In this issue of Journal of Thoracic Oncology (JTO), Tian et al.1 provided the first description of early pathology of coronavirus disease—2019 (COVID-19). As of today, February 26, 2020, there have been over 78,000 confirmed cases and over 2500 deaths in the People’s Republic of China, based on the official figure by the National Health Commission of the People’s Republic of China. The infection is rapidly spreading in the United States, Europe, South Korea, Iran, and other countries. COVID-19 has already caused havoc to travel and global markets and has the potential to become a devastating disease in the People’s Republic of China and globally. It is important to realize, however, that because we are in the early stages of this outbreak, many data are incomplete and some are unreliable.
In this early stage of the outbreak, the rate of positivity outside of the People’s Republic of China is influenced mainly by the following two factors: (1) whether the city or country has a large Chinese community or is visited by a large number of Chinese tourists and (2) the number of tests conducted. For example, among European countries, Italy has performed a high number of tests for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus that causes COVID-19: as of February 26, of 9587 individuals tested, 400 were positive for SARS-CoV-2 and are currently being retested to verify the results. Not surprisingly, Italy has a much higher number of positive cases than France, which tested less than 500/18 positive, Germany which tested a few hundred, 19 of them positive, etc. Even within Italy, there are major discrepancies: the press reported that infections are almost exclusively occurring in the regions of Lombardia and Veneto. A review of the data revealed that as of February 26, 2020, Lombardia had tested 3208 individuals mostly with flu-like and upper respiratory symptoms and 258 were positive; Veneto had tested 4900 and 71 were positive. In contrast, the Center/South of Italy, regions of Abruzzo, Basilicata, Calabria, Campania, Molise, and Sardinia, together, had tested a total of 27 people, and none were positive. In other words, the more tests are performed, the more individuals are found positive for SARS-CoV-2; obviously, unless people are tested, SARS-CoV-2 infections cannot be identified (Fig. 1 ). It is clear from these numbers that it makes little sense to restrict travel to those from Lombardia and Veneto—whose citizens are now prohibited from entering several foreign countries—while allowing Italians from other regions, where only few or no tests were performed, to travel. The same argument applies to other European countries where testing has been minimal and to the United States, where, as of February 25, only 426 patients had been tested.2 For example, Hawaii, a state with a large Chinese community and large numbers of tourists from the People’s Republic of China, is presumed to be free of SARS-CoV-2 infections. The problem is that nobody has been tested as of February 26 in Hawaii! We can predict that in the coming weeks, we will have to rethink much of what we heard about the spread of this disease.
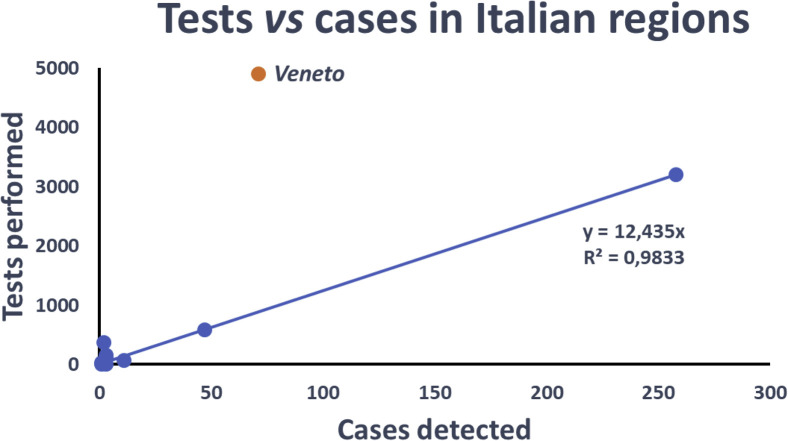
Figure 1.
As of February 26, the number of cases detected in different Italian regions is proportional to the number of polymerase chain reaction (PCR) tests performed. By sampling people in direct contact with infected individuals, one in 12 tested positive. The Veneto region is an outlier, possibly owing to testing on a larger population, not restricted to direct contacts of infected individuals. As the number of tests will increase, so will the slope of the represented line, owing to the expected decrease of the percentage of positive tests. Note that presently, owing to the relatively limited data, the curve’s fit is strongly dependent on the position of a few points.
