Abstract
Highly infectious diseases (HIDs) are defined as being transmissible from person to person, causing life-threatening illnesses and presenting a serious public health hazard. In most European Union member states specialized isolation facilities are responsible for the management of such cases. Ground ambulances are often affiliated with those facilities because rapid relocation of patients is most desirable. To date, no pooled data on the accessibility, technical specifications and operational procedures for such transport capacities are available. During 2009, the ‘European Network for HIDs’ conducted a cross-sectional analysis of hospitals responsible for HID patients in Europe including an assessment of (a) legal aspects; (b) technical and infrastructure aspects; and (c) operational procedures for ground ambulances used for HID transport. Overall, 48 isolation facilities in 16 European countries were evaluated and feedback rates ranged from 78% to 100% (n = 37 to n = 48 centres). Only 46.8% (22/47) of all centres have both national and local guidelines regulating HID patient transport. If recommended, specific equipment is found in 90% of centres (9/10), but standard ambulances in only 6/13 centres (46%). Exclusive entrances (32/45; 71%) and pathways (30/44; 68.2%) for patient admission, as well as protocols for disinfection of ambulances (34/47; 72.3%) and equipment (30/43; 69.8%) exist in most centres. In conclusion, the availability and technical specifications of ambulances broadly differ, reflecting different preparedness levels within the European Union. Hence, regulations for technical specifications and operational procedures should be harmonized to promote patient and healthcare worker safety.
Keywords: Ambulances, Communicable diseases, Critical pathway, European Union, Infection control, Patient isolation, Transportation of patients
Introduction
Highly infectious diseases (HIDs) such as viral haemorrhagic fevers (VHFs) are considered to be transmissible from person to person, causing a life-threatening illness and presenting a serious hazard to the public, demanding specific control measures [1]. Within the last decades, several events caused by imported VHFs raised the attention of the European Commission (EC) to strengthen the level of preparedness [2], [3], [4]. Furthermore, the emergence of highly-pathogenic respiratory infections (e.g. SARS coronavirus and zoonotic Influenza A viruses), the outbreak of enterohaemorrhagic Escherichia coli infections in Germany and the emerging trends of Crimean–Congo haemorrhagic fever depict the need of a well-prepared health system when facing a large number of patients with known or unknown infectious agents, routes of transmission and sources of infection [5], [6], [7], [8], [9], [10].
Following the United States anthrax events financial funds were allocated to train front-line care clinicians, to strengthen diagnostic infrastructure and to (re-)construct clinical facilities to identify, confirm and care for HIDs [1], [11], [12], [13], [14]. In Europe, specialized isolation facilities such as ‘High Level Isolation Units’ are held responsible for the management of cases in a safe clinical environment that minimizes risks for the personnel but allows state-of-the-art critical care [1]. Most often, isolation facilities are located in areas at risk for the occurrence of HIDs such as highly populated cities or are co-located with BSL-4 laboratories and international airports [15]. In contrast, experience gained from VHFs imported to Europe highlighted the fact that suspected cases are often not directly referred to isolation facilities but are encountered in standard hospitals not equipped to provide mid- or long-term care under strict infection control regimens [2], [16]. Hence, patients may need to be relocated to the closest isolation facility available if the clinical conditions allow transportation, although risks for personnel and patients en route must be considered [17].
The ‘European Network for Highly Infectious Diseases’ (EuroNHID) is a network of 16 European infectious diseases clinicians and public health specialists from 15 member states with experience in the management of HIDs, especially imported VHFs. Between 2007 and 2010 EuroNHID designed and conducted a cross-sectional analysis of European isolation facilities. The capacity, equipment and operational policy of 48 isolation facilities in 16 nations were assessed using checklists. Data collected represent the first pooled data set on the capacity of European isolation facilities [15], [18]. This article depicts results on transport capacities, focusing on ground ambulances with respect to legal aspects, technical and infrastructure aspects, and operational procedures.
