Tigecycline, in vitro studies
P801: Addition of a biocatalytic oxygen-reducing agent may be required in the absence of fresh media (<12 hours old) when testing tigecycline using broth microdilution
T. Stevens, B. Johnson, S. Bouchillon, J. Johnson, D. Hoban, M. Dowzicky, P. Bradford (Schaumburg, Pearl River, USA)
Objectives: Tigecycline (TGC), a new glycylcycline antimicrobial in development has demonstrated excellent in vitro activity against Gram-positive and -negative pathogens. Recent reports suggest that TGC MIC values, against some organisms, may be elevated if broth used in microdilution panels is (>12 hours old (aged). The NCCLS has tentatively recommended that testing of TGC be performed in broth that is (<12 hours old (fresh). This study looks at the difference between panels using fresh broth, aged broth and broth with a biocatalytic oxygen-reducing agent (BORA) added to compensate for any potential broth differences.
Materials and Methods: Testing was performed on approximately 120 organisms including: E. coli; K. pneumoniae; M. catarrhalis; S. epidermidis; and S. pneumoniae. The BORA used in this study is Oxyrase® for Broth at 2% concentration. TIG microdilution panels evaluated in this study include: panels and aged broth without oxyrase (Aged); panels and aged broth with oxyrase (AO); panels and fresh broth without oxyrase (Fresh); and panels and fresh broth with oxyrase (FO). Panels and aged broth were prepared by Microscan. Fresh broth was prepared internally. Each organism was tested on all four panel types. Quality controls were performed using NCCLS approved ATCC strains.
Results: Combined test results showed an MIC correlation (with in 1 log2 dilution) as follows: 97.5% between Fresh/AO; 85.6% between Fresh/Aged; 94.3% between FO/AO; and 87.9% between FO/Aged. Quality controls ranges for FO, Fresh and AO were all in compliance, but Aged panels were out of range 29.3% of the time.
Conclusion: The addition of a BORA to aged broth produced results equivalent to fresh broth without a BORA.
P802: Global in vitro antibacterial activity of tigecycline against methicillin-resistant and methicillin-sensitive Staphylococcus aureus isolates from the Tigecycline Evaluation Surveillance Trial (TEST)
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Objectives: Despite the introduction of new antimicrobials to treat resistant gram-positive bacteria, Staphylococcus aureus continues to be a therapeutic challenge for the clinician. Glycylcyclines are showing the promise of significant activity against many gram-positive pathogens including methicillin-resistant S. aureus. Tigecycline, the first glycylcycline to enter clinical trials, has shown excellent activity against Staphylococcus spp. This study was initiated to evaluate the in vitro activity of tigecycline as compared with those of 9 comparator agents (ampicillin, amoxicillin-clavulanic acid, imipenem, ceftriaxone, levofloxacin, minocycline, vancomycin, linezolid, piperacillin-tazobactam) against S. aureus including methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive Staphylococcus aureus (MSSA) from multinational evaluation centres in the TEST program.
Methods: A total of 1245 clinical isolates were identified to the species level at each of 15 sites in 8 countries and confirmed by the
central laboratory. Isolates were collected between January 2004 and November 2004. MICs were determined by each participating laboratory using supplied broth microdilution panels from Dade MicroScan. All testing was performed according to NCCLS guidelines and manufacturer's instructions.
Results: The MICs of tigecycline ranged from 0.06 to 1 mcg/mL for all isolates of S. aureus. Tigecycline's MIC50/MIC90 of 0.12/0.25 mcg/mL, respectively, against MSSA was similar to imipenem and minocycline and 4/8 fold lower than the remaining comparative agents. Tigecycline's MIC50/MIC90 of 0.25/0.5 mcg/mL, respectively, against MRSA was 8/4 fold lower than vancomycin, 2/4 fold lower than minocycline and 4/8 fold lower than linezolid. All isolates of S. aureus were inhibited by tigecycline at an MIC of 1 mcg/mL regardless of methicillin phenotype.
Conclusion: The in vitro activity of tigecycline was comparable in all S. aureus tested regardless of methicillin phenotype. Tigecycline activity against MRSA was more potent than all antimicrobial agents tested in this study including imipenem, minocycline, linezolid, and vancomycin.
P803: Tigecycline Evaluation Surveillance Trial (TEST) – global in vitro antibacterial activity against selected species of Enterobacteriaceae
B. Johnson, S. Bouchillon, T. Stevens, J. Johnson, D. Hoban, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Rapid increasing resistance in nosocomial pathogens has always been a challenge for clinicians and hospital infection control. Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most species of Enterobacteriaceae as well as Gram positives, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against members of Enterobacteriaceae (mainly E. coli, Klebsiella spp., Enterobacter spp., and Serratia spp.) collected from hospitals in North America, Europe and Asia.
Methods: A total of 3204 clinical isolates of Enterobacteriaceae were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Tigecycline's activity was equivalent to imipenem presenting a MIC50/MIC90 of 0.25/1 mcg/mL against all strains of Enterobacteriaceae. In comparison to other antimicrobials tested, the MIC90 of 1 mcg/mL for tigecycline was also the lowest being 8 fold lower than commonly prescribed broad spectrum antimicrobials such as ceftriaxone, levofloxacin, and minocycline and 16 fold lower than ceftazidime and piperacillin/tazobactam. The frequency of ESBL production among K. pneumoniae and E. coli was found to be 10.3% and 2.2%, respectively. Tigecycline inhibited >98% of all E. coli and K. pneumoniae ESBL producers at an MIC of 2 mcg/mL. Approximately 20% of Enterobacter spp. and Serratia spp. presented resistance to third generation cephalosporins (ceftazidime and ceftriaxone) suggestive of AmpC-type resistance. Tigecycline also inhibited a majority of these isolates with an MIC90 of 2 mcg/mL.
Conclusion: Tigecyclines in vitro activity was comparable to the activity of a broad spectrum antimicrobial, carbapenem (imipenem), and greater than other commonly prescribed broad spectrum agents tested in this study. The presented data suggest that tigecycline may be an effective therapeutic option against both susceptible strains of Enterobacteriaceae and multi-drug resistant strains regardless of degree or type of resistance.
P804: Tigecycline Evaluation Surveillance Trial (TEST) – in vitro antibacterial activity against selected species of Enterobacteriaceae in the United States
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have a potent expanded broad spectrum activity against most species of Enterobacteriaceae as well as gram-positive, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against isolates of Enterobacteriaceae collected from hospitals across the USA.
Methods: A total of 2446 clinical isolates, collected in 2004, were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: The efficacy of all broad spectrum antimicrobial agents still remain highly active against Enterobacteriaceae in the United States. The susceptibility rates for amikacin, cefepime, ceftazidime, ceftriaxone, imipenem, levofloxacin, minocycline and piperacillin/tazabactam are 99.3%, 97.5%, 89%, 92.2%, 98.8%, 85.5%, 85.7% and 91.8%, respectively. Tigecycline's activity was similar to imipenem presenting a MIC50/MIC90 of 0.25/1 mcg/ml against all strains of Enterobacteriaceae. The frequency of ESBL production among K. pneumoniae and E. coli was found to be 8.5% and 2.2%, respectively. Tigecycline successfully inhibited >98% of all E. coli and K. pneumoniae ESBL producers at a MIC of 2 mcg/ml. It was also noticed unusual resistance to imipenem in 29 of these isolates. While still under more detailed analysis, preliminary data have shown that tigecycline presented a MIC50/MIC90 of 1/2 mcg/ml against these multi-resistant isolates.
Conclusion: Most of broad spectrum antimicrobial agents still remain active against Enterobacteriaceae from the US. Tigecycline's activity was comparable to the activities of broad spectrum antimicrobials and with greater activity against most ESBL and AmpC producing isolates. Tigecycline also showed in vitro activity against isolates that were intermediate or resistant Table for P805
to imipenem, which in many instances is considered as a last therapeutic option. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both susceptible strains of Enterobacterieaceae and multi-drug resistant strains regardless of degree or type of resistance.
P805: Tigecycline Evaluation Surveillance Trial (TEST) – In vitro antibacterial activity against Gram-positive and Gram-negative pathogens in the United States
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered Gram-positive and Gram-negative species, including anaerobic pathogens responsible for community and hospital infections. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against gram negative rods in addition to linezolid, penicillin and vancomycin for the gram positive species. Isolates were collected from hospitals in the United States throughout 2004.
Methods: A total of 4100 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: As shown in the table below, tigecycline's activity was similar to imipenem against Enterobacteriaceae. It inhibited multi-resistant ESBL and AmpC producers with a MIC equal or lesser than 2 mcg/ml. Tigecycline also showed in vitro activity with a MIC90 2 mcg/ml against 29 imipenem resistant Enterobacteriaceae strains. Although similar to other classes of broad spectrum antimicrobial agents against non-fermenters, tigecycline was especially active against Acinetobacter spp. with the lowest MIC90 of 2 mcg/ml. Tigecycline inhibited S. aureus with MIC90 of 0.25 mcg/ml for both MSSA and MRSA isolates. Against enterococci, tigecycline's MIC90 was consistent regardless of vancomycin susceptibility.
Conclusion: Tigecycline's in vitro activity was comparable or greater than most commonly prescribed broad spectrum antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both susceptible common gram-positive and gram-negative pathogens, including multi-drug resistant strains regardless of degree or type of resistance.
|
Enterobacteriaceae (n=2,446) |
P. aeruginosa (n=390) |
Acinetobacter spp. (n=261) |
S. aureus (n=494) |
Enterococcus spp. (n=509) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | |
| Tigecycline | 0.03–16 | 0.250 | 1 | 0.25–>16 | 16 | >16 | 0.03–4 | 0.5 | 2 | 0.03–1 | 0.12 | 0.25 | 0.3–0.5 | 0.06 | 0.12 |
| Amikacin | 0.5–>64 | 2 | 4 | ≤0.5–>64 | 4 | 8 | ≤0.5–>64 | 4 | 32 | ||||||
| Ampicillin | 0.5–>32 | >32 | >32 | 4–>32 | >32 | >32 | ≤0.5–>32 | >32 | >32 | 0.06–>16 | 16 | >16 | 0.25–>16 | 1 | >16 |
| Cefepime | 0.5–>32 | 0.5 | 1 | ≤0.5–>32 | 8 | 32 | ≤0.5–>32 | 16 | >32 | ||||||
| Ceftazidime | 8–>32 | 8 | 16 | ≤8–>32 | ≤8 | 32 | ≤8–>32 | 32 | >32 | ||||||
| Ceftriazone | 0.06–>64 | 0.06 | 8 | ≤0.06–>64 | >64 | >64 | ≤0.06–64 | 64 | >64 | 0.5–>64 | 8 | >64 | 1–>64 | >64 | >64 |
| Imipenem | 0.12–>16 | 0.5 | 1 | 0.25–>16 | 1 | 8 | ≤0.06–>16 | 0.5 | 16 | 0.12–>16 | 0.250 | 16 | 0.25–>16 | 1 | >16 |
| Levofloxacin | 0.008–>8 | 0.06 | 8 | ≤0.008–>8 | 2 | >8 | 0.015–>8 | 8 | >8 | 0.06–>32 | 1 | >32 | 0.5–>32 | 32 | >32 |
| Minocycline | 0.5–>16 | 2 | 8 | ≤0.5–>16 | >16 | >16 | ≤0.5–>16 | 1 | 8 | 0.25–>8 | 0.25 | 0.25 | 0.25–>8 | 8 | >8 |
| Pip/tazobactam | 0.06–>128 | 1 | 16 | 0.12–>128 | 4 | 128 | ≤0.06–>128 | 32 | >128 | 0.25–>16 | 4 | >16 | 0.5–>16 | 2 | >16 |
| Penicillin | 0.06–>8 | >8 | >8 | 0.5–>8 | 2 | >8 | |||||||||
| Linezolid | 0.5–4 | 2 | 2 | 0.5–>8 | 2 | 2 | |||||||||
| Vancomycin | 0.25–4 | 0.5 | 1 | 0.25–>32 | 1 | >32 | |||||||||
P806: Tigecycline Evaluation Surveillance Trial (TEST) – In vitro antibacterial activity against Grampositive and Gram-negative pathogens in Europe
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline, and piperacillin/tazobactam against gram negative rods in addition to linezolid, penicillin, and vancomycin for the gram positive species. Isolates were collected from hospitals located in Germany, Italy, Spain, and United Kingdom throughout 2004.
Methods: A total of 1064 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: As shown in the table below, tigecycline's activity was similar to imipenem against Enterobacteriaceae. It inhibited multi-resistant ESBL and AmpC producers with MICs equal or lesser than 2 mcg/ml. Although similar to other classes of broad spectrum antimicrobial agents against glucose non-fermenters, tigecycline was especially active against Acinetobacter spp. presenting the lowest MIC90 of 1 mcg/ml. Tigecycline inhibited S. aureus with a MIC90 of 0.25 mcg/ml regardless of sensitivity or resistance to methicillin. The same results were noticed against enterococci where tigecycline's MIC90 of 0.25 mcg/ml was consistent regardless of vancomycin susceptibility.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both aerobic gram-positive and aerobic gram-negative bacteria, including multi-drug resistant strains regardless of degree or type of resistance.
|
Enterobacteriaceae (n=627) |
P.aeruginosa (n=101) |
Acinetobacter spp. (n=74) |
S. aureus (n=116) |
Enterococcus spp. (n=146) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | |
| Tigecycline | 0.03–4 | 0.250 | 1 | 0.5–>16 | 8 | >16 | ≤0.008–4 | 0.25 | 1 | 0.06–0.5 | 0.12 | 0.25 | 0.03–0.5 | 0.12 | 0.250 |
| Amikacin | 0.5–32 | 2 | 4 | ≤0.5–16 | 4 | 8 | ≤0.5–>64 | 4 | >64 | ||||||
| Ampicillin | 1–>32 | >32 | >32 | 4–>32 | >32 | >32 | ≤0.5–>32 | >32 | >32 | 0.06–>16 | 16 | >16 | 0.25–>16 | 1 | >16 |
| Cefepime | 0.5–>32 | 0.5 | 4 | 1–>32 | 4 | 32 | ≤0.5–>32 | 16 | >32 | ||||||
| Ceftazidime | 8–>32 | 8 | 32 | ≤8–>32 | ≤8 | 32 | ≤8–>32 | 32 | >32 | ||||||
| Ceftriazone | 0.06–>64 | 0.06 | 16 | 4–>64 | >64 | >64 | 0.12–>64 | >64 | >64 | 0.5–>64 | 4 | >64 | 4–>64 | >64 | >64 |
| Imipenem | 0.25–4 | 0.5 | 1 | 0.5–>16 | 1 | 16 | 0.12–>16 | 0.5 | 16 | 0.12–>16 | 0.25 | >16 | 0.25–>16 | 1 | >16 |
| Levofloxacin | 0.008–>8 | 0.06 | 8 | 0.03–>8 | 1 | >8 | 0.015–>8 | 4 | >8 | 0.06–16 | 0.25 | 8 | 0.25–>32 | 8 | >32 |
| Minocycline | 0.5–>16 | 2 | 8 | 2–>16 | >16 | >16 | ≤0.5–16 | 1 | 8 | 0.25–8 | 0.25 | 0.5 | 0.25–>8 | 8 | >8 |
| Pip/tazobactam | 0.12–>128 | 1 | 8 | ≤0.25–>128 | 4 | 128 | ≤0.06–>128 | 16 | >128 | 0.25–>16 | 0.5 | >16 | 1–>16 | 4 | >16 |
| Penicillin | 0.06–>8 | >8 | >8 | 1–>8 | 4 | >8 | |||||||||
| Linezolid | 1–4 | 2 | 4 | 1–>4 | 2 | 2 | |||||||||
| Vancomycin | 0.5–2 | 1 | 1 | 0.5–2 | 1 | 2 | |||||||||
P807: Tigecycline Evaluation Surveillance Trial (TEST) – In vitro antibacterial activity against Grampositive and Gram-negative pathogens in Asia
B. Johnson, S. Bouchillon, T. Stevens, J. Johnson, D. Hoban, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against gram negative rods in addition to linezolid, penicillin and vancomycin for the gram positive species. Isolates were collected from hospitals located in Asia throughout 2004.
Methods: A total of 424 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Tigecycline's activity was similar to imipenem against Enterobacteriaceae with MIC50/MIC90of 0.25/1 mcg/ml. Resistance to third generation cephalosporin was found in 63.2% of E. coli and 77.8% of K. pneumoniae consistent with ESBL phenotype. Tigecycline inhibited ESBL and AmpC producers with MICs equal or lesser than 1 mcg/ml. Although similar to other classes of broad spectrum antimicrobial agents against glucose non-fermenters, tigecycline was especially active against Acinetobacter spp. presenting the lowest MIC90 of 1 mcg/ml. Tigecycline successfully inhibited S. aureus with MIC90 of 0.25 mcg/ml regardless of sensitivity or resistance to methicillin. Same phenomenon was noticed against enterococci where tigecycline's MIC90 of 0.12 mcg/ml was consistent regardless of vancomycin susceptibility.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both aerobic gram-positive and aerobic gram-negative bacteria, including multi-drug resistant strains regardless of degree or type of resistance.
P808: Tigecycline Evaluation Surveillance Trial (TEST) – European in vitro antibacterial activity against selected species of Enterobacteriaceae
B. Johnson, S. Bouchillon, T. Stevens, J. Johnson, D. Hoban, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most species of Enterobacteriaceae as well as gram-positive, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against isolates of Enterobacteriaceae collected from hospitals in Germany, Italy, Spain and United Kingdom.
Methods: A total of 627 clinical isolates, collected in 2004, were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: It was observed that the in vitro activity of all broad spectrum antimicrobial agents still remains highly active against Enterobacteriaceae in Europe. The susceptibility rates for amikacin, cefepime, ceftazidime, ceftriaxone, imipenem, levofloxacin, minocycline, and piperacillin/tazobactamare 99.8%, 94.6%, 84.8%, 87.6%, 100%, 86.1%, 84.5%, and 92.2%, respectively. Tigecycline's activity was similar to the most effective antimicrobial agent, imipenem (100% susceptibility) presenting a MIC50/MIC90 of 0.25/1 mcg/ml against all strains of Enterobacteriaceae. The frequency of ESBL production among K. pneumoniae and E. coli was found to be 21.7% and 2.4%, respectively. Tigecycline inhibited 100% of all ESBL producing E. coli at a MIC of 0.5 mcg/ml and at a MIC of 4 mcg/ml for ESBL producing K. pneumoniae. Approximately 30% of Enterobacter spp. and 6% of Serratia marcescens presented resistance to third generation cephalosporins (ceftazidime and ceftriaxone) suggestive of AmpC-type resistance.
Conclusion: Most of the broad spectrum antimicrobial agents still remain active against European representatives of Enterobacteriaceae. Tigecycline's in vitro activity was comparable to the activities of all broad spectrum antimicrobials with greater activity against ESBL and AmpC producing isolates with a MIC 90 of 2 mcg/ml. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both susceptible strains of Enterobacterieaceae and multi-drug resistant strains regardless of degree or type of resistance.
P809: Tigecycline Evaluation Surveillance Trial (TEST) – Global in vitro antibacterial activity against Gram-positive and Gram-negative pathogens
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline, and piperacillin/tazobactam against gram negative rods in addition to linezolid, penicillin, and vancomycin for the gram positive species. Isolates were collected from hospitals in North America, Europe and Asia throughout 2004.
Methods: A total of 6383 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: As shown in the table below, tigecycline's activity was similar to imipenem against Enterobacteriaceae. It inhibited multi-resistant ESBL and AmpC producers with a MIC equal or lesser than 2 mcg/ml. Although similar to other classes of broad spectrum antimicrobial agents against non-fermenters, tigecycline was especially active against Acinetobacter spp. demonstrating the lowest MIC90 of 2 mcg/ml. Tigecycline successfully inhibited S. aureus with MIC90 of 0.25 mcg/ml regardless of sensitivity or resistance to methicillin. The same results were noticed against enterococci. Tigecycline's MIC90 was consistent regardless of vancomycin susceptibility.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against both aerobic gram-positive and aerobic gram-negative bacteria, including multi-drug resistant strains regardless of degree or type of resistance.
|
Enterobacteriaceae (n=3,804) |
P. aeruginosa (n=449) |
Acinetobacter spp. (n=612) |
S. aureus (n=733) |
Enterococcus spp. (n=785) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | |
| Tigecycline | 0.03–16 | 0.250 | 1 | 0.06–>16 | 8 | >16 | 0.008–4 | 1 | 2 | 0.03–1 | 0.12 | 0.25 | 0.3–0.5 | 0.06 | 0.12 |
| Amikacin | 0.5–>64 | 2 | 4 | ≤0.5–>64 | 4 | 8 | 0.5–>64 | 8 | >64 | ||||||
| Ampicillin | 0.5–>32 | >32 | >32 | 4–>32 | >32 | >32 | 8–>32 | >32 | >32 | 0.06–>16 | 16 | >16 | 0.25–>16 | 1 | >16 |
| Cefepime | 0.5–>32 | 0.5 | 2 | ≤0.5–>32 | 4 | 32 | 0.5–>32 | 32 | >32 | ||||||
| Ceftazidime | 8–>32 | 8 | 16 | ≤8–>32 | ≤8 | 32 | 8–>32 | >32 | >32 | ||||||
| Ceftriazone | 0.06–>64 | 0.06 | 8 | ≤0.06–>64 | >64 | >64 | 0.12–>64 | >64 | >64 | 0.5–>64 | 8 | >64 | 1–>64 | >64 | >64 |
| Imipenem | 0.12–>16 | 0.5 | 1 | 0.25–>16 | 1 | 8 | 0.25–>16 | 1 | 16 | 0.12–>16 | 0.25 | >16 | 0.25–>16 | 1 | >16 |
| Levofloxacin | 0.008–>8 | 0.06 | 8 | ≤0.008–>8 | 2 | >8 | 0.15–>8 | >8 | >8 | 0.06–>32 | 0.5 | >32 | 0.25–>32 | 32 | >32 |
| Minocycline | 0.5–>16 | 2 | 8 | ≤0.5–>16 | >16 | >16 | 0.5–>16 | 1 | 8 | 0.25–>8 | 0.25 | 0.5 | 0.25–>8 | 8 | >8 |
| Pip/tazobactam | 0.06–>128 | 1 | 16 | 0.12–>128 | 4 | 128 | 0.06–>128 | 64 | >128 | 0.25–>16 | 2 | >16 | 0.5–>16 | 4 | >16 |
| Penicillin | 0.06–>8 | >8 | >8 | 0.5–>8 | 4 | >8 | |||||||||
| Linezolid | 0 5–4 | 2 | 2 | 0.5–>8 | 2 | 2 | |||||||||
| Vancomycin | 0.25–4 | 1 | 1 | 0.25–>32 | 1 | >32 | |||||||||
P810: Tigecycline Evaluation Surveillance Trial (TEST) – Global in vitro antibacterial activity against selected species of Enterococcus spp.
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Resistance to glycopeptides in enterococci was first recognized in the late 1980s, and since then has been a major challenge to clinicians and infection control. Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to vancomycin, linezolid, ampicillin, imipenem, ceftriaxone, levofloxacin, minocycline, penicillin and piperacillin/tazobactam against members of Enterococcus spp. collected from hospitals in North America, Europe and Asia.
Methods: A total of 685 clinical isolates of Enterococcus spp. were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Of 437 E. faecalis evaluated, resistance to vancomycin in 15 (3.4%) isolates was observed. These isolates were all susceptible to linezolid and tigecycline. Tigecycline presented the lowest MIC50/MIC90 (0.06/0.12 mcg/ml) among all antimicrobial agents evaluated. Among 248 E. faecium, 50 (20.2%) were resistant to vancomycin, of which three isolates were also resistant to linezolid. Tigecycline also presented the lowest MIC50/MIC90 of 0.03/0.06 mcg/ml. Five isolates of vancomycin susceptibleE. faecalis and one vancomycin susceptible E. faecium were non-susceptible to linezolid. No abnormal resistance phenotype was observed in other Enterococcus species tested.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against Enterococcus spp. including multi-drug resistant strains regardless of degree or type of resistance.
P811: Tigecycline Evaluation Surveillance Trial (TEST) – Global in vitro antibacterial activity against selected species of glucose non-fermenting organisms
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Glucose non-fermenting gram negative rods are known to be highly resistant in hospital settings and have always been a challenge for clinicians and hospital infection control. The degree or type of resistance may be due to several sophisticated mechanisms such as production of broad spectrum beta-lactamases, efflux pumps and altered membrane permeability, inactivating most classes of antimicrobials that are available for treatment (cephalosporins, carbapenems, aminoglycosides, fluoruquinolones). Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most species of Enterobacteriaceae and selected species of non-fermenters, as well as Gram positives, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against members of Acinetobacter spp. and Pseudomonas aeruginosa collected from hospitals in North America, Europe and Asia.
Methods: A total of 2513 non-fermenting clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using supplied broth microdilution panels and interpreted according to NCCLS guidelines.
Results: The cephalosporins were ineffective towards A. baumannii (n = 424). Tigecycline showed the lowest MICs against A. baumannii with a MIC50/MIC90 of 0.5/2 mcg/ml, outperforming amikacin, 74.3% inhibition MIC50/MIC90 4/64, imipenem, 79.5% MIC50/MIC90 0.5/16, and minocycline, 85.4% MIC50/MIC90 1/8. Similar findings were found in other species of the Acinetobacter genus.
Conclusion: The presented data suggest that tigecycline may be an effective and reliable therapeutic option against strains of Acinetobacter spp., including multi-drug resistant strains regardless of degree or type of resistance.
P812: United States in vitro antibacterial activity of tigecycline against methicillin-resistant and methicillin-sensitive Staphylococcus aureus isolates from the Tigecycline Evaluation Surveillance Trial (TEST)
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M.Hackel, M.Person, M.Dowzicky (Schaumburg, Collegeville, USA)
Objective: Despite the introduction of new antimicrobials to treat resistant gram-positive bacteria, Staphylococcus aureus continues to be a therapeutic challenge for the clinician. Glycylcyclines are showing the promise of significant activity against many Gram-positive pathogens including methicillin-resistant S. aureus. Tigecycline, the first glycylcycline to enter clinical trials, has shown excellent activity against Staphylococcus spp. This study was initiated to evaluate the in vitro activity of tigecycline as compared with those of 9 comparator agents (ampicillin, amoxicillin-clavulanic acid, imipenem, ceftriaxone, levofloxacin, minocycline, vancomycin, linezolid, piperacillintazobactam) against S. aureus including methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive Staphylococcus aureus (MSSA) from 23 US centres in the TEST program.
Methods: A total of 794 clinical isolates were identified to the species level at each of participating sites and confirmed by the central laboratory. Isolates were collected throughout 2004. MICs were determined by each participating laboratory using broth microdilution panels from Dade Microscan. All testing was performed and interpreted according to NCCLS guidelines and manufacturer's instructions.
Results: Among the 794 isolates, 389 (49.0%) were found to be resistant to methicillin (MRSA). Besides the cross resistance of MRSA isolates to imipenem, ceftriaxone, penicillin, ampicillin, and piperacillin/tazobactam, it was observed a high rate of non-susceptibility to levofloxacin (74.9%). No resistance was observed against vancomycin and linezolid. The MICs of tigecycline ranged from 0.03 to 1 mcg/mL for all isolates of S. aureus, and tigecycline presented the lowest MIC50/MIC90 of 0.12/0.25 mcg/ml against MRSA isolates, being several folds lower than all the comparator agents. The MSSA isolates showed the expected profile of high resistance to ampicillin and penicillin. The only unusual pattern was the 20.4% non-susceptibility to levofloxacin. Tigecycline's MIC50/MIC90 of 0.12/0.12 was also the lowest among all MSSA isolates.
Conclusion: The in vitro activity of tigecycline was comparable in all S. aureus tested regardless of methicillin phenotype. Tigecycline activity against MRSA was more potent than all antimicrobial agents tested in this study including imipenem, minocycline, linezolid, and vancomycin.
P813: Tigecycline Evaluation Surveillance Trial (TEST) – United States in vitro antibacterial activity against selected species of Enterococcus spp.
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Resistance to glycopeptides in enterococci was first recognized in the late 1980s, and since then has been a major challenge to clinicians and infection control. Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to vancomycin, linezolid, ampicillin, imipenem, ceftriaxone, levofloxacin, minocycline, penicillin and piperacillin/tazobactam against members of Enterococcus spp. collected from hospitals in the USA.
Methods: A total of 509 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Of 276 E. faecalis evaluated, it was observed resistance to vancomycin in 8 (4.5%) isolates. These isolates were all susceptible to linezolid and tigecycline. Tigecycline presented the lowest MIC50/MIC90 (0.06/0.12 mcg/ml) among all antimicrobial agents evaluated. As a typical profile of E. faecalis, fluoroquinolone (levofloxacin) and tetracycline (minocycline) had limited activities against this species. Among 144 E. faecium, 35 (24.3%) were resistant to vancomycin, of which three isolates were also resistant to linezolid. Tigecycline also presented the lowest MIC50/MIC90 of 0.06/0.12 mcg/ml. Five isolates of vancomycin susceptible E. faecalis and one vancomycin susceptible E. faecium were non-susceptible to linezolid. No abnormal resistance phenotype was observed in other Enterococcus species tested.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against Enterococcus spp. including multi-drug resistant strains regardless of degree or type of resistance.
P814: Tigecycline Evaluation Surveillance Trial (TEST) – United States in vitro antibacterial activity against selected species of glucose non-fermenting organisms
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Glucose non-fermenting Gram negative rods are known to be highly resistant in hospital settings and have always been a challenge for clinicians and hospital infection control. The degree or type of resistance may be due to several sophisticated mechanisms such as production of broad spectrum beta-lactamases, efflux pumps and altered membrane permeability, inactivating most classes of antimicrobials that are available for treatment (cephalosporins, carbapenems, aminoglycosides, fluoruquinolones). Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most species of Enterobacteriaceae and selected species of non-fermenters, as well as Gram positives, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against members of Acinetobacter spp. and Pseudomonas aeruginosa collected from hospitals in the United States.
Methods: A total of 1687 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Tigecycline's activity against P. aeruginosa showed a MIC90 of (16 mcg/ml. Towards A. baumannii (n = 849), which cephalosporins were ineffective, Tigecycline showed the lowest MIC50/MIC90 of 0.5/2 mcg/ml outperforming amikacin MIC50/MIC90 4/32, imipenem MIC50/MIC90 0.5/16 and minocycline MIC50/MIC90 1/8. Similar findings were found in other species of Acinetobacter genus.
Conclusion: The presented data suggest that tigecycline may be an effective and reliable therapeutic option against strains of Acinetobacter spp., including multi-drug resistant strains regardless of degree or type of resistance.
P815: European in vitro antibacterial activity of tigecycline against methicillin-resistant and methicillin-sensitive Staphylococcus aureus isolates from the Tigecycline Evaluation Surveillance Trial (TEST)
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Objective: Despite the introduction of new antimicrobials to treat resistant gram-positive bacteria, Staphylococcus aureus continues to be a therapeutic challenge for the clinician. Glycylcyclines are showing the promise of significant activity against many gram-positive pathogens including methicillin-resistant S. aureus. Tigecycline, the first glycylcycline to enter clinical trials, has shown excellent activity against Staphylococcus spp. This study was initiated to evaluate the in vitro activity of tigecycline as compared with those of 9 comparator agents (ampicillin, amoxicillin-clavulanic acid, imipenem, ceftriaxone, levofloxacin, minocycline, vancomycin, linezolid, piperacillintazobactam) against S. aureus including methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive Staphylococcus aureus (MSSA) from 5 European centres in the TEST program.
Methods: A total of 216 clinical isolates were identified to the species level at each of participating sites and confirmed by the central laboratory. Isolates were collected throughout 2004. MICs were determined by each participating laboratory using broth microdilution panels from Dade Microscan. All testing was performed and interpreted according to NCCLS guidelines and manufacturer's instructions.
Results: Among the 216 isolates, 76 (35.2%) were found to be resistant to methicillin (MRSA). Besides the cross resistance of MRSA isolates to imipenem, ceftriaxone, penicillin, ampicillin, and piperacillin/tazobactam, it was observed that all of MRSA isolates were also non-susceptible to levofloxacin. No resistance was observed against vancomycin and linezolid. The MICs of tigecycline ranged from 0.06 to 0.5 mcg/mL for all isolates of S. aureus, and tigecycline presented the lowest MIC50/MIC90 of 0.25/0.25 mcg/mL against MRSA isolates, being several folds lower than all the comparator agents. The MSSA isolates showed the expected profile of high resistance to ampicillin and penicillin. Opposite to MRSA isolates, MSSA presented very little resistance to levofloxacin (2.5%). Tigecycline's MIC50/MIC90 of 0.12/0.25 was also the lowest among all MSSA isolates.
Conclusion: The in vitro activity of tigecycline was comparable in all S. aureus tested regardless of methicillin phenotype. Tigecycline activity against MRSA was more potent than all antimicrobial agents tested in this study including imipenem, minocycline, linezolid, and vancomycin.
P816: Tigecycline Evaluation Surveillance Trial (TEST) - European in vitro antibacterial activity against selected species of Enterococcus spp.
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Resistance to glycopeptides in enterococci was first recognized in the late 1980s, and since then has been a major challenge to clinicians and infection control. Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most commonly encountered species responsible for community and hospital acquired infections. The TEST program determined the in vitro activity of tigecycline compared to vancomycin, linezolid, ampicillin, imipenem, ceftriaxone, levofloxacin, minocycline, penicillin and piperacillin/tazobactam against members of Enterococcus spp. collected from hospitals in Germany, Italy, Spain and United Kingdom.
Methods: A total of 146 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Of 82 E. faecalis evaluated, resistance to vancomycin in 3 (3.6%) isolates was observed. These isolates were all susceptible to linezolid and tigecycline. Tigecycline presented the lowest MIC50/MIC90 (0.12/0.25 mcg/ml) among all antimicrobial agents evaluated. Among 40 E. faecium, 1 (5.0%) was resistant to vancomycin. Tigecycline also presented the lowest MIC50/MIC90 of 0.03/0.06 mcg/ml. No abnormal resistance phenotype was observed in other Enterococci species tested.
Conclusion: Tigecycline's in vitro activity was comparable to or greater than most commonly prescribed antimicrobials. The presented data suggest that tigecycline may be an effective and reliable therapeutic option against Enterococcus spp. including multi-drug resistant strains regardless of degree or type of resistance.
P817: Tigecycline Evaluation Surveillance Trial (TEST) – European in vitro antibacterial activity against selected species of glucose non-fermenting organisms
S. Bouchillon, T. Stevens, B. Johnson, J. Johnson, D. Hoban, M. Hackel, M. Person, M. Dowzicky (Schaumburg, Collegeville, USA)
Background: Glucose non-fermenting gram negative rods are known to be highly resistant in hospital settings and have always been a challenge for clinicians and hospital infection control. The degree or type of resistance may be due to several sophisticated mechanisms such as production of broad spectrum beta-lactamases, efflux pumps and altered membrane permeability, inactivating most classes of antimicrobials that are available for treatment (cephalosporins, carbapenems, aminoglycosides, fluoruquinolones). Tigecycline, a member of a new class of antimicrobials (glycylcyclines), has been shown to have potent expanded broad spectrum activity against most species of Enterobacteriaceae and selected species of non-fermenters, as well as Gram positives, atypicals and anaerobes. The TEST program determined the in vitro activity of tigecycline compared to amikacin, ampicillin, imipenem, cefepime, ceftazidime, ceftriaxone, levofloxacin, minocycline and piperacillin/tazobactam against members of Acinetobacter spp. and Pseudomonas aeruginosa collected from hospitals in Germany, Italy, Spain, and United Kingdom.
Methods: A total of 826 clinical isolates were identified to the species level at each participating site and confirmed by the central laboratory. Isolates were collected throughout 2004. Minimum Inhibitory Concentration (MICs) were determined by the local laboratory using broth microdilution panels and interpreted according to NCCLS guidelines.
Results: Tigecycline's activity against P. aeruginosa showed a MIC90 of (16 mcg/ml. The cephalosporins were ineffective towards A. baumannii (n = 552). Tigecycline showed the lowest MICs against A. baumannii MIC50/MIC90 of 0.25/1 mcg/ml, outperforming amikacin MIC50/MIC90 4/>64, imipenem MIC50/MIC90 0.5/16 and minocycline MIC50/MIC90 1/8. Similar findings were found in other species of Acinetobacter genus.
Conclusion: The presented data suggest that tigecycline may be an effective and reliable therapeutic option against strains of Acinetobacter spp., including multi-drug resistant strains regardless of degree or type of resistance.
P818: Antimicrobial activity of tigecycline tested against bacterial pathogens from intensive care units
H. Sader, T. Fritsche, R. Jones (North Liberty, USA)
Objectives: To evaluate the antimicrobial activity of tigecycline (TIG) and selected antimicrobials against bacterial pathogens isolated from patients hospitalized in intensive care units (ICUs) worldwide.
Methods: A total of 7129 were consecutively collected in >70 medical centres located in North America (3164), South America (1465), Europe (2428) and the Asia–Australia region (72). The isolates were collected from (no. of isolates/%): bloodstream (5349/75%), respiratory tract (746/10%), skin/soft tissue (323/5%), and urinary tract (182/3%) infections in the 2000–2004 period, and susceptibility tested by NCCLS broth microdilution methods.
Results: The antimicrobial activity of TIG and the frequency of occurrence of bacterial pathogens are summarized in the Table: All gram-positive pathogens (4817) were inhibited at <1 mg/L of TIG. Resistance (R) to oxacillin was detected in 43% of SA and 84% of CoNS, and R to vancomycin was detected in 19% of enterococci. TIG was very active against Enterobacteriaceae (ENT; 1468) with a MIC90 <1 mg/L, except for Serratia spp. 10% of E. coli and 30% of Klebsiella spp. showed an ESBL phenotype while 28% of Enterobacter spp. were R to ceftazidime. 14% of ENT showed R to ciprofloxacin. TIG and trimethoprim/sulfamethoxazole were the most active compounds against S. maltophilia (MIC90, 2 and 1 mg/L respectively). TIG was also highly active against ASP (MIC90, 1 mg/L), but PSA showed decreased S to TIG (MIC90, 16 mg/L). Non-S to imipenem (MIC, >8 mg/L) was observed in 16% of ASP and 31% of PSA isolates.
| MIC (mg/L) | Cumulative % inhibited at (mg/L): | ||||||
|---|---|---|---|---|---|---|---|
| Organism (no. tested/% of total) | 50% | 90% | 0.25 | 0.5 | 1 | 2 | 4 |
| S. aureus (SA; 2, 370/33) | 0.25 | 0.5 | 85 | 99 | 100 | ||
| Enterococci (1, 082/15) | ≤0.12 | 0.25 | 92 | >99 | 100 | ||
| Coag-neg staphylococci (CoNS; 997/14) | 0.25 | 0.5 | 74 | 97 | 100 | ||
| P. aeruginosa (PSA; 549/8) | 8 | 16 | <1 | 1 | 2 | 6 | 20 |
| E. coli (533/8) | 0.25 | 0.5 | 87 | 99 | 100 | ||
| Kiebsiella spp. (388/5) | 0.5 | 1 | 35 | 79 | 93 | 98 | 100 |
| Enterobacter spp. (285/4) | 0.5 | 1 | 21 | 75 | 91 | 96 | >99 |
| β-haemolytic streptococci (143/2) | ≤0.12 | ≤0.12 | 100 | ||||
| Acinetobacter spp, (ASP; 134/2) | 1 | 2 | 21 | 37 | 67 | 96 | 99 |
| S. pneumoniae (118/2) | ≤0.12 | ≤0.12 | 100 | ||||
| Total (7,129) | 0.25 | 2 | 68 | 84 | 89 | 91 | 94 |
Conclusions: Isolates from ICU patients showed high rates of antimicrobial R. The most alarming problems detected were vancomycin R among enterococci, ESBL mediated beta-lactam R and fluoroquinolone R among ENT, and carbapenem R among PSA and ASP. TIG exhibited potent in vitro activity against the vast majority of clinically important pathogenic bacteria (except PSA) isolated from ICU patients and may represent an excellent option for the treatment of infections in this clinical environment.
P819: Potency and spectrum of tigecycline tested against an international collection (1999–2003) of bacterial pathogens producing skin and soft tissue infections
T. Fritsche, H. Sader, M. Stilwell, R. Jones (North Liberty, USA)
Objective: Tigecycline (TIG) is the sentinel representative of the glycylcycline class to be developed as a parenteral agent targeting bacterial pathogens responsible for pneumonia, intraabdominal sepsis and SSTI. The aim of this study was to evaluate the activity and potency of TIG when tested against a large collection of bacterial pathogens causing SSTI.
Methods: Consecutive, non-duplicate bacterial isolates (3,421 strains) were collected from 1999 to 2003 from patients with documented community-acquired or nosocomial SSTI in >70 medical centres participating in the TIG surveillance program in North America (38.6%), Europe (54.0%), Latin America (3.7%) and the Asia–Pacific region (3.7%). All isolates were tested using NCCLS broth microdilution methods against TIG and representative comparator agents used for empiric and directed therapy of SSTI.
Results: SSTI pathogen rank order (top ten), potency and cumulative inhibition rates for TIG are in the Table: All SA, streptococci, enterococci, CoNS, KSP and EC were inhibited by ≤2 mg/L of TIG, along with 98% of ASP and 96% of ENT. The broad-spectrum of activity exhibited by TIG included tetracycline resistant subsets as well as MRSA, VRE, and ESBL-producing strains. Only PM and PSA isolates were less susceptible (MIC90 values at 8 and 16 mg/L, respectively).
| MIC (mg/L) |
% inhibited at MIC (mg/L) |
||||
|---|---|---|---|---|---|
| Organism (no. tested) | 50% | 90% | ≤1 | ≤2 | ≤4 |
| 1. S. aureus (SA; 1,943) | 0.25 | 0.5 | 100 | – | – |
| 2. Enterococcus spp. (328) | 0 25 | 0.5 | 100 | ||
| 3. P. aeruginosa (PSA; 209) | 8 | 16 | 6 | 12 | 34 |
| 4. β-haemolytic streptococci (184) | ≤0.06 | 0.12 | 100 | – | – |
| 5. E. coli (EC; 171) | 0.25 | 0.5 | 100 | – | – |
| 6. Coag neg staphylococci (CoNS; 168) | 0.25 | 0.5 | 99 | 100 | – |
| 7. Enterobacter spp. (ENT; 95) | 0.5 | 1 | 95 | 96 | 100 |
| 8. Kiebsiella spp. (KSP; 66) | 0.5 | 1 | 97 | 100 | – |
| 9. P. mirabilis (PM; 50) | 2 | 8 | 12 | 54 | 82 |
| 10. Acinetobacter spp. (ASP; 41) | 0.5 | 1 | 95 | 98 | 98 |
| Overall Total % Inhibited | 92 | 94 | 98 | ||
Conclusions: Among the top ten-ranked pathogens producing SSTI, 94% of isolates were inhibited by ≤2 mg/L of TIG and 98% were inhibited by ≤4 mg/L (the current NCCLS breakpoint for tetracyclines). TIG may represent a welcome choice among newer parenteral agents for the common Gram-positive and negative pathogens producing serious SSTI given in vitro testing results, thus warranting continued investigation for this indication.
P820: Tigecycline activity tested against 22,950 bloodstream infection isolates worldwide
R. Jones, H. Sader, M. Stilwell, T. Fritsche (North Liberty, USA)
Objective: To assess the activity of tigecycline (formerly GAR936), a novel glycylcycline, against recent bloodstream infection (BSI) pathogen isolates from six continents. Frequency of clinical occurrence of these pathogens was determined and their antibiograms assessed using NCCLS reference broth microdilution methods.
Methods: A total of 22,950 strains were tested by the M7–A6 (2003) method with interpretations from M100–S14 (2004). A tigecycline susceptible (S) breakpoint was defined as ≤2 mg/L for comparison purposes only, although ≤4 mg/L has been used for tetracyclines. The rank order of pathogens was: S. aureus (SA; 34.2%), coagulase-negative staphylococci (CoNS; 14.1%), E. coli (EC; 13.2%), enterococci (ENT; 12.7%), Klebsiella spp. (KSP; 5.3%), P. aeruginosa (PSA; 4.0%), Enterobacter spp. (EBS; 2.9), beta-haemolyticstreptococci (BST; 2.8%); S. pneumoniae (SPN; 2.4%), and viridans group streptococci (VgS; 1.6%). More than 20 comparison agents were tested including tetracycline (TC) and ciprofloxacin (CIP).
Results: BSI pathogens (Gram-positive and Enterobacteriaceae) tested against tigecycline are shown in the table. Tigecycline was consistently active against TC-resistant (R) strains (89–100% S versus 45–90%). MIC50:% S results for other BSI species were: P. mirabilis (4 mg/L:10), Acinetobacter spp. (0.5 mg/L:77), Serratia spp. (1 mg/L:81), S. maltophilia (1 mg/L:77) and indole-positive Proteae (1 mg/L:54). Tigecycline exhibited a broader spectrum of activity against BSI isolates when compared to CIP, TC, older aminoglycosides and imipenem. Tigecycline was not active against PSA (MIC50, 8 mg/L; 4.0% of BSI isolates).
| Organism (no. tested) | Tigecycline |
% inhibited at |
|||||
|---|---|---|---|---|---|---|---|
| 50% | 90% | ≤0.5 | 1 | *** | 4 | % *** (drug) | |
| SA (7,842) | ≤0.12 | 0.5 | 99 | 99 | 100 | – | 64 (CIP) |
| CoNS (3,230) | 0.25 | 0.5 | 97 | 99 | 100 | – | 83 (TC) |
| EC (3,022) | 0.25 | 0.25 | 99 | 99 | 99 | 100 | 65 (TC) |
| ENT(2,921) | ≤0.12 | 0.25 | 99 | 99 | 100 | – | 38 (TC) |
| KSP(1,218) | 0.5 | 1 | 84 | 95 | 98 | 99 | 89 (TC) |
| EBS (661) | 0.5 | 2 | 77 | 89 | 95 | 99 | 82 (TC) |
| βST (639) | ≤0.12 | ≤0.12 | 100 | – | – | – | 45 (TC) |
| SPN (562) | ≤0.12 | ≤0.12 | 98 | 99 | 100 | – | 45 (TC) |
| VgS (372) | ≤0.12 | ≤0.12 | 99 | 100 | – | – | 69 (TC) |
Conclusions: Tigecycline exhibited a wide spectrum of antimicrobial potency versus BSI isolates collected worldwide. Serious infections in nosocomial environments should benefit from tigecycline among the investigational Phase 3 agents focused on R strains.
P821: Evaluation of the in vitro activity of tigecycline against Gram-negative anaerobic bacteria
A. Katsandri, J. Papaparaskevas, A. Pantazatou, L.S. Tzouvelekis, G.L. Petrikkos, N.J. Legakis, A. Avlamis on behalf of The Hellenic Study Group on Gram-Negative Anaerobic Bacteria
Objectives: The evaluation of the in vitro activity of tigecycline in comparison to tetracycline, penicillin, piperacillin (tazobactam, cefoxitin, clindamycin, metronidazole and imipenem against recently isolated Gram-negative anaerobic bacteria.
Materials and methods: A total of 185 Gram-negative anaerobic clinical strains (116 Bacteroides fragilis group, 20 other Bacteroides spp. non-fragilis, 34 Prevotella spp. and 15 miscellaneous) isolated during the period 11/2002–11/2004 were tested using the E-test and the agar dilution methods on brucella agar plates supplemented with 5% horse blood, vitamin K1 and hemin. Incubation in a ChelLab Anaerobic Chamber was performed for 48 hours. Interpretation of the results was according to NCCLS guidelines. For quality control the strains B. fragilis ATCC25285 and B. thetaiotaomicron ATCC29741 were used.
Results: Overall MIC90 to tigecycline, tetracycline, penicillin, piperacillin + tazobactam, cefoxitin, clindamycin, metronidazole and imipenem were 8, 128, 256, 2, 64, 256, 1 and 0.5 mg/L, respectively, whereas MIC50 were 0.5, 16, 32, 0.125, 8, 1, 0.5 and 0.064 mg/L, respectively. Bacteroides fragilis group MIC90 were 8, 256, 256, 4, 128, 256, 1 and 0.5 mg/L, respectively, whereas MIC50 were 0.5, 16, 64, 0.25, 16, 1, 0.5 and 0.064 mg/L, respectively. At the tigecycline MIC90 concentration of 8 mg/L the compound inhibited a higher percentage of isolates than clindamycin, cefoxitin or tetracycline (which inhibited 76, 56 and 45% of the isolates, respectively). Only one strain was resistant to imipenem (MIC > 32 mg/L), having a tigecycline MIC of 8 mg/L. In addition, six of the eight strains with a metronidazole MIC > 16 mg/L had a tigecycline MIC < 1 mg/L.
Conclusions: In general, tigecycline showed better in vitro activity than clindamycin, cefoxitin, tetracycline or penicillin against Gram-negative anaerobic bacteria and somewhat lower activity than imipenem, metronidazole or piperacillin + tazobactam. Nevertheless, among most metronidazole and imipenem resistant isolates tigecycline displayed good activity. The results of this in-vitro evaluation show that tigecycline should be considered as a possible alternative for the treatment of mixed aerobic–anaerobic infections. Members of the Hellenic Study Group on Gram-Negative Anaerobic Bacteria are: A. Avlamis, C. Koutsia-Karouzou, C. Kontou-Kastelanou, A. Pangalis, E. Papafrangas, E. Trika-Grafakos, H. Malamou-Ladas and A. Vogiatzi
P822: Effect of medium type, age and aeration on the MICs of tigecycline and other tetracyclines
R. Hope, M. Warner, D.M. Livermore (London, UK)
Objectives: To ascertain the variation between MICs of tigecycline determined in broth and agar, and by NCCLS and BSAC methods. To assess the effect of adding tigecycline to the medium one day before use and of using media that had been aged for one week before addition of tigecycline and inoculation.
Method: MICs for 96 non-fastidious bacteria and 20 streptococci were determined in Mueller–Hinton broth (MHB), Mueller–Hinton agar (MHA), Iso-Sensitest broth (ISB) or Iso-Sensitest agar (ISA). Fresh antibiotic stock solutions (tigecycline, tetracycline and minocycline) were incorporated into bulk media by rolling, to minimise aeration. Preparation conditions otherwise were as follows: (a) freshly-prepared media, antibiotic added upon cooling, then inoculated; (b) freshly-prepared media, antibiotic added uponcoolingthenstoredfor1 daybeforeinoculationand(c)media stored for 7 days before addition of the antibiotic and inoculation.
Results: MICs in fresh MHB (the NCCLS reference method) were taken as a standard. For all the tetracyclines, these MICS were 0–2 doubling dilutions higher than on MHA or ISA (BSAC reference method), or in ISB. Media with tetracyclines added a day before use gave raised MICs, though rarely by more than one dilution. Tigecycline MICs were increased in 7–day-old MHB or ISB. This effect was greatest (2–3 dilutions) for the most susceptible strains (MIC ≤ 0.5 mg/L) and was absent for the resistant organisms (MIC ≥ 8 mg/L); it did not occur in agar. Minocycline MICs were not raised in aged media, and tetracycline MICs were only marginally affected. The addition of blood to the MHB largely abrogated the effect on tigecycline MIC, as did boiling the broth prior to adding the antibiotic.
Conclusion: The raised MICs of tigecycline in aged broth probably reflect inactivation by dissolved oxygen. This accords with lack of any MIC increase in newly boiled (i.e. degassed) MHB or on aged agar (which is boiled to melt before use). The effect of blood may be to add to the reducing capacity, protecting the tigecycline. At a practical level, broth MIC methods for tigecycline (e.g. the NCCLS reference method) require, freshly prepared or steamed medium; this is not a concern if agar dilution methods are used, such as that of the BSAC.
Sexually transmitted diseases
P823: Prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae in native and immigrant population (AmBITS study) in Barcelona (Spain)
M. Villa, M. Valls, A. Andreu, M. Saravanya, E. Loureiro, B. Sanz, E. Arellano, P. Saladié, M. Meroño, G. Codina (Barcelona, E)
Objectives: Assess the prevalence and the epidemiological characteristics of C. trachomatis and N. gonorrhoeae infection among patients attended in a sexually transmitted infection unit (STD) and in people who practice prostitution in the street.
Methods: 837 urine specimens (first-void), obtained from people, with or without symptoms, visited in the STD clinic and in a non-governmental organization (Ambit Dona), were studied from January 2002 to July 2003. The 342 male and 495 female were distributed in age groups (<20, 20–40, >40 years), and geographic origin: Spain (Sp) 196, South America 292, Magreb 57, Africa 88, East Europe 95, West Europe 29, and others 80. Detection of chlamydia and gonococci was performed with a standardised multiplex PCR Cobas amplicor assay.
Results: The overall prevalence of C. trachomatis was 4.4%, without differences regarding age and sex. The prevalence was 3.6% in native population and 4.7% in immigrant population, without significant differences regarding geographic origin: South America 3.8%, Magreb 1.6%, Africa 3.4%, East Europe 1.1%, West Europe 10.3%, others 2.5%. The overall prevalence of N. gonorrhoeae was 4.1%. In the native population was 4.4%, without differences regarding age and sex. The prevalence was 4.1% in the immigrant population, with no differences regarding geographic origin: South America 0.04%, Magreb 5.3%, Africa 0%, East Europe 5.3%, West Europe 6.9%, others 5%. The risk of transmission associated to the geographical origin was estimated with the odds ratio (OR), resulting for chlamydia: South America/Sp: 1.07, Magreb/Sp: 0.50, Africa/Sp: 0.95, East Europe/Sp: 3.18, West Europe/Sp: 3.12, others/Sp: 1.04 and for gonococci: South America/Sp: 1.01, Magreb/Sp: 1.31, Africa/Sp: 0.13, East Europe/Sp: 1.31, West Europe/sp: 1.74, others/Sp: 3.02.
Conclusion: The prevalence of C. trachomatis was 4.4% and for N. gonorrhoeae 4.1%. The highest OR for chlamidia and for gonococci were detected in the East and West European population. On the contrary, the African and South American countries display a similar risk of transmission compared to native population.
P824: Epidemic spread of at least one prolyliminopeptidase-negative Neisseria gonorrhoeae strain in Denmark
A. Friis-Møller, L. Berthelsen, U. Germer, H. Krogdahl, H. Fredlund, M. Unemo (Hvidovre, Copenhagen, DK; Örebro, S)
Since the year 2002 isolates of prolyliminopeptidase (PIP)-negative Neisseria gonorrhoeae (GC) have been diagnosed in Denmark especially from men, who have sex with men. Species confirmation of GC is commonly based on enzymatic reactions in commercial kits such as API NH, RapID NH, Gonocheck II and Neisseria PET, which among other reactions rely on a biochemical identification of the enzyme prolyliminopeptidase.
Objectives: To phenotypically and genotypically characterize a selection of PIP-negative GC isolates in Denmark and to investigate the possibility of a spread of one or several PIP-negative strain in the Danish community from 2002 to 2004.
Methods: Twenty-five PIP-negative GC isolated in Denmark from 23 male patients between 2002 and 2003 were genetically characterized by means of DNA sequencing of the entire porB gene and pulsed-field gel electrophoresis (PFGE) with the restriction enzymes SpeI and BglII. Phylogenetic tree was constructed with TREECON v1.3b by using neighbor-joining method. Phenotypic characterization was performed by serovar determination of the 25 isolates and antibiotic susceptibility testing of all Danish GC strains isolated in 2002–2004 (n = 953). Clinical and epidemiological data were obtained when possible.
Results: The 25 PIP-negative GC isolates were all designated as serovar IB-4 and similar MIC values were identified in the antibiograms of these isolates fingerprints were identified using SpeI and three using BglII among the 25 IB-4 isolates. Four distinguishable PFGE. However, all these isolates differed by less than six bands in both fingerprints. The phylogenetic tree analysis of the porB1b sequences, suggested that these minor differences represented the ongoing evolution of the same strain. During the period Jan. 2002 to Nov. 2004 the proportions of PIP-neg GC per year in Denmark were 15/332, 47/261 and 27/360, respectively, and the PIP-neg GC infected mostly men (only 5 women). The antibiograms of all Danish isolates 2002–2004 indicate a spread of at least one PIP-neg GC strain.
Conclusions: The results of the present study indicate a circulation of at least one N. gonorrhoeae prolyliminopeptidase-negative strain in the Danish homosexual community. An increased awareness for PIP-negative N. gonorrhoeae, which create large problems in diagnosis using e.g. API NH, RapID NH, Gonocheck II or Neisseria PET, is essential.
P825: A new recombinant antigen haemagglutination test for the serological diagnosis of syphilis
N. Chepurchenko, T. Ulanova, V. Puzyrev, L. Loginova, A. Burkov, A. Obriadina (Nizhniy Novgorod, RUS)
Introduction: Passive Treponema pallidum hemagglutination (HA) – the routine treponemal test has equal sensitivity with the fluorescent treponemal antibody absorption (FTA-ABS) test and with the enzyme immunoassay (EIA) in later stages of syphilis, but some studies have indicated that it is less sensitive in the primary stage of the disease. The use of recombinant T. pallidum antigens instead of a poorly defined mixture of antigens from wild-type T. pallidum has the potential for improving the sensitivity of hemagglutination test.
Objectives: The purpose of this study was to evaluate the diagnostic relevance of 4 recombinant proteins that efficiently model the antigenic epitope(s) of the Treponema pallidum proteins.
Methods: Four full-length recombinant proteins (TmpA, 47, 17, 15 kDa) were expressed in E. coli and then used individually to develop the hemagglutination test (HT) for the detection of anti-Treponema pallidum (anti-TP) activity in serum specimens. Serum samples (N = 267) from patients with clinically proven syphilis in various stages of the disease (primary (N = 36), secondary (N = 70), latent (N = 161)) and from normal blood donors (N = 505) were tested. 24 samples from patients with primary syphilis, 21 samples from patients with secondary and 17 samples from patients with latent stage were tested initially with commercially available hemagglutination test based on mixture of Treponema pallidum antigens (HTTP). All specimens were additionally tested for specific antibodies by commercially available enzyme immunoassay (EIA).
Results: The sensitivity of the HT for the detection of anti-TP activity in human serum specimens varied from 38.9% to 97.2% with primary syphilis sera, from 87.1% to 100% with secondary, and from 96.9% to 98.1% with latent stage sera for each protein. The TmpA was found as the most immunoreactive when serum samples from patients with untreated syphilis were tested. The sensitivity of TmpA HT was identical to those of the HTTP in cases of untreated secondary and latent syphilis and significantly higher with specimens from primary stage of disease. The overall specificity and sensitivity of the TmpA HT were comparable to those of EIA 99% and 99.6%; 98% and 99.6% respectively.
Conclusions: The results of this study indicate that the TmpA HT may be a reasonable alternative to the routine hemagglutination test and the ELISA as a confirmatory test for syphilis.
P826: Use of treponema + VDRL ViraBlot test as a useful ‘all in one’ confirmatory assay for Treponema pallidum antibodies
A. Kostoula, G. Vrioni, C. Bobogianni, C. Stergiopoulou, E. Papantoniou, S. Levidiotou (Ioannina, GR)
Objectives: As detection of Treponema pallidum subsp. pallidum by dark-field microscopy or direct immunofluorescence is possible only in the early stages of the disease, serology has become the method of choice for syphilis diagnosis. Except for conventional treponemal tests, the T. pallidum Western immunoblot assay has also been used as an alternative confirmatory assay for T. pallidum antibodies. The aim of the present study was the use of a multiparameter immunoassay, which simultaneously detects treponemal specific and lipoid antibodies, for the confirmation of syphilis antibodies.
Methods: A total of 86 serum specimens were tested including, 56 reactive sera from patients with documented treponemal infection; a specificity panel of 10 sera from normal subjects, 10 sera with Rapid Plasma Reagin (RPR) reactivity (FTA-ABS and TPHA negative), 5 Leptospira IgM serology-positive sera and 5 Borrelia burgdorferi IgG or IgM serology-positive sera. All serum samples were tested with conventional syphilis tests according to the manufacturers' instructions: RPR, Venereal Disease Research Laboratory (VDRL), T. pallidum haemagglutination (TPHA) at a serum dilution of 1:80, fluorescent T. pallidum absorption (FTA-ABS) and IgM capture enzyme immunoassay (EIA). Subsequently, the results were compared to those of the Treponema + VDRL ViraBlot IgG, IgM test (Viramed, Labor – Diagnostika), a immunoassay for the qualitative detection of specific IgG or IgM antibodies to T. pallidum using the specific treponemal proteins p47, p44.5, p17 and p15, and the quantitative determination of VDRL reaction on one nitrocellulose strip.
Results: Treponema + VDRL ViraBlot IgG and IgM tests confirmed the results for 56 serum specimens positive for T. pallidum antibodies: reactive VDRL band and at least two clear bands from p47, p44.5, p17 or p15 for IgG treponemal antibodies or at least one clear band p47, p17 or p15 for IgM treponemal antibodies. The 10 RPR reactive sera were VDRL ViraBlot reactive, but Treponema ViraBlot specific antibodies negative. None of the remaining sera reacted in tests with the Treponema + VDRL ViraBlot assay.
Conclusions: The Treponema + VDRL ViraBlot assay combining the necessary serologic markers in one test strip (i.e. specific and non-specific treponemal antigens) is a useful confirmatory test for syphilis because it increases the reliability of syphilis diagnosis with respect to current conventional techniques.
P827: The great imitator: syphilis with predominant acute severe hepatic involvement
R. Manfredi, S. Sabbatani, L. Attard, D. Pocaterra, F. Chiodo (Bologna, I)
Introduction: The liver involvement of syphilis is known since over 400 years, and proves particularly frequent in the rare congenital form. When secondary syphilis is of concern, >70% of patients (p) has a negligible or mild alteration of liver enzymes, while episodes with predominant or apparently isolated acute hepatitis are exceedingly rare.
Case reports: Two male p (one with concurrent HIV disease), were hospitalized with an initial diagnosis of acute hepatitis, on the ground of a significant increase of serum transaminiases (up to 2200 and 900 U/L of GPT, respectively), frank jaundice, elevated bilirubin (up to 11.7 and 9.6 mg/dL, respectively), and evident rise of serum alkaline phosphatase and gamma-GT. Clinical history did not show risk factors for viral hepatitis, and all laboratory examinations for major and minor hepatotropic viruses proved negative, as well as autoimmmune, dysmetabolic, or drug-induced liver damage. Repeated ultrasonography detected increased liver and spleen dimensions, in absence of other abnormalities. In the second p, histopathologic study performed after liver biopsy, showed an aspecific cholestatic hepatopathy, a moderate granulocyte and lympho-mononocyte intralobular infiltrate, appreciable necrotic foci, and a mild portal fibrosis (Knodell score 5). Only syphilis serology, performed despite the absence of significant history or clinical clues, allowed to recognize an IGM positive serology associated with TPHA titres ranging from 1:1250 and 1:680, respectively. Specific chemotherapy (i.v. penicillin G at 24 MU daily for 7 days, followed by 12 MU/day in the second p), led to a complete resolution of hepatic involvement, associated with an improvement of serology after 1 month.
Discussion: While in the majority of episodes of syphilis liver involvement remains missed or subclinical, an early diagnosis of syphilis with predominant hepatic disease remains an unresolved problem of differential diagnosis, due to the rare occurrence of isolated organ involvement compared with typical syphilis signs and symptoms, and the aspecific clinical, histopathological, and imaging picture (Jozsa L, Acta Hepatogastroenterol 1977;24:344–7; Young MF, J Clin Gastroenterol 1992;15:174–6). During the recent recrudescence of syphilis in Italy, a diagnostic suspicion should be maintained by Clinicians who face an apparent acute icteric hepatitis, and syphilis serology should be included among initial laboratory workout.
P828: The great imitator: syphilis with predominant meningoencephalitic features
R. Manfredi, S. Sabbatani, D. Pocaterra, F. Chiodo (Bologna, I)
Introduction: A significant recrudescence of syphilis was observed in recent years, not contained by prophylactic measures against HIV and other STDs. Meningeal and meningoencephalitic involvement may occur also in early stages of syphilis, thus posing problems of differential diagnosis.
Case reports: A young woman and an HIV-infected male developed a syphilis with predominant meningoencephalitis expression. In the first p, based on an isolated positive Borrelia burgdorferi serology (later deemed as a cross-reaction), early ceftriaxone was started, due to a suspected neurological Lyme disease. Also after the diagnosis of neurosyphilis (on the ground of positive CSF serology), antimicrobial therapy was left unchanged for 3 weeks at our Day-Hospital facilities, until complete clinical-microbiological cure. A second, HIV-infected p was hospitalized owing to mild fever lasting 2 weeks, associated with cephalalgia and anxiety. The favorable virological-immunological status (CD4 + count 439 cells/μL and undetectable HIV viraemia, under an effective HAART regimen), did not exclude all searchs for possible HIV-related disorders. Although serum examination detected a potential latent syphilis (isolated positive serum Treponema pallidum IgG, TPHA 1:640, IgG-positive RPR, and mute history for syphilis), only CSF examination disclosed an increased cell content (50/μL), altered brain-blood barrier indexes with increased intrathecal Ig synthesis, and frank VDRL, TPHA (1:1520), and borderline T. pallidum IgM serology. Penicillin G at 24 MU/day for 14 days led to a slow resolution of neurological signs and symptoms, and a tendency to improvement of specific CSF-serum syphilis serology during subsequent controls.
Discussion: Focusing on differential diagnosis, a luetic etiology should not be underestimated, when facing young p suffering from a meningoencephalitis of unclear origin. Our cases were characterized by a young age (34 and 44 years, respectively), when compared with usual mean age of tertiary neurosyphilis. In absence of suggestive history and other syphilis signs, the diagnosis was achieved only after the retrieval of elevated syphilis serology positivity on both CSF and serum, together with some clinical signs, such as seizures, altered mentation, cognitive abnormalities, and anisochoria in the first p, and persisting headache and anxiety in the second p. Our experience with ceftriaxone (started in the first p when neuroborreliosis was suspected), was favorable like that with high-dose i.v. penicillin G.
P829: Comparison of the genomes of pathogenic treponemes, Treponema pallidum ssp. pallidum, ssp. pertenue and Treponema paraluiscuniculi
D. Smajs, P. Matejkova, M. Strouhal, S.J. Norris, G.M. Weinstock (Brno, CZ; Houston, USA)
Objectives: Genomes of closely related treponemes, Treponema pallidum ssp. pallidum (strains Nichols and SS14) and Treponema pallidum ssp. pertenue (Gauthier, Samoan D) were compared with the genome of Treponema paraluiscuniculi using genomic techniques. T. pallidum ssp. pallidum is the causative agent of a highly invasive human disease syphilis, T. pallidum ssp. pertenue is the causative agent of yaws and T. paraluiscuniculi is not pathogenic to humans.
Methods: DNA microarray containing PCR products of all annotated ORFs of the strain Nichols was used for hybridization of labelled treponemal genomic DNA. In addition, whole genome fingerprinting was used to study treponemal genomes. PCR-amplified regions of genomic DNA were digested with BamH I, EcoR I, Hind III, or their combinations.
Results: After labelling of chromosomal DNA using random hexamers and hybridization to the DNA microarray, at least 15 T. paraluiscuniculi genes showed significantly lower signals when compared to signals of T. pallidum ssp. pallidum. These genes were clustered at least in five chromosomal regions and comprised tpr genes and genes encoding hypothetical proteins in their vicinity. No significant differences were observed when strains T. pallidum ssp. pertenue were compared to the Nichols and SS14 strains indicating high degree of sequence homology between pallidum and pertenue subspecies. PCR amplification and subsequent restriction analysis of the complete genomes of the strains Nichols, SS14 and Gauthier revealed 1 absent restriction site in SS14 and Gauthier. When compared to Nichols genome, 8 and 34 differences in the target restriction sites and 1 and 8 detectable deletions/insertions were found in the genome of Samoan D and T. paraluiscuniculi, respectively.
Conclusions: Presented data indicate close relationship of T. pallidum ssp. pallidum and ssp. pertenue on the DNA level with a relative distance from the T. paraluiscuniculi genome. Restriction profiles appear to be strain-specific rather than subspecies-specific.
P830: Sexually transmitted diseases in an area of Spain
J.L. Prada, F. Moreno, A. Del Arco, J. Aguilar, N. Montiel, J. De La Torre, J.M. Arango (Marbella, E)
Introduction: The incidence in sexually transmitted diseases (STD) in our region is unknown. Several factors suggest an increment in this frequency.
Objectives: To study the clinical profile and incidence of STD in our area.
Method: Retrospective and descriptive study of all the patients with STD diagnosis in Costa del Sol area among janury-2000 and september-2004. Our Microbiology Unit is the reference laboratory for an area in the south of Spain with a population of 300.000 inhabitants. Data from Microbiology Lab Database were analysed. We excluded hepatitis, herpes, papilomavirus and HIV.
Results: We have detected 145 cases of infection by Treponema pallidum (Tp), Neisseria gonorrhoeae (Ng) and Chlamydia trachomatis (Ct). The average age was 36 years (19–85) and 69.7% were males. Tp is the main cause with 102 cases (70.3%), Ng 32 cases (22.1%) and 11 Ct (7.6%). Mean age was 39, 31 and 28 years respectively and the rate of males 69.7%, 90.1% and 9.1% respectively. By years from 2000 to 2004 the cases respectively were 24, 18, 35, 24 and 44, the average of age 40, 39, 36, 36 and 34 years, Tp cases 20, 13, 26, 15 and 28, Ng cases 4, 4, 6, 8 and 10, and Ct cases 0, 1, 3, 1 and 6. 70.3% of total cases were diagnosed in the Primary Care System, the remains in the Hospital: 11.8% by General Internal Medicine, 10.3% by Gynecology, 1.4% by Dermatology, and 6.2% by other departments. The Ct diagnosis was made by Gynecology in 81.8%. Internal Medicine made Tp diagnosis in 15.7% and Ct in 9.1%.
Conclusions: We have observed a trend to increase the STD incidence and a decrease in diagnosis-age (from 40 to 34 years of average in the last 4 years). Males were principally affected (69.7%). The STD diagnosis was made particularly in the Primary Care Level.
P831: One-step detection and identification of human papillomavirus genotypes in Bulgarian women with cytologically normal cervical smears
Z. Kalvatchev, P. Draganov, D. Georgiev, A. Gancheva (Sofia, BG)
Objectives: The cervical human papillomavirus (HPV) infection is common among young sexually active women. Because the cytology tests have some limitations, including up to 30% false-negative results, molecular techniques are increasingly used for identification of HPV-induced cell changes in the cervix. The polymerase chain reaction (PCR) for HPV diagnostics was successfully introduced recently in Bulgaria. However limited data on specific prevalence and determinants of subclinical HPV infections are available. In this study we designed a multiplex primers PCR system for simultaneous identification of the most common low- and high-risk HPVs in women with cytologically normal cervical smears.
Materials & methods: DNA from 102 cervical cell samples from women aged between 18 and 40 years with normal Pap smear tests was extracted by standard procedure and studied for HPV presence. Six type-specific primer sets for E6 HPV gene were used in a single-tube reaction for detection and identification of HPV-6, -11, -16, -18, -31, and -33. Respective controls and statistic analysis were included.
Results: The overall HPV DNA prevalence was 23.5% (24/102). Ten of the HPV positive women (41.6%) were infected with high-risk (HPV-16 or HPV-18) virus types; eight (33.3%) with low-risk types (HPV-6 or HPV-11), and six (25%) were infected with both high- and low-risk types (3 HPV-6/-16; 2 HPV-6/-18 or 1 HPV-6/-33). HPV prevalence among women younger than 23 years was 58.3% (14/24). For low-risk types the peak prevalence was observed in women between 35–40 years. Besides age, there was a positive association between the detection rates of HPV infection and number of sexual partners and oral contraceptive use.
Conclusion: The used technique is simple, economic, rapid and reliable for screening studies of HPV infections. The prevalence of HPV in cytologically normal Bulgarian women is similar to the reported in other countries. Our findings suggest that molecular techniques for HPV detection might be useful as an adjunct to Pap smear screening.
P832: Group B streptococci carriage in pregnant women
M. Nishimura, G. Martínez, A. Meier, A. Oltoff, M. Pizzuto, E. Cecchini (La Plata, RA)
Objective: To determine Group B streptococci (GBS) carriage in pregnant women and its effects in delivery and newborn.
Methods: Retrospective and prospective observational study of 1504 pregnant women, the majority belonging to low income level. They were attended in a Mother to Child Hospital (Dr. Ollier) in the neighborhood of Buenos Aires city. Data for identification, gynecology and obstetrics history, microbiological findings, prophylaxis, route of delivery, and newborn status were recorded. They were screened for carriage of GBS: samples of cervix, fundus of vagina and anorectal area were performed between 35–37 weeks of pregnancy. EPI Info 6 was used to process the collected information.
Results: The study included 5100 clinical records of pregnant women. One thousand and five hundred four (29.5%) were screened with gestational age over 35 weeks. Seventy-eight per cent were aged 11–30 years (11–20 = 26% and 21–30 = 52%). First pregnancy was in 23.8%. Overall carriage was 11% (n = 162). Seventy seven per cent of colonized women was 11–30 years old and 24% younger than 21. There was not statistical difference in carriage among age groups. The events observed in GBS carriers were: premature delivery 4.4%, early rupture of membranes 16.7% (p 0.01 vs. no carriers). Children born from GBS carriers were alive in 99.0% (2 death fetus) and 3.3% (n = 5) had sepsis with isolation of GBS in two. GBS carriage was associated with sexually transmitted infections in 2% (p 0.1 vs. without colonization). Mothers of the ill newborns had not risk factors for colonization with GBS.
Conclusions: GBS carriage and the incidence of GBS sepsis were according the literature data 5–35% and 0.7–3.7%, respectively. It has to be emphasized: (1) routine universal screening must be performed for all pregnant women, (2) use of antibiotic prophylaxis in all colonized, (3) use of antibiotic prophylaxis in all with no performed obstetrics controls. These measures prevent mother-to-infant transmission of GBS. It ranges between 29–72% and incidence of GBS sepsis diminishes approximately 86% with antibiotic prophylaxis use.
P833: Mixed infections of the female low genital tract
C. Panagou, J. Spiliopoulou, A. Meletiou, E. Zagotzidou, D. Patili, M.-E. Alexandrou, A. Vogiatzi (Athens, GR)
Objective: The aim of this study was to determine the prevalence of the most common sexually transmitted pathogens in symptomatic and asymptomatic women.
Materials and methods: A number of 1284 women, aged 16–70 years, were examined for a period of 1 year. They were divided in three age groups: group A: 16–19 years (n = 62), group B: 20–50 years (n = 1090) and group C: 51–70 years (n = 132). Vaginal and cervical specimens for aerobic-anaerobic culture, a wet mount preparation and a Gram stained smear were examined. Mycoplasmas were determined by use of a commercially available system (Liofilchem s.r.l, Italy) and C. trachomatis antigen by DIF (Cellabs Pty Ltd, Australia).
Results: Of 1284 specimens, 1121 were positive. The isolated species in each age group are summarized in Table 1. In 818 cases of lower genital tract (LGT) infection, only one species was isolated. In all three age groups, Mycoplasmas were the most commonly identified. In particular, the species of the isolated pathogens were: (1) Group A (n = 43): Mycoplasmas 52%, Streptococcus spp 24%, Candida spp 8%, C. trachomatis 8% and anaerobes 8%, (2) Group B (n = 691): Mycoplasmas 65.26%, Candida spp 15.14%, Streptococcus spp 8.44%, B. vaginosis (B.V) (anaerobes 7.45%, C. trachomatis 3.22% and T. vaginalis 0.49%, (3) Group C (n = 84): Mycoplasmas 57.14%, Streptococcus spp 24.49% and Candida spp 12.25%. In 303 women a mixed infection was found. Especially in group B, Mycoplasmas + B.V (n = 93), Mycoplasmas + Candida spp (n = 83), Mycoplasmas + Streptococcus spp (n = 21), Mycoplasmas + T. vaginalis (n = 12), and Candida spp + C. trachomatis (n = 12) were isolated. In 39 women of this group a mixed infection with three species was found. From 818 women with positive cultures, 562 (68.70%) were symptomatic, while in 256 asymptomatic women (31.20%), sexually transmitted pathogens were identified. Noticeably 40.58% and 37.5% of the infected women with Candida spp and C. trachomatis respectively, presented no symptoms.
| GROUP A (n = 55) |
GROUP B (n = 951) |
GROUP C (n = 115) |
||||
|---|---|---|---|---|---|---|
| Microorganisms | N | % | N | % | N | % |
| Mycoplasmas | 31 | (46.27) | 679 | (55.29) | 76 | (52.05) |
| Candida spp | 14 | (20.89) | 229 | (18.66) | 17 | (11.64) |
| BV+ anaerobes | 3 | (4.49) | 163 | (13.27) | 19 | (13.01) |
| C. trachomatis | 5 | (7.46) | 48 | (3.91) | 3 | (2.06) |
| T. vaginalis | 0 | 22 | (1.79) | 7 | (4.79) | |
| Streptococcus spp | 14 | (20.89) | 87 | (7.08) | 24 | (16.45) |
Conclusions: (1) The rate of mixed LGT infections was 27.02% (2) Asymptomatic infections were 31.20% (3) All teenagers in group A were symptomatic.
P834: Ureaplasma MBA size variants in woman with spontaneous preterm delivery
J. Spergser, A. Witt, L. Petricevic, P. Husslein, A.M. Hirschl, R. Rosengarten (Vienna, A)
Objectives: Despite colonization of the lower urogenital tract, ureaplasmas reach the upper genital tract only in a subpopulation of women, and only in some of these individuals symptoms like preterm delivery ensue. While some studies indicated that certain serovars are more frequently implicated with particular diseases, others have suggested that size variability of the multiple banded antigen (MBA) may contribute to ureaplasmal pathogenesis. To address these hypotheses, vaginal and placental samples from women with spontaneous preterm delivery were tested for ureaplasma species, serovars and MBA size variants.
Methods: Placenta/amnion specimens and corresponding vaginal samples from women that delivered via caesarean section less than 34 weeks of pregnancy were collected. Samples were examined for ureaplasma species and serovars by cultivation and PCR assays. To determine MBA size variants, PCR with primers amplifying the non-repetitive and the C-terminal repeat region of the MBA gene were performed.
Results: Out of 100 cases examined so far, 32 placenta/amnion specimens and 40 corresponding vaginal samples were positive for ureaplasmas by cultivation and PCR. While ureaplasma positive samples from the lower genital tract were carrying U. parvum (100%) and U. urealyticum (50%), colonization of the placenta/amnion was restricted to U. parvum which was only recovered from women with preterm labor or preterm PROM. In contrast, ureaplasmas were not detected in samples from women with HELLP syndrome, IUGR and preeclampsia. As opposed to some previous studies, particular serovars were not implicated in adverse pregnancy outcome. However, significant differences between number and lengths of MBA PCR products among placental and vaginal ureaplasma isolates were obvious. Ureaplasma isolates from placenta/amnion membranes gave shorter PCR products than did corresponding vaginal isolates and while a majority of vaginal ureaplasma isolates were composed of multiple size variants, placental isolates were predominantly restricted to a singular MBA size variant.
Conclusion: Only U. parvum was found to be frequently present in the placenta/amnion of women with preterm delivery and certain serovars were not more frequently implicated with particular diseases. In addition, MBA size variation represents an additional level of phenotypic and genetic variability beyond the serovar category which may provide an important contribution to ureaplasmal pathogenesis.
P835: Use of kanamicin in the topical therapy of aerobic vaginitis
G. Tempera, G. Bonfiglio, E. Cammarata, S. Corsello, A. Cianci (Catania, Paternò, I)
Objectives: Demonstrate the efficacy of the topical therapy with kanamicin in a new pathology called aerobic vaginitis (AV).
Methods: Eighty-one patients with clinical diagnosis of AV in accordance to Donders's criteria, have been included in the study. The presence at least of four of the following symptoms were taken as diagnosis of AV: objective abnormal yellow vaginal discharge, foul smell (but negative to KOH test), elevated vaginal pH (>5), abundant vaginal leukocytes and lactobacillary grade IIa, IIb and III in accordance to Donder's classification. Other characteristics such as vaginal dyspareunia, vulva-vaginal itching, cervical erosion as well as the isolament of vaginal microorganisms were also documented. The patients were randomised treated, 45 with kanamycin (100 mg vaginal ovules per 6 days, consecutively) whereas, 36 with meclocycline (35 mg vaginal ovules per 6 days, consecutively). The patients were visited before starting the study, 1–2 days and 30 days after the end of the study.
Results: At the first follow-up the patients showed different level of symptoms reduction. Particularly, reduction of presence of leukocytes, burning of vaginal mucosa and itching were statistically significant in the group treated with kanamycin with respect to the group treated with meclocycline. Moreover, there was also a reduction of isolament of Enterobacteriaeae (97%) in the group treated with kanamycin versus 76% treated with meclocycline. At the second follow-up, vaginal homeostasis (normalisation of pH and presence of lactobacilli) was demonstrated only in kanamycin treated group.
Conclusion: Our data suggested that the topic use of kanamycin could be considered a specific antibiotic for the therapy of this new pathology.
P836: Comparison of Gram stain and culture for the characterisation of vaginal microflora
R. Verhelst, H. Verstraelen, G. Claeys, G. Verschraegen, M. Temmerman, M. Vaneechoutte (Ghent, B)
Objectives: Establishing the identity of Lactobacillus species colonizing the vagina of women is of importance, because clinical studies have demonstrated an association between the presence of H2O2-producing strains of Lactobacillus and a decreased prevalence of bacterial vaginosis (BV). Recently, culture based studies using molecular identification methods showed that L. crispatus and L. jensenii are the most common species of vaginal lactobacilli and that colonization by these species was positively associated with a lower frequency of BV. Here were report that L. crispatus can be distinguished from other lactobacilli using Gram staining of vaginal smears.
Methods: Several approaches were used to characterize 515 vaginal microflora samples obtained from 197 pregnant women at three time points in pregnancy: 1/Gram stained smears from vaginal swabs, scored according to modified Ison and Hay criteria; 2/identification of cultured isolates obtained after anaerobic culture, identified using tDNA PCR; and 3/species specific PCR for Atopobium vaginae and Gardnerella vaginalis. Grade I specimens, representing a normal microflora, were further characterized as grade Ia when only L. crispatus cell types were present, grade Ib when other Lactobacillus cell types were present, grade Iab when both L. crispatus and other lactobacilli were present and grade Ic when either gram-positive rods, small and short, or irregularly shaped gram-positive rods, with clubbing, curved edges and irregular staining (‘diphteroid cell types’) were seen.
Results: Out of the 515 samples, 86.4% showed a normal vaginal microflora (grade I), 8.9% were grade II, 3.7% grade III and 1.0% grade IV. Based on the presence of different Lactobacillus species, grade I specimens were further characterized as grade Ia (36.4%), grade Ib (40.9%), grade Iab (13.5%) and grade Ic (8.5%). This classification was supported by the finding that out of respectively 86.0% and 76.6% of grade Ia and Iab specimens L. crispatus was cultured while this species was present in only 13.1% and 2.6% of respectively Ib and Ic specimens. In addition, 55.1% of grade Ic specimens contained Bifidobacterium spp.
Conclusion: Further refinement of Gram stain based grading of vaginal smears is possible by distinguishing additional classes of normal microflora. These categories of Gram scores may facilitate and improve future studies regarding the interpretation of clinical data and therapeutic outcome.
P837: Isolation of Gardnerella vaginalis from semen
C. Marne, P. Palacián, Y. Martín, A. Betrán, M.J. Revillo (Zaragoza, E)
Objectives: The importance of the isolation of Gardnerella vaginalis in bacterial vaginosis is well known. The involvement in male urogenital infection is uncertain, probably due to low rate of isolation for inadequated specimens process. The objective of this study is to evaluate the possible pathogenic rol of G. vaginalis in male urogenital pathology.
Methods: Over a 3-year period (Oct 01–Sep 04) 1318 semen specimens were cultured, according to the Meares–Stamey method, using semen instead of prostatic fluid. Samples were cultured onto blood and chocolate agar, with microaerophylic incubation up to 48 h. Isolation of significative colony numbers of pinpoint growth, with negative or scanty growth in urethral and vesical urine, was evaluated. Grampositive difteroid cocobacilli, catalase negative with diffuse betahaemolysis in Vaginalis agar was reported as G. vaginalis. Confirmation of the results with new samples was recommended.
Results: G. vaginalis was isolated in high counts from semen of 7 patients. Results were confirmed with second samples in 3 of them. Age range was 28–61 years. Diagnostic was chronic prostatitis in 4 patients, orchitis in 1 and infertility in 2. Four semen samples were also positive for Ureaplasma urealyticum. Chlamydia investigation was negative in all 7 patients. Vaginal exudate was investigated in two couples with the same results (both positive for G. vaginalis and one also for U. urealyticum).
Conclusions: 1. Repeated isolation of G. vaginalis in semen from patients with urologic pathology, according to Meares–Stamey critheria, indicates the probable pathogenic rol. 2. In our experience, we do not consider necessary routine use of selective media for G. vaginalis. Blood and chocolate agar with microaerophylic incubation support good growth of this species. Selective media can be used latter for identification of the isolates. 3. Due to lack of information, our patients were treated empirically by temptative antibiogram results and antibiotic penetration in the prostatic gland. 4. According to bibliography revised, in extravaginal isolates metronidazole is not recommended. 5. Association observed between G. vaginalis and U. urealyticum suggest treatment active against both species. 6. The same microbiological investigations must be performed in the couple, for simultaneous treatment and prevention of relapses. 7. G. vaginalis should also be considered in men as sexually transmitted disease.
P838: Seminal microflora of healthy young men in relation to sexual experience
S. Türk, P. Korrovits, K. Ausmees, M. Punab, R. Mändar (Tartu, EST)
Semen is a recommended specimen in diagnosing of prostatitis. At the same time it also reflects normal genital tract microflora. Although its composition may be affected by the sexual activity, there are no data regarding the changes in genital tract microflora during the sexual debut.
Objective: To identify possible associations between sexual experience and the reproductive tract inflammatory parameters and microflora in healthy young men.
Methods: A total of 72 healthy men aged 17–22 years were included and divided into 3 groups based on their sexual experience (virgins n = 13, monogamous n = 11 and polygamous n = 48). A semen sample of each subject was assessed for basic semen parameters (semen volume, sperm concentration, sperm motility), white blood cell (WBC) counts and quantitative cultures for aerobic, microaerobic and anaerobic bacteria, and possible correlations between the type of sexual experience, WBC counts and seminal microflora were calculated.
Results: Basic semen parameters were similar in all groups. 5.5% of men had high (>1 M/ml) and 19.4% of men had medium (0.2–1 M/ml) semen WBC counts. There were no correlations between the type of sexual experience and semen WBC counts. In comparison to sexually active men in virgin subjects the total microbial counts in semen (4.4 vs 5.0 log CFU p < 0.05) and the number of different species (3 vs 5, p = 0.05) were lower, however, no differences between mono- and polygamous men were found. There was a positive correlation between the total microbial concentrations and number of different species (r = 0.54; p < 0.0001). Staphylococci, Corynebacterium seminale, other coryneforms, gamma- and alpha-haemolytic streptococci and peptostreptococci were the most prevalent organisms. No significant differences in microflora were observed between the groups yet the gram-negative anaerobic rods were more often seen in sexually experienced men than in virgins. The subjects with high WBC counts (>1 M/ml) tended to have higher number of different microorganisms than the rest of the men (median 7 vs 4, p = 0.05).
Conclusions: The sexual debut is associated with the enrichment of seminal microflora but not with the influx of WBC or changes in basic seminal parameters. Strong positive correlation can be observed between the total microbial concentration and the number of different species in semen.
P839: Sexually transmitted infections among registered female sex workers in Athens
A. Nicoloudi, T. Vlachou, C. Giannakakis, E. Zagotzidou, D. Patili, A. Terzi, M.-E. Alexandrou (Athens, GR)
Objectives: 1. To assess the prevalence of ST pathogens among registered asymptomatic sex workers. 2. To compare patterns of STDs among Greek and immigrant sex workers.
Materials and methods: A number of 442 asymptomatic prostitutes, aged 20–55 years (Group A) were examined for STIs, as well as a control group of 192 asymptomatic women of the same age (Group B) who attended the out patients gynaecology dpt of our Hospital, during 2-year period. Vaginal and endocervical samples were examined microscopically for T. vaginalis, yeast, clue cells and N. gonorrhoeae and cultured for aerobic and anaerobic bacteria.C. trachomatis was detected with DIF (Cellabs Pty Ltd, Australia).
Results: Of the 442 samples of Group A and 192 of Group B, ST pathogens were found in 171 (38.6%) and 68 (35.4%) respectively. Among STDs, in Group A, B. vaginosis (43.7%) was observed to be the most common in Greek and immigrant prostitutes, followed by Candida spp (34.2%), S. agalactiae (19.8%) and N. gonorrhoeae in 3 cases. Candida spp were isolated in higher rate (42.3%) in immigrant than in Greek prostitutes (26,2%). In Group B, Candida spp (45.6%) and BV (42.6%) were move often found, followed by S. agalactiae (11.8%). Not one case of N. gonorrhoeae was recorded. C. trachomatis was detected in 14 (3.2%) and 6 (3.6%) women of Group A and B, respectively. The prevalence of asymptomatic Chlamydial infection in Group A was 3.2% (0.8% for Greeks and 5.8% for immigrants). No obvious difference was observed in Group B: 3.6% (2.7% for Greeks and 4.5% for immigrants).
Conclusions: 1. BV (43.7%) was the most common infection in the STDs of female registered sex workers in Athens. 2. The prevalence of Candida spp (42.3%) was considered higher among immigrant prostitutes than Greek. 3. C. trachomatis was detected in significantly higher rate (5.8%) in immigrant sex workers than in Greek (0.8%).
P840: High rates of genital Mycoplasma infection in female of reproductive age
J. Spiliopoulou, C. Panagou, A. Meletiou, E. Zagotzidou, D. Patili, A. Terzi, M.-E. Alexandrou (Athens, GR)
Objective: Mycoplasma can be isolated with considerable frequency from the female urogenital tract and are thought to cause various syndromes such as nongonococcal urethritis, pelvic inflammatory disease or infertility. The aim of this study was to evaluate the incidence of Mycoplasma infection and other common sexually transmitted pathogens in women of reproductive age.
Material and methods: Vaginal and cervical specimens were collected from 1090 women, aged between 20 and 50 years, who referred to our outpatients gynaecology department during a 12-month period. Every woman was tested for the presence of Mycoplasma, Chlamydia trachomatis, Trichomonas vaginalis, Candida and Gardnerella vaginalis. Aerobic and anaerobic culture, a wet mount preparation and a Gram stained smear were examined. The identification of Mycoplasma and sensitivity test was performed using the Mycoplasma system (Liofilchem s.r.l, Italy). The detection of C. trachomatis was performed using DIF (Cellabs Pty Ltd, Australia).
Results: 951 out of 1090 women examined (87.25%) had a positive vaginal or cervical culture. The species of isolated pathogens were: Mycoplasma (679), Candida spp (229), Gardnerella vaginalis (anaerobes (163), C. trachomatis (48), T. vaginalis (22), Streptococcus spp (87). In 691 women (72.66%) only one species was identified. Mycoplasma were the most frequently isolated microorganisms (65.26%) followed by Candida spp (15.14%), Streptococcus spp (8.44%), Gardnerella vaginalis (anaerobes (7.45%), C. trachomatis (3.22%) and T. vaginalis (0.49%). In 221 women (23.24%) a mixed infection was found. In particular, Mycoplasma + Gardnerella vaginalis (n = 93), Mycoplasma + Candida spp (n = 83), Mycoplasma + Streptococcus spp (n = 21), Mycoplasma + T. vaginalis (n = 12), and Candida spp + C. trachomatis (n = 12) were isolated. Three species were present in 39 women (4.1%).
Conclusions: In our study group, there is a high prevalence of genital Mycoplasma (55.29%). Noticeably, Mycoplasma coexists with Gardnerella vaginalis and Candida spp in elevated rates (79.64%). Based on these findings, a more thorough examination for sexually transmitted pathogens might have clinical significance, in this setting of female population.
P841: Comparison of culture with the polymearase chain reaction for detection of Ureaplasma urealyticum in endocervical specimens
S. Najar Peerayeh, S.D. Siadat (Tehran, IR)
Objective: Ureaplasma urealyticum is associated with infection of the genitourinary tract, reproductive failure, and neonatal morbidity and mortality. The objective of this study was to compare PCR and cultivation methods to determine the incidence of U. urealyticum infection in infertile women.
Methods: Duplicate endocervical swab samples were taken from 312 infertile women. DNA was extracted by Cadieux method. Genus-specific (MGSO & GSO) and species-specific (U4 & U5) primers were used for detection of U. aurelyticum by PCR, and culture was done with liquid–solid methods in U broth and U agar media.
Results: U. urealyticum was detected in 26.2% specimen by both culture and PCR methods. 12.5% samples were PCR positive as well as culture positive, 23.7% were positive only by PCR, and 2.5% were positive only by culture. By using culture as the reference method, the PCR had a sensitivity of 82.9%. Overall agreement between results obtained by culture and PCR was 47.5%. No difference was detected on the incidence of U. urealyticum by age and with other clinical symptoms or signs.
Conclusion: PCR is a sensitive and reliable method for the detection of U. urealyticum in endocervical secretions. Detection by PCR (1–2 days) is more rapid than culture (2–5 days) however the use of molecular microbiologic techniques is likely to increase of the detection of U. urealyticum among infertile patients.
P842: Aetiologies of 121 cases of male genital ulcers examined in the microbiology laboratory of the central army hospital in Algiers from 1990 to 2003
M. Naim, D. Tiouit, A. Chabani, W. Amhis (Algiers, DZ)
Objectives: To determine the etiologies of the male genital ulcers examined in the microbiology laboratory of the military hospital and to know their respective frequency from 1990 to 2003.
Methods: Each patient addressed to our laboratory for a genital ulceration is interrogated and examined carefully by a physician microbiologist. Once over the semiotic analysis of the lesion (aspect, number, consistency, pain, adénopathy, etc.) we systematically practice: Dark field microscopy to search for Treponema pallidum. The microscopic exam after staining of Gram associated to the setting up in culture adapted to the isolation of Haemophilus ducreyi (GC agar +1% of Hemoglobin +1% of Isovitalex +5% of serum of foetal veal +3 μg/ml of Vancomycine). The direct Immunofluorescence with monoclonal antibodies for the research of antigens of the herpes simplex virus type 1 and 2 (Monofluokit herpes, Biorad *). The serologies for the Syphilis (VDRL and TPHA), for the HIV (ELISA), for Chlamydia trachomatis (Microimmunofluorescence). When the clinical and/or epidemiological context is in favour of another etiology we practice the appropriate tests (search DONOVAN'S bodies on the lesion biopsy smear after Warthin–Starry staining or Giemsa for Donovanosis and skin scrapping for Scabies).
Results: In total on 121 ulcerations examined, 103 (85%) have been diagnosed with precision but 18 (15%) remained undeterminate. The 103 positive cases are divided as follows: Haemophilus ducreyi = 76 (73.78%), Treponema pallidum = 11 (10.67%), Calymmatobacterium granulomatis = 4 (3.88%), Herpes simplex virus = 4 (3.88%), Sarcoptes scabiei hominis 3 = (2.91%), Candida albicans = 2 (1.94%), Staphylococcus aureus = 2 (1.94%) and Chlamydia trachomatis = 1(0.97%). We did not find any association with HIV
Conclusion: Our results recover the same usual etiologies in the genital ulcers but in different proportions in relation to other regions of the world. So in our country as in the other emerging countries and notably African ones it is the soft Chancroid that predominates extensively, whereas one knows that in the developed countries that is the genital herpes which is the most frequent etiology. All the cases of Donovanosis diagnosed in our laboratory come from Tamanrasset city, southern Algeria, border with endemic sub-Saharan African countries for this illness and other tropical infections. The cases of undeterminate etiology can be explained on the one hand by the possible non infectious causes that we did not search for and on the other hand by the insufficiency of our diagnostic means that we intend to improve very shortly with the acquirement in 2005 of the whole technology of the molecular biology.
P843: Influence of chlamydial cervicitis on vaginal microbiocenosis
M. Romanik, I. Wilk, B. Wiechula, A. Ekiel, D. Friedek, G. Martirosian (Katowice, PL)
Chlamydia trachomatis is the predominant causative agent of pelvic inflammatory disease and, as a result of damage of the fallopian tubes, accounts for up to half of all ectopic pregnancies. Infection with C. trachomatis can influence on vaginal microflora. Association between C. trachomatis, urogenital mycoplasmas and bacterial vaginosis (BV) was described recently. Vaginal discharge based on changes in a vaginal ecosystem (decreasing number of Lactobacillus spp. and increasing number of Mobiluncus spp., Gardnerella vaginalis, Prevotella spp., Peptostreptococcus spp., Mycoplasma hominis and others) appears to be a major cause of BV. The aim of this study was to evaluate the influence of chlamydial cervicitis on vaginal microbiocenosis and BV. Under investigation were 122 sexually active non-pregnant women aged from 18 to 40 years with diagnosed cervicitis by cytological examination and presence of muco-purulent discharge. Fifty five women were included in studied group – with confirmed C. trachomatis cervicitis and 67 women – in control group (with non-chlamydial/non-gonococcal cervicitis). BV was diagnosed using Amsel and Nugent (0–3 negative; 4–6 intermediate; 7–10 positive) criteria. By using Amsel criteria BV was suggested in 11% and 6% correspondingly among women in studied and control group. By using Nugent criteria BV was suggested correspondingly in 5.5% and 3%. These differences were not statistically significant and can be explained by the presence of muco-purulent discharge among studied women. Among women with chlamydial cervicitis statistically frequently were observed large morphotypes of Lactobacillus spp. and intermediate Nugent score. We did not observe significant differences in occurrence of Corynebacterium spp., Staphylococcus spp., Streptococcus spp. (GBS), Gram-negative Enterobacteriaceae, Pseudomonas spp. and urogenital mycoplasmas. Further studies require for evaluation of influence of chlamydial cervicitis on BV.
