Middle East respiratory syndrome (MERS), caused by the MERS coronavirus, has taken something of a back seat to Ebola among emerging diseases, but following the outbreak in South Korea earlier this year and a recent upsurge in cases in Saudi Arabia the disease is again in the limelight. 3 years after MERS was first reported, WHO has recorded 1517 confirmed cases worldwide with 539 deaths, a case fatality rate of 36%. Risk factors for infection include being aged at least 50 years and having an underlying medical condition such as diabetes. Yet gaps remain in our knowledge of the source, route of transmission, prevention, and treatment of MERS.
MERS cases have been recorded in 26 countries, but all can be traced back to the Middle East as the source of infection. Most cases—1223 with 520 deaths—have occurred in Saudi Arabia, with a case fatality rate of about 43%. At the time of writing (early September), Saudi Arabia is reporting new cases every day. South Korea contributes the next highest number of cases—186 with 36 fatal—with no new cases since July. The outbreak in South Korea began in May when a 68-year-old man returned to the country after a business trip to the Middle East. In the 9 days from developing symptoms to being diagnosed, the index patient attended several clinics and hospitals, which allowed the disease to spread to health-care workers, other patients, and visitors. Confirmed MERS cases occurred in hospitals or clinics in six cities in South Korea, thousands of schools were closed as a precaution, the number of tourists to the country fell, and there was a noticeable downturn in economic activity.
The South Korean outbreak was focused on health-care facilities, with some household transmission but no community spread. This experience echoes the situation elsewhere, and, indeed, the pattern of the related severe acute respiratory syndrome coronavirus outbreak in 2003. Infection prevention measures in health-care settings should include placing patients with suspected MERS in rooms separate from other patients with adequate ventilation, use of personal protective equipment, care by a specified group of skilled health-care workers, limiting visitors to patients, and, of course, rigorous hand hygiene. These precautions, and contact tracing and quarantine, were key to bringing the MERS outbreak in South Korea under control.
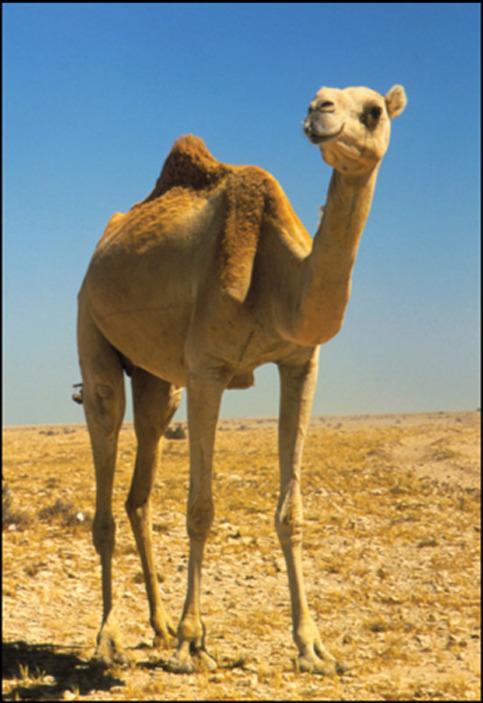
The epidemic curve of MERS follows a cycle of sharp peaks and troughs, which suggests repeated introduction of the causative virus into the human population from an external source followed by localised outbreaks. Indeed, dromedary camels—a common domestic animal in the Middle East—are undoubtedly the source of human MERS coronavirus infection. However, the virus seems to have been circulating in camels for decades, and people exposed to camels can be seropositive without symptoms, so why no human cases were detected before 2012 is unknown. Also, the specific route of—and risk-factors for—transmission from camels to people is not clearly understood. Development of a vaccine against MERS is still at the stage of animal experimentation, and there is no effective drug treatment for the disease.
An inability to control MERS outbreaks has prompted frequent changes of leadership at the Saudi Arabian Ministry of Health over the past 18 months. The Saudi Arabian government is responsible for the annual Hajj pilgrimage, which attracts millions of visitors and takes place Sept 21–26 this year. A MERS case has been reported in Medina, which, although not on the Hajj route, is visited by many pilgrims around the Hajj period. Although the Saudi Arabian government has advised against the very young, elderly, and people with chronic diseases visiting the country, there is still clearly the potential for export of MERS. A recent WHO report stated that “WHO expects that…cases will continue to be exported to other countries”. If export were to a country with a weak health infrastructure, a much larger outbreak than was seen in South Korea might occur.
A Lancet review cautioned that “health authorities, governments, and the research community should be prepared for the emergence of a MERS [coronavirus] with increased capacity for transmission and pandemic potential“. We support the WHO call for more research on how people become infected, identification of risk factors in health-care and occupational settings, and for enhanced surveillance for pneumonia. Given the situation in the Middle East, health-care facilities worldwide need to operate with a raised index of suspicion, and have in place policies for rapid screening and assessment of potential MERS cases.
For The Lancet Infectious Diseases Series on emerging respiratory tract infections see http://www.thelancet.com/series/emerging-respiratory-tract-infections
For WHO MERS summary see http://www.who.int/iris/bitstream/10665/179184/http://apps.who.int//iris/bitstream/10665/179184/2/WHO_MERS_RA_15.1_eng.pdf
© 2015 David Parker/Science Photo Library


