Abstract
Rhinovirus (RV) is a frequent pathogen in young children, eliciting symptoms ranging from common colds to wheezing illnesses and lower respiratory tract infections. The recently identified RV-C seems to be associated with asthma exacerbations and more severe disease, but results vary. We studied the prevalence and severity of infection with RV in an unselected birth cohort. Children with respiratory symptoms entered the symptomatic arm of the cohort and were compared with asymptomatic children. Severity of wheezing and other respiratory symptoms was registered. Respiratory viruses were evaluated using throat and nasopharyngeal swabs on first presentation and after recovery (wheezing children). RV genotyping was performed on RV-PCR positive samples. RV was the most prevalent respiratory virus and was found in 58/140 symptomatic children (41%), 24/96 (25%) control children and 19/74 (26%) wheezing symptomatic children after recovery (p <0.05) and did not differ between wheezing and non-wheezing symptomatic children—respectively, 42% (38/90) and 40% (20/50). RV-A was the most commonly detected species (40/68, 59%), followed by RV-C (22/68, 32%) and RV-B (6/68, 9%). RV-B was more frequently detected in asymptomatic children (5/6, p <0.05). There was no significant difference in the frequency of RV species between wheezing and non-wheezing symptomatic children. Children with RV mono-infection had more severe symptoms, but no association between RV species and severity of disease was seen. In an unselected birth cohort from the Netherlands with mild respiratory disease RV was the most prevalent respiratory virus. RV(-C) infection was not associated with more severe disease or wheezing.
Keywords: Children, Rhinovirus, RV type C, Unselected birth cohort, Wheezing
Introduction
Rhinovirus (RV) infections account for most respiratory infections in early life, being a major contributing factor to childhood morbidity (reviewed in Kieninger et al. [1]). Furthermore, episodes of RV-induced wheezing are strongly associated with the subsequent development of asthma in high-risk children [2].
Rhinovirus belongs to the genus Enterovirus in the family Picornaviridae. There are over 160 genotypes and serotypes, which are classified into three species; A, B and C [3]. RV infections in childhood cause a variety of clinical presentations ranging from mild ‘common cold’ symptoms to life-threatening lower respiratory tract infections [3]. Using novel molecular detection techniques, RVs were identified as a common cause of bronchiolitis [4], wheezing [5] and pneumonia [6], [7].
The variation in clinical presentation is the subject of ongoing research. Evidence suggests that symptomatic RV infections accentuate an underlying predisposition for the development of asthma, which may be modulated by genetic host factors [8]. On the other hand, RV may also play a causal role in the development of asthma through promoting exaggerated inflammation and airway hyper-responsiveness [9]. The recently identified RV-C [10] was found to be present in the majority of children admitted with wheezing or acute asthma exacerbations and was associated with increased severity of those exacerbations [11], [12], [13]. By contrast, asymptomatic RV-C infections have also been reported in healthy controls [14].
In this study, we studied the presence of RV in symptomatic pre-school children from an unselected birth cohort and compared this with asymptomatic controls and symptomatic children after recovery from wheezing respiratory illnesses of the same birth cohort. This recovered group of wheezing children is of specific interest because they have a high-risk phenotype for the development of asthma later in life [2].
Methods
Participants
This study is part of the EUROPA-trial (Early Unbiased Risk Assessment of Paediatric Asthma), a prospective cohort study in the Netherlands, focusing on prediction of early signs of asthma. Participants were recruited by targeted mailing from an unselected birth cohort of 12 033 infants born in greater Amsterdam and aged between 3 and 20 months at inclusion. Exclusion criteria were a gestational age of <31 weeks or the presence of any manifest illness at inclusion, specifically any pulmonary disorder. A total of 1216 infants were included in the trial after both parents provided consent (Fig. 1 ). At inclusion a structured baseline questionnaire was obtained.
Fig. 1.
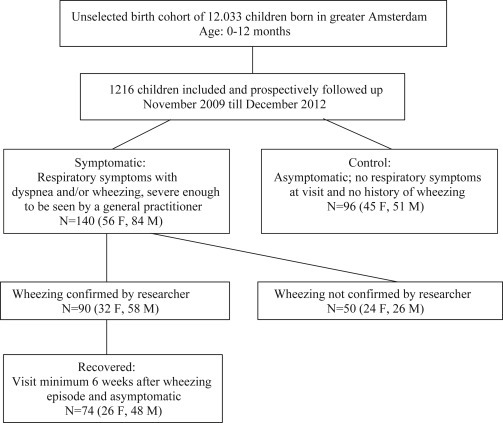
Selection process of children of the EUROPA birth cohort.