Helicobacter
P844: Identification system for Helicobacter species based on 16S and 23S rRNA gene polymorphisms
A. González, Y. Moreno, P. Piqueres, J. Hernández, M.A. Ferrús (Valencia, E)
Objectives: Helicobacter pylori is recognized as an important human pathogen but the differentiation of the species by classical phenotypic methods is really difficult. Therefore the objective of this study was the development of an identification method for Helicobacter species based on PCR-restriction fragment length polymorphism (PCR-RFLP) analysis of the 16S and 23S rRNA genes.
Methods: H. pylori NCTC 11637, H. pullorum NCTC 13153, H. fennelliae NCTC 11612, H. cinaedi NCTC 12423, and 31strains isolated from gastric biopsies were cultured on 10% (v/v) horse blood agar at 37°C under microaerobic conditions. DNA was extracted by the cetyltrimethyl-ammonium bromide (CTAB) method. The primers used in this study to amplify a 1004-bp fragment of the 16S rRNA were CAM16S1a (5′ AATACATGCAAGTCGAACGA 3′) and CAM16S1b (5′ TTAACCCAACATCTCACGAC 3′). To amplify an internal 2.6 kbp fragment of the 23S rRNA gene primers LS1 (5′ GGATTTCCGAATGGGGCAACCC 3′) and LS2 (5′ GTTTCGTGCTTAGATGCTTTC 3′) were used. Restriction endonucleases were selected by computer analysis using Reb sites (http://rebase.neb.com). DdeI and HpaII were used to digest 16S rRNA and 23S rRNA fragments respectively. The digestion mixture included 10 μl of the PCR product with 10 U of the restriction endonuclease and was incubated at 37°C for 3.5 hours. 12 μl of the digested product were analysed electrophoretically at 90 V for 3 hours with 2% (w/v) agarose gel.
Results: The internal region of the 16S rRNA gene was amplified in all the strains. The digestion of the amplicon with DdeI generated 3 different specific patterns, one for H. pylori, another for H. pullorum and H. cianedi, and the last one for H. fennelliae. The PCR-RFLP scheme failed to differentiate H. cianedi from H. pullorum. A 2.6 kbp PCR product of the 23S rRNA was amplified in all the strains, and the digestion of the amplicon with HpaII generated 4 different profiles, one for each one of the species studied. All of the 31 clinical isolated strains were identified as H. pylori by both PCR-RFLP assays.
Conclusion: PCR-RFLP analysis of 16S and 23S rRNA gene sequences allows for easy and quickly differentiating related Helicobacter species.
P845: Genotyping of H. pylori using DNA extracted from faeces
C. Williams, G. Mackay (Glasgow, UK)
Background: Helicobacter pylori causes peptic ulceration and is linked to the development of gastric cancer. Despite this little is known about the nature of transmission of this organism. It is likely that spread occurs in early life but whether this is within families or between peer groups is unclear. Until recently, it was only possible to type the organism from cultures derived from gastric biopsies. This required an endoscopy to be performed meaning that epidemiological studies on children were not possible. We have developed a method to detect H. pylori DNA in faeces and have extended this to perform non-invasive typing using a Line Probe Assay (LIPA).
Objectives: To extract and type H. pylori DNA from the faeces of family groups.
Methods: Children referred for breath testing were used as the index cases and faecal donations collected from parents and siblings in 7 families. DNA was extracted from faecal samples and analysed using a Line Probe Assay (LBP H. pylori virulence strips, Labo Biomedical Products, The Netherlands).
Results: H. Pylori genotypes were obtained from 17 out of 19 faecal samples analysed. 16 out of 17 were positive for the s1a region of the vacA gene. The m1 m2a region was present in all members of 3 families and 3 other individuals. There was no pattern to the distribution of the cagA gene.
Conclusions: This pilot study confirms the potential for LIPA analysis to provide data on the type of H. pylori present in family groups. In the 7 families studied there were no clear patterns that suggested whether transmission occurred from parents or peers and further studies using a larger number of families would be required.
P846: Multiple analyses of different regions of the 16S rRNA gene increase the diagnostic efficiency of PCR-DGGE technique for Helicobacter spp.
W. Abu Al-Soud, I.-S. Ouis, Å. Ljungh, T. Wadström (Lund, S)
Objectives: Since the first identification of Helicobacter pylori by Warren and Marshal in 1983, members of the genus
Helicobacter increased to more than 26 species, which have been detected in human and animals. The construction of species specific PCR assays is difficult due to the close relatedness between different Helicobacter species. The PCR-DGGE technique was developed for the identification of Helicobacter colonization. The aim of this study was to investigate the effect of multiple regions of the 16 rRNA gene on the diagnostic efficiency PCR-DGGE.
Methods: DNA was extracted from 40 Helicobacter strains, which represent 20 Helicobacter species. Amplification of ∼1.2 kb of helicobacter 16S rDNA, which contains V3 and V6-7 regions, was done using previously published Helicobacter genus specific primers C97 and C05. The PCR product can be used as a template for two Helicobacter genus PCR assays, the v6-7 regions 16S rDNA was amplified using the primers 1FC254 and 2RC686, the v-3 region was amplified using the primers BSF917 and BSR1114 published at (http://rrna.uia.ac.be/primers). DGGE analysis of the V3 and V6-7 regions was performed on 9% polyacrylamide gels containing urea and formamide gradient from 20–40% or 15–30%, respectively. Electrophoresis was performed in a DCode electrophoresis unit (BioRad) at constant voltage (200 V) at 60°C for 4 hours.
Results: DGGE analysis of two regions of Helicobacter 16SrRNA gene showed mobility patterns that allowed discrimination of most Helicobacter species except those which are closely related such as H. pullorum–H. pametensis, H. ganmani–H. rodentium and H. bizozeroni–H. felis–H. salmonis.
Conclusions: Helicobacter species are widely distributed in the gastrointestinal tract of mammals, birds and other animals. The PCR-DGGE technique has proven to be an easy, inexpensive and efficient tool for the identification of Helicobacter species and for the detection of colonisation by more than one Helicobacter species, without the need for species-specific PCR assays. In addition, the diagnostic efficiency of this technique was increased by analysis of multiple regions of the 16S rRNA gene.
P847: Helicobacter spp. in chronic pancreatitis, pancreatic adenoma and pancreas cancer
H.-O. Nilsson, U. Stenram, I. Ihse, T. Wadström (Lund, S)
Objectives: Helicobacter spp. efficiently colonise various hostile habitats such as the stomach, colon and biliary tract of animals and man. With the exception of H. pylori, many Helicobacter spp. are difficult to culture. Nucleic acid based detection has thus become a method of choice for analysis of Helicobacter spp. in chronic inflammatory gastrointestinal (GI) tract diseases and cancers. Pancreatic exocrine cancer, with few established risk factors and very poor prognosis, is a common cause of cancer death. Previously, serological studies found an association between H. pylori and pancreas cancer (PC).
Methods: Pancreatic tumour specimens of patients with PC (n = 40), tissues of chronic pancreatitis (n = 6), pancreatic adenoma (n = 8), and benign pancreatic tissue of patients with cancers of the choledochus, colon and duodenum (n = 6), were analysed by semi-nested Helicobacter-specific 16S rDNA PCR. Stomach (n = 23) and gallbladder (n = 12) specimens of the PC-patients were also analysed. PCR-products (360–400 bp) were characterized by DNA-sequence analysis.
Results: The Helicobacter spp. PCR was positive in 19 of 40 (47.5%) pancreas cancer patients, and in the pancreas in 4 of 6 (66.7%) patients with chronic pancreatitis. Adenoma and pancreas tissues of other GI-tract cancers, as well as gallbladder specimens, were all negative. Four of 23 (17.4%) stomach samples of the PC-patients were Helicobacter positive with sequences homologues to H. bilis by BLASTn analysis. DNA-sequencing of 13 PCR-products amplified in PCs were closely related to H. pylori (n = 9), H. flexispira sp. (n = 3) and H. cinaedi (n = 1). Two pancreatitis PCR-products matched H. pylori.
Conclusions: Helicobacter spp. were common in PC compared with benign pancreatic tissue.
P848: Helicobacter pylori infection and low IgG immunoglobulin
S. Kokkinou, K. Pavlou, A. Varouta, J. Villiotou, K. Papaefstathiou, A. Moutsopoulou, E. Papafrangas (Halandri Athens, Athens, GR)
It is established that Helicobacter Pylori (Hp) may cause haematological disturbances such as iron malabsorption and Idiopathic Thrombocytopenic Purpura (ITP). The aim of this study is to show that Hp is involved in human disease in a more complicated way, producing an abnormal immunologic profile.
Patients and methods: This work reports the presence of a significant low value of IgG immunoglobulin in 52 pts suffering from unidentified iron deficiency (ID)or iron deficiency anemia (IDA coexisting with megaloblastic anemia(MA), in 12 leukopenic pts and in 3 more pts having thrombocytosis, ITP and polycythemia respectively. The ratio Male/Female was 25/42, and their age ranged from 14–80 years. In the blood examination there was a10-fold titre of Hp-IgG type antibody in all, while in 23 there was also a high titre of Hp-IgA type using ELISA technique. The histopathological examination of an antral biopsy showed diffuse corpus gastritis, atrophic gastritis and achlorydria secondary to Hp infection that take place in gastric area.
Results: 52 pts had unidentified ID or IDA coexisted with megaloblastic anemia. Serum iron, transferrin saturation, serum ferritin and B12levels were found to be significantly low. All of them had also Hp infection. Their anemia existed for more than 10 years, was unresponsive to treatment and recurrent in nature. Twelve pts with undefined eukopenia (L:3.3 × 109/l) lasting for at least 8 years, had also an Hp infection. All of our pts had a significantly low value of IgG immunoglobulin. Mean value ranged from 551 to 868 mg/dl(normal value:850–1517 mg/dl). They subjected to eradication therapy. All but one responded well.
Conclusions: (1) Hp infection was found to coincide with ID, IDA, MA and leukopenia. (2) The normalization of haematological parameters after eradication started 6 months later. (3) The essential mechanism between the Hp infection and low IgG is unclear and its value remains low and after the eradication therapy. (4) Studies with larger samples should be done for a better evaluation of the Hp infection and it's involvement in human disease. (5) Hp infection acts in a catabolic way for the humans. It must be considered to search for it in haematological conditions of undefined origin.
P849: Helicobacter pylori from the dyspeptic patients in Thailand: diagnosis, antimicrobial susceptibility and correlation to clinical outcomes
C. Chomvarin, P. Kulsuntiwong, P. Mairiang, C. Kulabkhow (Khon Kaen, TH)
Objectives: To evaluate methods for routine clinical diagnostic use of Helicobacter pylori infection of gastric biopsies, to study the correlation of H. pylori infection to the clinical outcomes and to study antimicrobial susceptibility by disk agar diffusion in Thailand.
Methods: Gastric biopsies, obtained from 210 patients underwent at the endoscopy unit of Srinagarind Hospital, Faculty of Medicine, Khon Kaen University, were diagnosed by culture, rapid urease test (RUT, Pronto dry) and histological examination. A true positive criteria was indicated when culture or both RUT and histology tests were positive. One hundred and fifteen isolates of H. pylori isolates were tested for six antimicrobial agents by disk agar diffusion method.
Results: The H. pylori infection rate was 44.3% (93/210). The sensitivity vs. specificity of the culture, RUT and histology were 88.2% and 100%, 95.7% and 98.3%, and 96.8% and 59.8% respectively. The prevalence of H. pylori in gastritis (GT), duodenal ulcer (DU) and gastric ulcer (GU); and gastric cancer (GCA) patients were 41.2%, 57.9% and 70.6%, respectively. The chi-squared test showed that GCA patients were significantly more often infected with H. pylori than GT patients. The resistance of 115 H. pylori isolates to single antimicrobial agent as metronidazole (MTZ), clarithromycin (CLR), ciprofloxacin (CIP), amoxycillin (AML), and tetracycline (TE) were detected in 21.7, 0, 5.2, 1.7 and 0 percent, respectively. The combination resistance to MTZ & CLR, MTZ & CIP, MTZ & AML, MTZ & TE; and CLR & CIP were detected in 1.7, 1.7, 0.8, 1.7 and 0.8 percent, respectively. The 2.5 per cent of H. pylori isolates were resistance to three or more antimicrobial agents.
Conclusion: RUT method was highly sensitive and specific and appropriate for routine laboratory use. The correlation of the GCA patients to H. pylori infection was significant difference compared to GT patients. The high resistance rate to metronidazole indicated that the effective for eradication of H. pylori by metronidazole should be considered in the clinical management of H. pylori infection.
P850: Use of an indirect immunofluorescence test for the detection of CagA in H. pylori
C. Scherer (Essen, D)
Objectives: The cytotoxin associated gene (cagA) of H. pylori is a frequently discussed virulence factor which codes for a 128-kDa cytotoxin associated antigen (CagA). The cagA-gene is usually detected by PCR methods. Publications about phenotypic methods for the detection of CagA are rare. Aim of our investigation was to compare a slightly modified, recently published indirect immunofluorescence test (iIFT) for the detection of CagA with commonly used PCR assays.
Methods: H. pylori ATCC 43504 (cagA+/CagA+) was used as positive control strain, ATCC 51932 (cagA+/CagA+) as negative control strain. Nineteen clinical isolates of H. pylori were examined for their CagA- and cagA-status. CagA was detected by iIFT using monoclonal anti-CagA-antibody from mice, which were visualised for immunofluorescence microscopy with FITC-conjugated anti-mouse-antibody from rabbits. DNA was extracted by a standard phenol-chlorophorm procedure after proteinase K treatment of the cells from a 4-day old culture. 7 primer pairs and their published protocols were used: F1/B1 and D008/R008 as the most described primer pairs and further five primer pairs. All tests were performed in duplicate.
Results: 4 from 19 (22%) strains were CagA positive in the iIFT, and also cagA positive in each PCR. 13 from 19 (68%) strains were negative in the iIFT. 10 from these 13 were cagA-negative in each PCR and 3 showed varying results in the PCR-assays. 2 from 19 (10%) strains could not be interpreted by iIFT, both showed varying results in the PCR-assays.
Conclusion: The iIFT might be a simple to use tool in the determination of the cagA-status, since it showed no false positive result in neither tested PCR. The differing results in iIFT and PCR suggest that genotypic positive strains may not always express CagA in vitro and maybe also not in vivo. Therefore the CagA-iIFT may be an interesting parameter for the determination of strain virulence in addition to PCR-assays.
P851: Evaluation of ELISA serology for the primary diagnosis of Helicobacter pylori infection in Turkish dyspeptic patients: a prospective study from a developing country
B. Kocazeybek, Y. Erzin, S. Altun, A. Dobrucali, M. Aslan, S. Erdamar, A. Dirican (Istanbul, TR)
Aim: Hp is recognized as an important human pathogen by virtue of it's association with peptic ulcer disease, gastric cancer and gastric lymphoma and the high prevalence of infection worldwide. Both invasive and noninvasive tests are available to diagnose Hp infection but there is still no single gold standard. The aim of the present study was to evaluate the diagnostic accuracy of a commercially available anti-Hp IgG ELISA kit for the primary diagnosis of Hp infection.
Materials and methods: A total of 185 patients who were referred to our endoscopy unit were included. According to our gold standard, a patient was classified as being Hp(+) if the culture and/or both histology, rapid urease test were positive and as Hp(−) only if all of these tests remained negative. Standard methods were used to calculate sensitivity, specificity, predictive values of positive and negative results and 95% confidence intervals of these values.
Results: After excluding patients with discordant results131 of 152 patients (86%) were Hp (+). The sensitivity, specificity and diagnostic accuracy of the IgG-ELISA were 97%, 67%, 93% respectively.
Conclusion: Due to it's lack for specificity, we conclude that quantitative anti-Hp ELISA test may not be a suitable alternative for primary diagnosis of Hp in our country, where the prevalence of infection is still very high.
P852: Comparison of two different stool antigen tests for the primary diagnosis of Helicobacter pylori infection in Turkish dyspeptic patients
B. Kocazeybek, Y. Erzin, S. Altun, A. Dobrucali, M. Aslan, S. Erdamar, A. Dirican (Istanbul, TR)
Aim: To assess the reliability of two different enzyme immunoassays in detecting the Helicobacter pylori (Hp) status in stool specimens of Turkish dyspeptic patients.
Materials and Methods: 151 patients [74 with non-ulcer dyspepsia(NUD), 64 with duodenal ulcer(DU),13 with gastric cancer]who were admitted to the endoscopy unit of Istanbul University, Cerrahpasa Medical Faculty for upper gastrointestinal endoscopy due to dyspepsia were enrolled in the study. Hp infection was confirmed in all patients by histology, rapid urease test(RUT) and culture. A patient was classified as being Hp-positive if the culture alone or both histology, RUT were positive in the absence of a positive culture and as negative only if all of these tests remained negative. Stool samples of patients were obtained in order to assess the reliability of a monoclonal (FemtoLab H. pylori, Connex, Martinsried, Germany) and a polyclonal (Premier Platinum HpSA, Meridian Diagnostics Inc., Cincinnati, USA) stool antigen test and to compare their diagnostic accuracies. The χ2 test was used for statistical comparison of the values.
Results: Using a cutoff 0.19 for FemtoLab H. pylori and 0.16 for Premier Platinum HpSA the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy of the former and latter tests were 93%, 90%, 98%, 68%, 93% and 84 %, 67%, 94%, 40%, 81% respectively. The sensitivity, specificity, NPV and diagnostic accuracy of the former test were significantly superior to the latter one's (χ2 = 3.98; p < 0.05 for sensitivity and χ2 = 15.67; p = 0.000 for specificity, χ2 = 15.78; p = 0.000 for NPV and χ2 = 6.37; p = 0.012 for diagnostic accuracy). The bacterial load did not affect the sensitivity of both tests.
Conclusions: The monoclonal FemtoLab H. pylori, using a cutoff 0.19 is a very sensitive, specific and easy to perform diagnostic tool for the primary diagnosis of Hp infection in Turkish, dyspeptic patients.
P853: Evaluation of two different enzyme immunoassays for detection of Helicobacter pylori in stool specimens of Turkish dyspeptic patients after eradication therapy
B. Kocazeybek, Y. Erzin, S. Altun, S. Saribas, A. Dobrucali, M. Aslan, S. Erdamar, A. Dirican (Istanbul, TR)
Aim: To assess the reliability of two different enzyme immunoassays(EIAs) in detecting the Hp status in stool specimens of Turkish, dyspeptic patients in the post-treatment period.
Materials and methods: 48 patients with non-ulcer dyspepsia(NUD) who were positive for Hp underwent a one week regimen of triple therapy. Stool samples of patients were obtained 2–6 weeks and 13C-urea breath test(UBT) was performed 6 weeks after eradication therapy in order to assess the reliability of a monoclonal (FemtoLab H. pylori, Connex, Martinsried, Germany) and a polyclonal (Premier Platinum HpSA, Meridian Diagnostics Inc., Cincinnati, USA) stool antigen test and to compare their diagnostic accuracies. The χ2 and Fisher's exact tests were used for statistical comparison of the values.
Results: Using a cutoff 0.19 for FemtoLab H. pylori and 0.16 for Premier Platinum HpSA the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy of the former and latter tests were 93%, 67%, 56%, 96%, 75% versus 87%, 33%, 37%, 85%, 50% 2 weeks and 93%, 88%, 78%, 97%, 90% versus 67%, 70%,50%, 82%, 69% 6 weeks after completion of eradication therapy, respectively. Both at the 2nd and 6th weeks in the post-treatment period the diagnostic accuracy of FemtoLab H. pylori was significantly superior to Premier Platinum's (75% versus 50%, χ2 = 6.4; p = 0.011, and 90% versus 69%, χ2 = 6.316; p = 0.012 respectively).
Conclusions: The monoclonal FemtoLab H. pylori, using a cutoff 0.19 is sensitive and specific enough to monitor Hp infection in Turkish, dyspeptic patients 6 weeks after completion of eradication therapy.
P854: Helicobacter pylori cag pathogenity island genes cagA, cagE and vacA subtypes in Turkish dyspeptic patients
B. Kocazeybek, Y. Erzin, V. Koksal, S. Erdamar, S. Altun, A. Dobrucali (Istanbul, TR)
Objectives: Although more than %50 of the world's population is infected with Helicobacter pylori(Hp), only a minority of carriers develop serious gastroduodenal diseases. So, it is important to define whether strains with specific genotype are associated with the clinical outcome. The aim of this study was to determine the distribution of the cagA, cagE and vacA subtypes of Hp in patients with various gastroduodenal diseases in Turkey, and to explore the association between genotype and the clinical outcome of infection.
Methods: 93 strains of Hp were isolated from cultures and pathological archives of 30 patients with non-ulcer dyspepsia (NUD), 30 with duodenal ulcer(DU) and 33 with gastric carcinoma. The cagA, cagE and vacAs1a/s1b, m1/m2 genotypes were determined by polymerase chain reaction methodology.
Results: There were no statistically significant difference among three different clinical outcomes according to the positive rates of vacA s1b, s2 and vacA m1/m2. But the positive rates of vacA s1a, cagA and cagE were 66.7% (20/30), 50% (15/30) and 26.7% (8/30) in NUD; 93.3% (28/30), 83.3% (25/30) and 66.7% (20/30) in DU; 87.9% (29/33), 84.8% (28/33) and 81.8% (27/33) in gastric cancer group, respectively, showing statistically significant difference (p = 0.015, p = 0.002, p = 0.001, respectively). The prevalence of vacAs2 and m2 in NUD patients was higher than that in duodenal ulcer group, but this difference was not statistically significant.
Conclusions: Helicobacter pylori cagA, cagE and vacAs1a genotypes have a significant relation with duodenal ulcer and gastric carcinoma in Turkish population. There were no statistically significant association of the vacA s1b, s2 and vacA m1/m2 strains among disease groups.
P855: Clinical relevance of iceA1, iceA2 and babA2 genotypes of Helicobacter pylori in Turkish patients with non-ulcer dyspepsia, duodenal ulcer and gastric cancer
B. Kocazeybek, Y. Erzin, V. Koksal, S. Erdamar, S. Altun, A. Dobrucali, A. Oner (Istanbul, TR)
Objectives: The clinical relevance of the Helicobacter pylori(Hp) adherence factor, babA gene, and the other virulence determinant, iceA gene, has not yet been determined in Turkish clinical isolates to date. Therefore, the aim of this study was to evaluate the prevalence of iceA1, iceA2 and babA2 Hp genotypes in Turkish patients with non-ulcer dyspepsia(NUD), duodenal ulcer(DU) and gastric cancer.
Methods: 30 strains were isolated from patients with NUD, 30 were isolated from individuals with DU and 33 were isolated from patients with gastric cancer. Bacterial DNA was extracted from cultures and Hp positive paraffin-embedded biopsy samples and genotyping of iceA and babA2 was carried out utilizing polymerase chain reaction molecular technique by using specific primers.
Results: The iceA1, iceA2 and babA2 genotypes were detected in 75.3% (70/93), 24.7% (23/93), 53.8% (50/93) respectively, of the Hp strains studied. The prevalence of iceA1 in gastric cancer patients was higher than that in NUD group, 84.8% (28/33) and 60% (18/30), respectively (p = 0.045). The prevalence of iceA2 in NUD group was higher than that gastric cancer patients, 40% (12/30) and 15.2% (5/33), respectively (p = 0.045). The positive rates of babA2 were 23.3% (7/30) in NUD; 46.7% (14/30) in DU and 87.9% (29/33) in gastric cancer group, showing statistically significant difference (p = 0.0001).
Conclusions: BabA2 genotype distribution was evaluated in different gastric pathologies in Turkish population and was a good marker for the presence of DU and gastric adenocarcinoma. Thus, our current results confirm previous experimental studies indicating a central role of Hp's adhesin and Lewis antigens in the pathogenesis of ulcer disease and adenocarcinoma.
P856: Influences of interleukin 1B and interleukin 1RN polymorphisms on the development of non-ulcer dyspepsia, duodenal ulcer and gastric cancer in Turkish population
B. Kocazeybek, Y. Erzin, V. Koksal, S. Erdamar, S. Altun, A. Dobrucali (Istanbul, TR)
Objectives: IL-1B and IL-1RN gene polymorphisms (which encode interleukin 1B and interleukin-1 receptor antagonist, respectively) have been associated with development of gastric atrophy and with increased risk of gastric carcinoma. The aim of this study was to determine the influences of host IL-1B -31TC, IL-1B -511CT and IL-1B RN gene polymorphisms on the development of various gastroduodenal pathologies in 93 Helicobacter pylori (Hp) positive Turkish patients [(30 with non-ulcer dyspepsia (NUD), 30 with duodenal ulcer (DU) and 33 with gastric cancer (GC)].
Methods: Genomic DNA was extracted from Hp positive paraffin embedded gastric biopsy samples of 30 NUD, 30 DU and 33 GC patients. IL-1B and IL-1B RN gene polymorphisms were analysed by polymerase chain reaction-restriction fragment length polymorphism. These polymorphic sites include promoter regions of IL-1B at positions-511 (C–T transition) and - 31 (T–C transition), and IL-1 RN variable tandem repeats (intron2 VNTR).
Results: There were no statistically significant difference among three clinical outcomes in the frequencies of IL-1B -511CT + TT and IL-1B -31 TC + CC genotypes (as called proinflamatory genotypes) (p = 0.161 and p = 0.077, respectively). The prevalence of the proinflamatory IL-1B RN 1/2 + 2/2 alleles in GC group was higher than that in NUD and DU groups. The frequencies of IL-1B RN 1/2 + 2/2 alleles were 20.0% (6/30) in NUD; 31.0% (9/30) in DU; and 57.6% (19/33) in GC group, showing statistically significant differences (p = 0.006).
Conclusions: There were no statistically significant difference among three clinical outcomes in the frequencies of IL-1B - 511CT + TT and IL-1B -31 TC + CC genotypes, whereas proinflamatory IL-1B RN *2 allele (1/2 + 2/2) was associated with gastric cancer in Turkey.
P857: Rapid detection of clarithromycin-resistant Helicobacter pylori in patients with dyspeptic by fluorescent in situ hybridisation (FISH), in comparison with E-test
M. Moosavian, S. Tajbakhsh, A. Samarbafzadeh (Ahwaz, IR)
Objectives: Isolation of H. pylori from more than 90% of the patients with peptic ulcer have demonstrated a strong relationship between these bacteria and created ulcers or dyspeptic. Recovery of the patients will be accelerated, if clarithromycin be added to therapeutic protocol. The objectives of this study are: 1-Rapid detection of the susceptible or resistant strains of Helicobacter pylori to clarithromycin, in patients with dyspeptic by FISH technique. 2-Comparison of the results of FISH & Epsilometer test (E-test) techniques.
Methods: Frozen – sections of gastric biopsies of 50 patients with dyspeptic were hybridized in situ by 5 fluorescent oligonucleotide probes (FISH). The prepared slides were examined under a fluorescent microscope, after staining with DAPI. Also, susceptibility and resistance of isolated strains of H. pylori to clarithromycin were determined by E-test. Both results of E-test and FISH techniques were compared in final.
Results: 25 out of 50 examined gastric biopsy samples were positive for H. pylori by FISH. Out of these 25 H. pylori strains, 17 strains (68%) were susceptible, 6 strains (24%) were resistant and 2 strains (8%) were mixture of susceptible and resistance strains to clarithromycin. This study showed no significant different between FISH and E-test results, in view of number in susceptible or resistance strains.
Conclusions: Since the patient gastric biopsies are not routinely cultured in the most of clinical laboratories, also, for isolation of H. pylori, it is needed to enriched and selective media and the other way, clarithromycin is an expensive drug, so, it looks like that FISH technique is a suitable method for replacing of the culture, antibiotic sensitivity test and or E-test method.
P858: Diagnosis of atrophic gastritis from a blood sample
P. Douramani, S. Mavrea, A. Arkas, A. Adamopoulos, E. Anastasakou (Athens, Paros, GR)
Introduction: The majority of gastritis is related to infectious agents, where H. pylori is the most important and common. H. pylori gastritis could proceed, over time, to atrophic form of gastritis a serious disease that increases the risk of peptic ulcers and gastric cancer. A new test panel was developed for non-endoscopic diagnosis of atrophic antrum and corpus gastritis from a blood sample.
Aim: To investigate whether atrophic gastritis can be diagnosed and typed non-endoscopically if the serum levels of pepsinogen I (S-PGI) and gastrin-17 are assayed in connection with H. pylori testing.
Materials and methods: The study population consists of 50 selected dyspeptic outpatients with (cases) or without (controls) advanced (moderate or severe atrophic gastritis) who underwent a diagnostic gastroscopy for dyspeptic symptoms. Of the 50 selected patients,28 (cases) had an advanced atrophic gastritis or a resected stomach. Of these 28 cases, 4 had an advanced antrum-limited atrophic gastritis, 6 had resected antrum,15 had a corpus limited advanced atrophic gastritis. Two patients had an advanced atrophic gastritis in both the antrum and corpus (multofocal atrophic gastritis) and the whole stomach was removed in one patient. The controls comprise 22 patients of whom 10 had a non atrophic H. pylori gastritis; the antrum and corpus were normal and healthy in 12 patients. The sample for ‘postprandial’ gastrin -17 (S-G-17 prand) was taken 20 min after a protein drink. The S-G-17, S-PGI and IgG class antibodies to H. pylori were determined using ELISA methods.
Results: A low S-PGI (<25 mg/l) was found in 15 of 18 patients (83%) with and in 2 of 32 patients (6%) without corpus atrophy. A low S-G-17 prand (<5 pmol/l) was found in all 4 patients with H. pylori associated antral-atrophy and in 5 of 7 patients (71%) with resected antrum but in one of 10 patients (10%) with H. pylori-related non-atrophic gastritis. The mean values of both S-G-17 prand and S-PGI decreased with increasing grade of antral and corpus atrophy respectively. Among all patients with atrophic gastritis,24 of 28 patients (86%) had a low S-PGI and/or a low S-G-17 prand with positive IgG H. pylori antibodies. Such low values were found only in one of the 22 (4.6%) control patients.
Conclusions: Low serum levels of G-17 and S-PGI are diagnostic markers of atrophic antral and corpus gastritis, respectively. A low S-G-17prand is a sigh of the multifocal or antrum-limited atrophic gastritis in patients infected with H. pylori.
P860: Helicobacter pylori in gastric mucosa: an ultrastructural study
E. Ozbek, A. Ozbek, H. Dursun, O. Vuraler (Erzurum, TR)
Objectives: Helicobacter pylori are extraordinary among bacteria in their ability to colonize the human gastric mucosa, an inhospitable acidic environment, and to stay on there for long periods as decades in despite of host immune and inflammatory responses. In this study, we aimed to research where H. pylori are found within the stomach by transmission electron microscopy (TEM).
Methods: Gastroscopic biopsy samples from patients suspected with gastritis or peptic ulcer were processed for both of PCR and TEM. The presence of H. pylori in biopsy samples was investigated with PCR method by using specific 23 S ribosomal RNA primers. The samples for electron microscopic examination were fixed in 3% glutaraldehyde, postfixed in 1% osmic acid, dehydrated in acetone, and embedded in Araldite. Plastic blocks of positive samples for the presence of H. pylori confirmed by PCR were cut with a Nova LKB Bromma ultratome. Thin sections were stained with uranyl acetate and lead citrate, and examined by using a Jeol 100 SX transmission electron microscope.
Results: We observed that cross- and longitudinal-sectioned H. pylori within the mucus layer overlying gastric epithelium, in the intercellular spaces between gastric epithelial cells (figure 1), and between two microvilli protruding from the apical surface of an epithelial cell into the gastric lumen. Apart from the extracellular H. pylori, we found also intravacuolar H. pylori within the epithelial cells of the gastric mucosa. We observed H. pylori engulfed by pseudopod-like structures at the apical part of the epithelial cells. There were also late endosomal vacuoles containing H. pylori within the deeper cytoplasmic parts of the cell.
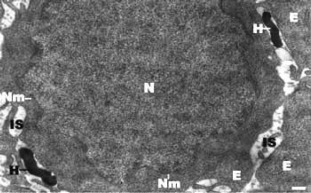
Conclusion: Although H. pylori is considered generally a noninvasive pathogen, our electron microscopic observations prove that H. pylori is able to invade gastric epithelial cells, and to enter large cytoplasmic vacuoles. That H. pylori is able to be found intracellularly might explain why the eradication of H. pylori infection is difficult with the antibiotics such as gentamicin that cannot easily cross the eukaryotic cell membrane. Abbreviations for figure 1: H, Helicobacter pylori; N, nucleus of a gastric epithelial cell; E, cross-sectioned epithelial cells; Nm, nuclear membrane; IS, intercellular space. Bar = 0.5 micrometre
P861: Helicobacter pylori and association with histological findings in endoscopic biopsies in western Greece
C. Petropoulos, E. Jelastopulu, M. Kardara, S. Spiropoulos (Erymanthia, Patras, GR)
Objectives: There is evidence that Helicobacter pylori (H. pylori) infection is strongly associated with gastric and duodenal lesions in general population. In this study we reviewed gastroscopic and histological records of patients who underwent gastroscopy for multiple reasons in a tertiary hospital in order to evaluate the frequency of H. pylori colonization in biopsy specimens and to examine the association between H. pylori infection and histological findings.
Methods: The medical records of 251 patients who presented to the General Hospital ‘Agios Andreas’ in Patras, Western Greece, during the period 2002–03 for upper gastrointestinal complaints and other specified symptoms were reviewed for the presence of H. pylori. All patients have been submitted to endoscopy with biopsy mainly of the gastric mucosa. The statistical analysis was performed using the SPSS.
Results: Gastroscopies and biopsies were undertaken in 251 patients (149 men, 102 women; mean age 58.5, range 16–95 years). In 140 (59.1%) of the patients dyspepsia was the main indication for gastroscopy, followed by 44 (18.6%) patients with anaemia, 12 (5.1%) patients with black faeces and 11 (4.6%) patients with reflux. Usual macroscopic findings were oedema (70%), hyperaemia (50%), erythema (22.3%), ulcer (16.8%) and erosions (7.5%). The histological examination revealed chronic gastritis in 209 (83.3%) subjects (in 39% of mild form, in 50% of moderate and in 11% of severe form), atrophic chronic gastritis in 8 (3.1%) and adenocarcinoma in 10 (3.9%) patients. The overall colonization of H. pylori was detected in 80 (34.2%) subjects. In case of H. pylori positive patients, chronic gastritis was found in 15.4% of mild form, in 61.5% of moderate and in 23.1% of severe form, whereas in absence of H. pylori infection the histological type of chronic gastritis was 52.5%, 43.2% and 4.3% respectively. In case of chronic gastritis of severe form H. pylori colonization was found in 75% (p < 0.001), whereas regarding the mild form H. pylori presence was observed only in 14% (p < 0.001).
Conclusions: The study reveals that H. pylori infection is strongly associated with the severe form of chronic gastritis. Thus, for the optimal management and treatment of the patients with gastritis a biopsy of the mucosa appears to be necessary.
MRSA – virulence, genes, VISA and treatment
P862: Molecular analysis of methicillin-resistant Staphylococcus aureus genes in isolates inhibited by natural products
N.S. Mariana, N.I. Mashan, S. Zamberi, A.R. Raha, V. Neela (Selangor, MYS)
Objective: The ultimate aim of the study is to explore potential natural products as alternative for treatment of infections from Staphylococcus aureus including methicillin resistant Staphylococcus aureus (MRSA). The specific objective of the paper is to assay for molecular changes in the genes of MRSA isolates upon inhibition by natural products. Five genes of MRSA isolates study include mecA, mecI and mecRI adaB and sav1017 and the non-MRSA isolates were adaB and sav1017 genes. The adaB gene encodes for methyltransferase activity for DNA repair mechanism while the sav1017 is the cell wall protein gene.
Methods: MRSA and non-MRSA isolates were obtained from patients receiving treatment in Malaysian hospitals. These isolates were subjected to growth in methanol extract of marine seaweed. Inhibition assay of extract on isolates including several genera of the gram-negative bacteria, were determined by the disc diffusion and minimum inhibitory (MIC) methods. Treated and untreated isolates inhibited by extract were
subjected to PCR amplification, followed by commercial sequencing, RT-PCR assay of the mRNA followed by sequencing of the cDNA and BLASTN analysis with the GenBank sequences.
Results: The inhibition assay of methanol extract showed activity only in MRSA and non-MRSA isolates but not in gram negative isolates. The nucleotide sequences changes were seen in four genes of treated MRSA isolates which were the mecA, mecRI, mecI and the adaB. The nucleotide changes in non-MRSA and MRSA were only seen in the adaB gene but not the sav1017. The BLASTN analysis showed variation in nucleotide changes in all genes involved in MRSA phenomenon.
Conclusions: These preliminary results utilizing genomics for study on nucleotide sequences of pathogen can aim at utilizing the biomolecules from natural products to target the affected nucleotides so as to inhibit growth of the organism. The research activity has the potential of speeding up drug discovery programme and the nucleotide changes in several genes treated with the extract indicates the potential target sites of the extracts. The inhibitory effect of extract on the nucleotide of some genes remained unchanged in the PCR and RT_PCR assay, indicating selective effect of extracts on the genes and the extracts has the potential to be applied as antibacterial agents. Implication of the findings is directed towards discovery of antibacterial drug target sites, which warrants further study.
P863: Phenotypic and genotypic characteristics of Staphylococcus aureus strains defective in species-specific proteins
A. Luczak, J. Krzyszton-Russjan, K. Nowak, W. Hryniewicz (Warsaw, PL)
Objectives: The objective of this study was to characterise phenotypically clumping factor and/or coagulase defective S. aureus.
Methods: The study was performed on 170 S. aureus isolates identified between 1996 and 2004 as clumping factor (CF) or free coagulase (FC) defective by clinical microbiology laboratories and submitted to National Institute of Public Health in Warsaw for verification. Reidentification included detection of clumping factor, coagulase, thermonuclease, and ability to ferment mannitol. Antimicrobial susceptibility testing was performed by disk-diffusion method according to the NCCLS. Glycopeptides susceptibility was determined by screening method, MIC evaluation and population analysis. PCR reactions were performed to confirm the presence of species specific genes, as cfa, cfb, coa, nuc, spa. To obtain isolates clonality, Multiple-Locus Variable-Number Tandem Repeat Analysis (MLVA) was applied.
Results: Based on the phenotypic reidentification methods, 114 (67%) isolates were phenotypically defective in respect to clumping-factor or coagulase production. All but one isolate exhibited the presence of the genes encoding CF or FC. Seventy-five (67%) isolates were resistant to methicilin (MRSA) and multiresistant. Twenty-six (22.8%) isolates showed reduced glycopeptides susceptibility in PAP. All hVISA and hGISA isolates were MRSA and all were defective mainly in clumping-factor production. Thirty-one different MLVA groups were distinguished. The A and L groups were the most common and variable. The A type was the most prevalent in hVISA/hGISA isolates and found in 18 centres.
Conclusion: The clonal spread of S. aureus defective in species specific proteins was revealed. The correlation between decreased susceptibility to glycopeptides and defective species specific proteins was observed.
P864: Detection of Panton-Valentine leucocidin and other staphylococcal toxins using oligonucleotide arrays
S. Monecke, R. Ehricht (Dresden, Jena, D)
Objectives: The recent outbreaks of community acquired MRSA (cMRSA) harbouring Panton-Valentine Leucocidin (PVL) caused serious concern worldwide. In order to screen clinical isolates, we designed and tested an oligonucleotide array which can detect both components of this virulence factor, six staphylococcal superantigens and the two exfoliative toxins as well as several resistance genes and species-specific controls.
Methods: Twenty-two clinical isolates (two suspected cMRSA and twenty randomly selected) from swabs obtained from a dermatological clinic in Saxony/Germany were cultured. DNA was isolated and subjected to a linear multiplex amplification incorporating biotin-labeled dUTP into the amplicon. Hybridization of the amplicons to the array was detected using an enzymatic precipitation reaction.
Results: In two cases of chronical furunculosis, PVL-positive cMRSA were identified. One case was a soldier returning from a peace mission to Kosovo where he apparently contracted the disease, the other one was his spouse. In three other cases of furunculosis/abscesses, PVL-positive but methicillin-susceptible S. aureus were found. Staphylococcal enterotoxins were found in four, toxic shock syndrome toxin in three isolates, and exfoliative toxin A in one isolate. In two cases, multiple toxins were found (PVL + tst + entC and entB + entK + entQ + etA).
Conclusions: While epidemic cMRSA strains often can presumably be identified due to their resistance profile (methicillin, tetracycline, fusidic acid), there is no easy method to detect PVL-positive, methicillin-susceptible S. aureus. Therefore, strains carrying PVL are more common than previously suspected. The high prevalence of this virulence factor as well as of other toxins found in the present study warrants further investigations.
P865: Characterisation of methicillin-resistant Staphylococcus aureus harbouring the Panton-Valentine leucocidine
A. Anders, M. Kaase, S. Friedrich, S.G. Gatermann (Bochum, D)
Objectives: Until now methicillin-resistant Staphylococcus aureus (MRSA) have been known only as a major problem in hospitals. Lately, a new kind of MRSA has been described. This MRSA is responsible for community-acquired infections (c-MRSA) and harbours the determinant for the Panton-Valentine leucocidine (PVL). As there are descriptions of c-MRSA possessing the PVL throughout the world with different MLST types we wanted to characterize eleven c-MRSA from our area possessing the gene for Panton-Valentine leucocidine.
Methods: The isolates were found from 1999 until the summer of 2004, the gene encoding PVL was verified by PCR. We determined the PFGE pattern, the MLST type, the SCCmec type and the agr allele type of the eleven isolates.
Results: So far all isolates belong to the ST 80 which has been also described elsewhere in Germany and in France but differs from the types found in the US (1 and 8) or in Australia (30 and 298). They possess a SCCmec element of type IVb and the agr3 allele type. All isolates were resistant to oxacillin, which was determined by mecA PCR, and all were resistant to fusidic acid. Only two were additionally resistant to erythromycin. No resistance could be found to fluoroquinolones. The average age of patients was 47 years and they all had severe community-acquired abscesses of the skin or soft tissue that caused hospital admission.
Conclusion: MRSA cannot be longer considered as affecting only hospitalized and elderly patients but we should also be aware of them in community-acquired infections.
P866: Accessory gene regulator group polymorphism in methicillin-resistant Staphylococcus aureus in Korea: an association with clinical significance
H.J Yoon, J.Y. Choi, J.M. Kim, D. Yong, K.W. Lee, Y.G. Song (Seoul, KOR)
Background: Genetic variation among S. aureus strains has been shown to be associated with pathogenic potential. Virulence gene expression in S. aureus is controlled by regulators such as accessory gene regulator (agr), and its locus of S. aureus is a quorum-sensing gene cluster of five genes (hld, agrB, agrD, agrC, and agrA) that upregulates production of secreted virulence factors, including the alpha-, beta-, delta-hemolysins, and downregulates production of cell-associated virulence factors. S. aureus strains can be divided into 4 major agr groups (agr I-IV) on the basis of a polymorphism in agrD and agrC. The purpose of this study is to know the proportion of agr I, II, and III polymorphisms and to compare clinical characteristics between group II and non-group II polymorphism of methicillin-resistant Staphylococcus aureus (MRSA) strains in a tertiary care teaching hospital in Korea.
Methods: Isolates were identified as S. aureus by conventional methods. Susceptibility to methicillin was determined by the NCCLS guideline. Agr locus was identified using restriction fragment length polymorphisms (RFLPs) analysis of agr BDC amplicons with DraI digestion. The factors assessed included the patients’ demographics, comorbidities (diabetes mellitus, congestive heart failure, peripheral vascular disease, dialysis-dependent renal failure, cirrhosis, malignancy, and alcoholism), infection site (central catheter-related bacteraemia, bacteraemia of unknown origin, device, endocarditis, intraabdominal, respiratory, skin, urine, and ear), receipt of mechanical ventilation and operation, the presence of nosocomial infection and treatment failure, creatinine level, and mortality.
Results: A total of 18 strains from 18 MRSA-infected patients (7 males and 11 females) were evaluated. Their mean age was 50.5 ± 24.3 years old. There were 4 (22.2%), 12 (66.7%), and 2 (11.1%) strains in agr group I, II, and III polymorphism, respectively. Only nosocomial infections were statistically significant clinical parameter according to univariate analysis (p = 0.009) and multivariate analysis (OR, 22.0 (1.540 – 314.292); P, 0.023).
Conclusion: Agr group II was most prevalent in this study and nosocomial infections were correlated with group II polymorphism. This result suggests virulence and nosocomial spread of MRSA strains are originated from group II polymorphism. A recruit of more strains will increase and clarify the clinical difference between agr groups.
P867: Distribution of toxic shock syndrome toxin-1, exfoliative toxins and enterotoxins SEG and SEI among methicillin-resistant Staphylococcus aureus clonal types
V. Chini, G. Dimitracopoulos, I. Spiliopoulou (Patras, GR)
Objectives: Staphylococcus aureus produces a variety of exotoxins including the toxic shock syndrome toxin-1 (TSST-1), the exfoliative toxins ETA and ETB and the enterotoxins SEG and SEI. The SEG and SEI genes (seg and sei) coexist in the same operon. The aim of this study was to investigate the presence of genes encoding the TSST-1 (tst), ETA (eta), ETB (etb), SEG (seg) and SEI (sei) among methicillin-resistant S. aureus (MRSA) clinical isolates, in relation to their clonal types.
Methods: The MIC of oxacillin was determined by the agar dilution method in Mueller–Hinton agar supplemented with 2% NaCl according to the guidelines of NCCLS. PBP2a production was investigated by a Latex agglutination test (bioMerieux) in all S. aureus isolates with MIC >0.5 mg/L. PCR amplification was performed for the detection of mecA gene to the aforementioned isolates, from different patients, during 2001–2003, resulting to 160 MRSA. The presence of tst, eta, etb, seg and sei genes was also investigated by PCR. Clonal types were determined by PFGE of chromosomal DNA SmaI digests.
Results: Among the 160 MRSA, 35 (22%) carried both seg and sei genes, 24 (15%) isolates carried the tst, 2 (1%) the eta, whereas no strains exhibited the etb gene. Precisely, during 2001 the tst gene coexisted in 12 out of 13 seg/sei-positive strains. Eleven strains belonged to PFGE type A, whereas the other two to type B, mainly associated with wound infections. Eight MRSA in 2002 belonging to PFGE type A, carried tst, seg and sei. Two more strains carrying seg/sei, belonged to PFGE type C. Two out of 3 seg/sei-positive additional MRSA which were characterized as a new clone F, carried also eta. In 2003, four MRSA carrying the tst, seg and sei belonged to clone A, whereas 5 more carrying the seg/sei were characterized as PFGE type C. Most isolates were associated with wound infections and abscesses.
Conclusions: During the study period (2001–2003) the incidence of the tst gene carriage among MRSA was reduced from 26% to 6%, while the seg/sei genes were almost constantly present. The distribution of these genes was mainly associated with strains of clonal type A, exhibiting a drift towards clone type C predominant during the last two years.
P868: Detection of decreased susceptibility to glycopeptides in Staphylococcus aureus using tablet (disc) prediffusion
S.V. Nielsen, J.B. Casals (Taastrup, DK)
Objectives: The aim of the study was to develop a screening and confirmatory method to detect Staphylococcus aureus with decreased susceptibility to glycopeptides (hVISA/VISA and GISA).
Methods: The glycopeptide resistance of 20 Staphylococcus aureus strains from our strain collection including well-known resistant strains (ATCC 700788, ATCC 700789, ATCC 700698, ATCC 700699) was examined. We compared: (i) zone sizes of Vancomycin 5 μg and Teicoplanin 30 μg Neo-Sensitabs (Rosco Diagnostica) when prediffused for 2 h (with disc) + 18 h (without disc) on Mueller–Hinton and BHI, both media supplemented with 5% horse blood, (ii) agar dilution MICs (iii) zone sizes around Cefoxitin 60 μg Neo-Sensitabs. The inoculum used was McFarland 0.5 and the plates were incubated for 24 h at 35°C.
Results: Regression lines were prepared and there was a good correlation between MICs for vancomycin and teicoplanin and the corresponding zone sizes. All hVISA/VISA/GISA strains tested showed zones less than 15 mm with Cefoxitin 60 μg and zones ≤ 21 mm (teicoplanin) and/or ≤ 23 mm (vancomycin) on MH Blood Agar, corresponding to MICs > 2 μg/ml for both antimicrobials. On BHI agar the zones were ≤ 17 mm (teicoplanin) and/or ≤ 21 mm (vancomycin) for the hVISA/VISA/GISA strains corresponding to MICs > 4 μg/ml for both antimicrobials.
Conclusion: Zones obtained by agar diffusion methods using prediffusion with Vancomycin and Teicoplanin Neo-Sensitabs correlated with MICs and predicted hVISA/VISA/GISA strains. For screening high resistance to Cefoxitin (zones <15 mm) may be used to select strains for further testing in a daily routine laboratory. The system should be evaluated further in the routine diagnostic laboratory.
P869: High rate of vancomycin intermediate Staphylococcus aureus among methicillin-resistant isolates in Taiwan
J. Lu, S.-Y. Lee (Taipei, TW)
Objectives: One thousand and five hundred consecutive methicillin-resistant Staphylococcus aureus (MRSA) isolates collected from 637 patients in the Tri-Service General Hospital in Taiwan were screened for vancomycin resistance and isolates with reduced susceptibility to vancomycin were further studied for their characteristics.
Methods: Brain heart infusion agar plates containing vancomycin (5 μg/mL) (BHIA-VA5) were using for vancomycin resistance screening. Minimum inhibitory concentration (MIC) of vancomycin was determined on both BHIA and the standard Mueller–Hinton agar (MHA) on screened-positive isolates. For strains with MICs equaled to 8 μg/mL, characteristics including population analysis, susceptibility to triton X-100 induced autolysis, van gene and pulsed field gel electrophoresis (PFGE) typing were further performed as previously described.
Results: Of the 230 isolates that grew on BHIA-VA5 plates (15.3%, 230/1500), 43 (2.9%, 43/1500) were with a minimum inhibitory concentration (MIC) of 8 μg/mL for vancomycin when BHIA was used. However, when the standard MHA was used, only 8 (0.5%, 8/1500) were confirmed to be vancomycin intermediate S. aureus (VISA). Population analysis also displayed a homogeneous intermediate-resistant to vancomycin among the 8 isolates. The remaining 35 isolates were classified as heterogeneous intermediate-resistant (28) or susceptible (7) to vancomycin according to the definition by Hiramatsu et al. Six of the 43 isolates were with reduced susceptibility to autolysis which was induced by triton X-100. The 43 MRSA with reduced susceptibility to vancomycin were isolated from 21 patients, 13 of whom had received glycopeptide treatment before the isolation. Five patients died despite vancomycin therapy. No enterococal vancomycin resistance genes were detected among the 43 isolates. Pulsed-field gel electrophoresis (PFGE) revealed that these 43 isolates belonged to 2 PFGE types (Types A and B). The type A was most prevalent in this survey.
Conclusion: We have demonstrated the first VISA reports and the high prevalence of VISA among methicillin-resistant isolates in Taiwan.
P870: Screening for methicillin-resistant Staphylococcus aureus with reduced susceptibility to glycopeptide in a Belgian hospital
Y. Glupczynski, O. Denis, C. Berhin, C. Nonhoff, A. Deplano, Y. Degheldre, M.J. Struelens (Yvoir, Brussels, B)
Background: MRSA isolates with decreased susceptibility to glycopeptides (GISA) have been reported worldwide since 1997. Most strains were isolated from catheters and other foreign bodies in patients treated with glycopeptides. We aimed to determine the prevalence of GISA isolates in a Belgian hospital where MRSA has been endemic for many years.
Methods: All MRSA isolates collected between 09/98 and 06/04 were screened for reduced susceptibility to glycopeptides on Mueller–Hinton agar and 5 mg/L teicoplanin (MH-teico) as recommended by the CASFM. The macromethod Etest (BHI agar, 2 McFarland (MF) inoculum, 48 h incubation) was performed as secondary screening for all isolates which grew 4 colonies on MH-Teico. GISA/h-GISA phenotypes were confirmed by E-test MIC determination on MH agar with 0.5 MF and 24 h incubation as well as by vancomycin (V) and teicoplanin (T) population analysis profiles (PAP). All confirmed GISA/h-GISA isolates identified were compared by PFGE to other strains identified in Belgium in order to delineate their clonality.
Results: Among 520 MRSA strains (from 468 patients), 14 isolates showed growth on MH-Teico and 8 of these (from 7 patients) yielded a positive macromethod E-test (MIC 8 μg/ml for V and T). Seven were confirmed by PAP as h-GISA and one as a GISA (T MIC: 32 μg/ml; V MIC: 8 μg/ml). Origins of the isolates were: lower respiratory tract (4), urine (2) and wound (2). All h-GISA strains had a similar antibiotic resistance phenotype by disk diffusion (gentamicin, rifampin, erythromycin, clindamycin, ofloxacin). By molecular analysis, the h-GISA/GISA isolates clustered in two different PFGE groups A (n = 6) and G (n = 1). The A PFGE group was previously described in h-GISA isolates in Belgium. In this study, it was subdivided in 2 types, both including 3 strains. One PFGE type resulted in a small outbreak in 3 patients during a stay in ICU. All 5 other isolates were sporadic with no apparent geographic or temporal relationship between cases.
Conclusion: GISA/h-GISA were found in only 7 out of 468 (1.5%) MRSA-positive patients. None of them presented with severe infection nor had any previous known exposure to glycopeptides. In view of the low prevalence of GISA/h-GISA in our hospital, screening should not be performed systematically but rather on an individual basis taking into account clinical data and risk factors. Whenever the occurrence of GISA is considered, Teico-MH agar appears as a suitable first screening approach.
P871: A case-control study to evaluate the economic outcome of early PO linezolid in patients with methicillin-resistant Staphylococcus aureus infections
S. Davis, M. Shieh, D. Levine, P. McKinnon (Detroit, St. Louis, USA)
Oral therapy with linezolid (LZD) has the potential to decrease hospital costs and shorten length of stay of patients with Grampositive infections who would otherwise continue to receive IV therapy.
Objective: To evaluate the impact of early PO conversion to LZD in patients receiving traditional IV therapy for methicillin-resistant S. aureus (MRSA) infections.
Methods: Patients with documented MRSA infection between 2001 and 2004 were evaluated in a matched case-control study. Cases included patients who were converted to PO LZD from IV LZD or IV vancomycin (VANC), and controls were patients who received only IV VANC. Patients were paired in a 1:2 ratio of cases to controls and matched based on infection type, age and comorbidities. Demographics, antimicrobial agents, concomitant infections, and clinical status were assessed daily from the onset of infection through the end of treatment or hospitalization. Antibiotic cost, length of stay (LOS), and clinical success rates were compared between the groups.
Table 1.
includes comparisons of cost, duration of therapy and LOS. Predictably, patients receiving LZD in the hospital had higher drug costs; however, a decreased LOS contributed to a $7000 lower cost of hospitalization.
| Table 1 | Linezolid (n=26) Mean +/− S D Median [range] | Vancomycin (n=52) Mean +/− SD Median [range] | P |
|---|---|---|---|
| Hospital LOS (days) |
|
|
.028 |
| Antibiotic-related LOS (days) |
|
|
NS |
| IV tx in hospital (days) |
|
|
NS |
| PO tx in hospital (days) |
|
|
<.001 |
| PO tx at home (days) |
|
|
<.001 |
| IV tx at home (days) |
|
|
<.001 |
| In-hospital antibiotic costs (US$) |
|
|
<.001 |
| Cost of hospitalization (US$) |
|
|
.027 |
Results: 78 patients were assessed. Demographic characteristics were similar between groups. Average age (mean ± SD) was 46 ± 14; APACHE II (median, range) was 6 [0–22], Charlson comorbidity score 2 [0–8], and 60% were male. 55% of patients were treated for skin/soft tissue infection, 19% pneumonia, 13% bone/joint infections, 11% bacteraemia, and 2% other infections. Clinical and microbiologic outcomes were similar between groups, with 100% clinical success at the end of therapy.
Conclusions: Oral therapy with linezolid shortens LOS decreasing hospital cost of patients with MRSA infections.
P872: Linezolid vs vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan
S. Kohno, K. Yamaguchi, N. Aikawa, Y. Sumiyama, S. Odagiri, N. Aoki, Y. Niki, S. Watanabe, M. Furue, T. Ito, R. Croos-Dabrera, K.J. Tack (Nagasaki, Tokyo, Kanagawa, Niigata, Okayama, Fukuoka, JP; Ann Arbor, USA)
Objectives: To compare the efficacy and safety of linezolid (LZD) with those of vancomycin (VAN) for the treatment of infections caused by methicillin-resistant Staphylococcus aureus (MRSA) in Japan.
Methods: This was a randomized, open-label study conducted in Japan. Patients with nosocomial pneumonia, complicated skin and soft tissue infections, or sepsis syndrome, caused by MRSA, were randomized (2:1 LZD: VAN) to receive LZD, 600 mg q12 h, or VAN, 1 g q12 h. Outcomes were evaluated at end of therapy (EOT) and at a follow-up (FU) evaluation 7–14 days after completion of therapy.
Results: 151 patients received study drug (100 LZD, 51 VAN); the treatment groups were similar with regards to demographics and risk factors. At EOT, clinical success rates in the MRSA-microbiologically evaluable population were 62.9% and 50.0% for the LZD and VAN groups, respectively; microbiologic eradication rates were 79.0% and 30.0% in the two groups, respectively (p < 0.0001). At FU, the clinical success rates were 36.7% for both groups, and the microbiologic eradication rates were 46.8%, and 36.7%, respectively. Clinical success rates in both groups reflect an automatic outcome of failure for patients receiving prohibited antimicrobials prior to FU. Reversible anemia (13%) and thrombocyotopenia (19%) were reported as adverse events more frequently in LZD patients. Analysis of laboratory data showed that platelet counts decreased more frequently in LZD patients with recovery by FU. The mean platelet count in LZD patients with an adverse event of thrombocytopenia was 101,000/mm3. Significantly low platelet counts (<50,000/mm3) were more frequently observed in VAN patients (6 % vs 3%). No difference was observed in mean changes in hemoglobin levels between the treatment groups.
Conclusions: LZD is as effective as VAN for the treatment of MRSA infections in seriously ill patients, and may be more effective in achieving microbiologic eradication. Although hematologic adverse events were reported more frequently in LZD-treated patients, analysis of laboratory data showed only a mild reversible trend toward lower platelet counts.
P873: Cost-effectiveness of linezolid versus vancomycin in complicated skin and soft-tissue infection due to suspected methicillin-resistant Staphylococcus aureus infection in Germany
D. Schürmann, E. De Cock, S. Sorensen, T. Baker, A. Resch, J. Hardewig, S. Duttagupta (Berlin, D; London, UK; Bethesda, USA; Karlsruhe, D; New York, USA)
Objectives: Linezolid, a novel antibiotic, has demonstrated efficacy in infections due to suspected or proven methicillin-resistant Staphylococcus aureus (MRSA). Among patients with complicated skin and soft-tissue infections (cSSTI) due to suspected or proven MRSA, clinical cure rate was higher and length of stay (LOS) in hospital was shorter in patients treated with linezolid versus vancomycin (Weigelt J et al. Posters 314 and 315 presented at: The 41st Annual Meeting of the Infectious Diseases Society of America; October 9–12, 2003; San Diego, Calif). The objective of the present analysis was to evaluate the cost-effectiveness of linezolid compared with vancomycin in the treatment of cSSTI due to suspected MRSA infection from the German perspective.
Methods: A decision-analytic model was developed to examine the costs and outcomes of using linezolid versus vancomycin in hospitalized patients with cSSTI in Germany. An expert panel of German physicians experienced in treating cSSTI provided resource-utilization data through structured interviews. Costs from published sources (Rote Liste, DKG-NT, EBM) were applied to clinical and laboratory tests, adverse events, isolation procedures, intravenous (IV) or oral (linezolid only) drug treatment, hospitalization by ward type (medical, intensive care), and outpatient physician consultation. If appropriate, patients could be discharged from hospital and treated in an ambulant setting. The model assumed 50% of suspected MRSA patients had proven MRSA. Outcomes included total costs per patient, cost per death avoided, cost per life-year gained, and cost per cure.
Results: An additional 4.4% of patients treated with linezolid (98.4%) versus vancomycin (94.1%) were cured. Average total cost per episode was €9352 versus €9474 for linezolid- versus vancomycin-treated patients, giving a €121 saving per episode. The model was sensitive to the LOS in hospital, days in isolation, duration of oral versus IV treatment, percentage of MRSA patients, and price of linezolid.
Conclusion: In this decision analytic model, more patients with cSSTI due to suspected MRSA achieved clinical cure in the linezolid group compared with the vancomycin group. Linezolid was cost saving versus vancomycin for the treatment of cSSTI. Linezolid resulted in a shorter treatment duration and shorter LOS that offset the higher acquisition cost of linezolid versus vancomycin in cSSTI in Germany.
Training, scientific output in infectious disease
P874: A bibliometric analysis of worldwide trends in research productivity in microbiology
P. Vergidis, A. Karavasiou, K. Paraschakis, I. Bliziotis, P. Papastamataki, M. Falagas (Athens, GR)
Background: Microbiology contributes significantly to the understanding and control of infectious diseases and has always been a field of extensive research. However, the literature lacks studies estimating the quantity and quality of worldwide research production. We evaluated the contribution of different world regions in research production in the field of Microbiology.
Methods: Using the Medline database we retrieved articles from 64 journals included in the ‘Microbiology’ category of the ‘Journal Citation Reports’ database of the Institute for Scientific Information for the period 1995–2002. The world was divided into 9 regions based on geographic, economic and scientific criteria. Using an elaborate retrieval system we obtained data on published articles from different world regions. In our evaluation we introduced an estimate of both quantity and quality of research produced from each world region per year using: (1) the total number of publications, (2) the mean impact factor of publications, and (3) the product of the above two parameters.
Results: Data on the country of origin of the research was available for 76,118 out of 77,080 retrieved articles (98.8%). Western Europe exceeds all other world regions in research production for the period studied, with USA ranking second (table). The difference in production between these two regions increased gradually from 1995 to 2002. However, the mean impact factor for articles published in microbiology journals was highest for the USA (3.34), while it was 2.79 for Western Europe and 2.31 for the rest of the world (7 regions combined).
Number of microbiology articles multiplied by the impact factor of the corresponding journal.
| 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Western Europe | 7,785 | 9,744 | 9,292 | 10,434 | 11,819 | 13,201 | 14,052 | 13,716 | 90,042 |
| USA | 8,297 | 10,061 | 8,331 | 8,792 | 9,680 | 10,748 | 11,142 | 11,286 | 78,337 |
| Japan | 1,346 | 1.348 | 1,716 | 1,710 | 1,794 | 2,153 | 2,138 | 2,268 | 14,472 |
| Asia (excl. Japan) | 566 | 752 | 822 | 924 | 1,081 | 1,209 | 1,589 | 1,740 | 8,683 |
| Canada | 893 | 985 | 882 | 982 | 1,019 | 1,067 | 1,098 | 1.268 | 8,195 |
| Oceania | 600 | 568 | 636 | 644 | 635 | 815 | 839 | 926 | 5,665 |
| Latin America | 330 | 327 | 432 | 553 | 520 | 613 | 808 | 922 | 4,504 |
| Eastern Europe | 234 | 264 | 305 | 377 | 386 | 482 | 687 | 705 | 3,439 |
| Africa | 135 | 126 | 131 | 211 | 238 | 266 | 359 | 270 | 1,737 |
| Total | 20,187 | 24,175 | 22,548 | 24,627 | 27,171 | 30,555 | 32,711 | 33,102 | 215,075 |
Conclusions: USA and Western Europe make up a striking 78% of the world's research production in terms of both quantity and quality. All world regions have increased their research production during the period studied. The highest increase was achieved by Asia (excluding Japan), Latin America, and Eastern Europe.
P875: From conference abstract to full paper: differences between data presented in conferences and journals
E. Rosmarakis, P. Vergidis, A. Kapaskelis, K. Paraschakis, M. Falagas (Athens, GR)
Background: On some occasions, we noted differences between data presented in conference abstracts and subsequent published papers. We studied the frequency and the type of these differences in the fields of Infectious Diseases and Microbiology.
Methods: We reviewed all abstracts from the first session of 7 out of 15 major research categories presented in the 1999 and 2000 ICAAC. For each selected pair of ICAAC abstract and related full paper published in journals indexed by Index Medicus, two independent investigators performed a comparison of all data in the abstract and the corresponding information in the published paper. Using Cox logistic regression models we analysed variables for association with differences of data.
Results: From 190 abstracts that were reviewed, 68 (35.8%) were subsequently published as papers by March 2004. From them, 52 referred to the same study period and population for both the abstract and the paper. Differences between data presented in conference abstracts and published papers were found in 28 out of 51 pairs which were analysed further (54.9%, 95% C.I.: 41.2%–68.6%). The identified differences were related to the numbers and/or rates of the studied patients (11/28), numbers or rates of isolates (9/28), MICs values or Ki values (5/28), other chemical properties of antibiotics (2/28), odds ratio (1/28), and duration of observation (1/28). The differences were substantial in several pairs. Time to publication of full paper was found to be independently associated with presence of differences (p = 0.029, OR = 2.043 per year), while the research category, type of presentation (oral or poster), number of publications of the presenting and last author, impact factor of the journal, and country of origin were not.
Conclusions: While there are several explanations for the noted differences between data presented in conference abstracts and full papers, it is likely that the research community may improve the accuracy of presentation of data.
P876: Worldwide trends in quantity and quality of published articles in the field of infectious diseases
I. Bliziotis, K. Paraschakis, P. Vergidis, A. Karavasiou, A. Kapaskelis, M. Falagas (Athens, GR)
Background: Trying to confront with the widespread burden of infectious diseases, the society worldwide invests considerably on research. However, the literature lacks studies estimating the quantity and quality of worldwide research production. We evaluated the contribution of different world regions in research production in Infectious Diseases.
Methods: Using the Medline database we retrieved articles from 38 journals included in the ‘Infectious Diseases’ category of the ‘Journal Citation Reports’ database of the Institute for Scientific Information for the period 1995–2002. The world was divided into 9 regions based on geographic, economic and scientific criteria. Using an elaborate retrieval system we obtained data on published articles from different world regions. In our evaluation we introduced an estimate of both quantity and quality of research produced from each world region per year using: (1) the total number of publications, (2) the mean impact factor of publications, and (3) the product of the above two parameters.
Results: Data on the country of origin of the research was available for 45,232 out of 45,922 retrieved articles (98.5 %). USA and Western Europe are by far the most productive regions concerning publications of research articles, as displayed in the Table. However, the rate of increase in the production of articles was higher in the developing world regions during the study period. The mean impact factor is highest for articles originating in the USA (3.42), while it was 2.82 for Western Europe and 2.73 for the rest of the world (7 regions combined).
Number of infectious disease articles multiplied by the impact factor of the corresponding journal
| 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| USA | 6527 | 7,155 | 6,737 | 7,912 | 8,136 | 9,106 | 9,447 | 8,784 | 63,804 |
| Western Europe | 4,114 | 5,241 | 4,773 | 5,729 | 6,403 | 7,647 | 7,787 | 7,338 | 49,033 |
| Asia (excl. Japan) | 400 | 417 | 557 | 783 | 779 | 917 | 993 | 1,081 | 5,927 |
| Canada | 446 | 467 | 440 | 537 | 596 | 674 | 639 | 711 | 4,510 |
| Japan | 294 | 455 | 496 | 385 | 515 | 663 | 632 | 673 | 4,113 |
| Oceania | 239 | 343 | 334 | 392 | 391 | 548 | 472 | 434 | 3,153 |
| Central and | 199 | 257 | 271 | 360 | 374 | 457 | 467 | 593 | 2,978 |
| Latin America | |||||||||
| Africa | 198 | 189 | 303 | 337 | 478 | 433 | 532 | 443 | 2,913 |
| Eastern Europe | 78 | 93 | 117 | 117 | 168 | 237 | 232 | 283 | 1,325 |
| Total | 12,495 | 14,617 | 14,028 | 16,552 | 17,840 | 20,682 | 21,201 | 20,341 | 137,756 |
Conclusions: USA and Western Europe make up a striking 80% of the world's research production in Infectious Diseases in terms of both quantity and quality. However, all world regions present a steady increase in the production of infectious disease articles with the developing countries displaying the highest rate of increase.
P877: Does training physicians in good clinical practice make a difference in quality of running clinical trials?
M. Akova, H. Akan, I.H. Ayhan, E. Kansu, O. Akbas, C. Ari, E. Tetik, E. Taylan (Ankara, Istanbul, TR)
Objectives: Quality of clinical trials requires the implementation of the rules of good clinical practice (GCP). However, formal training for this purpose has been lacking both in undergraduate and postgraduate curricula in most medical schools in Europe. During a series of 3-days educational programme, 4 interactive GCP courses were organized between December 2003 and October 2004.
Methods: The programme included several informative lectures covering knowledge about EU Directive 2001/20/EC and ICH GCP Guidelines and interactive sessions with several case-based scenarios. The faculty was composed of a pharmacologist, an oncologist, a hematologist, an ID physician and the director of a contract research organization. Excluding the latter, all faculty members had administrative responsibilities in different universities and/or goverment institutions (i.e. ethics committees). Financial support was obtained from a pharmaceutical company. However, the sponsor had no role in organizing the scientific content of the programme.
Results: 146 physicians including ID specialists were selected from several university hospitals or tertiary care government hospitals where running clinical trials has been a common practice. Pre-training queries revealed that among the trainee population, 30.5% never obtained an informed consent from a patient, 47% did not randomize any patients for trials, 44% did not run any Phase I–IV trials, 55% did not use placebo for trial purposes and 49% did not report any serious adverse events to local and or international authorities. A 24-question pre-and post-course tests about basic principles of GCP and local and EU regulations for running clinical trials were applied to determine and compare the knowledge of the trainees on these subjects prior and after the course. The percentage of correct answers ranged 35–91% before, and 51–98% after the course was completed (p < 0.01).
Conclusions: Training in GCP and other regulations about running clinical trials may increase the awareness and knowledge of physicians. These educational activities will also help to raise the quality of clinical trials.
P878: Learning appropriate use of antibiotics (PK/PD and guidelines): a CD-ROM course for healthcare professionals and students
E. Ampe, Y. Glupczynski, P.M. Tulkens, F. Van Bambeke (Brussels, Mont-Godinne, B)
Objectives: In a context of growing resistance and limited supply of new molecules, a rational use of antibiotics should be a high priority. Our objective is to train healthcare professionals and students in PK/PD and in a correct implementation of guidelines, since this could help to improve antibiotic use in both short and mid-terms.
Methods: We developed a PK/PD - guidelines course on CD-rom, targeted to both physicians and pharmacists but also usable by students. The course was prepared by a team of 2 pharmacists, 1 clinical microbiologist, and 1 pharmacologist. Sources of information were (i) textbooks, review papers and primary papers by internationally recognized experts (ii) materials presented at training workshops of the International Society for Antiinfective Pharmacology (ISAP; www.isap.org) during the last 3 years, (iii) national and, if not available, international guidelines for the management of respiratory tract or urinary tract infections.
Results: The course is organized as a series of Power Point presentations covering in a progressive fashion the followings topics: (1) bases in microbiology (in vitro properties of antibiotics); (2) pharmacokinetics (definition of the main parameters); (3) pharmacodynamics, with (A) the concepts, (B) the methods and pertinent models, and (C) the data, including the parameters to take into account to optimize the dosage of the main antibiotic classes; (4) resistance, including (A) the main mechanisms and (B) the use of pharmacodynamics to avoid the selection of resistance; (5) the appropriate use (including appropriate dosages) of antibiotics in (A) respiratory tract and (B) urinary tract infections.
Conclusions: This course promotes continuous education in the pharmacology and pharmacotherapy of antibiotics, in a format easily usable for courses and seminars to both students and professionals.
Pneumonia
P879: The efficacy of the long-term treatment with macrolides in patients with bronchiectasis colonised by P. aeruginosa
M. Schmidt-Ioanas, M. Allewelt, A. Polzin, H. Lode (Berlin, D)
Background: Although macrolides have no intrinsic antipseudomonal activity, these drugs appear effective in controlling infection by P. aeruginosa through mechanisms such as disruption of quorum sensing or anti-inflammatory effects.
Objectives: The aim of our prospective study was to evaluate the efficacy of macrolides in patients with bronchiectasis infected and colonised by P. aeruginosa.
Methods: The study included hospitalised patients with CT evidence of bronchiectasis and presenting an acute exacerbation by P. aeruginosa, isolated in sputum. Microbiological findings, clinical data and treatment recommendations were recorded at admission and at the end of therapy. Patients completed daily diary cards for symptoms and PEF values. Patients were followed for 1 year.
Results: Twenty-two patients (14 men, mean age 57.3 ± 14.5) with bronchiectasis and P. aeruginosa infection were included. During hospital stay, patients were treated with at least two susceptible antipseudomonal drugs, according to the antibiogram (usually beta-lactam plus aminoglycoside) for a period of 16.9 ± 1.6 days. An oral macrolide (azithromycin 250 mg × 3 days/week in 10 patients, clarithromycin 500 mg daily in 12 patients) was further administrated for 4.9 ± 1.9 months. At the end of long-term therapy, 11 (50%) patients showed no evidence of P. aeruginosa in sputum, 8 (36.3%) patients still presented P. aeruginosa in sputum and 3 (13.6%) discontinued the treatment after less that 1 month because of adverse events. All patients had a significant reduction of sputum volume (83.3 ml/day before therapy vs. 22.5 ml/day at the end of therapy, p = 0.03) and of the mean number of exacerbations during follow-up (2.4 in the previous year vs. 1.2 in the follow-up year, p = 0.01). An increase of the mean PEF value was also noted, although statistically not significant (373.2 ± 43.5 l/min before therapy vs. 489.2 ± 23.5 l/min at the end of therapy, p = 0.3)
Conclusion: These observational findings suggest that macrolides may have a role in modulation of P. aeruginosa colonisation in patients with bronchiectasis.
P880: Community-acquired pneumonia requiring hospitalisation in young adults: clinical features, causative organisms, and outcomes
A. Mykietiuk, J. Carratalà, N. Fernández-Sabé, S. Padrones, R. Verdaguer, F. Gudiol (Barcelona, E)
Objectives: There is little information on CAP requiring hospitalization in young adults (≤ 40 years). We analysed clinical features, causative organisms, and outcomes of CAP in this patient population.
Methods: Prospective observational study of non-immunocompromised adult patients with CAP (1995–2003). Patients with HIV infection, transplantation, and neutropenia were not included. For the purposes of the study, patients were divided into 2 age-groups, ≤ 40 years and > 40 years.
Results: We documented 1732 consecutive patients with CAP; 150 patients (8.7%) were ≤ 40 years and 1582 were > 40 years. Mean patient ages were 30.3 years in the former group and 69.6 years in the latter group. Main reasons for hospitalization in young adults were: hypoxia (PO2 < 60) 59 patients, PORT high severity risk class (IV–V) 13 patients, empyema 9 patients, and/or shock 7 patients. Young patients were more frequently current smokers (63% vs 22%, p < 0.001). Comorbid conditions were more common in older patients (20% vs 66%, p < 0.001), mainly diabetes mellitus, COPD, and chronic heart disease. Multilobar pneumonia was more frequent in young patients (56% vs 32%, p < 0.001). The most common causative organisms were Streptococcus pneumoniae (19% vs 24%, NS) and Legionella pneumophila (9% vs 7%, NS). Atypical agents were more frequent in young adults (11% vs 4%, p = 0.001), while Haemophilus influenzae (2% vs 7%, p = 0.026) and gram-negative bacilli (0% vs 1.4%, NS) were rarely identified in this group. The frequency of bacteraemia was similar in both groups (8% vs 12%, NS). ICU admission was more frequent in young adults (13% vs 7%, p = 0.006), but no differences were found regarding the need of mechanical ventilation (5% vs 4%). Median LOS was shorter in young patients (7 vs 9 days, p = 0.002). Five young patients died; shock (2 patients) and multiorganic failure (3). Early mortality (< 48 hours) was similar in both groups (1.4% vs 2.8%). Overall mortality (< 30 days) was higher in older patients (3.4% vs 8.7%, p = 0.026).
Conclusions: CAP requiring hospitalization in young adults, mainly smokers, is not uncommon, being respiratory failure the most frequent reason for admission. S. pneumoniae and atypical agents are the most frequent causative organisms in this group. Although overall mortality is relatively low, a number of young patients require ICU admission and have a complicated course.
P881: Corticosteroids in patients with severe community-acquired pneumonia: impact on mortality
C. Garcia Vidal, E. Calbo, C. Ferrer, V. Pascual, S. Quintana, J. Garau (Terrassa, E)
Background: Mortality in patients with severe CAP has been traditionally related to microorganism virulence and to host characteristics. Recently, there has been an increasing interest host-pathogen interaction, and inadequate immunologic response has been shown to be associated with a higher mortality. Immune modulation concomitant to antibiotic therapy has been postulated to improve outcome. The aim of our study was to determine the risk factors for increased mortality in patients with severe CAP and to evaluate the impact of administration of corticosteroids in outcome.
Methods: We reviewed the charts of all hospitalized CAP patients in our centre between October 2001 and December 2003. Severe CAP defined by Pneumonia Severity Index (PSI) categories 4 and 5 were included. Data on demographics, comorbidity measured by Charlson score, bacterial aetiology, the presence of immunosuppression, COPD, ICU admission, antibiotic therapy, use of corticosteroids and mortality were recorded.
Results: Of the 375 severe CAP patients included, 258 and 117, were categories 4 and 5, respectively. 256 patients(69%) were treated with standard antimicrobial therapy and 116 (31%) received also corticosteroids. Mean age (78 vs 77), Charlson score (2.5 vs. 2.6), neoplasm (22% vs. 21%), HIV (0.7% vs. 0.8%), chronic liver disease (9% vs.7%), diabetes mellitus (19% vs.22%), ICU admission (4% vs. 4%), monotherapy (63% vs. 66%), and aetiology (S. pneumoniae 34% vs. 36%; L. pneumophila 3% vs. 2%; others 8% vs. 11%; unknown 54% vs. 51%) were similar. Patients receiving corticotherapy had been exposed to another immunosuppressive treatment more frequently (6% vs. 12%; p = 0.04), COPD was commoner (20% vs. 66%; p < 0.001) and mortality was higher (5% vs. 11%; p = 0.03) than in the group not treated with corticosteroids. In multivariate analysis, severity of disease (OR 3.1; IC95% 1.3–7.1; p = 0.07) and the use of corticosteroids (OR 3.3; IC 95%, 1.3–8.0;p = 0.009) were found to be related to mortality.
Conclusions: In our experience corticosteroid treatment in patients with severe CAP appears to be associated with higher mortality.
P882: Use of levofloxacin in community-acquired pneumonia
J. Olalla, I. Escot, J.J. García-Alegría (Marbella, E)
Introduction and objectives: Community Acquired Pneumonia (CAP) is a prevalent and important disease, with an important consume of resources at Hospitals. Our aim is to study the profile of income patients with CAP diagnosis, the year of introduction of levofloxacin in our centre and compare the length of stay in order to different antibiotics treatments, adjusting the results by Fine's scale.
Methods: In our hospital (a second level hospital in Marbella, Spain) all the diagnosis at discharge are codified and included in the hospital database, so, all the diagnosis of CAP between September 2001 and March 2002 were collected, and clinical reports were examined. Demographic data were registered, so were all the parameters affecting Fine classification, antibiotic treatment, intensive care unit (ICU) incomes, deaths and length of stay.
Results: 129 cases of CAP were found (86 males, 43 females), with a mean age of 67 years (ys)-CI 95%: 64–70), no difference between gender. 4 patients (pts) were living in a residence. 11 pts (8.5%) had a previous diagnosis of Heart Failure -HF-(mean of age 78 vs 66, p < 0.005) and other 11 pts had Cerebrovascular disease -CVD- (mean of age 80.7 vs 66, p < 0.01), 12 pts had Chronic hepatopathy, 15 –11.5%- any form of cancer, 23–17.8%- pts Chronic renal failure (mean of age 74 vs 66, p = 0.049), 41 pts (32%) Chronic Obstructive Pulmonary Disease (COPD). 3 pts were admitted at ICU and 3 deaths were registered. Blood cultures were collected in 30% of cases, culture of sputum in 21%, Legionella antigen in urine in 13.2%. In according with Fine's classification the patients were stratified in group I (10.9%), II (16.3%), III (22.5%), IV (27.9%) and V (22.5%). In 40% cases corresponding to Fine I and II levofloxacin was used alone, vs 19% in Fine III, IV and V (p=0.021). When length of stay was analysed in patients Fine I and II, the use of levofloxacin was associated with a non significant reduction (MEAN + SE: 5.86 + 2.7 days vs 7.67 + 4.9 days), in people on groups III, IV and V use of levofloxacin do not showed any reduction of length of stay (6.67 + 5.06 days in people using levofloxacin vs 6.11 + 4.5 days). No readmissions in relationship with recurrent CAP was registered.
Conclusions: In our experience, use of levofloxacin is associated with less severe CAP, in which a non significant reduction in length of stay is observed.
P883: Telithromycin versus other first-line single-agent antibiotics in the treatment of community-acquired pneumonia: a randomised superiority trial
Y. Mouton, V. Thamlikitkul, R.B. Nieman, C. Janus (Tourcoing, F; Bangkok, TH; Bridgewater, USA; Paris, F)
Objectives: Macrolides and beta-lactams are commonly recommended for the treatment of outpatients with community-acquired pneumonia (CAP). The aim of this study was to demonstrate the superiority of the ketolide telithromycin (TEL) to other first-line, oral, single-agent antibiotics (comparators, COMP) in achieving clinical cure in outpatients with mild to moderate CAP in geographical areas of high pneumococcal resistance (erythromycin resistance rate ≥ 30%).
Methods: Patients with clinical and radiological evidence of CAP were randomised centrally to receive either TEL 800 mg once daily for 7–10 days or COMP (chosen by the investigator in accordance with local treatment guidelines/practices). Efficacy was assessed post-therapy (Days 17–21). Clinical outcomes in this open-label trial were validated by three independent experts who were fully blinded to treatment assigned.
Results: Of the 505 patients enrolled, 482 were included in the modified intent to treat (mITT) and 438 in the per protocol (PP) efficacy analyses. In the COMP group, 39% of patients had received macrolides, 44% beta-lactams and 17% fluoroquinolones. Resistance to penicillin and erythromycin among Streptococcus pneumoniae isolates was 28% and 31%, respectively. Clinical cure rates in the TEL group were significantly higher than those in the COMP group (as shown in the following table). TEL and COMP were similarly well tolerated.
| Post-therapy clinical cure rates, % (n/N) |
||||
|---|---|---|---|---|
| Population | TEL | COMP | Difference [95% Cl] | p-value |
| mITT (investigator's analysis) | 86.0% (208/242) | 78.8% (189/240) | [0.004, 0.140] | 0.04 |
| mITT (blinded experts' analysis))a | 92.1% (223/242) | 85.8% (206/240) | [0.008, 0.119] | 0.03 |
| PP (investigator's analysis) | 87.2% (191/219) | 79.9% (175/219) | [0.004, 0.142] | 0.05 |
| PP (blinded experts' analysis)a | 94.1% (206/219) | 87.7% (192/219) | [0.010, 0.118] | 0.03 |
Clinical failure = subsequent antibiotic for lower respiratory tract infection or CAP-related fever post-therapy.
Conclusions: In this outpatient CAP study, post-therapy clinical cure rates achieved with TEL were shown to be statistically superior to those achieved with other usual care first-line antibiotics – in both the mITT and PP populations, and according to evaluations by both the investigators and blinded experts.
P884: Changing epidemiology, clinical features, and outcome of acute community-acquired pneumonia among adults in India
D.D. Tariang, A. Ajaykumar, K.N. Brahmadattan, M.K. Lalitha, N. Paul, A. Zachariah, O.C. Abraham, J.-H. Song, D. Mathai (Vellore, IND; Seoul, KOR)
Background: Acute CAP is the third leading cause of mortality in India. Two prospective studies from our centre identified common causes of CAP in India to be Mycoplasma pneumoniae [MP] and Legionella pneumophila [LP] by serology in 11% each, and SPN in 10% by culture of respiratory secretions/blood/pleural fluid among 125 patients [pts] in the year [y] 1994; and Chlamydia pneumoniae [CP] in 6.5% among 80 pts in y 1998.
Methods: In a 14-month prospective study ending June 2003, 100 consecutive adults hospitalized with CAP were studied for epidemiology and mortality, and compared with data from previous studies.
Results: Among 100 pts [age 15–84 yrs], 21 were elderly [age > 65 yrs]. There were 63 males. Risk factors included: bronchopulmonary diseases (34 pts), cardiovascular (15), liver and renal (9 each), non pulmonary neoplasms (4), and cerebrovascular accidents (2). Cultures in 55 yielded: SPN (13) Klebsiella spp [KP] (12); PSA (9); Haemophilus influenzae [HI] and Staphylococcus aureus [SA] (5 each); and others (11). CP was detected serologically in 24% and LP urinary antigen was negative in all. SPN isolates were uniformly susceptible to PCN [table 1]. Mortality was 15%. Patients infected with PSA had the highest mortality (44.4%) > HI (40%) > KP (25%) and CP (12.5%). None infected with SPN or SA died. Pneumonia Outcome Research Team [PORT] risk classes I and II had low mortality (3.2%) compared to III (18.8%), IV (22.2%), and V (63.6%). Factors significantly associated with mortality included: renal failure [creatinine >1.4 mg/dL] (OR 8.3, 95% CI 1.5–44.4); tachypnea [rate >30/mt] (OR 5.6, 95% CI 1.5–21.1); PSA associated pneumonia (OR 5.8, 95% CI 1.1–30.9). Mortality in 1994 and 1998 was 3/125 and 5/80 respectively. Initial treatment was with PCN in 28 and flouroquinolones [FQR] in two.
Table 1.
Susceptibility of SPN Isolates to commonly used antibodies for CAP
| Antibiotic panel | % Susceptibility | Minimum Inhibitory Concentration (μ/mL) |
|---|---|---|
| Penicillin | 100 | <0.03 |
| Amoxicillin/Clavulanaie | 100 | <0.06/0.03 |
| Cefuroxime | 100 | <0.06 |
| *** | 100 | <0.12 |
| Erythromycin | 62.5 | >32 |
| Azithromcin | 62.5 | >32 |
| Clindamycin | 62.5 | >32 |
| Levofloxacin | 100 | 1 |
| Ga**floxxacin | 100 | 0.5 |
| Moxifloxacin | 100 | 0.12 |
Conclusion: Although SPN is the most common isolate, the rising numbers of gram negative organisms (38%) and atypical pathogens associated with increasing mortality stress the need for review of initial antibiotic choice for adults with higher PORT classes. In view of enduring susceptibility of SPN to PCN and minimization of resistance with narrow spectrum activity, this should be the drug of choice for SPN in India. FQR that has a wide coverage against most respiratory pathogens including atypicals, can be considered as an initial choice in both hospitalized and ambulatory setting. Continued surveillance of respiratory pathogens is needed.
P885: Fluoroquinolones in the treatment of community and hospital-acquired Legionella pneumonia
L. Mateu, M.L. Pedro-Botet, N. Sopena, A. Garcia Cruz, G. Tolchinsky, C. Rey-Joly, S. Ragull, M. Sabrià, D. Garcia Pares (Badalona, E)
Background: Fluoroquinolones (FQ) are highly active against Legionella and have been shown to be efficacious in animal models and clinical studies of patients with community and hospital-acquired Legionella pneumonia (CALP and HALP).
Objectives: To evaluate the efficacy of FQ in the treatment of CALP and HALP requiring hospitalization.
Methods: Observational non comparative study of intravenous followed by oral levofloxacin (L) or ofloxacin (O) for the treatment of patients with CALP and HALP diagnosed from 1995 to 2004 by Legionella pneumophila sg 1 urinary antigen test (UAT) and/or isolation of Legionella spp. in respiratory samples. Patients who previously received appropriate antibiotic therapy other than FQ were excluded, except in cases with antibiotic failure.
Results: 63 patients were identified (42 patients with CALP and 21 with HALP). 62 were treated with levofloxacin and 1 with ofloxacin. All had a positive UAT and 2 had a positive sputum culture. 52 (82.59%) were males with a mean age of 59.3 yr (19–93); 30 (47.6%) were smokers, 13 (20.6%) alcoholics; 41 (65.1%) had underlying diseases with neoplasms (14), chronic lung disease (13), diabetes (12), chronic heart failure (8), morbid obesity (8) and HIV infection (6), being the most prevalent; 9 (14.3%) were on immunosuppressors. Aspiration risk was present in 5 patients (7.9%). 3 patients (4.8%) required ICU care. Clinical manifestations included fever in 56 (88.99%), cough in 41 (65.1%), dyspnea in 24 (38.1%), gastrointestinal manifestations in 18 (28.6%) and neurological disorders in 24 (38.1%). Hyponatremia (Na <130/mm3) was present in 10 (15.9%), CK increase in 9 (14.3%), AST increase in 19 (30.2%) and pO2 <60 mm Hg in 18 (28.6%). Radiological infiltrate was unilobar in 52 (82.5%), with lower lobes (31) being the most prevalent. The mean time to apyrexia was 51.9 hours (range 12–240), and 31 (49.2%) presented complications, with respiratory failure (26) being the most frequent. Mortality was 6.3%. No patient developed severe adverse events.
Conclusion: Fluoroquinolones are safe and efficacious for the treatment of patients with moderate to severe Legionella pneumonia of community and hospital origin.
P886: Single-dose azithromycin microspheres versus 7 days of levofloxacin for the treatment of mild to moderate community-acquired pneumonia in adults
J. D'Ignazio, M.A. Camere, D.E. Lewis, D. Jorgensen (Montreal, CAN; Lima, PE; Groton, New London, USA)
Objective: Community-acquired pneumonia (CAP) is a major cause of morbidity and mortality worldwide. Inability or failure to comply with standard antibiotic regimens, which may last up to 10 days, may result in patients receiving suboptimal antibiotic treatment. Treatment with a single-dose antibiotic regimen maximizes compliance with prescribed therapy. A novel microsphere formulation of azithromycin makes it possible to administer more drug in a single dose while maintaining tolerability. The objective of this study was to test the hypothesis that a single 2.0 g oral dose of azithromycin microspheres was as effective as a 7-day regimen of oral levofloxacin 500 mg/day when used to treat adult patients with mild to moderate CAP (Fine classes I, II, III).
Methods: This was a phase III, multinational, multicentre, randomized, double-blind, double-dummy trial. The primary endpoint was the clinical response (cure or failure) in the Clinical Per Protocol (CPP) population at Test Of Cure (TOC) (Day 14–21).
Results: Of 427 patients randomized, 363 (85.8%) were included in the CPP population (azithromycin microspheres, n = 174; levofloxacin, n = 189). Clinical cure was achieved in 89.7% of azithromycin-treated patients and 93.7% of levofloxacin recipients (95% CI −9.7, 1.7). Clinical response was maintained at Long-Term Follow Up (Day 28–35): no azithromycin microspheres patients and only one levofloxacin patient (0.6%) relapsed. Clinical cure rates were comparable between both treatment groups for subjects with Haemophilus influenzae (including beta-lactamase positive and negative isolates), Moraxella catarrhalis, Streptococcus pneumoniae, and Chlamydia pneumoniae isolates. Clinical cure rates for subjects with Mycoplasma pneumoniae were lower in the azithromycin-microspheres group 71.4% (5/7) compared with the levofloxacin group 100% (18/18); however, the number of isolates in the azithromycin group was too small for meaningful analysis of results. Most treatment-related adverse events were GI in nature, with diarrhoea more common in the azithromycin-microspheres group (12.3% vs. 4.7%). In the majority (85%) of patients receiving azithromycin microspheres, diarrhoea was limited to study Day 1 or 2. No patients discontinued treatment due to treatment-related adverse events.
Conclusions: A single 2.0 g dose of azithromycin microspheres was as effective as a 7-day course of levofloxacin when used to treat adult outpatients with mild to moderate CAP.
P887: Preferred first line antibiotics in adult CAP admitted to hospital in Spain
A.M. Martín-Sánchez, M. De-la-Rosa, R. Landínez, R. Dal-Ré, J. Garau on behalf of the NACER Group
Objectives: Many guidelines have been issued for the treatment of CAP. We wanted to assess how frequently the national guidelines for treatment of CAP were followed in 10 Spanish acute care hospitals in patients admitted with CAP.
Methods: Retrospective review of the charts of patients admitted to the hospital with the diagnosis of CAP over a 1-year period (1Nov 01 to 31Oct 01) in 10 geographically scattered hospitals in Spain. Data were available from 3233 patients.
Results: Amoxicillin/clavulanate was the most common antibiotic choice (79.5% was given as monotherapy and 20.4% in association with clarithromycin). Levofloxacin (93.1% given only as monotherapy) follows closely. They were followed by third generation cephalosporins (ceftriaxone and cefotaxime) but up to 60% of them were given in association with clarithromycin. Clarithromycin was used mainly as a complement to both amoxicillin/clavulanate and cephalosporins since only 8.6% of its 25.8% was given as monotherapy. Other antibiotics were very uncommonly prescribed (cefepime 1.9%, and ciprofloxacin 1.4%).

Conclusions: 1) Monotherapy with levofloxacin, followed by amoxicillin/clavulanic acid were the most common first line antibiotic choices in these 10 Spanish hospitals. However, amoxicillin/clav alone or in combination with clarithromycin was the most common antibiotic prescribed. 2) Monotherapy with clarithromycin was relatively uncommon (2.2%). 3) These choices reflect quite well the recommendations of the different national guidelines issued in our country in an environment of high prevalence of resistance to penicillin and to macrolides in S. pneumoniae in Spain and the concomitant coverage of Legionella and other atypical pathogens.
P888: The microbiology of ABECB - potential predictive value of clinical criteria
J. Kahn (Raritan, USA)
Objectives: To explore the relationship between specific pulmonary disease severity criteria and the microbiology of acute bacterial exacerbations of chronic bronchitis (ABECB).
Methods: This was a double-blind, randomized clinical trial evaluating levofloxacin 750 mg qd for 3-5 days in ABECB. All potential subjects had to meet the ATS definition of chronic bronchitis but only those patients with Anthonisen type 1 or 2 exacerbations (N = 763) were enrolled. Stratification by disease severity was determined using parameters suggested by Grossman: FEV1 % of predicted value, defined co-morbidities, and number of exacerbations during the previous 12 months. Because different spectra of etiologic organisms were expected on the basis of the stratification, different comparator agents were used for uncomplicated patients (azithromycin for five days) and those considered complicated (amoxicillin/clavulanate for ten days).
Results: Initial microbiology from all intent-to-treat patients revealed notable differences between the two strata. Among isolates from uncomplicated cases, 55% were the ‘traditional’ triad of S. pneumoniae, H. influenzae, and M. catarrhalis. Inclusion of H. parainfluenzae raises this figure to 79%. In the complicated arm the figures were 48% and 68%, respectively. Gram-negative bacilli, primarily Enterobacteriaceae spp. and several Pseudomonads, represented 15% of the uncomplicated and 23% of the complicated isolates. Microbiological eradication rates and the percentage of organism persisting after therapy from the uncomplicated stratum were compatible with the unexpectedly large number of macrolide-resistant organisms isolated. In the complicated arm, both levofloxacin and amoxicillin/clavulanate had lower, but comparable, eradication and persistence rates. Clinical efficacy in microbiologcally-evaluable patients was consistent with these figures.
| Microbiological Eradication Rate (%) | Persistent Organisms (%) | |
|---|---|---|
| UNCOMPLICATED | ||
| Azithromycin | 82.8 | 17.2 |
| Levofloxacin | 93.8 | 6.3 |
| COMPLICATED | ||
| Amoxicillin/clavulanate | 79.8 | 18.0 |
| Levofloxacin | 81.4 | 18.6 |
Conclusion: While there was clearly overlap among the flora isolated from the two strata defined by application of the Grossman criteria, there was separation of the populations. This predictive approach seems to be of value in identifying the optimal antimicrobial regimen, especially for uncomplicated exacerbations. Further work to define and validate predictive clinical parameters may help optimize the choice and duration of antimicrobial agents for ABECB.
P889: Efficacy and safety of pharmacokinetically enhanced amoxicillin/clavulanate 2000/125 mg (PKE AMX/CA) in patients with community-acquired pneumonia, including cases caused by penicillin-resistant S. pneumoniae
K. Bhatt, V. Kalia, E. Berkowitz, M. Twynholm, B. Abraham-van Parijs, R. Hodge (Collegeville, USA; Greenford, Harlow, UK)
Objectives: To evaluate the efficacy and safety of PKE AMX/CA against CAP, a common, costly respiratory illness, particularly cases caused by Streptococcus pneumoniae, including penicillin-resistant (PRSP, penicillin MICs ≥2 mg/L) strains.
Methods: An open-label, non-comparative, multicentre study. Patients with a diagnosis of CAP received oral PKE AMX/CA, 2x 1000/62.5 mg tablets twice daily, for 7 days. Patients were required to provide a sputum sample or, if clinically indicated, an invasive respiratory sample for bacteriological evaluation. Positive pneumococcal urine antigen test and/or the presence of Gram+ diplococci by direct examination of a sample smear was added to inclusion criteria via protocol amendment. Patients were to attend clinic at screening (Day 0), on therapy (Day 3–5), end of therapy (EOT, Day 9–11) and follow-up (FU, Day 28–35).
Results: A total of 1903 patients were enrolled, 1888 of whom (including 984 post-protocol amendment) received study medication and had verifiable efficacy results (intent-to-treat [ITT] population). Of these, 665 had ≥1 typical pathogen identified at screening (bacteriology ITT population). The majority of patients (58.7%) were male and the mean age was 46.5 years. Bacteriological success (eradication or presumed eradication of screening pathogen) in the bacteriology ITT population at FU (primary efficacy endpoint) was 79.7% (530/665; 95% CI 76.4, 82.7) and at EOT was 87.4% (581/665; 95% CI 84.5, 89.7). Bacteriological success at FU against S. pneumoniae was 84.0% (331/394) in the bacteriology ITT population, including 81.4% (35/43) of patients with PRSP, and against Haemophilus influenzae was 79.0% (128/162). Clinical success (resolution of signs/symptoms of CAP such that no further antibacterial therapy was needed) and radiological success (improvement/resolution of radiological signs of CAP) were achieved in >77% of patients at FU and >80% of patients at EOT. In the safety population (N = 1900), diarrhoea was the most frequently reported adverse event (AE), occurring in 14.3% of patients. Headache (4.6%, 87/1900) and nausea (3.3%, 62/1900) were the only other AEs to occur in ≥3% of patients. The majority of AEs were mild to moderate in severity. Only 4.9% (93/1900) of patients in the ITT population withdrew from the study due to AEs.