Methods
Network structure
EuroNHID was funded by the EC/DG SANCO (EU contract No. 2006205) for a period of 42 months between 2007 and 2010, led by Dr G. Ippolito and managed by a Coordination Team, based at the National Institute for Infectious Diseases in Rome, Italy. For the identification of project partners, national health authorities in all European Union (EU) member states were contacted by the Coordination Team, and asked to suggest specialists with expertise in HID management as national representatives. A project Steering Committee including partners from France, Germany, Greece, the UK, and the Coordination Team, was constituted at the beginning of the project and actively contributed to all scientific aspects of the project.
Development of checklists for data collection
The Steering Committee identified topics and items to be explored by checklists, reflecting partners' experiences, available literature, preparedness plans, as well as guidelines of international authorities for the management of HIDs. Three checklists were developed: (a) hospital resources, (b) hospital procedures, and (c) healthcare worker safety [18]. With regard to patient transport capacities a literature search was conducted using, for example, the terms transportation of patients; MEDEVAC; ambulances, communicable diseases; communicable disease control/methods; containment of biohazards/methods; infection control; patient isolation.
In total, four aspects of patient transport were identified and reflected by 15 questions in chapter E of checklist (b). In detail, three questions covered legal aspects; five covered technical specifications and infrastructure, and seven covered operational procedures. The list of selected topics and questions was sent to, discussed with and approved by all national partners in August 2008. Checklists were designed as survey tools only, and were not intended to define mandatory requirements. To evaluate the feasibility of the checklists, network partners conducted a preliminary data collection at their isolation facilities (n = 4) and gave feedback on possible misinterpretations and gaps encountered.
Results
Identification of centres, data acquisition and analysis
A total of 48 centres in 16 European countries were identified by national representatives and surveyed (range 1–12 centres per country, median 2). Until the end of 2009 checklists were disseminated, data provided were verified by on-site visits of a Coordination Team member and analysed. Feedback rates for questions regarding patient transport ranged from 78% to 100% (n = 37 to n = 48 centres), defining the individual denominator for results presented.
Legal aspects
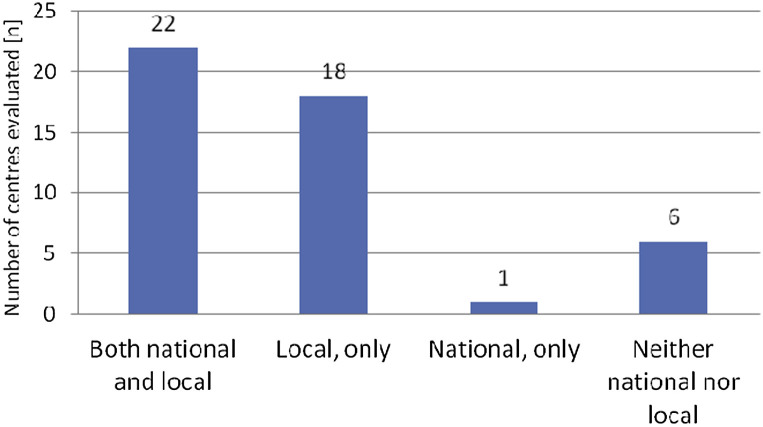
Twenty-two (46.8%) of the 47 centres did provide both national regulations and local protocols for patient transport, whereas six centres had none for the management of transport aspects (Fig. 1 ). National regulations for HID transport by ground ambulances existed in 24/47 centres (51%), whereas local protocols existed in 40/47 centres (85%). Half of the centres without protocols were located within the same country as other centres providing protocols, reflecting different levels of preparedness within single nations.
Fig. 1.
Availability of national and local protocols defining modes of transportation and technical specifications of ambulances used (number of valid answers: n = 47 from 48 centres).
When they existed, local protocols regulated both internal (within the hospital) and external (to or from the hospital) relocation of patients in the most cases (30/40; 75%). Regulations for internal transport only existed in 8/40 centres (20%). Furthermore, one-third of all centres indicated that they had regulations for the international repatriation of HID patients (15 centres from five countries; data not shown).