Design
This study was designed as a prospective case–control follow-up study. Participating parents were instructed and reminded throughout the study period to contact the study team whenever their infant experienced respiratory tract symptoms from November 2009 until December 2012. The presence of symptoms was assessed using a standardized telephone interview. Infants experiencing cough, wheezing, laboured breathing and/or dyspnoea sufficiently severe for parents to warrant a visit to their general practitioner entered the symptomatic arm of the study and were visited by the study team within 8 hours after establishing these symptoms. If parents refrained from contacting the study team or contacted the study team after visiting the general practitioner and obtaining medical treatment, these children were not included. During the visit, the presence and severity of acute respiratory symptoms were assessed by both parents and the on-site researcher. The researchers were well trained to recognize wheezing. The intra-class correlation was validated by means of evaluation of tracheal sound recordings by five paediatric pulmonologists in the first 30 patients, which reached a Crohnbachs α of 0.75. The study team assessed symptom severity (physician symptom score) by scoring the presence of suprasternal retractions, scalene muscle contraction, air entry and wheezing by auscultation, all part of the Paediatric Respiratory Assessment Measure [15]. Values of the physician symptom score range from 0 to 10 with increasing values indicating increased severity. Parents self-assessed the severity by Asthma Control Questionnaire [15] modified for by-proxy use, although it has not been validated for this application. If wheezing could not be confirmed during the first visit, children were revisited and re-assessed when symptoms recurred. For each child only one symptomatic visit was included in the study.
For our secondary aim we assessed the prevalence of RV infection in asymptomatic children by recruiting controls randomly from the same cohort, who had never experienced lower respiratory tract symptoms severe enough to contact their family physician. The aim was to recruit a control for every included child with confirmed wheezing within 1 month. If lower respiratory tract symptoms still occurred after being visited as a control a novel control was recruited.
Furthermore, children who were evaluated for an episode of respiratory symptoms in this study and were found to have wheezing illness were re-assessed after a symptom-free period of at least 1 week, minimally 6 weeks after their initial presentation. Symptom-free was defined as a physician and parent (Asthma Control Questionnaire-based) severity score of 0.
In addition, regardless of symptoms, parents were asked to fill in bi-annual questionnaires about respiratory symptoms and hospitalizations in the previous months.
This study was approved by the Medical Ethical Committee of the Academic Medical Centre Amsterdam (09/066) and the parents gave written informed consent. The EUROPA study is registered in the Dutch Trial Register (NTR-1955).
Virological analysis
At each visit the study team obtained nasopharyngeal and oropharyngeal swabs (Copan Swabs, Brescia, Italy). The collected nasopharyngeal and oropharyngeal samples were assessed within 1 day after sampling for the presence of respiratory-associated viruses (RV, human enterovirus (EV), human parechovirus, influenza virus A and B, parainfluenzavirus 1, 2, 3 and 4, human bocavirus, human coronavirus, respiratory syncytial virus, adenovirus and human metapneumovirus) using a multiplex PCR as described previously by Jansen et al. [16] with adapted primers for RV (see Supplementary material, Table S1). A Ct-value of 40 or more was considered to be negative [17]. Remaining samples were stored at –80°C and were used for RV typing.
RV typing
RV RNA was extracted from 200 μL RV-positive sample with the MagnaPure LC instrument® using the total nucleic acid isolation kit (Roche Diagnostics). Genotyping was performed by amplifying a 540-base pair fragment spanning part of the 5'- untranslated region, capsid protein VP4 and part of VP2 (VP4/VP2) of the RV-genome using a two-step semi-nested protocol [18].
First, 6 μL of RNA was reverse transcribed and amplified with the SuperScript III one-step RT/Platinum Taq polymerase kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions using primers adapted from Savolainen et al. [19] (see Supplementary material, Table S1) and cycling conditions described by Harvala et al. [20].
One microlitre of the combined RT-PCR product was then used as input for the second semi-nested PCR amplification. The reaction mix contained 1× PCR buffer, 2.5 mm MgCl2, 0.5 μm of each primer, 200 μm of each dNTP, 0.1 mg/L bovine serum albumin and 0.05 U of FastStart Taq polymerase (Roche, Basel, Switzerland) in a 20-μL reaction volume. Cycling conditions were as follows: 94°C for 2 min and 30 cycles each consisting of 94°C (18 seconds), 55°C (21 seconds) and 72°C (90 seconds). Amplicons were sequenced using primers used for the second step of the semi-nested protocol with the BigDye Terminator reaction kit (Applied Biosystems, Foster City, CA, USA). Species were determined by phylogenetically comparing sequences with published reference sequences as proposed and provided by McIntyre et al. [18].
Cross-reactivity of EV with RV was suspected when both EV and RV PCR were positive and typing resulted in an EV type (nine samples) or when only RV PCR was positive and typing resulted in an EV type (two samples). These samples were considered to be EV-positive and RV-negative.
Bacterial co-infection
At each visit a throat swab was collected, which was cultured for respiratory bacterial pathogens according to standard care procedures.
