Abstract
Over the past decade there has been a dramatic increase in international adoptions in the United States. While most adopted children will have common illnesses, others may have unique medical issues as a result of the conditions in their birth country requiring a broadened differential diagnosis. Knowledge of these issues is essential in the management of these patients. This review will predominately focus on infectious disease issues commonly seen in international adoptees but will also discuss other medical conditions and some of the psychosocial issues which may be encountered by caregivers in the emergency department.
THE DEMOGRAPHICS OF INTERNATIONAL ADOPTION have shown a significant increase in the number of internationally adopted children in the United States over the past decade. In 2002, US citizens adopted 20,099 children from more than 20 different countries, an increase from 6,472 international adoptees in 1992.1 In addition to the increase in the number of children internationally adopted, there has also been a shift in the countries where these children originate towards countries with a low per capita income (Fig 1) and children residing primarily in institutionalized settings. These shifting demographics account not only for changes in the epidemiology of infectious diseases but also an increase in developmental and psychological issues resulting from the effects of institutionalization. Today, the majority of internationally adopted children have resided their entire lives in orphanages. The exceptions to this are children from South Korea and Guatemala, where they are primarily cared for in foster care settings.2 There has also been a shift in recent years to a female predominance, with a larger number of children adopted from China where there is a birth parent preference of boys over girls, leaving many infant girls available for adoption. While children of all ages are available for adoption, 90% of internationally adopted children are younger than 5 years of age when they join their new families.1 There are several unique challenges in delivering medical care to international adoptees. While all international adoptees share a common history of the loss of their birth family, there are country-specific risks that should be considered. These risks may change over time as conditions in the birth countries change or as children are adopted from a broader range of countries. Children who are available for adoption are often the most impoverished children in their countries. Maternal health issues such as malnutrition, congenital infections, and tobacco, drug, and alcohol exposure are common, and these conditions may lead to prenatal insults resulting in long term medical and developmental issues for the child. Life in the orphanage also adds additional nutritional and infectious disease risks, and a lack of stimulation may lead to developmental delays and attachment issues. It is often difficult to fully assess the risk for any given child. If past medical information is available from the child’s birth country, the information may be unreliable or uninterpretable, but it is certainly important to review whatever information is available.3, 4, 5 While adoptees routinely have a medical evaluation in their birth country just before arriving in the United States, the examination is cursory, and infectious diseases and other conditions are often overlooked.6, 7, 8 Thus, it is recommended that all international adoptees be evaluated within the first two weeks of arrival in the United States, or immediately if there is an acute illness.3, 6, 7, 8 Parents may seek care for their children in the emergency department (ED) for emergencies or for less severe conditions because as new parents they are unaware of the severity of their child’s illness or because they have not yet found a primary care provider for their child.
Figure 1.
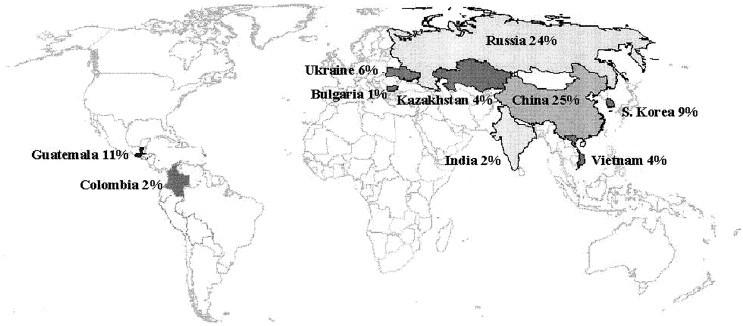
Top 10 countries of origin with percentages of international adoptees coming into the United States in 2002.1
General approach to the newly adopted child and their family
International adoptees often face challenges that can affect their transition to their new families. Some of these include language barriers, cultural differences, and environmental changes, which may result in disturbances in sleeping, eating, and overall behavior. Many adoptees will be malnourished and developmentally delayed.9, 10, 11, 12 In addition, life in institutionalized settings with limited caregiver involvement can result in self-stimulatory behaviors and altered responses to new sensory stimuli. Without knowledge of these issues, the initial presentation of some children can cause concern for the caregiver unfamiliar with internationally adopted children who have just arrived to the United States. While the transition of living in an orphanage to joining a loving family is often a difficult transition for internationally adopted children, it is also important to realize that the parents’ transition is often just as difficult. Parents are often physically and emotionally exhausted and frequently lack confidence in their role as new parents. Awareness of these issues can provide insight into the psychological state of the family so that the best care can be provided. Because parents often have little command of their child’s birth language, it is often difficult to obtain information about the child’s symptoms. Utilizing interpreter services, especially for children two years and older, can be extremely helpful.
Infectious disease issues
Infectious diseases are the most common medical issues identified in international adoptees. Because of the high prevalence of intestinal parasites and tuberculosis in resource-poor countries and the lack of perinatal screening for hepatitis B, syphilis, and HIV, international adoptees are at increased risk for these infections.7 The importance of an initial screening evaluation was demonstrated in a study where 67% of internationally adopted children were diagnosed with hepatitis B, intestinal pathogens, or tuberculosis.13 Most of these infections were only identified by doing these screening tests since infections with tuberculosis, hepatitis B, syphilis, and intestinal parasites are often asymptomatic. The American Academy of Pediatric’s Committee on Infectious Diseases recommends that international adoptees be screened for these infections shortly after arrival to the United States (Table 1). 7 In addition, specialists in the field have recommended other tests be done as well.3, 6, 13, 14, 15, 16 Some children may not have had their initial evaluation, thus the ED physician should determine whether testing has been done, and if not, these screening tests should be completed or recommended to the family. Other testing may be indicated based on the child’s symptoms and clinical findings as well as the child’s country of origin and other risk factors identified from their past medical history.
