Abstract
Fecal testing is a common component of most gastrointestinal work-ups. A multitude of diagnostic techniques are available for identifying parasites and pathogens, or showing abnormalities of flora. Optimal fecal assessment involves careful formulation of a differential list based on signalment, history, and clinical signs. Tests should be selected and interpreted based on their relative sensitivity and specificity for specific conditions. It is essential to use effective testing methods for the etiologies of concern. This article reviews the plethora of diagnostic techniques available for fecal assessment. Indications, limitations, and issues of specimen handling for each technique are discussed. The optimal approach to the diagnosis of some common parasites, pathogens, abnormalities of flora, and metabolic conditions are covered.
Fecal testing by flotation is a common component of most gastrointestinal (GI) work-ups. However, options for fecal testing go far beyond the traditional flotation for parasite ova. A multitude of diagnostic techniques are available for identifying parasites and pathogens, or showing abnormalities of flora. Optimal fecal assessment involves careful formulation of a differential list based on signalment, history, and clinical signs. Tests should be selected and interpreted based on their relative sensitivity and specificity for specific conditions. It is essential to use effective testing methods for the etiologies of concern.
This article reviews the plethora of diagnostic techniques available for fecal assessment. Indications, limitations, and issues of specimen handling for each technique are discussed. The optimal approach to the diagnosis of some common parasites, pathogens, abnormalities of flora, and metabolic conditions will be covered.
Sample collection, handling, and storage
Fecal sample collection, handling, and storage can highly affect the success of laboratory diagnosis. Different diagnostic techniques are optimized or compromised by different approaches. Have a diagnostic plan before collecting feces to optimize collection, handling, and storage.1
Timing
Feces begin to change after a stool is passed. Cellular infiltrates degenerate and become difficult to identify. Fragile organisms, such as Giardia and trichomonads, deteriorate rapidly with time, refrigeration, or processing. Feces that are not fresh (ie, <5 minutes) are useless for the detection of these organisms.2, 3 Nematode eggs will develop further or hatch, making them more difficult to identify. Hookworm eggs tend to hatch within 24 hours in warm humid weather, giving rise to motile larvae. Toxascaris eggs become embryonated within a few days in old feces.2 The bacterial flora to changes, leading to overgrowth and sporulation of some species.
Sample collection
Whenever possible, obtain fresh fecal samples at examination. This process avoids many potential problems. When owners collect feces, one must question the usefulness of the sample. Is it feces? Did it come from the right animal? How old is it? Where has it been? How was it stored?2
Several techniques are available, which make collection of fresh feces at examination possible. Feces can often be collected during digital rectal examination. Fecal loops are also available for animals in which digital collection is impossible or unsuccessful. Rectal lavage with saline is a reliable method of obtaining fresh samples.2 For rectal lavage with saline, use a number 8F red rubber catheter and 6 to 12 mL of saline in a syringe. Lubricate the catheter with a small amount of water-based lubricant. The catheter is passed through the anus and 5 to 10 cm into the rectum or colon. Once the catheter is in place, infuse and aspirate the saline multiple times to achieve a sample with mud-like consistency. The sample may be placed directly on slides for cytology or in a sterile, red top tube for other diagnostic tests.
Rectal lavage will obtain a sample containing relatively more mucous secretions from the mucosal surface and less fecal matter. This will affect the character of the sample. Motile protozoa and bacteria are more prevalent at the mucosal surface, and will be more prevalent in flush samples. Eggs and cysts are more prevalent in fecal material, and may be less prevalent in flush samples. Rectal lavage is ideal for cytology but may provide an inadequate amount of feces for some techniques.1, 4, 5 Concentration techniques, such as fecal flotation and sedimentation, require larger samples. When larger samples are required, it is necessary to collect voided feces. Defecation should occur in a clean area, followed by immediate recovery and proper storage.1, 4
Sample quantity
An adequate quantity of feces should be examined. Whenever possible, 1 to 2 g of feces should be examined for fecal flotation or sedimentation. Ideally, 2 to 3 g of feces should be submitted for fecal culture panels. For the Baermann technique, submit 5 to 10 g of feces.1, 4 For visualization purposes, 1 g of feces is approximately 1/4 teaspoon.
Storage and transport
For most fecal tests, appropriate storage methods are available. Cytology preparations may be fixed in ethanol or stained with preservative stains. Refrigeration adequately stabilizes feces up to 24 hours for flotation or sedimentation procedures. Formalin fixation can preserve feces for longer periods for flotation and/or sedimentation. Freezing will preserve feces for antigen detection methods. Special transport media are available for fecal culture panels.1, 4, 5
Laboratory diagnostic procedures
Indications and limitations of the more common tests will be described. Unique issues of fecal collection, handling, and storage for these tests will be discussed. Discussion of laboratory methodology, including morphologic identification of parasites and pathogens is beyond the scope of this article. Veterinary reference textbooks are available for this purpose.1, 6, 7, 8
Fecal cytology (wet mount)
Fecal wet mounts are particularly helpful for identification of motile organisms. Because of the small sample used, the sensitivity of this method is low for most other parasites. Protozoal trophozoites such as Giardia, trichomonads, and amoebae may be identified, as well as motile nematode larvae (eg, Strongyloides sp). Motile bacteria, such as Campylobacter, may be easier to detect on wet mounts than on dry mounts.1
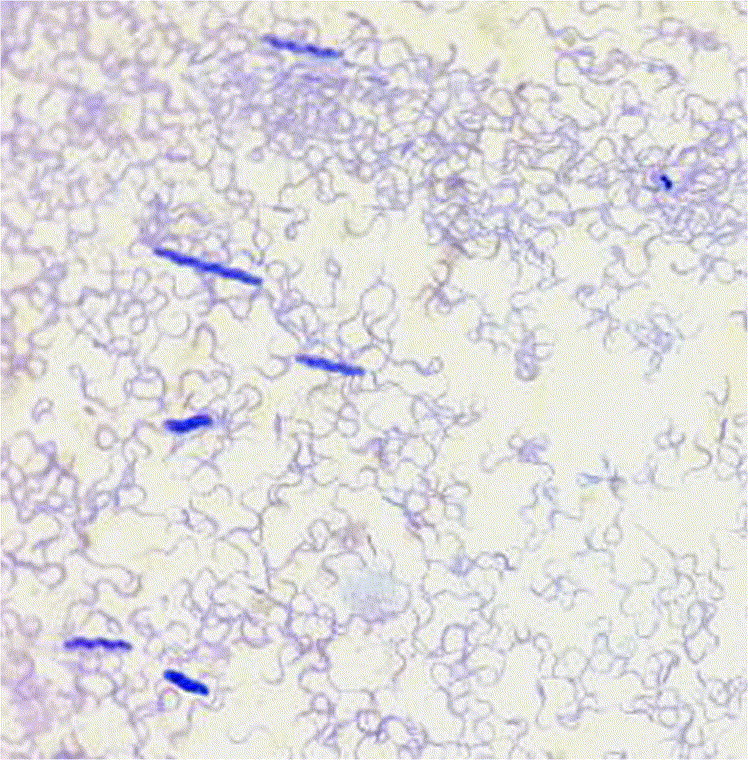
It is necessary to be familiar with the nonpathogenic motile flora of feces. Motile treponeme-like spirochetes are often seen on wet mounts. They are stiff, corkscrew-shaped, forwardly motile organisms (Fig 1). Increased numbers are often noted with diarrhea or on fecal samples obtained by rectal lavage. They are not considered pathogenic. Increased numbers are usually a result of diarrhea or sampling methods (see Spirochetal Diarrhea section).9 Trichomonads, such as Pentatrichomonas hominis, are generally considered nonpathogenic in dogs. However, disease associated with Tritrichomonas foetus has been described in cats (see Trichomoniasis section) (Fig 2). 10
Fig 1.
