Antibiotic sensitivity testing of anaerobic bacteria – Workshop arranged by ESGARAB
W4a: Genetic background of carbapenem and metronidazole resistance: detection of genes and mechanisms of expression
M. E. Hedberg (Stockholm, S)
Antimicrobial resistance is increasingly common among anaerobic Gram-negative bacteria, especially for the Bacteroides fragilis group. At present resistance has been described in this group of bacteria to almost all of the regularly used antianaerobic agents. Carbapenems and 5-nitroimidazoles are two of the most active antimicrobial agents against the B. fragilis group, but isolates resistant to these drugs seem to appear more frequently, although they still are quite rare. Metronidazole is often used as empiric therapy for anaerobic infections and susceptibility testing is not always routinely performed. Strains resistant to carbapenems have been found to produce metallo-beta-lactamase, an enzyme that hydrolyses various beta-lactam antibiotics and exhibits resistance to beta-lactamase inhibitors. B. fragilis metallo-beta-lactamase is encoded by the cfiA gene. Several diverse types of insertion sequence (IS) elements in the upstream region of cfiA in carbapenem-resistant B. fragilis strains have been found. The IS elements most likely provide a promoter to express the cfiA. It has been reported that about 2–4% of the B. fragilis strains carry the cfiA gene regardless of whether they express it. Also an IS-less activation mechanism of cfiA in B. fragilis strains has been detected. The 5-nitroimidazole molecule is a prodrug whose activation depends up on the reduction of the nitro group in the absence of oxygen. Decreased uptake and/or alteration in reduction are believed to be responsible for metronidazole resistance. Five nim genes (A–E) have been described in the B. fragilis group that confer reduced susceptibility to 5-nitroimidazole compounds. nim-Positive strains have been shown to be more prone to induction than nim-negative isolates. A nimF gene has been detected in a metronidazole susceptible strain. Isolates lacking nim genes but still highly resistant to metronidazole have also been demonstrated which probably means that other resistance mechanisms are involved. Studies of protein expression patterns in metronidazole susceptible and metronidazole resistant B. fragilis strains have revealed a complex shift in the resistant strain resulting in both down- and up-regulation of proteins with different molecular weight and isoelectric points. This might be part of a broader programme of genetic control that alters the physiology to protect and prevent metronidazole activation. Such alterations may also increase the virulence.
W4b: Unexpected resistance mechanisms behind known antibiotic resistance in anaerobic pathogen and their detection
L. Dubreuil, J. Behra, L. Calvet (Lille, F)
Despite resistance to all β-lactams (including imipenem) by production of a carbapenemase (cfiA gene), Bacteroides fragilis group strains may be resistant to the combination of β-lactams with β-lactamase inhibitor among imipenem susceptible strains. If a silent carbapenemase could be involved, in other cases the lack of porin in combination with the production of the chromosomal cephalosporinase (cep A gene) is responsible for the resistance to co-amoxiclav among B. fragilis (lack of the 45 kDa Outer Membrane Protein) or in B. thetaiotaomicron (lack of the 67 kDa OMP). In the last two years we were able to isolate metronidazole-resistant strains of B. fragilis (MIC from 16 to 256 mg/L). Their detection could be easily done using a disk-diffusion test if the incubation is prolonged for at least 48 hours. For one of these trains, the high-level metronidazole resistance was associated with the presence of two copies of the nim A gene on the chromosome (Marchandin H. et al.). Decreased susceptibility to metronidazole (MIC 8 and 16 mg/L) is still increasing in France and UK (Brazier et al.) as demonstrated by antibiotic surveys. With exception of the reference agar dilution method (NCCLS M11 A6), the detection remains problematic. Detection by disk-diffusion method is very difficult using 4 μg metronidazole disks and should be improved by using a 10 μg potency disk, Rosco disks or the E test method. Resistance to metronidazole is widespread as nim genes are nowadays found in Prevotella and Veillonella species. Intrinsic unknown resistance could be presumed from published studies such as low-level resistance to vancomycin, linezolid and ramoplanin for C. ramosum, to vancomycin and daptomycin for C. innocuum and to teicoplanin and ramoplanin for C. clostridioforme, respectively. With exception of C. innocuum (Leclercq et al.) most mechanisms had not been investigated.
History of medical microbiology in Denmark
S8: Danish medical microbiologists in the 19th century: Panum, Salomonsen & Gram
H. J. Kolmos (Odense, DK)
Three persons played a key role in the development of medical microbiology in Denmark in the second half of the 19th century: The physiologist and epidemiologist Peter Panum (1820–85), the bacteriologist Carl Salomonsen (1847–1927), and his assistant Christian Gram (1853–1938). Panum has gained international reputation for his epidemiological description of the measles epidemic in the Faroe Islands in 1846, but he also made significant experimental contributions to microbiology. In 1855–56, during his appointment as professor at the University of Kiel, he performed a series of laboratory experiments with dogs, in order to characterize the so-called ‘putrescent poison’, a substance claimed to be the causative agent of blood-poisoning. The dogs were given i. v. infusions of rotten meat juice in different modifications, and observed for symptoms and signs. His observations on the biological effects of putrescent poison bear striking similarities with present-day endotoxins, e. g. the characteristic symptoms and signs, the delay in onset of symptoms, and the preserved biological activity after long-term boiling. Panum at first rejected the possibility that the putrescent poison could be of bacterial origin, but later changed his opinion. From 1864 Panum served as professor of physiology at the University of Copenhagen, and in his institute he established the first laboratory facilities for bacteriological studies in Denmark. Salomonsen was the first to perform microbiological examinations on an infected patient. They took place in 1873 at the Municipality Hospital in Copenhagen, where he treated a patient with pyaemia. In pus aspirated from an inflamed knee joint he was able to demonstrate streptococci, and he could also isolate the streptococci from a rabbit that had been inoculated with pus from the patient. In his thesis, which he wrote under the supervision of Panum from 1876–77, he described one of the earliest methods for making pure cultures of bacteria, using capillary glass tubes. From 1883, Salomonsen held Europe's first chair in bacteriology at the University of Copenhagen, and he played a leading role in the foundation the State Serum Institute in 1902. Salomonsens assistant, Gram, invented the Gram-stain during a short visit to Friedländer's laboratory in Berlin in 1884. He is probably the most famous of all Danish microbiologists, which is somewhat paradoxical, since he left microbiology immediately after his invention, and never worked with Gram staining afterwards.
S9: Serum treatment of diphtheria: a controlled clinical trial performed in Copenhagen in 1898
A. Hróbjartsson (Copenhagen, DK)
In 1898, the Danish Nobel laureate Johannes Fibiger published a controlled trial of the effect of serum treatment on diphtheria. Fibiger was one of the first to discuss random allocation as a method to avoid bias in clinical trials. He stated: ‘A firm conclusion can in many cases only be reached when a large number of randomly selected patients are treated with a new remedy and an equally large number of randomly selected patients at the same time are treated as usual.’ Fibiger's trial included as many as 484 patients that were allocated depending on day of admittance: serum treatment was used every second day and standard treatment every second day. Furthermore, the flow of patients, and other methodological and clinical aspects of the trial, were reported precisely. Thus, the trial is a pioneering investigation in the history of clinical trials.
S11: Production of penicillin in Denmark during World War II. An early warning against development of antibiotic resistance
K. Jensen (Karlshamn, S)
It is well known to most people that penicillin was discovered in 1928 by Alexander Fleming in his laboratory at St. Mary's Hospital. It was extremely difficult to produce and to purify penicillin in sufficient amounts to be used to treat humans. It was not until 1938 that Florey, Abraham and Chain succeeded in isolating and purifying Penicillin in pure and stable form thus allowing further studies of its unique activity, extremely low toxicity, and high clinical efficiency. It was found that penicillin was a true wonder drug in treating infected wounds. The production in large scale was attempted in England, but in 1941 It became necessary to move the entire project to USA to avoid the harassment caused by the German air raids. In USA the production of penicillin was considered of millitary importance The War Production Board in cooperation with 22 medical companies united in the efforts to produce penicillin in sufficient amounts for use by the allied millitary forces and for civil use. All informations about the production and purification processes were considered as war secrets, and the penicillium strains used for production were kept under strict custody. However, today it may not be widely known, that Denmark was the only place outside England and USA where the production of penicillin was taken up during World War II. This fact is even more remarkable because it took place during the German occupation of Denmark, when exchange of information with the free world was practically impossible, and resources of nearly every kind became increasingly scarce. The attempts to produce penicillin in Denmark were started during the spring of 1943 at the University Institute of General Pathology, and as early as September 1944 the first patient was treated with Danish penicillin. This remarkable achievement was made by the head of the institute professor K. A. Jensen. He came from the Danish Statens Serum Institute where he worked as a world-known scientist within the field of tuberculosis. He had experiences in standardization of biological products and production of tuberculin and BCG vaccine, and he was deeply engaged in research on antituberculous chemotherapy. He was thus well equipped to start the research on penicillin when he in 1941 took over the chair in general pathology. The late owner of the Leo Pharmaceutical Industry: Knud Abildgaard Elling initiated this research by providing him with a reprint obtained from Sweden of Florey, Abraham and Chain's article about penicillin. K. A. Jensen started the search for a penicillin producing mould, found it, and developed his own methods of production, purification, standardization and clinical trials of Penicillin. He succeeded so well, that the further development and production of penicillin in large scale was taken over by the Leo Pharmaceutical Industry. After the end of World War II \“Leo\” was able to take up the international competition, and succeeded so well that within a few years they supplied a substantial part of penicillin to the world market. K. A. Jensen was asked by the Danish Board of Health to distribute and control the clinical use, not only of penicillin, but of all the other new antibiotics which were introduced during the postwar period. This gave him a unique opportunity to develop the new field of clinical microbiology to warn against development of resistance and restrict the misuse of antibiotics in Denmark. As son of K.A. Jensen, the author had the opportunity to follow the above mentioned development as a personal witness. He will describe some of the exiting features of this pioneering work, and some of the perils of the work with penicillin in Denmark during wartime and German occupation.
Update on toxoplasmosis (Symposium arranged with ESGT)
S13: ‘Virulence’ of Toxoplasma gondii in humans
M.-L. Dardé on behalf of the CRB ToxoBS group
The majority of Toxoplasma gondii strains have been grouped into 3 main genotypes, called type I, II, and III. Recently, multilocus studies revealed the existence of atypical and recombinant genotypes. The relationship between isolate genotype and virulence is well described in the mouse model, but is more difficult to approach in humans due to the opportunistic behaviour of this parasite. For instance, in France, where the isolates are systematically collected and typed (Biological Resource Centre, ToxoBS group), the vast majority of congenital toxoplasmoses are due to type II, whatever the clinical outcome (foetal death, neurological involvement, chorioretinitis, or subclinical toxoplasmosis), the main prognosis factor remaining the stage of pregnancy at the time of infection. Whether this predominance of type II in congenital toxoplasmosis is due to its predominance in humans and animals in France or to a higher tendency to cross the placental barrier remains to be determined. The very few type I or atypical strains isolated from congenital toxoplasmosis are found in severe disease, notably disseminated toxoplasmosis, suggesting a role for the strain genotype in the pathogenesis of these forms. In immunocompetent patients, the ‘serotyping’ method has never been applied to large series of asymptomatic patients, so the strains responsible for about 80% of toxoplasmic infections in humans are still unknown. The classical lymphadenopathies seem to be due to type II strains, but more severe acquired toxoplasmosis or ocular toxoplasmosis are associated with atypical or type I strains. In immunodeficient patients, the 3 main types, principally type II, but also atypical or recombinant strains, were detected. These studies were performed mainly in some European countries and U.S.A. and the situation might well be different in other continents as suggested by the higher genetic diversity – and pathogenicity – of isolates in French Guiana or Brazil, or by the frequency of recombinant genotypes detected in African patients. Physiopathological and immunological aspects of the behaviour of the different Toxoplasma genotypes in humans are totally ignored. All our hypothesis (widespread parasite dissemination in organs for type I strains, cyst formation and reactivation with type II strains) are derived from mouse experimental toxoplasmosis and studies are needed to better understand the influence of strain genotype on human toxoplasmosis.
S14: Congenital toxoplasmosis in Europe
E. Petersen (Aarhus, DK)
The policies for controlling and treating congenital toxoplasmosis differ between countries in Europe and include systematic monthly or three monthly screening during pregnancy, neonatal screening, widespread haphazard prenatal screening and a definite decision not to do anything. Treatment of newborns range from 3 months to 24 months with pyrimethamine and sulfadiazine or sulfadoxine. The diversity of policies is due to different perception of the size of the problem and a lack of good studies, which can be used for decision making. Several studies have shown that the risk of infection with Toxoplasma gondii has been declining over the past four decades and studies based on data collected more than two decades ago can therefore not be used to estimate the risk of infection in to days pregnant mothers. To address these problems European centres have over the past thirteen years performed a range of studies on congenital toxoplasmosis starting with the performance of diagnostics assays, standardization of antibody- and nucleic acid diagnosis and case definitions. In 1997 the European Multi-centre Study on Congenital Toxoplasmosis, EMSCOT, was started as a large, multi-centre, prospective cohort study to provide solid evidence of the benefit of prenatal and neonatal screening. The study included fourteen European centres and when recruitment stopped in 2002, more than 1300 women with proven Toxoplasma gondii infection during pregnancy were enrolled giving birth to more than 250 infected children. This and other studies performed on other European cohorts showed clearly that prenatal screening and treatment to the pregnant mother failed to prevent transmission of Toxoplasma gondii from the mother to the child. The EMSCOT study is still being analysed and data on treatment effect on signs and symptoms in children with congenital toxoplasmosis will be presented. Two on-going studies building on the EMSCOT results are still on-going: SYROCOT, Systematic Review of Congenital Toxoplasmosis, aim at performing a meta-analysis of data from several cohorts including more than 2500 infected pregnant women; and EUROTOXO aim at critically reviewing existing data to provide a new platform for designing rational studies of prevention and treatment of congenital toxoplasmosis. Key data from the different European studies will be presented.
European guidelines for diagnosis of tick borne diseases (Symposium arranged with ESCAR)
S16: Guidelines for the diagnosis of Lyme borreliosis
B. Wilske (Munich, D)
In Europe Lyme borreliosis is caused by at least 3 species, B. burgdorferi sensu stricto, B. afzelii and B. garinii. Thus microbiological diagnosis in European patients must consider the heterogeneity of Lyme disease borreliae for development of diagnostic tools such as PCR primers and antigens. According to guidelines of the German Society of Hygiene and Microbiology the serological diagnosis should follow the principle of a two step procedure (a strategy also recommended by the CDC). A sensitive ELISA (preferentially such differentiating IgM and IgG) is recommended as the first step. In case the ELISA is reactive, it is followed by immunoblots (IgM and IgG) as the second step. The reactive bands should be clearly identified, which is easy if recombinant antigens are used. The sensitivity and standardization of immunoblots has been considerably enhanced by use of recombinant antigens instead of whole cell lysates. Improved sensitivity resulted from use of recombinant proteins that are expressed primarily in vivo (e.g. VlsE) and combination of homologous proteins from different strains of borreliae (e.g. DbpA). It also appears promising to use recombinant proteins or synthetic peptides as ELISA antigens. At present, detection rates for serum antibodies are 20–50% in stage I (erythema migrans), 70–90% in stage II (i.e. acute neuroborreliosis), and nearly 100% in stage III Lyme disease (i.e. acrodermatitis and arthritis). The main goals for the future are to improve specificity in general and sensitivity for diagnosis of early manifestations (stage I and II). Detection of the etiological agent by culture or PCR should be confined to specific indications and specialized laboratories. Recommended specimens are skin biopsy specimens, CSF and synovial fluid. The best results are obtained from skin biopsies with culture or PCR (50–70%) and synovial tissue or fluid (50–70% with PCR). CSF yields positive results in only 10–30% of patients. Methods which are not recommended for diagnostic purposes are antigen tests in body fluids, PCR of urine and serum, and lymphocyte transformation tests. Interpretation of test results must always be done in context with clinical data. Here case definitions are helpful (1). The low predictive value of positive serology in case of nonspecific symptoms need to be considered. 1. Wilske, B. et al. MIQ 12 Lyme-Borreliose. Urban & Fischer, München Jena; 2000 (English version: http://www.dghm.org/red/index.html?cname=MIQ).
Vancomycin- and methicillin-resistant Staphylococcus aureus (VMRSA): how to cope with it in the hospital setting? (Symposium arranged with ESGNI)
S17: European epidemiology of vancomycin-resistant and intermediate resistant S. aureus: need for an ESGNI surveillance study?
B. Cookson (London, UK)
Thus far there have only been three known cases of vancomycin transposon A positive methicillin resistant S. aureus (MRSA) reported, all in the USA. Fortunately these strains were all susceptible to many other antibiotics and screening failed to detect any spread to other patients. Two of the cases were seen in patients with diabetic related leg ulcers and were co-colonised with glycopeptide-resistant enterococci. Other less vancomycin-resistant S. aureus isolates have been encountered (VISAs and hetero-resistant VISAs). In some instances there have been isolates that are only resistant to another glycopeptide teicoplanin (TISAs e.g. some isolates of EMRSA-17 in the UK). A case-controlled study has been performed on these. Interestingly there have been relatively few cases of infections reported world-wide of GISA infections; Japan, for example, where the first isolates were described has failed to see the epidemic that was predicted. Isolates have often proved to be unstable in their resistance when stored in the laboratory or when cross infecting other patients who have not received vancomycin treatment. We will describe the current situation with types of MRSA that are commonly seen in Europe and the reports of the types of GISAs that have been encountered in the world. We will also discuss a possible ESCMID Study Group on Nosocomial Infection (ESGNI) study looking at GISAs and other important aspects of MRSA in the EU that would complement other European and previous ESGNI studies.
Management of relapses and outbreaks of Clostridium difficile (Symposium arranged with ESGCD)
S19: Clincal management of relapsing Clostridium difficile diarrhoea
J.T. van Dissel (Leiden, NL)
C. difficile is a leading cause of nosocomial infectious diarrhoea. The condition typically affects the elderly patient with severe underlying disease who has received broad spectrum antimicrobial therapy during an extended stay in the hospital. These factors disrupt the endogenous bowel flora and are associated with acquisition and/or outgrowth of C. difficile. By consequence, individual cases of C. difficile- pseudo-membranous colitis occur, and these patients create a reservoir from which the bacterium may transmit to susceptible individuals and give rise to large hospital-associated outbreaks of diarrhoea. The infection may add significant costs to patient care. C. difficile-diarrhoea relapses in about 10 to 20% of cases. Treatment of C. difficile-diarrhoea optimally consists of the discontinuation of antibiotics to end disruption of endogenous bowel flora. All but mild cases receive therapy with metronidazole and/or vancomycin. Unfortunately, such additional cycles of antimicrobial therapy may trigger new recurrences. In relapsing diarrhoea, alternative treatments have been tried to reduce C. difficile bowel colonization and stop or neutralize toxin production, including toxin-binding resins, antimicrobial combinations comprising of, for instance, vancomycin and rifampin or bacitracin, probiotics like Saccharomyces boulardii, Lactobacillus GG, and even stools from healthy human relatives by tube or enema. Many of these treatments, however, appear to be only modestly effective. Recent developments to aid in the prevention of relapsing C. difficile-diarrhoea include, among other interventions, polyclonal antibody-enriched immune whey, intravenous antibodies, and vaccinations.
S20: Antibiotic-resistant toxin A-negative toxin B-positive Clostridium difficile in Dublin, Ireland
D. Drudy, N. Harnedy, S. Fanning, R. O'Mahony, L. Kyne (Dublin, IRL)
C. difficile is a major cause of infectious diarrhoea in hospitalised patients. Clinically important toxin A-negative, toxin B-positive strains of C. difficile that cause diarrhoea and pseudomembranous colitis in humans have recently been isolated world-wide. The aims of this study were to investigate a C. difficile outbreak in one university-affiliated hospital in Dublin, Ireland and to determine the prevalence of toxin A-negative, toxin B-positive C. difficile in other care institutions in the greater Dublin area. For the outbreak investigation, we prospectively studied all consecutive patients with nosocomial C. difficile diarrhoea between August 2003 and January 2004. For the prevalence study, toxin positive faecal samples (n = 123) were collected between February and August 2004 from a twelve different institutions in Dublin Ireland. C. difficile was cultured from faecal specimens. Toxin-specific enzyme immunoassays, IMR-90 cytotoxicity assay and PCR were used to analyse C. difficile isolates. Antibiotic sensitivities were determined using E-tests. Seventy-three cases of C. difficile diarrhoea were identified during the outbreak study period. Studies examining in vitro production of toxin A and B showed that ninety-five % of isolates tested negative for production of toxin A but were positive when investigated using the cell culture cytotoxicity assay. These toxin A-negative, toxin B-positive C. difficile isolates had a 1.7 kb deletion in the tcdA gene. PCR ribotyping determined that these isolates were clonal. The clonal outbreak isolates were resistant to all fluoroquinolones (MIC's of >32 μgml−1) and MLS antibiotics tested (MIC's of >256 μgml−1). In the prevalence study, 52 of 123 C. difficile isolates, (42%) were toxin A-negative, toxin B-positive. Prevalence rates per institution varied from 0–62%. In the three University teaching hospitals the prevalence rates were 18%, 40%, and 59% respectively. Using PCR, these toxin A-negative, toxin B-positive strains had the same deletion described for the outbreak study (toxinotype VIII strains e.g., C. difficile serotype F, 1470). Toxin A-negative, toxin B-positive C. difficile appears to be prevalent in hospitals in the greater Dublin area and caused at least one hospital outbreak. This report adds to the expanding body of literature reporting the increasing incidence and widespread geographical distribution of clinically important toxin-variant C. difficile strains.
Antibiotics for lower respiratory tract infections in primary care (Symposium arranged with ESPRIT)
S21: A randomised controlled factorial trial of antibiotic prescribing strategies and an information leaflet about natural history for acute lower respiratory tract infection
P. Little, K. Rumsby, J. Kelly, L. Watson, I. Williamson, M. Moore, G. Warner, T. Fahey (Southampton, Romsey, Dundee, UK)
Background: Acute LRTI is the most common condition managed in primary care. The systematic reviews of antibiotics are small and come to different conclusions, and many physicians still prescribe antibiotics.
Methods: 807 patients with acute LRTI were randomised to three prescribing strategies – immediate antibiotics, delayed prescription, and no offer of antibiotics. Half of each of these groups received an information leaflet.
Results: Cough rated at least ‘a slight problem’ lasted on average 11.7 days (25% lasted 17+days). An information leaflet had no effect on the main outcomes. Compared with no offer of antibiotics, other strategies did not alter cough duration (delayed +0.75 days, 95% confidence intervals −0.37 to 1.88; immediate +0.11 days, −1.01 to 1.24) nor other primary outcomes. Antibiotics reduced duration of ‘moderately bad’ symptoms, a secondary outcome, by one day (−1.08; −2.1 to −0.09). Compared with the antibiotic group slightly fewer patients were ‘very satisfied’ in the delayed and control groups (respectively 86%, 77%, 72%, p < 0.005), fewer used antibiotics (96%, 20%,16%, p < 0.001) and fewer believed in the effectiveness of antibiotics (75%, 40%, 47%, p < 0.001). There was lower re-attendance for cough within a month with delayed and immediate prescribing (mean attendances: no antibiotics 0.19, delayed 0.12, immediate 0.11, Kruskal Wallis p = 0.03).
Conclusion: For most patients with acute uncomplicated LRTI, no offer or a delayed offer of antibiotics was acceptable, associated with little difference in symptom resolution, and considerably reduced antibiotic use and beliefs in antibiotics. Delayed prescribing may have some advantages to not prescribing since fewer patients reconsulted.
S22: Cross-sectional study on antibiotics for lower respiratory tract infections: clinical determinants of under- and overtreatment in primary care
A.E. Akkerman, M.M. Kuyvenhoven, J.C. van der Wouden, T.J.M. Verheij (Utrecht, Rotterdam, NL)
Objectives: To assess the appropriateness of antibiotic treatment in acute lower respiratory tract infections (LRTIs) in primary care and to assess clinical patient characteristics that cause under- or overprescribing of antibiotics.
Methods: During four weeks in winter (2002–2003), 146 Dutch general practitioners (GPs) from the middle region of the Netherlands included all patients with lower respiratory tract complaints. They registered patient demographics (age and gender), clinical presentation (signs and symptoms, like duration of complaints, cough, fever and dyspnoe), severity of illness, whether they thought patients expected antibiotic treatment, diagnosis and management. Using the current guidelines of the Dutch College of General Practitioners on LRTIs, we assessed the appropriateness of antibiotic prescribing in cases of LRTIs. The association between clinical patient characteristics and under-/overtreatment was assessed by means of GEE (SAS) with odds ratios (ORs) (with 95% confidence intervals).
Results: In more than 60% of LRTI-consultations antibiotic treatment was according to national guidelines. In three out of each ten LRTI-consultations antibiotics were not indicated but prescribed. High severity of illness, fever, purulent sputum and if the GP thought the patient expected an antibiotic, were independent predictors of this overtreatment with antibiotics (ORs between 1.6 and 10.0). In about one of each twenty LRTI-consultations antibiotics were indicated but not prescribed (undertreatment). In these cases mostly symptomatic treatment, like analgesics and cough suppressants, were prescribed.
Conclusion: Incorrect interpretation of clinical patient characteristics and perceived expectation of patients were associated with overprescribing of antibiotics in cases of LRTIs in primary care. Overtreatment farly outweighs undertreatment.
Antibiotic use and policies: an in-depth look at ARPAC results (Symposium arranged with ESGAP)
S23: Patterns of antibiotic use in European hospitals
F.M. MacKenzie (Aberdeen, UK)
Aggregated hospital antibiotic use data from 2001, collected from 140 European ARPAC hospitals are presented. This work was carried out under the auspices of the ESCMID Study Group on Antibiotic Policies.
Methods: Antibiotic use was measured in DDD/100 occupied bed-days (BD), using DDDs described by the WHO (2004). Data are described for individual antibiotics as well as the ATC J01 classes. Data were analysed by various demographic characteristics. Relationships between antibiotic use and resistance were also explored.
Results: For all hospitals, the antibiotic use range was 5–129 DDD/100 BD (median = 55, IQR 40, 73). For all hospitals, J01C (penicillin B-lactams) were used most often, followed by J01D (non-penicillin B-lactams) and quinolones with median values of 22, 10 and 6 DDD/100 BD. Total and class antibiotic use varied significantly by geographical region. It did not vary significantly by hospital size, teaching status or case mix. Median total antibiotic use for the north, south-east, south, west and centre/east (regions 1–5 respectively) was 48, 45, 81, 63 and 37 DDD/100 BD respectively. Median use of J01C for regions 1–5 was 25, 13, 24, 29 and 12 DDD/100 BD. The most used sub-class were the B-lactamase inhibitor combinations (J01CR) making up 1, 27, 79, 67 and 48% of J01C for regions 1–5 respectively. There was a significant relationship between the number of individual antibiotics listed per hospital (maximum n = 80) and total antibiotic use; the higher the number of antibiotic available, the higher the total use. The North of Europe had the highest number of antibiotics listed but had relatively low total use; which may indicate better control. A large proportion of total antibiotic use was accounted for by a minority number of individual antibiotics; on average, the top 10 most frequently used antibiotics accounted for 75% of total use. The most frequently used individual antibiotics were amoxicillin + enzyme inhibitor (oral), amoxicillin + enzyme inhibitor (parenteral), ciprofloxacin (oral), cefuroxime (parenteral) and amoxicillin (oral). Of 7 groups of antibiotics tested, total antibiotic use (both including and excluding glycopeptide use) as well as use of 3rd generation cephalosporins showed a significant, positive correlation with MRSA prevalence (unadjusted, unweighted tests). After removal of variation in MRSA due to demographic factors, a strong statistically significant partial correlation was found between MRSA prevalence and macrolide use.
S24: The influence of antibiotic policies on antibiotic use patterns: ARPAC data
J. Bruce, J. Mollison, F.M. MacKenzie, I.M. Gould on behalf of the ARPAC Steering Group
Aim: One aim of the ARPAC study was to explore antibiotic policies and prescribing practices associated with antibiotic consumption.
Methods: Postal questionnaires and electronic spreadsheets were used for retrospective collation of hospital antibiotic policy and consumption data from European hospitals for 2001. A total of 170 hospitals provided policy data; 140 antibiotic consumption data and 124 hospitals provided both. Respondents provided data on antibiotic availability, formularies, policies, education, audit and the role of pharmacy and laboratory. Thirteen key questions were identified as indicators of good antibiotic policies and practice. Antibiotic consumption was measured using DDD per 100 bed-days (WHO, 2004). Data were analysed by hospital demographic characteristics, geographical region (N, W, S, SE, CE) and associations between policies and antibiotic consumption were explored.
Results: There was geographical variation in antibiotic policy factors, with hospitals from North and Western Europe more likely than those from other regions to have written antibiotic policies (N 79%, W 72%, CE 54%, S 46%, SE 25%; P < 0.01), written antibiotic formularies (W 94%, N 84%, CE 85%, S 59%, SE 42%; P < 0.01) and to have drugs and therapeutics committees in 2001 (N 100%, W 98%, CE 88%, SE 69%, S 68%; P < 0.01). Hospitals from the North were less likely than other regions to include a restricted list of antibiotics within formularies (N 39%, W 71%, S 78%, SE 78%, CE 82%; P < 0.01). However, for other policy indicators, no statistically significant differences were found in practice across geographical region or by hospital case-mix. There was no consistent pattern of reduced antibiotic consumption (total and other major sub-classes) by policy factor e.g. employment of an antibiotic utilisation co-ordinator, computerised prescribing, education of staff on antibiotic consumption and consequences of resistance. Issues relating to the measurement of antibiotic consumption and indicators of good antibiotic stewardship will be discussed.
Is the commensal anaerobic microflora involved in spreading antibiotic resistance? (Symposium arranged with ESGARAB)
S25: Antibiotics promote colonisation by resistant anaerobic bacteria
E. Nagy (Szeged, HUN)
The use and even more the overuse of antibiotics in some instances act not only on the pathogens, but also on the normal gut flora of the patients dominated by anaerobes, causing disturbance in the composition of it. This may lead to overgrowth of pathogens causing sever diarrhoea, the most well known side effect of antibiotic treatment. Disturbance in the composition of the normal flora however, can occur on all mucosal surfaces. During antibiotic usage not only the changes in the composition of the normal flora can be observed, but the increase of resistance to the antibiotics among the bacteria present. The consequences of the overuse of tetracycline, erythromycin and clindamycin in acne patients can be well followed by the increasing number of resistant Propionibacter acnes isolates among acne patients and their close contacts. Carbapenem resistant (or still susceptible, but cfiA positive) Bacteroides strains emerged not only among clinical isolates, but also among normal faecal flora isolates during the past 10 years, parallel with the increased use of this antibiotics in the clinical practice. The Helicobacter pylori eradication programmes may not only cause an increase in the amoxicillin or clarythromycin resistance of the aerobes and anaerobes in the normal flora, but the selection of the metronidazole resistant Bacteroides fragilis and related species. The increase of the antibiotic resistance among the indigenous anaerobic flora of the different body sites may cause the potential danger of the development of infections due to antibiotic resistant or multiresistant anaerobes. The impact of the antibiotic usage in the clinical practice is extremely high not only on the composition of the normal flora dominated by anaerobes, but also on the emergence and selection of resistance in these bacteria.
Malaria control – what is in the pipeline?
S37: Malaria in the developing and industrialised world
A. Schapira (Geneva, CH)
Malaria remains one of the main global communicable disease problems of our time. It is estimated that the malaria incidence in 2004 in 111 countries affected by malaria was 350–450 million cases. The disease is responsible for over 1 million deaths in the world per year, mainly in tropical Africa, where it is a principal cause of nearly 20% of all young child deaths; malaria mortality in eastern and southern Africa almost doubled over the period 1992–1998 compared with 1982–1989 possibly as a result of increasing resistance to chloroquine; in addition, malaria is an important indirect cause of death for example through malaria-related maternal anaemia in pregnancy and low birth weight. The disease impedes economic growth in tropical developing countries not only as a result of the mortality and morbidity burden and the expenditures for prevention and treatment but also because it is a powerful deterrent to foreign investment. For industrialized countries, malaria is mainly a problem in travelers, who suffer a total of about 10,000 acute disease episodes per year. Despite small outbreaks in industrialized countries around the world, there is no evidence that the disease is returning to temperate regions as a result of global warming or other factors. Effective tools for prevention, control and treatment are now available. Among the most important are long-lasting insecticidal nets, intermittent preventive treatment in pregnancy, artemisinin-based combination therapy, artemisinin-based suppositories, and rapid diagnostic tests. International transfers for malaria control have greatly increased since the establishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria and have now reached a level of about USD 400 million per year. The key challenge to developing countries is now to improve health systems and to recruit and maintain the health workforce, which is needed at all levels of the system for cost-effective use of resources and tools and documentation of results. The main challenge to the scientific community and industry is to develop new antimalarial treatments, new insecticides and methods for vector control, better diagnostics and, possibly, effective vaccines.
S40: Treatment of malaria: the present status and update on new antimalarials
S. Looareesuwan, P. Wilairatana, N. Tangpukdee, S. Krudsood (Bangkok, TH)
New antimalarial drugs that have been investigated at the Hospital for Tropical Diseases, Faculty of Tropical Medicine, Mahidol University, in recent years are as follows, atovaquone, a hydroxynaphthoquinone, was evaluated and it was found that atovaquone alone proved safe and effective. All patients treated had clinical cure, however, one third of patients had late recrudescence (RI). When it was combined with proguanil, the cure rate increased to 100%. This combination has now been developed into a fixed drug named Malarone. Artemisinine derivatives such as artesunate, artemether, arteether and dihydroartemisinin are also tested at the Bangkok Hospital for Tropical Diseases. Artesunate and artemether alone at a total dose of 600 to 750 mg. given over 5–7 days produced cure rates of 80 to 95%. Artesunate or dihydroartemisinin suppositories at a dose of 10 mg/kg/day have been proved successful for the treatment of severe malaria. The artemisinin derivatives, (4 mg/kg/day) when used in combination with mefloquine (8 mg/kg/day) given once a day for 3 days gave improved cure rates, up to 95–100%. Dihydroartemisinin alone with a total dose of 480 mg given over 5 days gave a cure rate of 90%. Arteether, a WHO/TDR supported drug, has been evaluated in the Hospital and now has been registered for use (the same dose of artemether) in severe malaria under the name Artemotil.® Other combinations (artemisinin derivatives combined with tetracycline or doxycycline and mefloquine combined with tetracycline or doxycycline) have also been evaluated with improvement in cure rates. Recently, a fixed drug (artemether plus lumefantrine) named Coartem® (six doses given over 72 hours) proved to be a safe and effective drug (cure rate over 95%) for the treatment of falciparum malaria and it has been registered for use in many western countries. At present, studies with combinations of artemisinin derivatives plus mefloquine (in various doses and durations of treatment) are being investigated. Recently we have finished the double-blind, randomized, comparative study of 200 patients (adults and children) with falciparum malaria treated by a pre-packed blister approach (4 mg/kg/day artesunate and 8 mg/kg/day given once a day for 3 days) and found that this approach proved safe and effective and this approach could translate clinically into a better patient compliance. Other fix-combinations (Artecom®, Artekin®) proved safe and efficious (cure rate over 98%) and could be an alternative antimalarial drugs. In general, artemisinin derivatives (12 mg/kg total dose given in 3 days) combined with mefloquine (25 mg/kg total dose given in 3 days) have been a standard regimen for the treatment of multidrug resistant falciparum malaria in Thailand. Until proven otherwise, drug combinations are still recommended for all adult patients suffering from acute uncomplicated falciparum malaria contracted in multidrug resistant areas. The treatment for uncomplicated malaria is aimed at producing a radical cure using the combination of either (1) artesunate (mg/kg/day) plus mefloquine (8 mg/kg/day) for 3 days; (2) a fixed dose of artemether and lumefantrine (20/120 mg tablet) named Coartem (4 tablets twice a day for three days for adults weighing more than 35 kg); (3) quinine 10 mg/kg 8-hourly plus tetracycline 250 mg 6-hourly for 7 days (or doxycycline 200 mg once a day for 7 days as an alternative to tetracycline) in patients aged 8 years and over; and (4) a combination of atovaquone and proguanil called Malarone (in adult, 4 tablets given daily 3 days). In treating severe malaria, early diagnosis and early treatment with a potent antimalarial drug is recommended to save the patient's life. The antimalarial drugs of choice are: intravenous quinine or a parenteral form of an artemisinin derivative (artesunate i.v./i.m. 2.4 mg/kg followed by 1.2 mg/kg injection at 12 and 24 hr and then daily for 5 days; artemether i.m. 3.2 mg/kg injection followed by 1.6 mg/kg at 12 and 24 hrs and then daily for 5 days; artemether i.m. (Artemotil) with the same dose of artemether; artesunate suppository (5 mg/kg) given rectally 12 hourly for 3 days). Oral artemisinin derivatives (artesunate, artemether, dihydroartemisinin with the dose 4 mg/kg/day should replace parenteral forms when patients can tolerate oral medication. Oral mefloquine (25 mg/kg divided into two doses 8 hrs apart) should be given at the end of the artemisinin treatment course to reduce recrudescence. The treatment of vivax malaria in Thailand is still using chloroquine and primaquine. However with the ineffective to primaquine (15 mg/kg/day for 14 days with relapse rate of 15%) the higher dose (30 mg/kg/day for 14 days) is recommended. The efficacy studies of primaquine in various regimen given together with Sulfadoxin/Pyrimethamine or artemisinin derivatives are in progress. Tefenoquine® phase III study in the planning stage for clinical trial in our setting in Thailand is in progress.
Pseudomonas aeruginosa: a rogue bacterium in the intensive care unit (Symposium arranged with ESICM)
S43: Role of efflux pumps in multiresistance of Pseudomonas aeruginosa
J. Vila (Barcelona, E)
Pseudomonas aeruginosa are an important cause of opportunistic nosocomial infections. A major feature of this microorganism is the increasing resistance to multiple antimicrobial agents. Three main factors contribute to this multiresistance: i. The intrinsic resistance; ii. Facility to acquire resistance and iii. Ability to survive in moist environments. Intrinsic multiresistance can be due to the interplay between the low permeability of the outer membrane which, for some antibiotics, is 10 to 100-fold less than that of Escherichia coli and the constitutive expression of some efflux pump(s). Currently, at least five main efflux pumps associated with the resistance to multiple antimicrobial agents have been shown (MexAB-OprM, MexCD-OprJ, MexXY-OprM, MexEF-OprN and MexVW-OprM). These efflux pumps have different substrate specificities. The constitutive expression of MexAB-OprM seems to play an important role in intrinsic multiresistance since mutations that prevent expression of this efflux pump result in hypersusceptibility to quinolones, tetracyclines, chloramphenicol, trimethoprim and some b-lactam antibiotics. On the other hand, MexXY-OprM may have a primary role in intrinsic resistance to aminoglycosides and erythromycin. However, the greatest therapeutic problems occur when these multi-drug efflux pumps are overproduced, generating a high level of multiresistance. This scenario can also be observed during the course of treatment of an infection caused by P. aeruginosa. Unfortunately, the emergence of resistance during therapy is not a rare event in this microorganism. An in depth study analysing the prevalence of the overproduction of each of the abovementioned efflux pumps in clinical strains of P. aeruginosa has not been performed. However, efflux pump-overproducing P. aeruginosa mutants selected during the treatment of infections may range from 50 to 80%. The acquisition of resistance during therapy is normally associated with specific mutations. Hypermutability is an important factor which, together with a high inoculum in the infection site and the ability of P. aeruginosa to produce biofilm, may contribute to therapeutic failures. Knowledge of the prevalence of efflux pumps in the acquisition of multiresistance in P. aeruginosa clinical isolates and the ability of the different antimicrobial agents to select resistant mutants would help in the selection of the appropriate therapy.
Tuberculosis: persistence and resistance
S48: Treatment in the modern era of resistance
F. Drobniewski (London, UK)
Drug resistant, and particularly multiple-drug resistant tuberculosis (MDRTB) is increasing globally particularly in Eastern Europe, but the actual incidence is unknown. Countries with effective TB programmes see low rates of MDRTB amongst new cases annually. Hot spots with high rates such as countries of the former Soviet Union exist and modelling of existing data suggest that between 250–500 000 new MDRTB cases occur globally. MDRTB is particularly difficult to treat, particularly when co-existing with HIV infection, and carries a high mortality compared to drug sensitive disease. Although modern rifampicin-based short course treatments are effective against drug sensitive and mono-resistant disease (apart from rifampicin resistance), MDRTB therapy is difficult and prolonged. Survival requires therapy with at least three agents to which the bacteria are susceptible. New research has produced many rapid and novel methods to diagnose drug resistance earlier which may confer some survival or public health advantage as may other processes that reduce diagnostic delay including the reduction of stigma. In high income countries, individualised therapy forms the gold standard of treatment but the substantial laboratory costs associated with this approach have led to studies of standardised treatment in middle/low income countries. Studies in Peru examined both approaches with comparable success. Nevertheless even standardized treatment requires an accurate survey of drug resistance and an understanding and correction of the initial causes of high rates of MDRTB. Few new drugs are available for treatment and the individual and health system costs of treating drug resistant cases are high emphasising the critical importance of curing drug sensitive tuberculosis at first presentation. The presentation will discuss some of the management options available for the treatment of resistant disease.
Clinical microbiology: what's new in conventional and molecular diagnostics? (Symposium arranged with ESGMD)
S49: The role of conventional diagnostic techniques in the diagnosis of respiratory tract infections
M. Ieven (Edegem, B)
In view of the increasing development of bacterial antibiotic resistance, proper and rapid diagnostic tests may result in better patient management with appropriate therapy or reduction of unnecessary antibiotic therapy. Therefore, a number of recent evidence based guidelines for the management of patients with respiratory tract infections also include guidelines on microbiological diagnosis, including both conventional and new techniques. Competition between traditional and new techniques are conditioned by: rapidity and quality of results, need for special infrastructure and trained personnel, possibility to deliver results 24/24 hours 7/7 days and cost. In pneumonia blood and pleural exsudate cultures are positive in only 4–18% and upto 40% of cases respectively. However, as they offer a highly specific diagnosis, blood cultures should be performed in hospitalised patients with CAP and thoracentesis when significant pleural fluid is present. Quantitative bacterial cultures may be important for the assessment of BAL and PSB fluid: advantages and limitations will be discussed. The most frequently submitted specimen is sputum. Criteria for good quality sputum are now universally accepted but there are still great controversies about the value of sputum Gram stain and culture. Gram strain of a valuable sputum showing a predominant morphotype correlates well with the results of boodcultures, is a rapid and low cost technique allowing a presumptive etiological diagnosis of pneumonia in many cases, allows correct interpretation of sputum culture results and therefore is recommended. Urine antigen detection is recommended for the diagnosis of L. pneumophila infections but for S. pneumoniae more studies are needed. Serological tests usually produce late results particularly for the ‘atypicals’, while the multitude of procedures for C. pneumoniae and M. pneumoniae produce divergent results. Some recent studies on the improved detection of these agents by molecular tests illustrate the often low predictive value of serology showing the limited application in the routine management of the individual patient. Based on recent studies and guidelines, indications for the use of a number of conventional diagnostic techniques in different clinical situations will be discussed. A compromise must often be found between the value of the test, feasibility turnaround time and cost.
S50: Urinary antigen testing for respiratory infections: for which pathogens and when to use them?
J.A. Domínguez (Barcelona, E)
Community-acquired pneumonia (CAP) is a frequently occurring disease with high morbidity and mortality, which causes numerous hospitalizations. Despite of advances in the development of vaccines and of the appearance of new antibiotics, the incidence of pneumonia does not decrease. This is probably due to the ageing of the population, an increase in the number of immunodepressed persons, and an increase in the prevalence of chronic diseases. Knowing the etiology of pneumonia is of great significance because it permits an empirical antibiotic therapy to be converted into a specific one, which contributes to optimizing costs and probably helps conserve bacterial ecology. The etiological diagnosis of CAP in the majority of cases remains uncertain. An adequate sputum specimen is often difficult to obtain, and even then, the specimen is frequently contaminated with oropharyngeal bacteria. The blood culture is positive in less of a 20% of cases. Serological tests requires to be performed preferably in paired serum samples, providing a retrospective diagnostic. Various recent studies from distinct geographical areas coincide in that the etiological yield is lower than 60% with conventional microbiological diagnostic techniques. The most frequent aetiological agents are Streptococcus pneumoniae, Haemophilus influenzae, Legionella pneumophila, Chlamydophila pneumoniae and Mycoplasma pneumoniae. In the severe cases of pneumonia the first 3 etiologies should always be considered. Techniques for antigen detection of L. pneumophila and S. pneumoniae in urine samples have, in the last few years, been demonstrated to be rapid, sensitive and specific. In addition, the use of urine samples concentrated by selective ultrafiltration procedure improves the sensitivity significantly. In our experience, these techniques have proven to be useful in the diagnosis of CAP. Given the large number of diagnostics, even when the patient has received prior treatment with antibiotics, the use of these techniques is highly recommendable as having the etiological diagnosis available allows antibiotic treatment to be adjusted, the importance of which it is not necessary to point out.
Antibiotic usage: practices and policy interventions
O53: Self-medication with antibiotics in Europe
L. Grigoryan, F.M. Haaijer-Ruskamp, D. Monnet, R. Mechtler, A. Tambic Andrasevic, A. Alkerwi, E.A. Scicluna, C. Stalsby Lundborg, J. Birkin, A. Di Matteo, R. Cunney, H. Edelstein, R. Valinteliene, R. Deschepper, R. Andrajati, P. Grzesiowski, J. Campos, C. Bara, T. Tesar, M. Cizman (Groningen, NL; Copenhagen, DK; Linz, A; Zagreb, HR; Luxembourg, LUX; Guardamangia, MT; Stockholm, S; Nottingham, UK; Maria Imbaro, I; Dublin, IRL; Afula, IL; Vilnius, LT; Brussels, B; Hradec Kralove, CZ; Warsaw, PL; Madrid, E; Craiova, RO; Bratislava, SVK; Ljubljana, SVN)
Objectives: To assess the prevalence of self-medication with antibiotics in 19 European countries, including actual use in the last 12 months and ‘at risk’ self-medication, i.e. intended use without contacting a doctor, storage of antibiotics at home; to explore sources of obtaining antibiotics, the reasons for self-medication and the relation between persons characteristics, prescribed use of antibiotics and self-medication.
Methods: A population survey conducted in each country (Austria, Netherlands, Sweden, UK, Ireland, Denmark, Italy, Malta, Luxembourg, Belgium, Spain, Israel, Romania, Czech rep, Slovakia, Lithuania, Slovenia, Croatia, Poland), with a self-administered postal questionnaire using a two-stage stratified sampling design. Study population in each country included a random sample of 1000–3000 adults equally distributed in urban and rural areas. Logistic regression was used to analyse the determinants of self-medication use.
Results: The overall response rate was 40% (ranging 18–70% between the countries). The rates of actual and ‘at risk’ self-medication as well as prescribed use of antibiotics tend to be high in southern and eastern European countries and low in western and northern countries (table 1). The main sources of self-medication were directly from pharmacy without prescription (58% of all self-medication courses), leftovers (32%) and friends/relatives (8%). The most common reasons for self-medication use reported by the respondents were throat symptom (20% of self-medication courses), teeth/gum symptom (15%), acute bronchitis (9%), influenza (7%), urinary tract infection (7%) upper respiratory infection (6%). Penicillins (J01C) was the most frequently used antibiotic group for self-medication (figure 1). Younger age, country, presence of chronic diseases and prescribed use of antibiotics were related to self-medication use. Gender and location (urban/rural) were not associated with actual self-medication with antibiotics.
Conclusions: Self-medication with antibiotics is a problem in all European countries in varying degrees, with low levels in North and West and high levels in South and East. This consistency underlines the relevance of health care system and cultural factors for antibiotic use. Broad spectrum penicillins tend to be used for self-medication more frequently in South and East.
Table 1.
Actual use of systemic antibiotics in the last 12 months and “at risk” self-medication in 19 European countries
| Rates per 1000 respondents (95% CI) |
||||
|---|---|---|---|---|
| Self-medication | Prescribed use | Intended self medication | Storage | |
| North | ||||
| Sweden | 4 (0.09–0.2) | 135 (109–161) | 118 (94–143) | 14 (2–26) |
| Denmark | 7 (4.12) | 172 (154–189) | 132 (116–147) | 42 (33–52) |
| West | ||||
| Netherlands | 1 (0.2−2) | 152 (134–170) | 85 (11–101) | 10 (6–17) |
| Austria | 9 (2.25) | 159 (134–145) | 73 (49–105) | 32 (14–55) |
| Belgium (Flanders) | 9 (5.15) | 222 (201–242) | 80 (67–95) | 1 (19–84) |
| Luxemburg | 9 (3.19) | 288 (212–324) | 83 (62–107) | 90 (69–114) |
| UK | 12 (5–23) | 121 (109–254) | 156 (137–295) | 33 (21–49) |
| Ireland | 14 (7–25) | 353 (330–306) | 150 (125–276) | 29 (19–43) |
| South | ||||
| Israel | 15 (6–31) | 330 (287–374) | 137 (150–223) | 120 (91–140) |
| Malta | 55 (38–79) | 422 (380–462) | 228 (152–354) | 156 (125–136) |
| Italy | 62 (33–103) | 512 (444–580) | 243 (185–301) | 379 (314–445) |
| Spain | 152 (103–201) | 315 (251–379) | 314 (249–380) | 260 (200–320) |
| East | ||||
| Czech Republic | 7 (3–13) | 253 (238–279) | 179 (156–201) | 45 (33–58) |
| Slovenia | 17 (10–26) | 293 (266–320) | 230 (253–307) | 119 (100–137) |
| Croatia | 31 (19–48) | 239 (399–478) | 205 (172–237) | 130 (103–156) |
| Poland | 33 (33–47) | 199 (172–225) | 115 (94–136) | 69 (53–87) |
| Slovakia | 43 (38–54) | 369 (537–512) | 324 (284–365) | 192 (159–225) |
| Romania | 190 (160–235) | 307 (263–351) | 431 (303–470) | 200 (162–230) |
| Lithuania | 210 (181–230) | 275 (243–308) | 119 (412–486) | 147 (142–201) |
Fig. 1.

