Abstract
Objective
To assess the concordance between transesophageal echocardiography (TEE) and transthoracic echocardiography (TTE) measures of right ventricular (RV) function by standard two-dimensional and Doppler methods. We hypothesized that there would be significant disagreement in tricuspid annular plane systolic excursion (TAPSE), fractional area change (FAC), right-sided index of myocardial performance (RIMP), and tricuspid annular systolic velocity (S`).
Design
Prospective observational
Setting
Cardiac operating room at a single academic medical center
Participants
All adult patients undergoing elective cardiac surgery at a single tertiary care academic medical center over the course of six months
Interventions
None.
Measurements and Main Results
We measured fractional area change, tricuspid annular systolic velocity, tricuspid annular systolic plane excursion, right-sided index of myocardial performance and tricuspid annular diameter by transesophageal echocardiography and transthoracic echocardiography. We assessed for concordance by concordance correlation coefficient and paired t-tests, including 95% confidence limits. We found that quantitative measures of right ventricular function by transesophageal echocardiography correlate poorly with transthoracic echocardiography measurements in close temporal proximity under similar hemodynamic conditions.
Conclusions
When performing an assessment of RV function, transesophageal echocardiographers should exercise caution when extrapolating data validated by TTE to transesophageal studies. Measures of right ventricular function by TEE tend to have fair agreement to TTE measurements obtained in close temporal proximity under similar hemodynamic conditions. Most importantly, our study showed that TAPSE and S` values obtained from the modified transgastric RV inflow view tend to have lower values than those measured by TTE. Given the propensity for underestimating measurements from the modified transgastric RV inflow view, we conclude that values equal to or greater than established norms for tricuspid annular motion may be utilized to establish normal, but not abnormal, RV function.
Keywords: Transesophageal echocardiography, Transthoracic echocardiography, Right ventricle, Right ventricular function
Introduction
Since the introduction of real-time two-dimensional echocardiography in the early 1970s, transthoracic echocardiography (TTE) has been the cornerstone of non-invasive cardiac function evaluation 1–3. Most, if not all, standard measures of cardiac size and function have been established utilizing this modality.4 With the advent of transesophageal echocardiography (TEE), these measures have continued to be used as the basis for evaluating cardiac function with the assumption that they are reasonably similar. While at times this may be true, even slight modifications of imaging planes have been shown to cause statistically significant differences in measured values, specifically when it comes to evaluating right ventricular (RV) function.5
The RV has long been a focus of research.6 Given its complex shape and function, multiple methods have been developed to evaluate its systolic function. These include: tricuspid annular plane systolic excursion (TAPSE), fractional area change (FAC), right-sided index of myocardial performance (RIMP), and tricuspid annular systolic velocity (S`).4 TEE poses a particular challenge in proper Doppler and M-mode alignment to assess tricuspid annular motion. Previous studies have compared TTE TAPSE results to TEE TAPSE results obtained by modified methods.7, 8 These were met with varying results, which is not particularly surprising since apical TTE assesses the lateral wall of the RV while TEE examines the inferior wall in the modified transgastric view.9–11 Previous authors have also demonstrated significant regional differences in tricuspid annular dynamics.12, 13 Despite this, normal values for both TTE and TEE are often used interchangeably in daily practice by echocardiographers. The objective of our study was to assess the concordance between TEE and TTE measures of RV function by standard two-dimensional and Doppler methods. We hypothesized that there would be significant disagreement in TAPSE, FAC, RIMP, and S`.
Methods
Study Population
We conducted a prospective observational study including all adult patients undergoing elective cardiac surgery at a single tertiary care academic medical center over the course of six months. Baseline preoperative patient characteristics can be found in Table 1. A sample size of 125 subjects was calculated allowing for a level of precision ±0.10 for a 95% confidence interval around an estimate of agreement between measures derived from TEE vs. TTE and allowing for 10% dropout. Exclusion criteria included patients with a contraindication to TEE, urgent/emergent surgery, preexisting open chest, intrathoracic hardware (ventricular assist device, thoracotomy tube, etc.), hemodynamically unstable patients as judged by the attending anesthesiologist, patients with body mass index > 40 kg/m2 due to likelihood of poor TTE image quality, non-English speaking patients due to lack of study funding for translator services, cognitively impaired adults, and pregnant patients. Patients were excluded from analysis if there was poor echocardiographic image quality at the time of image analysis as judged by the measuring anesthesiologist. The study protocol was approved by the local institutional review board and all patients provided written informed consent.
