisation of strains and evidence of age-related shedding. Anaerobe. 2014;28:163–167. doi: 10.1016/j.anaerobe.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 114.Hammitt M.C., Bueschel D.A., Kee A.K. A possible role for Clostridium difficile in the etiology of calf enteritis. Vet Microbiol. 2008;127(3–4):343–352. doi: 10.1016/j.vetmic.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Arroyo L.G., Rousseau J.D., Staempfli H.R. Suspected Clostridium difficile-associated hemorrhagic diarrhea in a 1-week-old elk calf. Can Vet J. 2005;46(12):1130–1131. [PMC free article] [PubMed] [Google Scholar]