Another problem is that the diagnosis for SARS-CoV-2 infection is currently largely based on reverse-transcriptase polymerase chain reaction (RT-PCR), and unfortunately, it is unreliable because of a high rate of false-negative and some false-positive results especially in places that perform this test in large numbers, as for example, during the Hubei crisis. In that context, the sensitivity of the PCR assay has been found largely inferior to that of a chest computed tomography.3
The main reason for the false-negative results has been traced to faulty science in the design of some PCR kits, connected to their production and standardization under pressure from the burgeoning epidemic. Faulty PCR tests have been connected to severe underdetection rates in the People’s Republic of China4 and were identified also in the United States.5
Another reason for the false negatives is that the swab used to collect the sample needs to reach the deeper pharynx, which is a delicate procedure: when many patients are in line for a test and there is pressure to hurry up, it is easy to miss. Patients with negative PCR results are sent home, and they infect more people. False positives are also common in these circumstances, because the tests are performed in hospitals with a fairly large number of patients, and thus in environments with high viral load: PCR, being a sensitive test, can easily produce false-positive results. Nevertheless, if the test is performed with a correct set of primers, and in “ideal” conditions, which means not in a hurry and not in an environment where there are many carriers, then it is probably reliable.6
Enzyme-linked immunosorbent assays, which since last week became available in the People’s Republic of China and elsewhere, are much more reliable and sensitive7 and should hopefully soon replace RT-PCR testing. Fortunately, about 80% of infected patients require no specific treatment; the disease for them is mild, like a common flu. Treatment is at the moment symptomatic; there is no scientific evidence that any specific antiviral drug works better than others—albeit several clinical trials reveal some promising results for a few compounds. By far, most people who develop a serious disease are over 70 years old. Among them, patients with cancer are at particularly high risk because they are immune-depressed. Patients with cancer are also more likely to develop a more aggressive disease and die of it.8
Why do patients die? Before this report, there had not been any data describing the early anatomical pathology lesions of this disease. This dearth of pathology description made it difficult to understand the pathogenesis of COVID-19. Therefore, for prevention, infection control, and treatment, we rely on current knowledge of SARS, which is caused by SARS-CoV. Justification for these practices stems from the genetic similarity of SARS-CoV to SARS-CoV-2, the virus that causes COVID-19, and to similarities in the clinical presentations of the illnesses caused by these viruses.
When did COVID-19 emerge? The emergence of a coronavirus not previously detected in humans was first reported in December 2019 in Wuhan, Hubei Province, in the People’s Republic of China. By the time the Chinese government decided to forbid residents to travel, about 5 million of the 14 million residents had already left Wuhan because of the Chinese New Year’s holidays and a last minute wave of “exodus,” which occurred as citizens fled Wuhan just before the “lockdown” of the city became effective at 10 am, January 23, 2020. According to official reports from the Chinese government and a peer-reviewed manuscript published in the past few days,9 the disease first manifested in early December when a small number of cases started to occur. The disease was characterized by fever, dry cough, and dyspnea. Tests for all known respiratory tract pathogens were negative.
Since then, we have learned that this disease causes death in a significant number of patients, particularly the elderly and patients with cancer.8 In the People’s Republic of China, the case fatality rate (ratio of deaths for the total number of people diagnosed with this disease) has been between 2% and 3%, although it has been as high as 4.6% in Wuhan, the epicenter of the outbreak. The cause of death among infected patients is respiratory failure. Patients manifest greatly impaired respiratory function, and they “supposedly” suffer alveolar damage, as even assisted oxygenation and intubation does not save their lives. Nevertheless, until the publication of this report1 in JTO, we did not know the underlying pathologic changes responsible for the respiratory failure in these patients. Anatomical pathology studies of lung biopsy material have not been performed because they are not necessary to make the diagnosis. Autopsies were prohibited in the People’s Republic of China for fear that those performing the autopsy could become infected. Only recently, the Chinese government allowed autopsies to be performed in P3 biosafety-level facilities—P3 suites for autopsy are not available in Wuhan. The first report of a postmortem biopsy in a single patient who died of COVID-19 was published a few days ago,10 after the article by Tian et al.1 had been submitted to JTO. These two articles allow us to see how the disease develops and progresses.
The article by Tian et al.1 was a result of an international collaboration among the senior author, Dr. Xiao, a Professor at the University of Chicago, USA, who also works several months of the year at Wuhan University, where he Chairs the Department of Pathology, and his colleagues in Wuhan. Dr. Xiao was in Wuhan when the city found itself at the center of an epidemic and when the hospitals were suddenly hit with an overwhelming number of patients, many of them severely ill: healthcare authorities and workers scrambled to offer as much care as possible to those who needed it, several of them got infected and died of COVID-19. To overcome the problem, conducting autopsies was prohibited and biopsies were not taken, and therefore nothing was known about the anatomical pathology changes that occurred in this disease. Dr. Xiao and collaborators hypothesized that the infectious rate was so high that some of the patients who were hospitalized for other diseases likely had a superimposed SARS-CoV-2 infection. By reviewing the clinical records of patients hospitalized there during the months of December 2019 and January 2020, the authors identified two patients who had underwent lobectomies to remove early-stage lung cancers with ground-glass opacities in their lungs, a characteristic radiological finding in patients infected with COVID-19. In addition, RT-PCR tests were performed for these patients, which verified the infection. The pathologic lesions identified in these patients and described in their report1 represent the early pathologic changes, as they were detected before the patients developed any clinical symptoms related to COVID-19. Both patients eventually became severely ill, and one of them died of respiratory failure.
To a certain degree, observing early-phase pathologic changes is more relevant than findings from autopsies, because the latter only offer a “glimpse” of the picture in the very end of the disease process. Therefore, this report that revealed the pathology in the lungs of two presymptomatic patients allows us, for the first time, to see the pathology of this disease at its earliest stages and understand the pathophysiology of a SARS-CoV-2 infection.