Table 1.
Baseline preoperative patient characteristics.
| Mean | Std Dev | |
|---|---|---|
| Age (years) | 64.8 | 12.83 |
| EF (%) | 51.6 | 10.67 |
| Surgery Type | ||
| CABG | 59 | |
| CABG + Valve | 7 | |
| AVR | 23 | |
| MVR | 14 | |
| Multivalve | 16 | |
| LVAD | 2 | |
| Other | 4 | |
Abbreviations: AVR = aortic valve replacement; CABG = coronary artery bypass grafting; EF = left ventricular ejection fraction; LVAD = left ventricular assist device; MVR = mitral valve repair/replacement.
Echocardiographic Image Acquisition and Data Collection
Echocardiographic images were obtained using a commercially available ultrasound system (Epiq 7; Philips Medical Systems, Best, the Netherlands) with a 1.5-MHz TTE transducer and an x7 TEE probe. Immediately following induction of anesthesia and insertion of the TEE probe as per standard protocol for surgery, the images were obtained by an attending anesthesiologist separate from the primary anesthesia team. All anesthesiologists involved were board certified in Advanced Perioperative Transesophageal Echocardiography as well as research team members with additional competencies in transthoracic echocardiography including Testamurs of Special Competence in Adult Echocardiography and Critical Care Echocardiography. Immediately following TTE image acquisition, TEE images were obtained. The two image acquisition sets were obtained within 5 minutes of one another and under similar hemodynamic conditions (heart rate and mean arterial pressure +/− 10%). No surgical stimulation or any other factors, such as patient position change, occurred during image acquisition using either modality. If patients became unstable or had hemodynamic changes >10% of baseline heart rate or mean arterial pressure, the images were excluded from data analysis. Images were stored in Digital Imaging and Communications in Medicine (DICOM®) format (National Electrical Manufacturers Association, Arlington, Virginia, USA).
Imaging Methods
The following TTE images were obtained over three consecutive beats: apical 4-chamber view, lateral tricuspid annulus M-mode, and lateral tricuspid annulus tissue Doppler pulsed wave spectral Doppler profile. The following TEE measurements were then obtained over three consecutive beats: midesophageal 4-chamber view with RV focus, lateral tricuspid annulus anatomic M-mode, modified transgastric RV inflow view M-mode and inferior tricuspid annulus tissue Doppler pulsed wave spectral Doppler profile. A single cardiac cycle from these image sets was then