The Ebola virus outbreak showed how unprepared the world was for an epidemic emergency. A new vaccine coalition hopes to prevent the same mistakes from being repeating. Talha Burki reports.
The World Economic Forum in Davos, Switzerland, saw the launch of an ambitious global initiative aimed at preventing epidemic emergencies. The Coalition for Epidemic Preparedness Innovations (CEPI) plans to develop vaccines that can be quickly deployed in the event of an infectious disease outbreak. It is the first concrete action to follow the recommendations of the various post-Ebola panels. The 2014–16 west African Ebola outbreak infected more than 28 000 people and killed in excess of 11 000. It caused chaos in the three nations at the centre of the epidemic, traumatising survivors and witnesses, and leaving lingering concerns about the long-term effects of Ebola virus infection. A vaccine might have made all the difference.
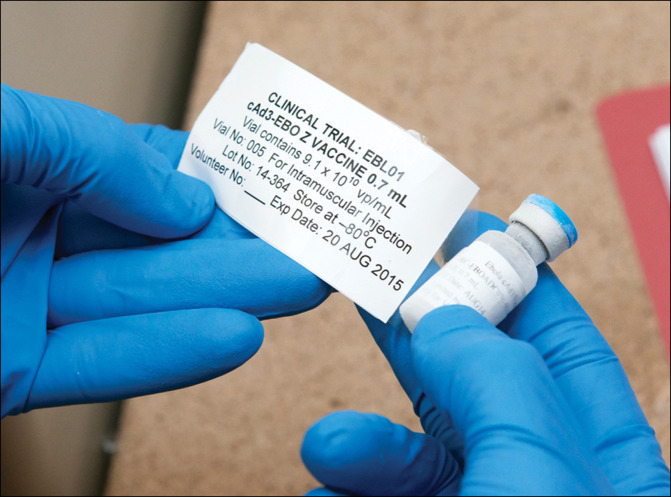
“There were potential Ebola vaccines that had shown effectiveness in animal models as far back as 2005”, explains John-Arne Røttingen, (Norwegian Institute of Public Health and interim CEO of CEPI). “If those vaccines had then been taken forward in clinical development, we could have had stockpiles of phase 3-ready vaccines to use both in larger trials and as an emergency countermeasure in the epidemic.” Thousands of lives could have been saved. In the midst of the Ebola crisis, vaccines were rushed through development; over a dozen clinical trials were planned and conducted in less than a year. But by the time the vaccines were ready for protection trials, the epidemic had all but burned out.
“Ebola was a huge wake-up call”, said Røttingen. The traditional approach of relying on the public sector for basic research and the private sector to develop specific technologies breaks down if there is no viable market, and this can have catastrophic consequences. “The reports from all the high-level panels and commissions that came afterwards pointed to one thing: we need a new financing mechanism for research and development for products for epidemics”, concluded Røttingen.
CEPI provides such a mechanism. A coalition of some 200 organisations, it intends to bring four to six vaccine candidates to the end of phase 2 trials by 2021. It will investigate vaccines for the non-Zaire strains of the Ebola virus, but its major focus will be Lassa, MERS-CoV, and Nipah. CEPI's scientific advisory board chose the three diseases based on a criteria that included epidemic potential and the public health benefit of a vaccine. Market failure is a prerequisite. “Our purpose is not to invest in things like the influenza vaccine, where the normal market mechanisms work reasonably well”, said Peter Piot, vice chair of the interim board and director of the London School of Hygiene and Tropical Medicine (LSHTM). The selected viruses all appear on WHO's 2017 list of priority diseases—a roster of pathogens identified by the organisation as being in urgent need of research and development (other priority diseases include Crimean Congo Haemorrhagic Fever and Rift Valley Fever).
In the sporadic outbreaks of MERS-CoV and Nipah to have occurred thus far, case fatality rates have exceeded one in three. Mortality from Lassa is much lower, hovering at around 1%. There are an estimated 200 000–300 000 cases per year. 80% of infected patients have mild or non-existent symptoms. But the remaining patients are badly affected, and among these cases mortality is high. When Lassa patients enter hospital, particularly in west Africa where the disease is endemic, there is a high risk of nosocomial infection. Indeed, the first identified case of Lassa fever was a nurse. The Ebola outbreak savagely demonstrated the mayhem that can ensue when infections take hold in health-care institutions.