Conclusions: PKE AMX/CA was effective in treating CAP, including cases caused by PRSP, and was well tolerated, with few patients withdrawing from the study due to AEs.
P890: Comparison of cefepime and ceftazidime in treatment of ventilator-associated pneumonia in severe trauma patients
D. Protsenko, S. Yakovlev, B. Gelfand, A. Yaroshetskiy, Y. Romanovsky (Moscow, RUS)
Objectives: Nosocomial pneumonia is the second most common nosocomial infection and, along with primary bacteraemia, the leading cause of death from infection acquired in the hospital. Despite the frequency of ventilator-associated pneumonia (VAP) and the threat it poses to patient survival, consensus on an appropriate antibiotic treatment of VAP has yet to be established. The uncertainty is compounded by a lack of well-controlled comparisons of specific treatment regimens and their impact on relevant outcomes, such as morbidity, mortality, and cost. The comparable analysis of clinical and microbiological efficacy of cefepime and a combination ceftazidime and amikacin in the treatment of VAP in severe trauma patients was the aim of present study.
Methods: This prospective, randomized study was approved by the institutional review board for human research. Thirty adult patients who admitted in ICU of an 1850-bed emergency municipal hospital with severe trauma complicated with VAP were included. The CPIS was used for diagnostics of VAP. A combination of ceftazidime (2 g TID, IV) and amikacin (1 g once daily, IV) was used as initial empiric therapy of VAP in 17 patients and monotherapy with cefepime (2 g BID, IV) – in 13 patients. These regimes of empiric therapy have been chosen according our local microbiological monitoring and P. aeruginosa was the prevalent pathogen of VAP. The cost-effectiveness analysis was performed to compare both costs and outcomes of competing regimes.
Results: There was no difference between groups in patients’ mean age, average time of mechanical ventilation before onset of VAP and CPIS. Mean APACHE II score was 23.1 in the group of combination therapy and 24.0 in the group of monotherapy. The positive clinical outcome was registered in 92.3% patients on cefepime and 88.2% patients on ceftazidime plus amikacin. The rate of eradication was 53.8 and 58.8% respectively. The duration of effective treatment with cefepime was from 7 to 12 days (mean 8.5 days), with combination therapy – from 7 to 18 days (mean 9.1 days). The mean cost of VAP treatment with cefepime was 452.8 Euro in comparison with 585.4 Euro when the empiric therapy was initiated with ceftazidime and amikacin.
Conclusions: Cefepime in a monotherapy regimen has the same clinical and bacteriological efficacy in comparison with a combination of ceftazidime and amikacin in VAP patients with severe trauma but the use of cefepime results in lower costs.
P891: Influence of antibacterial protocol in multiple trauma patients on incidence and mortality of VAP
D. Protsenko, A. Yaroshetskiy, S. Yakovlev, B. Gelfand (Moscow, RUS)
Objectives: The aim of present study was the evaluation of antibacterial protocol in multiple trauma patients on incidence and mortality of VAP.
Methods: A comparable analysis of incidence, attributive mortality (chi-square test) and pathogens of VAP in multiple trauma patients was performed during two periods: 2001 (before introduction of protocol) and 2003 (after introduction of protocol) years. The developed protocol included: 1. Abandoning of antibiotic prophylaxis of VAP; 2. Intrusion criteria of early diagnostics of VAP; 3. Exclusion of 1st, 2nd and 3rd generation cephalosporines, aminoglycosides and fluoroquinolones as empiric therapy of VAP; 4. Cefepime (APACHE II <20) or carbapenems (APACHE II >20) were used as initial empiric therapy of VAP; 5. Efficacy of antibiotic treatment was evaluated within 48 hours; 6. Carbapenems and/or vancomycin was added if initial therapy was inefficient. In the case of suspected diagnosis of VAP microbiological analysis of bronco-alveolar lavage fluid (BAL) was performed.
Results: We analysed all 399 patients admitted to 12-bed ICU of emergency hospital (220 pts in 2001 and 179 pts in 2003). The incidence of VAP was 10% in 2001 (22/220) and 14% in 2003 (25/179), difference was not significant. Attributive mortality due to VAP was 63% (14/22) in 2001 and 24% (6/25) in 2003, p < 0.01. In 2003 comparison with 2001 the consumption of the following antibiotics was increased (DDD): cefepime – from 40 to 663, imipenem – from 8 to 86, meropenem – from 8 to 216, vancomycin – from 15 to 279. A widespread use of broad spectrum antibiotics shifted the structure of nosocomial pathogens. We observed decrease of MRSA rate and significant increase (more than 10 times) in rate of Klebsiella pneumoniae (from 0.6 to 18.1%, most of strains were resistant to 3rd generation cephalosporines) and in rate of Acinetobacter baumanii (from 1.2 to 12.3%, most of strains were resistant to ceftazidime).
Conclusions: Introduction of strict antibacterial protocol in patients with multiple trauma and VAP results in significant decrease of attributive mortality without any change in incidence of VAP.
P892: Antimicrobial prophylaxis in cardiac surgery and postoperative pneumonia rate
E. Bachinskaya, N.V. Beloborodova, S. Kuznetcova (Moscow, RUS)
Objective: The purpose of this study was to assess the postoperative pneumonia rate according to antimicrobial prophylaxis regimens in patients after cardiac surgery with cardiopulmonary bypass.
Patients and methods: Cardiac surgery patients were included (n = 86) in the retrospective study. We observed 44 patients with postoperative pneumonia (pneumonia group) and 42 patients without infectious complications in postoperative period. The groups were compared by age, sex, volume of transaction, severity of disease. In a studied period is from 2001 to 2003 two main regimens of antimicrobial prophylaxis were used: ceftriaxone 1–2 g IV once before operation or cefuroxime 1.5 g IV before operation and additional dosage 0.75 mg in 2–3 hours after surgery beginning; then prophylaxis were conducted after operation during 48–72 hours. Data were compared by Fisher exact; we determined about significantly differences between groups when p < 0.05.
Results: Preoperative prophylaxis by cefrtiaxone was administered more often in pneumonia group than in patients without infection complications (56.3% vs. 33.3%, NS). Ceftriaxone was used significantly more often in comparison to cefuroxime in subgroup of patients with cardiopulmonary bypass less than 180 min who developed postoperative pneumonia (63.2% vs 30%, p < 0.05). During cardiopulmonary bypass longer than 180 min we did not reveal difference between antimicrobial prophylaxis regimens.
Conclusion: Cefuroxime is more preferable than ceftriaxone for antimicrobial prophylaxis of postoperative pneumonia in patients after cardiac surgery with cardiopulmonary bypass less than 180 min duration.
P893: Closed versus open tracheal suction system to prevent ventilator-associated pneumonia
M. Lecuona, L. Lorente, M. Cuervo, M.A. Miguel, I. Montesinos, B. Castro, S. Campos, A. Sierra (La Laguna, E)
Objective: The aim of this study was to analyze the incidence of ventilator-associated pneumonia (VAP) using a closed tracheal suction system (CTSS) versus an open system (OTSS).
Methods: Prospective and randomized study, between October 1, 2002 and December 31, 2003 in a 24-bed medical-surgical Intensive Care Unit of a 650-bed tertiary hospital. Patients requiring mechanical ventilation during more than 24 hours were included in the study, and were randomized in two groups: one group was suctioned with CTSS and another group with OTSS. Throat swabs were taken at the moment of admission and twice a week until discharge, to classify pneumonia in endogenous and exogenous.
Results: A total of 443 patients (210 with CTSS and 233 with OTSS) were included. There were not significant differences between both groups of patients in age, sex, diagnosis groups, mortality, number of aspirations per day and APACHE-II. No significant differences were found in the percentage of patients who developed VAP (20.47% vs. 18.02%) neither in the number of VAP per 1000 mechanical ventilation-days (17.59 vs. 15.84). There were also no differences in the VAP incidence by MV duration. At the same time we did not find any differences in the incidence of exogenous VAP. Likewise, there were also no differences in the microorganisms responsible for pneumonia. Patient cost per day for the closed suction was more expensive than the open suction system (11.11 ± 2.25$ vs. 2.50 ± 1.12$, p < 0.001).
Pharmacokinetics/pharmacodynamics of antibacterial drugs
P894: Pharmacokinetic/pharmacodynamic model for the tolerability of tigecycline in healthy volunteers
J. Passarell, A. Meagher, K. Liolios, B. Cirincione, T. Grasela, T. Babinchak, E.J. Ellis-Grosse (Buffalo, Collegeville, USA)
Objectives: Tigecycline (T), a first-in-class glycylcycline, is an antimicrobial agent with demonstrated in vitro activity against susceptible & multiple-drug resistant gram-positive & -negative bacteria. Similar to tetracyclines, nausea (N) & vomiting (V) are frequently reported adverse events. Exposure-response relationships & subject (subj) covariates predictive of the first occurrence of N&V in healthy volunteers were evaluated.
Methods: Subj with PK data from 3 single-dose (12.5, 25, 50, 75, 100, 200, 300 mg) Phase 1 studies were pooled for analysis. N&V (definitely, possibly, or probably related to T) reported from the start of infusion until 24 hrs post dose were included. Subj administered ondansetron or with severe/end-stage renal disease were excluded. Individual T exposure measures [AUC 0–infinity (AUC) and Cmax] were obtained from previously conducted noncompartmental analyses. Covariates included age, weight, gender, and geographic location. Logistic regression & Kaplan–Meier methods were used to evaluate the time to first occurrence of N&V.
Results: The dataset included 136 subj. Mean (SD) age & weight were 38 (20) years and 74 (12) kg. Approximately 87% were Caucasian, 84% were male, 38% were enrolled in USA & 62% in Europe. Single N occurrences were reported in 51 (38%); V in 25 (18%) subj. 2 N or V events were reported in 4 subj. N(V) was reported in 12% (4%) of placebo subj, 17% (0%) on T 25 mg, & 33% (0%) on T 50 mg. Females had a higher occurrence of N&V (45% & 19%) vs males (36% & 14%). France & USA had similar N rates (39% vs 35%); France had a much higher V rate (24% vs 10%). Most N (V) events occurred ≤4 hrs (≤6 hrs) of T infusion for all doses. For doses ≤100 mg, median duration of N&V was <1 hr & increased dramatically for 200 & 300 mg dose groups (<3 hrs). Most N (V) occurrences were mild [49% (20%)] & 27% (44%) were moderate. 111 subj had PK. Final statistical model concluded AUC & Cmax as significant predictors of N (p ≤ 0.0001, 0.0022) & V (p ≤ 0.0001, 0.0006). Increased exposures resulted in increased events. At the median AUC (Cmax) of 2599 ng × hr/mL (392 ng/mL) for the 50 mg dose group, N probability was 0.26 (0.29); V probability was 0.08 (0.11).

Conclusion: T exposure (AUC > Cmax) was a significant predictor of the probability of N&V events in Phase 1 subj. Model predicted rates of N&V were comparable with those seen with the tetracycline class of antibiotics, with tolerable rates predicted at the targeted T 50 mg q12 h dose.
P895: Dalbavancin penetration into skin supports once weekly dosing
J.A. Dowell, M. Buckwalter, E. Seltzer, M. Stogniew, T. Henkel (King of Prussia, USA)
Objectives: Dalbavancin is a novel, second generation lipoglycopeptide that has been shown to have clinical efficacy as a once-weekly treatment for complicated skin and skin structure infections (cSSSI). The dosage used in clinical studies is 1000 mg Day 1/500 mg Day 8. In vitro studies have determined dalbavancin MIC90s of less than or equal to 0.06 mg/L for target bacteria, principally staphylococci and streptococci, including isolates resistant to other antibiotics. The plasma protein binding of dalbavancin is 93%. As skin infections occur in extravascular space, antibiotic concentrations are assessed in blister fluid as a measure of skin penetration and to obtain pharmacokinetic observations that may correlate with efficacy.
Methods: A Phase I, open label, single-dose study was conducted in 9 healthy subjects. Subjects were administered a 1000 mg IV dose of dalbavancin. Blisters were induced by applying 0.25% cantharidin ointment to the skin. Blister fluid was collected prior to dose, and at 12 hours, Day 3, Day 5 and Day 7. Blood samples were collected throughout the study. Blister fluid and plasma were assayed for dalbavancin using a validated LC-MS/MS method and pharmacokinetic parameters were determined. Area under the concentration-time curve (AUC) was determined for blister fluid (AUCbf) and plasma (AUCp) through the first week. The degree of penetration into skin was determined by AUCbf/AUCp (%).
Results: Dalbavancin was well tolerated with no serious adverse events; most adverse events were mild and self-limited. Maximum observed dalbavancin blister fluid concentrations were achieved by the first collection (12 hours) and concentrations were maintained above 30.3 (±4.4) mg/L through Day 7. The mean (SD) AUCbf and AUCp were 6438 ± 1238 and 10806 ± 1926 mg h/L, respectively. Skin penetration was approximately 60%. Dalbavancin blister fluid concentrations were maintained well above MICs throughout the treatment interval, even when considering the possible effects of protein binding.
Conclusions: Blister fluid concentrations are maintained well above MICs of cSSSI target organisms for a week following a single dose of dalbavancin. These data support a once-weekly regimen and are consistent with the efficacy observed in clinical studies.
P896: The safety and pharmacokinetics of dalbavancin in subjects with renal impairment or end-stage renal disease
J.A. Dowell, E. Seltzer, D. Krause, T. Henkel (King of Prussia, USA)
Objectives: Dalbavancin is a novel, second generation lipoglycopeptide antibiotic in late stage clinical development for complicated skin and skin structure infections (cSSSI). The weekly dosage used in clinical studies is 1000 mg Day 1/500 mg Day 8. Since dalbavancin will likely be used in patients with various degrees of renal impairment, it is important to determine the safety and pharmacokinetics in this population, as well as to evaluate if a dosage adjustment is necessary.
Methods: Single intravenous doses of 1000 mg dalbavancin were examined in subjects with mild (CLCR of 50–79 mL/min) and moderate (CLCR of 30–49 mL/min) renal impairment. Doses of 500 mg dalbavancin were studied in subjects with end-stage renal disease (ESRD; dialysis-dependent). Single doses of 500 mg and 1000 mg dalbavancin were studied in subjects with severe renal impairment (CLCR <30 mL/min). Subjects with normal renal function were studied and used as controls. Pharmacokinetic data were analysed using non-compartmental methods; parameters included maximum concentration (Cmax) and area under the plasma concentration time curve (AUC).
Results: A total of 43 subjects received dalbavancin and were included in the pharmacokinetic analysis (6 mild, 6 moderate, 10 severe, 6 ESRD, and 15 normal). Dalbavancin was well tolerated in each of the renal impairment groups. The majority of adverse events were mild or moderate in severity and unrelated to study drug. There were no related serious adverse events. Dalbavancin pharmacokinetics were similar between subjects with mild and moderate renal impairment and subjects with normal renal function. Concentrations in subjects with ESRD were similar to subjects with normal renal function, indicating compensation in renal insufficiency due to regular dialysis (3 times/week). Subjects with severe renal impairment had increased concentrations and exposure. Concentrations were increased by no more than 40% through the first week post dose, but differences continued to increase through the rest of the profile. AUC was increased almost 2-fold.
Conclusion: Dalbavancin was well tolerated in subjects with various degrees of renal impairment. Patients with severe renal impairment (CLCR <30 mL/min) may require a modest dosage adjustment. No dosage adjustment is required for patients undergoing regularly scheduled dialysis.
P897: Effect of haemodialysis on single dose pharmacokinetics of telavancin
K. Duchin, J. Shaw, J. Seroogy, S. Barriere, R. Novack (South San Francisco, New Orleans, USA)
Background: TLV, a novel lipoglycopeptide antibiotic with multiple mechanisms of action, exerts rapid and concentration-dependent bactericidal activity against clinically important gram-positive bacteria, including methicillin-resistant S. aureus. The kidney is the primary route of elimination of TLV in man. Phase 3 studies are ongoing in skin and skin structure infections and hospital acquired pneumonia.
Objective: To compare the single dose PK of TLV in subjects maintained on hemodialysis with an aged and sex-matched group of healthy subjects without renal dysfunction.
Methods: Six hemodialysis subjects (5 males, 1 female) received a single 7.5-mg/kg dose of TLV intravenously over 1 hour approximately 2-4 hours prior to a 4-hour hemodialysis session. Six subjects (5 males, 1 female) with normal renal function (mean creatinine clearance 94 mL/min) also received the same dose of TLV over 1 hour. Blood and dialysate samples were obtained at specified intervals post dose and assayed for TLV with a validated LC/MS/MS assay. PK parameters were determined using non-compartmental methods.
Results: Average values for plasma PK parameters for TLV in both groups of subjects are shown below. The average (range) clearance of TLV via dialysis was 4.6 mL/min (4.0–5.8) and the per cent of dose removed by dialysis was 5.9% (3.0–7.6). Subjects tolerated TLV well.
| Parameter | Normal (n=6) | Hemodialysis (n=6) |
|---|---|---|
| Cmax (μ/mL) | 70.6 ± 11.2 | 52.1 ± 10.1 |
| AUC0-t (μ.hr/mL) | 498 ± 75 | 636 ± 148 |
| AUC0-∞ (μg.hr/mL) | 568 ± 97 | 1147 ± 441 |
| T1/2 (hr) | 8.1 ± 0.7 | 19.7 ± 4.9 |
| CL (mL/hr/kg) | 14 ± 2 | 7 ± 3 |
| MRT (hr) | 10.4 ± 0.9 | 27.8 ± 7.0 |
| Vss (mL/kg) | 139 ± 14 | 189 ± 26 |
Conclusions: Dose reductions of TLV of 50% are recommended in patients maintained on hemodialysis. Supplementation of a TLV dose post dialysis is not needed.
P898: Pharmacokinetics and tissue penetration of telavancin in healthy subjects
K. Duchin, H.K. Sun, J. Shaw, D. Nicolau (South San Francisco, Hartford, USA)
Background: TLV, a novel lipoglycopeptide antibiotic with multiple mechanisms of action, exerts rapid and concentration-dependent bactericidal activity against clinically important gram-positive bacteria, including methicillin-resistant S. aureus. The MIC90 for S. aureus, including MRSA and GISA, from pooled studies is 0.5 μg/mL. Phase 3 studies are ongoing in skin and skin structure infections and hospital acquired pneumonia. Objectives: To determine the steady-state PK profile of TLV in plasma and skin blister fluid in healthy subjects.
Methods: 8 subjects (7 males, 1 female) received three daily doses of TLV (7.5 mg/kg) intravenously over 1 hour. Cantharidin ointment (0.25%) was applied to the forearms to produce 7 blisters/subject beginning 12–14 hours prior to the third dose of TLV. Blood and blister fluid samples were obtained at specified intervals on days 3 and 4 and assayed for TLV with a validated LC/MS/MS assay. PK parameters in both matrices were determined using non-compartmental methods.
| Biological Matrices | Plasma | Skin Blister Fluid |
|---|---|---|
| N | 8 | 8 |
| Cmax (μg/mL) | 848 ± 5.3 | 16.0 ± 2.0 |
| Tmax (hr) | 1.0 ± 0.0 | 9.3 ± 2.4 |
| AUC ss (μg.hr/mL) | 604 ± 83 | 241 ± 33 |
| T1/2 (hr) | 6.26 ± 0.78 | 6.91 ± 0.53 |
| CL (mL/hr/kg) | 11.8 ± 2.1 | 27.5 ± 2.9 |
| Vss (mL/kg) | 98.0 ± 14.8 | ND |
| MRT (hr) | 6.57 ± 0.42 | 10.4 ± 0.6 |
Results: The average values for PK parameters for TLV in plasma and in blister fluid are shown below. Mean (SD) trough values of the ratios of concentrations of TLV in blister fluid to plasma on days 3 and 4 were 0.79 (0.2) and 0.82 (0.2), respectively. Most subjects reported transient mild taste disturbance following administration of TLV.
Conclusions: Penetration of TLV was excellent into skin blister fluid and concentrations throughout the dosing interval exceeded the MIC90 for S. aureus.
P899: Influence of dose and infusion duration on the time above MIC of ceftobiprole in healthy volunteers
A.H. Schmitt-Hoffmann, B. Roos, J. Spickermann, M. Roehrle, R. Pypstra (Basel, CH; Neu-Ulm, D)
Objective: To assess the influence of dose and infusion duration on the plasma concentration-time profiles of ceftobiprole.
Methods: This study compared two different dosing regimens in thirty six healthy volunteers. Nine male and nine female subjects assigned to regimen A received a single 30 minute intravenous constant rate infusion of ceftobiprole medocaril, corresponding to 750 mg of ceftobiprole. A further nine male and nine female subjects, assigned to regimen B, received a single 60-minute intravenous constant rate infusion of ceftobiprole medocaril, corresponding to 500 mg of ceftobiprole. Blood samples were collected immediately before start of infusion and 15 min, 30 min, 1 h, 4 h, 5 h, 6 h, 7 h, 8 h, and 24 h after start of infusion. Plasma concentrations of ceftobiprole were quantified using a validated specific LC-MS/MS assay.
Results: After single intravenous infusions of 750 mg equivalent (eq) ceftobiprole for 30 minutes or 500 mg eq ceftobiprole for 60 minutes, mean Cmax-values at infusion endpoint are 57.9 μg/mL and 34.2 μg/mL, respectively. The corresponding mean AUC0-inf-values are 154 μg h/mL and 116 μg h/mL. Intersubject variability of the parameters AUC and Cmax of ceftobiprole is below 20%. Mean systemic clearance is 4.9 and 4.5 L/h and mean steady-state volume of distribution is 13.7 and 11.0 L for the 750 mg and 500 mg dosing regimen, respectively. After infusion of 500 mg for 60 minutes or 750 mg for 30 minutes, the ‘Time above MIC (target MIC of 4 μg/mL for Methicillin Resistant Staphylococcus aureus) is 6 and 7 hours for the total plasma concentrations and 3.5 and 5.2 hours for the corrected unbound plasma concentrations, respectively. With twice-daily administration of 500 mg for 60 minutes or 750 mg for 30 minutes, the proportion of the dosing interval above the MIC of 4 μg/mL, would be 75% and 87% for the total plasma concentrations and 55% and 65% for the unbound plasma concentrations, respectively.
Conclusions: Ceftobiprole infusions of 500 mg eq for 60 minutes or 750 mg eq for 30 minutes, results in similar time above target concentration of 4 μg/mL well above the minimum efficacy requirement 25–30% required for MRSA.
P900: 2 hour versus 0.5 hour infusion of imipenem in healthy volunteers
S. Jaruratanasirikul (Hat-Yai, Songkhla, TH)
Introduction: The bactericidal activity of beta-lactam antibiotics is determined by the time that concentrations in plasma are above the MIC (T > MIC) for the pathogens during the dosing interval.
Objective: The aim of this study was to demonstrate the T > MIC of imipenem when administered by 2 h infusion compared with 0.5 h infusion.
Methods: The study was a randomized, three-way crossover study with 30 hours wash-out period in 8 healthy volunteers. Each subject received imipenem in three regimens : (i) 0.5 h infusion of 0.5 g every 6 h for 3 doses; (ii) 2 h infusion of 0.5 g every 6 h for 3 doses; (iii) 2 h infusion of 1 g every 6 h for 3 doses.
Results:
| 2 h infusion |
|||
|---|---|---|---|
| %T > MIC | 0.5 h infusion | 0.5g | 1g |
| 16 μg/ml | 21.51 (2.16) | 26.85 (8.49) | 51.55 (5.44)a,b |
| 8 μg/ml | 38.55 (3.51) | 48.04 (3.52)a | 677.3 (4.50)b |
| 4 μg/ml | 57.45 (3.95) | 65.41 (3.33)a | 87.79 (5.63)a,b |
p < 0.05 versus 0.5 h infusion.
p < 0.05 versus 2 h infusion of 0.5 g.
Conclusion: The 2 h infusion of 0.5 or 1 g of imipenem both give greater values for T > MIC than a 0.5 h infusion and that a 2 h infusion may be a useful mode of administration in tropical countries where drug instability may prevent the use of continuous infusion.
P901: Pharmacodynamic characterisation of LMB415 against Haemophilus influenzae in an in vitro hollow-fibre system
A. Meagher, P. Smith, A. Forrest, A. Odundele, P. Ambrose (Buffalo, Albany, USA)
Objectives: LBM415 is a peptide deformylase inhibitor with in vitro activity against those pathogens commonly associated with community-acquired respiratory tract infections. The purpose of these studies was to determine which pharmacokinetic-pharmacodynamic (PK-PD) measure is most strongly associated with drug response and to examine the relationship between drug exposure and response for LMB415 against Haemophilus influenzae (HI).
Methods: Two wild-type HI strains (MIC 2 and 8 mg/L) were studied. The hollow-fiber system (HFS) was inoculated with approximately 10E7–10E8 CFU/mL in log-phase growth. Simulating human pharmacokinetics (t1/2 = 2 hours), bacteria were exposed to escalating free drug LMB415 exposures (AUC ranging from 0 to 200 mg × h/L) using a dose fractionation study design and delivering drug q12 hours, q24 hours, and by continuous infusion (CI). Serial samples were collected to determine bacterial counts (CFU/mL) and drug concentrations. Drug effect was quantified as the log10 ratio (LR) of the 24 hour area under the bacterial growth/kill curves for drug and growth control (LR = log10 AUCdrug/AUCgrowth control).
Results: Overall, the greatest activity (at 6xMIC) was seen with the CI regimen (CI > Q12 >> Q24). Due to the short half-life, dosing q24 hours yielded no net kill compared to baseline. Neither per cent time above MIC, AUC:MIC ratio, nor peak:MIC ratio could co-model the q12 and q24 hour regimens with CI results. Separating these into 2 datasets (q12/24 vs CI), only the AUC:MIC ratio could adequately describe the CI results (Emax LR of (2 at an AUC:MIC ratio ≥50). The q12/24 dataset was reasonably fit by the AUC:MIC ratio and per cent time above MIC (Emax LR of (2 to (3 at an AUC:MIC ratio ≥120 and per cent time above MIC of ≥50–60%, respectively). The peak:MIC ratio was not informative.
Conclusion: For intermittent dosing regimens, per cent time above MIC and the AUC:MIC ratio adequately described drug response. Percent time above MIC and the AUC:MIC ratio associated with maximal decline were ≥50–60% and ≥120, respectively. CI regimens could not be co-modeled with intermittent regimens, suggesting that neither per cent time above MIC nor the AUC:MIC ratio completely described drug effect. Drug effect continued to increase beyond 100% time above MIC. Q12 hour dosing had more effect than q24 hour dosing, and would probably be an effective LBM415 regimen in humans for HI.
| Regimen | Maximum Decline from Baseline at 24 hrs (log10 CFU/mL) | Maximum Decline vs Growth Control at 24 hrs flog10CFU/mL) |
|---|---|---|
| Q12 hours | 1.4–2.0 | 3.0–4.4 |
| Q24 hours | 0.13 | 1.4 |
| Cl at 1×MIC | −1.0–0.6 | 0.9–2.0 |
| Cl at 2×MIC | 1.7–2.3 | 3.1–4.1 |
| Cl at 4×MIC | 2.6–2.7 | 4.1–4.5 |
| Cl at 6×MIC | 3.7–3.8 | 5.1–5.5 |
P902: Pharmacodynamics of antimicrobials for the empiric treatment of nosocomial pneumonia: a report from the OPTAMA program
H.K. Sun, J.L. Kuti, D.P. Nicolau (Hartford, USA)
Objectives: Appropriate empiric antibiotic therapy is vital for maximizing patient outcomes in the treatment of nosocomial pneumonia and is dependent on the drug exposure achieved in a patient and the causative pathogen's MIC. The purpose of this study was to compare the probability of achieving bactericidal exposures for commonly used intravenous antibiotics against the bacteria most commonly implicated in nosocomial pneumonia.
Methods: A 10,000-subject Monte Carlo simulation calculated target attainments for cefepime (FEP), ceftazidime (CAZ), imipenem (IPM), meropenem (MEM), piperacillin/tazobactam (TZP), and ciprofloxacin (CIP) as 30-minute infusions. Bactericidal targets were free drug concentrations above the MIC for 40% of the dosing interval for IPM and MEM, 50% for FEP, CAZ and TZP, and a total AUC/MIC ratio of 125 for CIP. MICs (in rank order) for S. aureus, P. aeruginosa, S. pneumoniae, Klebsiella sp., Enterobacter sp., E. coli, Serratia sp., Acinetobacter sp., P. mirabilis and Citrobacter sp. were taken from the MYSTIC 2003 surveillance study and weighted by the prevalence of each pathogen as the cause of nosocomial pneumonia according to published data. A sensitivity analysis varying pathogen prevalence was applied. Population pharmacokinetic parameters were taken from healthy volunteer studies. MRSA was excluded.
Results: Percent target attainments are listed in Table 1. The sensitivity analysis revealed that when P. aeruginosa incidence was high, target attainments for FEP, CAZ, and TZP decreased, but carbapenem target attainments remained the same regardless of pathogen prevalence.
Table 1.
% Target attainment rates for FEP, CAZ, IMP, MEM, TZP CIP
| Regimens | % Target Attainment |
|---|---|
| FEP 1g q12h | 89.8 |
| FEP 2g q12h | 94.9 |
| CAZ 1g q8h | 68.5 |
| CAZ 2g q8h | 92.8 |
| IPM 1g q8h | 98.4 |
| MEM 1g q8h | 97.8 |
| TZP 4.5g q6h | 92.3 |
| CIP 0.4g q8h | 34.9 |
| CIP 0.4g q12h | 11.3 |
Conclusions: Target attainments were greatest for IPM and MEM, followed by higher doses of FEP, CAZ and TZP. Because these antibiotic regimens provide optimal bactericidal exposure, they would be most suitable for the empiric treatment of nosocomial pneumonia along with an anti-MRSA antibiotic until pathogen identification and susceptibility results are available.
P903: Penetration of ertapenem into different pulmonary compartments of patients undergoing lung surgery
O. Burkhardt, J. Majcher-Peszynska, R.G. Mundkowski, K. Borner, B. Drewelow, T. Welte (Magdeburg, Rostock, Berlin, D)
Objective: Ertapenem, a new carbapenem, is approved for the treatment of community-acquired pneumonia, but its in vivo penetration into lung tissue (LT), epithelial lining fluid (ELF), and alveolar cells (AC) in humans is unknown.
Methods: Fifteen adult patients undergoing thoracotomy for suspected lung cancer were treated with 1 g intravenous ertapenem for perioperative prophylaxis. In all patients BAL was performed 1, 3, and 5 h after the start of ertapenem infusion. From 12 patients normal lung tissue were sampled simultaneously at the time of the extraction of the pulmonary segment, lobe or lung. Blood samples were collected before, and at different time points up to 24 h after medication, and at the time of taking the tissue samples. Samples were analysed by a validated HPLC method.
Results: Mean concentrations of ertapenem in plasma, ELF, and AC were: at 1.0 h: 63.1, 4.06, 0.004 mg/L; at 3.0 h: 39.7, 2.59, 0.003 mg/L; at 5.0 h: 27.2, 2.83, 0.007 mg/L. The mean (range) concentration in normal lung tissue was 7.60 (2.5–19.4) mg/kg of tissue 1.5–4.5 h after infusion. After a single dose ertapenem exhibited in plasma a mean (SD) Cmax of 90.3 (19.8) mg/L at a median Tmax of 0.5 h, a mean (SD) terminal elimination half-life of 6.6 (4.5) h, and an mean (SD) AUC of 591.4 (416.5) mg/L h. No serious adverse events were observed.
Conclusions: Like in other beta-lactam antibiotics penetration of ertapenem into AC was low. However, its concentrations in plasma, ELF and lung tissue exceeded to a large extent of the dosing interval the MIC90 of all important community-acquired respiratory pathogens. These results support the clinical efficacy of ertapenem in the treatment of community-acquired pneumonia.
P904: Pharmacodynamic comparison of intravenous antimicrobials against Pseudomonas aeruginosa in Hungarian hospitals – A report from the OPTAMA Program
E. Ludwig, D. Maglio, M. Konkoly-Thege, J. Kuti, D. Nicolau (Budapest, HUN; Hartford, USA)
Objectives: The treatment of multi-drug resistant Pseudomonas aeruginosa (PSA) infections is a growing problem worldwide. Since the clinical value of antimicrobials depends on local resistant patterns, the PD profiles of five Beta-lactams and ciprofloxacin were evaluated using Monte Carlo simulation against isolates collected in Hungary.
Methods: MICs for 180 nonduplicate PSA collected from 14 hospitals in Hungary were determined by E-test methodology. A 5,000 subject Monte Carlo simulation was performed to calculate the target attainment (TA) of obtaining bactericidal PD exposures for standard dosing regimens of meropenem (MEM), imipenem (IMI), ceftazidime (CTZ), cefepime (PIM), piperacillin/tazobactam (TZP), and ciprofloxacin (CIP). Bactericidal exposures were defined as free drug concentrations above the MIC for 40% of the dosing interval for MEM and IMI, 50% for CTZ, PIM, and TZP, and a total drug area under the curve (AUC) to MIC ratio of 125 for CIP. Pharmacokinetic data were obtained from healthy volunteer studies. A TA greater than 90% was defined as optimal. In the case of poor TA, PD optimized regimens were simulated for select agents by increasing infusion (INF) time, dose and frequency.
Results: No regimen obtained greater than 90% TA. The highest TA achieved with standard dosing regimens was MEM 1 g q8 and 0.5 g q6 h at 78% and 77%, followed by the CTZ 2 g q8 h at 75%, then IMI, TZP, PIM, and lastly CIP. Increasing INF, dose and frequency for MEM, PIM and TZP all increased TA, with the greatest TA acheived by MEM 2 g q8 h as a 3 hour INF at 88%, followed by 1 g q8 h as a 3 hour INF and TZP 4.5 g q6 h as a 4 hour INF.
Conclusions: Given the poor TA predicted with standard dosage regimens against these PSA, it seems prudent to evaluate patient outcomes in this population. When empirically treating suspected PSA infections in Hungary, alternative dosage strategies such as increasing doses, frequencies or prolonging the infusion time for the Beta-lactams along with combination therapy is justified.
P905: Single-dose pharmacokinetics of fosfomycin during continuous venovenous haemofiltration
R. Gattringer, B. Meyer, G. Heinz, C. Guttmann, P. Dittrich, F. Thalhammer (Vienna, Graz, A)
Objective: Fosfomycin (F) is an often employed antibiotic in critically ill patients with severe infections. Continous venovenous haemofiltration (CVVH) is an important supportive extracorporeal renal replacement therapy in treatment of intensive-care patients. This study was designed to find out recommendations of dosing F for patients undergoing CVVH.
Method: Twelve intensive care patients with acute renal failure and suspected or proven infection were included in the study. CVVH was performed using a polyethylene sulfone haemofilter with a membrane surface of 1.2 m2. Mean blood flow rate was 153.33 + 17.23 mL/min and ultrafiltration rate pump rate was adjusted to 25 mL/min. All patients received a single dose of 8 g F into a central venous catheter, different from the venous catheter used for CVVH. Blood samples were drawn from the arterial (input) and venous (output) line of the extracorporeal circuit before and 15, 30, 60, 90, 180, 360, 480 and 720 min after the start of the infusion. Ultrafiltration samples were collected at corresponding times. F in the samples was quantitated by gas chromatography after derivatisation. The area under the concentration time curve (AUC), the elimination half-life, the total clearance and the volume of distribution were estimated. The clearance of hemofiltration was also determined. The sieving coefficient and the total removal of the drug during hemofiltration were calculated.
Results: Peak serum concentrations were 442.78 ± 129.56 mg/L and 338.04 ± 128.19 mg/L at the arterial port and at the venous port, respectively. Trough serum levels were 102.10 ± 36.59 mg/L at the arterial port and 72.88 ± 35.94 mg/L at the venous port after 720 min. The mean arterial and venous elimination half-life was12.11 ± 5.41 and 11.77 ± 6.25 h, respectively. The mean arterial AUC0-12 was 2159.38 ± 636.92 mg * h/L and the arterial AUC0-24 2922,49 ± 795.83 mg * h/L. The mean venous AUC0-12 and AUC0-24 were 1550.23 ± 611.58 mg * h/L and 2135.32 ± 782.16 mg * h/L. The sieving coefficient was 0.71 ± 0.15, respectively. Mean total removal of the drug was 76.79 + 6.25%. The results of calculated clearance were 1.06 ± 0.22 L/h.
Conclusion: In conclusion a regimen of 8 g F every 12 hours should be an appropriate amtimicrobial treatment for patients undergoing CVVH. But because of fast resistance development and lack of postantibiotic effects F should be combined with antimicrobials where synergically activity was already shown.
P906: Telithromycin and azithromycin pharmacodynamics vs. genotypically characterised (mefA and ermB) macrolide-resistant strains of Streptococcus pneumoniae simulating free serum and free epithelial lining fluid concentrations
D.J. Hoban, A. Noreddin, T. Hisanaga, M. DeCorby, N. Laing, A. Wierzbowski, G.G. Zhanel (Winnipeg, CAN)
Objectives: Telithromycin (Teli) is a new ketolide with in vitro activity against macrolide resistant SPN. The purpose of this study was to compare the pharmacodynamics (PD) of Teli and azithromycin (Azi) versus macrolide-resistant SPN simulating free serum (S) and free epithelial lining fluid (ELF) concentrations in an in vitro model.
Methods: Five PCR-positive mefA, one PCR-positive ermB and a control PCR-negative mefA, ermB strain of SPN were studied. A one compartment in vitro pharmacodynamic model was used with starting inocula 1 × 106 CFU/ml. Teli was added to the model simulating a dosage of 800 mg PO OD (S: free drug Cpmax 0.7 μg/ml, t 1/2 10 hr, free AUC ∼4; ELF: free drug Cmax 6 μg/ml, t 1/2 10 hr, free AUC ∼35). Azi was added simulating a dosage of 500/250 mg PO OD (S: free drug Cpmax 0.2 μg/ml, t 1/2 68 hr, free AUC ∼2; ELF: free drug Cmax 1 μg/ml, t 1/2 68 hr, free AUC ∼10). Samples were obtained over 24 hours to assess viable growth and selection of resistance.
Results: Both S and ELF Teli concentrations eradicated (lowered inoculum below level of detection) all PCR-positive mefA, ermB and wild type SPN from the model within 6 hours. No difference in the rate or extent of killing (>3 log10 reduction) occurred between the test and control strains or between S and ELF concentrations. Azi S and ELF concentrations eradicated macrolide-susceptible SPN but did not eradicate macrolide-resistant SPN regardless of resistance phenotype.
Conclusion: Both Teli and Azi eradicated macrolide-susceptible SPN. Teli but not Azi, completely eradicated both mefA and ermB SPN from the model with no regrowth over 24 hour. Teli offers promise for the management of respiratory infections caused by macrolide-resistant SPN.
P907: Postantibiotic sub-MIC and subinhibitory effects of various antibiotics on B. anthracis
A. Athamna, M. Athamna, D.J. Bast, D. Farrell, E. Rubenstein (Kfar Qaraa, IL; Canada, CAN; London, UK; Ramat Gan, IL)
Objective: To determine the Post Antibiotic Effect of Sub Minimal Inhibitory Concentrations (PA-Sub MIC) and Sub
Minimal Inhibitory Concentration effect (SME) of 6 antibacterial agents against two strains of B. anthracis.
Methods: The PA-Sub MIC and SME were determined by exposing the bacteria to antibiotic concentrations 10 times the MIC for 2 h at 37 °C. Following repeated washings and centrifugations to remove the antibiotic, cultures were divided into four tubes. To three tubes, the tested antibiotic was added to make a final concentration of 0.5 MIC, 0.25 MIC and 0.125 MIC to the fourth tube no antibiotic was added. Optical Density was determined before exposure, immediately after washing and then hourly up to 9 h. For the determination of SME, the same procedure was performed except that the organisms were not pre-exposed to any antibiotic. The ODs were converted to CFUs by using a standard curve. The PA-Sub MIC was defined as PA-Sub MIC = Tpa − C, where Tpa is the time for cultures previously exposed to an antibiotic and then reexposed to different sub-MICs to increase 1 log10 above the counts determined immediately after washing and C is the corresponding time for the antibiotic unexposed control. The SME was defined as SME = Ts − C, where Ts is the time for the cultures exposed only to sub-MICs to increase 1 log10 above the counts determined immediately after washing and C is the corresponding time for the unexposed control.
Results: The PAE of ciprofloxacin and moxifloxacin on B.anthracis STi and Sterne strains were 3–4 h. The PA-Sub MIC of ciprofloxacin (0.5 MIC) was 5 h for both strains, while moxifloxacin PA-Sub MIC was >8 h for both strains. Tetracycline PAE was 1–2 h for both strains and the same result was found with the PA-Sub MIC. Linezolid PAE was 1 h while the PA-Sub MIC was 7 h. Penicillin PAE was 1–2 h, the PA-Sub MIC (0.5 MIC) was >8 h. Quinoprestin–Dalfoprestin PAE and PA-Sub MIC were 8 h. The SME of all antibiotics tested was 0 h.
Conclusion: Moxifloxacin, linezolid and penicillin at PA-SubMIC have a prolonged effect, which delayed the re-growth of B.anthracis. Our results suggest that longer dosing intervals may be possible for treatment of anthrax with these antibiotics.
P908: Pharmacodynamic profiling of cefepime in the cerebrospinal fluid of hospitalised patients through the use of population pharmacokinetic modelling and Monte Carlo simulation
T.P. Lodise, D.H. Rhoney, V.H. Tam, D. Parker, P.S. McKinnon, G.L. Drusano (Albany, Detroit, Houston, St. Louis, USA)
Background: Data on the disposition of cefepime in human CSF is limited and the ability of cefepime to achieve adequate T > MIC for 40–100% of the dosing interval (DI) [40–100% T > MIC] in the CSF of hospitalized patients for the range of MICs deemed susceptible by NCCLS has not been characterized.
Methods: Serum and CSF cefepime PK data was obtained from 7 hospitalized patients with pneumonia and external ventricular drains. The concentration-time profiles in serum and CSF were modeled using a three-compartment model with zero-order infusion and first order elimination and transfer. The apparent volume of the central compartment (VC), apparent volume in the CSF (VCSF), intercompartmental transfer rate constants (K12, K21, K13, and K31) and plasma clearance (CL) were identified in a population PK analysis (NPAG) [table 1]. For cefepime 2 g IV Q8 h (0.5 h infusion), a Monte Carlo Simulation of 10,000 subjects (ADAPT II) was performed to estimate the probability of attaining the targets of free cefepime serum concentration (assumed 20% protein binding) and total cefepime CSF concentration 40–100% T > MIC for MICs 0.25–8 mg/L (table 2). CSF/serum median penetration ratio was calculated.
Results:
Cefepime Population on PK Mean (SD) Parameter Estimates obtained by NPAG analysis
| Vc (L) | CL (L/h) | K12 (h−1) | K21 (h−1) | K13 (h−1) | K31 (h−1) | VCSF (L) |
|---|---|---|---|---|---|---|
| 21.1 (13.0) | 6.9 (2.0) | 5.4 (5.9) | 7.0 (5.0) | 3.4 (4.9) | 14.8 (9.4) | 45.1 (32.0) |
Post MAP-Bayesian observed-predicted regression and r2 for serum and CSF were as follows: (serum) observed = 0.984 × predicted + 2.570; r2 = 0.944. (CSF) observed = 0.785 × predicted + 0.868; r2 = 0.821. The penetration of cefepime as measured by median AUCcsf/AUC serum was 7.8% (25th–75th percentiles 2.9–21.4%).
| 2g Q 8 H | T > MIC | 0.25 mg/L | 0.5 mg/L | 1 mg/L | 2 mg/L | 4 mg/L | 8 mg/L |
|---|---|---|---|---|---|---|---|
| (S/CSF) | 0.4 DI | 1.0/0.94 | 1.0/0.88 | 1.0/0.75 | 1.0/0.60 | 1.0/0.41 | 1.0/0.25 |
| (S/CSF) | 0.5 DI | 1.0/0.92 | 1.0/0.85 | 1.0/0.71 | 1.0/0.55 | 0.99/0.37 | 0.99/0.23 |
| (S/CSF) | 0.6 DI | 1.0/0.89 | 1.0/0.81 | 1.0/0.67 | 0.99/0.52 | 0.99/0.34 | 0.91/0.21 |
| (S/CSF) | 0.7 DI | 1.0/0.87 | 1.0/0.78 | 1.0/0.63 | 0.99/0.48 | 0.97/0.32 | 0.93/0.19 |
| (S/CSF) | 1 DI | 0.99/0.78 | 0.98/0.67 | 0.97/0.52 | 0.94/0.39 | 0.89/0.24 | 0.78/0.13 |
Conclusion: In the setting of non-inflamed meninges, cefepime 2 g IV Q8 h does not provide adequate T > MIC in the CSF for >80% of patients for MICs ≥0.5 mg/L. The influence of inflammation on the calculated CSF target attainment rates is unknown. The definitive pharmacodynamic target in the CSF has not been elucidated and further research is needed.
P909: Application of microbiological and capillary electrophoresis methods to phenoxymethylpenicillin dissolution assay
W. Grzybowska, G. Pajchel, M. Zapasnik, S. Tyski (Warsaw, PL)
Objectives: Drug absorption from a solid dosage form after oral administration depend on the release of the active substance from the medicinal product. In some cases of drug analysis, especially when the results of tests are out of specification, it is necessary to use another assay, simultaneously with the reference method. In case of phenoxymethylpenicillin tablets, the reference method for dissolution assay is spectrophotometric method. The aim of the study was to apply parallel microbiological and capillary electrophoresis methods and compare the results with those obtained using UV assay.
Methods: Two preparations (tablets), containing 1 00 000 IU/mg of penicillin V: Taropen and Ospen were examined. The dissolution tests were performed at temperature 37°C ± 0.5°C, in phosphate buffer pH 6.8 (900 ml for Ospen and 1000 ml for Taropen) using baskets, rotation speed 100 rpm; samples were taken only at: 30 minute or at 10, 20 and 30 minutes in case of profile of dissolution analysis. The amount of penicillin V dissolved was assayed spectrophotometrically at 268 nm. Hanson Research dissolution system and CE apparatus: Quanta 4000 of (Waters) were used. Pharmacopoeal, microbiological agar diffusion method and Staphylococcus aureus ATCC 6538 P strain, were applied.
Results: The dissolution of penicillin V from Taropen preparation after 30 minutes was 100%, independently on method applied. In case of Ospen tablets these values were different, depending on the analytical assay. The statistical Fisher–Snedecor test for comparison of dissolution data obtained using three methods was performed. The Fisher Fcalc. value was lower than theoretical only in Taropen case. The dissolution profiles of two examined preparations were also compared and statistically evaluated according to the FDA method. The results of these calculations showed that dissolution profiles of phenoxymethylpenicillin from Taropen and Ospen tablets differ significantly.
Conclusion: Performed analysis proved that capillary electrophoresis and microbiological methods can be used alternatively but only for determination of Taropen dissolution.
P910: Penetration of penicillin G in combination with sulbactam into nasal tissues
U. Frank, S. Wenzler-Röttele, W. Maier, F. Knapp, R. Trittler, H. Egle, K. Kuemmerer (Freiburg, D)
Objective: The penetration of antimicrobial agents into target tissues is essential for treatment at the site of infection. We investigated the distribution of penicillin G in combination with sulbactam in human nasal tissues.
Methods: To determine the pharmacokinetics of penicillin G/sulbactam, informed written consent was obtained from 22 patients aged between 19 and 73 years scheduled for endonasal operations such as septoplasty and conchotomy. After infusion of 5 m IU of penicillin G and 1 g of sulbactam, the concentrations of these agents were determined in serum and various nasal tissues such as septal mucosa, septal cartilage and bone. Serum and nasal tissue concentrations were determined by liquid chromatography-mass spectrometry (LC-MS).
Results: Up to 1, 2, 3, 4 and 5 hours after infusion, the mean serum concentrations of penicillin G were 114.9 μg/ml (SD ± 24.2), 54.0 μg/ml (SD ± 29.8), 33.6 (SD ± 26.9), 12.7 μg/ml (SD ± 9.6), 17.6 μg/ml (SD ± 8.2) and 2.8 μg/ml, while the mean serum concentrations were 17.6 μg/ml (SD ± 8.2) 24.3 μg/ml (SD ± 15.2), 9.3 μg/ml (SD ± 3.5), 3.5 μg/ml (SD ± 0.6), and 1.9 μg/ml (SD ± 0.4). Mean penicillin G and sulbactam concentrations in septal mucosa decreased from 141.7 and 128.3 μg/g (1st hour) to 3.0 and 2.7 μg/g (5th hour), respectively. In septal cartilage, the highest tissue concentrations were observed 2 hours after infusion, with mean penicillin G and sulbactam concentrations of 59.4 and 80.1 μg/g, respectively. The mean penicillin G and sulbactam concentrations in bone decreased from 31.2 and 14.8 μg/g (1st hour) to 1.4 and 1.8 μg/g (5th hour), respectively. The regression analysis of the data showed that 3 h after administration of the drug combination, the levels still exceeded the 4-fold MIC90 of methicillin-susceptible Staphylococcus aureus, Streptococcus pyogenes, Moraxella catarrhalis and Haemophilus influenzae.
Conclusions: Our data support the use of the drug combination in perioperative prophylaxis and the treatment of ENT (nasal and paranasal) infections due to common bacterial pathogens.
P911: MIC vs. kill-curve based pharmacokinetic/pharmacodynamic modelling of activities of cefpodoxime and cefixime
H. Derendorf, P. Liu, K. Rand, B. Obermann (Gainesville, USA; Munich, D)
Objectives: Pharmacokinetic (PK)/Pharmacodynamic (PD) modeling of antibiotics usually consists of the comparison between plasma PK and the MIC, such as the T > MIC, Cmax/MIC, and AUC/MIC. These indices are limited due to the innate inaccuracy of the MIC and the fact that it does not reflect the in vivo scenario where concentrations are not static but fluctuate between doses. An alternative is to use time-kill curves that follow bacterial killing and growth as a function of time and concentration. This study provides a systematic comparison of MIC and kill-curve approaches to show the potential of both methods for antibiotic evaluation. In an example, we developed a mathematical pharmacokinetic/pharmacodynamic (PK/PD) model to integrate the in vitro antimicrobial activity with the PK profile of two oral cephalosporines at the tissue site.
Methods: Kill curves could be described with different combinations of maximum kill rate (kmax), drug concentration at half-maximum effect (EC50) and bacterial growth rate (k0) that resulted in the same MIC in each scenario. In the experimental part, bacterial time-kill curves of cefpodoxime and cefixime against four bacterial strains were compared in in vitro kinetic models in which previously measured human pharmacokinetic profiles of unbound antibiotic were integrated.
Results: Different combinations of kmax, EC50 and k0 can yield the same MIC and consequently the same MIC-based index. However, depending on the combination of PD parameters, kill curves may predict quite opposite outcomes in both scenarios. EC50 values of cefpodoxime and cefixime were consistent with their respective MIC values. Both antibiotics had similar high potency against H. influenzae (EC50: 0.04 mg/L) and M. catarrhalis (EC50: 0.12 mg/L), while the potency of cefpodoxime against S. pneumoniae strains was about 10-fold higher than that of cefixime (EC50s/sensitive: 0.02 vs 0.27 mg/L; EC50s/intermediate: 0.09 vs 0.69 mg/L). Simulations showed that cefpodoxime will have higher bacteriological success against S. pneumoniae than cefixime.
Conclusions: Simple comparison of exposure and MIC may not be sufficient to evaluate anti-infective efficacy. Kill curves provide a more detailed approach in predicting antimicrobial effects. The developed Emax model effectively described the pharmacodynamics of cefpodoxime and cefixime. Cefpodoxime (200 mg bid) has higher tissue penetration and antimicrobial efficacy than cefixime (400 mg qd) against S. pneumoniae.
P912: Bacteriologic efficacy of intravenous piperacillin/tazobactam and ampicillin/sulbactam for infected diabetic foot ulcers
L. Harkless, J. Boghossian, R. Pollack, W. Caputo, A. Dana, S. Gray, D. Wu (San Antonio, Belleville, Collegeville, USA)
Objectives: To test the efficacy of single-agent empiric treatment, either intravenously administered piperacillin/tazobactam (TZP) (4 g/0.5 gq8 h) or ampicillin/sulbactam (SAM) (2 g/1 g q6 h), of moderate to severe infected foot ulcers in patients with diabetes.
Methods: In this open-label trial, 314 adults were randomized to receive TZP or SAM for up to 21 days. Patients with polymicrobial infections involving methicillin-resistant Staphylococcus aureus also received vancomycin 1 g q12 h. Samples for bacteriologic evaluation were taken at baseline from infected ulcers and blood to document causative pathogen(s) and test for antimicrobial susceptibility; samples were taken as clinically indicated at the end-of-treatment and test-of-cure visits (14–21 days post-treatment). To minimize risk of contamination, samples were to be obtained by aspirate, curettage, or biopsy rather than by swabbing.
Results: A total of 123 of the 314 patients in the study were bacteriologically evaluable. The most common causative pathogens in monomicrobial infections were S. aureus, Streptococcus agalactiae, Enterococcus faecalis, and Pseudomonas aeruginosa. About 30% of patients in each treatment arm had polymicrobic infections. The combination of S. aureus plus S. agalactiae was most common. The median duration of treatment was 8 days for both groups. The by-pathogen bacteriological success rates were similar in both treatment groups for S. aureus, S. agalactiae, and E. faecalis. TZP had an eradication rate of 85.7% for P. aeruginosa; SAM is not active against P. aeruginosa, and patients with P. aeruginosa in the SAM group (n = 5) were discontinued from the study .
Conclusions: Previous studies have shown that TZP at a dose of 3 g/0.375 g q6 h was effective for treatment of diabetic foot infections. Our study confirmed that less frequent administration of TZP at 4 g/0.5 g q8 h was sufficient to attain bacteriologic success rates of 76.9% for S. aureus, 83.3% for S. agalactiae, 71.4% for E. faecalis, and 85.7% for P. aeruginosa in the bacteriologically evaluable population. This study differed from previous studies of infected diabetic foot ulcers, which found gram-negative enterics to be more common than P. aeruginosa as causative pathogens. However, it is consistent with data showing that P. aeruginosa has recently become the gramnegative pathogen most frequently isolated from soft tissue infections in Europe, North American, and Latin America.
P913: Penetration of beta-lactamase inhibitors tazobactam and sulbactam in severe acute pancreatitis
S. Förster, E. Eckleben, U. Werner, U. Adam, R. Wacke, E. Klar, B. Drewelow (Rostock, Freiburg, D)
Objectives: Despite of high standard intensive care and surgical management, acute necrotising pancreatitis is still related with an extremely high mortality rate. This is determined by local infectious complications, especially in necrotising areas. Limited penetration of antimicrobial drugs in these areas is considered to be a major cause for failure of therapy of severe infections. Combinations of betalactamase inhibitors (BLI) and beta-lactam antibiotics like broad-spectrum penicillines (BSP) have antibacterial activity against most of the common pathogens in severe necrotising pancreatitis. Co-administration leads to an increase of antibacterial activity due to an inhibition of beta-lactamases compared to those of beta-lactam antibiotics alone. Some BSP has been shown to penetrate rapidly and efficiently into pancreatic tissue. The penetration of BLI into inflamed pancreatic tissue has not been investigated yet.
Methods: Addressing the penetration capability of BLI, a clinical trial was designed to investigate the penetration of Tazobactam (Taz, n = 8) and Sulbactam (Sul, n = 5) in patients with severe necrotising pancreatitis undergoing pancreas surgery. Samples were taken from blood, necrotic areas of pancreatic tissue (PN), peripancreatic fatty tissue (PFT) and bursa secretion (BS) following intravenous administration of 0.5 g Taz or 1.0 g Sul. Concentrations of BLI were determined by HPLC/UV. The aimed concentration for full enzymatic effect of BLI should be 4 μg/mg (Taz) and 8 μg/mg (Sul), respectively.
Results: Mean plasma concentrations at 1.0 h after application were 20.6 ± 9.58 μg/ml (Taz) and 48.6 ± 18.8 μg/ml (Sul). Corresponding mean concentrations were in PN 2.95 ± 0.25 μg/mg (Taz) and 8.48 ± 0.68 μg/mg (Sul), in PFT 1.72 ± 1.09 μg/mg (Taz) and 4.70 ± 0.88 μg/mg (Sul), in BS 8.22 ± 2.12 μg/mg (Taz) and 14.3 ± 5.59 μg/mg (Sul). The penetration rate into PN was 14.5% (Taz) and 18.8% (Sul), into BS 44.4% (Taz) and 31.7% (Sul). The aimed concentration for both BLI was reached or exceeded in plasma, PN and BS but not in PFT.
Conclusion: Both BLI has been demonstrated to reach rapidly effective inhibitory concentrations into relevant areas and compartments of pancreatic and parapancreatic tissue. In combination with BSP Taz and Sul either may have a potential clinical benefit in prevention and treatment of local infectious complications of severe necrotising pancreatitis.
P914: PK/PD of beta-lactam antibiotics in experimental urinary tract infection
D. Jensen, N. Frimodt-Moller (Copenhagen, DK)
Background: UTI is one of the most common infectious conditions treated in general practice and represents a major part of antibiotic use in the community. It is of major importance to know, how we treat these infections correctly, i.e. maximum efficacy with the least amount of drug in order to reduce the risk of development of resistance.
Materials and methods: UTI was induced in anesthetized female NMRI mice via intraurethral inoculation of 10–8 CFU of E. coli. One day later, treatment was started with 12–24 hour dosing schedules with 12-16 different doses of each drug securing a wide variation of Time > MIC and AUC/MIC. 24 h after the last dose mice were sacrificed and urine collected, and the bladder and both kidneys removed. Bladder and kidneys were homogenized before CFU determination. The drugs used were the cephalosporins, cefuroxime (CEF, MIC = 0.3 mg/l) and ceftriaxone (CRO, MIC = 0.094 mg/l), and the penicillin, mecillinam (MIC = 0.1 mg/l). The PK of the drugs in serum was determined in similar mice as well. The two cephalosporins were studied together (CEF has a t 1/2 of 14 min and CRO a t1/2 of 56 min, respectively, in mice). PD parameters were calculated from serum total antibiotic concentrations, since protein-binding is a minor issue in the urine, and the relation to CFÚs estimated by the Hill-equation.
Results: All drugs reduced CFÜs in urine and kidney tissue by 3–4 logs, but little effect was found in the bladder tissue. For the two cephalosporins combined Time > MIC in % of dosing interval best described the correlation with CFÚs in urine (R2 = 0.69, P < 0.05) and in kidney tissue (R2 = 0.89, P < 0.05), respectively, while no such correlation was found in the bladder tissue, neither did AUC/MIC reveal any correlation with CFÚs in urine or any organs. The same was found for mecillinam, i.e. no correlation for AUC/MIC vs. CFÚs in urine or organs, while Time > MIC % significantly (P < 0.05) correlated with CFÚs in urine (R2 = 0.48), and kidney tissue (R2 = 0.82), respectively. The Time > MIC% for maximum efficacy was around 30–40% for all three antibiotics.
Conclusion: The optimal PKPD parameter for efficacy of betalactam antibiotics in UTI is the Time > MIC. Maximum effect is seen for Time > MIC for 30–40% of the dosing interval, when serum total drug concentration is used as surrogate parameter. In humans this would call for TID dosing of mecillinam and cefuroxime, and OD dosing for ceftriaxone.
P915: Comparative performance of different methods to simulate drug exposure variability in a population
V.H. Tam, G.L. Rosner (Houston, USA)
Objectives: Stochastic pharmacokinetic (PK) forecasting such as Monte Carlo simulations (MCS) are increasingly being used to predict the PK variability of antimicrobials in a population, based on data from relatively few subjects. However, various MCS approaches may significantly differ in the accuracy and precision of the predictions. We compared the performance of 4 different MCS approaches using a dataset with known parameter values and dispersion.
Methods: Concentration-time profiles for 10 subjects after an intravenous bolus of 1000 mg were randomly generated using elimination rate constant (K) 0.1 ± 0.025 h−1(mean ± SD) and volume of distribution (V) 20 ± 5 L. Normal distribution of parameter values and no correlation between K and V were assumed. System noise was incorporated as a linear function of drug concentration. Using these concentration-time profiles, the best-fit parameter estimates were determined by the standard two-stage method. Four methods were subsequently used to simulate the AUC0-inf of the population by MCS, using the central tendency and dispersion of the following in the subject sample: (1) K and V; (2) clearance and V; (3) dose/clearance; (4) AUC0-inf. In each scenario, 10,000 subject simulations were performed with ADAPT II, using normally distributed input parameter(s) with means and variances set to the fitted values.
Results: Reasonably good parameter estimates were obtained (K = 0.101 ± 0.034 h−1; V = 18.0 ± 7.2 L). Compared to true AUC0-inf of the population (581.1 ± 314.9 mg h/L), the simulated AUC0-inf by various methods were: (1) 911.1 ± 2416, (2) 1348 ± 23510, (3) 1348 ± 23510, and (4) 713.7 ± 430.1 mg h/L, respectively.
Conclusions: Our results suggest that various MCS approaches may predict PK variability in a population differently. The most realistic approach appeared to be based on the variability of AUC0-inf in the subject sample. Our observations are consistent with statistical principles concerning estimation. This method did not amplify variability of the model parameters and was the least likely to be associated with model misspecification.
P916: In vivo mutant prevention concentration (MPC) studies: quantification of fluoroquinolone antibiotics in chicken liver, caecal contents and serum
S.W. Cooles, K. Stapleton, N.G. Coldham, L.P. Randall, M.J. Woodward (Addlestone, UK)
Objectives: Fluoroquinolone treatment of humans and animals can rapidly select for organisms with increased resistance to these antibiotics. Animal models are key to investigating in vivo antibiotic concentrations that prevent selection of resistance (e.g. the mutant prevention concentration (MPC) concept), but use of such models requires validated procedures for extraction and analysis of fluoroquinolones from relevant tissues. Here, we report the validation of a method to quantify the concentration of enrofloxacin, and its metabolite ciprofloxacin, extracted from chicken liver, caecal contents and serum following treatment with Baytril™ (enrofloxacin).
Methods: The extraction procedure described by Wiuff et al. 2002 was validated for fluoroquinolone analysis, in pig tissues, by fortification of target matrices with enrofloxacin and ciprofloxacin. Norfloxacin was added as an internal standard to all samples. Samples were homogenised and extracted with acetonitrile (6 ml), centrifuged and the supernatants retained for analysis. The extracts were diluted with distilled water and analysed by HPLC equipped with fluorescence detection. The analytes were chromatographed on a C18 reverse phase column and eluted with an isocratic potassium phosphate buffer/acetonitrile system.
Results: Liver samples were fortified with 0.1, 1.0 and 5.0 μg/g enrofloxacin and provided recoveries of 114.5, 78.6 and 78.2% respectively. Quantification of ciprofloxacin at the 0.1 μg/g level was not possible due to interference from sample co-extractives, but the recoveries at 1.0 and 5.0μg/g were 73.7 and 91.1%. For caecal content samples, enrofloxacin recoveries were 70.6 and 69.1% at 1.0 and 5.0μg/g respectively, and ciprofloxacin 65.4 and 63.3%. The recovery from serum was much higher, samples fortified at 0.1, 1.0 and 5.0μg/mL, enrofloxacin and ciprofloxacin yielded recoveries of 94.7, 80.9 and 86.1%, and 91.1, 85.6 and 87.9% respectively. Selected samples were also analysed by zonal microbial growth inhibition bioassay and HPLC equipped with MS/MS detection; the data were broadly similar between all methods.
Conclusion: A valid method for the analysis of fluoroquinolones in chicken liver, caecal content and serum has been established, and will be applied to in vivo MPC studies. Where sample matrices interfere (e.g. liver, caeca), bioassay or LC-MS/MS must be used to provide valid results.
P917: The ecological effects of norfloxacin and pivmecillinam (PIV) on the periurethral and vaginal flora in women with recurrent urinary tract infection
B. Stattin Norinder, R. Norrby, A.-C. Palmgren, C.E. Nord (Stockholm, Solna, S)
Objectives: To compare the ecological effects on the periurethral and vaginal microflora and time to normalisation of orally administered norfloxacin (NFLX) and pivmecillinam (PIV) in women with recurrent lower UTI.
Methods: Women with recurrent lower UTI participated in a randomized, single blind parallel multi-centre study. Twenty-five women, aged 18–55 years, with a positive nitrite test and symptoms (urgency, frequency, dysuria and/or suprapubic pain) of lower UTI were included. Only patients with an UTI caused by E. coli or Klebsiella spp were evaluated. Key exclusion criteria were; menopause; pregnancy or breast feeding, known hypersensitivity to study drugs, antibiotics within the preceding month, impaired liver or kidney function, known or clinically suspected pyelonephritis, complicated UTI and/or gastrointestinal infection. Study drugs: Seven days treatment of either NFLX 400 mg BID or PIV 400 mg TID. Samples from midstream urine, periurethra and vagina were obtained before start of treatment Day 1 and at two follow-ups Day 12–4 and 28–35. Informed consent was obtained. The Ethical Review Committee and Medical Product Agency approved the study protocol.
Results: Nineteen patients (11 NFLX and 8 PIV) fulfilled the inclusion and exclusion criteria. No differences of patient characteristics were seen between the two groups. At the initial visit, more NFLX patients were colonized with aerobic bacteria, although no differences were seen for anaerobic bacteria. The E. coli strains were suppressed markedly by NFLX and PIV in both locations. S. epidermidis increased more markedly following PIV treatment compared to NFLX in the periurethral location. In the PIV group E. faecalis was less frequent initially, increased at visit 2, and returned to pre-treatment numbers at visit 3. For the NFLX group, more patients were colonized initially with E. faecalis, with a decrease at visit 3. Lactobacilli decreased slightly in the periurethra in the NFLX group, whilst no changes were seen for PIV. Bacteroides spp. decreased more markedly for NFLX. Restoration of the pre-treatment colonization levels occurred gradually, except for E. coli being markedly suppressed by NFLX throughout the study period. The bacteriological outcome of the urinary tract infection both at the short-term and long-term follow up was successful.
Conclusions: Limited ecological effects on the microflora were seen following treatment with NFLX and PIV, a benefit for antibiotics used for treatment of patients with UTI.
P918: Antibiotics influence release of IL-6 and IL-8 by KB cells and gingival fibroblasts
S. Eick, M. Lausse, S. Schwarz, P. Wachter, W. Pfister, E. Straube (Jena, D)
Objectives: In general, antibiotics are used in defense against pathogenic bacteria. Nevertheless, side effects such as immunomodulatory activity should be considered. The purpose of this study was to determine the effect of antibiotics normally used in periodontal treatment on the release of IL-6 and IL-8 by KB cells and gingival fibroblasts.
Methods: KB cells and primary gingival fibroblasts were infected with Actinobacillus actinomycetemcomitans Y4 (A.a.) and Porphyromonas gingivalis ATCC 33277 (P.g.). The antibiotics doxycycline, tetracycline, minocycline, metronidazole, and moxifloxacin were added in concentrations ranging from 0.25 MIC to 100 μg/ml. After 1, 6 and 18 h supernatants were obtained and the levels of IL-6 and IL-8 were measured by ELISA technique. Additionally, after 18 h the number of surviving bacteria was enumerated.
Results: Minocycline and moxifloxacin in concentrations predicted in serum as well as 100 μg/ml were effective in killing planctonic A.a. and P.g. as well as adherent and intracellular bacteria. Low levels of both interleukines released from KB cells and fibroblasts infected by P.g. were found only after addition of tetracycline up to 10 μg/ml. Metronidazole, moxifloxacin and tetracycline in subinhibitory concentrations enhanced the release of IL-6 from non-infected and A.a.-infected fibroblasts (up to 3200 pg/ml) after 18 h, contradictory 100 μg/ml tetracycline and minocyline reduced the release of IL-6. IL-6 in the supernatants of KB-cells was detectable only after addition of 100 μg/ml moxifloxacin. Each 100 μg/ml of tetracycline and minocycline suppressed totally the release of IL-6 and IL-8 from non infected and infected fibroblasts, but not from KB cells. Metronidazole and moxifloxaxin in high concentrations promoted the release of IL-8.
Conclusions: Antibiotics influence the release of IL-6 and IL-8. Besides the good antibacterial effect especially minocycline might suppress inflammation. Nevertheless, the killing of bacteria as well as a possible inhibition of virulence factors (bacterial proteases of P.g. by tetracycline) might influence the enhanced or reduced release of these cytokines.
Organ transplants
P919: Exceedingly infrequent infectious complications during orthotopic liver transplantation: tubercular peritonitis
R. Manfredi (Bologna, I)
Introduction: Tuberculosis (T) is a very infrequent complication in patients (p) who undergo solid organ transplantation: in liver transplant recipients a 0.9–2.3% rate has been retrieved by a literature update. In these p T occurs within 12 months, and less than 10% of cases are observed after a repeated transplantation. Pulmonary localization predominates (50% of p), followed by disseminated T (30%), while extrapulmonary T is an exceedingly rare event, reported only nu anectdotal p descriptions. Pathogenetically, a T peritonitis follows disseminated infection or a primary T enteric localization, and is borne by a 80% mortality rate.
Case report: A 57-year-old female p with a mute T personal and familial history and normal chest X-ray, underwent liver transplantation 9 years ago, because of a HCV-related decompensated cirrhosias. Four years later a novel graft was needed, after the development of end-stage hepatic insufficiency due to massive HCV re-infection. One year later (while of cyclosporin treatment), abdominal pain and ascites formation prompted admission, and M. tuberculosis sensible to all tested drugs was repeatedly isolated from an abdominal fluid with an elevated lymphocyte-monocyte count. Associated ethambutol, isoniazid, streptomycin and levofloxacin (this one replaced by cycloserine after 2 months), led to a complete clinical and bacteriological cure already achieved after 3 months, although a 3-drug anti-T treatment was continued for 1 year.
Conclusionas: In our rare case report, the selected anti-T chemotherapy showed a successful efficacy and tolerability profile, with contained untoward events despite a very critical clinical context, due to the severity of T complication, and the broad spectrum of problems related to graft and all associated issues. In order to obtain an early diagnosis, an elevated clinical suspicion should be maintained for this rare complication too, by recommending microscopy and culture search of mycobacteria on ascitic fluid.
P920: Nosocomial infections in the renal transplant recipient
S.R.P.E. Dantas, R.H. Kuboyama, M. Mazzali, M.L. Moretti (Campinas-SP, BR)
Objective: To determine the incidence of nosocomial infections in the renal transplant recipients and risk factors associated with urinary tract infection (UTI) and surgical site infection (SSI), in patients hospitalized in the Hospital and Clinics of the Universidade Estadual de Campinas, São Paulo, Brazil.
Methods: From January 2000 through December 2001, a prospective cohort study was conducted to determine the rate of bacterial nosocomial infection in renal transplant recipients. The patients were divided in two groups according to the origin of the allograft: cadaver or living donors. Enterobacter cloacae strains, the most prevalent multidrug-resistant bacterial organisms isolated from UTI were determined using genomic analysis with pulsed-field gel electrophoresis (PFGE).
Results: One hundred sixty-three patients who received renal transplants were reviewed during the hospitalization. One hundred and ten (67.5%) renal transplanted were from cadaver and 53 (32.5%) from living donor. The median of length of stay in hospital was 12 days (range, 9–75 days) from transplant of living donor and 26 days (range, 2–28 days) from transplant of cadaver (P < 0.0001). Twenty-one (39.6%) living donors recipients and 68 (61.8%) cadaver donors recipients had bacterial infection episodes (P = 0.019). Post-transplant nosocomial infections diagnosed during the hospitalization were UTI (44.8%), SSI (11%), pneumonia (6.1%), bloodstream catheter-related infection (4.2%) and others (1.8%). Risk factors for UTI in the multivariate analysis included cadaver donor recipient; substitution of the initial immunosuppressive regimen; days of urinary bladder catheterization and length of stay in hospital before the infection. Substitution of initial protocol of the post-transplant immunosuppressive regimen and the surgeon was also associated with SSI. Six different E. cloacae multidrug-resistant to antibiotics DNA profiles were detected in UTI of our recipients and hospital dissemination was documented.
Conclusions: UTI was the single most important type of hospital infection in renal transplant recipient and a significant difference in the incidence of UTI was found comparing living donor and cadaver donor recipient. The high incidence of UTI in the early period post-transplant suggested that the operative manipulation of the urinary tract may be an important causative factor for the development of UTI.
P921: Usefulness of CMV antigenaemia assay after liver transplantation
H.K. Ki, K.-M. Sohn, J.-Y. Rhee, Y.-M. Wi, C.S. Moon, W.S. Oh, K.R. Peck, N.Y. Lee, J.-H. Song (Seoul, KOR)
Objective: To evaluate the clinical manifestations of cytomegalovirus (CMV) infections among the liver transplant recipients in Samsung Medical Center.
Methods: All the recipients of liver transplantation during the period from Jan 1996 to Aug 2003 were enrolled. Medical records and microbiologic data for CMV infections were reviewed retrospectively. Preemptive therapy was initiated if CMV antigenaemia was positive (>/=3/200,000 cells) as preventive strategies for CMV infection.
Results: All the 284 enrolled patients received livers from CMV seropositive donors, and 281 recipients (98.9%) were CMV seropositive before transplantation. 133 recipients (46.8%) had evidences of CMV reactivation: 125 patients were positive for CMV antigenaemia, 15 patients for CMV culture, 14 patients for CMV PCR, 12 patients for pathology, and 10 patients for CMV IgM. Among the patients with CMV reactivation, 40 recipients were symptomatic (30.1%): 12 patients had organ-specific CMV diseases. Most of the CMV infections occurred within 180 days after transplantation except 9 patients (6.7%). Among the antigenaemia positive patients, the mean number of CMV antigen-positive WBC was 19.36 per 200,000 cells (19.36 ± 37.64 cells). The mean duration of CMV antigenaemia was 8.72 days (8.72 ± 9.99 days). Peak value of CMV antigenaemia was significantly higher (p = 0.002) in symptomatic patients compared to asymptomatic patients (41.38 ± 61.38 vs. 9.68 ± 13.97). Duration of CMV antigenaemia was significantly longer (p = 0.002) in symptomatic patients. Eleven recipients (8.3%) had experienced recurrent episodes of CMV infection detected by CMV antigenaemia. Recurrence rates were higher (p < 0.001) in symptomatic infections. Underlying liver diseases of the recipients, infectious complications other than CMV, rejection rates, and survival rates were not different between symptomatic and asymptomatic CMV infections (p > 0.05). Conclusion: About an half of the recipients experienced CMV reactivation, mostly within 180 days post-transplantation. Thirty percents of reactivation were symptomatic. Peak value and duration of CMV antigenaemia were significantly higher in symptomatic infections than those in asymptomatic infections.
P922: Toxoplasma gondii infection in bone marrow transplant recipients: the polymerase chain reaction-blood sample combination in diagnosis and early detection
A. Sensini, R. Castronari, C. Ferranti, T. Aloisi, F. Aversa, F. Bistoni (Perugia, I)
Objectives: Toxoplasmosis is a rare and frequently fatal complication in bone marrow transplant recipients. It presents with local brain lesions or disseminated infection. Usually, the diagnosis is based on histologic confirmation and observation of typical lesions on radiologic imaging, which resolve after appropriate therapy. The aim of this study was to stress the pivotal role of the polymerase chain reaction (PCR) in diagnosis and early detection of Toxoplasma infection.
Methods: From January 1999 to July 2004 two hundred and thirteen patients underwent allogeneic peripheral blood stem cell transplantation (PBSCT). In the presence of symptoms suggestive of cerebral, pulmonary and disseminated Toxoplasma infection, 992 biological samples (blood, serum, CSF, pleural fluid, BAL) were collected and examined by nested PCR.
Results: Fourteen cases of toxoplasmosis were identified, having an incidence of 6.6%. Ten patients manifested cerebral toxoplasmosis, two had pulmonary infection and two disseminated. The overall mortality in this group, not necessarily due to toxoplasmosis, was 57% (8/14). The pre-transplant recipient serostatus was known in 9 patients: 5 were seropositive, but it is to be noted that 4 were seronegative, whereas 5 were unknown. MRI study was performed in 12 patients. Typical lesions were observed in 7 patients (sensitivity: 58%). The pulmonary toxoplasmosis occurred very early (day 9 and 10) and cerebral toxoplasmosis from day 29 to day 240 (mean 80.4) after PBSCT. One case of disseminated infection had CNS localization (day 21) and then pulmonary (day 42), whereas the second case had first pulmonary involvement (day 8) immediately followed by CNS. Blood samples demonstrated higher sensitivity (10 PCR-positive/12) than CSF (6 PCR-positive/11) in identification of the etiologic agent. All patients with toxoplasmosis were treated with pyrimethamine and sulfadiazine.
Conclusion: The study confirms the pivotal role of PCR in early diagnosis of toxoplasmosis after PBSCT. In our experience, a positive PCR signal in blood was an early sign of Toxoplasma infection, therefore blood appears to be a suitable and reliable biological sample for diagnosis. Moreover, the samples were PCR-negative after the start of therapy and therefore PCR can be useful to monitor the effect of treatment. Finally, our study indicates that toxoplasmosis is a potential pathology even in pre-transplant seronegative subjects, suggesting primary infection.
P923: Cryptosporidium associated cholangitis in a liver-transplant patient
C. Denkinger, P. Harigopal, P. Ruiz, A. Tzakis, L. Dowdy (Würzburg, D; Miami, USA)
Cryptosporidium parvum is a parasite of the group coccidia. C. parvum causes self-limiting diarrhoeal illness in immunocompetent hosts and severe long standing diarrhoea in immunocompromised patients. Sclerosing cholangitis (SC) caused by C. parvum is frequently found in HIV-infected patients. In the transplant recipients only two case reports exist describing SC due to C. parvum; one in an adult renal transplant patient and the others in three children who underwent liver transplantation. We report herein the first case of C. parvum associated cholangitis in an adult liver transplant patient. This 52-year-old male patient underwent a liver transplantation three years prior to presentation. His initial transplant failed due to acute rejection requiring retransplant within one year. The second transplant was complicated by sepsis, tacrolimus induced hemolytic uremic syndrome, leaving the patient hemodialysis dependent. In 2004, he presented with pruritus, hypotension, severe dehydration and a three-week history of severe diarrhoea. Endoscopic biopsy revealed numerous organisms in the stomach and changes in the colon consistent with cryptosporidiosis. Stool cultures were negative. In addition, gamma gluytamyl transferase and alkaline phosphatase were elevated while bilirubin and AST were normal. The patient was diagnosed with colitis due to cryptosporidium and treated with azithromycin. Immunosuppression with tacrolimus was continued. The patient continued to have diarrhoea, low-grade fevers and fatigue. Two weeks later a cholangiogram and liver biopsy were performed. The liver biopsy revealed C. parvum lining the ductal epithelium. SC was diagnosed. The cholangiogram showed no sclerosing changes in the biliary tree, suggesting an early phase of disease. Paromomycin was added to the regimen. The patient improved, and was discharged home. We believe this to be the first case of SC associated with C. parvum in an adult liver transplant recipient.

P924: Risk of human herpesvirus 6 infection in seronegative solid organ transplant recipients
C. Cervera, M.A. Marcos, N. Benito, A. Sierra, J.C. Trullas, F. Cofan, J.M. Salmeron, M.J. Ricart, F. Orús, C. Regata, A. Moreno, T. Pumarola (Barcelona, E)
Objective: Human herpesvirus 6 (HHV-6) infection usually occurs during the first 2 years of life, and its prevalence is higher than 95% in adult population. Negative serostatus for HHV-6 in solid organ transplant recipients is a risk factor for fungal infection, but the incidence and severity of HHV-6 infections in seronegative patients has not been evaluated. Our objective is evaluate prospectively seronegative HHV-6 solid organ transplant patients for HHV-6 infection by means of quantitative PCR for HHV-6.
Methods: From February to August 2004, we prospectly evaluated all solid organ transplant patients. Patients must have a minimum follow-up of 3 months. Patients underwent basal determination of IgG for HHV-6. Seronegative patients were included for follow-up. Blood samples were obtained at 7, 14, 21, 28, 45, 60, 75, and 90 days post-transplant. For viral DNA analysis, following DNA amplification, it was determined by hibridation in microplaque (Affigene).
Results: In the study period, 112 patients were evaluated (58 kidney, 35 liver, 11 heart, 4 kidney and pancreas, liver and kidney 2, pancreas 1, heart and kidney 1). Nine patients were seronegative (7 kidney, 1 liver, and 1 heart). We analysed 67 plasma samples. All patients but one had a negative PCR for HHV-6. The patient with primary infection had a maximum of 78,002 HHV-6 DNA copies/ml. Clinically, the patient suffered from slight abdominal pain and discrete cholestasis in blood analyses; no fever or serious complications were detected. He did not receive pre-emptive treatment with Ganciclovir. No fungal infections were detected.
Conclusion: Primary infection by HHV-6 in seronegative solid organ transplant patients is not frequent, and in 1 patient it appeared with slight symptoms. However, a larger study with more seronegative patients is needed.
P925: Development and validation of a new real-time PCR assay for HHV-6 detection and differentiation of HHV-6A and HHV-6B
D. Becker, S. Ziegelmaier, S. Wach, T. Laue, T. Grewing (Hamburg, D)
Objectives: Human herpesvirus 6 (HHV-6) has been identified as the etiologic agent of roseola infantum in infants. In adults HHV-6 causes complications in immunocompromised patients such as AIDS patients and transplant recipients. Two virus variants can be distinguished: HHV-6A and HHV-6B. Several studies have shown variant specific clinical outcome. The objective of this work was the development of a reliable, sensitive and specific HHV-6 detection assay, based on real-time PCR technology, which enables the discrimination between HHV-6A and B. This assay ought to run with the same temperature profile as the RealArt LC PCR assays for HSV1/2, EBV, CMV and VZV (artus GmbH).
Methods: By sequence alignments, a region of the HHV-6 genome was defined, which allows the specific amplification by real-time PCR, and discrimination between HHV-6A and B by melting curve analysis. Assay specificity has been tested by analysing HHV-6 A/B reference material (ABI) and cell culture supernatant from clinical isolates. Cross reactivity was excluded by testing DNA from related viruses and bacteria. Analytical sensitivity was determined by probit analysis. A heterologous PCR system was incorporated, which serves as an internal control. A set of quantitation standards was established, for exact quantitation of the viral load.
Results: With the RealArt HHV-6 A/B LC PCR assay artus GmbH developed a ready-to-use assay for the detection and distinct differentiation of HHV-6A and B. Quantitation of the viral load within a broad linear range is possible for both variants. Simultaneous amplification and parallel detection of internal control and specific sample in one reaction tube excludes false negative results. The RealArt HHV-6 A/B LC PCR assay has the same temperature profile as the RealArt LC PCR assays for HSV1/2, EBV, CMV and VZV. 0
Conclusion: The RealArt HHV-6 A/B LC PCR assay allows sensitive and specific detection, as well as subtyping of HHV-6. This leads not only to a reliable HHV-6 diagnosis, but also to a better understanding of the role of HHV-6 variants in pathogenesis. Due to the same temperature profile, the RealArt HHV-6 A/B PCR assay completes the RealArt LC PCR assays for the detection of different herpes viruses. Now the parallel detection of HSV1/2, EBV, CMV, VZV, and HHV-6 A/B is possible in a single real-time PCR run. Thus, clinicians receive a reliable diagnostic tool for rapid detection of herpes viruses, and especially in transplant recipients.
P926: Quantitative CMV PCR in allogenic stem-cell transplant patients
L. Cardeñoso, C. Blazquez, R. Rodriguez, J. Diaz-Regañon, E. Lomas, P. Sanchez, R. Cámara (Madrid, E)
Objective: To assess the clinical value of a commercial quantitative plasma CMV-PCR assay (COBAS AMPLICOR CMV MONITOR test, Roche Molecular System) in allogeneic SCT patients by comparing the results obtained with the PCR with those obtained with antigenaemia. To evaluate the impact of an automatised DNA extraction method and a lower cut-off on PCR sensibility.
Methods: All patients were monitored until day 100 post-SCT with weekly antigenaemia and PCR. A total of 562 blood samples from 30 patients (23 mieloablative and 7 non-mieloablative; 25 HLA identical siblings and 5 from unrelated donors) were tested prospectively. Twenty-seven CMV seropositive patients (or negative with a seropositive donor) received high dose of acyclovir as prophylaxis. PCR was considered positive when more or equal 600 DNA copies/ml were detected. Antigenemia was considered positive when one or more positive cells were detected (in 2x105 PMNs). Positive samples by antigenaemia and/or PCR (n = 54 samples) were tested retrospectively with an automatised extraction method (MAGNAPURE).
Results: All CMV seronegative patients with a seronegative donor (n = 3) were antigenaemia and PCR negative. Seropositive patients (n = 27): 14 had a positive antigenaemia and/or PCR, with a total of 23 CMV infection episodes. None developed CMV disease. PCR detected 10 out of 23 CMV episodes. Overall there were 44 positive antigenemias (belonging to 13 patients): 23 were PCR+, 20 PCR negative and 1 PCR inhibited. Only 1 patient had a positive PCR with a negative antigenaemia. Automatised MAGNAPURE extraction increased the sensibility of the PCR. With this method PCR detected 19 out of 23 episodes in contrast with only 10/23 with the manual extraction. For samples with less than 600 DNA copies/ml a manual calculation of the number of copies was retrospectively done (using a new cut-off of 50 copies/ml). With this lower cut-off, PCR detected 20 out of 23 CMV episodes. None of the negative patients by antigenaemia and/or PCR gave a positive result with the automatised extraction method or with the lowered cutoff PCR.
Conclusion: Quantitative CMV PCR assay showed a lower sensibility for the detection of CMV infection in allogeneic SCT compared with antigenaemia. Two technical modifications increased the sensibility without a decrease in the specificity: automatised MAGNAPURE extraction, and lowering the cutoff.
P927: Trichosporon beigelii as a life-threatening pathogen in bone marrow transplantation recipients: the first case report from Iran
S.A. Ghiasian, A.H. Maghsood (Hamedan, IR)
Patients undergoing bone marrow transplantation (BMT) are profoundly immunosuppressed as a result of their intensive chemotherapy and are at high risk for opportunistic fungal infections mainly caused by Candida spp and Aspergillus spp. Trichosporon beigelii (T. beigelii) has emerged as a life-threatening opportunistic pathogen in immunocompromised hosts. Response to antifungal agents is poor, mortality is high and immunological recovery is the most important factor for a favorable outcome in patients with trichosporonosis. We present the first case of T. beigelii infection in patients undergoing allogeneic BMT in Iran. A 12-year-old female presented with aplastic anemia, cough and fever. She had received cytotoxic drug therapy, broad spectrum antibiotics and was neutropenic. T. beigelii was repeatedly demonstrated by appropriate morphological and physiological characteristics in her sputum, nose and mouth ulcers by direct microscopy and culture, and also isolated and histopathologically recognized in post-mortem from lung and liver. Trichosporonosis is likely to be recognized more frequently than apparent from the available reports.
Exotic infection – I: case series
P928: Trichinella infection in Greenland
L.N. Moeller, S. Andersen, M. Melbye, E. Petersen, C.M.O. Kapel, P. Laurberg, A. Koch (Frederiksberg, Aalborg, Copenhagen, DK)
Objectives: Trichinellosis is a well-known problem in Greenland. In West Greenland a number of large outbreaks took place during the 1940's and 1950's, but since then only sporadic cases have been registered. It is unknown whether the decrease in trichinellosis cases reflects the general transition in Greenland towards a more western lifestyle with less consumption of meat from wildlife, or whether it reflects insufficient case registration. The objectives of the present study were to determine the prevalence of human trichinellosis from the 1980'ies to present times in Nuuk, the capital of Greenland, and in Ammassalik district on the east coast of Greenland, where more traditional food is still eaten, and to evaluate if changes in lifestyle had an effect on prevalence.
Methods: Blood samples from 86 persons collected in 1981 and 533 persons collected in 1998 in Nuuk and Ammassalik district were tested for Trichinella-specific IgG antibodies using ELISA and Western blot analyses. Background information was obtained from questionnaires from the 1998 study.
Results: In 1981 the trichinellosis prevalence was 8.7% in Nuuk and 23.8% in Ammassalik district, while the prevalence in 1998 was 5.2% in Nuuk and 19.8% in Ammassalik district. Persons living in the settlements of Ammassalik district had higher Trichinella-specific antibody prevalence than persons living in the town of Tasiilaq. The following risk factors were significant in a univariate analysis: Ethnicity, age, place of living, dietary habits, intake of seal meat, and hunting. A multivariate model was constructed consisting of the variables: Ethnicity, age, place of living, diet group, intake of seal meat, and hunting. The variables were removed stepwise in the following order: seal meat (p = 0.73), hunting (p = 0.36), age (p = 0.3), and ethnicity (p = 0.16). The final multivariate model consisted of diet group and place of living, both being significant. Thus, living on a Greenlandic diet and living in the settlements in Ammassalik district implied higher relative risk of being Trichinella seropositive than living on a diet dominated by imported food items and living in Nuuk.
Conclusion: As lifestyle in the settlements is more traditional compared both with Tasiilaq and Nuuk, these results indicate that the decline in human trichinellosis cases in the 19th century most likely reflects the transition from traditional greenlandic lifestyle to more western dietary habits.
P929: Study on prevalence of Toxocara cati in vagrant cats of Sari township, Iran, 2004
M Sharif, P. Ziapoor, H. Ziaee, S. Kholami (Sari, IR)
Objectives: Toxocara cati is one of the important and prevalent parasites in cats and common between human and animals. Ingestion of larvae of this parasite and lack of it's maturation in human body, the infected persons develop visceral larvae migrans which is known as toxocariasis. Considering the significance of transmission of this parasite in human and due to the increase in vagrant cats in Sari township, this study was performed in order to determine the severity and prevalence of Toxocara cati in these cats in Sari township.
Methods: This cross sectional descriptive study was done on 100 vagrant cats (28 males and 72 females) during April to October 2004. Sampling was done randomly at different regions by net. The specification of vagant cats were recorded after hunting and were deeply anaesthetized by chloroform to annihilate them. The intestinal content were examined for the presence of parasites and counting of their number was done finally after fixation and staining by recommended kits of reference book for genus and species identification.
Results: In all, 42 (42 %) cats were infected with Toxocara cati, of which 8(19%)were males and 34 (81%)were females. Range of infection was 1-32 and mean severity of infection was 3.14 for each cat. The rate of infection at the west region was more than the other sites, and it was more in the females than males and also it was more in immature than the mature cats.
Conclusion: Considering the merely high prevalence of this zoonotic parasite and it's hygienic significance in causing toxocariasis in human particularly in children, who are in more contact with soil and also lack of control on vagrant cats population, which are the potential risk factors, it is recommended to control personal and dietary hygiene and avoid storing the garbages in unprotected wire boxes on the streets in order to prevent the gathering of vagrant street cats.
P930: Imaging in 100 patients of pulmonary hydatid disease; review of unusual imaging appearances
S. Zahirifard, M. Bakhshayeshkaram, M. Tahbaz, K. Kaynama (Tehran, IR)
Objective: To evaluate the chest radiography and CT scan characteristics of pulmonary hydatid disease.
Material and methods: 100 patients with surgically proven pulmonary hydatid cysts were enrolled for study. We reviewed clinical findings and imaging of patients. The radiological features (localization, diameter, architecture, density and other radiological signs and appearances) were determined.
Results: On CXR 124 cysts were determined. On 82 available CT scans a total of 112 cysts were detected. No discrete cyst was detected on 11 CXR. On 82 available CT, a total of 112 cysts were detected and in 5 CT scans no cyst was detected. 57 cysts were ruptured and 25 patients with ruptured cysts had hemoptysis. Single cysts were in 63 patients while multiple cysts were in 37. Median CT density was 24HU. Respectively, it was seen on CT and CXR waterlily sign in 18 and 22 patients, Air-fluid level in 12 and 17 patients and cresent sign on 11 and 5 of patients. Inverse cresent sign and calcification were not observed on CXR s but each one was recorded on 4 CT scans. On CT scan 90% of Cysts were smooth and 89% were uniloculated. 19% of cysts were infected.
Conclusion: CT scan should be done to elucidate cystic nature of the lung masses and for accurate localization in the preoperative period. In endemic regions like Iran, atypical imaging presentation of complicated pulmonary hydatid disease such as solid masses should be considered in differential diagnosis of pulmonary lesions (abstract truncated at 250 words)
P931: The seroprevalence of coxiellosis in farmers and cattle in north-eastern Turkey
S. Seyitoglu, Z. Ozkurt, U. Dinler, B. Okumus (Erzurum, TR)
Objectives: Coxiellosis is a worldwide zoonosis caused by Coxiella burnetii. The aim of this study was to determine the prevalence of coxiellosis in cattle and farmers in North Eastern Turkey.
Methods: A total of 230 cattle and 92 human sera were collected in 2003, and tested for antibodies against C.burnetii by commercial ELISA test.
Results: The antibodies of C. burnetii were detected in 22 (9.56%) cattle and 18 (19.5%) healthy farmers. Seropositivity was found in 12 of 53 (22.6%) cattle with abortion history, and 10 of 177 (5.6%) cattle without abortion history (p < 0.05). There was correlation between animals and human seroprevalance in same district. Thirteen of 18 farmers who were antibody positive had seropositive animals, and there were seropositive animals in the villages of remaining 5 cases. It was observed that seroprevalance of coxiellosis was higher in north districts (in animals 15.4%, in humans 32.4%), have drier and warmer climate, than in other districts (in animals 6.5%, in humans 12.1%) both for humans and animals (p < 0.05).
Conclusions: The study show that coxiellosis was an important health problem both in humans and in animals in our region.
P932: An unusual case of Gramineae in sublingual salivary gland
L. Doganci, M. Calgurel, Y. Gungen, G. Kiran (Ankara, TR)
Foreign bodies of organic nature and parasitic elements are very rare in oral cavity and in salivary glands in humans because of their structural and functional features. Here we report a very interesting case, with sublingual salivary gland involvement of Gramineae (Brachiaria spp.) which was thought to be a parasitic life cycle in the gland.
Case: 40 y/o female teacher with a recent history of travel to mountains where she drunk and had an exposure to unsafe spring water. She had a strong stinging pain right after she drunk the water in her mouth, radiating to her neck. She developed fever, pain, lymph node swelling, difficulty of eating, weight lost and remarkable eosinophilia. She also noted a self moving small tail-like object on the orifice of the sublingual salivary gland. Removal of the object revealed an interesting unusual living object. Then, definitive diagnosis is Gramineae (Brachiaria spp) after parasitological and pathological consultation.
Comment: To our best knowledge, this unusual case is the first presented patient related to travel in our region. Differential diagnosis has several entities including squid sperm bag sting, marine animal larvae and nematod and trematod life stages.
P933: Evaluation of Echinococcus granulosus prevalence using ELISA and abdominal ultrasonography in a group of students staying in a state hostel in Turkey
B. Arda, H. Pullukcu, T. Yamazhan, S. Tamsel, G. Demirpolat, M. Korkmaz (Izmir, TR)
Objective: Cystic echinococcosis, caused by larval form of Echinococcus granulosus is one of the most important and widely distributed parasitic zoonotic diseases in the world. Echinococcosis is a major problem in all regions of Turkey but particularly prevalent in rural areas, where domestic livestock raising is common. The reported epidemiologic findings are usually based on retrospective evaluation pf surgical findings or hospital charts. Well planned epidemiologic studies are limited. In this study our aim was to analyse the seroprevalance of cystic echinococosis and prevalance of lesions (with abdominal ultrasonography) in a group of young adult university students who were staying in a state hostel in Bornova-Izmir-Turkey.
Method: The study group consisted 750 students (360 woman, 390 men, aged 20.92 ± 1.82, min 17, max 29). Informed written consent was received from each student and they were requested to fill a questionnaire form. Blood sampling was performed by IV puncture and sera were obtained after centrifugation. Anti Echinococcus granulosus antibodies were detected by using ELISA tecnique. All participants were gven an appointment for abdominal ultrasonography.
Results: Of 750 students 99 (13.2%) were seropositive for anti Echinococcus granulosus Ig G (table 1). A total of 250 students (49 seropositive- 201 seronegative) were performed abdominal ultrasonography (3.5 MHZ transducer, Sonoline, Elegra-Siemens). Two of 250 students (1 in liver, 1 in kidney both seropositive) had cystic lesions and were referred to surgery.
Table 1.
Distributions of seropositive cases
| Age range | Female (%) | Male (%) | Total (%) |
|---|---|---|---|
| <20 | 17.33 (13/75) | 10.00 (8/80) | 13.54 (21/155) |
| 20–24 | 17.08 (42/281) | 14.67 (27/284) | 13.24 (75/665) |
| 25–29 | 25.00 (1/4) | 7.69 (2/26) | 10.00 (3/30) |
| Total | 17.22 (62/360) | 9.48 (37/390) | 13.20 (99/750) |
Conclusion: Well designed epidemiologic studies about cystic echinococcosis are lacking in Turkey. A previous study showed seropositivity rate of 13.7% for Echinococcus granulosus. Our findings suggest that cystic echinococcosis is prevalent in Turkey and epidemiologic studies combining ELISA and abdominal ultrasonograpy are warranted.
P934: Epizootiology and epidemiology of anthrax in Eastern Turkey between 1992–2004
Z. Ozkurt, M. Parlak, R. Tastan, U. Dinler, Y.S. Saglam, S.F. Ozyurek (Erzurum, TR)
Objective: Anthrax is an epidemic zoonosis in Eastern part of Turkey. This study was aimed to investigate the epizootiology and epidemiology of anthrax in this region.
Methods: Animal and human anthrax cases during 1992–2004 period were included in this study. Data were obtained formal records of Health Directorate, Institute of Veterinary Control and Investigation. The diagnosis of anthrax had based on clinical findings and/or microbiological procedures, including Gram strains and culture of materials obtained from lesions.