used to calculate post-hoc measures of RV function including both TTE and TEE RIMP, TAPSE, FAC, and S`. All measurements were performed by two anesthesiologist who were blinded to the original imaging anesthesiologist. For the initial 15 offline measurements, two anesthesiologists performed the measurements together for uniformity on measurement standards, after which subject data was equally divided and randomly assigned for independent analysis.
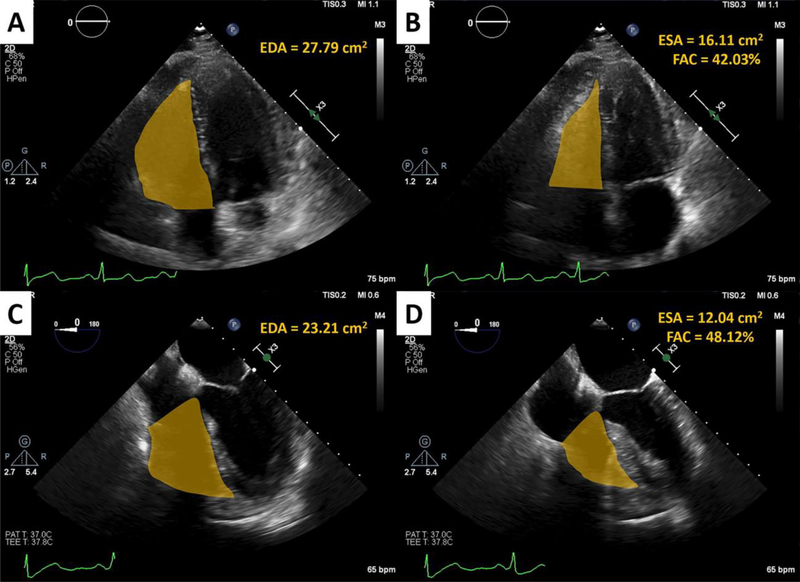
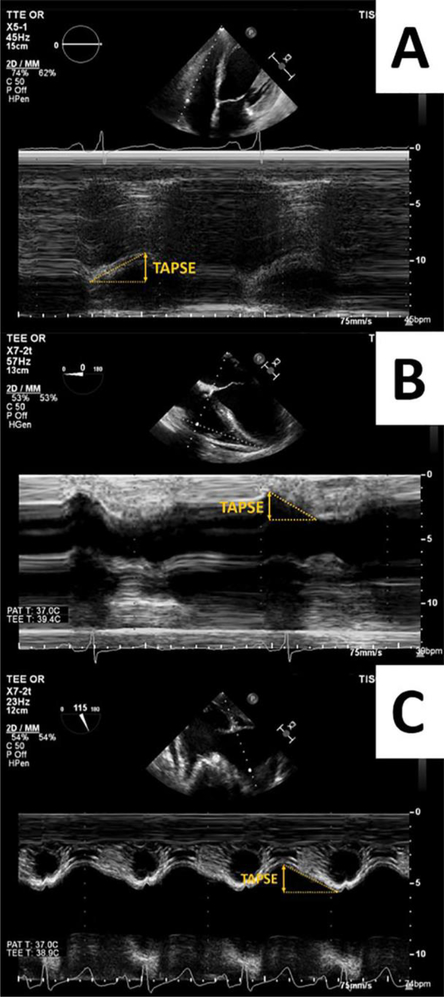
Example FAC calculations from the same patient are demonstrated in Figure 1. RIMP was assessed using tissue Doppler imaging by adding the isovolumetric contraction and relaxation times and dividing by the ejection time. TAPSE measurements were obtained by TTE (TTE TAPSE) and TEE via the midesophageal 4-chamber view using anatomic M-mode (AMM TAPSE) and by the modified transgastric RV inflow view (TG TAPSE) (Figure 2). The anatomic M-mode measurements were completed by placing the cursor on the lateral tricuspid annulus and the angle was adjusted such that the angle of measure was directed toward the apex (Figure 2, Panel B). The modified transgastric RV inflow view has been previously described and allows for improved Doppler alignment with the inferior tricuspid annular motion (Figure 2, Panel C).14 Tricuspid annular diameter was measured from the lateral to septal tricuspid annulus at end-diastole.
Figure 1:
FAC measurements using the TTE apical four-chamber view measuring end-diastolic area (EDA) (A) and end-systolic area (ESA) (B) compared to the TEE four-chamber view showing EDA (C) and ESA (D) with their respective FAC calculations, all in the same patient.
Figure 2:
Comparison of TAPSE methodologies using TTE apical four-chamber view (A), TEE four-chamber view using AMM (B), and the TEE TG RV inflow view (C).
Statistical Analysis
Distribution of RV function measures by both TTE and TEE were evaluated to confirm approximate normality. Agreement between each TTE and TEE measure was assessed graphically by viewing scatterplots of the data, and statistically by estimating the concordance correlation coefficient and corresponding 95% confidence interval (CI) for each measure. The concordance correlation coefficient measures variations in the linear relationship between two methods from the identity lines of two meaningful components: deviations in each measurement around the line (precision) and the distance between the identity line and the linear line (accuracy). According