Abstract
Disorders of taste and smell can present a challenge to the facial plastic surgeon. Obtaining a detailed history and examination is the key to the diagnosis and work-up of olfactory and gustatory dysfunction. Easy-to-administer tests are available for olfactory evaluation (University of Pennsylvania Smell Identification Test) and gustatory evaluation (taste sticks, tasting tablets). The prognosis and management of olfactory and gustatory disease depend on its causes. Despite ongoing research, the treatment of the disorders of smell and taste is limited.
Disorders of smell and taste should not be overlooked in a facial plastic surgery practice, especially among surgeons performing septorhinoplasty, turbinoplasty, or sinus surgery. Recognition and documentation of olfactory dysfunction before cosmetic or functional nasal surgery might save unnecessary anxiety in the postoperative period for both the patient and the surgeon and might even prevent a lawsuit. Patients undergoing rhinological procedures should be informed about olfactory loss as a potential risk of surgery. For the surgeon, understanding the anatomy and physiology of the olfactory and gustatory system will help avoid complications and facilitate counseling of patients with smell and taste disorders.
Olfaction triggers deeply rooted human emotions, both neuroanatomically and behaviorally. Any dysfunction of this special sense can be a major source of emotional stress to the patient [1]. The basic survival mechanism of the sense of smell alerts individuals to the presence of harmful environmental pollutants, smoke, and toxins. A healthy sense of smell also enables one to enjoy fine wines and gourmet food. Most patients with an olfactory dysfunction complain that they have “altered taste” when, in fact, they have a smell dysfunction. Up to 80% of a meal's flavor is due to olfactory input. Patients who sustain an injury to the olfactory system are no longer able to distinguish the subtle flavors that are characteristic of coffee, chocolate, strawberry, or root beer. Biologically, taste is only the sensation of five qualities: saltiness, bitterness, sweetness, sourness, and umami (monosodium glutamate).The goal of this article is to provide the facial plastic surgeon with an understanding of the anatomy and physiology of the olfactory and gustatory systems and with practical information about diagnostic tests and therapies that are currently available.
Olfactory system
Anatomy
Odors are experienced as a result of input primarily from the olfactory nerves (CN I), but also from trigeminal (CN V), glossopharyngeal (CN IX), and vagus (CN X) nerves. The trigeminal nerve has receptors for pungent odorants throughout the nasal and pharyngeal cavities. The glossopharyngeal and vagus nerves provide the minor chemosensory function in the pharyngeal area. The ciliated olfactory receptors are part of the olfactory neuroepithelium. From the nostril, these nerves are located 7 cm inside each nasal cavity. They branch from beneath the right and left cribriform plates Fig. 1, Fig. 2 and cover approximately 2 cm2 on each side of the nasal cavity. The olfactory region includes the superior nasal septum, superior/supreme turbinate, superior–lateral nasal wall, and sections of the middle turbinate [2], [3]. The cell bodies of the primary olfactory neurons are located within the nasal mucosa. The bundles of axons from these neurons (filia olfactoria) go up through the 15 to 20 foramina in the cribriform plate to synapse in the olfactory bulb (see Fig. 1, Fig. 2).
Fig. 1.
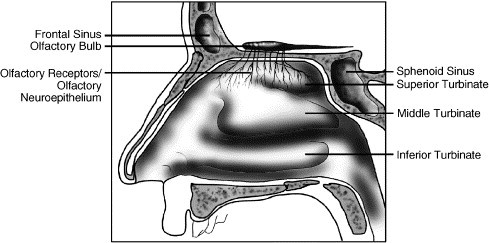
Distribution of olfactory neuroepithelium. Lateral nasal wall—sagittal view.
Fig. 2.
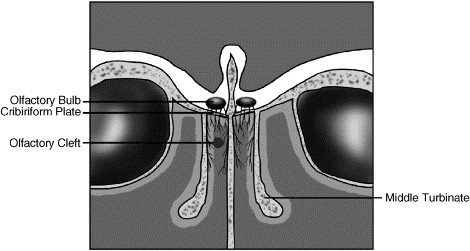
Distribution of olfactory neuroepithelium—coronal view.
It is estimated that humans have approximately 6 million olfactory axons. In addition to the main bipolar olfactory neuron receptors, the neuroepithelium contains the microvillar cells, as well as supporting or sustentacular cells, basal cells (horizontal and globose), and Bowman gland duct cells [2], [4]. The role of the microvillar cells is unknown. The sustentacular cells and Bowman duct cells contain cytochrome P450 and may play a role in deactivation of environmental toxins. The Bowman glands are the major source of mucus in the region of the olfactory epithelium.
The olfactory neuroepithelium has the unique ability to regenerate. All types of olfactory epithelial cells, including actual receptor neurons, are reconstituted from basal cells after injury or in natural cell turnover. The human olfactory neurons are thought to regenerate every 3 to 6 months, and this cycle continues as long as the basal cells remain healthy.
The olfactory pathway has a complex, multilevel organization. Odorant detection begins in the olfactory receptor area with the bipolar olfactory receptors, the primary-order neurons. These synapse with the second-order neurons, the dendrites of the mitral and tuffed cells of the olfactory glomerulus within the olfactory bulb. The signal is then transmitted along the olfactory tracts to the olfactory cortex, which is comprised of the anterior olfactory nucleus, olfactory tubercle, prepiriform cortex, lateral entorhinal cortex, cortical nucleus of the amygdala, and the periamygdaloid cortex.
The vomeronasal organ (VNO) (Fig. 3) is a bilateral membranous structure, 2 mm to 10 mm long, located in the base of the anterior septum, often appearing as a pit. Visible in 91% to 97% of healthy adults, it opens to the nasal vestibule through an orifice (diameter: 1.02 mm) 2 cm posterior from the nostril at the junction of the bony and cartilaginous septum. The VNO was previously considered a rudimentary organ because it has no neural connection to the brain. However, local electrophysiological responses have been recorded, and recent studies [5] demonstrate that the VNO system may mediate some autonomic, psychological, and endocrine responses. It is still possible that it could function to perceive pheromonal odorants, as occurs in other animals. Hence, it is prudent to avoid injury to this organ during nasal surgery.
