Abstract
BACKGROUND
Hospital readmissions for pneumonia occur often and are difficult to predict. For fiscal year 2013, the Centers for Medicare & Medicaid Services readmission penalties have been applied to acute myocardial infarction, heart failure, and pneumonia. However, the overall impact of pneumonia pathogen characterization on hospital readmission is undefined.
METHODS
This was a retrospective 6-year cohort study (August 2007 to September 2013).
RESULTS
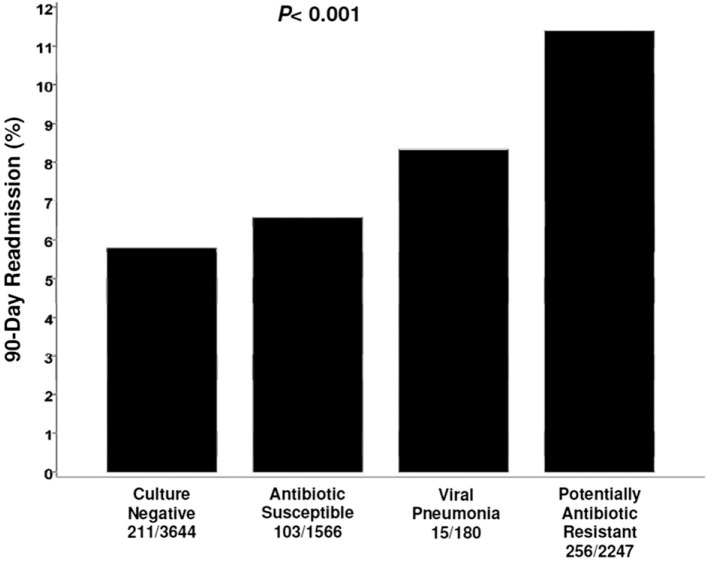
We evaluated 9,624 patients with a discharge diagnosis of pneumonia. Among these patients, 4,432 (46.1%) were classified as having culture-negative pneumonia, 1,940 (20.2%) as having pneumonia caused by antibiotic-susceptible bacteria, 2,991 (31.1%) as having pneumonia caused by potentially antibiotic-resistant bacteria, and 261 (2.7%) as having viral pneumonia. The 90-day hospital readmission rate for survivors (n = 7,637, 79.4%) was greatest for patients with pneumonia attributed to potentially antibiotic-resistant bacteria (11.4%) followed by viral pneumonia (8.3%), pneumonia attributed to antibiotic-susceptible bacteria (6.6%), and culture-negative pneumonia (5.8%) (P < .001). Multiple logistic regression analysis identified pneumonia attributed to potentially antibiotic-resistant bacteria to be independently associated with 90-day readmission (OR, 1.75; 95% CI, 1.56-1.97; P < .001). Other independent predictors of 90-day readmission were Charlson comorbidity score > 4, cirrhosis, and chronic kidney disease. Culture-negative pneumonia was independently associated with lower risk for 90-day readmission.
CONCLUSIONS
Readmission after hospitalization for pneumonia is relatively common and is related to pneumonia pathogen characterization. Pneumonia attributed to potentially antibiotic-resistant bacteria is associated with an increased risk for 90-day readmission, whereas culture-negative pneumonia is associated with lower risk for 90-day readmission.
Hospital readmissions occur often and are difficult to predict.1 In response to the recommendations in the 2007 Medicare Payment Advisory Commission report, many hospitals have dedicated staff efforts and resources to identify patients at risk for readmission as well as to prevent such readmissions.1, 2 The recommendations from the 2007 Medicare Payment Advisory Commission became the basis for the Hospital Readmissions Reduction Program in the Affordable Care Act altering the criteria for hospital payment reimbursement. The Centers for Medicare & Medicaid Services has been charged with enforcement of these criteria by reducing Medicare payments to hospitals that exceed preset all-cause readmission rates.1 For fiscal year 2013, the readmission penalties have been applied to three conditions: acute myocardial infarction, heart failure, and pneumonia. By 2015, the policy is expected to include readmissions for COPD, coronary artery bypass graft surgery, percutaneous coronary interventions, and other vascular procedures.3 In fiscal year 2013, the maximum payment reduction for hospitals with excess readmission rates was 1% but increases to 2% in 2014 and to 3% for 2015 and beyond.4
Interventions aimed at preventing readmissions have not been universally successful.5 One potential explanation for this is the inability to reliably predict which patients are at risk for readmission to target readmission prevention interventions. Predictors of hospital readmission can be disease specific, such as presence of multivessel disease in patients hospitalized with myocardial infarction,6 or more general, such as sex and timeliness of follow-up medical visits post discharge.7, 8, 9, 10 Specific pneumonia pathogens, generally antibiotic-resistant bacteria, have been associated with adverse patient outcomes to include greater lengths of stay and mortality.11, 12, 13 However, pneumonia pathogen characterization has not been evaluated as a potential risk factor for readmission. Therefore, we performed a study to examine the influence of pathogen characterization on the prevalence of 90-day readmission among hospitalized patients with pneumonia.
