Abstract
Emergencies come at the most inopportune times. Some are totally unexpected, others come with short warnings. Although rare, an emergency comes with the potential to wreak disaster and pose serious risk to the services provided to hematopoietic cell transplant (HCT) patients. Yet, the consequences of an emergency can be mitigated by thinking the unthinkable and having a plan for emergency preparedness in place. Each HCT center should develop a plan containing steps of mitigation, preparedness, response and recovery. This report provides the framework for a HCT-specific emergency preparedness plan that can be used by individual centers to develop customized guidelines on preparing for, responding to, and recovering from an emergency.
Introduction
Hematopoietic cell transplant (HCT) centers are at risk for many kinds of emergencies – viral epidemic, hurricane, flood, tornado, power outage, earthquake, fire, bomb threat, etc. No center is immune. The Severe Acute Respiratory Syndrome (SARS) outbreak arose first in Asia, and then spread elsewhere to places such as Toronto. The University of Toronto’s HCT Program was forced to halt transplants for weeks and to make provisions for their patients elsewhere. In its aftermath, the American Society of Blood and Marrow Transplantation called for the formation of a committee to formulate a set of recommendations for centers to consider in their own plans for emergency preparedness.
Emergencies come in many forms and no two are exactly alike, but they generally can be placed into two categories: those that arrive with some kind of advance warning (epidemics, hurricanes, floods) and those that offer little or no warning (tornado, power outage, fire). This report addresses both kinds of emergencies, offering advice on how to prepare and things to consider. It concludes with several case histories demonstrating how the HCT community has prepared for and addressed emergencies and what they have learned.
Roadmap for Preparedness
Using a framework categorizing the various elements of emergency planning provided by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (1), the committee offers the following suggestions that each center should consider in preparing for an emergency (JCAHO). The intent of this is not to provide detailed specifics since each center has its own characteristics that include unique strengths and vulnerabilities. Moreover, each type of emergency will confront the center with distinct challenges. Rather, this document is intended to provide an outline of issues that should be considered in the center’s emergency preparedness plan.
Several elements should be contained in each center’s plan. These include steps of mitigation, preparedness, response and recovery (Figure 1).
Figure 1.
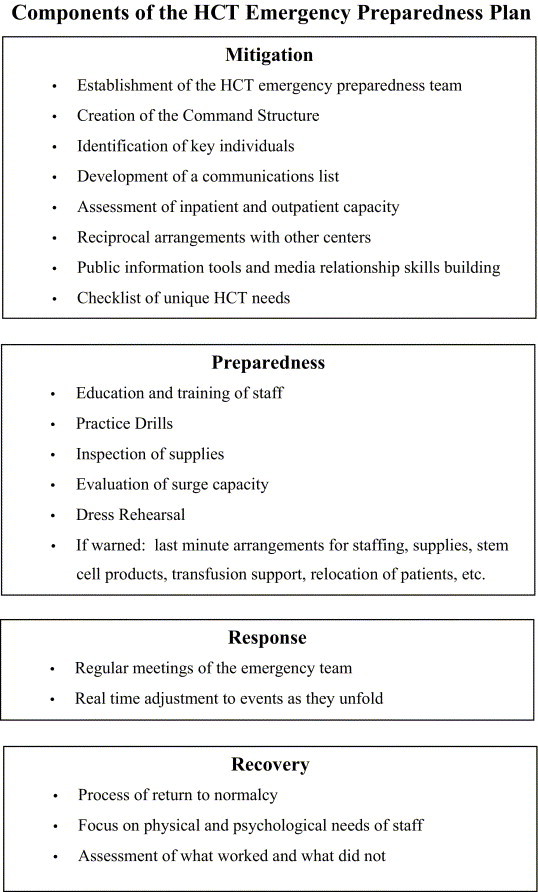
Components of the HCT Emergency Preparedness Plan.
