Abstract
Introduction
In March 2020, Coronavirus Disease 2019 (COVID-19) arrived in Bolivia. Here, we report the main clinical findings, and epidemiological features of the first series of cases, and a cluster, confirmed in Bolivia.
Methods
For this observational, retrospective and cross-sectional study, information was obtained from the Hospitals and the Ministry of Health for the cases that were laboratory-diagnosed and related, during March 2020. rRT-PCR was used for the detection of the RNA of SARS-CoV-2 following the protocol Charité, Berlin, Germany, from nasopharyngeal swabs.
Results
Among 152 suspected cases investigated, 12 (7.9%) were confirmed with SARS-CoV-2 infected by rRT-PCR. The median age was 39 years (IQR 25–43), six of them male. Two cases proceed from Italy and three from Spain. Nine patients presented fever, and cough, five sore throat, and myalgia, among other symptoms. Only a 60 y-old woman with hypertension was hospitalized. None of the patients required ICU nor fatalities occurred in this group.
Conclusions
This is the first report of surveillance of COVID-19 in Bolivia, with patients managed mainly with home isolation. Preparedness for a significant epidemic, as is going on in other countries, and the deployment of response plans for it, in the country is now taking place to mitigate the impact of the COVID-19 pandemic in the population.
Keywords: Coronavirus disease 2019 (COVID-19), Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Epidemiology, Bolivia, Latin America
1. Introduction
After its zoonotic emergence in China, during November–December 2019 [[1], [2], [3], [4], [5], [6], [7], [8]], the Coronavirus Disease 2019 (COVID-19), caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [9], spread significantly into other countries in Asia [[10], [11], [12], [13], [14]]. Then, to other continents such as the Pacific region [15], North America [16,17], Europe [[18], [19], [20], [21], [22]], and even Africa [[23], [24], [25], [26]].
On February 25, 2020, a Brazilian traveller returned home from Lombardy, northern Italy, to São Paulo, Brazil, presenting fever, dry cough, sore throat, and coryza, being tested by the real-time reverse-transcriptase polymerase chain reaction (rRT-PCR), and with a positive result, becoming the first confirmed case in Latin America [[27], [28], [29]]. After it, other countries in Latin America, such as Mexico [30], Costa Rica, Honduras [31], Panama, in Central America, as well as Argentina, Chile, Colombia, among others in South America, including also on March 2, 2020, Bolivia, have received travellers, and diagnosed imported cases of COVID-19 in their territories.
In most of the countries of Latin America, confirmed cases have been specially imported from Italy but also from Spain. Although this scenario, no case reports or series from South America are yet available in scientific journals.
During March 2–15, 2020, the first 12 cases of SARS-CoV-2-laboratory confirmed, arrived and were diagnosed in different areas of Bolivia. Herein, we report the main clinical findings and epidemiological features of them.
2. Methods
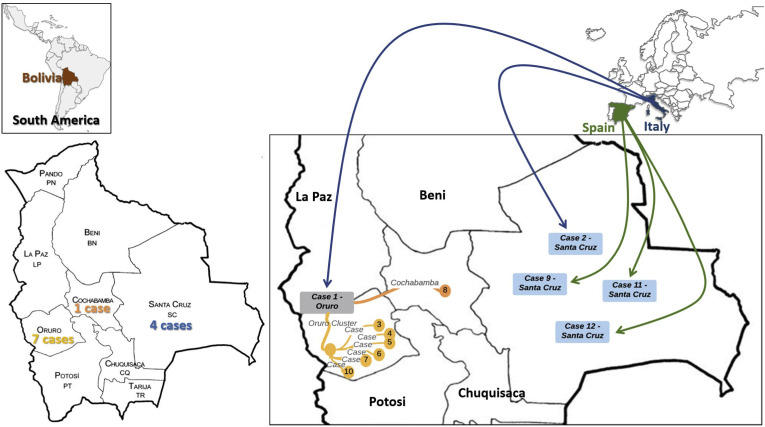
Bolivia is a South American country constituted by nine departments (main administrative level), 112 provinces (second administrative level) and 337 municipalities (third administrative level) (Fig. 1 ). The territory presents climatic, geographic, social, and epidemiological conditions suitable for the transmission of many infectious diseases (Fig. 1). Before SARS-CoV-2 arrival, Influenza and RSV, among other respiratory viruses, represent significant causes of hospitalization in different cities of the country, especially among children under one year of age [[32], [33], [34]].
Fig. 1.
Relationship and contacts between the cases of SARS-CoV-2 infection/COVID-19 in Bolivia, March 2–15, 2020.
