Abstract
Background
Climate change has myriad implications for the health of humans, our ecosystems, and the ecological processes that sustain them. Projections of rising greenhouse gas emissions suggest increasing direct and indirect burden of infectious and noninfectious disease, effects on food and water security, and other societal disruptions. As the effects of climate change cannot be isolated from social and ecological determinants of disease that will mitigate or exacerbate forecasted health outcomes, multidisciplinary collaboration is critically needed.
Objectives
The aim of this article was to review the links between climate change and its upstream drivers (ie, processes leading to greenhouse gas emissions) and health outcomes, and identify existing opportunities to leverage more integrated global health and climate actions to prevent, prepare for, and respond to anthropogenic pressures.
Methods
We conducted a literature review of current and projected health outcomes associated with climate change, drawing on findings and our collective expertise to review opportunities for adaptation and mitigation across disciplines.
Findings
Health outcomes related to climate change affect a wide range of stakeholders, providing ready collaborative opportunities for interventions, which can be differentiated by addressing the upstream drivers leading to climate change or the downstream effects of climate change itself.
Conclusions
Although health professionals are challenged with risks from climate change and its drivers, the adverse health outcomes cannot be resolved by the public health community alone. A phase change in global health is needed to move from a passive responder in partnership with other societal sectors to drive innovative alternatives. It is essential for global health to step outside of its traditional boundaries to engage with other stakeholders to develop policy and practical solutions to mitigate disease burden of climate change and its drivers; this will also yield compound benefits that help address other health, environmental, and societal challenges.
Key Words: adaptation, climate change, environmental change, global health, multidisciplinary collaboration, mitigation, prevention
Introduction
Over the course of the past decade, the hardening reality of anthropogenic climate change has demonstrated the need to understand its future effects on health outcomes as well as the critical need for collaboration across disciplines to find appropriate solutions that prevent, prepare, and respond to climate change. As of 2000, climate change was directly accountable for the loss of at least 5.5 million disability-adjusted life years.1 The Intergovernmental Panel on Climate Change (IPCC) projected average global temperatures will increase between 1.8°C and 4°C over the next century,2 and extreme weather events and shifting patterns of disease are expected to have significant effects on global disease burden, water and food security, and social conflict—although the extent and direction of these effects will be differentially felt.3, 4, 5 Given the complexity of social and environmental factors that influence disease and health outcomes, the precise degree of past and future effects on health is unclear; however, best estimates indicate that climate change will tip the scales of health outcomes unfavorably.6, 7 The World Health Organization (WHO), for example, estimated in the early 2000s that climate change was already accounting for 150,000 additional deaths globally (ie, deaths above the baseline) per annum. This number has been updated such that compared with a future without climate change (for the year 2030) an additional 38,000 deaths annually are projected due to heat exposure in elderly people, 48,000 due to diarrhea, 60,000 due to malaria, and 95,000 due to childhood undernutrition. This corresponds to an additional 250,000 deaths per year for the years 2030-2050—not including all climate-sensitive health effects (eg, pollution, injuries, nonmalarial infectious disease, and others for which projection data is lacking).8 Direct health costs are projected to increase from US$1.2 trillion to between US$2 and $4 trillion per year,8 and, when agricultural loss, damage due to extreme weather events, and decreased productivity are added, the estimated economic loss could reach 3.2% of global output.9
Many linear and nonlinear relationships exist between the environment and health, as anthropogenic activity influences health through a variety of ecosystem and climate-mediated pathways. Causal pathways can also be reversed: societal needs related to health can influence climate.10 For instance, health practices themselves have a large carbon footprint. Nutritional demands lead to land use change for agricultural expansion, increased carbon release, and pressure on water resources; the administration of vaccines and health support resources, particularly in rural locations, requires carbon-emitting transportation11; and public health infrastructure, especially in developed countries, entails significant electricity usage12—all of which increase greenhouse gas emissions and concomitantly compound pressures on natural systems.
Even for more linear causal links—mortality and morbidity caused by extreme weather events and disease—complexity reigns. The effects of climate change cannot be isolated from social and ecological determinants of disease that will mitigate or exacerbate forecasted health outcomes. Demographic factors, health status, culture or life condition, limited access to resources and services, and sociopolitical conditions have been characterized as affecting vulnerability to health effects of climate change.13 Geographically vulnerable regions, low-income countries, and refugees are more likely to bear a higher burden of adverse effects. In this regard, causal links may reinforce cyclical links between poverty and high health burden, whereas areas with higher human activity (land-use changes, urbanization, and rising populations) may motivate disease trajectories and adverse health outcomes.4
Because of this complexity, multidisciplinary and cross-sectoral collaboration will be critical to address health challenges related to climate change. This is reflected in the literature; for example, the hundreds of papers published relating to this topic (Web of Science search term [up to June 25, 2015] “health AND climate change AND collaboration”) cover an expansive range of expected challenges, broad sectors, and manifestations, including toxic algal blooms, food systems, pest control, built environment, remote-sensing technologies, health provider concerns, and environmental education. However, emphasis has been placed primarily on vulnerabilities, preparedness, adaptation, and resiliency. With notable exceptions, the explicit reference to collaboration aimed at outright prevention has been less prominent.
Collaboration is certainly pressing to address both realized and near-term effects of carbon emissions and copollutants. However, less attention has been given to the underlying drivers of climate change to prevent, rather than only respond to, health effects.14 Given that there is a critical 15- to 30-year window for greenhouse gas emissions—with projections exceeding the “tipping point” for stability if continued at current levels throughout that time frame, urgent action is required if we are to transcend disciplinary silos to find solutions.7 Climate change is also occurring parallel to, and in combination with, other change pressures on global health (Fig. 1 ), including widespread land-use change, a global population expected to increase more than 30% by 2050,10 and globalization.15 Such pressures often have geographic specificity; for example in Sub-Saharan Africa, increasing population growth and demands on natural resources (including those leading to environmental degradation) coupled with regional exclusion from global trade converge with climate-related agricultural productivity reduction and coastal flooding risks and an already disproportionately high infectious disease burden in the region.15 Action will therefore likely be most successful if it also addresses the underlying contributors of global environmental change, and other major and related challenges, including loss of biodiversity and infectious disease emergence.10
Figure 1.
