Abstract
Background:
We performed a study to assess the effects of a quality improvement (QI) initiative on rates of post-variceal bleeding surveillance EGD.
Methods:
We identified patients with cirrhosis hospitalized with variceal bleeding and assessed rates of timely (≤4 weeks) EGD before and after a QI initiative.
Results:
Pre-intervention, 16% (5 of 32) patients underwent timely surveillance EGD. We developed a standardized ordering template for gastroenterology fellows and reserved post-variceal EGD scheduling slots. Post-intervention 43% (12 of 28) patients underwent timely surveillance EGD.
Conclusion:
A QI intervention was associated with a 27% absolute increase in timely surveillance EGDs.
Keywords: varices, hemorrhage, EGD
Introduction
Esophageal variceal bleeding is a common complication of cirrhosis associated with high mortality (1). Use of non-selective beta blockers and endoscopic variceal ligation (EVL) after an episode of bleeding decreases rebleeding and mortality (2). As a result, major gastroenterology and hepatology societies recommend repeat upper endoscopy (EGD) with EVL at 2-4 week intervals until obliteration of varices (2, 3). Unfortunately, studies demonstrate that patients often fail to receive recommended secondary prophylaxis after an initial variceal bleeding episode (4-6) and there are few published quality improvement (QI) efforts aimed at addressing this issue (7).
Therefore, we aimed to design and assess a QI intervention at a tertiary care center to improve the receipt of timely surveillance endoscopy among patients with cirrhosis admitted with bleeding esophageal varices.
Methods
We included patients with cirrhosis hospitalized at University of North Carolina (UNC) for esophageal variceal bleeding. Exclusion criteria included death during hospitalization, discharge to hospice, transjugular intrahepatic portosystemic shunt (TIPS) placement or liver transplantation during the 4 weeks following the variceal bleed, or patient decision to receive surveillance EGD at outside facility.
The primary outcome was receipt of timely surveillance EGD, defined as receipt of upper endoscopy 1-4 weeks from initial EGD, in accordance with American Association for the Liver Diseases (AASLD) guidelines (2). For those who did not receive timely endoscopy, we identified the reason(s) including failure to place an EGD order, failure to schedule an EGD, scheduling the EGD >4 weeks from index bleed, and cancellations/no-shows. The study had a pre-implementation control period from July 2017 through June 2018 and post-implementation study period from December 2018 through November 2019, including two unique cohorts.
Based on data from the control period, we developed a fishbone diagram (Figure 1) and subsequent QI intervention that included a standardized ordering process for surveillance EGDs and two reserved post-variceal bleed EGD procedure visits per week. The intervention was presented at a Gastroenterology and Hepatology Division conference and was distributed via a division-wide email to all faculty and fellows. The ordering process and the importance of timely scheduling was also reviewed with the GI Procedures scheduling office.
Figure 1. Fishbone diagram outlining potential causes of low rates of post-variceal bleeding surveillance EGDs.
Diagram outlines the potential contributing causes for failure of patients to receive timely post-variceal bleed surveillance EGD. Each potential contributing cause is organized within categories including environment, place, policy, and people (patient and medical professional). Potential procedure and equipment issues were explored but none were identified as proximate causes.
The UNC Institutional Review Board (IRB) determined that this QI study did not require IRB approval because it did not constitute human subjects research as defined by federal regulations.