For this observational, retrospective and cross-sectional study, the epidemiological data records were collected from the Hospitals and the Ministry of Health of Bolivia, obtaining the clinical and epidemiological data of the COVID-19 cases that were laboratory-diagnosed during March 2–15, 2020. Samples were tested by rRT-PCR to SARS-CoV-2 at the Laboratory of the National Center of Tropical Diseases (CENETROP), 2020, following the protocol Charité, Berlin, Germany [35].
Given the small number of cases, the summary of continuous variables considered the median and interquartile ranges (IQR). All analyses were performed with the statistical software Stata®14IC, licensed for Universidad Tecnológica de Pereira.
3. Results
During March 2–15, 2020, 152 suspected cases were investigated in Bolivia, especially from international travellers, most from China, Italy and Spain. Although active enhanced surveillance for respiratory tract infection begun in January 2020, considering the international warning for the 2019 novel Coronavirus, later designated as COVID-19. The first suspected cases were investigated between February 2, and March 1, 2020, including ten travellers, all negative by rRT-PCR in that period.
A total of 12 cases (7.9%) were diagnosed with COVID-19 at different departments of Bolivia (Fig. 1). The median age of patients was 39.0 y-old (IQR 25.3–43.4); six of them were male. On March 2th, 2020, a 64-year-old woman (Case 1), a Bolivian from Oruro, visiting Lombardy, Italy, during the last 14 days, with no previous history of comorbidities, returned to Bolivia, arriving at Santa Cruz, then travelling to La Paz, Cochabamba, and finally to her home in Oruro. She presented at the outpatient department of the General Hospital of Oruro, on March 3rd, 2020, complaining with fever, cough, vomiting, malaise and abdominal pain, but with no other significant signs or symptoms. Nasopharyngeal swabs obtained, and she isolated at home. Her samples tested positive for SARS-CoV-2 on rRT-PCR assays at the Laboratory of the National Center of Tropical Diseases (CENETROP) on March 10th, 2020. She was in contact with seven relatives, six in Oruro (Cases 3–7 and 10) and one in Cochabamba (Case 8), all investigated and tested positive (Fig. 1) (Table 1 ). Although negative, cases have been investigated in the rest of the departments of Bolivia (Fig. 1), including initial phone call -telemedicine- for over 15,000 individuals in the first month.
Table 1.
Clinical and epidemiological characteristics of cases of SARS-CoV-2 infection/COVID-19 in Bolivia, March 2–15, 2020.
|
Case |
Date of March 2020 | Department | Age | Sex | Date Symptoms Initiated, 2020 | Date Consultation (month/day) | Days | Hospitalization | Clinical manifestations |
Comorbidities or history | Traveller from | Started day | Returning day | Long of travel | Link to cases | Sampling place | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Cough | Malaise | Vomiting | Abdominal Pain | Tachypnea | Myalgia | Sore throat | Diarrhoea | Cephalea | Conjunctival injection | ||||||||||||||||
| 1 | 8th | Oruro | 64 | F | 3/2 | 3/3 | 1 | Outp | Y | Y | Y | Y | Y | N | N | N | N | N | N | N | Italia | 3/1 | 3/2 | 3.01 years | N | Hospital |
| 2 | 9th | Santa Cruz | 60 | F | 2/29 | 3/8 | 8 | Hosp | Y | Y | Y | N | N | Y | N | N | N | N | N | HTA | Italia | 2/7 | 3/8 | 30 days | N | Hospital |
| 3 | 10th | Oruro | 41 | F | 3/9 | 3/9 | 0 | Outp | Y | N | N | N | N | N | Y | N | N | N | N | N | – | – | – | – | C1 | Home |
| 4 | 10th | Oruro | 13 | M | Unknown | 3/8 | Unknown | Outp | N | Y | N | N | N | N | N | Y | N | N | N | N | – | – | – | – | C1 | Home |
| 5 | 10th | Oruro | 44 | M | 3/10 | 3/10 | 0 | Outp | N | Y | N | N | N | N | Y | N | N | N | N | N | – | – | – | – | C1 | Home |
| 6 | 10th | Oruro | 39 | M | 3/2 | 3/11 | 9 | Outp | N | Y | N | N | N | N | N | Y | N | N | N | N | – | – | – | – | C1 | Home |
| 7 | 10th | Oruro | 39 | F | Unknown | 3/10 | Unknown | Outp | Y | Y | N | N | N | N | N | N | N | N | N | N | – | – | – | – | C1 | Home |
| 8 | 11th | Cochabamba | 43 | M | 3/6 | 3/9 | 3 | Outp | Y | Y | N | N | Y | N | Y | Y | Y | N | Y | Previous CAP | – | – | – | – | C1 | Home |
| 9 | 11th | Santa Cruz | 27 | M | 3/9 | 3/11 | 2 | Outp | Y | N | N | N | N | N | Y | N | N | Y | N | N | Spain | 2/23 | 3/8 | 14 days | N | Hospital |
| 10 | 11th | Oruro | 18 | M | 3/8 | 3/11 | 3 | Outp | Y | Y | Y | N | N | N | N | N | Y | N | N | N | – | – | – | – | C1 | Home |
| 11 | 13th | Santa Cruz | 20 | F | 3/9 | 3/10 | 1 | Outp | Y | Y | N | N | N | N | N | Y | N | N | N | N | Spain | 2/5 | 3/11 | 35 days | N | Home |
| 12 | 15th | Santa Cruz | 30 | F | 3/13 | 3/15 | 2 | Outp | Y | N | Y | N | N | N | Y | Y | N | Y | N | N | Spain | 3/9 | 3/11 | 2 days | N | Hospital |
F, Female; M, Male; Outp, Outpatient; Hosp, Hospitalization; Y, Yes; N, No; HTA, hypertension; CAP, Community-acquired pneumonia; C1, Case 1.