to Landis & Koch descriptions of estimates of agreement are: a coefficient of 0–0.20 slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement, and 0.81–1 almost perfect agreement.15 The average difference between results obtained by TTE and TEE was calculated for each measure of RV function to be able to determine whether TEE over- or underestimated those obtained by TTE. These differences were then evaluated with a paired t-test to determine whether they were significantly different from zero. Each of the measures was also dichotomized to create categorical variables indicating abnormal or normal values according to the American Society of Echocardiography (ASE) recommendations for abnormal values: TAPSE <1.7 cm, FAC <35%, S` <9.5 cm/s, RIMP >0.54. Kappa coefficients and 95% CIs were estimated to assess agreement between TTE and TEE measures with respect to categorical variables.4
Results
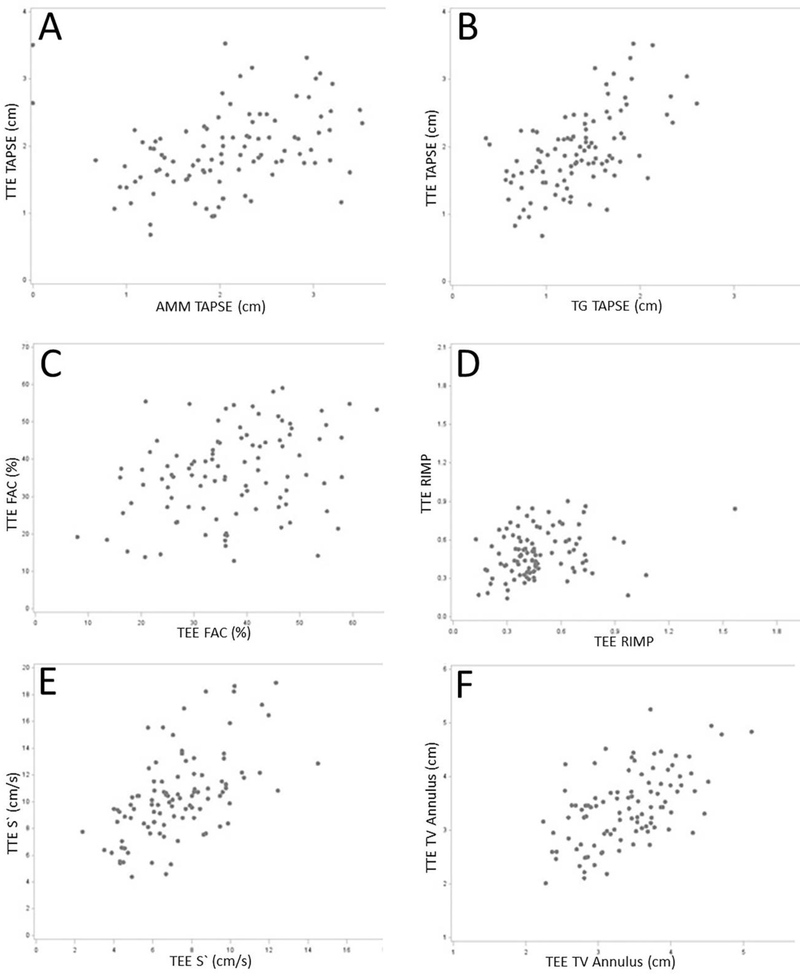
One hundred twenty six patients were consented for the study with 102 meeting inclusion criteria for data analysis. Reasons for screening failure were changes in hemodynamics >10% in 11 cases, poor TTE windows in 7 cases, no additional imaging personnel available in 4 cases, poor TEE windows in 1 case, and consent withdrawal in 1 case. The 102 patients enrolled in the study had an average heart rate of 72 bpm, and an average mean arterial pressure of 86 mmHg. Descriptive statistics were obtained for all measures of RV function (Table 2). The association between TTE and TEE for each of the measures of RV function is illustrated in Figure 3. Estimates of agreement (95% CI) between TTE and TEE were: FAC 0.31 (0.12, 0.48), S` 0.33 (0.22, 0.43), RIMP 0.13 (−0.05, 0.30), TV annular diameter 0.55 (0.40, 0.68), TG TAPSE 0.34 (0.23, 0.45), and AMM TAPSE 0.27 (0.08, 0.44) (Figure 2). Poor image quality resulted in individual images being excluded from analysis; however the remainder of the adequate images were analyzed; therefore there are discrepancies in the number of patients in Tables 2 and 3. According to the guidelines by Landis and Koch, the measures presented here indicate slight agreement for RIMP, fair agreement for AMM TAPSE, FAC, S’, and TG TAPSE, and moderate agreement for TV annular diameter. When the average differences were evaluated to determine whether TEE over- or under-estimated TTE according to the measures of RV function, our results indicate that TEE significantly underestimated TTE for S’ and TG TAPSE only (p<0.001 for each; Table 3).
Table 2.
