Abstract
Practical relevance Generalised ataxia is one of the most common neurological presentations identified in cats in practice. The causes can be subdivided into three forms on the basis of the neuroanatomical diagnosis: cerebellar, vestibular and sensory (spinal or general proprioceptive) ataxia. The type of ataxia will determine the diagnostic procedures and select the differential diagnoses, and an accurate neuroanatomical diagnosis is therefore essential. The differential diagnosis list can then be further tailored on the basis of patient signalment, clinical presentation and progression.

Global importance Irrespective of the world region, most of the causes of generalised ataxia in the cat are similar and many have been identified for a number of years (cerebellar hypoplasia has been recognised since the late 19th century). However, it is the advent of new technology, in particular veterinary access to magnetic resonance imaging, which has resulted in particularly rapid advances in our understanding, investigation and management of these different forms of ataxia.
Audience This article introduces the classification of patients with ataxia on the basis of their clinical presentation, discusses the common differential diagnoses associated with each form, and briefly reviews the more important diseases from a clinical perspective. It is aimed at all veterinarians who treat cats.
What is ataxia?
Ataxia is defined as incoordination, wobbliness or unsteadiness due to a failure to regulate truncal posture and the strength and direction of limb movements. In the clinical setting, ataxia most commonly refers to incoordination while assessing gait. There are three main forms of ataxia based on the neuroanatomical diagnosis (Fig 1):
Fig 1.

There are three main forms of generalised ataxia based on the underlying neuroanatomical diagnosis: cerebellar ataxia, vestibular ataxia and sensory (spinal or general proprioceptive) ataxia
Cerebellar ataxia;
Vestibular ataxia;
Sensory (spinal or general proprioceptive) ataxia.
If the underlying disorder is bilateral (or diffuse) then the ataxia will tend to be generalised; by contrast, if the lesion is asymmetrical then the ataxia may just be present on one side of the body (usually ipsilateral to the lesion).
Differentiation between the different forms of ataxia is on the basis of the findings of the neurological examination (Table 1) and is usually fairly straightforward. In cases where the ataxia is subtle there are techniques to temporarily exacerbate the clinical deficits in order to facilitate assessment (see box on page 350).
Table 1.
Diagnostic approach to the cat with generalised ataxia
| Cerebellar ataxia | Vestibular ataxia | Sensory (spinal or general proprioceptive) ataxia | |
|---|---|---|---|
| Head movement and position | Fine tremor at rest. Intention tremor with directed movements | Head tilt, usually towards lesion. No head tremor | Normal |
| Eyeball movement and position | Fine ocular tremor (visible on retinal examination)* | Spontaneous nystagmus and strabismus* | Normal |
| Gait | Hypermetric. No concurrent motor weakness | Falling to affected side. Ipsilateral circling or rolling. No concurrent motor weakness | Concurrent motor weakness. Decreased limb proprioception |
| Posture when standing stationary | Abnormal — wide-based, swaying and staggering | Relatively normal. Leaning to affected side | Relatively normal |
| Other signs | Menace response deficits and vestibular signs may be present | Cranial nerve deficits, Horner's syndrome or ear disease may be present. Vomiting may be seen during actue phase | Cervical pain or deformity may be present. Spinal reflexes may be normal to increased |
See box on page 352
Cerebellar ataxia
The clinical signs associated with cerebellar disease are one of the easiest syndromes to identify. The cerebellum has an important role in balance and in controlling and modulating movements of the limbs, trunk and head (including fine control of eyeball position). Motor strength is maintained in cerebellar ataxia.
Vestibular ataxia
The term vestibular ataxia describes the ataxia that is seen secondarily to dysfunction of the vestibular system. The vestibular system is responsible for controlling the position of the head, trunk and eyeballs. The clinical signs associated with acute, unilateral vestibular dysfunction are asymmetrical and may include ipsilateral head tilt (Fig 2), falling, rolling and vomiting, as well as nystagmus in both eyes and ventrolateral strabismus of the ipsilateral eye. Motor strength is maintained in vestibular ataxia.
Fig 2.

Domestic shorthair cat with a left head tilt due to left vestibular syndrome. The involvement of the head in cats with generalised ataxia is a useful means of differentiating between the three different neuroanatomical forms. In sensory ataxia, the head position is normal; in cerebellar ataxia there is frequently a fine head tremor or an intention tremor; in vestibular ataxia there is often a head tilt that is usually towards the side of the lesion
Differentiation between the different forms of ataxia is on the basis of the findings of the neurological examination and is usually fairly straightforward.
Sensory (spinal or general proprioceptive) ataxia
The term sensory ataxia is used to indicate the ataxia seen following damage to the ascending sensory tracts (most commonly general proprioceptive tracts) in the spinal cord. In contrast to cerebellar and vestibular ataxia, sensory ataxia is usually associated with concurrent motor involvement due to damage to adjacent motor tracts within the spinal cord. Lesions in sensory ataxia are usually confined to the upper cervical spinal cord (spinal cord segments C1-C5), with affected cats presenting with ataxia, but preservation of the segmental spinal reflexes, in all four limbs. Lesions further caudal may just affect the pelvic limbs; alternatively motor deficits, and not ataxia, will tend to dominate if the lesion is in the lower cervical region.
Vestibular ataxia can be further classified as peripheral or central
The neuroanatomical localisation is reasonably well defined in cerebellar and sensory ataxia. However, in vestibular ataxia, the lesions may be situated either within the peripheral vestibular structures (peripheral vestibular syndrome) — including the inner ear (semicircular canals) and vestibulocochlear nerve — or, less commonly, within the brain (central vestibular syndrome); the vestibular nuclei of the brainstem are the most common location for central vestibular disease, but other localisations include parts of the cerebellum or the thalamus.