In Santa Cruz de la Sierra, four cases were confirmed, three of them travellers from Italy and one from Spain (Fig. 1) (Table 1). None of these was initially detected by border officials, as suspected, but in hospitals. The median time between the initial symptoms and consultation was two days (IQR 0.25–3.00 days). From the total, only one patient was hospitalized, and the rest were isolated at home initially per 14 days. The hospitalized patient was a 60 y-old woman with hypertension, then as presenting more two risk factors, decided for close clinical observation.
Nine patients presented fever, and cough, five sore throat, and myalgia, among other symptoms (Table 1). Only two patients reported previous comorbidities, hypertension and community-acquired pneumonia (Table 1). None of the patients was previously immunized against Influenza.
Chest radiographs obtained for the patient showed no abnormalities. Real-time RT-PCR and ELISA assays for influenza A and B viruses, NS1 antigen rapid tests for dengue viruses, chikungunya, and Zika, were negative in all cases.
Patients did not receive antiviral anti-SARS-CoV-2 treatment, especially, as most of them were managed at home, symptomatically, and without further need of specialized medical care.
4. Discussion
Emerging infectious diseases, such as is the case of COVID-19 are currently prone for the risk of epidemics, or even, as has been this case, to became a Public Health Emergency of International Concern (PHEIC), and later a pandemic, as declared by the World Health Organization (WHO) [[36], [37], [38], [39]].
In this context, Latin America was the last significant region where COVID-19 arrived [27,40]. In this case, coming mainly from two European countries, Italy and Spain [[18], [19], [20], [21], [22]]. In Bolivia, the first two cases came from Italy. Especially in the north of that country, significant epidemics are going on. For the moment of the arrival of the first Bolivian COVID-19 case, there were 7,375 cases in Italy, with 366 deaths. The ninth, eleventh, and twelfth cases came from Spain. For the moment of the arrival of these cases, the last on March 15, 2020, there were 7,988 cases in Spain. That issue has been a common trend in Latin America now, imported cases from Italy and Spain [27,41,42]. This highlights the relevance of the spread of the COVID-19 due to population movements that has affected Bolivia, but also countries in South America, and most in the Latin American and the Caribbean region.
As has occurred in other affected countries elsewhere, there is a risk of local clusters of transmission from imported cases [1,[43], [44], [45], [46]]. Precisely, the first case in Bolivia, originated the transmission to other seven cases in two different departments of the country, as the patient travelled to Santa Cruz, Cochabamba, La Paz and Oruro (Fig. 1). Close contact with active cases of COVID-19 represents a significant risk for SARS-CoV-2 transmission, even during the asymptomatic or presymptomatic stage, especially for relatives or friends [19,[46], [47], [48], [49]].
None of the cases in this study required intensive care unit (ICU). The hospitalized case evolved good and was only hospitalized due to risk factors (age and hypertension) [[1], [2], [3], [4],6,16,50].