Results: In a 13-years period, 464 animal cases and 503 human cases with anthrax were detected. Of 464 animal cases, 20 (4.3%) were sheep, others (95.7%) were cattle. Most cases occurred between July and September in both animals and humans. Anthrax was seen most frequently in Erzurum, which is the important centre for animal commencement. When the first 6 years period (1992–1997) was compared with last 7 years period (1998–2004) the number of animal cases were 161 vs. 230 and human cases were 234 vs. 269. An analysis of the yearly case distribution shows that the incidence of anthrax in this region had not been changed.
Conclusion: Anthrax is an important health problem both animals and humans in this region. The preventive measures should be taken for decreasing the incidence of anthrax.
P935: Molecular ecological study of B. anthracis in Kazakhstan
Y. Sansyzbayev, A. Aikimbayev, L. Lukhnova, T. Meka-Mechenko, V. Dubiansky, Z. Sagiyev (Almaty, KAZ)
Objectives: Anthrax is endemic in Kazakhstan and occurs among humans at an incidence rate of 0.1 to 1 per 100,000 population per year. During the late 1990s, several epidemics occurred associated with home slaughter of infected animals, and a general increase in incidence was seen among animals and humans. Historically, Kazakhstan accounted for 15% of the anthrax cases reported from the Soviet Union; and the plains of Central Asia may have served as the historical source of B. anthracis for the rest of the world. In Kazakhstan, the geographic distribution of anthrax among animals and humans is focal and generally associated with areas considered to be ‘high-risk’. The determinants of this focal distribution are poorly understood. In addition, strains of B. anthracis isolated from outbreaks within these foci have not been compared on a molecular or pathogenic basis.
Methods: Work has been initiated to study the geographic distribution and potential environmental preferences of B. anthracis using geographic information system (GIS) technologies.
Results: The GIS was used to map a set of B. anthracis strains from several outbreaks between 1997 and 2003 to evaluate geographic patterns. The GIS is also being used to derive a historical database of spatially explicit human and livestock outbreaks from 1948 to 2003 for spatial analyses on the nationwide distribution of B. anthracis. This database contains information on the location of the anthrax incident, the year and month of the occurrence, whether the incident involved livestock or human, the outcome of the disease, and biological information about the strains.
Conclusions: Although in a preliminary stage of application, the ArcGIS software can be used to map loci of anthrax occurrence. In the future, these maps will be used to identify factors that influence the occurrence and spread of the pathogen and to prevent infection of livestock or humans. The research described in this abstract was made possible in part by support provided by the U.S. Defense Threat Reduction Agency (DTRA) under the project ≪ KB0-1950-AL-03≫ and administered by U.S. Civilian Research and Development Foundation (CRDF).
P936: Structure of anthrax morbidity in Kazakhstan
A. Aikimbayev, L. Lukhnova, T. Meka-Mechenko, Y. Pazylov (Almaty, KAZ)
Objectives: The anthrax situation in the country was unfavorable from the 1950s through the 1970s. Until the 1990s, anthrax in Kazakhstan was an occupational disease in animal husbandry. After 1991, the practice of raising livestock for private use increased. This report shows that, at the same time, the incidence of anthrax in persons involved in this practice increased significantly.
Methods: In order to characterize the epidemic process, we used methods of descriptive epidemiology, using epidemiological variables (who became ill, where and when, trends of disease by time, sources, transmission factors of B. anthracis, and the age, gender, and occupation of persons who become ill with anthrax).
Results: Anthrax occurs in rural areas among private owners of livestock and their families and persons hired to assist with the slaughter. In the last decade, 89.4% of cases of anthrax illness in
humans were caused by the slaughter of domestic livestock. Of these cases, 62.2% were unemployed rural residents, 2.3% were shepherds working for cooperatives, 11.7% were blue-collar workers, 5.4% were white-collar workers, and 18.1% were students. A single source, path and factors of transmission of B. anthracis are typical of this type of the disease. In recent years, the majority of cases involve infection of several persons during the slaughter of a single diseased animal. The source of infection is cattle in 48.2% of cases, sheep and goats in 15.7% of cases, horses in 31.2% of cases, and soil in 4.7% of cases. The factors of transmission of B. anthracis to humans are contact with the meat of livestock during slaughter and butchering in 91.9% of cases, vector-borne transmission in 2.7% of cases, and soil in 5.4% of cases. A large number of human cases occur in July through September.
Conclusion: In Kazakhstan today, the prevalent sub-type of anthrax disease in humans involves non-professional activity at home. This requires changes in the tactics of preventing the disease. The research described in this abstract was made possible in part by support provided by the U.S. Defense Threat Reduction Agency (DTRA) under the project KB0-1950-AL-03 and administered by U.S. Civilian Research and Development Foundation(CRDF).
P937: Establishment of non-productive infection and activation of inf-alpha and -gamma gene expression in normal lymphomonocytes by sars-cov
C. Castilletti, L. Bordi, E. Lalle, G. Rozera, F. Poccia, C. Agrati, I. Abbate, M.R. Capobianchi (Rome, I)
Objectives: Severe acute respiratory syndrome (SARS) is an emerging infection caused by a novel coronavirus known as SARS-CoV. During the early phases of the disease, the presence of the replicative intermediates of SARS-CoV has been shown in PBMC from patients. No information is available on the ability of SARS-CoV to stimulate IFN induction, although IFN-gamma may be activated in SARS patients. We investigate the capability of SARS-CoV to give rise to a productive infection in normal PBMC, in parallel with the ability to activate IFN-alpha and -gamma gene expression.
Methods: Normal PBMC were infected with a MOI 0.1. Virus progeny formation was measured at subsequent time points, by back-titration of cell lysates on Vero cells. Cell mortality and apoptosis were detected by trypan blue and propidium iodide staining. In order to detect virus-specific plus- and minus-RNA strand, total RNA extracted from SARS-CoV-infected PBMC was retrotranscribed in the presence of the sense and antisense primers, respectively, targeting the replicase gene. Measurement of SARS-CoV genomic RNA was performed by quantitative Real Time RT-PCR. IFN induction was performed by exposing PBMC to SARS-CoV at different MOI, ranging from 0.1 to 10. Induction of IFN-alpha and -gamma was analysed by measuring their mRNA levels by limiting dilution RT-PCR. Sensitivity of SARS-CoV replication to exogenous IFN-alpha and -gamma was tested in Vero cells pre-exposed to the individual cytokines of to a combination of both.
Results: In unstimulated PBMC, no infectious viral progeny formation was detected up to day 13 post-infection. Nevertheless, minus-strand and genomic SARS-CoV RNA peaked at 24 hours post-infection. Dose dependent induction of both IFN-alpha and IFN-gamma mRNA was observed, that was most evident at MOI 10. A combination of these two cytokines was shown to strongly inhibit SARS-CoV replication in Vero cells.
Conclusions: Our results show that SARS-CoV is able to infect normal PBMC. However, this appears to be only a transient phenomenon, followed by a progressive disappearance of both virus-specific RNA strands, with no infectious virus progeny production. Moreover, SARS-CoV appears to have the intrinsic ability to activate dose-dependently both IFN-alpha and -gamma gene expression in PBMC cultures. Our results can be pathogenically relevant to the inflammatory events occurring in the diseased tissues that can be mediated by the endogenous activation of INF system.
P938: Production of extracellular proteases and toxic metabolites by Trichoderma strains isolated from opportunistic infections
L. Kredics, J. Pakarinen, Z. Antal, M. Andersson, L. Manczinger, M. Salkinoja-Salonen, C. Vágvölgyi, E. Nagy (Szeged, HUN; Helsinki, FIN)
Objectives: Trichoderma species are potential candidates for biocontrol of plant pathogenic fungi and cellulase producers of biotechnological importance. On the other hand, they are emerging as opportunistic pathogens of immunocompromised and dialized patients. This study was designed to examine the ability of 10 clinical Trichoderma isolates to produce extracellular proteases and to screen them for toxicity to mammalian cells.
Methods: Supernatants from induced liquid cultures of the examined strains were screened for proteolytic enzyme activities with 11 different chromogenic p-nitroaniline substrates. Trypsin- and chymotrypsin-like activities were separated by Sepha-dex G-100 column chromatography and their pH-dependence was studied. Sperm toxicity bioassays were performed by exposing boar sperm suspension to Trichoderma-methanol extracts, the motility of spermatozoa was estimated by phase-contrast microscopy. Mitochondrial membrane damage in spermatozoa was studied by epiflurescence microscopy using the JC-1/propidium iodide staining.
Results: The production of trypsin-like, chymotrypsin-like and chymoelastase-like protease activities was common among the examined strains. Separation of trypsin- and chymotrypsin-like activities by column chromatography revealed, that both systems are complex consisting of several isoenzymes. Relatively high activity levels were detected between pH 5 and 9 suggesting that the different isoenzymes have different pH characteristics. More than 90% of the spermatozoa were motile in a non-exposed control sample and in a sample exposed to 5 microliter of methanol. More than 90% of the spermatozoa were immotile in samples exposed to T. longibrachiatum UAMH 9515, ATCC 201044, CM382 and T. harzianum CBS 102174 in a concentration of 1.25 mg biomass ml-1, indicating that these strains produce heat-stable substances toxic to sperm cells. These four strains were found to inhibit the motility of boar spermatozoa even at a low concentration (50% reduction of motility in the case of 5 microgramm ml−1 of extended boar sperm) and to induce dissipation of mitochondrial membrane potential. Other studied strains had no toxic effect.
Conclusions: Production of extracellular proteolytic enzymes and toxic metabolites are among the potential virulence factors of Trichoderma strains as emerging fungal pathogens. This work was supported by grants F037663 of the Hungarian Scientific Research Fund and 53305 of the Academy of Finland.
P939: Occurrence of scabies in patients and in the staff of healthcare facilities
K. Zitek (Prague, CZ)
Objectives: Scabies is an itching dermatosis which continues to be a frequent health problem. Long-term follow-up of the epidemiological situation confirms a thirty-year cycle for which there is no satisfactory explanation.
Methods: Standard methodology of diagnostics is based on a) subjective sensations in the patient b) objective dermatological finding c) positive epidemiological history d) laboratory demonstrations of causative agent e) remission of symptoms upon specific therapy. Cases of scabies diagnosed and reported by dermatologists nationwide are included by the public health service in the central system EPIDAT (NIPH, Prague).
Results: The last two documented epidemic waves of scabies affecting the Czech Republic peaked in 1970 and in 1993. Specific morbidity is the highest among persons 15–24 years of age (it closely connected with sexual activity-the source of infestation in 60% of adults was a sexual partner and that is confirmed by an almost identical trend in reported scabies morbidity and fresh cases of syphilis in 1965-1999 years), but the morbidity trend has been falling sharply after the year 1993. However, morbidity in persons over 65 years of age has been gradually rising over recent years. Group epidemics (86) have been repeatedly reported in such facilities as departments of gerio-psychiatry, institutions for long-term chronic patients, old folks homes, social care institutes and charity facilities. That occurs in bed-ridden subjects hospitalized on a long-term basis, the mentally retarded and the superannuated, in whom the scabies is of a nosocomial character. The affected staff of healthcare institution is very often the source of further transmission to others, namely to immobile patients, as well as to especially vulnerable individuals under higher risk of infection. Analysis of the reported cases revealed a 13% share of healthcare workers in this infection. Under greater risk are senior nurses (62%), junior nurses (21%), auxiliary paramedical staff (13%) and the last of all physicians (4%). Scabies as an occupational disease occurs almost exclusively in the healthcare sector.
Conclusions: Scabies poses on increased risk for the younger population (active scabies) and the elderly population (passive scabies). It poses a great occupational risk in the paramedical healthcare staff carrying out nursing or managing services. It is necessary to consistently observe preventive and repressive epidemiological measures in the population.
P940: Fire ants, the new public health problem in Iran
K. Akbarzadeh, M. Nateghpour, S. Tirgari (Tehran, IR)
Ants are probably the most successful of all insects. They are present almost in all countries and all places. A few of them can bite, sting and squirt formic acid. Formica rufibarbis and a few the others are secondary hosts of Dicrocoelium dentriticum in Iran. But the newest public health problem depending on ants in the country is biting and stinging of fire ant Pachycondyla sennaarensis (Formicidae; Hymenoptera) in south and southeastern Iran. Ecology, biology and morphology of P. sennaarensis were considered in Iranshahr County (southeast of Iran) where has been much infected because of the ant. According to the survey over 92% of questioned individuals had bitten at least once with the ant. Usually the effects of the stings are mild but this ant is capable of multiple stinging and this can induce annoyance people especially in children.
P941: A survey on the geographical distribution of soft and hand ticks in Buyer Ahmad and Dena cities, Kohgilouye and Boyer Ahmad province, Iran
M. Shayeghi, N. Piazak, A. Khoramro, S. Moosakazemi (Tehran, IR)
Objective: Tick play as important role in diseases transmission to human being. Different tick-borne diseasea including borreliasis, CCHF have been reported from iran.
Method: An attempt was made to determine the fauna and geographical distribution of soft and hard ticks in this area from October 2002 until April 2004. About 10% of the villages were selected randomly and tick collection was carried out using standard method. Ticks were collected from indoor resting and hiding places in 70 villages as well as inside stables, rodent borrows, on sheep, lamps, goat and cattel by monthly in each season.
Result: 3382 ticks were collected and identified using national systematic key. The copmosition and frequencies of them were as follows: Ornithodoros lahorensis (11%), Argas persicus (23.12%), Rhipicephalus bursa (4.3%), Rhipicephalus sanguines (1.53%), Haemaphysialis concinna (9.6%), Haemaphysialis sulcata (26.8%), Haemaphysialis punctata (1.54%), Hyaloma schulzei (8.16%), Hyaloma marginatum (7.21%), Hyaloma dentriticum (3.08%), Hyaloma asiaticum (1.53%).
Conclusion: Distribution and ferquency of tlck was differ in various season and location.
P942: Evaluation of the use of saliva to soothe bloodsucking arthropod bites
R. Romano, F. Curtale, F. Benvegnú, R. Zamburlini, V. Ascoli, M. Coluzzi (Rome, Portogruaro, I)
Objectives: Our study is based on the working hypothesis that a new category of medically important bloodsucking arthropods, ‘promoter arthropods’ (Coluzzi M et al, 2002, Parassitologia 44:123) is involved in the transmission of human herpes virus type 8 (HHV-8). This fits well with epidemiological evidences such as i) the prevalence of non-sexual intra-familial horizontal transmission (Mbulaiteye SM et al, 2003, J Infect Dis 187:1780), and ii) the possible role of human saliva, the only body fluid in which HHV-8 DNA is detectable (Dedicoat M et al, 2004, J Infect Dis 190:1068). The conditions for HHV-8 transmission are met when i) a child's skin responds to the bite of a blood-sucking arthropods, and ii) an HHV-8-seropositive mother (or caregiver) attempting to relieve the child's itching and to reduce scratching applies her infective saliva to the bite's site. The use of saliva is a traditional behavioural practice in sub-Saharan Africa, for healing with herbal leaves crushed and mixed with saliva and for medical practices and in the premastication of food (Wojcicki JM, 2003, Br J Cancer 89:2016). The human behaviour associated with the transfer of saliva from parents to infants and the use of herbal leaves treated with saliva in relation to arthropod bite could be a risk factor for HHV-8 infection and perhaps other infections too (such as the hepatitis B virus).
Methods: To evaluate to what extent saliva is used to heal insect bites on children's and adolescents’ skin, we draw up a questionnaire directed at students of elementary and intermediate school. Two groups were tested, one from Italy (a school near Rome, Latium, and schools in Veneto) and one from a
sub-Saharan African country known for high transmission levels (Uganda, between Kampala and Entebbe by Lake Victoria).
Results: The frequencies of the use of saliva were not significantly different in Latium (12.5%) and in Veneto (14.6%) so that an average frequency of 13.5% (96/712) has been compared with the frequency of 74.8% (119/159) from Uganda (P ≪ .0001). The frequencies in the two groups are related also to a different cultural and economic development and improvement in hygiene.
Conclusion: We suggest that blood-sucking promoter arthropods can play a role in the spread of HHV-8 infection particularly in Africa. Therefore, a behavioural change limiting the use of saliva on the skin and to prepare herbal leaves, could be an attempt to control the spread of HHV-8 infection.
P943: C-reactive protein and reduced glutathione in cerebrospinal fluid of patients with tick-borne encephalitis
I. Zeltina, A. Broduza, V. Sondore, N. Sevastjanova, B. Rozentale (Riga, LV)
Background: Prognosis of tick-borne encephalitis (TBE) is very difficult to appoint. Although the serious TBE virus-host cell interactions are involved in the development of pathological process, correlation of standard laboratory findings with clinical course and outcome of disease is problematic. The inflammatory and antioxidant changes in the cerebrospinal fluid (CSF) also are controversial in different CNS damages including TBE.
Aim of study – To find out in CSF some baseline markers of inflammation and redox status for the estimation of development tendences and clinical course of pathological process in TBE.
Patients and methods: 60 patients with meningeal and meningoencephalitic form of TBE treated at the Infectology Center of Latvia were included in this study. Diagnosis of TBE was confirmed by ELISA, Enzygnost, Anti-TBE IgM in blood and/or CSF. Traditional clinical criteria were used for the characterization of TBE severity degree. Some nontraditional lab methods were used: C-reactive protein (CRP) (immunoturbidimetrically) and reduced glutathione (GSH) concentration (colorimetrically) detection in CSF.
Results: Concentration of CRP in CSF was significantly higher in TBE patients in acute phase (5.55 ± 1.0 mg/l; n = 34) than in reconvalescence (2.41 ± 0.5 mg/l; n = 26), P = 99%. CRP and GSH in about 50% of TBE cases in CSF was under detectable values. The second part of TBE patients demonstrated tendency of the increasing of GSH during acute stage of disease (1.64 ± 0.20 mg%; n = 32) if compared with reconvalescence (1.41 ± 0.20 mg%; n = 24), P = 61%. No statistically significant differences of CRP and GSH concentrations in CSF were found in cases of moderate meningitis form of TBE if compared to severe meningoencephalitic form of TBE.
Conclusion: 1) Analysis of data obtained from patients with TBE gives evidence of substantial CRP and GSH changes in CSF in dependence on disease stage, but not on its severity degree. 2) These objective biochemical data from CSF investigation give proof that there are no separately moderate and severe TBE cases in clinic: they have to be interpreted always as equally severe. 3) The origin of CRP and GSH in CSF is unknown (production in CNS and/or from blood due to blood-brain barrier permeability increasing?).
P944: Vibrio cholerae is transported to water bodies by adult, flying chironomids
M. Broza, H. Gancz, M. Halpern, Y. Kashi (Haifa, IL)
Background: Cholera is a severe disease caused by Vibrio cholerae. The natural reservoir of this aquatic pathogenic bacterium is referred to as the ‘aquatic environment’. Our group showed that egg masses of the non-biting midge Chironomidae spp. (Diptera) harbour V. cholerae and provide nutrient source for their multiplication, thereby offering a new natural reservoir for the cholera bacterium.
Objective: The presence of viable V. cholerae on flying adult chironomids will suggest that V. cholerae can be carried through the air to other water bodies by the adult flying insects and hence a new route of infestation of water sources by the bacteria is suggested.
Methods: In field studies chironomid egg masses and adults were simultaneously collected from the same environment. In addition fresh, drinking quality water was left exposed or netted in the vicinity of adult chironomid hatching foci. The exposed water was monitored for chironomid egg masses and V. cholerae presence. In the laboratory those experiments were repeated with V. cholerae O9 tagged with Green Fluorescent Protein.
Results: To date, more then 30 V. cholerae serogroups have been isolated from chironomids egg masses and adults. In the field experiments, a clear-cut connection between netting and V. cholerae absence was noted implying that a relationship exist, between entrance of large invertebrate to water bodies and presence of V. cholerae in that water. In the laboratory experiments, the GFP tagged bacteria were found on the outer surface of the adult chironomid, in locations prone to microbial attachment.
Conclusions: The evidence shown here suggests that aerial transport of V. cholerae by chironomids flying adults is feasible and does lead to V. cholerae contamination of unprotected water bodies.
P945: Intracellular survival of Vibrio cholerae O1 El Tor strains in environmental protozoa- Acanthamoeba castellanii may induce bacterial phenotypic alterations
G. Sandström, A. Weintraub, H. Abd (Stockholm, S)
Objectives: Cholera is a severe and potentially life-threatening diarrheal disease caused by certain spices of the gram-negative bacterium Vibrio cholerae. Many millions of cases of cholera occur annually, in epidemic and pandemic forms due to V. cholerae O1 and O139, and also sporadically due to non-O1 and non-O139 V. cholerae strains. In this context, the survival of V. cholerae in nature is of interest from an epidemiological perspective. Although the natural reservoirs for survival and multiplication of V. cholerae are far from compeletly disclosed, our previous study has shown that free-living amoebae can be reservoirs for the seventh-pandemic V. cholerae O1 El Tor- Inaba strain N16961, which can survive and grow intracellularly in Acanthamoeba castellanii. The aim of this study was to examine the ability of different strains of V. cholerae O1 El Tor to grow and survive in Acanthamoeba castellanii, and to examine whether intra-amoebic survival of bacteria alter their pattern of resistance and sensitivity to different antibiotics.
Methods: V. cholerae O1 El Tor strains were co-cultured with A. castellanii for more than two weeks. The interaction between these microorganisms was followed by viable counts of alone- and co-cultivated microorganisms. Intra-amoebic growth and localization of each bacterial strain were estimated by gentamicin assay, viable count, microscopy, and PCR to detect cholera toxin gene and amoebic 18s RNA gene disclosing symbiont-host association.
Results: The results show that examined V. cholerae O1 El Tor strains multiplied and survived inside trophozoites and cysts of A. castellanii. The bacterial internalization was in cytoplasmic compartment of the amoebae cells. The relation between these microorganisms in co-cultures could be classified as symbiosis, since presence of the amoebae enhanced growth of bacterial strains, and presence of the bacteria did not affect amoebic growth. The intra-amoebic survival of bacteria did not alter their pattern of resistance and sensitivity to different antibiotics such as ampicillin, gentamicin, and tetracycline.
Conclusions: This study shows a facultative intracellular behaviour of examined V. cholerae O1 El Tor strains, which is in contrast to the general held view, which considers the bacterium to be extracellular microorganisms. The clinical importance of free-living amoebae is their possible role as ‘Trojan horse’.
P946: Genetic variability among serotype G4 human rotavirus strains circulating in Palermo in the period 1985–2003
G.M. Giammanco, S. De Grazia, V. Martella, C. Colomba, A Cascio, S. Arista (Palermo, Bari, Messina, I)
The genetic variation of VP7 and VP4 antigenic proteins was studied in 38 G4 strains recovered in Palermo from 1985 to 2003. VP7 sequence analysis showed that 14 strains, recovered during 1999–2003, though cross-reacting with G4-ST3:1 MAb, belonged in fact to genotype G9 and were 99% identical to G9 strains recovered in Palermo from 1999. Sequence comparison of 23 G4 strains grouped them into three sublineages (Ia to Ic) containing respectively viral strains collected in 1990–1994, 1995 and 1999–2003. Amino acid sequences were well conserved within each sublineage and a peculiar single amino acid insertion was observed in the variable region 4 of all sublineage Ic strains. Both G4 and G9 Italian strains exhibited P[8] genotype and their VP4-encoding sequences clustered in previously defined lineages following a temporal distribution: strains collected in 1989–1993 fell within lineage P[8]-1, while those recovered in 1995–2003 clustered in lineage P[8]-3. The variety of their deduced amino acid sequences enabled us to describe, respectively, two (1A and 1B) and six (3A–3F) different patterns of substitutions with regard to lineage P[8]-1 and P[8]-3 reference strains. Comparison of VP7 and VP4 gene sequences of Italian and European G4 strains indicates that different G4P[8] populations have been circulating in Europe over the years and that the latest Italian strains are more closely related to recent isolates from other countries than to the reference vaccinal ST3 strain. These results will help increase knowledge about G4 rotavirus epidemiology and evolution, and might be useful for future rotavirus vaccine formulation.
P947: Detection of rotavirus, adenoviruses and astrovirus in gastroenteritis cases among young children, first experience with adenovirus identification by PCR and microplate hybridisation assay
C. Christaki, G. Vrioni, E. Priavali, C. Gartzonika, V. Papatolis, S. Levidiotou (Ioannina, GR)
Objectives: The aim of the present study was the detection of Rotavirus, Adenovirus and Astrovirus in stool samples from young children hospitalized with acute gastroenteritis and Adenovirus species identification.
Methods: Stool specimens were collected from 684 young children, hospitalised in the University Hospital of Ioannina (NW Greece) from April 2002 to November 2004. The detection of Rota (group A), Adeno (all human serotypes) and Astroviruses antigens (seven human serotypes) was performed by Enzyme Immunoassay method (DAKO IDEIA Rotavirus, Adenovirus and Astrovirus Tests, respectively). All specimens positive for Adenoviruses were confirmed and identified by a PCR-microplate hybridization assay (PCR Adenovirus Consensus, Argene, Biosoft), which used Adenovirus genus-specific primers and one generic and six species-specific probes defined in the VA RNA gene. According to our results: Rotavirus was detected in 63 cases (9.2%), Adenovirus in 15 cases (2.2%) and Astrovirus in 15 cases (2.2%). PCR Adenovirus Consensus assay identified the Adenovirus species from all the 15 cases: Adenovirus species F (enteric Adenovirus serotype 40/41) in 11 cases (1.6%), Adenovirus species C in 2 cases (0.3%) and Adenovirus species A in 2 cases (0.3%). Rotavirus gastroenteritis presented a seasonal distribution in spring, while Adenovirus and Astrovirus gastroenteritis presented no seasonality.
Conclusions: Rotavirus gastroenteritis was significantly more common than Adenovirus and Astrovirus infections in young children in our territory. PCR Adenovirus Consensus technique was a useful method for the identification of Adenovirus in stool specimens. Eventhought enteric Adenoviruses 40/41 (species F) caused the majority of acute gastroenteritis due to Adenovirus, non-enteric serotypes (species A and C) were occasionally involved in the aetiology of acute diarrhoea. The study continues with the examination of great number of specimens and patients for the investigation of more useful and specific results.
P948: Immigrant inpatients from 1999 until today: ‘pressure’ exerted over infectious disease wards
R. Manfredi (Bologna, I)
Objective: Foreign individuals officially living in Bologna and province are 39186 with predominant origin from Northern Africa (31.5%), Eastern Europe (22%), and Far East (12%). The temporal trend of admissions of patients coming from outside of the European Union was examined according to a broad series of variables.
Methods: Through the electronic databases of our Hospital located in a metropolitan area of Northern Italy, informations related to all foreign patients (p) hospitalized or followed by Day-Hospital centres have been collected from January 1999 up to March 31, 2004. After recording all discharge diagnosis-related group (DRG) codes we focused attention on those regarding Infectious Diseases.
Results: Overall discharges were 339051, with 6670 regarding foreign p:a prevalence of the female sex (64.4%) was noticed. In 49.6% of foreign p, the mean age ranged from 20 to 35 years. The rate of foreigners compared with overall admitted p varied from 0.3 of year 1999 to a. maximum of 0.47% of year 2002. A major involvement was borne by Obstetrics-Gynecology (39.3%), Internal Medicine (13.1%), Specialistic Surgery (7.3%), Specialistic Medicine and Pediatrics (7.3% each), and Emergency Medicine (7.1%). When considering Infectious Disease-related DRGs, tuberculosis (142 cases), HIV-AIDS (25), chronic viral hepatitis and related complications (22), septicemia, central nervous system infection, and acute viral hepatitis (12 episodes each), were the most frequent discharge codes followed by other Infectious Disease DRGs (72 cases). The duration of admission of foreign p was very short (1–3 days) in 42.1% of cases, while it reached 4–7 days in 22.6% of p, and 8–14 days in 11.2% of cases, while the mean hospitalization time at Infectious Diseases ward was 8.6 ± 3.2 days (p < .002). Even 549 hospitalizations ended with voluntary discharge which occurred during the first day of admission in 61.8% of p.
Discussion: Our pilot study demostrates that the need for health care expressed by foreign p is increasingly frequent and covers a very broad spectrum of disorders with Infectious Diseases-associated illnesses gaining a increasing role through time. A significant problem is represented by the tendency to very short duration of hospitalization for foreign p, often ending with voluntary discharge while admissions carried out at our specialized Infectious Disease ward are significantly more prolonged, although they are expected to give an increased benefit in terms of effective management.
P949: Change of the characteristics of natural focuses of plague and microbiological properties of plague microbes as a result of consequences of the natural calamity on Aral Sea
A. Nematov, A. Mustanov, G. Bazarova (Tashkent, UZB)
Enzootics of plague as that of any other transmissible feral herd [feral nidal] infection are determined by the interaction of a disease's causative agent and its warm-blooded carriers under specific ecological environment.
Introduction and objectives: Change of the characteristics of natural focuses of plague and microbiological properties of plague microbes as a result of consequences of the natural calamity on Aral Sea.
Methods: Conventional microbiological research methods were used, when studying microbiological properties of 116 strains of plague microbe from Kyzylkum natural focuses of plague isolated from rodents, ticks and fleas.
Results: Strains from the Kyzylkum natural focuses of plague have all determinants of virulence, show characteristics that allow attributing them to the continental variety, i.e. glycerin digestion, do not ferment rhamnose and decompose arabinose; they have nutrient need that is typical for the strains from the Central Asian desert focus. There are differences in the need for amino acid leucine, whereas strains from Ustyurt and Gissar focuses are dependant on it. Out of 116 strains from the Kyzylkum natural focus only 8 turned out to be dependant on luecine. There were identified stains from the Kyzylkum natural focus that had essentially different properties as compared to the majority of isolated cultures, in particular, those can not synthesize fraction 1 of the plague agent; have growth factor of different nature, i.e. lower dependence on phenylalanine. Plague bacteria strains circulating in rodent populations in the Kyzylkum natural focus are characterized by low virulence in white mice and guinea-pig, although they have all the determinants of virulence. When studying resistance to antibiotics, there were identified strains non-susceptible to streptomycin (5%).
Conclusions: Thus, studying the properties of the causative agent of plague is of great importance for solving problems of natural focuses and understanding patterns of fluctuations in the epizootic situation in a certain territory. This understanding is an integral part of determining the epidemic potential of natural focuses, and is used in organizing epidemiological surveillance of the infection.
Infection and immunopathology
P950: Amyloid peptide beta 1–40 enhances the action of Toll-like receptor-2 and -4 agonists but antagonizes Toll-like receptor-9 induced inflammation in primary mouse microglial cell cultures
M. Lotz, S. Ebert, H. Esselmann, J. Wiltfang, J. Gerber, R. Nau (Gottingen, Erlangen, D)
Objectives: Toll-like receptors (TLR) play a key role in the recognition of products from virtually all classes of pathogenic organisms. Amyloid peptides also can stimulate the innate immune system. For this reason, we hypothetized that bacterial compounds and amyloid peptides may jointly stimulate the innate immune system.
Methods: The interaction of endogenous and exogenous stimulators of innate immunity was examined in primary cultures of mouse microglial cells after application of defined Toll-like receptor (TLR) agonists [lipopolysaccharide (LPS) (TLR4), the synthetic lipopeptide tripalmytoyl-cysteinyl-seryl-(lysyl)3-lysine (Pam3Cys) (TLR2) and single-stranded unmethylated Cytosineguanosine (CpG) oligodesoxynucleotide (TLR9)] alone and in combination with amyloid beta peptide (Abeta) 1–40. Supernatants from stimulated glial cultures and unstimulated controls were analysed for nitric oxide (NO), tumor necrosis factor-alpha (TNF-alpha) and interleukin-10 (IL-10) production.
Results: Coadministration of Abeta1–40 with LPS or Pam3Cys led to an additive release of NO and TNF-alpha. In contrast, co-application of Abeta1–40 with CpG led to a substantial decrease of NO and TNF-alpha release compared to stimulation with CpG alone. CpG was the only compound investigated, which induced the release of the anti-inflammatory cytokine IL-10.
Conclusion: The additive effect of LPS and Pam3Cys and Abeta may be one reason for the clinical deterioration frequently observed in patients with Alzheimer's disease during infections. The substantial decrease of NO and TNF-alpha release after CpG and Abeta application compared to stimulation with CpG alone suggests that not all microbial products enhance the stimulatory effect of Abeta on innate immunity. The cause for the divergent behaviour after activation of TLR9 versus stimulation of TLR2 and TLR4 probably lies in differences of the signaling cascade.
P951: HLA-B27 is a marker for susceptibility and severity of reactive arthritis after Salmonella, Shigella, and Yersinia infections but not after Campylobacter and E. coli enteritis
P. Schiellerup, H. Locht, K.A. Krogfelt (Copenhagen, DK)
Objectives: Reactive arthritis (ReA) is a well-known complication after infections with Salmonella, Yersinia, Shigella and Campylobacter. The presence of tissue-antigen HLA-B27 is associated with ReA, and HLA-B27 may be a marker of a prolonged disease course. We designed a case-case comparison study of ReA after gastrointestinal infections caused by Salmonella, Yersinia, Campylobacter, Shigella and E coli, to evaluate the impact of HLA-B27 on attack rate and severity of ReA between these 5 bacteria.
Methods: Between January 2001 and November 2002 consecutive patients were included from the Danish Registry of Gastrointestinal Infections, when culture positive for Salmonella, Yersinia, Campylobacter, Shigella, orE coli. All patients were addressed by a questionnaire. In this study ReA includes reactive arthritis and arthralgia. Debut of pain in a previously healthy joint was registered and patients were asked to mark swollen or tender joints on a drawing. A VAS-scale was used for assessment of pain caused by ReA. All patients were encouraged to donate blood samples for serology and HLA-B27 typing (PCR).
Results: A total of 2106 patients returned the questionnaire (response rate 67%). Only subjects with mono-infections were included. The male/female ratio was 40/60. Blood samples were obtained from 1558 (74%): Campylobacter (n = 693), Salmonella (n = 503), E. coli (n = 213), Shigella (n = 74) and Yersinia (n = 75). The overall prevalence of HLA-B27 was 9%, corresponding to the rate within the Danish population. Odds ratios for contracting ReA when the individual was HLA-B27 positive were; Campylobacter 1.70 (CI: 0.89; 3.43), Salmonella 3.4 (CI: 1.83; 6.37), E. coli 1.1 (CI: 0.23; 5.04), Shigella 33.5 (CI: 2.48; 452.78) and Yersinia 5.1 (CI: 1.03; 25.68). Thus, HLA-B27 was significantly more frequent among ReA-patients with Salmonella, Yersinia, and Shigella compared to Campylobacter and E coli. The VAS-score for ReA was significantly higher in the groups with Yersinia and Salmonella. There was a significant positive correlation between VAS-score and the fractions of patients that were HLA-B27+.
Conclusions: This large comparative study shows that HLA-B27 has a significant impact on the susceptibility to contract ReA after Salmonella, Shigella, and Yersinia, but not after Campylobacter or E. coli. Furthermore the severity of ReA as measured by VAS differed among bacterial species and was strongly correlated to the presence of the HLA-B27 antigen.
P952: A shift to Gram-negative bacteria in the intestinal microflora contributes to immunopathology of acute ileitis in the Toxoplasma gondii-driven mouse model of small intestinal inflammation
M. Heimesaat, A. Fischer, D. Fuchs, O. Goldenberg, H. Jahn, I. Dunay, R. Schumann, A. Moter, D. Gescher, H. Hahn, U. Göbel, S. Bereswill, O. Liesenfeld (Berlin, D)
Objectives: The normal gut microbiota triggers experimental colitis and large intestinal manifestations of human inflammatory bowel diseases (IBD). However, the availability of animal models for the study of ileitis is limited. Thus, only little is known hitherto in small intestinal IBD. Recently, parasite-induced ileitis in the mouse, mimicking characteristics of ileitis in human IBD, was proposed as a model for Crohn's disease (CD). Oral infection of susceptible C57BL/6 mice with Toxoplasma gondii induces a severe Th1-type immunopathology, which is restricted to the terminal ileum. In order to unravel the mechanisms underlying ileitis, we used this model to monitor microflora changes during ileal inflammation and determined contributions of the gut microbiota to ileal disease.
Methods: C57BL/6 mice were infected perorally with 100 cysts of T. gondii (ME49 strain). Ciprofloxacin, metronidazole, ciprofloxacin plus metronidazole (each 50 mg/kg body weight/d, p.o.), piperacillin plus tazobactam (200 mg/kg body weight/d, i.p.) were applied from day 0 until day 8 after T. gondii-infection. The ileal bacterial flora was analysed on day 8 p.i. by microbiological and molecular methods (16S rDNA-targeted denaturing gel electrophoresis (DGGE), sequencing of clone libraries).
Results: Microbiological and molecular approaches revealed that ileal inflammation leads to an increased total bacterial load and to drastic changes in the flora composition. In the acute stage of disease, the grampositive cocci and rods - predominant in the ilea of healthy mice - are displaced by gramnegatives, identified as Escherichia coli and Bacteroides sp., respectively. Antibacterial treatment (ciprofloxacin, metronidazole, a combination of both, or piperacillin plus tazobactam) ameliorated disease symptoms and reduced ileal inflammation. This was also seen in SPF-mice colonized by only one grampositive bacterial species.
Conclusions: The fact that gramnegative bacteria accumulate during acute ileitis and contribute profoundly to intestinal inflammation is well in line with similar observations in experimental colitis and in human IBD. This provides evidence that gut flora modulation is a valuable therapeutical strategy for IBD treatment. Finally, the contribution of gut microbiota to ileal disease supports the use of the parasite-induced small intestinal inflammation as a model for IBD research.
P953: Assessment of hydroxyproline as a marker for collagenolytic activity in neuroinflammatory disorders
J. Sellner, F. Simon, D. Meli, D. Grandgirard, B. Storch-Hagenlocher, U. Meyding-Lamade, S. Leib (Berne, CH; Heidelberg, D)
Objectives: Pathophysiologic mechanisms that contribute to brain injury in neuroinflammatory disorders include breakdown of the blood-brain-barrier, extravasation of leukocytes, cerebral hypoperfusion and vasculitis. Matrix-Metalloproteinases (MMPs) including the collagenases MMP-2 and -9 are crucially involved in all these steps. In this study we aimed to assess the extent of in-vivo collagenolytic activity in cerebrospinal fluid (CSF) by determination of the amino acid hydroxyproline, a major and exclusive degradation product of collagen.
Methods: Paired serum and CSF samples from patients with bacterial meningitis (n = 11), aseptic meningitis/encephalitis (n = 17), multiple sclerosis (n = 13), and normal CSF (n = 12) were assessed. Degraded collagen was hydrolysed to dissolve its major component hydroxyproline, which subsequently was determined spectrophotometrically. CSF levels of MMP-2 and -9 were studied by gel zymography. In a rat model of pneumococcal meningitis localization of collagenolytic activity was performed by in-situ zymography with intramolecularly quenched gelatin.
Results: Hydroxyproline in CSF from patients with bacterial meningitis was significantly increased compared to all studied groups (P < 0.001) while serum hydroxyproline did not differ significantly between the groups. The amount of hydroxyproline in CSF correlated significantly with the amount of MMP-9 (r = 0.8; p < 0.001). In the rat model in-situ zymography localized gelatinolytic activity to the subarachnoidal and ventricular space inflammation and in association to cortical lesions.
Summary & Conclusions: The study documents a significant increase of the collagen degradation product hydroxyproline in CSF of patients with bacterial meningitis. The close correlation of hydroxyproline and MMP-9 in the CSF validates the assessment of hydroxyproline as an index for CSF collagenolytic activity in neuroinflammatory diseases and supports a role for collagenases in the pathogenesis of bacterial meningitis.
Staphylococcal infections
P954: Toxic shock syndrome: a diagnostic difficulty
S. Thomas, D. Waghorn, M. Lyons (High Wycombe, UK)
Introduction: Toxic shock syndrome (TSS), is an acute, non-contagious systemic illness. It is caused by the toxin producing strains of S. aureus and the β-haemolytic streptococci and can occur in any non-immune person exposed to a TSS toxin. TSS is commonly associated with menstruation and tampon use, however can also be related to skin or soft tissue infections, particularly post surgical, skeletal infections or respiratory tract infection. TSS is often non-immunising and recurrent menstrual-associated TSS is well-described. Literature suggests that TSS is extremely rare, but diagnostic difficulties can lead to misdiagnosis and TSS can be fatal if left undiagnosed. We report a series of three cases of TSS, presenting within a short period of time.
Case Reports: Case 1. 17 year old female, presented with sudden onset collapse, diarrhoea, vomiting and abdominal pains. She gave no history of menstruation and an initial diagnosis of severe gastroenteritis was made. She failed to respond to conservative management and required ITU support. She was discharged with no firm diagnosis and re-presented one month later with similar symptoms, when a diagnosis of staphylococcal TSS was confirmed. Case 2. 15 year old female, presented during menses with sudden onset rash, rigors, severe diarhhoea, vomiting and abdominal pains. She was diagnosed with staphylococcal TSS on admission. Case 3. 28 year old female. Presented with sudden onset severe diarrhoea, vomiting, pyrexia and rash. She gave no history of menstruation. She responded poorly to treatment, required ITU support, high dose steroids and was eventually diagnosed with streptococcal TSS.
Discussion: Diagnostic criteria for TSS include high fever, hypotension, erythematous rash and a complicated multisystem disfunction. Patients often require aggressive management. The Public Health Laboratory Service reports an average of 18 cases of diagnosed TSS in the UK per year. However, because of the uncommon and difficult nature of the diagnosis, many cases are misdiagnosed and therefore go unreported. It is essential to maintain a high level of suspicion for patients who are epidemiologically at high risk, but importantly, also the less ill patient with suggestive symptoms who fails to meet all diagnostic criteria but are in an at-risk group. High morbidity and mortality has been reported for undiagnosed and untreated cases.
P955: Dressing changes under laminar flow conditions to prevent Staphylococcus aureus wound colonisation in patients admitted to a burn centre
A.M.D. Kooistra-Smid, M.K. Nieuwenhuis, E. van Zanten, J. Hiddingh, S.R. van Dijk, G.I.J.M. Beerthuizen, W.H.M. Vogels, A.A. van Zwet, H.A. Verbrugh (Groningen, Rotterdam, NL)
Objectives: Staphylococcus aureus colonization and infection of burn wounds increases morbidity and delays wound healing of patients suffering from burn wounds. A vulnerable moment in the route of transmission of S. aureus is the exposed burn wound during dressing changes. The aim of this study was to evaluate the effect of dressing changes under laminar flow conditions on burn wound patients with regard to S. aureus colonization.
Methods: From the first of February 2003 to the first of June 2003, 25 patients were included in this study at our 10-bed burn centre. In 12 of these patients the dressings were changed under laminar flow conditions. All patients were frequently screened for S. aureus in nose, throat and burn wounds. All S. aureus isolates were genotyped with Pulsed Field Gel Electrophoresis.
Results: At admission 17/25 (68%) patients had no S. aureus colonization in their nose, throat or burn wounds. Dressing changes under laminar flow conditions were carried out on 8/17 patients of this group. However, 6/8 (75%) patients acquired burn wound colonization with S. aureus during their stay at the centre. Six out of 9 patients (67%) whose dressing changes were not carried out under laminar flow conditions acquired burn wound colonization with S. aureus. A total of 12 patients acquired burn wound colonization; these patients also acquired carriage of S. aureus in nose or throat. The same type of S. aureus was carried in the nose or throat as well as the burn wounds in 7 (58%) of these patients.
Conclusion: The results of this study suggest firstly that dressing changes under laminar flow conditions does not prevent colonization of burn wounds with S. aureus, and secondly, that the exogenous route plays an important role in the transmission dynamics of this pathogen in burn wound centres. Future research should be focused on this mode of transmission of S. aureus in this special circumstance.
P956: Mupirocin prophylaxis to prevent Staphylococcus aureus wound colonisation in patients admitted to a burn centre
A.M.D. Kooistra-Smid, S.R. van Dijk, G.I.J.M. Beerthuizen, W.H.M. Vogels, A.A. van Zwet, H.A. Verbrugh (Groningen, Rotterdam, NL)
Objectives: Staphylococcus aureus (S. aureus) colonisation of burn wounds increases morbidity and delays wound healing. Many burn wound colonisations with S. aureus are endogenous in nature. The aim of this study was to evaluate the effect of eradication of nasal S. aureus with mupirocin in patients with regard to S. aureus colonisation of their burn wounds.
Methods: From September 2000 to March 2001, 42 patients admitted to our 10-bed burn centre were screened for S. aureus in nose and burn wounds. Isolates were genotyped with PFGE. All patients received nasal mupirocin at the time of admission to the burn centre. Fifty-five patients from the same unit who were followed from September 1997 till May 1998 and had not received mupirocin prophylaxis served as a historical control group.
Results: At admission 29/42 (69%) patients in the mupirocin trial had no S. aureus colonisation in their burn wounds. Of this group 25 patients were non-carriers and 4 patients were nasal carriers of S. aureus. Seven (28%) non-carriers and 2 (50%) nasal carriers acquired burn wound colonisation with S. aureus during their stay at the centre. Of the historical control group, 39 (71%) patients had no S. aureus colonisation of their burn wounds at the time of admission. Of this group 31 patients were non-carriers and 8 patients were nasal carriers; 18 (58%) non-carriers and 7(88%) nasal carriers acquired S. aureus wound colonisation during their stay. The overall probability of wound colonisation in the patients treated with mupirocin was significantly lower than in the historical non-treated group (p = 0.01, chi-square test with Yates correction).
Conclusion: The results of this study suggest that application of nasal mupirocin to all patients upon admission to a burn centre may reduce but not eliminate the risk of subsequent S. aureus colonisation of burn wounds. Other measures including improved infection control practices and eradication of exogenous S. aureus reservoirs, including S. aureus carriage among healthcare workers, may be necessary to further reduce the incidence of S. aureus burn wound colonisation.
P957: Controlling an outbreak of Staphylococcus aureus on a surgical ward
P.E.M. Haanen, M. van der Bijl, P.H.M. Savelkoul, E.R. van der Vorm (Amsterdam, NL)
Objectives: In February 2004 an increase of S. aureus infections was recognized on a surgical ward of the VU medical centre. Also, two healthcare workers (HCW A and B) on that ward appeared to have skin problems. After this observation, cultures were taken and HCW A and B were relieved from patient contact. The cultures were positive with S. aureus. The outbreak was characterised and the S. aureus infections were monitored by means of molecular surveillance.
Methods: From February until June 2004 the S. aureus strains were collected from clinical and policlinic patients from the surgical ward. The strains were characterised and compared by Amplified Fragment Length Polymorphism (AFLP).
Results: The characterisation of the S. aureus in February showed a cluster of identical strains in three patients and HCW A. The strains of two patients were similar to the strain of HCW B. Three patients had a unique strain. In the surveillance period a total of eighteen isolates in sixteen patients were found. In the surveillance period the epidemic-strains were found in other patients but only in patients who have been on the ward during the epidemic period. Two patients had an identical new isolate. That indicates that the exchange between patients of S. aureus may occur without notion. Another remarkable observation was that some of the patients lost their original strain and acquired a new isolate of S. aureus during hospitalisation.
Conclusions: A small outbreak of S. aureus could be traced to 2 HCW who proved to be carriers. Relieving them from patient contact stopped the outbreak. Molecular surveillance is an appropriate way to evaluate the success of measurements taken and to underscore the importance of hygienic measures.
P958: Risk factors for S. aureus carriage in health care workers
A. Widmer, M. Lang, R. Frei (Basel, CH)
Introduction: S. aureus (MSSA) carriage is common among health care workers (HCWs)and might be associated with type of care provided and other potential risk factors. Transmission of MSSA has been observed by “cloud adults”. Objectives: To determine risk factors for MSSA carriage in HCWs, and the percentage of methicillin-resistant S. aureus (MRSA) in a tertiary care centre.
Methods: Retrospective review of all data of staff health department and the microbiology laboratory. All HCWs who were working in a high MRSA prevalence country were routinely screened at the time they were hired by the institution. In addition, data were generated from MRSA screenings of HCWs if there was evidence for nosocomial transmission of MRSA in patients. MRSA was defined as S. aureus being oxacillin-resistant and expressing the PBP2’ and/or being positive for the mecA gene by PCR. Data of HCWs were collected by chart review in a case-report form that included demographic data, work place, skin diseases and other variables. Data were compared by univariate and multiple logistic regression analyses.
Results: A total of 3474 swabs were taken from 1217 HCWs between Jan 1997 and Dec.2001. Data were available from 1182 HCWs:50% originated from Switzerland, 27% from Germany, 4% from France, and 19% from other countries. The overall prevalence of MSSA and MRSA was 53% and 1%, respectively. More than one sample was available from 332 individuals: Of the repeat samples, 38% were negative, 32% were negative, but had one single positive culture, and 30% were consistently positive. Sex, profession, work place, number of years at the institution was not associated with S. aureus carriage (p > 0.2). The only significant risk factor for S. aureus carriage was young age, defined <35years (p = 0.02). The prevalence of MSSA increased from 51% (1997) to 63% (2001). Eight HCWs were carriers of MRSA: they were young and half of the them reported skin diseases.
Conclusion: S. aureus carriage among HCWs is common: Only young age remained a risk factor even after adjusting for other variables. MRSA was rare among HCWs.
P959: Prevalence of nasal carriage of methicillin-susceptible and methicillin-resistant Staphylococcus aureus among hospital personnel and outpatients
St. Fokas, Sp. Fokas, C. Tsamolia, M. Skoutari (Eghio, GR)
Objectives: To assess the nasal colonization of Staphylococcus aureus among hospital staff in the absence of an epidemic and to compare it with the nasal carrier status among outpatients, focusing on the MRSA rate.
Methods: The study included 150 hospital personnel and 150 adults admitted to outpatient clinics of our hospital. Given that a history of hospitalization is the most important facilitative factor for colonization of Staphylococcus aureus we exclude individuals with a history of hospitalization in the preceding year of our study. The specimens were obtained with swabs from the anterior nares-ecological niches of S. aureus- and cultured according NCCLS guidelines. ID 32 STAPH strips were used for identification and confirmed with Slidex Staph Plus kit (both by biomerieux). MRSA strains detection was achieved with Slidex MRSA Detection kit of the same company. Antibiotic susceptibility of MRSA strains was determined with ATB STAPH method (version 2000) according to the recommendations of the producer (biomerieux).
Results: Among hospital staff the carriage rates of MRSA and methicillin susceptible S. aureus were 2.7% and 20% respectively. None of the outpatients was found to be a nasal carrier of MRSA. In addition MSSA carriage in this group was 11%. The prevalence of MRSA nasal carriage rate among personnel working in the different medical wards was also examined. The difference in the rates among personnel working in the surgical ward, operating theaters and the rest of the staff was statistically significant (p < 0.001). All MRSA strains were susceptible to oral antibiotics.
Conclusions: Although the prevalence of MRSA is low among hospital personnel, education is needed as they are one of most important reservoirs for nosocomial MRSA infections. The low incidence of MRSA infections around the time of the study suggests that with usual infection control practices MRSA spread was avoided. All MRSA carriers were treated with intranasal muripocin for eliminating the nasal carrier status. Continuous monitoring of MRSA carriage is needed to avoid nosocomial spread.
P960: Understanding the Staphylococcus aureus nasal colonisation of HIV outpatients based on DNA genotyping
M.C. Padoveze, R. Pedro, D. Blum-Menezes, O.J. Bratfich, M.L. Moretti (Campinas Sao Paulo, BR)
AIDS patients are a special population related with high risk of infection due to Staphylococcus aureus. Previous colonization is a recognized predisposing factor for development of infection due to this organism. However, nasal carriage of S. aureus in HIV-patients is still not completely characterized.
Objectives: To describe the epidemiological features of community-acquired S. aureus nasal colonization in out care HIV-patients based on the molecular genotypes.
Methods: HIV-outpatients without previous hospitalization within the last two years were screened for S. aureus nasal colonization. Three samples from each patient were collected, and the variables associated with colonization were assessed. Nasal carriage was classified as: absent, transient colonization or persistent colonization. The persistent colonization was assessed according to the molecular profiles performed by Pulsed-Field Gel Electrophoresis, in: simple (same profile), multiple (different profiles) or combined (two with the same e and one with different profiles).
Results: 111 patients were enrolled in the study. Seventy patients (63%) had at least one culture positive for S. aureus and 99 patients concluded three samples collection. Only one isolate was a community acquired MRSA. The rates of colonization was higher when two or more samples were taken, ranging from 45.5% in the first sample up to 65.6% when 3 samples were collected. HIV-patients with AIDS were more likely to be colonized than non-AIDS patients (p=0.02). Among the patients with S. aureus nasal carriage, 39% were transient and 61% were persistent carriers, whose genomic subtype was: 61.5% simple, 20.5% combined and 18% multiple persistent colonization. Previous use of antibiotics was associated with absence of S. aureus colonization (p < 0.05).
Conclusions: HIV out care patients had high rates of oxacillin-susceptible S. aureus nasal colonization. Regardless, the recent literature, only one isolate was community-acquired MRSA. The most common characteristic of colonization is simple persistent colonization showing the same genomic profile.
P961: S. aureus bacteraemia: prospective study of 238 cases (2000–2003)
R. Baños, J. Gómez, E. García Vázquez, J. Ruiz, J.A. Herrero, V. Baños, M. Canteras, M. Valdés (Murcia, E)
Objectives: S. aureus bacteraemia (SAB) continues to be a major problem related to both community-acquired and nosocomial infection. We undertook an evaluation of a large cohort of patients with SAB to assess features of the infection and predictors of mortality.
Patients and Methods: 238 cases of SAB admitted to our hospital (2000–3) were prospectively studied. All patients had at least one positive blood culture for S. aureus and clinical symptoms of bacteraemia. SAB was considered to be nosocomial if the first positive blood culture specimen was obtained > 72 h after admission and there was no clinical evidence of infection on admission. Microbiological studies were carried under standard protocols. Epidemiological and clinical characteristics, antimicrobial treatment and outcome (relapse or mortality) were analysed.
Results: 434 cases of SAB were identified but only 238 were prospectively included in the study protocol. Incidence was the highest in year 2001 (4.21 per 1000). Out of the 238 cases, 167 (70%) were male with a mean age of 51 year (SD 24.89). Mean length of stay was 30.34 days (SD 29.54); 165 (69.3%) cases were nosocomial. Distribution of patients according to Wards was 46.2%, 24.8%, 20.2% and 8.4% in medical wards, surgical wards, intensive care unit and paediatric ward, respectively; 92.9% of the cases had an underlying disease; 52% of the patients developed complications; a primary origin of the bacteraemia was not identified in 37% cases; 35.7% occurred in patients with IV catheters and 16% had a cutaneous origin. 85 cases (35.7%) were due to MRSA. Overall, treatment was inadequate in 56%% of patients (rate of treatment inadequacy 63.3% in SAMS cases and 42.3% in SMAR bacteraemia). Overall, 44 (18.4%) of the 238 patients with SAB died during hospitalisation. Mortality in patients with SAMR bacteraemia was 34.11% versus 9.8% in patients with SAMS bacteraemia.
Conclusion: The knowledge of clinical and epidemiological factors of patients with SAB may allow to optimize its management and to reduce morbidity and mortality.
P962: Detection and interpretation of macrolide-lincosamide-streptogramin resistance among Staphylococcus with Phoenix Automated Microbiology System and BDXpert™ System
B. Turng, J. Sinha, M. Deal, J. Pollitt, D. Callihan, B. Brasso, T. Wiles, J. Reuben (Sparks, USA)
Objectives: The National Committee for Clinical Laboratory Standards (NCCLS) recently published recommendations for the detection of macrolide-lincosamide-Streptogramin (MLSb) resistance in Staphylococcus. These statements provide guidelines for laboratorians to detect the MLSb resistance phenotypes in macrolide resistant staphylococci. The Societe Francaise De Microbiologie (SFM) and Deutsches Institut fur Normung (DIN) have not yet implemented similar guidelines. This study evaluated the detection and reporting of MLSb results in Staphylococcus using the BD Phoenix™ Automated Microbiology System and BDXpert System with NCCLS, SFM or DIN as interpretative standards.
Methods: Comments regarding MLSb resistance as listed in the NCCLS M100–S14 were converted into expert rules. Special BDXpert rules were also constructed for the detection and reporting of MLSb resistance when applying SFM or DIN guidelines. A total of 177 strains of Staphylococcus (146 S. aureus, 12 S. epidermidis, and 19 coagulase-negative staphylococci) were tested in Phoenix panels containing erythromycin (E) and clindamycin (CC). NCCLS, SFM or DIN breakpoints were used to interpret the Phoenix MIC results. The double disk diffusion D-test (E and CC) was used as the reference method for the determination of MLSb resistance phenotypes.
Results: The Phoenix E and CC MIC values were interpreted based on the standard selected. The BDXpert rules were executed and applicable expert messages were displayed. The Phoenix correctly detected 38 out of 43 constitutive MLSb (cMLSb) phenotypes as compared to the D-test results. The remaining 5 cMLSb strains were interpreted by the BDXpert as potential inducible MLSb (iMLSb)/efflux phenotypes. A total of 69 iMLSb and 22 efflux phenotype isolates were all reported by the BDXpert
as iMLSb/efflux phenotype and the users were alerted to perform D-test before reporting the CC results. The CC interpretation was suppressed in these isolates. The NCCLS, SFM, or DIN showed identical detection and interpretation of MLSb resistant phenotypes by the Phoenix and BDXpert systems.
Conclusions: The Phoenix and BDXpert Systems can assist laboratories in rapid detection and accurate interpretation of MLSb results for Staphylococcus. Special messages can be used to communicate timely and accurate information to clinicians for proper therapy of staphylococcal infections with MLSb resistant phenotypes.
P963: In vitro activity of new compounds tested against multi-drug resistant S. aureus isolated in Latin American medical centres
A. Gales, H. Sader, D. Biedenbach, P. Strabala, R. Jones (Sao Paulo, BR; North Liberty, USA)
Background: Oxacillin-resistant S. aureus (ORSA) isolated in LAMCs shows high rates of co-resistance (R) with most antimicrobial classes used in the clinical setting. We evaluated the MDR patterns of ORSA strains collected in LAMC by the SENTRY Antimicrobial Surveillance Program in 2003. We also evaluated the susceptibilities (S) of new, investigational compounds against these important endemic pathogens.
Methods: Among 1.437 S. aureus collected, 507 (35.3%) were R to oxacillin. These strains were isolated from 10 LAMCs (5 countries) and tested against > 30 antimicrobials by NCCLS broth microdilution methods. ORSA strains were grouped by the MDR patterns for the 8 primary drugs (47).
Results: The MIC50 in mg/L/% S for the primary drugs were: erythromycin (ERY) > 8/8; clindamycin (CC) > 8/13; ciprofloxacin (CIP) > 8/8; tetracycline (TC) ≤ 4/61, co-trimoxazole (T/S) > 2/49, chloramphenicol (CHL) 16/47, rifampin 2/48, gentamicin (GM) > 8/14; and newer agents were: daptomycin (DAP) 0.5/100, dalbavancin (DAL) 0.06/-, linezolid (LZD) 2/100, quinupristin/dalfopristin (Q/D) 0.5/100, teicoplanin (TEI) ≤ 2/100 and vancomycin (VAN) 1/100. Table shows 6 MDR-ORSA patterns (77.5% of all ORSA):
| Pattern (no.) | R antibiogram | Geographic distribution (%) |
|---|---|---|
| 1 (126) | All primary drugs | Brazil (82%) |
| 2 (6) | CHL, CIP, CC, ER, GM | Chile (66%) |
| 3 (65) | CIP, CC, ER, GM | Argentina (51%). Brazil (48%) |
| 4 (51) | All, except CHL | Brazil (75%) |
| 6 (48) | All, except TC | Brazil (100%, 75% one site) |
| 6 (37) | CIP, CC, ER | Mexico (86%) |
Conclusions: All newer compounds (LZD, Q/D, DAP and DAL), TEI and VAN were very active against endemic and epidemic ORSA in LAMCs. These S. aureus having MDR patterns (ave. R to 6 agents) will require greater use of newer compounds particularly in Brazil.
P964: VGA-gene is responsible for the low-level resistance to quinupristin-dalfopristin among staphylococci in Greek hospitals
E. Petinaki, M. Maniati, Z. Bersos, V. Chini, A. Foka, A.N. Maniatis, I. Spiliopoulou (Larissa, Patras, GR)
Objectives: Quinupristin-dalfopristin (Q–D) is widely used for the treatment of infections caused by gram-positive cocci, except Enterococcus faecalis. Despite the prolonged use of streptogramins in animal husbandry, a limited number of staphylococcal isolates were found to be non susceptible worldwide. The purpose of this study was to investigate the rates of resistance among staphylococci to this agent in Greece, after a three year period of usage in our hospitals.
Methods: A total of 846 staphylococci (250 S. aureus and 596 coagulase-negative staphylococci, CNS) recovered from clinical specimens of different patients in two tertiary care Greek hospitals (University Hospital of Larissa, University Hospital of Patras) during 2003–2004 were investigated for their resistance to quinupristin-dalfopristin (breakpoints for susceptibility < = 1 mg/L, resistance >4 mg/L). Identification at species level was performed by Gram stain, catalase and coagulase production, and by the API Staph system. Susceptibility to various antimicrobial agents including Q-D was assessed by disk the diffusion method. Determination of MIC to Q-D was performed by the E-test and agar dilution method. Isolates with MICs greater than 1 mg/L were examined for the presence of vatA, vatB, vatC, vga, vgaB, vgb, vgbB genes by Polymerase Chain Reactions. The clonality of isolates was studied by PFGE of chromosomal SmaI DNA digests.
Results: All S. aureus isolates had MICs ranging from 0.19 to 0.75 mg/L (mean value: 0.25 mg/L). Among the CNS, 579 isolates expressed MICs between 0.125-1 mg/L (mean value: 0.33 mg/L), while 17 isolates had MICs that ranged from 1.5 to 4mg/L. All these 17 isolates, including one S. haemolyticus, one S.capitis, and fifteen S. epidermidis were vga-positives and expressed MLSB phenotype carrying the ermC-gene.
Conclusions: The presence of vga-gene, conferring resistance to streptogramin A by a putative efflux mechanism is responsible for the non-susceptibility of staphylococci to quinupristin-dalfopristin in Greece.
P965: Dynamics of nasopharyngeal colonisation by coagulase-negative staphylococci in patients with resectable lung cancer during short-term hospitalisation
A. Malm, M. Juda, R. Los, M. Sawicki, F. Furmanik (Lublin, PL)
Objectives: Coagulase negative staphylococci (CoNS) represent a part of physiological microflora. However, in recent years, they have also emerged as nosocomial pathogens of infections associated with indwelling medical devices (e. g. pleural drains), mainly in immuno-compromised patients. The aim of this study was to determine dynamics of nasopharyngeal colonization by CoNS in patients with resectable lung cancer during short-term hospitalization, especially those receiving routinely preoperative antimicrobial prophylaxis.
Methods: In present study CoNS species were selected from patients divided into two groups: (I) patients who were undergoing pulmonary resection and receiving preoperative prophylaxis (piperacillin, cefuroxime alone or in combination with amikacin) - ‘prophylaxis’ group and (II) control group. Throat and nasal specimens were taken from each patient twice, in four-days interval. All isolates were identified by the biochemical microtests API STAPH (bioMerieux) and tested for drugs susceptibility according to NCCLS reccomendations.
Results: 187 strains of CoNS strains were selected from clinical specimens: 137 strains from ‘prophylaxis’ group and 50 strains from control group. The most often isolated species was Staphylococcus epidermidis with the predominated API numerical profile 6606113. A detailed analyses of the API numerical profiles and resistance to antimicrobial agents indicated that during four-days interval of hospitalization, changes in phenotypes among CoNS colonizing nasopharynx were observed in both groups of patients. The changes in drug resistance patterns were found more often in ‘prophylaxis’ group compared to those in control group – 48/54 (88.9%) and 11/22 (50%), respectively. This difference was statistically significant (p = 0.0007 – Chi2 test with Yates correction).
Conclusion: Our data suggest that preoperative antimicrobial prophylaxis routinely used in patients with resectable lung cancer may be regarded as an important factor predisposing to changes in drug resistance patterns among CoNS isolates colonizing nasopharynx.
P966: The susceptibility of coagulase-negative staphylococci in a teaching hospital compared with a secondary care hospital
J.H. Sloos, L. Dijkshoorn, N.M. Bax, A.T. Bernards, E. van Strijen, P.H. van den Broek (Alkmaar, Leiden, NL)
Objectives: To compare the susceptibility of coagulase-negative staphylococci (CoNS) for teicoplanine (T) and vancomycine (V) in two hospitals, the Leiden University Medical Center (LUMC) and Medical Center Alkmaar (MCA), in which these antibiotics are respectively the first choice antibiotics in serious infections with these species.
Methods: Antibiotics tested were T, V, ciprofloxacin (C), moxifloxacin (M), levofloxacin (L), and linezolid (Li). Collections I comprised 44 isolates and were from the LUMC, whereas collection II comprised 27 isolates from the MCA. Susceptibilities were determined by agar dilution on Mueller Hinton agar.
Results: In total, six different species were identified in 71 isolates, 72% of which were Staphylococcus epidermidis. In the LUMC the species diversity was greater than in the MCA, with five isolates of Staphylococcus haemolyticus found in the first. No difference between the two hospitals was found in activity of the antibiotics tested, except for Li. The MIC90s were as follows: V 2 mg/L, T 4 mg/L, C 16 mg/L, M 2 mg/L, L 8 mg/L. Of Li the MIC90 was 2 mg/L in the LUMC and 1 mg/L in the MCA. According to Dutch guidelines, in total 7/71 isolates were found resistant to T and 21 intermediate resistant. All isolates were susceptible for V.
Conclusion: The first choice glycopeptide for serious CoNS infections, T or V, has no influence on the susceptibility of CoNS for these antibiotics. According to Dutch guidelines, the activity of T, C, and L against CoNS is relatively low, whereas the activity of M and Le is in the susceptible range.
P967: Characterisation of biofilm-forming Staphylococcus epidermidis clinical isolates
D. Petrelli, C. Zampaloni, L.A. Vitali, M. Prenna, S. D'Ercole, M.S. Pasquantonio, S. Ripa (Camerino, I)
Objective: Staphylococcus epidermidis is one of the bacterial species mainly implicated in foreign body associated infections. We have characterized several S.epidermidis clinical isolates for their ability to form biofilms and their resistance to antibiotics.
Methods: 76 S.epidermidis strains isolated from implantable medical devices have been collected from hospitals of Central Italy. Susceptibility to penicillin, methicillin, erythromycin and tetracycline has been determined in vitro by E-test according to NCCLS guidelines. The specific antibiotic resistance determinants have been checked by PCR (blaZ, mecA, ermA, ermB, ermC, msrA, tetK and tetM). The ability to form biofilms has been determined: (i) by PCR, detecting genes specific for attachment and biofilm development (icaADBC operon, aap, and atlE); (ii) by Congo Red Agar (CRA) plate test to assay the production of polisaccaridic intercellular adhesin (PIA); (iii) by crystal violet (CV) stain to determine the biofilm biomass development on polystyrene microtiter plates; (iv) and by CSLM microscopy observations to investigate biofilm structure.
Results: 94% of the strains under study was resistant to penicillin, 87% to methicillin, 72% to erythromycin and 25% to tetracycline. On the side of biofilm-specific genes detection, 66% of strains was positive to ica operon genes, 82% possessed atlE gene, and 42% aap determinant. In 89% of the population, the CRA test confirmed the correlation between the presence of ica genes and slime expression. The CV assay classified the quasi-totality of our strains (97%) as biofilm producers on plastic surface. In addition, the distribution of optical density values (OD540) obtained after CV stain, showed a significant statistical difference in biofilm biomass development between the ica-ADBC-positive strains and the icaADBC-negative ones. Finally, a correlation, although not always present, has been observed between ability of the strains to develop in a high-structureted biofilm and specific biofilm-formation determinants.
Conclusions: The investigated bacterial population shows a very high and alarming level of resistance to all tested drugs. Although the specific determinants for biofilms formation are not always present, nevertheless all the strains are able to develop in sessile form showing that different and not still identified factors could work together in the formation and organization of staphylococcal complex microbial communities.
P968: Genetic relatedness of coagulase negative staphylococci in sternal wound colonisation and sternal wound infection after open heart surgery
C. Balmelli, R. Hysenai, G. Senn, M. Spiess Pangrazzi, E. Schmid, M. Turina, C. Ruef (Zurich, CH)
Objective: Coagulase-negative staphylococci (CoNS) are frequently isolated in sternal wound infections (SWI) after open heart surgery. Our study had two principal aims. First, to establish the source and route of transmission of staphylococci found in SWI and sternal wound colonization during interventions under laminar flow ventilation (LVF). Second, to assess the source of strains found in the ultra clean area (UCA) and to define the role of airborne transmission.
Methods: Prospective evaluation of 50 patients undergoing elective open heart surgery. Swabs of noses and hands of HCW involved in patient care. Swabs of noses and sternal skin of patients before interventions. Three air samples done during each intervention in the vicinity of the surgical site. Genotyping of all 2413 cultured isolates of CoNS using pulsed field gel electrophoresis (PFGE).
Results: Two out of 50 patients developed SWI, one infection was caused by CoNS and needed surgical revision, the second was caused by coryneform bacteria. PFGE showed that the CoNS originated from the hands of a supporting staff member (SSM) who shaved the patient just before intervention. Another CoNS strain was found in the same wound during revision, and was traced to another SSM who took care of the patient just before reintervention.
Five out 50 patients had intraoperative sternal wound colonization with CoNS. None of these CoNS genotypes were observed among isolates from patients, HCW or from the air. Most air samples showed <10 CFU/m3. 17/216 (8%) of CoNS isolates from the air could be traced to HCW or patients, among which 50% originated from the non-scrubbed team.
Conclusions: Analysing the origin of colonization or infection in 6 patients with CoNS isolated from the operative site, the bacteria could only be traced in one patient who developed an infection. Transmission most probably occurred by direct contact. The low level of bacterial contamination in the UCA together with the lack of correlation of genotypes between isolates found in the UCA and in the wounds suggest that airborne transmission does not play a major role in the development of SWI. More than 90% of staphylococci found in air samples were not traceable to any investigated sources. Most probably, they originated from non swabbed parts of the HCW's bodies. Since 50% of the traceable isolates from the UCA originated from non scrubbed team members, protection of the operative site by LFV appears to be suboptimal.
P969: Clonality of endemic methicillin-resistant Staphylococcus epidermidis strains isolated in a neonatal intensive care unit
N. Ben Saida, A. Ferjani, N. Sfar, J. Boukadida (Sousse, TN)
Objectives: Methicillin-resistant staphylococcus epidermis (MRSE) is one of the important pathogen responsible for nosocomial infections particularly in newborns. The aim of our study was to establish if these infections are caused by endemic clones or by incidentally occurring bacterial strains of this ubiquitous species and to evaluate the performance of PCR iner-IS256 as a novel method for typing MRSE strains using pulsed-field gel electrophoresis (PFGE) as the reference method.
Methods: Twenty strains of MRSE (mecA+) has been collected during the period of survey (december 2003 to september 2004) from different pathological products of newborns hospitalized in a neonatal intensive care unit of a public maternity hospital in Sousse, Tunisia. Identification of strains was done by conventional procedures and the Api staph (Api-biomerieux. Sa). Susceptibility testing to antibiotics was determined according to CA-SFM recommendations. All strains have been characterized by genotypage in pulsed-field gel electrophoresis (PFGE) variety CHEF after SmaI macrorestriction. Genomic profiles have been interpreted according to criteria of Tenover (J. Clin. Microbiol 1995; 33:2223–2239). Strains were also characterized by electrophoretic profiles obtained by PCR-based analysis of inter-IS256 spacer polymorphisms.
Results: These MRSE represent 41.6% of the total strain of S.epidermidis collected from the neonatology ward during the period of survey. Majority of these strains come from blood sample (75%), other strains from vascular catheter (5%), pus (10%), sound (10%). 17 antibiotypes and 6 genotypic profiles according Tenover criteria were individualized: type A (with 5 subtypes), type B, type C (with 1 subtypes), type D (with 1 subtypes), type E (with 2 subtypes)and type F. A total of four PCR patterns were obtained based on the interpretation criteria that PCR patterns exhibiting more than one band difference were considered to represent distinct types, type 1, type2, type3, and type4.
Conclusion: MRSE appear to be endemic and multiclonal with a dominant clone in the neonatal intensive care unit. Our study demonstrates that a significant proportion of MRSE infections may be attributable to transmission among newborns and that certain strain can become endemic over long periods in this setting.
P970: Clonality of Staphylococcus haemolyticus strains isolated in a neonatal intensive care unit
N. Ben Saida, A. Ferjani, J. Boukadida (Sousse, TN)
Objective: Methicilllin-resistant Staphylococcus haemolyticus (MRSH) was increasingly important nosocomial pathogens particularly in critically ill neonates. The aim of our study was to establish if these infections are caused by endemic clone or by incidentally occurring bacterial strains of this species.
Methods: Thirteen strains of MRSH according CA-SFM recommendations and mecA+ (Murakami K. J.Clin.Microbiol 1991, 29:2240–4) has been collected during the period of survey (april 2004 to october 2004). Eleven strains come from different pathological products of newborns hospitalized in a neonatal intensive care unit of a public maternity hospital. Tow strains come from paediatric and internal medicine wards were used as control to ensure that endemic strains can be differentiated from outbreak strains. All strains were identified with the Api-staph method (Api bioMerieux). Strains have been characterized by genotypage in pulsed-field gel electrophoresis (PFGE variety CHEF) after SmaI macrorestriction. Genomic profiles have been interpreted according to Tenover criteria (J.Clin.Microbiol.1995; 33 :2223–2239).
Results: S. haemolyticus was quantitatively the second staphylococci (23.6 %) after S. epidermidis isolated in neonatology ward. MRSH represent 85. 7 % of the total strains of S. haemolyticus collected from the neonatology ward during the period of study. The majority of the strains come from blood sample 7 (63.63%), 4 (36.36%) from pus and 1 (9%) from CSF. Eight resistant antibiotyps profiles and 3 genotypic pattern according Tenover criteria were individualized: type A, type B (with 3 subtypes), and type C. The strains coming from paediatric ward present pattern type B3, but strains coming from internal medicine ward present distinct pattern.
Conclusion: MRSH is a major bacterium of nosocomial infection in neonatal intensive care unit. This bacterium is responsible as shown in our study, of endemic multiclonal nosocomial infections with a predominant clone.
P971: Staphylococcus haemolyticus bacteraemia in an intensive care unit
M. Galiè, P. Carfagna, F. Taglietti, O. Capelli, G. Testa, C. Santini (Rome, I)
Objectives: To analyse clinical and microbiological features of bacteremias due to S. haemolyticus (SHB) acquired in an ICU.
Methods: All SHB in a 8-bed ICU, from Jan 2003 to Aug 2004 were retrospectively evaluated.
Results: S. haemolyticus was isolated from 21% of all positive blood cultures and represented the 37.9% of the coagulase negative staphylococci. Twenty-nine cases of SHB occurred during the study period (5.6 episodes per 1000 patients-days). All cases were hospital-acquired and occurred after a mean hospitalisation of 24.5 days. The mean age was 68.4 years (range 20–90) and 16 patients (55.2%) were males. Twenty-eight patients (96.5%) had a central venous catheter (cvc). All patients received previously antimicrobial therapy. Thirteen patients (44.8%) had polymicrobial bacteraemia. In 18 cases (62.1%) the source of bacteraemia was the cvc. All isolates were resistant to oxacillin and gentamicin, 94.3% and 34.3% were resistant to ciprofloxacin and teicoplanin, respectively; all strains were susceptible to vancomycin. Sixteen patients (55.2%) had sepsis, 3 (10.3%) severe sepsis, and 7 (24.7%), all polymicrobial, septic shock.; in 3 patients (10.3%) SHB had no clinical significance. Twenty patients died (69%) and deaths were directly related to SHB in 1 patient (3.4%), and partially related in 2 (6.8%). Nine patients (31%) survived. The patient who died for SHB, developed a persistent cvc-related bacteraemia after a 6-week course therapy for streptococcal endocarditis. S. haemolyticus become resistant to teicoplanin during a teicoplanin-based therapy and the patient died 47 days after the onset of bacteraemia. The 2 patients, in which death was partially related to SHB, had a polimicrobial bacteraemia due to C. tropicalis and Enterococcus spp, respectively, and died after 22 and 6 days respectively, for septic shock, during adequate therapy. Among the 17 patients in which death was not related to SHB, 15 (88.2%) received adequate therapy that cleared the blood cultures, 2 patients improved after the removal of cvc without antimicrobial therapy.
Conclusions: S. haemolyticus is an emerging pathogen, responsible of sepsis, frequently cvc-related; most of strains are resistant to many antistaphylococcal agents currently used as empiric therapy, thus constituting a clinical concern. Nevertheless, this pathogen shows a low virulence and is associated with a low related mortality, probably representing a marker of severe underlying diseases.
P972: Staphylococci from the skin of patients: changes associated with treatment by isotretinoin
A. Thomas, R. Williams, N. Hepburn, T. Watts, R. Dixon (Lincoln, UK)
Objectives: Isotretinoin, a retinoid has been used to treat patients with moderate to severe acne despite the adverse effects of mucosal surface drying and the contraindication of use during pregnancy. In clinical practice, patients are frequently prescribed systemic isotretinoin because they have not responded to previous treatment with oral or topical antibiotics. Broad-spectrum antibacterial therapy has nevertheless promoted changes in the diversity and antibiotic resistance status of the patients’ skin microbiota and we are studying the effect of isotretinoin on these changes.
Methods: The present study investigated the recovery and analysis of skin organisms from 53 patients (mean age 23 y range 15–37y) before, during and after treatment with a 16-week course of isotretinoin (1 mg/kg body weight). The number of aerobic bacterial isolates (presumptive Staphylococci) recovered from Baird-Parker agar from each of three specific sites per patient were compared with age-matched controls of healthy volunteers.
Results: Both patients and controls had generally similar numbers of organisms on the nares, cheek and toe webs before treatment, whereas all patients showed a significant reduction in Staphylococci recovered from one site during and after 16 weeks of isotretinoin treatment. The majority of the patients had a greater reduction (1–2 log) for the cheek site than either nares or toe webs both of which showed minimal reduction.
Conclusions: Preliminary results from this study show a pronounced reduction in the number of presumptive staphylococci recovered from the treated group immediately following isotretinoin compared to untreated controls. Since isotretinoin has little known antibacterial activity against the Staphylococci the observed reductions would suggest that the effect is mediated through changes in the skin nutritional micro-environment.
Mechanisms of resistance in staphylococci
P973: Effect of erythromycin on the selection of linezolid resistance in hypermutable and clinical isolates of Staphylococcus aureus
S.E. North, M.J. Ellington, A.P. Johnson, D.M. Livermore, N. Woodford (London, UK)
Objectives: Emergence of mutational resistance to linezolid (lin) in Staphylococcus aureus has been associated with loss of erythromycin resistance methylase (erm) genes, both in vivo and in vitro. We tested the general validity of this claim, and examined whether the emergence of lin resistance is delayed in the presence of ery.
Methods: Six lin-susceptible S. aureus strains were used: 2 genetically-related, ery-resistant (ermC) and susceptible pairs of EMRSA-15, also the isogenic pair RN4220 and its hypermutable RN422mutS mutant, which harbours ermB. In 4 replicated experiments, ery-susceptible and ery-resistant isolates were grown on agar containing increasing concentrations of lin. In addition, ery-resistant isolates were grown with 100 mg/L ery and increasing concentrations of lin. The number of days for isolates to develop the ability to grow in the presence of 6 mg/L lin was recorded. The absence of erm genes was checked by PCR; MICs of lin and ery were determined by agar dilution, and PFGE profiles of mutants were verified.
Results: Thirty-three mutants were obtained from the 4 experiments; 24 from the 4 clinical EMRSA-15 isolates, 3 from RN4220 and 6 from RN422mutS. Lin-resistance emerged more slowly in ery-resistant clinical isolates grown with lin and ery than with the same isolates grown with lin alone: mean 20 days (SD 26.8) to emerge on 6 mg/L lin versus 30 days (SD 18.4) in the presence of lin and ery. Growing the hypermutable strain, RN422mutS, in the presence of lin and ery did not delay the emergence of lin-resistance (11 days with SD 8.7, in either case). In the absence of ery selection, loss of erm with the emergence of lin-resistance was only noted for one EMRSA-15 isolate in 1 of 4 experiments. All isolates grown in the presence of ery retained erm determinants. Ery 100 mg/L did not supress growth of ery-resistant strains and linezolid was stable within the ambit of the long-selection experiments.
Conclusions: Growing the clinical isolates in the presence of ery and lin slowed the emergence of lin-resistance. This merits further study with lower, clinically-relevant concentrations of ery.
P974: In vitro selection of linezolid resistance in hypermutable and wild-type Staphylococcus aureus
S.E. North, M.J. Ellington, A.P. Johnson, D.M. Livermore, N. Woodford (London, UK)
Objectives: Resistance to linezolid (lin) is rare, but can arise via mutations in the 23S rRNA genes. We hypothesised (a) that resistance would emerge preferentially in staphylococci with a hypermutable phenotype engineered by mutations in the mutS gene, and (b) that hypermutability might be co-selected with linezolid resistance. MutS is part of the DNA mismatch repair (MMR) system, which identifies and corrects genome alterations post-replication, thereby influencing the net mutation rate.
Method: Linezolid-resistant (LinR) mutants of Staphylococcus aureus RN4220, its hypermutable mutS deletion mutant RN4220mutS, harbouring an erythromycin resistance marker gene (ermB), and a genetically-related pair of clinical isolates were selected by repeated passage with increasing concentrations of lin. Mutant parentage was confirmed by PFGE and susceptibility was tested by agar dilution. An amplified 694-bp fragment of 23S rRNA genes was studied by sequencing and by RFLP analysis. Frequencies at which LinR mutants yielded variants resistant to fusidic acid and rifampin were calculated in triplicate experiments.
Results: Seventeen LinR mutants (MICs 8–64 μg/ml) were raised. Ten mutants had a G2447T mutation in their 23S rRNA genes; 4, all from RN4220mutS, had G2576T, typically seen in LinR gram-positive cocci from the clinic; 1 had T2504C; 2 had no identifiable mutations. Curiously 5/7 RN4220mutS mutants lost ermB during the course of the experiment, reverting to macrolide susceptible. LinR mutants had mutation frequencies for rifampicin and fusidic acid resistance comparable with those of their parents (10–6 to 10–9), implying no co-selection of stable hypermutability.
Conclusion: More LinR mutants were obtained from the hypermutable (RN4220mutS) strain than from the wild type strain, and G2576T mutants were only obtained from the hypermutable organism. These data suggest hypermutability facilitates the emergence of LinR, nevertheless, LinR mutants derived from wild-type parents did not have elevated mutation frequencies.
P975: Disproving the link between expression levels of tcaA and mprF and clinical isolates of glycopeptide-intermediate Staphylococcus aureus
M. Wootton, R.A. Howe, P.M. Bennett, A.P. MacGowan, T.R. Walsh (Bristol, UK)
Objectives: The mechanism of resistance in Glycopeptide Intermediate Staphylococcus aureus (GISA) and hGISA isolates is unknown. However the inactivation of certain genes has been shown to confer an increase in glycopeptide resistance. Two genes, tcaA and mprF, when inactivated in GISA strains cause a reduction in glycopeptide MIC. Overexpression of tcaA causes an increase in teicoplanin susceptibility and so both genes may play a role in the development of glycopeptide resistance. This study aims to investigate the expression levels of tcaA and mprF in a set of GISA, hGISA and glycopeptide-susceptible S. aureus (GSSA).
Methods: RNA was extracted from the following: 1 set of clinically related (CR) GSSA and hGISA (LLA and LLE), 2 sets of CR hGISA and GISA (PC1 and PC3, LIM1 and LIM3) harvested during exponential phase growth (EX) and during exponential phase growth in the presence of sub-MIC levels of vancomycin (EXV). RNA was extracted from a further hGISA, Mu3 and GISA, Mu50 as well as 4 clinical GSSA strains. RT-PCR was performed with customised primers and the products visualised by electrophoresis. Band intensity was taken as indicative of mRNA quantity, and hence expression level, at time of cell harvest.
Results: The expression of tcaA is similar in all strains tested. Each strain within the related strain sets all show similar band intensities, despite differing glycopeptide resistance phenotype. Both Mu3 and Mu50 also exhibited similar expression levels to those found for all other GISA, hGISA and GSSA strains. Levels of expression were not affected by the presence of sub-MIC levels of vancomycin in any strain tested. Sequence analysis of tcaA in these strains showed no mutations present as previously thought. Expression levels of mprF were found to be strain specific. No difference in gene expression was found in the CR related strain sets.
Conclusions: No reduction in expression levels of tcaA and mprF were found to correlate with clinical strains exhibiting higher glycopeptide resistance. Thus it it uncertain what role tcaA ot mprF play with mediating glycopeptide resistance in Staphylococcus aureus.
P976: Strain-specific expression levels of pbp4 exist in isolates of glycopeptide-intermediate Staphylococcus aureus (GISA) and hGISA
M. Wootton, R.A. Howe, P.M. Bennett, A.P. MacGowan, T.R. Walsh (Bristol, UK)
Objectives: GISA and hGISA strains all have a characteristic thickened cell wall with reportedly fewer cross-links. Fewer peptidoglycan cross-links create increased D-ala-D-ala penta-peptide termini and hence more vancomycin targets. PBP4 has been shown to have both transpeptidase and D, D-carboxypeptidase activity, cleaving terminal D-alanine residues from un-cross-linked muropeptides. Reduced levels of PBP4 have been reported in laboratory-generated GISA mutants and a few clinical GISA strains. This study aims to investigate the expression levels of pbp4 in a set of GISA, hGISA and glycopeptide-susceptible S. aureus (GSSA).
Methods: RNA was extracted from the following: 1 set of clinically related (CR) VSSA and hGISA (LLA and LLE), 2 sets of CR hGISA and GISA (PC1 and PC3, LIM1 and LIM3) harvested during exponential phase growth (EX), after overnight growth (ON) and during exponential phase growth in the presence of sub-MIC levels of vancomycin (EXV). RNA was extracted from a further 8 clinically unrelated (CU) GISA (including Mu50), 8 CU hGISA (including Mu3) and 8 GSSA (EX). RT-PCR was performed with customised primers and the products visualised by electrophoresis. Band intensity was taken as indicative of mRNA quantity at time of harvest and hence gene expression.
Results: The expression of pbp4 varies according to strain. The band intensities of the related strain set LLA (GSSA) and LLE (hGISA) reduce slightly with increasing intermediate vancomycin resistance. However in two other CR hGISA and GISA (PC1/PC3, LIM1/LIM3) strain sets no variation in expression was observed. Both Mu3 and Mu50 exhibited lower pbp4 expression than any other strain, with the presence of sub-MIC levels of vancomycin reducing expression further. pbp4 expression was found to be reduced in 3 other GISA and 1 other hGISA, which showed lower band intensities than GSSA.
Conclusions: The reduced levels of PBP4 suspected to be associated with reduced susceptibility to vancomycin in S. aureus is not exclusive. The expression of pbp4 is reduced in Mu50 and 3 clinical GISA, as reported previously. However 5 other GISA strains exhibit pbp4 expression levels similar to GSSA isolates. Therefore pbp4 expression levels appear to be strain specific and a lowered expression level is not an essential requirement in the development of the GISA phenotype.
P977: Does vancomycin resistance emerge during the treatment of methicillin-resistant Staphylococcus aureus in respiratory tracts?
E.S. Kim, H.B. Kim, A. Huh, S.H. Eun, Y.S. Lee, B.N. Kim, J.W. Jeong, D.H. Whang, B.-M. Shin, B.S. Kim, M.-D. Oh, K. Choe (Goyang-si, Seoul, KOR)
Objectives: The prolonged use of vancomycin is known to be the most important factor in inducing vancomycin resistance to
S. aureus. Methicillin-resistant S. aureus (MRSA) colonizing in respiratory tracts might be chronically exposed to subtherapeutic concentrations of vancomycin because the level of vancomycin within pulmonary lining fluids was much lower than the concentration of serum. Despite the continuous use of vancomycin MRSAs were still found to be presented in respiratory specimens of some patients.
Methods: All MRSAs which had been continuously isolated in respiratory specimens during vancomycin therapy were collected from Jul 2003–Mar 2004 at Seoul Paik Hospital. MRSAs were screened on Brain Heart Infusion plates containing vancomycin 4 μg/mL (BHI-4) and 6 μg/mL (BHI-6) for vancomycin resistance. Minimal inhibitory concentrations (MICs) were determined by E-tests, agar dilution methods, and broth dilution methods. The patterns of pulsed field gel electrophoresis were analysed.
Results: Nine patients and 27 isolates were assessed. Five patients had pneumonia and four patients had other MRSA infections. Twelve MRSAs were isolated from tracheal aspirates and 15 from expectorated sputum specimens. The duration of vancomycin use ranged from 7–22 days. Five isolates and one isolate were cultured on BHI-4 and BHI-6, respectively; the vancomycin MICs of these isolates revealed 3 μg/mL by E-tests. The MICs from agar dilution methods and broth dilution methods showed from 0.5–2 μg/mL.
Conclusion: Vancomycin resistance during the treatment of patients did not develop.
P978: Bactericidal activity of vancomycin and daptomycin tested against heterogeneous and homogeneous vancomycin-intermediate S. aureus (hVISA and VISA) strains
H. Sader, P. Rhomberg, R. Jones (North Liberty, USA)
Objective: To evaluate vancomycin (VAN) and daptomycin (DAP) bactericidal activity tested against S. aureus strains with decreased susceptibility to VAN (VISA and hVISA).
Methods: A total of 105 well-characterized S. aureus strains with decreased susceptibility to VAN (88 hVISA and 17 VISA) as well as 105 oxacillin-resistant wild-type (WT) S. aureus with VAN MIC ≤ 2 mg/L (MRSA-WT; isolated in 2003) were susceptibility (S) tested by reference NCCLS broth microdilution method against DAP and VAN. MBC values were assessed by plating the entire volume of the broth from each well above the MIC for each organism. The lowest concentration of antimicrobial agent that killed ≥ 99.9% of the initial inoculum was defined as the MBC endpoint. Bactericidal action was defined as a MBC/MIC ratio ≤ 2 and tolerance was defined as a MBC/MIC ratio ≥ 16.
Results: VAN MIC and MBC results for 3 subsets of S. aureus strains are summarized in the Table. Only two-third of the MRSA-WT isolates showed VAN MBC results ≤ 4 mg/L, and for hVISA and VISA groups, only 19.3 and 0.0% of isolates had a VAN MBC at ≤ 4 mg/L, respectively. Fourteen (13.3%), 61 (69.3%), and 17 (100.0%) strains respectively showed VAN MBC result ≥ 32 mg/L among the MRSA-WT, hVISA, and VISA groups. In contrast, all MRSA-WT and hVISA strains were inhibited by ≤ 1 mg/L of DAP, while the VISA strains showed slightly higher DAP MIC values (range, 0.5–4 mg/L). The highest DAP MBC result was only 4 mg/L and 93.3% of isolates showed a DAP MBC at ≤ 1 mg/L. Eight of 11 DAP MBC results of 2 mg/L and all 3 MBC results of 4 mg/L were observed among the VISA strains. DAP MBC/MIC ratio was not significantly affected by VAN susceptibility. All DAP MBC results were at the MIC or only 2-fold greater. 17.1% of MRSA-WT strains, 69.3% of hVISA and all VISA strains showed a VAN MBC/MIC ratio consistent with tolerance.
No. of isolates (cumulative %)
| VAN concentration (mg/L) | VISA (17) |
hVISA (88) |
MRSA-WT(105) |
|||
|---|---|---|---|---|---|---|
| MIC | MBC | MIC | MBC | MIC | MBC | |
| ≤0.5 | – | – | – | – | 9 (8.6) | 2 (1.9) |
| 1 | – | – | 9 (10.2) | 3 (3.4) | 84 (88.6) | 38 (38.1) |
| 2 | – | – | 61 (79.5) | 9 (14.9) | 12 (100.0) | 23 (60.0) |
| Susceptible 4 | 11 (84.7) | – | 18 (100.0) | 5 (19.3) | – | 9 (68.6) |
| 8 | 6 (33.3) | – | – | 3 (22.7) | – | 15 (82.9) |
| 16 | – | – | – | 7 (30.7) | – | 4 (86.7) |
| Resistant ≥32 | – | 17 (100.0) | – | 61 (100.0) | – | 14 (100.0) |
Conclusions: VAN showed bacteriostatic activity against the majority of VISA and hVISA strains. VAN also had high rates of tolerant MBC/MIC ratios, but DAP was highly bactericidal against MRSA-WT as well as VISA and hVISA strains.
P979: Genetic basis of fusidic acid resistance in staphylococci
A.J. O'Neill, G. Kahlmeter, A.S. Henriksen, I. Chopra (Leeds, UK; Vaxjo, S; Copenhagen, DK)
Objectives: Fusidic acid resistance (fusR) in Staphylococcus aureus usually results from acquisition of the fusB resistance determinant, or from mutations in the fusA gene encoding the drug target (Elongation factor G). Following a recent report of fusR in S. intermedius, and the detection in our own studies of fusR S. lugdunensis (unpublished), we have examined whether resistance in these strains results from fusA/fusB-type mechanisms.
Methods: Standard methodology was employed for strain identification, susceptibility testing, Southern hybridization (SH), PCR amplification and DNA sequencing. Primers for PCR amplification of the previously-unsequenced S. intermedius fusA gene were based on portions of the flanking genes (rpsG, tufA) that are conserved between B. subtilis and S. aureus.
Results: Three fusR S. lugdunensis (fus MIC = 4 ug/ml) and two fusR S. intermedius (fus MIC = 2 ug/ml) were probed for the presence of fusB by SH alongside their wild-type, fusS counterparts (fus MICs of 0.064 and 0.125 ug/ml, respectively). The fusR S. lugdunensis all carried fusB, but this gene was not detected in S. intermedius, or in the fusS strains. Furthermore, fusB appeared to be chromosomally-located, since no hybridization was observed with purified plasmid DNA. PCR analysis mapped fusB to a chromosomal region upstream of the groEL gene, the same locus at which this gene is carried in the epidemic fusR European S. aureus clone. To examine whether mutations in fusA are responsible for fusR in S. intermedius, PCR amplification and sequencing of fusA from the resistant and sensitive strains was performed. Relative to fusS S. intermedius NCTC 11048, the resistant strains carried six coding polymorphisms in fusA, although none of these correspond to reported fusR mutations in the fusA gene of S. aureus.
Conclusions: Fus resistance in recent strains of S. lugdunensis results from carriage of the fusB determinant on the chromosome, probably acquired horizontally from fusR S. aureus strains. The fusB gene was not detected in the S. intermedius strains, although multiple fusA polymorphisms were identified which may be responsible for the observed fusR phenotype.
P980: Analysis of mupA gene loci of high level mupirocin resistant staphylococci isolated from tertiary hospitals of Korea
J.I. Yoo, Y.S. Lee, E.S. Shin, J.K. Lee, B.S. Kim (Seoul, KOR)
Objectives: Methicillin-resistant S. aureus (MRSA) and methicillin-resistant coagulase-negative staphylococci (MRCNS) are the most important pathogens that cause nosocomial infections worldwide. One of the few antibiotics which is still effective against MRSA is mupirocin. But mupirocin-resistant S. aureus has been increased since first reported in 1987. And more than 5–10% of S. aureus isolated in tertiary hospitals in Korea was reported to be high level mupirocin resistant. In this study, we investigated the restriction fragment length polymorphism (RFLP) type for mupA gene loci of plasmid DNA and sequenced mupR plasmid containing mupA gene of high level mupirocin resistant (MuH) staphylococci from tertiary hospitals.
Methods: Susceptibility to antimicrobial agents including mupirocin was tested by the disk diffusion and MIC of mupirocin was determined by agar dilution method. The plasmid-encoded mupA gene was detected by PCR. mupA polymorphisms of plasmid DNA digested by Hind III, EcoR I, and Cla I restriction enzymes was investigated with southern hybridization using mupA probe. S. aureus isolate showing the most prevalent RFLP type was conjugated by filter mating method and selected the transconjugant showing only mupirocin resistant phenotype. The mupR plasmid of selected transconjugant was purified and analysed the plasmid DNA sequence.
Results: 9 MuH-staphylococci were isolated among the 680 staphylococci from tertiary hospital in Korea. MuH-MRSA (6 isolates), S. haemolyticus (1 isolates), S. hominis (1 isolates) and S. epidermidis (1 isolates) were isolated. 1.65kb mupA PCR product was detected in plasmid of MuH isolate. All isolates contained more than two plasmid molecules that were repeatedly purified with different efficiences. Three different polymorphs of the mupA loci were investigated. The most prevalent mupA polymorph was 4.2kb EcoRI- 8kb HindIII-2.1kb ClaI hybridizing fragment. The mupirocin resistant plasmid DNA was about 52kb and IS257-mupA-IS257 sequence was located.
Conclusion: The high-level mupirocin resistant staphylococci had the multiple plasmids of various size and the diverse RFLP type suggested the variation of mupA gene loci. The mupR plasmid contained transferable element such as IS257 with mupA gene.
P981: Genetic basis of macrolide, lincosamide, streptogramin resistance in coagulase-negative staphylococci
S. Gatermann, T. Koschinski, S. Friedrich (Bochum, D)
Objective: In S. aureus erythromycin resistance is almost exclusively caused by ermA or ermC genes whereas export of macrolide antibiotics by msrA or inactivation of lincosamides by linA is rare. Resistance may be inducibly (clindamycin appears susceptible) or constitutively (clindamycin appears resistant) expressed. During therapy of inducibly resistant strains with clindamycin mutations may occur that render them constitutively resistant. Therefore, in S. aureus, erythromycin resistant isolates may be considered clindamycin resistant. Much less is known about the basis of MLSB resistance in coagulase-negative staphylococci (CoNS) but reportedly resistance mechanisms other than methylation are more common. In this case unconditional reporting of erythromycin resistant strains as clindamycin resistant may lead to avoidance of lincosamides and induce increased usage of glycopeptides. As automated systems test for resistance to single antibiotics only but not for induction it is relevant to identify cases that are not correctly predicted by the software of these machines.