Materials and Methods
Study Population and Data Collection
The study was conducted at Barnes-Jewish Hospital, a 1,250-bed teaching hospital in St. Louis, Missouri. During a 6-year period (August 2007 to September 2013), patients with a discharge diagnosis of pneumonia were evaluated. The Washington University Human Research Protection Office approved the protocol (HRPO number 201205194). Baseline characteristics were recorded at hospital admission: age, sex, race, BMI, and Charlson comorbidity score.14 Hospital readmission was evaluated at 90 days. For purposes of pathogen characterization, patients were segregated according to the following categories: culture-negative pneumonia, pneumonia attributed to antibiotic-susceptible bacteria, pneumonia attributed to potentially antibiotic-resistant bacteria, and viral pneumonia.
Primary End Point
Readmission for any reason (ie, all-cause readmission) to an acute care facility in the 90 days following discharge served as the primary end point. The index hospital serves as the main teaching institution for BJC Healthcare, a large integrated health-care system of both inpatient and outpatient care. The system includes a total of 12 hospitals in a compact geographic region surrounding and including St. Louis, Missouri, and we included readmission to any of these hospitals in our analysis. People treated within this health-care system are, in nearly all cases, readmitted to one of the system's participating hospitals. If a patient who receives health care in the system presents to a nonsystem hospital, he/she is often transferred back into the integrated system because of issues of insurance coverage. Patients with a 90-day readmission were compared with those without a 90-day readmission. All data were derived from the informatics database provided by the Center for Clinical Excellence, BJC HealthCare.
Definitions
Pneumonia was considered to be present if patients had an International Classification of Diseases, Ninth Edition code indicative of pneumonia. Patients were also required to have the presence of a new or progressive radiographic infiltrate plus at least two of the following: leukocytosis (> 10 × 109 cells/L), leukopenia (≤ 4 × 109 cells/L), fever (> 38.3°C), hypothermia (≤ 36.0°C), purulent secretions from the lower respiratory tract, or Pao 2/Fio 2 < 300. The presence of a new or progressive radiographic infiltrate was based on the interpretation of the chest radiograph by board-certified radiologists blinded to the study. Pneumonia was classified as culture negative if all respiratory cultures failed to identify a pathogen. Culture-positive pneumonia was defined as growth of a pathogenic organism from sputum, tracheal aspirate, or bronchoscopic or blind BAL fluid. Additionally, a positive urinary antigen test for Legionella qualified as a positive culture, as did positive qualitative nucleic acid multiplex tests for respiratory viruses Bordetella pertussis, Chlamydophila pneumonia, and Mycoplasma pneumoniae (FilmArray Respiratory Panel; BioFire Diagnostics). If a patient had more than one episode of pneumonia during the index hospitalization, only the first case was included in the analysis.
Antibiotic-susceptible bacteria were classified as those most commonly associated with community-acquired pneumonia (methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis), whereas potentially antibiotic-resistant bacteria included those most often associated with nosocomial infections (methicillin-resistant S aureus, Pseudomonas aeruginosa, Acinetobacter species). Enterobacteriaceae, such as Klebsiella species, were classified according to their antibiotic susceptibility to ceftriaxone (ie, susceptible to ceftriaxone classified as antibiotic susceptible). Viral pneumonia was deemed present when the initial microbiologic evaluation demonstrated a known respiratory virus. Microbiologic identification of polymicrobial infection with antibiotic-susceptible and potentially antibiotic-resistant bacteria was classified as the latter. Pneumonia was classified as present on admission if radiographic and clinical criteria for pneumonia developed within 48 h of hospital admission. Hospital-acquired pneumonia was defined as the occurrence of pneumonia criteria more than 48 h after admission, and ventilator-associated pneumonia was defined as meeting the pneumonia criteria after the onset of mechanical ventilation.
Statistical Analysis
The number of patients admitted to Barnes-Jewish Hospital having a diagnosis of pneumonia during the study period determined the sample size. The assessment of readmission was performed among hospital survivors. We used a χ2 test or Student t test, as appropriate, for univariate analyses. The Mann-Whitney U test was used for continuous, nonparametrically distributed data. All analyses were two-tailed, and a P value of < .05 was assumed to represent statistical significance. We relied on logistic regression for identifying variables independently associated with 90-day readmission. Based on univariate analysis, variables significant at P < .10 were entered into the model. To arrive at the most parsimonious model, we used a stepwise backward elimination approach. We evaluated colinearity with correlation matrices. We report adjusted ORs and 95% CIs where appropriate. We conducted a cross-validation of the model to assess for overfitting. We reran the logistic model on 90% of the sample, sequentially dropping 10% of the population with each run. We contrasted the mean accuracy of these analyses with the overall accuracy of the model developed with the entire cohort. All analyses were performed with SPSS software, version 19.0 (IBM).