The clinical manifestations of these patients were according to the expected as reported in the literature [50], presenting mainly fever, and cough, among other symptoms. Ten of the twelve cases were younger than 60 y-old, and with no risk factors, except in two cases with hypertension and a history of community-acquired pneumonia. Then, the clinical evolution was favorable with no complications and no deaths among these patients. Early healthcare with appropriate training of healthcare works would be critical to keeping mostly this in a similar trend for future cases in the country that is now taken severe actions, such as home isolation and quarantine [[51], [52], [53], [54]], primarily to protect those with risk factors. According to the National Institute of Statistics of Bolivia, for 2019, there were 11,513,101 inhabitants. From them, 10.19% corresponded to people older than 60 years-old [55]. For some risk factors, such as diabetes mellitus, Bolivia is amongst the country with the lowest prevalence, around 6.6% in 2016 [56]. However, is estimated that a third of the Bolivian population presents high blood pressure [57], which is considered among the most prevalent risk factors in patients with COVID-19, for worse clinical progression [50], then the case 2 in Santa Cruz, was hospitalized for close monitoring while having age and hypertension as risk factors.
Bolivia is a developing country with limited resources. In this scenario, the previous overlapping health events, such as dengue [27], chikungunya, Zika, hantavirus and even hemorrhagic fevers caused by arenaviruses [[58], [59], [60], [61]], as well as regular viral respiratory infections [[32], [33], [34]], may pose a challenge for diagnosis, and the healthcare together the ongoing COVID-19 outbreak.
There has been a rapid surge in research in response to the outbreak of COVID-19 [62]. During this early period, published research primarily explored the epidemiology [63], causes, clinical manifestation and diagnosis [64], as well as prevention and control of the novel coronavirus. Although these studies are relevant to control the current public emergency, more high-quality research is needed to provide valid and reliable ways to manage this kind of public health emergency in both the short- and long-term, including therapeutic options [[65], [66], [67], [68], [69], [70], [71]].
During the current phase of COVID-19 outbreak in Bolivia, only of imported cases, all of them are being tested by rRT-PCR. However, the question is if the spread occurs rapidly in the country, with community-transmission as is now observed in other countries in the continent [[72], [73], [74]], Bolivia, as well as other low- and middle-income countries in the region, e.g. Haiti, Venezuela [75], Nicaragua, among others, will not be able to afford large-scale diagnostics [24]. Therefore, in the absence of testing, triage based on clinical case definition or presumptive diagnosis should be prioritized. A proposal for surveillance at that point, if diagnostics are limited, is to develop a definition of a clinical confirmed case. As occurred with chikungunya, and Zika, in most countries in Latin America, this would be “a patient with fever, cough and other respiratory symptoms, not explained by other etiological agents or causes, that is diagnosed in a municipality where at least a laboratory-confirmed case was identified” [[76], [77], [78]].
The number of patients that may require ventilatory support and attention at an intensive care unit (ICU) may collapse the health system of larger countries. In the case of Bolivia, there are only 35 ICU beds. Then, as expected, the health authorities are working on the general beds that can be rapidly converted to ICU beds and some general hospitals to be converted into critical care hospitals. Additional physicians and nurses are now widely trained in critical care medicine and specifically on COVID-19 in order to answer the epidemic. A national telehealth program is running for multiple purposes, including training on COVID-19. Albeit that, it is debatable whether countries such as Bolivia can fund the additional cost of critical care units from our limited health budgets [24,27], that need to attend not only the epidemic of COVID-19 but also other non-communicable diseases as well as communicable diseases, such as dengue, diarrhoea, malaria, HIV, tuberculosis, among many other diseases [27,75].
Finally, in the absence of vaccines and specific treatments available and approved for COVID-19, the only available public health tools to control person-to-person transmittable diseases are isolation and quarantine, social distancing, and community containment measures, and this is now in place in Bolivia, as well as in most countries of Latin America [54,79]. There is an urgent need to train most of the healthcare workforce on biosecurity, isolation, and quarantine, in order to be massively applied in the country. If these measures are implemented soon, more possibilities to control spreading will have the countries, which is even critical in countries, such as Bolivia, with limited resources.
In conclusion, while the global awareness and response to the COVID-19 pandemic are well known, each country faces its considerations and scenarios to face the epidemic in their territories. In the case of Bolivia, the less developed nation of South America, national and international cooperation, advise and support, lead to enhance surveillance and early case detection of COVID-19, scaling up the training activities at the healthcare sector and the community for proper education as well as quarantine. In this report, the first 12 confirmed cases were analyzed, showing that most of the evolve positively with no severe disease nor fatalities. Nevertheless, preparedness for a significant epidemic, as is going on in other countries, and the deployment of response plans for it, in the country is now taking place to mitigate the impact of the COVID-19 pandemic in the population.