Results
Pre-Intervention Data
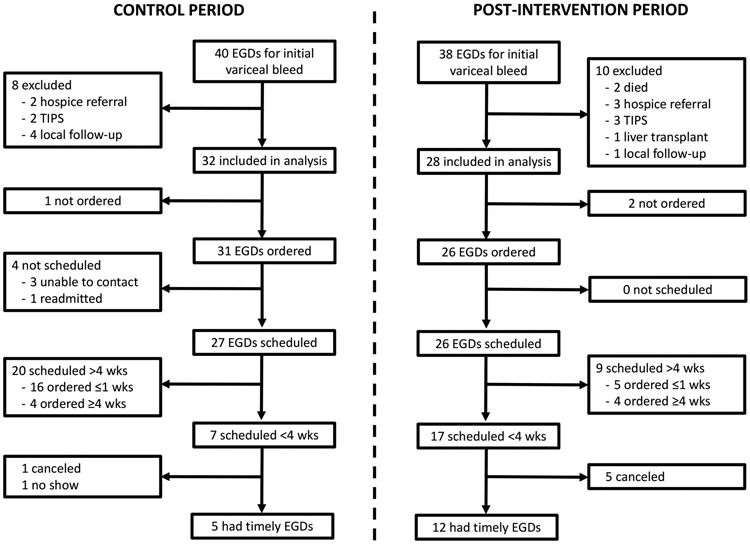
During the control period, 32 patients were eligible for inclusion, of whom 5 (16%) underwent timely surveillance (Figure 2). In the pre-intervention period, the median time to EGD after discharge was 41 days (IQR 29-77), including 23 days (IQR 21-25) in those with timely EGDs and 46 days (IQR 36-97) in those without timely EGDs. The most common reason for failure to receive timely surveillance EGD was the EGD being scheduled for a date >4 weeks after the index bleed (74%).
Figure 2. Flow chart of provision of surveillance EGD among patients hospitalized for variceal bleeding in the control and post-intervention periods.
In the control period, 40 patients were considered for analysis and, after exclusions, 32 were included in the analysis. Due to failure to order or schedule EGD, late scheduling, cancelations and no-shows, 27 did not receive timely EGDs. In the post-intervention period, 38 patients were considered and 28 were included in the analysis. Overall, 16 of 28 patients did not receive timely EGDs because they were not ordered, scheduled late or canceled.
QI Intervention
We determined that the most common reason for failure to schedule surveillance EGD within 4 weeks of the index bleed was due to lack of availability of procedure slots in the outpatient endoscopy schedule, particularly with hepatology providers. Thus, our primary QI intervention was the creation of two outpatient post-variceal bleed EGD procedure visits per week reserved for hepatologists. A second component of the QI intervention was to standardize the ordering process for surveillance EGDs, including a templated order to be placed by the hepatology consult fellow prior to the patient’s hospital discharge. As part of this intervention, all UNC gastroenterology fellows were emailed twice and instructed to use specific language in the order comment section specifying the required date range of the surveillance EGD and the use of the designated post-variceal bleeding scheduling slots.
Post-Intervention Data
Of the 28 patients included in the post-intervention analysis, 12 (43%) underwent timely surveillance EGD (Figure 2). In the post-intervention period, the median time to EGD after discharge was 22 days (IQR 17-37), including 17 days (IQR 14-21) in those with timely EGDs and 43 days (IQR 34-61) in those without timely EGDs. Reasons for failure to undergo timely surveillance EGD were scheduling the EGD >4 weeks after the index bleed (56%) and cancelations (31%), and lack of placing an EGD order (13%).
Discussion
Surveillance endoscopy with EVL is important for secondary prophylaxis of variceal bleeding. In this QI project, the development of post-variceal bleed EGD procedure slots and standardization of the ordering protocol resulted in a 27% absolute increase in the proportion of patients receiving timely surveillance EGD. However, a substantial proportion of patients in the post-intervention period still had their surveillance EGD performed >4 weeks after the index bleed. Several of these patients cancelled their procedures or had EGDs ordered ≥4 weeks after the index bleed and there were 5 instances in which an EGD order was placed in a timely and appropriate fashion and surveillance EGD was scheduled late. This suggests that the educational component of the QI intervention involving the EGD order template had limited effect. Despite the persistently low post-intervention receipt of timely EGDs, the relative distributions of EGD timing among those with non-timely EGDs in the pre-intervention (IQR 36-97) and post-intervention (IQR 34-61) cohort suggest our intervention may have had effects not fully captured by our primary outcome measure.
Our findings expand upon previously published work. A QI intervention in Australia resulted in dramatic and sustained improvement in variceal eradication rates after hiring of a dedicated nurse to coordinate patient follow up after variceal bleeding (8). Furthermore, a recent study in a Veterans Affairs endoscopy unit identified interventions focused on improving patient education and streamlining the process of cancelling and rescheduling procedures as the most effective at decreasing no-shows and late cancellations (9). These studies in combination with our findings suggest that QI efforts must extend beyond educational interventions alone to be effective.
