Abstract
Global warming is believed to induce a gradual climate change. Hence, it was predicted that tropical insects might expand their habitats thereby transmitting pathogens to humans. Although this concept is a conclusive presumption, clear evidence is still lacking—at least for viral diseases. Epidemiological data indicate that seasonality of many diseases is further influenced by strong single weather events, interannual climate phenomena, and anthropogenic factors. So far, emergence of new diseases was unlinked to global warming. Re-emergence and dispersion of diseases was correlated with translocation of pathogen-infected vectors or hosts. Coupled ocean/atmosphere circulations and ‘global change’ that also includes shifting of demographic, social, and economical conditions are important drivers of viral disease variability whereas global warming at best contributes.
Introduction
Transmission of infectious diseases exhibits spatial and temporal variations of incidence that reflects seasons, interannual weather fluctuations, strong single weather events, and other natural disasters [1•, 2]. →Climate,1 the average weather of a region, is primarily driven by seasonal variables such as temperature, precipitation, and winds. In interannual time scales, there is superimposing variability due to a number of coupled ocean/atmosphere systems. Best studied of which is the →El Niño/Southern Oscillation (ENSO), but roughly a dozen circulation indices also contribute ([3•] and literature cited therein). Climate of the Northern Hemisphere is further driven by the →Atlantic Multidecadal Oscillation (AMO) and the →Pacific Decadal Oscillation (PDO) that are quasiperiodic long-term fluctuations (up to 50–80 years) in the strength of thermohaline circulation [3•]. A fourth factor gained growing importance in recent years: the increase of the global temperature, apparently an unidirectional trend that is supposed to induce a gradual but significant →climate change. It is assumed that global warming is forced by the anthropogenic release of ‘greenhouse gases’ [4•]. A consistent assumption was to predict increased exposure of humans to tropical pathogens and their vectors. In 1991, Robert Shope presented the hypothesis that global climate change might result in a worldwide increase of zoonotic infectious diseases [5•], and others forwarded this intriguing idea (inter alia [6•]). Meanwhile, the rising incidences of many human diseases and the emergence/re-emergence of more than a dozen infectious diseases were perceived and Shope's hypothesis attracted attention of numerous scientists. In addition, the impact of global warming on infectious diseases was also considered in the Assessment Reports of the →Intergovernmental Panel on Climate Change, IPCC [7•]. Vector-borne infectious diseases, for example malaria, yellow fever, dengue, and some viral encephalitides as well as non-vector-borne diseases, such as salmonellosis, cholera, and giardiasis, were predicted to increase, whereas LaCrosse encephalitis and Lyme borreliosis were expected to decline [5•, 7•]. However, there is dissent about this hypothesis [8, 9, 10, 11, 12, 13, 14]. Despite the great attention, only few research articles provide reliable data on the interconnection of global warming and the epidemiology of infectious diseases. It is our aim to confine this review to viral diseases and to describe some of those mechanisms that have lead to an increase of virus activity in recent years.
Box 1. Glossary.
Atlantic Multidecadal Oscillation, AMO: a quasiperiodic long-term fluctuation up to 50–80 years in the strength of thermohaline circulation that results in variability of sea surface temperatures in the range of 0.4 °C. Its warm phases extended from 1860 to 1880 and 1930 to 1960, cold phases were recorded 1905–1925 and 1970–1990. In 1995, the AMO index turned positive again, indicating another warm phase.
Climate: average weather of a region; statistical description of mean and variability of surface variables (temperature, precipitation, wind) over a period of typically 30 years (as pinpointed by the World Meteorological Organization).
Climate Change: changes in the mean and variability of climate variables that persist for comparable time periods (decades or longer). This definition includes both natural processes and anthropogenic changes.
El Niño/Southern Oscillation, ENSO: a coupled ocean-atmosphere phenomenon that drives a complex global system of meteorological pertubations. Its periodically warm event, El Niño, is characterized by a warm-water current along the western coast of equatorial South America. The trade winds normally blowing westwards show a weakening or reversal. This leads to an altering of ocean currents. The characteristic equatorial ‘cold tongue’ of upwelling cool water fails to develop and sea surface temperatures increase by four to five degrees at the equatorial eastern Pacific. As a consequence fluctuations of the Walker Circulation as well as changes in regional temperatures and precipitation patterns occur. El Niño is associated with high atmospheric pressure over Indonesia and low pressure over the southeastern Pacific (as measured by the Southern Oscillation index). Numerous teleconnections occur in far distant regions. The cold phase of the ENSO with reversed effects is called a La Niña event.
Indian Ocean dipole, IOD: also known as Indian Ocean Zonal Mode [35, 36]; two modes of a zonal gradient of tropical SSTs during the boreal autumn. The positive mode is triggered by anomalous alongshore winds off Sumatra and the East African coast in summer that induce enhanced upwelling of cold water at Sumatra. In autumn, below-normal SSTs in Sumatra in the east and above-normal SSTs in Somalia in the west are accompanied with unusual easterly surface winds along the equator. Convectional rainfalls in autumn and winter due to moist air from the Indian Ocean ascending over the heated land mass of East Africa accompany the positive mode. The warming period ends or diminishes in a number of ways and results with the locus of convection moving back towards Indonesia and the equatorial wind pattern reverting its direction. The consequences are warm SSTs in the eastern Indian Ocean and cold SSTs in the western Indian Ocean (negative mode). Whether the IOD is linked to other coupled ocean-atmosphere phenomena (ENSO-monsoon system, North Pacific interdecadal variability) is still unclear [3•].