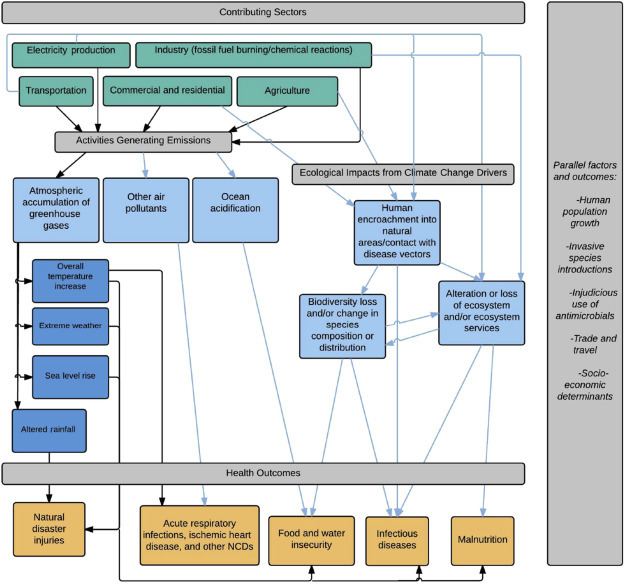
Examples of the links associated with direct health impacts of climate change (black arrows) and those associated with the drivers of climate change (blue arrows). Activities taken by sectors contributing to climate change may also have other ecological impacts (eg, from human encroachment into forests). Other forces are occurring in parallel, simultaneously altering ecological and human dynamics. Global health must expand its scope to work with other sectors to find solutions that can prevent, prepare and respond to negative outcomes. NCD, noncommunicable disease.
Figure adapted from reference 7.
To fully prepare for and respond to current and near-term challenges of climate change on health and affected societies, a firm understanding of the links—and their differential effects based on differential socioeconomic conditions—is needed.10 Furthermore, to truly get ahead of long-term negative health outcomes, a more preventive approach will be needed—one that tackles upstream drivers in new and effective ways. We conducted a literature review of pathways between climate change and health and drew on these findings and our collective expertise to review opportunities for both adaptation (defined herein as adjustment strategies to reduce vulnerability to negative effects, also within the domain of preparedness and response) and mitigation (prevention of effects) that demand genuine collaboration toward reducing global health risks posed by climate and other global environmental changes. The opportunities align with and emphasize the preventive measures of the recent recommendations put forth in the new Lancet Commission on Climate Change report including near-term investments in research, monitoring and surveillance on climate change and health effects, adopting mechanisms that facilitate intra- and intergovernmental collaboration with an emphasis on the extent to which additional global environmental changes influence health outcomes, phasing out of coal-fired energy generation, and transition to human- and planet-healthy cities.7
Health Outcomes: Impacts and Drivers of Climate Change
The outcomes of widely cited health effects related to climate change— direct injury from extreme weather events, increased noncommunicable disease (NCD) burden, increased burden of infectious diseases, reduction of food and water security, and loss of other ecosystem services including access to medicinal plants—10, 16 are likely to be both acute and chronic, having significant effects on affected communities. The wide scope of anticipated stakeholders provides ready and necessary collaborative opportunities for interventions, which can be differentiated by addressing the upstream drivers leading to climate change or the downstream effects of climate change itself. Ideally, these will be in the form of coordinated steps to effectively prevent climate-change drivers (ie, mitigation), although it will also be necessary to leverage these to prepare for and respond to such pressures (ie, adaptation).
Effects of Climate Change
Clear causal links between climate change and human health due to the direct effects of extreme weather events have been widely reported.4, 6, 14, 17 The deleterious effects of heat waves have already been realized over the past decade in several countries,7 and they are generally projected to increase in frequency and duration.2 The probability of mega-heat waves, such as those experienced in Europe in 2003 and Russia in 2010, is estimated to increase 5- to 10-fold by 2050.18 The summer 2003 heat wave killed more than 70,000 people across European countries19 and resulted in more than an estimated US$14 billion in economic damages.20
Although specific causal links between heat waves and morbidity have drawn less attention,21 chronic cardiovascular and respiratory conditions are projected to increase, disproportionately affecting vulnerable populations such as the elderly.22 Morbidity exacerbated by geography, socioeconomic and occupational status will be especially problematic for already fragile economies. Projections suggest that by the 2050s workdays lost due to heat could reach 15% to 18% above the current baseline in Southeast Asia, Central America, Oceania, and parts of Sub-Saharan Africa, with as much as 20% of gross domestic product in economic losses related to reduced productivity in Central America by 2080 without labor pattern adaptation.23
Similarly, the total annual number of natural disasters doubled between 1980 and 2014,24 and of the 245 disasters in 2009, 224 were weather-related and affected 55 million people, causing 7000 deaths and comprising the majority (US$15 billion) of economic damages attributed to natural disasters.25 Annual increases in the intensity of hydrological cycles worldwide will increase the frequency and severity of flooding linked to heavy rain, cyclones, and rising sea levels.6 Populations in low-lying, low-income regions without adequate protection will be especially affected as a 2% to 5% increase in the burden of diarrheal disease is anticipated to occur by 2020 due to increased heavy precipitation.26
Although parts of the world will become wetter, other regions will become drier. The proportion of Earth’s surface in extreme drought could rise from about 1% in 2015 to 30% by the end of this century.27 Between 1970 and 2008 in Africa alone, although less than 20% of disaster occurrences were associated with drought, they affected 80% the continent’s population.25 Wildfires spurred by the 1997/1998 El Niño in Indonesia left 40,000 hospitalized and an estimated loss of US$9.3 billion in property, agriculture, and disrupted transport.28 Estimated agricultural losses from the 1998-1999 summer drought across the United States were on the order of US$1.3 billion,29 and the 2015 ongoing drought in California has resulted in serious economic losses and spurred policy interventions.
Extreme climate and weather have widespread implications for food, water and nutritional security, economic loss, and mental health. For example, if flood and droughts become more severe and frequent, especially in semiarid and subhumid areas, this will likely result in fluctuations in food production. As much of this land is located in Sub-Saharan Africa and part of South Asia, the poorest regions with an already high level of chronic undernourishment will bear the largest burden of unstable food production.30 This is reflected in the IPCC Special Report on Emission Scenarios and climate-change scenarios where Sub-Saharan African will represent 40% to 50% of global hunger by 2080, and in some simulations will account for 70% to 75% of global undernourishment.31 Other climate modeling has estimated the number of undernourished people worldwide could increase from 40 to 170 million by mid-century.2
There are many categories of infectious disease that show some degree of climate sensitivity. Although commonly broadly grouped as vector-borne diseases (VBDs), zoonoses (emerging or endemic), neglected tropical diseases (NTDs), and water-borne diseases, the boundaries between the disease types are not always clear or well defined. For example, some NTDs are VBDs and also waterborne; many diseases transmitted by vectors are also zoonotic. Vector-borne diseases are one of the most studied health challenges pertaining to climate change.32 Although variation has been observed for specific diseases, according to the UN Food and Agriculture Organization (FAO),33 some regions reported expansion of vector range due to rising temperatures—this has been noted with latitudinal and longitudinal shifts of tick-borne encephalitis in Europe34 in addition to mosquito-borne malaria in eastern Africa associated with a warming trend beginning in the 1970s.17 Similar increases in malaria in southern Africa and South America35 have been associated with the heavy rainfall of the El Niño Southern Oscillation cycle (ENSO). However, it should be noted that other authors have disputed the influence of climate change on malaria distribution, suggesting that other issues such as the spread of drug resistance and effects of tightening or relaxing of control measures are more significant factors determining malaria risk.36 Based on minimal climate change scenarios, some African countries may see a 25% increase in the number of malaria cases per 1000 people and more than a 20% increase in treatment costs.37 Similarly, modeling has projected the expansion of transmission season and range for mosquitoes carrying West Nile virus, especially in the Canadian prairie provinces.38
El Niño patterns appear to have affected selected VBDs and pathogens such as Rift Valley fever (RVF) and chikungunya virus over the past decade. The largest RVF outbreak on record between 1997 and 1998 corresponded to a strong El Niño resulting in an estimated 89,000 possible human infections in northeastern Kenya and southern Somalia.39 Reflecting the la Niña phase of the ENSO cycle, regional droughts in East Africa in 2004 to 2006 aligned with the largest chikungunya epidemic on record.40
It is likely that zoonoses (infectious diseases transmitted between animal and humans) can be influenced by climatic changes affecting the behavior or movement of reservoir species due to shifts in resources, habitat range, or climate stress.4 In this scenario, climate-induced changes in the proximity or frequency of reservoir and human interaction would facilitate pathogen spillover between reservoir and host leading to spillover and emergence of pathogens. Although there are few examples where sufficient data have been collected or the correct analyses undertaken to prove the case, future research may be particularly fruitful in this field. Warming temperature has increased schistosomiasis transmission from snails to humans in China by changing the “freeze line” that had previously prevented northward movement. Expanding hospitable environments for the parasite’s host means over 20 million more people may be at risk by 2050.41 However, there are often other factors that have a key role in pathogen emergence, persistence, and spread, some of which also are associated with climate change drivers.