Both peripheral and central vestibular syndrome may present with additional evidence of deafness, facial nerve paralysis and, in some cases, even sympathetic dysfunction (Fig 3) (Table 2). However, certain deficits are only seen in either peripheral or central vestibular disease and therefore allow differentiation between these two sites (Table 3) (Fig 4).
Fig 3.

The right head tilt in this cat is indicative of right vestibular syndrome. The additional finding of right Horner's syndrome (manifest as miosis and protrusion of the third eyelid in the right eye) indicates that the lesion is peripheral — that is, related to the middle and inner ear, and adjacent structures
Table 2.
Features that may be present in either peripheral or central vestibular disease
| Peripheral | Central | |
|---|---|---|
| Head tilt | Ipsilateral | Ipsilateral or contralateral |
| Ataxia | Ipsilateral | Ipsilateral |
| Falling or rolling | Ipsilateral | Ipsilateral or contralateral |
Nystagmus
|
Slow phase is ipsilateral | Ipsilateral or contralateral |
| Facial nerve (CN VII) paralysis | Ipsilateral | Ipsilateral |
Table 3.
Features that allow differentiation between peripheral and central vestibular disease
| Peripheral | Central | |
|---|---|---|
| Circling | No | Yes |
| Postural deficits (usually conscious proprioceptive deficits or hypermetria) | No | Yes |
| Cranial nerve lesions (other than facial nerve [CN VII]) | No | Yes |
| Nystagmus | ||
| — vertical | No | Yes |
| — positional | No (except acute compensatory phase) | Yes |
| Pain on opening the jaw or ear disease | Yes | No (except very extensive lesions) |
| Horner's syndrome | Yes | No (except very extensive lesions) |
Fig 4.
Sympathetic supply to the eye in the cat. The concurrent demonstration of vestibular syndrome and Horner's syndrome on the same side is consistent with peripheral vestibular disease. Damage to the sympathetic innervation to the head may also occur on rare occasions in association with central vestibular lesions, but only in cases with extensive intracranial lesions and therefore profound evidence of central nervous system disease
Assessment of patients with subtle ataxia
Maintaining balance when standing in the stationary position requires proprioceptive, vestibular and visual inputs.
Cats with cerebellar lesions The affected animal is usually unable to maintain normal balance when standing in the stationary position. It adopts a wide-based stance and frequently demonstrates a truncal sway or even stumbling.
Cats with vestibular or sensory lesions The affected animal only requires two of the three inputs (proprioceptive, vestibular or visual) in order to maintain balance when standing in the stationary position. Blindfolding these patients removes the visual input and, if either vestibular or sensory inputs are affected, then the animal's ataxia will worsen and as a result it will sway or lose its balance. 1
Differential diagnoses for the cat with generalised ataxia
The differential diagnoses for the wobbly cat are subdivided on the basis of the underlying neuroanatomical diagnosis and have been classified using the ‘VITAMIN D’ mnemonic (V = vascular; I = iatrogenic, idiopathic, immune-mediated, infectious and inflammatory; T = toxic and traumatic; A = anomalous; M = metabolic; N = neoplastic and nutritional; D = degenerative) (Table 4).
Table 4.
Differential diagnoses for the main forms of ataxia
| Cerebellar ataxia | Peripheral vestibular ataxia | Central vestibular ataxia | Sensory (spinal or general proprioceptive) ataxia | |
|---|---|---|---|---|
| Vascular | Cerebellar cerebrovascular accident | — |
|
|
| Infectious |
|
|
|
|
| Idiopathic | — | Idiopathic vestibular syndrome | — | — |
| Toxic | Metronidazole | Aminoglycoside antibiotics (particularly streptomycin) | Metronidazole | — |
| Traumatic | Trauma | Trauma | Trauma | Trauma |
| Anomalous |
|
Congenital vestibular syndrome | Intracranial intra-arachnoid cysts |
|
| Neoplastic | Brain tumours | Tumours invading the inner ear and vestibulocochlear nerve (CN VIII) | Brain tumours |
|
| Nutritional | — | — | Thiamine deficiency | Hypervitaminosis A |
| Degenerative | Lysosomal storage diseases Cerebellar abiotrophy | — | — | Intervertebral disc disease |
FIP = feline infectious peritonitis, FSE = feline spongiform encephalopathy
Common causes of generalised ataxia in cats
Feline infectious peritonitis
Clinical signs of progressive neurological disease are common in cats with the dry form of feline infectious peritonitis (FIP), 2 especially in those younger than 2 years of age or older than 9 years of age. Cerebellar signs are the most common neurological abnormalities in these cases, but other abnormalities that are frequently seen include central vestibular signs, seizures, and pelvic limb ataxia and paresis. In addition to the neurological deficits, most affected cats manifest a fever and systemic signs such as anorexia and depression. Concurrent uveitis and chorioretinitis is common and should increase the clinical suspicion. Other signs of FIP may also be present.
The remainder of this review is devoted to some of the more common, and hence clinically important, causes of generalised ataxia in the cat that are listed in Table 4. Note that a condition may consistently present as one particular form of generalised ataxia (eg, thiamine deficiency always presents as central vestibular ataxia) or the presentation may be variable depending on the location of the underlying pathology (eg, FIP may present as cerebellar, vestibular or sensory ataxia).