Intergovernmental Panel on Climate Change, IPCC: established in 1988 by the World Meteorological Organization and the United Nations Environment Programme in order to assess scientific information related to climate change and to evaluate the environmental and socioeconomic consequences. Moreover, the IPCC was mandated to formulate realistic response strategies. So far, the IPCC produced four Assessment Reports (1990, 1995, 2001 and 2007), Special Reports, Technical Papers and Methodology Reports. The 4th Assessment Report (AR4) involved more than 500 Lead Authors and 2000 Expert Reviewers. The IPCC has been awarded the 2007 Nobel Peace Prize.
Pacific Decadal Oscillation, PDO: index of sea surface temperature fluctuations over the North Pacific north of 20° used to measure the Pacific decadal variability, a coupled ocean-atmosphere phenomenon with decadal-to-interdecadal fluctuations of sea surface temperatures, salinities, and atmospheric circulation throughout the whole Pacific Ocean. The ENSO cycle is modulated by the Pacific decadal variability.
Quasi-Biennial Oscillation, QBO: large-scale climate fluctuation describing periodic variation in the direction, either westerly or easterly, of tropical lower stratospheric winds. The mean QBO cycle is 28 months but there is considerable variability of the period ranging from 20 to 36 months and the amplitude (maximum amplitude of 40–50 m/s is seen at 20 mb). The QBO has been linked to Southern Oscillation, Indian monsoons and precipitations in South Africa and Australia.
Sea surface temperature, SST: temperature of the top few meters of the ocean (subsurface bulk) as measured by ships and buoys. Satellite measurements of the uppermost layer have to be corrected for compatibility with the bulk temperature.
Climate-forced diseases: which diseases are anticipated to increase in a warmer world and where?
The IPCC has elaborated a plethora of adverse effects of climate change to stress its impact on human health [7•]. This raises the question which of those effects will evoke serious problems and where? Following R. Shope's reasoning, ‘three-factor and four-factor complexes’ (i.e. arthropod-borne diseases and arthropod-borne zoonoses) are most likely to increase in the temperate countries [5•]. He also anticipated the emergence of new diseases, like Lyme disease [5•]. Seventeen years later, it can be stated that indeed most of the new viral diseases are zoonotics—but none of them is arthropod-borne and none of them emerged due to climate change (Table 1 )! However, quite a few re-emerging diseases are arthropod-borne and translocation of some pathogens lead to the dispersal of arthropod-borne diseases in remote areas. Those deserve a closer look (Table 2 ). In general, important factors that trigger the emergence/re-emergence of infectious diseases include population growth, migration, urbanization, international trade, poor socioeconomic conditions, famine, war, loss of biodiversity, deforestation, and land use change. Directly or indirectly, these factors either increase exposure of humans to pathogens or pose the societal problem to assure high levels of hygiene. Hence, several important viruses emerged independently of climate change, for example SARS virus, Nipah virus, Hendra virus, and the highly pathogenic avian influenza H5N1 virus. In modification of Shope's argumentation, one may conclude that mainly vector-borne, rodent-borne or water-borne diseases are due to the dependence on climate change because arthropod vectors, rodent hosts and water-transmitted pathogens are highly susceptible to weather variables.
Table 1.
Emerging and re-emerging human viruses (1975–2007).
| Year | Virus | Comment |
|---|---|---|
| 1975 | Parvovirus B19 (Parvoviridae) | Emerging |
| 1976 | Ebola virus (Filoviridae) | New, emerging, zoonotic, host: fruit bats |
| 1977 | Hantaan virus (Bunyaviridae) | Emerging, zoonotic, rodent-borne |
| 1980 | Human T-lymphotropic virus 1 (Retroviridae) | New, emerging, zoonotic primary infection |
| 1981 | Human immunodeficiency virus 1 (Retroviridae) | New, emerging, zoonotic primary infection |
| 1982 | Human T-lymphotropic virus 2 (Retroviridae) | New, emerging, zoonotic primary infection |
| Ockelbo virus (Togaviridae) | Emerging, zoonotic, vector-borne | |
| 1984 | Torovirus (Coronaviridae) | Emerging |
| Puumalavirus (Bunyaviridae) | Emerging, zoonotic, rodent-borne | |
| 1986 | Human immunodeficiency virus 2 (Retroviridae) | New, emerging, zoonotic primary infection |
| Human herpesvirus 6 (Herpesviridae) | Emerging | |
| European lyssavirus 2 (Rhabdoviridae) | New, emerging, host: bats | |
| Australian bat lyssavirus (Rhabdoviridae) | New, emerging, host: bats | |
| 1989 | Hepatitis C virus (Flaviviridae) | Emerging |
| 1990 | Human herpesvirus 7 (Herpesviridae) | Emerging |
| 1991 | Guanarito virus (Arenaviridae) | New, emerging, zoonotic, rodent-borne |
| 1993 | Sin Nombre virus (Bunyaviridae) | New, emerging, zoonotic, rodent-borne |
| 1994 | Sabia virus (Arenaviridae) | New, emerging, zoonotic, host: fruit bats |
| Hendra virus (Paramyxoviridae) | New, emerging, zoonotic, host: fruit bats | |
| Human herpesvirus 8 (Herpesviridae) | Emerging, Kaposi sarcoma associated | |
| 1995 | Alkhumra virus (Flaviviridae) | Emerging in Saudi Arabia, variant of Kyasanur Forest virus, zoonotic, arthropod-borne |
| 1996 | O’nyong nyong virus (Togaviridae) | Re-emerging in Uganda, zoonotic, arthropod-borne |
| 1997 | H5N1 influenza A virus (Orthomyxoviridae) | Emerging, zoonotic, host: birds |
| 1998 | Nipah virus (Paramyxoviridae) | New, emerging, zoonotic, host: fruit bats |
| 1999 | West Nile virus (Flaviviridae) | Emerging in America, zoonotic, host: birds, arthropod-borne |
| Aichi virus (Picornaviridae) | Emerging | |
| 2001 | Human metapneumovirus (Paramyxoviridae) | New, emerging |
| 2002 | Chikungunya virus (Togaviridae) | Re-emerging in riparian states of Indian Ocean, arthropod-borne |
| 2003 | SARS coronavirus (Coronaviridae) | New, emerging, zoonotic primary infection |
| O’nyong nyong virus (Togaviridae) | Emerging in West Africa, zoonotic, arthropod-borne | |
| 2007 | WU, KI-Polyomaviruses (Polyomaviridae) | Emerging |
Table 2.