Data analysis
Data were analysed using SPSS for Windows, version 20. Categorical variables were compared by means of chi-square test. Differences between continuous variables were analysed using Student's t-test and one-way analysis of variance test (if normally distributed) or Mann–Whitney U test and Kruskall–Wallis test and for paired continuous variables Wilcoxon signed rank test. A two-sided p-value <0.05 was considered to be significant.
Results
Participant characteristics
A total of 140 symptomatic and 96 asymptomatic children were included in the study (Fig. 1). The median age at inclusion was 9 months (range 3–20 months). Baseline characteristics of all included children are described in Table 1 . Of the 140 symptomatic children, wheezing was confirmed by the study team in 90 children. The median age of the control group (28 months) was significantly higher than of the symptomatic group both during symptoms (15 months, p <0.001) and after recovery (22 months, p <0.001).
Table 1.
Characteristics of included children
| Symptomatic |
Control | Recovered | ||
|---|---|---|---|---|
| RTI with confirmed wheezing | RTI without wheezing | |||
| Number of children | 90 | 50 | 96 | 74 |
| Median age (months, IQR) | 15 (10–25) | 15 (10–24) | 28 (26–31)a | 22 (17–27)a |
| Sex (male:female) | 1.8:1 | 1.1:1 | 1.1:1 | 1.8:1 |
| Bacterial co-infection | 2 (2%) | 1 (2%) | 2 (2%) | 3 (4%) |
| Use of inhaled corticosteroids | 18 (20%) | 10 (20%) | — | — |
| Use of inhaled β2-mimetics | 55 (61%)b | 15 (30%)b | — | — |
| Use of antibiotics | 9 (10%) | 1 (2%) | — | — |
| Hospitalization during visit period | 10/88 (11%) | 3/49 (6%) | 0/96 | |
| Physician symptom-score, median (IQR) | 2 (1–4)b | 0 (0–0)b | — | — |
| mACQ parents, median (IQR) | 15.5 (10–21)b | 11.5 (8–14)b | — | — |
Abbreviations: IQR, interquartile range; mACQ, modified Asthma Control Questionnaire; RTI, respiratory tract infection.
Significant (p <0.05) for symptomatic versus control and control versus recovered.
Significant (p <0.05) for RTI with confirmed wheezing versus RTI without wheezing.
Prevalence and seasonality of RV infections
Overall, in 86% of the symptomatic children a respiratory virus could be detected, compared with 40% in the control group (p <0.001) and 53% in the recovered group (p <0.001, Table 2 ). RV was the most prevalent virus in symptomatic (41%) as well as control (25%) children, and was found significantly more often in symptomatic children (p 0.009, Fig. 2 ). There was no difference in prevalence of RV infections between wheezing (42%) and non-wheezing (40%) symptomatic children. In the recovered group human bocavirus (35%) was the most prevalent virus, followed by RV (26%).
Table 2.
Prevalence of respiratory viruses in symptomatic and asymptomatic (control and recovered) children
| Virus | Symptomatic |
Control | Recovered | ||
|---|---|---|---|---|---|
| Total | Wheeze | No wheeze | |||
| Any virus | 120 (86%) | 79 (88%) | 41 (82%) | 38 (40%)a | 39 (53%)a |
| Rhinovirus | 58 (41%) | 38 (42%) | 20 (40%) | 24 (25%)a | 19 (26%)a |
| Human bocavirus | 41 (29%) | 30 (33%) | 11 (22%) | 7 (7%)a | 26 (35%)b |
| Respiratory syncytial virus | 33 (24%) | 26 (29%) | 7 (14%) | 0a | 2 (3%)a |
| Adenovirus | 18 (13%) | 11 (12%) | 7 (14%) | 0a | 1 (1%)a |
| Para-influenza virus type 3 | 15 (11%) | 11 (12%) | 4 (8%) | 1 (1%)a | 2 (3%)a |
| Enterovirus | 11 (8%) | 6 (7%) | 5 (10%) | 3 (3%) | 4 (5%) |
| Human coronavirus | 9 (6%) | 7 (8%) | 2 (4%) | 2 (2%)a | 8 (11%)b |
| Human parechovirus | 7 (5%) | 5 (6%) | 2 (4%) | 0a | 3 (4%)b |
| Human metapneumovirus | 6 (4%) | 3 (3%) | 3 (6%) | 1 (1%) | 1 (1%) |
| Para-influenza virus type 4 | 5 (4%) | 3 (3%) | 2 (4%) | 1 (1%) | 1 (1%) |
| Para-influenza virus type 2 | 3 (2%) | 2 (2%) | 1 (2%) | 0 | 0 |
| Para-influenza virus type 1 | 2 (1%) | 1 (1%) | 1 (2%) | 0 | 0 |
| Influenza A virus | 2 (1%) | 0 | 2 (4%) | 1 (1%) | 0 |
| Influenza B virus | 1 (1%) | 0 | 1 (2%) | 0 | 0 |
Significant (p <0.05) symptomatic versus control or symptomatic versus visit after recovery.