Fig. 3.
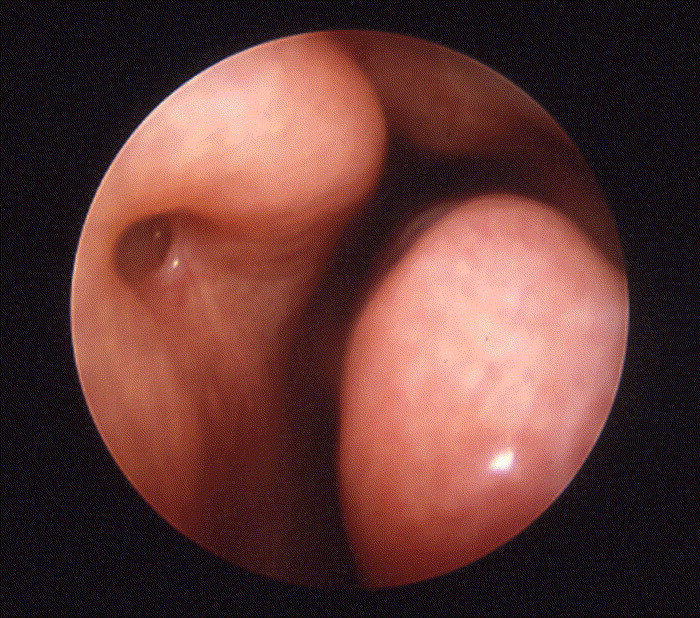
Vomeronasal organ (left nasal cavity).
The process of smelling
The molecules of any odorant need to reach the olfactory cleft to be recognized by the olfactory receptors. This process is facilitated by the nasal airflow during respiration. Approximately 10% to 20% of the airflow through the nasal cavity moves through the olfactory cleft [6]. Once the odorant chemical reaches the wall of the olfactory mucosa, it must adhere to it and dissolve in the mucus overlying that mucosa. More soluble chemicals penetrate more rapidly and effectively than less soluble ones. The chemical information is transformed into an electrical action potential. Activation of the olfactory receptors by means of G-protein and possibly cAMP intracellular messengers triggers depolarization and conduction of the signal along the axons. The signal is then propagated to the olfactory bulb and ascends ipsilaterally to the amygdala and primary sensory cortex. The process of odor identification is not well understood, but is clearly related to the number of receptors available for stimulation. Once an odor has been identified, multiple associations to time- and place-related memories can be made (eg, cinnamon and apple smells associated with Christmas). The olfactory memory, along with association areas, is stored in the medial anterior temporal lobes of the brain.
Types of olfactory dysfunction
The normal ability to smell is defined as normosmia. The olfactory disorders are defined as follows: anosmia, absence of ability to smell; hyposmia, decreased ability to smell; and dysosmia, altered perception of smell, which includes the subcategories of (1) phantosmia, perception of odor without stimulus present and (2) parosmia or troposmia, altered perception of an odor after stimulus.
Causes of olfactory disorders
The causes of the olfactory dysfunction can be separated into two main categories:
Conductive losses: secondary to obstruction of the nasal airflow to the olfactory cleft. Examples of causes of obstruction include chronic rhinosinusitis (CRS) (though a neural loss in CRS has also been documented), allergic rhinitis, polyps, and tumors.
Sensory/neural losses: secondary to damage to the olfactory nerves anywhere from olfactory receptors through the olfactory bulb to the processing centers in the brain. Examples include congenital loss of smell and loss of smell after upper respiratory infection (URI), head trauma, toxins, dementia, Alzheimer's disease, and multiple sclerosis.
Most olfactory dysfunctions caused by conductive factors are treatable. Olfactory disorders due to sensorineural factors are generally not amenable to therapy.
Nasal surgery and the risk to olfaction
Olfactory impairment can result from surgical intervention. Postsurgical scarring between the middle turbinate and the septum can alter the pathway for the airflow to the olfactory cleft. Olfactory impairment may also result from overresection of the superior or middle turbinate or avulsion of the olfactory neuroepithelium, especially in patients whose only remaining olfactory neuroepithelium is in an “exposed” location. Using “through-cutting” or powered instruments in the region of the middle or superior turbinate may prevent the potential stripping of the neuroepithelium [7], [8].
The risks to olfaction from rhinoplasty have been described. Champion [9] reviewed 200 rhinoplasties: 22 patients (10%) had temporary anosmia lasting 6 to 18 months after surgery, and one case lasted more than 3 years. No olfactory testing was used with this study; hence, the accuracy of these reports is unclear. Goldwyn and Shore [10] evaluated 97 patients before and after nasal surgery and found three patients (3%) with decreased postoperative olfactory ability. No long-term (greater than 2 months) olfactory loss was identified, however. In this study, no statistical analysis was performed, and testing was done using only three odorants presented to each nostril separately in open bottles. Stevens and Stevens [11] evaluated 100 patients undergoing septoplasty, septorhinolasty, turbinoplasty, polypectomy, and Caldwell-Luc. In eight patients (8%), the olfactory ability decreased, and one patient (1%) became anosmic. Briner et al [12] followed 184 patients who underwent sinus surgery, septoplasty, and rhinoplasty for 6 months. The Smell Diskettes Test and questionnaire were used as evaluating tools. Nineteen patients (10.3%) had impaired sense of smell preoperatively. Following surgery, four patients (2.5%) who had had normal preoperative sense of smell developed hyposmia. Six patients with preoperative hyposmia had improvement of sense of smell after surgery (two patients after septoplasty, two after sinus surgery, one after rhinoplasty, and one in the group of other operations). No patient developed anosmia. Kimmelman [13] tested 93 patients before and after nasal surgery that included ethmoidectomy, polypectomy, Caldwell-Luc, open- and closed-reduction of the nasal fracture, septoplasty, and rhinoplasty. For pre- and postoperative olfactory function testing, the author used the University of Pennsylvania Smell Identification Test (UPSIT). He found that 66% of patients had improvement or no change in the UPSIT scores. Thirty-four percent had a decline in their UPSIT score, but this decline was minimal. The study concluded that the risk of anosmia after nasal surgery was low at 1.1%. Kimmelman [13] proposed several mechanisms of injury to olfactory function from sinonasal surgery. We have modified this scheme according to our current understanding (Table 1) .