Viruses considered to be to sensitive to climate change.
| Pathogen | Disease | Region | Characteristics | References |
|---|---|---|---|---|
| Dengue virus (Flaviviridae) | Dengue fever, dengue hemorhagic fever, dengue shock syndrome | America | - re-emerging | [14] |
| - arthropod-borne | ||||
| - urban cycle: transmitted by canopy-dwelling mosquitos | ||||
| - dispersal of disease by incidental translocation of a pathogen-infected vector or host | ||||
| - upsurge after cessation of mosquito control measures | ||||
| Thailand | - endemic | [38••] | ||
| - disease incidence determined by ecological and immunological factors, but not ENSO | ||||
| Pacific Islands | - ENSO-associated precipitations (?) | [39, 40] | ||
| Yellow fever virus (Flaviviridae) | Yellow fever | Africa | - arthropod-borne | [41] |
| - jungle, intermediate cycles: more frequent contact of humans to vector due to deforestation, hunting, land use change | ||||
| - urban cycle: transmitted by canopy-dwelling mosquitos | ||||
| South America | - jungle cycle: contact of humans to vector due to deforestation, hunting, land use change | [41] | ||
| Murray Valley virus (Flaviviridae) | Murray Valley encephalitis | Australia | - arthropod-borne | [42, 43] |
| - La Niña-associated precipitations | ||||
| Alkhumra virus (Flaviviridae) | Encephalitis, hepatitis, hemorhage | Saudi Arabia | - emerging in Saudi Arabia | [21] |
| - variant of Kyasanur Forest virus (prevalent in India) | ||||
| - arthropod-borne | ||||
| - dispersal of disease by inadvertant translocation of a pathogen-infected host: importation of infected animals | ||||
| West Nile virus (Flaviviridae) | West Nile fever, encephalitis | USA | - emerging | [19] |
| - arthropod-borne | ||||
| - dispersal of disease by inadvertant translocation of a pathogen-infected host: importation of infected birds | ||||
| Romania, Volgograd region | - emerging | [19] | ||
| - dispersal of disease by inadvertant translocation of a pathogen-infected host: migratory birds | ||||
| Usutu virus (Flaviviridae) | Usutu encephalitis of birds | Austria, Hungary | - emerging | [20] |
| - arthropod-borne | ||||
| - dispersal of disease by inadvertant translocation of a pathogen-infected host: migratory birds | ||||
| TBE virus (Flaviviridae) | Tick-borne encephalitis | Sweden | - dispersal of disease by spread of pathogen-infected hosts and vectors: spread of roe deer | [12, 44] |
| - spread of ticks favored by elevated temp. (?) | ||||
| Latvia, Lithuania | - socioeconomic changes after 1990 | [25•, 26] | ||
| Chikungunya virus (Togaviridae) | Chikungunya fever | Riparian states of the Indian Ocean, Italy | - re-emerging | [16•, 17, 18•] |
| - arthropod-borne | ||||
| - dispersal of disease by inadvertant translocation of a pathogen-infected vector or host: translocation of Ae. albopictus, | ||||
| - mutation of virus improves vector competence | ||||
| Ross River virus (Togaviridae) | Ross River encephalitis | Queensland | - endemic | [45] |
| - arthropod-borne | ||||
| - disease incidence correlates with Quasi-Biennial Oscillation-associated precipitations (westerly phase) | ||||
| Ockelbo virus (Togaviridae) | Arthralgia, fever | Sweden, Finland | - arthropod-borne | [23] |
| - variant of Sindbis virus (prevalent in Egypt and Sudan) | ||||
| - dispersal of virus by migratory birds | ||||
| Bluetongue virus (Reoviridae) | Bluetongue disease | Northern Africa | - arthropod-borne | [27, 28] |
| - dispersal of disease by spread of pathogen-infected hosts and vectors: animal transportation, wind-borne spread of midges | ||||
| - elevated temperatures allow northward spread of midges | ||||
| Italy, Balearics, Greek Islands | - re-emerging | [27, 28] | ||
| - dispersal of disease by incidental translocation of a pathogen-infected vector or host: air-borne via Tunisia/Algeria and Turkey | ||||
| - elevated temperature allow northward spread of midges | ||||
| Central Europe | - emerging | [29•] | ||
| - incidental translocation of pathogen-infected host | ||||
| - use of indigenous vectors, vector competence facilitated by elevated temperatures (?) | ||||
| Northern, Eastern Australia | - disease incidence correlates with ENSO-associated precipitations | [46] | ||
| African horse sickness virus (Reoviridae) | Horse sickness | South Africa | - arthropod-borne | [37] |
| - epizootics after ENSO-associated rainfalls followed by drought | ||||
| Rift Valley fever virus (Bunyaviridae) | Rift Valley fever | East Africa | - arthropod-borne | [47] |
| - heavy Indian Ocean Dipole-associated precipitations (1961, 1997), interepizootic perpetuation is maintained by transovarial infection of Ae. lineatopennis | ||||
| Egypt | - dispersal of disease by spread of pathogen-infected hosts: importation of infected animals | [48] | ||
| Saudi Arabia, Yemen | - emerging | [22] | ||
| - dispersal of disease by spread of pathogen-infected hosts: importation of infected animals | ||||
| Sin Nombre virus (Bunyaviridae) | Hantavirus pulmonary syndrome | Four Corners region, USA | - emerging | [34] |
| - rodent-borne | ||||