Significant (p <0.05) control versus visit after recovery.
Fig. 2.
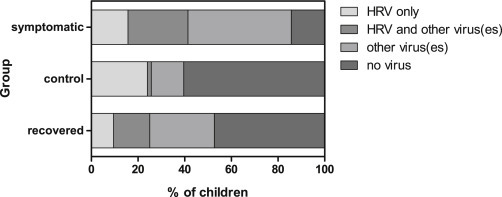
Prevalence of human rhinovirus and non-rhinoviruses in symptomatic and asymptomatic children (controls and recovered).
Symptomatic children with RV infection were significantly younger (median 13.5 months, interquartile range (IQR) 8–20) than symptomatic children who had a negative RV PCR (median 17 months, IQR 13–27, p 0.005). This was also significant in the recovered group (RV PCR-positive children, median 19 months, IQR 16–20, versus RV PCR-negative children, median 24 months, IQR 18–30, p 0.003).
RV was seen all year round (see Supplementary material, Fig. S1A) with a peak during autumn and winter. In the summer >80% of symptomatic children were RV positive compared with only 17% during the winter. The percentage of asymptomatic children (control and recovered) who were RV positive was relatively constant between seasons ranging from 17% to 31%.
Co-infection
In the symptomatic group 44% of the children were infected with two or more viruses, significantly more than children in the control group (2%, p <0.001) and recovered children (26%, p 0.010). In addition, the number of recovered children with two or more viruses was significant higher than in the control group (p <0.001), which was also reflected by a significantly higher total number of viruses detected (mean number of viruses 0.89) in recovered children compared with children in the control group (mean number of viruses 0.42, p <0.001). Co-infection of RV with other viruses was found in 36 of 58 (62%) symptomatic children compared with one out of 24 controls (4%, p <0.001; see Supplementary material, Table S2). For wheezing infants who had recovered from their symptoms, the rate of RV co-infections was similar to that of symptomatic infants (63%).
Prevalence of RV species
Of the RV PCR-positive samples, 68 (67%) could be genotyped (Table 3 ). RV-A and RV-C were equally detected in symptomatic wheezing and non-wheezing children, control and recovered children. RV-B was detected significantly more often in control children (31%) compared with symptomatic children (2%, p 0.001).
Table 3.
Results of molecular typing of human rhinovirus PCR-positive samples
| Rhinovirus species | Species A | Species B | Species C | Total typed/ RV PCR-positive |
|---|---|---|---|---|
| Symptomatic | 25 (58%) | 1 (2%)a | 17 (40%) | 43/58 |
| Wheeze | 17 (63%) | 0 | 10 (37%) | 27/38 |
| No wheeze | 8 (50%) | 1 (6%) | 7 (44%) | 16/20 |
| Control | 8 (50%) | 5 (31%)a | 3 (19%) | 16/24 |
| Recovered | 7 (78%) | 0 | 2 (22%) | 9/19 |
| Total | 40 (59%) | 6 (9%) | 22 (32%) | 68/101 |
Note: % indicates percentage of typeable human rhinoviruses.
p <0.05, symptomatic versus control.
In the subgroup of symptomatic wheezing children, children with RV-C infection were older (median 20 months, IQR 15–27) than children with RV-A infection (median 12 months IQR 8–19, p 0.01).
RV-A infection occurred most frequently in the summer and autumn, and RV-C in winter. RV-A, B and C were evenly distributed across the years studied (see Supplementary material, Fig. S1B).
Symptoms
RV and severity of symptoms
Overall, physician symptom scores were low (range 0–7), indicating that symptoms were generally mild in this unselected cohort. There were no differences in these scores between RV PCR-positive and RV PCR-negative children. In RV PCR-positive children a significantly higher physician symptom score was seen in children with an RV mono-infection compared with RV PCR-positive children co-infected with other viruses (see Supplementary material, Table S3). The physician symptom scores of children infected with different RV species were comparable.
Parental assessment of symptoms (modified Asthma Control Questionnaire) did not agree with the physician symptom score and showed a significantly lower score in RV PCR-positive children compared with RV PCR-negative children (see Supplementary material, Table S3, p 0.02). The modified Asthma Control Questionnaire assessed general symptoms of illness (like fever and intake) and upper respiratory tract symptoms whereas physician symptom-score only assessed the severity of lower respiratory tract symptoms.