Table 1.
Mechanisms of injury to the olfactory function from sinonasal surgery
| Mechanical injury/mechanical factors: | Direct trauma to the olfactory epithelium: |
| 1. Resulting from use of electrocautery. | |
| 2. Lasers direct or scattered to the olfactory region. | |
| 3. Traction on the olfactory filia due to cribriform plate motion with superior septoplasty or osteotomies. | |
| 4. Mechanical abrasion after direct trauma. | |
| Scarring in the olfactory region. | |
| Atrophic rhinitis secondary to aggressive resection of the sinonasal tissue, especially inferior turbinectomy, which can lead to excessive crusting, dryness and mechanical occlusion of the olfactory cleft by crust. | |
| Airflow modifiers: | Scarring or anatomical narrowing/widening that would alter airflow to the upper nasal olfactory neuroepithelium. |
| Vascular/neural injury: | Vascular compromise to the olfactory neuroepithelium secondary to surgically created ischemia. |
| URI in early post-operative period (Herpes, influenza, Rhino and Corona viruses are known to affect the olfactory pathway). | |
| Other: | Medications: |
| 1. Local anesthetics applied either topically or injected | |
| 2. Topical Zinc products | |
| Psychological factors: anxiety, stress which may lead to the complaints of olfactory dysfunction. | |
| Unrecognized preexisting anosmia/hyposmia. | |
| Loss of major areas of healthy olfactory epithelium with only few functioning areas that still give “normal” olfactory function. |
Obstructive nasal disease and sinus disease
Olfactory loss can be secondary to complete obstruction of the airflow by intranasal tumors such as inverting papiloma, hemangioma, squamous cell carcinoma, esthesioneuroblastoma, and sinonasal–undifferentiated carcinoma. Comparison smell testing will often show a loss on one side. In the past, CRS was viewed solely as a conductive cause of olfactory dysfunction, but there is growing evidence that olfactory dysfunction secondary to CRS is due to conductive and neural factors. Kern [14] looked at the histopathologic changes in the olfactory mucosa of patients with CRS undergoing endoscopic sinus surgery. Epithelial inflammation was found with olfactory deficits, suggesting that inflammation of the epithelium in addition to altered airflow may contribute to olfactory losses.
Effects of aging on olfaction
Decreased olfactory function can result from aging. Olfactory identification ability drops sharply in the sixth and seventh decades of life. More than half of the population in the 65 to 80 age group shows major olfactory decline secondary to extensive degeneration in the olfactory bulb associated with aging [4]. Whether this group is more susceptible to losses after surgery is unclear.
Alzheimer's disease and Parkinson's disease are both associated with decreased olfactory function. This decreased function most likely is a result of damage to the olfactory bulb or central olfactory cortex [15]. In fact, decreased sense of smell is often the first sign of these dementias. Neuronal loss has been identified in the olfactory bulb and neural tracts of individuals who died with Parkinson's disease, with a strong correlation to the duration of the disease process.
Congenital olfactory dysfunction
These patients usually have no memory associations with flavor or smell perception throughout their lives. The anosmia generally is not noticed until the end of the first decade of life. The differential diagnosis is small, but diagnosis can be difficult because other causes like head trauma and prior URI must be excluded. A few syndromes have been associated with anosmia. The best known is Kallmann's syndrome: hypogonadotropic hypogonadism. Failure to develop secondary sexual characteristics in an anosmic male should cause one to suspect the syndrome and prompt referral to an endocrinologist. MRI testing may demonstrate the absence of olfactory bulbs in these patients. Another congenital olfactory dysfunction, familial anosmia, has been associated with baldness and vascular headaches, along with other features.
Head trauma
A small percentage of patients with head trauma (5%–10%) experience a loss of olfactory function. In children the reported incidence of olfactory loss after head trauma is 3.2% for transient cases and 1.2% for permanent loss. The degree of loss usually correlates with the severity of trauma. Fractures in the frontal region are most commonly associated with olfactory losses, with occipital trauma being the second most common cause. Post-traumatic olfactory dysfunction can be the result of (1) shearing injury of the olfactory nerve axons, (2) brain contusion and hemorrhage in the olfactory regions, and (3) sinonasal tract alternation. The usual course of injury to olfactory function is an immediate onset, but it can also be delayed until months after the initial injury [16], [17]. In 10% of cases olfactory function returns, but it is usually diminished. Human olfactory biopsy studies after head trauma suggest that return of olfactory ability is impeded by the inability of regrowing olfactory neurons to find the olfactory bulbs or the holes in the cribriform plate [18].
Upper respiratory infection
This is the most frequent cause of neural olfactory loss. It most commonly affects women (70%–80% of cases) and follows the viral-like URI. One third of patients will show improvement after 6 months. Unfortunately, the longer the dysfunction is present, the worse the chances for recovery. Animal studies show viruses can cause severe damage to the olfactory neuroepithelium with replacement by respiratory epithelium, but this has never been proved in humans. Biopsies of the olfactory cleft in affected human patients show either decreased numbers of olfactory receptors or their complete absence [19], [20]. Corona virus was shown in mice to cause degeneration and destruction of the olfactory bulb and have little effect on the neuroepithelium [21]. Although olfactory loss related to upper respiratory infections is thought to be caused by viruses, this has not been proven, nor has the exact viral type been identified.