Descriptive statistics for measurements of RV function.
| Variable | N | Mean | Std Dev | Median | Min | Max |
|---|---|---|---|---|---|---|
| TTE FAC | 101 | 36.13 | 11.58 | 35.85 | 12.82 | 59.15 |
| TEE FAC | 101 | 36.82 | 11.69 | 36.05 | 7.97 | 64.61 |
| TTE S' | 102 | 10.38 | 3.13 | 10.19 | 4.4 | 18.9 |
| TEE S' | 102 | 7.28 | 2.26 | 7.01 | 2.4 | 14.51 |
| TTE RIMP | 102 | 0.49 | 0.18 | 0.48 | 0.14 | 0.9 |
| TEE RIMP | 102 | 0.49 | 0.26 | 0.44 | 0.13 | 2 |
| TTE TV Annular Diameter | 100 | 3.41 | 0.68 | 3.42 | 2.02 | 5.26 |
| TEE TV Annular Diameter | 101 | 3.39 | 0.6 | 3.46 | 2.24 | 5.12 |
| TTE TAPSE | 102 | 1.94 | 0.58 | 1.87 | 0.68 | 3.53 |
| TEE TG TAPSE | 100 | 1.33 | 0.47 | 1.32 | 0.36 | 2.61 |
| TEE AMM TAPSE | 100 | 2.06 | 0.74 | 2.03 | 0 | 3.53 |
| HR | 102 | 72.03 | 15.93 | 70 | 40 | 120 |
| MAP | 102 | 85.66 | 16.07 | 84.5 | 50 | 130 |
Abbreviations: AMM = Anatomic M-mode; FAC = Fractional area change; RIMP = Right-sided index of myocardial performance; RV = Right ventricle; S' = Tricuspid annular systolic velocity; TAPSE = Tricuspid annular plane systolic excursion; TEE = Transesophageal echocardiography; TG = Transgastric; TTE = Transthoracic echocardiography
Figure 3:
Scatter plots illustrating the relationship between TTE (y-axis) and TEE (x-axis) for each measure of RV function: (A) AMM TAPSE; (B) Transgastric TAPSE; (C) FAC; (D) RIMP (unitless measure); (E) S’; (F) Tricuspid annulus.
Table 3.
Differences calculated as TTE minus TEE for parameters of RV function.
| Variable | N | Mean | Std Dev | Median | Min | Max | Significance |
|---|---|---|---|---|---|---|---|
| FAC | 100 | −0.79 | 13.75 | 0.07 | −39.23 | 34.66 | NS |
| S' | 102 | 3.1 | 2.61 | 2.8 | −2.09 | 9.78 | p<0.001 |
| RIMP | 102 | 0 | 0.29 | 0.03 | −1.7 | 0.49 | NS |
| TV Annulus Diameter | 99 | 0.02 | 0.6 | −0.02 | −1.35 | 1.69 | NS |
| TG TAPSE | 100 | 0.61 | 0.49 | 0.6 | −0.58 | 1.77 | p<0.001 |
| AMM TAPSE | 100 | −0.12 | 0.81 | −0.14 | −2.14 | 3.51 | NS |
Abbreviations: AMM = Anatomic M-mode; FAC = Fractional area change; RIMP = Right-sided index of myocardial performance; RV = Right ventricle; S' = Tricuspid annular systolic velocity; TAPSE = Tricuspid annular plane systolic excursion; TEE = Transesophageal echocardiography; TG = Transgastric; TTE = Transthoracic echocardiography
Discussion
The objective of our study was to assess the concordance between TTE and TEE measures of RV function. Our hypothesis was that there would be significant disagreement in TAPSE, FAC, RIMP and S’. The results largely support our hypothesis. We demonstrated that the measurements obtained were not comparable in most patients. Our results suggest that when a patient requires precise RV function assessment, it should be clear that TTE and TEE provide different imaging planes for analysis. The standards developed for chamber quantification have been done so utilizing TTE in non-anesthetized patients.4 These are clinically relevant points when assessing RV function.