Use of major groups of antibiotics for self-medication in 17 countries.
O54: Antibiotic use in 2003 in Europe
M. Ferech, S. Coenen, E. Hendrickx, K. Dvorakova, H. Goossens and ESAC Project Group
Objectives: ESAC, European Surveillance of Antimicrobial Consumption, granted by DG/SANCO of the European Commission, is an international network of surveillance systems, aiming to collect comparable and reliable data on antibiotic consumption in Europe. Thirty-four countries have joined the second phase of the ESAC project (2004–2007), including all 25 EU countries and 4 current applicant countries.
Methods: Outpatient and hospital antibiotic use for 2003 were collected, using the ATC/DDD methodology, version 2004. Results were expressed as DDD per 1000 inhabitants per day (DID). Detailed information on the sources of antibiotic use data can be found at the ESAC website (www.ua.ac.be/ESAC). Of the 34 participating countries 21, 19 and 2 were able to deliver outpatient, hospital and total data, resp., for 2003. In view of the expected change of DDD for parenteral co-amoxicillin, a pilot study on the pattern of consumption of antibiotics with multiple DDDs was conducted, based on data subdivided by route of administration.
Results: Outpatient antibiotic use varied with a factor of 3.2 between the countries with the lowest and highest consumption, c.q. still the Netherlands (9.8 DID) and for the first time Greece (31.4 DID). Consumption in France decreased by 7.1% the year after their first national campaign. A similar reduction was seen in Belgium (−7.6%) after the first Belgian campaign. Hospital antibiotic use ranged between 1.4 DID in Norway and 3.6 DID in France. Nine substances with multiple DDDs were identified within the J01 ATC group: amoxicillin and enzyme inhibitor, cefuroxime, ciprofloxacin, clarithromycin, clindamycin, fosfomycin are available in oral and parenteral form, tobramycin in inhalatory and parenteral form, while DDDs for erythromycin and methenamine differ according to their chemical salts. Specifically consumption of parenteral co-amoxicillin was substantial in 4 out of 10 countries, which were able to deliver detailed data.
Conclusion: ESAC data underpin the success of two national campaigns on antibiotic prescribing (Belgium and France). An introduction or change of DDD for a specific form of any antibiotic can substantially influence the profile of antibiotic consumption in some countries. Thus the ESAC data collection protocol shall be adjusted to allow us to control for these changes retrospectively, by collecting data at a product presentation level.
055: Changing antibiotic prescribing for respiratory infections in primary care: systematic review
I. Welschen, M.M. Kuyvenhoven, T.J.M. Verheij, A.W. Hoes on behalf of ESPRIT
Objective: Almost 80% of outpatient used antibiotics are prescribed by general practitioners with up to 75% of these prescriptions being for acute RTIs. There is an international trend to prescribe more new and broad spectrum antibiotics, also in countries with relatively low prescribing rates such as the Netherlands. Several methods (clinical guidelines, postgraduate educational courses and prescribing feedback) have been used to reduce and optimise antibiotic treatment of acute RTI's, but changing towards a more frugal and rational prescribing behaviour seems to be difficult. However, there are no reviews available on the effectiveness of educational interventions aimed at optimising prescribing antibiotics for acute RTI's in primary care. That is why the purpose of this study was to evaluate the effectiveness of educational interventions aimed at changing professional behaviour: reducing prescribing antibiotics or increasing prescribing of first choice antibiotics for acute RTI's in primary care by systematically reviewing available randomised controlled trials (RCT's).
Methods: Data sources. Medline (1966–October 2003), Embase (1980–October 2003) and Cochrane Library (October 2003). Study selection. In the first phase, studies describing effects of interventions on changing prescribing antibiotics in primary care were included by screening titles, keywords and abstracts. In the second stage, the full text was retrieved using the following inclusion criteria: (1) involving an intervention aimed at improving and reducing prescribing antibiotics for RTI's, (2) control group in which no intervention relating to RTI's was present, (3) RCT with before and after measurements, (4) outcome measures: ‘antibiotic prescription rates’ for acute RTI's or ‘percentage of first choice antibiotics’. Data extraction. Reviewers independently extracted data. Methodological quality was assessed relating to selection procedure, the intervention, outcomes and statistics.
Results: Eight trials (12 interventions) were included. Mean quality was relatively low (56% of the maximum). Antibiotic prescription rates reduced by 6% (95% CI: 4 to 7), while proportion of first choice antibiotics increased by 12% (95% CI: 10 to 14).
Conclusions: Most interventions aimed at optimising prescribing antibiotics for acute RTI's were effective. However, changing to prescribing more first choice antibiotics seemed easier than reducing the number of prescriptions.
056: Differences in incidence and prescribing antibiotics in upper respiratory tract infections in Dutch general practice between 1987–2001: did publication of national guidelines make a difference?
T.J.M. Verheij, M. Kuyvenhoven, G.A. van Essen, F.G. Schellevis on behalf of ESPRIT
Objective: Most antibiotic prescriptions are prescribed in primary care with respiratory tract infections (RTI's) being the most common indication. Although Dutch antibiotic rates are low, even in the Netherlands up to 50% of antibiotic prescriptions for RTI's are assumed to be unnecessary. Overprescribing unnecessarily exposes patients to risk of side effects, encourages re-consulting for similar problems and enhances antimicrobial resistance. In the nineties the Dutch College of General Practitioners has published guidelines for management of upper RTI's with clear indications for antimicrobial treatment. It is unknown whether these guidelines have yielded a reduction in prescribing antibiotics. This study is aimed to assess differences in antibiotic prescribing and incidence rates of upper RTI's in Dutch General Practice between 1987 and 2001, before and after publication of Guidelines.
Methods: Data were collected in 96 general practices in 1987 (First Dutch National Survey of General Practice; practice population n = 344,449 patients) and in 90 general practices in 2001 (Second Dutch National Survey of General Practice; practice population n = 358,008 patients). Outcome measures: (1) percentage of contacts for AOM, common cold, sinusitis and acute tonsillitis in which an antibiotic was prescribed (= antibiotic prescription rate); (2) number of antibiotic prescriptions per 1000 patients per year; (3) incidence rates of urti's per 1000 patients per year.
Results: Antibiotic prescribing rates in AOM and common cold were increased in 2001 compared to 1987 (from 27% to 48% and from 17% to 23% respectively), while the rates for sinusitis and tonsillitis were the same. The number of antibiotic prescriptions per 1000 patients decreased except for AOM. Incidence rates of all upper rti's were lower in 2001 as compared to 1987.
Conclusion: Antibiotic prescribing rates have not declined several years after publication of urti-guidelines. The total volume of antibiotic prescriptions per 1000 patients/per year for common cold, sinusitis and tonsillitis has decreased mainly because of a reduction of incidences. The question arises whether patients’ reduced inclination to present illness to their GPs is an indirect consequence of a more selective use of antibiotics by their GPs or a concurrent trend among patients in community. Long term trends studies in antibiotic prescribing rates should include information about incidences in outcome measurement.
O57: Trends in penicillin-resistance rates among pneumococcal carriage strains in children's day-care centres in France: 1999–2004
M. Roussel-Delvallez, C. Laurans, H. Carsenti-Dellamonica, P. Dellamonica, M. Pecking, E. Bonnet, B. Dunais, S. Maurin, C. Pradier (Lille, Nice, Neuilly-sur-Seine, Paris, F)
Objectives: To monitor penicillin resistance trends among nasopharyngeal (NP) carriage strains of S pneumoniae (SP) in children's day-care centres (DCC)in the wake of interventions promoting prudent antibiotic use in France.
Methods: Cross-sectional surveys were conducted on a random sample of children attending DCCs in 2 areas of France, Alpes Maritimes (AM) and Nord (N), in January–March 1999, 2002 and 2004. Penicillin-susceptibility and serotype of SP isolates were tested on NP aspirates. An intervention programme began in AM in October 2000 to reduce unnecessary pediatric ATB prescriptions. A large scale national campaign was launched in 2002. Pneumococcal conjugate vaccine (PCV) is reimbursed since December 2002.
Results: Samples were obtained from 250, 240 and 233 children in N and 298, 294 and 334 in AM in 1999, 2002 and 2004, respectively. In N, SP carriage rates (CR) remained stable from 1999 to 2002 (47% vs 49%, respectively) and decreased between 2002 and 2004 (49% vs 36%, respectively; p < 0.01). In AM, CR remained unchanged (54%, 58% and 51% in 1999, 2002 and 2004, respectively). Among SP carriers, the proportion of PDSP increased in N between 1999 and 2002 (72% vs 85%, respectively; p = 0.01) but remained stable in AM (63% and 64%, respectively). This proportion declined in both areas between 2002 and 2004 (85% vs. 60% in N, p < 10−3, and 64% vs. 43% in AM, p < 10−3, respectively). In 1999, prevalence rates of PDSP among SP carriers were similar in N (72%) and AM (63%). In 2004, this rate was lower in AM (43%) than in N (60%) (p < 0.01). In AM, there was a decrease in proportion of serotypes 23F (31% in 1999, 17% in 2002 and 9% in 2004; p< 10−3), 6B (20% in 2002 vs. 12% in 2004; p = 0.04) and 14 (15% in 2002 vs. 7% in 2004; p = 0.01) and an increase of serotype 6A (6% in 2002 vs. 15% in 2004, p < 0.01). In N, serotype 23F decreased (27% in 2002 vs. 8% in 2004; p < 0.01), and serotype 6A increased (1% in 2002 vs. 14% in 2004; p < 0.01). In 2004, at least 28% of children in N and in 36% in AM had received PCV. SP and PDSP carriage was significantly lower among vaccinees in AM (43% vs. 56% for SP; p = 0.03; and 14% vs 26% for PDSP; p = 0.01) but not in N.
Conclusion: A 30% decrease in proportion of PDSP among SP carriage strains from children attending DCCs has occurred since the implementation of local and national campaigns promoting judicious antibiotic use in France. Serotype distribution has shifted significantly with fewer carriers of PCV strains.
O58: Prospective observational study on the empirical use of antibiotics and on the adjustment of antibiotic therapies in a university hospital
J. Mettler, M. Simcock, P. Sendi, A. Widmer, M. Battegay, U. Flückiger, S. Bassetti (Basel, CH)
Objectives: To study the adequacy of empirical antibiotic therapies and of adjusted antibiotic therapies, as well as the use of microbiological investigations at a Swiss university hospital where no restrictive measures regarding antibiotic use were in place.
Methods: A prospective study was conducted on alternating weeks over an 8 1/2-month period. All patients admitted through the emergency /department who received therapeutic antibiotic therapy (AT) within 24 hours of admission were included. Data on demographic characteristics, diagnoses, comorbidities, SIRS-parameters, microbiological investigations and antibiotic(s) used were prospectively collected. The first AT received by the patient and, if applicable, the adjusted AT were analysed. AT was considered adequate if the spectrum of activity, the dose and the duration of AT were appropriate, according to local recommendations and/or published guidelines.
Results: 2943 admitted patients were evaluated. Of these, 539 (18.3%) received an AT within the first 24 h and were analyzed. Most patients had respiratory tract (169 pts., 31%), urinary tract (109, 20%) and gastrointestinal (88, 16%) infections. 716 microbiological investigations were performed. Blood cultures were taken from 62% of pts. The 2 most frequently isolated pathogenic bacteria were E. coli (12% of pts.) and S. aureus (5%). 431 pts. (80%) received a monotherapy, 108 (20%) a combination therapy for empirical antibiotic therapy (EAT). The 3 most commonly used antibiotics for EAT were amoxicillin/clavulanate (279 pts., 52%), ciprofloxacin (88, 16%) and piperacillin/tazobactam (62, 11%). EAT was inadequate in 121 pts. (22%). 168 of the 539 pts. (31%) received an adjusted antibiotic therapy (AAT). AAT was inadequate in 27% of cases. The main reason for inadequacy of AT was the use of antibiotics with unnecessarily broad spectrums (24% of inadequate EAT and 53% of inadequate AAT). In 27% of pts. with inadequate AAT identified pathogens were resistant to the administered antibiotics, or antibiotics with the same spectrum were unnecessarily combined.
Conclusion: Despite the absence of a restrictive antibiotic policy, the rate of inadequate AT was similar to the rates reported from other institutions. Surprisingly, AAT were more frequently inappropriate than EAT. Interventions aiming at improving antibiotic prescribing should focus on streamlining and adjustment of AT once microbiological results become available.
O59: A simulation model of the cost of treatment failure in patients hospitalised with community-acquired pneumonia in the US
N. Neil, D. Lamm, K. Ogden, L. Noe, L. Peterson, R. Mallick (Highland Park, Evanston, Philadelphia, USA)
Objective: Managing patients hospitalized with community-acquired pneumonia (CAP) in the US is costly, particularly for those failing IV antibiotic therapy. We developed a simulation model to estimate the cost of treatment failure in this population.
Methods: The simulation is based on American Thoracic Society (ATS) treatment guidelines, published literature and expert opinion. The model simulates initial, empiric IV therapy through as many as three subsequent courses of therapy. Patients requiring third-line therapy are assumed to either achieve cure or expire. Base-case analyses include the most common pathogens, resistance patterns and treatment regimens, and consider immune-competent Usual Care, Penicillin-allergic, and PORT Class V subpopulations. The model considers only CAP-related costs. Therapeutic decisions are simulated on the basis of ATS guidelines and prioritized to minimize the use of fluoroquinolones early in treatment, minimize drug cost and maximize drug efficacy. Resource use is estimated from the payer perspective in 2002 US dollars; component costs include diagnostics, antibiotics, monitoring, ICU and non-ICU care, respiratory support and complications. At each line of therapy, our analysis focused on the subsequent costs of only those patients who failed therapy. We varied key parameters in sensitivity analyses.
Results: Each patient failing initial, empiric therapy generated an average of $5,393 in additional care costs before achieving cure or expiring. Average per patient cost of failure at first- and second-line treatment was $6,028 and $6,113, respectively. Our estimates were most sensitive to assumptions about case mix, bed costs and mortality.
Conclusions: Our findings indicate that failing initial, empiric therapy adds $5,393 per patient to the cost of care. On average, patients requiring three lines of antibiotic therapy before achieving therapeutic success cost about $11,830 more to treat than those cured with the initial, empiric regimen.
O60: Antibiotic cycling for control of extended-spectrum beta-lactamases – experience in an Indian intensive care unit
U. Sekar, V. Hemalatha, P. Sireesha, V. Kamat (Chennai, IND)
Objectives: To study the impact of antibiotic cycling on the prevalence of Extended spectrum beta lactamases [ESBL] producing enterobacteriaceae and the MIC levels of third generation cephalosporins [3GC] and beta-lactam inhibitor combination drugs of ESBL isolates.
Methods: A prospective study was done in a multidisciplinary ICU of a tertiary care centre in 2 phases. Phase 1 was before antibiotic cycling [Jan 2003–May 2003] and phase 2 was after antibiotic cycling [Jun 2004–Oct 2004]. The antibiotic cycling included use of quinolones, cefoperazone sulbactam and piperacillin tazobactam with restricted use of ceftazidime and cefotaxime. ESBL production was screened and confirmed by standard NCCLS protocols. MIC of cefotaxime, ceftazidime, cefoperazone sulbactam and piperacillin tazobactam for a total of 60 isolates in both phases was done by agar dilution method according to NCCLS guidelines. The usage of these drugs in grams/100 patient days and the cross-resistance pattern to fluroquinolones and aminoglycosides were determined.
Results: The prevalence of ESBL producing enterobactericeae decreased from 45.01% in phase 1 to 30.7% in phase 2[p < 0.001]. The usage of cefotaxime, ceftazidime, cefoperazone sulbactam and piperacillin tazobactam in grams/100 patient days was 742, 153, 184 and 113 in phase 1 and 620, 28, 256 and 350 in phase 2 respectively. All the isolates both in phase 1 and phase 2 had MIC levels to 3GC above the breakpoints. The percentage of isolates with MIC levels >64 μg/ml of cefotaxime and ceftazidime was 83.3% and 96.6% in phase1 and 56.6% and 80% in phase 2[p < 0.05] respectively. The percentage susceptibility to cefoperazone sulbactam and piperacillin tazobactam in phase 1 was 71.6% and 41.6% which changed to 53.35 and 70% in phase 2 [p < 0.05] respectively. The cross-resistance to quinolones and aminoglycosides was high in both phases.
Conclusion: Antibiotic cycling is an effective method to contain high ESBL prevalence. The period of cycling has to be more than a year for effective control. Strict infection control policies should be adhered to for ESBL eradication.
O61: Impact of an antibiotic restriction policy on antibiotic usage and cost
F. Jover, J. Cuadrado, V. Ortiz de la Tabla, C. Martin, V. Sanchez, M. Gonzalez, T. Aznar (Alicante, E)
Objective: To assess the impact of a programme to evaluate the quality of an antibiotic restriction policy at a University hospital.
Methods: A multidisciplinary antimicrobial management team (AMT) composed by Infectious Diseases (ID), Microbiology and Pharmacy members daily evaluated restricted antibiotic prescriptions. We designed a prospective study with two periods:observational (Oct 1st 2003–March 14th 2004) and interventional (March 15th–Sept 1st 2004). A specific prescription formulary aiming to evaluate the usage of broad spectrum antibiotics was introduced. Revision criteria were according to ID Committee guidelines and the Sanford Guide to Antimicrobial Therapy. Clinical, microbiological and pharmaceutical data were collected from each patient. Antibiotic therapy appropriateness, restricted therapy eligibility and economic outcomes were evaluated. During interventional period, antibiotic recommendation prescriptions were formulated. Statistical analysis with non-parametric tests were performed. A p value of <0.05 was accepted as significant.
Results: 480 patients were evaluated (54.3% observational and 45.7% interventional period). Overall, restricted agents prescribed were ceftazidime (27.9%), imipenem (24.8%), amikacin (14.6%), piperacilin-tazobactam (12.1%), vancomicin (6.5%) and cefepime (5%). Most frequent diagnostic groups were sepsis (40.3%), gastrointestinal (20.4%), respiratory (13.1%), soft-tissue and bone infections (12.9%) and prophylaxis (7.9%). Antibiotic therapy was not indicated in 7.1% of cases and the restricted antibiotherapy was suitable in 29.8%. Comparing both periods of study, we found several statistical significant features: a decrease of usage of ceftazime, amikacin, teicoplanin and piperacilin-tazobactam; however, imipenem and vancomicin usage increased. Adequate prescription of antibiotherapy increased from 81.7% to 96.8%. Restricted antibiotic prescription significantly improved from 58.5% to 86.3%, while concordance to AMT prescription increased from 53.3% to 78.5%. Economic outcomes were significantly reduced comparing both study periods. In the interventional period, recommendations were formulated in 38% of cases, while 70.2% of them were accepted.
Conclusions: The development of prophylactic and therapeutics local guidelines reached by consensus, and the evaluation and interventional policy by an AMT group have significantly improved the quality and economical costs of restricted antibiotic prescription in our hospital.
O62: Appropriateness of IV antibiotic therapy: impact of counselling based on standardised decisional algorithms 72 hours after prescription
O. Manuel, R. Kammerlander, B. Burnand, M. Vansantvoet, T. Swinnen, P. Francioli, G. Zanetti (Lausanne, CH)
Objectives: To estimate the impact of a therapeutic counselling intervention based on a standardized decisional approach aimed at fostering and guiding reassessment of antibiotic therapy 3 days after initial prescription on the appropriateness of IV antibiotic therapy in hospitalised patients.
Methods: Interim analysis of an ongoing prospective crossover cohort study in 2 similar internal medicine wards in a 850-bed university hospital. Predefined, standardized decisional algorithms based on chart review were used in the intervention group to evaluate 5 steps in IV antibiotic therapy: indication, choice of antibiotic, administration route, dose, and duration of therapy. Physicians in charge of included patients received a standardized, itemized evaluation form that included proposals if applicable. The present interim analysis included only patients hospitalised in the first intervention ward during the 6-month period before crossover. We compared appropriateness of IV antibiotic therapy 3 days after prescription during the first and the second trimesters of the intervention.
Results: 109 IV antibiotic therapies were evaluated, 43 in the first trimester and 66 in the second trimester. The proportion of fully appropriate antibiotic therapies was higher during the second trimester: 41/66 (62%) vs. 14/43 (33%, p < 0.01, Fisher exact test). For all specific items of the evaluation there was a trend towards better antibiotics use in the second trimester: appropriate indication (94% vs. 83%, p = 0.10), appropriate antibiotic choice (88% vs. 79%, p = 0.28), and appropriate administration route (80% vs. 63%, p = 0.05). Total antibiotic consumption was higher during the second trimester, however: 352 vs. 299 prescribed daily doses/1,000 patients-days (of which 68% vs. 62% were given by IV route, and 19% vs. 18% were broad-spectrum antibiotics). Since antibiotics were used more appropriately during the second trimester, this higher antibiotic consumption may reflect a higher burden of infection.
Conclusion: Although more definite results are expected after study completion, this interim analysis showed a promising potential of a counselling intervention based on standardized decisional algorithms to improve the use of IV antibiotics.
Hepatitis virus
O64: Hepatitis C virus-specific CD8+ T cell response and their phenotypic characteristics in chronic patients treated with interferon-alpha and ribavirin
J. Caetano, A. Paiva, A. Martinho, B. Pais, C. Valente, F. Regateiro, C. Luxo (Coimbra, P)
Objectives: Hepatitis C virus (HCV) shows a high propensity to establish chronic infection. Interferon-alpha in combination with ribavirin is standard therapy for hepatitis C. However, this treatment is still limited by a high non-response rate. As CD8+ cytotoxic T lymphocytes are thought to play a crucial role in the course of HCV infection, we evaluated the magnitude of HCV-specific CD8+−T cell response during therapy, and its effect on the dynamics of CD8+-T cell subsets: CD45RA+/CCR7+ (naive), CD45RA+/CCR7− (effector), CD45RA−/CCR7+ (central memory) and CD45RA−/CCR7− (memory/effector).
Methods: We studied 5 HLA-A2+ healthy controls and 11 HLA-A2+ patients chronically infected with HCV. Patients were treated with IFN-alpha and ribavirin, during 48 weeks for genotype 1, and 24 weeks for genotypes 2 and 3. Peripheral blood mononuclear cells were collected before treatment, and one, three and six months after the end of treatment. They were analyzed at specific time points by four-colour flow cytometry using HLA-A2 HCV-peptide specific tetramers, together with a panel of phenotypic markers of homing and differentiation: CCR7 and CD45RA, respectively.
Results: Patients infected with HCV displayed an increase in the percentage of HCV-specific CD8+T cells, when compared with healthy controls. Our results pointed to a more pronounced increase of HCV-specific CD8+T cells in patients who responded to treatment. The phenotypic pattern of the CD8+T-cell subsets studied was altered in therapy responders, when compared with healthy controls. The more significant differences were a decrease in the percentage of CD45RA+/CCR7− cells and an increase in CD45RA+/CCR7+ cells in therapy responders. In contrast, non-responder patients seemed to present a similar pattern for all CD8+-T cell subsets, as control individuals.
Conclusions: Our results seem to indicate that the success of treatment for hepatitis C is related to a significant increase in HCV-specific CD8+T cells. Moreover, the relative proportions of the CD8+ T cell subsets studied appear to be important for a successful outcome of response. The decrease in CD45RA+/CCR7− subset of HCV-specific CD8+-T cell observed in peripheral blood of responder patients could be explained with their massive recruitment to the liver, which leads to a relative increase in CD45RA+/CCR7+ cells. Further prospective large studies are needed to confirm these observations. Work partially supported by Roche Pharma Portugal.
O65: Treatment of acute C hepatitis in HIV infected patients
S. Audagnotto, F.G. De Rosa, O. Bargiacchi, S. Garazzino, L. Veronese, G. Cariti, G. Di Perri (Turin, I)
Objective: Chronic C hepatitis is an important cause of morbidity and mortality in patients with HIV infection. Although treatment with pegylated interferon (PEG-IFN) and ribavirin has significantly improved the outcome, HCV co-infection remains a major threat for HIV patients. Recent findings suggest that treatment of HCV infection in its acute phase may be very successful, but no data are available on acute infection in HIV-positive patients. We report four HIV-positive patients with acute C hepatitis treated with PEG-IFN alpha-2b for 12 weeks.
Methods: Inclusion criteria were documented seroconversion, positive HCV-RNA and elevated ALT levels with a known risk factor in the preceding 6 month in patients with HIV infection, naïve for antiretroviral therapy, with the CD4 cell count >400/mm3. Patients received PEG-IFN alpha-2b ranging from 1.1 to 1.5 μg/Kg once weekly for 12 weeks. ALT, CD4 cell count, HCV-RNA and HIV-RNA measurements were made at week 0, 1, 2, 3, 4, 8, 12, and 24 weeks after the end of treatment. The primary endpoint was the sustained viral response (SVR). Monitoring of critical HIV immuno-virological parameters was also performed.
Results: Two patients had HCV genotype 1. Risk factors for HIV and HCV transmission were intravenous drug use (50%) and sexual exposure (50%). At baseline, median HCV-RNA level was 1.478.000 copies/mL (range: 3.200–7.600.000); the median HIV-RNA level was 50.000 copies/mL (range: 20.000–2.600.000). Treatment was given within 120 days (range: 30–120) of the ALT level peak. At week 4 HCV-RNA was undetectable in all patients but one, who never had a negative HCV-RNA. SVR was achieved in three patients. The non responder patient received a lower interferon dosage. At week 1 there was a mean decrease of HIV-RNA of 0.6 log10, which did not change until the end of therapy. No significant decrease of CD4 cell count was observed.
Conclusions: Treatment with PEG-IFN administered for 12 weeks is effective, well tolerated and is not associated with any significant change of HIV infection parameters. As also seen in other settings, higher PEG-IFN dosage may be associated with SVR. According to recent studies the treatment of acute C hepatitis can provide a unique opportunity for a sustained control of HCV infection in HIV patients.
O66: High diversity in the interferon sensitivity determining region of HCV genome in HCV/HIV-coinfected patients
A. Peña, N. Martinez, J. Casado, J. Parra-Ruiz, B. Valero, F. Lozano, P. Muñoz de Rueda, J. Salmerón, J. Hernández-Quero, F. García (Granada, Seville, E)
Background: Mutations in the Interferon Sensitivity Determining Region (ISDR) in the NS5a of HCV genome have been related in some studies with an increased response to Interferon+ribavirin (IFN+RBV) therapy. Little information on PegIFN plus RBV therapy has been developed and, to our knowledge, none on HCV/HIV-coinfected patients undergoing combination therapy.
Aim: To investigate the differences between HCV/HIV-coinfected and HCV-monoinfected patients in terms of ISDR variability and its predictability over response to PegIFN plus RBV treatment.
Patients and Methods: ISDR was investigated by means of an in house protocol: RNA was extracted with Quiamp Viral RNA Kit (Quiagen), and subjected to an RT-PCR with ‘ONE STEP RT-PCR System’ (Roche), subsequently, a nested-PCR was performed. Specific primers were used for genotypes 1a, 1b and 3. ISDR sequences were obtained using the Open Gene System (Bayer). The study included 69 patients: 47 were HCV/HIV-coinfected and 22 were HCV-monoinfected. Baseline characteristics were similar amongst groups, except for sex (male 83% in coinfected, against 54% in HIV negative patients) and HCV genotype: for HCV/HIV-coinfected patients, 23 were genotype 3a and 24 were genotype 1 (8 1b and 16 1a). All HCV-monoinfected patients were by genotype 1 (17 1b and 5 1a).
Results: For the genotype 1 population, ISDR mutations were statistically more prevalent for HCV-monoinfected patients than for HIV-coinfected patients: only 2/24 (8%) coinfected patients harboured wild-type viruses while 9/22 (41%) of the monoinfected patients were wild type in the ISDR (p = 0.01). According to ISDR scorage (intermediate: 1-3 mutations; mutant > 3 mutations), no mutant ISDR strains were recorded for the monoinfected group while 2/24 (8%) from the coinfected group were mutant strains (p = 0.02). Sustained viral response (SVR) is available so far for 16 coinfected and for all the monoinfected patients: the number of mutations in the ISDR was statistically related to SVR only in the monoinfected group (p = 0.023). For genotype 3a coinfected patients, ISDR mutations were as follows: 15 wt, 4 intermediate and 4 were mutants; no relationship between ISDR mutations and a SVR was observed for these patients.
Conclusions: ISDR in HCV1a and HCV1b from HIV-coinfected patients shows a higher variability than HCV-monoinfected patients. SVR was associated with higher number of mutations in ISDR region only in HIV negative patients.
O67: Mortality in a cohort of hepatitis C patients
S.E. Ramsay, K.R. Neal on behalf of the Trent Hepatitis C Study Group
Objectives: Hepatitis C infection forms a significant burden of mortality as a result of severe liver disease and liver cancer. The aim of this study was to describe the pattern of mortality in a cohort of hepatitis C patients.
Methods: The cohort comprised of hepatitis C patients of the Trent region of UK and has been followed up since 1991. Subjects were recruited through secondary care referrals such as from general practice clinics, drug and alcohol clinics, and prisons. As of 1st January 2004, information on mortality for 1345 patients was available from death certificates sent by the National Health Service Central Register. Descriptive statistics and survival analysis were used to describe the mortality patterns.
Results: 8.3% of the cohort died during the follow-up period of 13 years. The approximate probability of surviving after 6 years of follow-up was 93% and after 10 years was 89%. The mean survival time was 6.47 years (standard deviation 2.73). The mean age at death was 50.95 years (standard deviation 15.68 years). The causes of death in the cohort were grouped into three categories – HCV related from liver disease, HCV unrelated from other medical problems such as cardiac diseases, and lifestyle factors like drug overdose, suicide and murder. Most subjects (40%) had died from HCV related liver disease while 37% died from unrelated medical causes. 22% of deaths were attributable to lifestyle factors such as injecting drug overdose, suicide and murder. The highest percentage (42%) of death was in the younger age group 36-50 years. Younger subjects (under 50 years) died mostly due to lifestyle related causes while maximum HCV related deaths were in 51–65 year olds (p < 0.001). Deaths unrelated to HCV infection occurred mostly in those over 65 years old.
Conclusions: There are two striking findings of this study on mortality in a highly representative sample of HCV patients. Firstly, majority of deaths occurred in the 36–50 years age group
and not in older subjects. Secondly, many young people died as a result of drug overdose and suicide. This higher mortality in younger subjects could be explained by the confounding effect of injecting drug use which was the main route of infection in these subjects. Thus, deaths in HCV patients could thus result not only from liver disease but also from factors related to their lifestyle.
O68: Arthritis associated with chronic hepatitis C virus infection
J.A. Bernal, M.A. Escobar, A.A. Garcia-Egido, F.J. Fernandez, S.P. Romero, D. Garcia-Gil, P. Ruiz, A. Michan, F. Briceño, F. Gomez (Cadiz, E)
Introduction: Arthritis is one of the numerous manifestations of hepatitis C virus infection (HCV).
Objectives: To determine the prevalence of HCV in patients presenting with chronic peripheral inflammatory arthritis (CPIA) and, the clinical forms of CPIAs associated with HCV in a 425 beds teaching hospital reference of the Bay of Cadiz (over 250,000 inhabitants).
Methods: Prospective case-control study in 1687 patients presenting with CPIA as their predominant symptom (excluding cristal induced and degenerative arthritis), mean age (±SD) 47.6 ± 17.3 years, 64% of them women (n = 1080). Control groups: 643 consecutive patients with non-inflammatory chronic arthritis (NICA), and 4315 consecutive first time blood donors (BD) matched for age and sex. HCV status was determined (3rd generation ELISA confirmation by RT-PCR, and HCV genotype).
Results: The prevalence of HCV antibodies (5.6%) in patients with CPIA was higher than that in patients with NICA (2.6%) or BD (0.88%) (p < 0.01 in both cases). The prevalence of chronic HCV infection was higher in patients with CPIA (4.3%) than in BD (0.88%). The prevalence of chronic HCV infection by final diagnosis as compared to BD was: 3.1% for Rheumatoid arthritis (RA) (p < 0.01), 6.4% for seronegative RA (p < 0.005), 11.9% for intermitent mono-oligoarthritis (p < 0.001), 6.0% for Sjögren's syndrome(p < 0.005), and 9.8% for systemic lupus erythematosus (p < 0.001). The prevalence of chronic HCV infection in psoriasic arthritis, seronegative spondyloarthropathies, and other final diagnosis was not different than that in BD. CPIA associated to HCV infection was non erosive/non deforming in 76% of the patients. Type II cryoglobulins and, decreased levels of C4/C3 were detected in 37% and 48%/22% of the patients with CPIA associated to HCV infection, respectively.
Conclusions: An increased prevalence of HCV infection exists in patients presenting with chronic peripheral inflammatory arthritis. HCV antibodies (3rd generation ELISA) overestimates the prevalence of HCV infection in those patients. A search for HCV infection should be performed in the diagnostic process of both inflammatory arthritis and collagen vascular diseases.
O69: A LightCycler Real Time PCR protocol for accurate quantification of HCV viraemia followed by sequencing of different genotypes
L. Tagliaferro, P. Menegazzi, M.A. De Donno, J.L. McDermott, O.E. Varnier (Lecce, Genoa, I)
Objectives: The main objectives of this project were the development of a rapid LightCycler Real Time PCR (RTiPCR) protocol for accurate quantification of HCV viraemia, its use in the testing of a large number of clinical samples and its cost-effective integration in the genotyping protocol. Methods: Serial ten-fold dilutions of two HCV RNA positive controls (Accurun, BBI), 170,000 and 910,000 IU/ml, respectively, were amplified and the data from the resulting calibration curve were stored in the LightCycler database for the quantification of plasma HCV RNA. Clinical samples were tested in a rapid single-tube RTiPCR reaction and cost-effective HCV RNA quantification was determined using one reference standard during each assay. The quantification obtained for the single reference standard was validated in a comparative analysis with the stored calibration curve followed by interpolation of the amount of HCV RNA in the clinical samples. HCV sequencing was directly performed using 10 μl of purified real time PCR amplicons.
Results: A total of 2,470 plasma samples were tested from Oct 2002 to Sept 2004. HCV RNA was quantified in 1,226 samples with a dynamic range of 57 to 2.5 × 10.9 IU/ml and the theoretical threshold was 53 IU/ml. The standard deviation (SD) and the coefficient of variation (CV) of the HCV RNA levels were 1.08 and 3.55% for the 170,000 IU/ml standard and 1.34 and 4.78% for the 910,000 IU/ml standard. In 266 samples the amplicons were purified and sequenced for HCV genotyping (Bayer Diagnostics). Thirty five different HCV strains were typed: the majority were genotype 1b (36%) and 2 (30%), but genotypes 4 and 5 were also identified.
Conclusions: Our study shows that this HCV RTiPCR protocol, which has been used for 2 years to test over 2,000 samples with minimal SD and CV values, allows accurate quantitation of HCV RNA in clinical samples. The characteristics of rapidity and accuracy have been extended to include cost-effectiveness due to subsequent use of the amplicons for sequencing.
O70: Revaccination of non-responder infants born from HBsAg positive mothers
M.R. Hasanjani Roushan, Y. Zahed Pasha, R. Saghebi, F. Kohi (Babol, IR)
Objectives: Infants born from HBsAg positive mothers who are not responding to primary vaccination schedule are likely to develop HBV infection. The purpose of this study was to evaluate anti-HBs response following administration of two doses of hepatitis B vaccine in this group of infants.
Methods: From April 1998 to September 2004, Thirty-four non-responder infants born from HBsAg positive mothers received two additional doses of hepatitis B vaccine one month apart at 15 months of age. Anti-HBs levels in these infants were evaluated two months after the later dose.
Results: Eighteen girls and 16 boys were evaluated in this study. The mothers of 4 infants (11.8%) were HBe Ag positive and in 30 infants (88.2%) were HBe Ag negative. HBs Ab production was seen in 32 (94%) cases of vaccine recipients (96.6%infants of anti HBe Ag positive and 75%infants of HBe Ag positive mothers) (p = 0.225). Mean HBsAb level in girls and boys was 232 and 215 IU/L, respectively (p = 0.142).
Conclusion: With administration of additional two doses of hepatitis B vaccine, protective levels of anti-HBs developed in 94% of non-responder infants.
O71: Vaccination against hepatitis B in patients with chronic renal failure – 16 year follow-up
L. Roznovsky, I. Orsagova, A. Kloudova, I. Lochman, L. Kabieszova (Ostrava, CZ)
Objectives: Hepatitis B virus infection is an important cause of liver disease among patients with chronic renal failure. The vaccination against hepatitis B can considerably decrease number of these infections. The vaccination against hepatitis B was performed in 769 patients with chronic renal failure from 4 dialysis units. Anti-HBs antibodies response after immunisation and breakthrough infections were investigated in these patients.
Methods: Active immunisation against hepatitis B was commenced in 1988. The number of immunised patients gradually increased and the group included 769 patients in November 2004. Of these patients, 328 died during investigation. The vaccination schedule was 0, 1, 6 months for pre-dialysis patients and 0, 1, 2 months for dialysis patients and patients with renal transplantation. Plasma-derived or since 1990 recombinant vaccines were administered intramuscularly, each vaccine contained 40 μg of HBsAg, but for pre-dialysis patients only 20 μg till 1998. The immunisation schedules were completed in 622 patients. Blood samples were obtained 6 weeks after third or next dose of vaccine and biannual thereafter. Samples were tested by ELISA for HBsAg, anti-HBs and anti-HBc. The patients without protective anti-HBs level after basic vaccination were once or twice re-vaccinated. The patients with vanishing of anti-HBs antibodies were also re-vaccinated.
Results: Anti-HBs antibodies after vaccination were investigated in 488 patients. Protective anti-HBs levels were proved in 241 of 488 patients (47%) after basic immunisation and in 309 (63%) or 347 (71%) patients after fourth or fifth dose of vaccine. The new HBsAg positive status was proved in 28 dialysis patients, most of them suffered from acute hepatitis B. These breakthrough infections were more frequent after initiation of vaccination programme, 27 of them in period 1988–1994, the latest breakthrough infection was proved in 2000. Asymptomatic infections with new appearance of anti-HBc antibodies were observed in 11 patients. Anamnestic response (double or higher increase of anti-HBs without revaccination) was observed in 42 patients.
Conclusion: Vaccination against hepatitis B in 769 patients with chronic renal failure was not quite satisfactory. Only 71% of them developed protective anti-HBs level after 5 doses of vaccine, but long-term vaccination considerably reduced hepatitis B incidence in our patients.
From mild to severe respiratory tract infection: what's new with azalides? (Symposium arranged by PLIVA)
S79: Single-dose treatment of respiratory tract infections
G.W. Amsden (Cooperstown, USA)
Several pharmacokinetic studies have demonstrated that when the same total dose of azithromycin is administered over shorter regimens a patient's exposure to azithromycin is actually higher than if the dose was administered over a longer period of time. As such, even though the 1.5 g regimen has been marketed as both a 5-day and 3-day course patients actually have a higher exposure to azithromycin when it is taken over 3 days. If administered as a single 1.5 g dose, patient exposure to azithromycin is even higher; exceeding that experienced with either the 3- or 5-day regimens. Not only would single dose administration of azithromycin potentially lead to more favorable outcomes due to higher systemic exposures but it also has the potential to achieve as close to perfect patient compliance as is possible. Single-dose azithromycin was approved for the treatment of childhood otitis media in 2003 after studies demonstrated equal safety and efficacy versus standard comparators such as amoxicillin/clavulanate and ceftriaxone. In these studies, single-dose azithromycin was found to be associated with significantly higher compliance (vs amoxicillin/clavulanate) and to have a clinical cure rate higher than if the same azithromycin dose was split over 3 days or compared to ceftriaxone. When the same concept has been applied to adults with community-acquired pneumonia, two studies to date have demonstrated equivalent safety and efficacy of a single 1.5 g dose vs the dose spread over 3-days or a comparable comparator such as 10 days of clarithromycin. The single-dose has also been shown to be efficacious in a small study of adults with uncomplicated tonsillitis. Based on these results, it appears that administering single oral doses of azithromycin is a safe and effective option for a variety of adult and pediatric respiratory tract infections, though further study of the concept is warranted. Expansion of these studies to the use of single intravenous azithromycin doses for the treatment of hospitalised patients with community-acquired respiratory infections should also be considered.
S80: Treatment of CAP in ICU – an intensivist perspective
B. Baršic (Zagreb, HR)
Severe pneumonia treated in intensive care units (ICU) represents a great therapeutic challenge. Usual defervescence of fever does not occur as in other patients, particularly not in mechanically ventilated patients. We evaluated 30 consecutive patients with community acquired pneumonia admitted in the ICU. Initial therapy was azithromycin intravenously for seven days plus beta-lactams (ceftriaxon or penicillin). Switch to oral treatment was possible after defervescence of fever. Treatment was finished as planned in 25 patients. In five patients it was stopped because of early therapeutic failure, isolation of resistant pathogens or adverse drug event. However, in 10/25 patients which completed planned treatment additional antibiotics were added despite improvement of pneumonia because of suspected or confirmed nosocomial infection. Treatment beta-lactams plus azithromycin was successful in 21 patients. Analysis of duration of fever in survivors showed that only in one patient defervescence of fever occurred after three days of treatment. Our results suggest that randomized clinical studies do not show exact clinical efficacy of antibiotics, as observational studies do, due to the selection of patients, even with severe pneumonia. Evaluation of treatment effect should be based more on meticulous estimation of respiratory function than on parameters representing systemic inflammatory response or x-ray findings.
S81: PK/PD modelling of antibiotics: the way of maximising clinical outcome
I. Francetic (Zagreb, HR)
Optimal dosing of antibiotics depends on pharmacokinetic and pharmacodynamic features of antimicrobials. Better understanding of pathophysiology of infection has brought up interest in pharmacokinetics of antimicrobials and relationship between PK and clinical outcome. As opposed to previous standpoint today antimicrobials are divided in two different cathegories, namely, concentrations dependent and time dependent killing. However, this division into two groups seems not to apply in total since certain groups of antimicrobials such as azithromycin, tetracyclines are somewhere in between. Time over the minimal inhibitory concentration with azithromycin and doxycycline has to be disregarded or minimized since the persistent effects are better represented by AUC24/MIC. This is especially relevant for intracellular microorganisms. Cellular pharmacokinetics of azithromycin makes the time over the MIC irrelevant since accumulation of the azithromycin intracellulary provides concentration well above MIC for period much longer than 24 hours. However, this is not the case with other macrolides. In defining relationship between PK and outcome one has to take into account the type of infection. In infections caused by intracellular microorganisms cellular PK of antimicrobial is essential, while in blood stream infections extracellular PK is important and defines the outcome of infection providing that activity against the causative agent is present. However, increasing the dosing of azithromycin is likely to enhance the microbiologic outcome especially in infections like acute otitis media (OAM) caused by extracellular microorganisms such as non-typeable Haemophylus influenzae (NTHI). Results from in vivo infection models and clinical trials indicate that for azithromycin 24 hour AUC/MIC ratio of 25 is associated with treatment efficacy.
S82: Additional benefits of macrolides in the treatment of community-acquired pneumonia
T.M. File (Rootstown, USA)
CAP is a common disorder that is potentially life threatening. Optimal management of these infections requires appropriate use of antimicrobials. Decisions concerning proper antimicrobial therapy are guided by several considerations such as spectrum of activity, pharmacokinetics (PK), efficacy in clinical trials, safety profile, and cost effectiveness. Because the azithromycin is active against the key pathogens of CAP, it is particularly useful to treat patients-either as monotherapy for mild infections or as part of combination therapy with a beta-lactam for serious infections. While numerous randomized clinical trials have documented the efficacy of azithromycin for the treatment of CAP from the standpoint of clinical and bacteriological endpoints, studies have also demonstrated ‘other’ benefits of this antimicrobial. Such benefits include: shorter dosing duration; excellent safety profile; decreased length of stay in the hospital; and cost-effectiveness. The unique PK properties of azithromycin, which include prolonged T1/2 and excellent respiratory tract penetration, allow for the reduced dosing regimens. This has several advantages that include better compliance, reduced adverse events, quicker change from IV to po therapy in hospitalized patients, and reduced costs. Several studies have demonstrated an advantage of azithromycin, when used as monotherapy in selected patients, as compared to other antimicrobials concerning the length of stay within the hospital. In a pharmacoeconomic study, Paladino et al. found that azithromycin was more cost-effective as empiric therapy for low-risk patients hospitalized with CAP compared to cefuroxime with or without erythromycin. In addition, several studies have found that use of a macrolide, such as azithromycin, which is part of an initial combination therapy for patients hospitalised with CAP is associated with decreased mortality or shorter hospital stay than with a cephalosporin alone. The specific aetiology of infection was not determined in these studies, however it is possible that the added coverage for ‘atypical’ pathogens may in part explain this observation. Additional retrospective studies suggest the benefit of this combination therapy applies not only to CAP in general but also to CAP specifically associated with S. pneumoniae bacteraemia. The possible coexistence of atypical pathogens or the immunomodulating effect of the macrolides may in part be responsible for this finding.
Emerging viral infections
O88: In vitro studies on interferon-inducing capacity and sensitivity to IFN of human severe acute respiratory syndrome coronavirus
C. Scagnolari, G. De Vito, F. Bellomi, E. Riva, G. Cappiello, A. Spanò, M. Clementi, F. Dianzani, G. Antonelli (Rome, Milan, I)
Objectives: No fully effective antiviral treatment are currently available against severe acute respiratory syndrome coronavirus (SCOV) infection. In this study, we investigated whether interferons (IFNs), used alone and in combination, exhibit in vitro anti-SCOV activity. In parallel experiments we examined the capacity of SCOV to induce human IFN alpha from peripheral blood mononuclear cells (PBMC) of healthy donors.
Methods: Anti-SCOV (Hsr1 strain) or anti-EMC/VSV/NDV activities of IFN alpha, beta and gamma were determined by using CPE inhibition test in epithelial kidney monkey Vero cell culture. Synergistic, additive or antagonistic interactions between IFNs were evaluated using the combination index analysis method developed by Chou & Talalay. Analysis of transcript levels for a series of IFN alpha (1, 2, 5, 6, 8, 10, 13, 17, 21) genes were determined by Real Time PCR. Antiviral activity of IFN secreted from PBMCs after incubation of SCOV were determined by an EMC assay performed in A549 cell line.
Results: All the tested IFNs showed anti-SARS virus activities on Vero cell culture but at different extent. Specifically the results showed that, compared to EMC/VSV/NDV, SCOV grown in Vero cell can be only moderately inhibited by pretreatment with IFN beta. IFN alpha and above all IFN gamma, by contrast, were less effective. We have however found that IFN gamma synergizes with the innate IFNs (IFN alpha and beta) to potently inhibit SCOV replication in vitro. Interestingly incubation of PBMCs with SCOV leads to early and strong IFN alpha mRNA synthesis. IFNs secreted from PBMCs after SCOV stimulation possesses antiviral activity in vitro.
Conclusions: The data document the synergistic antiviral activity of innate IFNs and IFN gamma to an extent that may be compatible with clinical use for SARS prevention and therapy. Moreover since IFNs are normally produced in the first phase of viral infections, it could be important to understand whether and to what extent the relative low sensitivity of SCOV to IFNs associated to its ability to induce the production of IFN alpha may have any relevance in determining the course of infection.
O89: A novel coronavirus, HKU1, from patients with pneumonia
P.C.Y. Woo, S.K.P. Lau, C.-M. Chu, K.-H. Chan, H.-W. Tsoi, Y. Huang, B.H.L. Wong, R.W.S. Poon, J.J. Cai, W.-K. Luk, L.L.M. Poon, Y. Guan, S.S.Y. Wong, J.S.M. Peiris, K.-Y. Yuen (Hong Kong, HK)
Objectives: To characterize and analyze the complete genome of a novel coronavirus, coronavirus HKU1 (CoV-HKU1), from patients with pneumonia.
Methods: We amplified a 440-bp fragment of the RNA-dependent RNA polymerase (pol)gene of coronaviruses by RT-PCR, using coronavirus conserved primers, from RNA extracted from the nasopharyngeal aspirate (NPA) of a 71-year old Chinese man with pneumonia. The complete genome of the coronavirus (CoV-HKU1) was amplified and sequenced using RNA extracted from the NPA as template and degenerate primers designed by multiple alignment of the genomes of other group 2 coronaviruses. Real-time quantitative RT-PCR was performed to quantify the amount of virus in the NPA obtained in the first to the fifth week of the illness. Specific antibody was detected by Western blot assay and ELISA using recombinant nucleocapsid of CoV-HKU1. Screening for CoVHKU1 on NPA obtained during the SARS period was carried out by RT-PCR.
Results: RT-PCR and sequencing of the 440-bp fragment of the pol gene showed that there were 89–91% amino acid identity between the sequence of the fragment and those of other group 2 coronaviruses. The genome of CoV-HKU1 is a 29926-nucleotide, polyadenylated RNA. The G + C content is 32%, the lowest among all known coronaviruses with available genome sequence. Phylogenetic analysis reveals that CoVHKU1 is a new group 2 coronavirus. Quantitative RT-PCR showed that the amount of CoV-HKU1 RNA were 8.5 to 9.6 × 106 copies per ml in his NPA during the first week of the illness and dropped progressively to undetectable levels in subsequent weeks. He developed increasing serum levels of specific antibodies against the recombinant nucleocapsid protein of CoV-HKU1 with IgM titres of 1:20, 1:40 and 1:80 and IgG titres of <1:1000, 1:2000 and 1:8000 in the first, second and fourth weeks of the illness respectively. Cultural, antigenic, RNA, or serological detection of other microbial pathogens were negative. Screening of 400 NPA collected during the SARS period identified the presence of CoV-HKU1 RNA in one specimen, with a viral load of 1.13 × 106 copies per ml, from a 35-year old woman with pneumonia.
Conclusion: Our data support the existence of a novel group 2 coronavirus in the NPA of patients with pneumonia. Resolution of the illness in the index patient was associated with the disappearance of the viral RNA and the development of specific IgG and IgM antibody response against the virus.
O90: Crimean-Congo haemorrhagic fever in the central Anatolian region of Turkey: a report of 92 cases
N. Elaldi, M. Bakir, I. Dokmetas, M. Sencan (Sivas, TR)
Objectives: Crimean-Congo haemorrhagic fever virus (CCHFV) belongs to the genus Nairovirus in the Bunyaviridae family and causes a potentially fatal disease, Crimean-Congo haemorrhagic fever (CCHF) is characterised by hemorrhage and fever. Previously, CCHF cases have been reported in Turkey. An outbreak of CCHF occurred in the Central Anatolian region of Turkey during April and October 2004. We report herein 92 cases who diagnosed as CCHF during the outbreak.
Methods: Patients with acute febrile syndrome characterized by malaise, bleeding, leukopenia, and thrombocytopenia were admitted to our hospital (Cumhuriyet University Hospital, an 800-bed teaching hospital in Sivas city, located in the Central Anatolian region of Turkey) during the spring and summer of 2004. Patients who had IgM antibodies or polymerase chain reaction (PCR) results positive for CCHFV in serum samples were included. Obtained serum samples from all patients both acute- and convalescent-phase of the illness were sent to the World Health Organisation (WHO) reference laboratories in Lyon, France, and London, England to test for the presence of CCHF virus.
Results: Ninety-two patients had immunoglobulin M antibodies and/or PCR results positive for CCHFV in serum samples during the outbreak. Forty-three (47%) were female and 49 (53%) were male. The mean age was 45.7 ± 2.2 (range 5–92 years). Malaise (94%), fever (91%) and muscle ache (90%) were the most common presenting symptoms, rash (57%) and conjunctival injection (50%) were the most common initial clinical findings among the patients. Forty-two per cent of patients had history of tick bite, and 80% of handling livestock. Complete blood counts at admittance showed thrombocytopenia in all patients leukopenia in 69 (75%), anaemia in 11 (12%) of 92 patients. Elevated serum aspartate aminotransferase (AST) levels were determined in 84 (91.3%), alanine aminotransferase (ALT) in 73 (79%), and lactate dehydrogenase (LDH) in 91 (98.9%) of 92 patients. Eighty-seven (95%) patients were treated with oral ribavirin. Six patients, died during the outbreak, 3 of them died because of bleeding. The overall mortality was 6.5%.
Conclusion: Herein we report an outbreak of CCHF in the central Anatolian of Turkey. Our CCHF cases had lower mortality rate. It could be explained by early defining of the disease during the outbreak, supportive therapy and ribavirin treatment.
O91: Complete L segment coding-region sequence determination of a Russian Crimean-Congo haemorrhagic fever virus
J. Meissner, S. Seregin, N. Yakimenko, O. Vyshemirskii, S. Netesov, V. Petrov (New Mexico, USA; Koltsovo, RUS)
Crimean-Congo haemorrhagic fever virus is the type species of the genus Nairovirus, family Bunyaviridae. CCHF virus is a spherical, enveloped virus with a single-stranded, tripartite RNA genome of negative polarity.
Objectives: The goal of this work was to establish L segment sequences of CCHF virus laboratory isolates representative of strains circulating in European Russia and Asia, and to compare these sequences with partial or full-length CCHF virus L segment sequences from Nigeria, Pakistan, and Iraq.
Materials and methods: Two laboratory-adapted CCHF virus strains were used in this work. After total RNA extraction using the RNeasy MiniKit (QIAGENE, Germany) RT-PCR was performed using the Access RT-PCR kit (-Dromega, USA). The goal of primer selection and design was to produce overlapping amplicons of 350–700 nucleotides spanning the entire L segment. Fragments were purified from 1% agarose gel using the Q-Biogene GeneClean extraction kit and directly sequenced using CEQ 2000 DTCS kit run on the CEQ 2000XL DNA Analysis System.
Results: The large (L) segment CCHF virus strain ASTR/TI30908 was amplified and sequenced. After removal of the 5′ and 3′ primer-generated ends, this L segment sequence is 12112 nucleotides long, and is 97% identical at the translated amino acid level to partial or full-length CCHF virus L segment sequences currently published or available in GenBank A complete L segment coding-region sequence for CCHF virus strain TADJ/HU8966 was also determined. The 30908 RdRp ORF shares 90% nt identity with IbAr10200 and 87% nt identity with Matin. In RdRp ORF we identified a variable region, approximately 50-aa, corresponding to nt positions 2346-2513 in 30908, which is flanked by well-conserved regions.
Discussion: This variable region serves a very useful practical purpose for both diagnostics and phylogenetic analysis, in that the flanking conserved regions could be used for to design amplification primers useful for any CCHF virus, while the internal variable region sequence, provided it is variable enough, can be used for classification and molecular epidemiology.
O92: Analysis of the mortality among the patients with Crimean Congo haemorrhagic fever virus infection
A. Celikbas, Ö. Ergonul, N. Baykam, S. Eren, H. Esener, B. Dokuzoguz (Ankara, TR)
Objective: To determine the causes and predictors of mortality among Crimean Congo Haemorrhagic Fever (CCHF) virus infected patients.
Method: Fifty-four patients with Crimean-Congo haemorrhagic fever (CCHF) were analysed for the causes of mortality. Forty-one patients had positive results of IgM, and/or IgG, and/or PCR results for CCHF virus in blood or tissue. Thirteen patients are highly suspected cases, and their confirmation is pending.
Results: Fifty-four patients were included, and 4 died. The overall case fatality rate (CFR) was 7.4%. Forty-eight per cent of the patients were male. The age, gender, and days from symptoms to admission were similar between survived and died patients (p > 0.05). Among the clinical findings, hematemesis (p = 0.009), melena (p = 0.001), and somnolence (p = 0.022) were significantly more common among died patients. The rate of the other symptoms and signs such as nausea-vomiting, diarrhoea, and maculopapular rash were similar in both groups. Among died cases, the median platelet count was significantly lower (10 600/ml versus 20 000/ml, p = 0.038), mean prothrombin time (27 sec vs 16 sec, p = 0.002), and mean activated partial thromboplastin time were longer (73 sec vs 44 sec, p < 0.001), and the mean ALT (1125 vs 331, p ≤ 0.001), and mean AST (3118 vs 913, p = 0.004) were higher. Serum IgM and IgG positivity against CCHF virus was detected in 33% and 0% of died cases, whereas 93% and 68% of survived cases, respectively. PCR positivity was detected in 100% of died cases. Twenty-five patients (46%) were intended to be given per oral ribavirin, but 3 among these couldn't get the drug because of gastrointestinal bleeding and somnolence. These three patients and the one who did not get ribavirin died.
Conclusion: The lack of antibody production against CCHF virus infection was observed as a strong indicator of mortality. Gastrointestinal bleeding and somnolence could be the reason for the ineffectiveness of oral ribavirin. Intravenous ribavirin should be given to the severe cases.
Advances in febrile neutropenia
O93: Influence of Mannan binding lectin serum levels on the risk of infection during chemotherapy-induced neutropenia in adult haematological cancer patients
M. Vekemans, A. Georgala, C. Heymans, F. Muanza, M. Paesmans, J. Klastersky, M. Barette, N. Meuleman, F. Huet, O.J. Robinson, O. Marchetti, T. Calandra, S. Costantini, A. Ferrant, K. Petersen, M. Axelsen, M. Aoun (Brussels, B; Lausanne, CH; Copenhagen, DK)
Background: Mannan Binding Lectin (MBL) is a C-type serum lectin produced by the liver and involved in innate immune response. Low level serum MBL concentration constitutes a risk factor for infection in pts receiving myelo-suppressive chemotherapy. Substitutive therapy methods are under development and will be tested in the future.
Methods: We conducted a prospective observational study focusing on assessment of MBL as a risk factor for infection. All pts with haematological malignancy hospitalized for administration of at least one chemotherapy cycle, between December 2001 through December 2003 were eligible for the study. Serum MBL concentration was measured by a Time Resolved Immune Fluoro-Metric Assay method. Deficiency was defined using serum MBL levels or MBL genotypes according to a pre-defined algorithm. Outcomes considered included the occurrence of febrile (N), severe infection (sepsis, pneumonia, bacteraemia or invasive fungal infection), bacteraemia, and the time to first development of one of these outcomes, from enrollment and across the cumulative cycles for each patient. We used logistic regression models for analyzing binary outcomes (and Fisher exact tests); Kaplan-Meier estimates and logrank tests for analyzing time to event variables
Results: 255 pts who received 569 cycles of chemotherapy were analyzed with a median number of received chemotherapy cycles of 1. Median number of days of (N) per cycle was 7 days (inter-quartile range 0–13).62 pts (24%) were considered as MBL deficient. 200 pts developed, at least once, febrile (N). No difference in the occurrence of febrile (N) per cycle or per pt between deficient and non deficient pts was observed. On pt-based analysis, there was a rate of severe infections in MBL deficient pts (1.96 per 100 days versus 1.34 per 100 days, p = 0.008) on the overall group of pts; this impact was even increased on the subgroup obtained by excluding acute leukaemic pts. On cycle-based analysis, MBL deficiency was associated with a trend to a higher rate of severe infection (13/72 (18%) vs 20/194 (10%); OR 1.92 [95%CI 0.90−4.09]; p = 0.09), excluding pts with acute leukemia's and BMT pts. On that subgroup, MBL deficiency was also associated with a greater rate of bacteraemia (14% versus 5%, p = 0.01).
Conclusion: These results show that MBL deficiency is associated with earlier and more severe infections in adult haematological cancer pts with chemotherapy-induced(N). The association was strengthened when acute leukaemic pts were excluded from the analysis
O94: Resurgent Gram-negative infections are not associated with increased morbidity and mortality in high-risk neutropenic inpatients with haematological malignancies not receiving fluoroquinolone prophylaxis
O.J. Robinson, T. Calandra, F. Bally, O. Marchetti (Lausanne, CH)
Background: Since the late 1980s, fluoroquinolone (FQ) prophylaxis is often used to reduce the incidence of G- infections in neutropenic cancer patients. However, while it is unclear whether it reduces morbidity and mortality, FQ prophylaxis has been associated with the emergence of FQ-resistant G-. Therefore this preventive measure was promptly discontinued in our hospital. Yet, investigators have argued about the appropriateness of stopping prophylaxis in light of recent reports of high mortality of G- infection among patients not receiving FQ (ICAAC 2004 Abstract K-1436).
Objectives: To assess the morbidity and mortality of G- infections in high-risk neutropenic inpatients with haematological malignancies not receiving FQ prophylaxis.
Methods: Prospective observational study of all consecutive adult neutropenic inpatients undergoing intensive chemotherapy +/− autologous stem cell transplantation for haematological malignancies between April 2002 and August 2003. Patient management according to IDSA guidelines (Hughes, CID, 2002). Febrile episodes (FE) were classified as microbiologically (MDI) or clinically (CDI) documented infections and fever of unknown origin (FUO) (ICHS, JID, 1990). Severe sepsis/septic shock were defined according to ACCP-SCCM (Bone, Chest, 1992).
Results: 208 FE occurred during 134 episodes of neutropenia in 96 patients with acute leukemia (53), lymphoma (20), and myeloma (23). Median days of neutropenia: 16 (3–114). MDI with and w/o bacteraemia occurred in 49 (24%) and in 20 (9%), respectively, CDI in 74 (36%), and FUO in 65 (31%) of the FE. Among 56 bacterial bloodstream isolates, 29 (52%) were G- (E.coli 10, Klebsiella 9, Pseudomonas 1, other 9) and 27 (48%) G+ (CNS 14, streptococci 7, other 6). Empirical antibacterial treatment was appropriate according to susceptibility testing in 26/29 (90%) G- (3 E. coli ESBL) and in 17/27 (63%) G+. Severe sepsis occurred in 5 /208 (2%) FE (1 E.coli ESBL bacteraemia, 3 CDI, 1 FUO), and septic shock was not observed. Overall in-hospital mortality in the entire study population was 0%.
Conclusion: Gram-negative bacteria accounted for 50% of bloodstream infections in high-risk febrile neutropenic patients not receiving fluoroquinolone prophylaxis. However Gram-negative infections were associated with low morbidity and zero mortality arguing against the need for prophylaxis in high-risk hospitalized patients with haematological malignancies.
O95: Haematological malignancies and bacteraemia. The impact of malignancy type and microbial agent on 30-day mortality
M. Nørgaard, H. Larsson, G. Pedersen, H.C. Schønheyder, H.T. Sørensen (Aalborg, Århus, DK)
Objectives: To examine the variation in mortality of bacteraemia in patients with different haematological malignancies and examine the prognostic impact of the different types of bacteraemia.
Methods: We conducted a population-based cohort study and included all patients >14 years living in North Jutland County, Denmark with a new diagnosis of a haematological malignancy registered in both the Hospital Discharge Registry and the Danish Cancer Registry from 1992–2002. The patients with bacteraemia were identified in the Bacteremia Research Database. Mortality within 30 days was determined through the Central Population Registry. Cox proportional hazard regression analysis was used to compare mortality rates between the major groups of haematological malignancies using acute myeloid leukemia as reference and between Gram-positive (reference group), Gram-negative, and polymicrobial bacteraemia or fungaemia. We adjusted for age, gender, co-morbidity, calendar time, and whether or not the empiric antibiotic therapy was appropriate.
Results: In total 1666 patients were registered with a new haematological malignancy and 358 (21%) of these had a successive episode of bacteraemia yielding an incidence rate on 96 bacteremias per 1000 person years. Overall 30-days cumulative mortality rate was 0.32 (95% confidence interval (CI): 0.27–0.37). Compared with acute myeloid leukemia the adjusted mortality rate ratios (MRR) for 30 days of follow-up were for Hodgkin's disease 1.3 (95% CI: 0.3–4.2), for multiple myeloma 1.0 (95% CI: 0.5–1.9), and for non-Hodgkin lymphoma or chronic lymphocytic leukemia 0.7 (95% CI: 0.4–1.1). Gram-positive organisms caused 35% and Gram-negative organisms 50% of the bacteremias. Fifteen % were polymicrobial or caused by yeasts. Gram-negative bacteremias did not have a substantially increased risk compared with Gram positive bacteremias (adjusted MRR 1.1 (95% CI: 0.7–1.6)). Adjusted MRR for polymicrobial bacteremias or fungaemias compared with Gram-positive bacteremias was 2.4 (95% CI: 1.3–4.1).
Conclusion: The 30-day mortality of bacteraemia showed little variation according to the underlying type of haematological malignancy. Polymicrobial bacteremias and fungaemias had the poorest prognosis whereas Gram-positive and Gram-negative bacteremias had similar impact on mortality.
O96: Antibiotic prophylaxis of bacterial infections in afebrile neutropenic patients following chemotherapy. Systematic review and meta-analysis
A. Gafter-Gvili, A. Fraser, M. Paul, L. Leibovici (Petah Tikva, IL)
Background: Bacterial infections are major causes of morbidity and mortality among neutropenic cancer patients. Antibiotic prophylaxis has been shown to reduce bacterial infections but not overall mortality, thus current guidelines do not advise its use.
Methods: Systematic compilation of all randomised trials comparing antibiotic prophylaxis vs. no prophylaxis; and different types of prophylaxis. The search included Medline, Embase, The Cochrane Library, conference proceedings and all references. No date, language, age or publication limits were imposed. Data were extracted independently by two reviewers. Meta-analyses were performed for each comparison. Relative risks with 95% confidence intervals were calculated using the fixed effect model.
Results: Comparing prophylaxis to no prophylaxis (51 studies 4379 patients), a highly significant reduction in overall mortality with prophylaxis was found, RR0.67 (0.55–0.81). Prophylaxis also significantly decreased infection-related mortality, RR0.58 (0.45–0.74); the occurrence of fever, RR0.79 (0.75–0.82); clinically documented infections, RR0.64 (0.59–0.71); microbiologically documented infections, RR0.54 (0.49–0.60); and bacteraemia, RR0.52 (0.46–0.59). Development of resistance to intervention drug was significantly more frequent in the intervention arm with trimethoprim-sulfamethoxazole (TMP-SMZ), RR2.42 (1.35–4.36), but not with quinolones, RR1.69 (0.73–3.92). Comparing different types of prophylaxis (44 studies 5023 patients), systemic antibiotics were superior to nonabsorbables, quinolones were superior to TMP-SMZ, and additional antibiotics directed against gram-positive bacteria (GP) did not enhance efficacy of quinolones alone (table). In trials in which quinolones were compared to TMP-SMZ, less resistance developed to quinolones in the quinolone arm than to TMP-SMZ in the TMP-SMZ arm, RR0.45 (0.27–0.74). Quinolone efficacy was not associated with study years. Most trials included adults with haematological malignancies (64 trials were restricted to haematological cancer patients). Nine trials included >80% patients with solid tumors. Prophylaxis was given for up to 6 weeks.
| All cause mortality | Febrile episodes | Clinically documented infections | Adverse events | |||||
|---|---|---|---|---|---|---|---|---|
| Comparison | RR (95 % Cl) | Studies (patients) | RR (95 % Cl) | Studies (patients) | RR (95 % Cl) | Studies (patients) | RR (95 % Cl) | Studies (patients) |
| Quinolones vs. TMP – SMZ | 1.07 (0.66–0.72) | 10 (917) | 0.95 (0.86–1.04) | 10 (931) | 1.33 (1.06–1.66) | 10 (931) | 0.74 (0.63–0.87) | 10 (1027) |
| Quinolones plus GP vs. quinolones | 1.23 (0.66–2.30) | 9 (1232) | 1.05 (0.98–1.12) | 8 (1133) | 1.01 (0.79–1.30) | 7 (1093) | 1.94 (1.28–2.94) | 6 (516) |
| Non-absorbable vs. systemic | 1.06 (0.74–1.50) | 8 (813) | 1.06 (1.00–1.13) | 8 (808) | 1.11 (0.95–1.31) | 10 (862) | 1.23 (1.01–1.50) | 10 (934) |
| Systemic plus non-absorbable vs. systematic | 0.9 (0.34–2.38) | 2 (83) | 0.93 (0.72–1.20) | 2 (103) | 0.54 (0.25–1.15) | 1 (63) | 1.75 (1.02–3.00) | 3 (146) |
Conclusions: Compilation of an extensive amount of evidence derived from randomised trials convincingly demonstrates that antibiotic prophylaxis reduces overall mortality within the timeframe of one chemotherapy course. In light of the present findings systemic prophylaxis should be considered for routine use in neutropenic patients.
O97: Antibiotic monotherapy for the empirical treatment of febrile neutropenia. Systematic review and meta-analysis
M. Paul, D. Yahav, A. Fraser, L. Vidal, L. Leibovici (Petah Tikva, IL)
Background: Broad-spectrum antibiotic monotherapy has become standard empirical treatment for febrile neutropenia. Several monotherapy options are recommended differing possibly in antibacterial spectrum, resistance induction, and adverse events. We conducted a systematic review of trials comparing these monotherapies.
Methods: We included randomised controlled trials comparing different beta-lactams (BLs) for febrile neutropenia. Combination with a glycopeptide (GP) in both arms was permitted. We searched the Cochrane Library, Medline, Embase, Lilacs, FDA and pharmaceutical company documents, conference proceedings and all references. No date, language, age or publication limits were imposed. Two reviewers extracted data supplemented by contact with authors independently. Outcomes for first episode by intention to treat were extracted. Relative risks and 95% confidence intervals are reported.
Results: Cefepime was compared to other antibiotics in 17 trials including 3144 patients. Overall 30-day mortality was significantly higher with cefepime than with comparator drugs RR1.58 (1.09–2.31, figure). Ceftazidime was the comparator in most trials. We did not find a disadvantage to cefepime with regard to infection-related mortality, treatment failure or modifications, microbiological failure and adverse events. Bacterial super-infections were more frequent in the cefepime arm RR1.70 (0.94–3.09). Comparing carbapenems to other BLs (19 trials, 4600 patients) the advantage to carbapenems in overall mortality was not significant RR0.86 (0.58–1.28), as for other efficacy outcomes. GPs were added more frequently to comparators, RR0.83 (0.70–0.99), while anti-fungals were added more frequently to the carbapenem arm, RR1.14 (0.94–1.38). Adverse events were significantly more frequent with imipenem (500 mg qid), including seizures, RR3.21 (1.04–9.88). Piperacillin-tazobactam (PT) was assessed in 5 trials, 973 patients. Success without modification was more frequent when compared to cefepime RR0.88 (0.77–1.00). Other outcome comparisons were small and differences were non-significant.