Exposure to toxin
Some patients have olfactory dysfunction after exposure to toxins, various gases, and aerosols. Common chemicals known to cause olfactory loss include formaldehyde, cyanoacrylates, herbicides, pesticides, and cigarette smoke. The concentration of the toxins and length of exposure correlate directly with potential damage to the olfactory system [22]. These losses are usually permanent.
Miscellaneous
Psychiatric disorders like depression and schizophrenia have been associated with olfactory losses. Patients with dementia, epilepsy, Down syndrome, or various endocrine abnormalities such as hypothyroidism, Addison's disease, Cushing's disease, and diabetes mellitus may have decreased or absent olfactory ability. Nutritional deficiencies (vitamin A, zinc, thiamine) have been found to affect olfaction. Anosmia can result from such intracranial tumors as Foster Kennedy syndrome–olfactory groove meningioma, frontal lobe gliomas, and pituitary adenomas. These patients often present with other cranial nerve abnormalities. Twenty-five percent of temporal lobe tumors cause olfactory dysfunction. Unfortunately, 30% to 40% of patients with olfactory dysfunction have an undetermined cause.
Causes of parosmia (troposmia) and phantosmia
Patients with phantosmia experience distortion of their sense of smell. These patients usually have decreased olfactory ability in at least one nostril on testing [23], [24]. This disorder sometimes follows damage to the olfactory neuroepithelium due to URI or head trauma, or it may be associated with aging. It can also be secondary to temporal lobe tumors or seizures. Often, however, there is no good reason for the olfactory loss or perceived distortion.
Clinical assessment of the sense of smell
The first and most important step in evaluating a patient with a smell disorder is to obtain a detailed history and clearly define the symptoms. Most patients with chemosensory deficits complain of taste alteration. Upon closer inquiry patients admit that they are still able to taste sweet, bitter, sour and salt, but complain that the food does not have any flavor. Perception of flavor therefore is lost mostly because of the olfactory damage, not a gustatory disorder. It is important to estimate the degree of olfactory loss and its duration. The examiner should inquire about events that occurred around the time of the initial loss, such as head trauma, exposure to toxins or fumes, or URI. Unilateral epistaxis or obstruction gives rise to the suspicion of sinonasal tumor. A fluctuating sense of smell is common in patients with rhinosinusitis and polyposis. Attention should also be paid to a history of sinus problems, allergies, nasal obstruction, visual changes, central nervous system complaints, delayed puberty, or endocrine abnormalities (hypothyroidism). Past medical history should be reviewed for occupational exposure and cigarette smoke. The patient's current medications and the ones used at the time of the onset of olfactory dysfunction also need to be reviewed, because many of them can affect the olfactory and gustatory function. Some examples include adrenal steroids, amino acids in excess (eg, cysteine or histidine), antimicrobials (neomycin, penicillins, macrolids), antithyroidals (methimazole, thiouracil), opiates (codeine, morphine), and cardiovascular and antihypertensive medications [25]. Usually, olfactory function will return after the medication is discontinued, but sometimes the change can be permanent. Inquiry should be made about signs of early dementia, Parkinson's disease, depression, or schizophrenia.
Physical examination
A complete ear, nose, and throat examination with emphasis on the nasal airways is necessary. Nasal endoscopy is especially helpful to identify obstructive causes of olfactory losses. Half of the cases of olfactory cleft obstruction are missed when anterior rhinoscopy is performed alone. This figure drops to less than 10% when endoscopy is included in the examination [26]. During the nasal endoscopy, attention should focus on the patency of the olfactory cleft and middle meatus and the presence of the air-space between the middle turbinate and septum, especially in the superior portion toward the olfactory cleft. The presence of polyps, tumors, sinonasal mucosal edema, adhesions, postoperative changes, or crusting is noted. A neurologic examination should be performed with emphasis on the assessment of cranial nerve function. A Mini-Mental examination can be performed if the patient is showing signs of dementia.
Imaging
If nasal obstruction secondary to anatomic deformity, tumor, or polyps is suspected, then CT scan of the sinuses is indicated. The presence of an intranasal mass warrants further evaluation with MRI to assess possible intracranial extension. In many patients who present with a loss of smell, imaging is not indicated. Brain tumors that present with isolated anosmia are extremely rare [27]. Imaging is indicated in individuals who present with unusual, ominous symptoms or a pattern that does not fit a standard diagnosis. For instance, a 42-year-old woman with olfactory loss that occurred 3 days after URI would not need imaging if her nasal endoscopy was normal.
Olfactory testing
Testing of gustatory and olfactory ability is mandatory in the work-up of a patient with chemosensory complaints [28]. Gustatory testing will be discussed in the Taste Disorders section. Most olfactory testing relies on measuring detection thresholds of a specific odorant or the ability to identify multiple odorants [29]. The University of Pennsylvania Smell Identification Test (UPSIT) is the most widely used test. It consists of four “scratch and sniff” booklets, each containing 10 microencapsulated odorants. The test is self-administered and usually takes 15 to 20 minutes to complete. The UPSIT has been extensively studied and validated for age and gender [30]. Test protocols also help to identify malingerers. The reliability of the test is very high, and it has versions available for many cultures [31]. The UPSIT can be used to assess a patient's olfactory ability before and after treatment and to follow disease progression. In Europe, a popular test uses odorant-impregnated felt tip pens (Sniffin'Sticks) for threshold and odorant identification. It is a forced-choice test that is easy to administer and can be reused [32], [33]. A simple olfactory screening test using a 70% isopropyl alcohol pad as a stimulant has recently been described [34]. With the patient's eyes closed, the alcohol pad is brought gradually toward the patient's nose. The patient reports the moment when he or she can detect the odor, and the distance from the nares to the pad is measured. The distance correlates with the degree of olfactory loss. The test also makes it possible to differentiate between unilateral and bilateral losses and between hyposmia and anosmia.