TABLE 1.
| Infectious Disease Screening: | Other Screening Tests: |
|---|---|
| Hepatitis B virus serology∗ | Complete blood count with red blood cell indices |
| Hepatitis B surface antigen | Hemoglobin electrophoresis |
| Hepatitis B surface antibody | Glucose-6-phosphate dehydrogenase level |
| Hepatitis B core antibody | Lead level |
| Hepatitis C virus antibody∗ | Thyroid stimulating hormone |
| Syphilis serology | |
| Nontreponemal tests (RPR, VDRL, ART) | |
| Treponemal tests (MHA-TP, FTA-ABS) | |
| HIV 1 and 2 serology∗ | |
| Stool for ova and parasites (3 specimens) | |
| Stool for Giardia lamblia and Cryptosporidia antigen (1 specimen) | |
| Mantoux (PPD) intradermal tuberculin skin test∗ |
ART, Automated reagin test; FTA-ABS, fluorescent treponemal antibody absorption; MHA-TP, microhemagglutination-T pallidum; PPD, purified protein derivative; RPR, rapid plasma reagin; VDRL, Venereal Disease Research Laboratory.
Also assess 6 months after arrival.
Common infections
Gastroenteritis, upper respiratory tract infections, and otitis media are common childhood infections in general and are also frequently seen in international adoptees. Internationally adopted children are at increased risk for many common infectious diseases because of poor sanitation and crowded living conditions in their birth countries. Recurrent and chronic otitis media are commonly seen in international adoptees. The prevalence of antibiotic resistance has not been well described but should be taken into consideration if an infection does not clear with an appropriate course of antibiotics. While lower respiratory tract infections may be caused by common viral or bacterial pathogens, tuberculosis must also be considered in any internationally adopted child with pneumonia. While viruses are the most common cause of diarrheal illness in US-born children, in international adoptees, the differential diagnosis must be broadened to include other infectious etiologies, post-infectious diarrhea, malnutrition, malabsorption, and dietary changes.
Vaccine-preventable diseases
Because vaccine-preventable diseases are infrequently encountered in the United States, the ED physician must have a heightened awareness of these infections when evaluating internationally adopted children. Reports of many vaccine-preventable diseases including pertussis,17 measles,18, 19, 20 mumps,20 hepatitis B,2, 5, 11, 14, 21, 22 hepatitis A,14, 23 and paralytic polio14 have been reported in internationally adopted children.
Immunization status of international adoptees
Diphtheria, tetanus, pertussis (DTP), polio, hepatitis B, and measles vaccines are available worldwide as part of the routine immunization schedule recommended by the World Health Organization. In addition, for tuberculosis prevention, the Bacillus Calmette-Guerin (BCG) vaccine is commonly used across the world in countries where tuberculosis is endemic. Other routine vaccines recommended in the US immunization schedule, such as Haemophilus influenzae type b, pneumococcal, varicella, mumps, and rubella, may not be available or routinely administered in the birth countries of international adoptees. Documentation of immunizations may not always be available,24 and similarly, children who have had varicella or measles may not have any documentation of these diseases. Several studies have been done to determine if documented birth country immunizations of internationally adopted children could be verified through serologic testing.24, 25, 26, 27, 28 The results of these studies are not in agreement, with some showing poor protection and others showing good protection. Differences in study design and laboratory methods likely account for the different results. With the lack of consensus in this matter, there are currently two acceptable approaches recommended to assure that internationally adopted children are protected against vaccine-preventable diseases.7, 29 The first approach is to reinitiate all immunizations regardless of documentation; the second approach is to use serologic testing to determine which immunizations are needed, with or without documentation of immunization. Because antibody testing for one vaccine may not be predictive for others, a combination of reimmunization and antibody testing could be utilized. Serologic testing is available for most vaccine antigens (Table 2). Testing for measles, mumps, rubella, and varicella should only be done in children older than 12 months of age because of the possible presence of maternal antibody. For varicella vaccine, serologic testing is likely to be cost-effecting in school-aged children30; however, cost-effectiveness analyses of serotesting for other vaccines has not been reported to date.
TABLE 2.
| Children ≥ 5 Months of Age: | Children ≥ 12 Months of Age: |
|---|---|
| Diphtheria IgG ELISA | Diphtheria IgG ELISA |
| Tetanus IgG ELISA | Tetanus IgG ELISA |
| Polio neutralizing antibody to serotypes 1–3 | Polio neutralizing antibody to serotypes 1–3 |
| Hepatitis B surface antibody | Hepatitis B surface antibody |
| Rubeola (measles) antibody | |
| Mumps antibody | |
| Rubella antibody | |
| Varicella antibody |
ELISA, Enzyme-linked immunosorbent assay; IgG, immunoglobulin G.
Diphtheria
While diphtheria has never been reported in an international adoptee, the diphtheria epidemic that occurred in Eastern Europe including Russia and Ukraine, and Central Asia in the 1990s points out the need to consider this diagnosis in children from countries where diphtheria is reported and immunization coverage is poor.31 The initial presentation of respiratory diphtheria is non-specific with a gradual onset of a sore throat and low-grade fever over 1 to 2 days. An adherent membrane over the tonsils, pharynx, or nose can be seen on physical examination. Symptoms may progress to diffuse cervical lymphadenitis or neck swelling with complications of upper airway obstruction, toxic myocarditis, and peripheral neuropathies. The diagnosis is made by obtaining cultures from the nose, throat, or mucous membrane lesions. The laboratory should be notified if there is a suspicion of diphtheria since special media and precautions are required.7 If the diagnosis is strongly suspected, local public health officials should be notified. Because infection can lead to rapid clinical deterioration, any clinical diagnosis or suspicion warrants administration of a single dose of equine antitoxin. In addition, erythromycin or penicillin should be given for a 14-day course.7
Tetanus
The concern about immunization coverage and protection in adoptees makes tetanus prophylaxis a challenge. Questions regarding tetanus prophylaxis may arise in the adoptee who presents to the ED with an open wound. Even with documentation of tetanus immunization from the child’s birth country, one cannot be assured the vaccine was effective. Thus, if tetanus protection has not been verified serologically and the child has a tetanus-prone wound, the child should be given human tetanus immune globulin and a tetanus toxoid vaccine (DTaP for children less than 7 years of age or Td for children 7 years or older).7
Pertussis