Right ventricular function has been shown repeatedly to have a clinically significant impact on outcomes following cardiac surgery. Bootsma et al. first showed a clear correlation between RV ejection fraction and long term mortality after cardiac surgery ranging from 4.1% to 16.7% when the RVEF ranged from >30% to <20%, respectively.16 Similarly, severe RV dysfunction prior to orthotopic heart transplant has been shown to carry a 6-fold increased risk of death when compared to patients with normal RV function.16, 17 RV systolic dysfunction likewise carries a significant increase in mortality one year after transcatheter aortic valve replacement.18 The clinical implications of an accurate assessment of RV function extend beyond the perioperative setting. RV systolic function has strong prognostic value in multiple settings including after myocardial infarction and cardiac arrest, peripartum cardiomyopathy, heart failure with preserved ejection fraction, and pulmonary hypertension.19–23 Clearly, finding reliable methods of accurate RV functional assessment carries significant clinical importance. Quantifying right ventricular function remains a challenge given its complex three-dimensional structure. Its crescentic shape and asymmetrical nature of systolic motion pose a challenge to traditional means of functional assessment. Unlike the LV, which relies largely on symmetrical circumferential shortening, longitudinal motion is a larger contributor to RV systolic function.24 For this reason, TAPSE is an important marker of RV function but does not tell the entire story as both the free wall and interventricular septum contribute equally to systolic function.24, 25 Many clinicians rely largely on 2D and Doppler measures of RV function in daily practice. We showed in a systematic way that these measurements differ significantly between TTE and TEE. Previous studies on LV function have identified similar findings of underestimation of volumes due to foreshortening of the transesophageal imaging planes.26 Echocardiographers should exercise caution when extrapolating data validated by TTE to transesophageal studies.
Previous authors have promoted the use of the modified transgastric RV inflow view to obtain appropriate alignment for assessing inferior tricuspid annular motion.14 Our results demonstrate that, despite visually appearing to provide adequate alignment on 2D imaging, both TAPSE and S` values measured from this view consistently underestimated the transthoracic value. We surmise that, despite appearing to have adequate alignment with annular motion, this TEE view does not truly assess the motion of the annulus toward the apex. Likewise, the diaphragm limits the excursion of the inferior wall compared to the lateral wall.27 Despite the fact that this view underestimates the value, it remains clinically useful. If the TAPSE and S` values measured from the transgastric RV inflow view are greater than 1.7 cm and 9.5 cm/s respectively, the echocardiographer can be confident that these values will be within the normal range if assessed by TTE.4 Other authors have recently demonstrated improved alignment by adding anatomic M-mode to the transgastric RV inflow view.10, 11
Our results are clinically significant given that most standard measures in echocardiography have been validated only by TTE and are assumed to be applicable to those obtained by TEE. Due to the slight differences in imaging planes and the complexity of RV dynamics, echocardiographers must recognize the differences and shortcomings involved in various imaging modalities. Our study is the first to show a comprehensive disagreement in multiple measures of RV function when comparing TTE to TEE: RIMP, TAPSE by AMM, and FAC. We have, however, validated the importance of the modified transgastric RV inflow view in providing useful measurements of TAPSE and S`. Most importantly, given the trend toward underestimation, normal values of TAPSE and S` measured from this view are reliable for detection of normal, but not abnormal, RV function.
Limitations
The sample size of this study was only powered to assess agreement between measured values. We were able to show consistent underestimation of values for only transgastric TAPSE and S` by TEE. We were unable to demonstrate a similar trend for the other measures. Further large studies would be helpful in establishing cutoff values for these measures as assessed by TEE. Future studies could relate our findings to 3D analysis and RV free wall strain values, as these modalities are becoming more widespread in their clinical use.
Conclusion
When performing an assessment of RV function, transesophageal echocardiographers should exercise caution when extrapolating data validated by TTE to transesophageal studies. Measures of right ventricular function by TEE tend to have only fair agreement to TTE measurements obtained in close temporal proximity under similar hemodynamic conditions. Tricuspid annular diameter does show moderate agreement which may prove useful in cardiac surgical decision-making. Given the propensity for underestimating measurements from the modified transgastric RV inflow view, we conclude that values equal to or greater than established norms for tricuspid annular motion may be utilized to establish normal, but not abnormal, RV function.
Table 4.