Electrophysiological tests like electro-olfactogram or electroencephalogram are currently used for research purposes only. Functional magnetic response is also used by the researchers to detect areas of brain activity in response to odorant presentation [35].
Treatment
General
All patients with olfactory loss have to be counseled about the safety issues: the need for smoke alarms and for eliminating the possibility of exposure to methane or propane gas in their household. Patients should be advised to live in an all-electric or oil-heated residence. As long as trigeminal nerve function remains intact, trials with pungent ingredients such as mustard or hot peppers may heighten the dining experience. Labeling food in the refrigerator and freezer with dates when the package was opened or stored will help track the freshness of the food products and prevent food poisoning.
Medical therapy
The only type of olfactory loss that can be successfully treated is that due to nasal obstruction [36]. There is no effective medical therapy or intervention for a neural olfactory loss. In patients with olfactory dysfunction secondary to nasal obstruction, the treatment is directed toward restoring the airflow to the olfactory cleft. Treatment with nasal corticosteroids, decongestants, antibiotics, allergy medications, allergy immunotherapy, and saline irrigations may be helpful. Application of topical nasal steroids in the head down and forward position may be especially helpful with olfactory cleft blockage [37]. Many publications suggest that various vitamins and minerals such as zinc, vitamin A, and vitamin B will help with olfactory disorders, but there have been no statistically valid, controlled studies to demonstrate the effectiveness of these therapies. A trial of 1-month therapy with a large dose of oral steroids (prednisone 1 mg/kg/day) might be helpful in the patient with recent olfactory loss.
Surgical therapy
Patients with an olfactory dysfunction secondary to nasal obstruction who do not respond to medical therapy may benefit from surgical intervention: endoscopic sinus surgery, turbinoplasty, or polypectomy [38], [39], [40], [41], [42]. Many studies have shown improvement in sense of smell after sinus surgery. However, in patients with CRS, no study has been able to document an association between olfactory test scores and intranasal airway access based on rhinoscopy, rhinometry, or acoustic rhinometry, except in cases of total or near-total blockage [4]. Patients with intranasal or intracranial tumors may benefit from surgical excision or combined therapy with chemo-radiation, depending on the pathology of the process. Severe cases of phantosmia have been treated with craniotomy and bilateral bulbectomy. This type of surgery alleviates the phantosmia but also results in anosmia [43]. A more conservative approach involves endoscopic excision of the olfactory mucosa from the bottom of the cribriform plate on the affected side. It provides relief to the patient with possible preservation of some olfactory function [23], [24], [44].
Gustatory system
Anatomy and physiology
The perception of taste begins in the taste buds: clusters of receptors cells located mostly on the tongue but also on the palate and laryngeal surface of the epiglottis. The taste buds have a limited life-span, approximately 10 days, and are continuously replaced. There are four types of taste papillae: fungiform, foliate, filiform, and circumvallate papillae. The fungiform papillae, visible as small red structures on the tip and anterior two-thirds of the tongue, are innervated through the chorda tympani (from nerve VII). Circumvallate papillae are raised circular structures located in the posterior tongue and innervated by the glossopharyngeal cranial nerve IX. Foliate papillae reside between folds at the lateral borders of the tongue and are also innervated by cranial nerve IX. The filiform papillae do not contain taste buds and do not play a role in the taste function. Other minor locations of the taste buds include the soft palate (innervated by cranial nerve VII via the greater superficial petrosal nerve), the laryngeal surface of the epiglottis (innervated by the superior laryngeal nerve, a branch of cranial nerve X), and the pharynx, with innervation from branches of cranial nerves IX and X.
The process of taste is initiated when a chemical compound physically interacts with the taste buds. The taste buds transform the chemical signals into electrical signals that travel to the nerve fibers. Taste fibers from cranial nerves VII, IX, and X terminate in the rostral nucleus solitarius in the medulla. From there, the taste pathway travels ipsilaterally to the ventroposteromedial nucleus in the thalamus and thence to the taste center in the parietal lobe of the brain. The five taste qualities (saltiness, sweetness, sourness, bitterness, and umami) can be detected in all regions of the tongue where the taste buds are located.
Disorders of taste
True loss of taste is extremely rare. Most patients who complain of a loss of taste actually suffer from olfactory dysfunction, with an inability to perceive the flavors of food. Pathologic conditions along each segment of the gustatory pathway could lead to the alteration of taste: hypogeusia is partial loss of taste, ageusia is a complete loss, and dysgeusia is a sensation of altered taste. Taste distortion with stimulus (parageusia) or without stimulus (phantgeusia) can also occur.
Numerous processes can contribute to the loss of taste or its alteration. Viral, bacterial, fungal, and parasitic infections of the oral and hypopharyngeal mucosa may lead to disturbance of taste. Radiation-induced mucositis may also cause impairment. Poor oral hygiene can cause distortion of taste. The aging process adversely affects the sense of taste, but to a lesser degree than it does the sense of smell. Bitter and sour tastes are most likely to diminish with age, but the loss is generally only partial [45]. Neoplastic involvement of the floor of the mouth, submandibular space, or infratemporal fossa may produce a loss of taste. Smoking may have an adverse effect on taste sensitivity and discrimination. Injury to the chorda tympani can also occur secondary to ear surgery or infections like chronic otitis media, Bell's palsy, Ramsay-Hunt syndrome, and Lyme disease. Patients with chorda tympani injuries actually complain of phantom taste (metallic, sometimes salty or bitter) more frequently than they do of complete loss of taste [46]. Trauma to the lingual or pharyngeal branches of cranial nerve IX during tonsillectomy or uvulopalatopharyngoplasty can also result in taste dysfunction. Pathologic involvement of nerves IX and X in glomus tumors, squamous cell carcinoma, or schwannoma, together with other neurologic deficits, will produce a loss of taste. Head injury rarely causes a loss of taste, with a reported incidence of 0.4% to 0.5% [47]. Some systemic diseases have been associated with a loss of smell or phantom smell. Renal disease may produce a phantom taste (metallic or bitter), which is most likely secondary to accumulation of uremic toxins, because improvement occurs after dialysis [48]. Patients with diabetes may experience taste disturbances as a consequence of related neuropathies.