Conclusions: We found that overall mortality is significantly higher with cefepime when compared to other monotherapies. Recommendations for its use should be reconsidered and this finding investigated further. Mortality may have been due to increased super-infection rates. No advantage justifying empirical use of carbapenems over ceftazidime or PT was found. Data for PT are limited.
The impact of beta-lactamases on clinical practice
S101: The impact of beta-lactamases on the management of community-acquired infections
R. Cantón (Madrid, E)
During the last decade extended spectrum beta-lactamase (ESBL) producing isolates were epidemiologically linked to nosocomial outbreaks whereas few isolates were encountered in the community setting. These isolates were recognized to produce ESBLs belonging to TEM or SHV families and they were mainly identified in Klebsiella pneumoniae and to a lesser extent in Escherichia coli isolates. Risk factors for the acquisition of infections due to these isolates included admission to intensive care units, recent surgery, urinary catheterization, prolonged hospitalization and previous beta-lactam and/or aminoglycoside exposure. Nowadays, an outburst of ESBL producing isolates, mainly E. coli with different CTX-M variants, has been recognized in the community. Complex population structures have been identified in different countries with high clonal variability and coexistence with the spread of specific clones. In these isolates, co-resistance with fluoroquinolones is a general feature rather than exception.
This fact has been suggested to play an important role in the dispersion of these isolates in the community. On the other hand the insertion of blaCTX-M genes in different genetic environments (ISEcp1, In60 like structures) participating in horizontal gene transfer processes may has also facilitated the spread of these genes and these enzymes producing isolates. Recent recognition of frequent fecal carriage of healthy volunteers and out-patients with ESBL producing isolates depicts future increase of these isolates in the community. Moreover the accumulation of different blaESBL-genes in bacterial populations, co-existence with other beta-lactamases, including cephamycinases, the recognition of extended-spectrum beta-lactamase variants with carbapenemase activity, and the association of certain blaESBL genes with new recognized resistance genes like qnr represents new threats in the antimicrobial resistance scenario. Intervention strategies to control the spread of these isolates in the community are limited for the frequent exhibited multirresistance phenotype and the absence of efficient oral alternatives for the management of infections due to ESBL producing isolates.
The year in HIV medicine
S103: The year in HIV medicine
J. Lundgren (Hvidovre, DK)
This session will focus on a discussion on recent publications related to the management of HIV. The following topics will be included: 1. Virology: Evolutionary pathways and how antiretroviral therapy (ART) affects this. Response to ART according to which of the viral subtypes the patient is infected with. 2. Effect of ART: New strategies, newer generation of drugs from the three main drug classes and new drug classes to manage patients harbouring HIV fully susceptible to all types of ART and patients harbouring HIV that has varying degrees of diminished susceptibility. When using ART, setting altered aims than complete viral suppression for patients harbouring HIV with widespread decreased susceptibility. 3. Adverse effects of ART: Emerging knowledge on metabolic toxicities associated with the use of ART. What are the mechanism of actions. Which drugs and drug classes are responsible? Individual patient management. 4. Use of ART in patients co-infected with hepatitis viruses. What is the extend of the problem? Can the hepatitis virus infection be cured? 5. Epidemiology: Assessing the risk of turning a fully drug susceptible HIV epidemic to a multi-drug resistant epidemic from widespread introduction of ART within a population. How effective can the introduction of ART within a population expect to attenuate the risk of transmission. 6. Vaccine development. How effective is the prime-boost approach to enhance anti-HIV cytotoxic T-lymphocyte (CTL) response. Which level of CTL response is required for clinical protection?. A listing of the publications to be reviewed will be available at the start of the session.
Coping with the severe acute respiratory syndrome
S107: The SARS Accelerated Vaccine Initiative (SAVI) and the search for a SARS vaccine
R.C. Brunham, B. Finlay on behalf of the SAVI research team
Canada was the most affected nation outside of Asia following the world-wide spread of SARS in 2003. Over 42% of the 251 cases occurred in healthcare workers and the rapid development of a vaccine was deemed an urgent public health priority for Canada. A novel research management structure called SAVI was developed in May 2003 and was predicated on accelerating vaccine research by parallel processing of multiple science projects. During 18 months of operations SAVI developed and evaluated 3 key vaccine strategies including whole killed virus (WKV), recombinant spike protein and viral vectored vaccines for SARS CoV. Two vaccines (WKV and adenovirus vectored) were compared head to head in two animal models (B129 mice and outbred ferrets). Overall WKV vaccine with or without alum adjuvant generated substantial neutralizing antibody titres and reduced viral shedding in the upper and lower respiratory tract of SARS CoV challenged experimental animals. WKV vaccine appeared more efficacious than adenovirus vector vaccines expressing the S and N genes. Nonetheless, inflammatory pathology occurred in the lungs of experimental animals following challenge despite favorable serological and virological response to vaccine.
Conclusion: The results suggest that human trials with WKV vaccine should proceed with caution.
Supported by: A grant in aid to the Michael Smith Foundation for Health Research from the government of British Columbia and by the CIHR.
Advances in foreign body infections
S108: Improved methods for detection of microorganisms in biofilms
A. Trampuz (Basel, CH)
Background: Implant-associated infections are typically caused by attached microorganisms growing in biofilms. These microbes are enclosed in an extracellular matrix and are organized in complex communities with structural and functional heterogeneity, resembling multicellular organisms. Existence within a biofilm represents a basic survival mechanism by which microbes resist against external (antimicrobial agents) and internal environmental factors (host immune system).
Challenge: Depletion of metabolic substances or waste product accumulation in biofilms causes microbes to enter a slow- or nongrowing (stationary) state, in which they are less susceptible to growth-dependent antimicrobial agents. These characteristics make biofilm microbes not only more resistant to antimicrobial killing as compared to planktonic bacteria, but also more difficult to detect. As a consequence, implant-associated infections are often difficult to diagnose with routine microbiological methods.
Routine diagnostic methods: Increased synovial fluid cell count and presence of acute inflammation in periprosthetic tissue correlate well with infection, however, the causing microorganism cannot be identified with this method. Gram staining has usually a low sensitivity. Periprosthetic tissue and synovial fluid cultures are frequently used as the reference standard for diagnosing infection, however, they do not have an ideal sensitivity and specificity. New diagnostic methods directed to identify microbes in biofilms are needed.
Potential new methods: By dispersing adherent bacteria from the surface and disrupting their multicellular structure, the recovery efficiency of diagnostic assays may be increased. Various potential strategies to dislodge microbial biofilms from surfaces have been used in research setting, including mechanical (sonication, vortexing, shock waves), biochemical (enzyme treatment), and electrical approaches. To date, mostly ultrasound has been studied for improvement of recovery of biofilm microbes. In addition, cultures may be false-negative because of prior antimicrobial exposure, a low number of organisms, inappropriate culture media, or fastidious or atypical organisms. Therefore, molecular (culture-independent) methods may be used to improve the diagnosis of infection, for example broad-range 16S rDNA PCR.
S109: Foreign body infections: when can we save the implant?
A. Widmer (Basel, CH)
Foreign body infections continue to challenge current diagnostic and therapeutic options. Orthopedic device related infections (ODRI) such as hip prostheses or fixation devices poorly respond to antimicrobial therapy and frequently require removal to cure the infection. Routine susceptibility testing do not predict cure. However, susceptibility testing against stationary-phase and adherent bacteria correlated well with the outcome in the ODRI guinea-pig animal model (Widmer AF. JID 1990). Representative pathogens have been tested from patients suffering from ODRI, and were treated according to a standard regimen (Zimmerli W. NEJM 2004). Data from patients were generated by full chart review from patients hospitalized between 1994–2003. Strains were tested with standard MIC, MBCs against bacteria in logarithmic and stationary phase of growth. Early ODRIs defined as signs and/or symptoms of infection not longer than 1–3 months can be cured without removal of the device, given the antibiotic is active against the pathogen even in these sophisticated tests, an appropriate debridement is performed and treatment duration is prolonged to 3–6 months. Multiresistant pathogens in ODRIs are a new challenge: Their treatment regimens remains poorly defined, and removal of the device is deemed necessary because sufficient evidence by in-vitro and in-vivo tests are still lacking.
Paediatric infections
O110: Borna disease virus infection in early childhood, a potential risk for developing brains
L. Bode, T. Scholbach, A.M. Patti, M. Vetterlein, H. Ludwig (Berlin, Leipzig, D; Rome, I)
Objectives: For the first time, the infection prevalence of children with Borna disease virus (BDV), an unusual neurotropic virus of humans and animals, has been addressed in Germany (D) and Italy (I) monitoring 2000 children of all ages.
Methods: BDV infection is detectable in blood. Plasma samples were investigated for BDV-specific immune complexes (BDV-CIC) by novel ELISA tests which use two monoclonal antibodies against the major antigens (proteins N and P). BDV-CIC are formed after periods of virus activity with antigenaemia and subsequent antibody formation.
Results: BDV is an unique negative stranded RNA virus targeting the limbic system of the brain. Its broad host spectrum covers humans and companion animals. In animals, behavioural and developmental brain disorders are confirmed. A world-wide impact of BDV on human mental health has been suggested in the mid 1990s, when psychiatric patients’ infections were confirmed by RNA/proteins in blood cells. New infection markers, namely BDV-CIC, estimated a fairly high BDV prevalence in healthy adults (20–30%) vs. 90% in depressed subjects. This multi-centre study for the first time unravels the prevalence of BDV-CIC through randomised cohorts of children in two European countries. German cohorts included healthy and diseased children (various diagnosis) (n = 770; 0–18 years) in Saxony, Italian cohorts focused on healthy children only (n = 1224; 0–15 years), but covered eight regions of residence. In both countries, an unexpectedly high but congruent mean prevalence of 60% was found, double as high as shown in healthy adults. More intriguingly, the age-dependent frequencies were congruently peaking in early childhood (D:1–3 and I:1–5 years), reaching 85% (one region, D) and 75% (mean of regions, Italy). In addition, the Italian cohorts revealed dramatic regional differences.
Conclusion: This multi-centre cross-sectional study on 2000 children provides first evidence that BDV infects children unnoticed very early in life, suggesting vertical transmission as a main route. Given the high impact of BDV for behavioural disorders in mammals, the high mean prevalence together with accumulating frequencies in young children suggests so far unconsidered age-dependent mental-health risks during brain development. The results point to the need for appropriate world-wide risk-assessment studies on BDV in children.
O111: Pertussis cases detected by active surveillance in Catalonia, Spain
M. Romero, N. Cardeñosa, G. Carmona, M.R. Sala, I. Barrabeig, M. Company, C. Planas, S. Minguell, P. Godoy, J. Cayla, G. Codina, A. Dominguez on behalf of the Catalonian Pertussis Working Group; Communicable Diseases Group of RCESP
Objectives: To know if distribution of cases of pertussis, detected from reported cases’ contact study is related to age.
Methods: From May 2003 to May 2004, pertussis-suspect-cases were reported from voluntary health care centres all over Catalonia (6.3 million inhabitants); patients were sampled by nasopharinx aspirate or swabs. Possible related cases were sought by telephone and home interview and swab sampling of suspect household contacts. We included in the study cases that matched the Program's case definition: cough lasting at least 2 weeks or cough lasting at least 1 week with paroxysmal cough, post-tussive vomiting, whooping or apnoea. We evaluated data from epidemiological interviews, from epidemiological and clinical reports and from B. pertussis PCR and culture tests. Data were compared using Chi-square test or Fisher's exact test, as convenient.
Results: 160 reported cases (RC) leaded to identification of 42 new detected cases (DC). 34 (21.25%) RC and 4 (9.52%) DC were confirmed by laboratory tests; overall, 38 (18.81%) cases were confirmed. DC were 3.4%(2) of all children under 1 year and 5.6% (1) of lab confirmed; in 1–13 years, 12.5% (14) and 5.9% (1); in 1–3 y, 13.8% (4) and 0; in 4–13 y 12% (10) and 8.3% (1); under 14y 9.4% (16) and 5.7% (2); in 14 and more years, 81.3% (26) and 66.7% (2); RC were 20.8% of all cases and 10.5% of confirmed cases. We found no statistically significant differences by case type (reported or detected) between age groups under 14 years; there was significant difference in RC and DC between under 14 years and 14 years and over age groups in the total of cases (P < 0.0001; OR: 41.71; CI: 13.65–134.46) and also in the confirmed cases (P = 0.0246; OR: 33; CI: 4.03–270.5).
Conclusions: Although reported cases of petussis in 14 years old and older group are few (15.8%), the proportion of cases detected investigating household contacts is higher in this group than in children under 14 (81.3% vs. 9.4% for the total of cases). In order to improve the knowledge of pertussis epidemiology and its control, its important to perform case finding in household contacts when a case is reported.
O112: Epidemiology of pneumococcal carriage among Warao children in the Delta Amacuro in Venezuela
I. Rivera, T. Bello, B. del Nogal, M. Sluijter, D. Bogaert, P. Hermans, J. de Waard (Caracas, VE; Rotterdam, NL)
Objectives: To determine the prevalence of nasopharyngeal carriage and the distribution of serotypes of Streptococcus pneumoniae in Warao children and to obtain insight in the transmission of pneumococci in 4 distinct geographically isolated communities.
Methods: A single nasopharyngeal swab was cultured from 202 children aged 3–60 months living in Murako(n = 40), Guayo (n = 53), Pedernales (n = 69) and Nabasanuka (n = 40) between March and June 2004. S. pneumoniae isolates were serotyped and their susceptibility for penicillin assessed by disk diffusion and E-test. The isolates were genotyped by restriction fragment end labeling (RFEL) analysis and the data were compared with the 26 RFEL types represented by the Pneumococcal Epidemiology Network and approximately 1000 RFEL genotypes present in the Dutch RFEL data library.
Results: In total, 114 pneumococcal isolates were collected. The overall nasopharyngeal carriage rate for S. pneumoniae was 56%. All isolates were susceptible to penicillin. The most important capsular serotypes were 23F (20.2%), 6A (18.4%). 15B (11.4%), 6B (8.7%) and 19F (7.0%). The theoretical coverage by the 7-valent pneumococcal conjugate vaccine was 45% when combining the four communities (See Table 1). When including the cross-reactive serotypes 6A and 19A the theoretical vaccine coverage increased to 66%. The 114 isolates represented 53 different genotypes, and 71% of these isolates belonged to 20 distinct genetic clusters. The most important cluster represented 15 isolates of serotype 23F. These isolates, which were invariably found in Pedernales, were genetically identical to the RFEL type 4 that was present in the Dutch RFEL data library. Two genetically closely related RFEL clusters representing 18 serotype 6A isolates were found in all the communities studied. The latter two genotypes were not present in the reference data libraries.
Table 1.
Distribution of pneumococcal serotypes in 4 Warao communities, Delta Amacuro, Venezuela
| Serotypes (%) | Murako (n = 26) | Guayo (n = 17) | Nabasanuka (n = 22) | Pedernales (n = 49) | Total (n = 114) |
|---|---|---|---|---|---|
| 23F | 23.1 | 9.1 | 30.6 | 20.2 | |
| 6A | 34.6 | 11.8 | 31.8 | 6.1 | 18.4 |
| 15B | 7.7 | 23.5 | 9.1 | 10.2 | 11.4 |
| 6B | 5.9 | 9.1 | 14.3 | 8.8 | |
| 19F | 5.9 | 18.2 | 6.1 | 7.0 | |
| 14 | 7.7 | 5.9 | 6.1 | 5.3 | |
| 11 | 7.7 | 17.7 | 4.1 | 6.1 | |
| 18C | 3.9 | 5.9 | 1.8 | ||
| 9V | 11.8 | 1.8 | |||
| 10 | 8.2 | 3.5 | |||
| 19A | 7.7 | 4.5 | 2.6 | ||
| Others | 7.7 | 12.5 | 18.1 | 14.3 | 12.3 |
| VCN7-v* (4.9 V, 14, 19F, 23F, 18Cy 68) | 34.7 | 35.2 | 36.4 | 57.1 | 44.7 |
| VCN7-v (including 6A) | 77.0 | 47.0 | 72.7 | 63.3 | 65.8 |
VCN7-V 7 valent pneumococcal conjugate vaccine
Conclusions: The prevalence of pneumococcal colonization in the pediatric population was found to be relatively high being 56%. No resistance to penicillin was observed. Coverage by the 7-valent pneumococcal conjugate vaccine is low. The presence of two genetically closely related clusters of serotype 6A isolates in all the communities studied is remarkable, since these communities are geographically very isolated, only reachable by boat and hardly any contact between their inhabitants. The remaining clusters were restricted to single communities, suggesting limited, local spread of these genotypes.
O113: Clonal diversity of invasive Streptococcus pneumoniae from Portuguese children
I. Serrano, J. Carriço, S. Aguiar, J. Melo-Cristino, M. Ramirez (Lisbon, Oeiras, P)
Objective: To identify the clones responsible for invasive disease among Portuguese children.
Methods: A recent (1999–2002) collection of 82 invasive isolates recovered from children <6 years old in Portugal was characterized using a combination of macrorestriction profiling, using SmaI and pulsed field gel electrophoresis (PFGE), and multi-locus sequence typing (MLST). The Bionumerics software was used to make UPGMA (unweighed pair group method with arithmetic mean) dendrograms of PFGE fragment patterns. The dice similarity coefficient was used with optimization and position tolerance settings of 1.0 and 1.5%. Among the 18 serotypes detected, serotypes 14 (25.6%), 23F (17.1%), 1 (12.2%), and 6B (9.8%) were the most prevalent.
Results: We found 42 sequence types (ST), including 12 novel STs, corresponding to 27 different lineages by e-BURST analysis. By combining the PFGE and MLST data we were able to infer the genetic lineages of the majority of the isolates. Among serotype 14, most isolates (16/21) were clustered with the Spain9V-3 clone, including representatives of ST156, 557, and the new ST790. Another cluster with 4 strains included ST15, related to the England14-9 clone, and ST409. Among serotype 23F the majority of the isolates (12/14) were grouped into a single cluster that included ST338, the same ST as the Colombia23F-26 clone, and the new ST1371. Serotype 1 was clustered into two main lineages, one including representatives of ST306 and 228 (7/10), and the other ST304 and 350 (3/10). In serotype 6B most isolates (5/8) were included in a cluster with ST273 the same ST of the Greece6B-22 clone, and the new ST1224. The other strain was ST887 related to Poland6B-20. Among penicillin non-susceptible strains 80.5% were related to two lineages, Spain9V-3 expressing serotypes 14 and 9V (18/36) and Colombia23F-26 (11/36), and the remaining isolates belonged to other internationally disseminated clones - Spain23F-1, Greece6B-22, and Poland6B-20.
Conclusions: Representatives of 6 internationally disseminated clones were found among invasive isolates recovered from children <6 years old, accounting for 91.6% of the penicillin non-susceptible isolates. The most frequent lineages were related to Spain9V-3 (23.2%) and Colombia23F-26 (14.6%). This study provides a baseline for detecting potential effects of the use of the 7-valent conjugated vaccine on the distribution of individual genetic lineages within this population.
O114: Attempt to rationalise antibiotic use in a paediatric intensive care unit
N. Goldman, D. Biarent, C. Fonteyne, F. Otte, A. Vergison (Brussels, B)
Objectives: To evaluate the impact of antibiotics policies in the Intensive Care Unit (ICU) of a 170-beds pediatric teaching hospital between 2001 & 2003. The ICU is a 16-beds medical and surgical unit (8 intensive and 8 medium care). Antibiotic guidelines in the ICU aimed at (1) decrease the share of broad-spectrum antibiotics, (2) switch to narrow spectrum antibiotics whenever possible (3) reduce the empirical treatment durations and (4) reduce amikacin and vancomycin consumption.
Methods: Starting in march 2002, regular information was provided on local epidemiology and antibiotic resistance (MRSA, ESBL,) during seminars (3/year) and bedside discussions were performed on a regular basis (minimum twice a week) with the infectious disease specialist. Antibiotics consumption were analyzed through pharmacy billing data. Data were expressed in DDD/100 patient-days (PD). Broad spectrum antibiotics included Amoxicillin-Clavulanate (AC), Ceftriaxone, Ceftazidime, Cefotaxime, Cefepime and Meropenem. Narrow spectrum drugs used were flucloxacillin, amoxicillin, ampicillin and penicillin.
Results: Broad spectrum antibiotics decreased from 33 to 26 DDD/100PD between 2001 and 2003. Amoxicillin-clavulanate reduction was the most important (11 to 5 DDD/100PD). Narrow spectrum drugs increased from 8 to 12 DDD/100PD. Amikacin decreased from 4.2 to 1.8 DDD/100PD and vancomycin from 8.65 to 6 DDD/100 PD. Cefuroxime increased from 2.83 to 9.05 DDD/100PD and oral ciprofloxacin from 0.7 to 1.95 DDD/100PD. Total AB consumption in the ICU remained stable (57 DDD/100PD.
Conclusions: Antibiotic use analysis for ICU showed: (1) a decrease in broad spectrum antibiotics together with an increase in Narrow spectrum drug use, (2) a reduction of Amikacin and Vancomycin use, (3) The data obtained represent encouraging information feedback for physicians in the ICU and emphasize the need for collaboration between ICU physicians and infectious disease specialist.
New typing approaches for MRSA control
O115: An automated DNA sequence-based early-warning system for detection of MRSA-outbreaks in hospitals
A. Mellmann, A.W. Friedrich, N. Rosenkötter, R. Reintjes, W. Witte, D. Harmsen (Munster, Hamburg, Wernigerode, D)
Objectives: Isolation of methicillin resistant Staphylococcus aureus (MRSA) in hospitals often implies rigorous infection-control measures. The use of rapid and accurate typing is required to monitor nosocomial spread. Prompt identification of epidemic MRSA is crucial to control an outbreak, in order to avoid unnecessary interventions for patients and staff unrelated to an outbreak. In this study we evaluated different early-warning algorithms for MRSA-outbreak detection in hospitals.
Methods: Between 1998 and 2003, 557 non-replicate MRSA-strains were collected from staff and patients admitted to Munster University Hospital (1480 beds), Germany. Of these strains, the DNA sequence of the repeat-region of the S. aureus protein A gene (spa) was analyzed by the Ridom StaphType software v2.0 beta. Different early-warning algorithms (frequency and clonal alerts, infection control professionals [ICP], Z-score) were evaluated for the year 2003 using spa typing results and epidemiological data. Outbreaks were detected on the level of minimally two MRSA-colonized or -infected patients or staff on the same or related nursing units exhibiting the same spa type within a two-week time window.
Results: 549 of 557 MRSAs were typeable by spa sequencing. In total, 79 different spa types were identified. Retrospectively analyzed, 42 of the overall 175 MRSA isolates formed 13 significant clonal outbreaks in 2003 (scantest, 5% significance level). These outbreaks were used as gold standard to evaluate the different algorithms in a prospective simulation. 100% sensitivity and 95.2% specificity for outbreak detection were reached using the combination of spa typing and epidemiological data (place and time). All other methods were less sensitive or less specific: using solely epidemiological data (frequency alert) resulted in 100% sensitivity and 47.3% specificity, whereas investigations of the ICP resulted in 62.1% sensitivity and 97.3% specificity, respectively.
Conclusion: A surveillance method based on both epidemiological and spa typing data gives infection-control professionals opportunities to intervene before limited clusters of preventable MRSA transmissions become expansive outbreaks. This innovative combined use of medical informatics and molecular laboratory technique provides a vision for future innovations that can expand our capacity to detect and treat clusters of infectious diseases, thus limiting their spread and improving the patients’ safety.
O116: Sequence-based typing of methicillin-resistant Staphylococcus aureus for real-time infection control
M. Christensen, K. Boye, A.R. Larsen, R. Skov, H. Westh (Hvidovre, Copenhagen, DK)
Objectives: After an epidemic in the late 1960's, Denmark has been almost free of MRSA. In 2003, however, a significant increase in the number of MRSA patients in Denmark was observed (from 100 in 2002 to 240 in 2003). At Hvidovre hospital, the number of patients with MRSA has increased from 33 in 2003 to an expected 118 in 2004. A rise in MRSA can lead to serious treatment difficulties since the MRSAs are resistant to all beta-lactam antibiotics and often also to other groups of antibiotics. Furthermore, patients with MRSA need to be isolated during hospitalization. In order to study the epidemiological relatedness of the MRSA isolates and potentially discover routes of transmission we selected a number of genes for typing by PCR and/or DNA sequencing.
Methods: 115 MRSA isolates from 2003 and 2004 were analyzed. The genes or gene clusters chosen for analysis were the following: the variable repeat region of the staphylococcus protein A gene (spa typing), the Staphylococcal Chromosomal Cassette (SCCmec typing), the Panton-Valentine leukocidin (PVL) genes, and multilocus sequence typing (MLST) of all novel spa types.
Results: One dominant spa type, t024 (SCCmecIV, PVL-, ST8), was found in 50 of the MRSA isolates (43 %) and was clearly associated with nursing homes. This spa type was also predominant during the MRSA outbreaks in Denmark in the 1960's. 15 isolates (13 %) were t019 (SCCmecIV, PVL+, ST30). ST30 is known as the CA-MRSA from Oceania, and all of these patients came from or had a connection to the same Asian country. spa type t044 (SCCmecIV, PVL+, ST80) was found in 9 isolates. ST80 is the most common CA-MRSA in Europe. spa type t008 (SCCmecIV, PVL+, ST8) was found in 7 and t002 (ST5) in 5 isolates. Of the remaining 28 patients with sporadic MRSA clones, 12 had acquired the MRSA in a foreign country.
Conclusions: MRSA is spreading in Denmark, primarily in the community, but these patients are often hospitalized with the risk of nosocomial spread. Most isolates carry the SCCmecIV. A clear connection to other countries can be found for several minor or sporadic clones. However, the most dominant MRSA clone, spa type t024, seems to be related to the archaic clone common in Denmark in the 1960's and 1970's.
O117: Rapid, reliable sub-typing of methicillin-resistant Staphylococcus aureus by denaturing high pressure liquid chromatography and DNA sequence analysis
F. Jury, M. Al-Mahrous, A. Fox, W. Ollier, M. Upton (Manchester, UK)
Objectives: Methicillin resistant Staphylococcus aureus (MRSA) is a significant cause of hospital and community acquired disease. Epidemic MRSA (EMRSA)strains are particularly successful pathogens able to spread rapidly. Detection and sub-typing of EMRSA can require a week of investigation. To be of true use, methods for identification of cross-infection events and outbreaks need to be highly discriminatory and easy to perform. The current methods for this purpose have numerous disadvantages including expense and a lack of standardisation and rapidity. Characterisation of the X region of the spaA gene provides a rapid, unambiguous, discriminatory sub-typing method that can inform outbreak investigation. Denaturing high-performance liquid chromatography (DHPLC) is a powerful technique for separation and quantitation of nucleic acids. We have used DHPLC to detect DNA sequence variation within the spaA gene of 32 samples to fully investigate the application of DHPLC approaches as a possible rapid and cheap alternative to spa typing by conventional methods.
Methods: Genomic DNA was extracted from cultured isolates and used as template in PCR to amplify the X region of the spaA gene. DHPLC was carried out by Transgenomic WAVE™ DNA fragment analysis. PCR products were screened for size variation by running 5 μl of each PCR sample through a linear acetonitrile gradient. The samples were run blindly so no prior assumptions could be made of the EMRSA type. Retention times were collected for each sample and comparisons to a size standard (pUC18 Haelll digest) were made. The number of repeat units for each sample was calculated. Sequence data were also obtained for each of the samples.
Results: Sequence data indicated a predominance of strains with 15 (n = 13; group A) or 16 (n = 8; group B) repeat units in the spaA X region. With the exception of a repeat unit that was inserted as the sixth unit in group B isolates, the succession of repeat units in group A strains was identical to that seen in those of group B. The number of repeat units in each sample matched exactly those predicted by WAVETM analysis.
Conclusion: DHPLC methods can rapidly detect repeat unit number with a very high correlation to sequence data. This indicates the ability of the WAVE to rapidly sub-type strains of MRSA, which differ by a single repeat unit. Expansion of the predominant repeat unit succession, by insertion of a new repeat unit, suggests possible local evolution of the spaA X region.
O118: Comparison of random amplification of polymorphic DNA with pulsed-field gel electrophoresis for the molecular typing of methicillin-resistant Staphylococcus aureus in an infection control setting
J.M. Caddick, A.C. Hilton, P.A. Lambert, T. Worthington, T.S.J. Elliott (Birmingham, UK)
Objectives: Methicillin-resistant Staphylococcus aureus (MRSA) is a significant cause of nosocomial morbidity and mortality with increasing reports of multiple-resistant (MR) hospital acquired (HA) strains and an emerging problem of community acquired (CA) infections. The objective of this study was to compare random amplification of polymorphic DNA (RAPD) with pulsed-field gel electrophoresis (PFGE) for the characterisation of MRSA and to assess the suitability of RAPD as a typing technique in an infection control setting.
Methods: A total of 129 MRSA isolates were typed: 28 MR-MRSA isolates (only sensitive to vancomycin, tetracycline and rifampicin), 66 HA-MRSA isolates from the University Hospital Birmingham NHS Trust, UK, (UHB) and 35 CA-MRSA isolates sent to the UHB by general practitioners in the Birmingham area. The RAPD reaction consisted of two separate reactions for which two arbitrary 10mer primers (designated s and l) were used and was optimised and tested for reproducibility, typability and discrimination. PFGE was performed following SmaI macrorestriction. Profile relatedness was calculated by the Dice coefficient and a dendrogram was constructed using UPGMA clustering.
Results: PFGE analysis revealed 30 profiles, type B (26 isolates) and type J (2 isolates) representing two MR-MRSA strains and type A (31 isolates) and type C (17 isolates) representing strains that shared the same genotype as the EMRSA-15 and EMRSA-16 respectively. All CA-MRSA strains shared the same genotype with 1 or more of the HA-MRSA strains excluding 9 CA-MRSA strains, which had unique PFGE profiles. RAPD analysis revealed ten profiles, type B(sl) (45 isolates) representing strains that shared the same genotype as EMRSA-16 and the MR-MRSA strains and type A(sl) (74 isolates) representing strains that shared the same genotype as EMRSA-15. The B(sl) type was associated with a higher resistance phenotype than the A(sl) type. The discriminatory capacities of PFGE and RAPD as determined by Simpson's Index of Diversity were 88% and 58% respectively.
Conclusion: This study indicates that RAPD has a limited discriminatory capacity compared to PFGE for typing of MRSA, however, RAPD was able to elicit results within a single working day and grouped all the MRSA isolates associated with a higher resistance phenotype. Such timely information is invaluable in directing appropriate infection control which is especially important in the management of MR-MRSA outbreaks.
O119: Staphylococcal cassette chromosome in methicillin-resistant Staphylococcus aureus: different methods resulting in different types
K. Becker, M. Schulte, B. Schuhen, G. Peters, C. von Eiff (Munster, D)
Background: Methicillin-resistant Staphylococcus aureus (MRSA) strains possess the mecA gene, which is carried by a unique mobile genetic element, Staphylococcal cassette chromosome (SCCmec), integrated into the S. aureus chromosome. A full characterization of MRSA strains requires structure determination of the complex SCCmec element. In addition to the SCCmec types I–V, several subtypes have been described. Most recently, a progressive replacement of type II SCCmec-bearing isolates with type IV SCCmec-bearing isolates, which coincided with >4-fold increase in methicillin resistance was reported.
Methods: In order to analyze the SCCmec (sub)types of 130 MRSA isolates recovered from patients admitted to our Hospital, two different multiplex PCR typing strategies reported by Oliveira & Lencastre (A) and by Okuma et al. (B) were used. For confirmation of the SCCmec type, the method of Branger et al. was used. The presence of the pls gene – described to be associated with type I – was also determined. Only one MRSA isolate per patient was included.
Results: Concordant results based on all methods used were found in only 59% of the isolates tested comprising MRSA strains exhibiting type I (n = 40, 52%), type II (n = 10, 13%), type III (n = 2, 3%), type IV (n = 20, 26%) and 5 nontypeable strains. All isolates tested positive for pls were shown to be type I. Regarding type I (A: n = 64, 49% [incl. type IA] versus B: n = 30, 23%) and type IV (A: n = 24, 18% versus B: n = 58, 45%) major discrepancies were detected. Using approach A, 13 (10%) and 3 (2%) MRSA strains showed type II and III (incl. IIIA), respectively, whereas method B yielded 15 (12%) and 7 (5%) type II and III, respectively, results. 26 isolates were not typeable using method A as were 30 isolates applying method B (no PCR bands or uncharacteristic band patterns).
Conclusions: The application of different approaches to determine the SCCmec type showed major discrepancies, in particular regarding types I and IV. As both methods failed in typing of some MRSA isolates, the structure of SCCmec may be more heterogenous than assumed so far.
Pharmacokinetics and pharmacodynamics of antibiotics
O120: Pharmacological comparison of antibiotics against intracellular S. aureus
M. Barcia-Macay, M.P. Mingeot-Leclercq, P.M. Tulkens, F. Van Bambeke (Brussels, B)
Objectives: The parameters governing the intracellular activity of antibiotics are still poorly understood. In this study, we have compared the concentration-effect relationships at 24 h of 4 antibiotics against extracellular and intracellular forms of S. aureus.
Methods: Infection of THP-1 human macrophages by S.aureus ATCC25923 and assessment of antibiotic activity was performed following the general procedure described in Seral et al. (AAC 47:2283-92) with minor adaptations for cells in suspension. Antibiotics were used at concentrations ranging from 0.05 X MIC to 1000 X MIC. Antibiotic content in cell lysates was measured by microbiological (OXA, GEN), fluorimetric (MXF) or radiochemical (ORI) assay.
Results: The table shows the parameters calculated from a sigmoidal regression of the concentration-effects relationships, with concentrations expressed in X MIC and the effect, as the change in CFU over 24 h, as compared to the initial inoculum (all R2 > 0.9). Extracellularly, all antibiotics reached a static effect and EC50 at a conc. close to their MIC and were highly cidal (4–5 log decrease) upon exposure to high conc. Intracellularly, OXA and MXF showed a static effect and EC50 at extracell. conc. 3–4 X those observed for extracellular bacteria, whereas conc. of approx. 10 X higher were needed for GEN and ORI. The intracellular max. effect was lower than the extracellular one for all drugs, but a cidal effect (2 log decrease) could still be achieved at clinically relevant conc. for OXA, MXF and ORI.
| Extracellularly |
Intracellularly |
||||||
|---|---|---|---|---|---|---|---|
| Antibiotics | Static conca | ECa50 | Max effectb | Static conca | ECa50 | Max effectb | Antibiotic cellular accumulation |
| OXA | 0.52 | 1.22 | −3.70 | 2.09 | 1.85 | −1.58 | 4.0 |
| MXF | 0.29 | 0.79 | −4.29 | 0.63 | 0.81 | −2.77 | 7.6 |
| GEN | 0.30 | 0.88 | −5.76 | 2.09 | 7.73 | −2.54 | 4.4 |
| ORI | 0.20 | 1.00 | −5.55 | 4.79 | 13.8 | −3.16 | 148.0 |
In multiples of the MIC
In difference of log CFU as compared to time 0 h
Conclusions: The model shows that the intracellular milieu weakens the overall effects of antibiotics while also increasing the concentration needed to reach a given effect, irrespective of the capacity of the drug to accumulate or not in cells.
O121: In vivo pharmacodynamic activity of gemifloxacin against multiple strains of Streptococcus pneumoniae
W.A. Craig, D. Andes (Madison, USA)
Background: The 24-hr AUC/MIC for free drug is the PK/PD parameter that best correlates with in-vivo activity of fluoroquinolones. We used the neutropenic murine thigh-infection models to determine the magnitude of the AUC/MIC needed for efficacy of gemifloxacin (GEM) against 61 strains of SP with varing fluoroquinolone susceptibility.
Methods: Mice had 10 to the 5.728.3 cfu/thigh when treated for 24 hrs with 0.073–1200 mg/kg of GEM every 12 hrs. Serial dilutions of thigh homogenate were plated for CFU determinations. A sigmoid dose-response model was used to estimate the dose (mg/kg/24 hr) required to achieve a net bacteriostatic effect over 24 hrs. The AUC for the static dose was estimated from serum levels following doses of 18.8, 75 and 300 mg/kg determined by microbiologic assay. Protein binding was determined by ultrafiltration.
Results: PK studies exhibited AUC/dose values of 0.12–0.18 and half-lives of 0.7–1.6 hrs; protein binding was 66%. MICs ranged from 0.008–2.0 mg/L and some strains had single or multiple parC, parE and gyrA mutations. Five strains had efflux (confirmed by 4- to 16-fold lower MIC with reserpine); the free drug 24-hr AUC/MIC values for the static dose for these strains were 2.1–5.7. For the 56 other stains, the static dose varied 275-fold (1.7–468 mg/kg q12h), while the free drug 24-hr AUC/MIC values for the static dose varied only 5-fold (16–82) and the mean AUC/MIC was similar at different MIC values.
Conclusions: The magnitude of the 24-hr AUC/MIC of free GEM required for in vivo bacteriostasis was similar for most strains of SP with and without gyrA, parC and parE mutations. However, for strains with higher MICs due to efflux, GEM was much more active than the MIC predicted. This suggests that efflux might be down-regulated in vivo.
O122: Comparison of pharmacodynamic target attainment calculated by Monte Carlo simulation with microbiological response for two carbapenems in the treatment of complicated skin and skin structure infections
J. Kuti, C. Ong, M. Lo, D. Melnick, N. Soto, D. Nicolau (Hartford, Wilmington, USA)
Objectives: Monte Carlo simulation (MCS) is commonly used to predict pharmacodynamic target attainment (TA) of antibiotics against specific bacteria. The relevance of these predictions to outcomes in humans, however, has not been well studied. This study aimed at determining the probability of attaining pharmacodynamic exposures for meropenem (MEM) 500 mg every 8 hours and imipenem (IMI) 500 mg every 8 hours against pathogens isolated from complicated skin and skin structure infections (cSSSI) during a randomized, multicentre, clinical trial and comparing TA with microbiological response (MR).
Methods: A subset of the clinically evaluable study population who had bacteria isolated and MICs performed for their respective randomized treatment was extracted. The MICs of these bacteria were treated as a single MIC distribution for each carbapenem. Free drug exposures for 5000 subjects were simulated using a one-compartment infusion model. Mean pharmacokinetic data and variability, including blister fluid penetration, was derived from published studies in healthy volunteers and incorporated using MCS. TA at 40%, 50%, 60%, and 70% time above the MIC (T > MIC) in both serum and blister fluid was calculated for each carbapenem and compared with its MR at the end of treatment.
Results: Of 548 clinically evaluable patients, 210 had bacteria with MICs reported and were included (MEM, n = 98; IMI, n = 112). MR for MEM and IMI against these pathogens was 87.8% (95% CI: 79.8–92.9) and 91.1% (95% CI: 84.3–95.1), respectively. For MEM, bactericidal TA (40% T > MIC) were 90.4 and 89.9 in serum and blister fluid and did not differ from MR. TA at all other T > MIC exposures also agreed with MR. In contrast, TA for IMI at 40% T > MIC in either matrix was not predictive of MR. Instead, only TA in serum at 60% and 70% T > MIC, and blister fluid at 50% and 60% T > MIC were similar to MR.
Conclusions: For these carbapenems in the treatment of cSSSI, an association between TA calculated by MCS and MR does exist, although the exposures needed for a successful response appear to be different between MEM and IMI.
O123: Overestimation of vancomycin therapeutic drug monitoring levels in haemodialysis patients
F. Fitzpatrick, T. McGaley, L. Rajan, R. Crowley, M. Turley, H. Humphreys, E. Smyth (Dublin, IRL)
Patients on haemodialysis are one of the largest populations in whom vancomycin therapeutic drug monitoring (TDM) is performed in our institution. Concern has been expressed in the past about the accuracy of polyclonal antibody-based fluorescence polarization immunoassays (pFPIA) for the detection of vancomycin serum concentrations in these patients. However, most laboratories in the Republic of Ireland and in the UK still use the Abbott TDx, which is based on pFPIA, for vancomycin TDM.
Methods: We evaluated the accuracy of our routine procedure for vancomycin TDM, on the Abbott TDx system, with a monoclonal antibody-based FPIA on the Abbott AxSYM system, in 62 serum samples from 19 haemodialysis patients over a one-month period.
Results: Compared with the Abbott AxSYM, the Abbott TDx consistently overestimated vancomycin TDM (from 15–59%) with the majority (23/62 samples, 37%) between 26–30% overestimation. Therapeutic decisions based on falsely elevated vancomycin concentrations in 17 samples (27%) from nine (47%) patients may have resulted in inadequately treated infections and potential therapeutic failure. Conclusion: Our data suggests that there is a clinically significant impact of end stage renal disease on the determination of vancomycin serum concentrations using the Abbott TDx. We therefore recommend that the mFPIA assay on the Abbott AXSYM be used in patients with ESRD.
O124: Pharmacokinetics of linezolid in bone tissue investigated by in situ microdialysis
L. Stolle, N. Plock, M. Arpi, M. Mueller, C. Joukhadar, C. Buerger, P. Riegels-Nielsen, C. Kloft (Aarhus, DK; Berlin, D; Herlev, DK; Vienna, A; Esbjerg, DK)
Objective: Knowledge concerning the distribution of antimicrobial agents in bone tissue is valuable for pharmacokinetic characterisation and clinical use. Unfortunately, appropriate techniques are difficult to apply. The aim of this investigation was to introduce microdialysis to corticocancellous bone tissue for pharmacokinetic investigations of the novel antiinfective linezolid.
Methods: 10 healthy pigs (weight: range 38–43 kg) were included into the study. Two microdialysis catheters were inserted in cancellous bone of the right tibia and calibration was performed according to the retrodialysis principle. After this each animal received 600 mg of linezolid as a 20 min. iv. infusion. Bone samples were harvested from the left and microdialysate samples (lateral catheter, lc, and medial catheter, mc) were obtained from the right tibia over a period of 6 hours. In addition, samples of serum and bone marrow were collected and drug concentrations were measured. All data presented are geometric mean ± geometric SD.
Results: Maximum serum and bone marrow concentrations of 26.14 ± 9.98 μg/mL and 21.90 ± 8.84 μg/mL were reached at a median tmax of 30 minutes respectively. Bone microdialysate yielded mean Cmax values of 13.15 ± 8.39 μg/mL (mc) and 11.81 ± 6.69 μg/mL (lc), while Cmax values for bone specimen were 5.87 ± 1.34 μg/g.
Figure 1.
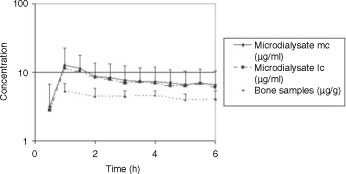
illustrates the mean tissue concentration-time profiles obtained from microdialysates and bone samples.
Conclusions: To achieve concentrations higher than the MIC for susceptible organisms (>4 mg/L) the chosen dose of linezolid was sufficient for bone, bone marrow and serum. It is not surprising that the observed bone concentrations are lower than bone microdialysate concentrations because bone concentrations are given in μg/g. With the use of microdialysis we here present the first results for linezolid bone penetration that are directly comparable to unbound concentrations in other matrices such as serum or bone marrow. From this we conclude that linezolid has an excellent penetration into bone tissue.
Genetic typing for important viral infections: recent technological and conceptual developments (Symposium arranged with ESGEM)
S126: Molecular diversity of new and emerging viruses
B. Mahy (Atlanta, USA)
During the past 15 years, at least 60 new viruses infecting humans have been recognized. In some cases the viruses have been infecting humans for many years, but have only recently been recognized (e.g. Sin Nombre and related viruses causing hantavirus pulmonary syndrome) but in other cases the virus has not previously entered the human population either because it recently emerged from a reservoir host (e.g. Nipah virus or the SARS coronavirus) or was newly introduced from a different geographic location (e.g. West Nile virus in the USA). In the case of the SARS coronavirus, sequence analysis of isolates from several different locations (Vietnam, Germany and Canada) revealed almost no sequence diversity, which is not surprising since these outbreaks could all be traced back to a single infected person in Hong Kong. Similarly, there has been little molecular variation noted in West Nile viruses isolated in the US following the single introduction from Israel to New York in 1999. However, some significant variation has recently been reported following sequencing of isolates from Mexico. It is of interest that the epidemic of haemorrhagic fever caused by Ebola virus in Kikwit, Zaire in 1995, some 19 years after a previous epidemic had occurred there, was caused by a virus with almost identical sequence. This may indicate that Ebola virus had emerged from a reservoir in which the virus is quite stable, with no pressure for sequence change.
Modifying the ribosome as a mechanism of resistance (Joint symposium arranged with ICAAC)
S129: Distinctive ketolide interaction and resistance mechanisms
S. Douthwaite, C. Toft Madsen, J. Poehlsgaard, L. Jakobsen (Odense, DK)
Macrolide antibiotics and their latest generation of derivatives, the ketolides, bind within the peptide tunnel of the bacterial 50S ribosomal subunit. Here, the drugs exert an effective blockade against the growing peptide chain to prevent the synthesis of new bacterial proteins. For inhibition to be effective it is essential that macrolides and ketolides attach securely to their binding site within the tunnel. The primary attachment site of all these drugs is at adenosine 2058 (A2058) in domain V of 23S rRNA. An additional interaction with domain II of the rRNA at around nucleotide A752 is made via the synthetic carbamate-alkyl-aryl substituent in the ketolide telithromycin, and contributes to telithromycin's improved activity. As a consequence of its stronger interaction, there are fewer bacterial isolates that are resistant to telithromycin compared to those resistant to the parent macrolide compound, erythromycin. However, telithromycin resistance has been noted in some strains of Streptococcus pyogenes and members of the Mycobacterium tuberculosis complex. We have analysed the rRNA of these strains to determine the molecular mechanisms of telithromycin resistance. In this presentation, these resistance mechanisms will be compared to those found in other strains of the same genera, which are resistant to macrolides while remaining susceptible to telithromycin.
S130: Resistance mechanisms and the site of action of oxazolidinone antibiotics in the ribosome
A.S. Mankin (Chicago, USA)
Linezolid, a first clinically useful representative of oxazolidinone antibiotics, was introduced in medical practice in 2001. It represented the first principally new class of antibiotics developed in the last 25 years. The site and mode of oxazolidinone action, the nature of side effects and mechanisms of resistance are only starting to be unraveled. Oxazolidinones bind to the ribosome and inhibit protein synthesis in sensitive bacteria. Though oxazolidinones inhibit cell-free translation they bind only weakly to isolated ribosomes, which complicated identification of the site of their action. Therefore, the majority of our knowledge about the site and mechanism of action of oxazolidinones comes from in vivo studies. Crosslinking of photoreactive oxazolidinones to their target in living bacteria revealed the ribosomal peptidyl transferase centre as the main site of oxazolidinone action. The use of various photoreactive derivatives allowed for the accurate modelling of the structure of oxazolidinone drug in the ribosome-bound state. Crosslinking results are in excellent agreement with mutational analysis: all the well-characterized oxazolidinone-resistance mutations are clustered in 23S rRNA at or near the ribosomal peptidyl transferase centre. However, ribosomes of different species show remarkable idiosyncrasy in the type and position of oxazolidinone resistance mutations, suggesting that mutations may have different cost of fitness in ribosomes of different organisms. Oxazolidinone resistance mutations in rRNA are co-dominant and confer resistance even in the presence of wild type ribosomes in the cell. The extent of resistance correlates with the number of ribosomal RNA operons carrying the mutation.
S131: Macrolide-lincosamide-streptogramin resistance by ribosome methylation
R. Leclercq (Caen, F)
Cross resistance to macrolides, lincosamides and streptogramins B (the MLSB phenotype) is spread in a variety of micro-organisms and is due to ribosomal modification by methylation. Nearly forty different erm gene classes responsible for ribosomal modification are distinguished. According to the class of erm gene, the Erm methylases can monomethylate or dimethylate adenine at position 2048 (E. coli numbering) in the 23S rRNA. Generally, each class of erm gene is found in a limited number of bacterial genera. This is the case for staphylococci where three erm genes, erm(A), erm(B), and erm(C) account for nearly all the isolates with the MLSB phenotype and for streptococci where the erm(B) and erm(TR) [a subset of the erm(A) class] genes are widely distributed. Resistance may be expressed constitutively or inducibly regardless the erm determinant. The inducible phenotype is related to translational regulation of resistance and is characterized by dissociated resistance to MLSB antibiotics due to differences in inducing capacity of the antibiotics. In staphylococci, the strains are resistant to 14- and 15-membered ring macrolides which are inducers whereas clindamycin which is not inducer remains active. The use of clindamycin for the treatment of an infection due to an inducibly resistant strain of S. aureus may lead to the selection of constitutive mutants and therefore should be discouraged particularly in the case of infections with heavy inoculum. For the erm(B) gene, when present in streptococci, the spectrum of inducer antibiotics is broader and includes clindamycin and 16-membered macrolides. The MLSB resistance phenotype results from both the type of ribosomal methylation (mono or dimethylation) and of the type of expression of methylase (inducible or constitutive).
S132: Resistance to aminoglycosides in Gram-negative bacteria by 16S rRNA methylation
P. Courvalin (Paris, F)
Despite the development of new β-lactams and fluoroquinolones, aminoglycosides are still used for the treatment of severe infections caused by Gram-negative organisms. There are three known mechanisms of resistance to aminoglycosides in bacterial human pathogens: (i) decreased intracellular accumulation of the antibiotic by alteration of the outer membrane permeability, diminished inner membrane transport, or active efflux; (ii) modification of the target by mutation in ribosomal proteins or 16S RNA; and (iii) enzymatic modification of the drug. Micro-organisms that produce aminoglycosides have developed an additional pathway to avoid suicide: posttranscriptional methylation of rRNA by use of S-adenosyl-methionine as a cofactor. The armA (aminoglycoside resistance methylase) gene was initially found on conjugative Inc L/M plasmid pIP1204 in Klebsiella pneumoniae BM4536. Cloning of the gene in Escherichia coli conferred to the new host high-level resistance to 4,6-disubstituted deoxystreptamines (amikacin, isepamicin, gentamicin, netilmicin, sisomicin, and tobramycin) and to fortimicin by conversion of G1405 N-7 to 7-methylguanosine within 16S rRNA. Plasmid conduction experiments indicated that the armA gene was part of composite transposon Tn1548 together with genes ant3′9, sulI, and dfrXII for resistance to streptomycin-spectinomycin, sulfonamides, and trimethroprim, respectively. The 16.6-kb genetic element is flanked by two copies of IS6 and migrates by replicative transposition. This observation accounts for the presence of armA on self-transferable plasmids of various incompatibility groups and its already world-wide dissemination in members of the family Enterobacteriaceae from human or animal origin and in Acinetobacter baumanni. The deduced sequence of ArmA displayed from 37 to 47% similarity to those of 16S rRNA m7G methyltransferases from various actinomycetes, which confer resistance to aminoglycoside-producing strains. However, the low GC content of armA (30%) does not favor an actinomycete origin for the gene. Two other closely related 16S rRNA methylases, RmtA and RmtB, have been recently reported. It therefore appears that post-transcriptional modification of 16S rRNA can confer high-level resistance to all the clinically available aminoglycosides, except streptomycin, in Gram-negative human pathogens.
Patterns of antibiotic stewardship, use and resistance in European hospitals (Joint symposium arranged with ARPAC and ESAC)
S134: Medical antibiotic use surveillance networks in Germany
W.V. Kern (Freiburg, D)
In Germany, a large country with over 80 million inhabitants and more than 2,000 hospitals in 16 federal states, there have been national surveys of antimicrobial drug prescriptions in ambulatory care published on a yearly basis while hospital antibiotic use databases outside private, economic and market research surveys have not been available until recently. Two antibiotic use surveillance networks, both supported by governmental funds and coordinated by physician-scientists from the University of Freiburg, are now operating in this country. One is, project SARI (Surveillance of Antibiotic Use and Resistance in Intensive Care, http://www.sari-antibiotika.de), an intensive care oriented surveillance programme similar to ICARE. The second is the MABUSE network (Medical Antibiotic Use Surveillance and Evaluation, http://www.if-freiburg.de) that aims at integrating ambulatory and hospital care antibiotic use, and resistance surveillance and research at regional levels. MABUSE projects initially included interhospital comparisons of antibiotic use and expenditures at university hospitals, and ambulatory care antibiotic use surveillance at regional level. The network has now established a hospital antibiotic use database designed for prospective data entry from selected convenience regional hospital samples. ATC/WHO DDDs are used in addition to prescribed daily doses defined according to current practice. Recent MABUSE projects include systemic antifungal use, overall (hospital and ambulatory) antibacterial drug use in selected regions, and linking drug use and resistance surveillance databases. Provided that further funds are available, projects will address a comparison of SARI/MABUSE databases with IMS databases and the definition of a suitable and representative national and regional hospital sample for drug use surveillance via quarterly online data exchange and retrieval. We will discuss our experience with the DDD versus PDD issue, appropriate drug classifications, and reasonable departmental data aggregation.
S136: ARPAC consensus recommendations on antimicrobial stewardship and control of resistance
I.M. Gould (Aberdeen, UK)
ARPAC (Antibiotic Resistance Prevention and Control) is a DG Research Concerted Action funded under the fifth framework. It involved collecting data on antibiotic policies, antibiotic consumption, resistance and infection control policies from over 200 European hospitals. Marked geographic differences were apparent in all but antibiotic policies. There were strong association between both infection control policies and antibiotic consumption versus resistance prevalence and weaker association between resistance and the presence of a hospital antibiotic formulary, drugs and therapeutic committee and educational programmes. The data were presented at a Consensus Conference held in Amsterdam in November 2003 at which expert opinion was synthesised with ARPAC data to draft guidelines for harmonization of policy in these areas at hospital, national and European level. These draft guidelines will be finalised at a meeting at the European Commission in Brussels in February 2005 and will be summarised for presentation at ECCMID. The proceedings of the Consensus Conferences and the draft recommendations are currently available at www.abdn.ac.uk/arpac/.
Combination antifungal therapy (Symposium arranged with EFISG)
S138: Neonatal Candidiasis
F.-M. Müller (Heidelberg, D)
Invasive Candida infections have not only emerged in the adult population, but also in children and especially in neonates (birth weight < 1500 g). Even a fullterm newborn is not immunocompetent and due to a high Candida colonisation rate of the mother during pregnancy, it may develop oropharyngeal candidiasis and diaper dermatitis or congenital cutaneous candidiasis. Candidaemia and disseminated candidiasis is inversely correlated with the gestational age and birth weight: Extremely low birth weight infants (ELBW) have a risk of up to 20% for developing neonatal candidiasis during their stay in the neonatal intensive care unit (NICU). From a recent epidemiological study conducted in Germany, 50% of ELBW infants are colonised with fungi, and from those that develop disseminated infection, the mortality rate is 30%. C. albicans is the most common isolated pathogen (70%), but 23% were non-albicans Candida spp. with C. parapsilosis the leading one. Others so far rare yeasts, such as Trichosporon and Rhodotorula spp. are as well as rare moulds emerging in neonatology. Unfortunately, in general almost 60% of the children and 90% of the newborns receive treatment with unlicensed drugs in Europe, so it's the paediatrician's choice either to prescribe a drug with high efficacy in adults that has not been tested in children or a drug with less efficacy that has been tested in children. Antifungals that are commonly used in paediatrics are conventional and liposomal amphotericin B as well as the azoles fluconazole and itraconazole due to their oral bioavailability. The new antifungals of the next generation triazoles (voriconazole, posaconazole and ravuconazole) as well as the echinocandins (caspofungin, micafungin, anidulafungin) have potentials for the paediatric population due to their broader spectrum, oral bioavailability for the azoles as well as their tolerability and excellent safety profiles. Before these drugs can be recommended in paediatrics clinical trials including pharmacokinetic and pharmacodynamic studies for the different age groups are warranted. In this interactive symposium, clinical cases of neonatal candidiasis will be discussed with special regard to management, potential combinations of new and old antifungals as well as strategies for prophylaxis and empirical treatment.
S140: Combined therapy for central nervous system invasive fungal infections
L. Pagano (Rome, I)
CNS fungal infections are rare but fatal complications, particularly in immunocompromised hosts. The most frequent CNS manifestations, excluding cryptococcosis, are aspergillosis and zygomycosis. These infections typically present with a CNS mass, while candidiasis primarily involves the meninges. The major causes of CNS aspergillosis are acute leukemia and AHSCT. Diagnosis is usually difficult because signs and symptoms are frequently aspecific, and the diagnosis can be often performed only using aggressive procedures, which are impaired by the bad clinical conditions, particularly in patients with acute leukaemia. Treatment includes surgery (removal of abscesses or stereotactic drainage) and the use of antifungal agents. The majority of old and new antifungal drugs do not reach therapeutic levels in brain tissue. Amphotericin B (AmB), also administered at the highest tolerable doses, showed very low efficacy. The efficacy of AmB lipid compounds is higher. In particular, liposomal AmB presents a high diffusion in CNS reaching high therapeutic peak. Furthermore recent published data show that voriconazole may be highly effective for the treatment of CNS aspergillosis. Few data have been reported on combined therapy of this complication and are only based on anedoctal reports. Zygomycetes are the second frequent cause of brain abscesses. They are observed not only in patients with acute leukaemia, but also in the course of other diseases, in particular during ketoacidotic diabetes. CNS involvement is more frequent that in invasive aspergillosis, it is characterized as well by a high mortality rate. In vitro and in vivo studies demonstrated that only posaconazole and L-AmB present some chances of success in the treatment of zygomycosis, but the pharmacological approach should always be associated to surgery. Considering the high mortality rate and the action of these antifungal drugs, the combination of L-AmB and posaconazole may represent in the future the best therapy for this complication
New diagnostic methods for the laboratory
O141: A novel and rapid method for determination of rubella virus immunoglobulin G avidity
M. Eggers, M. Enders, S. Strobel, J. Piche, I. Diz, G. Enders (Stuttgart, D; Marcy l'Etoile, F)
Objectives: Although rare in many industrialised countries, because of the success of vaccination programmes, rubella infection in pregnancy continues to occur where uptake of the vaccine is low and in immigrants of countries with no vaccination programme. As the clinical diagnosis of rubella is unreliable, serological tests are needed for a diagnosis, especially in pregnancy. Diagnosis is usually made by detection of rubella specific immunoglobulin M (IgM). However, in about 2.2% of clinical normal pregnant women investigated by us in prenatal care long persisting IgM antibodies following previous infection or vaccination are detected. Therefore an easy, rapid, and reproducible test to distinguish between long-persisting rubella virus IgM antibodies from IgM antibody response due to a primary infection in early pregnancy is of great importance. The measurement of the avidity of immunoglobulin G (IgG) antibodies has been shown by several investigators to be helpful in identifying or excluding primary rubella infections in pregnant women.
Method: In this study, we adapted this serological technique to the VIDAS system (bioMerieux) using 6 M urea as the dissociating agent. A total of 301 serum specimens were tested: 35 control sera, 50 specimens from women with acute infection, 51 serum samples from women with recent vaccination, 100 serum samples with long persisting IgM, 5 sequential sera from a woman with preconceptional vaccination, 10 sera from women with reinfection in pregnancy after vaccination, and 50 serum samples without IgM from women with past infection or vaccination. To evaluate the performance of this novel VIDAS Rubella IgG avidity test we compared it with the diethylamine denaturation (DEA) procedure used in an in-house version of the laboratory Enders since 1998.
Results: Our results show that the bioMerieux test is easy to use, and that an avidity index higher than 40% allows the exclusion of a recent infection or vaccination: <20% indicates acute infection or recent vaccination during the last 2 months, 20–40% is considered borderline, and >40% indicates past infection or previous vaccination.

Conclusion: This new VIDAS rubella IgG avidity assay is a rapid (50 min), reproducible test with very good performance and is of considerable practical value for decision on the need of prenatal diagnosis, to avoid requesting too many follow up sera and, most important, in preventing unnecessary termination of pregnancy.
O142: Quantitation of cytomegalovirus DNA by real-time polymerase chain reaction in the blood of solid organ transplanted patients: comparison with end-point PCR and pp65-antigen assay
T. Allice, M. Enrietto, F. Pittaluga, S. Varetto, V. Ghisetti (Turin, I)
Background: Cytomegalovirus (CMV) infection is an important cause of morbidity in solid organ recipients. Early markers to identify infection progress are required in order to apply a strategy of pre-emptive therapy whose efficacy relies on accurate laboratory tests to monitor CMV infection. The pp65-antigen test (antigenaemia) is the gold standard for the early identification of CMV infection but the technique is time-consuming with some pitfalls like long hands-on time and the need of a strong experience for the interpretation of the result. The evaluation of CMV DNA by quantitative Polymerase Chain Reaction (PCR) has been introduced for monitoring CMV infection but standardization of the techniques is essential for the clinical interpretation of its results. The recently introduced real-time PCR (RT-PCR) is aimed to offer a more reliable and standardized method than the end-point PCR (EP-PCR) for evaluating CMV dynamic.
Specific aim: The aim of the study was to compare the pp65-antigenaemia with two PCR systems working on peripheral blood leukocytes (PBL): the EP Cobas Amplicor Monitor (Roche, Brachburg, NY, US, detection limit: 100 copies/1 milion PBL) and the RT-PCR CMV (Amplimedical, Buttigliera, To, I, detection limit 100 copies/500,000 PBL). PCR results were referred as Log10/genome/500,000 cells. PBL (n = 158) from 32 solid organ transplanted patients (pts) with CMV infection (20/32 pre-emptive treated with ganciclovir and 12/32 not on therapy due level of pp65 < 30/200,000 PBL) were studied. A pannel of 58 negative specimens by a reference nested-PCR test (10 copies/500,000 PBL) was used to establish the specificity of the EP- and RT-PCRs.
Results: A good correlation was found between pp65 test and both EP-PCR (R2 = 0.88) and RT-PCR (R2 = 0.87) as well as between the two PCR methods (R2 = 0.76). A significantly higher DNA level was shown in pre-emptive treated pts (RT-PCR median value 3.8 Logs, EP-PCR 3.9 Logs) than in pts not on therapy (RT-PCR: 2.9 Logs, EP-PCR: 2.1 Logs: p < 0.0001 for both the two PCRs). Specificity was 98.3% for RT-PCR and 91.5% for the EP-PCR. Sensitivity of RT-PCR and EP-PCR were 100% and 29%, respectively, as tested with 10 copies of a known amount of the reference AD169 strain. In conclusion, our study shows that RT-PCR for CMV DNA quantitation is a highly sensitive and specific tool with a much lower turnaround time (3 hours) than EP-PCR (7 hours) allowing a rapid and early diagnosis of CMV infection in transplanted pts.
O143: Diagnosis of dengue infection by reverse transcription-nested polymerase chain reaction and enzyme linked immunosorbent assay using whole blood stored on filter paper
N. Jaimchariyatam, J. Pupaibool, S. Krajiw, K. Arunyingmongkol, P. Suandork, O. Prommalikit, R. Sittichai, A. Nisalak, C. Pancharoen, U. Thisyakorn, W. Kulwichit (Bangkok, TH)
Objectives: Dengue infection has emerged as a global public health problem. PCR and ELISA are used for diagnosis. We evaluated utilities of PCR and ELISA performed on dried blood spots on filter paper for dengue diagnosis in acute febrile patients.
Methods: A descriptive observational study was conducted in acute febrile pediatric and adult patients at King Chulalongkorn Memorial Hospital, between June 2003 to April 2004. Diagnosis of dengue infection was based on standard serum ELISA assay. Patients tested negative by serum ELISA served as controls. Whole blood (WB) was collected on the first day of admission and again 1–2 weeks after discharge. Dried blood spots were stored on filter paper which was kept at 4 degrees for at least 10 days before testing. Reverse transcription-nested polymerase chain reaction (RT-nested PCR) and ELISA were performed on extracts from the spots. Blood spots with IgM over 40 units and IgM/IgG ratio over 1.8 were considered primary infection cases. Spots with IgG over 100 units were considered secondary cases.
Results: We enrolled 102 patients with dengue infection (6 primary and 96 secondary cases) and 33 patients with other infectious diseases. Dried blood spots from 134 patients (101 cases and 33 controls) were tested by ELISA, and from 80 patients (65 cases and 15 controls) for RT-nested PCR. Positive RT-nested PCR was found in 43 of 65 dengue cases (4 in 5 of primary cases and 39 in 60 of secondary cases) and one of 15 control cases (sensitivity 80% and 65%, specificity 93.33% and 93.33%, positive predictive value (PPV) 97.5% and 97.73%, negative predictive value (NPV) 93.33% and 40% for primary and secondary cases, respectively). Positive ELISA was detected in all dengue and none of control cases (Table).
| Primary cases +ve/total (%) | Secondary cases +ve/total (%) | Controls +ve/total (%) | |
|---|---|---|---|
| Blood spot ELISA | 6/6 (100) | 95/95 (100) | 0/33 (0) |
| Blood spot PCR | 4/5 (80) | 39/60 (65) | 1/15 (6.7) |
Conclusions: RT-nested PCR and ELISA using dried blood spots on filter paper appear to be of diagnostic value for dengue infections. This would prove especially useful in certain areas where immediate laboratory testing is not available. In addition, molecular epidemiologic studies could also be performed in positive-PCR specimens.
O144: Shorter time to identification of pathogens in positive blood cultures by FISH in routine practice
R.P.H. Peters, P.H.M. Savelkoul, A.M. Simoons-Smit, S.A. Danner, C.M.J.E. Vandenbroucke-Grauls, M.A. van Agtmael (Amsterdam, NL)
Objectives: Evaluation of the effects on turnaround time and clinical management of routine implementation of fluorescent in situ hybridisation (FISH) for identification of pathogens from positive blood cultures.
Methods: FISH was performed on growth-positive blood culture fluids simultaneously to conventional identification. A selection of probes was used that should identify >95% of pathogens most commonly found in blood cultures. To determine the clinical impact of FISH identification, results and time points were compared between conventional identification and FISH.
Results: One-hundred and fifty blood cultures were included. FISH allowed identification of 117 pathogens (78%) at the species level (table 1). For pathogens identified at the genus level or with eubacterial probes no species specific probes are available, including Enterobacter cloacae and Proteus mirabilis. Identification was suboptimal in 3 cases: 2 with Staphylococcus aureus that were identified as Staphylococcus species and 1 with Escherichia coli that was identified as a lactose fermenting rod. In 8 cases no micro-organisms were found with Gram-stain and FISH. Average time to identification with FISH was 3.5 hours for gram-negative and 4 hours for gram-positive organisms. Compared to preliminary identification (coagulase, optochine, oxidase) FISH results were available 70 minutes earlier (p < 0.001); for definite conventional identification time gain was approximately 16 hours (p < 0.001).
Conclusion: Identification by FISH correlates well with conventional culture identification. In three cases identification with FISH was suboptimal because of difficult interpretation of fluorescence due to the presence of large amounts of protein and cells. The panel of probes should be extended to permit identification of >95% of pathogens; based on the results from our study probes for Enterobacter cloacae and Proteus mirabilis would be of interest. FISH allows faster identification compared to conventional methods in a routine setting. This can be especially useful for blood cultures that are growth-positive in the afternoon. For these, FISH results will be available the same day with treatment benefits for the patient, whereas conventional identification will require overnight incubation. If the turnaround time of the FISH procedure could be further decreased and the panel of probes extended, FISH would provide a valuable diagnostic improvement to the microbiological laboratory.
Table 1.
Maximum level of identification of pathogens identified in culture (n = 148)
| Pathogen in culture | Total | Species | Genus | Eubacterial |
|---|---|---|---|---|
| Gram-positive | ||||
| Coagulase negative staphylococci | 71 | 71 | – | – |
| Staphylococcus aureus | 14 | 12 | 2 | – |
| Streptococcus pneumoniae | 2 | 2 | – | – |
| Streptococcus pyogenes | 1 | 1 | – | – |
| Enterococcus faecalis | 2 | 2 | – | – |
| Enterococcus faecum | 1 | 1 | – | – |
| Other | 11 | – | 8 | 3 |
| Gram-negative | ||||
| Escherichia coli | 14 | 13 | – | 1 |
| Klebsiella pneumoniae | 5 | 5 | – | – |
| Pseudomonas aeruginosa | 5 | 5 | – | – |
| Enterobacter cloacae | 6 | – | – | 6 |
| Proteus mirabilis | 4 | – | – | 4 |
| Other | 8 | – | – | 8 |
| Yeast | ||||
| Candida albicans | 3 | 3 | – | – |
| Candida tropicalis | 1 | 1 | – | – |
| Total | 148 | 116 | 10 | 22 |
NB. Two pathogens were identified in 6 blood cultures
O145: Detection of Salmonella antibodies by flagella-based ELISA has potential for diagnosis of acute gastroenteritis
T. Dalby, M. Strid, K.A. Krogfelt (Copenhagen, DK)
Objectives: Diagnosis of human gastrointestinal salmonellosis is traditionally done by fecal culturing and agglutination assays. An automatized ELISA is an obvious candidate for a more reliable, fast and easy method of diagnosis. An indirect ELISA employing repolymerized flagella antigens was developed and evaluated.
Methods: Two automatized indirect ELISAs employing re-polymerized Salmonella flagella were developed; H:[g, m] flagella respectively H:[i:1,2] flagella were used. Both IgA, IgM and IgG antibodies were detected. Sera from 153 Danish patients diagnosed with infection by Salmonella enteritidis (SE) and from 150 Danish patients diagnosed with infection by Salmonella typhimurium (ST) were obtained and analysed. Most patients delivered blood-samples at approximately one, three and six months after onset of salmonellosis. Cut-off values were determined as the 90 percentile when analysing sera from more than 100 healthy, Danish blood-donors.
Results: The developed ELISAs proved reliable, and at approx. one month after onset of salmonellosis, anti-flagella antibodies were detected with 70% of the SE-patients and 77% of the ST-patients; in comparison, a combined O- and H-agglutination assay detected only 44% of the SE-patients and 8% of the ST-patients. Three months after onset of salmonellosis, just 46% of the SE-patients were detected as were 40% of the ST-patients. Six months after onset, these detection-rates had decreased to 34% and 38%. Crossreactions between H:[g, m] and H:[i:1,2] anti-flagella antibodies were found. Similarly, crossreactions to antibodies against other gastrointestinal flagellated bacteria were observed.
Conclusion: An indirect flagella-based ELISA was found to be superior to the standard O- and H-agglutination assay in identifying patients suffering from gastrointestinal salmonellosis. Moreover, the found sensitivities of 70% and 77%, respectively, will most likely improve if acute-phase sera are analysed; as will be the case if the ELISA is to be employed for diagnosis. The ELISA was not able to discriminate between infections caused by Salmonella enteritidis and Salmonella typhimurium, and crossreactions to other bacteria were observed as well. An improvement of the specificity could possibly be achieved by changing the antigen from re-polymerized flagella to monoclonal flagellin fragments. The level of anti-flagella antibodies was found to decrease rapidly succeeding a case of gastrointestinal salmonellosis.
O146: Exploring a pathogen's gut feelings: molecular characterisation of the mechanisms of gastrointestinal persistence of the foodborne pathogen Listeria monocytogenes
R. Sleator, C. Hill (Cork, IRL)
In 1999, the US Centres for Disease Control and Prevention estimated that ∼2500 cases of human listeriosis, including 500 deaths, occur annually in the United States. Given that the majority of human listeriosis cases are associated with consumption of contaminated food, the ability of Listeria monocytogenes to survive during gastrointestinal passage is fundamental to disease transmission.
Objectives: To identify the molecular mechanisms underpinning listerial growth and survival in the upper small intestine.
Methods: Pre-genome mutational analysis, using transposon (Tn917) and suicide plasmid (pORI19) approaches, based on functionality, coupled with post-genomic in silico analysis of the complete genome sequence, to identify potentially important loci, based on homology.
Results: On entering the upper small intestine Listeria first encounter an osmotic challenge, equivalent to 0.3 M NaCl (∼twice the osmolarity of the blood). Further along the intestinal tract the liver secretes up to a litre of the ‘biological detergent’ bile into the duodenum each day, representing an additional serious challenge to the pathogen. We identified three gene systems in L. monocytogenes which contribute to gastrointestinal persistence and virulence by allowing the bacterium to evade these stresses. Firstly, OpuC, a membrane transporter, facilitates the uptake of carnitine, an osmoprotective compound which allows the bacterium to overcome the osmotic challenge. Resistance to bile on the other hand is achieved initially by excluding the detergent from the bacterial cell and subsequently, if this defence is breached, by detoxifying internalised bile. We identified two bile resistance mechanisms; BilE which functions as a bile exclusion system, and BSH a bile salt hydrolase which degrades internalised bile. Furthermore we reveal that all three systems are co-ordinately regulated by the alternative stress related transcriptional factor SigB, and PrfA the master regulator of virulence potential in L. monocytogenes.
Conclusions: The salt and bile resistance mechanisms: OpuC, BilE and BSH, co-ordinately regulated by SigB and PrfA, play an important role in listerial gut colonisation and virulence potential.
O147: Epidemiological and microbiological investigation of a gastroenteritis outbreak caused by norovirus group II in a military unit
S.L.A. Tan, J.P.J. Loh, H.Y. Lo, B.H. Poon, C.W. Liaw, B.H. Tan (Singapore, SGP)
Background: A gastroenteritis outbreak affecting a total of 92 military personnel who attended a dinner function was detected in January 2004.
Objective: The objective of the investigation was to determine the cause of the outbreak and to institute appropriate preventive measures to prevent similar incidents from occurring in the organization.
Methods: The investigation consisted of epidemiological, laboratory and public health sanitation investigations. Epidemiological investigation included case definition formulation, case identification, contact tracing, active case surveillance, a case-control survey using a self-administered structured questionnaire and statistical analysis of the survey results. Laboratory investigation comprised of analysis for enteric bacterial and viral pathogens using culture and polymerase chain reaction (PCR) techniques. 9 stool samples were obtained from amongst the affected patients. 4 of these samples were sent for stool culture for Salmonella, Shigella and Vibrio spp. 5 of the samples were sent for PCR analysis for Vibrio cholerae, Vibrio parahemolyticus, Shigella spp and Norovirus. Public health sanitation investigations involved environmental inspection and hygiene practices auditing. Results: 92 cases were identified out of approximately 500 participants (∼18.4%) of the dinner function. The predominant symptoms among the cases were diarrhoea (92%), vomiting (80%) and fever (71%). The median onset of the symptoms was 28.5 hours from the time of the dinner function. Consumption of raw oysters was found to be significantly associated with illness (p < 0.001). All the stool cultures were found to be negative. PCR analysis of the 5 samples were negative for Vibrio cholerae, Vibrio parahemolyticus, Shigella spp. 4 of the 5 PCR samples tested positive for Norovirus Group II. Water samples were obtained from the venue and these were found to be negative for coliforms. The public health sanitation investigation showed that there was no lapse in the hygiene practices.
Conclusion: The outbreak was most likely to be due to the contamination of the raw oysters by Norovirus based on the symptomatology of the affected cases, results of the food survey and the positive results from the stool PCR analysis for Norovirus.
O148: Rapid culture-independent monitoring of gastrointestinal flora changes by PCR-based denaturing HPLC
O. Goldenberg, G. Marjoram, S. Herrmann, A. Fischer, M. Noyer-Weidner, S. Bereswill, U. Göbel (Berlin, D)
Objectives: Antibiotic treatment causes drastic changes in the gastrointestinal flora leading to complications such as diarrhoea. To acquire novel insights in the composition of the gastrointestinal microflora during antibiotic therapy, we established a rapid culture-independent molecular approach, allowing both global monitoring of the intestinal microflora, as well as identification of individual species.
Methods: Intestinal bacteria were detected in total DNA isolated from stool samples by amplification of the 16S rRNA genes (variable regions V6 to V8). The amplicons were separated by denaturing high-performance liquid chromatography (DHPLC) with the WAVE system from Transgenomics Inc..
Results: The DHPLC peak-profiles of the PCR products were representative for the dominant intestinal bacterial groups. The applicability of the method was evaluated on 100 stool samples taken from 45 patients at various points during antibiotic therapy. The comparison of DHPLC profiles with band patterns generated by denaturing gradient gel electrophoresis (DGGE) revealed that both techniques reproducibly detected the reduction in the bacterial diversity during antibiotic treatment. Furthermore, DHPLC and DGGE allowed the identification of resistant bacterial species.
Conclusions: PCR-based DHPLC allows a rapid monitoring of the intestinal microflora and the technique is superior to DGGE for identification of bacterial species by sequencing of DNA from individual DHPLC fractions, as the DNA is easily sampled and kept in solution. The technique is well-suited for the global analysis of changes in complex microbial communities. The identification of bacterial species residing in patients receiving antibiotic treatment will guide novel therapy regimens, reducing the risk of complications.
O149: Supplementation of CHROMagar with Pal's medium for rapid identification of Candida dubliniensis
S. Ismail, M.D. Moragues, E. Eraso, M. Villar Vidal, G. Quindós, J. Pontón (Bilbao, E)
Objective: To obtain a simple and rapid medium to identify C. dubliniensis.
Methods: 142 strains of Candida species were studied (30 C. albicans, 100 C. dubliniensis, 3 C. krusei, 3 C. glabrata, 3 C. guilliermondii, 2 C. parapsilosis, and one C. tropicalis). Strains were grown simultaneously on Pal's agar (sunflower seed agar) at 30°C for 48–72 h, CHROMagar Candida (CHROMagar, France) at 37°C for 24–48 h, and CHROMagar Candida supplemented with Pal's medium (CH-P agar) at 30°C for 24–48 h. Plates were examined visually by two investigators for colour and colony morphology. Chlamydospores were detected microscopically. The isolates were previously identified by conventional mycological methods and confirmed by PCR.
Results: Ninety-six out of 100 C. dubliniensis isolates (96%) formed rough colonies on Pal's agar, 75% showed hyphal fringe and 93% produced chlamydospores. All C. albicans formed smooth colonies without hyphal fringe and failed to produce chlamydospores. All C. parapsilosis and C. krusei isolates formed rough colonies. The remaining Candida species formed smooth colonies but none of them produced chlamydospores. Fifty-eight out of 100 (58%) C. dubliniensis isolates grew as smooth dark green colonies on CHROMagar Candida and 42% as smooth light green colonies. Thirteen out of 30 (43.3%) C. albicans isolates formed light green smooth colonies and the remaining 56.6% formed green and dark green smooth colonies. The other Candida species developed different colours. Ninety-six out of 100 (96%) C. dubliniensis isolates grew as rough colonies on CH-P agar. Seventy-five formed hyphal fringe and 93 produced chlamydospores. Ninety-four isolate gave a bluish green colour that was easy to distinguish from C. albicans colony colour. All C. albicans isolates formed smooth light green colonies failing to produce neither hyphal fringe nor chlamydospores. Other Candida species formed smooth or rough colonies but with a distinguishable colour, and none of them was able to form chlamydospores.
Conclusion: None of the individual media allowed a reliable identification of C. dubliniensis. However, the characteristic colour and colony morphology, as well as the abundant production of chlamydospores presented by most C. dubliniensis isolates on CH-P allows the rapid and reliable one step identification of this species.
Acknowledgements: This work has been funded by projects CO3/10 of FIS-Spain and IE019 of ETORTEK-Basque Government.
O150: Evaluation of multiplex real-time PCR assay to discriminate Staphylococcus aureus from coagulase-negative staphylococci and determine methicillin resistance from culture and human sera
S.A.H. Awad, M. Guiver, J.P. Burnie, I. Alshami, M. Upton (Manchester, UK)
Objectives: Methicillin-resistant Staphylococcus aureus (MRSA) is a major cause of Nosocomial infection with a world-wide prevalence. Early detection of MRSA is important in both patient management and the prompt implementation of infection control procedures. Molecular methods can be used to detect the presence of the mec A gene and hence methicillin resistance in both S. aureus and coagulase negative staphylococci (CNS). Furthermore, detection of a second target, fem A, which is specific for S. aureus and absent in CNS allows detection of both species and methicillin resistance. In the present study, a multiplex RT-PCR assay was established and evaluated to detect MRSA in culture and human sera seeded with MRSA using both of these gene targets and a Qiagen extraction kit. The new assay measures, in real-time, PCR product accumulation by means of dual labelled fluorogenic probes FAM and VIC.
Methods: Strains representing EMRSA types 1–17 were examined for mecA and fem B. In addition, 83 strains of MRSA collected from Manchester Royal Infirmary (MRI) were tested. 35 isolates of a number of different species, including Methicillin-sensitive Staphylococcus aureus (MSSA), Methicillin resistant Staphylococcus epidermidis (MRSE), Methicillin- sensitive Staphylococcus epidermidis (MSSE), Streptococcus pyogenes, Campylobacter and Escherichia coli from MRI and an in house culture collection, were tested to determine the specificity of the assay.
Results: Amplification of mecA and fem B was correct for all staphylococcal isolates with the exception of two strains. The first was mec A negative. The second was negative fem B, but after further investigations it was CNS. These two isolates were phenotypically methicillin resistant. Serial dilutions were done to determine the sensitivity of this method, which was able to detect as few as 1.5 × 102 cells per ml.
Conclusion: This multiplex RT-PCR assay represents a rapid, sensitive (% 99), specific (% 100) and accurate assay for the detection of MRSA with potential for direct detection of MRSA from clinical specimens.
Hospital infection: new sources and solutions
O151: Should doctors wear ties?
I. Ditchburn, P. Willson, A.P. Gibb (Edinburgh, UK)
Objectives: To assess the risks and benefits of doctors wearing ties.
Methods: Subjects were randomly selected at the New Royal Infirmary of Edinburgh. Samples from 40 doctors’ ties were incubated, bacterial colonies were counted, and Staphylococcus aureus and methicillin-resistant Staphylococcus aureus (MRSA) colonies were identified. Doctors were asked when the tie had last been cleaned. 100 participants were asked a questionnaire regarding attitudes to doctors not wearing ties. Previous related literature was reviewed.
Results: The mean bacterial colony count on a doctor's tie was 68 and the distribution of colony counts was broad (s.d: 94). 20% of doctors’ ties carried S. aureus. 2.5% carried MRSA. 70% of doctors had never cleaned their tie. 93% of respondents did not object to doctors not wearing ties. Factors that were considered to be more important were: wearing a shirt; being clean and tidy; being smart; wearing clear identification; and wearing trousers not jeans.
Conclusions: MRSA can be found on ties. Current research suggests that doctors’ ties can carry dangerous pathogens, that these pathogens can survive on ties for lengths of time long enough to allow cross-infection, that bacteria may be transferred to doctors’ hands, that bacteria may be transferred directly from dangling tie-to-patient and that ties are a potential source of cross-infection. A large majority of people do not object to doctors not wearing ties. The tie may be taken away without damaging a doctor's professional integrity or the doctor-patient relationship, provided other desirable attire remains. Ties are associated with a risk of transferring pathogens, and are of little obvious benefit.
O152: A hospital-wide outbreak of Pseudomonas aeruginosa infections associated with the use of bottled mineral water
T. Eckmanns, M. Martin, K. Weist, H. Rüden (Berlin, D)
Objectives: Mineral water (MW) should be free of P. aeruginosa according to the legal force of the mineral and table water act in Germany. We investigated an outbreak of P. aeruginosa where the pathogen was introduced into the hospital by MW in bottles.
Methods: One medical intensive care unit (ICU) noticed an increase of pneumonias with P. aeruginosa. Environmental samples (tap water samples, siphons, surfaces, equipment for oropharyngeal hygiene, MW bottle) from the unit were cultured and typed. Clinical P. aeruginosa isolates were collected from five further ICUs. Microbiologic results were reviewed to determine the numbers of P. aeruginosa on a weekly time scale for the ICUs. All isolates were genotyped by PFGE and an AFLP PCR-method.
Results: Clinical specimens from five medical ICU patients yielded the same P. aeruginosa strain. In 4 from 103 environmental samples (3 × siphon, 1 × MW) P. aeruginosa was isolated. The isolates of the siphons were different to all patient isolates. The MW isolate was genetically indistinguishable to the 5 ICU patient isolates. Later the same strain was isolated in 4 more MW bottles of the same batch and in clinical specimens from 3 more medical ICU patients and seven patients of five other ICUs, respectively. Ten of the total 15 patients with P. aeruginosa developed pneumonia. After recognising the outbreak and the potential source delivery of this mineral water to the patients was stopped. The mean number of all ICU patients with newly detection of P. aeruginosa was 3.8 per week (Std. Dev. 1.6) in the 42 weeks prior to the outbreak. During the 6 weeks of the outbreak the weekly occurrence of new P. aeruginosa was 6, 6, 10, 9, 3, and 9 respectively (mean 7.2). In the four weeks after the outbreak on the ICUs the mean weekly occurrence of new patient with P. aeruginosa was 3.3.
Conclusions: This hospital wide outbreak was related to bottled MW contaminated with P. aeruginosa. The water was drunken by patients with tracheostomy tubes and used for oral (enteral tube) drug preparation. The outbreak ceased after determining the delivery of MW of this brand to the patients. Production control of MW needs to be improved and use of MW for ICU patients, especially those with endotracheal ventilation may increase the risk of nosocomial pneumonia.
O153: Aerobiocontamination of moulds: epidemiology and influence of on invasive fungal infection in a tertiary care hospital
A. Imhof, M. Spiess Pangrazzi, C. Ruef (Zurich, CH)
Objectives: Nosocomial aspergillosis, is thought to be caused primarily by Aspergillus organisms in the air. We conducted this study to asses the role of mold concentrations of ambient air and the impact of various weather conditions on mold concentration inside the hospital.
Methods: Air sampling was conducted in 18 areas (6 outdoors) of our hospital (1000 beds, tertiary care) two times a week. The weather conditions were monitored at the day of sampling. Surveillance of Nosocomial Aspergillus infection was conducted by reviewing the records of all hospitalised neutropenic patients from 4/2004 to 10/2004.
Results: During the study period a total of 614 air samples were available of which 514 (84%) revealed at least one fungal colony. Aspergillus sp. (AS) were isolated most frequently (mean 12 cfu/m3 of air), followed by Zygomycetes (zyg) (0.6 cfu/m3) and other molds (3 cfu/m3). A. niger (mean 3 vs. 2 cfu/m3), A. flavus (1.5 vs. 0.3 cfu/m3) and A. terreus (0.2 vs. 0.01 cfu/m3) were found more frequently inside the hospital, whereas A. fumigatus was more common outdoors (10 vs. 7 cfu/m3). During a short time of renovation activity, colony counts of AS (OR: 2.93, 95% CI 1.58–5.43) and zyg (OR: 4.08, 95% CI 2.29–7.29) increased significantly. Fungal growth was highest at 19–22 °C (42% of isolates), in particular AS (OR: 1.62, CI 1.04–2.54) and zyg (OR: 3.53, CI 1.54–8.09). On rainy days, there were significantly higher chances of growth of AS (17 vs. 8 cfu/m3, p = 0.003) and zyg (0.5 vs. 1, p = 0.024) than during other weather conditions. High risk patient with leukemia or bone marrow transplantation were hospitalized during the study period. The number of neutropenic days was 635 with a mean of 31.6 days. Invasive mold infection was diagnosed In 10 patients (53%), and one of them died due to this infection.
Conclusion: Our observations show relatively high concentrations of A. fumigatus in all environments, with a significantly increased amount of AS spores on rainy days. Our investigation suggests that exposure of high risk patients to high concentration of spores is a continuous risk for invasive fungal infections.
O154: Detection of occult blood as a marker for IC practice
S. Mehtar, O. Shisana, T. Mosala, F. Gxamza (Cape Town, ZA)
Objectives: The purpose was to evaluate Infection Control (IC) practice using occult blood (OB)on clinical and non items used in dental and paediatric HCF as a marker for good IC practice.
Methods: In a South African province all dental and paediatric facilities were surveyed for IC practice. The presence of OB in the environment and on critical care items were tested just prior to use on the next patient. on site sampling was carried out using a rapid immuno-chromatographic method (OBTI) (used in forensic analysis), capable of detecting 1:100000 Hb; a negative result reflected adequate cleaning or heat sterilization.
Results: Overall, 31/110 (25%)and 15/41 (37%) of dental items tested were positive for OB, mainly found on extractor forceps, drill heads and probes. In the maternity & baby units, overall 25% o clinical equipment tested positive, particularly in the labour and maternity wards. The findings reflect poor levels of IC practice and training, but most importantly the cleaning & sterilization of critical equipment was inadequate.
Conclusions: We found the OBTI test kit useful as a rapid test method while investigating IC practice particularly in poorly resourced settings. The test can be performed by on site, with minimum training and is an effective tool in assisting with IC evaluation. In countries with a national HIV prevalence of 20%, the presence of visible or occult blood on critical items of clinical equipment services, the possible risk of nosocomial transmission cannot be ignored. It is therefore essential that a test which can help to visualise probable risk of transmission will also serve as an effective teaching tool in IC and hygiene.
O155: Nurse-to-patient-ratio as risk factor for nosocomial primary bloodstream infection in ICUs
T. Eckmanns, S. Bärwolff, M. Behnke, H. Grundmann, H. Rüden, P. Gastmeier (Berlin, D; Bilthoven, NL; Hannover, D)
Objectives: Nosocomial primary bloodstream infections (BSI) cause significant morbidity and mortality among hospitalized patients and have an enormous economic impact. In several studies understaffing was identified as a risk factor for outbreaks of BSI. However, little is known about the influence of nurse-to-patient-ratios on BSI in endemic situations on ICUs. We investigated the nurse-to-patient-ratio as a possible risk factor for BSI in an endemic situation.
Methods: A prospective cohort study was done to identify exposures associated with cases of BSI. During an 18-month period all patients who were in one of two ICUs (A = 12 and B = 24 beds) for more than 3 days were included. Data collected on admission and discharge: admission date, age, sex, SAPS II, infections on admission, discharge date. Additional data collected during hospital stay: days on ICU, intubation, urinary tract catheter, central venous catheter, dialysis, surgical procedure during the stay on the ICU, and SOFA. Daily bed occupancy and nurse staffing on the ICU were also recorded. Nurse-to-patient ratio was determined by dividing nurse staffing by the patient density. Risk factor analysis included univariable approach and Cox proportional hazards regression analysis.
Results: In total 801 patients were treated in the two ICUs. There was no difference between patients with BSI and patients without BSI concerning mean of age, distribution of sex, average stay on ICU of patients with no BSI and average duration between admission and diagnosis of BSI of case patients, and numbers of infections on admission in the two groups. Patients with BSI had a significant higher SAPS II on admission as patients who developed no BSI. 21 patients (2.6%) had a BSI. The nurse-to-patient ratio of ICU A was 0.86 and of ICU B 0.91. The overall nurse-to-patient ratio in patients without BSI was 0.90 and in patients with BSI was 0.87. The Hazard ratio of nurse-to-patient ratio in the Cox analysis was 0.61; p = 0.04, that means patients with average higher nurse-to-patient ratio per day had less BSIs.
Conclusions: BSI is highly dependent on hygienic behaviour. The result of the study underlines that staffing is an important point in patient safety in hospitals. To our knowledge is this the first study which investigated the influence of staffing on endemic BSI in one hospital where the patient was the unit of analysis.
O156: Efficacy of nosocomial infection control in urological patients: building benchmarking through active surveillance
A. Agodi, M. Barchitta, A. Anzaldi, F. Marchese, A. Bonaccorsi, P. Bellocchi, P. Cantaro, M. Motta (Catania, I)
Objectives: Many studies have suggested that disseminating Nosocomial infections (NI) risk-adjusted reliable infection rates obtained through surveillance to healthcare personnel (HCP) and establishing a link with prevention efforts is essential for successful control. Our study goals were: i) to evaluate the efficacy of feeding back NI surveillance data to HCP of a Urologic Clinic and ii) to provide indicators useful for benchmarking within and between surgical wards.
Methods: Active surveillance was performed at the Urologic Clinic of an Italian University Hospital, in accordance with the methods, protocols and definitions of the National Nosocomial infections Surveillance (NNIS) System, USA. A first 1 month-surveillance survey was conducted in June–July 2002 and data recorded and analyzed. Diagnosis was based on CDC definitions for NI. Each suspected infection was discussed and validated by the epidemiologists, infection control personnel and surgeons. Indicators were calculated including site specific NI incidence and incidence density rates. At the end of the study a feedback session was held and results were communicated and discussed with the staff. A second study was planned and performed as a 4 months-surveillance survey from April to July 2004. Surveillance data were analyzed and compared.
Results: The cumulative incidence of NI decreased from 8.0% patients in 2002 to 2.3% in 2004 and incidence density from 11.5‰ patient-days to 3.2‰ (p < 0.05, chi square test). Symptomatic urinary tract infections were not detected in 2002 while in 2004 their incidence was 1.4‰ patient-days, 13.04‰ catheterized patients and 3.04‰ patient-days of catheterization. Surgical site infections (SSI) incidence and incidence density decreased respectively from 5.4% patients to 1.3% and from 7.7‰ patient-days to 1.8‰ (p < 0.05). SSI rates by operative procedure and NNIS risk index category decreased from values above the 90th percentile of NNIS distribution to values between the 75th and the 90th percentile.
Conclusions: Few surveillance data have been published on NI rates in urological patients. Our study represents a contribution to building specific benchmarking and an example of successful control of NI in a urology ward. Several explanation may be suggested to have prevented infections, but the role of feeding back information to ‘those who need to know’, changing personnel behaviour and improving the quality of patient care is shown to have been critical.
O157: Validation and improvement of an automated surveillance system for nosocomial bacteraemia
C. Bellini, C. Petignat, P. Francioli, A. Wenger, J. Bille, A. Klopotov, Y. Vallet, R. Patthey, G. Zanetti (Lausanne, CH)
Objectives: We developed a computerized automated surveillance system (ASS) for bacteraemia in a 850-bed university hospital. The aims of this study were to validate ASS-generated results and to identify possible improvements.
Methods: The ASS was based on a computerized data warehouse that included laboratory data (date of all blood and catheter cultures, and species identification and antibiotic susceptibility testing in positive cultures) and demographic data (patients’ ID, ward, and date of admission). Algorithms distinguished true bacteraemia from contamination (culture of a possible contaminant in one of several blood samples), nosocomial bacteraemia (positive culture of blood drawn >48 hours after admission), and catheter-related bacteraemia among the latter (same bacteria with the same antibiotic susceptibility in blood and on IV catheter cultured simultaneously ±6 days). Bacteremias that occurred more than 3 days apart were considered distinct episodes. We reviewed all positive blood cultures classified by the ASS as nosocomial bacteraemia not related to a catheter in adult patients admitted over 2 years on the following wards: surgery, medicine, and medical and surgical ICUs. The gold standard for validation of classification by the ASS was a manual review of patients’ charts using the CDC criteria for nosocomial infections.
Results: The ASS identified 154 nosocomial bacteraemia not related to a catheter. 106/154 (69%) were confirmed by chart review (77% in medicine, 60% in surgery, and 73% in ICU). There were 3 reasons for misclassification by the ASS: a late documentation of community-acquired bacteremias in 3/154 (2%) cases; the absence of catheter culture in 25 (16%) cases of bacteraemia clinically attributed to catheter infection; and duplication of bacteraemia sustained over >3 days in 20 (13%) cases (13 of which being fungaemia in surgical patients). We explored 2 alternative uses of available data to improve ASS performance: 1) attributing all coagulase-negative bacteremias to catheter infections led to correct classification of 8/154 (5%) more cases at the price of 2 additional misclassifications; 2) expending the time interval to 10 days for definition of duplicates in case of fungaemia allowed correct classification of 11/154 (7%) cases at no cost. The ASS accurately classified nosocomial bacteraemia not related to catheter in 78% of the cases by implementing both strategies.
Conclusion: ASS is a promising alternative to manual surveillance of nosocomial bacteraemia.
O158: Rise and fall of Acinetobacter baumannii bloodstream infections: efficacy of a multifaceted intervention
M. Paul, B. Rubinovitch, R. Holinger, H. Konisberger, Z. Samra, S.D. Pitlik, M. Weinberger (Petah Tikva, IL)
Background: During the years 1997–2001 a hospital-wide sustained rise in the incidence of multi-drug resistant (MDR) Acinetobacter baumannii (AB) bloodstream infections (BSI) was observed in our centre, a 900-bed primary and tertiary care university hospital catering an adult population. While control of single source outbreaks has been reported, data on hospital-wide endemic situations are scarce.
Methods: A prospective BSI surveillance system in on going in the hospital since 1988. MDR AB was defined by resistance to all antimicrobials except carbapenems, ampicillin-sulbactam or amikacin (excluding colistin). Blood cultures were processed using Bactec 9240 (Becton Dickinson, USA) and antibiotic susceptibilities were tested by disc diffusion. Intervention: In 2002 intensive staff education and multiple interventions were initiated hospital-wide. Alcohol-based hand-rub solution was distributed in patients’ rooms and on patients’ beds in intensive care units (ICU). Hand hygiene guidelines were implemented and reinforced. All cleansing protocols and housekeeping procedures were reviewed and mended. A laboratory alert for AB isolates was installed; patients colonised or infected with MDR strains were placed in contact isolation for the duration of their hospitalisation. Infection control personnel rigorously surveyed isolation policy. Restriction of carbapenem use was reinforced.
Results: Between 1997–1999 the overall incidence of AB BSIs increased 3-fold from 0.8 to 2.4 per 1000 admissions and from 4.3 to 36.9 in ICU (9-fold, figure). Incidence persisted until 2002 and during this period AB was the primary BSI acquired in hospital. From 2002 to 2003 the incidence dropped by 42% overall (2.7 to 1.6 per 1000 admissions) and by 70% in the ICU (45.9 to 14.3). Carbapenem consumption in ICU decreased from 4.9 gram per admission in 2002 to 3.6 in 2003.