Preparedness in South America should include the increase in the diagnostic capacity for rapid testing for the virus, including not only imported but also secondary and tertiary cases. It is important to avoid the delay from identification of suspected cases to their confirmation and isolation, in order to affect the possible disease transmission [25]. Also, there is a need for improvement of the volume of personnel trained to run such tests, and to warrant an adequate stock of materials needed to do them. Health authorities should train, equip, and strengthen the diagnostic capacities of hospital laboratories close to infectious disease and emergency departments to reduce the time to deliver results, manage confirmed cases and contacts more rapidly, and preserve strict infection control measures [25]. Finally, in the differential diagnosis with other febrile conditions, especially in Latin America, also coinfections with dengue [75] and with respiratory viruses, such as Influenza and Metapneumovirus [[80], [81], [82]], among others, already reported together with SARS-CoV-2, should be considered.
5. Limitations
The main limitation of our study is the lack of long follow up of the patients, but this analysis is a rapid preliminary study for the outbreak assessment in Bolivia, focused on epidemiological and clinical aspects. Secondly, still, there are no available serological tests to assess the antibody response. Third, due to constraining in the use of the rRT-PCR, only initial testing was provided, although after ceased of symptoms, for the case hospitalized, it will be repeated to assess if became negative. More comprehensive contact tracing for these cases should be performed to assess the possibility of community transmission. Finally, soon, Bolivia will also need to have sequencing and phylogenetic studies that would be useful as this may diverge from other SARS-CoV-2 isolates or strain, that even, would be related to clinical evolution and outcomes.
Funding source
Universidad Franz Tamayo, Cochabamba, Bolivia. Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Study sponsors had no role in the study design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Ethical approval
Approval was not required.
CRediT authorship contribution statement
Juan Pablo Escalera-Antezana: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing - review & editing. Nicolas Freddy Lizon-Ferrufino: Data curation, Formal analysis, Writing - review & editing. Americo Maldonado-Alanoca: Data curation, Formal analysis, Writing - review & editing. Gricel Alarcón-De-la-Vega: Data curation, Formal analysis, Writing - review & editing. Lucia Elena Alvarado-Arnez: Data curation, Formal analysis, Writing - review & editing. María Alejandra Balderrama-Saavedra: Data curation, Formal analysis, Writing - review & editing. D. Katterine Bonilla-Aldana: Data curation, Formal analysis, Writing - review & editing. Alfonso J. Rodríguez-Morales: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing - original draft, Writing - review & editing.
Declaration of competing interest
All authors report no potential conflicts.
Acknowledgements
To the Epidemiology Department of the Ministry of Health of Bolivia for providing additional data of the patients. To CENETROP for rRT-PCR results.
References
- 1.Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020; 382(13):1199-1207 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 6.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonilla-Aldana D.K., Dhama K., Rodriguez-Morales A.J. Revisiting the one health approach in the context of COVID-19: a look into the ecology of this emerging disease. Adv Anim Vet Sci. 2020;8:234–237. [Google Scholar]
- 8.Rodriguez-Morales A.J., Bonilla-Aldana D.K., Balbin-Ramon G.J., Paniz-Mondolfi A., Rabaan A., Sah R. History is repeating itself, a probable zoonotic spillover as a cause of an epidemic: the case of 2019 novel Coronavirus. Inf Med. 2020;28:3–5. [PubMed] [Google Scholar]
- 9.Li X., Zai J., Zhao Q., Nie Q., Li Y., Foley B.T. Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2. J Med Virol. 2020 doi: 10.1002/jmv.25731. 10.1002/jmv.25731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bastola A., Sah R., Rodriguez-Morales A.J., Lal B.K., Jha R., Ojha H.C. The first 2019 novel coronavirus case in Nepal. Lancet Infect Dis. 2020;20:279–280. doi: 10.1016/S1473-3099(20)30067-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yan G., Lee C.K., Lam L.T.M., Yan B., Chua Y.X., Lim A.Y.N. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang X., Yu Y., Xu J., Shu H., Xia Ja, Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phan L.T., Nguyen T.V., Luong Q.C., Nguyen T.V., Nguyen H.T., Le H.Q. Importation and human-to-human transmission of a novel coronavirus in vietnam. N Engl J Med. 2020 doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsang K.W., Ho P.L., Ooi G.C., Yee W.K., Wang T., Chan-Yeung M. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 15.COVID-19 National Incident Room Surveillance Team . 2020. COVID-19, Australia: epidemiology report 2. [Google Scholar]