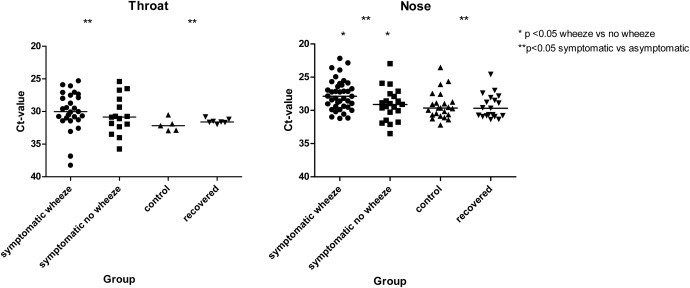
Ct-value and severity
Ct-value was used as a semi-quantitative read-out for viral load. RV PCR Ct-values were significantly lower (indicating a higher viral load) in symptomatic children (throat median Ct-value 30.6, nose median Ct-value 28.6), compared with asymptomatic children (throat median Ct-value 31.7 (p 0.009), nose median Ct-value 29.7 (p 0.006)). Wheezing children had a significantly lower Ct-value than non-wheezing symptomatic children (only nose, median Ct-value 27.9 versus 29.1 p 0.024, throat median Ct-value 30.0 versus 30.9, p 0.28; see Supplementary material, Fig. S2). However, a cut-off value for symptomatic disease could not be determined.
There was no correlation between Ct-value and severity of symptoms in RV-infected symptomatic children.
Discussion
In this study we showed that RV infections were highly prevalent in symptomatic and asymptomatic young children from the general population. RV was detected significantly more often in respiratory swabs from symptomatic children compared with asymptomatic children. Although RV mono-infections (in contrast to co-infections) were associated with a greater clinical severity, RV infections were equally detected in wheezing children compared with non-wheezing symptomatic children in this study, suggesting that other factors (e.g. genetic, immunological, anatomic) may play a role in the pathogenesis of wheezing in young children. However, wheezing RV-infected children had a significantly higher RV viral load.
RV-A and RV-C were the most prevalent species detected in our unselected population. This is in accordance with previous reports [11], [13], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31].
RV-B seemed to be associated with asymptomatic infection in our study, which is in accordance with the findings of Lee et al., who showed that RV-B is less virulent than RV-A and RV-C in a high-risk cohort of young children [21].
The lack of association between wheezing or more severe disease and RV-C infections was shown in other studies of unselected cohorts or non-hospitalized symptomatic children [30], [32]. Other studies, mainly in hospitalized patients, reported an association between RV-C and more severe disease and/or more asthma exacerbations [11], [13], [26], [31], [33]. However, this was not consistently reproduced [14], [22], [27]. A possible explanation for these conflicting studies could be that this association is only seen in susceptible children above a certain age and that in young children other factors (e.g. genetic, immunological, anatomic) play a more important role in the development of wheezing. This is supported by our observation, and those of others [31], that wheezing children with RV-C infection were significantly older than RV-A-infected wheezing children.
Our study indicated that a lower Ct-value (indicating a higher viral load) was associated with symptomatic disease, and within the symptomatic group, with wheezing. Kennedy et al. [34] found no difference in viral load between outpatient wheezing and non-wheezing children, whereas others found that a high viral load was associated with symptomatic disease [16] and an increased risk of lower respiratory tract infections [27], but not with more severe symptoms [35].
A significantly higher number of (co-infecting) viruses was found after recovery from symptoms compared with controls. It is possible that wheezing children are more prone to (asymptomatic) carriage of viruses, compared with non-wheezing children, although the number of detected viruses during the symptomatic visit was equal in wheezing and non-wheezing children. In our study, control children were significantly older than recovered children, making it impossible to draw conclusions from this observation alone.
There are several limitations of this study: as a result of the study design (a new control was recruited if a previous control became symptomatic), the children in the control group were significantly older than the symptomatic infants, which leads to a possible bias in the comparison of prevalence between symptomatic and asymptomatic children.
Of the symptomatic infants, 44% were infected by multiple viruses. Although this is in accordance with previous studies [13], [22], [29], [36], [37], it is likely to influence the analysis of associations between RV species and clinical severity. Remarkably, we found that children with an RV mono-infection had more severe symptoms compared with children with RV and a co-infection. Other hospital-based studies found that co-infection with RSV is associated with an increased severity and/or a longer duration of hospitalization [13], [37]. In our cohort the rate of co-infection with RSV was low.
Another limitation of this study is the sample size. In this cohort, which consists mainly of children with mild symptoms, small differences could have been missed. As the inclusion of symptomatic children was dependent on the reporting of parents, some episodes could have been missed because parents refrained from contacting the study team. Therefore it is difficult to draw clear conclusions from this study alone and larger studies are needed to confirm these results.
In conclusion, in an unselected birth cohort from the Netherlands with mild respiratory disease we found a high prevalence of (multiple) respiratory viruses with RV being the most prevalent. We found no difference in prevalence of RV or RV-C infection between wheezing and non-wheezing symptomatic children, although a higher RV viral load was seen in wheezing children. More studies in large populations are necessary to find out the role of RV-C in unselected young children.