Despite wide-spread immunization, pertussis continues to be prevalent in the United States and throughout the world. Under-immunized children and infants are at the greatest risk for pertussis in the United States.32 While pertussis has not been commonly reported in adoptees, a case in a 10-month-old adoptee from Russia with an upper respiratory infection and cough and no previous history of immunization has been published.17 Because initial symptoms in the catarrhal stage of pertussis are indistinguishable from the common cold, pertussis is often not recognized. The paroxysmal stage follows with sudden recurrent coughing episodes interspersed with inspiratory whoops. The diagnosis is made by obtaining a specimen from the nasopharynx by aspiration or swab for culture on special medium.7, 32 A direct immunofluorescence assay (DFA) can be done, but it is not as reliable as culture as there is variable sensitivity and low specificity.7 Polymerase chain reaction assays are available and can provide rapid and sensitive results.7 Lymphocytosis in a child with clinical symptoms of pertussis supports the diagnosis. Erythromycin estolate is the treatment of choice; however, azithromycin or clarithromycin may be as effective and may have fewer side effects with increased compliance. Antibiotic prophylaxis is recommended for contacts.7
Measles
Measles continues to be endemic in most developing countries. The number of international adoptees with measles has increased from 2% (1 case) in 1997 to 20% (10 cases) in 2001 in the United States.18 In 2001, an outbreak of 14 measles cases occurred in international adoptees from China, their family members, and close contacts.18 Because measles is so infrequently encountered in the United States, physicians need to be aware of the clinical findings of measles and have a high index of suspicion in any foreign-born child with a fever and rash. The classic presentation is fever, cough, coryza, conjunctivitis, an erythematous maculopapular rash, and pathognomonic enanthemas known as Koplik spots.7 Children may also have otitis media, bronchopneumonia, croup, diarrhea, and acute encephalitis.7 A rare post-infectious neurologic complication of measles, subacute sclerosing panencephalitis, was reported in an adoptee from Thailand 9 years after arrival in the US.19 The initial diagnosis of measles is made on clinical grounds and is confirmed by obtaining a single IgM serum antibody test for measles.7 Treatment is supportive, however Vitamin A supplementation is recommended for children 6 months to 2 years of age who are hospitalized with measles or its complications.7
Hepatitis B
Hepatitis B virus (HBV) is a major public health problem throughout the world (Fig 2). In international adoptees, rates have been highest among Romanian adoptees from the early 1990s where 53% had markers of past or present hepatitis B infection and 20% of children had active infection.21 More recent studies have consistently shown a 3% to 5% prevalence of HBV in international adoptees.2, 5, 11, 14, 21 Adoptees are most often infected from their birth mothers and are therefore at high risk of having chronic infection. Acquisition can also occur from exposure in the orphanage or from blood products or contaminated needles. Children are commonly asymptomatic and are therefore only identified through serologic screening. Initial serologic testing should include hepatitis B surface antigen (HBsAg), hepatitis B core antibody (HBcAb), and hepatitis B surface antibody (HBsAb). Children with HBsAb alone have evidence of HBV immunization. Those with HBsAg and HBcAb have either acute or chronic HBV infection. The diagnosis of chronic hepatitis B infection is made if the HBsAg persists for greater than 6 months. Children with HBsAb and HBcAb have recovered HBV infection and are not contagious and do not need further immunization. Because HBV has a long incubation period, negative serology may not reflect infection just before immigration; therefore, repeat testing 6 months after arrival to the United States is recommended.7 If a child is found to have hepatitis B infection, it is important to assess whether there have been any exposures and whether prophylaxis is needed. In addition, plans should be made to assure all family members have been immunized. Children with chronic hepatitis B infection should be referred to and managed by a pediatric hepatologist. Therapy with interferon-alpha and lamivudine have been effective in some patients with chronic hepatitis B infection but appear to be less effective in infections acquired during early childhood.7
Figure 2.
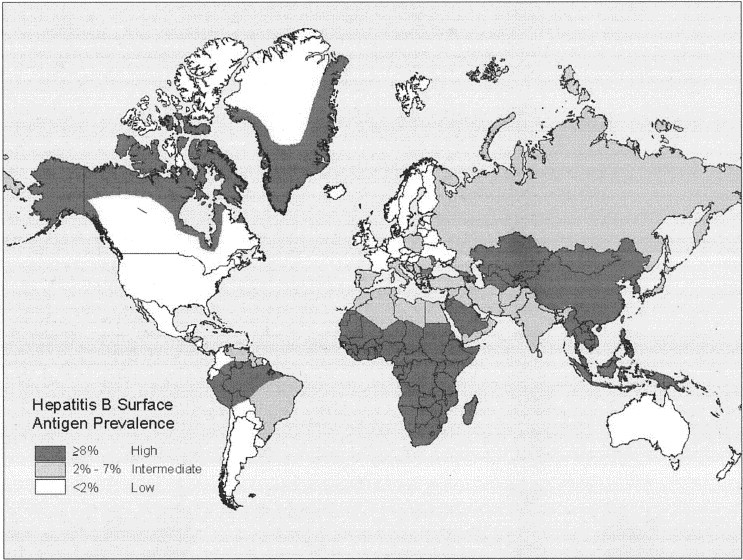
Geographic distribution of Hepatitis B prevalence.8
Other infectious diseases
Hepatitis A & C
Serology for infectious causes of hepatitis should be considered in any adoptee presenting with symptoms of hepatitis; however, it is important to remember that most children with hepatitis A, B, or C will be asymptomatic. Other infectious etiologies, such as cytomegalovirus and Epstein-Barr virus, as well as non-infectious etiologies, should also be considered in a child with hepatitis. While routine serologic screening for hepatitis A infection is not recommended, testing may be considered for children more than two years of age who live in states with a high prevalence of hepatitis A where hepatitis A immunization is recommended.7 Children with hepatitis A infection with or without symptoms can transmit infection to others.23 If hepatitis A is diagnosed, prophylaxis of family members may be indicated.7
Hepatitis C virus (HCV) infection has rarely been identified in international adoptees33 with no cases of HCV in the most recent case series of 504 international adoptees.2 Similar to HBV, most children with HCV have acquired the infection from their birth mothers and are asymptomatic. Screening for HCV is recommended for children from China, Russia, Eastern Europe, and Southeast Asia, or from countries with a high prevalence of HCV.7 Also, children with a history of blood product transfusion or maternal drug use warrant screening.7 The recommended serologic testing is an antibody test for hepatitis C. If this test is positive, a confirmatory polymerase chain reaction assay should be done.7
Tuberculosis
Tuberculosis is highly prevalent in the countries of origin of international adoptees.33, 34 Not surprisingly, international adoptees have tuberculosis infection rates four to six times higher than children born in the United States,8, 33, 34 with infection rates ranging from 0.6% to 19%.2, 5, 11, 14, 35, 36 In the most recent case series where the highest rates of infection were found, all tuberculosis skin tests (TST) were read by a health care professional.2 Most screenings in adoptees reveal latent tuberculosis infection (LTBI), defined as Mycobacteria tuberculosis infection in a person with a reactive TST and a normal physical examination and chest radiograph.7 Tuberculosis disease in international adoptees has only rarely been reported.36, 37 In one series of Korean adoptees, the overall prevalence was less than 1%.36 However, in the two children with active disease, both had negative TST pointing out the importance of having tuberculosis in the differential regardless of TST findings.36 One child had pneumonia caused by tuberculosis and recovered with treatment, while the other died from tuberculosis meningitis.36 In 1998, an adoptee from the Marshall Islands with tuberculosis infected his female guardian and 20% of the 276 contacts identified.37 Upon arrival in the United States, he had a tine test done which was never read. It was not until his guardian developed tuberculosis that he was diagnosed with cavitary tuberculosis.