Technical and infrastructure aspects
Technical aspects assessed included either specifically designed or reserved standard ambulances as well as stretcher isolators. Twenty-six (61.9%) of 44 centres providing information indicated that there was access to equipment, whereas 18/44 (40.9%) centres were fully unequipped. Specifically equipped ambulances were available in 13 centres, reserved standard ambulances in 17 centres, and stretcher isolators in 13 centres. One-third of all centres (15/44; 34.1%) provided more than one of those items (e.g. specifically equipped plus reserved standard ambulances in four centres).
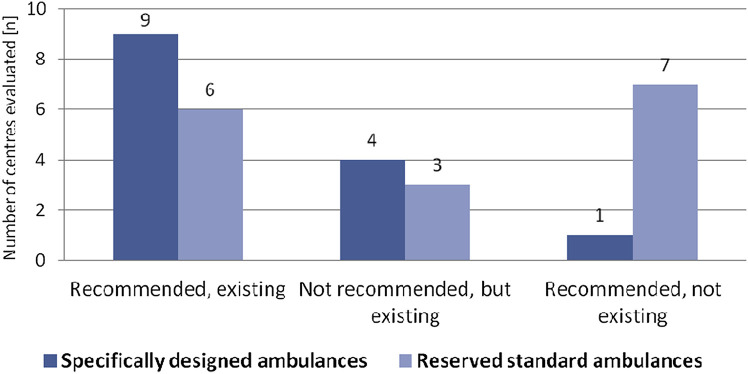
Specifically equipped ambulances or reserved standard ambulances are recommended by national authorities in three and two countries, respectively, representing 10 and 13 centres (Fig. 2 ). Hence, only 5 of 16 nations included in this survey do regulate the use and technical level of ground ambulances. When recommended, 90% of centres adhered to the use of specifically equipped ambulances (9/10). In addition, four centres had such ambulances although they were not recommended. In contrast, only half of all centres had access to reserved standard ambulances, if recommended (6/13; 46%), but four centres did provide such vehicles in the absence of a national regulation.
Fig. 2.
Existence of either specifically designed or reserved standard ambulances for HID patient transport with respect to national recommendations (number of valid answers: n = 44 from 47 centres).
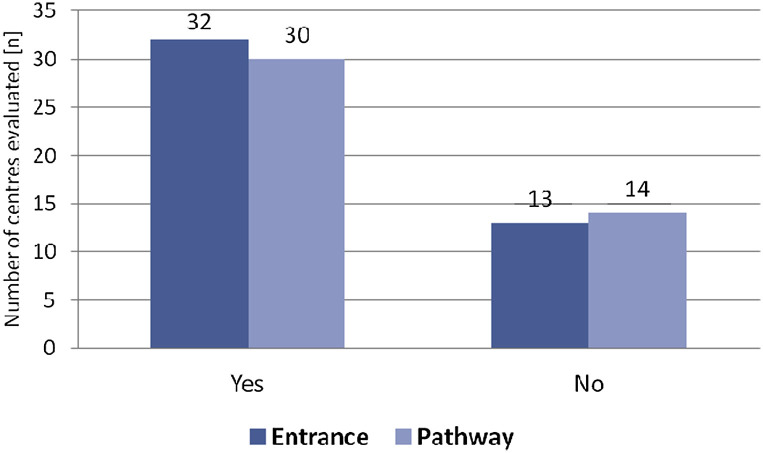
To promote bio-security and prevent nosocomial transmission of infections, exclusive and safe entrances and pathways for either unloading patients from ambulances or transporting them within a hospital are considered necessary. Such requirements were fulfilled in the majority of centres (32/45; 71% and 30/44; 68.2%, respectively) (Fig. 3 ). Except for one, centres providing none of these requirements did not have access to transportation equipment (8/9; 88.9%).
Fig. 3.
Existence of both exclusive and safe entrances and pathways when delivering at or transporting patients within a hospital (number of valid answers: n = 45 and n = 44 of 47 centres, respectively).