Mitigation (The Advance Plan)
Mitigation steps include those efforts to assess how your center’s services would be affected by a potential disaster. Each hospital has a disaster plan. Such plans generally include steps to deal with internal hospital situations such as fire, loss of utilities, loss of services, or bomb threat, and external exigencies such as casualty management, severe weather, or a terrorist action involving use of weapons of mass destruction. While such plans offer important strategies to deal with events that pose threats to the entire hospital, it is unlikely that the hospital-wide plan contains specific plans related to unique HCT issues. Thus, a detailed plan to address specific HCT issues is also needed. The HCT plan should address the things that one can and should address now: emergency team, command structure, channels of communications, inpatient and outpatient capacity, reciprocal arrangements with other centers, public information, etc. Especially critical for the HCT program are arrangements for longitudinal outpatient care services, since HCT patients are especially reliant on intensive outpatient services over a long interval.
The HCT emergency plan should address the following topics: 1) the team in charge of HCT emergency preparedness, 2) a command structure and identification of key individuals, 3) means of communications between individual staff members, 4) inpatient and outpatient capacity and staffing, 5) reciprocal arrangements with other centers, 6) public Information tools and media relationship skills building, 7) backup of patient and stem cell database, and 8) a checklist of unique HCT needs.
-
1
Establishment of a HCT emergency team. A HCT emergency preparedness team should be developed (Figure 2). This team will develop the specifics of the plan, organize the entire staff, be charged with conducting drills, overseeing training, monitoring performance during an emergency response, and ensuring that recovery efforts take place. The team should include representatives of multiple key services to gain as many perspectives as possible about what are potential vulnerabilities and to identify as many solutions as possible.
-
2
A command structure and listing of individual personnel in key roles. The team should develop a command structure list that identifies who is in charge of what. Listing the team by job title, rather than by individual, will make the structure more permanent and less subject to changes in personnel.
-
3
Mechanism of communication. A list of individual staff members by job title should also be maintained in multiple locations since individual nodes of the communication network may be disrupted. Contact information for the staff should include multiple types of communication and should be maintained in multiple media forms. Examples of types of communication include pagers, land-based telephones, cellular phones, internet, and public media. Locations that this information should be placed include inpatient and outpatient nursing stations, stem cell laboratories, homes of key individuals, etc. Because this information will become outdated, a schedule for routine replacement, e.g., monthly or bi-monthly, should be implemented.
-
4
Inpatient and outpatient capacity. An assessment of one’s program’s capacity, how it might be affected by an emergency, and planning for “surge” capacity or provisions for reduced capacity is advisable. One’s center may face a shortage of inpatient or critical care beds due to either an influx of patients hospitalized from injuries or illness from the emergency event or an inability to discharge patients because of a lack of community services, housing or transportation. Similarly, outpatient and home care services may be severely affected resulting in a need to hospitalize outpatients. One consideration to weigh is whether there are any possibilities to temporarily increase capacity and what steps would be needed to make it happen. One should consider delay of new transplant procedures wherever possible to free up beds. Strong consideration should be given to relocation of patients whenever possible to communities not affected (see below). For patients needing intensive outpatient care that is disrupted by the emergency, one may consider admitting them early to ensure an inpatient bed.
-
5
Reciprocal arrangements with other centers. Development of a relationship with one or more neighboring “buddy” centers that may assist in assuming care of patients if one’s center cannot accommodate needed patient care may be useful; joint practices and communications testing between the two centers periodically is advisable. One should consider a relationship of one center in the same FEMA district and one in a different FEMA district. Consider establishing videoconfenercing facilities to maintain educational programs in the event that some centers will be quarantined.
-
6
Public Information tools and media relationship skills building. Learning some basic media relations skills is important. Knowing in advance the contact numbers of local radio and television stations that are good conduits of public information is important and may be used to communicate with staff (see below under Response). This is best done in conjunction with the public relations department of the hospital which is well placed to co-ordinate announcements from the hospital, especially its command center, as well as municipal, state and federal authorities so that a consistent message is conveyed.
-
7
Backup of patient and stem cell database. All hospital patient information systems have extensive backup precautions to prevent loss of patient data. The BMT program’s customized database of patient and stem cell information may be part of the hospital system or maintained separately. If the latter, it is important to have backup systems in place, preferably with a copy of the database off site.