Results
Nine thousand six hundred twenty-four consecutive patients with a discharge diagnosis of pneumonia having respiratory samples submitted to the microbiology laboratory were included in the study. The mean age was 57.8 ± 26.1 years (range, 18-97 years), with 5,648 men (58.7%) and 3,976 women (41.3%) (Table 1 ). Four thousand one hundred seventy-two patients (43.3%) had pneumonia present at hospital admission, 4,400 (45.7%) had hospital-acquired pneumonia, and 1,052 (10.9%) had ventilator-associated pneumonia. Among these patients, 4,432 (46.1%) were classified as having culture-negative pneumonia, 1,940 (20.2%) as having pneumonia attributed to antibiotic-susceptible bacteria, 2,991 (31.1%) as having pneumonia attributed to potentially antibiotic-resistant bacteria, and 261 (2.7%) as having viral pneumonia. Charlson comorbidity scores were statistically greatest for patients who were culture negative and those with viral pneumonia (Table 1). There were 585 patients readmitted to the hospital within 90 days. The most common reasons for readmission included nonpneumonia infections (n = 163, 27.9%), nonpneumonia pulmonary conditions (COPD, asthma, bronchiectasis, cystic fibrosis) (n = 125, 21.4%), pneumonia (n = 62, 10.6%), respiratory failure (n = 45, 7.7%), nonpneumonia organ transplant complications (n = 43, 7.4%), non-congestive heart failure cardiac events (n = 26, 4.4%), GI conditions (n = 24, 4.1%), CNS conditions (n = 20, 3.4%), and congestive heart failure (n = 17, 2.9%).
TABLE 1.
Patient Characteristics
| Characteristic | Culture Negative (n = 4,432) | Antibiotic Susceptible (n = 1,940) | Potentially Antibiotic Resistant (n = 2,991) | Viral (n = 261) |
|---|---|---|---|---|
| Age, y | 58.7 ± 33.5 | 56.0 ± 17.0a | 57.7 ± 17.9b | 57.0 ± 16.9 |
| Male sex | 55.1 | 63.7a | 61.5a | 51.0b,c |
| Black | 30.4 | 28.9 | 24.1a,b | 23.4 |
| BMI, kg/m2 | 27.0 [22.8, 32.4] | 26.6 [22.6, 31.7] | 26.5 [21.6, 32.3] | 26.2 [22.3, 32.0] |
| Length of stay, d | 14.5 ± 16.1 | 17.9 ± 18.8 | 26.5 ± 1.8a,b | 21.1 ± 19.0a,b,c |
| Mechanical ventilation | 21.8 | 31.0a | 32.5a | 40.6a,b,c |
| Charlson comorbidity score | 4.0 [2.0, 6.0] | 3.0 [1.0, 5.0]a | 3.0 [1.0, 6.0]a | 4.0 [2.0, 6.0]b |
| Congestive heart failure | 20.4 | 14.8a | 18.1b | 17.2 |
| Myocardial infarction | 9.7 | 9.4 | 8.7 | 7.3 |
| COPD | 31.2 | 27.2a | 30.7 | 31.4 |
| Diabetes mellitus | 21.3 | 18.4a | 21.3 | 19.5 |
| Chronic kidney disease | 13.9 | 9.0a | 12.7b | 16.5b |
| Underlying malignancy | 10.2 | 9.6 | 9.7 | 7.3 |
| Leukemia | 8.5 | 3.2a | 4.5a | 13.8a,b,c |
| HIV | 2.8 | 1.0a | 0.7a | 1.9 |
| Cirrhosis | 8.8 | 7.7 | 7.5 | 8.4 |
| Pneumonia on admission | 49.8 | 56.7a | 25.7a,b | 36.0a,b,c |
| Hospital-acquired pneumonia | 44.0 | 34.1a | 55.5a,b | 49.0b |
| VAP | 6.2 | 9.2a | 18.8a,b | 14.9a,b |
| 90-d readmissiond | 5.8 | 6.6 | 11.4a,b | 8.3 |
| Hospital mortality | 17.8 | 19.3 | 31.0a,b | 24.9a, b, c |
Values expressed as mean ± SD, median [25th percentile, 75th percentile], or %. VAP = ventilator-associated pneumonia.
P < .05 compared with culture-negative group.