Acknowledgements
We would like to thank all children and parents participating in the EUROPA study.
Part of this work has been presented at the annual congress of the European Society for Paediatric Infectious Diseases and the European Respiratory Society and the European Congress of Virology.
Editor: E. Bottieau
Footnotes
Additional Supporting Information may be found in the online version of this article at http://dx.doi.org/10.1016/j.cmi.2016.05.022.
Funding
The EUROPA study was supported by a grant from the Dutch Lung Foundation.
Transparency declaration
The authors declare that they have no conflicts of interest.
Appendix A. Supplementary material
The following supplementary materials are available for this article:
Table S1. Primers used for rhinovirus PCR and genotyping. (a) Primers (5′ → 3′) used for rhinovirus PCR. (b) Primers used for genotyping human rhinovirus.
Table S2. Frequencies of human rhinovirus co-infections with different viruses.
Table S3. Severity scores and symptoms of symptomatic children.
Fig. S1.
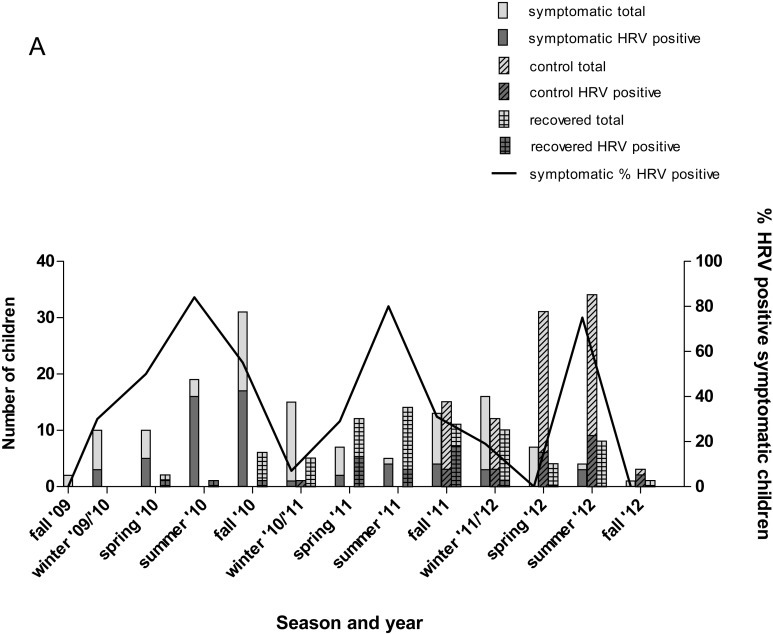
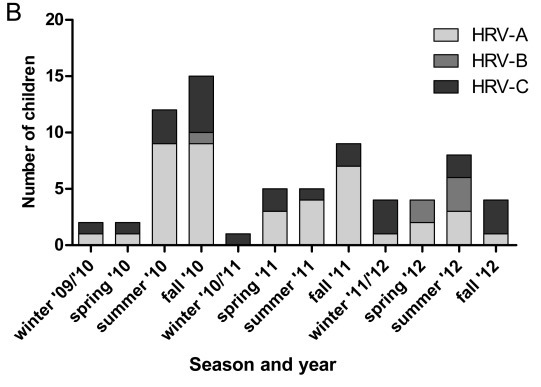
Human rhinovirus (RV) and RV types in different seasons and years. (a) Number of RV-positive children in different seasons and years in symptomatic, control and recovered children. (b) Distribution of RV-A, -B and –C across seasons and years.
Fig. S2.
Human rhinovirus (RV) Ct-value in symptomatic (wheezing and non-wheezing), control and recovered children.
