A decade on from the 2002–03 outbreak of severe acute respiratory syndrome coronavirus (SARS-CoV) infections, the world is again confronted by the possible international spread of a novel coronavirus, the Middle East respiratory syndrome coronavirus (MERS-CoV), which apparently originated in the Arabian peninsula.1 MERS-CoV is associated with severe respiratory tract infection, often renal failure, and mortality exceeding 40% in patients admitted to hospital.2 Similar to SARS-CoV, it is closely related to bat coronaviruses, but MERS-CoV has different cellular receptor specificity and a broader species range—camels seem to have a role as a natural host. Saudi Arabia has been most severely affected so far, but imported cases—either recent travellers or those transported for clinical care—have been seen in countries in Europe, Africa, Asia, and North America. Major nosocomial outbreaks have happened in the Middle East,3 and non-sustained human-to-human transmission events elsewhere,4 and many more clinical cases are likely to have occurred.5 There has been a recent surge in case reporting that could be the result of more human-to-human transmissions due to a change in exposure patterns, expansion of the virus in animal reservoir(s), seasonal variation, ongoing nosocomial clusters, or increased surveillance with reporting of mild or asymptomatic MERS-CoV detections, or both.5
Severe MERS-CoV disease has occurred primarily in older adults, particularly men, with comorbidities.2 However, data on disease pathogenesis, particularly viral replication patterns and clinical manifestations, are scarce at present. Despite more than 500 laboratory-confirmed MERS-CoV cases so far, only a handful of patients have had systematic virological and biomarker sampling.4, 6 Consequently, there are many unanswered questions regarding sites of infection, pathogen dynamics, innate and adaptive immune responses, and host genetic factors. Prolonged viral replication in the lower respiratory tract, extrapulmonary virus detection, severe lung injury with respiratory failure, and often renal failure are notable features, suggesting that an effective antiviral regimen, perhaps in combination with immunomodulatory agents, would provide clinical benefit.
Although supportive care is central to clinical management of coronavirus infections, appropriate antiviral and immunomodulatory therapy for both SARS7 and MERS-CoV infections remain uncertain because of a scarcity of quality evidence. An absence of good animal models for MERS-CoV poses a major challenge. Many agents have inhibitory activity in vitro for coronaviruses, including some licensed drugs,7, 8, 9 but it is unclear whether their human pharmacology and tolerability would enable sufficient doses to be given to exert antiviral effects in patients with MERS-CoV. One available drug that is inhibitory for coronaviruses in vitro at clinically achievable levels is the inosine-5′-monophosphate dehydrogenase (IMPDH) inhibitor mycophenolic acid,8 but animal data for this effect are scarce, and one patient developed infection while receiving mycophenolate mofetil.4 Ribavirin and interferon combinations are associated with modest antiviral effects in MERS-CoV inoculated rhesus macaques given high doses.9 Although the clinical relevance of these findings is uncertain, the combined use of antiviral drugs to enhance inhibitory effects and reduce the potential for resistance emergence makes sense.
At present, the strongest treatment evidence supports the use of convalescent plasma or other preparations that possess neutralising antibodies.10, 11 Convalescent plasma seemed to reduce duration of treatment in hospital and mortality when used early in patients with SARS.7 For MERS-CoV, low neutralising antibody responses and inability to acquire sufficient convalescent plasma from survivors with comorbidities might restrict the effectiveness of this treatment, although these limitations might not apply to infected health-care workers. Additionally, the availability of human neutralising monoclonal antibodies12 or polyclonal immune globulin produced in transgenic cows or other hosts13 could overcome these hurdles. The high seroprevalence of high-titre neutralising antibody to MERS-CoV or a closely related virus in dromedary camels in the region raises the possibility of using camel sera or engineered single domain camel antibodies for therapy.13, 14 Purified immunoglobulins or immunoglobulin fragments (nanobodies) might offer a therapeutic option for severely ill patients until more defined, genetically engineered, antibodies become available.
For any chosen intervention, we advocate that use must be accompanied by a prospective, protocol-based assessment of safety and effectiveness that includes sequential virological, clinical, and biomarker measurements. We wrote about the slow acquisition of such data in the 2009 H1N1 influenza pandemic.15 One outcome from this circumstance was the formation of the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC), a global federation of academic clinical research networks. ISARIC has collaborated with WHO to develop biological sampling protocols that are applicable for patients with MERS-CoV. Furthermore, working with colleagues in Public Health England, ISARIC experts have examined available data and ranked potential therapeutic options with regard to their priority for clinical study;10 this information will be updated as new data become available.