Routine haematology and biochemistry usually demonstrates an inflammatory leukogram and high serum globulin concentrations. Tests for coronavirus antibody are often non-diagnostic — although an extremely high titre in the presence of typical clinical findings suggests a diagnosis of FIP, a negative titre does not rule out the disease. Many cats have concurrent feline leukaemia virus (FeLV) infection. Cerebrospinal fluid (CSF) analysis is often the most useful test to confirm the diagnosis and typical findings include a dramatic elevation in protein concentration in the presence of non-septic inflammation with a large number of neutrophils, macrophages and lymphocytes. 3 The magnetic resonance imaging (MRI) features may also be highly suggestive, comprising obstructive hydrocephalus and marked contrast enhancement of post-gadolinium T1-weighted MRI scans around the third ventricle, mesencephalic aqueduct and brainstem (Figs 5 and 6). The risk of brain herniation is significant in these cases (Fig 6) and care should be taken when anaesthetising them or performing a CSF tap. The prognosis for cats with central nervous system (CNS) FIP is poor.
Fig 5.
Transverse T1-weighted MRI scans from a cat with CNS FIP. (a) There is obstructive hydrocephalus with dilation of the lateral (arrow) and third ventricles. (b) Following IV administration of gadolinium contrast medium there is enhancement around the third ventricle (arrow). These features are highly suggestive of FIP
Fig 6.
(a) Midline sagittal T1-weighted post-contrast MRI scan, (b) T2-weighted MRI scan and (c) gross pathology image from a cat with CNS FIP. There is marked contrast enhancement in the caudal fossa (hyperintensity in [a]), resulting in obstructive hydrocephalus and caudal transtentorial and foramen magnum brain herniation

Eyeball position and movement in cats with generalised ataxia
In addition to generalised ataxia, abnormalities of eyeball position or movement may be present in cats with cerebellar and vestibular ataxia. In cerebellar ataxia there may be a fine ocular tremor due to modulation of eyeball movements (voluntary and saccadic) by the cerebellum. In vestibular ataxia there may be a static alteration in gaze direction (strabismus or squint) or involuntary eye movements (nystagmus). In contrast, sensory (spinal or general proprioceptive) ataxia does not affect eyeball position or movement.
The extraocular muscles are innervated by the oculomotor, trochlear and abducens cranial nerves. Eyeball position and movement are further controlled by the vestibular and saccadic systems and these movements are modulated by the cerebellum. The function of the vestibular system with regard to vision is to maintain the visual image in a steady position on the retina in response to movements of the head. This is achieved by inducing eye movements (termed nystagmus), via the vestibulo-ocular reflex, that are equal to, but in the opposite direction to, the head movements. In contrast to the vestibular system, the saccadic system functions to change the line of sight to focus a new visual stimulus on the retinal region with the highest visual acuity. Saccadic eye movements occur in response to startle reflexes (sudden visual and auditory stimuli) and during the fast phase eye movements of the vestibulo-ocular reflex.
Evaluation of the normal vestibulo-ocular reflex allows assessment of the vestibular system. When the head is moved from side to side or up and down at a steady rate without the gaze being fixed on a single object, a nystagmus (also termed physiological nystagmus) is induced, with the fast phase movements of the eyeball occurring in the direction of the head movement. Physiological nystagmus should stop once the head movement stops. An exception to this is where the head movement continues for a prolonged period in the same direction and at a constant speed (eg, as a result of being spun on a revolving chair); in this situation the vestibular system has time to adapt, and the physiological nystagmus stops during the constant movement but briefly restarts when the speed or direction of movement changes or is stopped.
In contrast to normal physiological nystagmus, lesions affecting vestibular input to the extraocular muscles may result in a static alteration in gaze direction (strabismus or squint) or involuntary eye movements (nystagmus). The vestibular control of eyeball position and movement is assessed by evaluating for strabismus, spontaneous nystagmus and the presence of normal physiological nystagmus. This should include elevating the animal's head (with the ears level) and holding it briefly elevated to see if a strabismus can be induced, as well as altering the animal's position (including turning it on its back) to assess for positional nystagmus.

Spontaneous jerk nystagmus is seen in both central and peripheral vestibular syndrome. The nystagmus is described on the basis of the direction of the fast phase of the eyeball movement (arrows), but the site of the lesion is usually indicated by the direction of the slow phase of the eyeball movement. In rotatory nystagmus the 12 o'clock position of the eyeball is used to describe the direction of the nystagmus. Horizontal and rotatory nystagmus may be seen with peripheral or central vestibular syndrome, but vertical nystagmus is only seen in central vestibular syndrome
Metronidazole toxicity
The long-term use of metronidazole at high doses may result in a variety of progressive neurological deficits in cats. 4 This is seen less commonly in cats than in dogs, with most of the feline cases reported in the literature having been treated with very high doses of metronidazole. The dominant clinical signs are those of central vestibular dysfunction, but may include generalised ataxia, tremors, depression and even seizures. Once clinical signs develop discontinuation of metronidazole is important as continued use may result in irreversible clinical signs and death. Cessation of therapy in the early stages will usually result in complete and rapid resolution of the clinical signs. In dogs, the use of diazepam will significantly reduce the recovery time, but this has not been evaluated in cats.
Lysosomal storage diseases
Lysosomal storage diseases represent inborn disorders of metabolism resulting from an enzyme deficiency in the lysosomes, which are the small, membrane-bound intracellular organelles responsible for degradation of cellular and extracellular materials. The deficiency or loss of function is specific to a particular enzyme, with the consequence that the product normally degraded by that enzyme starts to accumulate. This accumulation then begins to interfere with cell functioning. While lysosomes are present in virtually every cell in the body, neurological dysfunction usually predominates. The clinical presentation tends to be very specific to the particular lysosomal storage disease, but the most common presentation is cerebellar ataxia.