- 16.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020; 382(10):929-936 doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silverstein W.K., Stroud L., Cleghorn G.E., Leis J.A. First imported case of 2019 novel coronavirus in Canada, presenting as mild pneumonia. Lancet. 2020;395(10225):734. doi: 10.1016/S0140-6736(20)30370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ECDC . 2020. ECDC statement following reported confirmed case of 2019-nCoV in Germany.https://www.ecdc.europa.eu/en/news-events/ecdc-statement-following-reported-confirmed-case-2019-ncov-germany [Google Scholar]
- 19.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020 doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Day M. Covid-19: surge in cases in Italy and South Korea makes pandemic look more likely. BMJ. 2020;368:m751. doi: 10.1136/bmj.m751. [DOI] [PubMed] [Google Scholar]
- 21.Porcheddu R., Serra C., Kelvin D., Kelvin N., Rubino S. Similarity in case fatality rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020;14:125–128. doi: 10.3855/jidc.12600. [DOI] [PubMed] [Google Scholar]
- 22.Giovanetti M., Benvenuto D., Angeletti S., Ciccozzi M. The first two cases of 2019-nCoV in Italy: where they come from? J Med Virol. 2020; 92(5):518-521 doi: 10.1002/jmv.25699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kapata N., Ihekweazu C., Ntoumi F., Raji T., Chanda-Kapata P., Mwaba P. Is Africa prepared for tackling the COVID-19 (SARS-CoV-2) epidemic. Lessons from past outbreaks, ongoing pan-African public health efforts, and implications for the future. Int J Infect Dis. 2020;93:233–236. doi: 10.1016/j.ijid.2020.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.4169 doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 25.Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boelle P.Y. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adepoju P. Nigeria responds to COVID-19; first case detected in sub-Saharan Africa. Nat Med. 2020 doi: 10.1038/d41591-020-00004-2. 10.1038/d41591-020-00004-2. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P., Mendez C.A., Zambrano L.I., Franco-Paredes C. COVID-19 in Latin America: the implications of the first confirmed case in Brazil. Trav Med Infect Dis. 2020:101613. doi: 10.1016/j.tmaid.2020.101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.da Cunha C.A., Cimerman S., Weissmann L., Chebabo A., Bellei N.C.J. Sociedade Brasileira de Infectologia; Sao Paulo, Brasil: 2020. Informativo da Sociedade Brasileira de Infectologia: primeiro caso confirmado de doença pelo novo Coronavírus (COVID-19) no Brasil – 26/02/2020. [Google Scholar]
- 29.Sao Paulo State Health Secretary . 2020. Plan of response of the sao Paulo state for the human infection due to novel coronavirus - 2019nCoV. [Google Scholar]
- 30.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zambrano L.I., Fuentes-Barahona I.C., Bejarano-Torres D.A., Bustillo C., Gonzales G., Vallecillo-Chinchilla G. A pregnant woman with COVID-19 in Central America. Trav Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101639. 101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chavez D., Gonzales-Armayo V., Mendoza E., Palekar R., Rivera R., Rodriguez A. Estimation of influenza and respiratory syncytial virus hospitalizations using sentinel surveillance data-La Paz, Bolivia. Influenza Other Respir Viruses. 2019;13:477–483. doi: 10.1111/irv.12663. 2012-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Delangue J., Roca Sanchez Y., Piorkowski G., Bessaud M., Baronti C., Thirion-Perrier L. Viral aetiology influenza like illnesses in Santa Cruz, Bolivia (2010-2012) Virol J. 2014;11:35. doi: 10.1186/1743-422X-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mamani O.Y., Salazar E.R.… . 2015. Perfil epidemiológico de la Influenza Humana A H1N1 en Cochabamba, Bolivia, gestiones 2009 a 2014: scielo.org.bo. [Google Scholar]
- 35.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K.W. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020:25. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization . 2020. Novel coronavirus (2019-nCoV) - situation report - 4 - 24 january 2020.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200124-sitrep-4-2019-ncov.pdf?sfvrsn=9272d086_2 [Google Scholar]
- 37.World Health Organization . 2020. Statement on the meeting of the international health regulations (2005) emergency committee regarding the outbreak of novel coronavirus (2019-nCoV)https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov [Google Scholar]
- 38.World Health Organization . 2020. Novel coronavirus (2019-nCoV) - situation report - 7 - 27 january 2020.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200127-sitrep-7-2019--ncov.pdf?sfvrsn=98ef79f5_2020 [Google Scholar]