Agreement between TTE and TEE assessed by concordance correlation coefficient (CCC) with 95%CI and average differences (SD and p- value) between TTE and TEE to determine over- or under-estimation.
| TTE vs. TEE |
||
|---|---|---|
| Measure of RV Function | CCC (95%CI) | Average TTE-TEE Difference (SD) p-value |
| FAC | 0.31 (0.12, 0.48) | −0.79 (13.75), p=0.57 |
| S' | 0.33 (0.22, 0.43) | 3.10 (2.61), p<0.001 |
| RIMP | 0.13 (−0.05, 0.30) | −0.00 (0.29), p=0.99 |
| TV Annular Diameter | 0.55 (0.40, 0.68) | 0.02 (0.60), p=0.70 |
| TG TAPSE | 0.34 (0.23, 0.45) | 0.61 (0.49), p<0.001 |
| AMM TAPSE | 0.27 (0.08, 0.44) | −0.12 (0.81), p=0.14 |
Abbreviations: AMM = Anatomic M-mode; FAC = Fractional area change (%); RIMP = Right-sided index of myocardial performance (unitless measure); RV = Right ventricle; S’ = Tricuspid annular systolic velocity (cm/s); TAPSE = Tricuspid annular plane systolic excursion (cm); TEE = Transesophageal echocardiography; TG = Transgastric; TTE = Transthoracic echocardiography
Acknowledgements
David Fehr, MD and Anita Malhotra, MD for their assistance in subject recruitment.
Patrick McQuillan, MD for his assistance in editing the manuscript.
Funding
RedCap Grant Support from The Penn State Clinical & Translational Research Institute, Pennsylvania State University CTSA, NIH/NCATS Grant Number UL1 TR000127 and UL1 TR002014.
Footnotes
Declarations of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bom N, Lancee CT, Honkoop J, et al. : Ultrasonic viewer for cross-sectional analyses of moving cardiac structures. Biomed Eng. 6:500–503, 505, 1971. [PubMed] [Google Scholar]
- 2.Gramiak R, Waag RC, Simon W: Cine ultrasound cardiography. Radiology. 107:175–180, 1973. [DOI] [PubMed] [Google Scholar]
- 3.Griffith JM, Henry WL: A sector scanner for real time two-dimensional echocardiography. Circulation. 49:1147–1152, 1974. [DOI] [PubMed] [Google Scholar]
- 4.Lang RM, Badano LP, Mor-Avi V, et al. : Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 28:1–39 e14, 2015. [DOI] [PubMed] [Google Scholar]
- 5.Genovese D, Mor-Avi V, Palermo C, et al. : Comparison Between Four-Chamber and Right Ventricular-Focused Views for the Quantitative Evaluation of Right Ventricular Size and Function. J Am Soc Echocardiogr. 32:484–494, 2019. [DOI] [PubMed] [Google Scholar]
- 6.Meineri M, Fassl J: The Forgotten Ventricle. J Cardiothorac Vasc Anesth. 31:1567–1569, 2017. [DOI] [PubMed] [Google Scholar]
- 7.Morita Y, Nomoto K, Fischer GW: Modified Tricuspid Annular Plane Systolic Excursion Using Transesophageal Echocardiography for Assessment of Right Ventricular Function. J Cardiothorac Vasc Anesth. 30:122–126, 2016. [DOI] [PubMed] [Google Scholar]
- 8.Naoum EE, Schofield PT, Shen T, et al. : Agreement Between Transesophageal Echocardiographic Tricuspid Annular Plane Systolic Excursion Measurement Methods in Cardiac Surgery Patients. J Cardiothorac Vasc Anesth. 33:717–724, 2019. [DOI] [PubMed] [Google Scholar]
- 9.Skinner H, Kamaruddin H, Mathew T: Tricuspid Annular Plane Systolic Excursion: Comparing Transthoracic to Transesophageal Echocardiography. J Cardiothorac Vasc Anesth. 31:590–594, 2017. [DOI] [PubMed] [Google Scholar]
- 10.Korshin A, Gronlykke L, Nilsson JC, et al. : The feasibility of tricuspid annular plane systolic excursion performed by transesophageal echocardiography throughout heart surgery and its interchangeability with transthoracic echocardiography. Int J Cardiovasc Imaging. 34:1017–1028, 2018. [DOI] [PubMed] [Google Scholar]
- 11.Flo Forner A, Hasheminejad E, Sabate S, et al. : Agreement of tricuspid annular systolic excursion measurement between transthoracic and transesophageal echocardiography in the perioperative setting. Int J Cardiovasc Imaging. 33:1385–1394, 2017. [DOI] [PubMed] [Google Scholar]