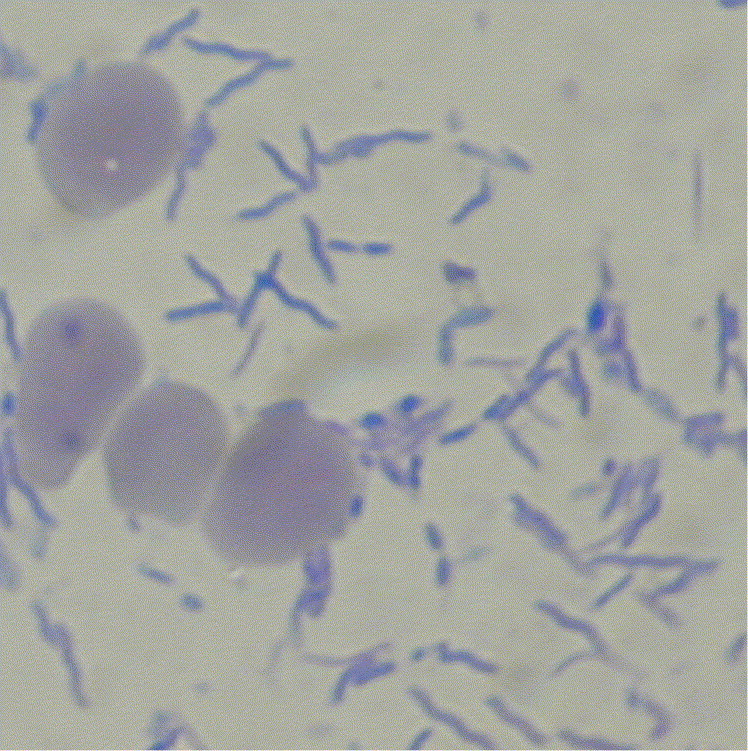
Treponeme-like spiral organisms on fecal cytology stained with Diff-Quik. Red blood cells show the size of the organisms. (Provided by Dr. J. Michael Harter.28)
Fig 2.
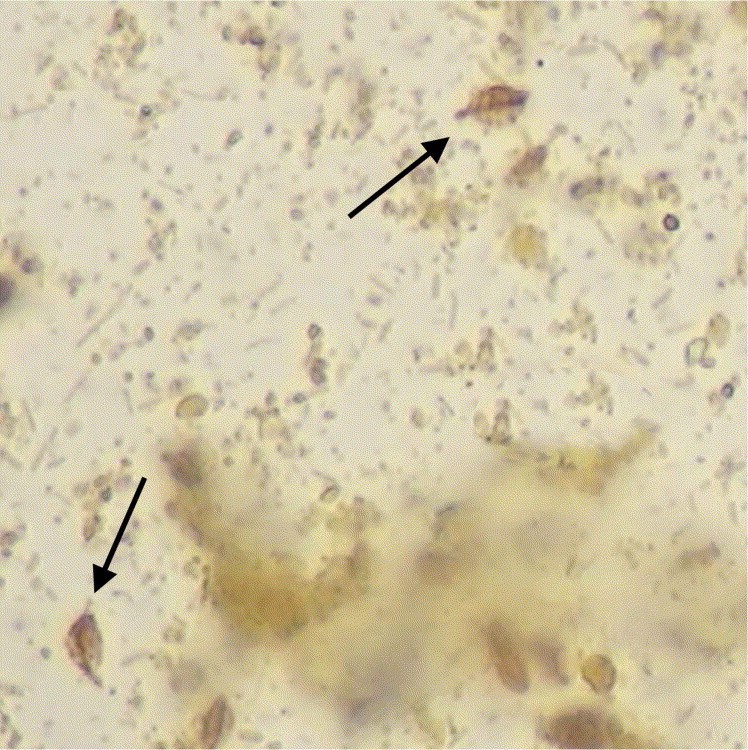
Tritrichomonas foetus trophozoites (see arrows) on wet mount cytology stained with iodine.
Direct smears should be performed on fresh feces, ideally less than 5-minutes old.1, 3, 10 Use warm or room temperature physiologic saline. For solid feces, place a very small sample into a drop of saline on the slide, and mix with a wooden applicator stick. For samples obtained by rectal lavage, simply place a drop of the lavage fluid on the slide. Place a cover glass over the drop. The wet mount should be thin enough to read newsprint through it. Too much feces will make a dense mixture that cannot be assessed. When examining the slide, adjust the contrast to see the minute aspects of the specimen.1 Scan the entire slide at low magnification (ie, 10×) for eggs, cysts, and larvae. Trophozoites are generally identified at 20× and 40× magnification, while motile bacteria may be assessed 100x under oil emersion.1 After initial examination, iodine may be wicked under an edge of the cover glass to stain organisms. Iodine will kill motile organisms but may aid in their identification. Motile organisms seen on wet mount can often be structurally assessed on stained, dry mount slides.1 Wet mount slides should not be sent to pathologists because they will rapidly dry and become unreadable. Instead, send dry mounts with a clear description of your findings on the wet mount.5
Fecal cytology (dry mount)
Dry mounts are particularly useful for identification of cellular infiltrates and assessing the bacterial flora. Increased numbers of neutrophils (Fig 3) can be a sign of bacterial enteritis. The absence of fecal neutrophils in a puppy with hemorrhagic diarrhea may be a sign of viral enteritis. Increased numbers of clostridial spores or yeast may be a sign of overgrowth.9 Pathogenic spiral bacteria, such as Campylobacter, may be identified (Fig 4). Rarely, coccidial merozoites or other protozoal trophozoites are seen.1
Fig 3.
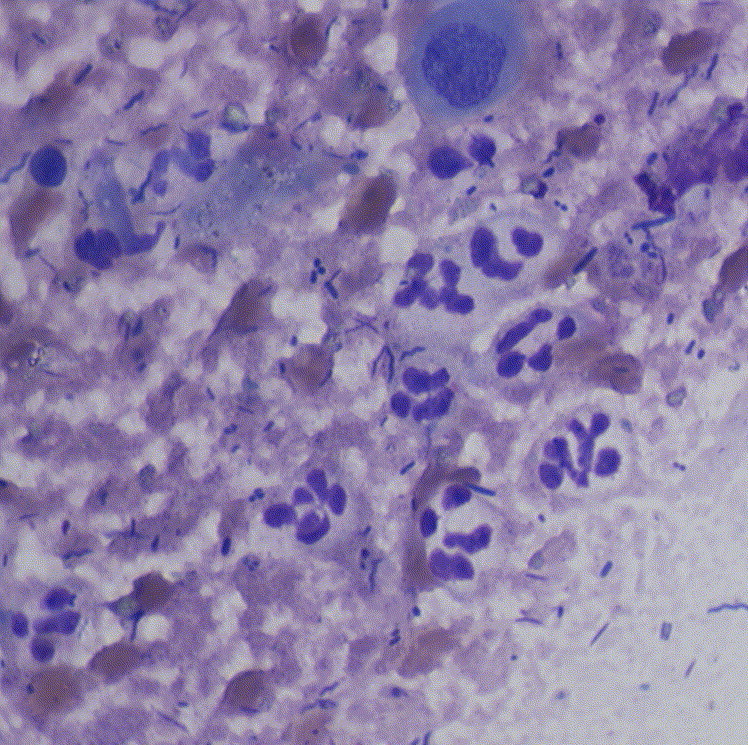
Leukocytes on Diff-Quik stained fecal cytology.
Fig 4.
Campylobacter-like organisms on fecal cytology stained with Diff-Quik.
It is important to be familiar with the microscopic appearance of normal flora. Not all spores are Clostridium perfringens (Fig. 5), and not all spiral bacteria are Campylobacter.9 At least 2 forms of spirochetes, treponeme-like organisms and Serpulina-like organisms, may be confused with Campylobacter on dry mounts Fig 1, Fig 4, Fig 6. The pitfalls of identification of these organisms are addressed later (see Campylobacteriosis, Clostridial Colitis, Spirochetal Diarrhea sections).9
Fig 5.