| - disease incidence correlates with ENSO-associated precipitations | ||||
| Toscana virus (Bunyaviridae) | Toscana virus meningitis | Riparian states of the Mediterranean Sea | - emerging in some South European countries | [49] |
| - dispersal of disease: reason unknown | ||||
| - reservoir host: vertebrate host unknown, vector is reservoir (?) | ||||
| Ebola virus, Marburg virus (Filoviridae) | Hemorrhagic fever | Africa | - emerging | [50] |
| - highly contagious | ||||
| - hunting, bush meat, land use change | ||||
| Nipah virus (Paramyxoviridae) | Nipah encephalitis | Malaysia | - emerging | [51] |
| - deforestation, land use change | ||||
| Hendra virus (Paramyxoviridae) | Hendra encephalitis | Australia | - emerging | [51] |
| - deforestation, land use change | ||||
| Avian influenza virus H5N1 (Orthomyxoviridae) | Bird flu | South and East Asia, Africa, Near and Middle East, Central and East Europe | - emerging | [24] |
| - reassortant virus | ||||
| - spread from domestic fowl to feral waterfowl | ||||
| - dispersal of disease by migratory birds |
Vector-borne diseases
A successful run through an infection cycle requires the pathogen's adaptation to a complex species-specific host-environment ecology (‘epidemiology is tied to ecology’). Dependence of a pathogen on an arthropod vector may further increase the complexity by characteristics of the vector biology. Only few pathogens of vector-borne diseases (e.g. dengue virus in America and Plasmodium falciparum) are strictly dependent on humans as a host, whereas most pathogens have the ability to productively infect a variety of hosts. Spreading of a disease occurs either by translocation or by dispersal of pathogen-infested vectors and hosts, and both modes may include anthropogenic contributions.
The emergence/re-emergence of several diseases was favored by the dispersal of two canopy-dwelling mosquitos, Aedes (Stegomyia) aegypti and Ae. albopictus. Ae. aegypti was translocated by the early seafarers from Africa to tropical Asia and America and transmits a considerable number of viruses including the yellow fever virus and the four serotypes of dengue virus. The virus–mosquito interactions are complex and exhibit region-specific characteristics. In the course of the yellow fever and malaria eradication programs in the 1960s, Aedes mosquitos were almost extinguished in the Americas, but after cessation of mosquito eradication efforts Ae. aegypti surged up again and extended its habitat [14]. In addition, the Asian mosquito Ae. albopictus was inadvertently translocated to Brazil and the USA in 1986 and spread mainly via the used tyre trade [15]. Notably, the recent epidemics of dengue and chikungunya fevers in the riparian states of the Indian Ocean and Italy as well as yellow fever outbreaks in America are associated with the upsurge of Ae. albopictus that readily allocates artificial vessels for breeding making it an ideal vector in urban areas [16•, 17]. In addition, genetic changes of the chikungunya virus have been made responsible for its rapid replication in Ae. albopictus and its enhanced virulence [18•].
Other, more recent examples are the emergence of West Nile virus and Usutu virus in Europe and America as well as the emergence of Alkhumra virus and Rift Valley fever virus in Saudi Arabia. Both the incidental and inadvertent translocation of pathogens by migratory birds and lifestock transportation, respectively, gave rise to unexpected epidemics and epizootics in far distant regions [19, 20, 21, 22]. Prerequisite is the acquisition of suited vectors and host species by the pathogen in the new habitat. Spread of the Sindbis virus-like Ockelbo virus in Fennoscandia in the 1960s [23] and the very recent dispersal of highly pathogenic avian influenza H5N1 virus by migrating birds from China through numerous countries of the Near and Middle East, Africa, and Europe [24] can be explained by the same mechanism. This mode is independent of climate change rather than its consequence.
The vector's habitat is constrained by a number of biotic and abiotic factors and due to its poikilothermy, it is vulnerable to meteorological factors. Hence, increase of vector-borne diseases is often attributed to climate change, for example the upsurge of tick-borne diseases (inter alia Lyme borreliosis and tick-borne encephalitis, TBE) in the Northern Hemisphere. However, increased TBE incidences may have region-specific causes [12]. The recent upsurge of TBE is an example indicating what effects the dispersal and changing population densities of hosts and vectors could have on virus activity. Increase of roe deer density in Denmark (as in most other European countries) resulted in higher tick densities. Similarly, increased roe deer density in Sweden allowed ticks to expand their areas. As a consequence, the incidences of Lyme borreliosis in Denmark and TBE in Sweden were raised [12]. In countries succeeding the former Soviet Union, socioeconomic changes rather than elevated temperatures of recent years are a conclusive explanation for the upsurge of tick-borne diseases [25•, 26].