P < .05 compared with antibiotic-susceptible group.
P < .05 compared with potentially antibiotic-resistant group.
90-d readmission assessed only for hospital survivors: culture negative (n = 3,644); antibiotic susceptible (n = 1,566); potentially antibiotic resistant (n = 2,247); viral (n = 180).
Among patients with pneumonia attributed to antibiotic-susceptible bacteria, methicillin-susceptible S aureus was most common, followed by H influenzae, S pneumoniae, Klebsiella pneumoniae, and Escherichia coli (Table 2 ). For pneumonia attributed to potentially antibiotic-resistant bacteria P aeruginosa was most prevalent, followed by methicillin-resistant S aureus, Enterobacter species, Acinetobacter species, and Stenotrophomonas maltophilia. Herpes simplex virus was the most common respiratory virus, followed by cytomegalovirus, influenza A, parainfluenza, and rhinovirus.
TABLE 2.
Pathogens Associated With Pneumonia
| Pathogen | No. | % |
|---|---|---|
| Antibiotic-susceptible bacteria (n = 1,940) | ||
| Methicillin-susceptible Staphylococcus aureus | 505 | 26.0 |
| Haemophilus influenzae | 324 | 16.7 |
| Streptococcus pneumoniae | 222 | 11.4 |
| Other Streptococci species | 475 | 24.5 |
| Klebsiella pneumoniae | 184 | 9.5 |
| Escherichia coli | 177 | 9.1 |
| Haemophilus parainfluenzae | 100 | 5.2 |
| Moraxella catarrhalis | 86 | 4.4 |
| Klebsiella oxytoca | 66 | 3.4 |
| Other Haemophilus species | 24 | 1.2 |
| Legionella species | 9 | 0.5 |
| Bordetella bronchiseptica | 6 | 0.3 |
| Neisseria species | 5 | 0.3 |
| Other Klebsiella species | 3 | 0.2 |
| Eikenella corrodens | 2 | 0.1 |
| Other Moraxella species | 2 | 0.1 |
| Pasteurella multocida | 1 | 0.1 |
| Potentially antibiotic-resistant bacteria (n = 2,991) | ||
| Pseudomonas aeruginosa | 1,176 | 39.3 |
| Methicillin-resistant Staphylococcus aureus | 1,016 | 34.0 |
| Enterobacter species | 304 | 10.2 |
| Acinetobacter species | 219 | 7.3 |
| Stenotrophomonas maltophilia | 208 | 7.0 |
| Serratia species | 142 | 4.7 |
| Proteus species | 78 | 2.6 |
| Citrobacter species | 64 | 2.1 |
| Achromobacter species | 62 | 2.1 |
| Extended-spectrum β-lactamase producing Enterobacteriaceae | 47 | 1.6 |
| Burkholderia cepacia | 35 | 1.2 |
| Nocardia species | 25 | 0.8 |
| Other gram-negative bacteria | 24 | 0.8 |
| Providencia species | 12 | 0.4 |
| Hafnia alvei | 8 | 0.3 |
| Carbapenemase-producing Klebsiella species | 6 | 0.2 |
| Morganella morganii | 5 | 0.2 |
| Respiratory viruses (n = 261) | ||
| Herpes simplex virus | 82 | 31.4 |
| Cytomegalovirus | 65 | 24.9 |
| Influenza A | 49 | 18.8 |
| Parainfluenza | 40 | 15.3 |
| Rhinovirus | 34 | 13.0 |
| Respiratory syncytial virus | 21 | 8.0 |
| Adenovirus | 20 | 7.7 |
| Human metapneumovirus | 11 | 4.2 |
| Influenza B | 8 | 3.1 |
| Coronavirus | 2 | 0.8 |
More than one listed pathogen could be present within each category.
The prevalence of 90-day hospital readmission among hospital survivors (n = 7,637, 79.4%) was greatest for patients with pneumonia attributed to potentially antibiotic-resistant bacteria (11.4%), followed by a viral cause (8.3%), pneumonia attributed to antibiotic-susceptible bacteria (6.6%), and culture-negative pneumonia (5.8%) (P < .001) (Fig 1 ). Similar distributions were identified for 30-day and 180-day readmission rates (30 day: 6.7%, 4.4%, 4.3%, 3.2%; P < .001; and 180 day: 14.6%, 9.4%, 8.6%, 7.6%; P < .001). Patients with a 90-day readmission had a lower BMI, were less likely to receive mechanical ventilation, had greater Charlson comorbidity scores, and were statistically more likely to have congestive heart failure, myocardial infarction, COPD, diabetes mellitus, chronic kidney disease, leukemia, and cirrhosis compared with patients without a 90-day readmission (Table 3 ). Pneumonia on admission and pneumonia attributed to potentially antibiotic-resistant bacteria were significantly more likely, whereas hospital-acquired pneumonia and culture-negative pneumonia were less likely, to be present in patients with a 90-day readmission.
