22 months after its discovery, and despite extensive investigation and research, the source and origin of the Middle East Respiratory (MERS) coronavirus remain unknown.1 As of April 26, 2014, 261 laboratory-confirmed cases of MERS coronavirus infection have been reported, including 93 deaths.2 Although sustained human-to-human transmission has not been reported,1 a global concern remains that the virus could become more contagious and deadly. An overabundance of caution is certainly prudent, but with the latest discovery—that the virus was documented in dromedary camels as long ago as 19923—interpretation of the epidemiology has become more difficult. Are the recently identified cases in Jordan, Qatar, the United Arab Emirates, and Saudi Arabia new, or a part of a long series of human disease? Improved collaboration between clinicians, scientists, and public health authorities will be necessary to understand the epidemiology and define the sources and modes of transmission.
Lessons from the SARS coronavirus outbreak4 in 2003 and the influenza H1N1 pandemic5 in 2009 suggest that effective, collaborative public health research in support of outbreak investigation and comprehensive risk management is encouraged by mutual respect—for others, authority, governance, information, and property (both intellectual and physical)—and a solid agreement. But the meaningful collaboration that helped the scientific community to rapidly identify the SARS coronavirus has not been seen recently. Collaborative research into MERS coronavirus has been scarce, with investigations marked by bitter disagreements between public health authorities and scientists about the virus' discovery and the ensuing publications, processes, and patenting of products.6
The recent disagreements played out in the media raise several issues that should be addressed. Key among them is the absence of a consensus-built governance agreement for public health investigation and research when an event is recognised as a global public health emergency. Such an agreement would include the controversial issues of how to share animal and human specimens, investigational products (eg, pathogens and viral isolates), and intellectual property (eg, public health surveillance data and scientific publications). Without agreement about the mutually beneficial roles, responsibilities, and legitimate contributions of clinicians, scientists, and public health authorities, parties end up either encroaching on one another or not communicating—both of which are happening now with respect to MERS coronavirus.
Public health authorities and academic scientists must work together to discover and pursue investigation of emerging or re-emerging infectious diseases, and clinicians and scientists must fulfil their legal responsibility to report relevant data to public health authorities through official mechanisms. Such reporting enables public health authorities to undertake their legitimate and crucial role in investigating, preventing, and controlling future transmission. Successful examples of this delicate yet important balance include the recognition, reporting, and research around Legionnaires' disease7 and Lyme disease8—outbreaks that were reported appropriately, while public health research ensued.
Four considerations are pertinent to an agreement: the immediate need to control the spread of disease by public health authorities; the intellectual curiosity of clinicians and scientists; the long-term commercial interests of the pharmaceutical industry; and the economic wellbeing of the farming and ranching communities. Governance should be built around One Health, an interdisciplinary collaboration between human and veterinarian medicine and health, because economic loss is an important consideration (as can be seen from the negative economic effect of the present influenza H7N9 outbreak9). Additional steps should be taken to protect the economic interests of farmers and livestock owners. Livestock insurance schemes, already used for protection against drought, could be used for reimbursement.10 The development of a global biological risk management fund to share the burden of economic loss would enhance the mission of the 2005 International Health Regulations (IHRs).
The sovereign rights of IHR state parties must be respected. National ministries of health are responsible for the detection, assessment, reporting, and response to public health issues that threaten their populations. The willingness of states to collaborate on comprehensive risk assessments is dependent on the perception that doing so will not conflict with their own national self-interest; the global scientific community cannot force a country to collaborate. Unfortunately, the IHRs offer no guidance for how to collaborate in this way.
Strengthened global collaboration in public health research requires trust. And trust can only be built through the transparency embodied in clearly defined norms that govern how research products and data will be used and who owns them. Although the IHRs require states to share timely and accurate reports about public health emergencies of international concern, they do not specify in any practical detail other important features of data sharing and public health research collaboration, including ownership and access to patient specimens, research data, and scientific products (eg, diagnostics, vaccines, and medical countermeasures). The pandemic influenza preparedness framework11 is a commendable start, but is limited in scope and does not provide guidance for data sharing for non-influenza viruses or other biological specimens. Recent discussions within the Convention on Biological Diversity in Nagoya, Japan,12 are also a step forward with respect to the ownership of biological materials.