Crude mortality was 62.2%. The most common identified source of BSIs was pneumonia (32%), followed by catheter-related infection (6%). Source remained unknown in 36.8% of cases. Resistance rates are shown in the table.
Resistance rates of AB BSI isolates %
| Hospital stay prior to positive culture |
||
|---|---|---|
| <48 hours (n = 68) | >48 hours (n = 464) | |
| Ampicillin-sulbactam | 5.4 | 14.4 |
| Imipenem | 10.7 | 48.3 |
| Amikacin | 43.3 | 65.4 |
| Ceftazidime | 73.1 | 85.9 |
| Ciprofloxacin | 76.1 | 89.7 |
| Colistin | 0 | 0.9 |
In the last study year, 2003, 45% of AB BSI isolates were resistant to carbapenems and 25% to ampicillin-sulbactam.
Discussion: A multifaceted intervention emphasizing environmental and hand hygiene, contact isolation and restriction of carbapenem use has contained a sustained epidemic of AB and reversed a dramatic increase in BSIs in our centre.
O159: Emphasis on quality of hand disinfection and catheter care increases quality of and compliance with hand disinfection and reduces the incidence of catheter-related bloodstream infections
W. Zingg, A. Imhof, E. Ehrenreich, C. Ruef (Zurich, CH)
Objective: To study the impact of teaching interventions on the compliance of hand disinfection by healthcare workers (HCW) in ICU and on the rate of central venous catheter-related bloodstream infection (CR-BSI) in ICU patients.
Methods: Prospective surveillance of CR-BSI in 5 ICUs (cardiac surgery, neurosurgery, general surgery, trauma surgery, internal medicine) of a large teaching hospital using CDC definitions and methods during two periods (baseline [period I, September–December '03, 501 patients, 6'648 catheter days], postintervention [period II, March–July '03, 501 patients, 7'382 catheter days]. Observation of compliance with hand disinfection during both periods. Teaching of standards of catheter care and proper technique of hand disinfection between the two periods during multiple teaching sessions in small groups.
Results: Compliance of HCW in ICU with hand disinfection was significantly higher during period II than during period I (65% versus 59% overall). Overall compliance with hand disinfection was higher after patient contact than before patient contact. The proportion of technically correct hand disinfection increased from 22.5 to 42.6% overall (before patient contact from 26% to 45%, after patient contact from 21 to 56%). The incidence density (infections/1000 catheter days) of CR-BSI was 4.4 during period I and 1.4 during period II (p < 0.001). CR-BSI was a highly significant risk factor for a lethal outcome (8.8% in both periods): odds ratio 2.7 [period I], 2.65 [period II]. Independent risk factors for the development of CR-BSI were: catheter use >7 days, length of stay >10 days, Charlson index 3, presence of a nosocomial infection at another anatomical site. Gram positive bacteria were responsible for 81% of CR-BSI, followed by Candida spp. (10.8%) and gram negative bacteria (8.1%).
Conclusions: Teaching of standards of catheter care as well as indications and proper technique for hand disinfection are successful interventions to reduce the rate of CR-BSI. While overall compliance with hand disinfection was relatively high compared with published studies, disinfection was frequently performed using inadequate technique. Monitoring of compliance with hand disinfection should include some parameters that allow to assess the quality of hand disinfection as well. As many identified risk factors of CR-BSI are not modifiable, strategies to reduce the risk of CR-BSI should focus on the quality of catheter care and hand disinfection.
O160: Prevention of urinary tract infection in spinal cord-injured patients: safety and efficacy of a weekly oral cyclic antibiotic programme
J. Salomon, P. Denys, C. Merle, J.L. Gaillard, C.M. Perronne, L. Bernard (Garches, F)
Background: Spinal cord injury patients with a neurogenic bladder have an increased risk for a UTI. Patients who have recurrent UTI receive multiple courses of antibiotic therapy, markedly increasing the incidence of antibiotic-resistant bacteria (ARB) and health care costs.
Aim: To determine the safety and efficacy of a weekly oral cyclic antibiotic (WOCA) regimen to prevent UTI in a prospective cohort study of paralyzed patients with neurogenic bladder undergoing intermittent catheterization for bladder drainage.
Method: We examined the impact of a WOCA programme upon the number of cases of UTI, antibiotic tolerance, and the occurrence of ARB (anal and urinary samples). The WOCA prophylaxis consists in the alternant administration of a dose of antibiotic (amoxicilline 3000 mg, cefixime 600 mg, fosfomycintrometamol 6000 mg, nitrofurantoin 200 mg, or trimethoprim-sulfamethoxazole 1600-320 mg) once weekly. During week A, the patient takes a single antibiotic (antibiotic A), and the following week (week B) the patient receives another antibiotic (antibiotic B). Antibiotic was specifically adapted according to the recent culture of a 6 week urine specimen.
Results: 32 patients (17 men, 15 women; mean age, 47 years) with neurogenic bladder were included. Before starting the WOCA program, patients had presented with 8.8 symptomatic UTI/year (included 162 febrile UTI: 37 prostatitis, 5 orchitis, 120 acute pyelonephritis; 45 hospitalizations). Following antibiotic prophylaxis (follow-up of 2 years), there were 2 symptomatic UTI/year (included 18 febrile UTI: 12 acute pyelonephritis, 6 prostatitis; 7 hospitalizations). Greater than 90 % of the patients were careful to take their prophylactic therapy as directed. No severe adverse events were reported and no new case of colonization with multi ARB was reported. Conclusion: WOCA prophylaxis reduces the number of UTI in patients with neurogenic bladder susceptible to recurrent infection.
New antibacterials for the decade: strategies to deliver agents with novel actions (Symposium arranged by GlaxoSmithKline)
S165: The medical need for new agents
P. Hawkey (Birmingham, UK)
Dramatic increases in the prevalence of antibacterial resistance have occurred in recent years as an inevitable evolutionary response to the extensive use of antibacterial agents. The efficacy of new and existing agents continues to be compromised, both by the transmission of existing mechanisms via clonal spread and by new, emergent mechanisms of resistance. Antibacterial resistance occurs across all bacteria, both Gram-positive and Gram-negative, and is widespread amongst community-acquired and nosocomial infections. In the community, instances of multi-drug-resistant Streptococcus pneumoniae, in which strains are resistant to three or more drug classes, are becoming common and increasingly include resistance to fluoroquinolones as well as beta-lactams, macrolides and other classes. Furthermore, community strains of MRSA are beginning to arise independently of nosocomial strains and can exhibit increased virulence. New surveillance data show that community strains of Enterobacteriaceae act as reservoirs for extended-spectrum beta-lactamase (ESBL) resistance, the extent and types of which are increasing. Fluoroquinolone resistance in E. coli is also increasing and exceeds 50% in much of S.E. Asia.
New patterns of resistance are being observed in hospital-acquired infections. MRSA is frequently observed in this environment and is becoming increasingly difficult to treat as strains become resistant to almost all available drug classes. In the mid-1990s, the first strains of MRSA with decreased susceptibility to vancomycin were detected, and the vanA gene has been identified in 3 independent strains of MRSA. Severe hospital-acquired infections are frequently caused by Gram-negative pathogens such as Pseudomonas aeruginosa, Acinetobacter spp. and Stenotrophomonas maltophila. These pathogens are resistant to many beta-lactams, and although resistance to many carbapenems remains rare, resistance to those of the IMP, VIM and OXA family is increasing.
S166: Options for sustainable antibacterials
T. File (Rootstown, USA)
The last two decades have seen a decline in antibacterial development productivity and, more recently, in the scale of antibacterial R&D. During the same time, the level and prevalence of antibacterial resistance have increased to worrying levels. The clinical impact of current resistance levels in hospital infections is well established, and accumulating evidence suggests that resistant bacteria are implicated in the clinical failure of antibacterials in the community setting. Given the current situation, it is vital to develop new, effective agents and to sustain the clinical utility of these and existing therapies. Many recent initiatives have recognized the importance of using antibacterials appropriately in order to sustain antibacterial efficacy. This requires a multifaceted approach. Firstly, an accurate clinical diagnosis and severity assessment is vital to avoid the use of antibacterials when they are not warranted, such as in viral infection. Secondly, agents with an appropriate spectrum of activity and pharmacodynamic profile should be selected, to provide maximal reduction of bacterial load and minimize the potential for selection and spread of resistance. Consideration of local resistance patterns is essential when selecting the type or dose of agent to address resistant isolates. Development of improved diagnostic techniques to differentiate aetiologies, and stratification of patients according to predictors of both bacterial resistance and outcome would further enable clinicians to tailor therapy choices for individuals. High-dose and shorter treatment may reduce risk factors for selection of resistant strains. Vaccines may also play a role in sustaining antibacterial efficacy by reducing the incidence of bacterial infections and their sequelae, but their effects on resistance may be limited by replacement of vaccine serotypes with non-vaccine serotypes that have emerging resistances.
Antibacterials from new classes are urgently required that will combat existing resistance, minimize the emergence of resistance and the risk of cross-resistance, provide high bacteriological efficacy against target organisms, possess a well-defined safety profile and provide a convenient dosing regimen. In the future, advanced techniques may enable the development of antibacterials designed to target specific indications or pathogens, while having a reduced ecological impact. Some novel agents are reaching the late stages of development and their appropriate use should be encouraged from the outset.
S167: Targets: hits and misses
D. Payne (Collegeville, USA)
The genomic era of antibacterial drug discovery was triggered by the completion of the H. influenzae genome in 1995. At that time, it was thought that the antibacterial therapy area was the ideal model to illustrate the ability of genomics to rapidly deliver novel mechanism medicines. Consequently, many large pharmaceutical and biotechnology companies set up genomic-based antibacterial programmes. It was generally believed that genomics would fuel a flow of targets that could be screened to rapidly identify new classes of antibiotics. This genomic exploitation was spectacularly successful in delivering hundreds of novel antibacterial strategies. A review of the literature from the last 9 years reveals a fraction of the substantial effort applied to this area, showing >35 different companies ran >120 screens on >60 different antibacterial targets. Clearly, investment in this area has been significant, but success based on the number of novel acting antibiotics in the industry pipeline is alarmingly low and there are some key scientific reasons for this poor success rate. First, screening metrics illustrate that the success of antibacterial High Throughput Screening (HTS) is significantly less productive than screening targets from other therapeutic areas. Second, optimizing hits and leads from HTS to molecules with all the requisite properties to be a safe and efficacious antibacterial can be exceptionally challenging compared to creating new generations of antibacterials from established classes where substantial background structure-activity relationships exist. Third, the initial bioinformatic and genomic analysis used to validate a target may not always extrapolate to a broader set of strains from the species or a range of target species. Consequently, a refocus of effort and resource is required to tackle antibacterial discovery in the post genomic world. Investment in new genomic technologies or novel target discovery is no longer merited. Focusing significant, consolidated medicinal chemistry and microbiology resources on advanced leads is essential for success rather than spreading effort across a large portfolio of targets. Furthermore, approaches for enhancing success at HTS and prioritizing effort on targets that are validated ‘beyond the genome’ are required. This presentation will illustrate some of the scientific challenges faced by GlaxoSmithKline in exploiting genomics to deliver new antibacterial agents and describe some of the strategies implemented in our ongoing efforts to seek new antibacterials in the post genomic world.
S168: The future, beyond the horizon
R. Finch (Nottingham, UK)
Development of novel antibacterial molecules, particularly from new drug classes, presents several challenges. The demonstration of utility against bacteria resistant to other antibacterial classes is essential for registration, reimbursement and marketing, but presents issues related to clinical trial size, costs and end-points. Furthermore, product labelling and use may be restricted in the future, at least at initial introduction, by regulators and policy makers. For some indications, such as self-limiting infections or indications where the value of antibacterials is debatable, paradigms for clinical trials are changing towards patient-reported outcome measures and demonstration of superiority over comparators. Additionally, antibacterial molecules of new classes present unknown safety liabilities, requiring extensive evaluation and tracking throughout the product's lifespan. The commercial potential of new products may be impacted by reduced use owing to continuing efforts to control resistance and costs through guidelines and reimbursement controls, as well as narrowed indications. Furthermore, a product's lifespan may be reduced by the development of antibacterial resistance if use is expanded greatly or inappropriately. Positive solutions must be found to encourage the development of new antibacterials. Strategies could include lowering R&D costs by introducing measures such as guaranteed ‘fast-track’ regulatory review or by focusing on the quality rather than the quantity of clinical trials. Regulatory agencies could further assist by providing direction on regulatory expectations and identifying areas of debate to be addressed during the development process. Additionally, research costs could be offset by partnerships between academia and industry, or by provision of public or private funding, tax breaks, and revision of patent terms. Given the delay between initial research and final approval, we must act now to improve future antibacterial development and introduction of new molecules. To achieve success, coordinated action by pharmaceutical companies, regulatory agencies, health organizations, government bodies and the scientific community will be required.
Staphylococcus aureus disease – from basic science to clinical practice
S182: Molecular basis of Staphylococcus aureus adherence to sqamous epithelium
T. Foster, E. Walsh (Dublin, IRL)
Staphylococcus aureus permanently colonizes the moist squamous epithelium of the anterior nares of ca 20% of the population, and transiently colonizes another 60%. Given that this is a risk factor for invasive infection, it is surprising that there has been so little interest until recently in the bacterial and host factors that determine colonization. To address this, a simple assay for measuring bacterial adhesion to desquamated epithelial cells from the nares of donors was developed. S. aureus strains defective in the surface proteins clumping factor B and serine-aspartate repeat proteins SdrC and SdrD showed reduced adherence. Conversely, expression of these proteins, as well as a novel surface protein SasG, in the surrogate host Lactococcus lactis, promoted adherence to squamous epithelial cells. Purified recombinant rClfB protein bound strongly in a dose-dependent and saturable manner to purified recombinant human cytokeratin 10 (K10; KD 1.4–1.7 micromolar) and to recombinant human loricrin, major proteins of the squamous cell interior and cornified surface layer, respectively. Also, bacteria expressing ClfB adhered strongly to immobilized keratin 10 and loricrin. In the case of K10 it was shown that rClfB bound to the C-terminal ‘tail’ region which is composed predominantly of unusual peptide sequences called glycine loops. A synthetic peptide mimicking a typical glycine loop YGGGSSGGGSSGGY inhibited ClfB binding to K10. It is noteworthy that loricrin has three glycine loop regions, any one of which could be involved in promoting ClfB binding. This is currently being investigated. Binding of ClfB to loricrin was inhibited by the K10 peptide.
S184: Molecular interactions with platelets – lessons for endovascular infections
C. Heilmann, S. Niemann, M. Hermann, G. Peters, B. Kehrel (Munster, Homburg/Saar, D)
Staphylococcus aureus has emerged as a predominant cause of infective endocarditis (IE), which often is fatal with mortality rates of 20–40%. The pathogenesis of IE is characterized by a series of events: initial endocardial damage results in exposure of the subendothelium and subsequent deposition of platelets and fibrin. The fibrin-platelet matrix on the damaged valves may serve as binding foci for adhering bacteria. The ability of S. aureus to adhere to platelets and to induce platelet aggregation is considered as a critical factor in S. aureus-associated IE. To identify and characterize bacterial factors involved in the S. aureus-platelet interaction, we generated a phage display library of S. aureus genomic DNA and a phagemid vector. The library was affinity-panned against gel-filtered, immobilized platelets. Repeatedly isolated clones contained either a portion of the C-terminal domain of the S. aureus coagulase or the N-terminal domain of the extracellular fibrinogen (Fg)-binding protein Efb. The S. aureus coagulase and Efb may interact with platelets via Fg as a bridging molecule. In another approach, repeatedly isolated clones contained overlapping DNA fragments encoding a portion of the S. aureus fibronectin-binding proteins (FnBPs). In a flow cytometric adherence assay, Staphylococcus carnosus producing either FnBPA or FnBPB showed increased adherence to activated, gel-filtered platelets. Adherence was promoted by the addition of Fn or Fg, which most probably act as bridging molecules. Interestingly, promotion of adherence mediated by Fn was in the same range with S. carnosus producing either FnBPA or FnBPB, whereas promotion of adherence mediated by Fg was significantly more pronounced with S. carnosus producing FnBPA than with S. carnosus producing FnBPB. Furthermore, FnBPA, but not FnBPB mediated platelet aggregation when present on S. carnosus cells indicating a substantial functional difference between both proteins. To identify platelet-binding sites involved in that interaction, platelets from knockout mice and from patients with selective inherited deficiency of membrane proteins or of granules were used. CD36, GPIIb/IIIa, and P-selectin were excluded as receptors for S. aureus and the contents of alpha-granules, such as Fg, Fn, and thrombospondin, have been shown to be essential for the S. aureus-platelet interaction. Furthermore, we found that soluble fibrin, but not Fg is the main mediator of that interaction.
Benchmarking nosocomial infections (Symposium co-organised by SHEA and ESGNI)
S192: Prevalence studies: what do they tell us, if anything?
J.F.H. Humphreys ESGNI/SHEA
Prevalent studies of nosocomial infection outline the number of cases of infection in a defined patient population either during a specific period or at a specified point in time. The major shortcomings of such studies are that they give us merely a ‘snapshot’ and do not convey the fully impact of infection. However, they are relatively easy to conduct, and if carried out regularly, can indicate trends over time. Furthermore, when done nationally with a common protocol, it is possible to assess variations in infection rates that may subsequently be investigated further. Issues that need to be addressed when carrying out prevalent surveys include the comprehensiveness of the database, the definitions used, and both the data recording and analysis. Whilst it may not be possible to conduct frequent prevalent studies covering all hospitalised patients in a large institution, intermittent studies or repeated studies in specific areas, where the infection rate is relatively high, e.g. the intensive care unit, are of considerable use, but the results must be fed back to the relevant health care personnel. Periodic national prevalence surveys of nosocomial infection, such as those conducted in many European countries over the last 15 years indicate areas requiring specific interventions. However, prevalence studies are not a substitute for a comprehensive incidence-based surveillance programme that captures all infections in a hospital or institution.
S193: The Dutch PREZIES network: national surveillance systems-more than just data collection
J. Kluytmans (Breda, NL)
Surgical Site Infections (SSI) are important complications of surgery. Although many advances have been made in asepsis, antisepsis and surgical technique over the last century, infections are still relatively frequent complications. The pathogenesis of SSI is complex and not completely understood. Therefore, prevention can only be partly achieved by control of the process and outcome measurement remains essential for optimal performance. Repeatedly it has been shown that measuring of SSI-rates with active reporting of these rates to the surgeons results in a reduction of the SSI-rate. Although this is generally accepted there is no consensus how to do this. There are many aspects that should be taken care of, to produce reliable and reproducible SSI-rates. Things get even more critical when these rates are used for comparisons. The following aspects are of major importance: Definitions, case-finding methods and control for confounding (risk factors should be taken into account). In the last decade several large, multicentre, surveillance projects have been performed and have shown that significant variations in the SSI-rates between different hospitals exist. However, these variations were for an important part caused by differences in the case-finding methods used or by differences in the population of patients operated on. Therefore, they do not necessarily reflect true differences in the performance of the participating centres. Also, it has been shown that centres that participate in such projects for several years achieve a significant reduction of the SSI-rates. It are true quality improvement projects. The conclusion is that measuring SSI-rates in a standardised way with reporting of the rates to those that can improve the outcome, improves the quality of care. Now those rates have been gathered, there is a demand from the public to know the hospital specific rates. One of the main reasons for this must be that patients should be able to make a more justified decision were they want to be operated. The question is if this is a justified assumption? There are several arguments against publication of SSI-rates: 1) It is likely that the SSI-rates will be less reliable (too low) when they are published in a way that the centre or even surgeon involved can be identified. 2) The risk factors involved are not known completely and therefore the observed differences do not necessarily reflect true differences in performance. In conclusion, although the public demand seems reasonable at a first glance it is not the way to go at this time. The SSI-rates cannot be used to make a reliable decision were to be operated most safely (apart from other aspects of the surgical procedure that are of importance). Moreover, if it is enforced to publish SSI-rates this will likely terminate one of the most important methods to improve quality in surgery currently available.
Exotic infections
O195: Vibrio cholerae O1 classical strains are facultative intracellular bacteria, which survive and multiply symbiotically inside the aquatic free-living amoebae
H. Abd, A. Weintraub, G. Sandström (Stockholm, S)
Objectives: Cholera is a severe intestinal disease, caused by different spices of Vibrio cholerae. While cholera affects many millions of people around the world, the main reservoir of the bacterium is not completely known. Since both free-living amoeba and V. cholerae inhabit aquatic systems, an association between them would be possible. Our previous study has shown that the seventh-pandemic V. cholerae O1 El Tor- Inaba strain N16961 behaves as a facultative intracellular bacterium during its survival in free-living amoebae. Here we address the question if strains of V. cholerae O1 classical have the same ability as strain N16961 to grow and survive inside Acanthamoeba castellanii.
Methods: V. cholerae O1 classical strains were co-cultivated with A. castellanii for more than two weeks. The interaction between these microorganisms was followed by viable counts of alone- and co-cultivated microorganisms. Intra-amoebic growth and localization of each bacterial strain was estimated by gentamicin assay, viable count, microscopy, and PCR to detect cholera toxin gene and amoebic 18 s RNA gene disclosing symbiont-host association.
Results: The results show that examined V. cholerae O1 classical strains multiply and survive inside trophozoites and cysts of A. castellanii. The bacterial internalization was in cytoplasmic compartment of the amoebae cells. The relation between these microorganisms in co-cultures could be listed as symbiosis since, presence of the amoebae enhanced growth of bacteria, and the presence of the bacteria did not affect amoebic growth. In addition, V. cholerae strains could not survive without A. castellanii more than a few days.
Conclusions: The symbiotic relation between these bacterial strains and A. castellanii showing a new environmental host of V. cholerae and a facultative intracellular behaviour of V. cholerae O1 classical strains, which is in contrast to the general held view of the bacterium.
O196: Regional-scale synchrony of cholera epidemics in the Equatorial Atlantic Coast (Gulf of Guinea)
G. Constantin de Magny, B. Cazelles, M. Petit, J.F. Guégan (Montpellier, Paris, F)
Cholera is an ancient disease which had disappeared from most of the developed countries in the last 50 years, but it still persists in many parts of the world with serious epidemics most often localized in tropical areas. This highly contagious disease is due to the bacteria Vibrio cholerae, after ingestion of contaminated water or seafood. V. cholerae is naturally present in the environment and is autochthonous to coastal and estuarine ecosystems. The bacteria is closely associated with many phyto- or zooplankton organisms. Thus any environmental, ecological impact on V. cholerae reservoirs density may have some incidences in bacterial population density. In this context, climatic and/or environmental, ecological changes influencing V. cholerae reservoirs density may be particularly involved in the emergence of cholera in human populations by increasing the probability of contacts between bacterial populations in the ecosystem and riverine human populations.
Objectives: The present work aims at determining and quantifying the relationships between climatic/environmental factors and cholera populations dynamics, i.e. the evolution of case numbers with time, across several countries in the Equatorial Atlantic Coast (Gulf of Guinea).
Methods: In a first part, cholera population dynamics is studied using wavelets analysis to characterize the observed dynamics and to synchronism between the different countries. Secondly, climatic indicators (e.g. S.O.I) and space oceanography variables (e.g. Sea Surface Temperature) are also analyzed with similar questions. Finally, results are crossed between environmental variables and disease time-series in order to detect the existence of correlations and phase delays.
Results: We observed an important synchrony between cholera epidemics for Benin, Ghana, Republic Demographic of Togo and Nigeria for the period 1987 to 1994, and this was highly synchronized with some climatic and/or oceanographic parameters.
Conclusion: This comparative approach should allow a better understanding and quantification of the importance of climatic and environmental fluctuations on cholera epidemics in human populations at both the global and regional scales. This work is then a first step toward the objective of building a predictive model for the risk of environmental emergence of Vibrio bacteria in human populations.
O197: Routes of transmission of cholera in Zahedan district, Sistan and Baluchestan province
S. Izadi, S.M. Tabatabaei, M.R. Miradi, K. Sheikhzadeh (Zahedan, IR)
Objectives: Within the past few years outbreaks of cholera has occurred in different points of Sistan and Baluchestan province of Iran, especially in the Zahedan district. The objective of this study was definition of the most important routs of transmission of cholera in the rural areas of Zahedan district involved in the outbreak of summer 2003.
Methods: The outbreak lasted about 50 days. 20 consecutive cholera cases positive for Vibrio cholera O1 in stool culture were compared with 89 controls sampled from the population. The cases have occurred during 28 July to 16 September 2003.
Results: Age, eating food in parties, absence of soap in hand-washing place, household size, getting ice from street vendors were significantly associated with cholera.
Conclusion: Different transmission principles have been mentioned in the literature for cholera, however every outbreak has its own special patterns of transmission.
O198: Giardia lamblia: different genotypes, different symptoms?
T.G. Mank, R. Jansen, L.M. Kortbeek, E.A.M. Andriessen, A. Vries de, J. Giessen van der (Haarlem, Bilthoven, NL)
Objective: In a previously described study, human Giardia Assemblage A isolates were associated with mild intermittent diarrhoeal complaints whereas infections with isolates belonging to the Assemblage B were associated with profound diarrhoea with weight loss and fatigue (Homan & Mank). Since the number of patients is that study was limited (N = 18) and inclusion of cases only took place in the Haarlem area, we expanded this study with a group (N = 100) patient suffering from symptomatic giardiasis visiting their General Practitioner in various areas in the Netherlands.
Methods: Besides stool collecion, patients were asked to fill out a comprehensive pre-coded questionnaire. From all included (N =100) patients with microscopically proven giardiasis, genotyping of the DNA isolated from the isolated cysts was performed. Genotyping comprised PCR restriction fragment length polymorfism (RFLP) analysis of the glutamate dehydrogenase (Gdh) locus and the A- and B- assemblage specific loci as well as Gdh and 18-S-rDNA sequence analysis.
Results: During this study, again, only a limited number of different genotypes were found (40 isolates belonging to the Assemblage A, predominantly A1, and 60 belonging to the Assemblage B). Furthermore, the earlier reported correlation between the severity of the diarrhoeal complaints and the presence of the genotype was found during this expanded study as well. Assemblage A isolates were predominantly found in patients with intermittent diarrhoeal complaints, while Assemblage B was strongly associated with persistent, profound diarrhoea.
Conclusions: Our results indicate that Giardia lamblia isolates infecting human consists of virulent and less virulent genotypes. In our opinion it can be postulated that the Giardia lamblia genotype contributes to the establishment of symptoms in human infection.
O199: Diagnostic possibilities in giardiasis
T.G. Mank, E.A.M. Andriessen, M. Ras (Haarlem, NL)
Microscopic examination of stool specimens is the cornerstone of detection of intestinal parasites in parasitology laboratories and is the best known and most frequently performed laboratory procedure. Although process has been made in non-morphologic diagnosis (e.g. ELISA- and PCR techniques) microscopy is still considered to be the gold standard in the diagnosis of intestinal protozoal infecions, including giardiasis. In the Netherlands, as in most other members of the European Union, fresh, nonpreserved stool specimens are generally used for examination. Specimens are initially screened as direct wet preparations using either Lugol's iodine or eosine for detection of vegetative stages of protozoa and are subsequently examined for protozoan cysts and helminth eggs using an ether- or ethylacetate sedimentation method or flotation concentration technique. Because intestinal parasites are shed intermittently, patients are asked to deliver at least three stool specimens. The limitation of this diagnostic approach is that detection of the vegetative stages of protozoa may be missed because of delays in processing and/or low compliance to the request to submit multiple stool samples. To overcome this limitation, a diagnostic test that combines multiple sampling (on 3 consecutive days), a fixative (Sodium Acetate Acedic Acid Formalin, SAF), a concentration method, and an easy to use permanent stain was developed for use in routine clinical practice. The results of the new test, called the “Triple Faeces Test” (TFT), a Giardia lamblia specific ELISA (Ridascreen Giardia, r-Biopharm), and fluorescence techniques were compared with those of the conventional diagnostic methods used for Giardiasis in routine clinical practice. These comparative studies (which formed the basis of our newly developed diagnostic flow chart) showed that the sensitivity of the diagnostic approach using TFT and the Ridascreen Giardia test improved significantly (p < 0.005) as compared to the conventional methods using a fresh non preserved stool specimen.
O200: Detection of Giardia cysts in waste water
O. Manso, M. Sousa, I. Machado (Oporto, P)
Objectives: The aim of this study was to evaluate the presence of Giardia cysts in wastewater treatment plants.
Methods: Collection of samples from two wastewater treatment plants in the north of Portugal, between March and July of 2002. Sampling was made in the beginning and in the end of the treatment process. The presence of the parasites was assessed by immunofluorescence with monoclonal antibodies. In addition, in each sample, microscopic examination was done after concentration techniques, to estimate contamination with other parasites. Physical and chemical parameters of wastewater samples were also analysed.
Results: Giardia cysts were detected in 57% of wastewater samples analysed, 27% of them from affluents, and 30% from effluents. Infectious forms of human pathogens were detected in affluent and effluent wastewaters.
Conclusion: These results demonstrate the persistence of protozoa even after the wastewater treatment process. The concentration of Giardia cysts observed alerts to a potential source of contamination for men, animals and the environment.
O201: Impact of dengue viral infection on liver function
S. Bhoi, A. Khera, A. Goel (New Delhi, IND)
Objective: Recent years has seen changing and unusual characteristics of dengue viral infection. This prompted us to study the impact of dengue viral infection on liver functions.
Material and methods: All patients; who tested positive for either IgM or IgG and IgM anti-dengue antibodies were included in the study. Classical Dengue fever (DF), Dengue haemorrhagic fever (DHF) and Dengue shock syndrome (DSS) were defined as per WHO criteria. Statistical analysis was done by Epi Info 2002.
Results: Out of 155 cases; 36 cases were excluded from the study, as they did not fulfill the inclusion criteria. Rest 119 cases were defined as DF in 58 (48.7%), DHF in 53 (44.5%) and DSS in 8 (6.75%) cases. The predominant presentations were fever (100%), rash (24.3%), abdominal pain (16.8%), seizures (1.6%) and retrorbital pain (0.8%). Bleeding manifestations were observed in 56 (47%) cases. Petichae (13%), hemetemesis (10.9%), gum bleeding (10.08%), subconjunctival hemorrhage (9.24%) and multiple site bleeding (11.7%) were noted frequently. The mean platelet count noticed in DF, DHF and DSS were [50 ± 27.4, 46 ± 31.05, 42 ± 26] × 103 respectively. The major unusual feature observed was moderate (£ 5 fold) elevation of transaminases, which started rising on the 3rd day, peaked on the 9th day and returned to baseline over a period of three to eight weeks. In DF, DHF and DSS; the mean serum bilirubin [0.83 ± 0.27, 0.89 ± 0.3, 0.9 ± 0.48] mg/dl (p = 0.9), SGOT [123 ± 88.5,120 ± 93, 112 ± 37] IU/L, SGPT [108 ± 48, 109 ± 70, 107 ± 36] IU/L (p = 0.01) and serum alkaline phosphatase (SAP) [138 ± 53, 124 ± 52, 153 ± 26] IU/L (p = 1.7) were noticed. USG revealed acalculous cholecystis in 17% (DF), 2.8% (DHF) and 2.5% (DSS) cases. All patients recovered except one (0.84%); who succumbed due to intracranial hemorrhage.
Conclusion: Statistically significant elevation of transaminases along with normal serum bilirubin and SAP was observed in all categories (DF, DHF, DSS); this is in contrast to previous reports where elevated transaminases were observed more frequently in DHF and DSS. These observations may suggest the changing trend of Dengue virus infection, where impact on liver occurs irrespective of severity of the disease.
O202: Human trichinellosis in Argentina
J. Bolpe, M. Ledesma, M. Benítez, D. Cecchini, S. González Ayala (Azul, Buenos Aires, La Plata, RA)
Objective: To describe the epidemiologic, clinical and laboratorial aspects of human trichinellosis.
Methods: Database of the Epidemiologic Surveillance System of Buenos Aires State, Argentina, 1/2000-9/2004 was processed with Excel and Statistics software. The outbreak investigation was routinely performed by county and state health authorities. Trichinosis case was suspected based on eosinophilia in conjunction with compatible symptoms and a dietary history (pork meat). Diagnosis was confirmed by serologic test (indirect immunofluorescence, IFI), and/or identification of larvae in the suspect meat (digestion of muscle tissue in artificial gastric juice followed by examination of the sediment for larvae).
Results: One thousand and one hundred twenty eight cases and 65 outbreaks were studied. The distribution by gender was asymmetrical, male 58.2% (n = 656). The median age was 33 years (range 1–97). Ninety eight per cent of the cases (n = 1103) occurred in the context of an outbreak. All cases were related to the consumption of pork meat, and 72.1% of the suspect food was from animals slaughtered and sold without sanitary inspection. Ninety seven per cent of the cases (n = 1094) presented clinical symptoms and/or signs. The most frequent were: myalgias 66.0% (n = 745), headache 50.3% (n = 567), periorbital edema 48.9% (n = 552), fever 45.2% (n = 510), diarrhoea 27.1% (n = 306), nausea and vomiting 14.7% (n = 166). The median for symptoms/signs was 3 (range 0–8). Eosinophilia over 6% was observed in 42.9% (n = 484). IFI was positive in 65.3% (n = 737). The suspect food was available for identification of larvae in 11.7% (n = 132) of the cases. The amount of larvae per gram ranged from 1 to 150.
Conclusion: Trichinellosis is a zoonotic infection related to the ingestion of undercooked pork meat. In our study most of the cases occurred in the context of an outbreak. We found a high percentage of cases related to the consumption of pigs and their derivatives that escaped from sanitary inspection. This shows the lack of adequate bromatological control in our environment. The frequency distribution of symptoms and/or signs was similar to other series. In an appropiate epidemiologic context, characteristic clinical symptoms strongly suggest the diagnosis of trichinellosis, which can be confirmed with serologic tests and/or identification of larvae in the involved meat. Health education for breeders, producers and consumers is very important in order to prevent future outbreaks.
O203: Artesunate-clindamycin versus quinine-clindamycin in the treatment of Plasmodium falciparum malaria: a randomised controlled trial
M. Ramharter, S. Oyakhirome, P. Klein Klouwenberg, A.A. Adegnika, S.T. Agnandji, M.A. Missinou, S. Issifou, W. Graninger, P.G. Kremsner (Vienna, A; Lambaréné, GAB)
Objective: Artemisinin based drug combinations are the mainstay in the fight against drug resistant malaria in Africa. Currently available antimalarial drug combinations including artemisinins are pharmacokinetically unmatched and are therefore potentially increasing the risk of selecting resistant mutants in areas of high malaria transmission. We aimed to test the potential value of short half-life artemisinin based combination therapy for uncomplicated falciparum malaria in sub-Saharan Africa.
Methods: We conducted an open label randomized controlled clinical trial to evaluate the efficacy and tolerability of 3 days twice daily, oral artesunate-clindamycin therapy (2 mg/kg and 7 mg/kg per dose) compared to a standard quinine-clindamycin regimen (15 mg/kg and 7 mg/kg per dose) in the treatment of uncomplicated falciparum malaria in 100 Gabonese children aged 3 to 12 years.
Results: Artesunate-clindamycin showed comparable activity to quinine-clindamycin in the per-protocol analysis of day-28 cure rates (87% versus 94%). No serious adverse events were reported and tolerability was similar in both groups. Fever and parasite clearance times were significantly shorter in the artesunate clindamycin group.
Conclusions: Artesunate-clindamycin and other matching short plasma half-life combinations of artemisinins merit further attention in regions with high malaria transmission.
O204: Microarray based analysis of gene expression in drug resistant Leishmania donovani isolated from Indian patients of Kala azar
P. Salotra, R. Singh, R. Duncan, H. Nakhasi (New Delhi, IND; Bethesda, USA)
Objective: Visceral leishmaniasis or kala azar (KA), fatal if not treated, is caused by protozoan parasites of Leishmania donovani complex. The prevalence of drug resistance to the traditional drug, sodium antimony gluconate (SAG), has reached alarming proportions in Indian patients of KA. There is an urgent need to identify novel targets to combat drug resistance.
Method: We developed a genomic microarray for L. donovani comprising of 4224 PCR amplified inserts(1.0 to 1.5 kb), 24 positive and 12 negative controls, each printed in triplicate. Two-color fluorescent (Cy3 andCy5) hybridizations were used to compare gene expression in drug resistant and sensitive strains. Sensitivity of the parasite isolates from bone marrow aspirates of KA patients (SAG responder and Non responders) was evaluated in vitro. ED50 from SAG resistant and sensitive isolates was 250 microgm/ml and 25 microgm/ml, respectively. The hybridized arrays were scanned in a GenePix Pro 4100 scanner (Axon) followed by analysis using software Acuity 3.0.
Results: Scatter plot comparing the log ratios against log products of fluorescence intensities is shown in Fig. 1. Approximately 2% (85) clones showed 31.5 fold abundant expression either in resistant or sensitive isolates. Partial nucleotide sequence of selected clones was determined and analyzed by BLAST analysis (Table 1).