Lysosomal storage diseases are uncommon. Affected cats are often normal at birth and usually present at an early age, demonstrating gradual progression of clinical signs. This progression is often the most useful way to distinguish these disorders from cerebellar hypoplasia, which is the most common cause of cerebellar ataxia in young kittens. There may be additional clinical signs, or the presentation may not be that of cerebellar ataxia, depending on the lysosomal storage disease. Retarded growth, forebrain dysfunction (including altered behaviour and seizures), ocular pathology (including corneal opacification [Fig 7], cataract and retinal changes), and skeletal and connective tissue changes (particularly in mucopolysaccharidosis) may also be evident (Fig 8).
Fig 7.

Corneal opacification in a cat with mucopolysaccharidosis, a lysosomal storage disease
Fig 8.

Cervical rigidity with decreased range of movement due to fusion of the cervical vertebrae in a cat with mucopolysaccharidosis. An important differential diagnosis for cervical fusion due to proliferative bony lesions is hypervitaminosis A; in both diseases the bony lesions may result in spinal cord compression and generalised ataxia
In litters with cerebellar hypoplasia, a variable number of kittens may be affected, with a varying spectrum of severity between kittens. Cerebellar hypoplasia is characterised by diffuse cerebellar signs with an absence of progression.
A strong presumptive diagnosis can often be made on the basis of the cat's age, clinical presentation and progression of signs. This clinical suspicion can be strengthened by demonstrating the accumulation of storage products or vacuoles in leukocytes or tissue biopsy samples (usually liver, spleen or lymph node). Confirmation of the diagnosis relies on lysosomal enzyme analysis in cases where the enzyme defect is known, and genetic testing where the genetic defect has been identified. 5 In some disorders the storage product may be demonstrated on urine analysis or muscle and nerve biopsy.
Regardless of the diagnosis, the prognosis is poor.
Cerebellar hypoplasia
Cerebellar hypoplasia (caused by feline panleukopenia virus) has historically been recognised in kittens, but it was only in the 1960s that experimental and spontaneous in utero infection of pregnant cats with the panleukopenia virus was demonstrated to cause cerebellar hypoplasia in the progeny. 6 Since this time most cases of cerebellar hypoplasia in kittens have been attributed to in utero panleukopenia virus infection and in dogs to parvovirus. 7 The panleukopenia virus has cytopathic effects on rapidly dividing cells, particularly the granule cell layer of the cerebellum. As a result, the cerebellum of affected kittens is grossly hypoplastic (Fig 9), with some having concurrent hydrocephalus or hydranencephaly.
Fig 9.
Cerebellar hypoplasia is common in young kittens and occasionally seen in young puppies. The cerebellum is grossly smaller (right) than in the normal kitten (left). Clinically this decrease in cerebellar size can be identified on MRI scans as a decreased size of the cerebellum or increased CSF dissecting between the folia of the cerebellum
In affected litters, a variable number of kittens may be involved, with a varying spectrum of severity between kittens. Clinical signs first become apparent when the kitten begins to walk at around 2–3 weeks of age, with affected kittens demonstrating evidence of diffuse cerebellar involvement. The clinical signs are non-progressive; in fact, some clinical improvement may become apparent in some kittens, presumably because of compensation through other senses such as general proprioception and vision.
The finding of diffuse cerebellar signs, with the absence of progression and lack of involvement of other areas of the CNS, is usually sufficient to make a diagnosis of cerebellar hypoplasia. Establishing a definitive ante-mortem diagnosis is difficult and usually rests on demonstrating a small cerebellum following advanced imaging (usually MRI). While there is no treatment for cerebellar hypoplasia, less severely affected kittens make acceptable pets, particularly if substantial compensation occurs.
Intracranial intra-arachnoid cysts
Quadrigeminal cysts are intracranial cystic accumulations of CSF within the arachnoid mater at the level of the quadrigeminal cistern. Controversy surrounds the clinical significance of these cysts, which are rare in cats, with many being detected as apparently incidental findings. Neurological deficits may become evident if gradual expansion of a quadrigeminal cyst results in increased intracranial pressure, compression of adjacent neural structures or obstruction of CSF outflow pathways (Fig 10). 8
Fig 10.
Typical appearance of a quadrigeminal cyst on a parasagittal T2-weighted MRI scan. The majority of quadrigeminal cysts are incidental findings; however, if a cyst becomes very large then it may result in compression of adjacent neurological tissues, as in this case
Otitis media/interna
This common cause of vestibular signs is usually associated with extension of otitis externa into the middle and inner ear, but may arise in the absence of external ear canal inflammation. Foreign bodies in the external ear canals (eg, grass awns) may penetrate the tympanic membrane or cause a chronic otitis externa with rupture of the tympanic membrane. In the absence of otitis externa, two other routes of infection include retrograde spread via the Eustachian tubes and haematogenous spread. The most common infectious agents are bacteria, including Staphylococcus, Streptococcus, Proteus, Pseudomonas species, Enterococcus species and Escherichia coli. If otitis media/interna is suspected, but bacterial culture results are not available, then the choice of antibiotic is usually based on sensitivity to the above bacteria. Ear mites (Otodectes cynotis) in cats may also result in rupture of the tympanic membrane and a secondary otitis media/interna.