Evaluation of taste
Patients who complain of inability to enjoy food flavor or who experience “unpleasant taste” are most likely suffering from olfactory dysfunction. Evaluation of chemosensory ability should include assessment of the quality and intensity of taste. The taste qualities can be affected to different degrees, and each needs to be tested separately. Typically, the following stimuli are used to test four taste qualities: NaCl (salty), sucrose (sweet), citric acid (sour), and quinine hydrochloride or coffee (bitter). Taste function in various areas of the tongue and oral cavity can be measured using a spatial test. The three-drop technique involves placing three drops of a given chemical on a random portion of the tongue. The concentration is titrated to obtain the threshold of sensitivity. Recently, several tests have been developed in Germany that resemble this technique but are more standardized in the form of “taste strips,” wafers or tablets with specific concentrations of the stimuli. Some allow testing of the whole mouth, while others facilitate testing of each side of the tongue separately [49], [50], [51].
Another important determination to make in gustatory testing is the differentiation between the genuine stimulus and the phantom taste. Patients are asked to rinse their mouths with water. Elimination of the unpleasant taste suggests that the stimulus is real. If the spatial testing subsequently reveals a normal taste system, this likewise suggests the presence of the genuine tastant. Topical anesthesia applied to the tongue or mouth can also eliminate taste that is due to the presence of genuine tastant or peripheral taste dysfunction. The source of the genuine tastant could be saliva, laryngopharyngeal reflux, or sinonasal drainage. Taste phantoms can actually intensify after the topical anesthesia has been applied to the mouth in some cases, such as that of a patient complaining of the metallic taste after ear surgery with injury to the chorda tympani.
Treatment
Treatment of gustatory dysfunction should be directed toward the causative factor. Patients with inflammatory or infectious diseases of the oropharyngeal mucosa, like oral candidiasis, may benefit from antifungal or antimicrobial therapy. Correction of postradiation mucositis with salivary stimulants or artificial saliva may improve taste function. There are conflicting reports in the literature about the efficacy of zinc therapy for patients with gustatory dysfunction. The promising data come, however, from studies of head and neck cancer patients with postradiation taste alteration who are showing positive response to zinc therapy [52].
Even with an identifiable cause, most gustatory deficits are untreatable, such as cases of nerve damage, central nervous system damage, and diabetes-related neuropathy. Psychological support may help these patients deal with the stress and anxiety produced by gustatory dysfunction [53].
Summary
Disorders of smell and taste can present a challenge for the facial plastic surgeon. Obtaining a detailed history and physical examination is the key to diagnosis and work-up of the olfactory and gustatory dysfunction. Understanding that most patients' “taste” complaints are actually symptoms of an olfactory dysfunction is essential. Distinguishing between true gustatory loss (the inability to perceive bitter, sweet, salty, sour, and umami) and olfactory loss (the inability to perceive complex flavors of food) will help clarify the patient's diagnosis. Easy-to-administer tests are available for olfactory evaluation (UPSIT) and gustatory evaluation (modified three-drops testing: taste sticks, tasting tablets). The prognosis and management of the olfactory and gustatory disease depend on its cause. Olfactory loss due to obstructive causes is amenable to treatment. Central losses are usually not treatable. True gustatory dysfunction is rare. In some cases, identifying and eliminating causative factors such as infection and inflammation may alleviate the taste dysfunction. For most patients with taste and smell disorders, no effective therapies are available. Psychological support and environmental protection play important roles under these circumstances.
References
- 1.Herz R.S., Cupchik G.C. The emotional distinctiveness of odor-evoked memories. Chem Senses. 1995;20:517–528. doi: 10.1093/chemse/20.5.517. [DOI] [PubMed] [Google Scholar]
- 2.Cullen M.M., Leopold D.A. Disorders of smell and taste. Med Clin North Am. 1999;83:57–74. doi: 10.1016/s0025-7125(05)70087-0. [DOI] [PubMed] [Google Scholar]
- 3.Leopold D.A., Hummel T., Schwob J.E., Hong S.C., Knecht M., Kobal G. Anterior distribution of human olfactory epithelium. Laryngoscope. 2000;110:417–421. doi: 10.1097/00005537-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Doty R.L., Mishra A. Olfaction and its alternation by nasal obstruction, rhinitis, and rhinosinusitis. Laryngoscope. 2001;111:409–423. doi: 10.1097/00005537-200103000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monti-Bloch L., Jennings-White C., Berlinger D.L. The human vomeronasal system: a review. Ann N Y Acad Sci. 1998;855:373–389. doi: 10.1111/j.1749-6632.1998.tb10595.x. [DOI] [PubMed] [Google Scholar]