Drivers of Climate Change
The drivers of climate change do not act in isolation from other anthropogenic pressures on our ecosystems. For example, deforestation leads to the loss of carbon sinks, fundamentally changes landscapes, and alters species composition. Viewed as a “threat multiplier,” climate change can exacerbate existing and growing challenges, such as food security and food safety.42 This may complicate seemingly linear pathways—health outcomes that appear to arise from climate change may emanate from shared upstream drivers or arise from a mix of factors.
Such complexities can be seen with infectious diseases. Although climate change has been projected to influence the distribution and behavior of pathogens, reservoirs, and vectors, compounding factors such as social, economic, and environmental conditions (such as land use patterns and human activity) affect transmission pathways. Such uncertainty reflects the difficulties in modeling the differential distribution of disease and the complex interactions among disease, climatic, and socioeconomic determinants. Whether climate change is driven by or itself serves as one of several factors changing ecological dynamics, the extent to which climate change influences infectious disease distribution remains heavily debated.14 For example, land-use change (eg, deforestation and other extractive industries) and agricultural intensification, both major contributors to greenhouse gas emissions, rank among the leading drivers of recently emerging infectious diseases in humans from wildlife.43
Factors often leading to or exacerbating climate change,44 as well as natural events exacerbated by climate change, also may increase the risk for NCDs. For instance, extreme temperatures have resulted in increased hospital admissions due to cardiovascular and respiratory conditions. Air pollution has also contributed to mortality and morbidity and is an increasing risk in developed and developing countries alike.45 In a first study of its kind in the WHO European region, the overall annual cost of health effects and mortality resulting from air pollution, including estimates for morbidity costs, was estimated to exceeded US$1.5 trillion (corresponding to 600,000 premature deaths).46 Separately, the Organisation for Economic Co-operation and Development (OECD) found that air pollution-related morbidities and mortalities correspond to $1.7 trillion annually in OECD countries, $1.4 trillion in China, and $0.5 trillion in India. In 2012, around 80% of the 3.7 million deaths from outdoor pollution came as a result of stroke and heart disease, 11% from lung diseases, and 6% from cancers.47 Although not commonly considered a pollutant with direct inhalation effect on health, one analysis extrapolates that carbon dioxide could result in more than 21,000 premature deaths per year globally related to ozone and air particles effects.48
Although the discussion of NCDs is often limited to countries characterized by urbanization, industrialization, and economic development, climate change appears to transcend disease patterns across country and income levels. In Delhi and São Paulo, the incidence of chronic cardiovascular issues increased during heat waves.49 Although the discussion of NCDs is often detached from climate change public health actions, there are numerous co-benefits between the implementation of climate control methods and its effect on the reduction of NCD prevalence.7, 10, 45, 50 Reduction of greenhouse gas emissions through more sustainable transportation, building, and land use will ameliorate cardiovascular and respiratory disease with improved air quality, and curtail some forms of obesity by influencing physical activity behavior.
Environmental degradation associated with climate change drivers can initiate a vicious cycle between vulnerable populations, especially those in low-income countries, and their susceptibility to disease. The implications of land-use change for biodiversity loss and the associated loss of ecosystem goods and services present deeper implications for social welfare. For example, decreases in pollination services and reduced access to wild foods may affect food and nutritional security and livelihoods; a potential decline in access to medicinal plants used by a large proportion of the developing world as a source of primary health care may lead to negative health outcomes across indigenous and local communities; inadequate nutrient cycling harms clean water sources and leads to soil erosion and may contribute to the prevalence of waterborne diseases, thereby decreasing ecosystem and community resilience to extreme weather events; and biodiversity loss threatens access to natural resources with biomedical and pharmaceutical importance and weakens ecosystem integrity and resilience to climatic changes. All of these ecosystem services are also correlated to quality of life, mental and physical health, and social welfare.10
The scope of climate change, its underlying drivers and health outcomes extends widely beyond measurable disease burden and immediate mortality. For example, the IPCC projects climate change will increase the displacement of people and potentially their exposure and vulnerability to extreme weather events, particularly in developing countries.51 This will modify risks for violent conflicts by amplifying well-documented drivers of conflicts such as poverty and economic shocks. Flow-on effects may include significantly increased risk for civil and political conflict over dwindling resources, and mental health issues arising from trauma, displacement, conflict, and more limited access to natural resources used for food, medicines, and cultural and spiritual fulfillment.52, 53 Such challenges relate to defense and peacemaking initiatives, with the US Department of Defense 2014 Climate Change Adaptation Roadmap anticipating growing need for disaster relief and humanitarian assistance abroad as well as potential international instability coupled with threats to operations and supply chains.54 The drivers of climate change may themselves result in displacement of populations. The propensity for climate change impacts and drivers to result in conflict (and vice versa) provide an additional compelling call to action for global health.53
Prevention Opportunities
One route to addressing climate change risks is preparedness and response, such as coastal flooding safeguards and adaptive agriculture. Public health may take a similar approach, preparing for and responding to disease with stockpiling and emergency measures and adaptation through vaccination or therapeutics. These scenarios are often expensive and result in inefficient use of limited resources, as in the Ebola crisis in western Africa in 2014 to 2015. Mitigation approaches, in contrast, can prevent negative outcomes and their financial losses, as well as yield co-benefits across sectors and help to address multiple health threats related to environmental change.