- 39.World Health Organization . 2020. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov [Google Scholar]
- 40.Rodriguez-Morales A.J., MacGregor K., Kanagarajah S., Patel D., Schlagenhauf P. Going global - travel and the 2019 novel coronavirus. Trav Med Infect Dis. 2020;33:101578. doi: 10.1016/j.tmaid.2020.101578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Millan-Oñate J., Rodríguez-Morales A.J., Camacho-Moreno G., Mendoza-Ramírez H., Rodríguez-Sabogal I.A., Álvarez-Moreno C. A new emerging zoonotic virus of concern: the 2019 novel Coronavirus (COVID-19) Infectio. 2020:24. [Google Scholar]
- 42.Rodriguez-Morales A.J., Sánchez-Duque J.A., Hernández-Botero S., Pérez-Díaz C.E., Villamil-Gómez W.E., Méndez C.A. Preparación y control de la enfermedad por coronavirus 2019 (COVID-19) en América Latina. Acta Méd Peru. 2020;37:3–7. [Google Scholar]
- 43.Cai J., Sun W., Huang J., Gamber M., Wu J., He G. Indirect virus transmission in cluster of COVID-19 cases, wenzhou, China, 2020. Emerg Infect Dis. 2020:26. doi: 10.3201/eid2606.200412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ji L.N., Chao S., Wang Y.J., Li X.J., Mu X.D., Lin M.G. Clinical features of pediatric patients with COVID-19: a report of two family cluster cases. World J Pediatr. 2020 doi: 10.1007/s12519-020-00356-2. 10.1007/s12519-020-00356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li P., Fu J.B., Li K.F., Chen Y., Wang H.L., Liu L.J. Transmission of COVID-19 in the terminal stage of incubation period: a familial cluster. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.027 doi: 10.1016/j.ijid.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu S., Lin J., Zhang Z., Xiao L., Jiang Z., Chen J. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. 10.1002/jmv.25776. [DOI] [PubMed] [Google Scholar]
- 47.Al Hammadi Z.M., Chu D.K., Eltahir Y.M., Al Hosani F., Al Mulla M., Tarnini W. Asymptomatic MERS-CoV infection in humans possibly linked to infected dromedaries imported from Oman to United Arab Emirates. Emerg Infect Dis. 2015;21:2197–2200. doi: 10.3201/eid2112.151132. May 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Al-Tawfiq J.A., Gautret P. Asymptomatic Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: extent and implications for infection control: a systematic review. Trav Med Infect Dis. 2019;27:27–32. doi: 10.1016/j.tmaid.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu Z., Song C., Xu C., Jin G., Chen Y., Xu X. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020 doi: 10.1007/s11427-020-1661-4. 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Trav Med Infect Dis. 2020:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cetron M., Landwirth J. Public health and ethical considerations in planning for quarantine. Yale J Biol Med. 2005;78:329–334. [PMC free article] [PubMed] [Google Scholar]
- 52.Khan S., Siddique R., Ali A., Xue M., Nabi G. Novel coronavirus, poor quarantine, and the risk of pandemic. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.02.002 doi: 10.1016/j.jhin.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lombardi A., Bozzi G., Mangioni D., Muscatello A., Peri A.M., Taramasso L. Duration of quarantine in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a question needing an answer. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.03.003 doi: 10.1016/j.jhin.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.INstituto Nacional de Estadística 2020. https://www.ine.gob.bo/
- 56.OPS Bolivia . 2016. Bolivia está entre los países con menor prevalencia de diabetes de las Américas.https://www.paho.org/bol/index.php?option=com_content&view=article&id=1853:dms20162&Itemid=481 [Google Scholar]
- 57.Naciones unidas Bolivia. 2020. http://www.nu.org.bo/noticias/uno-de-cada-tres-adultos-en-bolivia-tiene-hipertension/ [Google Scholar]
- 58.Escalera-Antezana J.P., Murillo-Garcia D.R., Gomez C., Unzueta-Quiroga R.C., Rodriguez-Morales A.J. Chikungunya in Bolivia: domestic imported case series in Cochabamba. J Formos Med Assoc. 2018;117:1133–1134. doi: 10.1016/j.jfma.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 59.Escalera-Antezana J.P., Murillo-Garcia D.R., Rodriguez-Morales A.J. Chikungunya in Bolivia: still a neglected disease? Arch Med Res. 2018;49:288. doi: 10.1016/j.arcmed.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 60.Escalera-Antezana J.P., Rodriguez-Villena O.J., Arancibia-Alba A.W., Alvarado-Arnez L.E., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Clinical features of fatal cases of Chapare virus hemorrhagic fever originating from rural La Paz, Bolivia, 2019: a cluster analysis. Trav Med Infect Dis. 2020:101589. doi: 10.1016/j.tmaid.2020.101589. [DOI] [PubMed] [Google Scholar]