-
8
Checklist of specific HCT needs. A checklist of specific HCT concerns should be created and maintained (Figure 3). For each concern, the center should develop specific local plans. Below are suggestions based on various committee members’ experiences of specific emergencies faced by their program.
-
•
Staff. Staffing shortages for both inpatient and outpatient services may occur. Shortages may arise from disruption of staff from getting to and from work or some may need to be excluded from patient care. This is most relevant for an infectious or radiation event where certain staff may have exposures that would be hazardous for patients. Pregnant women may need special provisions for either infectious or radiation events. Provision for staff support (child care, transportation, etc) may be necessary since some emergencies may result in school or childcare closures, affecting dependent children of staff members. Some centers have set up on-site temporary childcare for staff needed to provide essential services. Relief of on-duty staff should also be planned. One should ensure that multiple means of communication with individual staff members are maintained (as noted above) since disruption of one or more types of communication may occur. Setting up a list of volunteer staff in advance can be useful.
-
•
Stem cell products. Electricity may be disrupted in any number of emergencies. Generally, generator backup systems will quickly restore electricity. One should assess whether or not critical stem cell collection equipment and stem cell processing instruments have access to electrical outlets that are supplied by the backup electrical supply. If any key instruments are not, corrective action in advance or alternative planning will reduce the likelihood of a crucial process disruption. In the event of an anticipated disaster, facilities should consider ordering additional tanks of liquid nitrogen in order to have a back up supply.
Transportation of a stem cell product from collection site to transplant center may be disrupted and may jeopardize timely delivery (or collection) of stem cell products from other locales, especially of unrelated donor or cord blood products. Contact with the National Marrow Donor Program (NMDP) or other donor registry/bank to coordinate delivery is crucial. If there is advance warning, one may consider earlier collection and delivery. If the center is scheduled to provide stem cells for another center, as for example the NMDP, the coordinator should inform the NMDP that the center is not able to collect cells from an unrelated donor and ship.
Ability to conduct apheresis in patients or donors whose mobilization procedure has already begun may be affected. A donor or patient may be in the midst of mobilization when an emergency prevents timely collection of the product or the recipient may already have received an ablative conditioning regimen. Decisions as to aborting the collection or revision of the collection process may be needed.
-
•
Transfusion support. Supply of blood products for patients in need of transfusion support may be threatened. When a disaster strikes a community, volunteer activities such as blood donation may be seriously affected or disrupted. Changes in transfusion thresholds may be necessary. Close communication with one’s blood bank and regional blood collection center is crucial.
-
•
Infection control. Development of a close working relationship with the Infection Control Officer or team in one’s institution long in advance of an emergency is strongly encouraged. Infection control experts have much to teach transplant clinicians and likewise they have much to learn from transplant clinicians about the unique needs of HCT patients. Familiarity of the Infection Control team with specific HCT team’s concerns and practices will facilitate useful and constructive advice during an emergency. If the emergency is an infectious event, this relationship will have crucial meaning. Criteria for determining if certain staff should be excluded need to be developed with the coordination with Infection Control. An assessment of the availability of at least some easily accessible negative pressure rooms available to assess outpatients - really critical for BMT patients is important, especially in the event of an infectious event.
-
•
Relocation of patients. It may be necessary to consider the possibility of relocating patients away from the HCT center and dispersing them to local health care providers in communities not affected by disaster. If the center finds that it cannot provide key services, has a reduced capacity, or the public services outside of the center are compromised, then return of some (or most) patients to health providers in communities not affected may be the most prudent course of action. Whenever possible, this should be anticipated if there is advance warning, and, if not, done as early as possible once the need becomes apparent. This can alleviate pressure on overburdened staff and facilities and optimizes delivery of needed services to patients who cannot be relocated. If relocation is done, one should remember that arrangements for blood transfusion support is key, with appropriate communication as to provisions for irradiation and CMV appropriate products (or filtration alternatively).
