Concerns about avian influenza viruses have heightened as the number of human H7N9 cases continues to rise and new subtypes such as H10N8 are found to infect and cause severe disease in humans. Li and colleagues1 described the results of field investigations from the first 139 confirmed human cases of H7N9, reporting that most cases had recent exposure to poultry and were epidemiologically unrelated, although human-to-human transmission could not be ruled out in four families. Yu and colleagues2 reported that closure of live poultry markets in the spring of 2013 reduced the mean daily number of H7N9 infections by an estimated 97–99%, and recommended that closure of live poultry markets should be immediately implemented in affected areas in future outbreaks to minimise the risk of human infection. However, in a linked Comment, Fournié and Pfeiffer3 suggest that the apparent effect of closures of such markets on incidence could have been driven by strong consumer reactions to the threat of infection irrespective of market closures; they argue that closures alone could potentially promote informal marketing of poultry, which could enable spread of the virus and make targeted surveillance and risk management more difficult.
The importance of the animal–human interface has also been shown through the emergence of Middle East respiratory syndrome coronavirus (MERS-CoV). Meyer and colleagues4 reported that antibodies against MERS-CoV were common in samples taken from dromedary camels in 2003 (100% of 151 camel serum samples had detectable antibodies to MERS-CoV with 57% having high neutralising titres), well before the first human cases were identified in 2012. Azhar and colleagues5 reported identical full genome sequences from MERS-CoV isolates taken from a patient who died of MERS-CoV and the symptomatically infected dromedary camel belonging to the patient. This provided strong evidence that MERS-CoV could be transmitted from camels to humans and establishes camels as a potentially important source of infection, although other species such as bats might also be implicated.
Fortunately, unlike the 2009 influenza pandemic strain (H1N1pdm09), neither MERS-CoV nor influenza A H7N9 (or any other influenza subtypes recently identified to infect humans) have evolved the ability to spread efficiently between humans. National preparedness plans for influenza pandemic involved widespread stockpiling of antivirals, and the 2009 pandemic provided an opportunity to study their effectiveness. New research on the effectiveness of neuraminidase inhibitors to reduce mortality in patients admitted to hospital with influenza A H1N1pdm09 has been encouraging.6 Although the effectiveness of antivirals to reduce mortality would ideally be derived from randomised controlled trials, a recent meta-analysis of trials was only able to collect data for five reported deaths, only one of which was due to a respiratory cause.7 The comparative rarity of such events highlights the need for high quality observational research to inform policy and practice.
Muthuri and colleagues6 collected individual-level data from around the world on patients admitted to hospital with influenza A H1N1pdm09. After adjustment for treatment propensity and potential confounders, the results of their meta-analysis indicate that compared with no treatment, neuraminidase inhibitor treatment at any time during illness was associated with a reduction in mortality risk (adjusted odds ratio [OR] 0·81).6 This association was strongest in adults (OR 0·75), but weaker and not significant in children. The timing of treatment was also important because early treatment (within 2 days of symptom onset) was associated with a reduction in mortality (OR 0·48) compared with later treatment—treatment given later than 2 days and up to 5 days after symptom onset was not associated with reductions in mortality compared with no treatment except in severely ill adult patients admitted to critical care (adjusted OR 0·65). Questions remain about the most effective and cost-effective means to ensure that those most likely to benefit are treated early.