Operational procedures
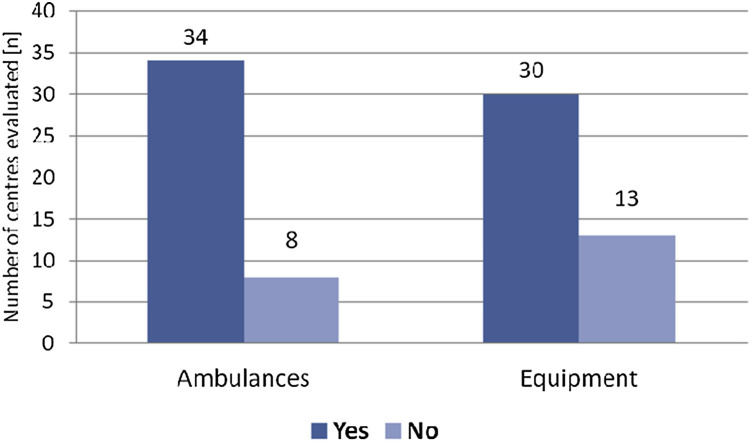
Protocols defining procedures for the disinfection of either ambulances or equipment existed in the majority of centres (34/47; 72.3% and 30/43; 69.8%, respectively) (Fig. 4 ). Both surface disinfection and fumigation of the ambulance cabin were conducted in 11/47 centres (23.4%), whereas surface disinfection only was considered sufficient in 18 other centres. For stretcher isolators, only 2/13 centres using such equipment could not provide specific disinfection protocols (data not shown).
Fig. 4.
Existence of protocols for the disinfection of ambulances and equipment used en route (number of valid answers: n = 40 of 48 centres).
Operational management procedures for loading and unloading of patients existed in 30 centres (data not shown). Most often, such procedures were promoted by practical exercises (20/30; 66.6%) or lectures (19/40; 47.5%). However, periodic training is conducted in a median of 6 months by 21 centres (range 1–24 months), and permanent reminders for procedures such as posters or other visual tools (e.g. videos) are infrequent (5/40 centres, each; 12.5%).
Discussion
Highly infectious diseases such as VHFs remain a public health concern in the EU. Efforts to harmonize first response, medical care or the design of isolation facilities have been the focus of funding in the last decade but to date no pooled data on the capacity and equipment of such facilities exist [1], [11], [12], [13], [14], [15]. Basic recommendations for transporting HID patients were agreed on in the EUNID consensus but the absence of EU-wide legally binding regulations led to a broad range of individual concepts adapted to local prerequisites [1]. Overall, the different solutions implemented depend greatly on national legislation, the availability of vehicles and funds, geography, population density and public health threats or challenges faced in the past in the affected country [17].
Within those member states assessed, the number of centres ranged widely, representing differences in population density, funds available, or experiences with and preparedness concepts for HIDs. Using checklists for this cross-sectional analysis highly depended on the reliability of centres included, although personal on-site visits helped to reduce misinterpretation of the questionnaire [18].
In the spirit of the EUNID consensus, centres included in this analysis are highly specialized facilities designed to provide care for single cases or small clusters of HIDs, only, and do not represent an alternative to surge capacity planning when facing major epidemics and a large number of cases in biological mass casualty incidents [1]. Hence, recommendations for ground ambulances affiliated with such facilities are not considered applicable to large outbreaks. In the USA, a comparable statement for small-scale events has been agreed on [19]. Hence, shortage of equipment or critical care capacity and the sufficient use of dispatch systems to prioritize capacities do not play a major role here as in other mass casualty incidents [20], [21]. However, providing adequate equipment and vehicles to relocate HID patients remains a critical aspect of preparedness as any mode of transport poses a risk to the patient, personnel on board and the public [17], [22]. The examples of imported VHFs mentioned here underline the need to cope with such situations [2], [3], [4], and in countries with endemic outbreaks of VHFs patients may also need to be transferred to specialized facilities to receive appropriate medical care.