Figure 1.
Bar graph depicting the prevalence of 90-d readmission for hospital survivors with culture-negative pneumonia, pneumonia attributed to antibiotic-susceptible bacteria, pneumonia attributed to potentially antibiotic-resistant bacteria, and viral pneumonia. P < .001 for the trend among groups.
TABLE 3.
Characteristics According to 90-Day Readmission Status
| Characteristic | 90-d Readmission (n = 585) | No 90-d Readmission (n = 7,052) | P Value |
|---|---|---|---|
| Age, y | 55.0 ± 17.8 | 56.8 ± 28.7 | .204 |
| Male sex | 57.3 | 58.3 | .627 |
| Black | 28.7 | 28.4 | .281 |
| BMI, kg/m2 | 24.7 [20.5, 30.1] | 26.3 [22.0, 31.6] | < .001 |
| Length of stay, d | 19.0 ± 29.3 | 23.0 ± 26.2 | < .001 |
| Mechanical ventilation | 20.9 | 24.6 | .044 |
| Charlson comorbidity score | 5.0 [3.0, 7.0] | 3.0 [1.0, 6.0] | < .001 |
| Congestive heart failure | 30.4 | 17.2 | < .001 |
| Myocardial infarction | 13.2 | 9.0 | .003 |
| COPD | 58.3 | 30.3 | < .001 |
| Diabetes mellitus | 38.6 | 19.9 | < .001 |
| Chronic kidney disease | 22.1 | 11.7 | < .001 |
| Underlying malignancy | 11.5 | 10.1 | .433 |
| Leukemia | 9.2 | 5.4 | < .001 |
| HIV | 2.9 | 1.8 | .063 |
| Cirrhosis | 13.8 | 8.0 | < .001 |
| Pneumonia on admission | 51.8 | 45.3 | .002 |
| Hospital-acquired pneumonia | 40.5 | 45.5 | .021 |
| VAP | 7.7 | 9.3 | .202 |
| Antibiotic-susceptible bacteria | 17.6 | 20.7 | .071 |
| Potentially antibiotic-resistant bacteria | 43.8 | 28.2 | < .001 |
| Viral pathogen | 2.6 | 2.3 | .731 |
| Culture-negative pneumonia | 36.1 | 48.7 | < .001 |
Values expressed as mean ± SD, median [25th percentile, 75th percentile], or %. 90-d readmission status among the hospital survivor cohort (n = 7,637). See Table 1 legend for expansion of abbreviation.
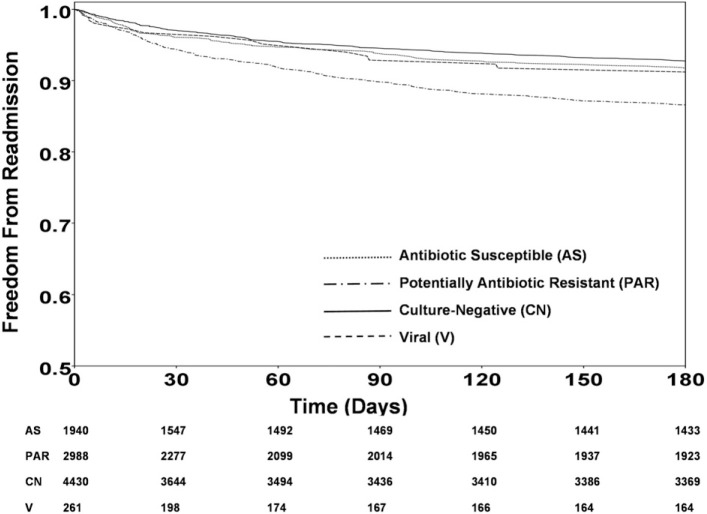
Kaplan-Meier analysis censoring for mortality demonstrated that 90-day readmission was statistically most common among patients with pneumonia attributed to potentially antibiotic-resistant bacteria (Fig 2 ). Multiple logistic regression analysis identified pneumonia attributed to potentially antibiotic-resistant bacteria to be independently associated with 90-day readmission (OR, 1.75; 95% CI, 1.56-1.97; P < .001). Other independent predictors of 90-day readmission were Charlson comorbidity score > 4, cirrhosis, and chronic kidney disease, whereas culture-negative pneumonia was associated with a lower risk of 90-day readmission (Table 4 ). The adjusted ORs for the variables that were significant predictors in the model in all of the 10 sequential reruns (with 90% of the cohort) did not differ from the findings in the complete population.
Figure 2.