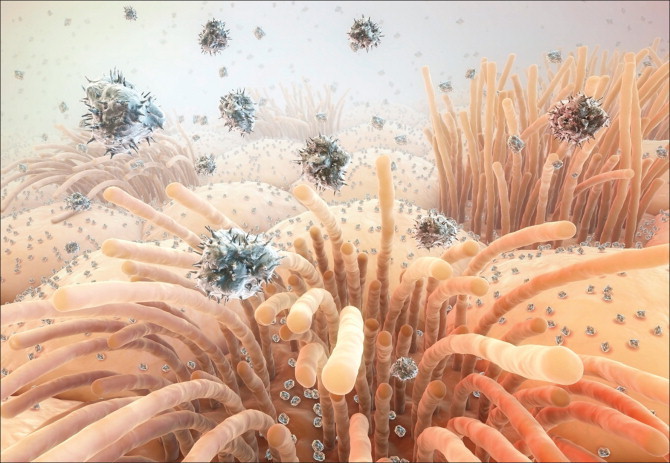
© 2014 Hybrid Medical Animation/Science Photo Library
By contrast with acute respiratory infections, which have the potential to emerge and spread rapidly, the inexorable emergence of drug resistant, multi-drug resistant (MDR), and now extensively drug-resistant (XDR) tuberculosis, has played out during the past seven decades since the discovery of streptomycin in 1944. Using whole genome sequencing of 1000 prospectively collected tuberculosis isolates from patients in Russia, Casali and colleagues8 provided evidence against the theory that acquiring drug resistance typically comes with a fitness cost and reduced transmissibility. Their findings show the crucial need to strengthen tuberculosis control to prevent the emergence and spread of MDR and XDR tuberculosis. Further evidence from South Africa shows the long infectious periods and alarmingly high levels of mortality in patients with XDR tuberculosis: at 60 months of follow-up, 78 (73%) patients with XDR had died and a further 11 (10%) had failed treatment.9 There has been a long-standing and continuing need to develop new drugs and treatment regimens for tuberculosis, which is underscored by this research.
Emerging respiratory infections highlight the complex interplay between organisms, the environment, animal and human host biology and behaviour and challenges in clinical management. Interdisciplinary approaches are needed to address these multifaceted issues and to ensure that research findings help to inform prevention, management, and control strategies.
This online publication has been corrected. The corrected version first appeared at thelancet.com/respiratory on January 5, 2015
Acknowledgments
We declare no competing interests.
References
- 1.Li Q, Zhou L, Zhou M. Epidemiology of human infections with avian influenza A (H7N9) virus in China. N Engl J Med. 2014;370:520–532. doi: 10.1056/NEJMoa1304617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu H, Wu JT, Cowling BJ. Effect of closure of live poultry markets on poultry-to-person transmission of avian influenza A H7N9 virus: an ecological study. Lancet. 2014;383:541–548. doi: 10.1016/S0140-6736(13)61904-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fournié G, Pfeiffer DU. Can closure of live poultry markets halt the spread of H7N9? Lancet. 2014;383:496–497. doi: 10.1016/S0140-6736(13)62109-1. [DOI] [PubMed] [Google Scholar]
- 4.Meyer B, Müller MA, Corman VM. Antibodies against MERS coronavirus in dromedary camels, United Arab Emirates, 2003 and 2013. Emerg Infect Dis. 2014;20:552–559. doi: 10.3201/eid2004.131746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azhar EI, El-Kafrawy SA, Farraj SA. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med. 2014;370:2499–2505. doi: 10.1056/NEJMoa1401505. [DOI] [PubMed] [Google Scholar]
- 6.Muthuri SG, Venkatesan S, Myles PR. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A H1N1pdm09 virus infection: a meta-analysis of individual participant data. Lancet Respir Med. 2014;2:395–404. doi: 10.1016/S2213-2600(14)70041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jefferson T, Jones M, Doshi P, Spencer EA, Onakpoya I, Heneghan CJ. Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments. BMJ. 2014;348:g2545. doi: 10.1136/bmj.g2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casali N, Nikolayevskyy V, Balabanova Y. Evolution and transmission of drug-resistant tuberculosis in a Russian population. Nat Genet. 2014;46:279–286. doi: 10.1038/ng.2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pietersen E, Ignatius E, Streicher EM. Long-term outcomes of patients with extensively drug-resistant tuberculosis in South Africa: a cohort study. Lancet. 2014;383:1230–1239. doi: 10.1016/S0140-6736(13)62675-6. [DOI] [PubMed] [Google Scholar]