In some cases, adaptation will lead to further environmental destruction, for example, in the form of agricultural changes that degrade freshwater quality.55 The dangers of anthropogenic environmental change are not newly recognized, nor are efforts to reduce anthropogenic climate change associated with greenhouse gases. The year 2016 marks the 20th year since the formation of the UN Kyoto Protocol aimed at a global commitment to emissions reductions, but in that time overall greenhouse gas emissions have steadily increased.7 Thus, new and innovative approaches are urgently needed to prevent global environmental pressures including climate change. In addition to guiding adaptation to reduce health effects of climate change, the health community can play a meaningful role by catalyzing major systems changes toward infrastructure and practices that are focused on addressing the drivers of climate and other environmental change. Multidisciplinary and cross-sectoral collaboration and the full involvement of civil society and local communities will be central to finding effective solutions.
Prevention at the Source
Considering the underlying driver of outcomes provides useful information for prevention opportunities, including those that can be prioritized across multiple sectors or to solve multiple challenges. For example, although climate change is a causal contributor to both infectious disease emergence and biodiversity loss, all 3 share many of the same underlying drivers (such as land-use change/habitat loss). Reversing the trajectory of outcomes requires addressing these underlying drivers, and determining the full scope of major mitigating or exacerbating factors is important for improving understanding of disease ecology dynamics; to look only at climate change could miss intricacies and causality from other factors. For example, climate change is commonly proposed as the reason for the expansion of vector range leading to VBD. However, despite sensitivity to climate, VBD spread may be more dependent on habitat loss and social factors56—issues likely to increase through large-scale land conversion to meet growing food demands and expansion of human settlements in the coming decades. Similarly, although pathogen evolution is the focus of intense research, anthropogenic environmental changes are likely to have more profound implications for infectious disease risk under climate change.57 New or more frequent human contact with other species, resulting in some novel interactions, is facilitating pathogen spillover, leading to outbreaks.
In addition to placing much-needed emphasis on preventing the ecological degradation and health outcomes associated with climate change drivers, mitigation is also crucial for preventing social vulnerability that could result from climate change. Societal disruption is typically associated with catastrophic events, such as emerging infectious disease outbreaks and natural disasters. Climate change effects may worsen susceptibility to already weak structures—such as the limited resilience of food systems under pandemic scenarios.58 However, endemic or otherwise persistent disease concerns can affect livelihoods, economic development, and other societal components. Climate-sensitive infectious diseases have been identified as an ongoing threat to the livestock industry. Despite their importance to more than 1 billion livestock holders globally, and the substantial contribution of livestock for global protein intake, investments in reducing vulnerability related to climate-sensitive diseases remain limited.59 Upstream disease prevention in this realm, including through disease surveillance, risk mapping, and long-term risk projections, and early warning systems, can reduce risks to livelihood and decrease health vulnerability downstream.59
Adopting a Systems Approach
There is a wide range of stakeholders whose health has been or will be affected by ecological change, all of whom can and should be engaged in finding preventive solutions that can yield co-benefits. An integrative approach that fully acknowledges the complexities of socioecological systems can help us more fully appreciate the interactions between each component, and identify areas where intervention could be synergistically beneficial. A One Health or ecosystems approach, which emphasizes the links between human, animal, and environmental health, provides a useful frame that can be used to begin understanding and addressing connections.60 This is especially pertinent as other global changes introduce pressures that may interface with climate change. For example, climate projections based on a “business-as-usual” emission scenario suggest an overall expanded suitable habitat for Pteropus spp. fruit bats, which serves as the reservoir for the deadly Nipah virus.61 Although climate change itself will not enable cross-continental movement of the bat, intentional or accidental introduction—for example, through the international wildlife trade—may allow its change in distribution, potentially also facilitating disease emergence. Similarly, climate-induced changes in pathways for invasive alien species will harm local biodiversity and related human health services in many regions, such as with the spread of the mountain pine beetle in North America; although most invasive species are relocated due to human activities, their overall effect is amplified under climate change.
Life-cycle analysis is increasingly used in engineering processes to assess material flows and impact, usually in terms of physical persistence. Incorporating a more comprehensive framework that shows all positive or negative effects, including flows of financial inputs and outputs and any short- or long-term health gains, can at least make development project funding decisions more transparent and potentially help keep companies or funders more accountable for anticipating and mitigating damages. As climate change and health data may use different metrics and be paired with different assumptions, a common framework for generating data may also lead to more united interpretations of results, allowing for evidence-based decision making.10
Levels of Collaboration
Health professionals work in a range of settings, allowing for integration into decision-making processes at many levels. Multidisciplinary, cross-sectoral, and intragovernmental collaboration on climate change prevention, preparedness, and response is not currently widely employed in the health community, but progress can be achieved within the current health domain. At the institutional level, while training programs typically operate in siloes, academic institutions can promote cross-training opportunities and invite researchers and practitioners from other disciplines and settings to explore points of shared relevance to initiate collaboration. Linking information resources, such as clinical decision support systems, local disease reporting, and ecological trend data, may help empower expanded stakeholder participation by making population health outcomes of environmental changes more visible. Health professionals can be role models by taking direct action to reduce their own carbon footprint and encourage their colleagues and patients to do the same62: for example, by turning lights off in unused exam rooms in their hospitals and clinics to reduce energy consumption, educating patients or populations on the health benefits of using public or active transport, exploring efficiencies with engineers to reduce hydrocarbon plastics use and packaging, working with hospital administrators and facilities departments to prioritize low-carbon energy sources, and implementing robust energy efficiency measures in health care facilities and institutions. As shown by the strong voice of International Physicians for the Prevention of Nuclear War, individual actions taken by health care providers can have a substantial collective effect.
At the governmental level, Ministries of Health should more systematically collaborate with other Ministries such as environment, agriculture, or transport to identify joint opportunities for coordinated action. Intragovernmental collaboration (with cross-sectoral inputs) is also essential to the development of climate adaptation and resilience indicators.10 Incentives for health professionals to engage with climate change and other environmental change issues are limited but could be developed out on a health systems level, including through collaboration integrated into existing health frameworks. The International Health Regulations (IHR) of the WHO, now in its second edition, represents the main governance mechanism to promote public health security of member countries. Primarily focused on reporting and response at a country level to aid in preparedness, the capacity established by the IHR could be expanded to include proactive approaches. Updates to the IHR could focus on disease prevention through risk reduction, including public and community engagement and health education, and closer integration with environmental, agricultural, and other sectors to encourage multidisciplinary understanding and solutions. Most directly, for a number of diseases with strong links to climate and weather, such as RVF, close working relationships between national and local public health and weather services, as well as agricultural or wildlife entities where sentinel monitoring may be possible, can help improve forecasting to enable risk-reduction strategies. The US Department of Defense and its partners have developed climate anomaly forecasting methods that provide weather-related disease projections (eg, El Niño conditions) up to 8 months in advance, including areas of heightened risk for specific infectious and NCDs (such as expected respiratory illness associated with forest fires during drought events).63 This information can help shape public health strategies and inform health providers for early detection or risk mitigation of disease.