- 6.Hahn I., Scherer P.W., Moxell M.M. Velocity profiles measured for airflow through a large-scale model of the human nasal cavity. Appl Physiol. 1993;75:2273–2287. doi: 10.1152/jappl.1993.75.5.2273. [DOI] [PubMed] [Google Scholar]
- 7.Bolger W.E., Keys A.S., Lanza D.C. Use of the superior meatus and superior turbinate in the endoscopic approach to the sphenoid sinus. Otolaryngol Head Neck Surg. 1999;120:308–313. doi: 10.1016/S0194-5998(99)70267-6. [DOI] [PubMed] [Google Scholar]
- 8.Orlandi R.R., Lanza D.C., Bolger W.E., Clerico D.M., Kennedy D.W. The forgotten turbinate: the role of the superior turbinate in endoscopic sinus surgery. Am J Rhinol. 1999;13:251–259. doi: 10.2500/105065899782102908. [DOI] [PubMed] [Google Scholar]
- 9.Champion R. Anosmia associated with corrective rhinoplasty. Br J Plast Surg. 1966;19(2):182–185. doi: 10.1016/s0007-1226(66)80030-9. [DOI] [PubMed] [Google Scholar]
- 10.Golwyn R.H., Shore S. The effects of submucous resection and rhinoplasty on sense of smell. Plast Reconstr Surg. 1969;41:427–432. doi: 10.1097/00006534-196805000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Stevens C.N., Stevens M.H. Quantitative effects of nasal surgery on olfaction. Am J Otolaryngol. 1985;6:264–267. doi: 10.1016/s0196-0709(85)80053-3. [DOI] [PubMed] [Google Scholar]
- 12.Briner H.R., Simmen D., Jones N. Impaired sense of smell in patients with nasal surgery. Clin Otolaryngol. 2003;28(5):417–419. doi: 10.1046/j.1365-2273.2003.00735.x. [DOI] [PubMed] [Google Scholar]
- 13.Kimmelman C.P. The risk to olfaction from nasal surgery. Laryngoscope. 1994;104(8 pt 1):981–988. doi: 10.1288/00005537-199408000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kern R.C. Chronic rhinosinusitis and anosmia. Laryngoscope. 2000;110:1071–1077. doi: 10.1097/00005537-200007000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Doty R.L., Reyes P.F., Gregor T. Presence of both odor identification and detection deficits in Alzheimer's disease. Brain Res Bull. 1987;18(5):597–600. doi: 10.1016/0361-9230(87)90129-8. [DOI] [PubMed] [Google Scholar]
- 16.Hong S.C., Leopold D.A., Oliverio P.J., Beuson M.L., Mellits D., Quaskey S.A. Relationship between CT scan findings and human sense of smell. Otolaryngol Head Neck Surg. 1998;118(2):183–186. doi: 10.1016/S0194-5998(98)80008-9. [DOI] [PubMed] [Google Scholar]
- 17.Schechter P.J., Henkin R.I. Abnormalities of the taste and smell after head trauma. J Neurol Neurosurg Psychiatry. 1974;37(7):802–810. doi: 10.1136/jnnp.37.7.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jafek B.W., Eller P.M., Esses B.A., Moran D.T. Post-traumatic anosmia: ultrastructural correlates. Arch Neurol. 1989;46(3):300–304. doi: 10.1001/archneur.1989.00520390066018. [DOI] [PubMed] [Google Scholar]
- 19.Jafek B.W., Murrow B., Michaels R., Restrepo D., Linschoten M. Biopsies of human olfactory epithelium. Chem Senses. 2002;27(7):623–628. doi: 10.1093/chemse/27.7.623. [DOI] [PubMed] [Google Scholar]
- 20.Yamagishi M., Fujiwara M., Nakamura H. Olfactory mucosal findings and clinical course in patients with olfactory disorders following upper respiratory viral infection. Rhinology. 1994;32:113–118. [PubMed] [Google Scholar]
- 21.Schwob J.E., Saha S., Youngentob S.L., Jubelt B. Intranasal inoculation with the olfactory bulb line variant of mouse hepatitis virus causes extensive destruction of the olfactory bulb and accelerated turnover of neurons in the olfactory epithelium of mice. Chem Senses. 2001;26:937–952. doi: 10.1093/chemse/26.8.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corvin J., Loury M., Gilbert A.N. Workplace, age and sex as mediators of olfactory function: data from National Geographic Smell Survey Gerontol Series B. Psychol Sci Soc Sci. 1995;50:179–186. doi: 10.1093/geronb/50b.4.p179. [DOI] [PubMed] [Google Scholar]
- 23.Leopold D.A., Schwob J.E., Youngentob S.L., Hornung D.E., Wright H.N., Mozell M.M. Successful treatment of phantosmia with preservation of olfaction. Arch Otolaryngol Head Neck Surg. 1991;117:1402–1406. doi: 10.1001/archotol.1991.01870240094016. [DOI] [PubMed] [Google Scholar]
- 24.Leopold D.A. Distortion of the olfactory perception: diagnosis and treatment. Chem Senses. 2002;27(7):611–615. doi: 10.1093/chemse/27.7.611. [DOI] [PubMed] [Google Scholar]
- 25.Doty R.L. Causes of olfactory and gustatory disorders. In: Getchell T., Doty R.L., Bartoshuk L.M., editors. Smell and taste in health and disease. Raven Press; New York: 1991. pp. 449–462. [Google Scholar]
- 26.Seiden A.M., Duncan H.J. The diagnosis of the conductive olfactory loss. Laryngoscope. 2001;11:9–14. doi: 10.1097/00005537-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Busaba N.Y. Is imaging necessary in the evaluation of the patient with an isolated complaint of anosmia? Ear Nose Throat J. 2001;80:892–896. [PubMed] [Google Scholar]
- 28.Smith D.V. Assessment of patients with taste and smell disorders. Acta Otolaryngol Suppl (Stockh) 1988;458:129–133. doi: 10.3109/00016488809125116. [DOI] [PubMed] [Google Scholar]