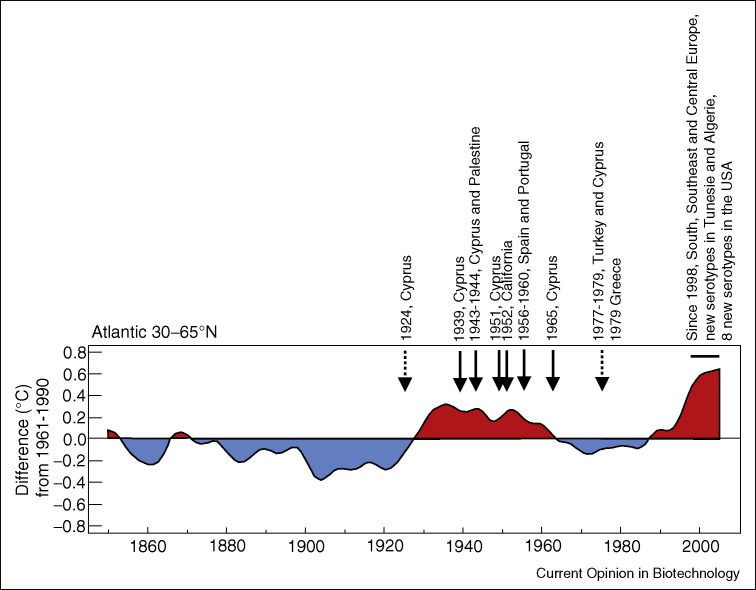
The bluetongue disease (BTD) of ruminants is transmitted by biting midges and exhibits seasonality. It was first described by D. Hutcheon in 1902, after introduction of Merino sheep in South Africa. Since then, BTD is spreading! It is restricted to tropical and subtropical areas of Africa, Asia, and the Americas where competent vectors are present (between 35°S and 40°N). Dispersal of BTD is aggravated by three factors: firstly, a worldwide extension of stock-breeding, secondly, the replacement of resistant, indigenous domestic animals by improved cattle and sheep, and thirdly, the adaptation of the principle Old World vector of the bluetongue disease virus, Culicoides imicola, to the microclimate of lifestock holdings. In three waves, BTD re-emerged in South Europe (since 1998) via Turkey, Tunisia/Algeria and Morocco [27]. Re-emergence of BTD was attributed to global warming [28] as it is linked to the northward and westward expansion of C. imicola, a highly dispersive midge spreading to Europe from sub-Saharan areas and the Asian part of Turkey. In August 2006, BTD emerged for the first time in Central Europe [29•]. Surprisingly, the etiologic agent was identified as an African strain of the bluetongue virus that has never been isolated in Europe before. The virus used indigenous Culicoides midges of the Obsoletus complex as a vector. How the virus reached Central Europe is obscure, but it appears that it was translocated inadvertently, whereas the South European virus strains spread naturally favored by both the wind-borne dispersal of infested vectors and the acquired competence of C. obsoletus after a couple of years with elevated temperatures in the past decade [27]. There is a striking co-incidence of former BTD outbreaks in Europe [30] and the USA and a previous warm phase of the AMO (Figure 1 ). It is unclear whether this time bluetongue virus stably establishes in Europe (e.g. owing to global warming).
Figure 1.
Bluetongue disease in Europe and the USA and the Atlantic Multidecadal Oscillation (AMO) index. Shown are decadal variations of annual SST anomalies from 1850 to 2005 in the extratropical North Atlantic (30–65°N). The time series is relative to the 1961–1990 mean (°C). Modified after [4•].
Rodent-borne diseases
Rodent-borne diseases exhibit fluctuations of incidences that may reflect regular effects of seasonality and irregular disturbances such as interannual climate variability and murine population dynamics. Mice densities are influenced by predators, food supply, and diseases. In arid ecosystems of the southwestern United States, rodent populations are strongly influenced by weather conditions [31, 32]. For the Sin Nombre hantavirus, the agent of hantavirus pulmonary syndrome, a correlation of human disease incidence and ENSO-driven rainfalls was described [33, 34].
Influence of coupled ocean/atmosphere phenomena
There is growing evidence that besides ENSO events, →Quasi-Biennial Oscillation and →Indian Ocean Dipole also influence the weather in the tropical and subtropical zone thereby promoting onset and development of epidemics and enzootics. It appears that the PDO drives not only Pacific Ocean →sea surface temperatures (SST) but also temperatures in America, Africa, and Asia. In its warm phase there are more El Niño events, whereas La Niña events dominate in the cold phase. A number of diseases including cholera, plague, malaria, hantavirus pulmonary syndrome, and probably dengue fever in some Polynesian islands are ENSO-associated (Table 2). Occasionally, the Indian Ocean Dipole may modulate the impact of ENSO events in the Indian Ocean. This became evident when in 1997 a gradient of strong positive SST anomalies in the western Indian Ocean and negative SSTs in the eastern Indian Ocean forced torrential rains in East Africa whereas the drought in Indonesia was more intense as usual. In the next year, the seesaw swung to the eastern Indian Ocean and caused heavy precipitations in Southeast Asia [35, 36]. As a result, devastating epidemics of Rift Valley fever, cholera, and plague were recorded in East Africa in 1997 whereas dengue fever, Japanese encephalitis, emerging Nipah encephalitis, and enterovirus 71 encephalitis afflicted Southeast Asia in the following year. Probably, a similarly strong dipole event unlinked to ENSO caused the Rift Valley fever epidemics of 1961–1963 in East Africa.
Concluding remarks
Presently, we undergo a substantial ‘global change’ with climate change being just one component. ‘Global change’ also includes shifting of demographic, social, and economic conditions. All together, these factors have an impact on human and animal health even though the contribution of each factor is difficult to quantitate. As explained in the previous paragraphs, only very few examples point toward global warming as a cause of excess viral activity. The situation may change in future, but sincere predictions are difficult and should be carefully pondered. A few years ago, several important circulation indices describing ocean/atmosphere oscillations have not been worked out and, as their contributions to climate variability have been neglected, many of the previous predictions are likely to be waste paper today.
It is considered that increased activities of many pathogens cannot exclusively be attributed to the effects of global warming. If it is not the rise of temperature—what are the reasons for the upsurge of some infectious diseases? There is an undoubted interconnection between ENSO events and certain disease outbreaks (Table 2). The more frequent and stronger ENSO events of the past decades [3•] and other climate phenomena may have influenced diseases (e.g. Ross River encephalitis—Quasi-Biennial Oscillation, Rift Valley fever—Indian Ocean Dipole). Future research will unravel more of such links. For example, outbreaks of African horse sickness correlate with some, but not all ENSO events recorded in the past 200 years [37]. Coupled ocean/atmosphere circulations and continuous anthropogenic disturbances (increased populations of humans and domestic animals, socioeconomic instability, armed conflicts, displaced populations, unbalanced ecosystems, dispersal of resistant pathogens etc.) appear to be the major drivers of disease variability and global warming at best contributes.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Footnotes
Arrow (→) indicates technical terms explained in the glossary of Box 1.