References
- 1.Kieninger E., Fuchs O., Latzin P., Frey U., Regamey N. Rhinovirus infections in infancy and early childhood. Eur Respir J. 2013;41:443–452. doi: 10.1183/09031936.00203511. [DOI] [PubMed] [Google Scholar]
- 2.Jackson D.J., Gangnon R.E., Evans M.D., Roberg K.A., Anderson E.L., Pappas T.E. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobs S.E., Lamson D.M., St G.K., Walsh T.J. Human rhinoviruses. Clin Microbiol Rev. 2013;26:135–162. doi: 10.1128/CMR.00077-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papadopoulos N.G., Moustaki M., Tsolia M., Bossios A., Astra E., Prezerakou A. Association of rhinovirus infection with increased disease severity in acute bronchiolitis. Am J Respir Crit Care Med. 2002;165:1285–1289. doi: 10.1164/rccm.200112-118BC. [DOI] [PubMed] [Google Scholar]
- 5.Korppi M., Kotaniemi-Syrjanen A., Waris M., Vainionpaa R., Reijonen T.M. Rhinovirus-associated wheezing in infancy: comparison with respiratory syncytial virus bronchiolitis. Pediatr Infect Dis J. 2004;23:995–999. doi: 10.1097/01.inf.0000143642.72480.53. [DOI] [PubMed] [Google Scholar]
- 6.Juven T., Mertsola J., Waris M., Leinonen M., Meurman O., Roivainen M. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19:293–298. doi: 10.1097/00006454-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Louie J.K., Roy-Burman A., Guardia-Labar L., Boston E.J., Kiang D., Padilla T. Rhinovirus associated with severe lower respiratory tract infections in children. Pediatr Infect Dis J. 2009;28:337–339. doi: 10.1097/INF.0b013e31818ffc1b. [DOI] [PubMed] [Google Scholar]
- 8.Caliskan M., Bochkov Y.A., Kreiner-Moller E., Bonnelykke K., Stein M.M., Du G. Rhinovirus wheezing illness and genetic risk of childhood-onset asthma. N Engl J Med. 2013;368:1398–1407. doi: 10.1056/NEJMoa1211592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneider D., Hong J.Y., Popova A.P., Bowman E.R., Linn M.J., McLean A.M. Neonatal rhinovirus infection induces mucous metaplasia and airways hyperresponsiveness. J Immunol. 2012;188:2894–2904. doi: 10.4049/jimmunol.1101391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee W.M., Kiesner C., Pappas T., Lee I., Grindle K., Jartti T. A diverse group of previously unrecognized human rhinoviruses are common causes of respiratory illnesses in infants. PLoS ONE. 2007;2:e966. doi: 10.1371/journal.pone.0000966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mak R.K., Tse L.Y., Lam W.Y., Wong G.W., Chan P.K., Leung T.F. Clinical spectrum of human rhinovirus infections in hospitalized Hong Kong children. Pediatr Infect Dis J. 2011;30:749–753. doi: 10.1097/INF.0b013e31821b8c71. [DOI] [PubMed] [Google Scholar]
- 12.Bizzintino J., Lee W.M., Laing I.A., Vang F., Pappas T., Zhang G. Association between human rhinovirus C and severity of acute asthma in children. Eur Respir J. 2011;37:1037–1042. doi: 10.1183/09031936.00092410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller E.K., Khuri-Bulos N., Williams J.V., Shehabi A.A., Faouri S., Al Jundi I. Human rhinovirus C associated with wheezing in hospitalised children in the Middle East. J Clin Virol. 2009;46:85–89. doi: 10.1016/j.jcv.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwane M.K., Prill M.M., Lu X., Miller E.K., Edwards K.M., Hall C.B. Human rhinovirus species associated with hospitalizations for acute respiratory illness in young US children. J Infect Dis. 2011;204:1702–1710. doi: 10.1093/infdis/jir634. [DOI] [PubMed] [Google Scholar]
- 15.Juniper E.F., O'Byrne P.M., Guyatt G.H., Ferrie P.J., King D.R. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14:902–907. doi: 10.1034/j.1399-3003.1999.14d29.x. [DOI] [PubMed] [Google Scholar]
- 16.Jansen R.R., Wieringa J., Koekkoek S.M., Visser C.E., Pajkrt D., Molenkamp R. Frequent detection of respiratory viruses without symptoms: toward defining clinically relevant cutoff values. J Clin Microbiol. 2011;49:2631–2636. doi: 10.1128/JCM.02094-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benschop K., Molenkamp R., van der Ham A., Wolthers K., Beld M. Rapid detection of human parechoviruses in clinical samples by real-time PCR. J Clin Virol. 2008;41:69–74. doi: 10.1016/j.jcv.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 18.McIntyre C.L., Knowles N.J., Simmonds P. Proposals for the classification of human rhinovirus species A, B and C into genotypically assigned types. J Gen Virol. 2013;94:1791–1806. doi: 10.1099/vir.0.053686-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Savolainen C., Mulders M.N., Hovi T. Phylogenetic analysis of rhinovirus isolates collected during successive epidemic seasons. Virus Res. 2002;85:41–46. doi: 10.1016/s0168-1702(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 20.Harvala H., Robertson I., William Leitch E.C., Benschop K., Wolthers K.C., Templeton K. Epidemiology and clinical associations of human parechovirus respiratory infections. J Clin Microbiol. 2008;46:3446–3453. doi: 10.1128/JCM.01207-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee W.M., Lemanske R.F., Jr., Evans M.D., Vang F., Pappas T., Gangnon R. Human rhinovirus species and season of infection determine illness severity. Am J Respir Crit Care Med. 2012;186:886–891. doi: 10.1164/rccm.201202-0330OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calvo C., Casas I., Garcia-Garcia M.L., Pozo F., Reyes N., Cruz N. Role of rhinovirus C respiratory infections in sick and healthy children in Spain. Pediatr Infect Dis J. 2010;29:717–720. doi: 10.1097/INF.0b013e3181d7a708. [DOI] [PubMed] [Google Scholar]