- 29.Cain W.S., Gent J.F., Goodspeed R.B., Leonard G. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope. 1988;98:83–88. doi: 10.1288/00005537-198801000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Doty R.L., Shaman P., Kimmelman C.P., Dann M.S. University of Pennsylvania Smell Identification Test: a rapid quantitative olfactory function test for the clinic. Laryngoscope. 1984;94:176–178. doi: 10.1288/00005537-198402000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Doty R.L., Marcus A., Lee W.W. Development of the 12-item Cross-Cultural Smell Identification Test (CC-SIT) Laryngoscope. 1996;106(3 pt 1):353–356. doi: 10.1097/00005537-199603000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Wolfensberger M., Schnieper I., Welge-Lussen A. Sniffin'Sticks: a new olfactory test battery. Acta Otolaryngol. 2000;120:303–306. doi: 10.1080/000164800750001134. [DOI] [PubMed] [Google Scholar]
- 33.Hummel T., Konnerth C.G., Rosenheim K., Kobal G. Screening of the olfactory function with a four-minute odor identification test: reliability, normative data and investigations in patients with olfactory loss. Ann Otol Rhinol Laryngol. 2001;110(10):976–981. doi: 10.1177/000348940111001015. [DOI] [PubMed] [Google Scholar]
- 34.Davidson T.M., Murphy C. Rapid clinical evaluation of anosmia. The alcohol sniff test. Arch Otolaryngol Head Neck Surg. 1997;123:591–594. doi: 10.1001/archotol.1997.01900060033005. [DOI] [PubMed] [Google Scholar]
- 35.Yousem D.M., Oguz K.K., Li C. Imaging of the olfactory system. Semin Ultrasound CT MR. 2001;22:456–472. doi: 10.1016/s0887-2171(01)90001-0. [DOI] [PubMed] [Google Scholar]
- 36.Davidson T.M., Murphy C., Jalowayski A.A. Smell impairment. Can it be reversed? Postgrad Med. 1995;98:107–118. [PubMed] [Google Scholar]
- 37.Golding-Wood D.G., Holmstrom M., Darby Y., Scadding G.K., Lund V.J. The treatment of hyposmia with intranasal steroids. J Laryngol Otol. 1996;110:132–135. doi: 10.1017/s0022215100132967. [DOI] [PubMed] [Google Scholar]
- 38.Eichel B.S. Improvement of olfaction following pansinus surgery. Ear Nose Throat J. 1994;73(4):248–250. [PubMed] [Google Scholar]
- 39.Jafek B.W., Hill D.P. Surgical management of chemosensory disorders. Ear Nose Throat J. 1989;68:398–400. [PubMed] [Google Scholar]
- 40.Min Y.G., Yun Y.S., Song B.H., Cho Y.S., Lee K.S. Recovery of nasal physiology after functional endoscopic sinus surgery: olfaction and mucociliary transport. ORL J Otorhinolaryngeal Relat Spec. 1995;57(5):264–268. doi: 10.1159/000276755. [DOI] [PubMed] [Google Scholar]
- 41.Yamagishi M., Hasegawa S., Suzuki S., Nakemura H., Nakano Y. Effect of surgical treatment of olfactory disturbance caused by localized ethmoiditis. Clin Otol. 1989;14(5):405–409. doi: 10.1111/j.1365-2273.1989.tb00394.x. [DOI] [PubMed] [Google Scholar]
- 42.Klimek L., Moll B., Amedee R.G., Mann W.J. Olfactory function after microscopic endonasal surgery in patients with nasal polyps. Am J Rhinol. 1997;11:251–255. doi: 10.2500/105065897781446621. [DOI] [PubMed] [Google Scholar]
- 43.Markert J.M., Hartshorn D.O., Farhat S.M. Paroxysmal bilateral dysosmia treated by resection of the olfactory bulbs. Surg Neurol. 1993;40(2):160–163. doi: 10.1016/0090-3019(93)90129-o. [DOI] [PubMed] [Google Scholar]
- 44.Leopold D.A., Loehrl T.A., Schwob J.E. Long-term follow-up on surgically treated phantosmia. Arch Otolaryngol Head Neck Surg. 2002;128:642–647. doi: 10.1001/archotol.128.6.642. [DOI] [PubMed] [Google Scholar]
- 45.Bartoshuk L.M., Duffy V.B. Taste and smell in aging. In: Masoro E.J., editor. Handbook of physiology. Oxford University Press; New York: 1995. pp. 363–375. [Google Scholar]
- 46.Bull T.R. Taste and chorda tympani. J Laryngol Otol. 1965;79:479–493. doi: 10.1017/s0022215100063969. [DOI] [PubMed] [Google Scholar]
- 47.Constanzo R.M., Zasler N.D. Head trauma. In: Getchell T., Doty R.L., Bartoshuk L.M., editors. Smell and taste in health and disease. Raven Press; New York: 1991. pp. 711–730. [Google Scholar]
- 48.Deems R.O., Friedman M.I., Friedman L.S., Maddrey W.C. Clinical manifestations of olfactory and gustatory disorders associated with hepatic and renal disease. In: Getchell T., Doty R.L., Bartoshuk L.M., editors. Smell and taste in health and disease. Raven Press; New York: 1991. pp. 805–816. [Google Scholar]
- 49.Hummel T., Erras A., Kobal G. A test for the screening of taste function. Rhinology. 1997;35(4):146–148. [PubMed] [Google Scholar]
- 50.Mueller C., Kallert S., Renner B., Stiassny K., Temmel A.F., Hummel T. Quantitative assessment of gustatory function in a clinical context using impregnated “taste strips”. Rhinology. 2003;41(1):2–6. [PubMed] [Google Scholar]
- 51.Ahne G., Erras A., Hummel T., Kobal G. Assessment of the gustatory function by means of tasting tablets. Laryngoscope. 2000;110(8):1396–1401. doi: 10.1097/00005537-200008000-00033. [DOI] [PubMed] [Google Scholar]
- 52.Ripamonti C., Zecca E., Brunelli C., Fulfaro F., Villa S., Balzarini A. A randomized, controlled clinical trial to evaluate the effects of zinc sulfate on cancer patients with taste alterations caused by head and neck irradiation. Cancer. 1998;82(10):1938–1945. doi: 10.1002/(sici)1097-0142(19980515)82:10<1938::aid-cncr18>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 53.Kventon J., Bartoshuk L. Taste. In: Bailey B.J., Pillsbury H.C., Newlands S.D., editors. Head and neck surgery–otolaryngology. 3rd edition. Lippincott Williams & Wilkins; Philadelphia: 2001. pp. 509–520. [Google Scholar]