Contributor Information
Roland Zell, Email: Roland.Zell@med.uni-jena.de, i6zero@rz.uni-jena.de.
Andi Krumbholz, Email: Andi.Krumbholz@med.uni-jena.de.
Peter Wutzler, Email: Peter.Wutzler@med.uni-jena.de.
References
- 1•.Altizer S., Dobson A., Hosseini P., Hudson P., Pascual M., Rohani P. Seasonality and the dynamics of infectious diseases. Ecology Lett. 2006;9:467–484. doi: 10.1111/j.1461-0248.2005.00879.x. [DOI] [PubMed] [Google Scholar]; Authors review the literature on mathematical modelling of seasonality.
- 2.Ivers L.C., Ryan E.T. Infectious diseases of severe weather-related and flood-related natural disasters. Curr Opin Infect Dis. 2006;19:408–414. doi: 10.1097/01.qco.0000244044.85393.9e. [DOI] [PubMed] [Google Scholar]
- 3•.Trenberth KE, Jones PD, Ambenje P, Bojariu R, Easterling D, Klein Tank A, Parker D, Rahimzadeh F, Renwick JA, Rusticucci M, et al.: Observations: Surface and Atmospheric Climate Change. In Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Edited by Solomon S, Qin D, Manning M, Chen Z, Marquis M, Averyt KB, Tignor M, Miller HL. United Kingdom, USA: Cambridge University Press, Cambridge, and New York, NY; 2007:235–336.; A thorough description of atmospheric climate changes. Patterns of atmospheric circulation variability are specified.
- 4•.Forster P, Ramaswamy V, Artaxo P, Berntsen T, Betts R, Fahey DW, Haywood J, Lean J, Lowe DC, Myhre G, et al.: Changes in Atmospheric Constituents and in Radiative Forcing. In Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Edited by Solomon S, Qin D, Manning M, Chen Z, Marquis M, Averyt KB, Tignor M, Miller HL. United Kingdom, USA: Cambridge University Press, Cambridge, and New York, NY; 2007:129–234.; A thorough description of the changes in atmosphere composition due to the accumulation of greenhouse gases.
- 5•.Shope R. Global climate change and infectious diseases. Environ Health Perspect. 1991;96:171–174. doi: 10.1289/ehp.9196171. [DOI] [PMC free article] [PubMed] [Google Scholar]; Probably not the first but a well-perceived early paper connecting climate change and infectious diseases.
- 6•.Patz J.A., Epstein P.R., Burke T.A., Balbus J.M. Global climate change and emerging infectious diseases. J Am Med Assoc. 1996;275:217–223. [PubMed] [Google Scholar]; By far the most cited article promoting the concept of infectious disease incidence increased by climate change.
- 7•.Confalonieri U, Menne B, Akhtar R, Ebi KL, Hauengue M, Kovats RS, Revich B, Woodward A: Human health. In Climate Change 2007: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Edited by ML Parry, OF Canziani, JP Palutikof, PJ van der Linden and CE Hanson. United Kingdom: Cambridge University Press, Cambridge; 2007:391–431.; A compilation of mostly adverse and some benificial effects of climate change to human health.
- 8.Taubes G. Global warming: apocalypse not. Science. 1997;278:1004–1006. doi: 10.1126/science.278.5340.1004. [DOI] [PubMed] [Google Scholar]
- 9.Reiter P. Climate change and mosquito-borne disease. Environ Health Persp. 2001;109:141–161. doi: 10.1289/ehp.01109s1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hay S.I., Rogers D.J., Randolph S.E., Stem D.I., Cox J., Shanks G.D., Snow R.W. Hot topic or hot air? Climate change and malaria resurgence in East African highlands. Trends Parasitol. 2002;18:530–534. doi: 10.1016/s1471-4922(02)02374-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reiter P., Lathrop S., Bunning M., Biggerstaff B., Singer D., Tiwari T., Baber L., Amador M., Thirion J., Hayes J. Texas lifestyle limits transmission of dengue virus. Emerg Inf Dis. 2003;9:86–89. doi: 10.3201/eid0901.020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Randolph S.E. Evidence that climate change has caused ‘emergence’ of tick-borne diseases in Europe? Int J Med Microbiol. 2004;293(Suppl 37):5–15. doi: 10.1016/s1433-1128(04)80004-4. [DOI] [PubMed] [Google Scholar]
- 13.Zell R. Global climate change and the emergence/re-emergence of infectious diseases. Int J Med Microbiol. 2004;293(Suppl 37):16–26. doi: 10.1016/s1433-1128(04)80005-6. [DOI] [PubMed] [Google Scholar]
- 14.Halstead S.B. Dengue virus-mosquito interactions. Annu Rev Entomol. 2008;53:273–291. doi: 10.1146/annurev.ento.53.103106.093326. [DOI] [PubMed] [Google Scholar]
- 15.Knudson A.B. Geographic spread of Aedes albopictus in Europe and the concern among public health authorities. Eur J Epidem. 1995;11:345–348. doi: 10.1007/BF01719441. [DOI] [PubMed] [Google Scholar]
- 16•.Reiter P., Fontenille D., Paupy C. Aedes albopictus as an epidemic vector of chikungunya virus: another emerging problem? Lancet Inf Dis. 2006;6:463–464. doi: 10.1016/S1473-3099(06)70531-X. [DOI] [PubMed] [Google Scholar]; The present Indian Ocean outbreak of chikungunya fever can be traced to Kinshasa, 1999–2000. Then, it spread to Kenya, 2004, and swept over to several Indian Ocean islands and riparian states in 2005–2006. More than one million people and numerous travellers were affected by the disease. Recommended are two recently published opinions by Reiter et al. and Charrel et al. describing the problems arising with Aedes albopictus as a new vector of the virus.