The clinical signs associated with otitis media/interna usually reflect an acute onset of peripheral vestibular syndrome, and a partial recovery may become apparent as the animal compensates for the vestibular deficits over the next day or two. In some cases there may be evidence of intracranial disease if the otitis media erodes through the calvarium (Fig 11), but these cats will also have obvious evidence of middle ear disease.
Fig 11.

Transverse T1-weighted MRI scan following IV administration of gadolinium contrast medium. Otitis media/interna (solid arrow) is usually associated with peripheral vestibular syndrome, but (particularly in cats) it is not unusual for infection to erode through into the calvarium and result in secondary meningitis (hyperintensity of the meninges and falx cerebri; open arrows). The investigation of cats with central vestibular disease (25% of cases of which may have concurrent seizures) should therefore still include an evaluation of the middle ear
In contrast to idiopathic vestibular syndrome (see later) there are usually secondary clinical signs related to the ear infection. These may include:
Discharge from the external ear canal, with head shaking, scratching or rubbing of the ears and frequent yawning;
Abnormalities on auroscopic examination of the tympanic bulla;
Pain on opening the mouth or palpation of the structures adjacent to the ear;
Damage to adjacent nervous system structures, in particular the facial nerve and sympathetic supply to the head (Horner's syndrome). Less commonly facial nerve dysfunction may also include damage to the parasympathetic supply to the lacrimal glands, resulting in a dry eye and nose;
Hemifacial spasm where there is early irritation of the facial nerve, although this is less common.
Diagnosis of otitis media/interna is based on findings of peripheral vestibular syndrome and typical clinical signs of ear disease, together with auroscopic examination of the tympanic membrane, radiography or advanced imaging of the head (Figs 12 and 13) and, possibly, surgical exploration. 9 If there is evidence of fluid accumulation in the middle ear (ie, discoloration and outward bulging of the tympanic membrane), then a sample should be collected for culture, cytology and sensitivity testing via a myringotomy. Owners need to be warned that the clinical signs related to the vestibular dysfunction may temporarily deteriorate post anaesthesia.
Fig 12.
MRI images from the cat pictured in Fig 3 with otitis media, showing inflammation affecting the soft tissues adjacent to the bulla. (a) Transverse T2-weighted scan; (b) T1-weighted pre-contrast scan; (c) T1-weighted post-contrast scan; and (d) subtraction scan (ie, image [c] subtracted from image [b] in order to demonstrate the contrast enhancement). The air cavity within the bulla is obliterated (arrows in [a] and [b]) and there is marked contrast enhancement adjacent to the bulla (arrows in [c] and [d])
Fig 13.
Dorsal T2-weighted MRI scan from the cat pictured in Fig 3, demonstrating obliteration of the air cavity within the bulla (closed arrow) by a hyperintense signal (open arrow)
Otitis media/interna is usually initially treated with antibiotics. The prognosis is generally good with a prolonged course of appropriate oral and topical antibiotics, selected on the basis of bacterial culture results. Where culture and sensitivity results are not available then empirical antibiotic treatment is usually attempted. Suitable choices include cefalexin (20–25 mg/kg PO BID) and amoxi-cillin-clavulanic acid (20 mg/kg BID) for 4–6 weeks. If there is evidence of keratoconjunctivitis sicca then additional use of artificial tears and ocular lubricants is recommended. In advanced cases, or where medical treatment is not successful, surgical drainage of the middle ear via a ventral bulla osteotomy may be required.
Inflammatory polyps
Middle ear polyps should be suspected as the cause of vestibular disease in cats with an acute onset of peripheral vestibular signs, which also show additional abnormalities suggestive of middle/inner ear disease, or clinical signs consistent with a nasopharyngeal polyp. 10 Affected cats are usually young at the time of onset of clinical signs (less than 2 years old). The polyps may be situated in the external ear canal and/or within the nasopharynx. The majority appear to originate in the Eustachian tube, with resultant blockage of drainage from the middle ear leading to clinical signs of ear disease.
Diagnosis may require examination of the external ear canal, tympanic membrane and pharynx under general anaesthesia, and imaging of the middle/inner ear by either radiography or MRI. In some cases exploratory surgery is required. The polyps are usually only attached by a narrow stalk to the Eustachian tube and can readily be removed by traction. In some cases a ventral bulla osteotomy may be necessary.
Idiopathic vestibular syndrome
This common cause of peripheral vestibular disease in the cat has an acute onset with no apparent cause. 11 The clinical signs reflect an acute peripheral vestibular disturbance. Affected cats are usually young to middle-aged and generally improve in 2–3 days, although residual deficits (especially head tilt) may take some time (usually 2–3 weeks) to improve; some cats may be left with a permanent head tilt. No cause has been identified, so if other neurological deficits are identified associated with the vestibular dysfunction then other causes should be considered.
No specific treatment exists, besides supportive care, and cases should resolve spontaneously, although the condition may recur. In north-eastern USA a seasonal occurrence of idiopathic vestibular syndrome has been recognised, with most cases presenting in July and August. So far this has not been demonstrated in southern USA or Europe.
Aminoglycoside antibiotic therapy, especially streptomycin therapy, is the most commonly reported cause of ototoxicity in the cat. This, in turn, may affect vestibular function and/or hearing.
Aminoglycoside antibiotics
A large variety of drugs have been associated with ototoxicity, either as a result of topical or systemic therapy. Notwithstanding, the topical use of drugs in the presence of an intact tympanic membrane is probably safe.
Ototoxicity may affect vestibular function and/or hearing, although with most drugs (streptomycin in cats being an exception) the auditory receptors are more sensitive to ototoxicity.