Table 1.
Ratio of micro array signal intensity in Drug resistant vs sensitive parasites of L. donovani from KA patients. The nucleotide sequence was analysed by BLAST analysis inGenbank (NCBI) and in Leishmania major sequence databases (Gene DB).
| Clone ID | Gene Identity | Ratio | E value |
|---|---|---|---|
| Upregulated in resistant parasite | |||
| 28G11 | Parasite surface antigen(PBA-2) (LmjF12.0760) | 2.8 | 7.0e–43 |
| 39B11 | PSA-2 (AY36511.1) | 3.0 | e-117 |
| 42A11 | PSA-2 (AY437087.1) | 2.5 | 0 |
| 34H7 | rRNA large sub unit (Lmj F 2 7.rRNA.2 6) | 2.63 | 3.1e-232 |
| 28B11 | Tetracyclin Res protein (LmjF 35.2810) | 1.6 | 1.9e-157 |
| 31E9 | 93% homology with proteasormne regulatory ATPase subunit, putative(Lmj F22.0620) | 2.36 | 4.5e-124 |
| 24E5 | Nucleoside transporter (Lmj F15.1240) | 1.8 | 1.1e-31 |
| 28C11 | 86% with hypothetical protein (Lmj F22.0730) | 2.15 | 6.5e-127 |
| 50F9 | hypothetical protein with Zn finger domain (LmjF22_0190) | 1.8 | 1.3e-38 |
| Upregulated in sensitive parasite | |||
| 67C6 | iron/zinc transporter protein-like protein (LmjF31.3070) | 2.36 | 2.5e-40 |
| 53F2 | Thioredoxin family protein (LmjF26.0670) | 1.4 | 2.1e-21 |
| 62D5 | Hypothetical protein (LmjF30.1680) | 1.8 | 4.1e-24 |
| 18A6 | conserved hypothetical protein (LmjF 18.0100) | 1.5 | 6.2e-94 |
Conclusion: The study led to identification of a number of transcripts showing over-expression in drug resistant isolates, some of which corresponded to known genes like PSA-2, nucleoside transporter (NT), tetracycline resistant protein homologue (TRH) and proteasome regulatory ATPases. Three clones corresponded to the PSA-2, a glycoprotein with leucine rich repeats that has a role in facilitating attachment and internalization of parasites by macrophages, resisting complement mediated cell lysis. NT and TRH may promote resistance to drug by inhibiting the drug intake by the parasite. Proteasome and associated ATPases help increased survival of Mycobacterium inside macrophage by lending resistance to nitric oxide. The over-expression of this protein in drug resistant Leishmania may help the parasite to persist in host. The study establishes the utility of genome-wide RNA expression profiling in Leishmania and identifies numerous genes with potential role in drug resistance.
Emergence and molecular evolution of antibiotic resistance
O205: A multidimensional screening of non-clinical isolates reveals metallo-beta-lactamases in the environment
S. Quinteira, H. Ferreira, L.V. Peixe (Porto, P)
Objectives: Even though increasingly reported in many countries, metallo-beta-lactamase (MBL)-producing Gram-negative bacilli have been associated to the hospital setting, suggesting a relative confinement within this ecological niche. In this study, the presence of MBLs and imipenem susceptibility in Gram-negative bacilli were evaluated among non-clinical sources in order to verify a possible spreading into new, previously undescribed, environments.
Methods: Samples (24 from healthy human volunteer faeces, 30 from poultry skin, 4 from swine faeces, 13 from rivers and 29 from hospital wastewaters-receiving urban sewage) were collected in Northern Portugal between 2001 and 2004. Sample aliquots were platted, in MacConkey agar and/or Pyocyanosel agar supplemented with imipenem (2 mg/L) and colonies with different morphology were collected. Species identification was performed with the API 32GN. Imipenem susceptibility was determined using the disk diffusion method. A bioassay method was employed in order to detect MBL production and positive results were later confirmed by a multiplex PCR assay designed to amplify both blaVIM and blaIMP genes. Characterisation of MBL-type was possible through sequencing.
Results: 190 Gram-negative bacilli (21 lactose-fermenters and 169 non lactose-fermenters) were isolated from different sources. Decreased susceptibility to imipenem was observed in 64 isolates from sewage (n = 25), rivers (n = 17), swines (n = 12) and healthy volunteers (n = 10). All poultry isolates showed imipenem susceptibility. Positive bioassays were detected in 49 out of the 64 isolates with reduced susceptibility to imipenem. blaVIM-2 gene was detected in three isolates: two Pseudomonas aeruginosa (river and hospital sewage) and a P. alcaligenes (hospital sewage). blaIMP was not detected in none of the isolates.
Conclusions: Carbapenems are in many cases the last therapeutic resort and the detection of carbapenem-hydrolyzing MBL producers in the hospital setting is a worrisome phenomenon. Although VIM and IMP-producing strains were not observed in animals and human healthy volunteers, these enzymes seem not to be restricted to the hospital setting anymore. Disturbingly, the results emerging from this study show that, even if in very low frequencies, the presence of VIM-2 loose in the environment, namely in sewage and rivers, may undermine the effectiveness of carbapenems, largely depending on the eradication or confinement of resistant bacteria.
O206: CTX-M-producing Escherichia coli now the dominant cephalosporin-resistant Enterobacteriaceae in London and SE England
N. Potz, R. Hope, M. Warner, A.P. Johnson, D. Livermore on behalf of the London & South East ESBL Project Group
Objectives: There is increasing concern about the spread of Enterobacteriaceae, principally E. coli, producing CTX-M-type extended-spectrum beta-lactamases (ESBLs) in the UK. This is reflected in increasing surveillance reports and submissions to the reference laboratories, with many isolates reportedly from community patients. To better assess the situation, a prospective survey of cephalosporin-resistance was undertaken for Enterobacteriaceae across London and Southeast England.
Methods: Eighteen laboratories participated: 10 in London and 8 elsewhere in southeast England. These screened all Enterobacteriaceae isolates using cefpodoxime or both cefotaxime and ceftazidime. Isolates resistant to any of these 3 cephalosporins were submitted for centralised susceptibility testing and identification. Interpretive reading was performed, allowing an inference of resistance mechanism(s).
Results: During a 12-week collection period, >1000 cephalosporin-resistant Enterobacteriaceae isolates were collected, mostly submitted on the basis of their cefpodoxime resistance. E. coli was by far the most numerous species (>50% of all isolates), with over 70% of these having an ESBL, usually conferring a CTX-M phenotype. Klebsiella and Enterobacter spp. were also well represented (each over 15% of resistant isolates). The majority of the resistant Klebsiella isolates had phenotypes indicative of ESBL production but two-thirds of enterobacters had phenotypes implying derepression of AmpC. ESBLs were detected in a few Citrobacter, Morganella and Serratia spp. isolates, but not in P. mirabilis. Approximately 60% of all cephalosporin-resistant Enterobacteriaceae were inferred to be ESBL-producers, mostly with CTX-M phenotypes, whereas isolates with AmpC phenotypes accounted for 20%. The remaining 20% comprised of isolates inferred to have other beta-lactamases, or non-enzymatic resistance. Conclusion: Until 2000 CTX-M-beta-lactamases were unknown in the UK and cephalosporin-resistant Enterobacteriaceae were mostly enterobacters with AmpC or Klebsiella spp. with TEM or SHV ESBLs. This survey shows a dramatic shift towards E. coli as the main host for ESBLs and cephalosporin resistance, and towards CTX-M phenotypes.
O207: Characterisation of blaBEL-1, a novel integron-located extended-spectrum beta-lactamase gene from a Pseudomonas aeruginosa clinical isolate in Belgium
L. Poirel, L. Brinas, A. Verlinde, L. Ide, P. Nordmann (Le Kremlin Bicetre, F; Roeselare, B)
Objectives: Characterisation of the expanded-spectrum beta-lactamase resistance determinant of a Pseudomonas aeruginosa isolate from a scrotal swab of a patient admitted with a dissecting aneurism of the left arteria renalis, complicated with renal insufficiency at the Heilig Hartziekenhuis Roeselare, Belgium. This strain was resistant to ticarcillin, and of intermediate susceptibility to piperacillin, ceftazidime and aztreonam.
Methods: Screening for extended-spectrum beta-lactamase (ESBL) genes was performed using double-disk synergy test and PCR techniques. Shotgun cloning was performed with Sau3AI-partially digested DNA of P. aeruginosa and pBK-CMV cloning vector. Selection was performed on amoxicillin-containing plates.
Results: E. coli DH10B (pBEL-1) recombinant strain with reduced susceptibility to ceftazidime was analyzed. Sequence analysis identified a novel Ambler class A beta-lactamase BEL-1 (pI 7.1) weakly related to any other ESBLs. BEL-1 shared 5 and 43% amino acid identity with the plasmid-mediated ESBLs GES-1 and CTX-M-8, respectively. BEL-1 activity was inhibited by clavulanic acid and tazobactam, and uncommonly also by cefoxitin, moxalactam, and imipenem. It hydrolysed significantly expanded-spectrum cephalosporins and aztreonam. The blaBEL-1 gene was as a form of a gene cassette in a class 1 integron, located downstream of an aacA4 gene cassette encoding an aminoglycoside acetyltransferase, and upstream of i) an aadA gene cassette encoding an adenylyltransferase and ii) the smr2 gene cassette similar to sugE-type genes and encoding a putative membrane transporter of cationic drugs. This integron was chromosome-located and part of a transposon.
Conclusion: A novel ESBL gene was identified in P. aeruginosa underlining i) the diversity of ESBL genes, ii) that P. aeruginosa may be a reservoir of these genes and iii) that integrons are common vehicles of these genes.
O208: Antimicrobial resistance and dissemination of class 1 and class 2 integrons in Portuguese Salmonella isolates from different sources
P. Antunes, J. Machado, L.V. Peixe (Porto, Lisbon, P)
Objectives: The purpose of this study was to determine the antimicrobial resistance patterns and to characterise class 1 and 2 integrons in 1183 Portuguese Salmonella isolates collected during 2002-2003 from different sources (human, food products and environment).
Methods: The minimum inhibitory concentration for 10 antimicrobial agents was determined by the agar dilution method. Sulphonamide resistant isolates were screened for class 1 and 2 integrons by PCR assays. The characterisation of resistance gene cassettes was investigated by PCR, PCR-RFLP with TaqI and sequencing. Clonality was assessed by PFGE following XbaI digestion.
Results: 46% of the isolates were susceptible to all tested antimicrobial agents, 33% presented a single type of resistance, and 21% were multiresistant. Resistance to nalidixic acid (30%), tetracycline (19%), streptomycin (18%), sulfamethoxazole (17%) and ampicillin (17%) were the most common. Resistance to sulphonamides (n = 200) was always associated with resistance to other antimicrobial agents, with 75% (n = 150) carrying one (1000 to 2000 bp) or two (1000 and 1200 bp) class 1 integrons and 3% (n = 5) simultaneously carrying a class 1 and 2 integrons. 7 RFLP integron types were found, with the aadA genes (aadA1, aadA2 and aadA5) alone or downstream of a trimethoprim resistance gene (dfrA1, dfrA12 and dfrA17) or of a beta-lactamase gene (blaOXA-30), detected in the variable region of 149 integrons. The spread of class 1 integrons occurred among several Salmonella serotypes and PFGE clones. However, some Typhimurium-specific integrons were found: 1000 (aadA2) and 1200 bp (blaPSE-1) simultaneously, or one of 2000 bp (blaOXA-30-aadA1). In contrast, the other profiles appeared in several serotypes, with the integrons carrying dfrA1-aadA1 or dfrA12-aadA2 the most disseminated. Interestingly, data did not suggest any difference in the distribution of resistance gene cassettes between human and foods of animal origin isolates.
Conclusion: The present study with Portuguese isolates indicates that antibiotic resistance mediated by integrons is common among diverse Salmonella serotypes. All types of integrons were shared among human and food isolates, suggesting that resistance determinants present among animals may contribute to the problem of multidrug resistant Salmonella in humans.
O209: Sporadic and outbreak cases of plasmid-mediated quinolone-resistance in German ICUs
D. Jonas, K. Biehler, D. Hartung, B. Spitzmüller, F.D. Daschner (Freiburg, D)
Objectives: The occurrence of a novel plasmid-mediated quinolone resistance has been reported in a few cases outside Europe. This transmissible quinolone resistance gene (qnr) was detected in isolates from patients in the USA, China and Egypt. Molecular analysis demonstrated the location of the qnr-gene in class I integrons. The aim of this study was to determine the prevalence of qnr-positve strains in German ICUs.
Methods: Six hundred and forty-eight fluoroquinolone or cephalosporin-resistant Enterobacteriaceae and Acinetobacter spp., obtained from 34 ICUs during the last three years were screened for the presence of integrons. One hundred and thirty-four strains containing integron cassettes as well as integrase sequences were tested for the presence of the qnr gene-locus by use of PCR.
Results: One isolate of Enterobacter spp. from a German ICU patient turned out to be qnr-positive as well as five Citrobacter freundii strains from three patients treated in a South-German ICU during a one month period. All C. freundii strains were indistinguishable by use of XbaI macrorestriction analysis. Moreover, none of these quinolone-resistant strains were susceptible to cefoxitin, ceftazidime or cefotaxime.
Conclusion: This is one of the first reports of qnr-positive strains obtained from patients in Europe. Molecular epidemiology suggests that qnr-positve strains were involved in an outbreak in one ICU. The spread of transmissible quinolone-resistance might be underscored.
O210: Clinical investigation of the new QNR-based mechanism of quinolone resistance in French teaching hospitals: dissemination among enterobacterial species and strains producing expanded spectrum beta-lactamase
E. Cambau, J. Robert, C. Lascols, W. Sougakoff, M. Renard, C. Bebear, C. Branger, J. Cavallo, F. Denis, L. Gutmann, R. Leclercq, J. Sirot, V. Jarlier, C. Soussy (Creteil, Paris, Bordeaux, Clichy, Saint Mandé, Limoges, Caen, Clermont-Ferrand, F)
Objectives: To investigate the new QNR-based plasmid-mediated mechanism of quinolone resistance in strains of gram-negative bacilli resistant to quinolones isolated in France, with regards to the production of extended spectrum Blactamase (ESBL).
Methods: 986 nalidixic acid (Nal) resistant strains (646 Escherichia coli, 162 Klebsiella spp., 96 Enterobacter spp., 41 Citrobacter spp., 16 Serratia spp., 14 Proteus spp. and 11 other gram negative bacilli) isolated between 2002 and 2004 from nine University Hospitals in France were screened for qnr by PCR amplifying an intragenic 543-bp fragment. Among them, 300 (30%) produced ESBL. Qnr sequencing and detection of mutation in the QRDR of DNA gyrase (gyrA, gyrB) and topoisomerase IV (parC and parE) were performed for qnr-positive strains. Molecular typing was applied to qnr-positive strains belonging to the same species.
Results: 20 strains were qnr-positive, distributed as 17 E. cloacae, 1 K. pneumoniae, 1 C. freundii and 1 P. mirabilis. A new qnr allele was observed for the P. mirabilis strain with 29 nucleotide and 3 amino-acid differences referring to the original sequence. For the other strains, the qnr sequence differed from the original strain by the mutation 537A/G described in isolates from USA and China. From the experiments performed on the first E. cloacae isolate, qnr was shown to be transferred by conjugation to E. coli BM13 resulting in a low level quinolone resistance (Cip MIC 0.1 μg/ml, levofloxacin MIC of 0.25 mg/L). All the qnr-positive strains were ESBL producers. Whereas strains with MIC of ciprofloxacin (Cip) above 16 mg/L harboured gyrA and parC mutations, the 3 strains with Cip MIC below 1 mg/L showed wild-type sequences for QRDR in gyrA, gyrB, parC and parE. RAPD and ERIC PCR analysis showed that among the 17 E. cloacae strains, 10 strains distributed into 3 clusters (6, 2 and 2 strains) and the other 7 were not genetically related.
Conclusion: We detected the qnr gene in strains from different enterobacterial species with a prevalence of 7% of the ESBL producers. Qnr-positive strains without additional topoisomerase mutations showed a low level of quinolone resistance that might be undetected by standard susceptibility testing.
O211: Persistence of vancomycin-resistant Enterococcus faecium isolates belonging to C1 lineage in a healthy human volunteer during a 4 year period
C. Novais, J.C. Sousa, T.M. Coque, L.V. Peixe (Porto, P; Madrid, E)
Objectives: To analyze the clonal relationship and antibiotic resistance genetic elements of different VREF isolates from a healthy human (HV) collected during a 4-y period.
Methods: Feces from a 53-y old Portuguese male, without exposure to antibiotics or hospital in the 3 and 12 months previous to the sample collection were analyzed (Feb2001–Jun2004). He had hospital exposure for 1 day for a colonoscopy (Sep-2001) and 5 days for a shoulder surgery (Sep-2003). Samples were pre-enriched in BHI plus 6 mg/L of vancomycin and then plated in the same media Antibiotic susceptibility was determined by the agar dilution method. Species identification, the presence of antibiotic resistance genes and virulence traits, and the Tn1546 backbone structure, were determined by a PCR. PurK was identified by PCR and sequencing. Clonal relatedness was established by SmaI- and ApaI- PFGE.
Results: Six VREF corresponding to 3 PFGE types were recovered. They were also resistant to ampicillin, tetracycline, erythromycin and HLRKm. All isolates contained vanA and ermB, while (aac(6′)-Ie-aph(2″)-Ia), aph(3′)-IIIa and vatE were only found in some cases. Isolates of each PFGE type contained purK-1 which is associated to E. faecium clonal complex C1 that includes VREF causing outbreaks world-wide. Three Tn1546 types were detected: PP-5 and PP-6 contain an ISEf1 insertion between vanX-vanY region (frequently found among Portuguese VRE faecalis clinical isolates) and type D (frequent among animals). No virulence factors were detected.
Conclusions: The persistence of VREF isolates belong to a C1 lineage carrying elements associated to both the hospital setting (Tn1546 with ISEf1 and purK1) and animal sources (Tn1546 type D) in community based humans is of concern since it might serve as a reservoir of clinical relevant genes or clones that can be spread to both hospital and environmental settings.
O212: Characterisation of the epidemic European fusidic acid-resistant impetigo clone of Staphylococcus aureus
A.J. O'Neill, A.R. Larsen, R. Skov, A.S. Henriksen, I. Chopra (Leeds, UK; Copenhagen, DK)
Objectives: The recent increase in fusidic acid resistance (fusR) in S. aureus strains causing impetigo in Europe is primarily the result of dissemination of a single successful fusR clone. We have designated this strain the Epidemic European Fusidic acid-resistant Impetigo Clone (EEFIC). To better understand the emergence, spread and success of the EEFIC, we have subjected it to detailed phenotypic and genotypic characterization.
Methods: Strain typing was conducted by PFGE, MLST and spa-typing procedures. Antibiotic susceptibility testing was performed using disk diffusion. Reversed passive latex agglutination kits were used to test for exfoliative toxin A (ETA) and toxic shock syndrome toxin 1 (TSST-1), whilst PCR was used to probe for the PantonValentine Leukocidin (PVL) gene. Established techniques were employed for cloning, shotgun DNA sequencing and bioinformatics.
Results: EEFIC was susceptible to the majority of antibiotics tested, but resistant to fus, macrolides (mac) and penicillin (pen). Shotgun sequencing of the single, large (40 Kb) plasmid carried by this clone revealed that it was closely related to staphylococcal plasmid pETB, and indicated the presence of exfoliative toxin B (ETB), epidermal cell differentiation inhibitor C (EDIN-C), and a cadmium resistance determinant. In addition, EEFIC tested positive for ETA, but negative for TSST-1 and PVL toxins. The fusR gene, fusB, was cloned from the chromosome on a HindIII fragment, and found to lie upstream of the groEL gene, at the hypervariable locus occupied in some strains by the SaPI1 pathogenicity island. Furthermore, this analysis revealed that fusB has been recruited to the chromosome as a fragment of the archetypal fusR plasmid, pUB101.
Conclusions: Exfoliative toxins are frequently found in S. aureus strains causing impetigo bullosa; EEFIC carries both ETA and ETB. In addition, the presence of the ADP-ribosylating exotoxin, EDIN-C, may contribute to this strain's ability to cause superficial disease. In conjunction with genes conferring resistance to antibiotics that are mainstays in the treatment of dermatological infections (fus, mac), and in particular the stable recruitment of fusB to the chromosome, the success of the EEFIC as a cause of impetigo bullosa is not surprising.
O213: Prevalence of non-typeable Streptococcus pneumoniae in carriers and insights into its population structure
R. Sá-Leão, A. Simoes, S. Nunes, N.G. Sousa, N. Frazao, H. de Lencastre (Oeiras, P)
Objectives: The study of 2,204 drug-resistant (DR) pneumococci (Pn) isolated from the nasopharynx of children in day-care centres in Lisbon between 1997–2003, showed that 9.1% of the DR isolates had been presumptively identified as non-typeable pneumococci (NTPn). Since this prevalence was not negligible and this group of atypical Pn is largely understudied, we aimed to unequivocally identify these strains and obtain insights into its population structure.
Methods: The presumptive identification of the isolates as NTPn was based on optochin susceptibility after incubation in 5% CO2 atmosphere, typical colony morphology, and non-typeability by the Quellung reaction. Definitive identification of the strains as Pn included bile solubility and PCR detection of lytA and psaA, genes ubiquitous in Pn. Capsular type determination was re-assayed by multiplex PCR serotyping. Antibiotic susceptibility testing was done according to the NCCLS guidelines. Genetic diversity was determined by pulsed-field gel electrophoresis (PFGE).
Results: Between 1997 and 2003, 201 DR NTPn-like strains were isolated. The majority (170 or 84.6%) were bile soluble and positive for lytA and psaA. By multiplex PCR serotyping, 155 of the 170 confirmed Pn yielded no result suggesting that the capsular polysaccharide (cps) locus was absent. These strains were considered to be true NTPn. The remaining 15 strains were positive by the multiplex serotyping PCR and could be assigned a capsular type upon retesting them by the Quellung reaction. Ninety-three per cent of the 155 true NTPn were multidrug resistant. The most common antibiotype was resistance to macrolides, lincosamides, tetracycline, cotrimoxazole, and intermediate resistance to penicillin. PFGE analysis of the true NTPn strains identified 29 clones. One major clone accounted for 46.5% of the isolates, was prevalent through time and was disseminated in several day-care centres.
Conclusions: The isolation of presumptive NTPn requires further confirmation tests since these atypical strains are not easily identified. The prevalence of true NTPn among carriers ranged from 2.9 to 13.0% of the DR strains (average 7.0%). These isolates are frequently multidrug resistant and appear to lack the cps locus. The high number of clones found suggests that NTPn have diverse evolutionary origins. Careful monitorization of NTPn is important since these strains are not targeted by any of the pneumococcal vaccines commercially available.
O214: Persistence of sulphonamide resistance in the community despite lack of selection
D.C. Bean, D.M. Livermore, L.M.C. Hall (London, UK)
Objectives: Strategies to limit spread or reduce the prevalence of antibiotic resistance commonly assume that resistance will decline in the absence of selective pressure. However sulphonamide resistance in Escherichia coli persisted in the UK from 1991 to 1999, despite a dramatic reduction in prescribing. The goal of this study was to examine whether this trend had continued in 2004, nine years since the UK restriction in prescription, and to investigate the mechanisms that have lead to the maintenance of sulphonamide resistance.
Methods: Urinary E. coli isolates were obtained from the diagnostic microbiology laboratory of the Royal London Hospital. All consecutive isolates from urinary specimens from January through to March 2004 were included. Sulphonamide resistance genes, sul1, 2 and 3, were detected by PCR.
Results: Of the 391 E. coli isolates recovered in 2004, 45.5% were sulphonamide resistant compared to 46.0% in 1999, and 39.7% in 1991. The sul2 gene continued to be the most prevalent resistance determinant, present in 81% of resistant isolates in 2004 (79% and 67% in 1999 and 1991 respectively); 28% of resistant isolates carried both sul1 and sul2 genes. The sul3 gene was not found.
Conclusion: Continued persistence of sulphonamide resistance has been confirmed in 2004. One explanation for the persistence and spread of sul2-mediated sulphonamide resistance is that sul2 could be stably linked to other factors that continue to be under positive selection pressure. Thirty-eight sul2 plasmids were therefore transferred to a fully susceptible E. coli host strain. Sul2 was frequently found to be co-transferred with other antibiotic resistance markers, most notably ampicillin (76%) and streptomycin (74%) resistance. Location of sul2 adjacent to the streptomycin resistance genes strA and strB has been noted before and was confirmed in most plasmids; however streptomycin is now rarely used in clinical practice. Preliminary results indicated that there was not a similar physical linkage with an ampicillin resistance determinant. DNA fingerprinting and the pattern of resistance profiles demonstrated that sul2 plasmids were extremely diverse. The data suggest that sul2 (with strAB) is borne on a discrete genetic element that is not stably linked to other selectively advantageous determinants, but has been able to mobilise and disseminate amongst a wide variety of plasmids in clinical E. coli.
Predictors of the clinical course of HIV infection and therapy
O216: HIV and non-HIV-related deaths and their relationship to immunodeficiency; the D:A:D study
N. Friis-Møller, R. Weber, C.A. Sabin, P. Reiss, A. D'Arminio Monforte, F. Dabis, W. El-Sadr, S. De Wit, L. Morfeldt, M. Law, C. Pradier, G. Calvo, C. Holkmann Olsen, A.N. Phillips, J.D. Lundgren on behalf of the D:A:D Study Group
Objectives: Deaths in people with HIV infection are often classified according to whether they are HIV-related or not. We aimed to study whether deaths generally supposed to be unrelated to HIV are in fact more likely to occur in people with a low CD4 count.
Methods: D:A:D is a prospective study of 23,441 patients (pts) from 11 existing cohorts in Europe, Australia and the US. Detailed information on deaths occurring between the initiation of D:A:D in 2000 and Feb 2004 was collected; causes of death were coded centrally. Relative rates (RR) of factors associated with deaths from each cause were calculated using Poisson regression.
Results: Of the 23,441 persons, 82% had used ART prior to enrolment (median exposure 2.8 years). Over the study period, 1248 (5.3%) pts died (incidence: 1.6 deaths/100 person-years). The leading cause of death was AIDS (30%) followed by liver-related death (14% – of which 79% were associated with chronic viral hepatitis), death from heart disease (incl. cardiovascular disease; 9%), and death from non-AIDS malignancies (8%). The proportion of deaths from these causes remained stable over time. AIDS-related deaths were, as expected, strongly associated with the latest CD4 cell count (RR of death from an AIDS-event in pts with latest CD4 count <50 cells/L versus >500 cells/L after adjustment for HIV RNA, age, cohort, race: 96.4 [95% CI: 61.6–150.7], p < 0.0001). Liver-related deaths (RR 26.6 [12.9–54.7], p < 0.0001) and deaths from non-AIDS malignancies (23.5 [9.4–58.7], p < 0.0001) were similarly strongly associated with latest CD4 count; the relationship with death from heart disease was less strong but remained significant (3.1 [1.2–8.2], p = 0.02). The trends persisted after lagging the analyses to associations with CD4 counts 3 and 6 months earlier.
Conclusions: Deaths from causes that are generally referred to as non-HIV related are more likely to occur in persons with lower rather than higher CD4 counts. Although residual confounding cannot be ruled out, it seems that low CD4 cell numbers contribute to a proportion of such deaths. It appears that deaths occurring in persons with a very low CD4 count can only be categorized as non-HIV-related if there is clear evidence that the patient's immunodeficiency did not contribute to the death.
O217: HIV-patients across Europe: regional differences in patient characteristics and AIDS diagnoses
D. Podlekareva, W. Bannister, L. Viksna, A. Mocroft, B. Knysz, P. Reiss, N. Chentsova, D. Duiculescu, J.D. Lundgren, O. Kirk on behalf of the EuroSIDA study group
Background: The HIV epidemic shows major differences across Europe, including marked differences in prevalence and incidence of AIDS defining disease (ADD). These data have previously been reported from the EuroSIDA study. However, results were based on HIV-patients (pts) not exposed to HAART and were restricted to Western Europe. Since 1999, the EuroSIDA study has expanded to Eastern Europe.
Objectives: To compare characteristics of pts within EuroSIDA in European regions and to assess any regional differences in the prevalence and pattern of ADD with special focus on Eastern Europe.
Methods: Analysis of 7104 HIV-pts under active follow-up in September 2003. ADD made more than 1 year prior to recruitment were excluded to minimise potential biases. The regions are: South (SE), West Central (WC), North (NE), East Central (EC) and East (EE).
Results: Pts in EE were younger and primarily intravenous drug users (IDU); a high percentage of them were co-infected with HCV. Data shows more a recent HIV epidemic in EC and EE regions (Table 1). Significantly fewer pts in EE were taking HAART in late 2003 (Table 1), this remained significant after adjustment. 1181 pts had experienced at least one ADD by September 2003. The regional differences observed include a higher proportion of Kaposi's sarcoma in SE, WC and NE (p < 0.001). EE is remarkable by a high prevalence of PCP, and HIV wasting syndrome while pulmonary Mycobacterium tuberculosis (TB) infections were more prevalent in EC (p = 0.002) (Figure 1).
Table 1.
Characteristics of patients followed in September 2003 in the EuroSIDA study
| SE (n = 1888) | WC (n = 1911) | NE (n = 1974) | EC (n = 890) | EE (n = 441) | p-value | |
|---|---|---|---|---|---|---|
| Age, yrs; median (IQR) | 41 (37–47) | 43 (39–51) | 44 (39–52) | 36 (31–44) | 30 (24–39) | <0.001 |
| Female, % | 28 | 23 | 18 | 30 | 31 | <0.001 |
| IDU, % | 29 | 14 | 11 | 30 | 51 | <0.001 |
| AIDS diagnosis, n(%) | 509 (27) | 588 (31) | 684 (35) | 214 (24) | 117 (26.5) | <0.001 |
| HCV, % | 30 | 17.5 | 13 | 34 | 33 | <0.001 |
| CD4 count cells/mm3; median (IQR) | 459 (291–679) | 429 (281–601) | 449 (300–620) | 484 (297–659) | 337 (185–593) | <0.001 |
| Nadir CD4 count cells/mm3; median (IQR) | 150 (57–263) | 131 (49–229) | 113 (42–200) | 144 (65–270) | 270 (131–476) | <0.001 |
| Time from HIV diagnosis, mths; median (IQR) | 122 (78–164) | 134 (96–177) | 136 (96–186) | 75 (39–119) | 32 (18–53) | <0.001 |
| On HAART, % | 77 | 80 | 84 | 78 | 30 | <0.001 |
SE: Spain, Portugal, Italy, Greece, Serbia and Montenegro, Israel, Argentina; WC: France, Belgium, south Germany, Luxembourg, Switzerland, Austria; NE: United Kingdom, Ireland, Netherlands, north Germany, Denmark, Sweden, Norway; EC: Poland, Czech Republic, Slovakia, Hungary, Romania; EE: Estonia, Latvia, Lithuania, Belarus, Ukraine, Russia
Fig. 1.

AIDS defining diseases at September 2003 according to regions
Summary: These preliminary results reflect substantial regional differences in demographic and clinical characteristics of HIV-pts across Europe and demonstrate a more recent epidemic in EC and EE. There is low usage of HAART in EE compared with other regions including EC, which requires further follow-up and monitoring of pts in this region. In EuroSIDA a high proportion of AIDS pts in EC have been diagnosed with pulmonary TB, and with longer prospective follow-up the prevalence in EE may also increase. A high prevalence of multi-resistant TB has been reported in these regions, thus further research is needed. The high prevalence of HIV wasting syndrome and low percentage of other diseases in EE might at least in part be due to the lack of complex diagnostic technologies, experience and resources. More detailed analyses are in progress and as follow-up accumulates, particularly in EC and EE, analyses can focus on prospectively characterising ADD patterns.
O218: Detection of HIV sequences in colon bacteria of AIDS positive patients
V. Zajac, M. Kovac, S. Ciernikova, M. Mego, P. Rauko, V. Stevurkova, D. Stanekova, M. Mokras (Bratislava, SVK)
Objectives: The hypothesis whether bacteria from intestinal tract of HIV-1 positive patients carry HIV-like sequences was examined.
Material and methods: Bacteria and Patients. Intestinal bacteria were isolated from 51 HIV positive patients from USA and Slovakia and 10 healthy individuals. PCR amplification. Polymerase chain reaction specific for HIV sequences was carried out using these primers: P38F: ATAATCCACCTA TCCCAGTAGGAGAAT; P39R: TTTGGTCCTTGTCTTATGTC CAGAATG; P1F: CATTTGGAAAGGACCAGCAAAACTACT; E1R: TCATATGCTTTAGCATCTGATGCACAA; E68F: AGCA GCAGGAAGCACTATGG; E69R: CCAGACTGTGAGTTGC AACAG; G3F: TTGGACATAAGACAAGGGCCAAAA; G4R: GTCGTTGCCAAAGAGTGATTTGAG; Hybridization. 32P-labeled probes were following: 38-39; 68-69, P1-E1 and G3-G4.DNA sequencing. The sequencing reaction was performed using Big Dye Terminator kit and sequences were resolved on 310 Genetic Analyzer. Gentamicin protection assay (GPA) HL-60 cells and human lymphocytes were infected with bacteria of HIV patients (number of cells: HL-60 5 × 106; bacteria: 1 × 108). Following GPA was performed as previously published.
Results: Colony hybridization with HIV-specific probes was found positive. In a control experiment, bacteria were diluted to concentration 10-10 and plates with single colonies were analyzed. Since at least 70% of these colonies were found positive for any of previously tested HIV fragments, contamination with human cell debris appears unlikely. DNA of all positive isolates was amplified in PCR reaction with all four sets of primers. Sequencing of these products revealed more than 90% homology with the reference HIV sequence. HIV sequences were not present in samples isolated from healthy persons. GPA was used to evaluate the ability of HIV-positive intestinal bacteria to enter HL-60 cells. As shown in the table 1, bacteria carrying viral sequences showed approximately 15 times higher affinity to HL-60 cells then bacteria isolated from carcinomas. DNA extracted from HL-60 cells carrying an intracellular bacteria showed a strong positivity in hybridization with HIV probes. The same results were obtained three weeks after the internalization, although, no intracellular bacteria could be detected by GPA.
| Patient/bacterial clone | Number of bacterial colonies |
|---|---|
| HIV positive patients | |
| P15/7 | 2264 |
| P1/4 | 1340 |
| P3/3 | 1680 |
| M1/6 | 481 |
| 725/5 | 1140 |
| M12/5 | lysis of HL-60 cells |
| K1/1 | lysis of HL-60 cells |
| Colon cancer patients | |
| TuSG/1 | 71 |
| 883S/3 | 104 |
| MZRa/3 | 44 |
| negative control | <5 |
Conclusions: 1. Sequences resolved from intestinal bacteria of AIDS patients revealed at least 92% homology with HIV-1. 2. These bacteria likely enter HL-60 cells and the viral content remains in the host cells even when bacterial carriers are not detectable.
O219: CCR5 polymorphism as potent factor affecting susceptibility to HIV-1 infection in Polish population
E. Piasecki, K. Rybka, K. Zwolinska, B. Knysz, J. Gasiorowski, A. Gladysz (Wroclaw, PL)
Objectives: CCR5 protein is one of the HIV coreceptors, particularly important in early stages of the infection when R5 HIV strains are predominant. An allelic form of CCR5 gene–CCR5-delta32 encodes an inactive receptor. Individuals homozygous for CCR5-delta32 are almost completely resistant to HIV infection. The heterozygosity is generally thought to be connected with delayed progression of the infection. However, there is no agreement whether the possessing of CCR5-delta32 gene is significant in particular subgroups of patients. Since the distribution of CCR5-delta32 gene is geographically-dependent, our analysis of Polish population is limited to Lower Silesia Region.
Methods: The genotype was determined by polymerase chain reaction method. Genomic DNA was extracted from peripheral blood by digestion with proteinase K and purification on columns according to manufacturer's protocol. The primers pair amplified a 182 bp fragment from wild type gene and 150 bp from gene with delta32 deletion.
Results: In control group consisting of healthy, non-infected, non-exposed to HIV individuals frequency of CCR5-delta32 allele was found to be 10.3% (16 of 78 individuals were heterozygous for CCR5). In HIV-1-infected patients significantly lower frequency was observed (6.3%; 34 heterozygotes among 268 tested patients). On the contrary, analysis of exposed uninfected group (sexual partners of HIV-1-infected patients) showed high frequency of the gene (19.0%; 8 of 21 tested individuals were heterozygous). Conclusion: Heterozygotic CCR5/CCR5-delta32 individuals were significantly less susceptible to HIV-1 infection. Gene frequency of CCR5-delta32 was found to be three times higher in exposed uninfected than in infected patients. Differences observed in Polish population were bigger than that described in papers based on American or Western European population suggesting significant clinical importance of CCR5-delta32 in Polish population of HIV-1 exposed patients.
O220: Reduced antibody-mediated immunity to malaria in Zimbabwean adults coinfected with HIV-1
L.S. Vestergaard, P. Kallestrup, R. Zyniama, B. Mudenge, J. Gerstoft, L. Hviid, H. Ullum (Copenhagen, DK; Harare, ZW)
Objectives: In sub-Saharan Africa, co-infection with HIV-1 has been shown to increase the susceptibility to Plasmodium falciparum malaria, suggesting that HIV-1 compromises acquired malarial immunity. As IgG antibodies specific for parasite-encoded variant surface antigens (VSA) on the surface of infected red blood cells are involved in naturally acquired immunity to P. falciparum, we examined these antibodies as a possible mechanism of the HIV-1 induced loss of protection.
Methods: VSA-specific plasma IgG was determined by flow cytometry in samples from 198 HIV-1-seropositive and 181 HIV-1-seronegative men and non-pregnant women living in a rural area in Zimbabwe with low-to-moderate malaria transmission. Antibodies against another malaria antigen, the repetitive R2-region of glutamate rich protein (GLURP-R2), and total IgG were also measured.
Results: Levels and repertoires of anti-VSA IgG were reduced among HIV-1-seropositive individuals, were positively associated with CD4+ T cells and were negatively associated with HIV-1 viral load. By contrast, anti-GLURP-R2 IgG levels were not affected by HIV-1, while the levels of total IgG were increased in HIV-1-seropositive individuals.
Conclusions: Our results point to a virus-induced reduction of variant-specific humoral immunity as an important cause of HIV-1 induced increased susceptibility to P. falciparum malaria.
O221: Risk of AIDS and death at given HIV-RNA and CD4 count levels, according to specific antiretroviral drugs in the CART regimen
C. Holkmann Olsen, J. Gatell, B. Ledergerber, C. Katlama, N. Friis-Møller, J. Weber, A. Horban, S. Staszewski, J. Lundgren, A.N. Phillips for the EuroSIDA Study Group
Objectives: It is unknown whether the relationship between the HIV-RNA/CD4 count and risk of clinical disease continues to hold true for newer antiretroviral drugs, as drugs licensed after 1997 have been approved on the basis of clinical trials only assessing short-term surrogate endpoints. We hypothesised that virological and immunological markers have the same meaning in terms of long-term clinical effect according to different drug regimens, rather than, for example, newer drugs having an additional effect leading to a higher or lower risk of AIDS/death for given HIV-RNA/CD4 levels when compared with others.
Methods: Analysis included patients taking combination-antiretroviral-therapy (CART) regimens containing two non-abacavir nucleosides plus a ‘third drug’ of a non-nucleoside reverse transcriptase inhibitor, a (possibly ritonavir boosted) protease inhibitor or abacavir. We compared rate ratios of AIDS and death at given, latest HIV-RNA & CD4 counts levels according to the nucleoside pair and specific third drugs patients received as antiretroviral therapy. In multivariate analysis we adjusted for latest CD4 count, HIV-RNA, age, exposure group, prior AIDS, calendar year, time from starting CART, time on current combination.
Results: Among a total of 9,802 patients, 6814 were included in this analysis and contributed a total of 22,766.6 person-years of follow-up. Over follow-up, median CD4 count was 353 cells/μL, HIV-RNA 199 copies/mL. 889 events of new AIDS or death occurred over follow-up of which 125 were deaths. AIDS/death incidence rates for any given CD4 or HIV-RNA category were similar regardless of specific drugs being used; see figure. Adjusted rate ratios (RR) for individual drugs compared with indinavir (for which clinical endpoint trials are available) were all close to 1 and with relatively narrow 95% confidence intervals (CI) all overlapping 1; e.g. nelfinavir RR 0.99 (95% CI 0.76-1.28); efavirenz RR 0.83 (0.57-1.20); abacavir RR 1.01 (0.64-1.60); see table. Results were similar for different nucleoside pairs with adjusted RRs overlapping 1 when compared with other.
Fig. 1.

Rates of AIDS/death according to latest CD4 count and specific drugs used
Table 1.
Crude and adjusted rate ratios (RR) for occurence of AIDS disease or death from a Poisson regression model
| Rate ratio (95% Cl) P-value | ||||
|---|---|---|---|---|
| Univariable | Multivariable | |||
| Nucleoside pair | ||||
| AZT/3TC | 1.05 (0.84–1.34) | P = 0.66 | 1.21 (0.93–1.58) | P = 0.15 |
| d4T/ddl | 1.08 (0.86–1.36) | P = 0.49 | 1.26 (0.97–1.62) | P = 0.08 |
| d4T/3TC | 0.98 (0.72–1.32) | P = 0.87 | 1.15 (0.84–1.58) | P = 0.38 |
| other | 1.00 | 1.00 | ||
| Third drug | ||||
| indinavir | 1.00 | 1.00 | ||
| ritonavir | 1.14 (0.84–1.54) | P = 0.41 | 0.88 (0.66–1.17) | P = 0.39 |
| saquinavir | 1.80 (1.36–2.41) | P < 0.0001 | 1.04 (0.78–1.38) | P = 0.80 |
| nelfinavir | 0.78 (0.59–1.02) | P = 0.069 | 0.99 (0.76–1.28) | P = 0.92 |
| IDV/r of SQV/r | 0.56 (0.41–0.77) | P = 0.0004 | 0.79 (0.59–1.05) | P = 0.10 |
| Iopinavir/r | 1.04 (0.69–1.57) | P = 0.83 | 1.08 (0.65–1.82) | P = 0.76 |
| abacavir* | 0.72 (0.49–1.05) | P = 0.09 | 1.01 (0.64–1.60) | P = 0.97 |
| nevirapine | 0.57 (0.42–0.78) | P = 0.0004 | 0.91 (0.65–1.28) | P = 0.59 |
| efavirenz | 0.62 (0.46–0.84) | P = 0.002 | 0.83 (0.57–1.20) | P = 0.31 |
NB. RR = rate ratio per extra year; # counted only when 3rd drug; Indinavir = IDV; Ritonavir = r; Saquinavir = SQV; AZT = ZDV = zidovudine; 3TC = lamivudine; d4T = stavudine; ddl = didanosine.
Conclusions: The results indicate that AIDS/death rates for given CD4 count and HIV-RNA categories are similar, regardless of CART regimen being taken. This provides reassurance that HIV-RNA-and CD4-values in individual patients receiving newer drugs have the same meaning in terms of AIDS/death risk, regardless of specific antiretroviral regimen.
O222: Variable prediction of clinical outcome of the GART interpretation system Guidelines 6.0 and Virtual Phenotype
F. García, I. Viciana, M.C. Nogales, F. Fernández, J.C Palomares, F. Lozano, M. Márquez, P. Viciana, J. Hernández-Quero, A. Pinedo, M.C. Maroto on behalf of RAERA study group Red Andaluza para el Estudio de las Resistencias a Antirretrovirales Andalucia, E
Background: A variable prediction of clinical outcome in terms of virologic response have been reported for genotypic antiretroviral resistance testing (GART) interpretation systems. In addition, serious discrepancies with Virtual Phenotype (vPh) in the interpretation of certain drugs have been also reported. Objective: To analyse the influence on clinical outcome, in terms of indetectable viral load three months after changing therapy, of two GART interpretation systems: Guidelines 6.0 (Bayer) and Virtual Phenotype (Virco).
Patients and Methods: Virological, clinical and immunological data from 258 patients from Andalucia (Spain) undergoing GART were collected. GART was interpreted with Guidelines and with vPH and was given to the clinician to change therapy. Virological and immunological data 3 and 6 months after changing therapy were also recorded, and a database with these data and with Guidelines genotypic sensitivity score (GSS) and vPh sensitivity score (vPhSS) was developed. Two ways of interpreting vPh were included: vPh1, based on the % of susceptible strains; and vPh2, based on the fold change on IC50 and the vPh cutoff. Results: 81% of the patients in this study had failed 2 or more lines of therapy. Mean No. of mutations in the protease was 4 ± 2.87, and in the RT was 5 ± 2.45 (2.78 ± 1.77 NAMs); adherence was greater than 80% for 78% of the patients and median CD4 count and Log Viral Load (copies/ml) was 324.5 and 3.94 respectively. Undetectable VL was achieved for 39.6% of the patients at 3 months and for 44.4% at 6 months; median decrease in Log VL from baseline was 1.64 and 1.66 at 3 and 6 months respectively. Mean number of active drugs in the new regimen was 1.78 using Guidelines 6.0 for interpretation and 2.08 and 2.4 for vPh1 and vPh2. Odds ratio for achieving indetectable viral load at month 3 was 1.45 for Guidelines (1.06–1.96), 1.53 for vPh1 (1.00–2.32) and 1.41 for vPh2 (1.00–1.98). In the multivariate analysis with the GART interpretation systems evaluated, only Guidelines was predictive of achieving indetectable VL at 3 months (OR, 1.42; 95% CI, 1.05–1.94).
Conclusions: Guidelines 6.0 is a better predictor of undetectable viral load at three months than Virtual Phenotype. Other participants from RAERA group: M. Alvarez, S Carlos, Martinez NM, Serrano MC, J Parra, MC Gálvez, J Pasquau, MA López-Ruz, V Gutierrez-Ravé, E Pujol, E Pérez Guzman, C Fernández, A de la Iglesia, A Terrón, A. Alle, D Peña, A del Arco, M Castaño.
O223: Clinical usefulness of the tonsillar HIV genotyping-guided change of therapy in HIV-1 infected patients with immune discordant response to HAART
J. Parra-Ruiz, M. Alañón, M. Martínez, L. Muñoz-Medina, M.A. Martínez-Pérez, F. García, M.A. López-Ruz, J. Hernández-Quero (Granada, E)
Introduction: Approximately 10–20% of HIV-1-infected patients receiving HAART show an immune discordant response defined as persistently low CD4 cell counts, despite a significant decrease in plasma virus load. Incidence of AIDS-defining events and deaths among patients with immune discordant responses are higher than among patients with complete response or virologic discordant response. Interventions to improve CD4 T cell response are needed.
Objective: To investigate the existence of active viral replication in tonsillar tissue of patients with complete pVL suppression and, if present, to make a genotyping test.
Material and methods: Nucleic acid was extracted using QIAamp DNA mini kit (Quiagen), with a subsequent HIV viral load determination (Cobas AMplicor HIV-1 Monitor – Roche). Resistance genotyping test was made using TruGeneTM HIV-1 (Bayer).
Results: Tonsillar biopsy was made in 13 patients, 12 men and 1 woman. Data are expressed for 11 patients (2 samples are being processed at the moment of writing this abstract). Amplification was possible in 8 of them (72%), being the genotype WT for the RT in 4 (50%) and for the protease gene in 3 (38%). Medium CD4 T-cell nadir was 37 cells/μL (range 1–96). Eight patients (73%) were on C3 status of the CDC, 4 of them because of visceral leishmaniasis (37%). Medium CD4 T cell count at the moment of tonsillar biopsy was 178 cells/μL (range 111–223), and all of them have HIV-1 pVL < 50 copies/ml for a prolonged period of time (medium 22,5 months, range 12–52). After genotyping, HAART was modified in 6 patients, with an increase of the CD4 T cell count >50 cells/μL at 6 months in 2 of them. Three other patients started on IL-2 therapy plus optimized HAART, with an increase of the CD4 T cell count >50 cells/μL at 6 months in one after three cycles of IL-2, being the other two waiting for the results of the 2nd and the 1st IL-2 cycle respectively. The remaining patient was lost to follow up. Of the other 6 patients that did not modify HAART based on the data from tonsillar genotyping test, only 1 patient has shown an increase of CD4 > 50 cells/μL in the next 6 months.
Conclusions: Despite prolonged complete viral suppression in sera, many patients with immune discordant response maintain viral replication in lymph nodes. Tonsillar HIV amplification and subsequent genotyping-guided change of therapy can be a useful tool to decide the best HAART and to evaluate the need IL-2 therapy.
Antimicrobial growth promoters in food animal production
K232: Antimicrobial growth promoters in food animal production
C. Wegener (Søborg, DK)
Feeding antibiotics to animals in order to make them grow faster has been common practice in intensive agricultural production systems since the late fifties. In December 2002 the European Union member states banned the use of antimicrobials as growth promoters from January 2006. What lies behind this change in attitude? In 1997 the World Health Organization recommended; that the use of antibiotics for growth promotion should be terminated if they are also used for treatment in animals or humans, and furthermore, that the use of other classes of antimicrobials as growth promoters should be gradually phased out and substituted with safer non-antimicrobials alternatives. In April 1998, the Danish poultry, cattle and pig producers terminated the use of antimicrobials growth promoters. The DANMAP programme monitors the impact of the withdrawal of antimicrobial growth promoters on antimicrobial resistance and antimicrobial usage in Denmark. The total volume of active antimicrobials used for food animals is reduced by more than 50%. Resistance to the most commonly used AGP's tylosin, virginiamycin, avoparcin and avilamycin has declined significantly. In a number of European countries the occurrence of VRE in humans in the community has declined. The producers in Denmark were concerned about terminating the use of AGP's. We have analyzed the national poultry productivity data. Productivity were not affected by the termination, and mortality rates were likewise unaffected. Feed efficiency has changed slightly however, the savings on antibiotics for growth promotion offsets the extra cost of feed. In finishing pigs no or only a very limited effect of the withdrawal of AGP's has been observed, however in weaned pigs, some herds have experienced problems with post weaning diarrhoea. The overall productivity has been increasing after the termination. The prevalence of Salmonella in broiler flocks and chicken products as well as in swine herds and pork in Denmark has continued to decline after the withdrawal of the growth promoters. The European Union will terminate the continuous feeding of antimicrobials to healthy animals for growth promotion. Experiences from Denmark, as well as from other countries, such as Switzerland, Finland and Sweden, show that banning antimicrobial growth promoters has a minimal impact on agricultural productivity, but leads to major reductions in antimicrobial resistance.
Crosstalk between bacterial pathogens and their host cells
K233: Crosstalk between bacterial pathogens and their host cells: the Listeria paradigm
P. Cossart (Paris, F)
To establish and maintain a successful infection, microbial pathogens have evolved a variety of strategies to invade the host, avoid or resist the innate immune response, damage the cells and multiply in specific and normally sterile regions. Based on their capacity to deal with these critical issues, bacteria can be grouped in different categories. This talk will focus on the tactics used by enteroinvasive bacteria (e.g. Listeria, Salmonella, Shigella and Yersinia) to trigger their uptake by epithelial cells and discuss their intracellular life-styles. During phagocytosis by phagocytes, bacteria play a passive role. In contrast during bacterial-induced phagocytosis, the bacterium is the key and active player in the complex interplay between the invading microbe and the host cell. Another critical element is the cytoskeleton whose plasticity is maximally exploited. After internalization, some bacteria remain in a vacuole, in which they replicate. They prevent the normal maturation and trafficking of the phagosome and impair its normal bacteriolytic activites. Other bacteria escape from the vacuole and replicate in the cytosol. In some cases, they also move and disseminate by means of an actin-based motility process. How the cell senses the bacterial intruders and adjust its transcription and translation programme to its new life with a parasite is an important issue. Apoptosis and anti-apoptosis, as well as cell cycle and inflammation related pathways, are reprogrammed after infection to help the cell to survive the stress induced by the infection. The success of an infection depends on the two messages that the two players – the bacterium and the cell-send to each other. At each step of the infectious process, the bacterium exploits the host machinery to its own profit. The two last decades have seen an accumulation of information concerning the molecular mechanisms underlying host-pathogens interactions during infection. A major issue is now to validate in vivo the molecular and cellular events analyzed in vitro. This raises the importance of having a relevant animal model. In some cases (e.g. Shigella) it is still lacking. In others, it is already existing or has been generated by use of sophisticated transgenesis approaches (e.g. Listeria). There is no doubt that progress should be done to provide clues in the ongoing battle against bacterial diseases and for elaborating new therapeutic strategies.
Infection control: challenges now and ahead
K235: Infection control: challenges now and ahead
W.H. Seto (Hong Kong, HK)
With the outbreak of Severe Acute Respiratory Syndrome (SARS) and the Avian Flu, Infection Control is finally receiving the priority it deserves. However it is important to ensure that this is a genuine resurgence of the field and not simply a reaction. The Joint Commission of the United States, when introducing their new Infection Control standards for 2005, pointed out that it must not be a ‘knee jerk reaction’, relegating hospital infection as merely the ‘problem of the month’ but rather it ought to be a long-term commitment to ensure patient safety. The challenge now is to use the opportunity for establishing the proper infrastructure for Infection Control and the essential ingredients would be discussed. Summary data of the situation in various countries including Hong Kong would be presented. The challenges ahead are for Infection Control to focus on the relevant issues, which can generate worthwhile long-term results. This would include a discussion on the ‘Seven Healthcare Safety Challenges’ for Infection Control presently promoted by the Center for Disease Control (United States) and the areas of focus for Infection Control by the World Alliance for Patient Safety of the WHO. One must avoid the tendency to over-react because of a severe outbreak like SARS. It includes the over emphasis on intricate protocols for outbreak management or the building of expensive isolation facilities. A summary of the actions resulting from the SARS outbreak for some hospitals in Hong Kong would be presented, with some examples of possible over-reactions in response.
Burkholderia, Pseudomonas and emerging infections in cystic fibrosis
S236: Diversity, ecology and identification of Burkholderia cepacia complex and other non-fermenting Gram-negative bacilli in cystic fibrosis specimens
P. Vandamme (Ghent, B)
Pulmonary infection in cystic fibrosis (CF) patients is typically characterised by a narrow spectrum of micro-organisms and is dominated in older patients by Pseudomonas aeruginosa. Burkholderia cepacia complex, Stenotrophomonas maltophilia, Achromobacter xylosoxidans and a growing number of non-fermenting gram-negative bacilli (NFGNB) have emerged as potential pathogens in CF lung disease. Several of these novel bacteria are naturally multiply resistant to antibiotics, cause chronic infection, and, although probably environmental in origin, are capable of patient-to-patient spread in the CF population. Several of the best known NFGNB in medical microbiology are considered ubiquitous. Organisms like Pseudomonas aeruginosa, Burkholderia cepacia complex, Stenotrophomonas, and Acinetobacter occur in a range of environmental and clinical niches and are metabolically and genetically versatile. In spite of their demonstrated potential for genetic adaptation and evolution, several clones of NFGNB are reported to occur in a very wide geographical area for prolonged periods of time. The considerable genomic versatility has allowed many of these NFGNB to occupy different environmental niches and to interact with their environment and hosts in several ways. The genus Burkholderia will be used to exemplify different types of environments and interactions. The accumulated evidence of reports of the natural behavior of near to forty Burkholderia species suggests that their ancestor was a soil bacterium that lived in close association with plants. Many plants leak nutrients in the rhizosphere environment to attract bacteria that protect them from harmful soil organisms, which include other bacteria, fungi, and nematodes. The Burkholderia ancestor and its offspring have developed a chemical warfare arsenal to compete for those nutrients present in the plant rhizosphere and interact with the plants through – among others – their nitrogen metabolism and the production of plant hormones. In this interaction process, burkholderias invaded the fungi of the plant mycorrhizal community, the root system, and the plant shoot tissues, and managed to colonize several ecosystems in the plant, thereby interacting mostly in a symbiotic manner with their hosts. Although we may know many isolation sites and sources for contamination of vulnerable patients, it is obvious that we only start to learn about the natural niche and the ecological role therein of many, if not most, of these NFGNB. One underlying reason is the heavily underestimated species richness in many of these groups of bacteria. Our knowledge of the biological diversity of several genera of NFGNB underwent dramatic changes during the past decades due to the detection of a large number of novel species, but also as a consequence of the criteria for bacterial genus and species delineation as established in the 1980s. Very often, this taxonomic complexity is associated with diagnostic problems. Recording this diversity will allow to design accurate identification procedures for those species that are of particular interest. Understanding the natural lifestyle of such organisms may however be instrumental to understanding their behavior in humans. The lecture will focus on the natural diversity of NFGNB which emerged as potential pathogens in CF lung disease. It will address the ecological role of these bacteria in the context of epidemiological investigations and will give an overview of recently developed identification tools.
S237: Stenotrophomonas, Achromobacter, Pandoraea and other emerging environmental pathogens
N. Høiby (Copenhagen, DK)
Cystic fibrosis patients suffer from recurrent and chronic lung infections caused by bacteria from the normal flora (S. aureus, H. influenzae, S. pneumoniae, M. catarrhalis) as well as bacteria from the environment, notably P. aeruginosa and the B. cepacia complex. The increasing life expectancy of CF patients due to the improved management of these infections, however, has revealed an increasing number of new environmental bacterial species, which have colonized CF patients, e.g. S. maltophilia, A. xylosoxidans, Pandoraea apista, Mycobacteria other than tuberculosis, and Nocardia. The clinical situation resembles the time when it was not realized, whether P. aeruginosa was a pathogen or merely an innocent colonizer of the respiratory tract of CF patients. Since the number of colonized/infected patients in each CF centre is restricted, and since co-infection is frequently present, the clinical dilemma whether to treat or not is difficult to solve. Experience from P. aeruginosa infection in CF patients, however, showed that it is possible to distinguish between innocent colonization and tissue-damaging chronic infection by measuring the specific antibody response to the offending bacteria, and this approach has been used successfully for several years in the Danish CF Center at Rigshospitalet.
Climate and environment: impact on infectious diseases
S238: The environment as a reservoir for non-culturable but infectious, antibiotic-resistant bacteria: a new risk for human health?
M. Lleo, C. Pruzzo, C. Signoretto, P. Canepari (Verona, Genoa, I)
Human pathogens are frequently transmitted from person-to-person, directly or via vectors/vehicles, thus perpetuating their parasitic cycle. However, they are also released into the environment, for example with faeces, where they encounter adverse conditions (oligotrophy, direct sunlight, extreme temperatures and salinity) which prevent cell division. Under stressing conditions, human pathogens and components of the normal microflora do not necessarily die but might persist even for long periods of time (several months) in that they are capable of activating a survival strategy known as the viable but nonculturable (VBNC) state. When in this phase, bacteria lose their ability to form colonies on culture media but are still viable and capable of metabolic activity and gene expression and show a specific protein profile and cell wall modifications. Moreover, VBNC cells, which are capable of maintaining their pathogenic potential (adhesion to animal tissues, toxin synthesis), may be able to resume division on returning to favourable environmental conditions such as those encountered in the human gut after ingestion of contaminated water or foods. A significant amount of data on VBNC bacterial forms derives also from our studies conducted on a waterborne pathogen such as Vibrio cholerae whose role as a seawater reservoir involved in cholera epidemics has been definitively demonstrated. Recently, using a vancomycin resistant Enterococcus faecalis model, we have demonstrated that bacteria are capable of maintaining and expressing antibiotic resistance during the VBNC state and after resuming their divisional capability when permissive conditions are restored. On the basis of their characteristics, VBNC cells could therefore represent a potential risk for human health in that (i) they might constitute a reservoir of infectious and antibiotic-resistant bacterial forms involved in disease transmission and persistence, and (ii) they are undetectable with the standard culture methods. For this reason, for reliable evaluation of the microbiological quality of the environment is now mandatory to re-design the currently used procedures in order also to detect nonculturable bacteria.
S239: Remote sensing and epidemiology
A. Güell (Toulouse, F)
MacLehose et al., (Issues on Public Health, 15 March 2002), warned us about the new European public health threat associated with communicable diseases. They express concern about European capacity to responding to such challenge. The picture gets grimmer when we know that the Rift Valley Fever (RVF), the dengue hemorragic fever, malaria, cholera, meningoccal meningitis, West Nile virus, are re-emerging world-wide. Half of the world population becomes at risk, and about 4 millions humans die per year (half under 5-year old). Increased migration, overuse of medicine in Europe, lack of medicine in the developing world, inappropriate funding do not facilitate proper responses to the challenge of control and prevention. Nevertheless since 1999, a French effort and a multidisciplinary consortium has been developing ‘innovative international space monitoring and surveillance schemes’. The French space agency (CNES), along with experts on public health i.e. Institut Pasteur, national institute for agronomic research, institute for space medicine (MEDES), databases and environmental factors in-situ and from space (MEDIAS-France), have been implementing integrated on epidemiology based upon new technologies such as ‘tele-medicine’. Following the Johannesburg Summit 2002, a new French project or ‘RED GEMS’ (Re-Emergent Diseases Global Environment Monitoring from Space), is born. Its two pillars i.e., tele-epidemiology, and tele-medicine will enable real-time monitoring of human and animal data (epidemiology, clinical data, …), socio-economical data (habitat, migration, turmoil, …), biosphere (land cover, …), hydrosphere (rainfall, stagnant waters, wind stress, sea surface temperature, altimetry, algae blooms, …) and atmosphere (winds, convection, aerosols, …). Products and databases accessible from a dedicated Website will be delivered to Early Warning Systems (EWS) and Health Information Systems (HIS) for effective disease control strategy. The EMERCASE project monitoring the RVF in Senegal, and the dengue fever project in French Guyana are already building blocks of ‘RED GEMS’. Two other projects on cholera and meningococcal meningitis (type C) are under way. It is believed that this French initiative on space and public health will contribute to solving the new health challenge, to capacity building and multidisciplinary networking world-wide.
Crimean Congo haemorrhagic fever in southeastern Europe
S240: The clinical and epidemiological characteristics of CCHF and the impact of ribavirin therapy
O. Ergonul (Ankara, TR)
Crimean-Congo haemorrhagic fever (CCHF) is a fatal viral infection described in parts of Africa, Asia, Eastern Europe, and Middle East. CCHF was first recognized during a large outbreak among agricultural workers in the mid 1940s in the Crimean peninsula, and a recent outbreak was reported from Turkey. The virus belongs to the genus Nairovirus in the Bunyaviridae family and causes severe diseases in humans, with the reported mortality rate of 3–30%. The mortality rate of CCHF virus (CCHFV) infection was lower in Turkey than the previously reported epidemics. Genetic analysis of the virus isolates from Turkey revealed a close relation with the isolates from former Yugoslavia and southwestern Russia. Humans become infected through the bites of ticks, by contact with a patient with CCHF during the acute phase of infection, or by contact with blood or tissues from viremic livestock. The occurrence of CCHF closely approximates the known world distribution of Hyalomma spp. ticks. After a short-incubation period, CCHF is characterized by a sudden onset of high fever, severe headache, dizziness, and myalgia. Additional symptoms can include nausea, vomiting, diarrhoea, and somnolence. In severe cases, haemorrhagic manifestations, ranging from petechiae to large areas of ecchymosis, develop. The levels of liver enzymes, creatinine phosphokinase, and lactate dehydrogenase are elevated, bleeding markers are elongated. In diagnosis, enzyme linked immunoassay and real-time reverse transcription-polymerase chain reaction (RT-PCR) are used. Treatment options for CCHF are limited. Ribavirin was suggested as an effective drug in recent studies, and it was found to be beneficial. No adverse event related to ribavirin therapy was noted. Based on our experiences in Turkey, ribavirin should be given to the patients suspected of CCHF infection who have severe thrombocytopenia, elevated ALT, AST, AST/ALT levels. The hospital health care workers (HCW) are under serious risk of transmission of the infection, particularly during the follow-up of the patient, with hemorrhages from the nose, mouth, gums, vagina, and injection sites. Simple barrier precautions were reported to be effective, but rigorously applied. Based on the results of our studies, we do not encourage prophylactic ribavirin use among HCWs, instead, in such cases, we suggest rigorous daily follow-up of the individual, by checking complete blood count, and biochemical tests if necessary.
S241: Crimean Congo haemorrhagic fever: laboratory diagnosis and epidemiology in Europe
H. Zeller, M.C. Georges-Courbot (Lyon, F)
Crimean Congo haemorrhagic fever (CCHF) is a severe viral disease with a widespread distribution in subsaharian Africa and Madagascar, the Middle East, Pakistan, Iran, Turkey, Russia, Western part of China and some countries in Southern Europe (Kosovo, Albania, Bulgaria, Greece, …). The virus is able to produce severe human disease with high mortality rates (up to 30% in hospitalized patients). Due to the occurrence of nosocomial cases, CCHF virus is a major public health concern and is classified among the class 4 agents. The virus belongs to the family Bunyaviridae, genus Nairovirus. It is transmitted by hard ticks (Hyalomma, Amblyomma, Dermacentor, … sp). The natural cycle involves small rodents, birds and domestic ruminants. Humans can be infected via tick bites which occur in during the peak activity of the vectors (from March to October in Southern Europe), or by direct contact with infectious blood products. Usually the incubation period in humans ranges from 3 to 7 days but can be shorter. Initial clinical symptoms are not specific: fever, headache, abdominal pain, nausea, vomiting; they precede the haemorrhagic phase. Laboratory findings show leucopenia (particularly neutropenia), thrombocytopenia, liver enzyme (AST/AST) and LDH elevations. The virological diagnosis includes the detection of CCHF viral genome by RT-PCR (semi-nested or real-time PCR) and/or detection of CCHF antigen, in association with serology (detection of CCHF IgM and IgG antibodies using ELISA or IFA). The viraemia may last up to 10–14 days, even in the presence of specific antibodies. New tools using recombinant antigens for CCHF antibodies detection are now available. Viral isolation attempts from blood samples can be conducted under biosafety level 4 conditions on VeroE6 cells. Phylogenic studies have shown a large diversity among CCHF viruses. Seven major genetic groups have been identified, based on analysis of a 260 bp of the S (small) segment coding for the nucleoprotein. Recent viral strains from the Balkans (Albania, Kosovo, Bulgaria) clustered in the same branch with some strains from Southern of Russia and strains from Turkey. A few studies were undertaken on the M (medium) and L (large) segments which encode for the glycoprotein precursor and the RNA-dependent RNA polymerase, respectively.
Computerised decision support for management of bacterial infections
S247: Building TREAT – computerised decision support for antibiotic treatment
L. Leibovici, M. Paul, S. Andreassen (Petah-Tiqva, IL; Aalborg, DK)
The mortality rate associated with bacterial infections in the hospital is significant, and so are the related costs. Empirical antibiotic treatment that matches the in-vitro susceptibility of the pathogen (appropriate antibiotic treatment) and given early in the course of infection increases chances for survival. However, in only a small minority of patients the pathogen of infection or its susceptibilities are known on initiation of antibiotic treatment. For empirical treatment, the physician balances the antibacterial spectrum and activity of the drugs against their costs, adverse events, and their potential to induce resistance. Many times these calculations are wrong: about a third of patients are given inappropriate treatment, while about 20% are given superfluous drugs. In the TREAT project we built a computerized decision support system for prescription of antibiotic drugs. The TREAT system uses data on signs and symptoms, underlying conditions of the patient, laboratory and imaging results; and the distribution of pathogens and their susceptibility in the particular setting in which the patient acquired the infection, to assign probabilities to sites of infection, pathogens and their susceptibilities to antibiotics. It then balances the benefit associated with the different drugs or combinations of drugs against their costs, potential for side effects, and potential to induce resistance. A few of the system's features merit emphasis. First, it assigns a specific cost to induction of future resistance. We used local data, and data available from the literature, to draw a curve relating consumption to rise in resistance for each drug. To assign a cost to future resistance, we used a model similar to the one proposed to deal with optimal use of non-renewable resources Secondly, its core is a causal probabilistic network, which allowed us to combine knowledge and data from different sources in the same system. Last, it was built for easy calibration to new sites, by differentiating between universal factors (e.g., sensitivity and specificity of diagnostic tests); and local factors (e.g., distribution of pathogens and susceptibilities) that have to be calibrated anew at each site. The system was calibrated to three locations: Rabin Medical Center, Petah-Tiqva, Israel (Petah-Tiqva); Freiburg University Hospital, Freiburg, Germany (Freiburg); and A. Gemelli University Hospital, Catholic University, Rome, Italy (Rome); and tried in 2 phases, a non-interventional one; and a randomized controlled trial.
Hepatitis C virus: new targets for drug and vaccine development and markers for therapy
S248: Innate immunity, adoptive immunity and vaccine development
S. Abrignani (Siena, I)
There is no vaccine for HCV and the only treatment which has proven efficacious is IFN-therapy. However, the success rate of this treatment is not satisfactory, thus there is a pressing need to develop prophylactic as well as therapeutic vaccines. HCV copes very well with the host's immune system. Once HCV enters the body, it is cleared naturally in a minority of cases. While most HCV infections do elicit immune responses, evidence of immunity is controversial. Obviously, an ideal vaccine should protect from infection in that it should elicit sterilising immunity. However, in the case of HCV where infection can only be assessed by PCR, a more realistic goal might be to look for vaccines capable of protecting from chronic infection. After all, HCV acute hepatitis is not a serious public health problem and most of us would be satisfied with a vaccine that allowed subclinical acute infection but which after a few months would be cleared by the immune response. Overall, our view is that a candidate HCV vaccine would be one that protects from infection and/or progression to chronic infection by the major genotypes. Our experience in chimpanzees demonstrates that a subunit vaccine composed by a recombinant form of the envelope glycoproteins can prime antibody and CD4+ T-cell responses that protect from chronic infection by heterologous HCV strains. Based on these results, we have now started prophylactic as well as therapeutic clinical trials for such a vaccine.
Focus on Mycobacterium tuberculosis
O250: Isolation of Mycobacterium species from respiratory specimens for the diagnosis of tuberculosis using an automated sample preparation system based on magnetic particles
J. Lysén, H.K. Høidal Berthelsen, M. Espelund, U.H. Refseth (Oslo, N)
Objectives: The causative agent of tuberculosis (TB), Mycobacterium tuberculosis, is today the single greatest cause of mortality due to an infectious agents with 2 million people dying every year and 8 million new cases. The rising incidence of multiresistance Mycobacterium tuberculosis (MDRTB) represent an additional problem to public health, with higher death-rates and the requirement for much more extensive antibiotic treatment. Routinely, mycobacterium infections are diagnosed by microscopic examination for the presence of acid-fast bacilli (AFB) and by conventional culture techniques. Whereas AFB testing lack sensitivity, cultivation may take up to 2–4 weeks to determine the presence of mycobacterium due to the slow growth. Compared to culture, sensitivity using various nucleic acid amplification techniques (NAAT) available is much lower. This may be due to either insufficient sample preparation from respiratory samples or incomplete lysis of the mycobacterium cells. Thus, the requirement for both a rapid and sensitive diagnostic system for TB is still largely unmet.
Method: Here we present a new automated system for sample preparation of mycobacterium DNA from respiratory samples utilizing magnetic particles. In this system (chlamCAP, Genpoint, Norway), mycobacterium cells are initially adsorbed to uniquely coated paramagnetic particles and magnetically separated from the respiratory sample. A rapid lysis at RT releases DNA, which is then adsorbed onto the same magnetic particles. After washing, purified DNA is transferred microwells for NAAT analysis. Mycobacterium bovis (BCG) of the MTC group was spiked in growth medium and isolation was performed using the chlamCAP system on a Tecan Miniprep 75 customized to this particular application. Following isolation of mycobacterium DNA, the samples were analyzed by real-time PCR using primers specific for species belonging to MTC.
Results: The sensitivity obtained was <103 CFU/ml (positive PCR signal) as determined by plating. In addition, results obtained from heat-inactivated sputum samples containing 50% sputasol from patients suspected to be infected with M. tuberculosis, were in agreement with data from cultivation, demonstrating the robustness of the chlamCAP system.
Conclusion: Based on these results, we believe that the automated chlamCAP system in the future can promote the implementation of NAAT based methods in mycobacterium diagnostics, complementing today's enrichment systems.
O251: Prospective MIRU-VNTR typing of Mycobacterium tuberculosis isolates in the Midlands, UK: detection of a previously unsuspected large cluster of cases
J. Evans, K. Boese, E. Smith, G. Hong, P. Hawkey (Birmingham, UK; Omaha, USA)
Objectives: Effective control of TB depends on rapid detection of links between patients with active disease. IS6110 RFLP cannot provide rapid results to direct control measures in outbreaks. MIRU-VNTR PCR typing of M. tuberculosis has comparable sensitivity to IS6110 RFLP. In July 2003, prospective MIRU-VNTR typing of all M. tuberculosis isolates received at Birmingham Regional Centre for Mycobacteriology was implemented to prospectively detect and confirm epidemiological links between patients with active TB disease.
Methods: DNA was extracted from positive M. tuberculosis MGIT cultures. Novel oligos were designed to amplify the 3 ETR and the 12 MIRU-VNTR loci. 5 L of each PCR reaction was loaded onto a WAVE® DNA Fragment Analysis System using the DNA Sizing programme. The gradient for separation was an 8.2-min gradient (20-900 bp) at a flow rate of 0.9 ml/min at 50°C. Using a Microsoft Excel spreadsheet the number of repeats at each locus was determined. IS6110 RFLP was performed on the largest MIRU-VNTR cluster using the standardised methodology.
Results: 1374 isolates have been typed (July 2003 to October 2004). 533 possess a unique MIRU-VNTR profile with 841 isolates belonging to 170 clusters containing >2 isolates (range 2–75 isolates, median 3), representing a clustering ratio of 61%. The median patient age was 36 years (range 0–98) in both clustered and unique isolates. The most prevalent MIRU-VNTR profiles were 32333-224325153314 (75 isolates, 5%), 42235-225425173533 (44 isolates, 3%), and 32433-223125153322 (19 isolates, 1%). Each of these strains exhibited distinct clusters of cases in three separate geographical locations. The most diverse VNTR clade was 22433 with a HGDI of 0.975. VNTR clade 32333 was most homogenous group with a HGDI of 0.816. The largest MIRU-VNTR cluster contained isolates obtained from 17 different laboratories. IS6110 RFLP has been performed on 50 isolates so far. 49 of 50 isolates possess an indistinguishable 7-band RFLP pattern. The other isolate has an extra band but can still be considered part of this cluster. 69 of 75 (92%) of these isolates are in the West Midlands with only 6 (8%) located in the East Midlands.
Conclusion: The high transmission rate and low median age in the Midlands, suggests newly acquired infection and not reactivation. Prospective MIRU-VNTR typing has detected a large previously unsuspected cluster and has allowed us to start to describe the epidemiology of TB in the Midlands.
O252: The identification of mycobacteria from solid media and directly from VersaTREK myco bottles using the MIDI HPLC system
V. LaBombardi, R. Katariwala, G. Pipia (New York, USA)
Objective: To minimize the time required to identify mycobacteria, the Sherlock MIDI HPLC system was used to identify mycobacterial isolates growing on solid media and directly from positive VersaTREK myco bottles.
Methods: The mycolic acids from mycobacterial isolates growing on 7H11 agar plates and from positive VersaTREK myco bottles were extracted, derivatized and subjected to analysis by HPLC. The resulting chromatograms were analyzed using the MIDI database library to obtain a species identification. The resulting identifications were compared to those obtained by using nucleic acid probes and conventional biochemicals. Many of the isolates used in the investigation were previously vetted as to species identification.
Results: Sixty-seven per cent of isolates tested from solid media were identified correctly to species. Twenty of 25 Mycobacterium avium complex isolates were identified correctly whereas none of the M. scrofulaceum isolates were identified to species owing to the absence of this organism from the database. Only 42.1% of the isolates obtained directly from positive VersaTREK myco bottles were identified correctly to species. A re-engineering of the database and a creation of a new library resulted in 90.1% of the isolates obtained from solid media and 82.9% of the isolates obtained from VersaTREK myco bottles being identified correctly. All 11 isolates of M. tuberculosis were identified correctly when tested directly from positive VersaTREK bottles using either library.
Conclusions: The use of the revised HPLC library with growth obtained directly from positive VersaTREK myco bottles allows for the identification of the majority of isolates within clinically relevant time frames.
O253: Mutator strains may contribute to the acquisition of drug resistance in Mycobacterium tuberculosis
R.M. Anthony, A.R.J. Schuitema, I.L. Bergval, L. Oskam, P.R. Klatser (Amsterdam, NL)
Spontaneous rifampicin resistant mutants of Mycobacterium tuberculosis (strain ATCC35801) were selected in vitro and the MIC of the resulting mutants measured for rifampicin and rifabutin. Of 105 colonies screened only a single mutant was isolated which was rifampicin resistant (MIC 32 μg/ml) but sensitive to rifabutin. The rpoB gene of this isolate was sequenced and found to contain a single C to T S522L mutation. This mutant was subjected to a second round of selection in parallel with the parent strain using rifabutin. The parent strain generated rifabutin resistant mutants with a frequency of 1.25 × 10−7 colonies per CFU plated and the R190 (S522L) mutant generated rifabutin resistant mutants with a frequency of 1.93 × 10−6 per CFU plated. Thus, spontaneous rifabutin mutants were generated by R190 with >15 times the frequency of the parent strain. DNA was extracted and the rpoB mutation hotspot region sequenced from twenty-six of these randomly selected rifabutin second round mutants. Additional mutations in the hot spot region of the rpoB gene were only detected in 12 of the 26 mutants studied; all isolates retained the original S522L mutation. Four strains had a mutation in codon 531, two in codon 526, four in codon 512 and two in codon 515. We did not detect any nucleotide changes in the mutT2, mutT4, or ogt gene regions previously suggested to be associated with a mutator phenotype. Selection of a mutator phenotype is recognised as a consequence of antibiotic challenge in many bacterial species, as the selection of strains with increased mutation frequencies will result in a greater chance of acquiring resistance to other drugs. The increased mutation frequency observed after selection with rifampicin suggests that mutator strains may also be relevant for the acquisition of drug resistance in Mycobacterium tuberculosis and may have serious implications for tuberculosis control.
O254: Epidemiology of Beijing strain family in Samara region, Russia
Y. Balabanova, V. Nikolayevskyy, M. Ruddy, S. Kuznetzov, S. Zakharova, A. Melentyev, I. Fedorin, F. Drobniewski (Samara, RUS; London, UK)
Background: Tuberculosis (TB) continues to increase globally and multidrug resistant TB (MDR TB) is a serious problem in Russia. Many TB cases originate among prisoners where the rates are the highest. Previous studies demonstrated the dominance of Beijing strains in some parts of Russia and other FSU countries and suggested its increased virulence and associations with resistance.
Objective: To address: (1) the extent of ‘Beijing strain’ transmission in the prison/civil sectors; (2) the association of drug resistance, clinical and social factors with the Beijing genotype.
Design: Prospective population-based molecular epidemiological study.
Setting: All civilian and penitentiary TB facilities in Samara Region, Russia
Patients: 880 consecutively recruited patients with tuberculosis.
Results: Beijing-family strains (comprised of two main MIRU types) were highly prevalent: 568/880 (66.6%, 95% CI 63.4–69.7%) with a significantly higher prevalence in the prison population (RR = 1.3 (95% CI 1.2–1.5) and those aged under 35 (RR = 1.2 (95% CI 1.0–1.3). It supports recent and active transmission particularly among prisoners who are younger than civil patients. Comparable proportions were coinfected with HIV (∼10%), hepatitis B/C (∼one-fifth), drank alcohol, smoked and had a similar sexual history. Univariate analysis demonstrated that male gender (OR 1.5, 95% CI 1.1–1.9), advanced pulmonary disease (OR 3.3, 95% CI 1.3–8.4), homelessness (OR 5.6, 95%CI 1.1–6.3) and previous imprisonment (OR 2.0, 95% CI 1.5–2.7) (but less association with night sweats (OR 0.7, 95% CI 0.5–0.9) were strongly associated with Beijing-strain family disease. Multivariate analysis supported previous imprisonment to be a risk factor (OR 2.0, 95% CI 1.4–3.3) (and night sweats to be less associated (OR 0.7, 95% CI 0.5–1.0) with Beijing disease. Multidrug resistance and resistance to isoniazid, rifampicin, streptomycin and ethambutol were twofold higher in prisoners than in civilians (RR = 2.4 (95% CI 1.9–3.0); RR = 1.9 (95% CI 1.6–2.3); RR = 2.2 (95% CI 1.7–2.7), RR = 1.9 (1.5–2.3), 2.2 (1.6–3.2) and respectively.
Conclusions: Drug resistance and previous imprisonment, but not HIV co-infection was significantly associated with Beijing-strain infection. There was limited evidence, that Beijing isolates caused radiologically more advanced disease. Larger clinical and immunopathological studies are needed to verify enhanced virulence of the Beijing family strain.
Diagnosis and management of sepsis in the critically-ill patient (symposium arranged with ISF)
S259: Association of statin therapy with 30- and 180-day mortality in patients with bacteraemia: population-based cohort study
R.W. Thomsen, H.H. Hundborg, S.P. Johnsen, H.T. Sørensen, H.C. Schønheyder, H.-H. Lervang (Aalborg, Aarhus, DK)
Objectives: Statins may decrease the risk of severe sepsis and death among patients hospitalized with bacterial infections, due to anti-inflammatory effects. We conducted this population-based cohort study to examine the effect of statin therapy on short- and long-term mortality in patients with bacteraemia.
Methods: We retrieved all patients hospitalized with bacteraemia in North Jutland County, Denmark, from January 1997 to December 2002 from the County Bacteremia Registry. Using civil registry numbers, patients treated with statins were identified by record-linkage with the County Prescription Database. Mortality within 180 days after the bacteraemia was determined through the Central Population Registry. Mortality rates were compared for patients with and without statin therapy, adjusted for gender, age, co-morbidity, use of antibiotic or immunosuppressive drugs, and focus of infection.
Results: Among 5353 patients older than 15 years hospitalized with bacteraemia, 176 received statin therapy before admission. The 30-day mortality in statin users vs. non-users was similar (20.0% vs. 21.6%, adjusted mortality rate ratio (MRR) 0.9, 95% CI 0.7–1.3). Among survivors 30 days after the bacteraemia, however, statin therapy was associated with a substantial decrease in mortality during the subsequent period up till 180 days after the infection (8.4% vs. 17.5%, adjusted MRR 0.4, 95% CI 0.2–0.8). The tendency towards similar short-term mortality and decreased long-term mortality rates in statin users was observed in both community-acquired and nosocomial bacteraemia episodes, and for various microbiologic agents and foci of infection. When analyses were restricted to patients with a prior medical indication for statin use (ischemic heart disease, stroke, peripheral atherosclerosis, or diabetes), the adjusted 30-day MRR among statin users was 1.1 (95% CI 0.8–1.6), and the adjusted MRR from 30 to 180 days was 0.5 (95% CI 0.3–1.0).
Conclusions: By contrast with previous smaller reports, in this population-based study statin use was not associated with a better prognosis within 30 days after an episode of bacteraemia, where most directly infection-related deaths may take place. Statins, however, seem to be associated with a substantially decreased long-term mortality after bacteraemia.
S263: Role of guidelines in the management of severe sepsis and septic shock
J.-L. Vincent (Brussels, B)
Septic shock is a common condition on our ICUs associated with considerable morbidity and high mortality. Until relatively recently, management of the patient with septic shock has relied on infection eradication with antimicrobial agents and surgery where needed, adequate fluid resuscitation, and organ support. However, research into therapeutic strategies is intense and advances in management are moving fast. Physicians are confronted with a wealth of study data that they are expected to apply to daily clinical practice. And in this age of evidence-based medicine and quality-assurance, each decision has to be backed by a sound rationale. Clinical Guidelines, defined as “systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances”,1 are designed to help clinicians achieve this goal, to assist in making appropriate decisions regarding management for individual patients. However, to be of any real value, guidelines need to be implemented and need to be flexible and adaptable. Medical research moves at a rapid pace and guidelines need to be continually updated as new discoveries are made and found, in high quality trials, to have an impact on outcomes. The Surviving Sepsis Campaign has recently published guidelines for the management of severe sepsis and septic shock,2 which include, among others, recommendations on appropriate antibiotic therapy, endpoints of fluid resuscitation, vasopressor preference, stress-dose steroid therapy for septic shock, use of recombinant activated protein C, and importance of blood glucose levels. Importantly, though, and unlike previous guidelines, the Surviving Sepsis Campaign has combined the development of the guidelines with a process to encourage their implementation and to assess the impact of the guidelines on mortality reduction. An annual update of the guidelines is also promised. Such evolving guidelines will help clinicians to apply results from the ever-increasing mass of literature and data to provide quality standard of care for their patients.
1. Field MJ, Lohr KN (editors). Institute of Medicine Committee to Advise the Public Health Service on Clinical Practice Guidelines. Clinical Practice Guidelines: Directions for a New Program. Washington DC: National Academy Press; 1990.
2. Dellinger RP, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004; 32: 858–873.
MRSA – new challenges in hospital and community settings
O264: National surveillance on methicillin resistant Staphylococcus aureus in Denmark, 1999–2003
R. Skov, A.R. Larsen, S. Böcher, M. Stegger, T. Klemmensen, D. Monnet (Copenhagen, DK)
Objectives: To present national surveillance data on methicillin resistant Staphylococcus aureus (MRSA) in Denmark from the 5-year period 1999–2003.
Methods: Since 1988 all methicillin resistant S. aureus (MRSA) isolates, both from infection and colonization cases, has been referred to and stored at the Staphylococcus Laboratory, Statens Serum Institut for national surveillance and since 1999 hospital discharge summaries or general practitioner records providing clinical and epidemiological data has retrospectively been obtained on all patients. Based on this information each case has been categorized as infection or colonisation as well as the probable source of acquisition giving the following catagories for infections: IMP: acquired outside Denmark; HA: Hospital acquired infection; CO: Community onset MRSA infection; CO-Health care associated (CO-HCA): patient has been hospitalized within the last 12 months; CO-community risk (CO-CR): close contact to another patient with a community acquired MRSA infection; CO-No Risk (CO-NR): No Risk factor has been identified. CA: Community acquired = CO-CR and CO-NR patients. All isolates has been subjected to PFGE - according to the harmony protocol, phagetyping and resistogram for 12 antibiotics. Presence of the mecA gene was confirmed with the EVIGENE kit.
Results: A total of 618 MRSA was found in the period. 131 were found by screening (will not be considered further) leaving 487 cases of infection. The number of infections increased from 54 in 1999 to 201 in 2003. In the same period the number of CO isolates increased from 26 to 113 (56%) of infections. In 2003, 17 patients had a community risk whereas 47 did not have any identified risk factors. Throughout the period ST80-IV accounted for 49% of CO-MRSA infections. Skin and soft tissue infections dominated CA-MRSA (82% vs 17% in HA infections).
Conclusions: The prevalence of MRSA has been very low in Denmark for more than 20 years. However, the number of cases is now increasing and the epidemiology of MRSA is changing towards primary acquisition within Denmark and community-onset infections, most of them without identifiable risk factors associated with previous health care. The ST80-IV clone has successfully established itself in the Danish community. However, the recent increase in MRSA infections is not due to the ST80-IV clone, which may indicate that new, well-adapted clones are now evolving in Denmark.
O265: Characterisation of ST125-MRSA-IV, a clone evolved in and spread from Norway?
A.E. Fossum, K. Alm-Kristiansen, G. Bukholm (Nordbyhagen, N)
Objectives: During the last few years several incidences of methicillin-resistant Staphylococcus aureus outbreaks have occurred in nursing homes in Norway. As residents in nursing homes often are transferred between different health care institutions, nursing homes can serve as a reservoir for MRSA strains resulting in outbreaks in other health care institutions. During the period 1999–2000 an outbreak was discovered in a nursing home (no. I) in the Southeastern part of Norway. The outbreak was discovered by amplified fragment length polymorphism (AFLP) typing, and thought to be cleared after infection control interventions in June 2000. In May 2003 another MRSA outbreak occurred at a second nursing home (no. II) situated in the same county as nursing home I. The two nursing homes have an exchange of residents and transfer residents to the same hospital. Reanalysis of all MRSA isolates from both outbreaks were done to investigate the possibility of an ongoing MRSA outbreak having lasted for 4 years.
Methods: The isolates were reanalyzed using multilocus sequencing analysis (MLST), staphylococcus cassette chromosome mec typing (SCCmec) and AFLP.
Results: All isolates were of the same sequence and SCCmec type, the novel ST125-IV. The AFLP analysis revealed a homology between the isolates of the first period (1999–2000) to be approximately 97%, and the homology between all isolates to approximately 89%.
Conclusion: The MRSA clones have survived in one or both of the nursing homes during a time period of 3–4 years, only having evolved slightly. ST125-IV has also been discovered in northern Norway and in a Spanish university hospital at Tenerife. In the Spanish hospital ST125-IV was first discovered in 2001, increasing rapidly and represented 22.8% of the clones in 2002. To our knowledge ST125-IV has not been discovered elsewhere. The ST125-IV clones are nearly related to ST5-IV, ‘pediatric clone’, differing with only one basepair in the yqiL allele. This might indicate that the strain has evolved from ST5-IV in Norway and spread to Tenerife e.g. by tourism. Another scenario is that the point mutation in the yqiL allele has occurred in several ST5 clones. The MRSA clones with sequence type 125-IV have shown the ability to establishment itself as an endemic strain in health institution environments, both in Norway and Spain.
O266: Genetic diversity among community isolates of methicillin-resistant Staphylococcus aureus in southern Stockholm
H. Fang, G. Hedin, A. Tammelin (Stockholm, S)
Objectives: Community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) strains are being isolated with increasing frequency around the world. The first CA-MRSA in the southern Stockholm area was documented year 2000. The present study is aimed at understanding the molecular epidemiology of CA-MRSA in the southern Stockholm area.
Methods: The CA-MRSA isolates detected during 2000 and 2003 were investigated. The strains were genotyped by pulsed-field gel electrophoresis (PFGE), multilocus sequence typing, and staphylococcal chromosomal cassette mec (SCCmec) analysis. The presence of the Panton-Valentine leukocidin (pvl) genes was detected by PCR. The antibiograms of the isolates were determined by disk diffusion method.
Results: 38 CA-MRSA isolates were detected during 2000 and 2003, which accounted for 21% of the 181 new MRSA cases under the period. These isolates presented 12 PFGE patterns and belonged to 10 MRSA clones. Among these clones, ST80-MRSA-IV was the only clone persistent through all the 4 years. Clone ST8-MRSA-IV emerged in 2001 and the frequency went down afterwards. ST150 was a new MLST type reported so far only from Sweden. In 2002, a cluster of five CA-MRSA isolates was found to be ST150, which could be further divided into two clones, ST150-MRSA-IIIC and ST150-MRSA-IIID. The year after, another two ST150-MRSA-IIIC isolates were detected in the same area. ST154-MRSA-IV was another new clone found in the study and so far only one strain belonged to this clone. Type IV was the most common SCCmec type in the study, which accounted for 63% of these strains and was present in diverse genetic backgrounds. Three new SCCmec types were observed in the study, i.e. SCCmec I variant, IIIC and IIID. Twenty-three of the 38 CA-MRSA isolates (61%) harboured the pvl genes, while no pvl genes were detected in hospital clones of MRSA under the period. However, the percentage of pvl-positive isolates among these community isolates of MRSA has declined by years, which was 91%, 57% and 36% in 2001, 2002 and 2003, respectively. In the present study, most CA-MRSA strains (95%) were non-multiresistant except clone ST59-MRSA-IIIC, which was co-resistant to erythromycin, clindamycin, chloramphenicol and tetracycline.
Conclusions: The present study reveals the genetic diversity of CA-MRSA strains in the southern Stockholm area and emphasizes the importance of typing in tracing the origin of isolates for controlling their spread in community.
O267: Polyclonal emergence of community-acquired methicillin-resistant Staphylococcus aureus strains harbouring PantonValentine leukocidin genes in Belgium
O. Denis, A. Deplano, H. De Beenhouwer, M. Hallin, G. Huysmans, M.G. Garrino, Y. Glupczynski, X. Malaviolle, A. Vergison, M.J. Struelens (Brussels, Aalst, Namur, Yvoir, B)
Background: Community-acquired (CA) methicillin-resistant S. aureus (MRSA) infections have been reported world-wide. Molecular studies suggest spread of a limited number of Panton–Valentine Leukocidin (PVL) producing MRSA clones that are genetically distinct from nosocomial strains. The objective of this study was to describe the molecular characteristics of the first PVL-positive MRSA strains isolated in Belgium.
Methods: Identification and oxacillin resistance were confirmed by triplex PCR for 16S rRNA, nuc and mecA genes. PVL genes (lukS-lukF) were tested by PCR. PVL-positive strains were genotyped by pulsed field gel electrophoresis (PFGE) after SmaI macrorestriction, staphylococcal cassette chromosome mec (SCCmec) typing, spa sequence typing and MLST. The accessory gene regulator (agr) polymorphism was determined by PCR. Susceptibility to 16 antimicrobials was determined by disk diffusion method.
Results: Among 65 putative CA-MRSA strains collected from 2002 to 2004, 15 isolates harboured lukS-lukF genes encoding the Panton–Valentine Leukocidin. By molecular typing, they belonged to PFGE type X1 ST80-SCCmec IV (n = 6), X2 ST80-SCCmec IV (n = 4), J4 ST30-SCCmecIV (n = 2), A23 ST8-SCCmec IV (n = 2) and Y1 new ST-SCCmec IV (n = 1). Strains had an agr type 3 (n = 13) or type 1 (n = 2) genotype. Strains were resistant to tetracycline (64%), fusidic acid (57%) and kanamycin (36%) and susceptible to other antimicrobial drugs including the quinolones. The mean age of patients with PVL-MRSA isolates was 26 years (range 1–70). All but one infections were community-acquired. including with skin or soft tissue infections (n = 13), bacteraemia (n = 1) and peritonitis (n = 1). One patient had skin colonisation. Five patients had previous beta-lactam therapy. Two cases were travel associated.
Conclusions: These results showed the emergence and importation in Belgium of PVL-positive CA-MRSA strains belonging to four MLST clones. CA-MRSA strains of genotype ST8-SCCmec IV and ST30-SCCmec IV were closely related with nosocomial PVL-negative strains. Strains were susceptible to most non beta-lactam antimicrobials except tetracycline, kanamycin and fusidic acid. PVL-positive strains caused skin or soft-tissue infections and rarely systemic infections. Surveillance should be intensified to monitor the incidence of MRSA and control its spread in the community.
O268: Panton–Valentine leukocidin positive methicillin-resistant Staphylococcus aureus in the Netherlands
X.W. Huijsdens, M.E.O.C. Heck, G.N. Pluister, E. Spalburg, M.G. van Santen, E. Tiemersma, H.A.J. de Neeling, W.J.B. Wannet (Bilthoven, NL)
Objectives: The world-wide emergence of hypervirulent methicillin-resistant Staphylococcus aureus (MRSA) strains carrying the loci for Panton–lentine leukocidin (PVL) is not limited to the community, but might also be emerging in the hospital environment. The National Institute of Public Health and the Environment (RIVM) serves as the national reference centre for the surveillance of MRSA in Dutch hospitals. Since the discovery of PVL positive MRSA strains in the Netherlands, all MRSA isolates of the national surveillance programme are routinely tested for the presence of the PVL loci. Because of the low (<1%) MRSA prevalence in the Netherlands, we are able to study virtually all hospital-acquired MRSA, which provides an accurate representation of the actual MRSA situation in our country. This report summarizes the results of PVL positive MRSA in the Netherlands in the period 2000 through 2003.
Methods: The PVL-MRSA isolates were obtained from clinics (40%), outpatient clinics (35%), and patients visiting general practitioners (25%). A multiplex PCR was used for the detection of PVL positive MRSA strains. The PCR detects not only the PVL loci, but also confirms the presence of the mecA gene and a S. aureus specific DNA fragment. Molecular typing also included pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST).
Results: In the period 2000 through 2003 approximately 10% of all Dutch hospital MRSA isolates carried the PVL loci, and molecular subtyping revealed two predominant PVL-MRSA genotypes: NL-28 (by PFGE) or sequence type (ST) 80 (by MLST) and NL-218 (PFGE type USA 300) or ST8. Molecular subtyping showed that most Dutch PVL-MRSA genotypes corresponded to well-documented global epidemic types. PVL-MRSA genotype ST80 is predominant in other European countries as well. Genotype ST8 has been found to be associated with outbreaks among jail inmates and gay men in the USA. Approximately 70% of the PVL-MRSA isolates were assigned staphylococcal cassette chromosome mec (SCCmec) type IV. Recent data have indicated the presence of SCCmec type IV in community-acquired MRSA.
Conclusion: Forty per cent of the Dutch isolates were obtained from clinics. The data presented here for PVL-MRSA isolates seem to confirm the hypothesis that PVL-MRSA might spread in the hospital environment and also might be (come) a hospital-associated public health threat.
O269: An MRSA strain associated with a community maternity hospital and carrying an exfoliative toxin gene
G.F.S. Edwards, I.M. Gould, D. Morrison, E.K. Girvan, B. Cosgrove, T.M.S. Reid, F.M. Mackenzie, L.A. McBeath, R.A. Browning, C.G. Gemmell (Glasgow, Aberdeen, UK)
Objectives: To follow-up the identification of MRSA isolates carrying the exfoliative toxin A (ETA) gene in patients associated with a community maternity hospital near Aberdeen.
Methods: We searched the SMRL database for isolates phenotypically and genotypically similar to those identified, characterised them further and looked at the clinical records of the patients.
Results: The index isolates were from skin infections in 1 adult and 7 babies. They had a characteristic PFGE pattern which resembled that of the US Paediatric Clone; this association was confirmed by MLST (ST5) and SCCmec (IV) typing. Toxin PCR showed that the isolates had the genes for ETA and enterotoxin D (SED) but not exfoliative toxin B (ETB) or Panton-Valentine leukocidin (PVL). Of the 55,000 isolates in the database, 110, nearly all referred from the Aberdeen Laboratory, resembled the index isolates. Of these, 60, mostly isolated in 2003 or 2004, were available for further testing. Nearly all these isolates were positive for the SED gene, about 60% were positive for the ETA gene and all were negative for the ETB and PVL genes. All the ETA positive isolates (and many of the SED positive, ETA negative ones) had closely related PFGE patterns but they were not all identical. The earliest isolate with the ETA toxin gene had been isolated from a wound swab taken in the community in 1998. The patients with the ETA positive isolates fell into three groups: (1) associated with the maternity hospital; (2) injecting drug users in the community; (3) hospital patients with clinical histories typical of those with hospital acquired strains.
Conclusions: We have shown that a phenotypically distinct group of ST5, SCCmec IV MRSA isolates carrying the ETA gene has been present in the Grampian region of Scotland for more than 5 years. Isolates have been present both in the community and in hospital patients; very similar isolates without the ETA gene have also been found. The ETA gene is usually carried on a plasmid and it is possible that the ‘outbreak strain’ has been generated on more than one occasion. As the strain is so widespread, attempts to contain it have been limited to the standard policy of decolonisation after treatment of any infection.
O270: Hospital transmission of a methicillin-resistant Staphylococcus aureus strain of increasing prevalence in the Scandinavian community
C. Ahrén, L. Larsson, C. Welinder-Olsson, B. Olsson-Liljequist, S. Haeggman, R. Skov (Göteborg, Stockholm, S; Copenhagen, DK)
Objectives: World-wide an increasing number patients with MRSA are found in the community. We report a smaller hospital outbreak caused by a strain of increasing prevalence in the community and most likely transmitted in the hospital by a healthy carrier.
Methods: The Infection Control unit at Sahlgrenska University hospital has been responsible for typing all MRSA strains isolated in the region as well as investigating epidemiological relationships of all possible outbreaks of MRSA since 1983. Strains are designated according to phenotypic characteristics, antibiograms and pulsed-field gel electrophoresis (PFGE)-patterns. To enable investigation of relationships between strains at the national level MRSA strains are further typed at SMI.
Results: Within a 2-month period in spring 2003 three women cared for in one of our maternity clinics were infected with the same MRSA strain, two developed febrile infection. Their newborns were later found to be throat carriers with this strain. No epidemiological relationship could be established between the mothers at that point. Co-patients and ∼90 employees were screened for carriage but none was found positive. A year later one additional mother developed mastitis with the same strain. Her baby was also found to be a throat carrier. Among co-patients and 200 personnel cultured, this time also including the staff at the neonatal unit, one doctor was found to be heavily colonised with the MRSA strain in question. The doctor was later found to have been involved in the care of all four neonates. The strain is sequence type (ST) 45, SCCmec IV, PVL-toxin negative MRSA strain with additional resistance only to tetracycline. It belongs to a clone with Berlin IV-like pattern on PFGE, widely spread both in Sweden and Denmark and presently increasing particularly in the community in Sweden.
Conclusion: It has not been possible to establish where and when the doctor was infected. Apart from being health personnel, no risk factors for MRSA carriage were encountered. Transmission most likely occured from healthy neonates to the breastfeeding mothers and not vice versa as initially believed. The extremely low prevalence of MRSA in Scandinavia, in Sweden <600 cases/year, makes it unlikely that the mothers, babies and the doctor have separate routes of transmission. The increase of MRSA in the community raises the questions of who and when to screen patients and employees to prevent spread of MRSA in hospitals.
O271: Comparison of genetic backgrounds of MRSA and MSSA isolated in Portuguese hospitals and in the community
M. Aires de Sousa, C. Simas, T. Conceição, H. de Lencastre (Oeiras, P)
Objectives: The nosocomial prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in Portugal was stable and estimated around 50% during the last decade. During this period there were successive waves of dominant MRSA clones in Portuguese hospitals, namely the Iberian (ST247-SCCmec IA), Brazilian (ST239-III) and EMRSA-15 (ST22-IV) clones. In order to understand the origins of these nosocomial major MRSA clones, we compared the genetic background of MRSA from three hospitals with methicillin-susceptible S. aureus (MSSA) isolates from those hospitals and from the community where they were located.
Methods: A total of 238 MSSA isolates, including 141 nosocomial and 97 community isolates, were characterized by pulsed-field gel electrophoresis (PFGE). Representatives of each PFGE pattern were studied by spa typing and multilocus sequence typing (MLST). Nosocomial isolates were recovered from three hospitals and the community isolates were recovered from healthy children attending day care centres and from draftees.
Results: The 238 MSSA isolates were grouped into 18 clones, of which 13 were present in both nosocomial and community settings. Half of the isolates belonged to three major clonal types: clone A (PFGE type A, spa type 33 or related, ST30), clone B (PFGE type B, spa type 295 or related, ST34) and clone C (PFGE type C, spa type 2 or related, ST5). Clone A, corresponds to a slight variation (MLST single locus variant) of the genetic background of the international MRSA clone EMRSA-16 (ST36-II) and clone C corresponds to the background of the New York/Japan (ST5-II) and Pediatric (ST5-IV) clones. To the best of our knowledge, the former two clones have never been detected in Portugal. However, the Pediatric clone was first described in a pediatric Portuguese hospital. Interestingly, the genetic backgrounds correspondent to the dominant MRSA clones in Portuguese hospitals (Iberian, Brazilian and EMRSA-15) were scarcely or not found among the present MSSA collection.
Conclusions: The Iberian, Brazilian and EMRSA-15 clones, which are the three major MRSA clones detected in Portuguese hospitals during the last decade, seem to have not originated from the introduction of SCCmec into dominant MSSA backgrounds present in the Portuguese nosocomial or community environment suggesting they were imported from abroad. In contrast, the MRSA Pediatric clone might have originated in our country by the acquisition of SCCmec type IV into MSSA clone C.
O272: Active MRSA surveillance decreases the incidence of MRSA bacteraemia
P. Shitrit, B. Gottesman, M. Katzir, A. Kilman, M. Chowers (Kfar Saba, IL)
Objectives: Methicillin-resistant Staphylococcus aureus (MRSA) colonization and infection in hospitals has increased during the last two decades world-wide. In May 2003 the society of hospital epidemiology of America presented new guidelines for prevention of nosocomial transmission of MRSA, stressing the need for increased surveillance. Therefore, the objectives of the current study were to evaluate the influence of active surveillance cultures for MRSA, on the incidence of nosocomial MRSA bacteraemia cases in our hospital.
Methods: In June 2003 new guidelines for MRSA active surveillance cultures were implemented in our hospital. Surveillance cultures were recommended for all high risk patients. Contact isolation was implemented for patients with positive cultures. The total number of surveillance cultures, the per cent of positive surveillance cultures and the number of MRSA bacteraemia cases before and after the intervention were compared (January 2002 to February 2003 – before intervention and July 2003 to October 2004 – after intervention).
Results: The number of surveillance cultures increased from a mean of 272 cultures per month before the intervention, to 836 cultures per month after the intervention. The per cent of positive surveillance cultures increased from 2.4% before, to 5.9% after the intervention. The number of positive MRSA bacteraemia cases per month decreased from a mean of 3.6 before the intervention to a mean of 1.9 cases after the intervention (p = 0.0003). Moreover, the trend line for new bacteremic patients changed from a slope indicating a constant increase (R2 = 0.2), to an almost flat trend line (R2 = 0.01) (Fig. 1).