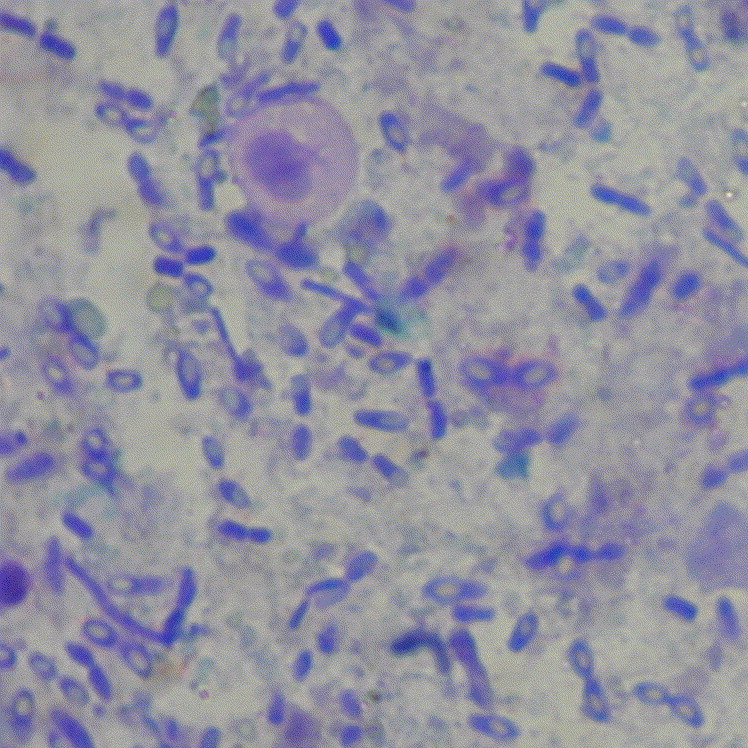
Clostridium perfringes-like spores throughout Diff-Quik stained fecal cytology. (Provided by Dr. J. Michael Harter.28)
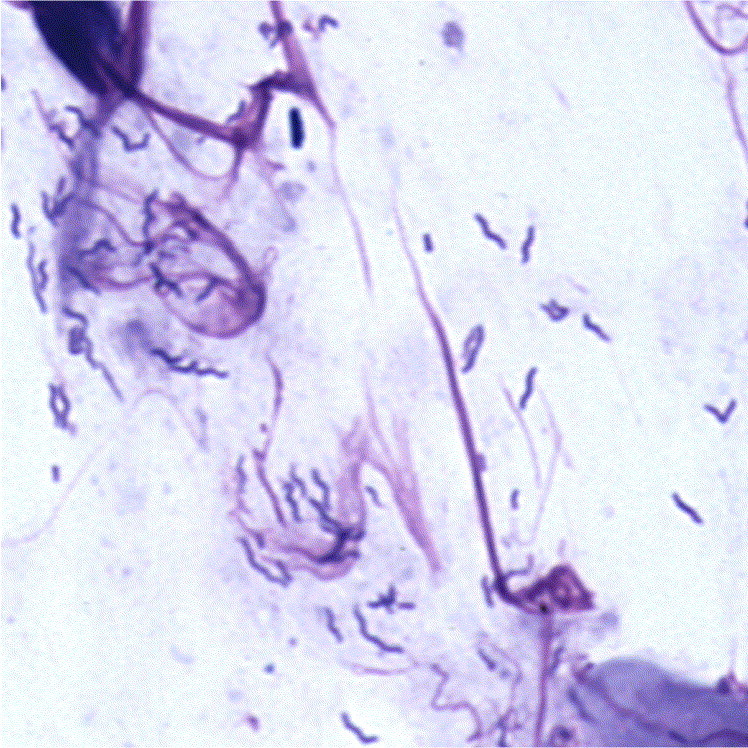
Fig 6.
Serpulina-like spiral organisms throughout Diff-Quik stained fecal cytology. A few, darker staining treponeme-like organisms are also seen. (Provided by Dr. J. Michael Harter.28)
The diagnostic quality of dry mounts is dependent on optimal sample handling and slide preparation, especially when assessing cellular infiltrates. Prepare the slide with a very small amount of fresh feces. It is a common mistake to make fecal smears too thick. Thick areas do not stain well and tend to fall off during processing. Solid feces should be mixed with saline, as discussed in “Wet Mounts” section, or a drop of rectal lavage fluid may be placed directly on the slide.1, 5 The sample should be spread thinly and evenly across the slide, using the same smearing technique as preparing blood smears. The slide should be air-dried, not heat fixed, to preserve cellular morphology. Stain the slide with wright-Giemsa or Diff-Quik (Hamilton Thorne Biosciences, Beverly, MA). If necessary, a portable hair dryer can be used to speed the drying process.5 Scan the entire slide at low magnification. Cellular morphology and bacteria are best assessed at 100× magnification under oil. Consider special stains based on initial fecal cytology and the clinical presentation. For better bacterial morphology, consider Gram stain. If there is a clinical suspicion of cryptosporidiosis, consider acid-fast stain. Slides that are to be preserved for later reexamination may be fixed with methanol for later staining or processed with a fixative stain, such as merthiolate iodine-formalin.1, 5
When sending fecal cytology to a pathologist, consider the following recommendations:
-
1.
Send at least 2 well prepared, unstained slides.
-
2.
For special stains, send an additional 2 slides for each stain requested.
-
3.
The slides should be air dried and then fixed for approximately 3 seconds in 70% to 100% methanol.
-
4.
Save at least 1 slide at the practice to be reviewed when the results are reported. This slide can also serve as a backup in case there are problems at the laboratory.
-
5.
Use slides with frosted ends to identify the correct side.
-
6.
Permanently mark all slides with the date and patient identification.
-
7.