As ground ambulances are prerequisites of any Emergency Medical Service in Europe, data collected in this study did not include aeromedical transport concepts. Despite the increasing role of aircraft in trauma care, their use for repatriation of VHF patients is limited and even prohibited by international regulations [23], [24], [25], [26]. In addition, training of paramedics for biological events and ground ambulances are broadly accessible, although varying in concepts and outcome [27], [28]. Although required by some of the member states evaluated, the absence of specifically equipped ambulances or of an infection control regimen exceeding the use of droplet precautions for staff did not result in secondary cases of imported VHFs to Europe [2], [3], [4], [17]. Hence, and in accordance with international guidelines applicable even to smallpox, specific equipment of ambulances is not considered essential by the EUNID consensus [1]. Also, the US consensus considers special air-handling system equipment an ‘ideal’ situation, not an absolute condition [19]. Nevertheless, allocation of ambulances for HID transport in reduced resource settings may lead to critical shortage for more common medical emergencies such as trauma care. However, in contrast to mass casualties, focusing on small numbers of patients allows an increased attention to the level of infection control policies applied en route and after a patient was delivered to the respective isolation facility. Although infection control regulations for multi-resistant bacteria or other less contagious agents may be sufficient for VHFs, the SARS outbreak in Canada led to a significant shortage of emergency medical service personnel [22], [29].
In conclusion, ground ambulance transportation of patients with HIDs lacks a common approach in Europe and remains a neglected problem of preparedness plans for small-scale biological events. Although the need for reserved or even specifically equipped ambulances is debatable and highly depends on the available resources, data collected depict the awareness for the problems even when specific equipment is not available or recommended nationally. Within the EU, cases can occur in close proximity to countries other than the one initially affected and a patient may have to be relocated to the closest isolation facility available, even if not in the same member state. Hence, besides a harmonized approach defining minimal technical requirements, a legal frame for cross-border relocations is needed (See Table 1 ).
Table 1.
Definitions
| Highly infectious diseases |
| Highly infectious diseases (HIDs) are bacterial or viral infections characterized as (a) being easily transmissible from person-to-person; (b) causing life-threatening illness; and (c) presenting a serious hazard in healthcare settings and in the community, requiring specific control measures [1]. |
| National regulations |
| National regulations are defined as laws and recommendations issued by either Ministries (e.g. Ministry of Health) or national institutions (e.g. for occupational health) that must be adhered to by hospitals included in the analysis. |
| Local protocols |
| Local protocols are defined as Standard Operation Procedures (SOPs) defining the operational management of HID transport within, to or from the respective isolation facility including clinical care, infection control, disinfection and team management en route. SOPs are written, regularly updated protocols and instructions covering operations, which lend themselves to a definite or standardized procedure without loss of effectiveness. SOPs should be accessible to all staff at any time-point to allow adherence to established procedures [1]. |
| Specifically designed ambulance |
| Ground ambulances are defined as ‘specifically designed’ for the transportation of HID patients if the ambulance itself and any fixed equipment used can be effectively decontaminated (by wiping, spraying, or fogging with an effective disinfectant) according to national policy. Specific technical features on board may include controlled ventilation, negative pressure, HEPA filtration, intercom systems, aerosol tight storage containers and separation of driver's cabin from patient's cabin [1], [16], [17]. |
| Reserved standard ambulance |
| Reserved ground ambulances for the transportation of HID patients are defined as standard ambulances without additional technical features (see above) but available on call when demanded. Reserved ground ambulances may have easy-to-decontaminate cabin walls and equipment. Strategies should be in place to protect both paramedics and drivers from infectious agents, including the availability of appropriate Personal Protective Equipment [16], [17]. |
| Stretcher isolators |
| Stretcher isolators are defined as portable, self-containment isolation beds, generating negative pressure inside the patient's cabin/area and exhausting HEPA-filtered air (so called ‘Trexler isolators’) [30]. |
Transparency declaration
The authors declare that they have no conflicts of interest.
Acknowledgements
The authors would like to thank all EuroNHID partners for the fruitful discussion and input given: Norbert Vetter (Austria), Mira Kojouharova (Bulgaria), Kremena Parmakova (Bulgaria), Peter Skinhoej (Denmark), Heli Siikamaki (Finland), Christian Perronne (France), Olga Adrami (Greece), John Lambert (Republic of Ireland), Simone Lanini (Italy), Robert Hemmer (Luxembourg), Michael Borg (Malta), Anne Lise Fjellet (Norway), Arne Broch Brantsæter (Norway), Andrzej Horban (Poland), Franc Strle (Slovenia), Antoni Trilla (Spain). We also thank Ramona Iacovino for administrative assistance and all European centres for data contribution.