Conclusions: Active surveillance cultures are important in order to identify the hidden reservoir of MRSA cases. Contact isolation can prevent new colonization and infection, thus resulting in significant reduction of morbidity and healthcare costs.
O273: Methicillin-resistant Staphylococcus aureus bacteraemia trends after control programme
A. Pan, G. Carnevale, P. Catenazzi, P. Mondello, L. Ferrari, B. Cadeo, S. Testa, L. Soavi, S. Lorenzotti, S. Magri, L. Signorini, G. Carosi (Brescia, Cremona, I)
Objectives: To evaluate trends in MRSA bacteraemia after the introduction of a nosocomial MRSA control system.
Methods: The study was of the before – after type. It was conducted at the hospital of Cremona – 850 bed community hospital – with intensive care unit (ICU), vascular surgery, neurosurgery, bone marrow transplant, and AIDS units. The study was performed in a hyperendemic setting, with a prevalence of methicillin resistance (MR) among nosocomial Staphylococcus aureus above 50%. Among all the hospitalized patients, MRSA bacteraemia was identified, origin of bacteraemia defined, and incidence rate calculated as per ward (ICU, surgical, or medical) and per origin (primary, central venous catheter – CVC – surgery, etc.). The MRSA control programme implemented, was based mainly on active identification of colonized patients through surveillance cultures, and isolation with contact precautions for all MRSA positive patients.
Results: From January 1,1996 through December 31, 2001, 69 MRSA bacteraemia were identified. When comparing the pre-intervention period, 1/1996 – 6/1997, with 1/2000 – 12/2001, the incidence rate of MRSA bacteraemia was reduced from 0.62 to 0.32 per 1000 admissions (relative risk (RR) = 0.51; 95% confidence interval (CI) = 0.28–0.96; p = 0.03). The effects were most striking in ICU, with an 89% reduction (RR = 0.11; 95% CI = 0.01–0.98; p = 0.03) and in CVC-related bacteraemia with an 82% decrease (RR = 0.17; 95% CI = 0.05–0.55; p = 0.002). Methicillin resistance among blood isolates decreased from 46% to 17% (RR = 0.37; 95% CI = 0.22–0.62; p = 0.0005).
Conclusions: A reduction in MRSA bacteraemia may be achieved through control of MRSA transmission in hospitals with very high MR prevalence. Patients in ICU and with a CVC may benefit the most from ‘search and isolates’ control interventions.
Focus on extraction and amplification controls in molecular diagnostics
O275: Automated nucleic acid extraction using the NucliSens easyMAG system for the recovery of DNA from various clinical specimen types
A. van den Brule, V. van Melick, P. van Deursen, J. Mollink, M. Jacobs, E. Boel, G. Onland (Veldhoven, Boxtel, NL)
Objective: Measure the efficiency of a new automated nucleic acid extraction system (NucliSens easyMAG, bioMérieux) for various clinical samples as compared to a reference extraction system.
Methods: 140 individual clinical samples (including plasma, serum, CSF, blood, stool, and sputum samples) were spiked with Phocine herpesvirus-1 (PhHV). Extracted samples were subjected to real time PCR to determine the extraction efficiency of the NucliSens easyMAG and compare it to a manual magnetic silica method (NucliSens miniMAG, bioMérieux). Next, serial dilutions of M. bovis were prepared in sputum to compare the extraction efficiency of both systems with a second model system. Run controls were included to measure the reproducibility. Carry over was addressed by processing highly positive samples in between negative samples. For the easyMAG method two different workflows were tested, lysis on board and lysis off board.
Results: PhHV DNA was detected in 96% (easyMAG) and 97% (miniMAG) of the samples when tested undiluted and was detected in all samples when tested 5-fold diluted. In total 6/20 (easyMAG) and 4/20 (miniMAG) stool samples were not detected when tested undiluted, for all other sample types 100% detection was measured. Mean Ct values were 27.7 ± 2.5 (easyMAG) and 27.6 ± 2.3 (miniMAG) for undiluted samples and 29.4 ± 1.8 (easyMAG) and 29.5 ± 2.0 (miniMAG) for 5-fold diluted samples. The calculated 50% hit rate obtained with M. bovis PCR was found at dilution 1:14,000 (easyMAG) and 1:17,000 (miniMAG). Both systems showed good reproducibility on the run controls, and no carry over was detected. Ct values of extracted control samples (easyMAG 25.6 ± 0.4, miniMAG 26.0 ± 0.6) were comparable to values obtained with PCR controls not subjected to extraction (PCR 25.8 ± 0.3). Regarding the two different workflows, Ct values measured were comparable for, respectively, the off board and on board lysis; undiluted 26.7 ± 1.6 and 26.9 ± 1.4, diluted 29.0 ± 1.4 and 29.3 ± 1.5.
Conclusions: In this study, for all samples tested, the new extraction system NucliSens easyMAG performs equal as compared to manual magnetic silica extraction (NucliSens miniMAG) that was used as reference. This means that both platforms are interchangeable. For both systems inhibition was observed in some of the stool samples when tested undiluted, but PhHV DNA was well detected when these samples were tested diluted. No inhibition was observed in any of the other sample types included in this study.
O276: Specific enrichment of prokaryotic DNA from human samples
S. Sachse, K.-H. Schmidt, M. Lehmann, S. Russwurm, E. Straube (Jena, D)
Objectives: Rapid identification of bacterial pathogens is crucial to manage efficient pathogen-adapted antimicrobial therapy. Current problems for pathogen detection in human samples with low bacterial load are patients under antibiotic pretreatment, non-cultivable microorganisms and a time-to-result delay of more than 4 days. Previous studies with patients of intensive care units showed that 80–90% of blood cultures fail to detect the triggering pathogen. Therefore, culture independent detection methods take a centre stage in scientific interest. However, compared to bacterial culture techniques, the sensitivity of molecular biological methods like PCR is inadequate. Here, we developed a method for the specific separation and concentration of prokaryotic DNA from eukaryotic environment, to enable culture independent molecular biological methods with significant increased sensitivity.
Methods: A protein (P-181) was identified that has a specific binding affinity for pro-karyotic DNA. P-181 was expressed in Escherichia coli. Validating the properties of P-181, we used spiked blood samples. Total DNA, isolated by means of phenol/chloroform extraction, was given to a column packed with P-181 immobilized to a special matrix. The separation of prokaryotic DNA was monitored by measurement of optical density and special PCR-techniques. After the enrichment of prokaryotic DNA, a PCR was performed to detect bacterial DNA. The amplicons were sequenced for identification of the pathogen.
Results: We showed that prokaryotic DNA is specifically retained by immobilised P-181. We successfully separated the DNA of Streptococcus pyogenes, Staphylococcus aureus and Escherichia coli in spiked blood samples. In a current clinical pilot study, we were able to detect bacterial DNA with different sequences in the 16SrRNA-gene in some whole blood samples from septic patients despite the corresponding blood cultures showed negative results.
Conclusion: The developed method offers a unique opportunity for concentration of prokaryotic DNA from human samples with low bacterial load, tissue or other clinical samples. This preanalytic procedure leads to an increased sensitivity of culture independent methods of bacteria detection in usually sterile clinical samples by means of common PCR protocols.
O277: Real-time PCR with an internal control detecting all 51 known adenovirus serotypes
M. Damen, P. Glasius, R. Mang, R. Minnaar, P. Wertheim, M. Beld (Amsterdam, NL)
Objectives: The gold standard for the diagnosis of adenovirus (AV) infection is culture. However, results are available after days to weeks and not all AV types grow in culture. Especially in immune compromised patients severe infections with AV are described and a rapid diagnosis would be important. Therefore, an AV real-time PCR was developed, detecting all 51 known AV serotypes.
Methods: Primers were chosen in the hexon region. In order to cover all 51 serotypes the forward primer is degenerated at three positions and the reverse primer at two positions. The internal control (IC) DNA contains the same primer binding sites, but has a shuffled probe region compared to WT virus. The IC DNA was added to the clinical sample in order to monitor extraction and PCR efficiency. Twelve (2-fold) serial dilutions were made from AV DNA and IC DNA in a background of AV negative throat fluid in order to assess the detection limit of the AV PCR. To investigate the linearity, 8 (ten-fold) serial dilutions from AV DNA (with 1000 copies IC DNA in every dilution) in a background of AV negative sputum were tested. A panel of AV prototype strains of all 51 AV serotypes, kindly provided by Dr J. de Jong, Erasmus University, Rotterdam, the Netherlands, was tested. To establish the clinical utility of the assay, a comparison of AV PCR and culture was performed in a panel of 157 clinical samples (90 faeces samples, 56 respiratory materials, 8 serum/plasma samples, three other materials).
Results: In the serial dilutions in throat fluid the 50% detection limit of AV DNA was 8 copies per PCR assay (400 copies/ml) and of IC DNA 16 copies per PCR assay (800 copies/ml). The real-time AV PCR was linear from 125 copies per PCR assay (6250 copies/ml) until 1.25 E8 copies per PCR assay (6.25 E9 copies/ml). All 51 AV serotypes were detected in the panel of AV prototype strains. Concordant results between culture or Ag detection and PCR were found in 138/157 (87.9%). In 10 cases, PCR was positive while culture or Ag was negative (6.4%). In one case, PCR was negative while culture was positive (0.6%) and in 8 cases PCR was negative without culture or Ag data
Conclusion: A sensitive AV real-time PCR assay was developed, detecting all 51 AV serotypes. The assay can be applied on different body fluids, among which faeces and respiratory materials. The assay has proven to be more rapid and more sensitive than AV culture.
O278: Rapid detection of Salmonella and Campylobacter jejuni DNA in faeces by real-time PCR without prior culture enrichment
T. Schuurman, R.N. Patty, A.M.D. Kooistra-Smid, A.A. van Zwet (Groningen, NL)
Objectives: Salmonella spp. and Campylobacter jejuni are the major causes of bacterial gastro-enteritis in The Netherlands. Conventional diagnosis is based on detection of both species in feces and consists of enrichment, selective culture and identification, which can take several days. Introduction of a PCR based screening of feces is cost-effective (ICAAC 2004 poster O-1626) and will decrease the turn around time significantly. However in this approach a sensitive PCR method is mandatory. This study describes the development of real-time PCR based methods for the direct detection of Salmonella spp. and C. jejuni in feces.
Methods: Real-time PCR assays for Salmonella spp. and C. jejuni were developed, based on the invA and mapA genes respectively, and combined with a very efficient ‘in-house’ DNA extraction from feces. The DNA extraction was validated in recovery experiments and the PCR assays were validated with culture positive [n = 229 (Salmonella spp.), n = 172 (C. jejuni)] and culture negative [n = 191 (Salmonella spp.), n = 224 (C. jejuni)] fecal specimens.
Results: In a panel of 136 fecal samples, the ‘in-house’ fecal DNA extraction performed with a high average recovery (97%) compared to miniMAG (70%) and MagNA Pure DNA III (64%). No samples proved troublesome (i.e. recovery <50%), whereas 16% and 27% scored lower recoveries (0–38%) with the commercial kits. However, final PCR results were only slightly influenced by low recoveries. Analytical sensitivities were determined at 500 CFU and 100 CFU/g feces for Salmonella spp. and C. jejuni respectively. In clinical fecal specimens sensitivity and specificity were 92%, 99% for Salmonella spp., and 96%, 96% for C. jejuni respectively. PCR inhibition was only observed in 0.15% of the samples.
Conclusion: Sensitive and cost effective molecular screening of fecal specimens for Salmonella spp. and C. jejuni is feasible and has great potential as a means of rapid detection of bacterial gastro-enteritis.
O279: Rapid detection of Clostridium difficile-associated diarrhoea in a prospective multicentre study, using a new immunoassay and real-time PCR
R.J. van den Berg, E.S. Bruijnesteijn, H.J. Gerritsen, H.P. Endtz, E.R. van der Vorm, E.J. Kuijper (Leiden, Rotterdam, Amsterdam, NL)
Objectives: Clostridium difficile-associated diarrhoea (CDAD) is usually diagnosed by the detection of enterotoxin A (TcdA) and/or cytotoxin B (TcdB) in faecal samples, or by culture of a toxinogenic strain. A recently introduced new rapid immunoassay (immunocard toxins A and B, Meridian) and an in-house developed real-time PCR were compared in a prospective multicentre study with conventional diagnostics.
Methods: In a prospective study of 4 months, 3 university hospitals participated and tested all faecal samples from patients with diarrhoea admitted to the hospital for 3 days or longer for CDAD, irrespective of the physicians request. A conventional enzyme-linked fluorescent assay (ELFA, Vidas CDA2) was used for detection of TcdA and the cytotoxicity assay on Vero-cells was applied as the gold standard. Additionally, the immunocard toxins A and B (ICTAB) and a real-time PCR for the detection of tcdB were included in the study (FICDS, abstr. p. 22, 2004). The sensitivity of the real-time PCR was 1 colony forming unit (CFU) in 0.9% saline and 2800 CFU/g faeces.
Results: Of 471 faecal samples from patients with diarrhoea, 102 (21.7%) were excluded due to a lack of sufficient material for all assays. Of 369 samples included, 75 (20.3%) showed a positive test result in one or more assays. The cytotoxicity test was positive for CDAD in 23 (6.2%) of 369 patients. Of 23 patients with a positive cytoxicity assay, the diagnosis CDAD was not considered in 10 (43%) by the physician. Using the cytotoxicity assay as the gold standard, sensitivity of ELFA, ICTAB and real-time PCR were 69.6%, 91.3% and 87.0%, respectively. The specificity of ELFA, ICTAB and real-time PCR were 95.4%, 96.2% and 95.4%, respectively. The positive predictive value and negative predictive value for ELFA, ICTAB, real-time PCR were 50% and 97.9%, 61.8% and 99.4%, and 55.6% and 99.1%, respectively. Culture of two discordant samples only positive by real-time PCR showed the presence of toxinogenic CD in both samples. Culture of five samples only positive in ICTAB revealed no toxinogenic CD.
Conclusions: The newly introduced rapid immunoassay is a very rapid and easy-to-perform test for the diagnosis of CDAD. It may be useful for guiding appropriate treatment. The real-time PCR is an excellent instrument to control nosocomial spread of toxinogenic C. difficile.
O280: Detection of norovirus in an outbreak of acute gastroenteritis at a nursing home in south-east Austria
I. Lederer, E. Schreier, A. Gränz, S. Richter, C. Berghold, F. Allerberger (Graz, A; Berlin, D; Vienna, A)
Objectives: In April 2004, residents and staff in a nursing home in south-east Austria fell ill with vomiting and diarrhoea: The index case was an 85-year-old man with clinical onset on April 27th. During the following days an increased number of cases with diarrhoea and vomiting among residents and stuff was observed. The outbreak peaked on May 7th. We describe the outbreak and its epidemiological investigation.
Methods and Results: At the time of the outbreak 77 persons aged 62-96 years lived in the nursing home and up to 44 staff members worked there. To stop the spread of the disease, all residents were invited taking their meals in their rooms instead of in the common dining room. Common social activities were restrained. Since all meals were prepared in the residential kitchen, water and food were sampled for routine testing of infectious agents (not including norovirus); all results were negative. Testing of stool samples for salmonella, shigella, campylobacter, enterohaemorrhagic Escherichia coli, rotavirus, adenovirus and cryptosporidia was also negative. These results raised the suspicion that norovirus was the causative organism in this outbreak. No indication of norovirus as causative agent could be found in the stool samples either by electron microscopy, or with routine RT-PCR in the polymerase gene of norovirus (ORF1). Finally, analysis with real time RT-PCR in the capsid region (ORF2) of the virus genome could identify norovirus of the genogroup II (GG II) as causative agent; detection was possible using a TaqMan probe. Nursing administration provided lists of residents and staff with corresponding symptoms and days of sickness for epidemiological evaluation; the attack rate (AR) was 52% for the residents. Five of the 40 residents affected had 2 episodes of illness and 2 residents had 3 episodes; the AR of personnel was 27.3% without any relapses. None of the kitchen staff became ill.
Conclusion: This outbreak demonstrates that in order to evaluate an outbreak with suspected norovirus involvement, molecular virus identification of 2 different genomic regions may occasionally be useful, especially when clinical symptoms and epidemiological features of the disease indicate norovirus infection as its cause.
O281: Detection of human metapneumovirus in nasopharyngeal aspirates from young children by real-time RT-PCR
W.A. Verstrepen, P. Bruynseels, A. Mertens (Antwerp, B)
Objectives: Human metapneumovirus (HMPV) was recently discovered as a new paramyxovirus responsible for a substantial proportion of acute respiratory tract infections. Our aim was to retrospectively determine the prevalence of HMPV infections in young children admitted to our hospital from December 2002 until April 2003.
Methods: Nasopharyngeal aspirates (NPA) from children with symptomatic respiratory tract infections but negative for common viral respiratory pathogens were stored at −80°C until analysis. Patient age ranged from 10 days to 12 years. NPA were defrosted, washed and spiked with an exogenous RNA transcript prior to RNA extraction. All extracts were tested in duplicate, both by an in-house developed real-time RT-PCR assay and by another recently described real-time RT-PCR assay. The in-house assay is based on TaqMan MGB probes directed to conserved sequences located in the nucleoprotein gene.
Results: All specimens tested were adequate as monitored by detection of the spiked RNA transcript. HMPV RNA was detected in 13 of 93 specimens (14%) by both real-time RT-PCR assays. Eleven of these children were admitted with a variety of respiratory symptoms ranging from cough to pneumonia. One child presented with fever, the other one was diagnosed with rachitis. The majority of children with a positive HMPV assay (10/13) was less than 2 years old, the oldest child with a positive HMPV assay was twelve. Remarkably, 10 of these 13 HMPV-positive specimens were clustered in a 2 weeks time period, strongly suggesting the occurrence of an epidemic outbreak. Whereas Ct values varied from less than 20 up to almost 40, differences in Ct values between both assays were not significant. Two other specimens from children admitted with symptoms of gastroenteritis were weakly positive with the previously described assay alone, albeit in just one of the duplicate reactions.
Conclusions: Real-time RT-PCR may prove to be a rapid, convenient and reliable method to detect the presence of HMPV RNA in NPA from children with acute respiratory infections. Further clinical validation in a prospective study is in progress.
O282: Parallel real-time PCR quantification of six human herpes viruses in patients with acute neurological infections
O.E. Varnier, J.L. McDermott, I. Martini, F. Bertolotti, D. Ferrari, C. Giacomazzi, L. Tagliaferro, E. Capello, G. Mancardi (Genoa, I)
Introduction: The onset of symptoms and clinical manifestations of the central nervous system (CNS) infectious diseases often makes a specific diagnosis difficult. The etiological agent and type of infection can determine potential prognoses as well as optimal treatment for the patient. Unfortunately, laboratory tests used for the diagnosis of CNS infections have the disadvantage of being either nonsensitive or nonspecific or giving results difficult to distinguish from the norm. With the advent of molecular diagnostic protocols, it is now possible to diagnose viral pathogens specifically and with high sensitivity and accuracy.
Materials and Methods: The LightCycler Real-time PCR technology was used to analyse 70 cerebrospinal fluid (CSF) specimens collected from 61 patients with encephalitis and/or meningitis and 9 patients with acute neurological symptoms. DNA was extracted from the CSF samples (1000 μl) using the MagNa Pure robot and eluted in a final volume of 100 μl, therefore achieving 10-fold DNA concentration. The DNA samples were analysed using 5 Real-time PCR protocols in a single LightCycler run (30 min) for the parallel detection of 6 herpes viruses (HSV-1, HSV-2, VZV, CMV, EBV and HHV-6).
Results: Herpes-type specific plasmid dilutions were amplified to produce external standard curves for accurate PCR product quantification. Following HSV amplification, HSV-1 and HSV-2 differentiation was performed by LightCycler melting curve analysis, which detects sequence differences between the PCR product and hybridisation probe: this results in a shift in the probe melting temperature (57°C for HSV-1 and 67°C for HSV-2). Viral DNA was detected in 13 of the 70 CSF samples: 4 were positive for HSV-1, 1 for HSV-2, 5 for VZV and 3 for HHV-6. The levels of quantified DNA varied from 100 to 22,630 copies/ml. In one case, 4800 VZV DNA copies per ml were detected in the CSF of a young woman (18 years) suffering from Runsay-Hunt syndrome: the patient was successfully treated with acyclovir. The combined use of an automated extraction procedure and rapid LightCycler PCR allowed a turn-around-time (TAT) of 90–120 min to be achieved.
Conclusion: These results suggest that the LightCycler Real-time PCR platform offers a fast, highly automated, sensitive and reproducible tool for the accurate quantitation of six herpes virus DNAs in CSF samples with a TAT of less than 2 h.
New developments in epidemiology of antibiotic resistance
O283: Rapid increase in development of multidrug resistance among Klebsiella pneumoniae during hospitalisation: surveillance of first isolates underestimates the resistance problem
M.A. Leverstein-van Hall, H.A.J. de Neeling (Utrecht, Bilthoven, NL)
Objectives: The Dutch national surveillance on the prevalence of resistance is based on first isolates per patient and therefore unable to detect resistance development during hospitalisation. Our aim was to design an analysis of surveillance data that reveals to what extent hospital stay contributes to the development of resistance to single as well multiple antimicrobial classes (AC) in pathogens isolated from patients during hospitalisation.
Methods: Klebsiella pneumoniae (KP) isolates (blood, respiratory tract, wound or pus) cultured from hospitalized patients and processed in one of 8 regional laboratories covering 27% of the Dutch population in the years 1996/1997 and 2001/2002 were studied. The percentage of patients who had acquired an (intermediate) resistant isolate was determined up to15 days, starting the first day (day 0) when a KP was isolated from a patient. This percentage was calculated for day 0 and for each subsequent 3-days interval. Per interval only 1 random isolate per patient was included if available.
Results: In 1996/1997, resistance percentages during hospitalization to amoxi-clav, third gen. cephalosporins and gentamicin remained stable while non-susceptibility to cotrimoxazole and ciprofloxacin rose 2.5-fold and 4-fold respectively (Table). Multidrug resistance (MDR; I/R to at least 2 AC) reached a maximum of 11% of isolates tested 4–6 days after the day 0 (Fig.). In 2001/2002, however, resistance to any single AC increased 3- to 5-fold during hospitalization and after one week 50% of isolates were resistant to two or more AC, of which half were resistant to all 5 AC tested.
| No. of days after first day of isolation |
|||||||
|---|---|---|---|---|---|---|---|
| Antimicrobial agent | Years | 0 | 1–3 | 4–6 | 7–9 | 10–12 | 13–15 |
| Co-amoxiclav | 1996–1997 | 5% | 7% | 7% | 8% | 6% | 6% |
| 2001–2002 | 9% | 15% | 24% | 32% | 35% | 35% | |
| Ceflazidime/Cefotaxime | 1996–1997 | 3% | 3% | 2% | 1% | 5% | 2% |
| 2001–2002 | 7% | 15% | 20% | 33% | 36% | 40% | |
| Gentamicin | 1996–1997 | 5% | 6% | 7% | 8% | 7% | 3% |
| 2001–2002 | 9% | 21% | 28% | 37% | 43% | 41% | |
| Cotrimoxazole | 1996–1997 | 8% | 12% | 19% | 14% | 19% | 21% |
| 2001–2002 | 13% | 22% | 32% | 45% | 41% | 48% | |
| Ciprofloxacin | 1996–1997 | 2% | 3% | 4% | 1% | 6% | 8% |
| 2001–2002 | 7% | 14% | 19% | 31% | 35% | 35% | |
| No of isolates (min–max) | 1996–1997 | 1111–1535 | 140–196 | 94–134 | 66–111 | 46–63 | 35–58 |
| 2001–2002 | 1416–1567 | 212–252 | 133–161 | 99–128 | 80–101 | 67–82 | |

Conclusions: Development of MDR among Klebsiella pneumoniae isolates during hospitalization in 8 Dutch regional hospitals has increased substantially in recent years. The analysis used in this study provides better insight in the resistance prevalence inside hospitals than an analysis based solely on first isolates and is a useful tool to monitor resistance development during hospitalization.
O284: Multidrug resistance among Streptococcus pneumoniae from Europe, Asia and South America: current data from the GLOBAL Surveillance initiative 1999–2004
M. Jones, R. Blosser, D.F. Sahm (Hilversum, NL; Herndon, USA)
Objectives: World-wide increases in the prevalence of multidrug-resistant (MDR)-SP demonstrate the importance of surveillance initiatives such as the GLOBAL Surveillance to monitor changes in the in vitro activity of important antimicrobial agents. The USFDA has recognized the importance of MDR among S. pneumoniae (SP) and approved an MDR-SP indication for levofloxacin and more recently, gemifloxacin.
Methods: The GLOBAL Surveillance initiative includes 15,878 non-repeat SP strains collected from patients in fourteen countries world-wide from 1999 through 2004. All isolated were susceptibility tested in a central laboratory using NCCLS standards. Data were used to investigate MDR [resistance (R) to ≥3 among penicillin (PEN), ceftriaxone (CTX), azithromycin (AZI), trimethoprim-sulfamethoxazole (SXT), and levofloxacin (LFX)] trends and phenotypes
Results: From 1999 to 2004, the prevalence of MDR strains ranged between 11.4% and 12.5%. Regardless of year or country, the most prevalent MDR phenotype was R to PEN, AZI, and SXT. Globally, LFX R was rarely associated with MDR with over 96% of MDR strains remaining susceptible. On a country basis for 2003–2004, the highest MDR rates were observed in Thailand (23.1%), South Korea (47.8%), and Hong Kong (44.0%); LFX R as part of the MDR phenotype remained low in these countries (1.6%, 1.0%, and 5.3%, respectively). The lowest MDR rates were observed in Germany (0.9%), United Kingdom (1.2%), and Belgium (1.6%). Overall among the MDR isolates collected, 92.6% were R to 3 agents, and 7.4% were R to 4 agents. No 5 drug-resistant MDR SP were encountered.
Conclusions: The MDR phenotype among SP is prevalent world-wide and most frequently involves resistance to beta-lactams, macrolides and SXT. Currently, and especially in EU countries, fluoroquinolone R is rarely associated with the MDR phenotype. However, the potential for this to emerge underscores the need for continued surveillance and new agent development.
O285: Spatial analysis applied to bacterial diseases and resistance transmission: early report from the EUREQA Project – Brazil 2004
C.R. Kiffer, A.M. Monteiro, P.C. Koga, C. Oplustil, J.L. Sampaio, G. Camara, C.M. Mendes on behalf of the EUREQA Project Team (São Paulo, BR)
Objectives: Understand the spatial dynamics of upper respiratory tract bacterial infections or colonizations and their resistance patterns within the city of São Paulo, Brazil, as part of the EUREQA Project.
Methods: Project EUREQA is a multi-phase study to interpret bacterial disease dynamics and distributions and its correlations with risk factors within the city of São Paulo. The city is located in southeastern Brazil and has around 10,000,000 inhabitants. Routine outpatient culture results for bacterial pathogens isolated from respiratory tract between 2002 and 2004 were entered in the database and geocoded in a digital map containing different information categories (layers). Spatial analysis technique used was Kernel function method (TerraView 3.01, INPE, Brazil) to analyse total sample and cases distribution. Comparisons between both patterns were done to explore possible cluster formations.
Results: Five thousand and fourteen (5014) respiratory tract cultures (one patient per day) were performed during the period, which yielded 725 isolates of H. influenzae and 295 of S. pneumoniae. So far 1795 occurrences were geocoded, with 243 (13.5%) H. influenzae and 111 (6.2%) S. pneumoniae. Of those, 11 H. influenzae isolates were beta-lactamase producers and 7 S. pneumoniae were intermediate or resistant to penicillin. A non-random pattern of total sample, H. influenzae, and S. pneumoniae distributions was observed, probably meaning higher population density. Early evidence of independent clusters was detected.
Conclusions: Kernel function is an easy-to-use and initial exploratory technique for interpolating and smoothing point events and it identifies possible clusters. However, it only considers the sampled population (biased samples influence result). Independent clusters of H. influenzae and S. pneumoniae is possible but needs further investigations. Geographical information systems and spatial methods can be applied to better understand epidemiological patterns and to discriminate target areas for public health interventions.
O286: Antimicrobial use and Streptococcus pneumoniae penicillin resistance: temporal relationship at the population level
R. Mera, L. Miller (New Orleans, Upper Providence, USA)
Objectives: To investigate the nature of the temporal relationship between antimicrobial consumption and Streptococcus pneumoniae penicillin resistance using population level data across time.
Methods: National outpatient antibiotic prescription data for 1998–2003 from France, Spain, Italy, Germany, the UK and the US was obtained from published reports, provided by IMS Health Global Services. Aggregate data for total use and several antibiotic classes was used to express outpatient consumption in defined daily doses per 1000 inhabitants per day. Surveillance data consists of S. pneumoniae isolates obtained from the TSN surveillance database (Focus Technologies) in the same geographic regions from 1996 to 2001. Additional data for 2002 and 2003 was obtained from published studies. A linear mixed model for repeated measures was used in modelling the association between resistance and several antibiotic classes through time.
Results: A multivariate random effects model shows that there is a strong linear relationship between overall levels of antimicrobial consumption and penicillin resistance, that the association of exposure and resistance is unique for every country and that there is no direct relationship between the year-to-year change in consumption and penicillin resistance. Changes in penicillin resistance through time in any country are better explained by the cumulative total antimicrobial consumption with a 2-year lag. A hypothetical 10% consumption reduction in all antibiotic classes would decrease by 2.6% the peak penicillin resistance rate in 2-years. A 15% reduction in macrolide consumption and broad to narrow spectrum penicillin ratio would independently decrease by 5.4% and 1.6% the peak penicillin resistance rate respectively. An increase of medium-narrow penicillins to mid-90s levels would diminish by 1.8% the peak penicillin resistance rate.
Conclusions: Large reductions in consumption at the population level are needed to affect resistance. There is a peak level of penicillin resistance associated with cumulative exposure to a combination of antibiotic classes. It may be possible for countries with low levels of penicillin resistance under a specific steady-state situation to retain that condition for a long period of time. For other countries reduction of consumption alone may not result in reversal of resistance and so they would need to rely on the use of new agents active against multiresistant clones.
O287: Comparative impact of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant Streptococci among healthy volunteers: a double-blind, placebo-controlled, longitudinal study
S. Malhotra-Kumar, C. Lammens, C. Mallentjer, J. Piessens, K. Van Herck, H. Goossens (Antwerp, B)
Objectives: The abilities of azithromycin and clarithromycin to promote carriage of macrolide resistant oral streptococci and the temporal persistence of the selected resistant commensals in healthy volunteers was investigated.
Methods: Volunteers (n = 204) included were adult with no sign of respiratory tract infection and had not been administered any antibiotic in the past 3 months. Throat samples were taken before antibiotic administration (d1) and the volunteers randomly allocated into four groups to receive azithromycin or placebo once daily for 3 days, or clarithromycin or placebo twice daily for seven days. Further samplings were done on the 8th day after commencing the antibiotic/placebo course (d2), on the 14th day (w1), 28th day (w3), 49th day (w6), and finally in the 6th month (m6). Quantitation of the aerobic streptococcal flora was done on streptococcal agar with and without erythromycin (2 μg/ml) using a spiral plater (Eddy Jet, The Netherlands), and the percentage of macrolide-resistant streptococci determined by colony counting. Mean resistance proportions were compared between both macrolides and their respective placebo groups as well as between the two macrolide groups. For this, Student's t-test and an analysis of variance with Bonferroni's post-hoc test were used.
Results: Comparative impact of the two macrolide regimens on the prevalence of macrolide resistant streptococci over a period of 6 months is presented in the graph. The mean resistance proportions at each time point following azithromycin or clarithromycin use when compared to their respective placebos, showed a significant increase (p ≤ 0.01 overall) in macrolide-resistant streptococci that persisted for >6 months. Comparing the two macrolides, differences in mean macrolide resistance were not significant immediately following azithromycin and clarithromycin use (p = 0.8), decreased significantly faster in the clarithromycin group than the azithromycin group in w1 and w3 (p ≤ 0.001), and became non-significant in w6 and m6 (p = 0.07 and 0.6, respectively).

Conclusions: This is the first study analyzing the temporal evolution of the oral streptococcal flora over a prolonged period following macrolide use. Both azithromycin and clarithromycin have a marked effect on macrolide resistance in oral streptococci and these effects persist for >6 months post-therapy.
O288: Colonisation and resistance dynamics of enterococci during and after hospitalisation
P.M.G. Filius, I.C. Gyssens, A. Ott, A.G. Vulto, H.A. Verbrugh, H.P. Endtz (Rotterdam, NL)
Objectives: Colonization and resistance dynamics of enterococci in the intestinal microflora of patients admitted to intensive care units (ICU) and general wards (GW) were investigated during and after hospitalization.
Methods: Specimens were obtained on admission, once weekly during hospitalization, at discharge from the ICU, at discharge from the hospital and 1 and 3 months after discharge. Five colonies per specimen were selected for identification and susceptibility testing by the VITEK 2 system.
Results: A total of 1669 specimens from 411 patients were collected. In the ICU population the frequency of isolation of E. faecium significantly increased from 10.8% on admission to 23.7% at discharge from the hospital, whereas the frequency of E. faecalis decreased from 76.7% to 56.3%. Upon discharge, no significant changes were observed during the first 3 months. Similar frequencies were found in the GW population. In both populations no differences were measured in the percentage of patients colonized with ampicillin-, high-level gentamicin-(HLG) or vancomycin-resistant enterococci between subsequent points-in-time. Ampicillin resistance was infrequent in E. faecalis. Vancomycin resistance was not detected at all. The percentage of patients colonized with HLG resistant E. faecalis at discharge from the hospital was significantly higher in the ICU than in the GW population. During hospitalization the prevalence of ampicillin resistant E. faecium and HLG resistant E. faecalis significantly increased with length of stay on the ICU and GW. Changes in resistance at two subsequent points-in-time were more often detected in ICU patients compared to patients in GW. PFGE typing of these strains revealed that 70% of these resistant enterococci appeared unrelated to the strain isolated at the previous point-in-time.
Conclusions: The risk of dissemination of resistant enterococci into the community appears to be low. However, changes in resistance in patients during hospitalization are observed and may complicate treatment of nosocomial enterococcal infections.
O289: Contribution of nitrofurans illegal use to the selection and persistence of Salmonella amongst humans and foods of animal origin in Portugal
P. Antunes, J. Machado, L.V. Peixe (Porto, Lisbon, P)
Objectives: Salmonellosis is one of the most frequent foodborne diseases, with poultry products a potential source of infection. Salmonella is naturally susceptible to nitrofurans, an agent authorised in EU until 90's for food animal production. In Portugal, during the last years, a widely illegal use of nitrofurans was detected, affecting several types of husbandries, especially poultry ones. In this study we evaluated the susceptibility to nitrofurantoin of 1183 Salmonella isolates (clinical humans, poultry products, other foods and environment), in order to assess the contribution of nitrofurans illegal use in the selection and persistence of Salmonella.
Methods: The minimum inhibitory concentration was determined by the agar dilution method. The presence and genetic content of class 1 integrons were investigated by PCR and sequencing. Clonality was searched by PFGE following XbaI digestion.
Results: Decreased susceptibility to nitrofurantoin (MIC ≥ 64 mg/L) was the most common amongst our isolates (n = 767/1183; 65%), although resistance to other antimicrobial agents was also observed. A different resistance rate to nitrofurantoin was observed in isolates from poultry (n = 62/84; 74%) and clinical humans (n = 618/870; 71%) comparing to those from other food products (n = 76/173; 44%) and environment (n = 11/56; 20%). Decreased susceptibility to nitrofurantoin was most common in isolates from serogroup D, mainly S. Enteritidis of different phagetypes (85% of poultry and 89% of human isolates). It is of note that multiresistant isolates from serogroup B of clinical and food sources also presented decreased susceptibility to nitrofurantoin: S. Typhimurium clone carrying an 2000-bp integron with blaOXA-30 – aadA1 and S. Typhimurium DT104 clone carrying 1000 (aadA2) and 1200 bp (blaPSE-1) class 1 integrons.
Conclusion: This study points out for another perspective related with antibiotic usage in food animal production: the contribution of one antimicrobial agent on the emergence of a particular bacteria implicated in human infections. In Portugal, the widespread use of nitrofurans especially in the poultry industry may have contributed to the prevalence of S. Enteritidis in chickens and consequently in human infection. It is tempting to speculate that the use of nitrofurans may also have been implicated in the selection and persistence of the two multiresistant national widespread S. Typhimurium clones.
O290: Risk factors for ciprofloxacin resistance among E. coli strains isolated from community-acquired urinary tract infections
H. Arslan, Ö. Kurt Azap, Ö. Ergonul on behalf of the Urinary System Infection Study Group
Objective: To determine the risk factors for community acquired ciprofloxacin resistant E.coli urinary tract infection.
Methods: The study was performed with isolates of community acquired urinary tract infections collected from 15 centres representing 6 different geographic regions of Turkey. All microbiological procedures were carried out in the central laboratory. Multivariate analysis was performed for detection of risk factors. Use of quinolone more than once within the last year, living in rural area, having urinary catheter, age > 50, complicated infections were included to the model as variables, and logistic regression was performed.
Results: A total number of 537 isolates from 537 patients with community acquired urinary infections were studied. Eighty-five per cent of the patients were female, the median age was 49 years (19–70). Ciprofloxacin resistance was detected in 33% of the patients. Extended spectrum beta lactamase (ESBL) was detected in 9% of the strains. Living in rural area (p = 0.039), having urinary catheter (p < 0.001), complicated infections (including male gender, urological operation, etc), age > 50 (p = 0.002), quinolone use in last 3 months (p = 0.002), receiving quinolone more than once within a year (p < 0.001) were found to be statistically significant. Use of antibiotic regimen other than quinolone was not associated with ciprofloxacin resistance (p = 0.222). The Marmara region had the lowest rate of cipro resistance (23%), although it was not significant (p = 0.230). In multivariate analysis, use of quinolone more than once within the last year (OR, 2.7; CI, 1.4–5.2; p = 0.003), age > 50 (OR, 1.6; CI, 1.06–2.4; p = 0.023), having urinary catheter (OR, 5; CI, 1.6–16.7; p = 0.007), and complicated infections (OR, 2; CI, 1.3–3.1; p = 0.001) were found to be the risk factors of ciprofloxacin resistance. Emergence of ESBL was found to be associated with quinolone use (p = 0.008).
Conclusion: The high rate (33%) of ciprofloxacin resistance among urinary E.coli isolates is an emerging problem. Quinolone use, older age, urinary catheters and complicated infections are important predisposing factors. Prescribing quinolones for community acquired urinary tract infections should be based on antimicrobial susceptibility results even for the uncomplicated cases.
O291: Community-acquired bacteraemia due to extended-spectrum beta-lactamase-producing Escherichia coli: an emerging clinical challenge
J. Rodríguez-Baño, M.D. Navarro, L. Romero, M.A. Muniain, M. de Cueto, M.J. Ríos, E.J. Perea, A. Pascual (Seville, E)
Objectives: To describe the emergence of extended-spectrum beta-lactamase-producing Escherichia coli (ESBLEC) as a cause of community-acquired bacteraemia and to investigate the epidemiology, clinical features and risk factors for this infection.
Methods: All episodes of community-acquired bacteraemia (according to CDC criteria) due to ESBLEC from January 2001 to October 2004 in our 950-bed hospital were included. ESBL production and antimicrobial susceptibility were studied by microdilution (NCCLS guidelines). ESBL were characterized by isoelectric focusing, PCR, and sequencing. Clonal relationships among the isolates were determined by Rep-PCR. Two control groups (2:1 in each group) were chosen: (A) randomly selected episodes of community-acquired episodes of bacteraemia due to non-ESBLEC, and (B) randomly selected patients admitted from the emergency department. Univariate and multivariate analysis (logistic regression) were performed.
Results: Sixteen cases were included. The features of the patients were: median age, 71 years (range, 28–89); 62% were male; 81% had some contact with healthcare during last year; 44% had a structural disease of the urinary tract; 56% had received antimicrobials during the last 2 months (fluorquinolones the most frequent, 31%); the origin of the bacteraemia was the urinary tract in 56%, an intraabdominal infection in 31% and unknown in 13%; 25% presented with severe sepsis or septic shock; related mortality was 6% and crude mortality 13%. All isolates were susceptible to meropenem, piperacillin/tazobactam and amikacin, 58% to amoxicillin/clavulanic acid and 25% to ciprofloxacin. By Rep-PCR, the 12 isolates studied to date were clonally unrelated. The most frequent ESBL produced was CTX-M-14 (75% of the 12 studied isolates). Independent risk factors associated with ESBLEC bacteraemia were (multivariate analysis): for control group A, previous antimicrobial use (OR = 8.6, p = 0.004), and for control group B, age (OR = 1.05 per year, p = 0.07), structural disease of the urinary tract (OR = 18.7. p = 0.03), and previous antimicrobial use (OR = 10.3, p = 0.01). Previous health care-relation was not a risk factor.
Conclusions: ESBLEC should be consider as a cause of community-acquired bacteraemia from urinary or intraabdominal origins in adult patients who had recently received antimicrobials, and particularly fluorquinolones.
O292: Excess mortality associated with inappropriate treatment of patients with severe sepsis due to antimicrobial-resistant pathogens in European ICUs
S. Harbarth, Y. Carmeli, C. Brun-Buisson, M.J.M. Bonten (Geneva, CH; Tel Aviv, IL; Paris, F; Utrecht, NL)
Objectives: Despite the increasing prevalence of antimicrobial-resistant pathogens (AMR-P) and the ongoing controversy about the most effective control strategies, surprisingly few studies attempted to quantify the mortality burden of AMR-P in Europe. In the belief that accurate data on the clinical impact of AMR-P are necessary to allow informed policy-decisions, we performed an exploratory ecologic analysis of the crude excess mortality associated with inappropriate initial antimicrobial treatment of patients with severe sepsis and septic shock due to AMR-P in European ICUs.
Methods: Based on a comprehensive review of the published literature, we examined population-based data from several large cohort studies and clinical trials of critically ill patients with severe sepsis and septic shock. We constructed a conceptual model of a hypothetical cohort of an average European ICU (1000 admissions/year) to determine the number of premature excess deaths associated with AMR-P and to extrapolate the overall mortality burden. The model was reviewed by a 4-member expert panel consisting of 1 critical care specialist, 1 epidemiologist and 2 infectious disease specialists with extensive research experience in severe sepsis and AMR-P.
Results: The conceptual model is shown in the Figure. Our review indicated that the average excess fraction of AMR-P-related deaths was 24 fatal cases per 1000 cases of severe sepsis, corresponding to an average of 3 excess deaths per 1000 ICU-admissions. The AMR-P-related mortality burden varied greatly across European countries with more than 1000 excess ICU-deaths in Germany and France and less than 100 ICU-deaths in Denmark, Finland and Norway. The estimated total number of AMR-P-related excess deaths in 15 European countries was at least 5800.