Kaplan-Meier curves for 90-d readmission with censoring of hospital nonsurvivors. Log-rank test: P < .001 comparing potentially antibiotic-resistant pneumonia to culture-negative pneumonia and comparing potentially antibiotic-resistant pneumonia to antibiotic-susceptible pneumonia; P = .004 comparing potentially antibiotic-resistant pneumonia to viral pneumonia; P > .05 for all other combinations of pairings.
TABLE 4.
Variables Independently Associated With 90-Day Readmission
| Variables | OR | 95% CI | P Value |
|---|---|---|---|
| Charlson comorbidity score > 4 | 2.48 | 2.25-2.74 | < .001 |
| Potentially antibiotic-resistant pathogen | 1.75 | 1.56-1.97 | < .001 |
| Cirrhosis | 1.32 | 1.15-1.50 | .038 |
| Chronic kidney disease | 1.35 | 1.21-1.52 | .008 |
| Culture-negative pneumonia | 0.75 | 0.66-0.84 | .016 |
Hosmer-Lemeshow goodness-of-fit test, P = .838.
The analysis was repeated for the subgroup of patients with pneumonia on admission, encompassing both community-acquired pneumonia and health-care-associated pneumonia. Similar to the entire cohort, the prevalence of 90-day hospital readmission among hospital survivors (n = 3,495) was greatest for patients with pneumonia attributed to potentially antibiotic-resistant bacteria (18.7%), followed by pneumonia attributed to antibiotic-susceptible bacteria (7.5%), viral pneumonia (6.6%), and culture-negative pneumonia (6.0%). Multiple logistic regression analysis identified pneumonia attributed to potentially antibiotic-resistant bacteria to be independently associated with 90-day readmission in this subset (OR, 2.90; 95% CI, 2.46-3.40; P < .001) (Hosmer-Lemeshow goodness-of-fit = 0.871). Charlson comorbidity score > 4 was also associated with 90-day readmission (OR, 1.99; 95% CI, 1.73-2.28; P < .001). Culture-negative pneumonia did not reach statistical significance in the logistic regression analysis (OR, 0.75; 95% CI, 0.64-0.88; P = .066). The adjusted ORs for pneumonia attributed to potentially antibiotic-resistant bacteria and Charlson comorbidity score > 4 were significant predictors in the model in all of the 10 sequential reruns (with 90% of the cohort) and did not differ from the findings in the complete population of patients with pneumonia on admission.
Discussion
We demonstrated that hospital readmission following hospitalization for pneumonia was associated with pneumonia pathogen characterization, with pneumonia attributed to antibiotic-resistant bacteria having the highest rate of readmission. Moreover, our multivariate analysis demonstrated that pneumonia attributed to potentially antibiotic-resistant bacteria was an independent predictor of 90-day readmission, whereas culture-negative pneumonia was associated with a lower risk of 90-day readmission. Pneumonia attributed to potentially antibiotic-resistant bacteria was also found to have the longest hospital length of stay and greatest hospital mortality. For the subgroup of patients having pneumonia on admission, encompassing community-acquired pneumonia and health-care-associated pneumonia, the association between 90-day readmission and pneumonia attributed to potentially antibiotic-resistant bacteria was quantitatively greater than for the entire cohort.
Predicting which patients with pneumonia will require readmission is problematic. Dharmarajan et al15 showed that readmissions following congestive heart failure, acute myocardial infarction, and pneumonia hospitalization were diverse and usually for a different reason than the original hospitalization problem. A Department of Veterans Affairs study identified predictors of readmission following a pneumonia hospitalization including increasing age, single marital status, increasing number of ED clinic visits in the previous year, hospital admission within the previous 90 days, increasing number of nonpharmacy clinic visits in the prior year, and shorter hospital length of stay.16 Interestingly, these risk factors were largely unrelated to the underlying pneumonia, supporting the findings of Dharmarajan et al.15 However, Cabré et al17 showed that oropharyngeal dysphagia in the elderly was an important risk factor for readmission following hospitalization for pneumonia, presumably by promoting recurrent aspiration.