What is now required is for the public health and research communities to rally around the design and adoption of a consensus-built global governance agreement for rapid, effective collaborative investigation in the event of emerging infectious disease threats with pandemic potential. This process could occur through the amendment of the existing IHRs, with the addition of clear codes of practice for the sharing of public health surveillance data and other intellectual property and for the conduct of the collaborative epidemiological research necessary for comprehensive risk assessment.
Enhancement of the IHRs in this way would clearly define international expectations about how essential public health data and products that emerge should be managed, shared, and owned. Likewise, it would clarify how states should interact when crucial information for risk assessment is needed by the global health security community. Such a development would improve the state of global health security.
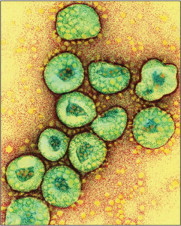
© 2014 Dr Gopal Murti/Science Photo Library
Acknowledgments
We declare that we have no competing interests.
References
- 1.PLoS Currents. PLoS Pathogens State of knowledge on MERS-CoV. PLoS Speaking of Medicine, 2014. http://blogs.plos.org/speakingofmedicine/2014/01/17/state-knowledge-mers-cov/ (accessed April 2, 2014).
- 2.WHO MERS-CoV summary updates. http://www.who.int/csr/disease/coronavirus_infections/archive_updates/en/ (accessed April 28, 2014).
- 3.Alagaili AN, Briese T, Mishra N. Middle East Respiratory Syndrome coronavirus infection in dromedary camels in Saudi Arabia. mBio. 2014;5:e00884. doi: 10.1128/mBio.00884-14. e00814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine (US) Foum on Microbial Threats, Knobler S, Mahmoud A, Lemon S, editors. Learning from SARS: preparing for the next disease outbreak—workshop summary. National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- 5.Del Rio C, Hernandez-Avila M. Lessons from previous influenza pandemics and from the Mexican response to the current influenza pandemic. Arch Med Res. 2009;40:677–680. doi: 10.1016/j.arcmed.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Butler D. Tensions linger over discovery of coronavirus. Nature News. Jan 14, 2013 http://www.nature.com/news/tensions-linger-over-discovery-of-coronavirus-1.12108 (accessed April 5, 2014). [Google Scholar]
- 7.Fraser DW, Tsai TR, Orenstein W. Legionnaires' disease: description of an epidemic of pneumonia. N Engl J Med. 1977;297:1189–1197. doi: 10.1056/NEJM197712012972201. [DOI] [PubMed] [Google Scholar]
- 8.Steere AC, Malawista SE, Snydman DR. Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three Connecticut communities. Arthritis Rheum. 1977;20:7–17. doi: 10.1002/art.1780200102. [DOI] [PubMed] [Google Scholar]
- 9.Minggao Shen BW. China equity strategy—avian flu H7N9 remains a risk. CITI Research; Beijing: 2013. [Google Scholar]
- 10.Economist.com. Livestock insurance in Kenya: no risk, no reward. Economist.com, 2014. http://www.economist.com/blogs/baobab/2014/04/livestock-insurance-kenya (accessed April 10, 2014).
- 11.WHO . Pandemic influenza preparedness framework for the sharing of influenza viruses and access to vaccines and other benefits. World Health Organization; Geneva: 2011. http://whqlibdoc.who.int/publications/2011/9789241503082_eng.pdf?ua=1 (accessed April 5, 2014). [Google Scholar]
- 12.Convention on Biological Diversity The Nagoya Protocol on Access and Benefit-sharing. https://www.cbd.int/abs/ (accessed April 5, 2014).