Health professionals can also have meaningful participation in other domains—and in addition to the many cross-cutting health impacts of climate and other environmental changes, the differing priorities and political and economic dynamics across countries and regions make it crucial to engage in multidisciplinary collaboration at many levels to reinforce commitments and solutions to environmental change and health challenges. For example, the UN’s Joint Liaison Group of the Rio Conventions serves as a platform for biodiversity, desertification, and climate-change discussions and intended collaboration; engagement of additional UN entities, including the WHO, FAO, and the United Nations Framework Convention on Climate Change, could provide broader utility, especially if concrete integration occurs to enable a united voice. On a national level, UN and other intergovernmental organization delegates can also mobilize across sectors, helping to routinize multidisciplinary policymaking and stimulate thinking on co-investments and co-benefits. For example, the WHO, the Convention on Biological Diversity, and the World Organisation for Animal Health have representatives in most countries, many of whom are based at national ministries, and most state parties to these organizations have focal points assigned to them; working groups could be formed to identify common priorities in individual countries or regions that can facilitate synergies or higher level liaison groups across these or other relevant organizations could help to identify key priorities and opportunities for effective action (Table 1 ).
Table 1.
Illustrative Opportunities for Multisectoral Collaboration to Influence and Protect Human Health in Light of Climate and Other Environmental Change∗
| Industry | Electricity | Health | Commercial/Building | Agriculture | Transportation | |
|---|---|---|---|---|---|---|
| Forestry | Health, environmental, and social effect assessment Labor laws affecting supply chain |
More efficient machinery | Selective logging Sustainable forestry Alternative sites |
Green space Density of development Joint planning to prevent sprawl Retrofitting |
Biosecurity Land conversion |
Consolidation of land use |
| Transportation | Solar/electric transport Shipping |
Increasing portion of transport that runs on renewable sources Increasing transportation density |
Active transit | Increasing density of development Mixed land use |
Local suppliers Efficient shipping routes |
|
| Agriculture | Fuel-efficient machinery | Reduce energy needs for food production Biodigesters |
Diversity and nutritional value of cultivars Food safety practices |
Composting/ community gardens | ||
| Commercial/Building | LEED standards Recycled materials | Efficient insulation | Green buildings following LEED standards | |||
| Health | Carbon pricing | Solar power Efficient cookstoves |
||||
| Electricity | Renewable electricity Combining energy stores Microgrids |
|||||
| Co-benefits | Investment in underserved markets and shifts in industry standards | |||||
| Hospital and laboratory capacity | ||||||
| Employee productivity and well-being | ||||||
| Civic engagement | ||||||
| Local businesses and tax base | ||||||
| Ecosystem services critical to human and animal health and well-being | ||||||
LEED, Leadership in Energy & Environmental Design
Opportunities can yield co-benefits that span multiple sectors; decision making can thus consider ways to maximize positive outcomes for health.
National collaborative opportunities would be especially timely as we transition toward the Sustainable Development Goals (SDGs).64 The SDGs will build on the unfinished agenda of the Millennium Development Goals, intended as a strategic direction for international development through 2030. Although the separate goals and detailed targets discussed to date appear to reinforce a siloed approach, there are many potential areas of horizontal integration toward the creation of more sustainable and healthy societies, especially if investments also promote cross-disciplinary implementation. Although goals 3 and 13 are specific to health and climate change respectively, all 17 goals directly or indirectly relate to health and ecological determinants or outcomes. For example, goal 7, to “Ensure access to affordable, reliable, sustainable and modern energy for all”64 is critical for functioning hospitals; as seen in the West Africa Ebola crisis, basic capacities are limited or nonexistent in parts of the world, plaguing health care delivery, diagnostics, and reporting. Ad hoc health care systems capacity investments have been made in the region, but the expected future projects to build capacity in West Africa provide a ripe opportunity to ensure solar energy production or other sustainable infrastructure (in terms of both low-carbon and low ongoing costs). Similarly, under the heading of resilient, safe, and sustainable cities and human settlements, proposed target b for goal 11 prescribes by 2020 “integrated policies and plans towards inclusion, resource efficiency, mitigation and adaptation to climate change, resilience to disasters, develop and implement. . . holistic disaster risk management.”64 Similarly, proposed goal 15 aimed at protecting, restoring, and promoting “sustainable use of terrestrial ecosystems, sustainably manage forests, combat desertification, and halt and reverse land degradation and halt biodiversity loss” is essential to the provision of multiple ecosystem services that promote health and well-being.10 Working from this frame can enable more proactive risk analysis and planning around environmental, social, financial, and health outcomes. Given their catastrophic effect, emerging infectious diseases (such as severe acute respiratory syndrome, estimated at costing the global economy of US$30 billion or more and disruption of trade and travel),65 are a logical inclusion when considering disaster risks faced by society.
Coordination on natural resource planning, in which health aspects are currently limited or superficially incorporated, may be a particularly important role for health professionals. For example, the UN Reducing Emissions from Deforestation and Forest Degradation program, which provides developing nations with monetary incentives to preserve forest areas, could be expanded with the help of health professionals to encompass health benefits or risks of forest conversion or protection scenarios. Financial effects related to disease prevention and preservation of other health-benefitting ecosystem services could be quantified into forest valuations, allowing a fuller assessment of the public good and short- and long-term costs, financial gains or savings expected from land planning decisions and providing a common platform for climate change mitigation and prevention of potential negative health effects associated with deforestation. Multidisciplinary collaboration in natural resource planning has utility for the health community as means for developing upstream intervention or reducing vulnerabilities that may be influenced by climate change or its drivers. For example, decision making on water resource allocation will ideally involve diverse stakeholders, including from public health, agriculture, energy, and natural resource management sectors to anticipate and weigh benefits and adverse effects (eg, positive or negative implications for sea shipping, irrigation access, energy generation, flooding and drought, waterborne disease, and water and food security). Working together, health, ecological, and other professionals can help assemble the expertise and information needed to understand the environmental components that may influence disease risks—for example, anticipating how factors such as forest cover and soil quality affect water absorption and the resulting implications for flooding and associated disease risks.
To promote science-driven decision making as well as research outputs with direct societal utility, full-spectrum collaboration must also occur between scientific communities and policymakers (which may represent governments, corporations, or the public empowered in decision making). This can occur in several ways, including the coproduction of knowledge (eg, coordinated research question generation) and, where findings are not interpretable to direct action, translating relevance to a given sector(s). For example, health scientists could take risk projection findings further to calculate the cost of inaction or the gains of solution scenarios or the scientific community could examine the cumulative health impacts associated with ecosystem alteration, and help to identify and refine implementation strategies to address these challenges in a more coordinated fashion. Even within the scientific community itself, however, collaboration is not routine, despite potential research, understanding, and intervention efficiencies. To promote collaboration across scientific disciplines and bridge research and policy oriented toward sustainability solutions, the Future Earth scientific platform was established in 2014, merging international global change projects representing atmospheric sciences, ecosystem services, health, urbanization, and other disciplines. For this model to be optimized, some baseline challenges will need to be overcome: common metrics and data sharing systems do not currently exist, research investments typically are still oriented to single-discipline approaches, understanding of long-term trends is limited by the short-term nature of research funding, and (outside of clinical medicine) pathways are generally not yet in place for wide-scale research-to-solution processes.