There are several potential future directions for improving timely surveillance EGD rates. This QI intervention was entirely clinician-focused and future efforts could intervene on patient-related issues including patient education on the importance of surveillance EGD, transportation issues or social issues that may adversely affect ability to follow up. Changes in the US health care system, including increased hospital consolidation and near-universal use of the electronic health record, may provide opportunities for improving rates of timely surveillance endoscopy. Distance from tertiary care centers and transportation issues could contribute to non-receipt of surveillance endoscopy. Enlarging health care networks may allow patients to schedule surveillance EGDs closer to home (10). In addition, reminders through the electronic health record could be used to improve ordering and scheduling of procedures, as has been successfully done for hepatocellular carcinoma screening (11, 12).
In conclusion, after employing a QI project including fellow education and flexible scheduling dedicated to variceal surveillance, rates of timely surveillance endoscopy improved and surpassed our goal of a 20% absolute increase in rates. Future efforts could be made to leverage hospital system networks and electronic reminders within the electronic health record to further improve surveillance EGD rates.
Acknowledgements:
We would like to acknowledge Patrick Wiginton from UNC Practice Quality & Innovation/Population Health Services for his assistance with this project.
Grant Support: This research was supported in part by NIH grant T32 DK007634 (AMM and HPK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations:
- AASLD
American Association for the Study of Liver Diseases
- EGD
esophagogastroduodenoscopy
- EVL
endoscopic variceal ligation
- GI
gastroenterology
- QI
quality improvement
- UNC
University of North Carolina
Footnotes
Disclosures: None
Conflict of Interest: There are no potential personal or financial conflicts of interest to disclose.
References
- 1.Fortune BE, Garcia-Tsao G, Ciarleglio M, et al. Child-Turcotte-Pugh Class is Best at Stratifying Risk in Variceal Hemorrhage: Analysis of a US Multicenter Prospective Study. J Clin Gastroenterol 2017;51:446–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65:310–335. [DOI] [PubMed] [Google Scholar]
- 3.de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol 2015;63:743–52. [DOI] [PubMed] [Google Scholar]
- 4.Buchanan PM, Kramer JR, El-Serag HB, et al. The quality of care provided to patients with varices in the department of Veterans Affairs. Am J Gastroenterol 2014;109:934–40. [DOI] [PubMed] [Google Scholar]
- 5.Singh H, Targownik LE, Ward G, et al. An assessment of endoscopic and concomitant management of acute variceal bleeding at a tertiary care centre. Can J Gastroenterol 2007;21:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hobolth L, Krag A, Malchow-Moller A, et al. Adherence to guidelines in bleeding oesophageal varices and effects on outcome: comparison between a specialized unit and a community hospital. Eur J Gastroenterol Hepatol 2010;22:1221–7. [DOI] [PubMed] [Google Scholar]
- 7.Tapper EB. Building Effective Quality Improvement Programs for Liver Disease: A Systematic Review of Quality Improvement Initiatives. Clin Gastroenterol Hepatol 2016;14:1256–1265 e3. [DOI] [PubMed] [Google Scholar]
- 8.Wundke R, Altus R, Sandford J, et al. Improving management of oesophageal varices in patients with cirrhosis. Qual Saf Health Care 2010;19:536–41. [DOI] [PubMed] [Google Scholar]
- 9.Finn RT, Lloyd B, Patel YA, et al. Decreasing Endoscopy No-Shows Using a Lean Improvement Framework. Clin Gastroenterol Hepatol 2019;17:1224–1227 e3. [DOI] [PubMed] [Google Scholar]
- 10.Muhlestein DB, Smith NJ. Physician Consolidation: Rapid Movement From Small To Large Group Practices, 2013-15. Health Aff (Millwood) 2016;35:1638–42. [DOI] [PubMed] [Google Scholar]
- 11.Aberra FB, Essenmacher M, Fisher N, et al. Quality improvement measures lead to higher surveillance rates for hepatocellular carcinoma in patients with cirrhosis. Dig Dis Sci 2013;58:1157–60. [DOI] [PubMed] [Google Scholar]
- 12.Beste LA, Ioannou GN, Yang Y, et al. Improved surveillance for hepatocellular carcinoma with a primary care-oriented clinical reminder. Clin Gastroenterol Hepatol 2015;13:172–9. [DOI] [PubMed] [Google Scholar]