- 17.Charrel R.N., de Lamballerie X., Raoult D. Chikunguya outbreaks—the globalization of vectorborne diseases. N Engl J Med. 2007;356:769–771. doi: 10.1056/NEJMp078013. [DOI] [PubMed] [Google Scholar]
- 18•.Schuffenecker I., Iteman I., Michault A., Murri S., Frangeul L., Vaney M.C., Lavenir R., Pardigon N., Reynes J.M., Pettinelli F. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 2006;3(7):e263. doi: 10.1371/journal.pmed.0030263. [DOI] [PMC free article] [PubMed] [Google Scholar]; A detailed analysis of the microevolution of chikungunya virus sequences of 127 patients from Indian Ocean islands. The authors present a plausible explanation for the atypical virulence of the virus as they describe the A226V substitution of the E1 envelope protein that appears to influence viral infectivity, dissemination, and transmission in Aedes albopictus.
- 19.Kramer L.D., Styer L.M., Ebel G.D. A global perspective on the epidemiology of West Nile virus. Annu Rev Entomol. 2008;53:61–81. doi: 10.1146/annurev.ento.53.103106.093258. [DOI] [PubMed] [Google Scholar]
- 20.Meister T., Lussy H., Bakonyi T., Sikutová S., Rudolf I., Vogl W., Winkler H., Frey H., Hubálek Z., Nowotny N., Weissenböck H. Serological evidence of continuing high Usutu virus (Flaviviridae) activity and establishment of herd immunity in wild birds in Austria. Vet Microbiol. 2008;127:237–248. doi: 10.1016/j.vetmic.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 21.Zaki A.M. Isolation of a flavivirus related to the tickborne encephalitis complex from human cases in Saudi Arabia. Trans R Soc Trop Med Hyg. 1997;91:179–181. doi: 10.1016/s0035-9203(97)90215-7. [DOI] [PubMed] [Google Scholar]
- 22.Madani T.A., Al-Mazrou Y.Y., Al-Jeffri M.H., Mishkhas A.A., Al-Rabeah A.M., Turkistani A.M., Al-Sayed M.O., Abodahish A.A., Khan A.S., Ksiazek T.G., Shobokshi O. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin Infect Dis. 2003;37:1084–1092. doi: 10.1086/378747. [DOI] [PubMed] [Google Scholar]
- 23.Laine M., Liikkainen R., Toivanen A. Sindbis viruses and other alphaviruses as cause of human arthritic disease. J Intern Med. 2004;256:457–471. doi: 10.1111/j.1365-2796.2004.01413.x. [DOI] [PubMed] [Google Scholar]
- 24.Yee KS, Carpenter TE, Cardona CJ: Epidemiology of H5N1 avian influenza.Comp Immunol Microbiol Inf Dis 2008, in press. [DOI] [PubMed]
- 25•.Sumilo D., Asokliene L., Bormane A., Vasilenko V., Golovljova I., Randolph S.E. Climate change cannot explain the upsurge of tick-borne encephalitis in the Baltics. PLoS One. 2007;2:e500. doi: 10.1371/journal.pone.0000500. [DOI] [PMC free article] [PubMed] [Google Scholar]; Detailed analysis of changes in TBE incidence and weather data in the Baltic states leading to the conclusion that climate change cannot be blamed for the increased incidence of TBE in several European countries.
- 26.Sumilo D., Bormane A., Asokliene L., Vasilenko V., Golovljova I., Avsic-Zupank T., Hubalek Z., Randolph S.E. Socio-economic factors in the differential upsurge of tick-borne encephalitis in Central and Eastern Europe. Rev Med Virol. 2008;18:81–95. doi: 10.1002/rmv.566. [DOI] [PubMed] [Google Scholar]
- 27.Mellor P.S., Wittmann E.J. Bluetongue virus in the Mediterranean Basin 1998–2001. Vet J. 2002;164:20–37. doi: 10.1053/tvjl.2002.0713. [DOI] [PubMed] [Google Scholar]
- 28.Purse B.V., Mellor P.S., Rogers D.J., Samuel A.R., Mertens P.P.C., Baylis M. Climate change and the recent emergence of bluetongue in Europe. Nat Rev Microbiol. 1999;3:171–181. doi: 10.1038/nrmicro1090. [DOI] [PubMed] [Google Scholar]
- 29•.Mehlhorn H., Walldorf V., Klimpel S., Jahn B., Jaeger F., Eschweiler J., Hoffmann B., Beer M. First occurrence of Culicoides obsoletus-transmitted Bluetongue virus epidemic in Central Europe. Parasitol Res. 2007;101:219–228. doi: 10.1007/s00436-007-0519-6. [DOI] [PubMed] [Google Scholar]; Several publications describe bluetongue disease in Central Europe. This study is a very thorough analysis of the outbreaks in Germany, 2006–2007.