In these presymptomatic SARS-CoV-2–infected lungs, Xiao et al.1 observed edema with proteinaceous exudates.1 The high-quality images reveal patchy changes of fibrin plugs mixed with macrophages and other inflammatory cells. In one of the two cases, abundant intra-alveolar pulmonary macrophages are present. The alveolar walls or septa are expanded by proliferating fibroblasts with parallel type II pneumocyte hyperplasia. There is no significant neutrophilic exudation or infiltration, in keeping with a viral infection. There are no hyaline membrane formations at this early stage—which were instead found at autopsy.10 Nevertheless, fibroblastic plugs have formed, albeit focally, even in this early phase of the disease. These findings indicate that there is progressive consolidation of the lung, which is ultimately the cause of respiratory failure and death. Lung consolidation is not caused by accumulation of granulocytes and fibrin, but rather by intra-alveolar organization and fibrosis. Therefore, because the respiratory surface of the lung is obliterated, these patients can no longer respond to intubation and oxygen therapy: this is why they die. From this important report,1 we learn that the virus can establish infection in the lungs where it produces tissue injury well before producing symptoms, including dry cough and fever that occur later on. At this early stage, the only clue of SARS-CoV-2 infection is imaging that reveals ground-glass opacities in the periphery of the lung. These imaging findings are of particular relevance to identify infected individuals, in light of the evidence for viral spreading by asymptomatic patients, including by individuals that may test negative to PCR for SARS-CoV-2 in their upper respiratory tract.11 Therefore, presently, any patient with ground-glass opacities in the lungs should undergo SARS-CoV-2 testing.
The lesions usually start in the peripheral lung zones close to the pleura, as single or multifocal ground-glass opacities. Only when the lesions become more intense or expand do patients develop symptoms. Often, the first symptom is a dry cough. Most patients recover. Nevertheless, some experience disease progression, and their lungs contain large areas of consolidations, at which point, there is severe loss of function leading to respiratory failure.
This important work helps us understand the pathogenesis of COVID-19 and to be better prepared to identify potentially infected patients. This work is the result of an international collaboration among a highly trained US pathologist, Dr. Xiao, who had studied hantavirus infections and West Nile virus disease for many years, and who is presently a senior diagnostic pathologist at the University of Chicago. Dr. Xiao’s experience allowed him to coordinate a team of pathologists and clinicians to circumvent the problem that autopsies were not allowed, biopsies were not necessary, and yet the world needed to know more about the pathology of this disease to be prepared to face this epidemic. In the end, the outcome of the study will benefit medicine and patients throughout the world, underscoring the value of teamwork and international collaborations in medical research.
Acknowledgments
MC reports grants from the National Institutes of Health, National Cancer Institute, the US Department of Defense, and the UH Foundation through donations to support research on “Pathogenesis of Malignant Mesothelioma” from Honeywell International Inc., Riviera United-4-a Cure, and the Maurice and Joanna Sullivan Family Foundation. MC has a patent issued for BAP1. MC has a patent issued for “Using Anti-HMGB1 Monoclonal Antibody or other HMGB1 Antibodies as a Novel Mesothelioma Therapeutic Strategy” and a patent issued for “HMGB1 as a Biomarker for Asbestos Exposure and Mesothelioma Early Detection.” MC is a board-certified pathologist who provides consultation for mesothelioma expertise and diagnosis.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S.Y. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCullough M. Coronavirus will spread in the U.S., CDC warns, and there might not be enough testing capacity to detect it. The Philadelphia Inquirer. February 25, 2020. https://www.inquirer.com/health/coronavirus-pandemic-cdc-flawed-test-pcr-undetected-cases-20200225.html Accessed March 13, 2020.
- 3.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases [e-pub ahead of print]. Radiology.https://doi.org/10.1148/radiol.2020200642. Accessed March 13, 2020. [DOI] [PMC free article] [PubMed]
- 4.Yanfeng P. Nucleic acid testing is inaccurate. Caixin. 2020 [Google Scholar]
- 5.Grady D. Coronavirus test kits sent to states are flawed, C.D.C. says. The New York Times. February 12, 2020 https://www.nytimes.com/2020/02/12/health/coronavirus-test-kits-cdc.html Accessed March 13, 2020. [Google Scholar]
- 6.Corman V.M., Landt O., Kaiser M. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang W., Du R.H., Li B. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China [e-pub ahead of print]. Lancet Oncol.https://doi.org/10.1016/S1470-2045(20)30096-6. Accessed March 13, 2020. [DOI] [PMC free article] [PubMed]
- 9.Cohen J. Wuhan seafood market may not be source of novel virus spreading globally. Science. January 26, 2020 [Google Scholar]
- 10.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome [e-pub ahead of print]. Lancet Respir Med.https://doi.org/10.1016/S2213-2600(20)30076-X. Accessed March 13, 2020. [DOI] [PMC free article] [PubMed]
- 11.Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19 [e-pub ahead of print]. JAMA.https://doi.org/10.1001/jama.2020.2565. Accessed March 13, 2020. [DOI] [PMC free article] [PubMed]