- 61.Escalera-Antezana J.P., Torrez-Fernandez R., Montalvan-Plata D., Montenegro-Narvaez C.M., Aviles-Sarmiento J.L., Alvarado-Arnez L.E. Orthohantavirus pulmonary syndrome in Santa Cruz and tarija, Bolivia, 2018. Int J Infect Dis. 2020;90:145–150. doi: 10.1016/j.ijid.2019.10.021. [DOI] [PubMed] [Google Scholar]
- 62.Adhikari S.P., Meng S., Wu Y.J., Mao Y.P., Ye R.X., Wang Q.Z. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bonilla-Aldana D.K., Holguin-Rivera Y., Cortes-Bonilla I., Cardona-Trujillo M.C., García-Barco A., Bedoya-Arias H.A. Coronavirus infections reported by ProMED, february 2000–january 2020. Trav Med Infect Dis. 2020:101575. doi: 10.1016/j.tmaid.2020.101575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bonilla-Aldana D.K., Quintero-Rada K., Montoya-Posada J.P., Ramirez S., Paniz-Mondolfi A., Rabaan A. SARS-CoV, MERS-CoV and now the 2019-novel CoV: have we investigated enough about coronaviruses? - a bibliometric analysis. Trav Med Infect Dis. 2020:101566. doi: 10.1016/j.tmaid.2020.101566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020; 30(3):269-271 doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Colson P., Rolain J.M., Lagier J.C., Brouqui P., Raoult D. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents. 2020:105932. doi: 10.1016/j.ijantimicag.2020.105932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cortegiani A., Ingoglia G., Ippolito M., Giarratano A., Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020 doi: 10.1016/j.jcrc.2020.03.005 doi: 10.1016/j.jcrc.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Devaux C.A., Rolain J.M., Colson P., Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020:105938. doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gao J., Tian Z., Breakthrough Yang X. Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. 2020;14:72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 70.Sahraei Z., Shabani M., Shokouhi S., Saffaei A. Aminoquinolines against coronavirus disease 2019 (COVID-19): chloroquine or hydroxychloroquine. Int J Antimicrob Agents. 2020:105945. doi: 10.1016/j.ijantimicag.2020.105945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Touret F., de Lamballerie X. Of chloroquine and COVID-19. Antivir Res. 2020;177:104762. doi: 10.1016/j.antiviral.2020.104762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cowling B.J., Aiello A. Public health measures to slow community spread of COVID-19. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa123 doi: 10.1093/infdis/jiaa123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kwon K.T., Ko J.H., Shin H., Sung M., Kim J.Y. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Kor Med Sci. 2020;35:e123. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu J., Liao X., Qian S., Yuan J., Wang F., Liu Y. Community transmission of severe acute respiratory syndrome coronavirus 2, shenzhen, China, 2020. Emerg Infect Dis. 2020:26. doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rodriguez-Morales A.J., Suarez J.A., Risquez A., Delgado-Noguera L., Paniz-Mondolfi A. The current syndemic in Venezuela: measles, malaria and more co-infections coupled with a breakdown of social and healthcare infrastructure. Quo vadis? Trav Med Infect Dis. 2019;27:5–8. doi: 10.1016/j.tmaid.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 76.Rodriguez-Morales A.J., Bonilla-Aldana D.K., Bonilla-Aldana J.C., Mondragon-Cardona A. Chikungunya and Zika in huila: mapping their incidence in a neglected area of Colombia. Arch Med Res. 2018;49:512–513. doi: 10.1016/j.arcmed.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 77.Rodriguez-Morales A.J., Galindo-Marquez M.L., Garcia-Loaiza C.J., Sabogal-Roman J.A., Marin-Loaiza S., Ayala A.F. Mapping Zika virus disease incidence in Valle del Cauca. Infection. 2017;45:93–102. doi: 10.1007/s15010-016-0948-1. [DOI] [PubMed] [Google Scholar]
- 78.Rodriguez-Morales A.J., Ruiz P., Tabares J., Ossa C.A., Yepes-Echeverry M.C., Ramirez-Jaramillo V. Mapping the ecoepidemiology of Zika virus infection in urban and rural areas of Pereira, Risaralda, Colombia, 2015-2016: implications for public health and travel medicine. Trav Med Infect Dis. 2017;18:57–66. doi: 10.1016/j.tmaid.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 79.Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30129-8. 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ding Q., Lu P., Fan Y., Xia Y., Liu M. The clinical characteristics of pneumonia patients co-infected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020 doi: 10.1002/jmv.25781. 10.1002/jmv.25781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Touzard-Romo F., Tape C., Lonks J.R. Co-infection with SARS-CoV-2 and human Metapneumovirus. R I Med J. 2013;103:75–76. 2020. [PubMed] [Google Scholar]
- 82.Wu X., Cai Y., Huang X., Yu X., Zhao L., Wang F. Co-infection with SARS-CoV-2 and influenza A virus in patient with pneumonia, China. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2606.200299. [DOI] [PMC free article] [PubMed] [Google Scholar]