Conclusions: AMR-P in critically ill patients appear to be an important public health problem in Europe. This report presents crude estimates rather than precise numbers due to the lack of validated surveillance data. Nevertheless, our results are likely to be conservative estimates and may allow further research to assess the cost-benefit of AMR-P control.
Bacterial biofilms
S315: Bacterial biofilms in nature and disease
B. Costerton (Los Angeles, USA)
Direct examinations of bacterial populations, growing in a very wide variety of natural and pathogenic ecosystems, have shown that the overwhelming majority of these organisms actually grow in matrix-enclosed biofilm communities. Single floating or swimming (planktonic) cells are rarely seen in any ecosystems except in nutrient-deprived systems, like the deep oceans, and in the acute bacterial infections that characterized the pre-antibiotic and pre-immunization eras. Between 65 and 80% of bacterial infections treated by physicians in the developed world have been shown to be caused by bacteria growing in biofilms, and all device-related infections belong to this category. Biofilm infections are generally characterized by a slow onset, by low-grade symptoms, and by their chonicity and their refractory response to antibiotic therapy. This inherent resistance to antibacterial agents, and to host defenses, has been demonstrated in vitro and its mechanism(s)has been elucidated to some extent. The extracellular matrix protects biofilm cells from antibodies and from phagocytes, and these sessile cells adopt a special phenotype that differs profoundly from that of planktonic cells, and mediates high levels of resistance to antibiotics and sterilants. Now that many of the salient characteristics of chronic bacterial infections have been attributed to the fact that the causative organisms live in biofilms, we can understand the etiology of dozens of infections ranging from otitis media to infections of native and mechanical heart valves. Bacteria colonize an inert or a tissue surface, they develop into biofilms, resist clearance by host or therapeutic factors, and damage surrounding tissues by stimulating inflammatory responses. Now that the central problem of chronic infection is perceived to be biofilm persistence, several methods of biofilm control can be ”borrowed” from nature and from engineering strategies. Many sessile plants and animals protect themselves from being buried in biofilms, by producing chemical blockers of biofilm formation, and these agents are now being used to control biofilms in industry. Engineers have discovered that biofilm bacteria can be killed by conventional antibiotics, if the structure of these sessile communities is disturbed by ultrasonic energy or by D.C. electric fields. We will describe instances in which these novel biofilm control measures are being used in medical and dental contexts.
S317: P. aeruginosa chromosomal beta-lactamase and biofilm resistance
O. Ciofu (Copenhagen, DK)
High-level expression of chromosomally encoded AmpC beta-lactamase is the main resistance mechanism to beta-lactam antibiotics of biofilm-growing P. aeruginosa from patients with cystic fibrosis and chronic lung infection. The aim of our studies was to establish the importance of this resistance mechanism for the resistance of biofilms to beta-lactam antibiotics. The AmpC expression in P. aeruginosa biofilms was studied in ceftazidime or imipenem treated biofilms (sub-MIC concentrations) of PAO1 with a reporter fusion of the ampC promoter to gfp (ASV) encoding an unstable version of green fluorescent protein. The effect of high-level expression of chromosomally encoded AmpC beta-lactamase on the survival of bacteria in a ceftazidime treated biofilm (10 times MIC) was studied in biofilms of Tn7gfp tagged clinical isolate stable derepressed for the production of AmpC due to an insertion sequence in the regulatory gene ampD and in the complemented strain expressing low basal level of beta-lactamase. The sub-MIC levels of ceftazidime and imipenem induced the monitor system, though imipenem was a better inducer. Sub-MIC levels of imipenem induced the monitor system in the periphery of the microcolonies while the centre remained uninduced, although the bacteria in the centre were physiologically active. The stable-derepressed expression of AmpC beta-lactamase played a protective role during the treatment with 10 times MIC ceftazidime. These results show that in biofilms, besides tolerance of P. aeruginosa to beta-lactam antibiotics due to low-growth rate, oxygen and nutrient deprivation, classical resistance mechanisms, like high-level expression of AmpC beta-lactamase have an important role for the therapeutic failure of biofilm eradication in the cystic fibrosis lung.
S318: Biofilm and virulence in staphylococci
P. Vaudaux (Geneva, CH)
The role of biofilm in staphylococcal diseases was revealed by the emergence of S. epidermidis clinical isolates producing an extracellular polysaccharide matrix and responsible for medical device infections and nosocomial bacteraemia. This discovery assessed that hospital conditions could transform non-virulent organisms into significant pathogens. In the following decades, numerous studies aimed to correlate qualitative or quantitative in vitro biofilm production with bacterial virulence in coagulase-negative staphylococci (CNS). Thus, biofilm production was considered as the major or sole factor of CNS virulence. Characterization of a major polysaccharide intercellular adhesin (PIA) component of staphylococcal biofilm and identification of the icaABDC operon opened the way to molecular studies of biofilm production in staphylococci. The prevalence of a highly conserved icaABDC operon in both S. aureus and S. epidermidis or some other CNS species represents a challenging observation that should be interpreted with caution in view of the significant differences in PIA expression by S. aureus versus CNS isolates. First, the extent of biofilm formation and its environmental regulation in vitro show significant differences between S. aureus and S. epidermidis. Second, S. aureus exhibits a much wider spectrum of virulence factors than S. epidermidis, which contribute to its multiple, alternative modes of virulence and persistence in human and animal hosts. Further work is needed to more precisely define the involvement of biofilm formation in the various categories of S. aureus diseases or colonization in humans.
Focus on new antibacterials
S319: The oxazolidinones
R. Moellering (Boston, USA)
The oxazolidinones represent the only unique class of antimicrobials developed in the past 20 years. Originally synthesized as monoamine oxidase inhibitors, molecular manipulation has resulted in compounds with acceptable toxic : therapeutic ratios and outstanding activity against resistant gram-positive pathogens. Linezolid is the first of these compounds to be successfully developed for clinical use. The oxazolidinones have a unique mechanism of action, inhibiting the formation of the initiation complex in ribosomal protein synthesis. Resistance develops via mutations in the 23S rRNA gene. Since most of the important gram-positive pathogens have multiple copies of this gene and it requires more than a single mutation to develop clinical resistance, bacteria have been slow to develop immunity to these compounds. The oxazolidinones also exhibit excellent bioavailability and outstanding tissue penetration. They show little or no interaction with the cytochrome P450 system and they have been shown to be clinically effective. Nonetheless, the currently available oxazolidinone, linezolid, does have certain disadvantages. The MICs are near the breakpoints for many susceptible organisms (and above for H. influenzae and M. pneumoniae). The drug is bacteriostatic or only slowly bactericidal and failures in endocarditis have been reported. Although toxicity has not been an issue in standard courses of therapy, myelosuppression, peripheral neuropathy, and optic neuritis have been seen in patients receiving the drug for long periods of time. This has proven to be a disadvantage in its application for infections such as Nocardia and tuberculosis (both organisms of which are susceptible to linezolid) because of the long duration of therapy involved. It has outstanding penetration in the CSF, but formal studies evaluating it in meningitis have not been performed. Because of its relatively short half-life, it must be given twice a day. A number of new oxazolidinones are being developed in an attempt to improve on the valuable properties of linezolid. Although none of these has yet reached the clinic, they will receive further discussion.
S320: New glycopeptides and lipopeptides
D. Livermore (London, UK)
Vancomycin and teicoplanin are treatment mainstays versus severe gram-positive infections, used increasingly with the spread of MRSA. They are however less-than-ideal-antibiotics, being only slowly bactericidal. Moreover, vancomycin is inferior to beta-lactams against infections due to methicillin-susceptible S. aureus and vancomycin resistance has emerged in enterococci and -rarely- staphylococci; teicoplanin resistance is common in coagulase-negative staphylococci (CoNS) and occurs in enterococci with VanA. Three new glycopeptides now in Phase III: dalbavancin, oritavancin and telavancin. Dalbavancin resembles teicoplanin in microbiological activity but is more active against CoNS. Its unique feature us a serum t1/2 of c. 10 days, allowing once-weekly regimens and facilitating outpatient therapy or early discharge. By contrast, telavancin and oritavancin break the microbiological mould of earlier glycopeptides, being rapidly bactericidal and retaining activity against all vancomycin-resistant enterococci, including VanA strains. These differences reflect a secondary mode of action, probably involving membrane disorganisation. Daptomycin, the first lipopeptide antibiotic licensed, resembles glycopeptides in spectrum but has a unique mechanism, disrupting membrane potential and causing cell leakage. It is rapidly bactericidal and is unaffected by established resistance mechanisms; nevertheless there are a few reports of resistance emerging during therapy. The coming challenge is determining how best to deploy these compounds in relation to earlier glycopeptides and to other new anti-gram-positive options. Is the rapid bactericidal activity of telavancin, oritavancin and daptomycin a major advantage in endocarditis, in immunocompromised patients or even in surgical prophylaxis vs. MRSA? Will multiple modes of action of guard against rapid accumulation of resistance? Will any impact be made on the prevalence of MRSA infections?
S322: Structure-activity relationship analysis and therapeutic potential of peptide deformylase inhibitors
T. Meinnel, C. Giglione, A. Boularot, A. Serero (Gif/Yvette, F)
Peptide deformylation is the first step of the N-terminal Met excision (NME) pathway in bacteria, unmasking the N-Met, making possible the action of Met aminopeptidase [1]. Deformylation is a crucial step in bacterial protein biosynthesis and is essential for bacterial growth [2]. At least one PDF gene has been found in all eubacterial genomes sequenced to date [3]. Peptide deformylase inhibitors (PDFI) appear to be one of the most exciting classes of antibacterial agents discovered to date. Rapid progress in the development of PDFI has been possible because (i) PDF is a metalloprotease, and this class of enzymes shows a high degree of structure-function conservation and (ii) the most potent PDFI are hydroxamate derivatives, a well known category of pharmacophores. The current challenge in structure activity relationship analysis is obtaining molecules with potent antibacterial activity in vivo against a range of drug resistant pathogens [4]. The PDFI now in clinical trials target community based bacterial infections, corresponding to a major pharmaceutical market [5]. Nevertheless, a transcribed gene encoding a homolog of bacterial PDF has been identified in the human genome [6]; the encoded enzyme was shown to be active as a PDF in vitro, located in the mitochondria and one of the two components of mitochondrial NME [7-9]. Although further studies are required to determine the precise function of human mitochondrial NME, PDF activity appears to be crucial for human cells growth [10]. In this context, the precautionary principle imposes a new schedule of conditions for the design of new PDFI that will take into account the absence of inhibition of human PDF. As PDF inhibitors seem to have only very low levels of toxicity in human cells, PDF is however truly an exciting new target for the design of novel antibiotics.
Emerging infections in the immunocompromised host (Symposium arranged with EORTC/IDSG)
S324: Infectious complications of anti-TNF strategies
J.W.M. van der Meer (Nijmegen, NL)
More than a decade ago, animal experiments demonstrated that treatment with antibodies against tumour necrosis factor (TNF) was deleterious in mycobacterial infections, fungal infections and abscesses Although the exact mechanisms by which interference with TNF produced these results were not fully elucidated, it was clear that the containment of microorganisms within granulomas and abscesses was not achieved or maintained. From these studies, it could be predicted that large-scale and prolonged anti-TNF treatment in humans would lead to infectious complications. Indeed, such complications (especially mycobacterial infections) are being encountered. The occurrence of these infections has implications for pretreatment assessment of patients, and guidelines are now appearing. The risk for opportunistic infections seems to be greater with monoclonal antibodies against TNF than with the TNF receptor construct. From a theoretical point of view one would assume differences between the types of anti-TNF drugs, as they differ in their capacity to interact with TNF-alpha and TNF-beta (lymphotoxin), and with membrane-bound TNF. As stated, it is not entirely clear how inhibition of TNF impairs host defence. Secondary inhibition of interferon-gamma may play a role, but more investigations are clearly needed.
S325: Empirical antifungal therapy in cancer patients with persistent fever
M. Akova (Ankara, TR)
Invasive fungal infections remain an unsolved misery in neutropenic cancer patients. It has long been accustomed to apply empirical amphotericin B or its lipid derivatives to those who did not respond to broad-spectrum antibacterial therapy and in whom no clues of infection apart from fever are present. However, such a practice is far from being ideal for decreasing mortality and morbidity due to disseminated fungal infections, since by this approach many patients are exposed unnecessarily to toxic and expensive drugs for an undetermined period of time. Recently, new improvements have significantly changed this picture. First, although conventional amphotericin B is still one of the most effective and broadest-spectrum antifungal agents, new less toxic and equally effective compounds have become available. Second, newer diagnostic tools tempted physicians to use these antifungal agents in a preemptive or targeted manner rather than empirical. The remaining piece in this puzzle is to develop a predictive model, as this has been a successful case for bacterial infections, in order to identify who will most benefit from empirical/preemptive antifungal treatment. Until then, the current approach to cancer patients with persistent fever must address antifungal treatment issues of effectiveness, safety and cost.
Community-acquired MRSA in Europe – evolution at work
S327: The evolution of community MRSA in Australia – lessons for Europe?
T.V. Riley, G.W. Coombs, F. O'Brien, J.W. Pearman, K. Christiansen, W.B. Grubb (Perth, AUS)
In the early 1980s, epidemic MRSA (EMRSA) appeared on the east coast of Australia. EMRSA were multiply resistant and they became endemic in many large hospitals throughout Australia, except Western Australia (WA). A statewide screening and control policy was implemented in WA following an outbreak of EMRSA in a Perth hospital after the admission of an interstate patient in 1982. This involved screening all patients admitted to hospitals from interstate or overseas and all new staff that had worked outside WA in the previous 12 months. Following screening, patients infected or colonized with MRSA were isolated and treated, while infected or colonized staff were prohibited from contact with patients until the organism was eradicated. In WA, MRSA infection or colonization has been a notifiable condition since 1985. The WA Department of Health electronically flags cases of MRSA, allowing carriers to be identified and isolated on admission to any WA public hospital. In the late 1980s, non-multiresistant community MRSA emerged in the north of WA. MRSA isolated from patients living in the remote Kimberley region were phenotypically and genotypically different to EMRSA and became known as WAMRSA. During the 1990s, WAMRSA spread to most regions of WA and, by 1997, a significant number of cases of infection and colonization were occurring in the Perth metropolitan area and other Australian states. WAMRSA have the community-associated SCCmec types IV and V that lack transposons, integrated plasmids and other antibiotic resistance genes. Since the screening and control policy was introduced, all MRSA clinical isolates, and those isolated through screening, have been sent to a reference laboratory where their identity was confirmed by standard procedures (mec/nuc PCR), complete antibiotic susceptibility was determined and the isolates typed, using initially PFGE and now MLST. In the 1990s, a different community MRSA was isolated in eastern Australia, frequently from people of Pacific Island decent. These were subsequently identified as ‘Western Samoan Phage Pattern’ strains, first described in New Zealand, and they can produce PVL. Most Australian community MRSA do not produce PVL, apart from the ‘Queensland’ clone. Although most Australian community MRSA do not spread when introduced into a hospital environment, some do have the capacity to cause outbreaks. Identifying the reasons for this and ways of identifying outbreak strains remains a challenge for us all.
S328: Clonal evolution and SCCmec in community-acquired MRSA
D.C. Oliveira, H. de Lencastre (Oeiras, P)
Community-acquired (CA) MRSA have recently emerged in several parts of the world suggesting a new trend on MRSA epidemiology with major impact on public health. Several pieces of evidence suggest that CA-MRSA may have evolved independently from hospital-acquired (HA) counterparts: (i) most CA-MRSA belong to specific genetic backgrounds (defined either by PFGE or MLST); (ii) they are less resistant to antimicrobial agents (usually resistant to b-lactam antibiotics only); (iii) they are more often positive for the PantonValentine Leucocidin (PVL) toxin genes; and (iv) they carry predominantly the smallest variant of the chromosomal cassette responsible for the resistance to b-lactam antibiotics (SCCmec type IV). The origin and dissemination of CA-MRSA is not clear but it seems that it was due to the independent acquisition of virulence traits (e.g. PVL gene) and resistant genes (e.g. SCCmec) by S. aureus lineages previously well adapted to the open community environment. This hypothesis explains the emergence of CA-MRSA in remote communities not exposed to the nosocomial milleu (e.g. Australia) and in countries where MRSA prevalence in hospitals is extremely low (e.g. Denmark). The SCCmec element carries the central element of methicillin-resistance (the mecA gene), so that its aquisition defines the evolutionary step from methicillin-susceptible S. aureus (MSSA) to MRSA. Moreover, since SCCmec also carries the genes responsible for its mobility (ccrAB locus) as well other acessory DNA sequences, it may be used as a marker for the origin and evolution of MRSA lineages. So far, four major SCCmec types have been described. HA-MRSA are mostly characterized by SCCmec types I–III, whereas CA-MRSA are mostly characterized by SCCmec type IV. Interestingly, SCCmec type IV seems to be the most mobile version since, besides being dominant among CA-MRSA, it is present among several HA-MRSA lineages and is also quite frequent among methicillin-resistant coagulase-negative staphylococci. Perhaps as consequence of its enhanced mobility, SCCmec type IV is highly variable and several structural variants have been described, which makes its proper identification problematic and a challenge for any SCCmec typing scheme. Nevertheless, it is now clear that studies on the genetic organization(s) of SCCmec type IV strains are a key strategy for a better understanding of the origin and evolution of MRSA in general, and CA-MRSA, in particular.
S329: Update on current community-acquired MRSA situation in Europe
W. Witte (Wernigerode, D)
Community acquired MRSA (cMRSA) are defined as affecting patients without the known risk factors for MRSA associated with nosocomial infections. The majority of cMRSA contains the lukS-lukF determinant (coding for Panton Valentine Leukocidin and SCCmec elements of group IV (the latter are, however, also in epidemic MRSA of multilocus sequence types (MLST) 22 and 45. cMRSA are often the cause of deep seated infections of skin and soft tissue, also cases of necrotizing pneumonia became known. cMRSA from Europe as well as from world wide sources belong to different MLST types (table).
Table 1.
Emergence and spread of MRSA with lukS-lukF in different geographical regions and countries.
| MLST type | Country where emerging |
|---|---|
| 80* | Australia, Belgium, France, Germany, Netherlands, Sweden, Switzerland |
| 30 | Germany Latvia, Sweden, US, Southern Pacific |
| 1* | Germany, Sweden, US |
| 5 | Netherlands, Slovenia |
| 8* | New Zealand, US |
| 22 | Germany, Scotland |
| 59 | Sweden, US, Taiwan |
| 152 | Sweden, Slovenia |
| 154* | Sweden, Mongolia |
| 290 | Australia |
also nosocomial spread known
Some MLST-types suggest a wide dissemination of particular strains. This needs to be confirmed by further subtyping. Of special concern is the emergence of until now epidemic nosocomial MRSA which have acquired lukS-lukF and cause infections in the community. The reservoirs and ways of transmission of cMRSA in Europe are largely unknown.
Recent trends in severe fungal infections
O334: Semi-national surveillance of fungaemia in Denmark: species distribution and antifungal susceptibility
M.C. Arendrup, K. Fuursted, B. Gahrn-Hansen, I.M. Jensen, J.D. Knudsen, B. Lundgren, M. Tvede, H.C. Schønheyder (Copenhagen, Århus, Odense, Herlev, Hvidovre, Ålborg, DK)
Objective: The epidemiology of fungaemia in Denmark is not systematically investigated. This study was undertaken to characterize species distribution and susceptibility pattern in different parts of the country.
Methods: Six departments of clinical microbiology in Copenhagen, Copenhagen county, Funen county, Aarhus county and Northern-Jutland county were included prospectively. The 6 departments serve a population of 2,870,000 which is about half the Danish population. From each episode of fungaemia, defined as isolation of the same fungus from blood culture with in a 21 day period, one isolate was to be sent to the unit of mycology and parasitology for verification of species identification and susceptibility testing. Species identification was done by use of colony morphology on CHROMagar plates at 35°C (CHROMagar CO., Paris, France), presence or absence of chlamydoconidia on Rice and Tween agar plates (SSI Diagnostica, Hilleroed, Denmark), growth at 35 and 42°C and by ID32C (bioMerieux, Marcy l'Etoile, France). Susceptibility testing for amphotericin B, caspofungin, fluconazole and itraconazole was performed according to the NCCLS document M27-A.
Results: A total of 298 episodes of fungaemia were registered. Candida species accounted for 97.5% of the fungal pathogens. Although C. albicans was the predominant species (64%) the proportion was lower than previously described (85% in 1994–5). However, the relative proportion varied considerably, i.e. from 57% at Hvidovre University Hospital to 72% at Herlev and Odense University Hospitals. C. glabrata was the second most frequently isolated fungus (overall 20%) but again considerable variation in frequency was demonstrated (8–32%). C. krusei was rarely isolated (3%) and only detected at two of the six microbiology laboratories. Amphotericin B and Caspofungin MICs were in agreement with the typical patterns predicted by species identification, however, decreased azole susceptibility, defined as fluconazole MIC >8 and/or itraconazole MIC > 0.125 μg/ml was detected among 11 non-glabrata, non-krusei Candida isolates (Table 1).
Table 1.
Candida isolates with either genuine or acquired reduced susceptibility to fluconazole and/or itraconazole among Danish blood pathogens.
| Species | Herlev Odense | RH | Arhus | Albong | Hvidovre | All |
|---|---|---|---|---|---|---|
| Genuine SDD or R Candida spp.* | 3 (8%) 8 (17%) | 13 (23%) | 14 (25%) | 18 (31%) | 14 (32%) | 70 (23%) |
| Aquired SDD or R Candida spp. | C. albicans |
|
|
|
|
11 (4%) |
C. glabrata and C. krusei
C. albicans: Highly resistant isolates with MIC's of itraconazole > 16 and fluconazole >64 μ/ml.
Conclusion: The species distribution of invasive fungal infections is shifting with an increase in non-albicans species. Reduced susceptibility to azoles was detected among 4% of non-glabrata/krusei isolates and more frequent in departments with a high proportion of C. glabrata isolates.
O335: Changing patterns of candida infection
S. Thomas, F. Dale, S. Ghoneim (Dumfries, UK)
Although Candida albicans remains the most common candidal fungaemia, treatment resistant, non-albicans species are becoming increasingly prevalent. There is little data available on the epidemiology of these non-albicans species
Aims: To examine the incidence of candida colonisation in ITU patients with emphasis on prevalence and infection patterns of non-albicans species.
Method: A retrospective analysis of patients admitted to the ITU in Dumfries and Galloway Royal Infirmary, over a 6 month period.
Results: A positive sputum culture was isolated from 54 patients. All patients had routine sputum samples sent, tracheal aspirates were sent from ventilated patients. 52% of patients were colonised with C. albicans. 48% of patients were colonised with non-albicans species, 74% of which were male patients. 85% of the non-albicans species were C. glabrata. C. tropicalis was isolated in 19% of patients (5 patients, 4 out of 5 of which was in combination with a second candida species). 24% of patients were colonised with both C. albicans and C. glabrata. The average age of patients with C. glabrata was 75 years, much higher than for patients with C. albicans (62 years). The mean APACHE II scores for patients with C. glabrata was 28 (range 79 to15), significantly higher than for patients with C. albicans 18, (range 32 to 8). All patients with C. glabrata had been treated with broad spectrum antibiotics, 78% with more than one type. Of the patients with non-albicans species, 77% had been ventilated, 82% had intravascular or urinary catheters in-situ. 26% had undergone abdominal surgery and 26% had severe underlying respiratory problems. Only 5 patients with initial C. albicans, who were treated with triazoles, subsequently became colonised with C. glabrata. Over the six month period, results suggest clustering of C. glabrata in months 1, 5 and 6.
Discussion: Studies suggest an increasing trend of C. glabrata in the acute clinical setting. Isolates are possible in the absence of C. albicans. Frail, immunocompromised patients, in particular those who have had interventional therapy, broad spectrum antimicrobial or antifungal therapy seem to be at a highest risk. Clustering may implicate contamination from healthcare workers in its transmission. This may be an understated risk factor in the acquisition of C. glabrata infection and emphasizes the need for strict infection control measures.
O336: Trends in incidence of invasive fungal infections at a tertiary cancer centre over a 14-year period: an autopsy study
G. Chamilos, G.P. Bodey, M. Luna, R.E. Lewis, K.V. Rolston, R. Chemaly, A. Safdar, I. Raad, D.P. Kontoyiannis (Houston, USA)
Objectives: Autopsy series remain the most reliable way to study epidemiology of invasive fungal infections (IFI). We sought to identify trends in incidence of IFI and associated risk factors in cancer patients in our institution over the last 2 decades.
Methods: Autopsies of cancer patients at MDACC were analyzed over 3 study-periods (A: 1989–1993, B: 1994–1998, C: 1999–2002), each associated with the introduction of a new antifungal (A: fluconazole, B: lipid formulations of amphotericin B, C: echinocandins).
Results: The median autopsy rate decreased significantly over the 3 study periods (219/year, 65/year, and 56/year respectively), (p = 0.02). 336 IFIs were identified in 1449 autopsies (23%). Most (94%) IFIs occurred in patients with haematological malignancies. The incidence of IFIs increased from 20% (1989–1993) to 30.5% (1994–1998) and 36.4% (1999–2002) in recent years (p < 0.0001). This trend was mainly associated by a significant increase in incidence of invasive aspergillosis after period A (8.4%, 16.5%, 20.4% in each period respectively, p < 0.0001). Non-fumigatus aspergilli were the most common causes of aspergillosis in our institution throughout all periods (65%, 56%, 63%, p = 0.28). In contrast, the incidence of candidiasis remained stable (8.4%, 10.1% and 8.0% respectively), (p = 0.68) while a predominance of non-albicans Candida strains occurred in period B and C (43%, 69%, 61%, p < 0.0001). A significant increase in incidence of zygomycosis (0.4%, 2.5%, 2.2%) (p = 0.002) and other non-Aspergillus mould infections was noted after period A (1.4%, 1,1% 5.3%) (p = 0.0002). Finally, Candida spp caused the majority of IFIs in patients with solid tumors (65% of all IFI), while aspergillosis and non-Aspergillus mould infections predominated in patients with hematologic malignancy and/or bone marrow transplantation (64% of all IFI).
Conclusions: Although Aspergillus and Candida continue to represent the majority of IFIs at autopsy, the epidemiology of IFIs is changing, with the emergence of resistant yeasts and moulds, especially among severely immunocompromissed cancer patients. The declining autopsy rates represent a challenge in the study of epidemiology of IFIs.
O337: Nosocomial candidaemia in a Brazilian paediatric population: a 9-year study comparing risk factors and the outcome of paediatric and adult candidaemia
A.C. Pasqualotto, W.L. Nedel, T.S. Machado, L.C. Severo (Porto Alegre, BR)
Objectives: To compare risk factors, etiology, therapy, and outcome of nosocomial candidemia between pediatric and adult patients with candidemia in a large Brazilian tertiary hospital.
Methods: A retrospective cohort study was performed in Santa Casa Complexo Hospitalar, Brazil, during the period comprising 1995 and 2003. Patients were considered pediatric if their age was <13 years-old. Medical charts were reviewed to record clinical and demographic characteristics presented in the period of 30 days before collection of the first blood sample positive for Candida.
Results: During this period, 78 pediatric and 113 adult patients with nosocomial candidemia were studied. Species other than C. albicans caused 78.2% of episodes of candidemia in pediatric patients. Compared to adults, pediatric patients received more frequently broad-spectrum antibiotics, H2 blockers, vasopressors, blood transfusions, arterial catheter, gastrostomy, chest tube, cardiothoracic surgery, mechanical ventilation, and parenteral nutrition. Candidemia caused by C. parapsilosis was more common in pediatric patients, as was the isolation of Candida spp. from catheters. Amphotericin B treatment was more common in pediatric patients. The 30-day mortality rate was higher in adults.
Conclusions: C. parapsilosis was the main etiology of candidemia in this large Brazilian retrospective cohort of pediatric patients. As expected for pediatric patients, C. glabrata was an infrequent species. The underlying diseases, predisposing conditions, and antifungal treatment were different between pediatric and adult patients, and Candida spp. were more commonly isolated from catheters in pediatric patients. Treatment with amphotericin B was more common in pediatric than adult patients. Although in-hospital crude mortality was similar between these groups, the mortality rates within 48h, 7 days, 15 days and 30 days after blood sample were all higher in adults. We reinforce the necessity of continuous epidemiologic surveillance to follow the dynamics of candidemia.
O338: Fluconazole susceptibility in Candida glabrata varies with clade
A.R. Dodgson, C. Pujol, M.A. Pfaller, D.W. Denning, D.R. Soll (Manchester, UK; Iowa City, USA)
Objectives: Candida glabrata is the second most prevalent Candida species in cases of bloodstream infection in the US. It is notable for its decreased susceptibility to the azole antifungal agents. Recent studies have shown that C. glabrata has a primarily clonal population structure. To date, seven major clades have been described, however there is no description of clinically relevant differences in the phenotypes exhibited by isolates of different clades. This study aimed to examine the relationship between fluconazole susceptibility and clade.
Methods: A collection of 445 US C. glabrata isolates from the SENTRY and ARTEMIS studies was used in this study. The fluconazole MIC of each isolate was determined using NCCLS M27-A methodology. Clade was determined using a reduced Multilocus Sequence Typing (MLST) method, whereby only 2 of the loci found to be most variable in previous studies (NMT1 and FKS) were sequenced. This methodology, while slightly reducing discrimination, allowed accurate determination of clade while decreasing both the cost and time involved in sequencing all 6 MLST loci.
Results: Of the 445 isolates typed in this study, 397 belonged to one of 8 major clades (named Groups I to VIII). Seven of these were previously described, the additional one being novel to this study. The number of isolates within each clade ranged from 5 (Group VII) to 82 (Group III). For the total collection of 445 isolates, the numbers in each of the NCCLS susceptibility categories were as follows: Susceptible (S, MIC < 16 μg/ml) 292 (66%); Susceptible Dose Dependent (S-DD, 16–32 μg/ml) 108 (24%); Resistant (R > 32 μg/ml) 45 (10%). For most clades the percentage of isolates within these categories was broadly similar to that seen for the whole collection. However, a number of clades showed distributions markedly different to the collection as a whole. For instance in Group I (49 isolates) only 53 % were S, whereas in Group VI (78 isolates) this value was 74%.
Conclusions: This study demonstrates that clinically relevant phenotypic differences exist between isolates from the major clades of C. glabrata. This is the first observation of the phenomenon in C. glabrata, though clade-specific differences in 5-FC resistance and alleles of the ALS family of adhesions have been described in C. albicans. Previous studies have shown geographical differences in the MIC's of C. glabrata, it remains to be seen if this is due to the clade-specific differences noted in this study.
O339: Aspergillus galactomannan antigen detection in different batches of piperacillin-tazobactam
M. Machetti, E. Furfaro, L. Boni, C. Viscoli (Genoa, I)
Objectives: Invasive aspergillosis (IA) is a serious life-threatening complication in patients with haematological malignances. The detection of circulating galactomannan (GM) in blood with the Platelia Aspergillus test (PA – Bio-Rad), is one of the criteria defining IA. In the last 2 years several authors found GM in patients treated with Piperacillin-Tazobactam (P/T) and in P/T vials (Maertens et al. NEJM 2003, Viscoli et al. and Adam et al. CID 2004), while others did not (Penack et. al, CID 2004). Therefore we decided to try to give an explanation to these apparently controversial results, by evaluating both the proportion of positive batches and vials and the extent of GM contamination.
Methods: Ninety P/T vials from 30 randomly selected batches were tested with the PA test (median vials per batch 3, range 1–4). The drug was diluted as for clinical use (4.5 mg/ml NaCl 0.9%) and the test was performed with the same method used for serum samples. NaCl 0.9% alone was tested as negative control. Samples with a GM index > 0.7 was considered as positive.
Results: Twenty-six batches (86%) tested positive (all vials), with a median GM index of 1.99 (range 0.77–6.98) among vials with quantifiable levels, while 4 tested negative (median index 0.28, range 0.19–0.3) and 4 (12 vials) had an index >7. No further quantification was performed in these 12 samples. There is an apparently bimodal distribution of GM levels in the 79 positive vials (Fig. 1). Indeed 40 vials had GM indexes ranging from 0.77 to 2.87, while 39 vials had indexes ranging from 3.86 to 6.98. Distinction of positive results into 2 groups was supported by analysis of frequency distribution (data not shown).