Aminoglycoside antibiotic therapy, especially streptomycin therapy, is the most commonly reported cause of ototoxicity in the cat. 12 Risk factors associated with the development of ototoxicity in animals on aminoglycoside therapy include:
High doses;
Prolonged therapy (> 14 days' duration);
Impaired renal function.
Due to the potential for compensation, vestibular signs frequently resolve once the inciting cause is discontinued. However, deafness is usually permanent.
Congenital vestibular syndrome
Congenital vestibular disease has been described in a variety of breeds of cat, including the Burmese, Tonkinese, Persian and Siamese, though potentially any breed may be affected. Cats with this syndrome may demonstrate a head tilt, ataxia, truncal deviation, nystagmus and, in some cases, deafness, with clinical signs usually becoming apparent by 3–4 weeks of age. Cases with bilateral disease may show side-to-side head movements and absence of normal physiological nystagmus. The clinical signs often persist throughout life, but in many cats there may be a degree of compensation (or even total improvement) by 2–4 months of age.
The cause of the vestibular abnormalities has not been determined, although some cases are thought likely to be inherited. Note that the pendular nystagmus and strabismus of the Siamese cats and related Himalayan breeds are due to a developmental abnormality of the visual pathways and not to a vestibular disturbance (Fig 14).
Fig 14.

Congenital abnormalities of the visual pathways are present in albino and partial albino animals. In the Siamese and related Himalayan cat breeds this manifests as a convergent strabismus and a pendular or oscillating nystagmus. This does not indicate dysfunction of the vestibular system
Congenital spinal anomalies
Spinal malformations can be subdivided on the basis of whether they affect the vertebral body or the spinal cord.
Malformations of the vertebral body occur less commonly in cats than in dogs and in most cases are incidental. However, in some cases the spinal canal may be compromised, resulting in spinal cord compression. These abnormalities include block vertebra, butterfly vertebra, hemivertebra and transitional vertebra.
Malformations of the vertebral arch and spinal cord, including diseases such as spina bifida and sacrococcygeal dysgenesis in the Manx cat, usually affect the caudal spine. 13 Affected cases, therefore, usually demonstrate signs of cauda equina disease, rather than generalised ataxia.
Fibrocartilaginous embolism
Fibrocartilaginous embolism is rare in cats, but has been reported.14,15 Clinically, it is peracute in onset, non-progressive, non-painful and often asymmetrical. Diagnosis is based on the history and clinical findings, and exclusion of a compressive spinal cord lesion on investigation. Myelography will usually demonstrate subtle spinal cord oedema during the early stages, while MRI will reveal asymmetrical hyperintensity within the spinal cord on T2-weighted images. Treatment involves nursing care and an early return to exercise.
Spinal trauma
Trauma is a common cause of spinal dysfunction in cats — be it endogenous trauma (eg, intervertebral disc prolapse) or, as is more common, exogenous trauma (eg, road traffic accident). The majority of cases of spinal trauma will present with profound motor weakness or total paralysis, rather than sensory ataxia.
Neoplasia
-
Intracranial neoplasia The most common intracranial tumours in cats are lymphoma (Fig 15) and meningiomas, and the site of the brain tumour determines the neurological deficits. Within the cerebellum, a specific tumour that may occasionally affect younger cats is a medulloblastoma (a primitive neuroectodermal tumour). The intracranial tumour types typically affecting the intracranial portion of the vestibulocochlear nerve (CN VIII) differ slightly from the rest of the brain and include meningiomas and choroid plexus papillomas.
Both of these tumours have a tendency to arise at the level of the cerebellopontine angle.
Spinal cord and vertebral tumours Spinal cord neoplasia is common in cats and the precise clinical signs depend on the localisation of the lesion (ie, the level of the spinal cord affected). Neoplasia of the spine is classified both with respect to the physical localisation in relation to the meninges and spinal cord, and the tumour type affecting the spinal cord. In general, cats with neoplasia of the spine are middle-aged or older (usually over 6 years of age); the exception is cats with lymphosarcoma, where the mean age of onset is around 3.5 years.16,17
Fig 15.

Abnormal lymphocytes within the CSF, consistent with a diagnosis of CNS lymphoma. Lymphoma is the only common neoplasm affecting the CNS that tends to shed tumour cells into the CSF, allowing a clinical diagnosis on the basis of CSF analysis alone
Hypervitaminosis A
Hypervitaminosis A is an uncommon disease that develops in cats fed a diet that is high in vitamin A, most commonly raw liver.18,19 Affected cats will appear chronically unwell (showing lethargy, loss of appetite and weight loss), and the head and neck are usually rigidly extended. Radiography will reveal proliferative bony lesions of the cervical and thoracic vertebrae (Fig 16). An important differential diagnosis in such cases is mucopolysaccharidosis.
Fig 16.
Proliferative bony lesions (particularly ventral) affecting the cervical and cranial thoracic spine of a cat with hypervitaminosis A
Intervertebral disc disease
While intervertebral disc disease is an important canine neurological problem, accounting for over 2% of all diseases diagnosed in the dog, it is uncommon in cats. 20 In most cats intervertebral disc disease is noted as an incidental finding (Fig 17), but in occasional cases it may be clinically relevant. In cats that do present with suspected intervertebral disc disease, there are clinical signs of pain or varying degrees of spinal cord dysfunction.
Fig 17.
Intervertebral disc disease is uncommon in the cat. In most cases it is identified as an incidental finding, as in this case with calcification of the nucleus pulposus of the discs between the T11-T12 and T12-T13 vertebrae
Intervertebral disc disease in the cat is usually Hansen type I, where herniation of the nucleus pulposus occurs through the annular fibres of the disc into the spinal canal (versus type II, where annular protrusion into the spinal canal is caused by shifting of the nucleus pulposus material).