While most children with tuberculosis infection have latent infection, disease should be considered in any adoptee from a country with endemic tuberculosis with pneumonia or non-specific symptoms such as fever, malaise, growth delay, weight loss, cough, night sweats, and chills.7 Chest radiographs may reveal hilar, subcarinal or mediastinal adenopathy, segmental or lobar infiltrates, pleural effusion, and, less commonly, cavitary lesions or miliary disease.7 Children with tuberculosis may have extrapulmonary manifestations involving the central nervous system, the middle ear and mastoids, lymph nodes, bones, joints, and skin.7
The Mantoux intradermal TST is recommended for screening all international adoptees for tuberculosis7 shortly after arrival, and in children with TST reactions < 10 mm of induration, repeat testing should be considered 6 months later. Induration of 5 mm or more is used when the patient has had close contact with an infectious case, is immunosuppressed, or has suspected disease by physical examination or a chest radiograph.7 False-negative tests may be seen in children who are malnourished or who have active disease. False-positive TST results can occur in children with a history of receiving the BCG vaccine. However, most adoptees have received the vaccine, and yet the vast majority of children do not have a reactive TST. A recent study conducted in Peru found the TST was frequently reactive in children who had received the BCG vaccine; however, the size of the reaction was rarely greater than 5 mm.38 A history of BCG immunization is not a contraindication to placing a TST, and a positive TST should not be attributed to the BCG vaccine.7
If the patient has a reactive TST, a thorough examination should be done and a chest radiograph should be obtained. If disease is suspected, it is important that every attempt be made to isolate the organism so that susceptibilities can be done to guide therapy. Early morning gastric aspirates should be obtained in children with suspected pulmonary tuberculosis.7 Latent tuberculosis is treated with a nine month course of isoniazid. Children with disease should be treated with a multi-drug regimen in consultation with an infectious disease specialist taking into consideration the most recent resistant patterns from the child’s country of origin.7, 15
It is not uncommon for children immunized with the BCG vaccine to develop a localized granulomatous abscess or suppurative lymphadenitis in a lymph node adjacent to the site of immunization. The granuloma is typically located on the upper arm and may or may not be draining. Culture of the drainage yields Mycobacterium bovis, the bacteria used in the BCG vaccine. There is no consensus regarding management of localized abscesses or lymphadenitis caused by BCG. Some lesions may resolve without treatment while others will require excision or treatment with isoniazid, erythromycin, or clarithromycin.39, 40
Congenital infections
Syphilis
Syphilis is infrequently reported in international adoptees, with fewer than 1% of cases identified in the studies done.2, 5, 11, 14, 21, 35 Even so, it is important to screen all adoptees for syphilis because systematic screening during pregnancy in resource poor countries is not reliably done, and there is insufficient documentation of evaluation and treatment in exposed children.7, 15 While most children with congenital syphilis will be asymptomatic, the diagnosis should be considered in adoptees with hepatosplenomegaly, snuffles, lymphadenopathy, mucocutaneous lesions, osteochondritis, pseudoparalysis, rash, hemolytic anemia, or thrombocytopenia. If untreated as infants, late manifestations may be seen in children older than 2 years of age resulting in disease of the central nervous system, bones, joints, teeth, eyes, and skin.7
Routine syphilis testing for Treponema pallidum is recommended for all adoptees regardless of history or reported treatment.7 Diagnosis is made by using both nontreponemal and treponemal testing.7 Nontreponemal tests include the Venereal Disease Research Laboratory (VDRL) slide test, the rapid plasma reagin (RPR) test, and the automated reagin test (ART), measuring antibody directed against T pallidum antigen with quantitative results. Treponemal tests include fluorescent treponemal antibody absorption (FTA-ABS) and microhemagglutination-T pallidum (MHA-TP) tests, and are used to establish the diagnosis. Any child with evidence of syphilis (a positive treponemal test) should have a thorough evaluation including a lumbar puncture to assess for central nervous system involvement. The treatment of choice is penicillin; however, the route and duration of treatment is dependent upon the age of diagnosis (less than a year of age or older) and whether there is any evidence of neurosyphilis.