-
•
Public services. Interruption of public services, such as transportation, potable water, sanitation, electricity, and other public services may have an enormous impact on one’s ability to provide clinical services even if the center’s internal operations are not affected. Interruption of public services will affect both patients and staff. If roads are blocked or public transportation disrupted, patients and staff may not be able to get to and from the center. This may lead to certain staff working overtime or the need to curtail services, especially outpatient clinics. Lack of basic services (or transportation) may make it impossible to discharge patients who could be ordinarily discharged. Flooding or structural damage to housing may lead to lack of residential facilities for patients who are temporary residents in the transplant center’s community.
Figure 2.
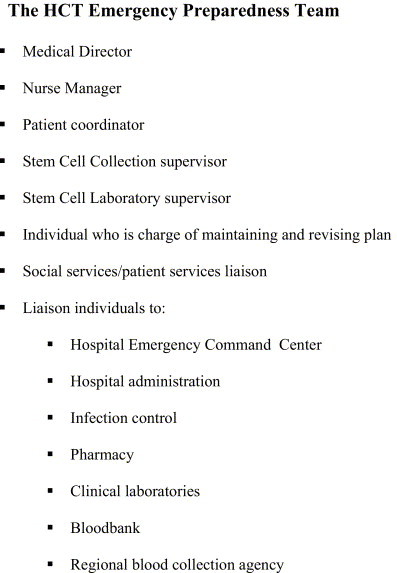
The HCT Emergency Preparedness Team
Figure 3.
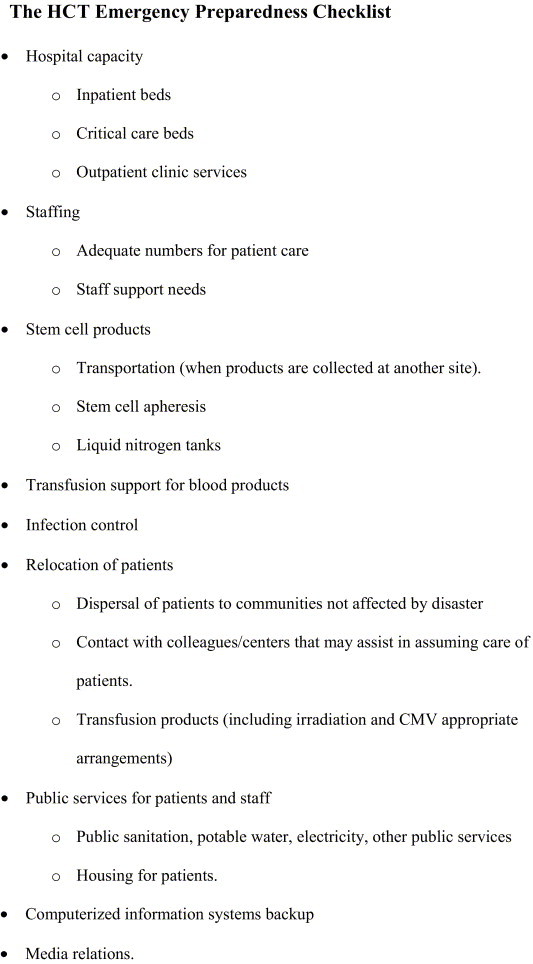
The HCT Emergency Preparedness Checklist
Preparedness (The People and their Training)
A recent study released by the Institute for Crisis Management (2) indicates that only one-fourth of business crises are wholly unexpected. Portending signs or warnings often are unheeded. Events that are of low probability (but with enormous potential for disaster) are disregarded. Instead of preparing for them, they are dismissed. Events such as Hurricane Katrina demonstrate the folly of such lack of preparation.
There are two principles. First, it is never too early to begin preparedness. Second, the most important resource one has to get one’s program through the emergency is one’s staff. Education and training of the staff is key. All of the staff will be called upon to deal with various concerns that arise. These include pharmacy, social services, laboratory staff, transportation services, etc.
