The 2002–03 severe acute respiratory syndrome (SARS) outbreak has changed public health in many ways in China and worldwide. This change is reflected in China's effective control of H1N1, H5N1, and H7N9 influenza outbreaks; response to imported cases of Zika virus infection, Rift Valley fever, and Yellow fever; and China's active involvement in the fight against Ebola virus disease in west Africa in 2014. After the SARS outbreak, intensified actions have been taken in China to reduce the burden of infectious diseases, such as substantial investment in public health, capacity building for laboratory testing, surveillance system enhancement, national intervention programmes for specific diseases, and maintenance of a close collaboration with international partners.1 Since the implementation of these efforts, how has the situation developed regarding infectious disease epidemics in China? What can the world learn from China's approach to infectious disease control? What role can China play in global public health?
A study published in The Lancet Infectious Diseases 2 addressed these issues and aimed to explore the epidemic features during the first decade after the SARS outbreak (2004–13) by analysing surveillance data on 45 notifiable infectious diseases. In their Article,2 Shigui Yang and his colleagues reported that the overall incidence of infectious diseases in China has maintained an increasing trend (annual percentage change 5·9%). Of 45 notifiable diseases, 20 presented a striking decreasing trend, while ten other diseases continued to rise. What are the implications of these comprehensive findings on various diseases?
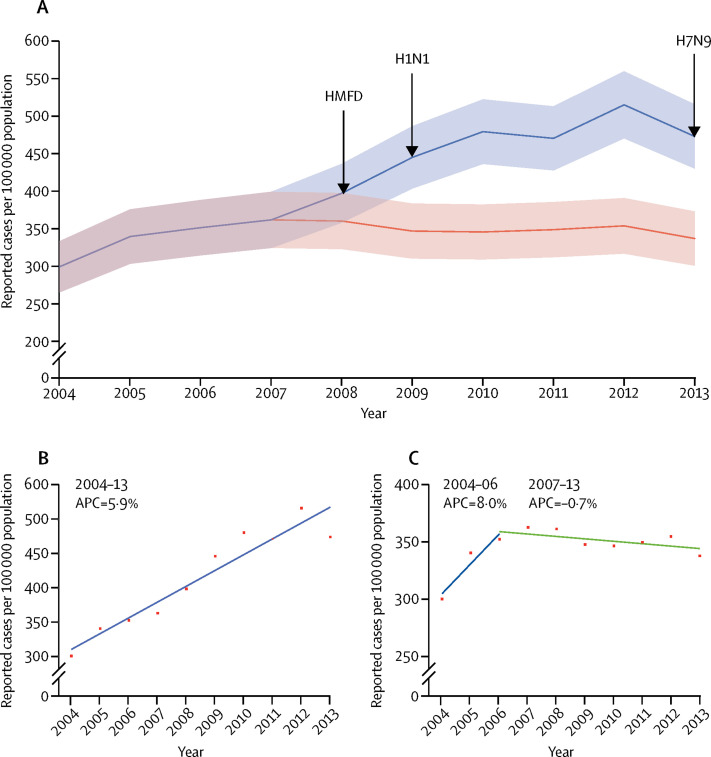
In an effort to combat emerging infectious diseases, the notifiable disease list in China was made adjustable on the basis of the threat assessment of the specific disease. Since 2004, three emerging diseases have been added as mandatory report diseases: hand, foot, and mouth disease in 2008; influenza A H1N1 pdm09 in 2009; and human infection with the avian influenza A H7N9 virus in 2013. Excluding these three new diseases, the overall incidence of the remaining consistently reported diseases, estimated by a joinpoint regression model,3 showed a two-stage feature of opposite changes. In the first stage, the overall rate of reported infectious diseases rose rapidly in 2004–06, with an annual percentage change of 8·9%, which is probably attributable to the improved sensitivity of the surveillance system by the adoption of a new web-based reporting approach since the SARS outbreak.1 In the second stage, the overall trend showed a slight reduction with an annual percentage change of −0·7% in 2007–13. Whether or not the three newly added diseases are considered, the pattern of the overall trend of infectious disease occurrence showed significant differences between the two stages (figure ). Unfortunately, this fact was overlooked in Yang and colleagues' report,2 but should be noted by readers .
Figure.