HIV
Despite the worldwide epidemic of HIV, infection in international adoptees is rare. Recent studies have not identified any children infected with HIV.2, 5, 11, 14, 21 In the early 1990s, the concern about HIV infection in adoptees was greater because many children were adopted from Romanian orphanages where the HIV incidence was high.41, 42 While estimates of HIV infection in international adoptees during this era is not available, there were case reports of 2 Romanian adoptees with HIV infection.43 Recent case series only report the prevalence of false-positive HIV ELISA serology with negative confirmatory testing.2, 14
Despite the low prevalence of HIV in international adoptees, recommendations are to screen all children for HIV. Most children have documentation of negative HIV testing from their country of origin, but results should not be considered conclusive as errors in testing and reporting can occur and initial negative serology does not reflect infection acquired just before testing. Screening recommendations include serologic testing for both HIV-1 and HIV-2 shortly after arrival to the United States with consideration for repeat testing 6 months later with antibody-based assays.7
Enteric infections
Enteric infections are common among international adoptees. While intestinal parasites are felt to be more prevalent than bacterial infections or viral infections, the latter have not been systematically examined in adoptees. The prevalence of intestinal parasites has varied from 9% to 51%, depending on age and country of origin, with an increased risk in older children and children originating from countries other than Korea.2, 5, 11, 14, 21 Giardia lamblia is the most commonly identified pathogen in all series, with as many as 19% of children infected.2 The highest rates of Giardia were in children from Eastern Europe (Bulgaria 67%; Romania 50%; Moldova 36%) with lower rates in Russia (25%) and China (15%). Other protozoal infections include Blastocystis hominis, Dientamoeba fragilis, Cryptosporidium parvum, and Entamoeba histolytica.2, 11, 14, 21 Helminth infections are seen less often but include Hymenolepis species (tapeworm) and Ascaris lumbricoides and Trichuris trichiura (roundworms).2, 11, 14, 21, 44 A number of non-pathogenic parasites may also be identified through ova and parasite testing2, 14, 45 (Table 3). While these pathogens do not require treatment, they should prompt further evaluation for pathogenic parasites. Children with intestinal parasites may be asymptomatic or have symptoms ranging from acute watery diarrhea, abdominal pain, or protracted intermittent diarrhea with foul-smelling stools, flatulence, abdominal distention, and anorexia. Anorexia and malabsorption can lead to weight loss, failure to thrive, and anemia. Asymptomatic infections are common and may not be identified until the adoptee has lived in the United States for some time.33
TABLE 3.
Pathogenic and Non-Pathogenic Intestinal Parasites
| Parasite Type | Pathogens | Non-Pathogens |
|---|---|---|
| Protozoa | Entamoeba histolytica | Endolimax nana |
| Giardia lamblia | Entamoeba coli | |
| Dientamoeba fragilis | Entamoeba gingivalis | |
| Balantidium coli | Entamoeba hartmanni | |
| Blastocystis hominis | Entamoeba polecki | |
| Isospora belli | Iodamoeba butschlii | |
| Cryptosporidium parvum | Chilomastix mesnili | |
| Cyclospora cayentensis | Enteromonas hominis | |
| Microsporidia species | Retortamonas intestinalis | |
| Trichomonas hominis | ||
| Trichomonas tenax | ||
| Helminthes | Ascaris lumbricoides (common roundworm) | |
| Nematodes (roundworms) | Trichuria trichuris (whipworm) | |
| Strongyloides stercoralis (threadworm) | ||
| Enterobius vermicularis (pinworm) | ||
| Necator americanus(hookworm) | ||
| Ancylostoma duodenale (hookworm) | ||
| Cestodes (tapeworms) | Hymenolepsis species | |
| Taenia saginata (beef tapeworm) | ||
| Taenia solium (pork tapeworm) |
The diagnosis of most intestinal parasites is done by examination of stool preserved in 5% to 10% formalin and polyvinyl alcohol (PVA) or sodium-acetate formalin for ova and parasite testing. Obtaining three stool specimens 2 to 3 days apart increases the sensitivity for identification of parasites.7, 15 One stool specimen should also be sent for G lamblia and C parvum antigen testing.7 Certain parasites such as Cyclospora species and Strongyloides stercoralis may not be detected by standard ova and parasite screening, and special testing for these parasites should be considered in patients with recurrent or refractory diarrhea.7 If a parasite has been identified, specific treatment for that parasite should be initiated. Eradication does not always occur, thus repeat testing to assure the infection has cleared is recommended.
Studies have not systematically evaluated children for bacterial pathogens; however, in select children, Salmonella, Shigella, Campylobacter, and Clostridium difficile were found in 2% to 10% of international adoptees.2, 11, 14 While routine bacterial stool cultures are not recommended for all international adoptees, in children with bloody diarrhea, the stool should be cultured.
Skin infections
Dermatologic infections are frequently identified on the initial evaluation of international adoptees.3, 8, 11, 14, 35 Scabies should be considered in any internationally adopted child with a pruritic skin rash and the hair should be carefully examined for lice. Impetigo and molluscum contagiosum may also be seen. Common fungal infections such as candida diaper dermatitis and thrush as well as tinea corporis and capitis have been described. A rare dermatophyte infection of tinea caused by Trichophyton soudanense was recently reported in two adoptees from Liberia.46 In addition, unusual infections caused by Tunga penetrans, a gravid sand flea, have been reported in three international adoptees. This infestation results in painful, pruritic black lesions on the soles of the feet and sometimes associated cellulitis.47, 48 Treatment consists of flea removal, local wound care, and tetanus prophylaxis.
Other skin findings
Internationally adopted children may have scars and other skin lesions.3 Typically the child’s parents have not been given any explanation as to how these were acquired. It is important that these findings be documented to prevent false accusations about child abuse in the adoptive family. In addition, many internationally adopted children will have Mongolian spots on their buttocks and back, which may be confused as bruising. The family and the child’s health care providers should be educated that these are normal pigmented lesions in children of color.
Country-specific issues
The general approach to acute care issues in international adoptees has been addressed; however, there are some unique issues specific for certain countries and regions that warrant further discussion. Some diseases, such as cysticercosis, involving the central nervous system (CNS) may have long incubation periods and thus may not be initially considered or identified. However, in a child adopted from Central or South America, seizures or other CNS signs or symptoms should prompt the physician to consider the diagnosis of neurocysticercosis.49 The severe acute respiratory syndrome (SARS) epidemic originating in China this year underscores the need for physicians to be watchful of the changing epidemiology of infectious diseases. Malaria must be considered in children with fever who arrive from malaria-endemic countries.