“We consider Lassa to be an important priority from a public health point-of-view; there is certainly the potential for outbreaks with serious clinical outcomes”, explains Røttingen. Moreover, the science is amenable. “There is a great opportunity here; a vaccine looks very achievable”, said Røttingen. As of mid-2016, there were seven potential vaccines in preclinical development for Lassa. Nipah had 20 agents at the same stage, while MERS-CoV had eight agents in preclinical development, and eight in phase 1 trials. “The essential idea is to have a stockpile of vaccine on hand for when there is an epidemic”, added Piot. CEPI will not be involved in early preclinical work, nor will it take the vaccines to full development. “You need an epidemic to test the vaccine's efficacy”, said Piot.
© 2017 Rob Judges/Oxford University Images/Science Photo Library
© 2017 Valeriano Di Domenico/World Economic Forum
Alongside its disease-specific activities, CEPI will work on developing adaptable vaccine technology platforms that can be deployed against new pathogens. All of which is expensive. Governments, the Wellcome Trust, and the Bill & Melinda Gates Foundation have already pledged US$540 million, and the European Commission has promised to invest an additional €250 million in investment and co-funding arrangements. That is over halfway to the $1 billion that CEPI has requested to fund its activities until 2021, but if the costs of pilot manufacturing and stockpiling are included in the calculations, CEPI would require something closer to $3·5 billion.
It is an investment worth making. The Ebola outbreak alone cost $2·2 billion. Røttingen draws a comparison with fire-fighting services. “Most places never need to call out the fire brigade, but that does not mean we should stop investing in fire stations and fire engines”, he told The Lancet Infectious Diseases. “We need to think in a similar way when it comes to technologies for epidemics; the only way forward is to set up an approach across governments and foundations so that we can collectively pay our global health insurance premiums.”
CEPI will co-ordinate and fund this approach. “But we are not going to be a passive research funder—we will definitely have a very active, portfolio approach to our investments”, said Røttingen. In order to deliver the targeted phase 3-ready vaccines, CEPI will probably have to invest in eight or nine candidates. “For sure, we will put money into vaccines which will fail, we will have to know when to cut our losses”, added Røttingen. The pharmaceutical and biotechnology companies that join the coalition do so on the understanding that this is not a venture in which profits can be made (although costs will be covered). There are sound business reasons for them to become involved nonetheless. In an epidemic, the large vaccine manufacturers are commonly called upon anyway, but they have not usually prepared for this eventuality. They may need to shut down ongoing production of other vaccines to accommodate demands for the new vaccine. During the Ebola crisis, the manufacture of the rotavirus vaccine was temporarily halted.
Moreover, the platforms developed for CEPI could be put to work to develop vaccines for high-burden diseases for which there are lucrative markets. Smaller companies that only have a single innovative technology may be looking for the chance to demonstrate that it works. CEPI offers such an opportunity. In fact, the coalition has had no trouble attracting participants. Pharmaceutical companies, biotechnology firms, donor nations, the low-income and middle-income countries who are likely to need the vaccines, the Wellcome Trust and the Bill and Melinda Gates Foundation have all signed up. “Everyone who is part of the solution is with us”, asserted Piot. “It is the first time we have had such an inclusive coalition—all the parties we need to produce the vaccine and make sure it gets to where it is needed”.
Harvard University's Ashish Jha was part of the Harvard–LSHTM Independent Panel on the Global Response to Ebola (as was Piot). He welcomed the new initiative. “CEPI is conceptually fantastic, it begins to get ahead of the old model, and what they have pulled off in terms of the coalition and its funding is remarkable”, he told The Lancet Infectious Diseases. But he cautioned against unrealistic expectations. After all, vaccines are only one part of the solution to emerging epidemics. The Ebola and Zika crises were exacerbated by the lack of rapid diagnostics. “These are an incredibly important tool for public health, and there has been substantial underinvestment for many years”, said Jha. And, of course, vaccines can do little to help patients who are already sick. Jha pointed out that during the Ebola outbreak, the dearth of good treatment meant that hospitals acquired a reputation as simply a place to die and patients began to stay away. “CEPI is a really important first step, and it is clearly part of the research and development response that we urgently need, but we cannot allow the post-Ebola agenda to stop here”, concluded Jha.
Aside from financing, the main obstacle facing CEPI is the uncertainty that surrounds any attempt at biomedical innovation. There is no guarantee that the targeted virus will not resist all attempts to craft a vaccine—just ask researchers toiling away at HIV. CEPI will remain in its start-up phase for the rest of the year. When it gets going in earnest, it will need a leader who can hold the coalition together and retain the energy and focus that has marked its inception. But given the expertise and experience of CEPI's participants, there is plenty of cause of optimism. From the horror of the Ebola virus outbreak, a safer world may emerge.