Provide a good history, including signalment, clinical signs, and issues of sample handling. If you have a clinical suspicion of a particular organism, tell the pathologist because special stains may be recommended.5
Fecal flotation
Fecal flotation is the optimal procedure for diagnosis of most, but not all, intestinal parasites. Flotation techniques take advantage of the fact that parasite ova and cysts can be separated from other fecal debris due to differences in density. Eggs, oocysts, and larvae are usually less dense than flotation solutions, and, therefore, will rise to the surface of the mixture. This method of concentrating parasites allows a larger, more representative sample of feces to be assessed.2 The efficiency of fecal flotation is dependent on the quality of the sample, type of solution, the specific gravity, and the timing of the procedure.1
Several techniques for fecal flotation are described and used in clinical practice. Techniques vary based on the type of flotation solution and the method of concentration (ie, standing or centrifugal). Solutions used for flotation include sugar (Sheather solution), magnesium sulfate (35%), zinc sulfate (33%), and sodium chloride.1, 2 Sugar solution is considered ideal for isolation of most eggs and oocysts. It has the advantage of not crystallizing and can, therefore, be assessed for a longer period. Sugar solution also will not distort most helminth eggs and oocysts. However, sugar solutions tend to distort Giardia, other protozoal cysts, and some lungworm larvae. Zinc sulfate is considered ideal for the isolation of Giardia cysts but will distort most helminth eggs. Flotation solutions must be maintained at the proper specific gravity to be effective.1, 2
Centrifugal flotation methods reduce the time that it takes for eggs to float to the surface. This is particularly important with sugar solutions, which have higher viscosity and would require longer standing time. When using standing flotation methods, it is best to use a salt solution (ie, zinc sulfate or sodium nitrate), and let the preparation stand at least 10 to 15 minutes. Adequate flotation time is essential.1 Centrifugal flotation using the Sheather sugar method is the gold standard of veterinary parasitology and is strongly recommended for routine use in practice. This is the most effective method of isolating most helminth eggs and coccidial oocysts.1 Centrifugal flotation using zinc sulfate is considered ideal for the isolation of Giardia cysts.1, 2
Fecal flotation should be performed on 1 to 2 g of fresh feces. Fecal samples submitted to laboratories should be stored at 2° to 8°C and shipped on ice within 24 hours. Formalin fixation can preserve fecal samples for flotation for longer periods.1
Fecal sedimentation
Sedimentation techniques are used for the detection of fluke eggs and embryonated nematode eggs, such as Physaloptera spp and Spirocerca lupi. Fluke eggs and embryonated nematode eggs are more dense, and do not float on standard flotation media. Sedimentation solutions include water, soap-in-water, or saline. Use saline for sedimentation of fluke eggs because they tend to hatch in water.1 Sedimentation methods may be centrifugal or standing. As with fecal flotation, centrifugal techniques decrease the required time for sedimentation. Fecal sedimentation should be performed on 1 to 2 g of fresh feces. Fecal samples submitted to laboratories should be stored at 2° to 8°C and shipped on ice within 24 hours.1, 4
Baermann funnel preparation
This is a method for isolation of nematode larvae from fecal specimens. It is best suited for isolation of active lungworm larvae (ie, Aelurostrongylus and Filaroides) and small intestinal larvae (ie, Strongyloides). The eggs of hookworms (ie, Ancylostoma and Uncinaria) can hatch in fresh fecal samples, yielding active larvae.1, 2 Some lungworms, Capillaria sp, are more readily diagnosed on fecal floatation. Lung flukes are more readily identified on fecal sedimentation.11 For this reason, fecal assessment for pulmonary disease may include the Baermann technique, as well as floatation and sedimentation techniques. Baermann funnel preparation must be performed on fresh feces, and 5 to 10 g of feces are required. Samples submitted to laboratories should be stored at 2° to 8°C and shipped on ice within 24 hours.1, 4
Bacterial culture
Primary bacterial gastroenteritis occasionally occurs in dogs and cats. Salmonella spp, Campylobacter spp, C perfringens, and Escherichia coli are important genera.3 Because latent carriers of enteric pathogens are common, the diagnosis of bacterial enteritis must be based on clinical presentation as well as organism isolation.12 Positive cultures for enteric pathogens are commonly reported in normal dogs with C perfringens, Salmonella spp, or Campylobacter jejuni.3, 12, 13
If possible, collect 2 to 5 g of fresh feces from the rectum. If a voided sample is used, avoid contamination with urine or soil. Because of the small sample size, do not submit rectal swabs in transport media or culturettes. The sample should be placed in a sterile container, stored at 2° to 8°C, and shipped on ice to the reference laboratory within 24 hours.4 Transport media, such as Para-Pak C&S (Meridian Bioscience, Inc, Cincinnati, OH), are commonly used when processing will be delayed. They also are used to maintain the viability of fastidious organisms such as Campylobacter.4 Because enteric pathogens have special culture requirements, always request a fecal culture panel or notify the laboratory of suspected pathogens. Standard culture procedures are not useful for fecal assessment.3, 4
Semiquantitative and quantitative fecal fat
Semiquantitative fecal fat analysis is an easily performed, inexpensive screening test used to detect fat malabsorption (positive for digested fat) or maldigestion (positive for undigested fat). It does occasionally yield misleading results. Quantitative fat analysis is labor intensive. It requires a dietary prescription for 3 days followed by collection of all feces for 24 to 72 hours. Feces are refrigerated or frozen while awaiting analysis. The entire collection of feces is submitted to the laboratory. This test is rarely performed in veterinary medicine.3, 4
A moderate-to-high fat diet is necessary to assess fecal fat. Feeding low-fat diets may cause the test to be negative.3 Samples must be submitted in a container free of fat, wax, or soap. For semiquantitative analysis, submit 1 to 2 g of fresh feces, stored at 2° to 8°C, and shipped on ice within 24 hours.4
Fecal tests for maldigestion
Fecal starch, fecal muscle fibers, and fecal proteolytic activity (fecal trypsin) are tests for maldigestion. These tests offer no advantage over serum trypsin-like immunoreactivity (TLI) in the diagnosis of exocrine pancreatic insufficiency (EPI) and lack specificity. For this reason, they have largely been replaced by serum TLI and are not recommended.3
Fecal antigen detection methods
Organism specific assays using enzyme-linked immunosorbent assay (ELISA) or immunofluorescent assay methods are available for some parasites, viruses, and bacterial enterotoxins. ELISA tests for Giardia and Cryptosporidium antigen are available at most reference laboratories and can be performed as an in-house assay.3 They are a reasonable alternative to special flotation techniques and achieve a similar level of diagnostic sensitivity.14 Effective fecal antigen screens for Parvovirus are available as bench top kits. Antigen assays for enterotoxins of C perfringens and Clostridium difficile are also available.3
All antigen detection methods require fresh feces. Samples may be placed in a sterile container and refrigerated at 2° to 8°C for up to 48 hours, or frozen for longer storage. Samples should be shipped on ice. Some antigen tests may be performed on feces preserved in formalin. The improper handling of feces can lead to false-negative results.3, 4
Fecal occult blood
Fecal occult blood tests are used to detect bleeding that is not grossly apparent. Multiple assays are available, and sensitivity varies markedly between assays. To avoid false-positives, the patient must be on a meat-free diet for at least 3 days before the feces are obtained. Diets containing hemoglobin from meat or peroxidases from uncooked vegetables can cause false-positive results. Tests performed on 3 or more bowel movements may help to avoid false-negative results. Avoid manual stool collection to prevent iatrogenic blood contamination. Fecal occult blood screening should be performed on fresh, voided feces. Samples submitted to laboratories should be stored at 2° to 8°C and shipped on ice within 4 days.3, 4
α-1 protease inhibitor (α-1 PI)
Fecal α-1 PI levels are useful for the assessment of hypoproteinemia of uncertain cause. It is a qualitative and quantitative measure of GI protein loss. As gastrointestinal protein loss can vary, the assessment of multiple fecal samples is necessary. Three, 1-g fecal samples from 3 different bowel movements should be obtained from freshly voided stools. Avoid manual stool collection to prevent iatrogenic blood contamination. Samples are placed in tubes provided by the laboratory, frozen, and shipped on a cold pack. Proper sample handling is essential to avoid false-positive or false-negative results.15
Fecal diagnosis of parasites and pathogens
Fecal testing is an essential part of the diagnosis of many etiologies. In this section, indications for the diagnostic work-up of these etiologies are discussed. Available laboratory diagnostics, and their relative efficacy for specific parasites and pathogens are considered. Prophylactic treatment is often an important part of the diagnostic approach. However, discussion of therapeutics is beyond the scope of this article.
Nematodes
Stomach worms
Etiology
Stomach worms include Physaloptera spp, the large stomach worm of dogs and cats (4 to 5 cm), and Ollulanus tricuspis, the small stomach worm of cats (0.7 to 0.9 cm).
Clinical signs
These worms are likely to cause vomiting. Other signs include anorexia, melena, and anemia, with heavy infestations.
Diagnostic indications
(1) Acute or chronic vomiting and (2) exposure to catteries or kennels.
Diagnosis
Stomach worms are rarely identified by standard fecal flotation methods. Physaloptera spp produce embryonated eggs, which are more dense than most nematode eggs and do not float in most concentration solutions. Diagnosis is usually made by fecal sedimentation methods, identification of adult larvae in vomitus, or on endoscopic evaluation of the stomach. O tricuspis produce microscopic larvae, which appear only in vomitus. Larvae that pass into the intestinal tract are digested. Diagnosis is usually made using Baermann concentration of vomitus or gastric lavage solution, or on the histopathologic assessment of gastric mucosa. In all patients presenting with acute or chronic vomiting, consider testing by fecal sedimentation and treating with an effective anthelmintic to exclude stomach worms.16, 17
Esophageal worms
Etiology and occurrence
S lupi occurs primarily in tropical regions of the southern United States.