Methods: We tested 494 consecutive non-copy clinical strains of CoNS. Species were identified with biochemical techniques; unclear or equivocal results were resolved by sodA sequencing. For phenotypic detection the disk approximation test with erythromycin, clindamycin and lincomycin was used. Multiplex PCR for erm genes and PCRs for the presence of msrA and linA were conducted to detect the basis for resistance.
Results: Erythromycin resistance was found in 62% of the isolates; three (0.6%) were resistant to lincomycin only. Of the 305 erythromycin-resistant strains, 50.8% were constitutively clindamycin resistant, 24.3% were inducibly resistant, and 76 (24.9%) were non inducible. S. haemolyticus was most often (91.2%) erythromycin resistant; S. epidermidis in 62.2% and S. warneri in 53.5%. The ermC gene was most common (68.8%), msrA (26.5%) was next, followed by ermA (5.5%) and ermB (2.3%). No significant differences in distribution of genes among resistant species was seen.
Conclusions: Our work extends the data of others who analysed unspeciated CoNS only. The data indicate that owing to a relatively high proportion of CoNS that harbour the exporter unconditional reporting of erythromycin resistant isolates as clindamycin resistant should not be done but relevant erythromycin isolates should be tested for induction of clindamycin resistance.
P982: Relationship between lysostaphin susceptibility and cell wall thickness in a vancomycin-resistant Staphylococcus aureus isolates
I. Alshami, J.P. Burnie, S.A.H. Awad (Manchester, UK)
Objectives: Lysostaphin is an antibacterial enzyme which is specifically capable of cleaving the cross-linking pentaglycine bridges in the cell walls of staphylococci. S. aureus cell walls contain high proportions of pentaglycine, making lysostaphin a highly effective agent against both actively growing and quiescent bacteria. Relationship between lysostaphin susceptibility, vancomycin susceptibility and cell wall thickness of passage-selected vancomycin-resistant Staphylococcus aureus isolates (VRSA) and their parent strains were studied in order to investigate Characterization of isolates with decreased susceptibility to vancomycin.
Methods: The susceptibility of lysostaphin for six VRSA and their parent strains were determined using the spectrophotometric and the macrodilution methods. Spectrophotometric determination of turbidity was measured as a decrease in A620 during incubation of the isolates samples at 37°C. MICs were determined by a broth macrodilution method in cation-adjusted Mueller-Hinton broth according to standards of the National Committee for Clinical Laboratory Standards. Cell wall measurement were determined using Transmission Electron Microscopy.
Results: Determination of lysostaphin activity revealed that there are significant decreases in per cent reduction in turbidity (activity of lysostaphin) of the VRSA. VRSA shown to be more resistant to lysostaphin than parent strains. The MICs of lysostaphin for the VRSA strains also increase. There were either a 2 or 4 fold increases in the MIC to lysostaphin. Electron Microscopy of the VRSA showed enhanced cell wall thickness, uneven surfaces and irregular shape in contrast of the thin and regular cell wall morphology of the parent strains. Those strains acquiring the highest thickness in cell wall demonstrating the highest resistant to lysostaphin.
Conclusion: The mechanism of lysostaphin resistance and its relationship to vancomycin resistance remains unclear. It is possible that the increase in cell wall thickness we observed prevented lysostaphin access to all pentaglycine targets or increased the number of cross-linkers requiring cleavage before the strain could lyse.
Typing and epidemiology of MRSA
P983: SeqNet.org: network of laboratories for sequence based typing of microbial pathogens
A.W. Friedrich, W. Witte, H. de Lencastre, W. Hryniewicz, J. Scheres, H. Westh and the SeqNet.org participants
Objectives: SeqNet.org is an initiative of currently 27 laboratories from 19 European countries in order to establish a European network of excellence for sequence based typing of microbial pathogens. The principle goal of SeqNet.org is to establish unambiguous, electronic portable, easily comparable typing data for local infection control and national and European surveillance of sentinel microorganisms. This will be achieved (i) by harmonization of sequencing methods for sequence based typing, (ii) by building capacity for DNA sequencing in diagnostic microbiology, (iii) by establishing quality control/quality assessment (QC/QA) for DNA sequencing in diagnostic microbiology, (iv) by improving the general access to sequence based microbial typing results and the transfer of data at international level and (v) by dissemination of the projects results through a web-portal.
Methods: Creation and distribution of a consensus document detailing the needed harmonization of sequencing technology in diagnostic microbiology will be followed by a certification program for sequence based typing, using methicillin-resistant S. aureus (MRSA) as a prototype organism. As typing method spa-typing will be used. Five strains, 5 DNAs, and 5 forward and reverse chromatogram files of well characterized MRSA strains will be distributed to all participating laboratories. An annual proficiency testing for sequence based typing of MRSA is planned.
Results: At the ‘kick-off’ meeting in Münster, Germany (November 2004) the participants decided to produce documents detailing the needed certification and annual proficiency tests (external QC) as well as the needed internal quality procedures for sequence based typing of MRSA. The development of a SeqNet.org web-portal and the networking of the partners by the Ridom StaphType™ software was decided. Thereby, SeqNet.org already achieved a fast cross-border detection of special clones, e.g. S. aureus harbouring the Panton-Valentine-Leucocidine (PVL) that are in Europe often associated with spa t044 and ST80.
Conclusion: The SeqNet.org initiative is a vivid European-wide network of laboratories for sequence based typing of microbial pathogens. It generates high quality typing data that are available ‘on the fly’ to all participants and the public through the web- portal. Moreover, the SeqNet.org typing data can already be used for trend analysis and early warning algorithms. Other laboratories are welcome to join this initiative.
P984: A prevalence study on carriage of methicillin-resistant Staphylococcus aureus in a Finnish nursing home
A.-M. Kerttula, O. Lyytikäinen, A. Virolainen-Julkunen, H. Finne-Soveri, N. Agthe, J. Vuopio-Varkila (Helsinki, FIN)
Objectives: Due to the increasing problem of MRSA in Finnish long-term care facilities, we carried out a prevalence study in the largest nursing home in Helsinki metropolitan area. Of the residents, 76 % were females, the mean age was 83 years and 62% suffered from dementia. The objective was to study MRSA colonization rate in such setting. In addition, the role of screening sites, and use of broth enrichment culture on sensitivity to detect S. aureus was analysed.
Methods: Of the 25 available wards, 9 such wards were chosen, where at least one of the residents had either indwelling catheter or open skin lesions but no previously known MRSA contacts. The patients volunteered had their nostrils, throats, perineums, skin lesions, and catheter exit sites swabbed, and catheter urines cultured. The specimens were cultured onto the non-selective (blood) and selective (ORSAB) agar, with or without enrichment in salt-containing trypticase soy broth (TSB). S. aureus was identified by routine methods and methicillin-resistance detected by oxacillin disk diffusion, and MIC E-tests, GenoType MRSA® -test (Hain Lifescience, Germany) was used for MRSA confirmation. MRSA genotypes were characterized by pulsed-field gel electrophoresis (PFGE).
Results: Total of 663 specimens (210 from nostrils, 197 throats, 207 perineums, 24 skin lesions, 9 catheter exit sites, and 16 from catheter urines) were obtained from 213 patients. 165 samples (25%) from 94 patients (44%) were positive for S. aureus, and three samples (0.4%) from two (0.9%) patients were positive for MRSA. Two different MRSA strains were found; a non-multiresistant MRSA strain from the perineum of one patient and a multidrug-resistant strain both from the nostrils and catheter exit site of another, respectively. Of 165 S. aureus isolates, 26 (16%) were found only from other sites than nostrils (25 MSSA, and 1 MRSA from a total of 25 patients). TSB enrichment detected an additional 29 (4 %) S. aureus isolates (28 MSSA, and 1 MRSA).
Conclusions: Carriage of S. aureus was high but prevalence of MRSA low in this long term care facility setting. Omission of surveillance sampling sites other than nostrils would have missed 12% (24 MSSA and one MRSA case) of S. aureus carriers. Addition of the broth enrichment step resulted in finding 7 (3%) additional S. aureus-positive carriers.
P985: Molecular epidemiology of an outbreak caused by methicillin-resistant Staphylococcus aureus in a health care ward and associated nursing home
A.-M. Kerttula, O. Lyytikäinen, J. Vuopio-Varkila, N. Agthe, M. Broas, H. Jägerroos, A. Virolainen-Julkunen (Helsinki, Rovaniemi, FIN)
Objectives: An outbreak of MRSA with 13 cases occurred in a health care ward and an associated nursing home of a small municipality in Northern Finland during autumn 2003. The MRSA strains were shown to possess a new pulse-field gel electrophoresis (PFGE) and multi-locus sequence typing (MLST) profile. The molecular epidemiology of MRSA screening results obtained by the local health authorities during 2003–4 were compared to the results of a point-prevalence survey in February 2004.
Methods: Health care ward (34 beds) and nursing home (46 beds) with 76 participating residents were studied. Information on MRSA screening samples from 2003–2004 was asked from the local clinical microbiology laboratory. In addition, all the patients had their nostrils, skin lesions, and urinary catheters swabbed (76. 10, and 4 samples, respectively) for MRSA in February 2004. The samples were cultivated onto MRSAselective and non-selective media. Oxacillin-resistance was determined by MIC-test, mecA-gene confirmed by PCR, and S. aureus genotypes characterized by PFGE.
Results: Twenty-four of 76 patients (32%) were S. aureus carriers; 5 (7%) were positive for MRSA. Two of the MRSA isolates were from patients recorded positive in autumn 2003, and 3 from new patients found to be carriers of another Finnish epidemic MRSA strain. Two of these were also methicillin-sensitive S. aureus (MSSA) carriers but the MSSA strains were of another genotype than the MRSA carried by the same person. All 5 isolates were resistant to oxacillin only, and two isolates, which expressed oxacillin MIC:s 2 and 4–6 mg/l, did not grow on the oxacillin screening agar plate having oxacillin 2 mg/l. A total of 25 MSSA strains were found: from the patients never found to be positive for MRSA, 3 of the MSSA strains were genotypically related to the new MRSA outbreak strain, and 3 to the another epidemic MRSA strain. In addition, 12 MSSA strains were related to other epidemic MRSA-strains, and 7 were sporadic strains.
Conclusions: The original MRSA outbreak was found to be confined, but 3 new MRSA cases not related to the epidemic were detected by repetitive screening. The current MRSA screening methods used routinely may not be sensitive enough for strains possessing low-level oxacillin resistance.
P986: Evaluation of Staphylococcus aureus nasal carriage rate among patients on haemodialysis - isolation of community-acquired methicillin-resistant Staphylococcus aureus
A. Szczepanik, M. Koziol-Montewka, I. Baranowicz, L. Jozwiak, A. Ksiazek, D. Kaczor, Z. Al-Doori, D. Morrison (Lublin, PL; Glasgow, UK)
Nasal carriage of Staphylococcus aureus (SA) appears to play a key role in the pathogenesis of infection, particularly in patients on haemodialysis. Compounding the problem is dissemination of methicillin-resistant Staphylococcus aureus (MRSA) and changing epidemiology of this microorganism. MRSA, besides having established itself as a major nosocomial pathogen, has also begun to appear outside hospital settings as community-acquired MRSA (CA-MRSA). The aim of the study was evaluation of SA nasal carriage rate in haemodialysed patients and molecular analysis of cultured isolates.
Methods: Nasal swabs were collected from 43 haemodialysed patients. SA isolates were identified using conventional diagnostic methods. Antibiotic susceptibility was determined using the Vitek automated system and the disc diffusion method according to recommendations given by the National Reference Centre for Antimicrobial Susceptibility Testing in Poland. SA isolates were analysed by Pulsed Field Gel Electrophoresis (PFGE) and PCR assays for staphylococcal cassette chromosome mec (SCCmec) typing and detection of the nuc and pvl genes.
Results: 12 (27.9%) patients were SA nasal carriers, but only 1 MRSA isolate was identified. The carrier of MRSA was a 56–year-old male suffering from chronic renal failure and malignancy (true polycythaemia). The patient had a history of previous hospitalization. The MRSA strain was resistant only to B-lactams and tetracycline. The remaining SA isolates were methicillin-susceptible (MSSA) and demonstrated high rates of resistance to penicillin (81.8%) and tetracycline (63.6%). Molecular analysis revealed that the MRSA strain had genetic markers of CA-MRSA: SCCmec type IV, a PFGE pattern corresponding to the common European CA-MRSA (MLST Type ST80) and the pvl locus encoding for Panton-Valentine leukocidin toxin. Among MSSA isolates, several genotypes were identified by PFGE, with the lack of one specific colonizing strain.
Conclusions: To our knowledge, this is the first report of CA-MRSA in Poland. The results of the study indicate that colonization and the increased risk of subsequent invasive infection associated with significant pathogenic potential of CA-MRSA can occur among persons with predisposing risk factors such as patients on haemodialysis. Although the rate of MRSA colonization was low among examined patients, the risk of endogenous infections associated with MSSA carriage must also be considered.
P987: Expansion of a single multiresistant methicillin-resistant Staphylococcus aureus clone carrying a variant of SCCmec type III in a university hospital
A. Szczepanik, M. Koziol-Montewka, D. Kaczor, Z. Al-Doori, D. Morrison (Lublin, PL; Glasgow, UK)
The purpose of the study was molecular characterization of methicillin-resistant Staphylococcus aureus (MRSA) isolates cultured from patients treated in various wards of the University Hospital in Lublin, Poland.
Methods: 16 MRSA isolates cultured from 11 hospitalized patients were analysed. Antibiotic sensitivity testing was performed using the Vitek automated system. Phenotypic identification of the isolates as S. aureus resistant to methicillin was confirmed by a multiplex PCR assay (S. aureus PCR diagnostic kit; DNA Gdansk, Poland) to detect the nuc and mecA genes, respectively. The MRSA were characterized by Pulsed Field Gel Electrophoresis (PFGE), 16S-23S rRNA spacer length polymorphism analysis and Oliveira and de Lencastre multiplex staphylococcal cassette chromosome mec (SCCmec) PCR assay.
Results: All MRSA isolates were positive for the nuc and mecA genes. The isolates were defined as multiresistant - in addition to resistance to B-lactams, they demonstrated resistance to ciprofloxacin, tetracycline, erythromycin and gentamicin. Resistance to clindamycin and trimethoprim/sulfamethoxazole was detected in 10 (62.5%) and 1 isolate (6.25%), respectively. The isolates were susceptible to rifampin and vancomycin. They were genetically identical and shared common PFGE and 16S–23S rRNA spacer length polymorphism profiles. By SCCmec typing all MRSA harboured a presumed new variant of SCCmec type III. The isolates were positive for the 162 - bp internal fragment of the mecA gene, Locus C (mecI, 209-bp) and Locus G (303-bp)corresponding to the plasmid pT181 insertion. The pattern differed from the typical SCCmec type III pattern by the lack of Locus E (243-bp) and Locus F (414-bp).
Conclusions: The results of the study are indicative of the expansion of a single, multiresistant MRSA clone in various wards of the University Hospital. The clone harboured a presumed new SCCmec type III variant.
P988: Epidemiological typing of MRSA using spa sequencing and PFGE
A.C. Petersson, S. Haeggman, B. Olsson-Liljequist, H. Miörner (Lund, Solna, S)
Objectives: The aim of the study was to evaluate the resolution of spa sequencing and PFGE in epidemiological typing of MRSA isolated within a low prevalence region.
Methods: MRSA isolates (180 isolates from 180 persons), collected at CMI in Lund between January 2000 and July 2004, were subjected to epidemiological typing. For spa typing the polymorphic X-region of protein A was amplified and sequenced using primers corresponding to nucleotides 1094–1111 and 1492–1475 or 1533–1516 of GenBank accession no. J01786. The Ridom StaphType software was used for sequence interpretation. PFGE was performed on SmaI digested DNA using S. aureus NCTC 8325 as standard reference for gel normalization. The PFGE patterns were analysed using the BioNumerics software. Dice coefficient was used for band matching and UPGMA for dendrograms. Each distinct band pattern was given a specific designation. Epidemiological data was obtained from the infection control unit at Lund University Hospital. The Simpson's diversity index with 95 % confidence interval was used to resolve the resolution of the two typing methods.
Results: Eighty-three isolates (46 %) were most likely acquired abroad and 58 (32 %) in Sweden (24 of which were considered to be community-acquired and 34 health care related). For 39 (22 %) of the isolates the origin could not be established. Epidemiological data allocated the 180 isolates to 107 unrelated episodes. Typing identified 39 spa types and 61 distinct PFGE patterns. The number of episodes where epidemiological data and typing results were concordant is presented in the table. PFGE showed higher discrimination than spa typing when looking at the single case episodes (44 % of these episodes were identified by unique PFGE patterns and 19 % by unique spa types). Both techniques correctly identified a majority of the episodes including two or more persons (spa typing 97 % (31/32), PFGE 84 % (27/32)). The resolution of the two typing methods was equally high, 98.3–99.3 % for spa typing and 98.4–99.5 % for PFGE, when combined with epidemiological data.
| No. of persons per episode | No. of episodes | No. of episodes identified by | |
|---|---|---|---|
| spa (No. of types) | PFGE (No. of patterns) | ||
| 1 | 75 | 14 (28) | 33 (49) |
| 2 | 15 | 15 (12) | 14 (14) |
| 3 | 10 | 10 (5) | 8 (7) |
| 4 | 4 | 4 (4) | 4 (4) |
| 7 | 1 | 1 (1) | 0 (2a) |
| 9 | 1 | 1 (1) | 1 (1) |
| 13 | 1 | 0 (2b) | 0 (2b) |
one isolate differed slightly from the other six
one isolate (the same in both techniques) differed slightly from the other twelve
Conclusion: In the present study spa typing gave equivalent resolution to PFGE, and is well suited for epidemiological typing of MRSA in a low prevalence region with a broad spectrum of strains.
P989: Resistance phenotypes of methicillin resistant S. aureus in a Greek hospital during 1998–2003
P. Panagiotou, E. Panagiotidou, E. Xatzilakou, A. Tatsiopoulos, B. Nikolopoulou (Athens, Thessaloniki, GR)
Objective: The prevalence of new Multidrug resistant strains of methicillin-resistant S. aureus (MRSA) in recent years, led us to evaluate the epidemiology and resistance phenotypes of MRSA.
Methods: We studied 900 nonduplicate strains of MRSA of a total of 2224 strains of S. aureus isolated during the period 1998–2003 in General University Hospital. The identification was based on the slide-coagulase test and the susceptibility of all isolates to oxacillin and other antimicrobial agents was tested by the disk-agar diffusion method as standardized by the NCLLS. The following antimicrobial disks were used: oxacillin, gentamicin(G), erythromycin(E), vancomycin(V), co-trimoxazole(S), ciprofloxacin(C), rifampicin(R), fusidic acid(F), clindamycin(L), and chlorampenicol(H).
Results: We document that the proportion of methicillin resistant isolates had progressively increased from 31% of total S. aureus in 1998 to 52% in 2003. The majority of MRSA strains were recovered from wound sites (n = 267), respiratory specimens (n = 219) and blood cultures (n = 116). The highest proportion of MRSA were observed in intensive care units (80% S. aureus), in medical (41%) and surgical units(37%). MRSA strains susceptible to all antibiotics had decreased remarkably from 35% in 1998 to 14.5% in 2003. Eight main different antibiotic resistance patterns were identified among the MRSA, with the commonest being that exhibiting multiple resistance to gentamicin, erythromycin, clindamycin, co-trimoxazole, ciprofloxacin, rifampicin and fusidic acid (phenotype GELSCRF). This phenotype had a mean incidence of 40.7% of all MRSA during the period 1998–2003 and an evolution ranging from only 3% in 1998 and 15% in 2000 to the alarming proportion of 54% in the last 2 years. The multi-drug resistant pattern was found mainly in ICU patients (73% of MRSA) and secondly in patients of medical (47%) and surgical (42%). Resistance to chlorampenicol was detected only in 3.5% of MRSA and no MRSA strain was found to be resistant in vancomycin.
Conclusions: A progressive increase of MRSA is well documented. Since 1999, the predominance of a well-defined multidrug resistance hospital strain (susceptible only to glycopeptides and chlorampenicol) is observed. The prevalence of multi resistant strains leads to an increase in mortality and morbidity and demands appropriate control, surveillance procedures and awareness for development of glycopeptide resistance.
P990: Phenotypical differences in antibiotic resistance between MRSA and MSSA strains isolated from clinical samples of patients treated at the clinics of the Semmelweis University
K. Kristóf, Z. Szabó, V. Cser, S. Kardos, Á. Ghidán, F. Rozgonyi (Budapest, HUN)
Objectives: The aim of this study was to reveal any significant difference in the co-resistance to antistaphylococcal agents between methicillin-resistant (MRSA) and methicillin-sensitive
(MSSA) strains of S. aureus. In this presentation the results of the antimicrobial susceptibility testing of a total of 4097 S. aureus strains isolated from clinical speciments between 1 January 2001 and 31 December 2003 are shown.
Methods: The identification of the S. aureus strains was performed by traditional and molecular methods (catalase, coagulase, nucA). The antibiotic susceptibilty tests were carried out by disc diffusion methods according to the NCCLS recommendations, and the multiplex PCR method was used for detecting the mecA gene. The phage typing was carried out with both conventional and MRSA phages.
Results: In the whole examination period 7.8% of the total S. aureus isolates proved to be MRSA. A continuous increase in the incidence of MRSA was found in the period examined (2001: 3.73%, 2002: 7.08%, 2003: 10.59%). The coresistance of MRSA strains to a variety of antimicrobials was significantly higher than that of the MSSA strains. The ratios of coresistance of MRSA/MSSA strains were as follows: erythromycin, 92/13; clindamycin, 90/2; ciprofloxacin, 89/1; doxycycline, 98/1; mupirocin, 7/1; gentamicin, 69/2; tobramycin, 76/2; amikacin, 65/7; and netilmicin, 22/1. But the resistance rate was invert to trimethoprim+sulphamethoxazole, 0.5/98. Neither vancomycin nor teicoplanin nor linezolid resistant strains were found. Phage type 623 and 629 predominated the MRSA strains with 53% and 33%, respectively.
Conclusion: During the whole examination period the number and the proportion of the MRSA isolates increased and also their resistance against different kinds of antibiotics. There was found a significant difference between the MRSA and MSSA isolates in the coresistance to antistaphylococcal drugs. Vancomycin, teicoplanin and linezolid were fully effective.
P991: Antibiotic resistance of Staphylococcus aureus: a Tunisian multicentre study 1999–2003
R. Ghozzi, F. Mahjoubi, H. Smaoui, W. Jouahia, A. Hammami, A. Kéchrid, A. Ben Hassen, S. Ben Redjeb (Tunis, TN)
Staphylococcus aureus is an important human pathogen related to its ability to develop resistance to many antimicrobial agents. Methicillin resistance of S. aureus (MRSA) has become a major public health problem especially in nosocomial infectious. More over community acquired MRSA is a growing concern, the rate of MRSA vary importantly within countries, the highest rates were reported especially in Southern European countries. A multicentric study was done to establish antimicrobial resistance of S. aureus isolated from clinical specimens of hospitalized patients over five years period (1999–2003). S. aureus was identified by conventional methods and antibiotic susceptibility testing was performed by disk diffusion method according to NCCLS standards. A total of 5186 strains of S. aureus were collected, they were recovered mainly from pus (60%), blood cultures (15%), respiratory samples (8%) and urines (7%). 34% of the strains were from in medicine, 18% from surgery, 16% from orthopaedics, 14% from paediatrics and 13% from intensive care units. The rates of resistance to different antibiotics was 15% to oxacilline,9% to gentamicin, 23% to amikacin,8% to ofloxacin, 23% to erythromycin and 8% to clindamycin. All isolates were susceptible to vancomycin. According to this data the rate of MRSA remained relatively low (< 20%) with no significant change during this time period, however, MRSA presented high rates of associated resistance to gentamicin (48%), to amikacin, (91%) to erythromycin (38%), to clindamycin (20%), to ofloxacin (40%) and to trimethoprim-sulfamethoxazole (33%).MRSA were not of great concern in our country and meticillin remains an effective antibiotic for treatment of S. aureus infections.
P992: Characterisation of gentamicin-susceptible strains of methicillin-resistant Staphylococcus aureus in two Spanish hospitals
C. Potel, M. Alvarez, C. Lopez-Melendez, I. Otero (Vigo, E)
Objectives: Characterize gentamicin-susceptible methicillin-resistant Staphylococcus aureus(GS-MRSA)by two molecular typing methods. Find out whether some GS-MRSA clones are related to GR-MRSA. Describe the spread of these clones.
Methods: One hundred and twelve SAMR were isolated in two hospitals between 1997–2001. The epidemiological relatedness was studied by repetitive element sequence-based PCR and coa gene restriction fragment length polymorphism. The genes ant(4′) and aac(6′)-aph(2′), that codify two aminoglycoside modifying enzymes, were detected by PCR. We analysed the gentamicin consumption and its relation with the emergence of GS-MRSA.
Results: Thirty nine strains were GS-MRSA. The 80% of these GS-MRSA belonged to two epidemic clones, the clone A was tobramycin sensitive and the clone B was tobramycin resistant. The clone A was only isolated at hospital-I and was replaced by an epidemic GR-SAMR clone (clone C). The clone B was only isolated at hospital-II and displaced the clone C.GR and GS-MRSA strains were not genetically related. The aac(6′)-aph(2′) gene was detected in the GR-MRSA strains (clon C) but not the ant(4′) gene. In the clone B only the ant(4′) gene was detected. The gentamicin consumption remained stable in both hospitals during the studied period.
Conclusions: The GS-MRSA clones were not linked to GR-MRSA. Therefore, the emergence of GS-MRSA was due to new MRSA clones that have an epidemic mode of transmision. Moreover, the clone B (GS-MRSA and tobramycin resistant) did not come from GR-MRSA by means of the loss of the aac(6′)-aph(2′) gene. The gentamicin consumption was not related with the evolution of the different studied clones. *Complejo Hospitalario Universitario de Vigo and Clinica Fatima de Vigo
P993: The prevalence of mupirocin resistant MRSA of long-term care facilities
J.I. Yoo, E.S. Shin, J.O. Cha, J.K. Lee, S.H. Eun, B.S. Kim, Y.S. Lee (Seoul, KOR)
Objectives: The long-term care facilities (LTCFs) patients are those with serious underlying disease, poor functional status, wounds such as pressure sores, invasive devices of urinary catheters. There is increasing concern about the emergence of resistance to antimicrobial agents including methicillin resistant S. aureus in LTCFs and mupirocin has been used in LTCFs to prevent the occurrence and spread of MRSA. But the prevalence of mupirocin resistant MRSA in LTCFs has not been known yet in Korea. In this study, we investigated the prevalence of mupirocin resistant MRSA from LTCFs and their molecular epidemiological analysis.
Methods: 749 specimens were obtained from 632 patients of 8 LTCFs from July to August 2002. Specimens were cultered on staphylococcal medium and species were identified by PCR and biochemical test. Antimicrobial susceptibility tests to 12 antibiotics were performed by disc diffusion method, MICs of oxacillin, mupirocin were confirmed by agar dilution method and E-test method. Mupirocin resistant isolates were divided into low level mupirocin resistant (MuL) and high level mupirocin resistant (MuH) by according to criteria ≤ 256 μg/ml and ≥ 512 μg/ml, respectively. PFGE and RFLP typing were performed for molecular epidemiological analysis of mupirocin resistant isolates.
Results: 365 S. aureus (48.7%) were isolated from the LTCFs specimens and 259 isolates (70.9%) were identified resistant to oxacillin. mecA gene was detected in all tested 259 MRSA isolates with MICs of 16 - >128 μg/mL. The mupirocin resistance was 19.3% range from 1.3% to 72.4% of MRSA depending on LTCFs. In one LTCF, 20 out of 39 MRSA isolates were MuH including 15 isolates showing the same PFGE pattern. In the other one LTCF, 19 out of 29 MRSA isolates were MuL with the same PFGE pattern in 17 isolates. Among 26 MuH MRSA detected in 4 LTCFs of 8 LTCFs, the most predominant mupA RFLP type was 4.2 kb EcoRI-8 kb HindIII-2.1 kb ClaI (22 isolates) hybridizing fragments.
Conclusion: Mupirocin resistant MRSA in LTCFs was 19.3%, range from 1.3 to 72.4%. And it is supposed that there was mupirocin resistant MRSA outbreak in two LTCFs. This suggests that the mupirocin resistant MRSA is spread in LTCFs and need the prevention strategy.
P994: Epidemiological relationship of methicillin-resistant Staphylococcus aureus on an intensive care unit using staphylococcal interspersed repeat units
K.J. Hardy, B.A. Oppenheim, F. Gao, P.M. Hawkey (Birmingham, UK)
Objectives: To establish if variable number tandem repeats could be used to investigate the epidemiology of endemic MRSA on an ICU during 2 different study periods.
Methods: During two eight month periods, all patients admitted for > 48 h to a general ICU were screened 3 times a week for MRSA. Multiple isolates from each patient were then epidemiologically typed using 7 previously described variable number tandem repeats (VNTRs) which have been termed staphylococcal interspersed repeat units (SIRU) The numbers of repeats at each locus were determined and a 7 digit profile generated. The ability of SIRU to identify predominant strains and transmission events was compared with pulse field gel electrophoresis (PFGE). Strains were defined as having >1 band difference (PFGE) and >1 repeat number at any loci.
Results: During the two eight month periods 56/215 (26%) and 61/197 (31%) patients were colonised with MRSA. A total of 19 different SIRU and 21 different PFGE profiles were observed overall, with 7 SIRU and 9 PFGE profiles being present in the 1st study period only, and 3 SIRU and 4 PFGE only present in the 2nd. The most predominant SIRU and PFGE profiles were the same during both study periods. Forty eight patients in the 1st study period and 49 in the 2nd had a high degree of similarity with the UK EMRSA-15 by both SIRU and PFGE. Fifteen subtypes of EMRSA-15 were identified by SIRU and PFGE. However, within indistinguishable PFGE profiles variation within the SIRU was observed, and similarly within the same SIRU variation within the PFGE type was observed. Seven and 13 patients in the 1st and 2nd had a high similarity to the UK EMRSA-16. Dual colonisation with different MRSA strains was observed in 7 patients.
Conclusion: SIRU provides a rapid transportable typing method for typing epidemiologically related isolates within an endemic ICU setting. It has discriminatory powers similar to that of PFGE, thereby allowing identification of transmission events.
P995: Genomic backgrounds of major methicillin-resistant Staphylococcus aureus epidemic clonal lineages present in fully susceptible isolates collected in the 1960s in Denmark
A.R. Gomes, H. Westh, M. Chung, H. de Lencastre (Oeiras, P; Copenhagen, DK; New York, USA)
Objectives: Most methicillin-resistant Staphylococcus aureus (MRSA) isolates identified among blood isolates collected in Denmark between 1957 and 1970 belonged to either phage group III or the closely related 83A complex and had a PSTM antibiotype. Recently, some of these strains were shown to belong to the same genetic backgrounds as contemporary epidemic MRSA by MLST and spa typing and Danish MSSA strains from the 60s with a PST antibiotype were proposed to have been the recipients of the mecA gene in those lineages. Among these were strains that belonged to ST247, ST5 and ST30, a single locus variant of ST36. In this study we sought to investigate the genetic backgrounds of isolates that were fully susceptible or resistant to penicillin only from phage group 83A in order to try to trace the evolutionary trajectory of those MRSA lineages. We also studied MSSA and MRSA from other phage groups in order to investigate whether these were associated with genetic backgrounds that reached an evolutionary ‘deadend’.
Methods: Eighty-two MSSA and MRSA strains isolated from the blood between 1957 and 1973 in Denmark were characterized by MLST, spa and SCCmec typing.
Results: Most susceptible or P-resistant isolates from phage groups 83A or III belonged to ST8 or ST5, while four isolates were ST254, the first MSSA strains identified with this genetic background. STs 30, 45 and 25 were represented by MSSA strains from other phage groups, which also included several singletons. ST250 was the most common genotype among nontypeable MRSA isolates.
Conclusions: Representatives of some of the current major epidemic MRSA lineages were identified among fully susceptible isolates collected in the 60s suggesting that these were lineages which carried genetic traits important for a superior epidemicity before acquisition of antibiotic resistance while singletons may represent less fit genotypes. In particular, ST254 MSSA provided the first evidence to the existence of this derivative of ST8 before the introduction of the mecA gene.
P996: Multidrug resistance among methicillin-resistant Staphylococcus aureus in long-term care facilities in Greece
V. Grammelis, G. Tsekes, D. Chalkiadaki, G. Salpigktis, K. Orlandou, K. Kanellakopoulou, H. Giamarellou, M.C. Lazanas (Athens, GR)
Objective: A multicentre point-prevalence survey was conducted in order to determine the prevalence and risk factors for colonization with multidrug-resistant (MDR) MRSA in residents of LTCF in Greece estimate the corresponding rates of antimicrobial resistance (ÁR)
Methods: A total of 28 LTCF were randomly selected from the public sanitation list of Attica province. Nasopharyngeal and wound samples were collected from 862 elderly residents. We chose randomly 30% of the existing population from each LTCF (minimum sum 35 residents). Cultures and susceptibilities were performed, following NCCLS guidelines. The minimal inhibitory concentrations (MICs) of methicillin-susceptible S. aureus (MSSA) and MRSA to 15 alternative antibiotics were also compared. Results were analysed using either the Fischer's exact or chi-square test. Risk ratios and p values were calculated.
Results: 905 samples were collected and 286 strains of S. aureus were isolated. From them, 214 (74.8%) were MSSA and 72 (25.2%) MRSA. In contrast to MSSA, most of MRSA isolates (90% versus 22%) were MDR. Among MDR-MRSA, 49.6% were resistant to chloramphenicol, 39.4% to erythromycin and 34.2% to clindamycin. Also, the ÁR to gentamicin and ciprofloxacin were 29.5% and 19.2% respectively. The most effective agents were linezolid and vancomycin, to which no resistant strains were found, followed by quinupristin/dalfopristin, fucidic acid, trimethoprim-sulfamethoxazole and rifampicin with ÁR lower than 10%. Overall, MRSA vs. MSSA exhibited a significantly higher incidence of resistance to 10 out of the 15 antibiotics examined. In multivariate analysis, colonization with MDR-MRSA was significantly associated with recent hospitalization (p = 0.001), poor functional status (p = 0.001), decubitus ulcers (p = 0.01) and feeding tube (p = 0.01).
Conclusions: 1. Colonization with MDR-MRSA is worrisome in Greek LTCF 2. Macrolides and lincosamydes should be used with caution in case of infections caused by S. aureus, due to increasing antibiotic resistance. 3. According to our survey, significant risk factors for colonization with MDR-MRSA in Greek LTCF are recent hospitalization, poor functional status, decubitus ulcers and usage of feeding tube.
P997: Molecular characterisation of MRSA by spa-typing, MLST and PFGE in the Cologne metropolitan area from 1984 to 1998
H. Wisplinghoff, S. Wisplinghoff, B. Ewertz, D. Stefanik, F. Perdreau-Remington, H. Seifert (Cologne, D)
Background: MRSA continues to be one of the most important nosocomial pathogens. This study was conducted to evaluate the molecular evolution of MRSA in a large metropolitan area in Germany from the beginning of the epidemic in 1984 to 1998.
Methods: MRSA isolates have been prospectively collected at the IMMIH, University of Cologne, from 1984 to the present day. Among 800 isolates recovered from different patients hospitalized in various teaching and non-teaching hospitals in Cologne, Germany between 1984 and 1998, 430 strains were characterized by IS256-PCR and PFGE. Based on the PFGE data, a total of 120 representative isolates were selected for the current study. MLST and spa-typing profiles of all isolates were determined.
Results: Overall, there were 11 MLST sequence-types and 33 spa-types. Most prevalent MLST sequence-types were ST239 (38% of isolates), ST247 (27%) and ST228 (19%). Most prevalent spa-types were 37 (36%) and 51 (27%). While the same PFGE pattern was not observed among strains with different MLST-type, spa-type 8 was seen in strains of 2 different MLST-types, spa-type 37 was observed in strains of 3 different MLST-types (8. 239. 241). which did belong to the same clonal complex as single locus variants. Over time. spa-type 37 was the most prevalent between 1984 and 1990; spa-type 51 between 1991 and 1994 and spa-types 1. 458 and 143 between 1994 and 1998.
Conclusion: Molecular diversity of MRSA increased from 1984 to 1998. Some of the more prevalent spa-types were shared by strains with different MLST-types. While between 1984 and 1994 there was one prevalent spa-type. after 1995 three different spa-types accounted for most of the isolates.
P998: The incidence and risk factors of MRSA nasal carriage among healthcare workers in a Turkish university hospital
S. Hosoglu, M.F. Geyik, S. Akalin, M.K. Celen, C. Ayaz (Diyarbakir, TR)
Objective: Few data are available concerning the prevalence and risk factors of MRSA carriers among HCWs. To assess the prevalence and risk factors of methicillin-resistant Staphylococcus aureus (MRSA) carriage among healthcare workers (HCWs).
Methods: The incidence and risk factors of nasal carriage of MRSA was evaluated prospectively among HCWs in Dicle University Hospital, Diyarbakir, Turkey, during an 18-month period. Epidemiological and clinical data of the HCWs were evaluated using a standardized data form. At the same time, nasopharyngeal swab samples were taken for bacterial cultures of MRSA strains. These swabs were inoculated on blood and mannitol salt agar plates and incubated at 37oC. The isolate(s) were identified as S. aureus on the basis of colony morphology, Gram staining, catalase and coagulase tests. Sensitivity to Oxacillin was determined using standard Kirby Bauer technique.
Results: During the study period, 31 out of 360 (% 8,6) HCWs were found as MRSA nasal carriers. One hundred and sixty-four HCWs were employed in the surgical departments. In the last three months, 123 of the HCWs (34.2%) had used antibiotics. In a univariate analyses, being a nurse (OR = 0.58, CI = 0.46–0.74, p = 0.001), working at a surgical department (OR = 0.68, CI = 0.51–0.91, p = 0.027), and living in a crowded family (OR = 0.63, CI = 0.46–0.88, p = 0.02) were found to be significant factors for MRSA nasal carriage. Besides these significant factors, working at intensive care unit (ICU) (OR = 0.82, CI = 0.71–0.96, p = 0.065) and female gender (OR = 0.84, CI = 0.67–1.05, p = 0.179) were included into a multivariate analyses model. In the multivariate analyses, being a nurse (OR = 0.29, CI = 0.12–0.68, p = 0.004) and living in a crowded family (OR = 0.44, CI = 0.20–0.95, p = 0.037) were found to be independent risk factors for MRSA carriage.
Conclusion: Close contact with patients and some familial characteristics (being a nurse and living at a crowded family) could be important factors which identify the status of MRSA carriage among HCWs.
P999: Methicillin-resistant Staphylococcus aureus: colonisation and infection of respiratory tract in cystic fibrosis patients
A. Molina, R. Del Campo, L. Maiz, H. Escobar, F. Baquero, R. Cantón (Madrid, E)
Introduction: Cystic fibrosis (CF) is an autosomal recessive disorder caused by mutation in the cystic fibrosis transmembrane conductance regulaor gene on chromosome 7, leading to recurrent and chronic respiratory infection which is the most important cause of morbidity and mortality in these patients. S. aureus is frequently the first organism found in the respiratory tract of CF patients, and an increase in the Methicillin-Resistant S. aureus (MRSA) pulmonary infection was observed. The aim of this study was analysed the MRSA infective population in CF patients.
Material and methods: A total of 72 MRSA isolates obtained from 15 CF-patients were included (1–24 isolates per patient). Susceptibility to different antibiotics was performed by the microdilution method (Wider system, Francisco Soria Melguizo, S.A., Madrid, Spain). PFGE-Sma I was applied to analyze genetic relatedness among the isolates, and the patterns obtained were compared by the software Phoretrix 5.0, using the Dice coefficient.
Results: All MRSA isolated presented susceptibility to linezolid and vancomycin, and different resistance levels to other antibiotics. Twenty-four different pulsotypes were found among the 72 isolates. Existence of a single clone among all isolated recovered from the same patient was detected in 8 cases, whereas the existence of 2 different clones was observed in 5 patients, and finally 2 patient carried along the time 3 different MRSA clones. Persistence during five years of the identical MRSA clone in an individual that have 24 different isolates was corroborated. It has been detected clonal relationships among MRSA isolates of different patients, being much of the strains closely related.
Conclusion: Although selected MRSA clones were able to colonized the same patient, a genetic close relation exists among the different clones of 15 different CF-patients. Additional studies are needed to understand the colonization/infections of MRSA in the CF patients, and the role of this bacteria in the prognostic of this pulmonary disease.
P1000: Emergence of community-acquired MRSA in Hungary
Á.Tóth, E. Ungvári, M. Gacs, J. Pászti, M. Füzi (Budapest, HUN)
Objectives: The methicillin-resistant Staphylococcus aureus typically causes infections in inpatients. However, there are MRSA infections arising also in the community without common risk factors. These community-acquired MRSA (CA-MRSA) infections can cause serious or even fatal infections in otherwise healthy people. Recently, CA-MRSA have been reported in many European countries (France, Switzerland, Scotland, Germany). The aim of this study was to characterize 6 CA-MRSA isolates and compare the data of European CA-MRSA isolates.
Methods: The 6 isolates were selected from 2312 MRSA strains collected between January 2002 and June 2004 on the basis of epidemiological data and antibiotic resistance profiles. Testing of antimicrobial susceptibility was performed using E-test according to E-test technical manuel. The presence of the mecA, lukF-PV and lukS-PV genes was detected by PCR. The SCCmec type of isolates was determined by a multiplex PCR-based assay (according to the designation of Oliveira). The genetic background of the isolates was analysed by pulsed-field gel electrophoresis (PFGE).
Results: All of isolates were resistant to beta-lactams and kanamycin. Four of the six strains had identical non-betalactam antibiotic resistance pattern, being resistant to fusidic acid and intermediate resistant to ciprofloxacin. All strains shared the Panton-Valentine Leukocidin (PVL) locus and type IV SCCmec element that is typical of CA-MRSA isolates. According to PFGE analyses 5 of 6 strains shared the same pulsotype and the remaining strain that proved resistant to tetracyclin was closely related to the others. All six strains substantially differed from predominant Hungarian hospital-acquired MRSA (HA-MRSA) strains.
Conclusions: This is the first investigation of CA-MRSA in Hungary. Our results showed that PVL-positive CA-MRSA strains are present in Hungary and the antibiotic resistance pattern of the Hungarian isolates is very similar to those reported from other European countries. The Hungarian CA-MRSA isolates belonged to a single clonal type.
P1001: Community-acquired methicillin-resistant Staphylococcus aureus nasal carriage: prevalence and risk factors
M. Kompoti, S. Drimis, K. Kotsomytis, A. Papadaki, K. Tryfinopoulou, M. Kimouli, O. Zarkotou, D. Gianneli, D. Voutsinas (Athens, GR)
Objective: To assess the prevalence of community-accuired methicillin-resistant Staphylococcus aureus (MRSA) nasal carriage at hospital admission among patients of a tertiary-care hospital.
Methods: All patients admitted to our department between November 2003 and September 2004 were included in the study, provided that they had not been hospitalized for the previous three months. Nasal swabs were drawn from both anterior nares upon admission. Cultures were performed by conventional methods, identification was carried out using the API Staph system and antimicrobial resistance was evaluated by disk diffusion method.
Results: Five hundred-forty five consecutive patients, 278 females (51%) and 267 males (49%), were enrolled in the study and an equal number of samples were screened for MRSA. Mean age (± SD) was 69.1±16.8 years. Major comorbidities included arterial hypertension (41.8%), diabetes mellitus (23.5%), cerebrovascular disease (17.4%), coronary heart disease (14.9%), malignancy (10.5%), chronic obstructive pulmonary disease (6.6%). The prevalence of MRSA nasal carriage was 0.9%, while the overall prevalence of S. aureus was 14.1%. The most common isolate was S. epidermidis (52.5%), as expected. In univariable analysis, risk factors for S. aureus nasal carriage were long-term corticosteroid therapy [odds ratio (OR) = 7.997, 95% confidence intervals (CI) 2.086 – 27.689, p < .001] and immunosuppression (OR = 1.658, 95% CI 1.091 – 2.518, p = .022), while in multivariate analysis, only long-term corticosteroid therapy attained statistical significance [OR = 5.878, 95% CI 1.449 –23.840, p = .013].
Conclusions: The prevalence of MRSA nasal carriage at hospital admission in patients referred from a community setting is low. Long-term corticosteroid therapy is independently associated with an increased risk of S. aureus nasal carriage.
P1002: Clinical isolates of Staphylococcus aureus in the Arkhangelsk region, Russia: prevalence of antimicrobial resistance and molecular epidemiology of methicillin-resistant strains
V. Vorobieva, T. Bazhukova, N. Semenova, B. Haldorsen, G. Skov Simonsen, A. Sundsfjord (Tromso, N; Arkhangelsk, RUS)
Objectives: This study was conducted to examine the prevalence of antimicrobial resistance in clinical isolates of Staphylococcus aureus from hospitalized and non-hospitalized patients in the Arkhangelsk region, Russia and to analyze the molecular epidemiology of methicillin-resistant S. aureus (MRSA).
Material and methods: A total of 130 clinical consecutive isolates of S. aureus were collected in Arkhangelsk during June–September 2004; 76(58%) and 54(42%) strains from in- and out-patients, respectively. Strains were identified as S. aureus with standard microbiological methods. Antimicrobial susceptibility testing was performed by agar disc diffusion (AB, BIODISK, Solna, Sweden) with the following antibiotics: gentamicin (GM), tetracyclin (TC), cefoxitin (FX), ciprofloxacin (CI), fucidic acid (FU), trimethoprim-sulfamethoxazole (TS), and with the double-disk test (erythromycin (EM) and clindamycin (CM)) for inducible MLS-resistance. Nitrocefin discs were used for beta-laktamase detection after induction with cefoxitin and/or oxacillin. The oxacillin (4 mg/L) agar method was used for MRSA screening. MRSA was confirmed by mecA and nuc PCR and further analysed by SmaI-pulsed-field gel electrophoresis (PFGE).
Results: A total of 102 strains (78%) were betalactamase positive. Other resistance prevalence rates were: TC (29%), EM (19%), CM (19%), CI (11%), GM (11%), TS (0%) and FU (0%). Thirteen strains (10%) were MRSA-screen positive, both with the oxacillin-agar test and the cefoxitin disc, and confirmed MRSA by mecA and nuc PCR. All MRSA strains were isolated from hospitalized patients and expressed multiple resistances. PFGE-analysis revealed that the MRSA-strains belonged three different PFGE-types. Type 1 consists of 8 strains from the department of general surgery and ICU. The type 2 group consisted of 3 strains from general surgery department. Finally, one strain from a patient at the Department of pulmonary medicine belonged to the type 3 group. We were not able to type one strain. MLST-typing of MRSA-strains will be performed.
Conclusion: (i) The high prevalence of resistance to penicillin (78%), TC (29%) as well as EM/CM (19%) and the low prevalence of resistance to TS and FU probably reflect the pattern of antibiotic use in the Arkhangelsk region. (ii) The prevalence of methicillin resistance was 10% and MRSA occurred only in hospital patients. (iii) MRSA strains expressed a multiple resistant profile and clustered in three different PFGE-types.
P1003: Validation of the MRSA protocol in a district health board in New Zealand, which has remained free of endemic MRSA in its hospitals
M.I. Schousboe, T. Anderson, L. Seaward (Christchurch, NZ)
Objective: Analysis of key variables important for the detection of MRSA in colonised Health care workers and patients. Three variables were evaluated:
-
•
Adequacy of specimen collection
-
•
Relevance of sampling multiple body sites for MRSA culture.
-
•
The role of the selective enrichment broth in recovery of MRSA from swabs.
Material and methods: The MRSA screening protocol requires bacterial swab samples from Nose, Groin, Perineum, and any wounds. The Microbiological procedure for processing of swabs were: 1. Inoculation onto 5% sheep blood agar (SBA) to detect presence of normal bacterial flora 2. Direct inoculation onto MRSA selective media 3. Incubation in a selective enrichment broth which was subcultured onto MRSA selective media. 4. Inoculated media processed at 24 and 48 hours. Archived computer records of positive MRSA cultures from 1995-2004 were used to analyse the relevance of sampling multiple sites. A subset population (1999–2000) was further analysed for laboratory factors.
Results: During 1999 and 2000, 4500 and 5700 MRSA screens were submitted respectively per year. 1.2–1.6 % of screens had at least one body site with no growth on the SBA. The nose swab represented 0.6–0.7% of such screens while other sites ranged from 0.2–0.5%.531 persons had positive MRSA cultures in the period 1995–2004. Of these, 127 (23.9%) had one positive wound culture on the 1st MRSA screen. The remaining 404 (76.1%) persons had at least one screening body site positive. The nose screen was positive in 282 (69.8 %) while an extra 122 (30.2 %) was detected from other sites only. During 1999 to 2000, 41 new MRSA positive patients were detected. 18 (44%) were detected on direct inoculated MRSA selective media but 23 (56%) were isolated from an enrichment broth only.
Conclusion: The control of MRSA is dependent upon the reliable detection from screening swabs and adequate Infection control procedures in dealing with colonised persons. This review documents some of the variables that influence the Microbiology Laboratory's ability to recover MRSA from colonised patients and staff. It is important not only to sample the nares but to screen additional sites and samples must be subcultured through an enrichment broth for maximum sensitivity.
P1004: Comparison of patient and environmental strains of MRSA using PFGE
E. O'Neill, T. Sexton, T. Dillane, P. Clarke, J. O'Gara, E. Smyth, H. Humphreys (Dublin, IRL)
Objectives: Environmental cleaning and decontamination of horizontal surfaces reduces airborne spread of methicillin-resistant Staphylococcus aureus (MRSA). Failure to eradicate from environmental sources in clinical areas is recognized as contributing to persistence and continued spread. We investigated the relationship between the patient and the environment over time in the rooms of patients in isolation for MRSA.
Methods: Over a two year period we collected environmental samples in rooms of patients in isolation for MRSA in Beaumont hospital which is a 600 bed tertiary referral centre in Dublin, Ireland. Environmental samples were collected by either air sampling or environmental swabs of horizontal surfaces in the patient's room. Using pulsed-field gel electrophoresis (PFGE) we compared patients’ strain of MRSA with two environmental strains of MRSA collected from the same room at the beginning and end of the patients stay. Gel analysis was performed by visual interpretation of the banding patterns and use of a computer software programme to generate a dendogram.
Results: A total of 20 patient isolates were compared with their corresponding environmental isolates. 5 patients had only one environmental isolate collected due to short duration of stay in the room or subsequent environmental samples not yielding MRSA. PFGE was therefore performed on a total of 55 isolates. PFGE illustrated identical or similar relationships in 14/20 (70%) of the patient and environmental sub-groups analysed.
Conclusion: The findings of this study represent an ongoing potential source of endemic MRSA in our hospital and emphasises the importance of enhanced environmental cleaning as part of an effective programme of MRSA control.
P1005: Methicillin-resistant Staphylococcus aureus colonisation and its association with infection in infants hospitalised at neonatal intensive care units
Y.C. Huang, L.-H. Su, Y.H. Chou, R.I. Lien, T.Y. Lin (Kweishan, Taoyuan, TW)
Objectives: To assess the association between methicillin-resistant Staphylococcus aureus (MRSA) colonization and infection in infants hospitalized at MRSA-endemic neonatal intensive care units (NICUs).
Methods: During March 2003 and February 2004, the infants admitted to our NICUs-1 and 2 were included in this study and specimens from the naris, postauricular area, axilla and umbilicus were obtained weekly for the detection of MRSA. All the colonized and clinical isolates from each study infant were further genotyped with pulsed-field gel electrophoresis (PFGE) with Sma-1 digestion.
Results: A total of 793 infants were included in this study. MRSA colonization was detected in 331 infants (42%) during NICU stay and 89% were detected by the first 2 samplings. Naris (71%) and umbilicus (60%) were the 2 most common sites of colonization. Clinical MRSA isolates were identified from 92 infants (12%). Among the 92 infants, MRSA colonization, either preceding or later acquiring, was noted in 84 infants (91%). 121 clinical isolates from 64 infants with 84 episodes of possible MRSA infection were available for genotyping analysis. Prior colonization was detected in 68 episodes (81%), among which both the colonized and clinical isolates were indistinguishable in 63 episodes (93%), highly related in 2 episodes and distinct in 3 episodes. Among the 16 episodes without prior colonization, colonization was acquired following infection in 9 episodes (53%), among which indistinguishable or highly related colonized strain was acquired in 6 episodes.
Conclusion: More than 40% of hospitalized infants were colonized with MRSA during their stay in MRSA-endemic NICUs. Most infants with MRSA clinical isolates had prior colonization of the same strain.
P1006: Phage typing of Belgian MRSA isolates (2003): two new epidemic phage types
C. Wildemauwe, C. Godard, R. Vanhoof (Brussels, B)
Objectives: In 2002, in Belgium, a methicillin-resistant Staphylococcus aureus (MRSA) frequency of 28% was estimated. Since several years, the National Reference Centre for Phage Typing has followed the evolution of the phage type patterns and has seen a continual evolution among these patterns. In this work, we show the phage type distribution found in 2003 and newly recognized epidemic phage types.
Methods: 2169 MRSA isolates of hospitalized patients were examined. Phage typing was done with the International Typing Set (ITS) at Routine Test Dilution (RTD) and 100RTD. The Minimal Inhibitory Concentration (MIC) of oxacillin was done by plate test.
Results: Of the 2169 isolates, only 73 isolates (3%) were not typable with the ITS, though a low number (21%) was typable at RTD. The phage type groups [A] and [C], at RTD, were still present with 7 (<1%) and 93 (4%) isolates belonging to [A] and [C] respectively. The majority of the isolates (40%) belonged to the phage type group [J]* at 100RTD. The phage group [O]* was detected in 18% of the isolates. The group ‘Other’ represented 34% and in this group, two phage types were rather significant: 29/(42E)/54/(D11)* (123 isolates) and HK2* (55 isolates). The oxacillin MICs of those two phage types were high (>256mg/L and 256mg/L respectively). They appeared in 9 and 8 hospitals respectively.
Conclusions: The increasing importance op MRSA, associated with hospital outbreaks, has been recognized in many countries. The determination of MRSA strains remains an important tool to control MRSA problems. With this in mind, we followed, in Belgium, during several years, the phage type patterns of Belgian MRSA isolates. We obtained, until now, a good typability of our isolates at least at the 100 fold concentration, whereas low typability of MRSA with the phage typing technique has been mentioned in other countries. The high prevalence of phage type groups [J]* and [O]* is in agreement with the results found in the 2002 survey. Striking phage types in 2003 were: 29/(42 E)/54/(D 11)*, already noticed in 2002 but at a rather low frequency, and HK2*. Both types became epidemic. To follow the local and/or temporal MRSA epidemiology in Belgium, phage typing remains a good, cheap and reliable method.
P1007: Empirical treatment of serious infections due to health care-related methicillin-resistant Staphylococcus aureus
J. Rodríguez-Baño, A.B. Milán, M.A. Domínguez, B. Almirante, E. Cercenado, B. Padilla, M. Pujol on behalf of GEIH/GEMARA/REIPI
Objectives: To analyze the empirical treatment in a series of infections due to health care- associated methicillin-resistant Staphylococcus aureus (MRSA) and the variables associates with inappropriate empirical treatment.
Methods: Prospective cohort of cases of MRSA infection from 60 hospitals in Spain during June 2003. Cases of MRSA infections were included in this analysis if the patients presented with systemic inflammatory response syndrome (SIRS) and/or invasive infection. Empirical treatment was considered inappropriate if the patient did not received any active antimicrobial agent (according to in vitro susceptibility data) during the first 48 hours after the onset of the infection. Percentages were compared by the chi-squared test. Relative risks and their 95% interval confidence were calculated.
Results: During the study period, there were 370 cases of colonization/infection due to health-care associated MRSA; 118 cases presented with SIRS and/or had an invasive infection and were included. The more frequent types of infections were: skin and soft tissues, 33%; pneumonia, 19%; catheter infection, 17%, and primary bacteraemia, 10%; 42% of the cases were bacteremic; 16% presented with severe sepsis or septic shock. With regard to the type of units of admission: ICU, 22%; medical services 41%, and surgical services 37%. Crude mortality was 32%, and infection-related mortality was 23%. The most frequent empirical antimicrobials were: betalactams, 63%; glycopeptides, 24%, fluorquinolones, 22%; aminoglycosides, 10%. Empirical treatment was considered inappropriate in 77%. The following variables were associated with increased risk of receiving inappropriate empirical treatment: neoplasia (RR = 1.2, p = 0.04), <7 days of previous stay (RR = 1.2, p = 0.01); the following variables were associated with diminished risk: chronic renal disease (RR = 0.5, p = 0.006), hemodialysis (RR = 0.3, p = 0.03), ICU admission (RR = 0.6, p = 0.006), central venous catheter (RR = 0.6, p = 0.001), previous antimicrobial treatment (RR =0.8, p = 0.05).
Conclusions: Inappropriate empirical antimicrobial treatment is frequent among patients with serious infections due to MRSA and is more frequent in patients with neoplasia or shorter previous stay. ICU patients, renal disease, hemodialysis, central venous catheter and previous antimicrobial use were associated with diminished risk of inappropriate empirical treatment.
P1008: Correlation of antimicrobial use and MRSA rates: data from the project Surveillance of Antimicrobial Use and Antimicrobial Resistance in Intensive Care Units (SARI)
E. Meyer, F. Schwab, D. Jonas, P. Gastmeier, H. Rüden, F.D. Daschner (Freiburg, Berlin, Hannover, D)
Objectives: To analyse MRSA rates and antimicrobial consumption in intensive care units (ICUs) participating in the SARI surveillance system from 2000–2003; to look for temporal changes and to establish differences between ICUs with increasing and ICUs with decreasing MRSA rates over three years.
Methods: Prospective unit and laboratory based surveillance in 38 German ICUs from 2000–2003. Antimicrobial use was defined by defined daily doses per 1000 patient days (pd); temporal changes in individual ICUs were calculated by Wilcoxon signed rank test.
Results: From 2/2000–12/2003, 38 ICUs reported data on 499.694 pd, 9.552 S. aureus isolates, including 2.249 MRSA, and 660.029 DDDs of antimicrobials. Cumulative MRSA rates ranged from 0% - 64.4% with a mean of 23.6%, the MRSA rate/1000pd ranged from 0-38.2 with a mean of 2.77. MRSA rates and imipenem and ciprofloxacin use data showed a positive correlation (p < 0.05). Overall, comparison of the years 2001 and 2003 showed that MRSA rates had increased in 18 (median 13.2%, range 1.6%–38.4%) and decreased in 14 ICUs (median 12%, range 1.0%–48.4%). Increased use of third generation cephalosporins, glycopeptides or aminoglycosides correlated significantly with the increase in MRSA rates. Cumulative nosocomial MRSA infections/1000pd in 141 ICUs without feedback data showed an increase over three years from 0.26 to 0.35 while SARI-ICUs were able to decrease their rate from 0.63 to 0.40.
Conclusion: The MRSA situation in German ICUs is still heterogeneous. Ciprofloxacin and imipenem use correlated significantly with MRSA rates. Increased use of third generation cephalosporins, glycopeptides or aminoglycosides correlated significantly with the increase in MRSA rates. Further studies are required to substantiate findings that no change in MRSA rate and a decrease in MRSA incidence in SARI-ICUs reflect the impact of an active surveillance system.
P1009: Analysis of epidemiological situation of MRSA infections in selected hospitals in the Czech Republic
B. Mackova, P. Urbaskova, O. Melter (Prague, CZ)
Objectives: Infections caused by MRSA (methicillin-resistant Staphylococcus aureus) have been historically considered as hospital infections. Nevertheless, MRSA is becoming increasingly involved in community infections as well. The incidence of MRSA infections in the Czech Republic varies widely with the regions and population groups.
Methods: Since 2000 the Czech Republic has been taking part in the European Antimicrobial Resistance Surveillance System monitoring the incidence of five pathogens in invasive isolates from blood and cerebrospinal fluid. One of the causative agents under surveillance is Staphylococcus aureus. The incidence of MRSA has been monitored in blood specimens from 95 hospitals of the Czech Republic. Data on patients, hospitals and phenotypes of antibiotic resistance in the bacterial strains isolated have been recorded. We used genetic methods for analysis of selected strains. Basic statistical methods are used for epidemiological analysis.
Results: Between 2000–2003, 4144 Staphylococcus aureus strains were analysed. Out of these strains, 5.7% were MRSA (see Table). The incidence of MRSA varied with types of hospitals, hospital wards, age groups and time. Geographical distribution of MRSA strains in the Czech Republic was mapped. Thanks to collaboration of 47 laboratories, highly valid data covering 82 % of the Czech population have been available.
| Year | S. aureus | MRSA |
|---|---|---|
| 2000 | 525 | 20 (3.8%) |
| 2001 | 1091 | 63 (5.8%) |
| 2002 | 1188 | 70 (5.9%) |
| 2003 | 1408 | 88 (6,2%) |
| Total | 4212 | 241 (5.7%) |
Conclusion: Surveillance of MRSA strains as a basis for active antibiotic policy has become of increasing concern to both health care providers in hospitals and community general practitioners. There is a need for better awareness of MRSA infections among both health care professionals and the public. The incidence of MRSA infections in last years in the Czech Republic shows a slightly increasing trend. Very interesting is local distribution of MRSA strains. The development of the incidence of MRSA infections in their spread will be the subject of further study.
P1010: Comparison of phenotypic typing methods and PFGE of methicillin resistant S. aureus isolated from two university hospitals in Thailand
C. Chomvarin, K. Chaicumpar, S. Srigulbutr (Khon Kaen, TH)
Objectives: Comparison of phenotypic typing methods and genotypic typing method to differentiate MRSA isolates obtained from the two University hospital in Thailand.
Methods: Seventy-four MRSA isolates were randomly collected from the two University hospital (central and northeastern) in Thailand. They were confirmed with the presence of mecA gene. Antibiograms, phage typing and enterotoxin productions were used for the phenotypic typing analysis. Pulsed-field gel electrophoresis (PFGE) with SmaI digestion of chromosomal DNA was used for the genotypic typing analysis.
Results: We found 19 distinct profiles by phenotypic typing methods and 18 PFGE types designed as 5 major types (A to E) and 13 subtypes. The most frequently types and their related subtypes found in both hospital, were A and C with represented 54.1% and 27%, respectively. All isolates resistant to penicillin, cephalosporin, erythromycin, gentamicin, kanamycin, tetracycline and oxacillin; and variably resistant to cotrimoxazole, lincomycin, chloramphenicol, ciprofloxacin. All isolates were susceptible to vancomycin and fosfomycin. Ten (13.5%) MRSA isolates produced enterotoxin A. Forty-five (60.8%) isolates were nontypable by phage typing method. No significant correlation between the phenotypic typing methods and the genotypic typing method were found.
Conclusions: The phenotypic typing methods were not significantly correlated with the genotypic typing (PFGE). Our results demonstrated that PFGE types A and C were the common endemic MRSA clone of both hospitals in Thailand.
P1011: Risk factors for intensive care unit – acquired MRSA infections
N. Öztoprak, M.A Çevik, E. Akinci, M. Korkmaz, A. Erbay, S.S Eren, N. Balaban, H. Bodur Ankara, TR
Objectives: MRSA infections are frequent in intensive care units (ICUs) of our hospital. A prospective study was implemented to investigate the risk factors for ICU - acquired MRSA infections.
Methods: This study was conducted in surgical and neurological ICUs from May to October 2003. The patients staying at ICU more than 48 hours were included in the study. All of the patients were visited daily and data were recorded on individual forms for each patient until discharge or death. Nasal swab cultures were done in 48 hours of ICU admission and repeated every week until the patients colonizied with MRSA or discharged. ICU-acquired MRSA infections were defined according to the criteria of CDC in which MRSA was isolated as causative agent. SPSS-10 was used for all statistical analyses.
Results: Overall 249 patients were included in the study. Male patients accounted for 143 (57.4 %) of the patients. Mean age was 52.1 + 23.2 years and mean hospitalization period in ICU was 6.45 + 9.3 days. MRSA infection was detected in 21 (8.4 %) of these patients. The most frequent infection was primary blood stream infection (74 %). It was followed by pneumoniae (38 %) and surgical site infection (14 %). Nasal MRSA colonization was detected in 58 patients and 12 of them (20.7%) developed MRSA infection. The following parametres were found significant (p < 0.05) risk factors for MRSA infection in univariate analysis:Hospitalization period in ICU, intra-abdominal and orthopedics pathologies, central venous catheter insertion, entubation, mechanical ventilation, total parenteral nutrition, previous antibiotic use, nasal MRSA colonization and presence of more than two patients having nasal colonization in the same ICU at the same time. In multivariate analysis; hospitalization period in ICU (OR:1.090, 95%CI:1.038–1.144, p:0.001), central venous catheter insertion (OR:1.822, 95%CI:1.095–3.033, p:0.021), previous antibiotic use (OR:2.337, 95%CI:1.326–4.119, p:0.003) and presence of more than two patients having nasal colonization in the same ICU at the same time (OR:1.398, 95%CI:1.020–1.917, p:0.037) were independently associated with MRSA infection.
Conclusion: Prolonged hospitalization, central venous catheter insertion, previous antibiotic use and nasal MRSA colonization are the risk factors for MRSA infection in ICUs.
P1012: Genotypes of methicillin-resistant Staphylococcus aureus isolated from neonates: the same genotypes of well-known CA-MRSA strains
K.S. Ko, S. Park, S. Kim, W.S. Oh, J.-H. Song, K.R. Peck (Seoul, KOR)
Objective: To investigate the molecular characteristics of methicillin-resistant Staphylococcus aureus (MRSA) strains isolated from neonates transferred from primary care obstetric clinics.
Methods: Twelve MRSA strains were isolated from 11 neonates in 2004. Ten MRSA strains were also isolated from nurses and facilities in corresponding primary care obstetric clinics. Molecular features of MRSA strains were analysed by using multilocus sequence typing (MLST, arcC-aroE-glpF-gmk-pta-tpi-yqiL), spa typing, and SCCmec typing. Presence of Panton-Valentine leukocidin (PVL) gene was investigated by PCR method.
Results: All 22 MRSA strains analysed in this study contained SCCmec type IVA. Of six isolates from neonates of clinic A, five showed ST1 (1-1-1-1-1-1-1) and resistance to only gentamicin and tetracycline. The remaining one showed novel ST (25-1-1-1-1-1-1), shared with one isolate from nurse of clinic A. Four MRSA strains from neonates of clinic B showed ST1 (1-1-1-1-1-1-1) and resistance to erythromycin and gentamicin, which is the same characteristics with three isolates from nurses and environment of clinic B. The other two MRSA strains from neonates of clinic B showed ST493 (62-1-1-1-1-1-1), which is shared by six strains from nurses and environment of clinic B. spa type of these 22 MRSA strains was identical as UJEBKBP and all strains were negative for PVL gene.
Conclusion: MRSA strains isolated from neonates, hospital workers, and environment of the same primary care obstetric clinics showed genotypes not found commonly in hospital-acquired MRSA (HA-MRSA) strains, instead represented close relatedness with those of CA-MRSA strains. This suggests that CA-MRSA can spread by mediation of primary clinics with low antibiotic pressure, and there is a possibility that CA-MRSA is transmitted into hospitals.
P1013: Band-based versus sequence-based typing: comparison of typing results for Staphylococcus aureus obtained from PFGE and spa typing
B. Strommenger, C. Kettlitz, B. Pasemann, G. Werner, J. Rothgänger, D. Harmsen, W. Witte (Wernigerode, Würzburg, Münster, D)
Objectives: Over the last years there has been a dramatic increase in the prevalence of methicillin- and multiresistant Staphylococcus aureus (MRSA) leading to a major health problem, especially in the nosocomial setting. To support infection control measures typing of MRSA is essential. The present ‘gold standard’ for strain typing is pulsed field gel electrophoresis (PFGE), but several sequence based methods including spa typing have recently been introduced. Therefore this study was initiated to compare typing results obtained from PFGE with those from spa typing.
Methods: 90 well characterized S. aureus strains of different evolutionary origin including methicillin sensitive and resistant isolates were included. Strains were selected from a variety of clonal groups prevalent in Germany and middle Europe during the last ten years. The collection comprised hospital derived strains as well as isolates from the community, including the recently emerging community acquired MRSA. All isolates were subjected to PFGE with subsequent cluster analysis; additionally the polymorphic X-region of the protein A gene was sequenced and a spa type was assigned using the Ridom StaphType software. The newly developed algorithm BURP (based upon repeat patterns) was applied to the spa sequences to cluster the resulting spa types into different groups. Clustering results were compared to those obtained from PFGE and MLST.
Results: Overall the results obtained from the different typing approaches were in agreement. In some cases where PFGE results were inconsistent despite uniform epidemiological background spa typing was able to group the corresponding strains together. Only two strongly related epidemic clones could not be separated by spa typing.
Conclusion: Spa typing in combination with BURP analysis is an easy, rapid and reliable method for epidemiological analyses in S. aureus. It is superior to PFGE in cases where PFGE might be ‘overdiscriminatory’. In rare cases a second discriminatory locus (for example a single MLST locus) might be helpful for an ultimate classification.
P1014: The antibiotic susceptibility of methicillin-resistant Staphylococcus aureus
L. Gavriliu, G.A. Popescu, E. Benea, C. Popescu, G. Badea, M. Ivan, M. Popoiu, S. Botea (Bucharest, RO)
Methicillin-resistant staphylococci (MRSA) are often multidrug resistant and represent a major problem for the antimicrobial therapy. Glicopeptides are the golden standard for these infections but resistance and toxicity concerns limit their usage. MRSA antibiotic resistance may be divided into two distinctive profiles: multidrug resistance (probably nosocomial infections) and variable resistance, usually to 1 or 2 non-betalactamic antibiotics (often correlated with community-related MRSA infections).
Objective: To characterize the susceptibility of MRSA to non-betalactamic antibiotics, in order to evaluate the therapeutical alternatives when a MRSA infection is suspected.
Methods: A retrospective study of 65 MRSA strains isolated and drug-susceptibility tested in ‘Matei Bals’ Institute of Infectious Diseases in 2003.
Results: The most active of all the tested antibiotics proved to be linezolid (100%), vancomycin (95.48%) and clindamycin (77.58%) and less active were tetracycline (16.08%), cloramphenycol (33.3%), rifampin (45.65%) and fluorquinolones (42.3%).25 MRSA isolated strains (38.46%) were sensible to less than 4 antibiotics; the most active have been linezolid (100%) and vancomycin (95.48% - two VISA strains). For the 40 MRSA more sensible strains, the efficiency was similar for linezolid, vancomycin (1 strain VISA), clindamycin (90%) and trimethoprim/sulfamethoxazole (77.56%).
Conclusions: The therapeutic alternatives are linezolid and glicopeptides, for nosocomial or health-related infections, TMP/SMX and clindamycin, for community-acquirred infections. The decision to use one of these should be correlated to the clinical findings.
P1015: Associated factors and mortality in elderly patients with methicillin-resistant vs. methicillin-susceptible Staphylococcus aureus bacteraemia
B. Marí, G. Serrate, M. Canals, G. Bejarano, M. Barè, E. Antón, F. Segura (Sabadell, E)
Objectives: To assess the impact of methicillin-resistance on selected aspects of the infectious process and outcome in patients over 65 years of age with S. aureus bacteraemia.
Methods: Prospective case-control study of patients older than 65 years with methicillin-resistant S. aureus (MRSA) or methicillin-susceptible S. aureus (MSSA) bacteraemia, matched for age and sex. Microbiologically documented bloodstream infections between 1997 and 2004 were used to search for patients. Death was attributed to the infection if it occurred before the resolution of symptoms or within 7 days of the onset of bacteraemia in the absence of other explanations.
Results: There were 51 patients in each group. Mean age was 77.2 + 7 and most (68.6%) were male. Bacteremia was hospital-0acquired in 51%. Differential characteristics of patients are shown in the table 1 A quarter of the patients in each group had a Barthel Index < 55. A high-risk source of bacteremia was observed in 17% of the MRSA group and 23% of MSSA (p = NS). No differences were found between groups for in-hospital mortality (45% vs 41%) or for mortality associated with bacteremia (29% vs 27%). The results of the univariate analyses of the association between clinical variables and associated mortality are show in the table 2. MRSA was not an independent predictor of mortality. In the logistic regression analysis, inappropriate therapy and high-risk source of bacteraemia were independently associated with mortality due to bacteraemia.
| Clinical characteristic | MSSA % | MRSA % | P |
|---|---|---|---|
| Diabetes | 29 | 49 | 0.04 |
| COPD | 12 | 39 | 0.001 |
| Sore | 10 | 37 | 0.001 |
| Hemodialysis | 28 | 72 | 0.03 |
| Prior hospitalization | 25 | 51 | 0.008 |
| Median duration of stay prior to bacteremia (d) | 8 | 19 | 0.03 |
| Prior antibiotic therapy | 31 | 72 | 0.0001 |
| Inappropriate empirical therapy | 90 | 62 | 0.001 |
| Associated-mortality |
|||
|---|---|---|---|
| Clinical characteristic | Yes (n = 29) % | No (n = 73) % | P |
| MRSA | 48 | 51 | 0.82 |
| Barthel index ≤ 55 | 43 | 20 | 0.02 |
| Median duration of stay prior to bacteremia (d) | 22 | 10 | 0.04 |
| High-risk source of bacteremia | 34 | 15 | 0.08 |
| Inappropriate empirical therapy | 39 | 19 | 0.03 |
Conclusions: Our results confirm that MRSA bacteraemia is associated to factors previously reported to predispose to MRSA infection. In our series of elderly patients, high-risk source of bacteraemia and inappropriate therapy were related to increased mortality due to S. aureus bacteraemia, regardless of whether the bacteria were susceptible or resistant to methicillin.
P1016: Failure to control MRSA in LTCF by restricting admissions or implementing strict isolation procedures
C. Petignat, M. Attinger, D. Blanc, P. Francioli (Lausanne, CH)
The optimal strategy to control the circulation of MRSA between acute care and long-term care facilities (LTCF) is not well defined. The study region has 2 acute care facilities (ACF)one of which being a tertiary care centre (CHUV) and over 50 LTCFs. The vast majority of LTCFs denied admission to MRSA patients until repeated cultures were negative. The few LTCFs accepting MRSA patients would implement strict isolation measures. In 2001 this strategy induced increasing problems for the transfer of patients from ACFs to LTCFs, due to the fact that ACFs experienced an abrupt increase in the total number of new MRSA cases (approx 30-40 cases per year until 2001, over 230 cases after 2001). The goal of the study performed in 2003 was to investigate if the present strategy indeed ‘protected’ the LTCFs from MRSA and what was the role of LCFTs as a potential reservior for MRSA for the ACFs. A prevalence survey performed in 993 residents of 17 LTCFs showed that 39 residents (5.3%) were MRSA carriers, of which only 5 were previously identified. All but 2 LTCFs hosted positive patients. Nine residents had never previously been hospitalised. None of the nine MRSA carriers who were observed for one year, developed MRSA infection. On the other hand, the rate of MRSA carriers on admission at the ACFs in 2002 was 13/418 (3%) for patients transferred from LTCFs, as compared to 131/30.000 admissions (0.4%) for those from other healthcare facilities or from home. Molecular typing showed the 5 different genotypes were circulating in the region.
Conclusions: Most of the MRSA carriers in LTCFs were not previously known, indicating that the control strategy was at least partially ineffective. The results also indicate that colonised LTCF residents appear to be at low risk of developing infection, in the absence of predisposing conditions. This led to the modification of the control strategy for MRSA in the region: no special MRSA control measures in LTCFs except for standard precautions unless obvious predisposing factors for infection or planned hospitalisation, screening of patients transferred from LTCFs in acute-care hospitals.
Antibiotic-resistant pneumococci and streptococci
P1017: Pneumococcal resistance surveillance in Canada, 1993–2004
K. Green, S. Pong-Porter, D.E. Low for the Canadian Bacterial Surveillance Network
Objectives: To monitor resistance trends in Canadian isolates of Streptococcus pneumoniae (SP).
Methods: The Canadian Bacterial Surveillance Network is a collaborative network of microbiology laboratories from across Canada that submit bacterial isolates to a central laboratory for standardized antimicrobial susceptibility testing. Since 1993, 192 laboratories have submitted 22,531 SP isolates to the central study lab where susceptibility testing was performed according to NCCLS protocols.
Results: Of the 22,531 SP isolates tested, 37.5% were from blood/CSF, 33% from sputum, 17.1% from eyes, and 7.2% from ears. The trends in antimicrobial susceptibility are expressed below as percentage resistant (R). Rates of ciprofloxacin (Cip) and levofloxacin (Lev) use increased annually since 1993 with Cip use peaking at 51/1000 pop'n in 2000 and Lev at 14.3/1000 pop'n in 2001. Subsequently Cip use has stabilized at 48/1000 pop'n and Lev use has decreased modestly to 13/1000 pop'n in 2003. In 2003 we observed the first significant decrease in Cip and Lev resistance rates since their introduction to market; (Cip 2.7%–1.8% p = 0.02; Lev 1.9%–1.2%, p = 0.04). Preliminary data from 2004 show another increase in 2004 (Cip 2.3%, p = ns; Lev 1.8%, p = ns). Despite decreased macrolide use, rates of macrolide resistance continue to rise as evidenced by the erythromycin resistance rates of 14%, 16%, and 17.7% (Chisq for trend 10.2, p = 0.001) in 2002, 2003 and 2004 respectively.
| 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pen NS | 5.7 | 8.1 | 8.8 | 12.2 | 13.4 | 14.8 | 13.6 | 12.6 | 14.5 | 15.2 | 14.6 | 15.0 |
| Pen R | 0.9 | 1.3 | 2.2 | 4.1 | 6.5 | 5.6 | 5.9 | 5.9 | 6.9 | 6.5 | 6.2 | 5.6 |
| Eryth R | 1.9 | 3.4 | 3.1 | 5.1 | 6.8 | 10.5 | 10.0 | 11.2 | 12.9 | 14.0 | 16.0 | 17.7 |
| ClindaR | 0 | 1.7 | 1.3 | 2.4 | 3.6 | 5.1 | 4.9 | 5.6 | 5.8 | 6.5 | 7.4 | 8.0 |
| Tmp/Smx R | 3.8 | 4.6 | 9.6 | 12.6 | 14.7 | 12.0 | 12.0 | 11.4 | 11.9 | 13.2 | 13.3 | 14.0 |
| Tet R | 1.4 | 2.3 | 3.4 | 2.4 | 6.3 | 9.0 | 7.9 | 8.1 | 9.1 | 9.8 | 9.7 | 10.5 |
| Ceftriax R (mening) | 0 | 0.2 | 0.1 | 0.7 | 1.3 | 2.4 | 1.5 | 2.0 | 2.4 | 1.5 | 1.8 | 2.7 |
| Ceftriax R (non-mening) | 0 | 0.04 | 0 | 0.2 | 0.1 | 0.1 | 0.3 | 0.1 | 0.1 | 0.2 | 0.2 | 0.1 |
| Cipro R | 0.5 | 0.8 | 0.7 | 0.8 | 1.8 | 1.8 | 1.6 | 1.4 | 2.4 | 2.7 | 1.8 | 2.3 |
| Levo R | 0 | 0.4 | 0.1 | 0.2 | 0.5 | 0.3 | 0.4 | 0.9 | 1.2 | 1.9 | 1.2 | 1.8 |
| Moxi R | NT | NT | 0 | 0 | 0.3 | 0.2 | 0.2 | 0.4 | 0.4 | 0.3 | 0.4 | 0.8 |
Conclusions: Data from 2004 show no statistically significant changes in rates of resistance for any class of antibiotics with the exception of macrolides. This trend of continued increasing rates of macrolide resistance is of concern. Although rates of flouroquinolone resistance decreased significantly in 2003, preliminary analysis of 2004 data suggests that resistance rates may be increasing again in 2004. These trends need to be monitored further to determine if these changing patterns of resistance continue.
P1018: Phenotypic and genotypic resistance to macrolides in S. pneumonia and S. pyogenes – a nationwide surveillance
K. Ekeund, A.M. Hammerum, B. Gahrn-Hansen, M. Kaltoft (Copenhagen, Odense, DK)
Objectives: Erythromycin is the second drug of choice used for treatment of infections caused by Streptococcus pneumoniae (S. pn) and Streptococcus pyogenes (S. pyo). Knowledge of resistance towards the most often used antibiotics is very important since fast and effective treatment is needed to reduce morbidity and of course mortality. erm(B) encodes macrolide/lincomycin/streptogramin resistance in S. pn and S. pyo whereas erm(A) only can be detected in S. pyo. Resistance resulting from efflux is mediated by a surface protein encoded by the mef(A) gene both in S. pn and S. pyo.
Methods: Between 1 January 2003 and 30 September 2004, a total of 2,183 invasive S. pn and 273 invasive S. pyo (mainly from blood) were collected from hospitals all over Denmark and send to the National Reference Centre for Streptococcus at Statens Serum Institut. During the same period, 217 noninvasive S. pyo isolates (pharyngitis and skin specimens) were received from the Department of Clinical Microbiology at Odense University Hospital. All isolates were examined at the National Reference Centre for Streptococcus at Statens Serum Institut. Susceptibility to erythromycin was determined by disc diffusion method for S. pn and S. pyo. In addition, MICs of erythromycin were determined by E-test for the erythromycin resistant isolates. Clindamycin resistance was determined by double disc diffusion test. The erythromycin resistant (ery-res.) isolates were tested for erm(A), erm(B) and mef(A) by PCR.
Results: In total, 4.5 % (98) of S. pn was resistant to erythromycin and 2.9% (8) of invasive and 4.6% (10) of non-invasive S. pyo were resistant to erythromycin. None of the isolates were resistant to clindamycin. Among the ery-res S. pn, the most frequent gene was mef(A) 83.7%, while erm(B) was found in 13.3%. In two isolates no resistance genes were identified. 81 out of 82 mef(A) carrying isolates had serotype 14.erm(A) and mef(A) was present in 62.5% and 37.5% of the invasive ery-res. S. pyo isolates. None of the isolates were positive for erm(B). In non-invasive ery-res. S. pyo isolates 40%, 10%, 50% were PCR-positive for erm(A), erm(B) and mef(A) respectively.
Conclusion: In contrast to S. pyo, ery-res. S. pn is dominated by one serotype, carrying mef(A). The overall resistance profile of S. pn and S. pyo is still favourable, but the resistance to macrolides is of growing concern in Denmark.
P1019: Resistance in Streptococcus pneumoniae: AUC/MIC breakpoints differ between gatifloxacin, gemifloxacin, levofloxacin, and moxifloxacin
K. LaPlante, M. Rybak, B. Tsuji, G. Kaatz (Detroit, USA)
Objective: The potential for resistance development in Streptococcus pneumoniae (SP) secondary to varying exposure to gatifloxacin, gemifloxacin, levofloxacin, and moxifloxacin was examined at high inoculum (108.5–9 log 10 CFU/ml) over 96 hours in an in vitro pharmacodynamic model.
Methods: Various AUCfree/MIC exposures, 16 through 449 of the tested fluoroquinolones (FQ), were evaluated against two clinical (WT) FQ-susceptible isolates of SP (ATCC 49619; BSP 2443). Pharmacokinetics of each drug were simulated to match various areas under the concentration-time curve (AUCfree) for each FQ. The QRDR regions of GyrA and ParC of isolates with raised MICs were sequenced to identify mutations, if any.
Results: Gatifloxacin, gemifloxacin, levofloxacin, and moxifloxacin MICs for ATCC 49619 were 0.19, 0.03, 0.75, and 0.125 mg/L, respectively, and for BSP 2443, the corresponding results were 0.25, 0.03 0.75, 0.25 mg/L. Simulated free gatifloxacin exposure led to S52G, S79Y, and N91D parC & S81Y and S114G gyrA mutations at AUCfree/MIC of 35 & 60, (corresponding to doses of 100 & 198 mg). Gemifloxacin exposure led to S52G, S79Y, and N91D parC & S114G gyrA mutations at AUCfree/MIC of 37 (corresponding to a free dose of 50 mg). Leqwvofloxacin AUCfree/MIC of 55 through 86 (corresponding to doses of 500 mg through 843.5 mg/day) led to isolation of S79Y parC & S81Y and E85G gyrA mutants as early as 32 hrs. Moxifloxacin exposure led to S52G, S79Y, and N91D parC & S81Y gyrA mutations at AUCfree/MIC of 16–32 (corresponding to free doses of 50–75 mg). For each compound evaluated, a delay of first- & second-step mutants was observed with increasingly higher AUCfree/MIC ratios.
| Agent | AUC/MICffree Breakpoint to Prevent Resistance | Corresponding dose | Recommended Dosages |
|---|---|---|---|
| Gatifloxacin | >66 ± 10 | 175 mg to 235 mg | 400 mg qd |
| Gemifloxacin | ≥50.5 ± 2.0 | 75 mg | 320 mg qd |
| Levofloxacin | ≥97 ± 0.0 | 843.5 to 875 mg | 500–750 mg qd |
| Moxifloxacin | ≥31 ± 0.1 | 100 mg | 400 mg qd |
Conclusions: Recovery of topoisomerase mutations in SP was related to the AUCfree/MIC exposure. Clinical doses of gatifloxacin, gemifloxacin, and moxifloxacin exceed the AUC/MIC-free resistance breakpoint against WT SP. The cited exposure breakpoints differed between FQs & may be related to structural differences within the class.
P1020: Serotype 11A prevalence and clonal diversity in Streptococcus pneumoniae isolated from children attending day-care centres in Lisbon, Portugal
N.G. Sousa, S. Nunes, N. Frazão, R. Sá-Leão, H. de Lencastre (Lisbon, P)
Objectives: The characterization of 1172 drug-susceptible Streptococcus pneumoniae (DSPn) isolates from carriage and recovered from the nasopharynx of children attending eight day-care centres in the Lisbon area, during 2001–2003, showed that serotype 11A was the second most prevalent (12.0%) just preceded by serotype 6A (13.8%). Since serotype 11A was rarely found (0.2%) among the 2,067 drug-resistant isolates we have previously characterized from collections recovered between 1996 and 2003 in the same geographical area, in the present study, we aimed to assess the genetic diversity of serotype 11A DSPn isolates.
Methods: Isolates were characterized by pulsed-field gel electrophoresis (PFGE) after SmaI restriction of total DNA. PFGE patterns were analysed with Bionumerics software.
Results: The molecular analysis of one hundred and forty serotype 11A DSPn isolates revealed six clonal types. However, the vast majority (95%) belonged to a single clone. The prevalence of this dominant clone during the study ranged from 6.3% to 13.9% and it was disseminated in all day-care centres.
Conclusions: Serotype 11A is not a capsular type with an important representation in drug-resistant collections which are the most commonly studied worldwide. However, it seems to be common among DSPn strains. This serotype 11A collection showed little genetic variability. In fact, one genotype was found to be dominant and disseminated successfully in all day-care centres studied. These findings suggest that this serotype 11A clone is frequent in colonization and thus its monitoring is of importance particularly after the introduction of the seven-valent pneumococcal conjugate vaccine.
P1021: New cefotaxime/ceftriaxone NCCLS susceptibility breakpoints: effect on reported Streptococcus pneumoniae resistance in European surveillance
N. Bruinsma, G. Kahlmeter, E. Tiemersma, J.C.M. Monen, H. Grundmann on behalf of EARSS participants
Objectives: In January 2003, the National Committee for Clinical Laboratory Standards (NCCLS) finalised new cefotaxime and ceftriaxone susceptibility breakpoints for S. pneumoniae (SPN) isolates. The majority (70%) of the laboratories that participate in the European Antimicrobial Resistance Surveillance System (NCCLS) use NCCLS guidelines.
Methods: Since 1999 EARSS collects routine antimicrobial susceptibility results of invasive SPN isolates from blood or cerebrospinal fluid (CSF). According to the EARSS protocol laboratories report cefotaxime and/or ceftriaxone minimal inhibitory concentrations (MICs) for penicillin non-susceptible SPN isolates (PNSP). The former NCCLS criteria of MIC breakpoints for cefotaxime and ceftriaxone were ≤ 0.5 (Susceptible), 1 (Intermediate), and ≥ 2 μg/ml (Resistant). The new criteria of MIC breakpoints for non-CSF isolates (mainly blood isolates) are ≤1 (S), 2 (I), and ≥ 4 μg/ml (R). In the present study, the proportion of cefotaxime resistance based on the MICs reported to EARSS according to the former and new NCCLS guidelines were compared.
Results: In the period 1999–2002, cefotaxime MICs were reported for 2034 of the 2710 PNSP isolates, mostly isolated from blood (92%). Interpreting the MIC values according to the former NCCLS guideline resulted in an overall proportion I, and R of 20.9% and 3.8% respectively. Interpreting the MIC values according to the new NCCLS guidelines resulted in an overall proportion I, R of 4.3% and 0.5% respectively.
Conclusions: The proportion of cefotaxime resistance among PNSP when interpreted by the new NCCLS guideline decreased almost 7–fold. The rates from those countries that do not use NCCLS guidelines were unchanged since breakpoints from the national breakpoints committees in Europe were unchanged. The effect of change of cefotaxime breakpoints implemented by NCCLS illustrates that caution is needed when comparing data according to S, I, R interpretation.
P1022: The International Circumpolar Surveillance System for population-based surveillance of invasive pneumococcal disease 1999–2003
M. Bruce, T. Cottle, D. Parks, S.L. Deeks, T. Tam, M. Lovgren, L. Jette, K.G. Kristinsson, G. Sigmundsdottir, K. Brinklov Jensen, O. Lovoll, P. Nuorti, E. Herva, A. Koch, T. Hennessy, A.J. Parkinson (Anchorage, USA; Toronto, Ottawa, Edmonton, Quebec, CAN; Reykjavik, IS; Nuuk, GRL; Oslo, N; Helsinki, Oulu, FIN; Copenhagen, DK)
Background: The International Circumpolar Surveillance (ICS) Project is a population-based surveillance network for invasive bacterial disease in the US Arctic, Alaska (AK), Northern Canada (N Can), Greenland (GN), Iceland (IC), Norway (Nor) and Finland (Fin). Among circumpolar countries, the 7-valent conjugate vaccine (pcv7) has been used for routine infant immunization in AK since 2001 and in selected areas in N Can since 2002.
Methods: We defined a case of invasive pneumococcal disease (IPD) as illness in a surveillance area resident with isolation of Streptococcus pneumoniae from a normally-sterile site. We analysed data on IPD from AK and N Can (Jan 1999–Dec 2003), and from GN, IC, Nor, Fin (Jan 2000–Dec 2003) to determine: 1) Common clinical syndromes, 2) Rates of disease by country, 3) Serotype distribution and 4) Antimicrobial susceptibility patterns.
Results: A total of 7196 cases of laboratory-confirmed IPD were reported from AK (547), N Can (195), GN (38), IC (183), Nor (3664), and Fin (2569). Case-fatality ratios varied from 5.0–22.0%. Pneumonia (46%), septicemia (28%), and meningitis (8%) were the most common clinical presentations. Rates of IPD in aboriginals in AK and N Can were 42 and 38 cases per 100,000 persons, respectively. Rates of IPD in children <2 years of age and persons >2 years of age ranged from 35–144 and 8–24 cases per 100,000 persons, respectively. In AK, the rate of IPD in children <2 with pcv7 serotypes declined by 85% after routine vaccination; from 137 in 1999–2000 to 21 in 2001–2003 (p < 0.001). Rates of non-pcv7 serotypes in AK increased from 26 in 1999–2000 to 49 in 2001–2003 in children <2 years of age (p = 06). Overall, 89% of isolates from persons >2 years of age were serotypes contained in the 23-valent polysaccharide vaccine. The proportion of isolates fully-resistant to penicillin varied by country from <1% in Fin to 7.5% in AK.
Conclusions: Rates of IPD are high in aboriginals and children <2 years of age residing in Arctic countries. After introduction of pcv7 in AK, rates of disease in children <2 years of age with pcv7 serotypes rapidly declined; however, increasing rates of non pcv7 serotypes are concerning and merit further surveillance. Continued surveillance is needed to determine the impact of pcv7 in AK and areas of N Can. High IPD rates in children <2 warrant consideration of pcv7 use in other circumpolar countries.
P1023: Phenotypic and genotypic diversity of penicillin non-susceptible pneumococci isolated from nasopharynx of children in Lublin, Poland
I. Korona-Glowniak, A. Malm (Lublin, PL)
Objectives: Currently, the most penicillin non-susceptible Streptococcus pneumoniae (PNSP) isolates belong to serotypes 6B, 9V, 14, 19F and 23F. Majority of them have also acquired resistance to other drugs, including erythromycin, chloramphenicol, trimethoprim-sulfamethoxazole, and tetracycline. It was shown that young children have a high carriage rate of PNSP which suggests the critical role of nasopharynx of children, particularly those of pre-school age and attending day care centres (DCCs), in the emergence and spread of resistant to penicillin and to other drugs S. pneumoniae. Epidemiological typing of S. pneumoniae is essential to determine strain relatedness and also to trace resistant clones. The antimicrobial resistance, serotyping and BOX PCR assay were used for characterization of the clonal relationship of PNSP isolates from nasopharynx of children attending 4 DCCs in Lublin, Poland.
Methods: Nasopharyngeal isolates of 56 PNSP had been isolated from 241 children attending 4 DCCs between May and June 2002. Susceptibility to penicillin (P), erythromycin (E), clindamycin (CC), tetracycline (Te), chloramphenicol (C) or trimethoprim-sulfamethoxazole (SXT), and capsular serotypes were determined. Clonal relationship between isolates was investigated by BOX PCR assay using the Box A primer.
Results: All of the isolated PNSP strains belonged to paediatric serotypes 6B (12.5%), 9V (5.4%), 14 (53.6%) and 19F (28. 6%). 9 strains showed high level resistance (PenR) and 47 strains – low level resistance (PenI) to penicillin. MIC 50/90 (mg/L) were determined to penicillin 1.0/1.0 and cefotaxime 0.38/0.5. All of the strains from serotypes 6B and 19F have the same drug resistant phenotype PECCTeCSXT, whereas 18 strains of serotype 14 were resistant to P and 12 strains – to PSXT. 3 isolates of serotype 9V have PSXT resistance pattern. When genotypic method was used 4, 8, 5 and 1 different patterns were identified among 14, 19F, 6B and 9V serotypes, respectively. The isolates of serotype 14 were very clonal irrespective of DCCs, while isolates of serotypes 19F and 6B showed greater genetic diversity but within the same DCC higher similarity of genotypes was found.
Conclusions: Clonal spreading of S. pneumoniae among children attending the same DCC indicates that local PNSP strains can also easily disseminate in the community. In addition, there is need to monitor an appearance and extension of the major international resistant clones of pneumococci in Poland.
P1024: Genetic diversity of Streptococcus pneumoniae resistant strains isolated in Western Pomeranian Region of Poland in 2001–2003
M. Nowosiad, M. Mnichowska, S. Giedrys-Kalemba (Szczecin, PL)
Introduction: Streptococcus pneumoniae is a main causative agent of upper respiratory tract infections and severe systemic diseases. An abrupt antimicrobial resistance increase and clonal spread of resistant pneumococcal strains has resulted in serious therapeutic problems in recent years. The aim of this study was to analyze resistance patterns and genetic diversity of S. pneumoniae resistant strains isolated in our region during three years (2001–2003).
Methods: Using E-test method and the NCCLS criteria for benzylpenicillin (P), erythromycin (E), clindamycin (L), tetracycline (T), cotrimoxazole (S), ceftriaxone (C), chloramphenicol (H), vankomycin (W), imipenem (I), fifty nine resistant or intermediate to at least one drug strains were obtained. Strains were submitted to molecular characteristic by PFGE with SmaI restriction enzyme and computer analysis using Molecular Analyst software application. For each strain resistance pattern and PFGE profile was determined.
Results: Resistance to 8 out of 9 determined antibiotics (except vancomycin) was described. Strains showed 22 different resistance patterns and TSH (13%strains), PSI (11.8%) and ELTS (10.1%) were the most often. Resistance degree reached 7 drugs (5% strains) and 69% strains were MDR. We have found 26 PFGE profiles: 15 of them (U 1–15) were unique single isolates, 11 clusters (A-K) were represented by 2–10 strains, which were more than 78% of similar. The most numerous clusters (A-K) consists of strains that were isolated over three years of study and showed the same or very similar resistant patterns: A-TSH (8 of 10 strains), TH (2); B-PSI (7 of 8), S (1); C-PELSHI (3 of 6), PTSHI (2), PTSCHI (1); D-ELTS (3 of 4), ELS (1); E-SH (2 of 4), TS (1), T (1). All strains of TSH and PSI resistance patterns were found in one cluster A(A1–A9) or D (D1–D6) respectively but strains with ELTS and PELSHI patterns belonged to different (2–3) clusters and unique PFGE profiles. Another clusters (F–K) were represented by two strains with different resistant patterns each.
Conclusions: Population of S. pneumoniae resistant strains in our region presents high genetic diversity and numerous different resistance patterns. The majority of strains with the same resistance pattern showed different PFGE profiles but there were observed some strains of the same resistance pattern, which belonged to only one cluster and were isolated over three years of study.
P1025: Characterisation of penicillin-resistant Streptococcus pneumoniae circulating in Italy during 2000–2003
D.L. Rocca, L. Gualco, A. Marchese, G.C. Schito (Genoa, I)
Objective: Recent epidemiological surveys have shown increasing resistance to penicillin in pneumococci circulating in our Country (from <5% in 1992 to >20% in 2003). This phenomenon has worsened in the last two years. Because only limited data on the molecular characterization of these strains are available, the present study was aimed at providing more information on this subject.
Methods: 139 S. pneumoniae refractory to penicillin isolated recently (2000–2003) from 23 centres widely distributed in Italy and causing respiratory infections have been analysed for antibiotic susceptibility (broth microdilution method, NCCLS 2004) and chromosomal relatedness (pulsed-field gel electrophoresis: PFGE). Serotyping was done by the capsular reaction using commercially available sera.