Although the natural tendency is to plan for specific events, e.g., Here’s what we do for a flood. Here’s what we do for a terrorist attack. Here’s what we do for a terrorist attack during a flood… with and without electrical disruption. This type of planning quickly gets totally impractical and overwhelming. Instead, the emphasis should be to have a general plan that works for all possible disasters. (This can be fairly simple - collect information, convene the team, get the tickler list, start talking, make assignments [including collecting more information], decide on next meeting time, get started with implementation). Once the plan is in place, you can add some event-specific details, like in Florida or Gulf coast, add the hurricane. In Oklahoma, add the tornado, etc. Some planning for specific types of emergencies one’s center is most likely to face is advisable. For infectious event emergencies, minimizing the risk for spread of the infection is of highest priority. Brainstorming ways to compensate for possible disruption of public services and a discussion of how the staff can help each other may be useful.
Periodic review of the plan by the emergency preparedness team is important. Specific kinds of emergencies may be more likely than others and customized plans for such events are prudent. The conduct of periodic practice drills is crucial.
For an event in which some warning is present, several measures may be useful:
-
•
Preparation and updating of lists of part-time or retired staff or staff willing to work extra may be quite useful.
-
•
Careful consideration for removal of patients to other communities not expected to be affected.
-
•
Review of the hospital emergency preparedness plan (to understand how patients’ needs will fit into the larger context of what the hospital’s capacity is and to identify administrative authorities one should consult when help is needed).
-
•
Determine if surge capacity of inpatient beds or outpatient clinic capacity can be boosted.
-
•
Review equipment and food supplies and bring in extra supplies or equipment if needed.
-
•
Determine if extra supplies or preparations are needed for the specific emergency one faces or is likely to face. For example, in emergencies involving an infectious agent, ensuring adequate supplies of protective wear and equipment and setting aside additional isolation rooms may be possible. For a high wind or water emergency, movement of patients away from windows or areas prone to flooding would be prudent.
Response
Once an emergency occurs, one must manage its consequences. This may include triage of patients who need inpatient or outpatient services, institution of isolation procedures, clinical management of patients as medical issues arise, or abatement of infection spread between patients and among staff. The team should aim to be flexible, ready to improvise, and to adjust its actions if they are not working as anticipated. It is important to remember that even events that had been anticipated by the plan may unfold differently and unforeseen developments may occur and improvisation may be crucial for success.
The emergency team should meet on a regular basis throughout the response period and into the recovery phase. Each time the team meets, they should consider methodically, “What’s happening today?”, “What will happen tomorrow and within the next few days?” and, importantly, “What will happen when this is all over?” In some instances it is appropriate to subdivide the team and assign specific responsibilities. Depending upon the magnitude of the event, individuals may need to have their energies, which may be limited, focused upon manageable tasks. Because of the importance of the HCT program within the institution, a representative of the HCT emergency team should be a member of the institutional command center committee, thereby ensuring two-way communication – a critical component for effective action during a potentially very confusing time.
Addressing the media may become important and can represent a useful means of communication with patients and staff, serving as an early warning system to notify patients of clinic closures, sharing information among staff in the event of failure of other means of communication, providing local expertise to educate the public, and dispelling needless fears. Important to remember is that how you deliver your message is as important as the content of your message; one should aim to emphasize compassion for victims of the emergency, demonstrate that your team is in charge and indicate what steps are being taken to address the situation (3). Coordination with one’s hospital public relations staff is essential.
Recovery
After the acute crisis abates, then measures must be taken to return the service back to normal activities. The team should meet to determine when and how to phase in functions that had been placed on hold, dependent on availability of staff, capacity, supplies, etc. Timing is key and should be coordinated with hospital administrative staff.
An important issue to remember is the emotional toll on the staff of handling the emergency (as well as the impact of the emergency on the staff’s families). Similarly, there may also be physical exhaustion from extra work shifts worked. Special efforts are necessary to address both collective and individual staff concerns.
The team should conduct an assessment of what worked, what did not work and what occurred that was unanticipated. The plan should be carefully reviewed and revisions should be made as needed for future emergencies.