However, no MERS-CoV patients have yet been enrolled on therapeutic protocols incorporating systematic sampling through ISARIC or any other organisation. Consequently, we are not learning what might benefit or potentially harm such patients. Whatever agent or agents are selected for testing, systematic harmonised data collection involving robust observational studies or, when possible, controlled trials, is needed to assess both disease pathogenesis and candidate therapeutics for MERS-CoV. Clinicians and public health officials in affected Middle Eastern countries, particularly in Saudi Arabia, are uniquely positioned to undertake such studies. With support as needed from international partners like WHO and ISARIC,11 regional governments, and funders, Middle Eastern colleagues have both the opportunity and the responsibility to undertake studies to advance the understanding of effective prevention and treatment strategies for MERS-CoV and any future novel CoV outbreaks. Thus far, MERS-CoV is yet another emerging infection threat for which the clinical research response has been too slow and uncoordinated. New investigative frameworks, possibly incorporating mandates into the International Health Regulations, are urgently needed.
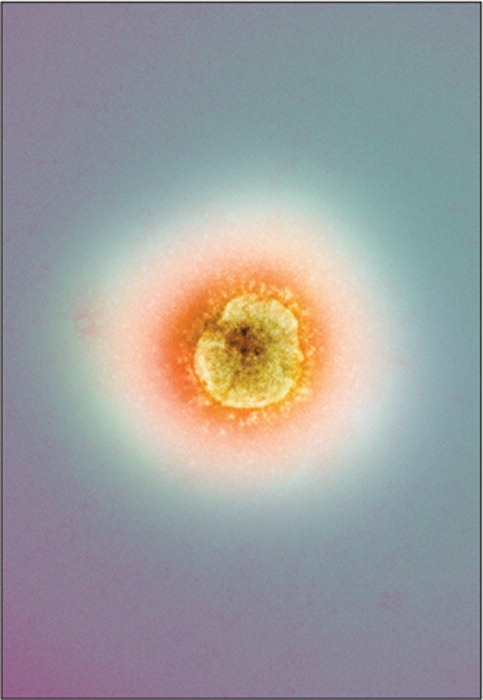
© 2014 Centre For Infections/Public Health England/Science Photo Library
Acknowledgments
We declare no competing interests relevant to this Comment. JSMP has received research funding from the National Institutes of Health (NIAID contract HHSN266200700005C). JF served as Chair of the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) from 2011 to 2013, and FGH as acting Chair of ISARIC from October, 2013, to April, 2014. ISARIC has received funding from the Bill and Melinda Gates Foundation, Wellcome Trust, Medical Research Council, Institut National de la Santé Et de la Recherche Médicale (INSERM), Fondation Merieux, Li Ka Shing Foundation, and the government of Singapore. We thank Lisa Cook for her assistance with the references.
References
- 1.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 2.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Assiri A, McGeer A, Perl TM. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guery B, Poissy J, el Mansouf L. Clinical features and viral diagnosis of two cases of infection with Middle East Respiratory Syndrome coronavirus: a report of nosocomial transmission. Lancet. 2013;381:2265–2272. doi: 10.1016/S0140-6736(13)60982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cauchemez S, Fraser C, Van Kerkhove MD. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drosten C, Seilmaier M, Corman VM. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013;13:745–751. doi: 10.1016/S1473-3099(13)70154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hui DS, Chan PK. Severe acute respiratory syndrome and coronavirus. Infect Dis Clin North Am. 2010;24:619–638. doi: 10.1016/j.idc.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan JF, Chan KH, Kao RY. Broad-spectrum antivirals for the emerging Middle East respiratory syndrome coronavirus. J Infect. 2013;67:606–616. doi: 10.1016/j.jinf.2013.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falzarano D, de Wit E, Rasmussen AL. Treatment with interferon-α2b and ribavirin improves outcome in MERS-CoV-infected rhesus macaques. Nat Med. 2013;19:1313–1317. doi: 10.1038/nm.3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Public Health England ISARIC. Clinical decision making tool for treatment of MERS-CoV v.1.1, July 29, 2013. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317139281416 (accessed May 9, 2014).
- 11.WHO WHO-ISARIC joint MERS-CoV Outbreak Readiness Workshop: Clinical management and potential use of convalescent plasma. 2013. http://www.who.int/csr/disease/coronavirus_infections/MERS_outbreak_readiness_workshop.pdf?ua=1 (accessed May 9, 2014).
- 12.Jiang L, Wang N, Zuo T. Potent neutralization of MERS-CoV by human neutralizing monoclonal antibodies to the viral spike glycoprotein. Sci Transl Med. 2014;6:234ra59. doi: 10.1126/scitranslmed.3008140. [DOI] [PubMed] [Google Scholar]
- 13.Houdebine L-M. Production of human polyclonal antibodies by transgenic animals. Adv Biosci Biotechnol. 2011;2:138–141. [Google Scholar]
- 14.Tillib SV, Ivanova TI, Vasilev LA. Formatted single-domain antibodies can protect mice against infection with influenza virus (H5N2) Antiviral Res. 2013;97:245–254. doi: 10.1016/j.antiviral.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Hien TT, Ruiz-Palacios GM, Hayden FG, Farrar J. Patient-oriented pandemic influenza research. Lancet. 2009;373:2085–2086. doi: 10.1016/S0140-6736(09)61131-4. [DOI] [PubMed] [Google Scholar]