- 23.Franco D., Delfraro A., Abrego L., Cano M., Castillo C., Castillo M. High genetic diversity and predominance of Rhinovirus A and C from Panamanian hospitalized children under five years with respiratory infections. Virol J. 2012;9:257. doi: 10.1186/1743-422X-9-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henquell C., Mirand A., Deusebis A.L., Regagnon C., Archimbaud C., Chambon M. Prospective genotyping of human rhinoviruses in children and adults during the winter of 2009-2010. J Clin Virol. 2012;53:280–284. doi: 10.1016/j.jcv.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 25.Lau S.K., Yip C.C., Lin A.W., Lee R.A., So L.Y., Lau Y.L. Clinical and molecular epidemiology of human rhinovirus C in children and adults in Hong Kong reveals a possible distinct human rhinovirus C subgroup. J Infect Dis. 2009;200:1096–1103. doi: 10.1086/605697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pierangeli A., Ciccozzi M., Chiavelli S., Concato C., Giovanetti M., Cella E. Molecular epidemiology and genetic diversity of human rhinovirus affecting hospitalized children in Rome. Med Microbiol Immunol. 2013;202:303–311. doi: 10.1007/s00430-013-0296-z. [DOI] [PubMed] [Google Scholar]
- 27.Piralla A., Lilleri D., Sarasini A., Marchi A., Zecca M., Stronati M. Human rhinovirus and human respiratory enterovirus (EV68 and EV104) infections in hospitalized patients in Italy, 2008–2009. Diagn Microbiol Infect Dis. 2012;73:162–167. doi: 10.1016/j.diagmicrobio.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 28.Rahamat-Langendoen J.C., Riezebos-Brilman A., Hak E., Scholvinck E.H., Niesters H.G. The significance of rhinovirus detection in hospitalized children: clinical, epidemiological and virological features. Clin Microbiol Infect. 2013;19:E435–E442. doi: 10.1111/1469-0691.12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fry A.M., Lu X., Olsen S.J., Chittaganpitch M., Sawatwong P., Chantra S. Human rhinovirus infections in rural Thailand: epidemiological evidence for rhinovirus as both pathogen and bystander. PLoS ONE. 2011;6:e17780. doi: 10.1371/journal.pone.0017780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackay I.M., Lambert S.B., Faux C.E., Arden K.E., Nissen M.D., Sloots T.P. Community-wide, contemporaneous circulation of a broad spectrum of human rhinoviruses in healthy Australian preschool-aged children during a 12-month period. J Infect Dis. 2013;207:1433–1441. doi: 10.1093/infdis/jis476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Linder J.E., Kraft D.C., Mohamed Y., Lu Z., Heil L., Tollefson S. Human rhinovirus C: age, season, and lower respiratory illness over the past 3 decades. J Allergy Clin Immunol. 2013;131:69–77. doi: 10.1016/j.jaci.2012.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moreira L.P., Kamikawa J., Watanabe A.S., Carraro E., Leal E., Arruda E. Frequency of human rhinovirus species in outpatient children with acute respiratory infections at primary care level in Brazil. Pediatr Infect Dis J. 2011;30:612–614. doi: 10.1097/INF.0b013e31820d0de3. [DOI] [PubMed] [Google Scholar]
- 33.Piralla A., Rovida F., Campanini G., Rognoni V., Marchi A., Locatelli F. Clinical severity and molecular typing of human rhinovirus C strains during a fall outbreak affecting hospitalized patients. J Clin Virol. 2009;45:311–317. doi: 10.1016/j.jcv.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy J.L., Shaker M., McMeen V., Gern J., Carper H., Murphy D. Comparison of viral load in individuals with and without asthma during infections with rhinovirus. Am J Respir Crit Care Med. 2014;189:532–539. doi: 10.1164/rccm.201310-1767OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jansen R.R., Schinkel J., Dek I., Koekkoek S.M., Visser C.E., de Jong M.D. Quantitation of respiratory viruses in relation to clinical course in children with acute respiratory tract infections. Pediatr Infect Dis J. 2010;29:82–84. doi: 10.1097/INF.0b013e3181b6de8a. [DOI] [PubMed] [Google Scholar]
- 36.Jartti T., Lee W.M., Pappas T., Evans M., Lemanske R.F., Jr., Gern J.E. Serial viral infections in infants with recurrent respiratory illnesses. Eur Respir J. 2008;32:314–320. doi: 10.1183/09031936.00161907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mansbach J.M., Piedra P.A., Teach S.J., Sullivan A.F., Forgey T., Clark S. Prospective multicenter study of viral etiology and hospital length of stay in children with severe bronchiolitis. Arch Pediatr Adolesc Med. 2012;166:700–706. doi: 10.1001/archpediatrics.2011.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