Clinical signs
It is a rare cause of regurgitation and esophageal pathology in dogs. Vomiting may occur due to gastric spread.
Diagnostic indications
(1) Regurgitation or vomiting; (2) esophageal nodules, or fibrosarcoma; (3) gastric nodules; and (4) tropical and/or subtropical environment.
Diagnosis
Spirocerca are spirurid nematodes similar to large stomach worms, Physaloptera, and produce high density, embryonated eggs. Diagnosis is made by identification of embryonated eggs on fecal sedimentation, or observation of nodules produced by encysted larvae on esophagoscopy or gastroscopy.16, 17
Ascarids
Etiology and occurrence
Ascarids of clinical significance include Toxocara canis in dogs, and Toxascaris leonina and Toxocara cati in cats.
Clinical signs
Ascarid infestation leads to clinical symptoms primarily in puppies and kittens. Clinical signs most often include a pot-bellied appearance, poor weight gain, vomiting, diarrhea, and, occasionally, cough associated with larval migration through the respiratory tract. Most adults with ascarid infestation are asymptomatic.
Diagnostic indications
(1) GI symptoms, (2) young animals, and (3) screening for zoonosis.
Diagnosis
Ascarids eggs are readily identified on fecal flotation. Adults are occasionally seen in vomitus or feces.
Public health concerns
Periodic screening of dogs and cats for ascarid infestation is recommended due to the potential for visceral larval migrans or ocular larval migrans in humans.16, 17
Hookworms
Etiology and occurrence
Hookworms of clinical significance include Ancylostoma caninum in dogs, Ancylostoma tubaeforme in cats, and Uncinaria stenocephala in dogs and cats.
Clinical signs
Hookworm infestation is usually unapparent in adults. In puppies and kittens, anemia, hypoproteinemia, diarrhea, and poor weight gain are common. Soft cough from verminous pneumonitis can occur in association with somatic migration of A caninum larvae.
Diagnostic indications
(1) Anemia, hypoproteinemia; (2) GI symptoms; (3) young animals; and (4) screening for zoonosis.
Diagnosis
Hookworms produce large amounts of eggs and are readily diagnosed by standard fecal floatation methods.
Public health significance
Hookworm larvae can penetrate human skin. As they migrate under the skin, they cause a dermatitis called cutaneous larval migrans.16, 17
Strongyloidosis (thread worms)
Etiology and occurrence
Strongyloides spp are nematodes that occur worldwide, and are most prevalent in tropical and subtropical countries, including the southern United States. They most commonly affect dogs and humans, and, less frequently, cats.
Clinical signs
Larval migration through the lungs may cause coughing. Pododermatitis may be associated with larval penetration of the footpads. Enteritis is rare and is usually seen in young animals. Diarrhea may be watery, and contain mucous and blood.
Diagnostic indications
(1) Cough, (2) pododermatitis, (3) diarrhea in young animals, (4) tropical and subtropical location, and (5) screening for zoonosis.
Diagnosis
Larvae may be observed on Baermann technique. Embryonated eggs may be observed on direct smear of fresh feces.
Public health significance
Human strongyloidiasis is caused by Strongyloides stercoralis. Humans are the major source of infection for dogs and cats. Infected pets can transmit the disease to humans.16, 17
Whipworms
Etiology, occurrence, and clinical signs
Whipworm (Trichuris vulpis) infestation is a common cause of colitis, like signs in dogs and, occasionally, cats. Bouts of diarrhea, often with large amounts of mucus and blood on the stool, are seen in heavy infections. Occasionally, whipworm infestation leads to an abnormality of serum sodium and potassium known as pseudoaddison syndrome.
Diagnostic indications
(1) Colitis and (2) pseudoaddison syndrome.
Diagnosis
Standard, fecal floatation methods are optimal for the concentration and detection of their eggs. However, whipworms produce eggs intermittently and in low numbers. In patients with large bowel signs, exclude whipworms by testing at least 3 fecal samples and treating with an effective broad-spectrum anthelmintic.16, 17
Trematodes (flukes)
Intestinal flukes
Etiology and occurrence
Nanophyetus salmincola, the salmon poisoning fluke, occurs in the northwest United States, southwest Canada, and Siberia. Alaria spp are intestinal flukes with worldwide distribution. Many nonpathogenic intestinal flukes are reported throughout the world. Definitive hosts are dogs, cats, and wild carnivores. These inhabit the small intestine.
Clinical signs
Large infestations of intestinal flukes can cause diarrhea. N salmincola harbors and transmits the rickettsia, Neorickettsia helminthoeca, which is the causative agent of salmon poisoning. Signs of salmon poisoning include hemorrhagic enteritis and lymphadenopathy.
Diagnostic indications
(1) Signs consistent with salmon poisoning, (2) diarrhea, and (3) northern Pacific region for N salmincola.
Diagnosis
Eggs may be identified in feces after concentration with fecal sedimentation. Clinical signs consistent with salmon poisoning support a presumptive diagnosis of N salmincola.14, 16, 17
Biliary and pancreatic flukes
Etiology and occurrence
Platynosonum fastosum occurs in the bile duct of cats and, rarely, dogs in the southern United States, Caribbean Islands, South America, and Africa. Eurytrema procyonis is the pancreatic fluke of cats. Metorchis albidus and Metorchis conjunctus are found in the bile ducts and gall bladder of dogs, cats, and other carnivores in North America, Europe, and Asia.
Clinical signs
Light infections are usually asymptomatic. Heavy infections with P fastosum may cause so-called “lizard poisoning” syndrome in cats. This is characterized by diarrhea, vomiting, anorexia, and icterus.
Diagnostic indications
(1) Signs of biliary obstruction, (2) GI signs, and (3) tropical or subtropical region.
Diagnosis
Eggs may be identified in feces, usually by fecal sedimentation.16, 17
Cestodes (tapeworms)
Tapeworms
Etiology and occurrence
Diphylidium caninum is the most common tapeworm of dogs and cats. Other common tapeworms include Taenia taeniaeformis in cats and Taenia pisiformis in dogs. Some tapeworms, such as Echinococcus sp and Mesocestoides sp, are rare but have public health significance because humans or other domestic animals acting as intermediate hosts may have extraintestinal cyst formation.
Clinical signs
Tapeworms generally do not cause clinical disease.
Diagnostic indications
(1) Proglottids noted on feces or pet and (2) screening for zoonosis.
Diagnosis
Tapeworms are generally diagnosed by identification of proglottids on the feces or eggs on fecal flotation. D caninum produces egg packets.
Public health significance
Humans are infected as intermediate hosts by ingesting the eggs of some species.16, 17
Protozoa
Coccidiosis
Etiology and occurrence
Species of Isospora have been associated with a subclinical infection or an enteritis of varying severity, particularly in puppies and kittens.
Clinical signs
Overcrowding, poor sanitation, inadequate nutrition, impaired immunity, and other stresses predispose to clinical coccidiosis. Clinical signs include intermittent diarrhea with hematochezia.
Diagnostic indications
(1) Diarrhea, (2) young animal, and (3) multi-pet environments.
Diagnosis
Showing of large numbers of oocysts on fecal flotation or direct smear is suggestive of clinical disease. Clinical coccidiosis is unlikely when low numbers are seen in adult, immune competent patients.14, 16, 17
Giardiasis
Etiology and occurrence
Giardiasis is a protozoal intestinal infection of humans and many domestic animals, which occurs worldwide. The cause is Giardia duodenalis. This flagellated protozoan (trophozoite) inhabits the lumen of the small intestine where it produces microscopic lesions on villi.