Industry and private-sector collaboration are also crucial for multidisciplinary solutions, but programmatically, health organizations face resource challenges in raising awareness and combatting the ill effects of fossil fuel-related pollution. For example, the WHO’s entire 2014-2015 approved budget (US$3.98 billion) is a stark contrast to the almost $550 billion granted in annual global fossil fuel subsidies.66 The short-term societal focus on profits derived from fossil fuel extraction and consumption have overall represented a major barrier to stronger climate-change regulation. In turn, the public sector has not developed an effective mechanism for protecting global public goods including disease prevention.
Despite these incongruences, private-sector collaboration can be a crucial and high-yield opportunity for global health engagement on climate change threats. Co-investments across sectors, or at least reinforcing ones, have practical value as well. Although typically applied to for-profit contexts, we can consider the process of innovative disruption, which circumvents incumbents to effectively provide an alternative that catches an underserved market or outperforms. Shifting a portion of global health investments from reactionary approaches to preventive capacity could support development of needed renewable technologies such as solar microgrids; building local capacity for installation and maintenance could reduce cost and technological barriers for uptake and use. Capitalizing on voluntary corporate collaboration may be highly fruitful; as of 2012, 1.6% of publically traded companies held more than half of the market value globally, representing enormously powerful interests; gaining their collaboration in sustainable investments could lead to new industry standards.67 Finally, although a survey of company managers suggested only 27% view climate change as a business risk,68 compelling industry losses are at stake from broader ecological changes. For example, outbreaks of Marburg virus in Eastern Africa, associated with human encroachment into wildlife habitat for natural resource extraction, prompted mine closures.69 Adding health to routine environmental and social impact assessment processes for development projects can help identify and mitigate public health risks. There are many opportunities for engagement among those organizations already conscientious of the range of effects (positive and negative) that their investments may have. Multilateral development banks and bilateral aid agencies may be best positioned to lead here given their long histories undertaking impact assessments and diverse expertise, including health. These assessments might include assessment of health inequities of disease burden or disproportionate health-related financial impact to certain populations—infrastructure or systems resiliency can also be assessed and improved to reduce vulnerability of investments under climate change. Risks are also highly relevant to reinsurance companies, as their clients increasingly face climate-related losses that add to volatility of risk management. Reinsurer Swiss Re has articulated that the severity of flooding events will require public-private partnerships in addition to adaptation measures to tackle upcoming challenges.
Prioritizing solutions across many sectors—such as integrating environmental education in curriculum, expanding green energy investments through health grants, encouraging the development of citizen science in civil society, and establishing industry working groups—can help reduce redundancy and increases protection against volatile political situations. Likewise, ensuring the full involvement of local communities, who are in the first line of defense against ecosystem degradation and unsustainable use of resources and are those most affected when these resources are depleted, is equally critical to the success of any prevention, preparedness and response strategy that seeks to jointly optimize health outcomes. Moreover, systematic planning to optimize co-benefits is also essential, and could have enormous cost savings from prevention of negative outcomes. For example, built environment modifications that encourage physical activity (eg, active transit) can help address obesity rates, and if using low-carbon alternatives, in the long term may feed into measures for climate change control.70 Large-scale building investments may rely on privatized investments, but the public sector can take measures to require cross-sectoral land use planning and project review and provide industry incentives, as well as the public infrastructure required for successful business growth.
Conclusion
Benefits yielded from other sectors to human health are already provided every day; for example, engineers design sanitation systems that reduce the prevalence of waterborne diseases through waste removal and increase access to potable water, and farmers (and pollination services) are essential to sustaining food security and nutrition. However, these gains have typically been outside of the direct purview of global health, with the latter largely emphasizing interventions when upstream systems fail (or do not exist at all) and a health risk emerges. Anthropogenic changes are placing novel or exacerbating pressures on health that require complex solutions; to fully address anticipated risks in a meaningful capacity, the global health community must embrace a focus on prevention of known and potential health threats and develop coordinated, coherent, and cross-sectoral strategies that are both representative of and adequately respond to the magnitude of the challenges that we face.
Although we have focused on the importance of global health’s collaboration with other sectors, the role of global health practitioners cannot be overstated for meeting complex societal challenges such as climate change. Health can serve as a leveraging point for other sectors concerned about global environmental change; for example, ecological sciences often state outcomes in abstract language, expressing caveats and parameter limits in outputs from theoretical models, tipping points, or measures such as parts-per-million greenhouse gas concentrations. In contrast, number of lives lost, quantitative impact to productivity, or visible signs of morbidity can be far more tangible to a community and individuals.
Global health professionals can help convey the need for “local solutions for global health” that address context-specific determinants of health (eg, socioeconomic, environmental, behavioral) to promote successful implementation. However, to foster these benefits for shared value, the global health community must more actively engage other sectors to be more proactive in finding preventive solutions, effectively broadening the scope of what constitutes public health. Doing so can yield considerable co-benefits from synergies that may also help address and prevent other current and future health threats—the need is clear and pressing.
Acknowledgments
CM, WBK, and PD acknowledge the generous support provided by the DIVERSITAS-Future Earth ecoHEALTH project and the PREDICT project of the United States Agency for International Development (USAID) Emerging Pandemic Threats program. The authors acknowledge the 2 anonymous reviewers for their constructive comments that improved this paper, as well as Virginia Porter for editorial assistance. All authors had a role in the conceptual development of the paper, compiling background research, writing and reviewing the manuscript.
Footnotes
The authors declare they have no conflicts of interest.
References
- 1.Mutangadura G. World Health Organization; Geneva, Switzerland: 2002. The World Health Report 2002—reducing risks, promoting health life. [Google Scholar]
- 2.IPCC . World Health Organization; Geneva, Switzerland: 2007. Contribution of Working Groups I, II and III to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. [Google Scholar]
- 3.Hajat S., Vardoulakis S., Heaviside C., Eggen B. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68:641–648. doi: 10.1136/jech-2013-202449. [DOI] [PubMed] [Google Scholar]
- 4.McMichael A.J. Globalization, climate change, and human health. N Engl J Med. 2013;368:1335–1343. doi: 10.1056/NEJMra1109341. [DOI] [PubMed] [Google Scholar]
- 5.Confalonieri U., Menne B., Akhtar R. Human health. Climate change. In: Parry M.L., Canziana O.F., Palutikof J.P., editors. Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; Cambridge, UK: 2007. pp. 391–431. [Google Scholar]
- 6.IPCC . IPCC; Geneva, Switzerland: 2014. Climate change 2014: synthesis report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. [Google Scholar]
- 7.Watts N., Adger W.N., Agnolucci P. Health and climate change: policy responses to protect public health. The Lancet. 2015;386(10006):1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva, Switzerland: 2014. Quantitative risk assessment of the effects of climate change on selected causes of death. 2030s and 2050s. [Google Scholar]
- 9.DARA. Climate vulnerability monitor 2nd Ed.: a guide to the cold calculus of a hot planet. Spain 2012. Available at: http://www.thecvf.org/web/publications-data/climate-vulnerability-monitor/2012-monitor/. Accessed August 13, 2015.