Contributor Information
for the EuroNHID Study-group:
Norbert Vetter, Mira Kojouharova, Kremena Parmakova, Peter Skinhoej, Heli Siikamaki, Christian Perronne, Olga Adrami, John Lambert, Simone Lanini, Robert Hemmer, Michael Borg, Anne Lise Fjellet, Arne Broch Brantsæter, Andrzej Horban, Franc Strle, and Antoni Trilla
References
- 1.Bannister B., Puro V., Fusco F.M. Framework for the design and operation of highlevel isolation units: consensus of the European Network of Infectious Diseases. Lancet Infect Dis. 2009;9:45–56. doi: 10.1016/S1473-3099(08)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timen A., Koopmans M.P., Vossen A.C. Response to imported case of Marburg hemorrhagic fever, the Netherlands. Emerg Infect Dis. 2009;15:1171–1175. doi: 10.3201/eid1508.090051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitching A., Addiman S., Cathcart S. A fatal case of Lassa fever in London, January 2009. Euro Surveill. 2009;14 pii:19117. [PubMed] [Google Scholar]
- 4.Atkin S., Anaraki S., Gothard P. The first case of Lassa fever imported from Mali to the United Kingdom, February 2009. Euro Surveill. 2009;14 pii:19145. [PubMed] [Google Scholar]
- 5.Drosten C., Preiser W., Günther S. Severe acute respiratory syndrome: identification of the etiological agent. Trends Mol Med. 2003;9:325–327. doi: 10.1016/S1471-4914(03)00133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quoilin S., Thomas I., Gérard C. Management of potential human cases of influenza A/H5N1: lessons from Belgium. Euro Surveill. 2006;11(1) doi: 10.2807/esw.11.04.02885-en. [DOI] [PubMed] [Google Scholar]
- 7.Ruggenenti P., Remuzzi G.A. German outbreak of haemolytic uraemic syndrome. Lancet. 2011;378(9796):1057–1058. doi: 10.1016/S0140-6736(11)61217-8. [DOI] [PubMed] [Google Scholar]
- 8.Hauri A., Gotsch U., Strotmann I., Krahn J., Bettge-Weller G., Westbrock H. Secondary transmissions during the outbreak of Shiga toxin-producing Escherichia coli O104 in Hesse, Germany, 2011. Euro Surveill. 2011;16(31) pii:19937. [PubMed] [Google Scholar]
- 9.Maltezou H.C., Andonova L., Andraghetti R., Bouloy M., Ergonul O., Jongejan F. Crimean–Congo hemorrhagic fever in Europe: current situation calls for preparedness. Euro Surveill. 2010;15(10) pii:19504. [PubMed] [Google Scholar]
- 10.Ergönül O. Crimean–Congo haemorrhagic fever. Lancet Infect Dis. 2006;6:203–214. doi: 10.1016/S1473-3099(06)70435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed J., Bouloy M., Ergonul O., Fooks A., Paweska J., Chevalier V. International network for capacity building for the control of emerging viral vector-borne zoonotic diseases: ARBO-ZOONET. Euro Surveill. 2009;14(12) pii:19160. [PubMed] [Google Scholar]
- 12.Brouqui P., Puro V., Fusco F.M. Infection control in the management of highly pathogenic infectious diseases: consensus of the European Network of Infectious Disease. Lancet Infect Dis. 2009;9(5):301–311. doi: 10.1016/S1473-3099(09)70070-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baka A., Fusco F.M., Puro V. A curriculum for training healthcare workers in the management of highly infectious diseases. Euro Surveill. 2007;12:E5–E6. doi: 10.2807/esm.12.06.00716-en. [DOI] [PubMed] [Google Scholar]