Clinical signs
Infections in adult dogs and cats are usually subclinical, but clinical disease is also seen. The subclinical carrier rate varies from approximately 2% to 10%. Acute and chronic diarrhea occurs mainly in kittens and puppies. Infestation with large numbers of organisms interferes with digestion and assimilation. Signs include soft to diarrheic stools, poor hair coat, flatulence, and weight loss.
Diagnostic indications
(1) Acute or chronic diarrhea, (2) immune compromise, (3) young animals, and (4) screening for zoonosis.
Diagnosis
Identification of cysts on centrifugal zinc sulfate flotation is considered the gold standard for diagnosis. Cysts are shed intermittently, so examination of feces from 3 nonconsecutive stools over 6 to 10 days is necessary for adequate sensitivity.11 Store samples at 2° to 8°C or in preservative solution (ie, formalin). Samples may be mixed for analysis to save money. An ELISA is used to detect antigen in feces. The assessment of a single stool sample approaches but is not higher than the diagnostic sensitivity of 3 zinc sulfate floats. Similar indirect immunofluorescence assays are also available. Motile flagellated trophozoites may be detected on wet mount cytology of fresh feces (<5 minutes) or duodenal fluid. Sensitivity of this method is low because trophozoites are intermittently shed, and only a small amount of feces is examined. Giardia may be confused with other motile trophozoites, such as trichomonads. However, they may be identified by their characteristic bouncing motion. Addition of iodine to the wet mount may aid in the observation of characteristic internal structures.
Public health significance
Giardia is the most common intestinal parasite affecting humans in North America. It is uncertain whether cross infection occurs between humans and domestic animals. It is prudent to regard Giardia-infected pets as a potential source of human infection.14, 16, 17
Cryptosporidiosis
Etiology and occurrence
This is a widespread, worldwide infection of humans and domestic animals caused by the coccidian parasite Cryptosporidium parvum.
Clinical signs
Clinical disease is rare in dogs and cats. When it occurs, there may be predisposing factors (eg, feline leukemia virus or feline immunodeficiency virus infection) or immunosuppression. Kittens and puppies are most susceptible. Both the small intestine and colon are affected. Diarrhea is usually mild but can be severe.
Diagnostic indications
(1) Diarrhea; (2) young animals; (3) immune compromise (eg, feline leukemia virus, feline immunodeficiency virus); and (4) screening for zoonosis.
Diagnosis
Fecal floatation using sucrose or zinc sulfate solutions is useful for concentrating organisms. Because the oocysts are shed intermittently, repeated sampling may be necessary. ELISA and immunofluorescent assay tests are available for detection of Cryptosporidium antigen in feces. Heat-fixed fecal smears are stained by the acid-fast technique. The small oocysts (ie, 4 to 8 um) stain red.
Public health significance
The feces of infected dogs and cats can infect humans. Although the disease in humans is usually subclinical, immunocompromised patients can be severely affected.14, 16, 17
Trichomoniasis
Etiology and occurrence
P hominis is a nonpathogenic resident of the colon of mammals, including humans, dogs, and cats. Although numbers may be increased with diarrhea, it is not considered pathogenic. T foetus has recently been described as a pathogen in cats with chronic diarrhea. This is the same organism that has previously been described as a vaginal pathogen in cattle and nasal pathogen in pigs. T foetus affects mostly kittens with a history of exposure to shelters or catteries.10
Clinical signs
Tritrichomonas is associated with chronic large and small bowel diarrhea in kittens. It is usually not associated with clinical signs when seen in adult cats.10
Diagnostic indications
(1) Chronic diarrhea, (2) young cats, and (3) exposure to shelters or catteries.
Diagnosis
Most infestations of clinical significance are associated with large numbers of motile trophozoites visible on wet mount cytology of fresh feces. The flagellated trophozoites have a characteristic rapid progressive motion. Morphologic features, including a central axostyle, are visible when wet mounts are stained with iodine (Fig 2). These fastidious and fragile organisms are generally destroyed by routine flotation techniques, refrigeration, or delayed examination.10 Culture media for isolation of T fetus from vaginal fluid samples of cattle may also be used for fecal culture in cats. The media are inoculated with a small amount (<0.1 g) of fresh feces and monitored for growth of organisms for 1 to 11 days when incubated at 25°C.18 Polymerase chain reaction (PCR) test for identification of T fetus antigen in feces has been developed and validated, and may be commercially available in the future.19
Amoebiasis
Etiology and occurrence
Entamoeba histolytica is a protozoal parasite of humans that sometimes affects dogs. It most commonly occurs in tropical regions but has been reported in dogs in the United States.
Clinical signs
E histolytica can produce hematochezia or a profuse watery diarrhea.
Diagnostic indications
(1) Diarrhea, (2) hematochezia, and (3) screening for zoonosis.
Diagnosis
Cysts may be identified on fecal flotation. Motile trophozoites may be identified on wet mount cytology of fresh feces. Trophozoites are occasionally identified in colonic biopsy specimens.
Public health significance
Humans appear to be the major source of canine infection. Transmission occurs by ingestion of cysts in food or water contaminated with fecal material.20, 21
Balantidiasis
Etiology, occurrence, and clinical signs
Balantidium coli is a large bowel pathogen of many animals, including humans. It has been identified in dogs with ulcerative colitis, often with concurrent whipworm infestation. Clinical signs may include abdominal pain, weight loss, and bloody, mucoid stools.
Diagnostic indications
(1) Colitis signs, (2) whipworm infestation, and (3) screening for zoonosis.
Diagnosis
Cysts may be identified on fecal floatation. Motile ciliated organisms are seen on wet mount cytology of fresh feces. Trophozoites may be identified in colonic biopsy specimens.
Public health significance
B coli is readily transmitted between species, including humans. Transmission occurs with ingestion of cysts water or food contaminated with feces.20, 21, 22
Bacterial enteritis
Campylobacteriosis
Etiology and occurrence
Campylobacteriosis is a contagious disease of dogs and cats caused by C jejuni. A considerable percentage (10% to 40%) of dogs carry and shed C jejuni, but, in most of them, enteritis and diarrhea do not develop. A considerable number of cats are also carriers of C jejuni.12, 16 Distribution of C jejuni is probably worldwide in dogs, cats, and other animals. Dogs younger than 6 months are more severely affected. There is some question as to whether or not this organism causes enteritis and diarrhea in normal cats other than kittens. Debilitated cats and those with parasitic or microbial infections are predisposed. Immunosuppression may also have a predisposing role.
Clinical signs
Patients often present with acute diarrhea. Symptoms may last 1 to 2 weeks or become chronic. Other signs include mild fever, anorexia, vomiting, and weight loss. The organism has caused abortion in bitches. Leukocytosis may be seen on complete blood count.
Diagnostic indications
(1) Diarrhea, sometimes with hematochezia; (2) young animals; (3) exposure to kennels or catteries; (4) multiple pets affected; (5) increased fecal leukocytes; (6) characteristic organisms on fecal cytology; and (7) screening for zoonosis.