Case Histories
Severe Acute Respiratory Syndrome (SARS)
The SARS epidemic, starting in March 2003, caught Toronto, and indeed, Canada unprepared. By the time it was contained in Toronto it had involved more than 250 probable cases, resulted in 43 deaths and cost an estimated one billion dollars. A striking aspect to the healthcare workers directly involved at the onset of the epidemic was the uncertainty surrounding the mode of transmission of the disease, its surveillance, containment and management. While initially this led to some confusion, healthcare workers experienced a rather steep learning curve as the epidemic progressed and more information about the nature of the infective organism became known and available. In retrospect, several issues emerge as important to the management of a HCT Program during this period. One was surveillance at the hospital entrance of patients with clinic appointments. Requirements of surveillance included obtaining a history of contact with possible or probable cases, a history of symptoms, including fever, and a tympanic temperature measurement. The challenge was to distinguish possible symptoms of SARS from the expected symptoms and signs in the many patients with febrile neutropenia visiting the clinic. Some of these patients required further evaluation, and because they were initially to be regarded as possible cases of SARS, physical examination needed to be conducted in a negative pressure room. This was a particular challenge for those medical facilities that lacked adequate numbers of (or indeed, any) negative pressure rooms. Moreover, patient (and staff- separate entrance) surveillance invariably resulted in queuing at hospital entrances at peak times which was uncomfortable to those waiting outside in the cold. The lessons here include the need for an adequate number of negative pressure rooms in the out-patient clinic setting and the importance of regular information sessions to medical staff regarding the outbreak so that they can interact effectively with patients (and their co-workers).
One approach in containing the outbreak was to quarantine healthcare workers to their home because they exhibited fever and/or respiratory symptoms (in most cases an innocuous URI) and had no likely contact or individuals who had contact with possible cases of SARS. These individuals were monitored regularly by public health personnel. Either way they were no longer available as healthcare workers resulting in reduced staffing in medical units, including HCT programs. The lesson here is that transplant volume needs to be adjusted nimbly to accommodate the considerable reductions in healthcare staff that can occur quickly.
Another, perhaps unexpected issue was the initial shortage of N95 masks for healthcare workers and the need to have them fit-tested. A number of cases of SARS arose in healthcare workers who were inadequately protected. The lesson here is that it is vital to show strong support to front-line staff at risk of exposure. It was particularly important to protect staff in regular contact with immunocompromised patients not only for their own sake but to ensure the safety of the transplant unit.
Another important issue arose from decisions by government agencies regarding restrictions on the transfer of patients from one institution to another. For institutions performing HCT that lacked their own intensive care units, this posed a major logistical issue in planning transplants. In some cases, they were postponed because of the lack of availability of acute care services or were transferred to other institutions if this was permitted by government directives. The lesson from this experience is that input from transplant directors is important when planning is done and should be integrated at all levels of decision-making.
Another, and perhaps minor issue when viewed in the context of a serious event such as SARS, is that clinical research came to a virtual standstill during this period. Moreover, the often touted virtue of closer interaction between clinician researchers and basic scientists (extending to the location of scientists within hospitals) served to work against both, but especially the latter, when directives requested “non-essential” staff to not enter the hospital. Nonetheless, much is to be gained by the physical location of basic with clinical investigators in medical centers and the lack of productivity during periods of crisis is probably a small price to pay.
Terrorist attack (Sept 11)
Within a span of a few hours on September 11, 2001, all commercial air traffic in the United States was halted. Three National Marrow Donor Program (NMDP) collections were underway when their couriers’ flights were cancelled. Two more NMDP couriers were already en route on international flights that were ordered to return to Europe. But these were merely the collections in progress on September 11; more than 35 additional collections were already planned to occur over the next seven days. Most of the intended recipients had already begun conditioning therapy.
The NMDP was pushed into emergency management. Many questions had to be posed and addressed over the next few hours and days. Among them: How many collections could be postponed? Which planned transplants were non-myeloablative? How likely was ground transport? Could some products be frozen for a few days? Surely someone would be able to fly urgent products, but who? The military? Private corporations? Private couriers? The questions arose as quickly as the shock surrounding the magnitude of the disaster.