- 10.World Health Organization and Convention on Biological Diversity . WHO and SCBD; Geneva, switzerland and Montréal: 2015. Connecting global priorities: biodiversity and human health, a state of knowledge review. [Google Scholar]
- 11.Lloyd J., McCarney S., Ouhichi R., Lydon P., Zaffran M. Optimizing energy for a ‘green’ vaccine supply chain. Vaccine. 2015;33:908–913. doi: 10.1016/j.vaccine.2014.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown L.H., Buettner P.G., Canyon D.V. The energy burden and environmental impact of health services. Am J Public Health. 2012;102:e76–e82. doi: 10.2105/AJPH.2012.300776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . World Health Organization; Geneva, Switzerland: 2013. Protecting health from climate change: vulnerability and adaptation. [Google Scholar]
- 14.Haines A., Kovats R.S., Campbell-Lendrum D., Corvalan C. Climate change and human health: impacts, vulnerability, and mitigation. Lancet. 2006;367:2101–2109. doi: 10.1016/S0140-6736(06)68933-2. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien K.L., Leichenko R.M. Double exposure: assessing the impacts of climate change within the context of economic globalization. Glob Environ Chang. 2000;10:221–232. [Google Scholar]
- 16.Ziska LH, McConnell LL. Climate change, carbon dioxide, and pest biology: monitor, mitigate, manage [e-pub ahead of print]. J Agric Food Chem. Available at: http://pubs.acs.org/doi/abs/10.1021/jf506101h. Accessed June 25, 2015. [DOI] [PubMed]
- 17.Patz J.A., Frumkin H., Holloway T., Vimont D.J., Haines A. Climate change: challenges and opportunities for global health. JAMA. 2014;312:1565–1580. doi: 10.1001/jama.2014.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barriopedro D., Fischer E.M., Luterbacher J., Trigo R.M., García-Herrera R. The hot summer of 2010: redrawing the temperature record map of Europe. Science. 2011;332:220–224. doi: 10.1126/science.1201224. [DOI] [PubMed] [Google Scholar]
- 19.Robine J.-M., Cheung S.L.K., Le Roy S. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biologies. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 20.UN Environmental Program. Impacts of summer 2003 heat wave in Europe. Environmental Alert Bulletin. March 2004.
- 21.Li M., Gu S., Bi P., Yang J., Liu Q. Heat waves and morbidity: current knowledge and further direction—a comprehensive literature review. Int J Environ Res Public Health. 2015;12:5256. doi: 10.3390/ijerph120505256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson H., Kovats R.S., McGregor G. The impact of the 2003 heat wave on mortality and hospital admissions in England. Health Stat Q. 2005;(25):6–11. [PubMed] [Google Scholar]
- 23.Kjellstrom T., Kovats R.S., Lloyd S.J., Holt T., Tol R.S. The direct impact of climate change on regional labor productivity. Arch Environ Occup Health. 2009;64:217–227. doi: 10.1080/19338240903352776. [DOI] [PubMed] [Google Scholar]
- 24.Cutter S.L., Ismail-Zadeh A., Alcantara-Ayala I. Global risks: pool knowledge to stem losses from disasters. Nature. 2015;522:277–279. doi: 10.1038/522277a. [DOI] [PubMed] [Google Scholar]
- 25.United Nations Office for Disaster Risk Reduction . UNISDR; Geneva, Switzerland: 2009. 55 million people affected by extreme weather disasters in 2009. [Google Scholar]
- 26.Cann K.F., Thomas D.R., Salmon R.L., Wyn-Jones A.P., Kay D. Extreme water-related weather events and waterborne disease. Epidemiol Infect. 2013;141:671–686. doi: 10.1017/S0950268812001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burke E.J., Brown S.J., Christidis N. Modeling the recent evolution of global drought and projections for the twenty-first century with the Hadley Centre Climate model. J Hydrometerol. 2006;7:1113–1125. [Google Scholar]
- 28.Arnold W. The New York Times; New York, NY: 2005. Indonesia's Yearly Smoke Cloud Reaches Malaysia and Thailand. Section A5. [Google Scholar]
- 29.Rosenzweig C., Iglesias A., Yang X.B., Epstein P., Chivian E. Climate change and extreme weather events; implications for food production, plant diseases, and pests. Global Change Hum Health. 2001;2:90–104. [Google Scholar]
- 30.Food and Agriculture Organization of the United Nations . FAO; London: 2003. World Agriculture: Towards 2015/2030, An FAO Perspective. [Google Scholar]
- 31.Schmidhuber J., Tubiello F.N. Global food security under climate change. Proc Natl Sci Acad U S A. 2007;104:19703–19708. doi: 10.1073/pnas.0701976104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patz J.A. A human disease indicator for the effects of recent global climate change. Proc Natl Sci Acad U S A. 2002;99:12506–12508. doi: 10.1073/pnas.212467899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Food and Agriculture Organization of the United Nations. Climate-Related Transboundary Pests and Diseases. Paper presented at the Climate Change, Energy and Food Conference; Rome; June 2008.