Diagnosis
Wet mount fecal cytology may reveal characteristic curved organisms with “swarm of bees” like motility. Dry mount fecal cytology often reveals increased fecal leukocytes (Fig 3). Campylobacter may be identified on dark field or phase contrast microscopy. On Gram stained fecal smears, Campylobacter appears as gull-wing shaped, pale staining, Gram negative rods (Fig 4).14, 16, 20 It is important to differentiate Campylobacter from fecal spirochetes, such as treponeme-like bacteria (see Spirochetal Diarrhea section) (Fig 1).9, 14 Cytology may provide a quick presumptive diagnosis but should always be confirmed with culture.9, 20 For culture, 2 to 5 g of fresh feces should be placed in a sterile container or special transport media, such as Para-Pack C&S. Samples should be refrigerated and delivered to the laboratory on ice for processing within 24 hours.4 Isolation of this fragile and fastidious organism requires special culture media (Campy blood agar) and incubation in a microaerophilic atmosphere. Antimicrobial susceptibility tests should be performed on positive cultures. Isolation of the organism in itself does not necessarily mean the patient has campylobacteriosis. Positive culture should be interpreted based on the clinical presentation, results of other diagnostic tests, and response to antimicrobial therapy.12
Public health significance
C jejuni is an important cause of gastroenteritis in infants, children, and adults. Potential sources of this organism for humans include poultry and a number of animals, including dogs and cats. Owners of pets with clinical disease should be advised to exercise appropriate hygienic measures to prevent possible exposure to C jejuni. Pets with evidence of clinical disease should be treated to arrest shedding.12, 14, 16, 20
Enteric colibacillosis
Etiology, occurrence, and clinical signs
Pathogenic strains of E coli are a common cause of diarrhea in humans and food animals, and are likely to cause enteritis in dogs and cats. Pathogenic E coli cause disease by a number of mechanisms. Strains are classified based on virulence factors, including epithelial attachment, toxin production, and cellular invasion. Pathogenic E coli has been implicated in acute diarrhea in puppies, and may play a role in hemorrhagic gastroenteritis (HGE) and chronic enteritis in adult dogs.11, 14
Diagnostic indications
(1) Acute watery or hemorrhagic diarrhea, (2) young animals, (3) sepsis, and (4) increased fecal leukocytes.
Diagnosis
Attaching and effacing lesions typical of pathogenic E coli may be seen on histopathologic examination of intestinal biopsies. Fecal leukocytes may be increased on cytology (Fig 3). Rapid response to appropriate antibacterial therapy may support the diagnosis of colibacillosis. Isolation of E coli on fecal culture is not diagnostic. Enteric pathogens must be differentiated from normal flora by evaluating cultured isolates for specific surface antigens or production of enterotoxins. Isolates can be tested for toxin or other virulence encoding genes by deoxyribonucleic acid hybridization or PCR. These tests are unlikely to be useful in a clinical setting.11, 14, 20
Public health significance
Some pathogenic E coli can potentially be carried by dogs or cats and transmitted to humans.20
Clostridial colitis
Etiology, occurrence, and clinical signs
C perfringens is an anaerobic, spore forming, Gram positive bacillus that is part of the normal flora of the GI tract. Under the right conditions, pathogenic strains can produce a number of enterotoxins. Dogs and cats with C perfringens associated diarrhea frequently show colitis signs, including increased frequency of bowel movements, tenesmus, fecal mucous, and hematochezia.9, 11 Enterotoxigenic C perfringens may play a role in acute HGE syndrome in dogs. C difficile is the major cause of pseudomembranous colitis in humans and has been associated with diarrhea in dogs.11, 14
Diagnostic indications
(1) Transient or episodic colitis, (2) HGE, and (3) increased fecal leukocytes.
Diagnosis
An ELISA kit for detection of C perfringens enterotoxin (CPE) in feces is available. The diagnosis of C perfringens-associated diarrhea is made based on detection of CPE in the feces in conjunction with typical clinical signs. Toxin production may be linked to sporulation. It is reported that seeing large numbers of sporulating cells (>5 per oil immersion field) on cytology may suggest the presence of C perfringens-associated diarrhea.14 C perfringens is a large, Gram positive rod with a central spore that gives it a “safety pin” appearance (Fig 5). Unfortunately, studies have shown a poor correlation between spore counts and detection of CPE. Not all clostridial spores produce CPE. Also, clostridial spores may be confused with other spore forming rods, especially those of Bacillus spp, and soil-borne aerobes that are ubiquitous and usually nonpathogenic.9, 11 Quantitative fecal culture for C perfringens does not correlate with the presence of CPE. Up to 75% of normal dogs culture positive for C perfringens.11 There is an ELISA for the detection of C difficile toxins A and B.11
Salmonellosis
Etiology and occurrence
Salmonellosis is a contagious disease of dogs, cats, other domestic and wild animals, and humans. The disease is worldwide in distribution, and a number of different serotypes are involved. The most common serotype recovered from dogs and cats is Salmonella typhimurium.
Clinical signs
Salmonellosis is manifested by 1 of the following 3 syndromes (1) septicemia, (2) acute enteritis, and (3) chronic enteritis. The septicemic form develops most frequently in young animals, while acute and chronic enteritis is seen most commonly in adult animals. Clinical signs vary with the severity of the infection and include gastroenteritis, episodes of fever, vomiting, depression, occasionally pneumonia, and, sometimes, abscesses in lymph nodes and internal organs. Although clinical salmonellosis develops in few dogs and cats, a considerable number are carriers.12, 16
Diagnostic indications
(1) Acute diarrhea; (2) sepsis, especially young animals; (3) leukocytosis or leukopenia; (4) fever; (5) increased fecal leukocytes; and (6) screening for zoonosis.
Diagnosis
Fecal culture for Salmonella spp is sensitive in animals with clinical disease. Because carriers are common, positive culture should be interpreted based on the clinical signs, results of other diagnostic tests, and response to antimicrobial therapy. Carriers shed organisms intermittently. Three negative fecal cultures on successive days are necessary to exclude the carrier state.12
Public health significance
Humans are readily infected with animal salmonellae. Care should be taken to avoid exposure to feces and other potentially infectious materials.14, 16, 20
Spirochetal diarrhea
A variety of motile spiral bacteria are commonly seen on fecal cytology in animals with diarrhea. Historically, they are considered nonpathogenic, and increased numbers have been considered a result and not a cause of disease. They are believed to inhabit the crypts of the colon and get mechanically dislodged during periods of diarrhea. Also, changes in the flora may occur secondary to diarrhea.14, 20
The most commonly identified spirochetes in diarrheic feces are motile treponeme-like organisms, which are not considered pathogens. They are rapidly motile, stiff, “cork-screw” like bacteria that dart across the field on wet mount cytology. On dry mount cytology, they show several complete convolutions and are 4 to 18 μm in length (Fig 1).23 On fecal cytology, it is important to differentiate nonpathogenic treponeme-like organisms from other potentially pathogenic motile spiral bacteria (eg, Campylobacter and Serpulina) Fig 4, Fig 6. Recently, there has been growing evidence that some large bowel spirochetes may cause enteritis.24, 25 Most investigation has focused on Serpulina pilosicoli (Brachyspira pilosicoli).24, 25, 26, 27
Etiology and occurrence
S pilosicoli is thought to cause colonic disease in human beings, nonhuman primates, dogs, pigs, and birds. The disease is characterized by colonization of the surface and crypt mucin, and intimate attachment of the spirochetes to the apical membrane of cecal and colonic enterocytes. Diarrhea associated with S pilosicoli has been described in children and immunocompromised adults. It has also been observed in puppies with diarrhea.24, 25, 26, 27 Several species of the genus Serpulina are found in animals that do not show virulence factors. Serpulina canis, which has been isolated from dogs, has not been associated with disease.24
Clinical signs
Severe diarrhea has been described in puppies with S pilosicoli. In humans, it occurs as a subclinical disease in mature immunocompetent hosts. Diarrhea may be associated with either massive infection, which occurs in a poor hygienic environment, or compromised intestinal function because of concurrent disease.24
Diagnostic indications
(1) Acute diarrhea, (2) young animals, (3) kennels, and (4) immune compromise.