Severe acute respiratory syndrome
The outbreak of SARS underscored the true global nature of infectious diseases. Although SARS was never identified in international adoptees during this outbreak, the potential for such transmission in a population involving global travel raises the issue as being pertinent to this review, especially with 25% of all adoptees originating from China. The ED may serve as the first medical encounter for patients with this acute infection. Following standard infection control guidelines on a daily basis and being aware of which children are at risk for SARS can help identify children who may have this infection and prevent the spread of disease. Because the clinical features of SARS are indistinguishable from most febrile respiratory illnesses, the clinician will need to base their clinical suspicion of SARS on both clinical and epidemiologic data. Patients with fever and a respiratory illness as well as a history of travel to a SARS-infected area or close contact with a SARS patient meet the case definition as a probable case of SARS requiring further evaluation. If SARS is suspected, there should be a coordinated effort between the child’s physician, infection control, the infectious disease physician, and the clinical laboratory to identify the cause of the child’s illness as well as to assure prevention of transmission. The diagnosis is made through laboratory testing done at the Centers for Disease Control and Prevention (CDC). Reverse transcriptase-polymerase chain reaction testing of nasopharyngeal aspirates and stool can be performed. Serologic testing can be done within the first week of symptoms.50 Treatment is supportive as there is no specific therapy of proven efficacy.
Malaria
Malaria is infrequently seen in international adoptees because most adoptees come from countries or cities were malaria is not endemic. However, malaria should always be considered in the differential diagnosis in any febrile child from tropical areas of the world where malaria is endemic Figure 3, Figure 4. Classic symptoms of malaria are cyclical high fevers with chills, rigor, sweats, and headache.7, 49 Other symptoms may include nausea, vomiting, diarrhea, cough, arthralgia, and abdominal and back pain. Signs of malaria include anemia, thrombocytopenia, pallor, jaundice, hypotension, and hepatosplenomegaly.7, 49 The clinical presentation of malaria varies by species type. Plasmodium falciparum infections are seen within the first weeks after arrival and commonly present as a nonspecific febrile illness. Severe complications may occur including cerebral malaria and shock. Patients with other malaria species may present later after arrival. P vivax and P ovale infections commonly manifest as anemia and hypersplenism, while P malariae infections are often asymptomatic or presenting with nephrotic syndrome.
Figure 3.
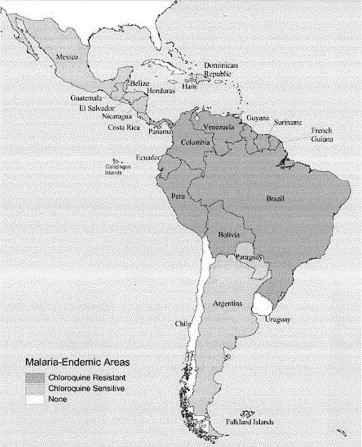
Malaria-endemic countries in the Americas, 2002.8
Figure 4.
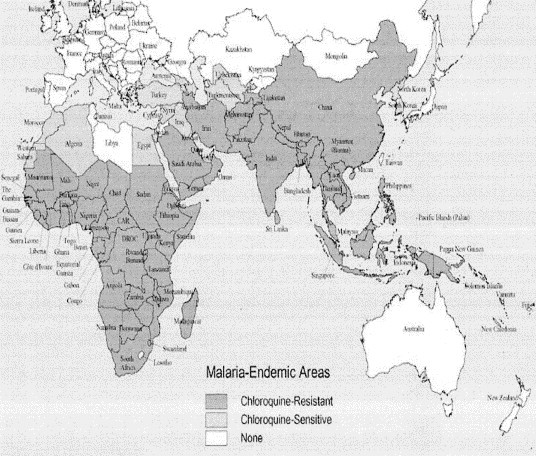
Malaria-endemic countries in Africa, the Middle East, Asia, and the South Pacific, 2002.8
The diagnosis of malaria is made by obtaining thick and thin blood smears. During a febrile episode, a complete blood count may reveal thrombocytopenia or anemia.49, 51 Electrolytes should be evaluated for hypoglycemia or acidosis associated with complications of respiratory or renal failure and a blood culture obtained to evaluate for bacteremia. Severe malaria is defined as parasitemia with greater than 5% of red blood cells, CNS or end-organ involvement, shock, acidosis, or hypoglycemia. Treatment is based on the infecting species, possible drug resistance, and disease severity. If the species type cannot be determined, treatment for drug-resistant P falciparum should be initiated. Oral therapy can be given if disease is not severe and oral medications can be tolerated. Parenteral treatment should be given for severe malaria until the parasite density decreases to less than 1%.7
Nutritional issues
Malnutrition is prevalent among newly adopted children with as many as one third of adoptees below normal weight.10 Anemia is common, affecting as many as 35% of international adoptees.6, 11, 12 While iron deficiency anemia accounts for most cases, other conditions such as alpha- or beta-thalassemia trait, lead poisoning, or glucose-6-phosphate dehydrogenase (G6PD) deficiency should also be considered. In addition, malaria or malabsorptive disorders may be associated with anemia.6, 16 A complete blood count with erythrocyte indices with an electrophoresis is suggested for evaluation of international adoptees. Because G6PD deficiency is relatively common in Asian, Mediterranean, and African populations, screening for this disorder should be considered before prescribing drugs such as trimethoprim-sulfamethoxazole and isoniazid, which can cause hemolysis in children with this deficiency.8 Anemia with eosinophilia may indicate intestinal or tissue helminthes.
Vitamin D deficiency rickets is a common diagnosis in international adoptees from Russia and Eastern Europe. While confirmation of this diagnosis has not been reported in published case series, a recent case report describes rickets in three institutionalized children adopted from the former Soviet Union which resulted in unusual bowing of the distal tibiae.52 If there is a clinical suspicion of rickets, radiographs of long bones are diagnostic and reveal classic and healing rachitic changes. Vitamin D levels and chemistry levels are often not helpful since multivitamin supplementation given to adoptees prior to evaluation may affect the results. Most cases respond to normal diet and multivitamin supplementation.3, 6, 52
Lead poisoning
Elevated blood lead levels have been reported in as many as 14% of international adoptees from China,11 Cambodia, Russia, and Eastern Europe.53 Exposure is felt to be from leaded gasoline exhaust, ceramic ware, lead-based paint, and industrial waste.8 It is recommended that all international adoptees have a lead poisoning screening done as a part of their initial evaluation.