- 14.Nisii C., Castilletti C., Di Caro A., Capobianchi M.R., Brown D., Lloyd G., for the Euronet-P4 Group The European network of Biosafety-Level-4 laboratories: enhancing European preparedness for new health threats. Clin Microbiol Infect. 2009;15:720–726. doi: 10.1111/j.1469-0691.2009.02946.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fusco F., Puro V., Baka A. Isolation rooms for highly infectious diseases: an inventory of capabilities in European countries. J Hosp Infect. 2009;73:15–23. doi: 10.1016/j.jhin.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.No authors listed E-alert 24 July: case of Lassa fever imported into Germany from Sierra Leone. Euro Surveill. 2006;11 E060727.1. [PubMed] [Google Scholar]
- 17.Schilling S., Follin P., Jarhall B. European concepts for the domestic transportation of highly infectious patients. Clin Microbiol Infect. 2009;15:727–733. doi: 10.1111/j.1469-0691.2009.02871.x. [DOI] [PubMed] [Google Scholar]
- 18.Fusco F., Schilling S., Puro V. EuroNHID checklists for the assessment of high level isolation units and referral centres for highly infectious diseases: results from the pilot phase of a European survey. Clin Microbiol Infect. 2009;15:711–719. doi: 10.1111/j.1469-0691.2009.02874.x. [DOI] [PubMed] [Google Scholar]
- 19.Smith P.W., Anderson A.O., Christopher G.W. Designing a Biocontainment Unit to care for patients with serious communicable diseases: a consensus statement. Biosec Bioterr. 2006;4:351–365. doi: 10.1089/bsp.2006.4.351. [DOI] [PubMed] [Google Scholar]
- 20.Rubinson L., Nuzzo J.B., Talmor D.S. Augmentation of hospital critical care capacity after bioterrorist attacks or epidemics: recommendations of the Working Group on Emergency Mass Critical Care. Crit Care Med. 2005;33(Suppl. l):E2393. doi: 10.1097/01.ccm.0000173411.06574.d5. [DOI] [PubMed] [Google Scholar]
- 21.Maguire B.J., Dean S., Bissell R.A., Walz B.J., Bumbak A.K. Epidemic and bioterrorism preparation among emergency medical services systems. Prehosp Disast Med. 2007;22:237–242. doi: 10.1017/s1049023x0000474x. [DOI] [PubMed] [Google Scholar]
- 22.Silverman A., Simor A., Loutfy M.R. Toronto emergency medical services and SARS. Emerg Infect Dis. 2004;10:1688–1689. doi: 10.3201/eid1009.040170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.PromedMail Crimean–Congo hemorrhagic fever, fatal — Germany ex Afghanistan Archive Number 20090919.3286 Published date: 19 September 200.
- 24.Teichman P.G., Donchin Y., Kot R.J. International aeromedical evacuation. N Engl J Med. 2007;356:262–270. doi: 10.1056/NEJMra063651. [DOI] [PubMed] [Google Scholar]
- 25.No authors listed . International Air Transport Association; Montreal — Geneva: 2006. Infectious substances shipping guidelines Ref. No: 9052–07. [Google Scholar]
- 26.WHO. International Health Regulations. Geneva: World Health Organization. Available at: http://whqlibdoc.who.int/publications/2008/9789241580410_eng.pdf (Accessed 14.11.11).
- 27.Reilly M.J., Markenson D., DiMaggio C. Comfort level of emergency medical service providers in responding to weapons of mass destruction events: impact of training and equipment. Prehosp Disaster Med. 2007;22:297–303. doi: 10.1017/s1049023x00004908. [DOI] [PubMed] [Google Scholar]
- 28.Johannigman J.A. Maintaining the continuum of en route care. Crit Care Med. 2008;36:S377–S382. doi: 10.1097/CCM.0b013e31817e31e1. [DOI] [PubMed] [Google Scholar]
- 29.Verbeek P.R., McClelland I.W., Silverman A.C., Burgess R.J. Loss of paramedic availability in an urban emergency medical services system during a severe acute respiratory syndrome outbreak. Acad Emerg Med. 2004;11:973–978. doi: 10.1197/j.aem.2004.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson K.E., Driscoll D.M. Mobile high-containment isolation: a unique patient care modality. Am J Inf Control. 1987;15:120–124. doi: 10.1016/0196-6553(87)90165-9. [DOI] [PubMed] [Google Scholar]