Results: Lack of susceptibility to other drugs among strains possessing high-level resistance to penicillin (HLPR) (74/139, 53.2%) was: erythromycin 58.1%, clindamycin 40.5%, tetracycline 43.2%, co-trimoxazole 85.1% and chloramphenicol 49.7%. Among low-level penicillin resistant isolates (LLPR) (65/139, 46.7%) 63.1, 44.6, 66.1, 38.5 and 23.1% were refractory to erythromycin, clindamycin, tetracycline, co-trimoxazole and chloramphenicol respectively. After PFGE analysis, 49 of 74 (66.2%) HLPR strains showed a profile identical or related to two epidemic clones: Spain23F-1 and Spain9V-3. The remaining HLPR pneumococci belonged to unique or rare clones. LLPR isolates were characterised by more variable backgrounds in terms of PFGE patterns and serotypes than HLPR strains. In fact, 27.7% showed an identical or related profile (arbitrarily called D, serotype 15A) previously not described in Italy and 10 (15.4%) exhibited the PFGE patterns typical or related to the Spain23F-1 and Spain9V-3 clones. The remaining 37 LLPR isolates (56.9%) belonged to 22 different profiles and to 11 distinct serotypes. In this study, the 23F ‘Italian clone’ circulating in 1993–1996 was not found.
Conclusions: The recent increase of total penicillin-resistance in Italy can be ascribed to the emergence of a new clone and to the diffusion of two well known international clones, whose ability to spread is higher than that of the autochthonous Italian clone described in 1996. Changing antibiotic prescribing habits, including the recent strict limitation to the consumption of parenteral drugs, may also explain the variations described.
P1026: Characterisation of macrolide-resistant Streptococcus pneumoniae isolated in Austria
S. Forsthuber, H. Lagler, K. Stich, W. Graninger, A. Georgopoulos (Vienna, A)
Objectives: The aim of this study was (i) to evaluate the in vitro activity of antimicrobial agents against erythromycin resistant Streptococcus pneumoniae (ERSP) and (ii) to detect the genetic mechanisms of macrolide, penicillin and tetracycline resistance.
Methods: Fifty-seven ERSP were isolated from 20 adults and 37 children between 2002 and 2003. MICs to erythromycin (ERY), clarithromycin (CLA), azithromycin (AZM), josamycin (JOS), clindamycin (CLI), telithromycin (TEL), penicillin (PEN), cefpodoxime (CPD), cefotaxime (CTX), linezolid (LNZ), quinupristin/dalfopristin (Q-D), ciprofloxacin (CIP), levofloxacin (LVX), gatifloxacin (GAT), moxifloxacin (MXF) and tetracycline (TET) were determined by the broth microdilution method according to NCCLS. Macrolide resistance phenotype (c-MLSB, i-MLSB, M) was characterized by using a triple-disk test with ERY, JOS and CLI. Species identification (ply, lytA, psaA) and detection of genes coding for resistance to macrolide (ermB, ermTR, mefE), penicillin (pbp1A, pbp2B) and tetracycline (tetM, tetO) were done by PCR.
Results: Following macrolide phenotype/genotype distribution was found: 24 (42%) with c-MLSB/16 ermB, 2 ermB + mefE; 8 (14%) with i-MLSB/4 ermB, 2 ermB + mefE, 1 ermTR; 25 (44%) with M/23 mefE. 20 strains showed reduced susceptibility to PEN (with altered pbp1A and/or pbp2B) and 29 ERSP were resistant to TET (24 tetM, 1 tetO). 19 isolates (33%) demonstrated MDR (multidrug resistance, defined as resistance to three or more different classes of antimicrobials), however all ERSP were sensitive (100%) to TEL, LNZ, LVX, GAT, MXF.
Conclusions: (i) MefE was the most common macrolide resistance gene although ermB was also often present. (ii) One third of ERSP strains were multidrug resistant. (iii) New antibiotics like TEL have shown excellent activity against these strains.
P1027: Streptococcus pneumoniae invasive disease. Study of susceptibility to frequently used antimicrobial drugs over a 4-year period
S. Solis del Baño, A. San Pedro Garrido, A. Sanchez Garcia, I. Gestoso, J.J. Picazo (Madrid, E)
Objectives: Study the incidence of S. pneumoniae invasive disease in the health district of our hospital (600,000 inhabitants) between March 2001 and October 2004, and the prevalence of resistance to the main antimicrobial drugs (penicillin, cefotaxime and erythromycin).
Material and methods: Retrospective analysis of 143 isolates of S. pneumoniae in blood and CSF during the study period at the Hospital Clínico San Carlos, Madrid (1130 beds). We studied the seasonal and age-group distribution (0–15 years, 16–65, >65 years). Sensitivity to antimicrobial drugs was measured following NCCLS criteria.
Results: During the study period, 143 strains of S. pneumoniae were isolated: 6 (4.2 %) in CSF and 137 (95.8%) in blood. Total incidence was 6 cases/100,000 inhabitants/year, with maximum incidence in winter and spring. The largest number of cases, 76 (54%), were in the over 65s. In children, 11 (7.7%) were detected, all in the under 5s. The total number of strains whose sensitivity to penicillin fell was 43 (30%), of which 20 (46.5%) had an MIC 2 mg/ml. 46.5% of the penicillin-resistant strains were also resistant to erythromycin. 16 (11%)/143 had reduced sensitivity to cefotaxime, and most of these (63%) had intermediate sensitivity. Resistance to erythromycin was detected in 34 (24%). During the study period, resistance to antibiotics decreased gradually in such a way that the resistance percentages each year were: penicillin 41%, 30%, 27%, 23%; cefotaxime 28%, 14%, 4%, 4%; erythromycin 34%, 19%, 29%, 8%. No differences were observed in the resistance percentage in the different age groups.
Conclusions: The prevalence of CSF and blood strains of S. pneumoniae with reduced sensitivity to penicillin in this study was 30%. The treatment of choice in S. pneumoniae invasive disease was third-generation cephalosporins, due to their low level of resistance. Resistance to the main antimicrobials from this type of strain has fallen. During the study period, resistance to penicillin fell by 43.9%, 58.5% for cefotaxime 63.4% for erythromycin. The fall in resistance among invasive S. pneumoniae could be due to vaccination in children and the elderly from 2002 onwards, since the vaccination includes the most common and resistant serotypes. The low number of isolates in children could be due to the low number of samples processed.
P1028: Change in distribution of macrolide-resistant Streptococcus pneumoniae genotypes over 4 years – data from PROTEKT 1999–2003
D.J. Farrell on behalf of the PROTEKT Study Group
Objectives: This analysis of data from 39 countries over the first 4 years (1999–2003) of the PROTEKT global surveillance study was undertaken to investigate longitudinal and regional trends in the distribution of macrolide resistance mechanisms among Streptococcus pneumoniae, and the susceptibility of these isolates to antibacterials, including the ketolide telithromycin.
Methods: Isolates were tested centrally for antibacterial susceptibility using NCCLS methodology; macrolide (erythromycin-resistant [ERY-R; MIC ≥1 mg/L]) isolates were genotyped using PCR.
Results: Overall, 31.4% (1077/3435) of S. pneumoniae isolates in Year (Y) 1 (1999–2000), 32.7% (1391/4256) in Y2 (2000–2001), 36.9% (2329/6320) in Y3 (2001–002) and 36.4% (2451/6739) in Y4 (2002–003) were ERY-R. erm(B) alone or mef(A) alone were the most prevalent macrolide resistance genotypes, accounting for 58.5% and 30.9% of all ERY-R isolates over the 4 years, respectively. erm(B) was particularly common in France and Spain (95.3% and 91.2%, respectively, overall), whereas mef(A) predominated in Latin American countries and the USA. While the proportion of ERY-R isolates with erm(B) or mef(A) alone was stable between 1999 and 2003, the proportion positive for both genes increased from 6.6% in Y1 to 10.5% in Y4 (Y2, 5.0%; Y3, 10.2%). In Y4, dual erm(B)/mef(A) strains were particularly prevalent in South Korea (26.0%), South Africa (40.0%) and the USA (22.3%). Overall, 46.6% of ERY-R isolates were resistant to penicillin (MIC ≥2 m/L) and a further 22.3% exhibited intermediate susceptibility (MIC 0.12–1 mg/L) to this agent. Co-resistance to other antibacterials was markedly high in dual erm(B)/mef(A) isolates (penicillin, 89.8%; cotrimoxazole, 82.2%; tetracycline, 97.2%). Telithromycin continued to exhibit potent activity against ERY-R S. pneumoniae, irrespective of their genotype: 99.1% of erm(B), 100% of mef(A) and 99.2% of erm(B)/mef(A) isolates collected over the 4 years were fully susceptible (MIC ≤1 mg/L) to this antibacterial.
Conclusions: The marked geographic variability in the distribution of macrolide resistance genotypes among S. pneumoniae isolates highlights the need for continued international surveillance. Isolates positive for both erm(B) and mef(A) exhibit high rates of multidrug resistance and are increasing in prevalence in most regions. Telithromycin remains highly active against macrolide-resistant S. pneumoniae isolates, regardless of genotype.
P1029: Changes in the global distribution of Streptococcus pneumoniae serotypes from paediatric isolates collected in PROTEKT Year 1 (Y1; 1999–2000) compared to Year 4 (Y4; 2002–2003)
D.J. Farrell, S.G. Jenkins, R.R. Reinert (London, UK; Charlotte, USA; Aachen, D)
Objectives: The 7-valent formulation of the pneumococcal conjugate vaccine (PCV7) was introduced in the USA in February 2000. There is a general recommendation for its use in all children <2 years of age, and the vaccine is licensed for children up to 5 years of age. In Europe, the vaccine is licensed for children up to 5 years of age, but most countries do not have a general recommendation for use. PROTEKT – a global, longitudinal study of the antimicrobial susceptibility of bacterial respiratory tract pathogens – has now completed its fourth year. A comparison was made between serotype distribution and PCV7 coverage between Y1 and Y4.
Methods: Analysis was performed only on Streptococcus pneumoniae isolates obtained from paediatric patients at the 31 centres common to both years (Y1, n = 553; Y4, n = 682). Serotyping was performed by Neufeld's Quellung reaction using Statens Serum Institute antisera (SSI, Denmark).
Results: PCV7 coverage decreased from 67.7% and 62.5% in Y1 to 51.0% and 41.0% in Y4 in the USA and Latin America, respectively (Chi-squared; p = <0.001 and 0.007, respectively). Serotypes that showed the greatest increase (Y1, Y4) in the USA were 19A (7.0%, 22.2%), 6A (1.8%, 9.9%), 3 (1.8%, 6.2%), 15 (1.8%, 6.2%), and 11 (0%, 6.2%). In Brazil, a similar pattern was seen although there was no change in the proportion of isolates with the 19A serotype. In contrast, no change in serotype distribution was observed in Canada, Western Europe, and the Far East, where the PCV7 vaccine is not routinely used for paediatric vaccination.
Conclusions: Results from this analysis of PROTEKT data indicate that the proportion of S. pneumoniae isolates from paediatric patients covered by the PCV7 vaccine has decreased significantly over 4 years in regions where the vaccine is routinely used. Other serotypes, such as 19A, which is known to be highly resistant to antimicrobials and is not covered by PCV7, have increased in these regions. This study demonstrates the importance of serotyping antimicrobial surveillance study isolates in order to monitor such changes and any potential future implications for therapy and vaccine formulations.
P1030: Population structure and MURm gene analysis of early and contemporary high penicillin resistant Streptococcus pneumoniae isolates in Spain
R. Del Campo, M.I. Morosini, A. Fenoll, E. Gómez G-de la Pedrosa, J. Liñares, F. Cafini, F. Baquero, R. Cantón, J. Prieto on behalf of the Spanish Pneumococcal Infection Network
Background: Sequential alterations in PBP sequences constitute the classical mechanism to acquire penicillin resistance in S. pneumoniae, that is reflected in changes in the cell wall peptidoglycan structure. murM gene controls the addition of the first amino acid of the dipeptide bridge of the pneumococcal muropeptide. Mutations in this gene are apparently required for high penicillin and cefotaxime resistance. The aim of this study was to compare the murM gene sequence within the earlier and the latest highly penicillin resistant pneumococcal populations recovered in Spain.
Material and methods: A total of 56 S. pneumoniae isolates (10 of them from 1987–88 and 46 from 2002–04) with resistance to penicillin (MIC 2–8 μg/ml) were included. Susceptibility to different β-lactams, macrolides, tetracycline, levofloxacin, chloramphenicol, and trimethoprim-sulfamethoxazole (SxT) were determined by the agar dilution method. All isolates were grouped according to serotype and pulsotype (PFGE-SmaI pattern) and the murM gene was sequenced.
Results: A high percentage of resistance (intermediate plus resistant) was observed for cefotaxime (100%) and SxT (96.6%). All isolates remained susceptible to telithromycin but not to levofloxacin (93% of susceptibility). All isolates recovered during 1987–88 were genetically unrelated and mainly belonged to serotypes 23F (40%) and 6B (40%). In contrast, the most frequent serotypes during 2002–04 were 14 (30%), 9V (26%), and 6B (17%). In this period, a predominant Spain9V-3clone was detected in 10 out of 14 isolates of serotype 14, and in 11 out of 12 isolates of serotype 9V (capsular switch). All 8 isolates of serotype 6B belonged to a single clone (Spain6B-2). The analysis of murM sequences of isolates from both periods revealed the existence of different alleles. Homologous sequences to the murMA (identical to that described for R6 penicillin susceptible strain), were replaced in part by murMB5, and murMB6 (different variants of these alleles were detected in our collection).
Conclusion: Early high penicillin resistant S. pneumoniae isolates in Spain were genetically unrelated and corresponding to 23F and 6B serotypes. On the contrary, recent isolates showed dissemination of selected clones, particularly Spain9V-3. Many S. pneumoniae isolates with high-level resistance to penicillin retain (or reacquired) the murM gene of susceptible strains, but different allelic variants was also detected.
P1031: mef(E) and mef(A) gene characterisation in Spanish Streptococcus pneumoniae clinical isolates
E. Gómez G-de la Pedrosa, M.I. Morosini, J.C. Gakán, R. del Campo, E. Loza, F. Baquero, R. Cantón (Madrid, E)
Objectives: To determine among 712 S. pneumoniae clinical isolates recovered from different Spanish hospitals during three different periods (1999–2000, 2001–2002 and 2002–2003) the prevalence of erythromycin resistance phenotypes and resistance genes associated to this resistance.
Methods: Susceptibility testing was performed by the standard microdilution technique (NCCLS). A PCR assay was carried out to identified erythromycin resistance genes (erm or mef) and a multiplex-PCR was designed to distinguish between mef(A) and mef(E) genes within mef positive isolates. Clonality was studied using the Sma-I-PFGE technique.
Results: Resistance values (intermediate plus resistant isolates) during the studied period ranged from 48.3% (first studied period) to 45.2% (third studied period) for penicillin, 39% (first studied period) to 32.9% (third studied period) for erythromycin, and 32% (first studied period) to 30.3% (third studied period) for clindamycin. Levofloxacin resistance was only found in 2.4% of isolates and were recovered during the third studied period. M phenotype was observed in 3.2% of all tested isolates. Considering non-susceptible erythromycin isolates, ermB and mef genes was found in 87.1% and 9.5% of isolates, respectively, as a sole erythromycin resistance gene. The concomitant presence of both determinants was found in 3.3% of isolates. Interestingly, among the isolates with mef PCR positive result, only one (3.2%) carried the mef(A) gene whereas the mef(E) gene was detected in the others (96.8%). An increase in mef prevalence was observed between the first and the second studied periods (2% to 5.8%) and a slightly decrease (4.9%) in the third period. PFGE analysis revealed a polyclonal structure of mef positive isolates.
Conclusions: Prevalence of mef positive isolates among erythromycin-resistant strains remains low in our country (4.3%) being the mef(E) gene the most prevalent mef determinant among these isolates (96.8%).
P1032: Molecular mechanisms of tetracycline resistance and clonal diversity of Streptococcus pneumoniae isolated from respiratory tract infections in Poland
R. Izdebski, E. Sadowy, W. Hryniewicz (Warsaw, PL)
Objectives: The objective of this project was to study molecular mechanisms of tetracycline resistance and clonal diversity of tetracycline-resistant Streptococcus pneumoniae isolated in Poland to clarify which mechanism predominates in the strikingly high spread of tetracycline resistance in the Polish population of S. pneumoniae.
Methods: Eight hundred and nineteen clinical isolates of S. pneumoniae from respiratory tract infections collected in Poland between 1998 and 2003 were investigated by disk diffusion method for tetracycline susceptibility as recommended by the NCCLS. Serotyping of resistant isolates was performed by capsule swelling reaction (Statens Serum Institut, Denmark) and PCR. Clonality of the resistant isolates was studied by PFGE of SmaI-digested bacterial DNA. Selected isolates representing main PFGE types were analysed by the multilocus sequence typing (MLST). Resistance determinants (tetM, tetO) were detected by PCR.
Results: Two hundred and fifty two (30,8%) isolates were non-susceptible to tetracycline. The majority of isolates (49.6%) possessed serotype 19F (69 isolates) or 23F (56 isolates). Serotype 19F isolates had 12 PFGE types. The main type in this group (55 isolates) had 8 subtypes. The representatives of the most numerous subtype (43 isolates – 17% of whole resistant isolates) had ST423. Isolates of the 23F serotype group had 21 PFGE types. Among isolates of 23F serotype STs 440 (16 isolates), 81 (Spain 23F-1; 13 isolates) and 173/272 (Poland 23F-16; 5 isolates) were identified. All isolates were positive for the tetM gene and one isolate carried additionally the tetO gene.
Conclusion: The observed high level of resistance to tetracycline among S. pneumoniae isolated in Poland is caused by spread of relatively few epidemic clones, harbouring the tetM gene as resistance determinant.
P1033: Streptococcus pneumoniae resistance in young children: differences between European countries
N. Bruinsma, W. Hryniewicz, K.G. Kristinsson, E. Tiemersma, J.C.M. Monen, H. Grundmann on behalf of EARSS participants
Objectives: The highest levels of erythromycin and penicillin resistance in S. pneumoniae (SPN) are found among isolates from young children that are most vulnerable to pneumococcal infections. In the present study, the prevalence of SPN resistance among young children (less than 5 years of age) reported to the European Antimicrobial Resistance Surveillance System (EARSS) was compared between countries.
Methods: The EARSS has been collecting routine antimicrobial susceptibility results of primary invasive SPN isolates from blood or cerebrospinal fluid (CSF) since 1999. The eight countries reporting more than 100 isolates for the under five-years-olds for the period 1999–2003 (Belgium, Denmark, Finland, Ireland, Netherlands, Sweden, United Kingdom, and Spain) were included in the analysis (total number of SPN isolates = 17,123). The proportion of resistance was described as the per cent of SPN with single penicillin (PEN) (non-susceptible), single erythromycin (ERY), or dual resistance.
Results: Among young children, single ERY resistance was most prominent in all countries, (from 6% in Sweden to 38% in Belgium), except for Spain where the proportion of dual resistance was highest (33%). For the other countries dual resistance among young children ranged from 0% in Denmark to 13% in Belgium. Except for Ireland (12%) and Spain (21%), single PEN resistance remained below 5%.
Conclusion: Between countries, large differences in the patterns of S. pneumoniae resistance were found among young children. ERY resistance was most common among young children, which may indicate greater use of macrolides in this age group. In order to assess the effectiveness of interventions like vaccination, resistance and serotype data should be monitored carefully.
P1034: Evolution in the pattern of sensitivity to penicillin and cefotaxime of Streptococcus pneumoniae
I. Bonilla, E. Martin, F. Lopez Fabal, A. San Pedro Garrido, F. De la Torre, J.J. Picazo (Madrid, E)
Background: The increase in resistance to penicillin, and more recently to cefotaxime, means that it is necessary to study the prevalence of resistance to these antibiotics, giving them huge clinical importance. This study compares the sensitivity of S. pneumoniae to penicillin and cefotaxime during 1991, 1995, 2000, 2001, 2002, 2003 and 2004.
Methods: A total of 892 strains of S.pneumoniae from significant respiratory tract isolates were studied. These corresponded to the years 1991(130); 1995(126); 2000(142); 2001(121); 2002(126); 2003(137) and 2004(110). MICs were determined according to National Committee for Clinical Laboratory Standars (NCCLS) guidelines. Break points for cefotaxime were established for non-meningeal infections (sensitivity ≤ 1, intermediate resistance = 2, resistance 4).
Results: The results are summarized in the following table:
| % Penicillin |
% Cefotaxime |
|||||
|---|---|---|---|---|---|---|
| S | I | R | S | I | R | |
| 1991 (n = 130) | 64.6 | 30.8 | 4.6 | 98.5 | 1.5 | 0 |
| 1995 (n = 126) | 66.7 | 30.1 | 3.2 | 99.2 | 0.8 | 0 |
| 2000 (n = 142) | 43.7 | 31.7 | 24.6 | 97.9 | 2.1 | 0 |
| 2001 (n = 121) | 51.2 | 29.8 | 19 | 95.1 | 4.1 | 0.8 |
| 2002 (n = 126) | 46.8 | 31 | 22.2 | 95.2 | 3.8 | 1 |
| 2003 (n = 137) | 40.1 | 55.5 | 4.4 | 95 | 4.4 | 0.6 |
| 2004 (n = 110) | 59 | 30 | 11 | 96.2 | 3.8 | 0 |
Conclusions: A five-fold increase in resistance to penicillin was observed with respect to the year the study started: 4.6% in 1991 to 22.2% in 2002. During the last two years, we observed a slight resistency decrease. This is probably due to increase of the vaccine use. The resistance profile of cefotaxime shows a slow but stable increase. Using breakpoints for meningeal infections, resistance increases significantly.
P1035: Sensitivity to different antimicrobials of S. pneumoniae isolated in a university hospital
E. Martin, A. San Pedro Garrido, A. Sanchez Garcia, S. Solis del Baño, F. De la Torre, J.J. Picazo (Madrid, E)
Background: S. pneumoniae is one the most important pathogens in respiratory tract infections. The use of the most common antibiotics such as penicillins, cephalosporins and macrolides has led to an increase in resistance. Consequently, new antimicrobial agents are needed.
Methods: We studied 350 strains of S. pneumoniae in clinical isolates from the respiratory tract during 2002, 2003 and 2004. A total of 41 strains were resistant to penicillin. The MICs for the 10 antibiotics (including new antimicrobial drugs) were tested according to National Committee for Clinical Laboratory Standards (NCCLS) guidelines.
Results: The results are expressed in the following table:
| Antibiotic | 2002 (n = 103) |
2003 (n = 137) |
2004 (n = 110) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| %S | %I | %R | %S | %I | %R | %S | %I | %R | |
| Penicillin | 46.6 | 31.1 | 22.3 | 39.5 | 55.5 | 5 | 59 | 30 | 11 |
| Amoxicilin-Clavulanic | 86.4 | 12.6 | 1 | 94.4 | 5 | 0.6 | 92.5 | 7.5 | 0 |
| Cefotaxime | 95.2 | 3.8 | 1 | 95 | 4.4 | 0.6 | 96.2 | 3.8 | 0 |
| Clarithromycin | 58.8 | 0 | 41.8 | 61.3 | 0 | 38.7 | 64.5 | 1 | 34.5 |
| Erythromycin | 56.9 | 0 | 43.1 | 59.8 | 1.4 | 38.8 | 64.5 | 0 | 35.5 |
| Levofloxacin | 96 | 3 | 1 | 97.8 | 0.7 | 1.5 | 100 | 0 | 0 |
| Moxifloxacin | 96 | 3 | 1 | 98.5 | 0 | 1.5 | 100 | 0 | 0 |
| Linezolid | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | 0 |
| Quinupristin-Dalfopristin | 94.2 | 5.8 | 0 | 100 | 0 | 0 | 99 | 1 | 0 |
| Vancomycin | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | 0 |
Conclusions: No strains resistant to vancomycin, linezolid or dalfopristin were found. For dalfopristin there is a 6% rate of intermediate strains during 2002, and 1% during 2004. Cefotaxime maintains a low level of resistance and intermediate sensitivity. The quinolones analysed may be a good alternative in the treatment of S. pneumoniae. New antimicrobial agents seem promising in treating infections caused by this pathogen.
P1036: Characterisation of the first telithromycin resistant pneumococcal isolate in Germany
A. Al-Lahham, N. Neuberger, S. Barbosa, I. Klawiter, M. van der Linden, C. Heeg, R.R. Reinert (Aachen, D)
Background: S. pneumoniae is a serious infectious agents of the respiratory tract and its resistance to new antibiotics is increasing worldwide. In this study, the first telithromycin resistant S. pneumoniae isolate in Germany was characterized.
Methods: In a German nationwide study including 16 clinical microbiological laboratories, a total of 206 S. pyogenes (pharyngitis and wound infections) and 485 S. pneumoniae (respiratory tract infections) isolates were colleced between January 2003 and April 2004. MICs of penicillin G (PEN), cefotaxime (CEF), erythromycin A (ERY), clindamycin (CLI), tetracycline (TET), quinupristin-dalfopristin (Q-D), telithromycin (TELI), and levofloxacin (LEV) were determined using the microdilution method according to the latest NCCLS guidelines. Macrolide resistant genotypes were checked by RT-PCR with the LightCycler and macrolide resistant phenotypes and sequencing of L4, L22, ermB and 23S rRNA were performed according to standard methods.
Results: Resistance rates of S. pyogenes isolates were as follows (I + R): PEN (0%), ERY (7.0%), CLI (0.5%), TET (7.0%), Q-D (0%) and TELI (1%). S. pneumoniae isolates showed the following resistance rates (I + R): PEN (7.2%), ERY (18.9%), CLI (5.3%), TET (11.3%), and TELI (0.2%). The new ketolide telithromycin was 99.8% active against S. pneumoniae isolates (MIC50 and MIC90 equal 0.016 mg/L and 0.125 mg/L, respectively). The telithromycin resistant pneumococcal strain showed 7 mutations in the 23S rRNA (T107G, A1745T, A1535G, 1513T, T1514A, A1530T, T1531A) and one amino acid alteration in L4 protein (T20G). The strain was serotype 15A and MLST 63. It was resistant to penicillin G, erythromycin A, clindamycin and tetracycline. 26 macrolide resistant strains of pneumococci (28.9%) harboured the ermB and 62 isolates (68.9%) had the mef A resistance determinants. Two macrolide resistant strains had neither ermB nor mefA. Two macrolide resistant S. pyogenes isolates (14.3%) had the ermB gene and were telithromycin resistant. Eleven S. pyogenes isolates (78.6%) contained the mefA resistance determinant and one strain (7.1%) contained the ermTR gene. Only two strains of S. pyogenes were inducible showing the iMLSB-C phenotype.
Conclusions: Telithromycin resistance was observed in a multiply resistant serotype 15A (ST63)isolate, which may have the potential for further spread in Germany.
P1037: Characterisation of quinolone-resistant Streptococcus pneumoniae isolates in Germany
A. Al-Lahham, M. ven der Linden, C. Heeg, R.R. Reinert (Aachen, D)
Background: S. pneumoniae belongs to the main human infectious agents worldwide. In several nationwide studies on resistance development in pneumococcal disease pneumococcal isolates were collected.
Methods: Strains were serotyped using Neufeld's Quellungreaction and MICs of penicillin G (PEN), cefotaxime (CEF), amoxicillen (AMOX), erythromycin A (ERY), clindamycin (CLI), tetracycline (TET), ciprofloxacin (CIP), levofloxacin (LEV), sparfloxacin (SPA), grepafloxacin (GRE), clinafloxacin (CLX), moxifloxacin (MOX), gatifloxacin (GAT) and gemifloxacin (GEM) were determined using the microdilution method according to the latest NCCLS guidelines. Flouroquinolone resistant genotypes were checked by PCR followed by DNA-sequencing of gyrA, gyrB, parC and parE according to standard methods.
Results: Between Jan. 1992 and Dec. 2003 10.700 isolates from 315 laboratories were included in this study. A total of 40 fluoroquinolone resistant strains (MIC CIP >2) were identified (0.3–0.8%). The predominant serotypes were 23F (17.5%) and 9N (10%). The moxifloxacin MIC50 of the resistant strains was 0.5 μg/ml. Most mutations leading to fluoroquinolone resistance were found in parC (corresponding amino acid positions: 78, 79, 80, 83, 91 and 137), and parE at amino acid positions 460 and 435. Only one strain was found to possess a gyrB mutation. 20 strains (50%) were analysed by MLST. Predominant sequence types were ST81 (10%), ST 9 (10%) and ST 66 (10%). MLST data of the isolates did not show clonal relatedness of quinolone resistance.
Conclusions: Fluoroquinolone resistant strains remain rare in Germany. A clonal relatedness of strains could not be affirmed using MLST.
P1038: Antimicrobial resistance of pneumococci isolated from the nasopharynx of healthy children and clinical isolates in Greece in 2004
I. Katsarolis, G. Poulakou, I. Matthaiopoulou, S. Tsiodras, E. Roilides, D.A. Kafetzis, I. Paraskakis, G.L. Daikos, V. Syriopoulou, S. Kanavaki, I. Kavaliotis, A. Kansouzidou, S. Leveidiotou, G. Samonis, I. Pneumatikos, H. Giamarellou on behalf of the Hellenic Study Group for the Susceptibility of Streptococcus pneumoniae 2004
Objective: To present data from a nation-wide surveillance study on the susceptibility of Streptococcus pneumoniae strains from nasopharyngeal colonization (NPC)and from patients with pneumococcal infections in year 2004.
Methods: Nasopharyngeal sampling from healthy children (2–6 years old) attending day-centres was performed from February to May 2004. Clinical strains were also collected during the same period in the collaborating laboratories. Pneumococci were identified by use of optochin sensitivity, bile solubility and slide agglutination (Pneumolatex) assays. Susceptibility testing was performed for penicillin (PG), ceftriaxone (CXT), erythromycin (ERY), tetracycline (TET), cotrimoxazole (COT), levofloxacin and moxifloxacin by E-test. Ciprofloxacin (CIP) MICs were measured only in the NPC strains. NCCLS methodology and breakpoints for intermediate resistance (IR) and resistance (R) were used. The breakpoint used for CIP resistance was ≥4 mg/L.
Results: A total of 762 NPC pneumococcal strains and 35 clinical strains were studied. For the NPC strains, results for IR and R respectively per antibiotic (as %) were: PG (20.3/14.8), CXT (0.8/0.1), ERY (0.8/33), TET (1.6/24.8), COT (18.7/25.6), CIP (3.7). Twenty-eight NPC PG resistant strains (i.e. 3.7%) had an MIC≥4 mg/L, (range 4–8). PG and EM R strains account for 10.5% of the total. Susceptibility patterns varied among different geographic departments. For the clinical isolates, results were as follows: PG (14.3/11.4), CXT (0/0), EM (5.7/22.9), TET (3/12.1), COT (14.7/17.6). No resistance to the respiratory fluoroquinolones was observed in both groups.
Conclusions: Data suggest an increasing trend in the resistance rates for both penicillin and erythromycin. Results from the colonizing and the clinical strains had good correlation, although clinical strains had lower resistance rates. Respiratory fluoroquinolones did not display resistance in vitro, but the emergence of CIP resistant colonizing strains needs further evaluation and attention. Despite increasing trends in resistance, the low number of strains beyond clinical resistance cut-offs (MIC for PG >4 mg/L) render beta-lactams still potent agents against pneumococcal disease.
P1039: Susceptibility of pneumococci causing meningitis in England and Wales to recommended antimicrobials, 2001–2003
N. Potz, M. Warner, U. Gungabissoon, R. George, D. Livermore, R. Pebody, A. Johnson (London, UK)
Objectives: Streptococcus pneumoniae is the second commonest cause of bacterial meningitis in the UK after Neisseria meningitis. The present national recommendations for treatment of pneumococcal meningitis in the UK is cefotaxime, with penicillin substituted if the isolate proves to be susceptible in laboratory tests. In cases involving cephalosporin-resistant pneumococci, cefotaxime should be supplemented with vancomycin or rifampicin. Resistance to these antibiotics was investigated for the period 2001–2003.
Methods: Cases of pneumococcal meningitis reported routinely to the Health Protection Agency were reconciled with cases identified from reference laboratory submissions of pneumococci during 2001-2003. Inclusion criteria were cases where S. pneumoniae was isolated from CSF, and those where pneumococci were isolated from blood with meningitis given as a clinical diagnosis.
Results: A total of 813 cases of pneumococcal meningitis were identified in England and Wales. Of the 673 case reports submitted, 433 were accompanied by penicillin susceptibility data, with 26 cases (3.9%) indicating reduced penicillin susceptibility. Only one of the 549 isolates (0.2%) with cefotaxime susceptibility data was reported as resistant. No resistance to rifampicin or vancomycin was reported. Among the referred isolates with reduced penicillin susceptibility, the commonest serotypes were 9V, 14and 6B.
Conclusions: This study provides a reasonably robust estimate of the prevalence of antibiotic resistance for pneumococcal meningitis in England and Wales during 2001–2003. Results obtained show that resistance to cefotaxime, the recommended empirical treatment for pneumococcal meningitis, was very low during this period.
P1040: Antibiotic resistance among invasive pneumococcal isolates from Southwest Sweden 1998–2001
E. Backhaus, S. Berg, B. Trollfors, B.E.B. Claesson, R. Andersson (Skövde, Göteborg, S)
Objectives: Streptococcus pneumoniae is a major human pathogen. In Southwest Sweden, with a population of 1.8 million, 200 patients are diagnosed each year with invasive pneumococcal disease. The rapid emergence of isolates with decreased susceptibility to several antibiotics is an increasing problem in many parts of the world. The aim of the present study was to investigate the pattern of susceptibility among invasive isolates, in order to see if the current treatment policies are appropriate, and to see if there seems to be a trend of increasing antibiotic resistance.
Methods: All clinical isolates of S. pneumoniae from blood, cerebrospinal and joint fluid were collected at the laboratories in Göteborg, Skövde, Borås, Uddevalla and Halmstad during 1998–2001. The MIC-values for seven commonly used antibiotics (penicillin G, erythromycin, clindamycin, tetracycline, moxifloxacin, cotrimoxazole and cefotaxime) were determined with E-test (AB Biodisk) according to standard methods.
Results: 868 invasive strains were tested. Of these, 808 were fully susceptible and 60 were classified as Indeterminate (I) or Resistant (R) for any of the tested antibiotics, according to the Swedish Reference Group for Antibiotics system of species related breakpoints. No isolate had a MIC >1.0 mg/L against penicillin (R). 15 (1.7%) isolates had MIC ≥0.5 mg/L and 8 isolates had MIC's between 0.094 and 0.38 mg/L. Among these 23 isolates classified as I to penicillin (MIC >0.06, ≤1.0 mg/L), 16 isolates were also I against cefotaxime (MIC <0.12, ≤1.0 mg/L) (1.8%). The other tested antibiotics showed the following results: Erythromycin R (MIC >0.5 mg/L) 33 isolates (3.8%), clindamycin R (MIC >0.5 mg/L) 6 isolates (0.7%), tetracycline R (MIC >2 mg/L) 17 isolates (2.0%), and moxifloxacin R (MIC >2 mg/L) 1 isolate (0.1%). There were no isolates classified as I for those antibiotics. There were 23 isolates classified as I against cotrimoxazole (MIC >16, ≤32 mg/L), but no R (MIC >32 mg/L).
Conclusion: The proportion of invasive isolates of pneumococci with decreased sensitivity to commonly used antibiotics is very low.
P1041: Antimicrobial susceptibility of Streptococcus pyogenes isolated in 2004 in Spain, and comparison with previous studies (1998 and 2001)
J. Tamayo, J.I. Alós, J.L. Gómez-Garcés on behalf of the Study Group IAP-SEIMC
Objectives: To examine the susceptibility to penicillin G, macrolides, clindamycin and telithromycin of Streptococcus pyogenes isolated in 2004 in Spain, and to compare the results with those obtained in previous studies performed in 1998 and 2001 with the same methodology.
Methods: A total of 530 unique isolates of S. pyogenes collected in 21 laboratories were studied by the agar dilution method, in accordance with NCCLS guidelines. The number of strains collected was proportional to the number of inhabitants of each geographical area. We also determined the different macrolides-lincosamides-streptogramins phenotypes of resistance.
Results: (See table 1 and table 2) If we compared the results obtained in 2004 with those obtained in 1998 and 2001, we observed an statistically significant increase in the prevalence of the MLSB constitutive phenotype (p < 0.001, Chi square test).
Table 1.
In vitro susceptibilities of 530 recent S. pyogenes isolated in 2004
| Antibiotic | MIC range (mg/L) | MIC90(mg/L) | %S | %R |
|---|---|---|---|---|
| Penicillin G | ≤ 0.008-0.03 | 0.015 | 100 | 0 |
| Erythromycin | ≤ 0.12->16 | 4 | 78.3 | 21.7 |
| Azithromycin | ≤ 0.12->16 | 4 | 78.5 | 21.5 |
| Miocamycin | ≤ 0.12->16 | 0.5 | 93.4 | 6.6 |
| Clindamycin | ≤ 0.12->16 | ≤ 0.12 | 93.2 | 6.6 |
| Telithromycin | ≤ 0.008->16 | 0.25 | 94.0 | 5.8 |
Table 2.
Frequency of different phenotypes of resistance in the studies performed
MLSB c: MLSB constitutive
MLSB i: MLSB inducible
Conclusions: In 2004, (1) 14.9 % of the isolates were erythromycin-resistant and clindamycin- and miocamycin susceptible (M phenotype), a smaller percentage than in previous studies; (2) There was a significant increase in 2004 of isolates with the MLSB constitutive phenotype; (3) There was a high prevalence of resistance to telithromycin (88.6 %) in the 35 strains with MLSB constitutive phenotype.
P1042: Patterns of macrolide resistance determinants among S. pyogenes and S. pneumoniae isolates in Saudi Arabia
A. Shibl (Riyadh, SA)
Objective: To characterize the macrolide sensitivity of recent isolates of S. pyogenes and S. pneumoniae collected from different hospitals around Saudi Arabia and to investigate the resistance determinants carried by macrolide-resistant isolates.
Methods: Susceptibility testing was performed using standard NCCLS methodology on 335 S. pyogenes and 350 S. pneumoniae isolates. Macrolide resistance mechanism phenotypes were identified using double disk diffusion.
Results: All S. pyogenes were penicillin sensitive, while 6.4% were macrolide resistant, the main mechanism of which was of M-phenotype (96%). Approximately 51% of S. pneumoniae was penicillin non-susceptible. Macrolide resistance in S. pneumoniae accounted for 18.8%, the majority of which was M phenotype (92%). Low-level resistance mediated by mef-bearing strains predominated.
| Resistance % |
||||
|---|---|---|---|---|
| Penicillin |
Macrolide |
|||
| Isolate (no.) | S | I | R | |
| S. pyogenes (335) | 100 | – | – | 6.4 |
| S. pneumoniae (350) | 49 | 42 | 9 | 18.8 |
Conclusions: Efforts should focus not only on antibiotic resistance surveillance and the development of guidelines but also on appropriate use of antibiotics. Strategies have been proposed which include restricting access, compliance promotion and reduction in our prescriptions and inappropriate use of antibiotics. Newer macrolides, including azithromycin, are still considered drugs of choice for empirical treatment of respiratory infection in such circumstances.
P1043: Tetracycline resistance in erythromycin resistant beta-haemolytic streptococci of Lancefield groups A, B, C and G
M.R. Amezaga, L. Ford, H. McKenzie (Aberdeen, UK)
Objectives: MLSB phenotype erythromycin resistance (EryR) is often associated with tetracycline resistance (TetR) and in Streptococci is mediated by the methylase genes erm(B) or erm(TR). In Streptococcus pneumoniae, erm(B) is carried in transposons such as Tn1545 which also carry the TetR gene tet(M). M phenotype EryR is associated with the efflux genes mef(A) or mef(E). These genes are carried in genetic elements that do not commonly include TetR genes, but the mef(E) element in S. pneumoniae can be inserted in a transposon that carries tet(M). Our objective was to investigate TetR in EryR beta-haemolytic streptococci of groups A, B, C and G.
Methods: 129 EryR beta-haemolytic streptococci of groups A (26), B (42), C (9) and G (52) were collected over two years. TetR was determined by disc diffusion and MICs by E-test. PCR was performed for tet(M), tet(O) and tet(L); EryR genes had been characterised previously.
Results: The prevalence of TetR amongst EryR MLSB isolates was high in groups A (73%, 11 of 15), B (92%, 34 of 37) and C (100%, 2 of 2) but lower in group G (38%, 18 of 47). The range of MICs in TetR isolates was 4 ≥ 256 (mg/l). The tet(M) gene was responsible for most TetR in groups A (100%, 11 of 11), B (85%, 29 of 34), C (100%, 2 of 2) and G (56%, 10 of 18); tet(L) and tet(M) were both found in the same isolates in groups B (2) and G (1). At least 80% of erm(B) isolates and 57% of erm(TR) isolates of groups A, B and C carried tet(M). In contrast, only 21% of erm(TR) isolates in group G carried tet(M). Amongst M phenotype isolates, the prevalence of TetR was high in groups B (100%, 5 of 5) and G (80%, 4 of 5) and lower in group C (14%, 1 of 7). TetR was not detected in M phenotypes of group A. In M phenotypes, tet(M) was responsible for 100% TetR in group B (5 of 5) and 25% in group G (1 of 4); 1 isolate of group C carried tet(O). tet(M) and tet(O) were found in mef(E) isolates but not in mef(A) isolates. There were TetR isolates in groups B (5) and G (11) in which no TetR gene was identified.
Conclusions: 1) The prevalence of TetR in EryR beta-haemolytic Streptococci was high in MLSB isolates of groups A, B and C and in M isolates of groups B and G. 2) tet(M) was the predominant TetR gene. 3) tet(M) was strongly associated with erm(B) and to a lesser extent with erm(TR). 4) tet(M) was found in association with mef(E) but not mef(A).
P1044: Predominance of three emm-types among Streptococcus pyogenes isolates from invasive diseases in Greece
A. Stathi, L. Zachariadou, P.T. Tassios, A. Pangalis, N.J. Legakis, J. Papaparaskevas on behalf of The Hellenic Strep-EURO Study Group
Objectives: Based on the enhanced surveillance of Streptococcus pyogenes (group A Streptococci; GAS) invasive disease in Greece during the period 2003–2004, we aimed to determine the predominant emm-types and their possible association with erythromycin resistance and toxin gene production.
Materials and methods: A total of 60 invasive GAS isolates were collected during the period 1/2003–6/2004 from 10 hospitals in Greece. MIC determination of erythromycin, clindamycin and tetracycline was performed using the Etest method. MLS phenotype detection was performed using the erythromycin-clindamycin double disk method. PCR was used for detection of MLS resistance determinants mefA, ermB and ermTR as well as erythrogenic toxin genes speA, speB and speC. T-serotyping was performed using commercially available antisera. OF detection was performed using the agar method. M-type assignment was performed using the CDC emm-gene amplification and sequencing protocol.
Results: Isolates were from blood, deep tissue infections, synovial, pleural and cerebrospinal fluid (27, 22, 5, 4 and 2, respectively). Mean patient age was 19 years (range 1–80 years). Seven strains (12%) were resistant to erythromycin (EryR; MIC >0.5 mg/L). Four of these belonged to MLS phenotype M, two to the IR and one to the CR phenotype. Fifteen strains (25%) were resistant to tetracycline (MIC >4 mg/L). All four M phenotype isolates possessed only the mefA gene, both IR strains possessed only ermTR, whilst the CR strain possessed only ermB. Twenty isolates possessed only the speB toxin gene, nineteen possessed both speB and speA, nineteen possessed both speB and speC, and two possessed all three toxin genes. Of the 21 emm-types detected, three were predominant: emm1, emm12 and emm6 (33%, 10% and 6.6% of all isolates, respectively). Erythromycin resistance amongst these types was only detected in three emm12 strains. Three of the four M phenotype strains belonged to the emm4 type. All but one of the 20 emm1 type strains possessed the speA toxin gene, whilst only two of the 40 strains belonging to all other emm-types possessed the speA toxin gene (p < 0.0001).
Conclusions: A total of 12% of invasive GAS isolates were resistant to erythromycin, with phenotype M being predominant. Half of the isolates belonged to three emm types, with the remaining 30 being distributed among 18 emm-types. Type emm1 was predominant, and presented a strong association with the speA toxin gene.
P1045: Distribution of mefA-containing genetic elements in Italian isolates of Streptococcus pyogenes
S. D'Ercole, D. Petrelli, C. Zampaloni, L.A. Vitali, F. Marmocchi, M.S. Pasquantonio, S. Ripa, M. Prenna (Camerino, I)
Objectives: Erythromycin resistance M phenotype in Group A Streptococci (GAS, Streptococcus pyogenes) is due to an efflux system coded by the mefA gene, which is carried by a mobile genetic element, named either Phi10394.4 or Tn1207.3. This element is essentially composed of a transposon inserted into a prophage and its chromosomal insertion site has been mapped into the comEC gene. The aim of the present study was to analyze the genetic localization of the mefA gene by determining the general structure variability of the genetic element and its insertion site into the bacterial chromosome in 124 erythromycin resistant S. pyogenes clinical Italian isolates.
Methods: comEC gene was amplified in all isolates to test for its integrity. Negative reaction was taken as an indication of the insertion of the mobile genetic element. Subsequently, a set of oligonucleotide primers was constructed and used in PCR experiments to screen for the presence of distinctive parts along the entire sequence of the Phi10394.4/Tn1207.3 chimeric element (i.e. flanking regions and R-6, mefA, ABC-transporter, umuC-mucB, type II methylase genes).
Results: 20 out of 124 isolates (16.1%) were negative to the comEC gene amplification. The analysis of the insertion point flanking regions indicated that the Phi10394.4/Tn1207.3 element is present and inserted into the comEC gene. 9.7% of the population showed a mixed genotypic pattern, where comEC gene was amplified but the prophagic element was still present. This result was additionally confirmed by sequencing of the PCR products obtained. The remaining comEC positive population (74.2%) was Phi10394.4/Tn1207.3 negative, as none of the mobile element genes tested was amplified.
Conclusions: A very low portion of the population (16.1%) has the mefA gene carried by the Phi10394.4/ Tn1207.3 prophage element inserted into the comEC gene. About a tenth of the population contains an intact form of the comEC gene while presenting a Phi10394.4/Tn1207.3 positive pattern. Unexpectedly, the vast majority of isolates (74.2%) has the mefA gene vectored by neither forms of the prophagic chimeric element previously described. However, since it has been largely demonstrated that streptococci efflux mediated resistance can be transferred among bacteria by means of a transformation process, other mobile genetic elements should be present in Streptococcus pyogenes that act as molecular hosting vector for the mefA gene.
P1046: Prevalence, phenotypes, genotypes and molecular epidemiology of macrolide resistant clinical isolates of Streptococcus pyogenes in Norway 1993 and 2002
P. Littauer, M. Sangvik, B. Haldorsen, K. Dahl, D. Caugant, A. Høiby, A. Sundsfjord, G. Simonsen (Tromsø, Oslo, N)
Background: We have limited knowledge regarding the prevalence and molecular epidemiology of macrolide resistant Streptococcus pyogenes in Norway.
Objectives: i. Examine the prevalence of macrolide resistance in clinical S. pyogenes–isolates in Norway. ii. Further caution of macrolide resistant isolates of S. pyogenes strains with regard to resistance phenotype, genotype and different typing schemes including T-typing, emm-typing and multilocus sequence typing (MLST).
Methods: A total of 1657 isolates of S. pyogenes from respiratory tract and wound specimens were collected in Norway in three periods in 1993–97 and 2002 by 24 participating laboratories within the NORM surveillance programme for antimicrobial resistance in human pathogens. Erythromycin susceptibility testing was performed by E-test. Further analyses for their susceptibility to eight different antibiotics by E-test and double-disk-diffusion as well as opacity factor (OF), T-typing, emm typing and MLST. Genotypic analyses were performed by erm and mef specific PCRs.
Results: Reduced susceptibility (MIC >1 mg/L) was detected in 44 (2.7%) S. pyogenes isolates. A total of 32 (73%) S. pyogenes isolates demonstrated a MLSB phenotype resistance. The dominating gene was erm(A) (n = 27), encoding resistance in 27 strains, whereas erm(B) was detected in only five of the strains isolates. While one of the cMLSB strains carried both erm(A) and the mef(A) gene, another cMLSB strain was reproducibly negative in erm and mef PCR analyses, and will be further investigated. The remaining 11 (25 %) isolates all carried the mef(A) gene and showed a consistent with their M phenotype resistance. Thirty (68%) strains were resistant to tetracycline and carried the erm-positive strains (n = 30) genes, while all the Mtype strains were susceptible to tetracycline. Typing analyses revealed T-type 4 and ST39 dominated in nine 9 out of 10 with Mtype phenotype, whereas T-type 3 was associated with ST46 in 8 of 9 erm(A)-positive and tetracycline resistant strains. Results from emm typing supported these clonal observations.
Conclusions: (i) The prevalence of macrolide resistance among S. pyogenes in Norway is low, and the (ii) MLSB resistance, erm(A) or erm(B) was the most prevalent resistance type and co-resistance to tetracycline was frequently observed. (iii) Clonal observations were discerned in MLSB-strains (T3 and ST46; n = 8) as well as Mtype isolates (T4 and ST39; n = 9)
P1047: Evaluation of the Phoenix Automated Microbiology System in identification and antimicrobial susceptibility of clinical isolates of Streptococci
F. Luzzaro, G. Brigante, F. Meacci, G. Lombardi, B. Pini, A. Toniolo (Varese, Siena, I)
Objectives: Streptococci are important pathogens causing both community- and hospital-acquired infections. Prompt and correct identification of clinical isolates at the species level is essential for therapeutic management and epidemiology. Classical criteria (colony size, hemolysis, and group carbohydrate antigens) represent a useful tool for streptococcal identification, but recent taxonomic changes tend to revaluate biochemical identification.
Methods: The Phoenix™ Automated Microbiology System (Becton Dickinson, Sparks, MD) was evaluated for its capability of identifying clinical isolates belonging to the genus Streptococcus and quantitatively determining the susceptibility to antimicrobials. One hundred clinical isolates were investigated: S. pneumoniae (n = 46), S. agalactiae (n = 15), S. pyogenes (n = 14), S. dysgalactiae (n = 20), other streptococcal species (n = 5). Thirteen isolates of S. pneumoniae with reduced susceptibility to penicillin were included in the study. Species identification obtained by the Phoenix System was evaluated in comparison to results given by the API System (API 20 STREP; bioMérieux sa, Marcy l'Étoile, France). Discrepancies were resolved by direct sequencing of 16S rDNA. Quantitative antimicrobial susceptibility results for eight clinically relevant drugs (penicillin, cefotaxime, cefepime, erythromycin, clindamycin, chloramphenicol, levofloxacin, and vancomycin) were compared to MIC values measured by the Etest (AB Biodisk, Solna, Sweden). Based on NCCLS criteria, a reference broth dilution method was used to resolve discrepancies.
Results: The Phoenix System correctly identified 93% test isolates within 16 hr. When not identified or misidentified organisms were retested, correct identification rose to 98%. AST results interpreted according to current NCCLS guidelines showed essential and categorical agreement of 92% and 99%, respectively. No very major or major errors were produced. The overall percentage of minor errors was approximately 1%. The average time (±SD) to results was 12.3 ± 2.2 hr and appeared to depend on the species.
Conclusion: Identification and AST results provided by the Phoenix System appeared to be satisfactory in terms of accuracy and speed of diagnosis for the therapeutic management of streptococcal infections.
P1048: Incidence and mechanisms of reistance to macrolides in S. pyogenes in the West of Ireland
A. Coleman, M. Cormican, D. Kilmartin, M. NiChulain (Galway, IRL)
Aims and Objectives: Macrolides are an important alternative to penicillin for treatment of Streptococcus pyogenes infection. Rates of resistance to macrolides vary from region to region and these rates are important in defining the role of macrolides in empiric therapy. Macrolide and lincosamide resistance are mediated by 3 distinct mechanisms, (1) mefA encodes resistance to erythromycin but not clindamycin, (2) ermB encodes resistance to erythromycin and clindamycin, (3) ermA encodes resistance to erythromycin and inducible resistance to clindamycin.
Methods: Consecutive pharyngeal isolates of Streptococcus pyogenes isolates were collected between January 2003 and April 2004. Isolates were confirmed as S. pyogenes by Lancefield grouping using the Pastorex STREP rapid agglutination kit. Erythromycin susceptibility testing was performed by NCCLS disc diffusion. Erythromycin resistant isolates were tested for susceptibility to erythromycin and azithromycin by Etest. The mechanisms of resistance was assessed using the erythromycin/clindamycin disc approximation test and by PCR, with primers specific for the ermA, ermB and mefA genes. Positive controls were kindly provided by Ralf R. Reinert.
Results: Four (4) of 360 consecutive isolates (1%) were resistant to erythromycin. Erythromycin resistance was confirmed by Etest and these isolates were also resistant to azithromycin. All 4 erythromycin-resistant study isolates and 3 of 4 previously collected erythromycin-resistant isolates were confirmed as ermA positive by PCR and exhibited inducible resistance by disc approximation. One previously collected isolate was susceptible to clindamycin and was mefA positive by PCR.
Conclusion: These data show that macrolide resistance in S. pyogenes is very uncommon in this area and is encoded primarily by ermA.
P1049: Prevalence of multiresistance among Streptococcus pneumoniae strains in Finland
M. Rantala, J. Jalava, P. Huovinen (Turku, FIN)
Objectives: Multiresistance among Streptococcus pneumoniae strains is becoming alarming problem. Aim of this study was to evaluate the prevalence of multiresistant strains in Finnish pneumococci.
Materials and methods: Study was based on two groups of pneumococci: 1007 pneumococcal strains isolated both from noninvasive and invasive infections in 2002. The other group consisted all invasive pneumococcal isolates (n = 1011) that had been reported into National register Infectious Disease Register at the National Public Health Institute between January 2003 and April 2004. Antimicrobial susceptibility testing was performed by agar plate dilution method. Strain was defined as multiresistant if it showed resistance to three or more antimicrobial classes. Detection of macrolide resistance determinants [mef(A/E), erm(B), erm(TR)] was done by multiplex PCR from erythromycin non-susceptible and multiresistant strains isolated in 2002. Mef(A) and mef(E) subtypes were differentiated by separate PCR reactions.
Results: In year 2002 10.5% (106/1007) of pneumococci were multiresistant. Prevalence of multiresistant strains varied from 2% to 25% in different hospital districts. Non-invasive strains were more commonly multiresistant compared to invasive strains (10% vs. 4%). Among invasive strains the proportion of multiresistance was 5.1% in 2003–2004. Of 106 multiresistant strains, 91 (86%) strains carried either erm(B) methylase gene (m = 58) or subtype mef(E) efflux gene (n = 33). Double mechanism was detected in four strains. Most common multiresistant phenotype was [MLSB or M]-penicillin-tetracycline-trimethoprim-sulfomethoxazole (n = 34). Strains from young children (two years or younger) were more frequently resistant compared to strains from older patients.
Conclusions: When compared to previous years, the significant increase in multiresistance among invasive strains was detected between periods 1999–2000 and 2003–2004 (from 0.3% to 5.1%). The high prevalence of multiresistant pneumococci in Finland is a matter of concern. Additional studies are on progress to verify whether the spread of multiresistance is due to horizontal gene transfer or spread of resistant clones.
Wound and fungal infections
P1050: Does initial choice of antimicrobial therapy affect length of stay for patients with complicated intra-abdominal infections?
S. Wilson, R. Turpin, X.H. Hu, E. Mansley (Irvine, West Point, USA)
Objective: Complicated Intra-abdominal infections (IAIs) often require surgical intervention and antimicrobial therapy, frequently resulting in lengthy hospital stays. Common diagnoses include acute appendicitis with peritonitis or abscess (APP), cholecystitis (CHO), diverticulitis (DIV), acute pancreatitis (PAN), and post-operative infections (POI). Outcomes are influenced by many patient-related factors and aspects of medical management, including antimicrobial treatment choice. We studied a multiple hospital database to explore the length of stay (LOS) associated with initial choice of antimicrobial therapy for complicated IAIs.
Methods: We utilized Premier's Perspective Comparative Database to assess LOS for all 2150 admissions between February 2002 and June 2003 at 33 hospitals. The study population was all patients ≥18 years with diagnoses described above, receiving 1st line ampicillin/sulbactam (A/S), ceftriaxone (CEF), ertapenem (ETP), levofloxacin (LEV), or piperacillin/tazobactam (P/T). A regression tree using CART software was performed to select important variables, their interactions, and their order of importance in explaining LOS. A linear regression model was then utilized to formally compare the five treatment groups in terms of their LOS, controlling for patient variables (diagnosis, ICU stay, co-morbidities, age, sex and ethnicity) and hospital variables (region, urban/rural and teaching designation).
Results: Table 1 indicates mean LOS by initial antimicrobial therapy and diagnosis; italics indicate shortest LOS per diagnosis; n's are in parenthesis (X2 = 186.9; p < 001). Table 2 presents the adjusted LOS from the linear regression model; n's are in parenthesis. Controlling for variables listed above, LOS with ETP was not significantly different from A/S (p = 31). Both ETP and A/S were significantly different from LEV, P/T and CEF (all p < 05). Adjusting for all other factors, the variables associated with severity (diagnosis, ICU stay and co-morbidities) had the greatest impact on adjusted LOS (all p < 0.0001).
Table 1.
LOS for Diagnosis by Therapy
| A/S (791) | CEF (276) | ETP (172) | LEV (505) | P/T (406) | |
|---|---|---|---|---|---|
| APP (734) | 3.3 | 4.1 | 3.9 | 4.7 | 4.6 |
| CHO (851) | 4.4 | 5.5 | 3.3 | 5.4 | 4.6 |
| DIV(213) | 9.2 | 17.6 | 9.4 | 9.7 | 9.9 |
| PAN (296) | 8.6 | 11.7 | 6.0 | 9.8 | 12.4 |
| POI (55) | 11.0 | 11.8 | 5.5 | 10.3 | 9.9 |
Table 2.
Adjusted LOS by Therapy
| A/S (791) | CEF (276) | ETP (172) | LEV (505) | P/T (406) | |
|---|---|---|---|---|---|
| Adjusted LOS | 12.4 | 13.4 | 11.9 | 13.1 | 13.1 |
Conclusion: Findings indicate ETP and A/S were associated with shorter hospital stays, though this may be explained by underlying severity of infection. A randomized trial to test a treatment effect may be warranted.
P1051: Evaluation of surgical prophylaxis in heart surgery
C. Buke, O. Sipahi, M. Tuncel Basoglu, E. Bascesme, H. Posacioglu, S. Ulusoy (Izmir, TR)
Objective: Aim of this study was to evaluate antimicrobial prophylaxis (AP) practice and its cost in Intensive Care Unit of Heart Surgery Depertment in our hospital.
Method: Study was performed prospectively between January–December 2002. AP lasting >1 day was considered inappropriate, unless the patient was in high risk group (heart transplantation or repeated by-pass). In addition AP with two beta lactam agents; beta lactam+aminoglycoside (only beta lactam+gentamicin was allowed); 3rd generation cephalosporins; quinolones or glycopeptides were considered inappropriate. In high risk patients, AP lasting up to 3 days and AP with glycopeptides were considered appropriate. Cost of inappropriate AP was calculated by using August-2004 prices in EURO. Cost of inappropriate AP in patients who received cefazolin or beta lactam/beta lactamase inhibitors (ampicillin/sulbactam or amoxycillin/clavulanate) was calculated by substraction of cost of 1 day lasting AP from total AP cost. In case of inappropriate glycopeptide or quinolone or aminoglycoside usage, one day lasting cefazolin cost was substracted from total AP cost. In high risk patients cost of inappropriate glycopeptide usage was calculated by substracting 3 days lasting AP cost from total cost. Infections were diagnosed according to the criteria of Center for Diseases Control and Prevention (CDC). Data were analysed with chi square and Student's t-tests.
Results: Among 168 patients (50 females, 118 males, aged 41.2 ± 26) who received AP, only one patient (0.6%) received appropriate AP. Only 71 patients (42.2%) received ≤ 3 days AP. Patients who received (3 days AP developed more nosocomial infections than patients who received <3 days AP (15/97–15.4% vs 5/71–5.6%, p < 0.05). Mortality rate was 12.3% (12/97) in >3 days AP group and 4.2% (3/71) in <3 days AP group (p > 0.05). Average cost of AP was higher in >3 day group. (23.68 ± 18.97 EURO vs 217.12 ± 270.62 EURO, p < 0.05). Total cost of AP was 22.778 EURO, and cost of inappropriate or >1 day AP was 21.065 EURO.
Conclusion: Although it is not a randomized study, it is seen that AP longer than known criteria does not mean less nosocomial infections. Education and other interventions about AP may be necessary in order to resolve the situation.
P1052: Perioperative anti-infective prophylaxis with teicoplanin or second generation cephalosporins in vascular and orthopaedic surgery involving prosthetic material: a meta-analysis of randomised control trials
K. Vardakas, E. Soteriades, S. Chrysanthopoulou, P. Papagelopoulos, M. Falagas (Athens, GR; Boston, USA)
Objective: To evaluate the effectiveness and safety of teicoplanin compared to second-generation cephalosporins for perioperative anti-infective prophylaxis in orthopedic and vascular surgery involving prosthetic material.
Design: Meta-analysis of randomized controlled trials (RCTs)
Data sources: Data were obtained from PubMed (1/1950–10/2004), Current Contents, Cochrane central register of controlled trials, and references from relevant articles. Study selection: RCTs comparing teicoplanin with second generation cephalosporins in vascular and orthopaedic surgery were included in the study.
Data extraction: Two independent reviewers extracted data concerning development of infections at the site of operation or in remote areas, reported adverse effects, and mortality.
Results: Six RCTs were included in the analysis. Publication bias and statistically significant heterogeneity was not observed among the analysed studies. There were no differences in the development of infection at the site of operation (OR = 0.95, 95% CI 0.58–1.56) or in remote areas of the body (OR = 0.94, 95% CI 0.73–1.22) between teicoplanin and cephalosporins. In addition, there was no significant difference in reported adverse effects (OR = 0.77, 95% CI 0.50–1.18).
Conclusions: Teicoplanin is not more effective than second-generation cephalosporins as perioperative anti-infective prophylaxis in orthopedic and vascular operations involving prosthetic material.
P1053: Postoperative infection in posterior spinal fusion surgery in children
M. Syrou, I. Hager, A. Makri, H. Papavasileiou, G. Kanellopoulou, D. Demetriades, A Voyatzi (Athens, GR)
Objectives: The aim of the present study was to investigate the frequency and the type of wound infections, as well as the bacteria involved, after posterior spinal fusion in children, especially with spinal deformities, over a 6-year period (1999–2004).
Materials and methods: A total of 133 spinal fusions were performed on 110 children, with or without instrumentation, because of spinal scoliosis (120), spondylolisthesis (4), fractures (4), and for other reasons (5). The average age at operation was 13 years (range 4–17). Metal instrumentation was used in all the posterior spinal surgery. Out of 115 posterior spinal fusion cases 15 patients developed deep wound infections. 289 consecutive specimens were obtained from the infected wounds and cultured on appropriate media, for aerobic and anaerobic bacteria. The identification was based on conventional methods.
Results: 15 patients (13%) developed an early (2–7 days) or delayed (6 months–2.5 years) infection after surgery (11 early, 4 delayed). Out of 289 wound specimens, 219 were found positive for pathogens. From these in 19 (8.6%) were isolated 2 bacteria and only in 1 three. The most common organisms from 240 isolated bacteria were: coagulase-negative Staphylococci (CNS) (46.2%), following by Gram negative bacteria(36.2%), Staphylococcus aureus (10.9%), Anaerobes (4.6%), Steptococci spp (1.7%) and Candida spp (0.4%).25 S. epidermidis slime-producing strains were isolated from 6 patients with persistent wound infections. CNS were resistant against penicilline (63. 9%), oxacillin (32.4%), erythromycin (38.7%), fusidic acid (35.1%), clindamycin (27.9%), gentamicin (26.1%) and co-trimoxazole (21.6%). Low resistance was recorded against rifampicin (8.1%) and quinolones (9.9%), while all isolates were sensitive to glycopeptides.
Conclusions: 1. The most predominant pathogens were CNS and Gram negative bacteria. 22.5% of CNS pathogenic strains were slime producers. 2. Infection rate after posterior spinal instrumentation was found 13%. 3. In comparison with the rate of infection 20% of previous reported study in our hospital, the reduction to 13% should be correlated with the improvement of surgical technique and operation room conditions.
P1054: Lucilia sericata: latest results of antibacterial activity
M. Reinecke, G. Mayer, P. Heisig (Hamburg, Barsbüttel, D)
Objectives: Therapy of chronic wounds with Lucilia sericata presents a promising alternative to the classical approach with antibiotics. Larvae are placed in wounds free-roaming or in biobags. The therapy often stimulates the process of wound healing. This effect is based on different mechanisms. Maggots’ saliva contains collagenases, trypsin and chymotrypsin-like enzymes which dilute necrotic tissue. Furthermore, an antibacterial effect has been described. In our study, we focused on the question whether this effect could be explained by the ingestion of bacteria by larvae.
Methods: Free roaming maggots were placed on agar plates with Escherichia coli. These bacteria had been transformed with Green fluorescent protein (GFP)-containing plasmids. GFP-free Escherichia coli XL1 blue served as a control. Two days old maggots were put on agar plates in groups of ten at room temperature. Every thirty seconds, a maggot was displaced from the agar plate and washed with sterile saline (0.9%). Dead larvae which could not have taken up bacteria served as a control. Maggots were tested for flourescence under a fluorescence microscope [Zeiss Axioskop; HPO50/AC, Axiocam MRmZeiss]. Larvae were examined by an independent observer as well.
Results: Maggots that had been placed on GFP-labelled Escherichia coli showed an intensive green fluorescence, especially at the back of the head and in the intestines. The controls did not show any fluorescence. After three to four minutes GFP-labelled Escherichia coli could be detected inside the maggots’ body. At this early stage of digestion GFP-fluorescence could mainly be examined in the area of the head. This fluorescence results of the ingestion of GFP- labelled Escherichia coli by larvae.
Conclusion: We have proven that the uptake of bacteria represents a further mechanism of antibacterial activity of larvae. Not only diluting necrotic tissue, but also minimizing the rate of infections, maggot therapy which is also well-known
Antibiotic resistance: nosocomial pathogens
P1055: Antimicrobial resistance patterns of bacterial pathogens from blood culture of cancer patients in a single cancer institution
M. Faiz, H. Aziz, T. Bashir, S. Asghar (Lahore, PAK)
Objective: The widespread emergence of resistance to antimicrobial agents among bacterial pathogens is well known and has an impact on our ability to treat patients effectively. Blood stream infections (bacteraemia) among cancer patients that develop during the course of disease are potentially life threatening because of suppression in their immune systems. The changing spectrum in the incidence and epidemiology of microbial pathogens has resulted in an increase in resistance to many antibiotic compounds emphasizing the need to monitor the prevalence of resistance in these strains.
Methods: Susceptibility and resistance pattern of clinically significant bacterial isolates from positive blood cultures collected during 2000–2004 was studied. The isolated strains were tested against a wide range of antibiotics belonging to cephalosporins, aminoglycosides, carbapenems and quinolones derivative groups by disc diffusion method and the results were interpreted according to British standard for antimicrobial chemotherapy.
Results: A total of 250 bacterial pathogens were isolated with 60% gram positive and 40% gram negative bacteria. The dominating pathogens were Staphylococcus aureus, Streptococci, Pseudomonas, Enterobacter and Klebsiella. Among gram negative strains, highest level of resistance (98%) to third generation cephalosporins was observed followed by carbapenems and penicillin (79%, 80%) respectively. Similarly, high resistance to aminoglycosides were found (69% to ampicillin, 50% to tobramycin and 62% resistant to quinolone derivates group of antibiotics. However only 29% were resistant to ciprofloxacin. In gram positive bacteria, high resistance to ciprofloxacin (40%) was observed as compared to gram negative bacteria. A still higher resistance level (100%) was observed for aminoglycosides and third generation cephalosporins (97%) respectively.
Conclusion: The spectrum of isolates among our patients were shifting towards gram positive bacteria with high resistance to different groups of antimicrobial agents limiting few choices for alternative therapies for infection control. Antimicrobial resistance continues to increase and ongoing surveillance of microbial pathogens is essential. This study also warrants the need of infection control measures, rational antibiotic policies and rapid laboratory detection of resistance to prevent the spread of resistance among these strains.
P1056: Antimicrobial susceptibility of bloodstream infections has no impact on outcome in intensive care unit patients with acute renal failure
E. Hoste, S. Blot, G. Verschraegen, J. De Schuijmer, S. Claus, J. De Waele, J. Decruyenaere, N. Lameire, R. Vanholder, A. Dhondt, F. Colardyn (Ghent, B)
Objectives: Bloodstream infections (BSI) have a worse outcome when the microorganisms involved are antimicrobial resistant as biosurgery could be a beneficial alternative to the use of antibiotics. As the mechanical uptake is a non-specific process, there might not be a risk of resistance. (AM-R), compared to BSI with antimicrobial susceptible (AM-S) microorganisms. We evaluated whether this is also true in intensive care unit (ICU) patients with acute renal failure who are treated with renal replacement therapy (ARF-RRT), a particular severely ill cohort of ICU patients.
Methods: All ICU patients with ARF-RRT in the period '95–'01 (n = 704) were evaluated. A comparison was made between patients with AM-S BSI and patients with AM-R BSI. Enteroccci were defined AM-R when R to vancomycin, staphylococci when R to methicillin, gram-negative bacteria when R to ceftazidim, Pseudomonas when R to ceftazidim, quinolones, piperacilin, or imipenem, and Candida when R to fluconazole. Data are presented as median (IQR) or %.
Results: BSI occurred in 62 patients, incurring 68 microorganisms; BSI was AM-S in 25 and AM-R in 37 patients. AM-S and AM-R patients had the same age (62 (55–69) vs. 58 (40–66) yr, P = NS) and APACHE II score (28 (18–37) vs. 28 (20–34), P = NS). The time between ICU admission and BSI was longer for AM-R patients (4 (1–16) vs. 13 (6–26) d, P = 0.02). AM-R BSI involved more gram-positive bacteria and primary BSI compared to AM-S BSI (76% vs. 24% P < 0.01, resp. 54 vs. 12 %, P < 0.01). More AM-S patients received adequate antimicrobial therapy (96 vs. 76 %, P = 0.03); the delay of adequate therapy was equal (0 (0–0) vs. 0 (0–0.8) d, P = NS). Vasopressor use was equal in both groups (92 vs. 95 %, P = NS), as was mechanical ventilation (92 vs. 87 %, P = NS). There was no difference in length of hospital stay and hospital mortality between AM-S and AM-R patients (29 (15–77) vs. 46 (31–70) d resp 76 vs. 65 %, both P = NS). Hospital mortality in non-BSI patients with ARF-RRT was 70 %. In a Cox proportional hazards model only increasing age (HR 1.3/10 yr, P = 0.04) and secondary BSI (HR 3.2, P = 0.01) were associated with mortality.
Conclusion: In this cohort of patients with high baseline mortality, AM-R of BSI had no impact on outcome.
P1057: Antimicrobial-resistant bacteria isolated from nosocomial bacteraemia
C. Sartor, P. Barthelemy, P. Berger, C. Zandotti, M. Bimar, B. La Scola (Marseille, F)
Objectives: Although a monthly surveillance of the antimicrobial-resistance of bacteria is performed in our institution, the bacterial resistance in nosocomial infections was unknown. We focused this study on the nosocomial bacteraemia.
Methods: We studied the bacteria that had been isolated from the blood cultures collected in our institution, a 3500 bedded acute care hospital, from January 1st, 2002 to June 30th, 2004. We also analysed the bacteraemia identified by the active surveillance of nosocomial infections in our institution, during the same period. The study concerned the distribution of the bacteria and the antimicrobial-resistance of Staphylococcus aureus, Pseudomonas aeruginosa and enterobacteria. The analysis were performed using VIGIact and SPSS softwares.
Results: During the study period, 8313 blood cultures have been isolated. Of them, 1214 nosocomial bacteraemia had been identified by the surveillance of nosocomial infections, whom 11% had been acquired out of the hospital. The following bacteria were more frequently isolated from the nosocomial bacteraemia: 275 (23%) S. aureus, 166 (14%) Staphylococcus epidermidis, 165 (14%) Escherichia coli and 84 (7%) P. aeruginosa. Of the S. aureus, 30% were resistant to oxacillin, and 32% to ofloxacin. Of the P. aeruginosa, 54% were resistant to ticarcillin, 32% to ceftazidime, 31% to imipenem and 36% to ciprofloxacine. Of the 363 enterobacteria, 12% were resistant to third-generation cephalosporins (C3G), 15% to ciprofloxacine and 22% to trimethoprime/sulfamethoxazole.
Conclusion: The results suggest a strong level of the antimicrobial-resistance of the bacteria isolated from nosocomial bacteraemia. This was in accord with the results of the local laboratories network, although the resistance of P. aeruginosa to imipenem and enterobacteria to C3G seems greater.
P1058: Antibiotic use and bacterial resistance in German intensive care units: data from project SARI (Surveillance of Antibiotic Use and Bacterial Resistance in German Intensive Care Units) from 2000 to 2004
E. Meyer, F. Schwab, D. Jonas, H. Rüden, P. Gastmeier, F.D. Daschner (Freiburg, Berlin, Hannover, D)
Objective: To study data on antibiotic resistance, prophylactic or therapeutic use of antibiotics in ICUs, on changes over time, and on the correlation between antibiotic use and resistance rates in intensive care units (ICUs) in Germany.
Methods: Prospective, unit-based surveillance in which ICUs collected data on patient days, antibiotic use (defined daily doses = DDD according WHO) and resistance rates of selected non-duplicate pathogens. Antibiotic use density (AD) is calculated in DDDs/1000 patient days. The data were recorded, analysed centrally and communicated to the participants every six months (www.sari-antibiotika.de).
Results: Starting in 02/2000, by 6/2004) SARI had recorded data provided by 40 ICUs covering a total of 1571 months, 578,760 patient days and 773,306 defined daily doses. On average, each patient received 1.2 doses of an antibiotic per ICU-day. Antibiotic usage rates were highest for penicillins with lactamase inhibitor (AD 297) and chinolones (AD 156). Resistance data were collected on 53,038 isolates of 13 pathogens: S. aureus (n = 11750; 22.2%), S. pneumoniae (n = 881; 1.7%), coagulase-negative Staphylococci (n = 8373; 15.8), E. faecalis (n = 5463; 10.3%), E. faecium (n = 1888; 3.6%), E. coli (n = 8614, 16.2%), K. pneumoniae (n = 3310, 6.2%), E. cloacae (n = 3033, 5.7%), Citrobacter spp. (n = 970, 1.8%), S. marcescens (n = 1011; 1.9%), P. aeruginosa (n = 5109; 9.6%), A. baumannii (n = 1247; 2.4%) and S. maltophilia (n = 1389; 2.6%).
Conclusions: The resistance situation in Germany is still highly heterogenous: MRSA-rates range from 2.9% to 66.7% (mean 21.2%); according to DIN testing ciprofloxacin resistant E. coli rates range from 0.8% to 50.0% (mean 12.5%) and imipenem resistant P. aeruginosa rates range from 0.0% to 47.8% (mean 25.0%). Over a period of three years (2001–2003), a significant increase was only seen in ciprofloxacin resistant E. coli by Wilcoxon sing rank test for paired samples. Antibiotic use and bacterial resistance rates are still highly heterogenous in German ICUs. The large differences between ICUs indicate that initiatives may be most effective when undertaken at the local level. Over a period of three years (2001–2003), a significant increase was only seen in ciprofloxacin resistant E. coli.
P1059: Klebsiella oxytoca outbreak in the department of neonatology of a university hospital in Gdansk, Poland
B. Rybak, E. Czarniak, E. Augustynowicz, A. Nowaczek, A. Samet, J. Szczapa (Gdansk, Warsaw, PL)
Objective: The aim of this study was to analyse outbreak of Klebsiella oxytoca in neonatology patients from of the Medical University of Gdansk.
Materials and methods: Teaching hospital of the Medical Universityt contains four neonatal wards: Neonatal Intensive Care Unit [NICU], Pathology Unit [PU], Septic Unit [SU] and Rooming-in Unit [RU]. This department serves an average of about 160 of patients per month. We analysed patients recovered from May 2004. Strains were identified by classical methods and VITEK cards (BioMerieux). Sensitivity was determined by the agar diffusion method according to NCCLS guidelines. Clinical data were retrospectively collected from the medical records of patients admitted to the department during the study period. The following sociodemographic variables and potential risk factors were assessed: gender, gestational age, mode of delivery, Apgar score, birth weight, mechanical ventilation, parenteral nutrition, length of hospital stay, and antimicrobial treatment. K. oxytoca isolates were analysed by RAPD-PCR method.
Results: We analysed 30 isolates from 18 patients from two days. Isolates were recovered from urine (9), and epidemiological swabs from throat and rectum (21). We found two susceptibility groups: group 1 (7 patients) resistant to amox/clavul.acid, pip/tazobactam, aztreonam, cefuroxime, and group 2 (11 patients) susceptible for these antibiotics. RAPD profiles corresponded with the susceptibility testing results. Drug resistance profile in group 1 could be attributed to overproduction of chromosomal encoded K1 beta-lactamase. Group 1 was from RU and group 2 from NICU, PU and SU. Analysis of sociodemographic variables and potential risk factors showed differences between analysed groups in mean birth weight, length of hospital stay, antimicrobial treatment and invasive therapeutic procedures usage.
Conclusions: The outbreak analysis revealed concurrent isolation of two K. oxytoca clones, normal and K1 overproducer. RAPD results were supported antibiotyping results. The epidemic of K. oxytoca K1 was stopped by strict infection control measures.
P1060: Multi-resistance in K. pneumoniae: epidemiological results from the GENARS Project
I. Noll, J. Beer, K. Huppertz, W. Pfister, T. Pietzcker, S. Schubert, T.A. Wichelhaus, S. Ziesing, B. Wiedemann (Bonn, Leipzig, Jena, Ulm, Kiel, Frankfurt a.M., Hannover, D)
Objectives: Clones of K. pneumoniae were involved in nosocomial infections with fatal consequences in the late 1960s. They became rare with the introduction of 3rd and 4th generation cephalosporins. Today this species again seems to play a major role in nosocomial infection due to resistance to the modern drugs. The GENARS-project (German Network for Antimicrobial Resistance Surveillance) is designed to provide epidemiological data for German university hospitals. Since 2002 resistance data are collected for all clinical relevant pathogens.
Methods: Analysis was based on first isolates of K. pneumoniae from six laboratories, collected from January 2002 to June 2004. Minimal inhibitory concentrations (MICs) were determined by broth microdilution method (DIN) for ceftazidime (CAZ), cefotaxime (CTX), ciprofloxacin (CIP), gentamicin (GEN), meropenem (MER) and piperacillin (PIP). Resistance patterns were evaluated by using breakpoints according to DIN, grouping resistant and intermediate as non-susceptible; multi-drug resistance was defined as non-susceptibility to at least four of the six agents.
Results: A total of 3077 isolates was analysed. 51.4% of these isolates were non-susceptible to at least one agent, the highest proportion is due to mono-drug resistance to piperacillin (39.6%). 4.8% of the strains were classified as multi-resistant, the most frequent patterns were PIP/CAZ/CTX/GEN (2.1%) and PIP/CAZ/CTX/GEN/CIP (1.7%). Two strains were resistant to all six antibiotics. Significant differences in multi-drug resistance rates were associated with ward type with highest rates for ICU-patients (8.8%). Furthermore, multi-resistance rates varied significantly between the centres involved with a range from 0.9% to 7.2%. The centres differed not only in respect to the multi-drug resistance rates, but also in respect to the dominating phenotype.
Conclusions: The relevance of multi-resistance in K. pneumoniae as a major clinical problem is proved by an overall rate of almost five per cent for German university hospitals and an even higher proportion for ICU-patients. Among the agents tested piperacillin plays an eminent role in regard to its mono-resistant rate as well as a component of the most frequent resistance patterns. Resistance to the combination of PIP with Tazobactam however is rare.
P1061: The development of antimicrobial resistance in German hospitals
K. Huppertz, J. Beer, I. Noll, W. Pfister, T. Pietzcker, S. Schubert, T.A. Wichelhaus, S. Ziesing, B. Wiedemann (Bonn, Leipzig, Jena, Ulm, Kiel, Frankfurt, Hannover, D)
Objectives: Since the end of 2001, six laboratories for medical microbiology at German university hospitals are taking part in the GENARS-project (German Network for Antimicrobial Resistance Surveillance). These laboratories regularly send data obtained in the laboratory routine to the central office of GENARS in Bonn. Here they are merged in the database and analysed. The goal of this investigation was to find out, if significant trends in the development of antimicrobial resistance in GENARS-hospitals are detectable.
Methods: MIC-values from species listed were determined for 25 antibiotics, considering all relevant antibiotic classes: E. coli, E. cloacae, P. mirabilis (ciprofloxacin, gentamicin, ampicillin, piperacillin and cefotaxime), P. aeruginosa (ciprofloxacin, imipenem, ceftazidime, gentamicin and piperacillin) and S. aureus (penicillin, oxacillin, erythromycin, doxycyclin und linezolid). Only the values of non-copy strains of five GENARS hospitals entered the statistics.
Results: For many antibiotic–species-pairs no obvious trends could be detected. However some species show continuous changes in their resistance rates. A highly significant increase in ciprofloxacin resistant strains of E. coli and P. aeruginosa could be observed. Detailed percentages of resistant strains for the 1st half of 2002 and the 1st half of 2004 are shown in Table 1. For S. aureus strains resistant to Oxacillin (MRSA) increased significantly to a level of 11.6 % (Table 1). In means for all GENARS-hospitals the resistance rate to Oxacillin increased. Nevertheless, in two of these hospitals a clear decrease was observed. The level of resistance and resistance development for all species evaluated can vary considerably from hospital to hospital.
Conclusions: In the time under observation, in GENARS-hospitals for most of the selected species and antibiotics no significant changes in antimicrobial resistance could be detected. Nevertheless, as shown for E. coli and P. aeruginosa resistance to ciprofloxacin and for S. aureus resistance to oxacillin increased significantly. This demonstrates that an early detection of any alterations in antimicrobial resistance by a continuous surveillance is of great importance.
Table 1.
Percentages of strains of E. coli, P. aeruginosa and S. aereus resistant to Ciprofloxacin (CIP) and Oxacillin (OXA) for tin 1st half of 2002 and the 1st half 2004.
| 1st half 2002 | 1st half 2004 | |
|---|---|---|
| E. coli/CIP | 9.6 | 13.8 |
| P. aeruginosa/CIP | 11.5 | 18.8 |
| S. aureus/OXA | 9.0 | 11.6 |
P1062: Staphylococcal bacteraemias in internal medicine and oncology patients in a university hospital
S.G. Kalpadakis, I.S. Kourbeti, M. Rovithi, A. Christidou-Stefanaki, G. Samonis (Heraklion, GR)
Objectives: To determine the epidemiology, the clinical presentation and the resistance patterns of Staphylococcus aureus (SA) and Coagulase Negative Staphylococci (CNS) Blood Stream Infections (BSI) in Internal Medicine (IM) and Oncology (ON)wards.
Methods: Medical records of patients >18 years old hospitalized over a one year period (2003) in the IM and Oncology ON wards were retrospectively reviewed.
Results: In the year 2003 there were 11 patients with S. aureus bacteraemia (SAB) in the IM and 1 the ON ward. During the same time period there were 2 clinically significant CNS BSI in the IM and 7 in the ON ward. The IM patients with SAB and CNSBSI had the same average age (59 years). The maximum temperature upon the diagnosis was in average 38.1 for the SAB and 37.8 for CNSBSI. The men predominated among the SAB (72%). The average numbers of the White Blood Cells (WBC) were 16,020 for the SAB and 9,600 for CNSBSI. The infections were community acquired (CA) in 54% of the SAB and in 50% of the CNSBSI. The ON patients with CNSBSI had an average age of 63 years and the female predominated (71%). The average WBC was 8,600 and the temperature was 38.6. The infections were catheter-related in 72% of the cases. The bacteremias were mixed in 43%. No infection was associated with neutropenia in the ON population. The infections were more severe in the IM ward where most of the cases were associated with abscesses or endocarditis where in the ON wards the infections were mainly catheter associated. The average length of stay was 11.3 days in the ON ward where in the IM ward it was 23.7 days. No death could be attributed to the SAB or the CNSBSI either in the IM or ON ward. The percentage of MRSA in the IM patients was 18.8% when in Greece the MRSA percentage for the year 2003 in medical wards was 44%. Among the ON patients, the only SAB was caused by an MRSA. The CNS BSI were caused by methicillin R organisms in 57%.
Conclusion: The percentage of MRSA in our IM ward is considerably lower than in the average percentage in the national surveillance. This is probably due to the fact that most cases were community acquired. The SAB comprised only 0.56% of the 2003 IM ward admissions. The staphylococcal infections in the non-oncologic patients required longer length of stay. On going prospective surveillance is in progress to determine the differences in the profile of the staphylococcal infections in IM and ON patients and the pathogen resistances.
P1063: A four-year analysis of antimicrobial use and antimicrobial resistance among Gram-negative bacilli in an Italian intensive care unit
M. Bassetti, E. Righi, R. Fasce, A. Costa, E. Cantagalli, B. Rebesco, M. Cruciani, C. Mengoli, F. Bobbio Pallavicini, D. Bassetti (Genoa, I)
Obiectives: Assess rates of antimicrobial resistance of the common gram-negative isolates in ICU and to evaluate the impact of antibiotic use on the emergence of resistant organisms.
Methods: Retrospective analysis for a four years period (1999–2002) in a medical and surgical ICU. Duplicate isolates were not considered. A hospital-acquired infections (HAI) was defined, according to CDC definitions. Susceptibility was evaluated for piperacillin (P), piperacillin/tazobactam (PT), cefotaxime (CX), ceftazidime (CZ), ciprofloxacin (CP), gentamicin (GT) and imipenem (IM). We analysed resistance patterns and DDDs per 1000 patient-days. Data were analysed by Chi square for linear trend and logistic regression, with a level of significance defined as p < 0.05.
Results: 1476 clinical strains were isolated from 1237 patients with an HAI. A prevalence of Gram-negatives isolates (>60%) was observed. High resistance rates were observed for almost all the antibiotic tested. Exceptions were IM (100% strains susceptible) and GT (93–99%) toward K. pneumoniae (Kp), IM toward Serratia spp. (90–100%), and GT toward Kp (93–99%). Steady levels of resistance to all the antibiotics tested were observed for P. aeruginosa (Pa) and Serratia spp. By contrast, a significant trend toward an increase in resistance rate to P, CX, CZ, and CP was observed for Kp. A linear and significant trend toward a decrease in resistance rate to PT was observed. Overall, we recorded a continual increase in the antibiotics use from 1999 through 2002. The most remarkable trend in antimicrobial use was represented by huge increases in utilization of broad spectrum penicillins, 3rd generation cephalosporins, IM, and CP. A significant drug-usage vs susceptibility relationship was found with Kp and Proteus spp. (Pr). Increasing use of CX, CZ, P, and CP was associated with decreased susceptibility of Kp to themselves. The increase in the consumption of PT was associated with increasing susceptibility of Kp. Moreover, increasing use of CX and IP were associated with decreased susceptibility of Pr to these drugs. No other significant relationships were found.
Conclusion: The data demonstrated the correlation between antimicrobial consumption for extended spectrum cephalosporins, quinolones and carbapenems and selection of resistances in Kp, Pr and Pa. In contrast, an increased usage of PT was associated with increasing susceptibility in Kp, suggesting a protective role of PT for ESBL in Kp.
P1064: Colonisation of long-term care facilities residents with multidrug-resistant Escherichia coli in Greece
V. Grammelis, N. Tsogas, M. Mbomboli, A. Kapaskelis, G. Greka, K. Kanellakopoulou, H. Giamarellou, M.C. Lazanas (Athens, GR)
Objective: Resistance to antimicrobials of different structural classes has arisen in a multitude of bacterial species. A survey was performed to determine the prevalence and resistant rates of MDR E. coli isolates colonizing the elderly residents of Greek LTCF.
Methods: A total of 28 LTCF were randomly selected from the public sanitation list of Attica province. Urine, nasopharyngeal and wound samples were collected from 668 elderly residents. We chose randomly 35% of the existing population from each LTCF (minimum sum 25 residents, age above 65 years). E. coli isolates were identified by API strips and underwent antimicrobial disk susceptibility testing, following the NCCLS guidelines. Confirmation of ESBL-R was done by MIC broth microdilution and double disk diffusion, as per NCCLS.
Results: The mean age of the residents was 86.2 years. 302 E. coli strains were isolated from 1448 samples (20.8%). 76 MDR (i.e., those resistant to ≥3 antimicrobial agents including ampicillin, ceftazidime, trimethoprim-sulfamethoxazole, gentamicin, and ciprofloxacin) E. coli isolates (25.2%) were recovered. The majority of them were isolated from urine samples (83%). Resistance to ampicillin (AMP), trimethoprim-sulfamethoxazole (TMP/SMX), ampicillin-sulbactam, ciprofloxacin (CIP), gentamicin (GM), and ceftazidime was found in 57.5%, 47.6%, 33.8%, 22.2%, 9.4% and 2.3% of isolates, respectively. Beta-lactam resistance phenotypes essentially comprised penicillinase production (36.8%), overexpression of chromosomal cephalosporinase (5.6%), and synthesis of inhibitor-resistant TEM/OXA enzymes (5.5%) or ESBL (2.0%). 66.5 % of the previous ESBL-producing strains were resistant to CIP. Resistance to non-betalactam antibiotics (ST, CIP and GM) was more prevalent in AMP-resistant strains and ESBL-producing strains. The most prevalent phenotype was resistance to AMP, TMP/SMX and CIP, which was detected in 62.5% of MDR resistant isolates and 0.3% of strains overall.
Conclusions: 1. Colonization with MDR-E. coli is relative high in Greek LTCF. 2. The close relationship between resistance to non-beta-lactam antibiotics and ESBL-producing E. coli strains is worrisome. 3. Resistant rates of E. coli to ampicillin, TMP/SMX and ciprofloxacin are relatively high and must be considered in case of urinary infections in residents of Greek LTCF.
P1065: Colonisation of long-term care facilities residents with quinolone-resistant Gram-negative bacteria in Greece
V. Grammelis, G. Tsekes, M. Nikolakopoulou, M. Gika, D. Katsala, K. Kanellakopoulou, H. Giamarellou, M.C. Lazanas (Athens, GR)
Objectives: Quinolones (Q) are among the most frequently used agents for treating LTCF-acquired infections. Consequently, bacteria exhibit increasing resistance to Q. A multicentre survey was conducted in order to determine (I) the prevalence and risk factors for colonization with QRGN in Greek LTCF (II) the corresponding antimicrobial resistant rates (ÁR).
Methods: A total of 28 LTCF were randomly selected from the public sanitation list of Attica province. Urine, nasopharyngeal and wound samples were collected from 668 elderly residents. We chose randomly 35% of the existing population from each LTCF (minimum sum 25 residents, age above 65 years). Gram negative bacteria were identified by API strips and underwent antimicrobial disk susceptibility testing, following the NCCLS guidelines. Data were also collected on resident factors and institutional variables. Univariate and multivariate analyses were performed. Odds ratios (OR) and P values were calculated.
Results: 412 Gram negative (GN) strains were isolated from 1448 samples (prevalence rate 28.5%). The majority of them were recovered from urine samples (86.8%). 53% of the residents had been taking systemic antibiotics during the preceding month. Q were the leading class (38%). ÁR of GN to ciprofloxacin (CIP) were estimated (Table). Multi-drug QRGN accounted for 11.5% of the isolated strains. The most prevalent phenotype was resistance to ampicilline, CIP and trimethoprim-sulfamethoxazole. In the multivariate analysis, only prior exposure to antimicrobial agents (P < 0.001; OR = 2), specifically to Q (P < 0.001; OR = 14), and the presence of a urinary catheter (P < 0.001; OR = 2) were significantly associated with colonization with QRGN.
| Species | % of isolates | % AR to CIP |
|---|---|---|
| Escherichia coli | 40.2 | 22.1 |
| Proteus spp. | 21.3 | 25.1 |
| Klebsiella spp. | 18.2 | 27.1 |
| Enterobacter spp. | 2.4 | 21.2 |
| Citrobacter spp. | 2.3 | 5.2 |
| Morganella spp. | 5.5 | 41.5 |
| Acinetobacter spp. | 2.2 | 66.3 |
| Pseudomonas spp. | 3.5 | 35.2 |
| Providencia spp. | 1.9 | 4.3 |
| Serratia spp. | 1.5 | 6.5 |
| Other | 1.0 | 4.2 |
| Total/Mean | 100 (412) | 21.2 |
Conclusions: 1. Colonization of residents in Greek LTCF with QRGN is relatively high. 2. Given the high rate of colonization with QRGN, empiric use of quinolones may not be appropriate. 3. Significant risk factors for colonization with QRGN are prior exposure to antimicrobial agents, specifically to quinolones, and the presence of a urinary catheter.
P1066: Colonisation and resistance dynamics of Gramnegative bacteria during and after hospitalisation
P.M.G. Filius, I.C. Gyssens, A. Ott, A.G. Vulto, H.A. Verbrugh, H.P. Endtz (Rotterdam, NL)
Objectives: Colonization and resistance dynamics of gramnegative bacteria in the intestinal and oropharyngeal microflora of patients admitted to intensive care units (ICU) and general wards (GW) were investigated during and after hospitalization.
Methods: Specimens were obtained on admission, once weekly during hospitalization, at discharge from the ICU, at discharge from the hospital and one and three months after discharge from the hospital. Five colonies per specimen were selected for identification and susceptibility testing by the VITEK 2 system.
Results: A total of 3316 specimens from 411 patients were collected. In both patient populations, the gram-negative colonization rates in oropharyngeal specimens increased during hospitalization and did not decrease in the three months after discharge. In rectal specimens, colonization rates decreased during hospitalization and increased after discharge. There was a change in species distribution among the dominant microflora during hospitalization. Klebsiella spp., Enterobacter spp., Serratia marcescens and Pseudomonas aeruginosa were more often isolated, whereas the frequency of E. coli declined. The percentage of ICU patients colonized with ampicillin and/or cephalothin resistant faecal E. coli was significantly increased at discharge from the hospital and did not change in the three months after discharge. Emergence of multi-drug resistance was observed in many gram-negative species during stay on the ICU. Resistance frequencies in E. coli significantly increased with length of stay on the ICU. For the GW population, no significant changes in resistance frequencies were found during hospitalization.
Conclusion: From a population perspective, the risk of dissemination of resistant gram-negative bacteria into the community through hospitalized patients appears to be low in GW patients, but is noticeably higher among ICU patients.
P1067: Association of antibiotic resistance phenotypes and the presence of class I integrons in a sample of bacterial isolates from U.S. hospitals
A.N. Rao, M. Barlow, L.A. Clark, F.C. Tenover, J.E. McGowan Jr. (Atlanta, USA)
Objective: We assessed the association between class 1 integrons and patterns of resistance to aminoglycosides, beta-lactams, quinolones, and chloramphenicol in Escherichia coli and Klebsiella species isolates from U.S. hospitals participating in Project ICARE.
Methods: A convenience sample of 320 E. coli and Klebsiella species isolates was collected between October 2002 and December 2003 from 19 U.S. hospitals as part of Phase IV of Project ICARE and tested for susceptibility to a variety of antimicrobial agents. These organisms were submitted in response to a request for organisms resistant to 3rd generation cephalosporins (ceftazidime, ceftriaxone, cefotaxime) and/or fluoroquinolones. The isolates were screened for the presence of class I integrons using sets of primers specific for 5′ and 3′ conserved segment of the integrase gene. We obtained measures of association between the presence and absence of integrons and resistance phenotypes.
Results: Of the 320 E. coli and Klebsiella species isolates screened, 181 (57%) contained a class I integron. A significant association was seen between the presence of the class I integron and resistance to amikacin, gentamycin, tobramycin, ampillicin, chloramphenicol, aztreonam, ceftazidime, cefotaxime, and cefpodoxime. Resistance to ciprofloxacin and cefepime was not significantly associated with the presence of an integron.
Conclusions: The presence of class I integrons in 57% of our convenience sample of E. coli and Klebsiella species isolates, along with the differential association of those integrons with resistance to some drugs, but not others, suggests that integrons may play an important role in determining how the epidemiology of bacterial resistance results from antimicrobial agent selective pressure.
| Antimicrobial | Integron | No Integron | χ2 (p value)* | Odds Ratio (95% CI)** | |
|---|---|---|---|---|---|
| Amikacin | S*** | 162 | 136 | 8.54 (0.0035) | 5.32 |
| NS | 19 | 3 | (1.54, 18.35) | ||
| Gentamicin | S | 81 | 112 | 42.15 (<0.0001) | 5.12 |
| NS | 100 | 27 | (3.07, 8.55) | ||
| Tobramycin | S | 72 | 109 | 47.77 (<0.0001) | 5.5 |
| NS | 109 | 30 | (3.33,9.09) | ||
| Ampicillin | S | 9 | 21 | 9.51 (0.002) | 3.4 |
| NS | 172 | 118 | (1.51,7.69) | ||
| Ciprofloxacin | S | 41 | 43 | 2.79 (0.0951) | 1.53 |
| NS | 140 | 96 | (0.93,2.52) | ||
| Chloramphenicol | S | 46 | 62 | 12.95 (0.0003) | 2.36 |
| NS | 135 | 77 | (1.47,3.79) | ||
| Ceflazidime | S | 89 | 91 | 8.48 (0.0036) | 1.96 |
| NS | 92 | 48 | (1.24,3.09) | ||
| Cefotaxime | S | 98 | 94 | 5.95 (0.0147) | 1.77 |
| NS | 83 | 45 | (1.12,2.80) | ||
| Cefpodoxime | S | 69 | 69 | 4.25 (0.0392) | 1.6 |
| NS | 112 | 70 | (1.02,2.50) | ||
| Cefepime | S | 161 | 124 | 0.005 (0.9415) | 1.03 |
| NS | 20 | 15 | (0.51,2.09) | ||
| Aztreonam | S | 97 | 93 | 5.78 (0.0162) | 1.75 |
| NS | 84 | 46 | (1.11,2.77) |
from Chi Square
odd ratios and 95% confidence intervals for non-susceptibility
NS - not susceptible (resistant plus intermediate where applicable); S - Susceptible
P1068: Characterisation of the AcrAB locus in two Citrobacter freundii clinical isolates
J. Sánchez-Céspedes, S. Marti, M. Ruiz, J. Vila (Barcelona, E)
Objectives: The main purpose of this study was to investigate the mechanisms of resistance to fluoroquinolones in two isogenic Citrobacter freundii clinical isolates, which led us to characterize the acrA and acrB genes of this microorganism.