- 30.Mellor P.S., Carpenter S., Harrup L., Baylis M., Mertens PPC: Bluetongue in Europe and the Mediterranean Basin: History of occurrence prior to 2006. Prev Vet Med. 2008;87:4–20. doi: 10.1016/j.prevetmed.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Kuenzi A.J., Morrison M.L., Madhav N.K., Mills J.N. Brush mouse (Peromyscus boylii) population dynamics and hantavirus infection during a warm, drought period in southern Arizona. J Wildl Dis. 2007;43:675–683. doi: 10.7589/0090-3558-43.4.675. [DOI] [PubMed] [Google Scholar]
- 32.Thibault K.M., Brown J.H. Impact of an extreme climatic event on community assembly. Proc Natl Acad Sci U S A. 2008;105:3410–3415. doi: 10.1073/pnas.0712282105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Engelthaler D.M., Mosley D.G., Cheek J.E., Levy C.E., Komatsu K.K., Ettestad P., Davis T., Tanda D.T., Miller L., Frampton J.W. Climatic and environmental patterns associated with hantavirus pulmonary syndrome, Four Corners Region, United States. Emerg Inf Dis. 1999;5:87–94. doi: 10.3201/eid0501.990110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hjelle B., Glass G.E. Outbreak of hantavirus infection in the Four Corners region of the United States in the wake of the 1997–1998 El Niño-Southern Oscillation. J Infect Dis. 2000;181:1569–1573. doi: 10.1086/315467. [DOI] [PubMed] [Google Scholar]
- 35.Webster P.J., Moore A.M., Loschnigg J.P., Leben R.R. Coupled ocean-atmosphere dynamics in the Indian Ocean during 1997–98. Nature. 1999;401:356–360. doi: 10.1038/43848. [DOI] [PubMed] [Google Scholar]
- 36.Saji N.H., Goswami B.N., Vinyachandran P.N., Yamagata T. A dipole mode in the tropical Indian Ocean. Nature. 1999;401:360–363. doi: 10.1038/43854. [DOI] [PubMed] [Google Scholar]
- 37.Baylis M., Mellor P.S., Meiswinkel R. Horse sickness and ENSO in South Africa. Nature. 1999;397:574. doi: 10.1038/17512. [DOI] [PubMed] [Google Scholar]
- 38••.Wearing H.J., Rohani P. Ecological and immunological determinants of dengue epidemics. Proc Natl Acad Sci U S A. 2006;103:11802–11807. doi: 10.1073/pnas.0602960103. [DOI] [PMC free article] [PubMed] [Google Scholar]; Readable study using long-term datasets to demonstrate that both ecological factors and temporary heterologous cross-immunity contribute to dengue epidemics whereas variation in dengue virus virulence and antibody-dependent enhancement cannot explain patterns of serotype-specific notification data in Thailand. Supporting Fig. 4 of their paper demonstrates the three-year signature in dengue dynamics that cannot be explained by ENSO or global warming.
- 39.Hales S., Weinstein P., Woodward A. Dengue fever epidemics in th South Pacific: driven by El Nino Southern Oscillation? Lancet. 1996;348:1664–1665. doi: 10.1016/S0140-6736(05)65737-6. [DOI] [PubMed] [Google Scholar]
- 40.Hales S., Weinstein P., Souares Y., Woodward A. El Niño and the dynamics of vectorborne disease transmission. Environ Health Persp. 1999;107:99–102. doi: 10.1289/ehp.9910799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barrett A.D.T., Higgs S. Yellow fever: a disease that has yet to be conquered. Annu Rev Entomol. 2007;52:209–229. doi: 10.1146/annurev.ento.52.110405.091454. [DOI] [PubMed] [Google Scholar]
- 42.Nicholls N. El Niño-Souhern Oscillation and vector-borne disease. Lancet. 1993;342:1284–1285. doi: 10.1016/0140-6736(93)92368-4. [DOI] [PubMed] [Google Scholar]
- 43.Broom A.K., Lindsay M.D., Johansen C.A., Wright A.E., Mackenzie J.S. Two possible mechanisms for survival and initiation of Murray Valley encephalitis virus activity in the Kimberley region of Western Australia. Am J Trop Med Hyg. 1995;53:95–99. [PubMed] [Google Scholar]
- 44.Lindgren E., Tälleklint L., Polfeldt T. Impact of climatic change on the northern latitude limit and population density of the disease-transmitting European tick Ixodes ricinus. Environ Health Perspect. 2000;108:119–123. doi: 10.1289/ehp.00108119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Done S.J., Holbrook N.J., Beggs P.J. The Quasi-Biennial Oscillation and Ross River virus incidence in Queensland, Australia. Int J Biometeorol. 2002;46:202–207. doi: 10.1007/s00484-002-0137-z. [DOI] [PubMed] [Google Scholar]
- 46.Ward M.P., Johnson S.J. Bluetongue virus and the southern oscillation index: evidence of an association. Prev Vet Med. 1996;28:57–68. [Google Scholar]
- 47.Linthicum K.J., Anyamba A., Tucker C.J., Kelley P.W., Myers M.F., Peters C.J. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science. 1999;285:397–400. doi: 10.1126/science.285.5426.397. [DOI] [PubMed] [Google Scholar]
- 48.Abd el-Rahim I.H., Abd el-Hakim U., Hussein M. An epizootic of Rift Valley fever in Egypt in 1997. Rev Sci Tech. 1999;18:741–748. doi: 10.20506/rst.18.3.1195. [DOI] [PubMed] [Google Scholar]
- 49.Charrel R.N., Gallian P., Navarro-Mari J.M., Nicoletti L., Papa A., Sanchez-Seco M.P., Tenorio A., de Lamballerie X. Emergence of Toscana virus in Europe. Emerg Inf Dis. 2005;11:1657–1663. doi: 10.3201/eid1111.050869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Groseth A., Feldmann H., Strong J.E. The ecology of Ebola virus. Trends Microbiol. 2007;15:408–416. doi: 10.1016/j.tim.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 51.Field H.E., Mackenzie J.S., Daszak P. Henipaviruses: emerging paramyxoviruses associated with fruit bats. Curr Top Microbiol Immunol. 2007;315:133–159. doi: 10.1007/978-3-540-70962-6_7. [DOI] [PMC free article] [PubMed] [Google Scholar]