What happened over the next several days was, in short, a little bit of everything. The NMDP emergency management team met twice daily to receive updates and address issues. Innumerable inquiries were made to transplant centers, donor centers, collection facilities, potential air carriers, and couriers. International colleagues without hesitation subjected the collected products to cryopreservation and offered to freeze others as needed. Several transplants and collections were rescheduled. Multiple products were driven within and between states, including a marathon relay trip from Ohio to Texas. The NMDP investigated several air transportation options, but in the end chartered several flights from commercial medical carriers, including a roundtrip to Europe to deliver one product and retrieve stranded couriers with their frozen products.
In the end, an additional critical effort was planning for the aftermath. NMDP needed to anticipate the new screening for air travelers, including fears of couriers and the inevitable insistence upon x-ray inspection of products. The NMDP needed to anticipate the surge of activities that would follow the post-911 decline. The NMDP needed to formalize the emergency responses that we had made so that we could learn from this disaster and prepare for the next.
A stormy day in Gainesville
The clouds replaced the sunny skies one week in August, 2004. The wind grew. The hurricane approached Gainesville’s direction, but the projected path looked like “the city” would be only minimally affected. The BMT leadership team met, laid out plans, and felt confident that they were prepared. Or, so they thought. Call schedules had been reinforced. A plan for clinic closure had been put in force. The storm’s path veered in Gainesville’s direction. As the winds grew and the rain whipped the community, residents bunkered down.
After the winds and rains passed, the BMT team assessed the damage. Fortunately, the hospital remained physically intact and fully functional. A beleaguered staff persevered and all services during that frightful 48 hours were rendered successfully. However, the effect on the community outside was quite different. The treasured tree canopy that cooled the city in the summer now was strewn all around, crushing homes, knocking down power lines, and blocking roads. Electricity was out for two-thirds of homes, potable water was unavailable for many, sanitation systems became non-functional and dumped sewage into rivers and streams. Flooding from 15 inches of rain covered many neighborhoods, making many homes uninhabitable and roads impassable.
The lingering aftereffects were worse. For most of a week residents and staff spent digging out and putting their lives back together. Staff could not get to work due to flooded or impassable roads. Those that could get to work had to bring their children because schools were now evacuation centers. The BMT team set up childcare in part of the BMT clinic. It was a struggle relieving the fatigued staff at work all week long. The team quickly ran out of inpatient beds. Patients could not be discharged since they had no place to go to; the staff was unable to admit neutropenic patients to treat infections since not only were the HCT unit’s beds filled, the entire hospital was at capacity; there were no home care agencies to help out. Blood supplies ran low initially, but recovered quickly.
The team staggered through the recovery period. Gradually the team resumed more and more services. Within two weeks the service had returned to its usual operations.
Several weeks later another hurricane headed in the direction of Gainesville. The HCT leadership team met again to prepare again. This time, the team was smarter. In advance, the team began dispersing patients back to their communities not in the path of the storm. Stem cell collections were cancelled. Transplant admissions were cancelled. The team emptied as many beds as possible. Those receiving intensive outpatient care were admitted, if they could not return to another community out of the storm’s path. The storm veered away from Gainesville at the last minute and the center was unaffected. But, the team was convinced that had it kept on course it would have fared much better.