Methods: Two C. freundii strains (1.44 and 1.38) sequentially isolated from the same patient were characterized. The relationship was determined by REP-PCR and PFGE. The susceptibility to ciprofloxacin and chloramphenicol was determined by Etest. Mutations in the quinolone resistance determining region of the gyrA and parC genes, the outer membrane protein profile and the accumulation of ciprofloxacin was also investigated. The expression of genes in both strains was analysed using DNA microarrays for E. coli and the expression of the acrA and acrB genes was verified by RT-PCR using the gapA gene as the control. The acrA gene was cloned and DNA sequenced.
Results: Both C. freundii belong to the same clone by both REP-PCR and PFGE. The MIC of ciprofloxacin was of 8 (strain 1.44) and 32 mg/L (strain 1.38). The MIC of chloramphenicol was of 16 and 96 mg/L, respectively. The two strains showed the same substitutions in the GyrA and ParC (Thr-83-Ile and Asp-87-Tyr in GyrA and Ser-83-Ile in ParC). No major differences were found between the outer membrane protein profiles. However, differences were observed in the amount of ciprofloxacin accumulated, with strain 1.38 showing less accumulation. Eleven genes were overexpressed in strain 1.38 compared to strain 1.44. Among these genes the acrA was overexpressed. This result was further corroborated by RT-PCR. The nucleotide similarity between the partially sequenced acrA (1027 bp) and acrB (420 bp) genes of C. freundii and E. coli was of 81.5% and 86%, respectively.
Conclusion: The acrA and acrB genes of C. freundii are similar to those described in E. coli and in collaboration with mutations in the gyrA and parC genes, their overexpression may play an important role in modulating the final MIC of fluoroquinolones.
P1069: High prevalence of aac(3)-II encoding gentamicin resistance in Escherichia coli obtained from patients with urinary tract infections in a Danish hospital
L. Jakobsen, D. Sandvang, D.S. Hansen, H. Westh, A.M. Hammerum (Copenhagen, Hvidovre, DK)
Background: Aminoglycosides are administered intravenously and are thus reserved for hospitalized patients in Denmark. Gentamicin in combination with a Betalactam antibiotic is the recommended empirical therapy for patients with suspected septicemia in Denmark. Thus, a spread of gentamicin resistance (gmR) genes is undesirable. The three most common genes causing gmR in Gramnegative bacteria in Denmark are aac(3)-II, aac(3)-IV and ant(2)-I. The objective of this study was to investigate the prevalence of gmR genes among clinical isolates of Escherichia coli from a hospital collected during a period of 13 months and to determine their clonal relationship.
Methods: Between Sep. 1st 2002 and Sep. 30th 2003, 38 gmR E. coli were isolated from patients with urine tract infections at Hvidovre Hospital. Only one isolate from each patient was included in this study. The gmR isolates were sent to National Center for Antimicrobials and Infection Control at SSI. Susceptibility to gentamicin (1-32 mg/l) was determined by the micro broth dilution method and a breakpoint of ≥16 mg/l was used. GmR isolates were investigated for the presence of aac(3)-II, aac(3)-IV and ant(2)-I by PCR. To investigate clonal relationship, the isolates were typed by PFGE using XbaI. The PFGE-types were analysed by Bionumerics resulting in a dendrogram.
Results: aac(3)-II was detected in 30 (79%) isolates among the 38 tested isolates. Neither aac(3)-IV nor ant(2)-I were detected in any of the tested isolates. It was not possible to determine the background for the gmR in eight isolates. Of the 38 isolates, 35 had 33 different PFGE-types and three were not typable. Despite the many PFGE-types, two clones occurred: One clone consisted of two isolates from Oct. 2002 and Mar. 2003. The other clone likewise consisted of two isolates detected in Apr. and Aug. 2003. aac(3)-II was detected in both clones. Furthermore, two groups of three and six isolates, respectively, obtained in different months, had related PFGE-types.
Conclusion: The gentamicin resistance was largely due to aac(3)-II gene. Even though the isolates had many different PFGE-types, isolates obtained in different months could share the same PFGE-type. This indicates persistence of aac(3)-II gentamicin resistant clones at the hospital up to a six months period.
P1070: Multidrug resistance of Gram-negative bacilli and consumption of third generation cephalosporins and imipenem in a Tunisian hospital
S. Ben Redjeb, M.A. Ben Hadj Kacem, S. Ennigrou, A. Kosontini, M. Saïdani, M. Mediouni (Tunis, TN)
Objectives: Multidrug resistance of gram negative bacilli (GNB) has become a major public health problem in Tunisia. Surveillance of both antimicrobial resistance and antimicrobial consumption has now been recognised as essential for planning future strategies to control resistance. The aim of our study is to examine for the whole hospital and wards with risks the correlation between resistance of GNB and the consumption of third generation cephalosporins (3rd GC) and imipenem for the period from January 2003 to September 2004.
Methods: A surveillance of antibiotic resistance and antibiotic consumption was established respectively by the laboratory and the department of pharmacy. Data on antimicrobial resistance and antibiotic consumption were collected quarterly and antibiotic consumption was calculated in defined daily doses (DDD) using ABC Calc. Results were expressed per 1000 bed-days (bd). Statistical analysis was done using SPSS software for the calculation of the Spearman rank correlation (rs) with an alpha risk of 5%.
Results: For the whole hospital, resistance to 3rd GC ranged from 0.9 to 1.7 GNB/1000 bd. The highest rates were observed in intensive care unit (ICU: 4.7–12.7 GNB/1000 bd) and the lowest rates in orthopaedic ward (0–2 GNB/1000 bd). A statistically significant correlation was observed between C3G consumption and resistance of GNB for the whole hospital (rs = 0.95; p = 0.001), ICU (rs = 0.82; p = 0.02) and orthopaedic ward (rs = 0.75; p = 0.05). A parallel variation was observed with imipenem consumption. Concerning general surgical wards and urology, there was not a significant correlation. For the whole hospital, during the year 2003, antibiotic consumption cost reached 26.6% of total drugs; 3rd GC and imipenem consumption cost represented 40.3% of total antibiotics. The highest rate was observed in ICU (69.8%).
Conclusion: Regarding our results, more effective strategies may be developed to combat antibio-resistance including the implementation of an antibiotic policy.
P1071: Prevalence and risk factors of acquiring MRSA and ESBL+ Enterobacteriacae vis-à-vis usage of antimicrobials
J B. Sarma (North Shield, UK)
Objectives: A point prevalence study performed in a Indian tertiary hospital (surgery, orthopaedic, medicines, n = 182, male) in 2001 to find the prevalence and risk factors of acquiring MRSA and ESBL+ Enterobacteriacae vis-à-vis usage of antimicrobials.
Methods: Dry swabs were collected (nose, throat, wounds). Isolates were carried to the Microbiology department, RVI, Newcastle, UK where works were done. A subset of S. aureus was characterised by phage typing. MRSA were typed by PFGE. A case-control study was performed.
Results: Usage of antimicrobials: 93(surgery), 60 (orthopaedic) and 53(medicine) DDD/100 bed-days. All MRSA isolates, except 2, belonged to phage group III. Majority of MSSA isolates were distinct strains. PFGE confirmed that MRSA isolates were indistinguishable.
Colonization rates: orthopaedic(MRSA, 34%;ESBL, 41%), surgery (MRSA, 18%;ESBL, 23%) medicine (MRSA, 1%;ESBL, 14%). All MRSA isolates were resistant to multiple classes of antimicrobials whereas MSSA were sensitive (p < 0.001). All ESBL+ bacteria were resistant to multiple classes but sensitive to meropenem, colistin, amikacin (82%), cotrimoxazole (50%) and chloramphenicol (50%). Resistance in non-ESBL+ bacteria was detected to ampicillin (73%), cefalexin (32%), 2nd/3rd generation cephalosporin (0%), chloramphenicol (32%), cotrimoxazole (11%), ciprofloxacin (5%), trimethoprim (21%), gentamicin (5%), netilmicin (53%) and tobramycin (11%). Potentially community acquired isolates showed lower rates of resistance (0% to trimethoprim, ciprofloxacin, gentamicin, amikacin, tobramycin, 2nd/3rd generation cephalosporin). Duration of hospital stay was not a risk for acquiring either ESBL+ bacteria or MRSA whereas having a surgery was associated. Exposure to quinolone was a risk factor for MRSA but not ESBL+ bacteria. Aminoglycoside and cephalosporin were risks for ESBL+ bacteria. Acquiring both MRSA and ESBL+ Enterobacteriacae together did correlated with the duration of hospital stay in addition to exposure to aminoglycoside and cephalosporin.
Conclusion: Majority of patients remained free from resistant bacteria implying that cross-transmission alone was not sufficient in absence of risk factors, particularly exposure to antimicrobials. Good hand-hygiene and prudent use of antimicrobials are realistic options for resource poor countries to reduce the burden of resistant bacteria. There is a unique opportunity to sequentially introduce specific infection control measure and evaluate its effectiveness.
P1072: Antimicrobial resistance in an intensive care unit before adopting an antibiotic rotation programme for empiric therapy of ventilator-associated pneumonia
G. Corti, V. Mangani, P. Pecile, B. Borchi, E. Grilli, P. Nicoletti, G. Tulli, F. Paradisi (Florence, I)
Objectives: A high prevalence of morbidity, mortality, antibiotic use, antimicrobial resistance (AR), and economic costs is generally encountered in the intensive care unit (ICU). The adoption of an antibiotic rotation programme (ARP) can minimize the emergence and spread of AR. Before initiating an ARP for empiric therapy of ventilator-associated pneumonia (VAP) in our ICU, we evaluated the AR profile of major bacterial pathogens that generally cause severe infections in the ICU.
Methods: During a 16–month period, a total of 533 nonrepetitive bacterial strains were isolated from clinical samples (primarily blood, tip of vascular catheters, bronchial aspirate and/or bronchoalveolar lavage, and urine) of adult patients admitted to a 7-bed mixed ICU of a 350-bed non-teaching hospital. Bacterial isolates were identified by automated methods (VITEK°) and tested for AR using NCCLS guidelines; they were 175 Staphylococcus aureus, 82 Pseudomonas aeruginosa, 76 coagulase-negative Staphylococci (CNS), 32 Escherichia coli, 24 Enterococcus faecalis, 18 Klebsiella pneumoniae, and other species with <15 isolates each.
Results: Among gram-negative aerobic bacilli, we found P. aeruginosa strains to be meropenem and piperacillin/tazobactam-resistant in 22% and 14.6% of cases, respectively; P. aeruginosa, E. coli and K. pneumoniae were resistant to ceftazidime in 29.3%, 6.25%, and 0% of cases, respectively, and resistant to ciprofloxacin in 54.9%, 12.5%, and 5.6% of cases, respectively. Neither E. coli nor K. pneumoniae were resistant to either meropenem or piperacillin/tazobactam. Among gram-positive aerobic cocci, oxacillin-resistant S. aureus and CNS were 55.8% and 82.7%, respectively; S. aureus isolates were very susceptible to cotrimoxazole (resistance 7.65%) and rifampin (11%), whereas resistance exceeded 40% for clindamycin, gentamicin, and norfloxacin. Ampicillin- and penicillin-resistant E. faecalis were 20.8% and 33.3%, respectively. Neither S. aureus nor E. faecalis were resistant to vancomycin, whereas one CNS strain was resistant to it (1.3%) and 6 out of 76 to teicoplanin (7.9%).
Conclusion: In our ICU, where a careful policy of antibiotic use with no predetermined restrictions has been applied for years, AR among both gram-negative and gram-positive microorganisms is generally lower than in the ICUs of Italy and other Mediterranean countries. We expect that the institution of an ARP for empiric therapy of VAP can further minimize AR in our ICU.
Difficult to treat nosocomial infections
P1073: Cure of post-traumatic recurrent multiresistant Gram-negative rod meningitis with intraventricular colistin
S. Kasiakou, P. Rafailidis, K. Liaropoulos, I. Bliziotis, F. Chelvatzoglou, M. Falagas (Athens, GR)
Background: Although newer antibiotics have been introduced to the market during the last years, they have not solved the problems arising in the management of infections due to multiresistant Gram-negative bacteria. Colistin, an antibiotic almost forgotten for decades has proved itself helpful, when used parenterally in patients where a lot of the classic and newer antibiotics fail.
Methods: We report our experience with the management of the case of a young patient who, after head trauma, had five episodes of meningitis due to multidrug-resistant Gram-negative microorganisms.
Results: A 28-year-old patient was admitted in our hospital because of coma. Three months prior to his admission, he sustained acute brain injury due to a fall and was hospitalized elsewhere for this entire period. A computerized tomography scan of his brain at his admission in the first hospital, showed multiple cerebral contusions, and an intracerebral hematoma causing deviation of the midline. He underwent a decompressive craniotomy with removal of the hematoma. During his long-standing hospitalization, he developed 5 episodes of meningitis, i.e. on day 65, 96, 108, 147, and 165 after head trauma. The pathogens isolated from each episode of meningitis were multiresistant strains of Pseudomonas aeruginosa (1st and 2nd episodes), Acinetobacter baumannii (3rd episode), Enterobacter cloacae (4th episode), and Acinetobacter baumannii (5th episode). The two episodes of Acinetobacter baumannii meningitis were managed only when colistin and amikacin were given by the intraventricular in addition to the intravenous route for long period of time (six weeks for the last episode) and in high doses (40,000 IU of colistin and 10 mg of amikacin).
Conclusion: Intraventricular colistin should be considered to be a life-saving therapeutic intervention in cases of multi-resistant Gram-negative rod meningitis.
P1074: Intravenous colistin for treatment of infections due to multidrug-resistant Gram-negative bacteria in patients without cystic fibrosis
S. Kasiakou, A. Michalopoulos, E. Soteriades, G. Samonis, G. Sermaides, M. Falagas (Athens, GR; Boston, USA; Iraklion, GR)
Background: Colistin, an antibiotic almost abandoned for intravenous administration for many years, due to its reported toxicity, has been recently reintroduced in clinical practice due to the emergence of multidrug-resistant Gram-negative bacteria and the lack of development of new antibiotics to combat them. Objective: To assess the safety and effectiveness of intravenous colistin in the treatment of serious infections in patients without cystic fibrosis.
Design: Retrospective cohort study.
Setting: 450-bed tertiary-care hospital in Athens, Greece.
Patients: Patients who were hospitalized during the period from 1/October/2000 to 31/January/2004 and received intravenous colistin for more than 72 hours.
Measurements: Primary outcome measure was the in-hospital mortality; secondary end points were the clinical outcome of the infections and the occurrence of colistin toxicity.
Results: Fifty patients received intravenous colistin with a median (mean) daily dose of 3 (4.5) million IU for 16.5 (21.3) days for the management of 54 episodes of infections due to multidrug-resistant Gram-negative bacteria. The predominant infections were pneumonia (33.3%), bacteraemia (27.8%), urinary tract infection (11.1%), and intra-abdominal infection (11.1%). The responsible pathogens were Acinetobacter baumannii (51.9%), Pseudomonas aeruginosa (42.6%), and Klebsiella pneumonia (3.7%) strains (no pathogen was isolated from one case). In-hospital mortality was 24% (12/50 patients). Clinical response (cure or improvement) of the infection was observed in 66.7% of episodes (36/54). In the studied group, serum creatinine levels were decreased, at the end of colistin treatment, by an average of 0.2 ± (1.3) mg/dl compared to baseline levels. Deterioration of renal function during colistin therapy was observed in 4/50 patients (8%).
Limitations: Co-administration of other antimicrobial agents with spectrum against Gram-negative microorganisms and the absence of a control group.
Conclusions: Use of intravenous colistin for the treatment of infections due to multidrug-resistant Gram-negative bacteria appears to be safe and effective.
P1075: Aerosolised colistin for the treatment of nosocomial pneumonia due to multidrug-resistant Gram-negative bacteria in patients without cystic fibrosis
A. Michalopoulos, S. Kasiakou, Z. Mastora, K. Rellos, A. Kapaskelis, M. Falagas (Athens, GR)
Background: The clinical and economical consequences of the emergence of multidrug-resistant Gram-negative bacteria in the intensive care unit (ICU) setting in combination with the high mortality rate among patients with nosocomial pneumonia have made the medical community to search for alternative therapeutic options. The use of adjunctive therapy with aerosolized colistin represents one of them. Extensive experience with aerosolized colistin exists in patients with cystic fibrosis. However, the literature lacks data regarding the use of aerosolized colistin in non-cystic fibrotic patients.
Methods: To assess the safety and effectiveness of aerosolized colistin as an adjunctive to the intravenous antimicrobial therapy for the treatment of Gram-negative nosocomial pneumonia, we retrospectively reviewed the medical records of patients, who were hospitalized in a 450-bed tertiary-care hospital during the period from October/2000 to January/2004, and received aerosolized colistin as an adjunctive therapy for multidrug-resistant pneumonia.
Results: Eight patients received aerosolized colistin. All were admitted to the ICU with a mean Acute Physiological and Chronic Health Evaluation II (APACHE II) score on the day of ICU admission and on the 1st day of aerosolized colistin administration of 14.6 and 17.1, respectively. Six of the 8 patients had ventilator-associated pneumonia. The responsible pathogens were Acinetobacter baumannii (7/8 cases) and Pseudomonas aeruginosa (1/8 cases) strains. Half of the isolated pathogens were sensitive only to colistin. Daily dosage of aerosolized colistin ranged from 1.5 to 6 million IU (divided into 3 or 4 doses) and the mean duration of administration was 10.5 days. Seven out of 8 patients received concomitant intravenous treatment with colistin or other antimicrobial agents. Clinical response of pneumonia was observed in 7 out of 8 patients [4 cured, 3 improved (they were transferred to another facility)]. One patient deteriorated and died due to septic shock and multiple organ failure. Aerosolized colistin was well tolerated by all patients; no bronchoconstriction or chest tightness was reported.
Conclusions: Aerosolized colistin may be a beneficial adjunctive treatment in the management of nosocomial pneumonia (VAP or not) due to multidrug-resistant Gram-negative bacteria.
P1076: Toxicity after prolonged (more than four weeks) administration of intravenous colistin
M. Falagas, M. Rizos, I. Bliziotis, K. Rellos, S. Kasiakou, A. Michalopoulos (Athens, GR)
Objective: To study the toxicity of prolonged intravenous administration of colistin
Design: Observational study of retrospective cohort.
Setting: ‘Henry Dunant’ Hospital, a 450-bed tertiary care centre in Athens, Greece.
Participants: Patients who received intravenous colistin for more than 4 weeks for the treatment of multidrug resistant Gram-negative infections.
Main outcome measures: Serum creatinine, blood urea, liver function tests, symptoms and signs of neurotoxicity.
Results: We present our experience with the use of 19 courses of prolonged intravenous colistin [mean duration of administration (±SD) 43.4 (±14.6) days, mean daily dosage (±SD) 4.4 (±2.1) million IU, mean cumulative dosage (±SD) 190.4 (±91.0) million IU] in 17 patients. The median creatinine value increased by 0.25 mg/dl during the treatment compared to the baseline (p < 0.001) but returned close to the baseline at the end of treatment (higher by 0.1 mg/dl, p = 0.67). No apnea or other evidence of neuromuscular blockade was noted in any of these patients who received prolonged treatment with colistin.
Conclusions: No serious toxicity was observed in patients who received prolonged intravenous colistin. Colistin should be considered as a therapeutic option in patients with infections due to multidrug resistant Gram-negative bacteria.
P1077: Colistin-resistant Acinetobacter baumannii: report of a case
O. Bargiacchi, G. Fucale, F.G. De Rosa, E. Carretto, S. Garazzino, S. Audagnotto, D. De Vitis, D. Barbarini, G. Di Perri (Torino, Pavia, I)
Acinetobacter baumannii is an important nosocomial pathogen and outbreaks by multi-drug resistant (MDR) strains have been reported worldwide, especially in burn and intensive care units. The most effective drugs are carbapenems, colistin and new glicilcyclines, even if reports of carbapenem-resistant strains are increasing worldwide. To date, susceptibility rates to imipenem and colistin of nosocomial strains are reported as high as 88% and >98%, respectively. In particular, resistance to colistin has been rarely described and the mechanisms of this resistance are poorly understood. We report a case of colistin resistant A. baumannii infection in a patient without previous administration of colistin.
Case report – Methods: A colistin resistant (MIC >2 mcg/ml) A. baumannii was isolated from 3 sets of blood cultures in a patient admitted in a burn unit without previous colistin exposure. The patient was treated with ampicillin/sulbactam and colistin, despite the documented resistance to all antibiotics. MDR A. baumannii was repeatedly isolated from different sites and the patient died after 61 days of hospitalization. Strain identification and susceptibility tests were performed using Phoenix automated microbiology system®. Resistance to ampicillin, ampicillin/sulbactam, ceftazidime, imipenem, meropenem, cotrimoxazole, amikacin, ciprofloxacin and colistin was confirmed by disk diffusion test and broth microdilution, in accordance with the NCCLS guidelines. The susceptibility results were confirmed by a reference laboratory.
Conclusion: Colistin is one of the few effective drug available against MDR Acinetobacter infections and acquired resistance is exceptional. Our report points out that colistin resistant A. baumannii may be found in hospitalized patients without previous exposure to colistin. Nosocomial infections by colistin-resistant A. baumannii could represent a new therapeutic challenge. Programmes of active surveillance cultures and contact precautions should be implemented to control the spread of this MDR microorganism.
P1078: Intrathecal colistin treatment of central nervous system infections due to multi-resistant Acinetobacter baumannii
C. Suárez Fernández, P. Fernández-Viladrich, F. Tubau, L. Corral, A. Mateu, J. Ariza (Barcelona, E)
Objectives: The optimal therapy of CNS infections due to Multi-resistant Acinetobacter baumannii (MRAB) is not established. In 1999 we published the first two cases of ventriculitis due to MRAB treated with intrathecal (it) colistin. One patient received 10 mg colistin base/12 hours after delayed CSF sterilization was documented with initial dosage of 5 mg/12 hours. Here we describe our extended experience with this kind of treatment .
Methods: We retrospectively reviewed all documented CNS infections due to MRAB diagnosed in our terciary 1000-bed hospital from 1999 to 2004. MRAB was defined as those strains with only susceptibility to colistin (MIC < 4 mg/L). CNS infections were defined as those cases with suggestive clinical features plus ventricular or lumbar CSF with both characteristic cytochemical alterations and positive culture.
Results: There were 7 cases with documented nosocomial CNS infection due to MRAB. Six of them were acquired after neurosurgical procedure through surgical wound infection or local catheter infection. One case was caused by hematogenous spread after urological manipulation. Intrathecal therapy was administered through a ventricular catheter in five cases, lumbar catheter in one case and both ventricular and lumbar catheter in one case. The usual doses administered was colistin base 10 mg (equivalent to colistimethate sodium 24 mg) every 12 hours with CSF continuous drainage being interrupted for about 3 hours. Length of treatment were 8–21 days with any apparent adverse effect. Six of these patients received simultaneous intravenous colistin therapy. Culture sterilization was documented in all patients. Two patients died (one from unclear cause after initial favorable evolution; one after receiving only two doses of it colistin). The rest of them cured with sequela attributable to their previous neurological diseases.
Conclusions: In our experience, combined treatment with both intrathecal and intravenous colimicin seems safe and effective. When administered by local route to patients with continuous CSF drainage we suggest a dosage of colistin base of 10 mg every 12 hours with temporary interruptions of the drainage.
P1079: Bacillus cereus – the forgotten pathogen. An unusual infection in an orthopaedic patient
S. Thomas, A. Pillai, J. Arora, A.C. Ogden (Dumfries, UK)
Background: Infection with Bacillus cereus has been well documented in the literature for over a century. Infection is generally associated with the gastrointestinal effects of food poisoning and linked to the consumption of infected rice dishes. However, the Bacillus genus is extremely heterogenic. It can occupy a wide variety of ecological niches and bacillus spores are found ubiquitously in the environment. Even so, Bacillus cereus isolated from the hospital and clinic setting in any material other than vomitus or faeces is commonly dismissed since it is a known contaminant of blood cultures and most bacillus bactereamias are transient and usually insignificant.
Case Report: We report a case of Bacillus cereus wound infection in a previously healthy 31-year-old male admitted to the orthopaedic ward with a comminuted fracture of the right distal tibia. He developed compartment syndrome one day later and was taken to theatre for fasciotomy. Within 48 hours, he developed chest complications and was admitted to the High Dependency Unit. After three days he was taken back to theatre for wound inspection and change of dressing. Seven days later external fixation was applied. Subsequently, the wound site became red, inflamed and tender and was associated with an acute rise in inflammatory markers. Microbiological reports showed Bacillus cereus growth from the suture sites, sensitive to ciprofloxacin. No source was identified.
Discussion: This report merits concern, because it highlights the risk of wound cross infection with this unlikely pathogenic species. Bacillus cereus has been known to be a contaminant of dressings, intravenous catheters, theatre scrub suits and linens pointing to an array of possible infective sources within the hospital. It emphasizes the need for theatre and hospital sterility and stresses the importance of vigilance against this infrequent cause of a potentially serious non-gastrointestinal bacillus infection. This is of particular importance because alcohol-based cleaning solutions are known to be ineffective against bacillus spores and infections dismissed as contaminants may lead to rapid clinical deterioration.
P1080: Antibacterial effect of phenytoin in wound healing
S. Abolghasemi, B. Mostanfar (Tehran, IR)
Objectives: Phenytoin is an antiseizure medication, has since been reported to promote wound healing when applied as a topical agent. This effect is due to rapid infiltration of fibroblasts, collagen deposition, new vessel formation as well as antibacterial activity. This study was undertaken to evaluate it's effect on chronic skin ulcers with different causes and compare it with normal saline.
Methods: Fifty inpatients with chronic skin ulcers were included in this case-control study: diabetic foot (20%), fracture and surgery wounds (40%), decubitus ulcers resulting from war-related (40%). The patients were matched for age, sex, severity and size of wounds and randomly assigned to two group: 25 phenytoin treated (pht) and 25 control (ctl). Each group included 15 men and 10 women, age range was between 20 and 60. Surface areas of the ulcers was 12–200 cm2. The ulcers were debraded of necrotic tissue (if required). Cultures of ulcers were taken at the beginning of treatment and on day 7, 14. In pht, thin dusting of phenytoin powder and dry gauze dressing were applied daily after washing with normal saline. Ctl group received only daily washing with normal saline and plain dressing.
Results: Bacteriologic culture in both group confirmed some strains (Staphylococcus aureus, Kelebsiella, Proteus and Psudomonas). At the beginning of treatment, there was 17 culture positive in pht. 13 case became negative by day 7 and 4 case became negative by day 14. In ctl, we had 15 culture positive that they didn't become negative by day 7 and 14 (seventy-six per cent of pht had negative cultures by day 7 compared to 0% of ctl). The mean time for appearance of granulation tissue was 13.48 days in pht compared with ctl that was 37.5 (p = 0.006). The average time to complete healing in pht was 24.76 days compared to 43.36 in the ctl (p = 0.0001). In pht only 13 patients required to analgesics (mean 1/day) compared with ctl that all patients required to analgesics about 3–4/day (p = 0.0001). Age, sex and kind of wounds didn't effect the healing time in both group.
Conclusions: This study with statistical analysis demonstrated good improvement and efficacy of phenytoin in treatment of chronic ulcers compared with normal saline. 1. prompt pain relief, 2. reduction in ulcer size, 3. changing bacterial culture to negative, 4. more rapid granulation and healing time, characterized the pht group. We recommend wider use of this safe, inexpensive, readily available and easy to use agent because of it's positive effect on wound healing especially in our country that a lot of patients suffer from decubitus ulcers resulting from war-related wounds and limited access to more expensive wound care therapies.
P1081: Recurrent osteomyelitis secondary to different bacteria
I. Uckay, M. Assal, L. Legout, P. Rohner, R. Stern, D. Lew, P. Hoffmeyer, L. Bernard on behalf of the Osteomyelitis Group Study
Objective: Recurrence of osteomyelitis due to the same bacteria from a prior site of infection without evidence of trauma or bacteraemia is an entity well-known in the literature and clinical practice. The objective of this study is to try and determine if all these reactivations are actually due to the same bacteria, as has been assumed in previous case reports.
Case reports: We report three cases of osteomyelitis recurring in the same bone in otherwise healthy patients. In all three patients, there was no history of illness or trauma to assume another origin. Surprisingly, the strains were different from the two infectious episodes.
Conclusion: Reactivation of osteomyelitis can be caused by different strains of bacteria, many years after the initial episode without trauma or evident bacteraemia. Former infected and therefore altered bone surface might be a region of diminished resistance for a new infection during silent transient bacteraemia, reminiscent of the clinical entity of (recurrent) infectious endocarditis on altered valve surfaces.
P1082: Aetiological factors of vascular grafts infection and their antimicrobial susceptibility
J. Niedzwiadek, E. Mazur, S. Misztal, B. Ziemba, P. Terlecki, J. Ligieza, M. Koziol-Montewka, J. Wronski (Lublin, PL)
Objectives: Vascular graft infection proved to be the most dangerous complication in vascular surgery patients. The aim of our study was the identification of microorganisms causing vascular graft infections and the evaluation of their antimicrobial susceptibility. 25 patients with infected vascular grafts, treated in Vascular Surgery Department, took part in our research. In 76% of patients, the late type of infection was recognized, in 24% of patients the infection was qualified as early.
Methods: Purulent discharge obtained from the fistula was inoculated on the bacteriological media. Antimicrobial susceptibility was assessed by disc-diffusion method.
Results: Staphylococcus aureus and Pseudomonas aeruginosa, present in 16,7% of patients, proved to be the most frequently isolated microorganisms. Staphylococcus epidermidis and E. coli were isolated in 13.3% and 10% of patients, respectively. Mixed infection, caused by two distinct bacteria, occurred in 20% of patients; in all cases one species belonged to Gram-positive, and the second one to Gram-negative bacteria. In 50% of patients with early type infection different species of Gram-negative rods were present, in 37.5% of patients, Staph. aureus and Staph. epidermidis were isolated, Enterococcus faecalis occurred in 12.5% of patients. In late type infection Gram-negative rods were isolated from 54.5% of patients and Gram-positive bacteria from 31.5% of patients. The most frequently isolated species appeared to be Pseudomonas aeruginosa. In one patient Candida crusei was isolated. The isolated species of bacteria varied depending on the degree of infection (according to Shilagy and Samson). In IIIA degree of infection Staph. epidermidis and E. coli were present in 67.7% and 33.0% of patients, respectively. Pseudomonas aeruginosa and Staph. aureus were isolated in 21,1% of patients with IIIB degree of infection. Various species of Gramnegative rods were isolated from 80% of patients with IIIC degree of graft infection.
Conclusions: Most isolated bacteria appeared to possess the resistance patterns typical for hospital flora; among them methicillin-resistant Staph. aureus (MRSA) and methicillin-resistant coagulase-negative Saphylococci (MRCNS) strains, Gramnegative rods producing extended spectrum of beta-lactamases (ESBL) or AmpC beta-lactamases, and Enterococcus faecalis with high level of aminoglicosides resistance (HLAR).
P1083: Treatment failure due to emergence of resistance to imipenem during therapy for Shewanella algae bacteraemia
D.M. Kim, M.-D. Oh (Gwang-Joo, Seoul, KOR)
Objective: We describe here a case of bacteraemia caused by S. algae, which was initially susceptible to imipenem, but the bacteria later became resistant during the treatment. In addition, we investigated the propensity of S. algae to develop resistance to imipenem by using a serial passage technique.
Method: In vitro test for resistance induction 1. Bacterial strains Resistant variants selection
(a) single step resistant variants were obtained from clinical Isolate on Mueller-Hinton agar containing increasing amounts of imipenem (1xMIC, 2xMIC, 4xMIC, 8xMIC),
(b) serial passage experiment S. algae strain and P. aeruginosa ATCC 27853 were grown overnight in Mueller–Hinton agar and then grown overnight in Mueller–Hinton agar and then swabbed onto Mueller–Hinton agar plates containing one-half the MIC of imipenem. The surface growth at 24 h was swabbed to Mueller–Hinton agar containing twice the prior concentration of imipenem.
Results: Single step resistant variants were selected from Isolate 1 at up to 4 times the MIC, whereas the resistant variant from P. aeruginosa ATCC 27853 could be selected at up to 2 times the MIC. All the resistant variants of S. algae selected either by a single step or by a sequential stepwise passage exhibited at up to 8–16 μg/ml of MIC, whereas those of P. aeruginosa ATCC 27853 showed up to 16 μg/ml of MIC
Conclusion: We documented that S. algae, which was initially susceptible to imipenem, subsequently became resistant to imipenem during the treatment. We also demonstrated in vitro that the initial isolate of S. algae could easily develop resistance to imipenem when the organism was exposed to imipenem, suggesting that S. algae organisms have a propensity toward resistance to imipenem.
P1084: Micro-organisms from peritoneal fluid of patients on continuous ambulatory peritoneal dialysis
M. Dimoutsos, E. Platsouka, E. Perivolioti, E. Patsouris, C. Moularogianni, S. Kallia, G. Margariti, O. Paniara (Athens, GR)
Objective: Peritonitis remains a common and serious complication of peritoneal dialysis. In this study, we evaluated the frequency of microorganisms isolated from peritoneal fluids of patients on continuous ambulatory peritoneal dialysis (CAPD).
Methods: During a 2.5 year period, 321 peritoneal fluid samples were collected from 107 CAPD patients with peritonitis symptoms. The specimens were inoculated on appropriate media after 10-min centrifugation. Gram stained smears and aerobic, anaerobic and broth cultures were performed. The isolates were identified by commercial ID panels. MICs were determined with a microdilution method according to NCCLS guidelines.
Results: Fifty two out of 321 samples were positive (16.2%), six of the positives were polymicrobial. The following microorganisms were obtained: Pseudomonas aeruginosa (8), Staphylococcus epidermidis (7), Escherichia coli (7), Staphylococcus aureus (6), Streptococcus viridans (6), Klebsiella pneumoniae (4), Enterococcus faecalis (4), Stenotrophomonas maltophilia (4), Enterobacter aerogenes (2), Acinetobacter baumannii (1), Enterococcus faecium (1), Proteus mirabilis (1), Pseudomonas fluorescens/putida (1), Acinetobacter lwoffii (1), Salmonella group D (1), Bacteroides spp. (2). Fungi were isolated in three patients: Candida tropicalis (1), Candida krusei (1) and Candida parapsilosis (1). Three out of 6 of S. aureus strains and three out of 7 of S. epidermidis isolates were found resistant to methicillin. All Saphylococci and Enterococci were susceptible to vancomycin and linezolid. Gram-negative pathogens were sensitive to used antibiotics.
Conclusion: Thirty five patients (32.7%) developed peritonitis The most prevalent etiologic agents of peritonitis on CAPD patients were Pseudomonas aeruginosa, Staphylococcus epidermidis, Escherichia coli, Staphylococcus aureus and Streptococcus viridans. Since CAPD patients are commonly outpatients, the antimicrobial resistance in the Gram-negative strains is low compared to the nosocomial isolates. Appropriate antibiotic therapy based on microbiologic results needs for the management of peritonitis on CAPD patients.
Susceptibility surveillance studies
P1085: In vitro activity of cefepime and other broad spectrum antibiotics against Gram-negative and Gram-positive pathogens causing severe infections in hospital patients. Results of a German surveillance study
F.-J. Schmitz (Minden, D)
Objectives: Cefepime is a fourth generation cephalosporin with a broader spectrum of activity against Gram-negative and Gram-positive pathogens in comparison with all other cephalosporins. Due to the excellent antibacterial activity including Pseudomonas aeruginosa and Enterobacter spp. together with low rates of resistance and favourable pharmacokinetic and clinical properties, cefepime is a drug of choice for initial empiric treatment of severe nosocomial infections. Nevertheless, in addition to recommendations in guidelines, the surveillance of local resistance data is important for empiric treatment decisions in hospitals.
Methods: In this study, the in vitro activity of cefepime (CEP), imipenem (IMI), piperacillin tazobactam (P/T), ceftazidime (CAZ) and cefotaxime (CFT) has been investigated against 1130 bacterial strains, isolated in the year 2004. MICs have been determined by microdilution method according to DIN 58940. Reference test strains were E.coli ATCC 25922, S. aureus ATCC 29213, P.aeruginosa ATCC 27853, and S.pneumoniae ATCC 49619.
Results: Highest in vitro activity against Gram negative Enterobacteriaceae were determined for CEP and IMI with susceptibility rates for Enterobacter spp. 98%,98%, M.morganii 96%,92%, Proteus spp. 98%,96% and Citrobacter spp. 96%,100% whereas the susceptibility rates for P/T, CAZ and CFT were much lower (E.spp. 68%,72%,68%; M.m. 88%,72%,66%; P.spp. 96%,96%,66%; C.spp. 68%,76%,72%). For Pseudomonas aeruginosa (n = 100), susceptibility rates were 76% (CEP), 73% (CAZ), 72% (IMI) and 55% (P/T) with lowest resistance rates for CEP (6%) followed by CAZ (11%), P/T (14%), IMI (23%). The study confirmed excellent cefepime activity against Gram positive isolates (pneumococci, Streptococcus viridans and β-hemolytic Streptococci) and high cefepime susceptibility rates for Staphylococci (MSSA 99% and MSSE 98%) on contrary to ceftazidime (MSSA 44% and MSSE 42%).
Conclusion: Regarding our in vitro data, CEP is a reliable treatment option for empiric therapy in patients with severe nosocomial infections, demonstrating high activity against Gram positive isolates, comparable activity in Gram negative Enterobacteriaceae to carbapenems (IMI) and lowest resistance rates in Pseudomonas aeruginosa.
P1086: Antimicrobial activity and spectrum of cefepime tested against 65,746 clinical strains from North American medical centres: report from the SENTRY Antimicrobial Surveillance Program, 1998–2004
H. Sader, D. Biedenbach, T. Fritsche, R. Jones (North Liberty, USA)
Objectives: To evaluate antimicrobial spectrum and potency of cefepime (CPM) and selected comparators against clinical bacterial strains collected in North America (NA) over a 7-year period (1998–2004).
Methods: Isolates were consecutively collected from bloodstream (44%), respiratory tract (41%), urinary tract (6%) and skin/soft tissue (5%) infections in 48 medical centres. 75% of isolates were from hospitalized patients. Isolates were susceptibility (S) tested by reference NCCLS broth microdilution methods in a central laboratory. Oxacillin-resistant (R) Staphylococci (ORS) and Enterococci were excluded.
Results: The activity of CPM against the key organisms tested is summarized in the Table. Overall, 99.8% of Gram-positive cocci (GP) tested were S to CPM. Imipenem (IMP; MIC90, 1 mg/L; 99.9% S) was the most active compound tested against ENT, followed by CPM (MIC90, 0.25 mg/L; 99.5% S) > amikacin (AMK; 99.4% S) > ceftriaxone (95.6% S) > aztreonam (95.1% S). The lowest S rate for ENT was observed with ciprofloxacin (CIPRO; 92.8%). IMP was also the most active compound against ESBL-producing KSP and E. coli (99.3 and 100% S, respectively), followed by AMK (81.4 and 97.2% S) and CPM (92.5 and 93.8% S). CPM activity against PSA (85.2% S) was similar to that of IMP (86.9% S). Against OSSA, CPM was 4-fold more potent than ceftazidime (CAZ; MIC90, 16 mg/L, 86.4% S) and showed higher activity than CIPRO (93.2% S). CPM was the most active compound against SPN after gatifloxacin and levofloxacin (99.2% S). Against VGS, CPM was 8-fold more potent than CAZ and 4-fold more potent than piperacillin/tazobactam. The activity of CPM remained very stable during the period evaluated with the % S varying from 99.5 to 99.3% among ENT, 85.2 to 88.4% among PSA, 98.1 to 97.6% among SPN, and 94.4 to 92.6% among VGS.
| MIC (mg/L) |
Cumulative % inhibited at MIC (mg/L): |
|||||||
|---|---|---|---|---|---|---|---|---|
| Organism (no. tested) | 50% | 90% | ≤0.5 | 1 | 2 | 4 | 8 | 16 |
| E. coli (10,361) | ≤0.12 | ≤0.12 | 98.5 | 99.1 | 99.4 | 99.6 | 99.7a | 99.18 |
| Klebsiella spp. (KSP; 5,166) | ≤0.12 | 0.25 | 94.4 | 96.0 | 97.5 | 98.6 | 99.3 | 99.7 |
| Enterobacter spp. (2,836) | ≤0.12 | 2 | 85.9 | 89.9 | 94.1 | 97.3 | 99.0 | 99.6 |
| Serratte, spp (1,412) | ≤0.12 | 0.25 | 95.6 | 97.2 | 98.5 | 99.0 | 99.3 | 99.6 |
| P. mirabilis (1, 225) | ≤0.12 | ≤0.12 | 98.6 | 98.9 | 99.0 | 99.3 | 99.5 | 99.7 |
| All Enterobacteriaceae (ENT; 22,860) | ≤0.12 | 0.25 | 95.5 | 97.0 | 98.1 | 99.0 | 99.5 | 99.7 |
| H. influenzae (7,975) | ≤0.06 | 0.12 | 99.9 | 100.0 | ||||
| P. aeruginosa (PSA; 5,517) | 4 | 16 | 1.9 | 13.8 | 45.1 | 67.0 | 85.2 | 94.5 |
| Oxacillin-S S. aureus(OSSA; 10,835) | 2 | 4 | 0.6 | 2.4 | 68.3 | 99.5 | 100.0 | |
| S. pneumoniae (9,249) | ≤0.06 | 1 | 85.3 | 97.4 | 99.7 | 99.9 | 100.0 | |
| β-haemoytic strept (2,703) | ≤0.12 | <0.12 | 99.9 | 100.0 | ||||
| viridans gr. strept. (VGS; 783) | ≤0.12 | 1 | 88.8 | 94.1 | 99.7 | 999 | 100.0 | |
Underline values indicate % S.
Conclusions: CPM was very active against ENT, PSA and GP cocci (except ORS and Enterococci) isolated in NA medical centres. CPM activity remained stable in the 7-year period of the study with low level of cross-R to third-generation cephalosporins. Continued R surveillance is necessary to monitor the effectiveness of widely used antimicrobials.
P1087: The prevalence of multidrug resistance among Streptococcus pneumoniae in the United States
R. Blosser, G. Tillotson, R.K. Flamm, D.A. Styers, D.F. Sahm, M. Jones (Herndon, Waltham, USA; Hilversum, NL)
Objectives: In the U.S., recent approval of antimicrobial agents (e.g. gemifloxacin [GEM]) with indications for multiple drug resistant (MDR) S. pneumoniae (SP) demonstrates a positive industry and governmental response to the need for development of agents against resistant (R) pathogens. This mandates the need for surveillance initiatives to track MDR, as opposed to tracking a single agent's resistance (e.g. penicillin [PEN]). We investigated the current status of MDR among recent clinical isolates of SP distributed throughout USA.
Methods: TSN Database-USA (Jan–Dec, 2003) was used to evaluate the current prevalence of the MDR SP in nine geographic urban areas (Atlanta, Baltimore/DC, Carolinas, Central Florida, Chicago, Dallas, Los Angeles, Ohio, South Florida). MDR prevalence was also analysed on the basis of specimen source (upper respiratory [UR], lower respiratory [LR], blood [BL]). MDR was defined as resistance to ≥2 among PEN, erythromycin (ERY), and trimethoprim-sulfamethoxazole (SXT). We also selected 30,2003 MDR SP clinical strains to evaluate the relative in vitro activities of respiratory fluoroquinolones (GEM, gatifloxacin [GAT], moxifloxacin [MXF], and levofloxacin [LFX]).
Results: Among SP from all regions combined, the MDR rate was 19.2%. R to PEN, ERY, and SXT was the most common phenotype. Regionally, MDR ranged from 9.1% in Los Angeles to 32.2% in South Florida. R to PEN, ERY, and SXT was the most common MDR phenotype in all regions except Baltimore/DC (R to ERY and SXT was most common). By specimen source, 15.5% of blood, 21.0% of LR, and 29.0% of UR isolates were MDR with R to PEN, ERY, and SXT being the most common phenotype regardless of specimen source. For the 30 strains tested, the fluoroquinolone MIC ranges were: 0.008–0.03 mg/L (GEM), 0.12–0.25 mg/L (GAT), 0.06–0.25 mg/L (MXF), 0.5–1 mg/L (LFX).
Conclusions: MDR among SP is a phenotype that is widely dispersed geographically and is likely to be encountered regardless of the site of infection. Fluoroquinolones show activity against most MDR isolates. As the use of fluoroquinolone compounds increases, surveillance to monitor the prevalence of MDR and track the in vitro activity of agents such as GEM used for these resistant strains must be continued.
P1088: Comparative activity of oral and parenteral cephalosporins against multi-drug-resistant Streptococcus pneumoniae: report from the SENTRY Antimicrobial Surveillance Program (1997–2003)
S. Pottumarthy, T. Fritsche, H. Sader, R. Jones (North Liberty, USA)
Background: multi-drug resistant (MDR) S. pneumoniae strains are increasing at an alarming rate worldwide. The therapy of respiratory tract infections due to these strains is challenging with an urgent need for antimicrobials with reliable activity against the MDR strains. Comparative activity of oral cephalosporins and parenteral cephalosporins against various pneumococcal MDR phenotypes was analysed in a large, multi-year international collection of clinical strains of S. pneumoniae.
Methods: S. pneumoniae strains (21,605) collected during 1997–2003 from worldwide participants of the SENTRY Program were tested and interpreted using NCCLS (M7-A6, M100-S14) guidelines. The antimicrobial agents analysed included penicillin (PEN), erythromycin (ER), clindamycin (CM), tetracycline (TET) and trimethoprim/sulfamethoxazole (TS); cephalosporins monitored included oral (cefpodoxime, cefuroxime) and parenteral (ceftriaxone, cefepime) agents.
Results: The rank order of occurrence rates of the various resistance phenotypes were: PEN only (32.0%) > PEN and ER (17.6%) > PEN, ER and CM (8.6%) > PEN, ER, CM and TET (7.6%) > PEN, ER, CM and TS (6.5%) > all five drugs (5.7%). The susceptibility rate of all strains to the orally administered cephalosporins, cefpodoxime (77.6%) and cefuroxime (77.3%), dropped to only 16.1% and 14.5% respectively, for the five-drug MDR phenotype. The parenteral cephalosporins retained excellent activity for all MDR phenotypes, with resistance rates being lower for cefepime than ceftriaxone (cefepime, 1.3–1.9%; ceftriaxone, 3.0–4.4%) or the oral cephalosporins (cefpodoxime, 64.4–74.1%; cefuroxime, 69.3–79.1%) using respiratory infection breakpoints (NCCLS).
Conclusions: Our in vitro findings confirm that the parenteral cephalosporins, cefepime and ceftriaxone, retain excellent activity against the MDR phenotypes analysed, and remain useful drugs in the armamentarium to treat MDR pneumococcal respiratory tract infections.
P1089: Antibiotic resistance surveillance over a 5-year period in Spain: results of the MYSTIC Programme
A. Pascual, E.J. Perea, M. Alvarez, M. Casal, J. García-de-Lomas, J.A. García-Rodríguez, R. Martin, J. Zapardiel and the Spanish MYSTIC group
Objective: To monitor resistance trends to meropenem (MEM) and other broad-spectrum antibiotics among bacteria isolated over a five-year period in 7 Spanish hospital units involved in the MYSTIC programme, a global study providing in-vitro surveillance data on antimicrobial susceptibility in centres prescribing meropenem.
Methods: Organisms were tested using National Committee for Clinical Laboratory Standards (NCCLS) methodology. Minimum inhibitory concentration (MIC) values and percentage susceptibilities at NCCLS breakpoints (%S) were obtained for MEM and a range of comparators including imipenem (IPM), ceftazidime (CAZ), piperacillin + tazobactam (TAZ), ciprofloxacin (CIP) and gentamicin (GM).
Results: Three ICUs, two neutropenia units and two general wards provided a total of 4.022 Gram-negative and Gram-positive isolates during the period 1999–2003. The most common species tested were Escherichia coli (14.3%), methicillin-susceptible Staphylococcus aureus (13.8%) and coagulase-negative Staphylococci (13.5%), Pseudomonas aeruginosa (12.2%), Enterobacter cloacae (7.2%), Klebsiella pneumoniae (5.7%) and A.baumannii (5.6%). In general, the carbapenems (MEM and IPM) were the most active antimicrobial agents tested against the common organisms (range of %S:100% to 71% and 100% to 67%, respectively). Among Enterobacteriaceae, 100% of Enterobacter spp, Citrobacter spp and Serratia spp were susceptible to carbapenems. E. coli and K. pneumoniae susceptibility to carbapenems were 100% and >98% respectively. The %S of MEM was the same as or higher than IPM against every organism tested. CIP resistance in E. coli was around 20%. CAZ and TAZ were the least active antimicrobial agents against Enterobacter sp (74% and 77% S, respectively) and Citrobacter spp (67% and 68% S, respectively). MEM and TAZ were the most active agents against P. aeruginosa (89% and 88%S, respectively). A. baumannii were 61–90% susceptible to carbapenems, but only 6–1% susceptible to CIP. In this period, around 100% of methicillin-susceptible Staphylococci were susceptible to MEM.
Conclusion: There was no significant decrease in susceptibility to the carbapenems throughout the five-year period. MEM and IMP appear to remain reliable options for the treatment of serious nosocomial infections. The clinical use of MEM did not increase bacterial resistance to this agent in the Spanish centres evaluated.
P1090: Surveillance of antimicrobial susceptibility of anaerobes in a Belgian University hospital
Y. Glupczynski, H. Nizet, C. Berhin (Yvoir, B)
Background: Antimicrobial resistance is becoming a growing concern among anaerobes involved in human infections. Since there are only scarce data on the in vitro susceptibility of anaerobes in our country, we aimed to determine the susceptibility and resistance profiles of anaerobic bacteria isolated in our hospital.
Methods: Minimum inhibitory concentrations (MICs) of 151 consecutive clinically significant isolates of anaerobes recovered from various anatomical sites between 09/2003 and 10/2004 were determined against penicillin (PEN), amoxicillin-clavulanate (AMC), piperacillin-tazobactam (PTZ), imipenem (IMP), meropenem (MER), clindamycin (CLI), metronidazole (MET) and moxifloxacin (MOX) by E-test using NCCLS interpretative guidelines. Referencse strains B.fragilis (ATCC 25285), B. thetaiotaomicron (ATCC 29711) and E. lentum (ATCC 43055) were used as quality control reference strains. The organisms were: B. fragilis group (BFG) (n = 75) including B. fragilis (n = 42), B. theaiotaomicron (9), B. ovatus (5), B. distasonis (5), B. caccae (6), B. vulgatus (n = 7), and B. uniformis (n = 1), Prevotella spp. (n = 27), Clostridium spp. (n = 11), Fusobacterium spp. (n = 9), Peptostreptococcus spp. (n = 18) and other Gram-negative anaerobic species (OGNA) (n = 12). They were isolated from blood (8), sterile body fluids (31), abominal or deep wounds (49) and surgical biopsies (12).
Results: The overall MIC50, MIC90 and % resistance were as follows: PEN: 4/>256, 56%, AMC: 0.125/2, 3%; PTZ: 0.064/16, 3%; MER: 0.06/0.25, 1%, IMP: 0.12/1, 1%; CLI: 0.19/>256, 27%; MTZ: 0.25/1.5, 1%, MOXI: 0.5/8, 3%. Group/species specific resistant rates (%) at breakpoint are listed in the Table.
Conclusion: b-lactams-b-lactamases inhibitors, carbapenems, and MET remain highly active against anaerobes including the more resistant BFG of organism. Resistance in CLI actually almost reaches 30% and is observed among almost all different species of anaerobes. MOX, as a representative of the newer fluoroquinolones exhibits a broad spectrum and potent activity in vitro against all anaerobes tested and looks promising for the treatment of mixed infections involving anaerobes.
| Organisms (n) | PEN | AMC | PTZ | IMP | MER | CLI | MET | MOX |
|---|---|---|---|---|---|---|---|---|
| B. fragilis (42) | 94,3 | 2,8 | 0 | 0 | 0 | 29,4 | 0 | 5,6 |
| Other members of BFG (33) | 97,0 | 6,1 | 6,1 | 2,8 | 2,8 | 37,6 | 0 | 2,8 |
| Prevotella sp. (27) | 59,3 | 0 | 0 | 0 | 0 | 29,6 | 0 | 0 |
| Fusobacterium sp. (9) | 11,1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| OGNA species (12) | 25,0 | 0 | 4,2 | 8,3 | 8,3 | 33,3 | 8,3 | 0 |
| Clostridium sp.(11) | 9,1 | 0 | 0 | 0 | 0 | 36,3 | 0 | 0 |
| Peptostreptococcus sp. (17) | 0 | 0 | 0 | 0 | 0 | 23,5 | 0 | 0 |
Pharmacokinetics/pharmacodynamics of quinolones
P1091: Retrospective analysis of electrocardiogram following oral or intravenous garenoxacin in five phase I studies
Z. Wang, G. Krishna, D. Wexler, D. Grasela (Kenilworth, Princeton, USA)
Objective: Garenoxacin (GRN) is a novel des-F(6)-quinolone effective against a broad spectrum of pathogens, including anaerobes. Some of the fluoroquinolones have the potential to prolong QTc. To determine the effect of GRN on QTc, a retrospective analysis was performed on manually read ECGs from five Phase I studies.
Methods: Serial ECGs were collected in 5 randomized, double-blind, placebo-controlled studies in healthy adult subjects administered oral (PO) or intravenous (IV) GRN 50- to 1200-mg doses (therapeutic dose ≤600 mg) with dosing duration 1 to 28 days (therapeutic duration ≤14 days). The QT interval was corrected for heart rate using Bazett's (QTcB) and Fridericia's (QTcF) formulas, and the effect of GRN was assessed by counts of outliers and linear regressions. Single- and multiple-dose pharmacokinetics of PO and IV GRN were derived from plasma concentration versus time data.
Results: A total of 149 subjects received GRN and 55 received placebo. GRN plasma exposure (AUC and Cmax) increased with increasing dose. No subjects experienced a prolonged QTcB interval (>450 msec for males, >470 msec for females). Only one subject experienced a prolonged (>60 msec) QTcB change from baseline which occurred on day 7, but not on subsequent days despite continued dosing. The incidence of borderline QTcB (change between 30–60 msec) was comparable between placebo and GRN. Means for QTcB Max, QTcB Avg and QTcB at Tmax and their changes from baseline for GRN were similar to those for placebo, with the exception of QTcB Max, QTcB at Tmax, and their changes for 600 mg IV GRN on day 14. Although 1200 mg PO and 800 mg IV GRN produced higher plasma exposures than 600 mg IV on day 14, the means for the derived QTcB values were comparable to placebo. All 95% confidence intervals for the linear regression slopes of derived (delta)QTcB on Cavg(0–12 h) were equal to or less than 0, except for (delta)QTcB at Tmax on day 7, indicating that GRN had no effect on QTcB. Results obtained for QTcF were similar to those for QTcB.
Conclusions: GRN does not appear to have dose-, route of administration- or concentration-dependent effects on QTc interval in healthy subjects.
P1092: Tissue and fluid penetration of garenoxacin
Z. Wang, C. Edmiston, K.V. Rolston, D. Grasela, D. Gajjar (Kenilworth, Milwaukee, Houston, Princeton, USA)
Objective: Garenoxacin (GRN) is a novel des-F(6)-quinolone being developed for a variety of indications because of its
efficacy against a broad spectrum of pathogens, including anaerobes. The objective of this study was to assess the tissue or fluid to plasma ratios of GRN following a single oral dose.
Method: An open-label study was conducted in subjects ≥18 years of age with a body mass index ≤33 kg/m2 undergoing abdominal surgical procedures that would permit the removal of tissue or fluid without increased risk to the subject. A single 600 mg oral dose of GRN was administered based on the scheduled operative time. The tissue or fluid (with corresponding plasma sample) was collected 3 to 5 hours post-dose. Concentrations of GRN in biological fluids and tissues were determined using validated LC/MS/MS assays. Safety was assessed by measurement of vital signs, physical examination, and electrocardiographic and clinical laboratory evaluations. Adverse event (AE) monitoring was performed from time of consent until discharge from the study.
Results: Thirty-one subjects were enrolled in and completed the study. Mean fluid or tissue GRN concentrations greater than that found in plasma (mean fluid or tissue to plasma ratio >1) occurred in large and small bowel tissue, gallbladder, and liver. Mean fluid or tissue GRN concentrations less than that found in plasma occurred in adipose tissue, bone, sinus mucosa, striated muscle, incisional skin, and subcutaneous tissue. Mean GRN concentrations in bile and lymph node tissue were roughly similar to that found in plasma. Tissue and fluid concentrations of GRN exceeded the MIC90 of most target organisms involved in skin and soft tissue, bone, and intra-abdominal infections and sinusitis ≥2-fold. No treatment-emergent AEs or serious AEs were considered to be related to GRN.
Conclusion: A 600 mg oral dose of GRN penetrates well into most of the tissues and fluids studied, with concentrations exceeding the MIC90 of most pathogens causing sinusitis, skin and soft tissue infections, bone infections, and intra-abdominal infections. These results suggest that adequate concentrations of GRN can be achieved to treat infections at these sites.
P1093: Penetration of garenoxacin into lung tissues in patients undergoing lung biopsy or resection
M. Gotfried, K.V. Rolston, Z. Wang, D. Grasela, D. Gajjar (Phoenix, Houston, Kenilworth, Princeton, USA)
Objective: Garenoxacin (GRN) is a novel des-F(6)-quinolone effective against a broad spectrum of pathogens, including those commonly found in the respiratory tract (RT). This study was conducted to determine the penetration of GRN into lung parenchyma (LP) and bronchial mucosa (BM) following a single 600 mg oral dose. Penetration of GRN into bone was also assessed.
Methods: This was an open-label, nonrandomized study in subjects undergoing an invasive procedure to the lung (other than percutaneous lung biopsy) which facilitated the removal of macroscopically normal healthy lung tissue without exposing the subject to undue risk. Penetrance of GRN into bone was determined when removal of rib bone was part of the normal surgical procedure. A single 600 mg oral GRN dose was administered based on the scheduled operative time. LP and, if possible, BM and/or bone samples and corresponding plasma samples were removed at 2 to 4, 4 to 6, 10 to 12, or 20 to 24 h post-dose. Concentrations of GRN in these samples were determined using validated LC/MS/MS assays. Safety was assessed based on the occurrence of adverse events (AEs) and changes in physical examinations, vital signs, clinical laboratory results, and electrocardiographic results.
Results: Twenty-seven subjects were enrolled; samples were taken from a minimum of 6 patients at each time interval. Mean GRN concentration in LP increased between the 2–4 and 4–6 h post-dose, suggesting rapid penetration into LP, then declined similar to the decrease seen in plasma concentration. Concentrations of GRN in LP exceeded the MIC90 of organisms associated with RT infections by 62- to 466-fold over a 24 h period. GRN concentrations in BM over a 24 h period exceeded the MIC90 of respiratory pathogens 51- to 380-fold. Concentrations of GRN in bone exceeded the MIC90 of the organisms associated with bone infections (except Pseudomonas aeruginosa, MRSA, Fusobacterium species, and Enterobacter species) by 6- to 101-fold over a 12 h period. Across the 4 time intervals, mean ratios of tissue to plasma GRN concentration in LP, BM, and bone reached 2.80, 0.99, and 0.56, respectively, suggesting adequate penetration. No GRN-related AEs were reported, indicating that a single 600 mg oral GRN dose was well tolerated in subjects undergoing invasive procedures.
Conclusions: GRN penetrates rapidly into LP, BM, and bone tissue, producing sustained concentrations that predict adequate coverage of GRN-susceptible pathogens at these sites.
P1094: Bioavailability and safety in healthy volunteers unaltered when crushed garenoxacin tablets are administered via a nasogastric tube with or without enteral feeding
R. Noveck, R. Vargas, G. Krishna, D. Grasela (New Orleans, Kenilworth, Princeton, USA)
Objective: The purpose of this trial was to assess, in healthy volunteers, the bioavailability and safety of single doses of the novel des-F(6)-quinolone garenoxacin (GRN) administered as crushed tablets with and without concomitant enteral feeding compared with intact tablets.
Methods: In this randomized, crossover, single-dose study, healthy adult volunteers (aged 18 to 45 y) received GRN 600 mg (one 200 mg and one 400 mg tablet) orally in 3 regimens: A) intact tablets; B) crushed tablets suspended in water and delivered via nasogastric (NG) tube; C) regimen B plus concomitant enteral feeding (Osmolite, 600 mL at 100 mL/hr). Subjects were randomized to receive all 3 regimens in 1 of 6 crossover sequences (ABC, ACB, BAC, BCA, CAB, CBA) separated by 7-day washout intervals. For each treatment, subjects entered the facility 1 day before and were confined for 72 hours after drug administration. Subjects were discharged from the study after final assessments on day 4 of the third treatment. Post-screening assessments included vital signs; plasma drug levels for PK analysis; and physical, laboratory, and ECG examinations for drug safety.
Results: 18 male subjects were enrolled (4 white, 14 black; mean age, 30 y). PK analysis for GRN administered as crushed tablets with and without concomitant enteral feeding vs intact tablets showed no differences in the adjusted geometric means for Cmax (8.5 and 8.3 μg/mL vs 8.3 μg/mL) or AUC(INF) (97.2 and 93.4 μg*hr/mL vs 103.3 μg*hr/mL). The 90% CI for log-transformed Cmax and AUC(INF) for B and C compared to A were contained within the protocol-specified ‘no effects’ limit of 70% to 143%. Mean GRN half-life was similar among the 3 groups (mean range of 12–13 h). Tmax was 1 hour following administration of intact tablets compared with 0.5 hour in the other 2 groups. A single oral 600 mg dose of GRN was well tolerated whether administered as crushed tablets suspended in water and delivered via NG tube with or without enteral feeding, or as intact tablets. Three adverse events (AEs) were reported; 1 (nausea) was deemed probably related to study drug. There were no serious AEs, meaningful changes on safety examinations, or discontinuations due to AEs.
Conclusions: The bioavailability of GRN was similar for crushed versus intact tablets, regardless of whether an enteral feeding was given with crushed tablets. These results show that GRN may be administered as crushed tablets with or without concomitant feeding.
P1095: Garenoxacin pharmacokinetics in subjects with severe renal impairment
G. Krishna, T. Marbury, S. Swan, D. Wexler, D. Grasela (Kenilworth, Orlando, Minneapolis, Princeton, USA)
Objective: Garenoxacin (GRN) is a novel des-F(6)-quinolone effective against a broad spectrum of pathogens. The absolute bioavailability of GRN after oral intake is 92% and approximately 40% of GRN is excreted unchanged in the urine. The objective of this study was to evaluate the pharmacokinetics of GRN in subjects with severe renal impairment.
Methods: This non-randomized, open-label study enrolled patients into 1 of 4 groups: healthy control subjects (HC) with normal renal function (CLcr > 80 mL/min); subjects with severe renal impairment (SRI) (CLcr < 30 mL/min) not requiring dialysis; subjects with SRI receiving hemodialysis (HD); and subjects with SRI receiving continuous ambulatory peritoneal dialysis (CAPD). A single 600 mg oral dose of GRN was administered on day 1 for all groups except HD patients. HD patients received a single 600 mg oral GRN dose both before (HD1) and after (HD2) HD, with dosings separated by a 14-day washout. Blood, urine, and dialysate samples were collected up to 144 h post-dose and concentrations of GRN were determined using validated LC/MS/MS assays. Safety was assessed by physical examination, vital signs, and electrocardiographic and laboratory evaluations.
Results: Twenty-five subjects received GRN (HC, n = 6; SRI, n = 6; HD1, n = 7; CAPD, n = 6). Six subjects in HD2 received GRN. Mean GRN exposure [AUC(I)] was similar in HC and HD1 but was 51%, 15%, and 21% higher in SRI, HD2 and CAPD, respectively, than in HC. However, many of the individual values were within the range observed for HC, and these average increases in AUC(I) did not exceed values previously shown to be well tolerated. Decreases in Cmax were observed in SRI, HD1, CAPD, and HD2, but were not considered clinically relevant. Approximately 11%, 1.5%, and 3% of GRN dose was removed in the dialysate for HD1, HD2, and CAPD, respectively. A total of 34 treatment-emergent adverse events (AEs) were reported, all mild or moderate in severity; 5 were considered to be probably or possibly related to GRN. One treatment-emergent but not treatment-related serious AE was reported.
Conclusions: A single dose of 600 mg GRN was well tolerated in patients with SRI, including those requiring HD and CAPD.
There was no clinically significant increase of GRN exposure in patients with SRI based on the broad therapeutic index of GRN. Therefore, no GRN dosage adjustment is recommended in subjects with SRI.
P1096: The effect of omeprazole on the bioavailability and safety of garenoxacin in healthy volunteers
J. Kisicki, G. Krishna, S. Olsen, D. Grasela (Lincoln, Kenilworth, Princeton, USA)
Objective: The novel des-F(6)-quinolone garenoxacin (GRN) is more soluble in acidic conditions than at neutral pH. Therefore, this study was designed to determine if omeprazole affects the bioavailability of GRN.
Methods: This non-randomized, open-label pharmacokinetic study was conducted in healthy adult subjects. On day 1, the single-dose pharmacokinetics of 600 mg of oral GRN (one 200 and one 400 mg tablet) were determined in fasting subjects, with serial blood samples obtained through 72 hours post-dose. Omeprazole 40 mg was administered once daily on days 4 to 7 to achieve steady-state inhibition of gastric acid secretion. On day 8, single doses of GRN and omeprazole were administered concomitantly. Omeprazole treatment was continued on days 9 and 10 throughout the period of pharmacokinetic blood sampling. Study assessments included vital signs and physical, laboratory, and electrocardiographic examinations for safety.
Results: Fourteen subjects (8 male; mean age, 25 years) were enrolled and 12 completed the study. Concomitant administration of omeprazole did not affect the AUC (INF) or Cmax of GRN. The geometric mean (GM) for GRN AUC(INF) was 132.0 mcg.h/mL, compared with 140.4 mcg.h/mL for concomitant GRN and omeprazole [90% confidence interval (CI) 101–111%]. The GM Cmax value for GRN and GRN/omeprazole co-administration was 9.6 and 9.3 mcg/mL, respectively, with 90% CI of 90% to 104%. Half-life (mean range 12.9 to 14 h) and Tmax (median range 1.5 to 1.8 h) were similar after administration of GRN either alone or concomitantly with omeprazole. Concomitant administration of garenoxacin and omeprazole was well tolerated. Nine of 14 subjects (64%) experienced a total of 33 adverse events (AEs). The majority of AEs were mild, and only 12 were deemed possibly or probably related to the study drug. The most frequently cited AEs, headache, nausea and abdominal pain, were mild to moderate in severity. Two subjects withdrew from the study; neither discontinuation was due to AEs.
Conclusions: The concomitant administration of omeprazole had no effect on garenoxacin bioavailability. These findings indicate that garenoxacin can be administered with omeprazole or other agents that affect gastric pH to a similar or lesser extent.
P1097: The effect of Maalox on bioavailability and safety of garenoxacin in healthy volunteers
J. Kisicki, G. Krishna, S. Olsen, D. Grasela (Lincoln, Kenilworth, Princeton, USA)
Objective: Garenoxacin (GRN) is a novel broad-spectrum des-F(6)-quinolone antibiotic. Quinolones are known to chelate with cations such as aluminum, impairing antibiotic absorption. This study was therefore designed to assess the effect of a 20-mL dose of Maalox® (containing 900 mg aluminum hydroxide and 800 mg magnesium hydroxide) on the pharmacokinetics of GRN when administered concomitantly with, 2 and 4 hours before, and 2 and 4 hours after, Maalox.
Methods: This was a randomized, open-label, 6-treatment, control-balanced, residual effects design pharmacokinetic study. The 6 oral treatments consisted of 600 mg GRN (one 200 and one 400 mg GRN tablet) given alone, with concomitant Maalox, 2 h before Maalox, 4 h before Maalox, 2 h after Maalox, and 4 h after Maalox. Each healthy adult subject received 3 of the above treatments, with a 7-day washout period between treatments. In each treatment, serial blood samples for pharmacokinetic analysis were collected before and up to 72 h after GRN dosing. Study assessments included vital signs and physical, laboratory, and electrocardiographic examinations for drug safety.
Results: Twenty subjects (12 male, 8 females; mean age, 27 years) were enrolled. Exposure to GRN [AUC(INF)] was reduced by 58% when coadministered with Maalox. Exposure to GRN was also reduced when administered 2 or 4 hours after Maalox, by 22% and 16%, respectively. In contrast, when administered 4 hours before Maalox, GRN exposure was not affected. When GRN was administered 2 hours before Maalox, a small reduction (12%) in GRN exposure was observed that is unlikely to be clinically relevant. Half-life (mean range 11.5 to 14.2 hours) and Tmax (median range 1.5 to 2 hours) were similar across treatment groups. A single oral 600 mg dose of GRN was well tolerated. Mild adverse events were reported by 2 subjects; 1 subject discontinued due to mild abdominal pain and blood in the stool.
Conclusions: Maalox does not affect GRN bioavailability when GRN is administered at least 2 h prior to Maalox. However, a reduction in GRN exposure is observed when GRN is administered concomitantly or up to 4 h after Maalox. Therefore, GRN can be administered 2 h before or 4 h after administration of Maalox or other products containing a high content of cations, particularly aluminum.
P1098: Mutant prevention concentrations of fluoroquinolones authorised for use in poultry against Salmonella enterica serovar Typhimurium DT 104
L.P. Randall, S.W. Cooles, K. Stapleton, N.G. Coldham, L.J.V. Piddock, M.J. Woodward (New Haw, Birmingham, UK)
Objectives: It has been demonstrated that fluoroquinolone treatment of humans and animals can rapidly select for bacteria with reduced susceptibility to fluoroquinolone antibiotics. In recent years, there has been considerably interest in the concept of the mutant prevention concentration (MPC). The MPC has been defined as that concentration of antibiotic at which no mutants are selected from 10,000,000,000 organisms. In previous studies MPCs of ciprofloxacin and enrofloxacin were determined in vitro against Salmonella enterica serovar Typhimurium DT 104. Here the use of a chick model to investigate the MPC of enrofloxacin in vivo is reported.
Methods: Chicks were experimentally infected with S. Typhimurium and treated with Baytril (enrofloxacin) at 50 ppm/10 mg/kg for 5 days (recommended therapeutic dose) or 2 days or 125 ppm/25 mg/kg for 2 days or 250 ppm/50 mg/kg for 1 day. Chicks received the dose in the drinking water (ppm) or by oral gavage (mg/kg). During and 24 hours after dosing, birds were killed and tissue samples (caecal contents, liver and sera) were taken and the levels of enrofloxacin and ciprofloxacin were determined in these tissues by HPLC or bio-assay. Caecal contents were also monitored for the presence of Salmonella during dosing and for up to 4 weeks after dosing. Selection of resistance was monitored by replica plating of colonies to media containing 4x the ciprofloxacin and nalidixic acid MIC of the strain before treatment. Results: The only conditions where the antibiotic treatments did not select for reduced susceptibility (e.g. 4x MIC of parent strains) were in birds that received the antibiotic at 2.5x the dose for 2 days by oral gavage or 4x the dose for 1 day in the water. This oral gavage treatment also significantly reduced the counts of Salmonella compared to all other oral gavage treatments. For the oral gavage study, concentrations of fluoroquinolones in caecal contents were above the MPC for at least 6 hours after dosing for all treatment regimes.
Conclusion: It was of interest to note that whilst the fluoroquinlone antibiotics are regarded as concentration rather time dependent antibiotics, the 2 day at 2.5x the dose was more effective at reducing the counts of Salmonella in both experiments than the 1 day at 5x the dose. These results would suggest that length of treatment as well as dose and route of administration, is critical in minimising the selection of fluoroquinolone resistance in vivo.
P1099: Effect of levofloxacin coadministration on the international normalised ratios during acenocumarol therapy
J. de Otero, M. Payeras, C. Carratala, A. Artigues, M. Sanz, P. Nadal (Manacor, E)
Levofloxacin (L) showed no effect on warfarin pharmacokinetics in healthy volunteers but several recent descriptions reveal elevated international normalised ratios (INR) in patients receiving concurrent L and warfarin. To our knowledge no cases of L-acenocumarol (A) interaction have been reported.
Objectives: To report 6 cases of hypoprothrombotic response resulting from addition of L therapy to chronic A therapy.
Methods: A 9-month retrospective analysis of adult patients receiving A who were admitted to our ward under L prescription on the basis of clinical diagnosis and judgement. Descriptive statistical measurements were performed.
Results: Six patients, 74–89 years old (median 81.5), were included. Four were men (66.6%). They suffered from a median of 4 (range 2–6) concurrent chronic medical problems (including coronary heart disease, atrial fibrillation, hypertension, obstructive pulmonary disease, renal insufficiency, cardiomyopathy and heart failure) and took a median of 7 (range 4–10) different kind of drugs (including digoxin, furosemide, antihypertensives and inhaled bronchodilators). Types of infection for which the patients were treated with L included acute bronchitis (4 cases) and pneumonia (2 cases). Three patients had an INR range of 2.0–3.0 and experienced an increase in INR to 5.36, 14.51 and 5.76 on L-treatment days 8, 5 and 2. Two patients had a low INR (1.84 and 1.86) and experienced an increase to 4.25 and 2.77, on days 5 and 2, despite no changes in A dosage were performed. The sixth patients had a high INR (4.03) at the time of admission and, in spite of stopping A administration, INR increased to 4.66. Two patients experienced minor bleeding but only one required L stopping. Patient with the highest INR presented L-related diarrhoea, and it was prescribed L discontinuation and vitamin K. A median of 4 days (1–6) were required to completely control INR in a therapeutic range of all patients.
Conclusion: We provide some evidence of an increase in INR observed during concomitant L and A treatment. Further studies are required to better determine that possible effect. Due to the demonstrated clinical efficacy of L in many infections we must recommend its use. But, to our opinion, until the clinical significance of an interaction between these two drugs is well defined, a patient's INR values during A therapy should be closely monitored, during, and after L coadministration.
P1100: Ciprofloxacin accumulation and intracellular activity against L. monocytogenes are reduced in ciprofloxacin-resistant macrophages due to increased efflux
M. Heremans, M.P. Mingeot-Leclercq, P.M. Tulkens, F. Van Bambeke (Brussels, B)
Objectives: CIP is substrate for an MRP efflux pump in J774 mouse macrophages (Michot et al, AAC 48:2673–82), which reduces its cellular accumulation. We have recently shown that CIP-'resistant’ macrophages can be selected upon chronical exposure of these cells to CIP, in which CIP accumulation becomes negligible because of an increased activity and/or expression of the efflux transporter (ICAAC 2004, abstract A-1304). We have now examined whether this reduced accumulation affects CIP intracellular activity using a model of intracellular infection by L. monocytogenes (L.m.) and comparing resistant cells to the wild type parent cell line.
Methods: Infection was carried out using a bacteria: macrophage ratio of 7:1, according to the procedure described in Seral et al (JAC 51:1167–73). CFU/mg cell protein was determined after 5 h exposure to increasing concentrations of CIP ± 10 mM probenecid (inhibitor of MRP transporters). CIP cellular concentration was measured by fluorimetry (AAC 48:2673–82).
Results: In wild cells, an extracellular concentration corresponding to 3 X the MIC was sufficient to obtain a static effect, and this value rose to 30 X in CIP-resistant cells. This value was decreased to 1 X and 1.5 X the MIC, for wild and CIP-resistant cells respectively, in the presence of probenecid. In cells incubated with 20 mg/l CIP (10 X MIC), CIP accumulation was 4.8 ± 0.3 and 0.3 ± 0.1 in wild and CIP resistant cells, but increased to 21.3 ± 0.8 and 10.6 ± 0.5 in the presence of probenecid.
Conclusions: Increase in expression and/or activity of the CIP efflux transporter causes a reduction of the antibiotic efficacy against intracellular infection, which can be reversed upon inhibition of the efflux transporter.
P1101: Quinolone-induced changes in tenocytes are intensified by dexamethasone in vitro
J. Sendzik, M. Shakibaei, M. Schäfer-Korting, R. Stahlmann (Berlin, D)
Objectives: Quinolones can cause tendinitis and tendon ruptures. Retrospective studies and case reports reveal that an additional therapy with glucocorticoids increases the risk of quinolone-induced tendon disorders.
Methods: We investigated possible combination effects of quinolones and glucocorticoids in an in vitro model with human tendon cells. Tenocytes were cultured for 1, 2, 3 and 4 days as monolayers and incubated with (a) ciprofloxacin or levofloxacin (3 mg/l), (b) 0.1 nM dexamethasone, and (c) ciprofloxacin or levofloxacin (3 mg/l) plus 0.1 nM dexamethasone. Immunoblotting was used to quantify changes in the amount of beta1-integrin, activated src homology collagen (shc) and of activated caspase-3 (casp-3). Furthermore, ultrastructural alterations were analysed by electron microscopy.
Results: At 3 mg/l, ciprofloxacin caused a significant decrease of the amount of beta1-integrin from day 3 onwards, while no effect was seen with 3 mg levofloxacin/l medium or 0.1 nM dexamethasone compared to the untreated control. The combination of both quinolones (3 mg/l) with 0.1 nM dexamethasone resulted in an earlier onset of the beta1-integrin reduction: for ciprofloxacin + dexamethasone from the first day of incubation, for levofloxacin + dexamethasone from day 3 onwards. Quinolone-induced changes in signalling proteins, such as activated shc, are not fortified by dexamethasone at the concentration tested. Interestingly, the time and concentration dependent increase of the apoptosis marker activated casp-3 was intensified with dexamethasone. The results of immunoblotting with respect to the induction of apoptosis were confirmed by electron microscopy.
Conclusions: Our results show that quinolone-induced changes in the amount of the beta1-integrin as well as of the apoptosis marker activated casp-3 are enhanced by dexamethasone in vitro. The addition of the glucocorticoid caused an earlier onset of the quinolone-induced changes. Our results support the clinical observations that glucocorticoids are an additional risk factor for quinolone-induced tendopathies.
P1102: Pharmacokinetics and pharmacodynamics of a novel extended release formulation of ciprofloxacin as compared to levofloxacin against extended spectrum beta-lactamase producing Enterobacteriaceae
S. Schubert, H. Stass, U. Ullmann, A. Dalhoff (Kiel, Wuppertal, D)
Background: An extended release formulation of ciprofloxacin (CIP XR, 1000 mg qd, p.o.) has been developed, delivering peak concentrations which are 40% to 50% higher than following the administration of the conventional formulation (CIP IR, 500 mg bid, p.o.) while the areas under the curve (AUC) were comparable.
Objectives: First, CIP is used for the treatment of infections due to Enterobacteriaceae, frequently being ESBL producers. Thus, the PK/PD characteristics of CIP XR vs. IR against ESBL strains was examined. Second, CIP is used in urinary tract infections (UTIs). Thus, the PK/PD profiles of CIP XR vs. IR in serum and urine were studied. Third, the PK/PD characteristics in either BHI or artificial urine were compared.
Methods: Genotypically characterised ESBL producing E. coli (Ec) and K. pneumoniae (Kpn) and their wild type counterparts were exposed to the geometric mean plasma and urine concentration profiles following CIP 1000 mg XR qd, 500 mg IR bid and LEV (500 mg qd). The CIP and LEV urine concentrations were fitted from Phase I study data by compartmental modeling using TopFit 2.0. Bacteria were cultivated in a modified Grasso model at 37°C in brain-heart infusion broth as well as artificial urine acc. to Griffith et al.; viable counts were quantitated at 0.5, 1, 1.5, 2, 3, 4, 6, 8 and 24 h. The areas under the bacterial kill curves normalised to the inoculum were calculated.
Results: First, irrespective of the PK profiles simulated, the WT were eliminated rapidly. The ESBL producing Ec and Kpn were moderately to negligibly affected upon simulation of serum PK profiles of both CIP and LEV. Second, simulation of urine concentrations by using artificial urine IR and XR resulted in an elimination of the ESBL producers from the test system. LEV eliminated the ESBL producing K. pneumoniae but not the E.coli strain, which regrew. CIP XR killed the ESBL Kpn strain more rapidly than CIP IR or LEV. Third, PK/PD surrogates derived from studies in conventional media or artificial urine are significantly different.
Conclusions: This model and the use of artificial urine predicts a more rapid and pronounced effect of CIP XR as compared to CIP IR or LEV.
P1103: Moxifloxacin concentrations in plasma and tonsillar tissue in adult patients
S. Esposito, S. Noviello, G. D'Errico, G. Motta, D. Passali, C. Aimoni, S. Pilucchi, S. Fallani, M. Cassetta, T. Mazzei, A. Novelli (Naples, Siena, Ferrara, Florence, I)
Objectives: The antibacterial spectrum of moxifloxacin includes all the major respiratory pathogens and its pharmacokinetics demonstrates high peak concentrations in plasma as well as at respiratory sites. Nevertheless, the tonsillar tissue concentrations have never been investigated. In the present study we determined the moxifloxacin concentrations in plasma and tonsils after the administration of three doses of 400 mg to adult patients with chronic or recurrent tonsillitis undergoing tonsillectomy.
Methods: This was an uncontrolled, open-label, randomised, parallel group study including 35 patients randomly assigned to 5 groups of 7 patients each, depending on the time between the last dose of moxifloxacin and that of plasma and tissue sampling (2, 3, 6, 12 and 24 h). Moxifloxacin was given orally od for 3 days. Moxifloxacin concentrations were measured by a validated HPLC assay and fluorescence detection. Each sample was analysed twice and the mean value obtained used for statistical analysis. Pharmacokinetic data were analysed by presenting descriptive statistics of moxifloxacin levels in plasma and tonsillar tissue.
Results: Cmax occurred at 3h in plasma (mean value 3.20 mg/ L) and in tonsillar tissue (mean 8.96 mg/L). Tonsillar tissue/ plasma ratios (mean values) were constantly >2 mg/L at any collecting time, ranging between 2.37 mg/L (after 2 h) and 2.93 mg/L (after 24 h), which indicates a prolonged maintenance of moxifloxacin level in tonsillar tissue compared to plasma. Variability among pts was present at 6 h, the tonsillar tissue/plasma ratio ranging between 0.8 and 3.4 mg/L.
Conclusions: Moxifloxacin achieves a good penetration in tonsillar tissue, which favourably compares with that reported for other fluoroquinolones. The moxifloxacin concentrations that we observed exceed the MICs of the usual respiratory tract pathogens.
P1104: Penetration kinetics of moxifloxacin in human pancreas: comparison of intravenous vs oral administration
R. Wacke, S. Förster, S. Park, R.G. Mundkowski, U. Adam, W. Schareck, E. Klar, B. Drewelow (Rostock, Freiburg, D)
Objectives: Acute necrotizing pancreatitis is still related to a high mortality rate, based on local infectious complications, particularly due to bacterial infections of the necrotic pancreatic and parapancreatic areas. Limited penetration of antimicrobial drugs in these areas/compartments is considered to be a major cause of failure of therapy of severe local pancreatic infections. However, fluoroquinolones (e.g. ciprofloxacin, levofloxacin) have been shown to penetrate sufficiently into pancreatic tissue. On that score, the value of new quinolones such as moxifloxacin (MXF) has not been investigated yet. Using a rat model of acute necrotizing pancreatitis MXF has been demonstrated to penetrate rapidly and efficiently into pancreatic tissue, also into the inflamed and necrotic pancreas.
Methods: Addressing the penetration capability of MXF following intravenous (IV) or oral (PO) administration with respect to the human pancreas, a prospective clinical trial was designed using a single IV (20 patients) or PO dose (40 patients) of 400 mg MXF for antimicrobial prophylaxis in patients undergoing pancreas resection. Samples were taken from blood and from resection area of pancreatic tissue at two time points after application (1st sample at the beginning, 2nd sample at the end of resection). Concentrations of MXF were determined by HPLC/UV using ofloxacin as internal standard.
Results: Mean plasma concentrations of MXF IV and PO at first sampling time (3 - 3.7 h) were 1.8 ± 0.5 and 1.2 ± 0.6 μg/ml, respectively. At the end of resection (4.3–5.3 h) 1.5 ± 0.4 and 1.0 ± 0.5 μg/ml were measured. Corresponding mean concentrations of MXF in pancreatic tissue were 2 to 3times higher (3.1 ± 0.9 and 2.7 ± 1.4 μg/g 1st sample; 3.6 ± 1.5 and 3.1 ± 1.8 μg/g 2nd sample). The MXF concentrations in pancreatic tissue exceeded the MIC90 s of the relevant pathogens encompassed by MXF (e.g. E. coli 0.008–0.06 μg/ml, Klebsiella spp. 0.13 μg/ml, and S. aureus 0.06– 0.12 μg/ml) for at least five hours at the dosing interval.
Conclusion: MXF has been demonstrated to penetrate efficiently into human pancreatic tissue following IV as well as PO administration. In this study MXF concentrations after PO administration were found to be slightly lower than those observed in healthy subjects probably due to diminished or delayed intestinal absorption prior and during surgery.
P1105: Effects of enteral feeding on the oral bioavailability of moxifloxacin
O. Burkhardt, H. Stass, U. Thuss, K. Borner, T. Welte (Magdeburg, Wuppertal, Berlin, D)
Objective: In clinical practice on ICU wards moxifloxacin (MFX) may be occasionally administered through a nasogastric (NG) feeding tube. In absence of an oral liquid formulation and since the divalent cations contained in enteral feeds may potentially impair absorption of MFX given via this way, we wanted to study the effect of concomitant enteral feeding on the pharmacokinetics and tolerability of MFX passed as a crushed tablet through a NG tube, firstly in healthy volunteers.
Methods: In a randomized 3-way crossover study the oral bioavailability of MFX was investigated in 12 healthy volunteers (9 f, 3 m). Each subject received separately an intact 400 mg MFX tablet (A), a crushed tablet as a suspension through an NG tube with water (B), and while receiving enteral feeding (C). The concentrations of MFX in serum were measured by a validated HPLC. AUC and Cmax were analysed statistically assuming log normally distributed data using ANOVA.
Results: All MFX treatments were well tolerated. The AUC was slightly, but not significantly decreased in treatments B and C [geo means (A) 39.6 vs. (B) 36.1 vs.(C) 36.1 mg*h/L; point estimates (PE) 91% for B/A and C/A and 90% confidence interval (CI) 86 to 97% for B/A and C/A] indicating equivalence of the treatments. Likewise the maximum serum concentrations after MFX administration through NG tube with water (B) and with tube feed (C) were slightly decreased [Cmax; geo means
(A) 3.20 versus (B) 3.05 and (C) 2.83 mg/L; PE 95%, CI 88 to 103% for B/A and PE 88%, CI 82 to 95% for C/A]. They were within the range seen in other studies with oral administration of the drug. No statistically significant differences were observed in time to reach Cmax [Tmax; median (A) 1.75 h versus (B) 1.00 h and (C) 1.75 h]. Thus, rate of absorption was not affected by NG tube administration. This route of ingestion seems to be associated only with a slight loss of bioavailability - independent of the carrier medium used (water vs. enteral feed). No clinically relevant interaction with the multivalent cations contained in the enteral feed was observed indicating that MFX and enteral nutrition can be administered concomitantly.
Conclusion: There was no clinically relevant effect of enteral feeding on the pharmacokinetics of oral MFX in healthy volunteers. This results has to be evaluated in patients, especially those from ICU, who are characterised by severe infectious and/or concomitant diseases, which might influence absorption of MFX.
Pharmacokinetics/pharmacodynamics of antifungals
P1106: Comparison of posaconazole adverse event profiles in healthy volunteers and in patients with invasive fungal infections
L. Pedicone, A. Ullmann, J. Graybill, A. Sansone, R. Courtney, M. Laughlin, I. Raad (Kenilworth, USA; Mainz, D; San Antonio, Houston, USA)
Objectives: To better define the adverse event (AE) profile of posaconazole (POS), we compared the safety profiles of patients with invasive fungal infections (IFIs) enrolled in POS clinical trials with those of healthy volunteers enrolled in clinical pharmacology studies.
Methods: AE analyses from 428 patients with IFIs from 2 open-label clinical trials and from 449 healthy volunteers from 18 clinical pharmacology trials were compared. In the healthy volunteer studies, compliance with dosing regimens was strictly enforced and participants had no significant underlying diseases or concomitant medications that could confound interpretation of safety data. Therefore, for the purpose of this analysis, the healthy volunteers served as a control group for the patient population. In both groups, most subjects received POS 800 mg/d in divided doses.
Results: Treatment-related AEs (TRAEs) occurred in 44% (196/ 449) of healthy volunteers; the most common were headache (17%), dry mouth (9%), and dizziness (6%). In patients, many AEs were consistent with underlying diseases. TRAEs occurred in 38% of patients (164/428); the most common were nausea (8%), vomiting (6%), headache (5%), abdominal pain (4%), and diarrhoea (4%). Notably, gastrointestinal (GI) TRAEs occurred in 18% of healthy volunteers and 19% of patients. Treatment-related abnormal liver function test results were observed in 2% of healthy volunteers and up to 3% of patients. There were no clinically significant differences in mean QTc interval change from baseline in either population. Serious AEs (SAE) considered possibly or probably related to POS occurred in 35 (8%) patients and 1 healthy volunteer. The most common SAEs in patients were altered drug level, increased hepatic enzymes, nausea, rash, and vomiting (1% each). No significant trends related to age, sex, or race were observed in either group. Additionally, no unique TRAEs were identified in patients during long-term exposure (>6 months) compared with those identified during shorter-duration therapy.
Conclusion: The safety profile of POS in patients was similar to that observed in a controlled population of healthy volunteers and is likely indicative of what will be observed in the clinical setting. Headache and GI events (nausea, vomiting, abdominal pain, diarrhoea) were the most common TRAEs observed in patients. Given its favorable safety profile, POS should provide an additional treatment option for severely ill patients with IFIs.
P1107: Evaluation of the drug interaction potential of posaconazole: summary of 7 clinical pharmacology studies
A. Sansone, R. Courtney, G. Krishna, D. Wexler, M. Martinho, M. Laughlin (Kenilworth, New Jersey, USA)
Objective: We evaluated the drug interaction (DI) potential of posaconazole (POS), an extended-spectrum triazole antifungal agent, in 7 phase 1 studies. POS is an inhibitor of cytochrome P450 (CYP) 3A4 activity, but it does not affect the activity of other CYP enzymes. These studies were conducted to evaluate potential changes in the pharmacokinetics of POS and the coadministered medication, when given in combination.
Methods: Seven open-label DI studies were conducted in which subjects received POS (200-800 mg) for 8 to 14 consecutive days, alone or in combination with single or multiple doses of cimetidine, cyclosporine, glipizide, phenytoin, rifabutin, tacrolimus, or antiretroviral medications (zidovudine, lamivudine, ritonavir, and indinavir). In the cyclosporine and antiretroviral studies, patients received established doses (ED) of these drugs, and plasma concentrations were presumed to be at steady state (SS) before POS administration. Bioavailability, based on log-transformed AUC values, was expressed as the ratio of the combination treatment to POS or concomitant drug given alone.
Results: The effects of coadministration on the AUC values of POS and each concomitant medication are summarized in the table.
| Bioavailability (AUC %) |
||||||
|---|---|---|---|---|---|---|
| Study | N | Drug (mg) | Duration (d) | POS (mg) | POS | Concomitant Drug |
| 1 | 12 | Cimetidine (800) | 10 | 200 qd | 61 | ND |
| 2 | 4 | Cyclosporine (ED) | SS | 200 qd | ND | Doses reduced −14-29% in 3 of 4 |
| 3 | 12 | Glipizide(10) | 1 | 400 bid | 91 | 118 |
| 4 | 36 | Phenytoin (200) | 10 | 200 qd | 50 | 115 |
| 5 | 24 | Rifabutin (300) | 17 | 200 qd | 51 | 172 |
| 6 | 34 | Tacrolimus (0.05a) | 1 | 400 bid | ND | 458 |
| 7 | 17 | Zidovudine (600) | SS | 200 qd | ND | 112 |
| 17 | Lamivudine (300) | SS | 200 qd | ND | 107 | |
| 17 | Ritonavir (1200) | SS | 200 qd | ND | 130 | |
| 17 | Indinavir (3200) | SS | 200 qd | ND | 116 | |
ND = not determined.
mg/kg;
Conclusion: No dose adjustments are required for glipizide, zidovudine, lamivudine, indinavir, or ritonavir when coadministered with POS, as the small differences in exposure are not considered clinically significant. However, when POS was given with glipizide, glucose concentrations decreased in some healthy volunteers more so than after glipizide administered alone. Monitoring of cyclosporine and tacrolimus blood levels is warranted with POS coadministration, and dose adjustments of cyclosporine and tacrolimus should be made accordingly. Concomitant use of POS with rifabutin, phenytoin, or cimetidine should be avoided unless the benefits outweigh the risks, due to the decrease in POS concentrations.
P1108: Posaconazole pharmacokinetics in elderly healthy volunteers and elderly patients
A. Sansone, R. Courtney, G. Krishna, D. Wexler, M. Martinho, L. Pedicone (Kenilworth, USA)
Objectives: The pharmacokinetics (PK) of many medications may be altered in the elderly population. Because alterations in PK can potentially affect clinical outcomes, the PK parameters of Posaconazole (POS), an extended-spectrum investigational triazole antifungal agent, were examined in healthy elderly persons (>65 years), and the clinical implications of age-related PK differences were evaluated.
Methods: We conducted a meta-analysis of POS steady-state PK data from 5 clinical studies in healthy volunteers. PK data from elderly healthy volunteers were compared with those of elderly patients with invasive fungal infections (IFIs) who participated in an open-label trial that evaluated POS efficacy and safety. Study participants received POS oral suspension 800 mg/day in divided doses. Because POS plasma concentrations at steady state are relatively constant, AUC values in healthy subjects could be directly compared with the average steady-state plasma concentration in patients.
Results: Out of a total of 174 healthy volunteers in the meta-analysis, 24 (14%) were ≥ 65 years. POS exposure was approximately 24% higher in elderly than that in adult (18-64 years) subjects. Mean AUC values for adult (n = 150) and elderly subjects were 28.495 and 35.444 ng·h/mL, respectively. These observations were consistent with PK data from elderly patients with IFIs. The IFI study included 330 patients; 33 (10%) were elderly, of whom 25 were included in the PK analysis. The average concentration values were 1056 ng/mL and 817 ng/mL in elderly patients and patients 18 to 64 years, respectively. Although POS exposure was approximately 29% higher in elderly than that in the adult patients <65 years, treatment-related adverse event (TRAE) occurrence rates were similar in elderly patients (48%) and the overall population (42%). The most common TRAEs were similar in both populations: nausea (15% vs 9%), vomiting (9% vs 6%), and headache (9% vs 5%). Efficacy was evaluated in 31 elderly patients, and 27 (74%) had successful outcomes.
Conclusion: POS exposure is slightly higher in the elderly healthy volunteers and patients compared to those <65 years old, but the difference in exposure is not clinically relevant. Safety profiles between elderly and younger patients were similar, and POS was well tolerated in both populations. POS may be useful against IFIs in elderly patients because of its favorable safety profile and demonstrated clinical activity against IFIs.
P1109: The long-term visual safety of voriconazole
K. Tomaszewski, A. Laties, J.M. Goodrich (Sandwich, UK; Pennsylvania, New London, USA)
Objectives: Long Term Visual Safety of Voriconazole (VORI) is an extended-spectrum antifungal agent, with activity against Candida and moulds such as Aspergillus, Fusarium, and Scedosporium. While displaying an overall favorable safety profile, VORI is associated with transient visual adverse events (VAEs). In clinical trials, between 23–35% of VORI-treated subjects reported VAEs, including blurred vision and altered light perception. Over 28 days of treatment with VORI, the VAE was non-progressive and fully reversible following discontinuation. The objective of this study was to investigate and better understand the visual safety of VORI beyond 28 days.
Methods: In a multicentre, open-label, comparative study, 53 patients with paracoccidioidomycosis were randomized to receive VORI (po 200 mg bid) or itraconazole (ITRA) (po 100 mg bid) in a 2:1 ratio over a period of at least 6 months. Visual function tests (VFTs) and safety assessments were performed at baseline, Week 12, Week 24, end of treatment (EOT) and at 8 weeks post EOT. The VFTs included color vision (Farnsworth-Munsell 15 Hue), visual acuity (ETDRS), contrast sensitivity (Pelli-Robson), visual field (Humphrey), funduscopy and slit lamp examination. Other adverse events and laboratory evaluations were recorded at the same visits as VFTs.
Results: 32/35 VORI and 17/18 ITRA patients completed 3 months treatment, with 14/35 and 11/18 respectively receiving >6 months treatment. 1 subject receiving VORI prematurely discontinued due to unrelated sarcoidosis and 2 due to elevated liver enzymes. 16/35 VORI and 0/18 ITRA subjects experienced drug-related VAEs; none were considered serious or severe or resulted in discontinuation. There were 22 separate VAEs in the 16 subjects reporting eye findings. 19 o 22 VAEs started on day 1 of dosing and had resolved by day 3. No VORI or ITRA subject had a significant deterioration (>2 lines) in visual acuity at anytime whilst on drug. There were no differences in other VFTs between the two groups. VORI had no long-term effect on ocular structure, as assessed by funduscopy and slit lamp. There was therefore no relationship of visual function to occurrence of VAEs in either treatment group.
Conclusions: Clinical assessment of the results of VFTs in this study found no evidence of an effect of VORI on long term visual function or new concerns about VORI's effect on the eye.