It is biologically plausible that pneumonia pathogen characterization could influence readmission and other outcomes by impacting the effectiveness of antibiotic therapy in some patients, especially because of the presence of antibiotic resistance, as well as by identifying a population with greater disease severity and comorbidities. Previous pneumonia studies have shown that inappropriate initial antibiotic therapy due to infection with antibiotic-resistant bacteria is associated with increased risk of mortality.18 Micek et al19 recently demonstrated that inappropriate initial therapy for community-acquired pneumonia in the ED setting was associated with a significantly greater risk of hospital readmission. Multivariate analysis using hospital readmission as the dependent outcome identified antibiotic exposure in the previous 30 days, presence of peripheral vascular disease, and increasing CURB-65 (confusion, blood urea nitrogen > 7 mmol/L, respiratory rate > 30/min, BP < 90 mm Hg, systolic or diastolic BP ≤ 60 mm Hg, ≥ age 65 years) scores as predictors for readmission. Like the Department of Veterans Affairs study,16 pneumonia-related variables did not predict readmission. However, Micek et al19 also found that antibiotic exposure in the previous 30 days was independently associated with inappropriate antibiotic therapy, thus providing a link between inappropriate therapy and hospital readmission. However, it is likely that for most patients, infection with antibiotic-resistant bacteria is a marker for greater underlying disease severity and comorbidities, further supporting a plausible link between pathogen type and readmission risk.13, 20, 21
Understanding the risk factors for hospital readmission in patients with pneumonia could provide insights into whether such readmissions are preventable as well as how to best tailor strategies to prevent readmissions. Moreover, such data could more objectively identify hospitals caring for patients at higher risk for readmission because of case mix, potentially mitigating financial penalties for readmission in those patients. The latter is supported by a study by Shorr et al,22 who found that patients with health-care-associated pneumonia were more than seven times as likely to be readmitted to the hospital compared with patients with community-acquired pneumonia. These investigators showed that admission from long-term care, underlying immunosuppression, prior antibiotic exposure, and prior hospitalization within the preceding 90 days were predictors for readmission. None of these risk factors would be amenable to direct intervention by the treating clinicians to reduce the likelihood of readmission. These investigators were also unable to establish a relationship between appropriateness of antibiotic therapy and being rehospitalized, thus illustrating that care delivery may have only a limited causal role in driving rehospitalization. The absence of a nexus between initial antibiotic therapy for the index pneumonia and readmission underscores that nonmodifiable patient or pathogen characteristics are likely key determinants of whether a subject with pneumonia is eventually readmitted. Our data would support this hypothesis by identifying pneumonia pathogen characterization as an important risk factor for readmission.
Our study has several important limitations. First, this was a retrospective analysis. It is possible that we did not identify all patient variables and processes of care that are important determinants of 90-day readmission in this population. Moreover, the retrospective nature of this investigation did not allow an assessment of specific treatment considerations such as the response to antibiotic therapy and pneumonia recurrence, and limited our ability to identify readmissions to nonsystem hospitals. Second, we focused on pathogen type as a determinant of readmission and not the appropriateness of antibiotic therapy. This was purposefully done, given the established strong association between antibiotic-resistant bacteria and host-specific risk factors (eg, prior antibiotics, recent hospitalization), as well as with the administration of inappropriate antimicrobial therapy.11, 12, 13, 18, 19 Pathogen type seems to be a simple marker encompassing these risks, to include the administration of inappropriate therapy, and is in line with the Centers for Medicare & Medicaid Services goal to discover more easily identifiable objective measures to assess patient risks and quality of care.23 Third, we simply categorized pathogens into broad categories without determining whether certain pathogens, or pathogen subtypes, were more likely to be associated with 90-day readmission.
Another limitation of our study is that we did not have access to outpatient visits following the index hospitalization to assess the influence of follow-up care on readmission rates. Several studies have identified early posthospital follow-up visits as important means of preventing readmissions.9, 10 Additionally, even though all patients had respiratory cultures obtained, it is possible that some of these cultures may represent inadequate specimens. Moreover, a proportion of the culture-negative samples may have been due to inadequate specimen collection. This could have underestimated the number of patients with antibiotic-resistant pathogens in our study, potentially influencing our results. Finally, the patient population at Barnes-Jewish Hospital may not be representative of that at other centers. This is supported by the high percentage of S aureus infection we observed, likely due to the high prevalence of health-care-associated risk factors in the population.21 However, a strength of our study is that we did not limit inclusion to patients with a specific type of pneumonia but included all types, except for those due to opportunistic pathogens.
In conclusion, our data suggest that readmission following hospitalization for pneumonia is relatively common and is related to pneumonia pathogen characterization. Pneumonia attributed to potentially antibiotic-resistant bacteria is associated with an increased risk for 90-day readmission, whereas culture-negative pneumonia is associated with a lower risk for 90-day readmission.