Positive and negative vials GM indexes distribution (12 vials with indexes >7 are not included)
Conclusion: The rate of P/T batches testing positive with the PA test is in agreement with previous reports (75–100%). A recent study indicates that the positivity of PA test with P/T is likely due to a contamination of the drug with GM and not to a cross-reaction with the antibiotic (Mennink-Kersten et al. ICAAC 2004). So, while the origin of this contamination could be due to the use of Penicillium cultures for the production of P/T, it remains unclear why GM content differ substantially by batch and why some batches are negative. Our results show that not all P/T batches contain GM, and that the extent of contamination is highly variable.
O340: Prospective evaluation of sequential Aspergillus galactomannan antigen detection and CT scan of the chest for early diagnosis of invasive pulmonary aspergillosis in recipients of allogeneic stem cell transplantation
A. Busca, G. Limerutti, A. Mele, R. Serra, A. Barbui, L. Godio, F. Locatelli, M. Falda (Turin, I)
Early diagnosis of invasive pulmonary aspergillosis (IPA) is important as early treatment with antifungal drugs may increase patient survival.
Objectives: Our study investigated the efficiency for IPA diagnosis of the Aspergillus galactomannan antigen (AGA) detection routinely used in combination with chest CT scan.
Methods: From February 2002 to June 2004, we prospectively measured serum AGA levels in a consecutive series of 74 adult hemato-oncological patients who underwent allogeneic SCT from matched sibling donors (n = 48), partially matched related donors (n = 7) or matched unrelated donors (n = 19). Serum samples were taken twice weekly, starting at the beginning of conditioning regimen until the end of hospitalisation, while outpatients were monitored once per week if received immunosuppressive therapy. AGA positivity was defined as an OD index of galactomannan × 1.0 in 2 subsequent sera. High resolution chest CT scans were performed when fever of unknown origin had lasted 3 days of broad-spectrum antibacterial therapy, or when chest radiographs showed abnormalities.
Results: IPA was diagnosed in 9 of 74 patients (12%): according to the EORTC/MSG criteria, 7 patients were classified with probable IPA, 2 patients were classified with proven IPA, whereas 65 patients did not fulfill criteria of IPA. Fourteen patients showed positive results for AGA. Five patients (8%) had a false-positive result, while no false-negative tests have been observed in our series. The sensitivity and specificity of the test were 100% and 93% respectively; the PPV and NPV were 64% and 100% respectively. All patients with probable or proven IPA showed abnormal CT signs. In 4 cases imaging signs followed AGA positivity (median 5 days;range 0–9), whereas in 5 cases preceded the positive results of serological tests (median 8 days;range 1–12). Based on the presence of positive AGA combined with imaging signs suggestive of IPA, antifungal therapy was promptly instituted including lipid formulations of amphotericin B (n = 5) or caspofungin (n = 4). In only 2 of the 9 patients (22%) with IPA, the primary cause of death was the fungal infection; 4 patients (45%) died of recurrent disease (in 2 cases fungal infection contributed to death) and 3 patients (33%) are currently alive with no evidence of infection.
Conclusions: The combination of AGA detection and early chest CT scans might be considered useful tools to detect minimal changes of IPA. Based upon these findings, aggressive antifungal therapy should be initiated.
O341: Predisposing risk factors and outcome in ICU patients with invasive aspergillosis
K. Vandewoude, S. Blot, P. Depuydt, D. Benoit, J. Decruyenaere, J. De Waele, E. Hoste, F. Colardyn (Ghent, B)
Objective: To investigate outcome in ICU patients with invasive aspergillosis (IA) and to evaluate whether patients with predisposing risk factors have a worse outcome.
Methods: Retrospective cohort study (1997–2003). Definite IA was defined as: (1) positive microscopic examination with septate hyphae and positive Aspergillus culture on tissue biopsy, or (2) positive culture of a normally sterile site obtained by aseptic invasive techniques. Probable IA is defined as (1) clinical symptoms of infection, (2) any positive culture from a nonsterile site, (3) chest X-ray or CT of lungs suggestive for IA and (4) either (a) positive results of microscopic examination and culture of BAL fluid or (b) predisposing host risk factors for IA. Haematological/oncological malignancy treated with cytotoxic agents, neutropenia, glucocorticoid treatment, and congenital or acquired immunodeficiency were considered as risk factors for the acquisition of IA.
Results: During the study period 83 patients developed IA whereof 50 with and 33 without risk factors. Definite IA was diagnosed in 16 patients; 8 in each group (respectively 16% and 24.4%). Patients with risk factors had higher APACHE II scores (32 ± 6.8 vs. 23 ± 9.2; p = 0.002). Patients with and without risk factors had the same age (60 ± 14.0 vs. 55 ± 15.0 year; p = 0.060) and there was no difference in the proportion of patients needing mechanical ventilation (94% vs. 100%; p = 0.273), renal replacement therapy (34% vs. 48%; p = 0.252) or vasoactive therapy (86% vs. 94%; p = 0.306). Length of ICU stay (18 ± 18.4 vs. 28 ± 23.5 days; p = 0.027) and length of mechanical ventilation (16 ± 14.9 vs. 25 ± 21.1; p = 0.041) were significantly longer in patients without risk factors. 86% of patients with and 85% of patients without risk factors received antifungal therapy (p = 0.999). There was no difference in delay of administering antifungal therapy between patients with and without risk factors was observed (respectively 2.3 ± 3.0 vs. 2.1 ± 1.9 days; p = 0.723). No difference was found between patients with and without risk factors in 14-days mortality (70% vs. 55%; p = 0.251), 28-days mortality (76% vs. 64%; p = 0.322) and in-hospital mortality (82% vs. 70%; p = 0.285). A logistic regression model could not identify independent risk factors for mortality.
Conclusion: The hospital mortality in ICU patients with IA is high (77%). No difference in mortality was found between patients with (82%) and without risk factors (70%) for the acquisition of IA.
O342: Results of a double-blind, placebo-controlled trial in patients with culture-confirmed invasive candidiasis, treated with a human recombinant antibody to hsp90 and liposomal amphotericin B
R.C. Matthews on behalf of the Mycograb Study Group
Objectives: To determine whether combination therapy with a human recombinant antibody to hsp90 (Mycograb) plus a lipid preparation of amphotericin B was superior to monotherapy with liposomal amphotericin B.
Methods: This was a prospective, double-blind, randomised, comparative study of the efficacy and safety of a 5 day course of Mycograb (1 mg/kg iv) plus liposomal amphotericin B versus placebo (saline iv) plus liposomal amphotericin B in adult hospitalised patients with culture-confirmed deep-seated candidiasis. Patients were stratified on the basis of their germ tube test result. Efficacy was assessed on the basis of clinical and mycological response at Day 10, Candida-attributable mortality (28 days after last dose of study drug) and speed of culture-confirmed resolution of the infection. The primary efficacy variable was overall response at Day 10 i.e. clinical and mycological resolution of the infection. There were 137 patients in the modified ITT population, recruited from 10 European countries and 2 US Centres.
Results: A complete overall response was obtained in 48% (29/61) of the placebo group compared to 84% (47/56) of the Mycograb-treated group (p < 0.001). The following secondary efficacy criteria were also met: clinical response (52% versus 86%, p < 0.001), mycological response (54% versus 89%, p < 0.001), Candida-attributable mortality (18% versus 4%, P < 0.025), and rate of culture-confirmed clearance of the infection, being over twice as fast in the Mycograb-treated group (P 0.001). Mycograb was well-tolerated.
Conclusion: Combining Mycograb with amphotericin B produced a highly statistically significant improvement in outcome in patients with culture-confirmed invasive candidiasis, mirroring the synergy observed between these two drugs in pre-clinical studies. This is the first time a double blind, placebo controlled trial has shown synergy between two antifungals in the treatment of invasive candidiasis.
O343: Efficacy of high-dose caspofungin in 22 cancer patients with invasive fungal infections
A. Safdar, G. Rodriguez, K.V. Rolston, H. Kantarjian, R. Champlin, I. Raad, D. Kontoyiannis (Houston, USA)
Objective: Echinocandins exhibit concentration-dependent efficacy in animal models of mycosis (Winderhold et al, ICAAC 2003; Andes et al, AAC 2003). We sought to determine the safety and efficacy of high-dose caspofungin (HD-CAS) therapy in cancer patients with invasive fungal infections (IFIs).
Methods: We retrospectively evaluated patients during 2002–2004 who had received HD-CAS (100 mg daily) after obtaining IRB approval. All values are given in median ± s.d.
Results: Age was 46 ± 18 years, 9 (41%) were men, 10 (45%) were neutropenic and APACHE II score was 15 ± 5. All 22 patients (100%) had hematologic malignancies; 15 had leukemia. In 7 (32%) hematopoietic stem cell transplant recipients, 6 patients received allogeneic grafts and 3 (14%) had acute graft-versus-host disease. Fifteen patients (68%) had refractory cancer. Six (27%) were receiving substantial dose systemic corticosteroids (> 600 mg equivalent prednisone dose) during antifungal therapy. The range of cumulative CAS dose was 300-4400 mg per patient and numbers of HD-CAS doses were 21 ± 17 (range, 3–60). Nine patients (41%) had definite IFIs, 6 (27%) sino-pulmonary infections (5 Aspergillus; 1 Scedosporium apiospermum) and 3 patients (14%) had disseminated disease (2 Fusarium and 1 Aspergillus fumigatus). In 13 patients (59%) with probable IFIs, 10 (45%) had fungal pneumonia and 3 (14%) with sino-pulmonary involvement. Twenty-one patients (95%) received HD-CAS in combination with another antifungal agent, 6 (27%) received HD-CAS upfront, whereas in 16 patients (72%) initial therapy included AmBisome, voriconazole, and conventional-dose CAS. The 12-week crude mortality was 41% and IFI-attributable deaths were 32%. Overall, HD-CAS was tolerated without serious adverse reactions; 2 patients (9%) developed fatal liver failure, which was deemed unrelated to HD-CAS.
Conclusions: In our high-risk patient population HD-CAS in combination with other antifungals was well tolerated and appears to have favorable impact on short-term mortality in patients with invasive mycosis.
Antibiotic and antibiotic resistance mechanisms
O344: Long-term effects of antibiotic administration on clonal stability and emergence and persistence of resistance genes in the intestinal microflora
S. Löfmark, C. Jernberg, C. Edlund (Stockholm, S)
Objectives: To study emergence and persistence of antibiotic resistance genes in the intestinal flora after antibiotic administration over a two-year period, and to monitor the stability of clonal selection and changes in the fingerprint patterns of the dominant members of the bacterial community. The commensal flora of the human intestine is a complex ecological system involved in host beneficial activities and disturbances of the microflora by antibiotic administration can lead to clinical implications. Exchange of resistance genes among the intestinal bacteria and bacteria passing through the colon might also be a serious threat to human health.
Methods: Four healthy subjects receiving clindamycin for seven days and four non-treated subjects were included in the study. Faecal samples collected at nine different time points prior to and during a two-year period following the antibiotic treatment were cultured for Bacteroides spp. strains. Twenty representative colonies were collected and phenotyped and tested for antimicrobial susceptibility to clindamycin, tetracycline and ampicillin according to NCCLS. Screening of specific resistance genes were performed by RealTime PCR. Resistance to the different antibiotics has shown to be connected and presence of tetQ, ermF, ermB, cepA and cfxA involved in these resistances were investigated. Specifically ermF and tetQ are common in the B. fragilis group and often reside on the same conjugative transposons. rep-PCR was used for clonal genotyping of the isolates and T-RFLP was used for fingerprinting of the total faecal bacterial community.
Results and Conclusion: Short-term administration of clindamycin resulted in major long-term ecological disturbances up to at least 24 months after administration. The trend showed a decline in species diversity, which did not return to pretreatment levels for up to 18 months after administration. An increased frequency of resistance to clindamycin and tetracycline and a long-term enrichment of resistance genes (ermF and tetQ) among Bacteroides spp. were seen in exposed subjects. A broad baseline variation of clonal stability and antibiotic resistance between subjects were observed in both groups. This fingerprinting pattern of the total bacterial community challenges the common view of the intestinal microflora as a stable environment.
O345: Prevalence of antibiotic resistance among commensal Escherichia coli from farm animals in the UK
V.I. Enne, M.D. Aguas, C. Cassar, K. Sprigings, P.M. Bennett (Bristol, Weybridge, UK)
Objectives: To determine the incidence of antibiotic resistance and expressed and silent resistance genes among commensal Escherichia coli from healthy farm animals.
Methods: 1798 E. coli were isolated from rectal swabs taken from pigs, sheep and cattle upon entry to the abattoir. Their susceptibility profiles to a panel of 16 antibiotics were determined by disc susceptibility testing. The prevalence of 11 resistance genes as well as the Class 1 integrase gene was determined among 615 of these isolates by PCR. Both resistant and susceptible isolates were screened to identify expressed as well as unexpressed resistance genes.
Results: The prevalence of antibiotic resistance among these isolates was low; only 9.1% of isolates were resistant to at least one agent. Of these, 5.2% were multi-resistant (defined as resistance to three or more agents of different classes). In terms of individual agents, resistance was 1.1% to apramycin, 2.4% to ampicillin, 0.1% to co-amoxiclav, 0.1% to cefoperazone, 1.2% to chloramphenicol, 3.5% to colistin, 1.6% to co-trimoxazole, 0.3% to furazolidone, 0.2% to gentamicin, 0.1% to nalidixic acid, 3.6% to neomycin, 4.3% to streptomycin, 4.6% to sulfonamide and 7.4% to tetracycline. There was no resistance to ceftazidime or amikacin. Of the ampicillin resistant isolates tested, 64.5% produced TEM type beta-lactamases, 19.4% produced OXA-2 type beta-lactamases and 0% produced SHV type beta-lactamases. Of the tetracycline resistant isolates tested 36.0% carried tetA and 73.0% carried tetB. Of the co-trimoxazole resistant isolates tested 12.5% carried dhfr17 or related genes and 16.7% carried dhfr12 or related genes. Of the streptomycin resistant isolates tested 62.0% carried the strAB gene pair and 53.5% carried aadA1 or related genes. Of the sulfonamide resistant isolates tested 27.4% carried sul1 and 71.0% carried sul2. 18.2% of isolates tested were positive for the for type1 integrase. We found five incidences of strains that were PCR positive for a given resistance gene but susceptible to the corresponding antibiotic. Further investigation by sequencing revealed that in each case either the promoter was absent or the gene was truncated.
Conclusion: The incidence of antibiotic resistance among commensal E. coli isolated from healthy farm animals is low. The resistance that does exist is due to a wide variety of resistance genes. The incidence of unexpressed resistance genes is low and generally due to lack of promoter activity.
O346: Growth of Pseudomonas aeruginosa in biofilms results in elevated mutation frequencies
K.L. Driffield, K. Miller, J.M. Bostock, I. Chopra (Leeds, UK)
Objectives: Pseudomonas aeruginosa colonises the lungs of cystic fibrosis (CF) patients forming biofilms that are difficult to eradicate due to intrinsic expression of resistance and rapid development of acquired resistance. P. aeruginosa with elevated mutation frequencies (MFs) have been isolated from the lungs of CF patients, but have yet to be isolated from non-CF patients. Hypermutators may arise during biofilm growth as a consequence of enhanced mutability in DNA repair genes leading to permanent hypermutator strains. To address this possibility we compared MFs of P. aeruginosa grown as planktonic cells and as biofilms. We also examined the effect of a methyl-directed mismatch repair (MMR) deficiency on MF.
Methods: MFs of planktonic P. aeruginosa PAO1 and PAOdelta mutS::Km, a MMR mutant, were determined by selecting mutants at 4xMIC rifampicin (rif) after incubation at 37°C for 48 h. Colony counts were expressed as a proportion of total viable cell numbers after incubation at 37°C for 24 h. P. aeruginosa biofilms were created using a modified Sorbarod model. Sorbarod filters were inoculated, perfused with media and maintained at 37°C for 72 h. Bacteria were harvested from the filter. MFs were determined as described.
Results: P. aeruginosa PAO1 and PAOdelta mutS::Km biofilm cultures showed significantly elevated MFs when compared to planktonic cells. RifR PAO1 were recovered from the biofilm at a frequency of 3.42 ± 2.02 × 10−8, and from planktonic cultures at 2.63 ± 1.76 × 10−9. PAOdelta mutS::Km showed an elevated MF when compared with PAO1. PAOdelta mutS::Km rifR mutants were recovered from the biofilm at a frequency of 1.00 ± 0.88 × 10−5 and from planktonic cultures at 3.54 ± 1.66 × 10−6.
Conculsion: P. aeruginosa may benefit from an increased mutation rate when confronted with the stressful situation of biofilm growth in the CF lung. The elevated MF of cells grown in the biofilm may give insight into the high occurrence of antibiotic resistant P. aeruginosa leading to treatment failure in CF patients. Increased mutability in biofilms may enhance the opportunity to derive permanent hypermutators through mutation in DNA repair genes. MF observed in planktonic culture of PAOdelta mutS::Km was further elevated in the biofilm suggesting that in addition to mutS activity, expression of other mut genes may also influence mutability in the biofilm.
O347: Horizontal gene transfer as a cause of fluoroquinolone resistance in an invasive Streptococcus pyogenes isolate
M.W.R. Pletz, L. McGee, C. van Beneden, S. Petit, M. Barlow, K.P. Klugman (Atlanta, Hartford, USA)
Objectives: To date fluoroquinolone (FQ) resistance has been described only anecdotally in Streptococcus pyogenes. Similar to other streptococci, efflux and/or mutations in the topoisomerase type II enzymes seem to account for fluoroquinolone resistance in this species. Mutations can arise spontaneously or be transferred by intraspecies or interspecies recombination. We analyzed an invasive ciprofloxacin-resistant (MIC 8 mg/l) S. pyogenes isolate (emm-type 83) collected by the CDC's Active Bacterial Core surveillance programme to determine the mechanism through which it had become resistant.
Methods: Efflux was tested for by comparing ciprofloxacin MICs in the presence and absence of reserpine (10 mg/l). The quinolone resistance-determining regions (QRDR) of gyrA and parC were sequenced. For parC, phylogeny was constructed by the Bayesian method. Recombination was statistically confirmed by using the maximum chi-squared test.
Results: MICs were 8 mg/l for ciprofloxacin and 4 mg/l for levofloxacin. There was no evidence for an efflux pump. There was no mutation in gyrA and a S79F mutation was found in parC that is known to confer fluoroquinolone resistance. The parC nucleotide sequence of the isolate showed an increased diversity compared to the S. pyogenes reference strain, and there was a region of repeat nucleotide mismatches on both sides of the S79F mutation. Phylogenetic analysis of the parC sequence revealed homologies to the parC of S. dysgalactiae. Statistical analysis for recombination suggests interspecies recombination of at least 90bp sequence containing the S79F mutation with S. dysgalactiae.
Conclusion: Interspecies recombination as cause of FQ resistance has to date not been described for S. pyogenes. We have found an invasive isolate with evidence for the acquisition of FQ resistance from S. dysgalactiae.
O348: Evidence of allelic variants of MEF carried on Tn1207.3-like genetic elements in Streptococcus pyogenes
S. Malhotra-Kumar, F. Iannelli, C. Lammens, G. Pozzi, H. Goossens (Antwerp, B; Siena, I)
Background: The M phenotype in macrolide-resistant Streptococcus pyogenes is mediated by an efflux transport system of the ATP-binding cassette (ABC) superfamily, in which mef(A) encodes the transmembrane domains, and msr(D) (previously called mat(A)) the ATP-binding domains. Both genes are carried on the Tn1207.3 element that integrates at a specific site, the comEC coding region, in the S. pyogenes chromosome.
Methods: Two S. pyogenes (SP1 and SP2) isolated from wound and respiratory tract infections in Belgium were identified as macrolide-resistant and exhibited the M phenotype by the conventional disc-diffusion test. Primers consensus for mef(A)/(E) were developed. RFLP analysis was done using BamH1, HindIII, and NheI followed by double-strand sequencing to distinguish mef(A) from mef(E). Moreover, primers to detect the left and right junctions of Tn1207.3 in comEC were used. A DNA microarray containing oligonucleotides designed to target each of the 58 Orfs of Tn1207.3 was used to detect presence of Tn1207.3. Emm types and clonality were investigated by reverse line blotting and PFGE, respectively.
Results: The mef gene in SP1 and SP2 could be successfully detected by the consensus mef(A)/(E) primers. RFLP analysis proved inconclusive; a restriction pattern similar to mef(E) with BamH1 and HindIII, and one similar to mef(A) with NheI was observed for both isolates. Emm and PFGE typing found SP1 to belong to the emm4 serotype and SP2 to emm12 and both were clonally unrelated. Microarray analysis showed that only 19 out of 58 probes had reactivity with SP1 DNA. No reactivity was detected with SP2 DNA. DNA sequence analysis showed that the mef gene from SP1 and SP2 were different (91% homology at the nucleotide level), and were also different from the canonical mef(A) and mef(E) genes. Mef from SP1 showed 88% homology to mef(A) and 89% to mef(E). Mef from SP2 showed 90% homology to mef(A) and 95% to mef(E). In SP1, the Tn1207.3-like element was integrated in comEC.
Conclusions: We present here evidence of novel Tn1207.3-like genetic elements that carry allelic variants of mef in S. pyogenes. The complete sequence of these elements and their integration sites in S. pyogenes are currently under investigation.
O349: Antipneumococcal activity of telithromycin in comparison with other drugs in relation to the presence of different resistance genes
S. Stefani, M. Santagati, M. Mezzatesta, C. Cascone, G. Nicoletti (Catania, I)
Objectives: The antistreptococcal activity of telithromycin and 11 different comparators was evaluated in 26 multidrug resistant Streptococcus pneumoniae collected during 2002–2003 as part of the ongoing PROTEKT (Prospective Resistant Organism Tracking and Epidemiology for the Ketolide Telithromycin) Italian Surveillance Program. The strains were characterized for their susceptibility to antibiotics both at the phenotypic and genotypic levels; furthermore, the association of resistance genes and the mobile genetic elements that carry them was also evaluated.
Methods: MICs of antibacterials were performed by following NCCLS guidelines. The presence of erm(B), erm(A), mef(A) and tet(M) genes, as well as the mobile elements carrying them was determined using previously published methods1, 2, 3.
Results: The strains in this study were resistant to penicillin (MIC > 2 mg/l) in 19.2% of cases, resistant to tetracycline in 88.5%, to cotrimoxazole, cefuroxime and amoxicillin in 23.1% while only telithromycin retained 100% activity against all microorganisms. A total of 88.5% of isolates were co-resistant to all macrolides and to tetracycline, 23% were co-resistant to all macrolides, to tetracycline and to cotrimoxazole and 19.2% to macrolides, to tetracycline and to penicillin. All isolates showing MLSB phenotype of resistance possessed the erm(B) genes and in 71.9% of cases this gene was associated with tet(M). In these strains the resistance determinants were carried by the Tn-1545-type element. Isolates showing the M phenotype generally possessed mef(A) genes alone, carried by Tn-1207.1 and only in one isolate the class mef(A) was associated with tet(M) and carried by Tn-2009. Although genotypically diverse, strains included in the study carried erm(B) associated with tet(M) in the same ApaI fragment of different sizes.
Conclusion: Telithromycin is highly active against multidrug resistant Streptococcus pneumoniae carrying many genes responsible for resistance to different classes of antibiotics. Our study shows that erm(B) is the most frequent gene responsible for macrolide-resistance found in S. pneumoniae and this was always associated with tet(M) on the same Tn-1545–like element, while the association between mef(A) and tet(M) is carried by Tn-2009.
1. Cascone et al – MDR 2002; 8:129.
2. Doherty et al – AAC 2000; 44:2979.
3. Santagati et al – AAC 2000; 44:2585.
O350: Activity of cathelicidin peptides against Chlamydia spp.
R. Cevenini, M. Donati, K. Di Leo, M. Benincasa, F. Cavrini, S. Accardo, A. Moroni, R. Gennaro (Bologna, Trieste, I)
Objectives: To study the in vitro activity of six cathelicidin-derived peptides (Bac7, BMAP-28, SMAP-29, LL-37, PG-1, BMAP-27) against purified elementary bodies (EBs) of 25 Chlamydia strains.
Methods: Chlamydial strains were grown in LLC-KM2 cells and EBs purified by sucrose gradients. The cathelicidin peptides were synthesized by the solid phase method using Fmoc chemistry. After purification by reversed-phase HPLC the peptides were lyophilized and stored at 4°C. Peptides were twofold diluted in test tubes containing PBS and a total volume of 0.15 ml of a suspension of purified EBs in SPG medium was added to the tube. The suspensions were incubated at room temperature for 2 hours and inoculated onto LLC-MK2 cells. After incubation cell cultures were fixed and stained with fluorescein-conjugated monoclonal antibody reactive with the chlamydial specific genus antigen.
Results: A different sensitivity of chlamydiae to cathelicidin peptides was observed. C. trachomatis was the most sensitive of chlamydiae and SMAP-29 was the most active peptide. The treatment of C. trachomatis EBs with SMAP-29 reduced by over 50% the inclusion number of all the 10 strains tested, at a concentration of 10 μg/ml. BMAP-27, BMAP-28 and Bac7 displayed a similar activity at a concentration of 80 μg/ml. In contrast, LL-37 did not exert any inhibitory activity and PG-1 was only active against serotypes D, H and LGV2. C. pneumoniae strains (n° tested = 5) were sensitive only to SMAP-29 at a concentration of 10 μg/ml. Chlamydia strains of animal origin (n° tested = 10) were not susceptible to cathelicidins, with the exception of four strains of C. felis. Electron microscopy analysis of C. pneumoniae EBs treated with SMAP-29 showed striking morphological changes of EBs with the loss of their integrity, the appearance of amorphous and membranous material and empty vescicles.
Conclusions: Previous studies and the present one suggest that cathelicidin peptides have substantial in vitro activity against several microorganisms. Much remains to be done to evaluate their in vivo efficacy and safety, in particular with respect to their interaction with constituents of biological fluids. Therefore, studies in animal models of chlamydial infection are needed to prove whether they will parallel in vitro results.
O351: Evolution of the primate cathelicidin: effect of structural variations on modulating antimicrobial and cytotoxic activities
I. Zelezetsky, A. Pontillo, N. Antcheva, M. Boniotto, S. Crovella, A. Tossi (Trieste, I)
The growing number of antibiotic-resistant microbial strains and the appearance of new human pathogens require the development of novel antibiotics with different mechanism of action. Antimicrobial peptides (AMPs) are very promising candidates in this direction, as they kill target microbes rapidly, have broad activity spectra that can cover bacteria, fungi and some enveloped viruses, including the more serious antibiotic-resistant pathogens, while it is relatively difficult to select resistance against them in vitro. AMPs are an important component of the innate immune system, an ancient form of host defence, which is shared by effectively all multicellular organisms and provides a rapid first line of antimicrobial host defence.
Objectives: To determine the mechanisms of natural selection underlying variations in one of these peptides, the amphipathic, alpha-helical cathelicidin-derived LL-37 and its variants in numerous primates and to relate these variations to functional properties.
Methods: We have cloned, sequenced and investigated the evolutionary relationship of the genes for 22 LL-37 primate variants. Selected peptides have been synthesised using optimised solid phase peptide synthesis. We have then analysed and compared the capacity of the peptides to assume a helical structure in different salt and membrane mimicking conditions by circular dichroism spectroscopy. This structural data has then been correlated to biological activity in vitro.
Results: The tested peptides showed broad but differing medium- and salt-sensitive spectra of activity against Gram-positive and Gram-negative bacteria as well as fungi. Killing kinetics and membrane permeabilisation kinetics of reference Gram-positive and Gram-negative bacteria indicated that the mode of action may vary in a manner dependent on both structure and charge. Unlike other AMPs that act selectively on bacterial cells, LL-37 and its variants also exhibit structure dependent cytotoxic effects against mammalian cells.
Conclusion: The results suggest that the evolution of these peptides works to vary the charge, while conserving the amphipathic structure in a manner that markedly affects the capacity to aggregate under physiological conditions. This process appears to be subjected to positive selection, possibly caused by direct interaction of the peptides with specific pathogens or biotas, although the added role of the immune functions, such as signalling and chemotaxis, remains to be determined.
O352: GES-5, a novel variant of the extended-spectrum beta-lactamase GES-1 with an increased hydrolysis of aztreonam identified in a Pseudomonas aeruginosa clinical isolate in France
L. Poirel, L. Brinas, N. Fortineau, P. Nordmann (Le Kremlin Bicetre, F)
Objectives: Characterization of the expanded-spectrum beta-lactamase resistance determinant of a Pseudomonas aeruginosa clinical isolate recovered from a rectal swab of a patient hospitalized at the Bicêtre hospital, K.-Bicêtre (France) in March 2004. This strain was resistant to most beta-lactams except to imipenem.
Methods: Double disk synergy test performed with clavulanic acid-containing disks was used for detection of the extended-spectrum beta lactamase (ESBL). PCR experiments and cloning were used for identification of the corresponding gene.
Results: A blaGES-like gene was identified by PCR that was cloned in Escherichia coli. The beta-lactam susceptibility pattern of E. coli DH10B harboring recombinant plasmid (pDEJ/GES) showed resistance to expanded-spectrum cephalosporins and aztreonam. Amino acid sequence analysis revealed a novel GES variant, GES-5, that had a single amino acid change as compared to ESBL GES-1, differing by a Gly to Ser substitution in position Ambler 242. Kinetic measurements revealed that GES-5 hydrolyzed penicillins and cephalosporins at a higher level than GES-1. In addition, GES-5 hydrolyzed aztreonam at a higher level than the other GES-type enzymes. GES-5 activity was inhibited by clavulanic acid and tazobactam but also by imipenem. The blaGES-5 gene was located in a class 1 integron together with an aacA4 gene cassette, both cassettes being separated by an ISPa21 insertion sequence element.
O353: Comparative minimal inhibitory concentration and mutant prevention concentration of moxifloxacin against clinical isolates of penicillin susceptible, intermediate and resistant Streptococcus pneumoniae
J. Blondeau, S. Borsos (Saskatoon, CAN)
Objective: Mxf is amongst the most potent of newer fluoroquinolones (FQ) against SP. Previous MIC testing has shown an MIC90 of 0.25 μg/ml and an MPC90 of 1 μg/ml. Concern over the possible escalation of FQ resistant SP prompted us to evaluate MIC and MPC values for Mxf on a large number of SP isolates collected prior to and after the introduction of the drug into clinical use.
Methods: A total of 454 clinical isolates collected between 1994–2003 were used: 365 PS, 76 PI, 13 PR. MIC testing was by microbroth dilution in accordance with NCCLS guidelines. For MPC testing, 10 billion organisms were applied to agar plates containing drug and incubated for 24 and 48 hours. The lowest drug concentration preventing growth was the MPC.
Results: Against PSSP isolates (susceptibility μg/ml), MIC50/90, range and MPC50/90, range were as follows: 0.125/0.25, 0.031–4 and 0.5/1, 0.05–8; PI 0.125/0.25, ≤0.031–4 and 0.5/1, 0.25—≥8; PR 0.031/0.05, 0.31–0.5 and 0.5/1, 0.05–1. Only 1/454 (0.2%) strains had an MIC ≥2 μg/ml and 8/454 (1.7% had MPC > 2 μg/ml). No difference in the MIC or MPC drug inhibition distributions were seen against PS, PI or PR strains nor were there any changes in these distributions over time. Modal MIC and MPC values were constant. Greater than 99% of strains by MIC were inhibited by ≤1 μg/ml compared to 95% by MPC and 98% by ≤2 μg/ml.
Conclusion: Mxf has enhanced in vitro activity against SP by both MIC and MPC measurements. Penicillin susceptibility of SP does not effect Mxf activity. No change in MIC nor MPC values of SP isolates collected prior to after release of the drug were seen. These studies confirm Mxf to be highly active in vitro and use of this compound does not appear to select for FQ resistance. This observation has long term implications for the use of FQs for treating SP infections.
Infections in the community: epidemiology, diagnosis and outcome
O354: Evaluation of 4 serological tests for the detection of Mycoplasma pneumoniae in patients with lower respiratory tract infections
K. Loens, D. Ursi, L. Daniëls, H. Goossens, M. Ieven (Edegem, B)
Objectives: Serology and PCR are widely used for diagnosis of M. pneumoniae (MP) in respiratory tract infections, but studies comparing the different methods are rare. The aim of this study was to evaluate PCR, NASBA and 4 different IgM and IgG EIA assays for the detection of MP in patients with lower respiratory tract infections.
Methods: 205 paired sera from 224 patients with CAP and 10 paired sera from 20 MP PCR positive patients without CAP were available. From 29 patients only an acute phase serum sample was available. Four different EIA's were evaluated: ImmunoWell IgG and IgM EIA (Genbio); Medac IgM, and IgG EIA (Medac); AniLabsystems IgM and IgG EIA (Biomedical Diagnostics); and Euroimmun IgM, and IgG EIA (Biognost). PCR and NASBA were applied to respiratory specimens. An expanded gold standard was used to calculate the sensitivities and specificities of all tests: 1) positive by PCR and NASBA or 2) positive by 1 amplification test and at least one serological test (either IgM or a seroconversion or significant rise of IgG antibodies), or 3) a seroconversion or a significant rise of IgG antibodies in at least two different EIA's.
Results: 39 patients met the criteria of the expanded gold standard. The sensitivities of the EIA's ranged from 10%–31% for IgM in the acute phase serum and from 19%–42% for IgM in the convalescent serum. IgG seroconversion or a significant rise in titre ranged from 41%–68%. Higher sensitivities were obtained for PCR and NASBA: 82% and 72%, respectively. The specificities ranged from 81%–99% for IgM in the acute phase serum, from 82%–99.5% for IgM in the convalescent phase serum, and from 95%–99% for IgG. The calculated specificities of PCR and NASBA were 98% and 97%, respectively. The MP IgM assay with the best combined values for sensitivity and specificity was the AniLabsystems EIA. The best MP IgG assay was the Medac EIA. MP PCR and NASBA positive patients had usually higher rises in IgG titre than MP PCR and NASBA negative patients. False positive IgM results occurred most frequently with the Immunowell assay.
Conclusion: Evaluation of the 4 EIA's and 2 independent amplification tests for MP showed substantial differences between the performances of the assays. Amplification methods are the most sensitive tests to diagnose an acute MP infection. IgM antibodies are of limited value. IgG serology has usually a moderate sensitivity but results in late diagnosis.
O355: Comparison of real-time PCR and conventional methods to determine aetiology of community-acquired pneumonia
K.E. Templeton, S.A. Scheltina, W.C.J.F.M. van den Eeden, A.W. Graffelman, P.H. van den Broek, E.C.J. Claas (Leiden, NL)
Objectives: To compare conventional microbiological methods, including serology and culture, with real-time PCR for diagnosis of 12 respiratory viruses and Mycoplasma pneumonia, Legionella Spp and Chlamydophila Spp (atypical bacteria) in patients with community-acquired pneumonia (CAP) and to assess the use of real-time PCR for microbiological diagnosis in patients with CAP.
Methods: Conventional techniques and multiplex real-time PCR for atypical bacteria and respiratory viruses were performed and compared on samples collected from 105 adults enrolled in a prospective study in a defined geographical area. All patients had an infiltrate on chest radiograph and a pneumoniae severity index (PSI) score was obtained at admission.
Results: Microbiological diagnosis was obtained in 52/105 (50%) patients by conventional techniques and in 80/105 (76%) by real-time PCR. Results could be obtained in one working day using real-time PCR whereas 2–3 weeks was required for serological diagnosis. Respiratory viral infections were detected in 15/105 (14.2%) of the infections by conventional methods but in 59/105 (56.2%) by real-time PCR methodology. Mixed infections were seen in 28/105 (26.6%) when real-time PCR was performed compared to 3/105 (2.8%) with conventional methods. The presence of a mixed infection by real-time PCR was significantly associated with severe pneumoniae (p = 0.002). Human rhinoviruses and coronaviruses, OC43 and 229E were frequently identified pathogens in mixed infections but were also identified in 4 cases of severe pneumonia as the only microbiological pathogen.
Conclusions: The real-time PCR assays enabled sensitive diagnosis for the main viral and atypical bacteria in comparison to conventional methods in a way that clinically relevant results can be obtained. The presence of mixed infections may be important in the severity of pneumonia.
O356: Comparative study of Legionella pneumophila pneumonia according to sporadic and outbreak presentation
N. Sopena, L. Force, M.L. Pedro-Botet, P. Barrufet, G. Sauca, M. García-Nuñez, G. Tolchinsky, J.A. Capdevila, M. Sabrià (Badalona, Mataró, E)
Objective: To compare the risk factors, the clinical presentation and the outcome of community acquired pneumonia (CAP) caused by Legionella pneumophila (LP), according to sporadic and outbreak presentation.
Methods: We included 138 patients with sporadic LP pneumonia diagnosed from 1996 to 2004 and 113 patients from an outbreak occurring in 2002, attended in two hospitals in Catalonia (Spain). Data about epidemiological and clinical features, blood chemistry values, radiological findings and outcome were analyzed by univariate analysis.
Results: The following variables achieved significance on univariate analysis (p < 0.05). Sporadic cases were more frequently male (81.8 vs. 64.6%), had a higher frequency of chronic lung disease (19.6% vs. 9.7%), HIV infection (11.6% vs. 1.8%) and corticoid therapy (5.8% vs. 0%), and had also more frequently cough (70.3% vs. 51.8%), expectoration (39.1% vs. 14%), thoracic pain (23,2% vs. 12,6%), dyspnea (45.3% vs. 28.6%) and confusion (16.7% vs. 7.5%) on presentation, while headache (56.5% vs.23.6%) prevailed in outbreak cases. Concerning blood chemistry, Na < 130/mm3 (21.3% vs. 6.7%), AST (48.8% vs.31.3%) elevation, BUN × 13 mmol/l (14.6% vs. 2%) and pO2 <60 mmHg were more frequently observed in sporadic cases. FINE severity index III (56.4% vs. 41%), ICU admission (16.1% vs. 4.4%) and complications (54.3% vs.32.7%), mainly respiratory failure, were more frequent in sporadic cases. There were no differences in the delay and the rate of appropriate treatment. The mortality related to LP pneumonia was higher in sporadic cases (6.3% vs. 1.8%), although this variable did not achieve statistical significance on univariate analysis.
Conclusion: Sporadic cases had a higher frequency of some underlying diseases, such as chronic pulmonary diseases and HIV infection, and corticoid therapy. Respiratory symptoms at clinical presentation, confusion and blood chemistry alterations, such as hyponatremia, AST and BUN elevation were more frequent in sporadic cases, while headache prevailed in outbreak cases. Sporadic cases were more severe and had a worse outcome than outbreak cases.
O357: CURB65 outperforms generic severity assessment tools in stratifying and predicting 30-day mortality in community-acquired pneumonia
G.D. Barlow, D. Nathwani, P.G. Davey (Hull, Dundee, UK)
Objectives: Severity assessment is the key determinant of management strategy in community-acquired pneumonia (CAP). Lim et al recently developed CURB65, which divides patients into 3 groups based on 5 prognostic indicators. There is evidence that hospital medical staff, however, have suboptimal knowledge about assessing severity in CAP. Potentially this could be improved by using a generic rather than the disease specific tools currently used in acute medicine. This study assessed the performance of two generic tools, the Scottish Early Warning System (SEWS) and the Systemic Inflammatory Response Syndrome (SIRS), with CURB65 in CAP.
Methods: As part of a quality improvement programme, data were collected prospectively over two winters (November–April 2001 and 2002). Prognostic indicators were recorded at admission and a severity score assigned for each of the tools. Mortality was assessed at 30 days. For each tool, sensitivity, specificity, positive predictive value (PPV) and negative predictive value were calculated and a receiver-operating curve (ROC) produced.
Results: Full prognostic data were available on 435 (CURB65), 426 (SEWS) and 439 (SIRS) patients. 30-day mortality for CURB65 scores of 0–1 (home therapy), 2 (non-severe, but manage in hospital) and 3 or more (severe) was 2%, 16% and 35%. Mortality for SEWS scores of 0–1 (routine observations), 2–3 (hourly observations) and 4 or more (doctor review within 30 mins.) was 9%, 17% and 27%. Mortality for patients with 0–4 SIRS criteria was 0 = 13%, 1 = 20%, 2 = 20%, 3 = 21% and 4 = 6%. Adding a severe sepsis stratification to the SIRS criteria was not useful as some patients without sepsis (SIRS 0–1) appear to have organ dysfunction/hypoperfusion; these patients have high mortality. Sensitivity and specificity for severe versus non-severe illness (defined as a CURB65 score of 3 or more, a SEWS score of 4 or more and two or more SIRS criteria) for each of the rules were 71% and 70% (CURB65), 52% and 67% (SEWS), and 74% and 31% (SIRS). The ROC is shown below.
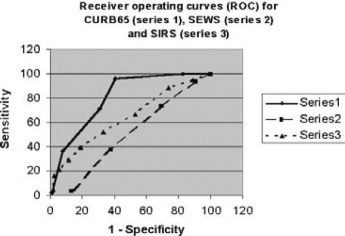
Conclusion: SIRS criteria on admission did not adequately stratify mortality in CAP. SEWS did stratify mortality (from 9% to 27%), but failed to identify a low risk group; it may be useful in guiding management in hospitalised patients. CURB65 outperformed SIRS and SEWS and had higher sensitivity/specificity when delineating severe from non-severe illness. It would be interesting to investigate the performance of CURB65 as a generic severity tool.
O358: Molecular and clinical characteristics of invasive Group A streptococcal infections in Sweden
J. Darenberg, B. Luca, C. Schalen, A. Jasir, V. Romaus, A. Norrby-Teglund, B. Henriques Normark (Solna, Lund, Stockholm, S)
Objectives: To investigate the epidemiology, molecular epidemiology and clinical characteristics of invasive Group A Streptococcal (GAS) disease, and to compare invasive and non-invasive isolates.
Methods: Invasive GAS isolates were sent to SMI from the Swedish microbiological laboratories between April 2002 and December 2004. Also, during 18 months 10 non-invasive isolates were collected each month at 6 of the laboratories. Questionnaires for clinical and epidemiological data were sent to the responsible MD for each patient with invasive disease. All isolates were characterized with respect to T-type, emm-sequence type, gene detection for 9 superantigens and antibiotic susceptibility. The clonal relationship within subgroups of isolates was investigated with PFGE and MLST.
Results and Conclusions: Until November 2004 we received 675 invasive isolates and 548 (81%) returned questionnaires. So far 70% of the patients had underlying chronic diseases, predisposing factors or drug abuse. 60% of patients were reported to have skin as site of entry of infection, 16% the respiratory tract, and 7% had a puerperal or genital infection. 12% of patients had no identified focus. Further, 13% of patients developed streptococcal toxic shock syndrome (STSS) and 40% of these patients died. The over all mortality was 14%. When looking at the outcome of STSS patients receiving IVIG as compared to those who did not, a significant difference was seen in survival in favour of the treatment (p = 0.0122), which is in agreement with our previous studies. The most common T-type in Sweden during this period was the T3/13/B3264 cluster that accounted for about 34% of invasive isolates and 20% of controls (isolated from patients with skin- or throat infections). Resistance to MLS antibiotics was rare (0.2%) whereas a high rate of tetracycline resistance (33%) was observed.
Acknowledgement: The study was supported by the European Commission.
O359: Modification of basic epidemiological characteristics of hepatitis A, from a food- and waterborne disease to a predominant sexually-transmitted disorder. An emerging matter of public health
R. Manfredi, L. Calza, F. Chiodo (Bologna, I)
Introduction: Hepatitis A virus is transmitted through oral-fecal contact, including exposure to water or food contaminated with stools of infected patients (p). Recent outbreaks of hepatitis A were observed world-wide, with special attention on homosexual men, but also illicit drug users.
Patients and Methods: An prospective observational survey of all admissions due to hepatitis A occurred in our metropolitan area and was carried out from 1999 to October, 2004.
Results: 132 consecutive p were hospitalized in the examined period. Since October 2002, acute hepatitis A largely prevailed over acute HBV, HCV and HEV hepatitis. Adult female p and children represented only 19 cumulative patients out of 132 (14.4%). The temporal trend of male adults admitted for hepatitis A showed a significant increase from 1999 to the first 10 months of 2004: a ∼300% increase vs 1999, leading to a crude rate of 7.8 per 100.000 residents per year). Among the 132 p diagnosed with hepatitis A, the prevalence of immigrants had a temporal increase from 1–3 cases/year from 1999 to 2001, up to 20 cases in the 22 months from 2003 to June 2004 (p < 0.03). Even 113 p of 132 (85.6%) were represented by male adults aged 22–44 years, who recognized unprotected homo-bisexuals contacts in the 2 months preceding the onset of hepatitis A in 89 cases (78.8%). Nobody reported contacts with p with a recently diagnosed hepatitis A and nobody underwent specific anti-HAV vaccination. Among the 113 adult males with HAV, concurrent STD were seen in 35 p (p < 0.004) including chronic hepatitis B in 6 cases, hepatitis C in 14, syphilis in 7 and HIV in 12 patients.
Discussion: Despite the availability of anti-HAV vaccination and information campaigns aimed against the spread of HIV and STD in general, the continued spread of hepatitis A clearly recognize an increased prevalence of homo-bisexual transmission. Our experience shows a strict link between novel diagnoses of acute HAV infection and homo-bisexual behavior which remained unchanged in proportion since 1999, but showed a significant increase of absolute number of detected cases from late 2002 until now. A careful report and monitoring, specifical educational campaigns, and enforced public health measures (such as recommendation of anti-HAV immunoprophylaxis for p at risk), are expected to contain the rising outbreak of hepatitis A among homo-bisexual men in our community and concurrently stop the spread of other common and potentially severe STD such as HIV, hepatitis B and C, and syphilis.
O360: Candidaemia in the elderly
P. Sandven, L. Bevanger, A. Digranes, H.H. Haukland, T. Mannsåker, P. Gaustad (Oslo, Trondheim, Bergen, Tromsø, N)
Objectives: A prospective nationwide candidemia study has been ongoing in Norway since 1991. Population-based surveillance studies makes comparisons of incidence and species distribution in various age groups possible. This report provides a description of the epidemiological characteristics of candidemia in the elderly.
Methods: Yeast blood culture isolates in all microbiological laboratories in Norway (population 4.5 mill) have been recorded prospectively. Isolates have been sent to the national mycology reference laboratory for identification and susceptibility testing.
Results: For the period 1991–2003 a total of 1400 candidemia episodes were diagnosed in Norway. The total number of yeast strains recovered were 1421 (21 patients with 2 species). The overall candidemia incidence was 2.5 per 100000 inhabitants. The annual incidence in patients aged ≥80 years is especially high and has increased markedly the last 3 years compared to patients in younger age groups (Table 1). The species distribution is also different in the old age group. The percentage of C. glabrata isolates was 5% the age group <50 years, 13% in patients aged 50–79 years and 31% in patients ≥80 years.
Table 1.
Annual incidence of candidenia in patients aged => 50 years. Norway 1991–2003
 |
Conclusion: In Norway both the candidemia incidence and species distribution is markedly different in old patients (≥80 years) compared to younger aged groups. This finding has important therapeutic implications.
O361: Infections in nonagenarians
M. Hemmersbach-Miller, A. Conde Martel, J. Ruiz Hernández, J. Arencibia Borrego, M.A. Cárdenes Santana, P. Betancor León (Las Palmas de Gran Canaria, E)
Objective: Perform a study of infections in nonagenarians in an Internal Medicine Department of a third level hospital, focusing on prior conditions, specific laboratory abnormalities, mean stay and mortality in the hospital.
Methods: 400 consecutive nonagenarians admitted during a 5 year period in an Internal Medicine Department were included. Specific prior conditions, laboratory values (WBC, lymphocytes, hemoglobin, creatinine, glycaemia, albumin and lipids), site of infection, Charlsons co-morbidity index and outcome (mean hospital stay, intra-hospital mortality, place of discharge) were recorded. The variables of the group with an infectious condition were compared with the group that was hospitalised for any other reason. Chi Square test, Student's t-test and the Mann-Whitney U test were used for statistical analysis.
Results: Out of the 400 nonagenarians (148 males, 252 females), with a mean age of 92.5 years, 245 (61.3%) presented with some kind of infection. Prior conditions related to infections were exclusively dementia (p = 0.001) and cognitive impairment (p < 0.001). Hemoglobin, creatinine and glycaemia did not differ between both groups. Total WBC was significantly higher (12,917 vs 10,019; p < 0.001), albumin significantly lower (2.7 vs 3.4 g/dl; p = 0.003) as well as total cholesterol (151.3 vs 162.6 mg/dl; p = 0.012). Sites of infection: urinary tract (24.5%;98), pneumonia (22%;88), respiratory tract infection (18.5%;74), sepsis (4.8%;19), abdominal infection (2%;8), gastroenteritis (1.5%;6), meningitis (0.8%;3). No relation with Charlsons co-morbidity index was observed. Mean hospital stay did not differ between both groups (10.6d vs 11.3d in infections; p = 0.7). Intra-hospital mortality was significantly higher in patients with an infectious condition (27.9% vs 15.6%:p = 0.005). Those who survived were discharged more frequently to other hospital facilities than back home (14.3% vs 7.1%; p = 0.028).
Conclusion: Dementia and cognitive impairment are conditions related to a higher incidence of infections in nonagenarians. The most frequent site of infection in hospitalized nonagenarians is the urinary tract (24.5%), followed by pneumonia (22%) and respiratory tract infection (18.5%). Laboratory values do not differ from those already known to be acute phase reactants, such as elevated WBC and a low albumin level. Intra-hospital mortality is significantly higher in nonagenarians presenting with an infectious condition.
O362: High incidence of intravascular infection in zoonotic nontyphoid Salmonella bacteraemia in elderly patients
H. Nielsen, K.O. Gradel, H.C. Schønheyder (Aalborg, DK)
Objectives: Bacteremia and invasive disease with zoonotic nontyphoid Salmonella spp. are well known to occur in subjects with co-morbidity. Especially, aortitis and endocarditis are described in patients with arteriosclerosis and aortic aneurysms. However, the incidence of these complications and the age-dependency are not well established.
Methods: We recorded all cases of bacteremias with nontyphoid Salmonella in North Jutland County, Denmark, for a 10-year period, 1994–2003. Data sources were medical records, the Bacteremia Research Database, the Hospital Discharge Registry, and the Central Population Registry, all linked by the unique Danish personal identification number. Cases with secondary intravascular focal infection were analysed.
Results: A total of 109 patients with nontyphoid Salmonella bacteraemia was identified, and 77 of these were > 50 years old. In this age group, seven patients (9%) had an intravascular Salmonella focus, five with mycotic aorta aneurysm, and two patients had endocarditis. We detected S. enteritidis in 3 cases, S. typhimurium in 2 cases, S. dublin in 1 case and S. sandiego in 1 case, which is not different from the overall bacteraemia species distribution. As North Jutland County had a 10-year cumulated population of 1,665,094 subjects >50 years, the population-incidence was 0.04/100,000 person-years. Mortality was 1 out of 7 within 30-days and 3 out of 7 within 180-days after detection of bacteraemia. Four patients were long-term survivors.
Conclusions: In elderly patients >50 years a high percentage of zoonotic nontyphoid Salmonella bacteraemia cases has secondary intravascular focal infections, which requires special treatment. Clinical examinations for a secondary intravascular focus are recommended in this age group.
O363: First pan-European epidemiological and microbiological surveillance programme for severe S. pyogenes disease
A. Jasir, C. Schalen on behalf of Strep-EURO study group
Objectives: The project Strep-EURO started by September 2002 to improve understanding of severe group A streptococcal (GAS) disease in Europe and achieve an integrated picture of these infections.
Methods: An European case definition was agreed upon amongst participants and a clinical questionnaire containing background identification data was used. Enhanced surveillance of GAS invasive disease commenced on 1 January 2003 for a two years period. Collected isolates were characterized by both serological T, OF and M typing and more advanced molecular methods e.g. emm-sequencing, PFGE and MLST. Strains were screened for antibiotic susceptibility and MIC was determined by E-test. For standardization of methods and detection of possible errors two sets of EQA strains for antibiotic susceptibility and one set for typing were sent to all centres. Data file specification for collection of patient and microbiological data was developed and each partner submitted their results to a central database in Finland.
Results: By July 2004 over 5000 invasive GAS isolates were collected. The population based incidence for year 2003 varied between countries from 0.1 to 3.8 per 100,000 inh. The type distribution of GAS also varied markedly. In a few countries types 1, 3 and 28 were predominant; however, an overall increase of new invasive types was noticeable. A high level of MLS antibiotic resistance in some countries (France, Italy) and very frequent tetracycline resistance in almost all countries was noted.
Conclusion: The Strep-EURO project created a European network for epidemiological analysis and surveillance of severe streptococcal disease in ten EU and one Associated Countries. We expected 1,000 cases/year to be found but after 18 mounts over 5,000 were reported. The overall increase of invasive cases partly depend on the role of Strep-EURO in establishment of a new surveillance system and development of an European network. Any defined conclusion has to wait until the data are carefully analysed. Report on increasing frequency of unusual emm types is a concern. There is also a need of studying the background of increasing tetracycline resistance despite lack of use of this drug for treatment of streptococcal diseases.
Acknowledgment: The Strep-EURO project is funded by the European Commission.
Metallo-beta-lactamases: a last frontier for beta-lactams?
K371: Metallo-beta-lactamases: a last frontier for beta-lactams?
G.M. Rossolini, J.D. Docquier (Siena, I)
Beta-lactams remain a cornerstone for antimicrobial chemotherapy of a large number of bacterial infections, but their efficacy has been increasingly thwarted by dissemination of acquired resistance determinants among pathogenic bacteria. Metallo-beta-lactamases (MBLs) are a family of beta-lactam-degrading enzymes present in some environmental species, that only recently have emerged as resistance determinants of notable clinical importance. Their overall impact is still lower than that of serine-beta-lactamases, but during the last decade at least 4 different types of MBLs (IMP, VIM, SPM and GIM), encoded by genes associated to mobile DNA, have been recruited from unknown genomes into major gram-negative pathogens, including members of the family Enterobacteriaceae, Pseudomonas aeruginosa, Acinetobacter spp. and other nonfastidious gram-negative nonfermenters. These acquired MBLs, of which some are already distributed on a world-wide scale, represent a formidable challenge to antimicrobial chemotherapy due to their extremely broad substrate specificity and mechanistic uniqueness: most beta-lactams (including carbapenems and expanded-spectrum cephalosporins) are efficiently degraded by these enzymes, while conventional beta-lactamase inactivators, such as clavulanate, sulbactam and tazobactam, are useless against them. MBLs exhibit a remarkable structural plasticity and it remains unclear whether they share a common reaction mechanism: this explains, at least in part, the difficulties encountered in finding broad-spectrum inhibitors and underlines the importance of comparative studies aimed at the identification of relevant molecular targets for inhibition. Several important issues concerning MBLs remain open: epidemiological distribution/magnitude of the problem, laboratory diagnosis, clinical significance in different settings, spreading mechanisms, original sources and evolutionary history, structure-function relationships and catalytic mechanism. The scope of this presentation will be to discuss over recent advances on open issues, and how they are likely to contribute to combating resistance mediated by MBLs, which are now considered among the most worrysome emerging resistance determinants in gram-negative pathogens.
Acknowledgements: The work on MBLs in our laboratory is supported by grants from the European Commission (HPRN-CT-2002-00264, LSHM-CT-2003-503335) and from the Italian Ministry of Education and University (MIUR-COFIN 2001068755_003).
Social-political consequences of the HIV pandemic: are we turning the tide?
K372: Social-political consequences of the HIV pandemic: are we turning the tide?
L. Kallings (UN Secretary-General's Special Envoy for AIDS)
The enormous size of the HIV/AIDS pandemic and its devastating social and economic consequences have made it a geopolitical threat of prime importance to the world and placed it on the agenda of the UN Security Council and the General Assembly. According to the Millennium Goal further spread of HIV should be stopped by 2015. Is this a realistic goal? The odds to succeed within such a limited period of time do not seem favourable as we after 20 years still are in the beginning of the pandemic which is in a dynamic phase spreading to populous regions such as India, China and the former Soviet Union. The pandemic is continuing unabated with some five million new infections and three million fatal cases per year. Forty million are currently living with HIV/AIDS in the world and 30 million have already died. Another 45 million is predicted to be HIV infected within the next ten years. It is easy to be paralysed by the sheer numbers. However, mankind can mobilise immense resources once the awareness and political will are present. That has unfortunately not happened yet on a scale which is commensurate to the threat. It is true that more political leaders now are talking about AIDS than before and that considerably more funding has been made available but it is far from enough to make a difference. The fight against AIDS is hampered by many obstacles of social and cultural nature that is embedded in human behaviour. Sexually transmitted infections are notoriously difficult to control. Syphilis is still rampant in many parts of the world after 500 years and in spite of efficient and inexpensive treatment since long. The subordinated status of women, particularly in developing countries, is at the root of the difficulties to control the spread of HIV. The infidelity of husbands and their refusal to use condoms are putting married women at a particularly high risk. It will take long time to influence male attitudes and to change laws, e.g. to empowering women to inherit properties and to make independent decisions in order to be economically emancipated and to be able to say no to unwanted sex. The proportion of women among people newly infected is increasing each year; fifty per cent of all infected persons in the world are women, in Africa it is sixty percent. The nature of the causative agent makes the AIDS epidemic uniquely difficult to control. The retrovirus attacks and resides in the immune system and hides in cellular sanctuaries. It has an extreme ability to mutate to avoid immune control and to develop resistance to antiretroviral drugs. Furthermore, HIV is transmitted vertically. What can we do against this formidable enemy? The introduction of efficient antiretroviral treatment was a revolutionary achievement but will not stop the HIV epidemic. In 2004 about 35,000 new HIV infections occurred in Western Europe and 45,000 occurred in North America in spite of the wide use of antiretroviral treatment since many years. To which extent antiretroviral treatment will be made available in a sustained way in developing countries is still an open question. Hopefully, prevention and treatment will work hand in hand. A cure is not yet at sight. We do not know if it is possible to develop an effective vaccine but we keep hoping so. However, in spite of the long list of difficulties there are some progresses as in several East African countries; the most heralded is the example from Uganda with the decline of HIV prevalence in pregnant women from 30 to 5 per cent (!) through sustained behaviour change. Prevention of mother-to-child transmission is another success – where it has been introduced.
Evolution and function of the haemagglutinin of the influenza virus
K374: Evolution and function of haemagglutinins of influenza viruses
J. Skehel (Mill Hill, UK)
Comparison of the structures of haemagglutinins representative of the four influenza clades suggests that aspects of haemagglutinin stability and activation for membrane fusion may be involved in clade formation. The structural details on which this possibility is based will be described in relation to irreversible changes in structure that are known to be required for membrane fusion activity and that can result from thermal inactivation.
Streptococcus pneumoniae: a clonal war?
S375: The role of pneumococcal factors in virulence and carriage
T.J. Mitchell (Glasgow, UK)
Streptococcus pneumoniae is a major pathogen of man, causing diseases such as pneumonia and meningitis. The mechanisms by which this organism causes disease are still unclear but certainly involve over-activation of inflammatory pathways. The organism produces a range of factors that may be involved in the pathogenesis of infection. These include a toxin (pneumolysin) as well as a range of surface proteins and enzymes. The polysaccharide capsule is essential for virulence of the organism. The availability of genome sequences of several strains of pneumococcus has allowed the identification of putative virulence factors and regulatory pathways. Use of this information in conjunction with in vitro systems and animal models allows the study of the role of these factors in disease. I will describe data we have on the role of surface proteins, the toxin pneumolysin and the heat shock protein HtrA in the virulence of Streptococcus pneumoniae. Pneumolysin is a major virulence factor of the organism and induces inflammation in the lung. Very small amounts of the toxin are able to induce inflammatory cytokine production. Surface proteins such as pneumococcal surface protien C (PspC) play a role in both attachment and interaction of the organism with the immune system. I will describe the use of genetically defined mutants of the pneumcooccus lacking PspC in animal models of infection. These studies show that the role of PspC in the disease process is different for different strains of the organism. HtrA is a heat shock protein of the pneumococcus and is probably acts as both a chaperone and protease to control protein folding and degrade misfolded proteins. We have shown that deletion of the gene for HtrA attenuates the pneumococcus in animal models of infection. This will allow us to investigate the possibility of using HtrA mutants as live vaccination vehicles. Several strains of the pneumococcus have have been subjected to total genome sequencing. Availability of these genome sequence allows the construction of microarrays and I will describe our use of these chips to study regulatory pathways in the pneumococcus. Analysis of gene expression in different serotypes of the pneumococcus suggests that there may be serotype specific regulatory pathways within the organism. This has implications for treatment and vaccination.
S376: Impact of conjugate vaccine on the epidemiology of Streptococcus pneumoniae
H. Peltola (Helsinki, FIN)
Pneumococci cause various diseases of which non-bacteremic or bacteremic pneumonia, bacteraemia with unidentified focus, true sepsis, meningitis, other focal infections, and otitis media especially in small children are the most important manifestations. There is no doubt that a functioning vaccination would be of great individual and societal relevance. For 30 years, a 23-valent vaccine has been available, but because of the inheritant problems of polysaccharide antigens, this product – as such good – left a room for a better immunogen. Hence, a 7-valent conjugate vaccine (7CV) was highly welcomed, when it arrived to the market a few years ago. The past few years have taught us the most important pros and cons of this vaccine. So far, data on the impact of 7CV have gathered only from vaccination of small children for whom a vaccine against acute otitis would be mostly welcomed. Unfortunately, more than one study has now showed that the effectiveness is, at most, meagre. A slightly better effect is observed in endpoints secondary to otitis (such as the need of tube insertion), but in this respect, children have not gained much of 7CV overall. Interestingly, the use of antimicrobials has sometimes declined by ±20% in settings where conjugate vaccine was used. On the other hand, replacement of the vaccine-type pneumococci by other serotypes in children's nasopharynx is documented. The clinical relevance of this finding is unsettled. The positive side of the coin is that 7CV indisputably prevents serious pneumococcal diseases, meningitis being the gravest manifestation. In developing countries, this information would be great news – should they afford this extremely costly vaccine. In the industrialized world these entities are, however, very rare. A recent analysis of invasive pneumococcal infections in the largest pediatric hospital of Finland (85 cases during 13 years) showed only meningitis – 1–2 cases a year – to be a meaningfully dangerous disease; all other manifestations were rather benign in which a short course of penicillin led to full recovery. Exceptions to this rule were rare. Because the cases were caused by 24 different serotypes, wide-scale use of 7CV would potentially have protected 57% of the cases, at maximum. Since the experience is similar in other industrialized countries, one has to put various demands in scales before 7CV is taken among the society-paid vaccines. For well-defined risk groups, and in private practice, 7CV should be readily available. The effect in the nasopharyngeal carriage of 7CV has brought a surprising benefit among elderly people in the USA among whom pneumococcal disease has declined by ±20%. This strong herd immunity effect is to be taken into account in future strategies. Since 7CV's high price is a critical issue, one has sought for a solution in reduction of vaccine doses. Australia has selected a 3-dose 7CV-schedule, and it is more than likely it will work. Another solution might be to trigger the T-cell response with 1–2 doses of 7CV, and to continue with polysaccharide vaccine. In theory, this approach would offer several major advantages.
Recent advances in chlamydiology
S379: Genomes of Chlamydiae
R.S. Stephens (Berkeley, USA)
The first genome sequence for Chlamydia was released in 1997 and this information abruptly altered existing paradigms of chlamydial biology. The wealth of information inferred from the chlamydial genome sequence has had a large and broad impact on the chlamydial research arena. There are now complete genomes for more than six different chlamydial species/biovariants and four genomes from different strains of C. pneumoniae. One of the conspicuous findings is that the three main phylogenetic groups, C. trachomatis, C. psittaci, and C. pneumoniae, have fundamentally identical gene content and gene order (synteny), although orthologous genes have low nucleotide identities. One point of reference is that genomes of different strains of Escherichia coli share only 40% of their gene content. The high level of genome identity for chlamydiae is even more remarkable in that these organisms cause diseases in numerous different host species and tissues. One can conclude that the high genome synteny reflects the paucity of acquisition of exogenous genes from other organisms and even a lack of within-organism recombination. Although these species have been separated for tens of millions of years and show their divergence by accumulation of point mutations, their biological relationships are extremely similar. All chlamydiae essentially share the same gene set, the same metabolic pathways, the same complex developmental cycle and the same mechanism for causing disease. Thus, time alone has not resulted in meaningful biological diversification at the genus level and this data is not consistent with proposals for a new genus separation for Chlamydia such as Chlamydophila.
S380: Chlamydia proteomes
S. Birkelund, G. Christiansen (Aarhus, DK)
Chlamydia are obligate intracellular gram negative bacteria, with an unique bi-phasic life cycle, in which extracellular infectious elementary bodies (EB) of 300 nm in diameter alternate with the intracellular replicating form, the reticulate bodies (RB), of 1000 nm in diameter. The extracellular EB attach to the cell surface where it mediates its uptake in a phagosome. During the intracellular stage Chlamydia grow inside the phagosome, the chalmydial inclusion, within the host cell cytoplasm. EB transform to RB that divide for 24–48 hours where after they reorganize into EB. At the end of the cycle the host cell burst and EB are liberated and can infect new cells. During the intracellular phase the chlamydiae are surrounded by the inclusion membrane. Chlamydia have small genomes of 1.04 mega basses (Mb) for C. trachomatis and 1.23 Mb for C. pneumoniae, and a coding capacity of 875 and 1073 proteins, respectively. Such numbers of proteins are well separated by 2-dimentional gel electrophoresis (2D-PAGE). Due to their bi-phasic life cycle we purified EB and RB from infected cells and in addition we purified the outer membrane complex of EB. These samples were separated by 2D-PAGE, and protein spots were identified by peptide mass fingerprinting. These systematic proteome maps have given an understanding of the protein composition in the EB, RB and COMC, the metabolic possibilities of EB, and an understanding of components that may be localized at the chlamydial surface. Chlamydia have gene homologs for bacterial type II, III, and IV secretion systems and can therefore secrete proteins into the inclusion membrane and into the host cell cytoplasm. Type II and IV secreted proteins do have a leader sequence and type IV secreted proteins have characteristic structural motifs, but not-secreted proteins can also show these characteristics. Type III secreted proteins have no known motifs so the only way to identify such proteins is by identifying them in the host cell cytoplasm or in the chlamydial inclusion membrane. We have used a proteomics approach to identify secreted proteins, comparing the proteins from the cytoplasm, inclusion membrane plus the RB/EB and finally comparing that to the proteoms of RB/EB. This lead to identification of proteins secreted to the host cell cytoplasm by both type II and type IV secretion. Our proteomics work have lead to an understanding of both structural components of the microorganism and its interaction with its host cell.
S381: Genital chlamydial infections are increasing: what can we do?
B. Herrmann (Uppsala, S)
Rates of genital chlamydia have been increasing for several years in Europe. In Sweden infection rates reached new record levels in 2004, with the sharpest rise in teenagers. This epidemic is expected to grow further in coming years. The continuing increase is not explained by the introduction of nucleic acid amplification tests. Increasing levels of sexual risk taking behaviour are a more likely explanation. Pioneering studies in Sweden showed that chlamydia can lead to severe sequelae. In some countries huge resources are being devoted to the opportunistic detection and treatment to prevent salpingitis, ectopic pregnancy and infertility, despite a lack of evidence of its effectiveness. Annual screening in specific age groups has been widely recommended, but this has not been accomplished in any country. In Sweden free testing and treatment, and widespread testing among women were introduced in the1980s. Concurrent declines in rates of chlamydia-associated sequelae were widely interpreted as being due to opportunistic screening. However, recent analysis of a large Swedish cohort of women, followed for up to 15 years, indicates that the efficiency of chlamydia screening was low. In most years only 5–10% of 15–24 year old women were screened and half of all women screened were only ever tested once. This cohort study also showed that the risk of reproductive complications was lower than previously thought. Contact tracing can be used to detect chlamydia, especially in asymptomatic men not reached by opportunistic screening. However, its efficiency is suboptimal even in Sweden, where contact tracing is mandatory. Improved outcomes have been observed when home-sampling kits are offered to male partners of infected women, and by designating professional contact tracers in a central location for cases detected in primary care and non-specialized clinics. In 2003 lymphogranuloma venereum entered the European arena. Outbreaks amongst men having sex with men, many of whom are HIV positive, have been reported from the Netherlands and now several other countries. The appearance of this neglected chlamydial infection highlights the need for effective and integrated surveillance systems in Europe. To conclude, current chlamydia control activities have not controlled the spread of chlamydia. Large-scale randomised trials to determine the most effective approach to chlamydia screening in both men and women and to contact tracing are urgently required, and the risk of sequelae must be better determined.
S382: Development of a chlamydia vaccine
G. Christiansen, S. Birkelund (Aarhus, DK)
Chlamydia are obligate intracellular bacteria with a bi-phasic developmental cycle. The two human pathogenic species are C. trachomatis and C. pneumoniae, C. trachomatis is a leading cause of sexually transmitted bacterial infections with severe sequelae as tubal factor infertility and ectopic pregnancy and infections can be asymptomatic. So far no vaccine has been developed but studies that may lead to the development of a highly warranted vaccine have been performed. The first attempt to vaccinate children with a whole cell vaccine resulted in initially protection but the protection was short-lived. In animal models whole cell vaccination resulted in hypersensitivity reactions and therefore new strategies were developed. The most immunogenic molecule is the major outer membrane protein (MOMP) and therefore this molecule has been studied in great details as a vaccine candidate in animal models. Even though complete protection was not obtained reduced shedding was observed and vaccine trials using naked DNA as a vaccine resulted in stimulation of both the humoral and cellular immune response indicating progress in the vaccine development. MOMP varies, however, between serovars that are causing genital infections and therefore additional components may be needed. C. pneumoniae is causing respiratory tract infections and is associated to the development of coronary heart disease. Antibodies to conformational surface exposed epitopes are generated upon infections but MOMP is not the major immunogen. A large family of proteins, the polymorphic membrane proteins (Pmp) consisting of 21 members of which most are expressed were found to be localized in the C. pneumoniae outer membrane. As the Pmps are highly expressed in the outer membranes of C. pneumoniae we investigated whether they are recognized by a cell-mediated immune response. A mouse model for lung infections was developed. Following an experimental lung infection the spleen was removed and spleen cells were tested for production of interferon-gamma upon stimulation with C. pneumoniae elementary bodies (EB), recombinant MOMP and recombinant Pmps in an EliSpot assay. Using C. pneumoniae EB, recombinant MOMP and Pmp proteins as antigens it was found that EB elicited a strong interferon-gamma response in the EliSpot assay, MOMP did not respond but Pmp6, Pmp8, 20 and 21 were found to stimulate spleen cells to secrete interferon-gamma. The response was shown to be mediated by CD4+ T-cells. Pmp8 elicited the strongest response making it a good candidate for a subcomponent vaccine.
Resistance to antifungal drugs
S384: The epidemiology of antifungal resistance
A. Pfaller (Iowa City, USA)
Invasive fungal infections are a significant cause of morbidity and mortality world-wide. They exert a growing clinical and economic burden on healthcare systems and patients. The increasing concern regarding antifungal resistance among both common and uncommon fungal pathogens over the past 10–15 years further drives this burden of disease. Typically species such as Candida albicans, C. glabrata, C. krusei, Cryptococcus neoformans and Aspergillus species exhibit different resistance phenotypes. The impact of resistance has only recently been fully appreciated with clinical failures due to both established and recently introduced agents being reported. As both acquired and intrinsic resistance continues to emerge it is recognized that a successful clinical outcome depends on several factors including the patient, selection of the appropriate agent, and the local epidemiology of the likely pathogen. Persistent drug pressure may result in acquired resistance in normally susceptible species or select for intrinsically resistant fungi from the patients endogenous flora or the extrinsic environment. In the hospital setting nosocomial transmission coupled with drug pressure may produce an endemic strain with progressively developing resistance. It is now apparent that the antifungal susceptibility profiles of Candida and Cryptococcus species may vary considerably from region-to-region or even among different hospital settings. Detection of specific DNA clades that are enriched for antifungal resistance phenotypes is a recent finding of great interest. Although new antifungal agents with novel mechanisms of action may temporarily improve our ability to treat certain fungal infections, the emergence of resistant fungi is inevitable and deserves our constant attention.
S385: The importance of susceptibility testing
E.M. Johnson (Bristol, UK)
Whilst antifungal drug resistance has not proved to be as problematic as that experienced with antibacterial agents, both intrinsic and emergent resistance are encountered and antifungal susceptibility testing can help in the guidance of prescribing practices. The expanding armamentarium of antifungal agents dictates that the clinician has some guidance in selecting the most appropriate agent for a particular infection and relative susceptibility of the infecting organism is an important factor in the decision. There are many test parameters that can potentially impact on the susceptibility test result and in the early years of testing differences in test methods produced confusing and conflicting results. In recent years standardized methods for susceptibility testing of yeast and mould isolates have been introduced and for some drugs it has been possible to define breakpoints. Whilst there are still certain reservations over the test methods and their application to certain organism-drug combinations, their widespread adoption makes national and international comparisons of susceptibility trends possible. Intrinsic resistance, which is generally consistent and predictable, is encountered in an increasing number of yeast and mould species and highlights the need for accurate speciation of infecting organisms. Susceptibility testing is of great importance in detecting intrinsic resistance in a species and therefore establishing the spectrum of activity of new and developmental agents. There is the possibility that general use of an agent will lead to the development of emergent resistance in a previously susceptible organism. Currently there are few problems with emergent resistance during a course of treatment which is potentially a more serious scenario than the more predictable innate resistance. Far more likely to occur in yeast rather than mould infections, this has been encountered predominantly with flucytosine and fluconazole mainly as a consequence of inappropriate prescribing practices for specific infections in certain patient groups. It is therefore important that testing mechanisms are introduced with the capacity to identify potential problems as they occur.
Emerging enteric pathogens: responding to the challenge
S392: Towards predicting cholera disease outbreaks within the Mediterranean Basin
J.F. Guégan, G. Constantin de Magny (Montpellier, F)
New insights into population dynamics of infectious diseases have shown the existence of regular cycles in the number of cases over time, with alternance of periods of booms and busts. The dynamics of infectious diseases is determined by a large number of complex processes acting over a large range of spatio-temporal scales. However, studies have been restricted so far to tiny hierarchical scales, which cannot really capture what may still happen at upper scales. Recent discoveries on both Vibrio cholerae life-cycle and cholera cases dynamics started to disentangle the many intrinsic and extrinsic environmental factors that may be involved in the evolution of disease within communities. Findings show that cholera cases may fluctuate with periods of outbreaks and quasi-extinction, depending on both local and large-scale environmental conditions, which influence V. cholerae kinetics within the environment. Based on statistical analysis and ecological modelling, we will show how we can model cholera cases dynamics within the Mediterranean area in taking account large-scale environmental conditions. Both studying the evolution of cholera cases in countries of northern Africa (using sophisticated wavelet analyses), and modelling the Vibrio life-cycle (using differential equations systems) based on environmental, ecological parameters obtained from remote-sensing and oceanographic surveys, we here present models that really mimic cholera disease patterns observed over time within the area. Results on cholera time-series in the southern part of the basin indicate that outbreaks are mainly associated with an elevation of local sea surface. The ecological modelling of outbreaks, which considers the many processes involved, shows that the existence of an environmental reservoir may help to explain cholera dynamics. This work constitutes one of the few studies on cholera dynamics which clearly show the influence of large-scale environmental factors on the evolution of cholera cases. More specifically, it is the first study which really demonstrates for the Mediterranean Sea that common processes to other regions of the World are at work in producing more or less periodic cholera outbreaks in the sub-southern region of the Basin. As climate temperature should increase in the future, the consequences on cholera outbreaks might be highly sensitive. Accordingly, this study is then the first step towards producing a predictive model of Vibrio bacteria emergence within the Mediterranean basin based on an integrated environmental surveillance.
Influenza vaccination
O395: Effectiveness of revaccination against influenza in the Dutch influenza vaccination programme
E. Hak, E. Buskens, T.J.M. Verheij on behalf of the PRISMA Study Group
Objectives: It has recently been suggested that a first vaccination against influenza is less effective than revaccination among elderly persons (Voordouw B, et al. JAMA, 2004). This might negatively influence first starters, especially persons with high-risk medical conditions younger than 65 years in whom vaccine uptake is considerably lower. We therefore aimed to assess the clinical effectiveness of influenza vaccination among first starters of any age in the Dutch influenza vaccination programme in preventing morbidity and mortality.
Methods: We conducted a case-control study nested in a cohort of 75,227 patients requiring vaccination. During the 1999–2000 influenza A(H3N2) epidemic, incident cases who died during the influenza epidemic or who required primary or secondary care for influenza, pneumonia, acute lung disease, myocardial infarction, stroke or heart failure were compared with controls regarding vaccination status. Estimates of the effectiveness of vaccination in reducing these endpoints were adjusted for confounding using stratified multivariate logistic regression analysis.
Results: After adjustments, vaccination prevented 46% of GP visits (95% confidence interval [CI]: −6% to 72%, p = 0.068) among first starting high-risk children aged under 18 years. Among first starting high-risk persons aged between 18 and 64 years, 14% (95% CI: −28% to 41%, p = 0.463) of GP visits, 97% (95% CI: 27% to 99%, p = 0.030) of hospitalisations and 63% (95% CI: 1% to 84%, p = 0.047) of deaths were prevented. Corresponding figures for elderly persons were −32% (95% CI: −78 to 3%, p = 0.063), 32% (−44% to 68%, p = 0.308) and −60% (−177 to 7%, p = 0.097).
Conclusion: These data confirm low effectiveness of influenza vaccination among first starting elderly persons. However, younger adults and children with high-risk medical conditions benefit from the vaccine even when receiving the vaccine for the first time.
O396: Effectivity of influenza vaccination of employees in reducing sick leave days, a meta-analysis
M. Damen, K. Wolthers, L. Spanjaard (Amsterdam, NL)
Objectives: Since the introduction of influenza vaccination several studies have been performed on the effectivity of vaccinating employees to reduce sick leave days. However, results were conflicting, and the statistical power was often too small. To overcome these problems a meta-analysis was performed.
Methods: A PUBMED and EMBASE search was conducted with the terms: ‘influenza’ AND ‘vaccine’ AND ‘sickness absence OR employees OR personnel’. Thirty papers were selected which were possibly suitable for the analysis. These papers were scored by two independent investigators with the help of a standardised form for methods and results. The most important selection criteria were: the study should be a double blind, randomised trial and the paper should contain data on the number of sick leave days of vaccinees and non-vaccinees. The meta-analysis was performed in Review Manager 4.2.
Results: Six papers were suitable for analysis. None of the studies recorded whether sick employees were tested for influenza. The total number of vaccinated persons was 4346 and of non-vaccinated persons (controls) 2881. The mean difference of sick leave days between vaccinated and non-vaccinated employees was 0.05 days in favour of vaccinated employees (95% CI 0.01–0.08, p = 0.01).
Conclusion: Employees vaccinated for influenza have significantly less sick leave days, however the mean difference with non-vaccinated employees is very small. Therefore, the cost-effectiveness of vaccinating employees in daily practice is questionable.
O397: Influenza immunization of healthcare workers in a paediatric hospital: getting to 73% vaccination coverage
O. Engels, M. Doyen, N. Goldman, A. Vergison (Brussels, B)
Background: In winter 2002, influenza immunization was offered to the healthcare workers (HCWs) of our hospital. Since then, the infection control team performed vaccination campaigns: seminars, posters, and face to face discussions. These campaigns targeted mainly at patients protection. Two problems were faced : 1) the trade unions saw these campaigns as a harassment of HCWs. 2) occupational medicine doctors were not convinced of the need of influenza immunization for HCWs. Objectives: Immunization rates reached 48 % in 2002 and 47% in 2003. In order to improve our next campaign, we wanted to know why the HCWs were accepting or refusing the vaccine and to evaluate the impact of infection control team interventions.
Methods: From June to August 2004 we addressed an anonymous questionnaire to the HCWs of our 170-beds pediatric hospital. The questionnaires were distributed in the different departments via the responsible doctor, nurse, paramedics and administrative staff.
Results: The answer rate was 44% (260/594). 48% of the answering persons received the influenza vaccine in 2002 and 59% in 2003. The immunization rates during these two vaccination campaigns were 84%, 60%, 44% and 18% for doctors, nurses, paramedics and administrative staff respectively. 32% of the HCWs had their decision influenced by the infection control practitionners. The face to face discussions were the most important for 48% of HCWs. Protection of both themselves and the patients was the main reason of immunization for 69% of HCWs. The main reasons for refusal in 2003 were feeling of good health (49%), not being convinced by the vaccine efficacy (35%), fear of adverse events evoked by the media (17%) and reactions to previous vaccination (8%). After getting the results of this audit, we targeted the next campaign towards patients and self-protection, insisted on vaccine efficacy and safety and provided a feedback showing a reduction of nosocomial influenza since vaccination. In 2004, the immunization rate obtained was 73% in mid-november.
Conclusions: Infection control practitionners’ vaccination campaigns allowed to reach a good immunization rate among our HCWs. Most HCWs do get vaccinated for both self protection and patients protection. Face to face discussions were important to convince HCWs about vaccine efficacy and safety. Vaccination coverage was highest in doctors and lowest in administrative staff.
O398: Reduction of the nosocomial influenza A burden in a paediatric hospital by immunisation of the healthcare workers
O. Engels, N. Goldman, M. Doyen, M. Duyse, D. Van Beers, A. Vergison (Brussels, B)
Background: Before 2002, the immunization rate of the healthcare workers (HCWs) of our hospital was negligeable. Since then, influenza immunization has been offered to HCWs. Vaccination coverage reached 48% in 2002 and 47% in 2003. Current national vaccine recommendations do not include flu vaccine except for children with underlying conditions.
Objectives: To study nosocomial influenza A in our 170 beds pediatric hospital and to evaluate the impact of vaccination of HCWs on nosocomial influenza rate.
Methods: We retrospectively reviewed nosocomial influenza A cases during 5 seasons from 1999 to 2004. We compared the first period of the study (3 seasons) with the second period (2 seasons post implementation of vaccination). Nosocomial cases were defined as a positive culture from nasopharyngeal aspirate obtained 48 h after admission and prompted by newly appeared symptoms compatible with influenza.
Results: Influenza A was recovered in 579 flu episodes during the 5 seasons. Out of 237 (146 for period 1 and 92 for period 2) influenza A positive cultures recorded in inpatients, 62 (26%) were hospital acquired. 18/62 patients with hospital acquired influenza (29%) had a prolonged hospital stay (median = 2 days, range 1 to 5 days). For 8/62 (13%), an antibiotic treatment was initiated. 22/62 (35%) had a chest x-ray performed. Nosocomial influenza rate dropped from 34% (49/146) of hospitalized influenza cases during period 1 to 14% (13/92) during period 2 (p < 0.001). Among the 62 nosocomial influenza patients, 26 (42%) were less than 24 months old and 33 (53%) had an underlying disease. The rate of at risk patients was unchanged during the 2 study periods (27/49 versus 6/13). The majority (15/33) of patients with underlying disease were cardiac patients from Algeria (no influenza immunization). Their nosocomial influenza rate decreased from 9% (13/146) to 2 % (2/92) between the 2 periods (p = 0.05). In children <2 years old without risk factor, nosocomial flu rate was reduced from 5% (7/146) to 0% (0/92) (p < 0.05).
Conclusions: Influenza A disease was associated with a longer length of stay in 29% of the nosocomial cases and chest x-ray were performed in 35% of the patients. A significant decrease in nosocomial influenza A disease was observed in children after immunization of nearly 50% of the HCWs in our pediatric hospital. It was observed in children with underlying cardiac disease but also in young children of less than 24 months without risk factor.
New drugs to fight the resistance challenge
O400: Development of novel antipathogenic drugs
T.B. Rasmussen, T. Bjarnsholt, M. Skindersoe, R.K. Phipps, T.O. Larsen, J. Nielsen, L. Eberl, M. Givskov (Kgs. Lyngby, Frederiksberg, DK; Zurich, CH)
Pseudomonas aeruginosa, a well known opportunistic pathogen and biofilm former, utilizes intercellular communication – quorum sensing – to coordinate virulence expression during invasion of and establishment in the hosts. Traditional treatment of infectious diseases is based on compounds which kill or inhibit growth of bacteria. A major concern with this approach is the frequent development of resistance to antibiotics. Furthermore, traditional antibiotics have little or no effect on bacteria in the biofilm mode of growth. In recent years, we have put much effort into the development of quorum sensing inhibitors in order to establish a non-antibiotic chemotherapy for patients infected with ‘quorum sensing’ bacteria such as Pseudomonas aeruginosa. Our approach is based on natural signal antagonists isolated from the environment. Fungi, plants, sponges and seaweeds are devoid of advanced immune systems but some have evolved to rely, at least in part, on secondary metabolite chemistry for protection against colonizing or competing bacteria. Hence, the study of cross-kingdom signal interference might turn out to be the source of new antimicrobial compounds. We present the design and demonstrate the usefulness of a novel tool for screening purposes the quorum sensing inhibitor selector (QSI-selector). QSI activity in the extracts of fungi, plants, sponges and seaweeds was verified by means of transcriptome analysis using Pseudomonas aeruginosa DNA micro arrays. The influence on Pseudomonas aeruginosa biofilm structure and antibiotic tolerance was established using the flow cell biofilm system. Whether the selected extract had an effect on the pathogenecity of Pseudomonas aeruginosa was evaluated using a nematode, Caenorhabditis elegans and a mouse pulmonary model. We have also assessed the molecular mechanism of inhibition and assessed the probability of development of resistance towards the QSI compounds. Our results demonstrate that eukaryotic organisms produce compounds capable of interfering with prokaryotic communication. Furthermore, these organisms contain quorum sensing’ bacteria indicating that the plants and fungi does not produce these compounds by happenstance. Using DNA micro arrays we have identified genes involved in interactions between biofilms and neutrophils and assessed the effect of QS and QSIs on these genes.
O401: Structural characterisation and susceptibility testing of epilancin 15X, a novel antibiotic
M.B. Ekkelenkamp, D. Milatovic, M. Hanssen, A. de Jong, S.D. Hsu, N.A.J. van Nuland, J. Verhoef (Utrecht, Bilthoven, NL)
Objectives: Epilancin 15X is a novel lantibiotic peptide, produced by a clinical isolate of Staphylococcus epidermidis. The objectives of this work are: 1. to determine the structure of this peptide and 2. to test an array of Gram-positive bacteria, including methicillin resistant Staphylococcus aureus (MRSA) and vancomycin resistant enterococci (VRE), for their susceptibility to epilancin 15X.
Methods: NMR-spectra of purified epilancin 15X were recorded by total correlation spectroscopy (TOCSY), nuclear Overhauser enhancement spectroscopy (NOESY), natural abundance 1H-13C heteronuclear single quantum correlation (HSQC) and 1H-13C heteronuclear multiple bond correlation (HMBC). From these spectra a putative peptide structure was derived, which was then confirmed by nano-scale liquid chromatography/tandem mass spectrometry. Minimal inhibitory concentrations (MICs) for epilancin 15X were determined for Staphylococcus aureus (10 methicillin susceptible and 10 methicillin resistant strains), coagulase negative staphylococci (10 strains) and enterococci (10 vancomycin susceptible and 5 vancomycin resistant strains) in a microtiter assay in accordance with NCCLS guidelines.
Results: Epilancin 15X contains 31 amino acids and has a molecular weight of 3,173 Daltons. It contains ten post-translationally modified amino acids, three lanthionine ring structures and a hydroxy-propionyl N-terminal moiety. The peptide was found to highly resemble the previously identified lantibiotic epilancin K7, with 68% amino acid sequence identity and three nearly identical lanthionine rings. The MIC for Staphylococcus aureus strains (both methicillin susceptible and methicillin resistant) ranged from 0.25 to 0.5 μg/ml, for enterococci from <0.125 to 1.0 μg/ml and for coagulase negative staphylococci from <0.125 to 0.25 μg/ml.
Conclusion: We here present the structure of epilancin 15X, a novel lantibiotic peptide which exhibits a high activity against Gram positive organisms; further studies will have to establish whether it could be of clinical use.
O402: Oleuropein: a novel antioxidant agent for treatment of experimental sepsis induced by multidrug-resistant Pseudomonas aeruginosa
V. Koussoulas, T. Geladopoulos, J. Vassiliadis, P. Koutoukas, L. Sabracos, H. Giamarellou, E.J. Giamarellos-Bourboulis (Athens, GR)
Objective: To clarify the potential antioxidant properties of oleuropein, a phenolic secoiridoid glucoside present in olive trees and virgin olive oil, in experimental sepsis induced by multidrug-resistant P. aeruginosa.
Methods: Sepsis was induced in 17 rabbits by a single injection of a multidrug-resistant P. aeruginosa isolate into the right renal pelvis following ureter ligation. Rabbits were divided into two groups; A: controls, and B: treated with one single iv dose of 1 ml of oleuropein (20 mg) diluted to 30 ml with D/W 5% upon signs of sepsis. Survival was recorded and blood was sampled for the estimation of malondialdehyde (MDA), tumor necrosis factor alpha (TNF) and total antioxidant status (TAS). MDA was determined by the thiobarbiturate assay followed by HPLC analysis; TNF by a bioassay on L929 fibrosarcoma cell line; and TAS by a colorimetric assay. Results: Survival curves are shown in Figure 1. Mean concentration of MDA before and 1.5, 3.5, 24, 48 hours after bacterial challenge were 1.43, 1.68, 3.34, 3.42 and 1.70 μl for group A; and 6.85, 5.44, 7.63, 4.73 and 8.74 μl for group B, respectively. Respective mean concentrations of TNF for group A were 16.29, 21.77, 13.52, 17.84 and 7235 pg/ml; and for group B 37.11, 9.07, 20.52, 19.56 and 40.13 pg/ml. Respective mean concentrations of TAS for group A were 1.54, 1.16, 1.26, 1.45 and 1.59 mM (TROLOX units); and for group B 1.62, 1.53, 1.48, 1.51 and 1.43 mM. Comparison of TAS between groups was found statistically significant (P between group A and group B 0.043). Negative correlation was found between MDA and TAS for group A (p = 0.017), but not for group B. Significant differences in bacterial load of liver, kidney, spleen and lower right lung lobe between two groups were not recorded.
Conclusion: Administration of oleuropein prolonged survival in experimental sepsis induced by multidrug-resistant P. aeruginosa. Its effect might be connected to enhancement of TAS accompanied by decreases of TNF.

O403: Garlic blocks the Pseudomonas aeruginosa communication systems and promotes rapid clearing of pulmonary Pseudomonas aeruginosa infections
T. Bjarnsholt, P.Ø. Jensen, T.B. Rasmussen, L. Christophersen, M. Hentzer, H. Hougen, J. Rygaard, C. Moser, L. Eberl, N. Høiby, M. Givskov (Kgs. Lyngby, Copenhagen, Valby, DK; Zurich, CH)
The opportunistic human pathogen Pseudomonas aeruginosa is the predominant microorganism of chronic lung infections in cystic fibrosis patients. P. aeruginosa colonizes the lungs by forming biofilm microcolonies through out the lung. Quorum sensing (QS) renders the biofilm growing bacteria highly tolerant to otherwise lethal doses of antibiotics, and protect from the bactericidal activity of polymorphonuclear leukocytes (PMNs). We have previously demonstrated that QS is inhibited by garlic extract. In this study we have evaluated the effect of garlic for the interaction between P. aeruginosa and tobramycin and the PMNs and outcome of pulmonary infection. P. aeruginosa was grown in vitro in continuous-culture once-through flow chambers with and without garlic extract. 3 day old biofilms were treated with 340 μg/ml of tobramycin continuously for 48 hours or human PMNs. The garlic treated biofilm was susceptible to both tobramycin and grazing of PMNs. The PMNs showed an increased activation, when incubated on the garlic treated biofilm. The differences in sensitivity were observed by confocal laser scanning microscopy of ‘live-dead’ stained biofilms, and the degradation of GFP tagged biofilms. The activation of PMNs was visualised by staining the PMNs with 123-dihydrorhodamine, which is oxidised to 123-rhodamine when H2O2 is produced - respiratory burst. Mice were treated with garlic extract or saline for 7 days, 2 day profylactic. P. aeruginosa was instilled in the left lung of the mice for up to 5 days. Bacteriology, mortality, histopathology, and cytokine production was used as endpoints. The results indicate that a QS inhibitory extract of garlic renders Pseudomonas aeruginosa sensitive to both tobramycin and, phagocytosis, and respiratory burst of polymorphonuclear neutrophile leukocytes. Garlic treatment of a pulmonary mouse model initially provokes a higher degree of inflammation and improved clearing of the infecting bacteria.
O404: Oral Ipsat P1A is a novel product to prevent antimicrobial resistance and antibiotic induced disturbance in gastrointestinal tract in humans
T. Heinonen, M. Carson, R. Jõgi, A.-M. Tarkkanen, S. Mentula, C.J. Donskey, C.E. Nord (Espoo, FIN; Tartu, EST; Helsinki, FIN; Cleveland, USA; Stockholm, S)
Objectives: Antibiotic administration may disturb the indigenous intestinal microflora and diminish colonization resistance against pathogenic microorganisms. Ipsat's novel beta-lactamase product aims to prevent such disturbance due to beta-lactam antibiotics by degrading the portion of antibiotic excreted into the small intestine without affecting systemic antibiotic levels. The aim of this Phase II study was to administer Ipsat's product, P1A, simultaneously with i.v. ampicillin and investigate the preventive effects and safety.
Methods: The study included three parallel groups of 12 healthy volunteers (males and females) per group. For 5 days, Group 1 received 1 g ampicillin qid, Group 2 received 8.2 mg Ipsat P1A qid and Group 3 received both treatments simultaneously. Stool samples were collected before, during and 7 days after treatment. Changes in stool microflora were measured using 16S rRNA fingerprints of bacteria and quantifying the major anaerobic and aerobic bacterial groups. The emergence of resistance was assessed by quantifying ampicillin-resistant coliforms and by measuring the changes (increase) in ampicillin resistant marker genes (TEM-family).
Results: Ampicillin treatment caused greater than a 50% change (p < 0.0001) in the microflora, greater than an 80% increase (p < 0.0001) in ampicillin-resistant coliforms and a highly significant increase in ampicillin resistant marker genes, whereas concurrent treatment with Ipsat P1A completely prevented these changes. Ipsat P1A also prevented the selection of multidrug resistant species including Klebsiella. No side effects or other safety concerns were noted with the Ipsat product.
Conclusions: Oral administration of Ipsat P1A eliminated ampicillin-induced alterations of the intestinal microflora of healthy volunteers and prevented the ampicillin-induced emergence of bacterial resistance. These results suggest a new strategy for reducing antimicrobial resistance in humans.
O405: Efficacy and safety of DB289, a new oral drug for treatment of Pneumocystis jiroveci pneumonia in AIDS patients
P. Yeramian, J. Leon, E. Huarcaya, L.A. Castagnini, J.L. Allen, J. Longstreth, E. Gotuzzo (Chicago, USA; Lima, PE)
Objectives: Trimethoprim sulfamethoxazone (TMP-SMX) remains the first line agent for treatment of PCP, although individuals with AIDS have a high rate of side effects during treatment and SMX resistance has been reported. We have evaluated the efficacy, safety and pharmacokinetics of new oral DB289 in an open-label, dose escalation, Phase II trial in patients with AIDS and mild-moderate PCP, who were intolerant to or failed prophylaxis or treatment with TMP-SMX. DB289 is the orally bioavailable prodrug of DB75, a novel diphenylfuran diamidine, that is active in vitro against P. carinii and in murine models of PCP.
Methods: Patients were ≥18 year with weight ≥45 kg and had documented PCP and HIV. Baseline PO2 was ≥60 mmHg. Two dose regimens were tested sequentially, 50 mg and 100 mg DB289 twice a day for 21 days. Patients were followed for 42 days with scoring of symptoms, ECG, chest X-ray, blood gases, and laboratory safety evaluations. DB289/DB75 plasma kinetics were evaluated on Days 7 and 14 throughout 12 hours, and pre-dose levels were taken on Days 4, 7, 10, 14, and 21.
Results: 35 patients were enrolled; 8 in the 50 mg group and 27 in the 100 mg group. All patients responded to treatment. Patients treated with 100 mg had a faster reduction of their symptom scores and normalization of blood-gases parameters compared to patients treated with 50 mg, with maximal effect observed by Day 10. There were no treatment failures with 100 mg DB289. Tolerance with DB289 treatment was good. Treatment was withdrawn for a patient after 12 days due to progression of underlying renal insufficiency. Other significant adverse events included two cases of moderate muscle pain/weakness. Treatment with DB289 resulted in sustained DB75 plasma levels throughout the dosing interval. Mean DB75 exposure after 100 mg was 6-times that observed after 50 mg. Pre-dose trough levels indicated some DB75 accumulation, consistent with the long terminal half-life observed for DB75 of over 80 hours, with steady state achieved between Days 10–14. At steady state, mean metabolite ratio (DB75/DB289) was 6 and 13 for the 50 mg and 100 mg doses, respectively, demonstrating excellent bioconversion of DB289.
Conclusion: Treatment with DB289 100 mg BID for 21 days provided rapid symptom relief and normalization of lung function in AIDS patients with PCP, Further trials are being planned for evaluation of DB289 as first line therapy of PCP.

O406: A comparative, investigator-blind study of topical tea tree oil versus erythromycin gel in the treatment of acne
R. Darabi, M.A. Hafezi, N. Akbarloo (Tehran, IR)
Background: Acne vulgaris is commonly treated with topical antibacterial agents but unfortunately there are increasing reports of bacterial resitance to most commonly used antibiotics such as erythromycin. Tea tree oil (TTO) has recently emerged as an effective topical antibacterial agent for the treatment of local skin infections including acne.
Objectives: This study sought to evaluate TTO efficacy in comparison to topical erythromycin for the treatment of acne.
Patients/Methods: Sixty volunteer patients with mild to moderate inflammatory acne lesions, aged between 15 to 25 years old were selected, randomly devided into two groups and treated with topical 5% TTO or 2% erythromycin gel twice daily for six weeks on an investigator-blinded protocol. Severity and number of acne lesions were evaluated before and after the study course.
Results: The average reduction of acne lesions was higher in the TTO compared to erythromycin treated group (Fig. 1, P < 0.001). Meanwhile, in the TTO group, 87.5% of cases had more than 50% reduction in acne lesions, which was significantly higher as compared to 53.8% in erythromycin group (Fig. 2, P < 0.01). The drop out rate due to severity of side effects in erythromycin group was significantly higher compared to TTO (P < 0.01). There were not any significant differences between frequency of side effects and relapse rate between two groups.


Conclusions: These results indicate that topical 5% tea tree oil in gel base is an effective and safe topical antibacterial agent for treatment of mild to moderate inflammatory acne vulgaris.
O407: Efficacy and safety of ertapenem compared with piperacillin/tazobactam for diabetic foot infections: The SIDESTEP Study
B. Lipsky, D. Armstrong, D. Citron, T. Erb, T. King, D. Morgenstern, S. Rawlins, M. Abramson for the SIDESTEP Study Group
Objectives: Diabetic foot infections (DFI) are a frequent cause of hospitalization for diabetics and the most common non-traumatic cause of lower extremity amputations world-wide. Few randomized controlled trials have compared the efficacy of different antibiotic regimens for DFI. Most previous studies were small and not blinded.
Methods: This double-blind randomized study was designed to determine noninferiority of intravenous (IV) ertapenem (E) to piperacillin/tazobactam (P/T) (3.375 g qid) for the treatment of patients with moderate to severe DFI. IV antibiotic therapy was required for a minimum of 5 days. Patients could be switched to oral therapy (amoxicillin/clavulanate) for a maximum cumulative treatment of 28 days. Baseline and follow-up visits included evaluation of tissue wound cultures and quantitative wound scores. Assessments were made at discontinuation of IV therapy (DCIV) and at day 10 post-treatment (IV or IV and oral if given) follow-up.
Results: 576 patients were randomized to treatment (E: 289; P/T: 287); 445 were clinically evaluable at the end of IV therapy (E: 226; P/T: 219). The mean duration of IV therapy was 11.1 d for E and 11.3 d for P/T. Clinical success rates were similar between the treatments at DCIV (E: 94.2%, P/T: 92.2%; between treatment difference: 1.9; 95% CI: −2.9, 6.9). In the microbiologically evaluable population, the overall rate of eradication (presumed or documented) at the 10 d follow-up was also comparable (E: 87.8%, P/T: 84.4%; between treatment difference: 3.4%; 95% CI: −4.5, 11.9). Clinical response rates were similar in both treatment groups across baseline wound scores and the response rates generally decreased with increasing baseline wound scores. There were no differences in drug-related adverse events during parenteral therapy (E: 15.2%, P/T: 19.9%; RR E/(P/T): 0.77; 95% CI: 0.54, 1.10; p = 0.147) or discontinuations due to drug-related adverse events during parenteral therapy (E: 1.0%, P/T: 2.1%; RR E/(P/T) 0.50; 95% CI: 0.15, 1.94; p = 0.341).
Conclusions: This study, the largest and most comprehensive randomized controlled trial of antibiotics for DFI, found that clinical and microbiological outcomes for patients treated with E once daily were equivalent to that of patients treated with P/T q6h. Both E and P/T were generally well-tolerated.
References
- 1.Giglione Cell. Mol. Life Sci. 2004;61:1455–1474. doi: 10.1007/s00018-004-3466-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giglione Mol. Microbiol. 2000;36:1197–1205. doi: 10.1046/j.1365-2958.2000.01908.x. [DOI] [PubMed] [Google Scholar]
- 3.Guilloteau J. Mol. Biol. 2002;320:951–962. doi: 10.1016/s0022-2836(02)00549-1. [DOI] [PubMed] [Google Scholar]
- 4.Boularot Curr. Opin. Investig. Drugs. 2004;5:809–822. [PubMed] [Google Scholar]
- 5.Yuan Drug Discov. Today. 2001;6:954–961. doi: 10.1016/s1359-6446(01)01925-0. [DOI] [PubMed] [Google Scholar]
- 6.Giglione EMBO J. 2000;19:5916–5929. doi: 10.1093/emboj/19.21.5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serero J. Biol. Chem. 2003;278:52953–52963. doi: 10.1074/jbc.M309770200. [DOI] [PubMed] [Google Scholar]
- 8.Lee Biochem. Biophys. Res. Commun. 2003;312:309–315. doi: 10.1016/j.bbrc.2003.10.123. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen Biochemistry. 2003;42:9952–9958. doi: 10.1021/bi0346446. [DOI] [PubMed] [Google Scholar]
- 10.Lee J. Clin. Invest. 2004;114:1107–1116. doi: 10.1172/JCI22269. [DOI] [PMC free article] [PubMed] [Google Scholar]