Summary
With the marked increase of international adoptions in the United States over the past decade and the ever-changing epidemiology and global nature of infectious diseases, increasing numbers of acute infectious diseases will be encountered by the ED physician. While a broadened differential must be exercised, focus needs to be placed on commonly encountered and suspected diseases in this unique population, including vaccine-preventable diseases, tuberculosis, congenital infections, intestinal parasites, and country-specific diseases.
References
- 1.US Department of State: Immigrant visas issued to orphans coming into the US. Available at: http://travel.state.gov/orphan_numbers.html. Accessed November 12, 2003
- 2.Saiman L, Aronson J, Zhou J. Prevalence of infectious diseases among internationally adopted children. Pediatrics. 2001;108:608–612. doi: 10.1542/peds.108.3.608. [DOI] [PubMed] [Google Scholar]
- 3.Aronson J. Medical evaluation and infectious considerations on arrival. Pediatr Ann. 2000;29:218–223. doi: 10.3928/0090-4481-20000401-07. [DOI] [PubMed] [Google Scholar]
- 4.Jenista J.A. Preadoption review of medical records. Pediatr Ann. 2000;29:212–215. doi: 10.3928/0090-4481-20000401-06. [DOI] [PubMed] [Google Scholar]
- 5.Albers L.H, Johnson D.E, Hostetter M.K. Health of children adopted from the former Soviet Union and Eastern Europe: Comparison with preadoptive medical records. JAMA. 1997;278:922–924. [PubMed] [Google Scholar]
- 6.Jenista J.A. The immigrant, refugee, or internationally adopted child. Pediatr Rev. 2001;22:419–429. doi: 10.1542/pir.22-12-419. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics, Committee on Infectious Diseases . 2003 Red Book: Report of the Committee on Infectious Diseases. American Academy of Pediatrics; Elk Grove Village, IL: 2003. [Google Scholar]
- 8.Centers for Disease Control and Prevention . Health information for international travel, 2003–2004. US Department of Health and Human Services, Public Health Service; Atlanta, GA: 2003. Available at: http://www.cdc.gov/travel/other/adoption.html Accessed November 12. [Google Scholar]
- 9.Mitchell M.A, Jenista J.A. Health care of the internationally adopted child: Part 2: Chronic care and long-term medical issues. J Pediatr Health Care. 1997;11:117–126. doi: 10.1016/s0891-5245(97)90063-8. [DOI] [PubMed] [Google Scholar]
- 10.Miller L.C. Initial assessment of growth, development, and the effects of institutionalization in internationally adopted children. Pediatr Ann. 2000;29:224–232. doi: 10.3928/0090-4481-20000401-08. [DOI] [PubMed] [Google Scholar]
- 11.Miller L.C, Hendrie N.W. Health of children adopted from China. Pediatrics. 2000;105:e76. doi: 10.1542/peds.105.6.e76. [DOI] [PubMed] [Google Scholar]
- 12.Miller L.C, Kiernan M.T, Mathers M.I. Developmental and nutritional status of internationally adopted children. Arch Pediatr Adolesc Med. 1995;149:40–44. doi: 10.1001/archpedi.1995.02170130042009. [DOI] [PubMed] [Google Scholar]
- 13.Hostetter M.K, Iverson S, Dole K. Unsuspected infectious diseases and other medical diagnoses in the evaluation of internationally adopted children. Pediatrics. 1989;83:559–564. [PubMed] [Google Scholar]
- 14.Hostetter M.K, Iverson S, Thomas W. Medical evaluation of internationally adopted children. N Engl J Med. 1991;325:479–485. doi: 10.1056/NEJM199108153250706. [DOI] [PubMed] [Google Scholar]
- 15.Staat M.A. Infectious disease issues in internationally adopted children. Pediatr Infect Dis J. 2002;21:255–258. doi: 10.1097/00006454-200203000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Stauffer W.M, Kamat D, Walker P.F. Screening of international immigrants, refugess, and adoptees. Primary Care. Clinics in Office Practice. 2002;29:879–905. doi: 10.1016/s0095-4543(02)00035-0. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention Pertussis in an infant adopted from Russia—May 2002. MMWR Morb Mortal Wkly Rep. 2002;51:394–395. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Measles outbreak among internationally adopted children arriving in the United States, February-March 2001. MMWR Morb Mortal Wkly Rep. 2002;51:1115–1116. [PubMed] [Google Scholar]
- 19.Bonthius D.J, Stanek N, Grose C. Subacute sclerosing panencephalitis, a measles complication, in an internationally adopted child. Emerg Infect Dis. 2000;6:377–381. doi: 10.3201/eid0604.000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jenista J.A. Medical issues in international adoptions. Pediatr Ann. 2000;29:204–252. [Google Scholar]
- 21.Johnson D.E, Miller L.C, Iverson S. The health of children adopted from Romania. JAMA. 1992;268:3446–3451. [PubMed] [Google Scholar]
- 22.Zwiener R.J, Fielman B.A, Squires R.H., Jr Chronic hepatitis B in Romanian children. J Pediatr. 1992;121:572–574. doi: 10.1016/s0022-3476(05)81147-3. [DOI] [PubMed] [Google Scholar]
- 23.Wilson M.E, Kimble J. Post-travel hepatitis A: Probable acquisition from an asymptomatic adopted child. Clin Infect Dis. 2001;33:1083–1085. doi: 10.1086/323200. [DOI] [PubMed] [Google Scholar]
- 24.Schulte J.M, Maloney S, Aronson J. Evaluating acceptability and completeness of overseas immunization record of internationally adopted children. Pediatrics. 2002;109:e22–e26. doi: 10.1542/peds.109.2.e22. [DOI] [PubMed] [Google Scholar]
- 25.Schulpen T.W, van Seventer A.H, Rumke H.C. Immunization status of children adopted from China. Lancet. 2001;358:2131–2132. doi: 10.1016/s0140-6736(01)07188-4. [Letter] [DOI] [PubMed] [Google Scholar]