- 34.Mills J.N., Gage K.L., Khan A.S. Potential influence of climate change on vector-borne and zoonotic diseases: a review and proposed research plan. Environ Health Perspect. 2010;118:1507–1514. doi: 10.1289/ehp.0901389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kovats R.S., Bouma M.J., Hajat S., Worrall E., Haines A. El Niño and health. Lancet. 2003;362:1481–1489. doi: 10.1016/S0140-6736(03)14695-8. [DOI] [PubMed] [Google Scholar]
- 36.Gething P.W., Smith D.L., Patil A.P., Tatem A.J., Snow R.W., Hay S.I. Climate change and the global malaria recession. Nature. 2010;465:342–345. doi: 10.1038/nature09098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Egbendewe-Mondzozo A., Musumba M., McCarl B.A., Wu X. Climate change and vector-borne diseases: an economic impact analysis of malaria in Africa. Int J Environ Res Public Health. 2011;8:913. doi: 10.3390/ijerph8030913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen C., Jenkins E., Epp T., Waldren C., Curry P., Soos C. Climate change and West Nile Virus in a highly endemic region of North America. Int J Environ Res Public Health. 2013;10:3052–3071. doi: 10.3390/ijerph10073052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CDC (Centers for Disease Control and Prevention). Rift Valley fever—East Africa, 1997–1998. Morbidity and Mortality Weekly Report 1998;47:261–264. [PubMed]
- 40.Anyamba A., Linthicum K.J., Small J.L. Climate teleconnections and recent patterns of human and animal disease outbreaks. PLoS Negl Trop Dis. 2012;6:e1465. doi: 10.1371/journal.pntd.0001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhou X.N., Yang G.J., Yang K. Potential impact of climate change on schistosomiasis transmission in China. Am J Trop Med Hyg. 2008;78:188–194. [PubMed] [Google Scholar]
- 42.Black P.F., Butler C.D. One Health in a world with climate change. Rev Sci Tech Ser Sci Hum. 2014;33:465–473. doi: 10.20506/rst.33.2.2293. [DOI] [PubMed] [Google Scholar]
- 43.Loh E.H., Zambrana-Torrelio C., Olival K.J. Targeting transmission pathways for emerging zoonotic disease surveillance and control. Vector Borne Zoonotic Dis. 2015;15:432–437. doi: 10.1089/vbz.2013.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Friel S., Bowen K., Campbell-Lendrum D., Frumkin H., McMichael A.J., Rasanathan K. Climate change, noncommunicable diseases, and development: the relationships and common policy opportunities. Ann Rev Public Health. 2011;32:133–147. doi: 10.1146/annurev-publhealth-071910-140612. [DOI] [PubMed] [Google Scholar]
- 45.Haines A., McMichael A.J., Smith K.R. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet. 2009;374:2104–2114. doi: 10.1016/S0140-6736(09)61759-1. [DOI] [PubMed] [Google Scholar]
- 46.WHO Regional Office for Europe and OECD . WHO Regional Office for Europe; Copenhagen: 2015. Economic cost of the health impact of air pollution in Europe: Clean air, health and wealth. [Google Scholar]
- 47.World Health Organization . WHO; Geneva, Switzerland: 2011. Burden: mortality, morbidity, and risk factors. [Google Scholar]
- 48.Jacobson M.Z. On the causal link between carbon dioxide and air pollution mortality. Geophys Res Lett. 2008;35(3) L03809. [Google Scholar]
- 49.Hajat S., Armstrong B.G., Gouveia N., Wilkinson P. Mortality displacement of heat-related deaths: a comparison of Delhi, Sao Paulo, and London. Epidemiology (Cambridge, Mass) 2005;16:613–620. doi: 10.1097/01.ede.0000164559.41092.2a. [DOI] [PubMed] [Google Scholar]
- 50.Younger M., Morrow-Almeida H.R., Vindigni S.M., Dannenberg A.L. The built environment, climate change, and health: opportunities for co-benefits. Am J Prev Med. 2008;35:517–526. doi: 10.1016/j.amepre.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 51.Intergovernmental Panel on Climate Change (IPCC) IPCC; Geneva, Switzerland: 2014. Working Group II Contribution to the Fifth Assessment Report. [Google Scholar]
- 52.United Nation Refugee Agency . UNHCR; Washington, DC: 2009. Climate change could become the biggest driver of displacement: UNHCR chief. [Google Scholar]
- 53.Stoett P.J. University of Toronto Press; Ontario, Canada: 2012. Global Ecopolitics: Crisis, governance, and justice. [Google Scholar]
- 54.Department of Defense . Office of the Deputy Under Secretary of Defense for Installations and Environment; Washington, DC: 2014. 2014 Climate Change Adaptation Roadmap. [Google Scholar]
- 55.Fezzi C., Harwood A.R., Lovett A.A., Bateman I.J. The environmental impact of climate change adaptation on land use and water quality. Nat Clim Change. 2015;5:255–260. [Google Scholar]
- 56.Kilpatrick A.M., Randolph S.E. Drivers, dynamics, and control of emerging vector-borne zoonotic diseases. Lancet. 2012;380:1946–1955. doi: 10.1016/S0140-6736(12)61151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karesh W.B., Dobson A., Lloyd-Smith J.O. Ecology of zoonoses: natural and unnatural histories. Lancet. 2012;380:1936–1945. doi: 10.1016/S0140-6736(12)61678-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huff A.G., Beyeler W.E., Kelley N.S., McNitt J.A. How resilient is the United States’ food system to pandemics? J Environ Stud Sci. 2015;5(3):337–347. doi: 10.1007/s13412-015-0275-3. Available at: http://link.springer.com/article/10.1007%2Fs13412-015-0275-3#page-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bouley T., Gilbert M., Whung P.-Y., Le Gall F., Plante C. World Bank Group; Washington, DC: 2014. Reducing climate-sensitive disease risks. Agriculture and environmental services discussion paper; no. 7. Available at: http://documents.worldbank.org/curated/en/2014/04/19567115/reducing-climate-sensitive-disease-risks. Accessed June 30, 2015. [Google Scholar]
- 60.Karesh W.B., Cook R.A. The human-animal link. Foreign Aff. 2005;84(4):38–50. [Google Scholar]
- 61.Daszak P., Zambrana-Torrelio C., Bogich T.L. Interdisciplinary approaches to understanding disease emergence: the past, present, and future drivers of Nipah virus emergence. Proc Natl Acad Sci U S A. 2013;110(Suppl 1):3681–3688. doi: 10.1073/pnas.1201243109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Karesh W.B., Cook R.A. One world—one health. Clin Med. 2009;9:259–260. doi: 10.7861/clinmedicine.9-3-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Anyamba A., Small J., Tucker C.J. U.S. Department of Defense Armed Forces Surveillance Center’s Global Emerging Infections Surveillance and Response System (DoD-AFHSC/GEIS), et al.; Washington, DC: 2015. Global Climate Anomalies and Potential Disease risks: 2015-2016—Update: 2015-2016 Disease Risks. [Google Scholar]
- 64.Donoghue D, Kamau M. Zero draft of the outcome document for the UN Summit to adopt the Post-2015 Development Agenda. Available at: http://reggional.blogspot.com/2015/06/post-2015-co-facilitators-release-zero.html. Accessed August 16, 2015.
- 65.Bank World. World Bank; Washington, DC: 2012. People, pathogens and our planet: the economics of one health. [Google Scholar]
- 66.The World Bank . World Bank; Washington, DC: 2015. Mobilizing the billions and trillions for climate finance. [Google Scholar]
- 67.Eccles RG, Serafeim G. Top 1,000 companies wield power reserved for nations. Bloomberg. September 11, 2012.
- 68.Winston A. How much do companies really worry about climate change? Harvard Business Review. March 4, 2015.
- 69.Amman B.R., Nyakarahuka L., McElroy A.K. Marburgvirus resurgence in Kitaka Mine bat population after extermination attempts, Uganda. Emerg Infect Dis. 2014;20:1761–1764. doi: 10.3201/eid2010.140696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Beaglehole R., Bonita R., Horton R. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]