Temporal trend of overall rate of reported cases of notifiable infectious diseases in China, 2004–13
(A) Overall trend of notifiable infectious diseases, 2004–13. Red line denotes the overall trend of 42 consistently reported diseases; pink shading denotes 95% CI. Blue line denotes overall trend of all 45 notifiable diseases; light blue shading denotes 95% CI. Solid vertical arrows at years 2008, 2009, and 2013 denote the addition of new diseases to the notifiable infectious disease list. (B) Yearly APC of overall rate of reported cases in 2004–13 including newly added diseases. Red squares denote the observed values; blue line represents the slope of the APC. (C) Yearly APC of overall rate of reported cases in 2004–13 excluding newly added diseases. Red squares denote the observed values; the blue line indicates the slope of the APC for 2004–06; and the green line indicates the slope of the APC for 2007–13. APC=annual percentage change. HFMD=hand, foot, and mouth disease. H1N1=influenza A H1N1 pdm09. H7N9=human infection with avian influenza A H7N9 virus.
From 2004 to 2013, similar to the striking rate of increase in annual gross domestic product in China (7·7–11·9%),4 the epidemic trend of many infectious diseases showed notable increases or decreases, comprehensively driven by evolving socioeconomic, environmental, and causal factors.
Active introduction of new vaccine-preventable diseases into the National Immunization Program in China, which included 15 diseases since 2007, led to a sharp reduction in the overall number of cases of vaccine-preventable diseases according to routine surveillance data and the nationwide seroprevalence survey.5, 6
In response to WHO's activity in the worldwide fight against neglected tropical diseases, a large-scale, active, case-screening strategy was adopted in China for specific parasitic diseases (eg, schistosomiasis and hydatid), which led to a large increase in reported cases. However, the national survey of parasitic infection showed that the real overall incidence of parasitic diseases declined constantly.7 Under the leadership of the national and local governments and implementation of a one-health strategy, along with close joint multisectoral collaboration between the departments of health, agriculture, and the environment, some parasitic diseases have reached or approached elimination status. The elimination of filariasis throughout China was certified in 2007 by WHO. Furthermore, the goal of nationwide malaria elimination by 2020 was established, and schistosomiasis is close to being eliminated.
Additionally, in China, screening of blood donors and surgical patients for HIV, hepatitis B virus, hepatitis C virus, and syphilis have been successively required since the 1990s, which facilitated the active identification of new and past infections of these pathogens.8, 9 However, further studies are needed to assess actual incidence trends.
As a whole, due to the unprecedented rapid development of urbanisation and industrialisation in China in the past three decades, the pattern of interaction between human beings and pathogens has changed greatly, substantially altering disease epidemiology. Therefore, to better understand the epidemiological features, changing trends, and severity of diseases, a well functioning public health surveillance system, integrated with population-based studies on specific diseases, should be continually intensified to effectively plan, implement, evaluate, and improve disease control strategies. China's experience can be shared with the rest of the world.
Acknowledgments
We declare no competing interests. We thank experts from the Chinese Center for Disease Control and Prevention (Liping Wang, Qiaohong Liao, Xiang Ren, Mengjie Geng, Lingjia Zeng, Shan Lu, Xiaofang Wang, Guomin Zhang, Dan Wu, Lijuan Zhang, Yan Cui, Lin Pang, Lixia Wang, Daxin Ni, Xiaochun Wang, and Songwang Wang), and experts from the Beijing Center for Disease Control and Prevention (Jiang Wu and Hongyan Lu), who attended the discussion meetings and made contributions to this Comment.
References
- 1.Wang L, Wang Y, Jin S. Emergence and control of infectious diseases in China. Lancet. 2008;372:1598–1605. doi: 10.1016/S0140-6736(08)61365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang S, Wu J, Ding C. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017;17:716–725. doi: 10.1016/S1473-3099(17)30227-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 4.National Bureau of Statistics of the People's Republic of China Annual national report of statistics. http://www.stats.gov.cn/tjsj/tjgb/ndtjgb/ (accessed July 24, 2017; in Chinese).
- 5.Cui F, Shen L, Li L. Prevention of chronic hepatitis B after 3 decades of escalating vaccination policy, China. Emerg Infect Dis. 2017;23:765–772. doi: 10.3201/eid2305.161477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang X, Bi S, Yang W. Epidemiological serosurvey of hepatitis B in China—declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27:6550–6557. doi: 10.1016/j.vaccine.2009.08.048. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Utzinger J, Zhou XN. Schistosomiasis control: experiences and lessons from China. Lancet. 2008;372:1793–1795. doi: 10.1016/S0140-6736(08)61358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li L, Li KY, Yan K. The history and challenges of blood donor screening in China. Transfus Med Rev. 2017;31:89–93. doi: 10.1016/j.tmrv.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Song Y, Bian Y, Petzold M, Ung CO. Prevalence and trend of major transfusion-transmissible infections among blood donors in western China, 2005 through 2010. PLoS One. 2014;9:e94528. doi: 10.1371/journal.pone.0094528. [DOI] [PMC free article] [PubMed] [Google Scholar]