Cerebral ischaemic necrosis
A syndrome of cerebral infarction has been recognised in cats — so-called cerebral ischaemic necrosis or feline ischaemic encephalopathy. The lesion usually affects the cerebral cortex, but the brainstem is affected in some cats and multiple regions in other cats. The underlying cause of the vascular lesion is usually not identified, although it has been demonstrated to be associated with cuterebriasis in some cases. 21 The disease affects adult cats of both sexes and a number of breeds. The clinical signs are peracute in onset, non-progressive and usually resolve completely over a period of several weeks. Computed tomography or MRI support the diagnosis and CSF analysis usually demonstrates mild elevation of protein, without inflammation. Treatment is largely supportive, but corticosteroids may help to reduce brain oedema and anticonvulsants are indicated in cats with seizures.
Thiamine deficiency
Thiamine (as thiamine pyrophosphate) is important in carbohydrate and amino acid metabolism. Thiamine deficiency causes a progressive encephalopathy in cats, other animals and in human patients, with species-specific selective vulnerability within specific brain regions. 22
Thiamine deficiency in cats can be due to a variety of causes, including a diet high in fish, excessive heating of food and excessive levels of sulphite preservatives in the food. Affected cats frequently demonstrate a period of anorexia preceding the onset of neurological signs. The neurological deficits are usually multifocal, but evidence of vestibular dysfunction predomi nates. Typically, ataxia, intermittent vertical nystagmus, bilateral absent menace responses, anisocoria and episodes of severe vestibular disturbance are seen. There may also be evidence of cervical ventroflexion, muscle weakness and fixed, dilated pupils. The condition can progress to seizures, coma and death.
The preferred diagnostic method is measurement of transketolase activity in fresh erythrocytes. If this is not possible the metabolic effects of thiamine deficiency can be demonstrated by urinary organic acid analysis. Dietary thiamine can be determined by high performance liquid chromatography.
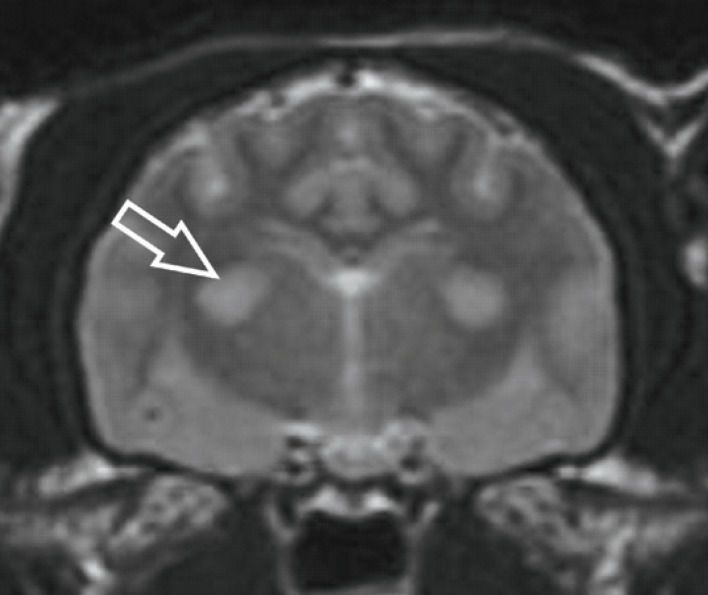
Magnetic resonance imaging can be used to confirm a suspected case; thiamine deficiency is demonstrated by a characteristic pattern of bilaterally symmetrical hyperintensity on T2-weighted and FLAIR images within a variety of brain nuclei and regions, including the lateral geniculate nuclei, caudal colliculi, periaqueductal grey matter, medial vestibular nuclei, cerebellar nodulus and facial nuclei (Fig 18). 23
Fig 18.
Transverse T2-weighted MRI scan demonstrating bilaterally symmetrical hyperintensity of the lateral geniculate nuclei (arrow) in a cat with thiamine deficiency. Hyperintensity in a variety of brain nuclei supports the clinical suspicion of thiamine deficiency in affected animals
Treatment should be started as soon as possible with intravenous fluid therapy, nasogastric tube feeding and intramuscular thiamine injections (Vitamin B1 Injection; Bimeda Veterinary Pharmaceuticals) at 25 mg once daily. Thiamine therapy should continue until the cat demonstrates improvement or a satisfactory oral intake of thiamine; generally around 5 days should suffice.
KEY POINTS
Generalised ataxia may be due to disease affecting the cerebellum, vestibular system or cervical spinal cord, and each of these regions has characteristic clinical signs.
Cerebellar hypoplasia is the most important cause of generalised ataxia in young kittens, and is characterised by diffuse, non-progressive cerebellar signs.
Feline infectious peritonitis is an important cause of generalised ataxia in juvenile and older cats; it usually affects the cerebellum, but may also affect the central vestibular system and spinal cord.
Otitis media in cats may erode through into the calvarium, resulting in signs of brain disease (including seizures). Evaluation of the ear canals is therefore important, even if cats present with evidence of central vestibular disease.
Thiamine deficiency should be considered in any cat with a previous history of anorexia that subsequently develops evidence of progressive central vestibular disease.
Acknowledgements
The author is grateful to Mr Richard Irvine, Veterinary Pathological Sciences, University of Glasgow, for the gross pathological image in Fig 6, Dr Hal Thompson, Veterinary Pathological Sciences, University of Glasgow, for the gross pathological image in Fig 9, and to Mr Ronny Barron, Companion Animal Diagnostics, University of Glasgow, for the image of lymphoma cells within the CSF (Fig 15).