Acknowledgments
Author contributions: M. H. K. is the guarantor of the content of the manuscript, including the data and analysis. A. A., S. T. M., Y. S., and M. H. K. contributed to concept and design; A. A., S. T. M., N. H., B. C., and S. M. contributed to acquisition of data; A. A., S. T. M., Y. S., and M. H. K. contributed to analysis and interpretation of data; and A. A., S. T. M., Y. S., N. H., B. C., S. M., and M. H. K. contributed to drafting the submitted article or revising it critically for important intellectual content, have provided final approval of the version to be published, and have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial/nonfinancial disclosures: The authors have reported to the following conflicts of interest: Dr Kollef's effort was supported by the Barnes-Jewish Hospital Foundation. Drs Andruska, Micek, Shindo, and Hampton; Mr Colona; and Ms McCormick have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Footnotes
FUNDING/SUPPORT: The authors have reported to that no funding was received for this study.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Marks E. Complexity science and the readmission dilemma. JAMA Intern Med. 2013;173(8):629–631. doi: 10.1001/jamainternmed.2013.4065. [DOI] [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission Refining the hospital readmissions reduction program. http://www.medpac.gov/documents/reports/jun13_ch04.pdf?sfvrsn=0 Accessed June 27, 2014.
- 3.Fontanarosa PB, McNutt RA. Revisiting hospital readmissions. JAMA. 2013;309:398–400. doi: 10.1001/jama.2013.42. [DOI] [PubMed] [Google Scholar]
- 4.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–1795. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 5.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 6.Kociol RD, Lopes RD, Clare R. International variation in and factors associated with hospital readmission after myocardial infarction. JAMA. 2012;307(1):66–74. doi: 10.1001/jama.2011.1926. [DOI] [PubMed] [Google Scholar]
- 7.Sharif R, Parekh TM, Pierson KS, Kuo YF, Sharma G. Predictors of early readmission among patients 40 to 64 years of age hospitalized for chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(5):685–694. doi: 10.1513/AnnalsATS.201310-358OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taha M, Pal A, Mahnken JD, Rigler SK. Derivation and validation of a formula to estimate risk for 30-day readmission in medical patients. Int J Qual Health Care. 2014;26(3):271–277. doi: 10.1093/intqhc/mzu038. [DOI] [PubMed] [Google Scholar]
- 9.Kangovi S, Mitra N, Grande D. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. 2014;174:535–543. doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 10.Hochhalter AK, Basu R, Prasla K, Jo C. Retrospective cohort study of medication adherence and risk for 30-day hospital readmission in a Medicare Cost Plan. Manag Care. 2014;23(1):43–47. [PubMed] [Google Scholar]
- 11.Vidaur L, Planas K, Sierra R. Ventilator-associated pneumonia: impact of organisms on clinical resolution and medical resources utilization. Chest. 2008;133(3):625–632. doi: 10.1378/chest.07-2020. [DOI] [PubMed] [Google Scholar]
- 12.Kollef MH, Chastre J, Clavel M. A randomized trial of 7-day doripenem versus 10-day imipenem-cilastatin for ventilator-associated pneumonia. Crit Care. 2012;16(6):R218. doi: 10.1186/cc11862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Sax FL, MacKenzie CR, Fields SD, Braham RL, Douglas RG., Jr Assessing illness severity: does clinical judgment work? J Chronic Dis. 1986;39(6):439–452. doi: 10.1016/0021-9681(86)90111-6. [DOI] [PubMed] [Google Scholar]
- 15.Dharmarajan K, Hsieh AF, Lin Z. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang VL, Halm EA, Fine MJ, Johnson CS, Anzueto A, Mortensen EM. Predictors of rehospitalization after admission for pneumonia in the veterans affairs healthcare system. J Hosp Med. 2014;9(6):379–383. doi: 10.1002/jhm.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cabré M, Serra-Prat M, Force L, Almirall J, Palomera E, Clavé P. Oropharyngeal dysphagia is a risk factor for readmission for pneumonia in the very elderly persons: observational prospective study. J Gerontol A Biol Sci Med Sci. 2014;69(3):330–337. doi: 10.1093/gerona/glt099. [DOI] [PubMed] [Google Scholar]
- 18.Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH. Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest. 2002;122(1):262–268. doi: 10.1378/chest.122.1.262. [DOI] [PubMed] [Google Scholar]
- 19.Micek ST, Lang A, Fuller BM, Hampton NB, Kollef MH. Clinical implications for patients treated inappropriately for community-acquired pneumonia in the emergency department. BMC Infect Dis. 2014;14:61. doi: 10.1186/1471-2334-14-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(6):3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 21.Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568–3573. doi: 10.1128/AAC.00851-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shorr AF, Zilberberg MD, Reichley R. Readmission following hospitalization for pneumonia: the impact of pneumonia type and its implication for hospitals. Clin Infect Dis. 2013;57(3):362–367. doi: 10.1093/cid/cit254. [DOI] [PubMed] [Google Scholar]
- 23.Magill SS, Klompas M, Balk R. Developing a new, national approach to surveillance for ventilator-associated events. Crit Care Med. 2013;41(11):2467–2475. doi: 10.1097/CCM.0b013e3182a262db. [DOI] [PMC free article] [PubMed] [Google Scholar]