Diagnosis
Serpulina may be seen on cytology of fresh feces. They are a very thin, long “S” shaped spirochetes. They are difficult to see on wet mount cytology, but, in large numbers, you can recognize their rapid whipping motion. They can also be identified on dry-mount cytology (Fig 6).9 Because not all Serpulina spp are pathogenic, diagnosis requires identification of typical organisms on cytology, a consistent clinical presentation, and elimination of other possible etiologies.24 It is important to differentiate Serpulina spp from motile treponeme-like spirochetes. S pilosicoli may be identified by ELISA and PCR methods in research settings.24 Complete response to antibacterial therapy within 2 to 3 days may support the diagnosis.9
Enteric fungi
Low numbers of fungi are part of the normal intestinal flora. Overgrowth of yeasts, such as Candida sp, may occur when antibiotics alter the normal intestinal flora. Mucosal invasion and systemic spread may occur with severe immunosuppression.20
Viral enteritis
Viral enteritis induced by Parvovirus or Coronavirus is suspected in animals with fever and small bowel diarrhea, particularly if neutropenia is present. The diagnosis of Parvovirus is usually made by detection of fecal shedding of viral antigen. Fecal ELISA tests are available, which accurately detect shedding of Parvovirus in acute cases. The specificity of the assay is good, but it cannot differentiate vaccine strains of Parvovirus from virulent strains. This leads to false-positive tests after vaccination. False-negative reactions can occur.3 These assays may also detect feline Parvovirus.14 Virus isolation or electron microscopy is required to identify canine or feline Coronavirus in feces.3, 14
Conclusion
Optimal fecal assessment involves several steps. Formulate a differential list based on the clinical presentation. Select effective diagnostic tests for the etiologies of concern. Set up optimal protocols for in-house diagnostics, like fecal cytology and flotation. Collect, store, and ship fecal samples in a manner that is appropriate for each test. Finally, consider the sensitivity and specificity of diagnostics when interpreting results.
References
- 1.Kazacos K.R. 2002 Proceedings, Western Veterinary Conference. Western Veterinary Conference; Henderson, NV: 2002. Diagnostic methods for internal parasites. [Google Scholar]
- 2.Williams J.F., Zajac A. Diagnosis of Gastrointestinal Parasitism in Dogs and Cats. Ralston Purina Co; St. Louis, MO: 1980. [Google Scholar]
- 3.Willard M.D., Twedt D.C. Gastrointestinal, pancreatic and hepatic disorders. In: Willard M.D., Twedt D.C., Turnwald G.H., editors. Small Animal Clinical Diagnosis by Laboratory Methods. (ed 3) Saunders; Philadelphia, PA: 1991. pp. 172–207. [Google Scholar]
- 4.Idexx Veterinary Services . Laboratory Directory of Tests and Services. Idexx Laboratories Inc; Westbrook, ME: 2000. [Google Scholar]
- 5.Walberg J. Personal communication. 2003. August. [Google Scholar]
- 6.Bowman D.D. Georgis’ Parasitology for Veterinarians. (ed 7) Saunders; Philadelphia, PA: 1999. [Google Scholar]
- 7.Foreyt W.J. Veterinary Parasitology Reference Manual. (ed 4) Washington State University; Pullman, WA: 1997. [Google Scholar]
- 8.Sloss M.W., Kemp R.L., Zajac A.M. Veterinary Clinical Parasitology. (ed 6) Iowa State University Press; Ames, IA: 1994. [Google Scholar]
- 9.Harter J.M. Veterinary Information Network, Inc; Davis, CA: 2003. Microbiology image library. Available at: http://www.vin.com/Members/Library. Accessed September 29, 2003. [Google Scholar]
- 10.Levy M.G., Gookin J.L., Poore M. Tritrichomonas foetus and not Pentatrichomonas hominis is the etiologic agent of feline trichomonal diarrhea. J Parasitol. 2003;89:99–104. doi: 10.1645/0022-3395(2003)089[0099:TFANPH]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Marks S.L. 2000 Proceedings, Fall Meeting of American Association of Feline Practitioners. American Association of Feline Practitioners; Nashville, TN: 2000. Gastrointestinal parasitology: Update on diagnostic and therapeutic options. [Google Scholar]
- 12.Marks S.L. 2001 Proceedings, World Congress, World Small Animal Veterinary Association. World Small Animal Veterinary Association; Vancouver, Canada: 2001. Diagnosis of infectious diarrhea in dogs and cats: A critical appraisal. [Google Scholar]
- 13.Marks S.L. 2002 Proceedings, American College of Veterinary Internal Medicine Forum. American College of Veterinary Internal Medicine; Lakewood, CO: 2002. Bacterial-associated diarrhea in dogs: A critical appraisal. [Google Scholar]
- 14.Greene C.E. Gastrointestinal and intra-abdominal infections. In: Greene C.E., editor. Infectious Diseases of the Dog and Cat. (ed 2) Saunders; Philadelphia, PA: 1998. pp. 595–613. [Google Scholar]
- 15.Murphy K.F., German A.J., Ruaux C.G. Fecal alpha 1-proteinase inhibitor concentration in dogs with chronic gastrointestinal disease. Vet Clin Pathol. 2003;32:67–72. doi: 10.1111/j.1939-165x.2003.tb00316.x. [DOI] [PubMed] [Google Scholar]
- 16.Carter G.R., editor. A Concise Guide to Infectious and Parasitic Diseases of Dogs and Cats. International Veterinary Information Service; Ithaca, NY: 2001. Available at: http://www.ivis.org. Accessed September 29, 2003. [Google Scholar]
- 17.Nolan T. Diagnosis of Veterinary Endoparasitic Disease. University of Pennsylvania: Computer Aided Learning Project; Philadelphia, PA: 2003. Available at: http://www.cal.vet.upenn.edu. Accessed September 29, 2003. [Google Scholar]
- 18.Gookin J.L., Foster D.M., Poore M.F. Use of a commercially available culture system for diagnosis of Tritrichomonas foetus infection in cats. J Am Vet Med Assoc. 2003;222:1376–1379. doi: 10.2460/javma.2003.222.1376. [DOI] [PubMed] [Google Scholar]
- 19.Gookin J.L., Birkenheuer A.J., Breitschwerdt E.B. Single-tube nested PCR for detection of Tritrichomonas foetus in feline feces. J Clin Microbiol. 2002;40:4126–4130. doi: 10.1128/JCM.40.11.4126-4130.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guilford W.G., Center S.A., Strombeck D.R., editors. Strombeck’s Small Animal Gastroenterology. (ed 3) Saunders; Philadelphia, PA: 1996. [Google Scholar]
- 21.Wittnech C. Entamoeba histolytica infection in a German shepherd dog. Can Vet J. 1993;17:259–262. [PMC free article] [PubMed] [Google Scholar]
- 22.Dubey J.P. Intestinal protozoal infections. Vet Clin N Am. 1993;23:37–55. doi: 10.1016/s0195-5616(93)50003-7. [DOI] [PubMed] [Google Scholar]
- 23.Kasbohrer A., Gelderblom H.R., Arasteh K. Intestinal spirochetosis in HIV-infection: Prevalence, isolation and morphology of spirochetes. Dtsch Med Wochenschr. 1990;115:1499–1506. doi: 10.1055/s-2008-1065183. [DOI] [PubMed] [Google Scholar]
- 24.Duhamel G.E., Trott D.J., Maniuppa N. Canine intestinal spirochetes consist of serpulina pilosicoli and a newly identified group provisionally designated: “Serpulina canis” sp. nov. J Clin Microbiol. 1998;36:2264–2270. doi: 10.1128/jcm.36.8.2264-2270.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dumhamel G.E., Maniappa N., Mathiesen M.R. Certain canine weakly beta-hemolytic intestinal spirochetes are phenotypically and genotypically related to spirochetes associated with human and porcine intestinal spirochetosis. J Clin Microbiol. 1995;33:2212–2215. doi: 10.1128/jcm.33.8.2212-2215.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fellstrom C., Pettersson B., Zimmerman U. Classification of Brachyspira spp. isolated from Swedish dogs. Anim Health Res Rev. 2001;2:75–82. [PubMed] [Google Scholar]
- 27.Oxberry S.L., Hampson D.J. Colonization of pet shop puppies with Brachyspira pilosicoli. Vet Microbiol. 2003;93:167–174. doi: 10.1016/s0378-1135(03)00017-8. [DOI] [PubMed] [Google Scholar]
- 28.Harter J.M. Images provided. 2003. August. [Google Scholar]