References
- 1.Khasnis A, Gokula R. Romberg's test. J Postgrad Med 2003; 49: 169–72. [PubMed] [Google Scholar]
- 2.Bradshaw JM, Pearson GR, Gruffydd-Jones TJ. A retrospective study of 286 cases of neurological disorders of the cat. J Comp Pathol 2004; 131: 112–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boettcher IC, Steinberg T, Matiasek K, Greene CE, Hartmann K, Fischer A. Use of anti-coronavirus antibody testing of cerebrospinal fluid for diagnosis of feline infectious peritonitis involving the central nervous system in cats. J Am Vet Med Assoc 2007; 230: 199–205. [DOI] [PubMed] [Google Scholar]
- 4.Caylor KB, Cassimatis MK. Metronidazole neurotoxicosis in two cats. J Am Anim Hosp Assoc 2001; 37: 258–62. [DOI] [PubMed] [Google Scholar]
- 5.Skelly BJ, Franklin RJ. Recognition and diagnosis of lysosomal storage diseases in the cat and dog. J Vet Intern Med 2002; 16: 133–41. [DOI] [PubMed] [Google Scholar]
- 6.Kilham L, Margolis G, Colby ED. Congenital infections of cats and ferrets by feline panleukopenia virus manifested by cerebellar hypoplasia. Lab Invest 1967; 17: 465–80. [PubMed] [Google Scholar]
- 7.Schatzberg SJ, Haley NJ, Barr SC, et al. Polymerase chain reaction (PCR) amplification of parvoviral DNA from the brains of dogs and cats with cerebellar hypoplasia. J Vet Intern Med 2003; 17: 538–44. [DOI] [PubMed] [Google Scholar]
- 8.Lowrie M, Wessmann A, Gunn-Moore D, Penderis J. Quadrigeminal cyst management by cystoperitoneal shunt in a 4-year-old Persian cat. J Feline Med Surg. doi:10.1016/j.jfms.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sturges BK, Dickinson PJ, Kortz GD, et al. Clinical signs, magnetic resonance imaging features, and outcome after surgical and medical treatment of otogenic intracranial infection in 11 cats and 4 dogs. J Vet Intern Med 2006; 20: 648–56. [DOI] [PubMed] [Google Scholar]
- 10.Muilenburg RK, Fry TR. Feline nasopharyngeal polyps. Vet Clin North Am Small Anim Pract 2002; 32: 839–49. [DOI] [PubMed] [Google Scholar]
- 11.Burke EE, Moise NS, de Lahunta A, Erb HN. Review of idiopathic feline vestibular syndrome in 75 cats. J Am Vet Med Assoc 1985; 187: 941–43. [PubMed] [Google Scholar]
- 12.Reder MS, Mathog RH, Capps MJ. Comparison of caloric and sinusoidal tests in the vestibulotoxic cat. Laryngoscope 1977; 87: 2008–15. [DOI] [PubMed] [Google Scholar]
- 13.James CC, Lassman LP, Tomlinson BE. Congenital anomalies of the lower spine and spinal cord in Manx cats. J Pathol 1969; 97: 269–76. [DOI] [PubMed] [Google Scholar]
- 14.Bichsel P, Vandevelde M, Lang J. Spinal cord infarction following fibrocartilaginous embolism in the dog and cat. Schweiz Arch Tierheilkd 1984; 126: 387–97. [PubMed] [Google Scholar]
- 15.Mikszewski JS, Van Winkle TJ, Troxel MT. Fibrocartilaginous embolic myelopathy in five cats. J Am Anim Hosp Assoc 2006; 42: 226–33. [DOI] [PubMed] [Google Scholar]
- 16.Marioni-Henry K, Van Winkle TJ, Smith SH, Vite CH. Tumors affecting the spinal cord of cats: 85 cases (1980–2005). J Am Vet Med Assoc 2008; 232: 237–43. [DOI] [PubMed] [Google Scholar]
- 17.Lane SB, Kornegay JN, Duncan JR, Oliver JE. Feline spinal lymphosarcoma: A retrospective evaluation of 23 cats. J Vet Intern Med 1994; 8: 99–104. [DOI] [PubMed] [Google Scholar]
- 18.Seawright AA, English PB. Hypervitaminosis A and deforming cervical spondylosis of the cat. J Comp Pathol 1967; 77: 29–39. [DOI] [PubMed] [Google Scholar]
- 19.Polizopoulou ZS, Kazakos G, Patsikas MN, Roubies N. Hypervitaminosis A in the cat: A case report and review of the literature. J Feline Med Surg 2005; 7: 363–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knipe MF, Vernau KM, Hornof WJ, LeCouteur RA. Intervertebral disc extrusion in six cats. J Feline Med Surg 2001; 3: 161–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams KJ, Summers BA, de Lahunta A. Cerebrospinal cuterebriasis in cats and its association with feline ischemic encephalopathy. Vet Pathol 1998; 35: 330–43. [DOI] [PubMed] [Google Scholar]
- 22.Jubb KV, Saunders LZ, Coates HV. Thiamine deficiency encephalopathy in cats. J Comp Pathol 1956; 66: 217–27. [DOI] [PubMed] [Google Scholar]
- 23.Penderis J, McConnell FJ, Calvin J. Magnetic resonance imaging features of thiamine deficiency in a cat. Vet Rec 2007; 160: 270–72. [DOI] [PubMed] [Google Scholar]