- 12.Malinowski M, Jazwiec T, Goehler M, et al. : Sonomicrometry-derived 3-dimensional geometry of the human tricuspid annulus. J Thorac Cardiovasc Surg. 157:1452–1461 e1451, 2019. [DOI] [PubMed] [Google Scholar]
- 13.Addetia K, Muraru D, Veronesi F, et al. : 3-Dimensional Echocardiographic Analysis of the Tricuspid Annulus Provides New Insights Into Tricuspid Valve Geometry and Dynamics. JACC Cardiovasc Imaging. 12:401–412, 2019. [DOI] [PubMed] [Google Scholar]
- 14.David JS, Tousignant CP, Bowry R: Tricuspid annular velocity in patients undergoing cardiac operation using transesophageal echocardiography. J Am Soc Echocardiogr. 19:329–334, 2006. [DOI] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics. 33:159–174, 1977. [PubMed] [Google Scholar]
- 16.Bootsma IT, de Lange F, Koopmans M, et al. : Right Ventricular Function After Cardiac Surgery Is a Strong Independent Predictor for Long-Term Mortality. J Cardiothorac Vasc Anesth. 31:1656–1662, 2017. [DOI] [PubMed] [Google Scholar]
- 17.Ravis E, Theron A, Mancini J, et al. : Severe right ventricular dysfunction is an independent predictor of pre- and post-transplant mortality among candidates for heart transplantation. Arch Cardiovasc Dis. 110:139–148, 2017. [DOI] [PubMed] [Google Scholar]
- 18.Ren B, Spitzer E, Geleijnse ML, et al. : Right ventricular systolic function in patients undergoing transcatheter aortic valve implantation: A systematic review and meta-analysis. Int J Cardiol. 257:40–45, 2018. [DOI] [PubMed] [Google Scholar]
- 19.Alhamshari YS, Alnabelsi T, Mulki R, et al. : Right ventricular function measured by TAPSE in obese subjects at the time of acute myocardial infarction and 2year outcomes. Int J Cardiol. 232:181–185, 2017. [DOI] [PubMed] [Google Scholar]
- 20.Ramjee V, Grossestreuer AV, Yao Y, et al. : Right ventricular dysfunction after resuscitation predicts poor outcomes in cardiac arrest patients independent of left ventricular function. Resuscitation. 96:186–191, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blauwet LA, Delgado-Montero A, Ryo K, et al. : Right Ventricular Function in Peripartum Cardiomyopathy at Presentation Is Associated With Subsequent Left Ventricular Recovery and Clinical Outcomes. Circ Heart Fail. 9, 2016. [DOI] [PubMed] [Google Scholar]
- 22.Guazzi M, Dixon D, Labate V, et al. : RV Contractile Function and its Coupling to Pulmonary Circulation in Heart Failure With Preserved Ejection Fraction: Stratification of Clinical Phenotypes and Outcomes. JACC Cardiovasc Imaging. 10:1211–1221, 2017. [DOI] [PubMed] [Google Scholar]
- 23.Sano H, Tanaka H, Motoji Y, et al. : Right ventricular function and right-heart echocardiographic response to therapy predict long-term outcome in patients with pulmonary hypertension. Can J Cardiol. 31:529–536, 2015. [DOI] [PubMed] [Google Scholar]
- 24.Tan TC, Dudzinski DM, Hung J, et al. : Peri-operative assessment of right heart function: role of echocardiography. Eur J Clin Invest. 45:755–766, 2015. [DOI] [PubMed] [Google Scholar]
- 25.Kaul S, Tei C, Hopkins JM, et al. : Assessment of Right Ventricular-Function Using Two-Dimensional Echocardiography. American Heart Journal. 107:526–531, 1984. [DOI] [PubMed] [Google Scholar]
- 26.Smith MD, MacPhail B, Harrison MR, et al. : Value and limitations of transesophageal echocardiography in determination of left ventricular volumes and ejection fraction. Journal of the American College of Cardiology. 19:1213–1222, 1992. [DOI] [PubMed] [Google Scholar]
- 27.Dreyfus J, Durand-Viel G, Raffoul R, et al. : Comparison of 2-Dimensional, 3-Dimensional, and Surgical Measurements of the Tricuspid Annulus Size: Clinical Implications. Circ Cardiovasc Imaging. 8:e003241, 2015. [DOI] [PubMed] [Google Scholar]