Conclusion
Catastrophic events such as terrorist attacks, tsunami, hurricane, regional blackouts, earthquakes, and SARS have reminded all of us of our vulnerabilities. We have all been witnesses to responses that have at times been gratifying and life-saving and yet at other times have seen responses that embarrassed us and seemed to magnify rather than alleviate suffering. Effective response and recovery begin with preparedness. Each HCT program should develop an emergency preparedness plan that accommodates local resources and addresses local vulnerabilities. Adequate preparedness has the potential to safeguard our efforts to alleviate suffering of our patients. [1, 2, 3]
References
- 1.Joint Commission on Accreditation of Healthcare Organization (JCAHO) Guide to Emergency Management Planning in Health Care, Joint Commission Resources. 2002. Oakbrook Terrace, IL. [Google Scholar]
- 2.Vol 14. The Institute for Crisis Management; 2005. (Annual ICM Crisis Report News Coverage of Business Crises During 2004). May, No 1. http://www.crisisexperts.com/04report.htm. [Google Scholar]
- 3.Leahigh A. Crisis Management: Getting It Right When “Things” Go Wrong. In: Heilbrunn J., editor. Marketing Encyclopedia: Issues and Trends Shaping the Future. NTC Business Books; Lincolnwood, IL: 2005. [Google Scholar]
Suggested readings
General
- 1.Auf der Heide E. Principles of hospital disaster planning. In: Hogan D.E., Burstein J.L., editors. Disaster Medicine. Lippincott Williams & Wilkins; Philadelphia: 2002. [Google Scholar]
- 2.The San Mateo County Health Services Agency, Emergency Medical Services . Hospital Emergency Incident Command System, 3rd edition. 3rd edition ed. 1998. San Mateo, CA. [Google Scholar]
- 3.Masci J.R., Bass E. Bioterrorism: A Guide for Hospital Preparedness. CRC Press; Boca Raton, FL: 2005. [Google Scholar]
- 4.“Disaster Preparedness Guide (chemical, biological, radiological),” prepared by the Navy Environmental Health Center. 2005. April. http://www-nehc.med.navy.mil. [Google Scholar]
- 5.“Hospital Disaster Readiness,” American Hospital Association, February 2002. http://www.hospitalconnect.com/aha/key_issues/disaster_rediness/content/MetroProceedings.pdf.
- 6.Mass Casualty Disaster Plan Checklist: A Template for Healthcare Facilities: http://www.gnyha.org.eprc.general.templates/ASPIC_MassCasualtychecklist.pdf.
- 7.Links to Every state’s Public Health Web Site: http://www.astho.org/index.php?template=regional_Links.php&PHPSESSID=244ef061bd98b568c923747be5a1c35a
- 8.Public Health Emergency Preparedness and Response: http://www.bt.cdc.gov
- 9.Hogan D.E., Lariet J. Triage. In: Hogan D.E., Burstein J.L., editors. Disaster Medicine. Lippincott Williams & Wilkins; Philadelphia: 2002. [Google Scholar]
- 10.Markenson D., Redlener I. Pediatric Preparedness for Disasters and Terrorism: A National Consensus Conference, executive summary of Mailman School of Public Health’s National Center for Disaster Preparedness consensus conference. 2003. [Google Scholar]
Infectious Event
- 1.Osterholm M.T. Preparing for the next pandemic. N Engl J Med. 2005;352(18):1839–1842. doi: 10.1056/NEJMp058068. [DOI] [PubMed] [Google Scholar]
- 2.Biological Weapons Defense . Infectious Diseases and Counterbioterism. Humana Press; Totowa, NJ: 2005. [Google Scholar]
- 3.Weinstein R.S., Alibek K. Biological and Chemical Terrorism: A Guide for Healthcare Providers and First Responders. 2003. New York. [Google Scholar]
- 4.Grow R.W., Rubinson L. The challenge of hospital infection control during a response to bioterrorist attacks, Biosecur and Bioterror. 2003. [DOI] [PubMed] [Google Scholar]
- 5.Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 6.Loutfy M.R., Wallington T., Rutledge T., Mederski B., Rose K., Kwolek S., McRitchie D., Ali A., Wolff B., White D., Glassman E., Ofner M., Low D.E., Berger L., McGeer A., Wong T., Baron D., Berall G. Hospital preparedness and SARS. Emerg Infect Dis. 2004;10(5):771–776. doi: 10.3201/eid1005.030717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.State of California Emergency Medical Services Authority, Hospital Bioterrorism Preparedness Program, 2003, Implementation Plan, accessed at EMSA website: http://www.emsa.cahwnet.gov/hbppc/hbppc_imp_plan2003.asp
Radiation Event
- 1.Radiation disasters and children. Pediatrics. 2003;111(6 Pt 1):1455–1466. [PubMed] [Google Scholar]