- 26.Miller L.C, Comfort K, Kely N. Immunization status of internationally adopted children. Pediatrics. 2001;108:1050–1051. [Letter] [PubMed] [Google Scholar]
- 27.Hostetter M.K, Johnson D.E. Immunization status of adoptees from China, Russia, and Eastern Europe. Pediatr Res. 1998;43:147A. [Abstr] [Google Scholar]
- 28.Staat M.A, Daniels D. Immunization verification in internationally adopted children. Pediatr Res. 2001;49:468A. [Abstr] [Google Scholar]
- 29.Atkinson W.L, Pickering L.K, Schwartz B. General recommendations on immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP) MMWR Morb Mortal Wkly Rep Recomm Rep. 2002;51:1–35. [PubMed] [Google Scholar]
- 30.Barnett E.D, Christiansen D, Figueira M. Seroprevalence of measles, rubella, and varicella in refugees. Clin Infect Dis. 2002;35:403–408. doi: 10.1086/341772. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Update: Diphtheria epidemic—New independent states of the former Soviet Union, January 1995 March 1996. MMWR Morb Mortal Wkly Rep. 1996;45:693–697. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention Pertussis-United States, 1997–2000. MMWR Morb Mortal Wkly Rep. 2002;51:73–76. [PubMed] [Google Scholar]
- 33.Chen L.H, Barnett E.D, Wilson M.E. Preventing infectious diseases during and after international adoption. Ann Intern Med. 2003;139:371–378. doi: 10.7326/0003-4819-139-5_part_1-200309020-00013. [DOI] [PubMed] [Google Scholar]
- 34.Zuber P.L, McKenna M.T, Binkin N.J. Long-term risk of tuberculosis among foreign-born persons in the United States. JAMA. 1997;278:304–307. [PubMed] [Google Scholar]
- 35.Lange W.R, Warnock-Eckhart E. Selected infectious disease risks in international adoptees. Pediatr Infect Dis J. 1987;6:447–450. doi: 10.1097/00006454-198705000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Lange W.R, Warnock-Eckhart E, Bean M.E. Mycobacterium tuberculosis infection in foreign born adoptees. Pediatr Infect Dis J. 1989;8:625–629. doi: 10.1097/00006454-198909000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Curtis A.B, Ridzon R, Vogel R. Extensive transmission of Mycobacterium tuberculosis from a child. N Engl J Med. 1999;341:1491–1495. doi: 10.1056/NEJM199911113412002. [DOI] [PubMed] [Google Scholar]
- 38.Santiago E.M, Lawson E, Gillenwater K. A prospective study of Bacillus Calmette-Guerin scar formation and tuberculin skin test reactivity in infants in Lima, Peru. Pediatrics. 2003;112:e298. doi: 10.1542/peds.112.4.e298. [DOI] [PubMed] [Google Scholar]
- 39.Torres-Rojas J.R, Rondon-Lugo A, Vidal R. Short course of clarithromycin in an immunocompetent patient with BCG-induced regional complications. Dermatol Online J. 2002;8:6. Available at: http://dermatology.cdlib.org/DOJvol8num2/case_reports/BCG/Torres.html Accessed November 12, 2003. [PubMed] [Google Scholar]
- 40.FitzGerald J.M. Management of adverse reactions to Bacille Calmette-Guerin vaccine. Clin Infect Dis. 2000;31(Suppl 3):S75–76. doi: 10.1086/314074. [DOI] [PubMed] [Google Scholar]
- 41.Rudin C.H, Berger R, Tobler R. HIV-1, hepatitis (A, B, and C), and measles in Romanian children. Lancet. 1990;336:1592. doi: 10.1016/0140-6736(90)93380-8. [DOI] [PubMed] [Google Scholar]
- 42.Patrascu I.V, Constantinescu S.N, Dublanchet A. HIV-1 infection in Romanian children. Lancet. 1990;335:672. doi: 10.1016/0140-6736(90)90466-i. [DOI] [PubMed] [Google Scholar]
- 43.Kurtz J. HIV infection and hepatitis B in adopted Romanian children. Br Med J. 1999;13:741–749. [letter] [Google Scholar]
- 44.Macariola D.R, Daniels D, Staat M.A. Intestinal parasites in an international adoptee. Infections in Medicine. 2002;19:13. [Google Scholar]
- 45.Zeibig E.A. Clinical Parasitology. (ed 1) W. B. Saunders; Philadelphia, PA: 1997. [Google Scholar]
- 46.Markey R.J, Staat M.A, Gerrety M.J. Tinea capitus due to Trichophyton soudanense in Cincinnati, Ohio, in internationally adopted children from Liberia. Pediatr Dermatol. 2003;20:408–410. doi: 10.1046/j.1525-1470.2003.20507.x. [DOI] [PubMed] [Google Scholar]
- 47.Fein H, Naseem S, Witte D.P. Tungiasis in North America: A report of 2 cases in internationally adopted children. J Pediatr. 2001;139:744–746. doi: 10.1067/mpd.2001.118530. [DOI] [PubMed] [Google Scholar]
- 48.Darmstadt G.L, Francis J.S. Tungiasis in a young child adopted from South America. Pediatr Infect Dis J. 2000;19:485–487. doi: 10.1097/00006454-200005000-00024. [DOI] [PubMed] [Google Scholar]
- 49.Long S.S, Pickering L.K, Prober C.G, editors. Principles and Practice of Pediatric Infectious Diseases. (ed 2) Churchill Livingstone; Philadelphia, PA: 2003. [Google Scholar]
- 50.Centers for Disease Control and Prevention . Severe acute respiratory disease syndrome (SARS) US Department of Health and Human Services, Public Health Service; Atlanta, GA: 2003. Available at: http://www.cdc.gov/ncidod/sars Accessed December 5, 2003. [Google Scholar]
- 51.Fleisher G.R, Ludwig S, editors. Textbook of Pediatric Emergency Medicine. (ed 4) Lippincott; Philadelphia, PA: 2000. [Google Scholar]
- 52.Reeves G.D, Bachrach S, Carpenter T.O. Vitamin D-deficiency rickets in adopted children from the former Soviet Union: An uncommon problem with unusual clinical and biochemical features. Pediatrics. 2000;106:1484–1489. doi: 10.1542/peds.106.6.1484. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention Elevated blood lead levels among internationally adopted children—United States. MMWR Morb Mortal Wkly Rep. 1998;49:97–100. [PubMed] [Google Scholar]