P1110: Caspofungin bioassay using the hypersusceptible C. albicans cell wall sensor mutant delta-mid2
A. Pascual, D. Sanglard, J. Bille, T. Calandra, O. Marchetti (Lausanne, CH)
Background: Caspofungin (CSP) is the first member of a new class of antifungal agents, the echinocandins, approved for clinical use in patients with candidiasis and aspergillosis. Pharmacokinetics of CSP may be altered in critically ill patients with severe invasive mycoses. Blood levels measurement may therefore help to monitor antifungal therapy. Available HPLC and LC-MS methods for measurement of CSP blood levels are labor-intensive and need sophisticated equipments. A bioassay would be a useful alternative.
Objective: To develop a bioassay for measurement of CSP blood levels using the hypersusceptible C. albicans cell wall sensor mutant delta-mid2.
Methods: The C. albicans mutant delta-mid2 (MIC for CSP: 0.008 mg/L) was constructed by targeted deletion of the gene encoding for a cell wall sensor putatively involved in the maintenance of cell wall integrity. The bioassay was validated according to international guidelines (Shah et al, 2000; FDA, 2001). Standard curve included 8 CSP concentrations over the range 0.4 to 25 mg/L. Four quality controls were used (0.5, 2, 8, 16 mg/L) to study: i) stability of CSP concentrations over time at different pre-analytical storage conditions, ii) accuracy (measured/nominal value × 100, validation range 85–115%), iii) precision (coefficient of variation: SD/mean of measured values × 100, validation range 15%). The validation procedure included 6 intra-run and 6 inter-run measurements.
Results: The limit of detection and quantification was 0.2 and 0.4 mg/L (corresponding to 5 and 10 ng of CSP in a sample volume of 25 ml), respectively. Reproducible standard curves were obtained over the clinically relevant concentration range (0.4 to 25 mg/L) (r ≥ 0.99). Analytical time was 16 h. CSP concentrations with a deviation from nominal values < 15% were measured: i) over 4 days in plasma, and 3 days in whole blood, at 4 C, ii) over 3 and 2 days, respectively, at 21 C, iii) over 6 months in plasma at - 80 C, iv) after 5 freeze/thaw cycles. Intra- and inter-run validation with the four quality controls (mean % value, ± SD) are shown in table 1.
| Intra-and inter-run bioassay validation I | ||
|---|---|---|
| Intra (n = 6) | Inter (n = 6) | |
| Accuracy | 93.1 ± 1.9 | 96.0 ± 2.5 |
| Precision | 1.3 ± 1.7 | 5.8 ± 3.0 |
Conclusions: A rapid bioassay for caspofungin with high accuracy and precision was developed using the hypersusceptible C. albicans cell wall sensor mutant delta-mid2. This new analytical tool may offer an easy to use alternative to sophisticated HPLC/LC-MS methods
P1111: In vitro interaction of albumin and of local anaesthetics with antifungal susceptibility profile of Aspergillus species
R. Araujo, A.G. Rodrigues, C. Pina-Vaz (Porto, P)
Objectives: To evaluate the effect of combination of drugs commonly used in critical care patients, like albumin (Alb) and local anesthetics (lidocaine (Lid) and bupivacaine (Bup)), upon the susceptibility profile of Aspergillus to antifungals.
Methods: Clinical isolates of A. fumigatus (5 strains), A. flavus (3 strains) and A. niger (3 strains) were used. The checkerboard dilution method1 was used for determination of minimal inhibitory concentration (MIC) or minimal effective concentration (MEC) while testing combinations of drugs. Concentration of antifungals (amphotericin B (AMB), itraconazole (ITC), voriconazole (VRC) and caspofungin (CPF)) ranged between 0.03 and 16 μ g.ml−1. Alb 2% and 4% was tested. Final Lid concentrations ranged between 0.125 and 2 mg.ml−1, while Bup serial ranged between 0.06 and 1 mg.ml−1. Data were compared at significance level of 0.05.
Results: Alb was associated to a systematical increase within one to three dilutions of the MIC of AMB and ITC, in all the three species of Aspergillus. Such differences were significant for both antifungal agents. However, MIC values to VRC did not change significantly, after 48 hours, in presence of both tested concentrations of human albumin (P > 0.05). The activity of AMB, ITC and CPF was significantly enhanced in presence of both Lid and Bup, upon all Aspergillus strains. Synergistic activity was found with the highest concentrations of both local anesthetics (0.5-2 mg.ml−1 of Lid and 0.25–1 mg.ml−1 of Bup) associated to these antifungals, upon 2 strains (A. fumigatus). VRC showed a completely diferent pattern in comparison with the other antifungals. In fact, in almost all isolates an indifferent effect was found, while antagonistic effect occurred with Lid (4 strains: 2 of A. flavus, 2 A. fumigatus and 1 of A. niger) and Bup (1 strain of A. niger).
Conclusion: The distinct mechanisms of action of antifungal agents may explain different behaviour of VRC comparing to AMB, ITC and CPF. Drug interactions should be fully evaluated and later taken into account when establishing antifungal therapeutic regimens, particularly in patients receiving multiple medications, e.g. patients admitted in intensive care units or neutropenic patients which represent the main targets for such microbial agents.
1- Arikan S, Lozano-Chiu M, Paetznick V, Rex JH. In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother. 46:245–7, 2002.
P1112: Findings of Candida species in critically ill patients in context with pharmacokinetic-pharmacodynamic properties of antifungal therapy
J.D. Knudsen, M.C. Arendrup, J.S. Andersen, T.H. Jensen, L. Heslet, M. Tvede (Hvidovre, Copenhagen, DK)
Objective: To identify the pharmacokinetic and pharmacodynamic (PKPD) parameters of antifungal therapy predictive for invasive fungal infections in patients admitted to an intensive care unit (ICU).
Methods: The medical records of all ptt admitted to a tertiary hospital ICU in a 6 month period in 2002 were retrospectively reviewed, and the antifungal therapies were recorded and correlated to the findings of fungi from the ptt. The PK-PD-parameters for each pt was estimated from the treatment given and the MIC of the isolated Candida, i.e. AUC/MIC-ratio (in h) for the azoles, and Peak/MIC ratio for the free fraction of amphotericinB. Candida isolated from various infectious foci, or from the surveillance samples taken routinely three times a week, were susceptibility tested using E-tests for fluconazole, itraconazole and amphotericinB.
Results: In total 120 ptt were included. Among the 14 ptt with invasive fungal infections, 3 ptt had bloodstream infections at admission. One of the remaining 11 (9%) received systemic prophylactic therapy before getting colonized, and 3 ptt (27%) were prophylactic treated when colonized, 3 ptt with fluconazole (AUC/MIC: 66–1600), and one pt with liposomal amphotericinB (Peak/MIC = 3). The 1-year survival was 21%. Of the 66 ptt colonised, 7 (11%) received systemic antifungal therapy before colonisation, in total 27 (41%) received systemic antifungal therapy when the colonization was detected, 21 ptt received fluconazole (AUC/MIC: median 267, range <1–1600), 3 ptt received itraconazole (AUC/MIC: 2.500–10,000), 6 ptt received amphotercinB (Peak/MIC>8), 4 ptt received caspofungin. The 1-year survival was 47%. Among the 40 patients without any findings of Candida, systemic antifungal therapies were given in 15%. The 1-year survival was 51%. Statistically significant lower AUC/MIC ratios were found for the prophylactic treatments with azoles for ptt with invasive fungal infections compared to ptt only colonized (p < 0.05). A significant higher morbidity and mortality rate was found among ptt with invasive fungal infections.
Conclusion: An aggressive diagnostic attitude and antifungal treatment directed against the specific infecting Candida species in critical ill patients is highly warranted. The identity and susceptibility of colonizing Candida strains must be determined to give a sufficient preemptive therapy for prevention of invasive fungal infections in patients admitted to intensive care units.
P1113: Tacrolimus pharmacokinetics are not affected by concomitant anidulafungin
J.A. Dowell, J. Schranz, M. Buckwalter, M. Stogniew, D. Krause (King of Prussia, USA)
Background: Fungal infections in transplant recipients are a major cause of morbidity and mortality. Antifungal drugs have been shown to be effective in the prevention and treatment of serious fungal infections, but may interact with immunosuppressive agents. Anidulafungin is a novel echinocandin in late-stage development for the treatment of serious fungal infections. Tacrolimus is a potent macrolide immunosuppressant for prophylaxis of organ rejection in patients receiving allogeneic liver or kidney transplants. Drug interactions with tacrolimus have been observed for caspofungin, another echinocandin. A study was done to assess a possible pharmacokinetic interaction following co-administration of tacrolimus and anidulafungin.
Methods: An open-label, single sequence pharmacokinetic interaction study was conducted in healthy male subjects, ages 18 to 55 years. Subjects received a single oral 5 mg dose of tacrolimus on Days 1 and 13. Anidulafungin was given intravenously as 200 mg on Day 4 followed by 100 mg/day (Days 5–13). Pharmacokinetic parameters were assessed for tacrolimus alone and in combination with anidulafungin. Maximum plasma concentration (Cmax) and area under the plasma concentration versus time curve (AUC) were determined and compared.
Results: Thirty-six healthy males were enrolled in the study. Thirty-five of these subjects completed all treatments. No dose-limiting toxicities occurred in the study. No differences were observed in the pharmacokinetic parameters when tacrolimus was administered alone, compared to concomitant administration. Mean (standard deviation) tacrolimus pharmacokinetic parameters are shown in the table.
| Treatment | Cmax (mg/L) | AUC (mg.h/L) |
|---|---|---|
| Tacrolimus | 0.025 (0.011) | 0.0296 (0.11) |
| Tacrolimus + Anidulafungin | 0.024 (0.008) | 0.0289 (0.08) |
Conclusions: Anidulafungin and tacrolimus can be administered together. The combination was well-tolerated. Pharmacokinetic parameters are not affected when tacrolimus and anidulafungin are administered concomitantly.
P1114: Prediction of human pharmacokinetic properties of BAL4815, a new azole antifungal, from animal data
A.H. Schmitt-Hoffmann, J. Spickermann (Basel, CH)
Objective: To predict the pharmacokinetic properties of BAL4815 a new azole antifungal, in humans. Methods: BAL8557 (the water-soluble pro-drug of BAL4815) was incubated at 10 μg/mL in pooled heparinized rat, cynomolgus monkey and human plasma for 5 minutes at 37°C. BAL4815 was incubated at 1,10 and 100 μg/mL equivalent BAL4815 with rat, cynomolgus monkey and human liver microsomes for 120 min at 37°C in the presence of 1 mg/mL proteins. The extent of plasma protein binding of BAL4815 in rat, cynomolgus and human plasma was measured using the red blood cell partitioning method and 14C-BAL4815. Rats received a single oral dose of 10 mg/kg equivalent BAL4815 and a single intravenous dose of 5 mg/kg equivalent BAL4815 as BAL8557. Cynomolgus monkeys received single oral and intravenous doses of 3 mg/kg as BAL8557. Serial blood samples were obtained. Plasma concentrations of BAL4815 and BAL8557 were quantified using an HPLC/fluorescence method or a LC-MS/MS assay.
Results: In plasma, BAL8557 is converted within minutes to BAL4815 in all species investigated. In the presence of rat, cynomolgus monkey and human liver microsomes, less than 10% of BAL4815 is metabolized during a 120 min period. BAL4815 is bound to plasma proteins with a free fraction of 3.5%, 3.6% and 2.2% in rat, cynomolgus monkey and human, respectively. After intravenous administration, the pro-drug BAL8557 is converted to BAL4815 within minutes. BAL4815 has a large volume of distribution with values greater than the total body water: 15 L/Kg and 5 L/kg in rat and cynomolgus monkey, respectively. BAL4815 is slowly eliminated with half-lives of 5 h in rat and 10 h in cynomolgus monkey. After oral administration of the pro-drug, BAL4815 reaches Cmax-values between 2.0 to 3.5 hours. We observed high bioavailability of BAL4815: 62% in rat and 87% in cynomolgus monkey.
Conclusions: Based on these in vitro results and animal data, we predict that the pro-drug BAL4815 is very rapidly converted to BAL4815 in man. Due to the protein binding and in vitro metabolic stability, BAL4815 is expected to behave as a low intrinsic clearance drug in human (clearance < 10 % of liver blood flow). This combined with a large volume of distribution explains the long half-life > 30 hours observed in man. Animal data suggest a good oral bioavailability as is confirmed in humans.
P1115: Pharmacokinetics and fungicidal activity of aminocandin (HMR3270), a novel echinocandin in healthy volunteers
B. Sandage, G. Cooper, N. Najarian, J. Lowther (Lexington, USA; Romainville, F)
Objective: Aminocandin (AC), an echinocandin, is being developed for treatment of systemic fungal infections. A study was carried out to determine the pharmacokinetic (PK) and fungicidal activity of AC in plasma samples against 2 strains of C. albicans and 1 strain of A. fumigatus following single IV doses.
Methods: Single IV doses of 75–300 mg of AC were administered to 12 healthy, male volunteers in a single-blind, randomized, placebo-controlled trial. Individual plasma samples were collected from active and placebo (PBO) treated volunteers, serially diluted in 25% control plasma/75% growth medium, and the fungicidal titre determined on 2 C. albicans strains and inhibitory titre against 1 A. fumigatus strain. Titres and PK results are the mean values (n = 3). Due to the dilution factor in test medium, the limit of detection was a titre of 4.
Results: The Cmax and AUC of AC increased in proportion to its dose. Mean Cmax was 4.9–16.1 mcg/mL after infusion of 75–300 mg of AC, with respective AUC values of 239–849 mcg*h/mL. The elimination half-life of AC was 48–58 hours, the volume of distribution was 23.5–26.2 L, and the total systemic clearance was 0.328–0.358 L/h. Susceptibilities of the strains to AC were: C. albicans 444 and C. albicans 26, MIC/MFC (mg/L) 0.06, 0.125 and 0.12, 0.5 respectively. A. fumigatus Afu6, MEC/MFC (mg/L) 0.06 and >128, respectively. Samples from all subjects dosed with 75–300 mg of AC showed fungicidal concentrations against both C. albicans strains. Mean peak titres ranged from 16 (75 mg) to 128 (300 mg). The duration of measurable fungicidal titres ranged from 48 hours (75 mg) to 168 hours (300 mg). Inhibitory titres of plasma samples against A. fumigatus Afu6 ranged from a peak of 8, to 4 at 48 hours (75 mg). For 300 mg, dose titres ranged from 64 at the peak, to 4 at 168 hours. No antifungal effect was noted in PBO samples, as expected. AC was well tolerated with few reported adverse events.
Conclusion: AC exhibited a long half-life and significant dose-dependent fungicidal titres over the range evaluated. The 300 mg dose retained antifungal activity even up to 168 hours post administration. Infrequent dosage regimens may be possible with AC and further studies are warranted.
Infection control: environmental and hand disinfection
P1116: Disinfection of patient rooms, using dry mist of hydrogen peroxide
B.M. Andersen, M. Rasch, K. Hochlin, J.-E. Fredriksen (Oslo, N)
Background: To control the spread of pathogens in hospital environments, good hygienic routines based on cleaning and disinfection of surfaces contaminated with biological materials are obligatory requirements. Chemicals like chlorine and 5% chloramine have traditionally been used for surface disinfection purposes for a final room disinfection in Norway. In this study a patented programmable device which provides a dry mist of hydrogen peroxide disinfectant is tried for room and surface decontamination.
Materials and methods: The technology produces hydrogen peroxide particles of such a small size that they cirkulate freely in the air-as a mist- making disinfectant accessible to all surfaces (Sterinis, Gloster Sante Europe). The test room was closed and all openings taped to control the concentration of the mist. The concentration of hydrogen peroxide was programmed according to the volume of the enclosed room. The robot was placed in a corner to get the most effective mist concentration ca 2 m in front. Three preset cycluses of hydrogen peroxide dry, 17.4 ppm, mist were done. Each time the diffusion time was 26 min, followed by increasing contact time; 30 min, 60 min and 120 min. Spores of Bacillus Subtilis Raven 1162282 were placed on a table, on walls, and outside different medical equipments in the middle of the room. The spore envelopes were either opened or unopened before the disinfection test was performed. The spores were removed after 18–20 hours.
Results: Preliminary results from disinfection of the enclosed room showed no groth in 6/6 tests. Repetitive tests were done for 11 days. The hydrogen peroxide treatment disinfected 33/42 spores (78.6%) in opened envelopes, and 94/104 spores (90.4%) in closed envelopes. The treatment was effective in 127/146 (87%) of all tests.
Conclusion: The use of hydrogen peroxide dry mist programmed to a preset concentration, may be an effective method to decontaminate critical enclosed areas, including isolation units, clean rooms, and general areas contaminated with pathogens. Further studies are needed.
P1117: Disinfection of ambulances, using dry mist of hydrogen peroxide
B.M. Andersen, F.-H. Jensen, K. Hochlin, M. Rasch, J.-E. Fredriksen (Oslo, N)
Ambulances trasporting patients with infectious diseases may easily be contaminated. Special construction and narrow space inside, the ventilation system, and all the equipments and devices present are difficult to disinfect. In this study a patented, programmable device which provides a dry mist of hydrogen peroxide disinfectant is tried for decontamination of ambulances.
Materials and methods: Hydrogen peroxide particles of such a small size that they circulate freely in the air–as a mist- make disinfectant accessible to all surfaces (Sterinis, Gloster Sante Europe, www.sterinis.com). The ambulance was placed in closed garages A and B, with all openings to the garage taped to control the concentration of the mist, and with the ventilation system shut down. The doors of the ambulances were open during the disinfection period and afterwards closed. The concentration of hydrogen peroxide was programmed according to the volume of the enclosed garages. Spores were placed inside and outside the ambulance, and inside devices, equipment and in drivers cabin. 1) Garage A- three cycluses; diffusion time 29 min, concentration ca 36 ppm, followed by increasing contact time; 30 min, 60 min and 120 min. 2) Garage B – one and two cycluses; diffusion time 27 min, concentration ca 42 ppm, followed by contact time; 30 min in first cyclus and 60 min in second. 3)Garage B- three cycluses; diffusion time 27 min, concentration of ca 42 ppm, contact time; 30 min, 60 min and 120 min.
Results: 1) Garage A – three cycluses: No growth in 24/24 spore tests from two separate experiments. 2)Garage B- one and two cycluses: Growth after one and two cycluses in 6/6 and 12/12 spore samples, respectively. 3) Garage B- three cycluses: No growth in 36/36 spore samples, even after placement inside equipments and in drivers cabin. The penetration of hydrogen peroxide into equipment, devices and drivers cabin inside and outside an ambulance was effective when using three cycluses of disinfection.
Conclusion: The use of hydrogen peroxide dry mist, programmed to a preset concentration, may be an effective method to decontaminate critical enclosed areas and devices that are difficult to decontaminate, like ambulances. Further studies are needed, concerning hydrogen peroxide concentration, number of cycluses and contact time.
P1118: Disinfection of surfaces in hospital isolation rooms with ultraviolet C (UVC) light, compared with chloramine
B.M. Andersen, H. Bånrud, E. B0e, O. Bjørdal, F. Drangsholt (Oslo, Rud, Trondheim, N)
The germicidal effect of ceiling- and wall mounted ultraviolet C (UVC) light at 254 nm in isolation units with negative pressure (−45 pascal) was examined and compared with disinfection with chloramine during end-disinfection after patient stay. Microbial samples were taken from surfaces before and after disinfection with UVC (33–47 min) and chloramine (5%, 1 h exposure) using standard contact plates (20cm2). The UVC-distribution in the isolation units was monitored at 165 positions. The output on the floor varied between 0.08 and 3.2 W/m2, with an average (± SD) of 2.2 ± 0.5 W/m2 in the patient room, 2.0 ± 0.7 W/m2 in the sluice and 1.4 ± 0.5 W/m2 in the bath/ decontamination room. On other places, the values varied from 0.08 to 6.82 W/ m2. The units were UVC-disinfected for 33–47 min, corresponding to doses ranging from 160 J/m2 in shadowed area to 19 230 J/m2 at the highest exposed site. According to published UVC-dosimetry, the survival of bacteria and bacterial spores are reduced by 90% with doses ranging from 4–120 J/m2 and 100–365 J/m2, respectively. Thus, UVC doses used in this study should be high enough to inactivate most bacterial organisms, including spores, even on surfaces not directly exposed to UVC. UVC-disinfection significantly reduced the bacteria on surfaces directly or indirectly exposed to UVC to a very low number (from ca 30 to 1–2 cfu/plate), as did 5% chloramine disinfection (fom ca 30 to 1–2 cfu per plate) alone; p < 0.001, and p < 0.001, respectively. Since cleaning before disinfection may be a risk for the staff in isolation units, disinfection with UVC- or chemicals should always be performed first. The presence of completely shadowed areas in the isolation unit (the bed rail, lockers, matresses etc.) still needs disinfection by chemicals before cleaning. Therefore, UVC may not be used alone, but is a good additive to chemical disinfection, to lower the biological burden of infectious agents in isolation units for high risk infectious patients.
P1119: Disinfection of medical equipment, using dry mist of hydrogen peroxide
B.M. Andersen, K. Hochlin, P. Wismar, M. Rasch, W. Svendsen, J.-E. Fredriksen (Oslo, N)
Background: Internal parts of medical equipments, like different ventilators, CPAP, and other equipment associated with the respiratory tract, infusion pumps, suction equipments, etc may be difficult to disinfect. Most equipments have an air cooled motor that takes air from the patients room/environment. Internal parts may then be contaminated. In this study a programmable device which provides a dry mist of hydrogen peroxide disinfectant is tried for surface and internal decontamination of medical equipments.
Materials and methods: Hydrogen peroxide particles of small size circulate freely in the air - as a mist, making disinfectant accessible to all surfaces (Sterinis, Gloster Sante Europe). The test room was closed and openings taped to control the concentration of the mist. The concentration of hydrogen peroxide was programmed according to the volume of the room. Three preset cycluses of hydrogen peroxide dry mist were done. Each time the diffusion time was 12 min, giving a concentration of 12 ppm, followed by increasing contact time; 30 min, 60 min and 120 min. The medical quipment tested: Freedom nebulizer, Micro Air U22, compressor CR 60, Walk boy Pari, pulse oxymeter (SN P 1020601402-N-550), CPAP (Autoset Sprint), Medela suction apparatus, ventilator (Lifecare PVL-100), and 571 infusion pump. Spores of Bacillus Subtilis Raven 1162282 were placed inside and outside different medical equipments. The medical equipment that had motors were started and run during the period of disinfection.
Results: The hydrogen peroxide treatment disinfected opened spores placed inside medical technical equipments in 37/82 (45.1%) cases, and closed (enveloped spores) in 47/88 (53.4%) cases. The treatment was effective in 84/170 (49.4%) of all tests. All the spore tests at inside of medical equipment were, however, negative, when the device was run and ventilated during the period of disinfection; 27/27 tests.
Conclusion: The inside of medical equipment may - by the use of hydrogen peroxide dry mist, be disinfected in ca 50% of all cases. The method seems to be effective when the internal parts are ventilated during disinfection.
P1120: Antimicrobial effect of pine core wood against organisms causing hospital-acquired infections
M. Strehlein, J. Wirmer, E. Schmidt-Eisenlohr, D. Mlangeni, F.D. Daschner (Freiburg, D)
Objective: To compare the antimicrobial efficacy before and after disinfection of pine core wood surfaces with surfaces made of polyethylene and synthetic laminate against organisms typically causing hospital-acquired infections.
Methods: S. aureus (MRSA), E. faecium, E. coli, P. aeruginosa. C.albicans, M. terrae and P camembertii were uses as test organisms. After inoculation of the test organisms on surfaces made of pine core wood, polypropylene and synthetic laminate, samples were collected on RODAC plates before and after disinfection with commonly used hospital germicides (alcohol, aldehyde, glucoprotamine and a quaternary ammonium compound). Bacterial colonies were counted after 0 min, 30min, 1 h, 4 h and 24 h, respectively, according to a standardised microbiological method.
Results: Substantially lower colony counts were measured on pine core wood surfaces before application of the disinfectant compared with counts on polypropylene and synthetic laminate surfaces. After bacterial contamination of the surfaces, significant colony counts were not observed on the surfaces after disinfection with alcohol, aldehyde and glucoprotamine. However, after disinfection with a quaternary ammonium compound, significant elevations in colony counts were found on the pine core wood surfaces in comparison to the polypropylene and synthetic laminate surfaces.
Discussion: The poor efficacy of quaternary ammonium compound on wooden material might be explained by the interaction between wood and the anionic polyphenols and cationic surfactants contained in the disinfectant.
Conclusion: The study findings corroborate the antimicrobial effect of pine core wood against organisms typically causing nosocomial infections. With the exception of a quaternary compound, all the germicides displayed good disinfecting properties. From a hygienic point of view, pine core wood is suitable for use in hospitals.
P1121: Survey of the microbiological quality of drinking water supply in hospitals. Drinking water cooler vs tap water fed dispenser vs bottled water
S. Adler, M. Eikenberg, D. Mlangeni, F.D. Daschner (Freiburg, D)
Objectives: Hygienic, economic and ecologic comparison of drinking water coolers versus tap (mains) water-fed dispensers versus bottled drinking water.
Methods: Samples were taken from each system without preflow or cleaning of the nozzle. These comprised 2 samples from 20 drinking water coolers each over 2 months, 1 sample per week from the tap water dispenser over 6 months, and samples from 6 different bottles of drinking water. Total colony counts were analysed at 22°C and 36°C, respectively. Total P. aeruginosa, E. coli, and coliforms, as well as sulphite-reducing clostridia were examined according to European Norms (EN ISO) for compliance with the German Drinking Water Ordinance 2001 (limit value for total colony counts at 22 ± 2°C: 100 cfu/ml, at 36 ± 1°C: 100 cfu/ml and 20 cfu/ml for bottled
water). Costs per litre were calculated and compared based on the economic data supplied by the manufacturers. The ecological impact of the different systems was evaluated based on expert opinion.
Results: All the samples from the water cooler system exceeded German Drinking Water Ordinance threshold values. All the samples taken from the tap water dispenser, and, with one exception, all the samples from the bottled water complied with the German Drinking Water Ordinance. If more than 400 l of water are consumed per month, the tap water dispensing system and bottled water are more economical than the water cooler system (¢ 0.57 per 1 for water cooler, ¢ 0.45 for month tap water dispenser, ¢ 0.49 per l for bottled water). In economic terms, the water cooler system can only be recommended for consumption levels below 400 l per month. From an ecological point of view, the tap water dispenser is most favourable (expressed in CO2-emissions per year for 403.720 l at Freiburg University Hospital), followed by the water cooler system and finally the bottled water.
Conclusion: For reasons of hygiene, the use of water cooler systems cannot be recommended in hospitals. Furthermore, drinking water cooling systems are only economic for low consumption rates. Tap (mains) water-fed dispensers feature the best hygienic, economic and ecologic properties.
P1122: Citrofresh, a revolutionary new, natural, broad spectrum disinfectant
Z. Nack, R. Narain (North Geelong, AUS)
Objectives: The objective of this presentation is the evaluation of the effectiveness of Citrofresh- a revolutionary new, organic, non-toxic, non-carcinogenic, non-irritative, non-rinse, biodegradable sanitizer and disinfectant- against the three major group of multiresistant bacteria; Methicillin Resistant Staphylococcus sp. (MRSA and MRSE), Vancomycin Resistant Enterococcus sp. (VRE) and Gentamicin Resistant Gram Negative Bacteria,(Acinetobacter sp. and Pseudomonas sp.) Citrofresh has been classified by the FDA (USA) as a “GRAS” product,-“Generally Regarded As Safe”.
Methods: The investigation was performed using TGA (Therapeutic Goods Administration, Australia) Disinfectant test, given by Kelsey & Maurer, evaluating disinfectant's performance. The test consisted of challenging the diluted disinfectant (Citrofresh 4%–6% and 10% in sterile hard water) with bacterial inoculum (108 to 109 orgs/ml, grown in ‘Wright and Mundy Dextrose medium), withdrawing a sample after a given time (8 min.) and culturing it in a suitable recovery medium (5 bottles of Nutrient Broth). After sampling (takes 2 min), the mixture was challenged again with a second inoculum for 8 min, (total of 18 min) than sampled for culturing in other 5 Nutrient Broth, at 37 degree Celsius for 48 hrs. The test was passed or failed according to the extent of growth- there is no growth in at least two out of the five recoveries broths-shown in the two cultures sampled. The test was performed with the addition of sterile yeast (organic soil, dirty condition. For test validation, we used Virkon S -a registered, broad spectrum disinfectant-in 1% concentration.
Results: The effective concentration against Methicillin Resistant Staphylococcus sp. (MRSA or MRSE)is from 4%. The effective concentration against Vancomycin Resistant Enterococcus faecium and Enterococcus faecalis is from 4%. The effective concentration against Gentamicin Resistant Acinetobacter sp. is from 8%, and against Gentamicin Resistant Pseudomonas aeruginosa, is from 10%.
Conclusion: The above mentioned testing procedure imitates the real situation of a cleaning process in a highly contaminated area or surface. According to our results, Citrofresh can be regarded a very effective and safe, broad spectrum sanitizer. Its recommended concentration is minimum 10% (from 4% for Gram positive cocci only) in hospitals, nursing homes, child care centres and in any other community or health organizations.
P1123: Comparison assessment of antibacterial efficiency of finishes used in medical areas
B. Jakimiak, E. Röhm-Rodowald, M. Staniszewska, M. Cieslak, G. Malinowska, A. Kaleta (Warsaw, Lodz, PL)
Objectives: The application of antimicrobial finishes to textiles can prevent bacterial growth and might reduce the risk of infection resulting from fabrics that are contaminated with pathogenic microorganisms in hospitals. The main aim of this study was the determination of the antibacterial activities of chemical treatments applied to textiles. Comparison of testing methods assessing antibacterial efficiency was conducted. These studies were performed in order to select the right methods of evaluating the antibacterial and bacteriostatic activity of finishes.
Methods: Fibers and fabrics made from cotton (100%) applied with quaternary ammonium salts were tested. Finishes treated with bactericidal agent were compared with samples (not treated with the disinfectant). The European Standards ISO / DIS 20645/2002 and AATCC 147/1998 suitable for assessment of antibacterial activity were applied. The bacterial strains recommended by the above standards such as: Klebsiella pneumoniae (ATCC 4352), Staphylococcus aureus (ATCC 6538), Escherichia coli (ATCC 11229) were tested. Due to its high resistance to quaternary ammonium salts, additionally P. aeruginosa (ATCC 9027) was examined. Bacterial suspension 1 – 2,9 × 108 cfu/ml was prepared according to the standards’ requirement. The samples impregnated with biocidal products were examined with agar diffusion plate test. The specimens were located transversely across the bacterial inoculum on the nutrient agar. The level of antibacterial activity was assessed by examining the extent of bacterial growth in the contact zone between agar and the specimens. Additionally, the extent zone of inhibition (minimal 1 mm) around the specimens was considerate.
Results: Tested fibers did not show antibacterial activity. The fabrics showed antibacterial activity against K. pneumoniae and S. aureus (inhibition zone 4 mm). The examined specimens showed no bacteriocidal activity against Escherichia coli and Pseudomonas aeruginosa. The results obtained in two applied methods were comparable in assessing antibacterial activity of finishes. The antymicrobial finishes did not fulfill requirements of the standards.
Conclusion: Based on the obtained result the tested antimicrobial finishes may not be considered effective in preventing bacterial transfer at contaminated areas in hospitals.
P1124: A new interactive approch to improve hand hygiene compliance
J. Holt, E. Tvenstrup Jensen, D. Buhl (Copenhagen, DK)
Introduction: The compliance of guidelines for hand hygiene is well below 50 % despite several at-tempts to improve. When planning an educational outline to promote a behavioural change in the hand hygiene practice in the aim of lowering the incidence of Nosoco-mial Infections the mapping of critical factors and implications that affect this practice is of utmost importance.
Objectives: This study was an empirical investigation of the aspects of the hand hygienic practice as it takes place in the Danish health care system today. The study attempted to answer the question: “How can the health staff's lack of compliance with hand hygiene be explained and understood as basis for planning an educational material to support a behavioural change.”
Methods: Literature studies of hand hygiene, a questionnaire based done survey (1700 per-sons/294 respondents) and qualitative interviews (N = 15) was performed in order to uncover the explanations for this low rate of compliance. The data was analysed and discussed on the basis of theories on action, experience, reflective thinking, control and rituals in order to aim for a broader view and under-standing of this field.
Results: Both the questionnaire and interviews showed that hygiene still is a field that has great implications on the interactions between individuals. Furthermore it seemed difficult for the staff to draw a professional and not a private line between “the clean and the unclean” and thereby perform hand hygiene without compromising each other. Further the interviews showed that it is difficult for the staff to react on something they cannot see and that not gives an immediate result when staff does not act as pre-scribed.
Conclusions: Hand hygiene training should be targeted using a new approach which puts focus on the interpersonal relations and who allows interactivity to build up experience with what happens when you do not perform hand hygiene. The training should aim for an open minded dialogue and should be taught in a media that allows reflection, experi-mental learning and shows the invisible. On the basis of this study a web based training program in hand hygiene who allows staff and all others with interest in this field has been developed and is now available in Danish on the Statens Serum Institut web-site (www.ssi.dk). The training program contains facts on hand hygiene, latest litera-ture and gives room for visualising, experiments and testing.
P1125: Spread of a carbapenem-resistant Pseudomonas aeruginosa associated with contamination of hand-washing facilities on an intensive care unit
S. Jamdar, J.S. Cargill, R. Catlin, A.O. Qamruddin, C. Williams (Manchester, UK)
Objectives: An increased rate of isolation of carbapenem-resistant P. aeruginosa was noted on an intensive care unit (ICU) between August and September 2004. We here report the clinical and epidemiological features of this spread.
Methods: A regular six-monthly assessment of the antibiotic resistance profiles is made for our 12-bed ICU, showing that carbapenem sensitivity (based on BSAC guidelines for disc diffusion testing) for P. aeruginosa usually runs at at least 85% (Nov 2003–April 2004, 116 isolates from 41 patients; May–October 2003, 81 isolates from 25 patients). Between August and September 2004 18 isolates from 7 patients (from a total of 45 isolates, 10 patients) were shown to be carbapenem resistant. All 7 patients were intubated and were on treatment for pseudomonal infections of varying degree. None received carbapenem treatment during this period. Swabs were taken to exclude the presence of an environmental source of resistant Pseudomonas.A selection of isolates from 2 patients and the environmental isolates were sent to a reference laboratory for PFGE typing.
Results: PFGE typing showed that at least two types of P. aeruginosa serotype 01 were present within the patient population. The environmental screening revealed the presence of carbapenem-resistant Pseudomonas in the drainpipes of some of the hand basins in the ICU, but not the taps. PFGE typing showed that this strain was indistinguishable from one patient's strain.
Conclusion: This shows that the spread of resistant Pseudomonas within a unit may be partly associated with contamination of the hand washing facilities. Infection control measures were effective in eradicating the organism from the basins. No further carbapenem-resistant isolates have been noted from any later patients.
P1126: Impact of hand hygiene on hospital-acquired infections in the cardiosurgical department of a Greek university hospital
S. Metallidis, N. Harokopos, A. Tsona, E. Koumentaki, G. Batanis, P. Kollaras, P. Nikolaidis (Thessaloniki, GR)
Objective: The purpose of the present study was to estimate the incidence of Hospital Acquired Infections (HAIs) after increasing the compliance of hand hygiene in the cardiosurgical department of a Geek University Hospital.
Methods: Data concerning the year 2002 and 2003 were derived from the database of HAIs of our hospital. The Infectious Disease Division is responsible for the surveillance of HAIs in a daily base. Hand hygiene compliance for the year 2002 was estimated from questionnaires that were given to all medical stuff. Hand hygiene compliance during the year 2003 was estimated from the same questionnaires as well as from random visits of nurses of infection control committee. The increase of the hygiene compliance the year 2003 was achieved by monthly lectures to the personnel of the department and by using pictures of the proper way to wash hands in many visible places. Between all beds there were alcoholic solutions for the stuff to use.
Results: In year 2002 1243 patients were hospitalized, 900 of them had at least one operation. 106 HAIs (8.2 %) were detected (21 LRIs, 42 SSIs, 32 BSIs, 6 UTIs and 5 others). The hand hygiene compliance was estimated 38%. In year 2003 1369 patients were hospitalized, 857 of them had at least one operation. 71 HAIs (5.1%) were detected (8 LRIs, 25 SSIs, 30 BSIs, 4 UTIs and 4 others). The hand hygiene compliance was estimated 62%. MRSA infections were also reduced from 27 in year 2002 to 14 in year 2003
Conclusion: The increase of hand hygiene compliance has significantly reduced the incidence of HAIs, especially SSIs and LRIs and contributed in the reduction of MRSA infections. We did not observe any reduction in the BSIs.
Exotic infection – II
P1127: Prevalence of Leishmania infantum antibodies in central northern Spain
M.A. Bratos, M.P. Gutierrez, M.P. Zarzosa, I. Garrote, R. López Izquierdo, S. Garcinuño, A. Almaraz, C. Cañavate, A. Rodriguez Torres, A. Orduña (Valladolid, E)
Introduction: Leishmaniasis has increased in importance in recent years as HIV-infected patients have emerged as a risk group for the disease. However, real prevalence in the general population is unknown.
Objetive: The objective is to know the antibody seroprevalence for infection by Leishmania infantum in the general population of Castilla-Leon (Spain).
Methods: A random sample from the general population (4825 sera) and from HIV-infected patients in the Autonomous Community of Castilla-Leon was collected in 1996. Seroprevalence of antibodies against L. infantum was determined by an indirect enzymoimmunoanalysis (EIA) test designed in the laboratory.
Results: Anti-Leishmania infantum antibody seroprevalence in the general population was 4.9%. There is a significant increase in seroprevalence with age (P = 0.001), from 3.96% in the 14–20 years group up to 7.2% for those over 70 years old. There were no significant differences between women and men (5.0% versus 4.9%; P = 0.9534). Seroprevalence was significantly higher in people from rural areas than in those from cities (6.0% versus 3.4%; P = 0.001). HIV-infected patients had a seroprevalence against L. infantum of 64.0%. No differences were observed between women and men, nor was there a prevalence increase with age.
P1128: Efficacy of intralesional pentavalent antimony in combination with oral azole for treatment of old-world cutaneous leishmaniasis
A. Beltrame, A. Arzese, F. Cristini, G. Rorato, C. Romano, M. Tavio, P. Viale (Udine, I)
Objective: Systemic treatment of Old-world cutaneous leishmaniasis (CL) lesions is burdened by unacceptable high rate of adverse events related to pentavalent antimonial compounds and by unproved efficacy of monotherapy with azoles. We describe the treatment of 3 cases with combined intralesional and systemic treatment.
Methods: Diagnosis was histologically and microbiologically confirmed. Treatment consisted of oral fluconazole (200 mg once daily) and intralesional injections of meglumine antimoniate (0.8–1 ml/lesion at alternate days). Clinical follow-up (iconographically documented) was conducted weekly during treatment and 1–3 months afterwards. Cure was defined as complete healing of all lesions by the end of treatment and by the 3-month follow-up.
Results: A 30-year-old man presented with a 6-month history of slowly growing round lesions on his right arm and leg. He had a history of travel in the Mediterranean area (Including North African And Middle East Countries) 6 months prior to presentation. Examination showed one nodular lesion (1 × 1 cm) with margin induration and depressed central ulceration on the right arm, a second nodular lesion (0.5 × 0.5 cm) on the right leg, and a red papule (0.5 × 0.5 cm) on the left arm. A 52-year-old man with an history of a 4-month stay in Iraq until 1 months prior to presentation, showed 6 lesions, which had grown during the last three months: two nodular lesions (3.5 × 1 cm, 4.5 × 2 cm) with erythematous margins and a thick crust on the left arm, 4 round lesion (2.5 × 2.5 cm) with depressed central ulceration, at the left arm, right arm, right leg and second finger of the right hand. A 49-year-old man with a 5-month stay in Iraq until 5 months prior to presentation, showed two painless confluent nodular lesions (5.5 × 3.5 cm) with depressed central ulceration at the right elbow, which had grown over 4 months, two round lesions (1 × 0.5 cm and 0.8 × 0.7cm) with a thick crust on the left poplitea fossa and one nodular lesion (1.5 × 1 cm) at right leg. All patients received 12 alternate-days intralesional injections of meglumine antimoniate and 6 weeks of oral fluconazole. All lesions healed completely at the end of therapy and at the 3-month follow-up. None of the patients complained of any adverse events during treatment or follow up.
Conclusion: Treatment with intralesional pentavalent antimony in combination with azole is effective and absolutely safe, in that it reduces the total amount of antimonial exposure.
P1129: Entomological study of sandflies (Dipthera: Psychodidea) in three foci of endemic cutaneous leishmaniasis in Iran
H. Nekouie, M. Razavi, M. Assmar, S. Nadaf (Tehran, IR)
Human leishmaniasis is a globally widespread parasitic disease caused by members of the genus leishmania. Currently, leishmaniasis is considered to be endemic in 82 countries including Iran. Phlebotomine sandflies the vectors of leishmaniasis have received considerable attention in recent years due to the resurgence of leishmaniasis in some endemic areas of Iran, so extensive studies have been conducted on the ecology of sandflies in different parts of the country in recent years.
A total 8026 sandflies were collected by using funnel traps of rodent burrows in rural district of the 3 province of Iran (Shiraz, Yazd, Khozestan). These sandflies identified in 3 Maine croups: Phlebotomus. papatasi(61%), P. sergenti (10%), P. sergentomya (29%). These findings indicate that P. papatasi could be a vector of humans and the gerbils (Merion libycus). The close contact between vectors and resevoirs have created a very efficient cycle for the transmission of the disease in these areas and the villages around these 3 provinces.
P1130: Erysipelas like cutaneous leishmaniasis: a case report
A. Erdogan, D. Balaban, E. Dervis, G. Sengoz, G. Barut, A. Karaoglu (Istanbul, TR)
Cutaneous leishmaniasis is an infectious disorder of the skin caused by leishmania major, tropica, aethiopica and infantum which are transmitted by phlebotomine sandflies. We present here a patient who demonstrated a morphologically rare form of erysipelas like cutaneous leishmaniasis. A 74-year-old woman with a four-month history of erythema and edema on her nasal and left malar area was referred to our clinic for further evaluation. Her dermatological examination revealed an erythematous, edematous and fine desquamative plaque on her nose and left malar region resembling erysipelas. Other physical and laboratory findings were normal. Punch biopsy taken from the lesion and dyed with H.E revealed dense lymphocytic infiltration between the layers of just beneath the epidermis and deep dermis. In addition, a huge number of amastigots were found in macrophages and histiocytes that formed granulomas. In light of these findings the patient was diagnosed with cutaneous leishmaniasis and commenced a regimen of meglumin antimonat 425 mg b.i.d. After two weeks of therapy the lesion was gradually disappeared without any scar formation. In conclusion, cases with cutaneous leishmaniasis are still observed in our country not always with usual clinical appearance, but also like the present case, it may clinically resemble erysipelas and provides difficulties in the differential diagnosis.
P1131: Study of human infection of cutaneous leishmaniasis in a focus of the disease, southern Iran
A.A. Hanafi-Bojd, M.R. Yaghoobi-Ershadi, R. Jafari, A. Barzekar, G. Zamani (Tehran, IR)
Objectives: In the last decade cutaneous leishmaniasis (CL) is reported increasingly from 3 parts of the Hormozgan province, southern Iran. Hajiabad County is one of the important foci CL in Hormozgan province. This investigation was conducted to determine the kind and agent of the disease, and it's prevalence in the area.
Methods: For this study, three villages were chose. About one hundred of each villages and all students of their schools were visited and related forms were completed with asking and examination them about the disease. Smears were prepared from all patients with acute lesions. Also, obtained samples from lesions of 4 patients were injected at the base of the tail of 12 Balb/c mice. Infected mice were transported to the School of Public Health, Tehran University of Medical Sciences for isolation and detection of parasite.
Results: A total of 310 households with 1392 inhabitants (48.4% male, 51.6% female) were visited. Study of prevalence showed 116 cases (8.3%) with scar and 14 cases (1%) with ulcers. The mean of acute lesions and scars per infected cases was 1.64 and 1.87, respectively. Totally 129 cases were observed with sores and scars, and 122 out of them were infected in the area. The highest rate of the acute lesion was observed in 0–4 years old age group (4.5%); meanwhile the highest rate of scars was in 10–14 years old age group (12.9%). Sores were located on hands (8.7%), foot (65.2%) face (4.4%) and other parts of body (21.7%). In the study of schools, 1201 students (53.5% boys, 46.5% girls) were visited. The infection rate to acute lesion was 0.6% and 22.6% of students had scar. There is no significant difference between males and females based on the acute infection (P > 0.05), but this difference was significant based on scar (X2 = 9.84, P < 0.05). The highest infection rate was observed in Tashkooieh village (2.7%). Two injected mice were developed the acute lesion and the agent of the disease was identified as Leishmania major by PCR test.
Conclusion: The infection rate of the sores and scars shows that the disease is located in the studied area in recent years. The disease had one peak during 1995–2000 and has been increased from 2002 up to now. This is the first time that the parasite isolated from human in the area. Therefore, this focus must be added to the Zoonotic Cutaneous Leishmaniasis foci of Iran. The disease is endemic in the area because more than 95% of cases were infected locally.
P1132: Giardia and Cryptosporidium in the Netherlands
L.M. Kortbeek, T.G. Mank (Bilthoven, Haarlem, NL)
Objectives:
-
•
The studies were designed to get an insight into the incidence of protozoal-, bacterial-, and viral infections in patients with diarrheal complaints in different groups: patients consulting their general practioner and the dutch population. Here we focus on Giardia and Cryptosporidium
-
•
To decrease diagnostic deficit
-
•
Study the risk factors
Methods: Three studies were designed and conducted :
-
•
'Haarlem'study: 1994–1996, general practitioners, Haarlem region
-
•
NIVEL: Case-control study in sentinel General practitioners practices (1996–1999)
-
•
SENSOR: prospective population based cohort study with a nested case-control study in the Dutch population. (1999)The studies differ in inclusion criteria and the diagnostic laboratory techniques used, esp. virological stool examinations
Results: Incidence of gastroenteritis in the NIVEL (GP) study (after correction) was 79.5 per 10,000 personyears. This means that 80.000–130.000 persons will consult a GP annually for gastroenteritis. Incidence of gastroenteritis in the population-based study was 283 per 1000 personyears. Giardia was detected in 14.8% of the cases in Haarlem, in 5.4% of the cases in the NIVEL study and 3.3% of the controls. For Cryptosporidium this was resp 3.3%, 2.1% and 0.2%. The diagnostic deficit decrease substantialy by testing for viral pathogens like NLV. Detection of pathogens was influenced by age, season and duration of symptoms. We were able to construct an algoritm for diagnostic workup in GI patients. The main riskfactors for Giardia are:
-
•
swimming OR: 6.8 (95%CI: 2.4–19.3) multivariate OR: 15.6 (3.2–77.1);
-
•
contacts with person with GE 7.1 (1.8–26.6); Multivar. OR 28.6 (3.2–255.6)
-
•
family member attending primary school: 2.8 (1.4–5.8); multivar. OR 2.5 (1.0–6.3) . The population attributable risk fraction (PARF) for all these factors was 49% in the GP patients and 76% for patients in the general population.
Conclusion:
-
•
Giardia lamblia and Cryptosporidium are important pathogens in gastro-enteritis patients in the Netherlands.
-
•
If transmission through water, infected persons and through school contacts could be eliminated, about 50–76% of Giardia gastro-enteritis could be prevented.
-
•
Giardia lamblia is the most frequently found potentially pathogenic intestinal protozoal species in patients with diarrheal complaints in the Netherlands
P1133: Climate impact on seasonal patterns of diarrhoeal diseases in a tropical country
A. Teshima, M. Yamada, T. Hayashi (Uji, Kyoto, JP)
Statistical surveys have been made for the effect of the climate on the epidemic diseases in tropical area, but not so much has been clarified on the relation between the variations of meteorological elements and of the number of patients. In this paper, we apply EOF analysis method to time series of diarrhoea patients and meteorological elements in Bangladesh, to understand effects of the meteorological variation to the prevalence of the diarrhoea disease. The EOF analysis of the time series of patients and meteorological elements averaged every two weeks for 21 years from 1981 to 2001 shows that in the dominating component, the anomaly of the number of the diarrhoea patients has different signs for the periods before and after June, corresponding to the two seasonal peaks of the number of the patients. Higher maximum temperature and more humidity in the pre-monsoon period are found to have a tendency to enhance the first peak of the diarrheal occurrence. We will also report the result for the different types of diarrhoea as V. Cholera, Rota and Etec.
P1134: Serologic evidence for babesiosis in the northern and eastern Tyrol (Austria) and the southern Tyrol (Italy)
G. Walder, R. Edelhofer, J. Simeoni, G. Morosetti, D. Schönitzer, R. Würzner, P. Kreidl (Innsbruck, Vienna, A; Bozen, I)
Objective: Recently, human infections with Babesia strain EU 1 have been reported from Austria and Italy. The aim of this study was to assess the percentage of seropositives against Babesia strain EU 1 among healthy blood donors in the Austrian and Italian part of the Tyrol.
Methods: 1607 volunteer donors were obtained from the institutes of transfusion medicine, representing the demographic situation in the Tyrol regarding gender and residence. Sera were tested for IgG with an in-house Immunofluorescence assay coated with an isolate of strain EU 1 obtained from a human patient. Positive samples were confirmed by a second test with a different charge. False positve results due to antibodies reactive to cells were ruled out by testing with uninfected cells. The proper cut-off was assessed with 120 samples of a low-risk collective according to the guidelines of the WHO.
Results: The cut-off titre was set at 1:64. over all, 70 samples were found positive (4,4%). in detail, 38(3,8%) samples from the Austrian part of the region and 32 (5,2%) samples from the Italian part of the region were found positive.
Conclusions: Evidence was found for the occurrence of babesiosis in all parts of the region, particularly in the lower Inn valley and te eastern Tyrol. Physicians should be aware of this illness and consider it in febrile ilnesses following tick-bites.
P1135: Acute leptospirosis: experience at a tertiary care referral centre
K.K. Sharma, A. Mohan, S. Bollineni, A. Gururajkumar, V. Siva Kumar, A. Sharma (Tirupati, IND)
Objective: Retrospective study of the epidemiology, clinical spectrum and laboratory abnormalities in 36 patients (mean age 42.6 ± 17.1 years; 22 males) with acute leptospirosis seen between January 2001 and April 2004.
Methods: Leptospirosis was diagnosed by leptospiral IgM enzyme linked immunosorbent assay (ELISA) and the serovar was confirmed by the microscopic agglutination test (MAT) using a battery of 12 live leptospiral strains as antigens.
Results: Most of them were outdoors manual workers (52%), housewives (29%), indoors non-manual workers (16%) and unknown (3%). Mean duration of symptoms was 12.4±21.2 days. Majority of the patients presented with fever (89%), jaundice (55%), chills and rigors, vomiting (47% each), cough (28%), abdominal pain (25%), diarrhoea, and altered sensorium (19% each), purpura/bleeding (11%). Salient laboratory abnormalities included anaemia (50%), leucocytosis (59%), thrombocytopaenia (64%), elevated erythrocyte sedimentation rate (ESR) (55%), hyponatremia (50%), hypokalemia (23%). Acute renal failure occurred in 47%. Hepatic function derangement occurred in 64%. Three patients had pulmonary infiltrates and sputum revealed haemosiderin laden macropahges in them. Two others manifested exudative pleural effusion which was bilateral and sequential in one of them. The common serovars encountered included L. autumnalis (30%), L. hebdomadis (22%), L. grippotyphosa (18%), L. icterohaemorrhagiae and L. javanica (11% each), L. australis (8%). All patients were treated with parenteral crystalline penicillin, oral doxycycline and were managed conservatively. Haemodialysis was required in four patients. Two patients died, both of whom developed multiorgan system failure.
Conclusions: Leptospirosis is an important cause of acute febrile illness with renal, hepatic dysfunction and bleeding abnormalities. A high index of clinical suspicion is required confirm the diagnosis early as the condition responds well to conservative management.
P1136: Determination of FR900098, a promising antimalarial agent, in human serum by capillary electrophoresis for pharmacokinetic studies
S. Bronner, C. Renault, M. Hintz, J. Wiesner, H. Jomaa, H. Monteil, F. Jehl (Strasbourg, F; Giessen, D)
The acetyl derivative of fosmidomycin, FR900098, was demonstrated to be twice as active against Plasmodium falciparum in vitro and in the Plasmodium vinckei mouse model. FR900098, as fosmidomycin, is an inhibitor of 1-deoxy-D-xylulose-5-phosphate (DOXP) reductoisomerase, an essential enzyme of the non-mevalonate pathway of isoprenoids biosynthesis. The biosynthesis of isoprenoids in Plasmodium is depending on this DOXP pathway, as found in eubacteria, algae and plants, but not in human. In plasmodium, the DOXP pathway is localised inside a plastid like organelle, the so-called apicoplast. Here, we report on the development of a high-performance capillary electrophoresis (HPCE) technique for the determination of FR900098 in serum. Various instrumental setting for migration (voltage, capillary temperature) were tested and the buffer properties (pH values, component molarities) were optimized. The assay was submitted to standard quality control procedures: within-, between-days reproducibility, accuracy, limits of detection (LOD) and quantification (LOQ), linearity, short and long term stability. Finally, the working buffer used was 14 mM KH2PO4/56 mM K2HPO4,15% methanol, and 0.2 mM hexadecyltrimethylammonium bromide (HTAB). The pH was adjusted to 10.9. The electroosmotic flow was modified by the cationic ion pairing reagent, HTAB. The assays were linear over the large concentration range tested, from 0.25 to 100 μg/ml. The recovery of the sample pre-treatments was higher than 100%. Good precision was obtained, with between-days reproducibilities resulting in coefficients of variation (CV%) of 2.1, 2.0 and 3.2%, and within-days reproducibilities of 0.6, 1.8, and 4.9% (CV%), for 100, 10, and 1 μg/ml, respectively. The LOD was 0.25 μg/ml, and the LOQ was 0.5 μg/ml. The studies of short and long-term stability of FR900098 in serum showed a good stability of the molecule, at room temperature, +4°C or −80°C. Moreover, FR900098 was resistant to numerous cycles of freezing and thawing. Indeed, after four freeze-thaw cycles (4 days), 94.9%, 101.0%, and 97.5% of FR900098 were recovered from the 100, 10, and 1 μg/ml samples, respectively. In conclusion, we have developed a convenient CE technique for the determination of FR900098 in serum which offers advantages of speed, sensitivity, and accuracy. At present, the procedure is applied for pharmacokinetic studies in an animal model of Göttingen mini-pig.
P1137: Present and future of malaria in Kahnouj endemic area, southern Iran
H. Basseri, H. Moosakazemi (Tehran, IR)
Objective: Kahnouj district is associated with one of the malaria regions in southeast of Iran. The anopheleine fauna does not appear to have changed much over several decades.
Methods: Entomological studies and mosquito collection were performed every 15 days from indoor and out door shelters. Malaria surveillance was carried out by Health Centers, Ministry of Health. Microscopy was performed on out patients with fever or suspected malaria. Malaria cases detection were mostly performed passive and rarely actively. The positive cases were treated with chorolquien/primaquen.
Results: In the present study five vectors species of malaria were found in this study which had been previously recorded 3 decades ago. This district like other malaria endemic areas in Iran has been under pressure of anti malaria programmes including case finding and residual spraying insecticide as well as larviciding against the vectors since 1958. Annual incidence of malaria declined from 10.27 to 3.86 during ten years. The most transmission occurred in October to December when the temperature was suitable for vector activity in Kahnouj area. Electricity was recently supplied into the rural area where most malaria cases were found. Therefore, most houses equipped with air conditioner and the resident keep windows close, so they are secured from mosquitoes bites during hot season but not in beginning of spring and autumn when temperature is mild enough, in order to save the electricity cost, the residents do not use air conditioners whereas they leave windows open and no other protection against mosquito bites is provided. Residual spraying insecticide of indoor shelters have been stopped for five years and the most activity of antimalaria programme set up base on case finding. Conclusion; In order to control malaria, indoor residual spraying of insecticide would not assist effectively, so given knowledge to people to use bed net particularly in season people are more expose to mosquitoes bite may be considered as an effective measure in controlling malaria in Khanouj district. Also development in this area is effectively pushing back malaria in near future.
P1138: Application of complementary techniques to diagnosis of malaria
V.M. Martínez, A. Amor, A. Morente, N. Portocarrero, M. Baquero, M. Subirats (Madrid, E)
Objectives: Increase in internacional travels and population migration from endemic areas of malaria have caused a growth in the prevalence of cases in our area. Because the diagnosis of malaria in low parasitemia cases has significant limitations, in suspected samples other techniques may serve as a complementary diagnostic strategy. The aim of the present study was to evaluate different approach to routine diagnosis of malaria.
Methods: From January 2003 until September 2004, we carry out 147 blood samples submited from Pediatric, Tropical Medicine and Emergency Departments of Hospital Carlos III to our laboratory. Inclusion criteria were positive sample by microscopy or negative sample with highly suspicious level (negative samples with indirect sights of malaria) of patients with epidemiological risk factors. Each sample was tested by four diagnostic techniques: microscopical examination of thick and thin films with modified Fields stain, two rapid inmunocromatographic tests (OptiMAL-IT, Diamed; and NOW Malaria, Binax) and in house multiplex PCR assay. Parasitemia levels was determined by a semiquantitative method in thin film.
Results: Of 105 specimens from 96 patients we found 69% of blood samples were collected of travelers/inmigrants from Equatorial Guinea. 21% of positive microscopy results had a parasitemia <0.1%. Microscopy, antigen detection and PCR for the 105 blood samples had an overall agreement of 65.71%. Fourty two specimens were negative and twenty seven were positive with the 4 tests. In the case of PCR-microscopy correlation, it was 91,42% (96/105). Of seven discordant cases 2 have been treated and 5 no treatment data were collected. Regarding agreement in species diagnosis, it was 97.6% (41/42) for P. falciparum, 100% (2/2) for P. ovale, 50%(3/6) for P. vivax. In three cases direct examination of thick and thin film was inconclusive at the species level.
Conclusions: Only direct view of parasite allows to quantify parasitemia level as well as asses response to treatment. Although molecular techniques may achieve potentially elevated power detection, thick and thin films remain as reference method in diagnosis of malaria. Nevertheless in selected cases molecular techniques could be useful as complementary diagnosis.
P1139: Some ecological aspects of Anopheles stephensi liston, the main malaria vector in an endemic focus of malaria in Bandar Abbas district, south of Iran
H. Ladonni, S. Moosakazemi, H. Basseri, A. Podat, A.A. Hanafi-Bojd (Tehran, IR)
Objectives: Bandar Abbas district is one of the Malaria regions in south of Iran, Anopheles stephensi is the vector of malaria in this area. Studies on different aspects of its ecology are essential for establishing the diseases control programme. Method: Following the annual report of cases of malaria from different area of Bandar Abass district, Hormozgan provience, an investigation on some ecological aspects of this malaria vectors was carried out from April 2002 to December 2003. Entomological studies and mosquitoes collection were performed every 15 days from indoor and outdoor shelters as well as breeding places with the aid of suction tube and dipper.
Results: Entomological researches were found that five vectors species of malaria in this study had been previously recorded 2 decades ago. Anopheles Stephensi was recognized as the main vector of malaria in this area with two peaks, one in May and the other in December. The most malaria transmission occurred in June and December. The larval habitats includes draying river bed with pools, rocky river pools, stagnant streams, slow foothill streams, temporary pools, slow moving water with or without vegetation.
Conclusion: Operational of insecticides for adult and larval control, as well as surveillance of malaria cases, would not assist effectively to control of malaria, so given another malaria control methods as impregnation of bed nets as well as repellent particularly in seasons that people are more expose to mosquitoes bite, may be considered as an effective measure in controlling malaria in this area.
P1140: Evidence of infection in humans with West Nile virus in Delta de l'Ebre (a wetland in the south of Catalonia), Spain
N. Cardeñosa, D. Bofill, M. Oviedo, J. Alvarez, J. Zaragoza, S. Minguell, G. Carmona, F. de Ory, C. Domingo, A. Dominguez, A. Tenorio and the research network EVITAR (Virus Diseases Transmitted by Arthropods and Rodents)
Objectives: The objective of this study was to evaluate the seroprevalence of West Nile Virus (WNV) in the human population of Delta del Ebre and to determine possible risk factors associated to exposition to this virus transmitted by arthropods (mostly by mosquitoes). The Delta del Ebre wetland is a stopping-off point for birds migrating from Africa and an area where different WNV vectors and reservoirs have been found so is a high-risk area as regard this infection, as well as other arthropod-borne virus infections.
Methods: A total of 952 serum samples from people living in five different municipalities of Delta del Ebre were analysed. IgG (suggesting past infection) and IgM (suggesting recent infection) were determined by ELISA (Focus Technologies). 128 subjects accepted to answer an epidemiological survey. Variables surveyed were gender, age, profession, living place, time living in the actual residence, outdoors activities, mosquitoes bites, use of insecticides and repellents, and clinical symptoms related to WNV infection. Statistical analysis was performed using X2 or Fisher test. Odds ratios and their 95% confidence intervals were calculated and a p<0.05 was considered significant.
Results: Seroprevalence of WNV was 1.3% (12/952) and in one serum Ig M antibodies were detected suggesting recent infection. No statistical differences among positive subjects were found by any of the studied variables but the risk of past infection in those where mosquitoes bites were more frequent was higher (OR: 8.62 (0.44–169 Woolf correction). All positive cases related a background of frequent mosquitoes bites. No clinical symptoms related to WNV infection were reported by the IgM positive subject, but he was born in the area, never been abroad, he was frequently bitten by mosquitoes and he works outdoors.
Conclusions: These results confirm the presence of past infections by WNV or other flaviviruses in people from the wetland of Delta del Ebre in South Catalonia. The detection of one IgM positive serum could signify the present circulation of WNV or other flaviviruses in this area. Diagnosis for these viruses should be also considered in cases of viral meningitis and encephalitis from this risk area.
P1141: Dengue in the Dutch Caribbean
B. Kesztyus (Willemstad, ANT)
Objectives: Dengue is a mosquito borne arboviral illness endemic in tropical and subtropical regions. The illness is characterized by sudden unset of fever, headache, severe myalgia and athralgia, abdominal discomfort, rash and liver enzyme abnormalities. In some cases it develops into Dengue hemorrhagic fever (DHF) or even fatal Dengue Shock Syndrome (DSS). Dengue is caused by a flavivirus of which four serotyes can be distinguished: DEN-1–4. On the Netherlands Antilles there have been epidemics throughout the year with peaks during the rainy season, but no severe DHF or DSS have ever been reported. Most of the cases occur in Curaçao, the biggest island of five with a population of 130,000 and a surface of 90 square kilometers situated 50 miles offshore Venezuela. Over the last 10 years all laboratory requests are filed at the health department and the national laboratory in Curaçao, the Analytic Diagnostic Center (ADC). The purpose of this study is to describe the incidence of Dengue infections on the Netherlands Antilles over the last 4 years in order to create an overview of this emerging disease and its endemic reach.
Methods: Since 2000 all serum samples of suspected cases were tested by Dengue IgM ELISA in the acute and if available also in the convalescent phase. If positive IgM was detected, the serum was send to the Erasmus Medical Center Rotterdam (EMCR) in The Netherlands for serotyping by Reverse-Transcriptase Polymerase Chain reaction (RT-PCR). Since 2002 the laboratory started to use the IgG and IgM ELISA (Focus). The analysis of the data is based on the ELISA results.
Results: In the year 2000 there were 112 requests for Dengue testing of which 21 positive. In 2001 there were 666 requests with 173 positive sera. In 2002 752 suspected sera reached the lab in Curacao of which 277 were positive. In 2003 there were 268 suspected cases of which 50 were positive. In the first 10 month of 2004 522 sera were tested of which 67 positive. Of the 138 sera which were send on dry ice and −20 degree Celsius to Rotterdam for RT-PCR, 24 could be serotyped. No Den-1 and DEN-4 were found, 8 DEN-3 and 15 DEN-2.
Conclusion: Dengue is endemic in the Dutch Caribbean. Diagnostic tools as RT-PCR or serospecific ELISA are not available yet on the islands. Serotyping of sera done The Netherlands indicates that only DEN-2 and 3 are endemic on The Netherlands Antilles. No severe DHF and DSS occurred in the last 4 years.
P1142: Dengue 3 outbreak in Peru
E. Cáceda, J. Perez, A. Huamán, R. Castillo, C. Guevara, J. Olson (Lima, PE)
Objectives: Surveillance of febrile illnesses in 7 cities of Peru provides a means of monitoring newly introduced illnesses as well as describing their spread. Dengue (DEN) is considered the most important arboviral disease because of the significant morbidity and mortality it causes worldwide. In 1990, DEN-1 was isolated during an outbreak of dengue fever among residents of the city of Iquitos in the northeastern Amazon region of Peru. In 1995, an outbreak was associated with the introduction of DEN-2 in the same area. Finally, DEN-3 outbreaks occurred during 2002 in Tumbes and Loreto. Multiple serotypes of dengue virus have circulated in Peru since 1990, but until now, no DHF or DSS outbreaks have occurred. Although the percentage of cases has decreased, new confirmed cases continue to present in the northern regions of our country.
Methods: Patients with fever >38°C and typical symptoms of dengue fever were included in the study. Dengue virus etiologies were confirmed by virus isolation and/or serologic testing.
Results: A total of 7.982 study subjects, ranging from 0 to 85 years of age were enrolled. We confirmed DEN-3 in 1048 patients, 363 (35%) by virus isolation only, 402 (38%) by serology only, and 283 (27%) by both methods. The prevalence of dengue was 13% (1048/7982). No significant association was found between age and confirmed cases. DEN-3 was confirmed in 92(29%) of 312 patients in Tumbes, 936(15%) of 6088 in Loreto, 12(3%) of 480 in Junin, 6(1%) of 474 in Piura, and 2(2%) of 128 in Lima. In the year 2000, DEN-3 cases comprised 1% of the total (9/609), in 2001 it was 1% (16/1557), in 2002 it was 25% (679/2694), in 2003 it was 8% (123/1567), and in the first 8-months of 2004 DEN-3 accounted for 14% (221/1555).
Conclusion: Virologic cultures and serologic data have confirmed that DEN-3 caused and outbreak of classical dengue fever in the northern areas of Peru (Tumbes & Loreto). Since the detection of DEN-3 in 2000, it has spread to other areas of Peru where it has become the predominant serotype.
P1143: Generalised cowpox infection after exposure to infected rat
B. Hönlinger, N. Romani, C.P. Czerny, R. Höpfl, H.P. Huemer (Innsbruck, A)
Case report: A 16 year old boy presented with fever and a generalized exanthema at the local dermatology clinic. The mixed appearance of pustules and umbilicated non purulent vesicles led to the suspicion of an Orthopoxvirus infection. The patient reported that little red dots had occurred 2 weeks earlier at the extremities after contact with a sick pet rat. 1–2 weeks later a generalized pustular exanthema appeared, which was associated with high fever (>39°C) and a pronounced feeling of sickness. Histologically no viral inclusion bodies were found in pustule material but poxvirus particles were detected by ELMI in swabs from pustule ground. Following the anamnestic suspicion of transmission by an infected rat, which unfortunately had perished soon afterwards, and the experience made at the recent monkeypox outbreak in the USA initiated by imported rats, one of the major aims was the exclusion of monkeypoxvirus. This was accomplished by PCR typing, which like ELMI had been established on occasion of the implementation of the Austrian plan for poxvirus preparedness ('Pockenalarmplan') and despite the diagnostic means for detection of variola vera also included the ability to discriminate between animal Orthopoxviruses. Additionally serological diagnosis was performed and presumably due to the protracted course of infection cowpox specific IgG antibodies were already present at admission with a titre of 1:800. Interestingly the humoral immune response initially seemed to be rather cowpox specific as there were no antibodies crossreacting with vaccinia virus detectable in indirect immunofluorescence. As an exclusive immune reaction with one species alone would be a very rare situation observed with orthopoxviruses we did more extensive testing by western blot analysis. Although not exclusively directed against cowpoxvirus antigens a very restricted reactivity of the patient serum was observed in the early course of infection using different recombinant and virus-derived Orthopoxvirus antigens. This would suggest that also serological methods might be able to give a hint towards rapid determination of Orthopoxvirus species, which certainly is also the case with immunological antigen detection methods.
P1144: Crimean-Congo haemorrhagic fever in Eastern Turkey: clinical features, risk factors, prognostic factors and efficacy of ribavirin therapy
Z. Ozkurt, I. Kiki, S. Erol, F. Erdem, N. Yilmaz, M. Parlak, M. Gundogdu, M.A. Tasyaran (Erzurum, TR)
Objective: Crimean-Congo hemorrhagic fever is being epidemic in recent years in Turkey. We assessed the clinical features, risk and prognostic factors of this disease, and efficacy of ribavirin therapy.
Methods: From 2002 to 2004, 60 cases (26 confirmed and 34 suscepted) admitted to our hospital were included in this study. The diagnosis was confirmed with ELISA and/or RT-PCR.
Results: Age, farming, handled livestock, to be housewive, living in rural area, bitten by tick, removing tick from animal and living in north part of our city (Erzurum) were determined as the risk factors for the CCHF in our region. Fever during hospitalization, confusion, bleeding from multiple sites, presence of petechia or ecchymosis, very high levels of ALT, AST, LHD and CK, long PTT, high INR and urea level, and severe thrombocytopenia were poor prognostic factors. The clinical outcome was better in ribavirin group, and white blood cell (WBC), PLT, ALT-AST returned to normal levels in a short period in cases with treated ribavirin (p = 0.001, 0.006, and 0.031 respectively). The need of blood and blood product was not different between both groups. But, number of patients with bleeding more in ribavirin group (63% vs. 36%, and p = 0.04). Mean hospitalization duration was not different (7.7 days in ribavirin groups vs 10.3 days in the control group). Fatality rates were 9% (2/22) in ribavirin group vs 10.5% (4/38) in the control (p = 0.85). Of ribavirin group, diagnosis and therapy were late in first case who died, and absorbsion of the oral drug did not possible due to massive hematemesis and melana in second case. The hospital expenditure was not different in both groups.
Conclusion: In Estern part of Turkey the risk and prognostic factors of the disease were similar in other outbreaks of CCHF. Ribavirin decrease recovery duration of the disease, but not hospitalization time and expenditure. Further studies need for evaluation of ribavirin therapy respect to need of blood or product and mortality in CCHF.
P1145: Demographic, epidemiological and clinical data analysis of 81 confirmed cases of Crimean-Congo haemorrhagic fever in Iran
M. Mardani, MA. Keshtkar Jahromi, K. Holakouie Naieni, B. Haghighat (Tehran, IR)
Objectives: In order to report epidemiological, demographic and clinical features of Crimean-Congo Hemorrhagic Fever (CCHF) cases in Iran, we evaluated 81 confirmed cases that were reported to the ministry of health since June 1999 up to September 2001.
Methods: Confirmed cases were defined as those who had signs and symptoms compatible with those of CCHF cases in association with serological test results that were positive for IgM and/or IgG by ELISA. Confirmed cases were evaluated for sex, age, occupation {at risk (physician, butcher or nurse) and low risk (teacher and household worker)}, place of residence, animal contact, human contact, clinical findings and laboratory data such as fever, hemorrhage and thrombocytopenia.
Results: 72% (59 cases) were male. 51% (42 cases) were 33 year old or older. 48% (39 cases) were reported from only one province in the south of Iran (Sistan VA Balouchestan). 79% (64 cases) had history of animal contacted, but only 16% (13 cases) had history of contact with a human case of CCHF. 98% (80 cases) were febrile. 98% (80 cases) had hemorrhagic manifestations and 98% (80 cases) were thrombocytopenic.
Conclusion: Most CCHF cases in Iran were male, 33 year old or older, with low risk occupation, had history of animal contact and from a major province that borders upon Afghanistan and Pakistan which are endemic for CCHF. Nearly all of the cases were febrile, had hemorrhage and were thrombocytopenic. It seems that importing infected animals from countries endemic for CCHF may be a major risk factor for acquiring the disease in our country. We conclude that in endemic areas, febrile illnesses with hemorrhagic manifestations and thrombocytopenia should be evaluated for CCHF. This project has been supported by Infectious Diseases and Tropical Medicine Research Centre of Shaheed Beheshti University of Medical Sciences, Tehran, Iran.
P1146: The analysis of occupational Crimean Congo haemorrhagic fever virus, Brucella spp., and Coxiella burnetii infections among veterinarians in Turkey
Ö. Ergonul, H. Zeller, S. Kilic, S. Kutlu, M. Kutlu, S. Cavusoglu, A. Gozalan, B. Esen, B. Dokuzoguz (Ankara, TR; Lyon, F; Aydin, Tokat, TR)
Objective: To investigate the prevalence of the infections by Crimean-Congo Hemorrhagic Fever (CCHF) virus, brucella spp., Coxiella burnetii among veterinarians.
Methods: The study was conducted in two provinces of Turkey, one is an endemic region both for CCHF and brucella infections, and the other is not. The sera from veterinarians were collected in October 2003, and tested for antibodies to CCHF virus, Brucella spp, and Coxiella burnetii.
Results: Forty veterinerians from endemic region (Tokat), and 43 from non-endemic region (Aydin) were included. Demographic characteristics in two groups were similar, whereas professional activities of veterinarians in non-endemic region were more intense (p = 0.001). The CCHF IgG positivity (2.5% vs 0%), brucella agglutination titre of >1/160 (27.5 vs 4.6%) were more common in endemic region than non-endemic region. Three veterinarians in Tokat had malaise, myalgia, and fever. In multivariate analysis to detect the risk factors for serum tube agglutination of > 160, the veterinarians living in endemic area were found to have 7.8 times higher risk of brucella infection than the ones living in non-endemic area (OR; 7.8, Confidence interval; 1.4–40.9, p = 0.015). The prevalence of Coxiella burnetii serology was equal in both regions as 7%, and none of the seropositives had complaints. The history of tick bite was significantly more common in the endemic region than the non-endemic region (35% versus 12%, p = 0.011).
Conclusions: CCHF and brucellosis compose infection risks for veterinarians in endemic region, despite the veterinarians in endemic region perform less riskfull professional activities. Veterinarians in CCHF endemic regions should be warned to protect themselves against tick bites according to universal precautions. The use of masks should be employed to prevent inhalational transmission of brucellosis in endemic regions.
P1147: Changes in temperature and the Crimean Congo haemorrhagic fever outbreak in Turkey
O. Ergonul, S. Akgunduz, I. Kocaman, Z. Vatansever, V. Korten (Ankara, Istanbul, TR)
Objective: To investigate the role of the climatic factors that could effect the activation of Hyalomma marginatum marginatum population, and consequently the emergence of Crimean-Congo Hemorrhagic Fever (CCHF) epidemic.
Methods: The meteorological data were obtained from three meteorology stations (Tokat, Sivas, and Yozgat), where the majority of the CCHF cases were reported in the last 2 years. These 3 provinces are located at the northern parts of eastern Anatolia and southern parts of Black sea region. Temperature data have been observed and recorded by the Turkish State Meteorological Service (TSMS), and were available for 70 years in Sivas, for 40 years in Tokat, and for 60 years in Yozgat. Meteorology stations are located at the city centres, not at the airports. Temperature variations and trends for Turkey were analysed by using a data set including monthly averages of daily mean, and minimum temperatures. Annual rainfall, and the number of days in April with the temperature of > 5°C were also included in the analysis. In order to detect homogeneity in mean annual series, first a homogeneity analysis was performed by using the non-parametric Kruskal-Wallis (K-W) test. The non-parametric Mann-Kendall (M-K) rank correlation test (13) was used to detect any possible trend in temperature series, and to test whether or not such trends are statistically significant. Statistical significance was set as <0.05 in both K-W and M-K tests.
Results: The monthly mean temperature and the monthly minimum temperatures over 70 years in Sivas increased homogenously with a significant increasing trend (p < 0.05). Within a smaller period, from 1990 to 2003, the daily mean temperature in April, increased significantly in these provinces. The number of days with the temperature of >5° C increased homogenously in January, February, March, and April in Sivas, and the trend was significant for April. A significant increase in yearly rainfall was detected in Tokat.
Conclusion: Recent climatic changes will inevitably coincide with any recent epidemiological phenomena, but this does not necessarily indicate causality. A significant increasing trend of temperature was detected in only one (Sivas), and rainfall in another (Tokat), of the three provinces where a CCHF epidemic occurred in 2002–2004. At the same time, changes in biotic environmental factors, of the sort that could be beneficial for survival of large numbers of hyalommas, have also occurred.
P1148: Epidemiological measures of Crimean-Congo haemorrhagic fever infection in Sistan va Baluchestan province, Iran
K. Holakouie Naieni, S. Izadi, S. Chinikar, A. Nadim (Tehran, Zahedan, IR)
Objectives: Since 1999, many cases of Crimean-Congo Hemorrhagic Fever have been reported from different parts of Iran. This study intends to define CCHF seroprevalence, incidence rates, and the most important risk in Sistan va Baluchestan province, Iran.
Methods: Using cluster sampling with probability proportional to size, 310 subjects were selected from various Zahedan and Zabol districts in the northern part of the province. Blood samples were drawn from consenting subjects, once at the beginning of the study and then 6 months later. A total of 18 out of 285 subjects who consented to give blood samples were actually positive on IgM and IgG capture ELISA tests.
Results: The calculated seroprevalence was 6.32% (95% CI: 3.24% to 9.40%). Of the subjects who were sampled for the second time (226 persons), only one had experienced seroconversion. The calculated incidence rate was 0.48 (95% CI: 0.00% to 1.44%). 14 out of the 18 subjects with definitely positive IgG or IgM were females. In multivariate analysis, age, education, and history of slaughtering livestock were significantly related to the risk of infection. History of travel to the rural areas was inversely related to the risk of infection. Only one of the seropositive subjects had a history of tick bite.
Conclusion: This study shows the importance of subclinical infections in the epidemiology of this disease in Iran. It also seems that the risk of infection for housewives is high. Regardless of the high female to male ratio of seropositive subjects, it appears that the epidemiologic characteristics of the infection in this region are not so different compared to other parts of the world. This investigation received financial support from the WHO's Eastern Mediterranean Regional Office (EMRO), Division of communicable Diseases (DCD) and the WHO Special Programme for Research and Training in Tropical Diseases (TDR): The EMRO DCD/TDR Small Grants Scheme for Operational Research in Tropical and Other Communicable Diseases.
Fungal susceptibility testing
P1149: Antibacterial and antifungal activities of some new acrylate complexes
M. Badea, R. Olar, D. Marinescu, V. Lazar, R. Cernat, M. Balotescu (Bucharest, RO)
The interest in the coordination properties of acrylate acid and its homologues was generated by the facile synthesis of the ‘metal-containing monomers’ (MCM) materials. These compounds can be polymerised with a lot of organic monomers leading to various metal-containing polymers. Polymeric transformations of MCM led to a new research field of current interest due to the practical importance of the obtained products which exhibit a number of unique features: high catalytic activity, unusual magnetic, electro-physical and biological properties. These polymers are especially appropriate for biological applications (tissue engineering, implantation of medical devices, dentistry, bone repair etc.) because of their molecular weight, compositions and architectures which can be regulated through controlled reactions. We report here the antibacterial and antifungal activity of new complexes of type M(phen)(C3H3O2)2(H2O)y ((1) M: Mn, y = 0; (2) M: Ni, y = 2; (3) M: Cu, y = 1; (4) M: Zn, y = 2; phen = phenantroline and C3H3O2 is acrylate anion), representing the first step products in the synthesis of polymeric materials. The in vitro antimicrobial testings were performed by broth microdilution method, in order to establish the minimal inhibitory concentration (MIC), against Gram-positive (Bacillus subtilis, Listeria monocytogenes, Staphylococcus aureus), Gram-negative (Psedomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Salmonella enteritidis), as well as Candida sp., using both reference and clinical, multidrug resistant strains. Our results showed that the tested compounds exhibited a specific antimicrobial activity, both concerning the microbial spectrum and the MIC value. The MICs values widely ranged between 4 mg/ml and 16 mcg/ml. All the tested compunds were highly active against Salmonella and Listeria (MIC = 16 mcg/ml). The compound no. (2) proved to be very active against Candida species (MIC 16 mcg/ml). S. aureus and P. aeruginosa were resistant to all of the metal complexes only compund no.(1) showing intermediate activity against multidrug resistant P. aeruginosa (MIC 64 mcg/ml). Our studies demonstrated that the tested new acrylate complexes exhibit selective and effective antimicrobial properties that could lead to the selection and use of these compounds as efficient antimicrobial agents, especially for the treatment of multidrug resistant infections.
P1150: Voriconazole, amphotericin and fluconasole susceptibility for keratitis and endophthalmitis fungal pathogens
I. Fedotova (Kharkov, UKR)
Objectives: Investigate in vitro efficacy of voriconazole and other antifungals.
Methods: Microbiology database was scanned and fungal isolates associated with keratitis (186) and endophthalmitis (97) were analysed for classification and isolate frequency. The Sensititre YeastOne microdilution antifungal susceptibility test was used to evaluate susceptibility (MICs) of 34 common fungal pathogens against viriconazole, amphotericin, fluconazole.
Results: Fusarium species remains the most frequent corneal fungal pathogen (57.2%). Colletotrichum species (5.4%) has emerged as the fifth most common mold in keratitis. Top yeast isolates from cornea included Candida albicans (58.6%) and Candida parapsilosis (36.8%). Half of the intraocular pathogens were Candida species. Paecilomyces (3.1%) and Philophora (2.8%) were unusual pathogens. In vitro susceptibility profiles were voriconazole (100%), amphotericin (71.4%), fluconazole (57,8%). Voriconazole MIC(90) were lowest for Candida species (0.014 microg/ml) and highest for Fusarium species (1.5 μg/ml). Reference laboratory MICs correlated 100% for yeast isolates (0.016 μg/ml) but were fourfold higher for Fusarium species (7 μg/ml). MIC(90) for Aspergillus species was 0.4 μg/ml.
Conclusions: Candida, Fusarium, and Aspergillus species remain frequent fungal pathogens. Voriconazole may have a role in the therapeutic management of Candida and Aspergillus ocular infections. Human use and animal models will determine its use in the clinical setting.
P1151: Changes in azole susceptibility and electrophoretic karyotype in sequential bloodstream isolates from patients with Candida glabrata candidaemia
J.H. Shin, D.H. Shin, S.I. Jung, B.J. Oh, D. Cho, S.J. Kee, M.G. Shin, S.P. Suh, D.W. Ryang (Gwangju, KOR)
Objectives: C. glabrata is innately less susceptible to azole than most other species of Candida and it acquires azole resistance after short-term exposure to fluconazole, as recently noted in oropharyngeal isolates. Since C. glabrata has emerged as a significant cause of candidemia, we examined the change in azole MIC and karyotype in sequential isolates of C. glabrata during the course of fungaemia, and its relationship to antifungal therapy.
Methods: Serial bloodstream isolates of C. glabrata were obtained from 15 patients with fungaemia over periods of up to 38 days. Forty-seven C. glabrata isolates from 15 patients (6 patients who received antifungal therapy and 9 patients who did not receive antifungal therapy) were analysed using electrophoretic karyotyping (EK) and tested for antifungal susceptibility to fluconazole, voriconazole, and itraconazole.
Results: The overall rates of resistance to fluconazole (MIC ≥ 64 μg/mL) and itraconazole (MIC ≥ 1 μg/mL) for all 47 isolates were 8 and 50%, respectively. For most patients, the sequential strains from each patient exhibited the same or similar azole susceptibilities. However, sequential isolates from two patients showed three- or four-fold increases in the MICs of all three azole antifungals, while they retained the same karyotypes. Azole-resistant strains were isolated from both patients after fluconazole therapy was discontinued and the intervals after the first blood isolation were 24 and 38 days, respectively. The isolates from one of these patients exhibited increased expression of the CgCDR1 efflux pump. The sequential strains from each patient had identical karyotypes in 10 (67%) patients, but two or four different karyotypes in 5 (33%) patients. The sequential isolates from these five patients exhibited the same or similar antifungal susceptibilities, showed only one or two chromosome band differences, and had no association with previous antifungal therapy.
Conclusion: This study showed that sequential bloodstream isolates of C. glabrata were able to acquire azole resistance in association with fluconazole therapy, and that they developed two or four different karyotypes in some patients, during the course of fungaemia.
P1152: Antifungal susceptibility of clinical isolates of Cryptococcus neoformans
K. Baba, A. Hoosen (Pretoria, ZA)
Crytococosis is a leading mycological cause of morbidity and mortality among HIV/AIDS patients especially in developing countries where anti-retroviral therapy is not easily available. In this study clinical isolates of Cryptococcus neoformans obtained from blood and cerebrospinal fluid (CSF) cultures from patients admitted for meningitis were tested for their in-vitro susceptibility to 3 antifungal agents. A total of 50 clinical isolates obtained from AIDS patients admitted to the George Mukhari Hospital, Pretoria with a diagnosis of meningitis were available for analysis. Antifungal analysis were done by microbroth dilution (M27-A) for amphotericin B and fluconazole. The E test and the disc diffusion tests were performed for voriconazole and fluconazole. All isolates tested were fully susceptible to amphotericin B and voriconazole. For fluconazole, two isolates were resistant by the E test and microbroth dilution method. This has implications for maintenance therapy for the patients who are HIV positive and have cryptococcal meningitis. Voriconazole may be an appropriate alternative in this group of patients. The availability of anti-retroviral therapy may also be beneficial to this subset of patients.
All isolates tested were C. neofermans var neoformans. The antifungal susceptibility test results (according to NCCLS breakpoints - M27A) were follows.
| Disc Diffusion |
Etest |
Broth Dil |
|||||
|---|---|---|---|---|---|---|---|
| S | SDD R | S | SDD | R | Range | Mic 90 | |
| Fluconazole | 46 | 13 | 46 | 2 | 2 | 0.125 > 64 | 8 |
| Voriconazole | 50 | 00 | 50 | 0 | 0 | 0.003-0.38 | 0.125 |
| Amphotericin B | ND | ND | 0.03-0.25 | 0.25 | |||
P1153: Susceptibility to azoles of Cryptococcus neoformans: pre-HAART and HAART eras
R. Claro, A.I. Aller, F. Colom, M. Ramírez, C. Castro, E. Martín-Mazuelos (Seville, Alicante, E)
Objectives: To study the susceptibility to azoles of C. neoformans isolates from HIV patients and establish possible differences between pre-HAART and HAART eras.
Methods: 76 C. neoformans isolates from HIV patients were studied. 29 of them were obtained from patients without HAART from 1994 to 1996; the other 47 were obtained from patients with HAART from 1997 to 2003. The susceptibility to
fluconazole, voriconazole and itraconazole of the first group and the susceptibility to fluconazole and voriconazole of the second one were performed by the broth microdilution method according to the NCCLS guidelines (M27-A2 document). Fluconazole and voriconazole were provided by Pfizer and itraconazole by Janssen. Fluconazole was dissolved in sterile distilled water, whilst voriconazole and itraconazole were dissolved in dimethylsulphoxide. RPMI medium (Sigma) was used for all drugs. Inocula were adjusted to a cell density of 1 McFarland, and microtiter plates were incubated for 72 h at 35°C with agitation (Ghannoum et al. ‘Susceptibility testing of Cryptococcus neoformans: a microdilution technique’. 1992. J Clin Microb. 30, 2881–2886). The final concentrations were 0.12–64 mg/l for fluconazole and 0.015–8 mg/l for voriconazole and itraconazole. For all drugs, MIC values were the lowest drug concentration wich inhibited growth by the 50% (prominent inhibition of growth) compared with the control.
Results: The next table shows the MICs obtained for the tested drugs. From the three isolates with voriconazole MIC > 1 mg/l, two of them had a fluconazole MIC ≥ 16 mg/l. Six isolates with voriconazole MIC = 1 mg/l were found: the fluconazole MIC for one of them was 4 mg/l, for another four was 8 mg/l and for the last one was 32 mg/l.
| Number (%) of isolates |
|||
|---|---|---|---|
| Drug | MIC (mg/l)* | Pre-HAART | HAART |
| Fluconazole | >16 (R) | 4 (13.8%) | 0 (0%) |
| Voriconazole | <16 (S) | 25 (86.2%) | 47 (100%) |
| >1 (R) | 3 (10.3%) | 0 (0%) | |
| Itraconazole | ≤1 (S) | 26 (89.7%) | 47 (100%) |
| >0.5 (R) | 5 (17.24%) | – | |
| ≤0.5 (S/SDD) | 24 (82.76%) | – | |
Arbitrary breakpoint were chosen.
Conclusions: a. There wasn't found any fluconazole or voriconazole ‘resistant’ isolate in the HAART era. b. The percentage (11.84%) of isolates with voriconazole MIC > 1 mg/l is higher than it has been described in other works. c. The 75% of the voriconazole ‘resistant’ isolates were fluconazole ‘resistant’ too, so a cross resistance mechanism could be implicated.
P1154: In vitro susceptibiility testing of micafungina (fk-463) and anidulafungin (ly303366) against candida spp.
M. Ramirez, C. Castro, E. Lopez, R. Claro, C. Martin, A. Romero, E. Martin-Mazuelos (Seville, E)
Objectives: The incidence of invasive fungal infections has increased in the last 20 years also have witnessed an increased resistance to established antifungal agents. Antifungal drug resistance is becoming a mayor problem in certain population, especially in immunosuppressed patients. Micafungin (FK463) and Anidulafungin LY303366 are a new echinocandins with in vivo and in vitro antifungal activity against Candida spp. The aim of these study was to compare the susceptibility of Candida spp two both antifungal agents.
Methods: A total number of 219 Candida spp.(183 C. albicans, 12 C. glabrata, 11 C. krusei, 10 C. tropicalis, 3 C. parapsilosis) isolated from different clinical specimens were included in this study. We determined minimal inhibitory concentration (MIC) of both antifungal agents by following the NCCLS M27 A-2 broth microdilution method. Endpoints were defined as the lowest concentration of drug resulting in prominent inhibition (MIC80) and total inhibition (MIC100) of visual growth compared with the growth in the control wells containing no antifungal.
Results: The MIC90–50 determined at 48 hours and total inhibition (MIC100) are as follows:
| FK-463 |
LY302 |
||
|---|---|---|---|
| Range | MC50/90mcg/ml | Range | |
| (183) | 0.008–1 | 0.01/0.25 | ≤0.03–≥16 |
| (12) | 0.008—4 | 0.06/1 | ≤0.03–0.5 |
| (1) | 0.01–0.5 | 0.5/0.5 | ≤0.03–0.5 |
| (10) | 0.06–0.25 | 0.06/0.25 | ≤0.03–0.12 |
| basis (3) | 2–4 | 2/4 | ≤0.06–2 |
| (219) | 0.008–4 | 0.03/0.5 | ≤0.03–≥16 |
Conclusion: These data suggest that both antifungal agents shows a good in vitro activity against Candida spp. except Candida parapsilosis. The value of these in vitro results as predictors of therapeutic outcome is to be established in clinical trials.
P1155: Synergism of micafungin with voriconazole against clinical Aspergillus, Fusarium and Scedosporium spp.
K. Heyn, A. Tredup, S. Salvenmoser, F.-M. Müller (Heidelberg, D)
Objectives: The combination of Micafungin (MCF) and Voriconazole (VRC) against 100 clinical isolates of Aspergillus fumigatus, flavus, niger and nidulans, Fusarium solani as well as Scedosporium apiospermum and prolificans was analysed by in vitro checkerboard analysis. As the drugs have a different mode of action, it can be expected that their combination may be synergistic.
Methods: The interactions have been evaluated by in vitro checkerboard analysis with determination of FIC indices. The spectrophotometric reading has been performed by 50% growth inhibition (MIC-2) using XTT colorimetric method. The in vitro drug interactions were calculated on the basis of fractional inhibitory concentrations (FIC) index.
Results: Synergism, was observed for 64% of all tested isolates. 80% of A. fumigatus strains showed synergism. Also for S. prolificans, a pathogen with enhancing frequency of occurrence, which causes various types of human infections with high mortality rates, 75% synergistic effects were found. When synergy was not achieved (36% of the isolates), there was still a decrease in the MIC-2 of one or both drugs used in the combination (indifference 0.5 > FIC index < 4). One the basis of the single drug MIC-2s (VRC 0.35 μg/ml, MCF 44.66 μg/ml) for all filamentous fungi we observed that in combination just 32% of VRC (0.11 μg/ml) and 7% of MCF (3.04 μg/ml) is sufficiently to reach the same inhibition. Taking into account the values for the FIC indices, the majority of all indifferent FIC indices were close to the cut-off from synergism to indifference. To clarify this effect, for example F. solani, the FIC index averages 0.5005. None of the isolates yielded antagonistic effects (FIC index > 4). We also investigated significant reductions in the MIC50 and MIC90 values. For VRC the MIC50 and MIC90 of all filamentous fungi reduced from 0.125 and 0.5 μg/ml to 0.03125 and 0.25 μg/ ml and for MCF from 2 and 256 μg/ml to 0.0625 and 8 μg/ml, respectively.
Conclusion: Combination of VRC and MCF demonstrated synergism in the majority of the strains. This study demonstrates that the in vitro activity of both drugs can be enhanced by using them in combination. Their relative lack of toxicity also makes them an attractive option as add-on therapy. Clinical trials to investigate the effectiveness of MCF combined with VRC are warranted.
P1156: Effect of media composition and in vitro activity of new antifungal agents against zygomycetes
C. Gil-Lamaignere, R. Hess, S. Salvenmoser, K. Heyn, R. Kappe, F.-M. Müller (Heidelberg, Erfurt, D)
Objectives: Despite antifungal therapy, mortality in disseminated zygomycosis is still too high. We analysed the in vitro activity of Posaconazole (POS), Voriconazole (VRC) and Caspofungin (CAS) against 59 strains of the genera Rhizopus, Mucor, Absidia, and Cunninghamella in different media compositions.
Methods: The following five media compositions were compared: RPMI 1640 ± 2% glucose, AM3 ± 2 % glucose and HR-Medium. MICs were determined by microdilution method following NCCLS guidelines with minor modifications. Each well was read visually, the growth in each well was compared with the growth control. Two endpoints were evaluated for each drug: an inhibition of growth >90% war recorded as MIC1 and an inhibition of growth >50% was recorded as MIC 2. The final concentrations of the antifungal agents were 0.015–8 mg/l for POS and VRC, and 0.03–16 mg/l for CAS.
Results: POS was significantly more active than CAS and VOR, both in R + G and in HR media (P < 0.05 when comparing the MIC1 of POS in HR medium to that of VRC; P < 0.001 for all other comparisons). Growth in RPMI and AM3 media supplemented with glucose was more robust than in the corresponding media lacking glucose. Glucose had little influence on MIC values. The agreement when comparing the MIC1 evaluated in AM3 ± glucose was > 85%, while the use of MIC2 endpoint yielded 100% agreement for all genera. When comparing the data obtained in RPMI ± glucose to that in HR, the agreement was good. The percentage agreements using the MIC2 and MIC1 endpoints were 100% and > 70%, In contrast, the agreement between AM3 ± glucose and the other media was generally poor. Moreover, the average MICs obtained in AM3 medium were lower than those obtained in either HR or RPMI which was due to a difference among genera.
Conclusions: Our results suggest the following: a) POS is active in vitro against zygomycetes at clinically relevant concentrations. b) within zygomycetes, there are differences between genera in terms of their antifungal susceptibilies. c) growth medium is an important variable for MIC determination in zygomycetes, and the more relevant medium appears to be RPMI supplemented with 2% glucose.
P1157: Effect of micafungin against biofilm of six different Candida spp.
M. Seidler, S. Salvenmoser, F.-M. Müller (Heidelberg, D)
Objectives: Patients with peripheral vein and implanted catheters (e.g. Hickman catheters) have an increased risk for development of candidaemia and invasive candidasis. Candida spp. attach on polymers, create a biofilm protecting the yeast and pose a reservoir for entering the bloodstream. Candida spp. in biofilm are less susceptible to the antifungal drugs currently in use. We investigated the in vitro antifungal activity of Micafungin (MCF) against biofilms of C. albicans, C. parapsilosis, C. dubliniensis, C. tropicalis, C. glabrata and C. kefyr.
Methods: Biofilm formation was performed in vitro on polystyrene 96-well plates and on Hickman catheter discs with minor modifications to Kuhn (1). MCF was tested at six concentrations (0.25–32 μg/ml). Measurements were done by XTT reduction assay at 490nm, % inhibition was calculated in comparison to the growth control. The biphasic structure of biofilms were imaged by reverse light-through microscopy.
Results: On polystyrene plates and on Hickman catheters all Candida spp. produced intermediate biofilm after 24–48h incubation. At all concentrations on polystyrene plates Micafungin reached at maximum 50% inhibition in biofilm against all Candida spp.: C. albicans (47% at 16 μg/ml), C. parapsilosis (49% at 16 μg/ml), C. dubliniensis (42% at 16 μg/ml), C. tropicalis (28% at 16 μg/ml), except for C. glabrata (73% at 8 μg/ml) and C. kefyr (53% at 1 μg/ml). At max. concentration (16 μg/ml) on Hickman catheter discs Micafungin reached at maximum 80% inhibition, except for C. glabrata (84% at 8 μg/ml).
Conclusion: Micafungin is in vitro more active against Candida biofilm on Hickman catheter discs in comparison to polystyrene plates, but 100% inhibition cannot be reached at all. Further investigations are required to assess combinations of different antifungals for increased antifungal activity in biofilm. Ref. 1 Kuhn DM et al. (2002) AAC 46(6):1773–80
P1158: Caspofungin resistant C. glabrata
K.J. Dodgson, A.R. Dodgson, C. Pujol, S.A. Messer, D.R. Soll, M.A. Pfaller (Iowa City, USA; Manchester, UK)
Objectives: Here we describe first clinical case of a caspofungin resistant C. glabrata infection. The patient was a 43 year old male with AML. He received a matched unrelated HSCT, 9 months prior to his death. He had a complicated hospital course which included C. glabrata sepsis. C. glabrata was cultured from his stool, from the time of transplant to death. Initial blood culture isolates were azole resistant and Amphotericin B was started. This was stopped due to renal insufficiency and caspofungin was started (MIC 0.12 μg/ml). He had a prolonged duration of therapy which comprised of alternating courses of IV voriconazole and caspofungin. Four months after initial fungaemia C. glabrata was cultured which was
Table for 1159 both caspofungin resistant (MIC > 8 μg/ml) and azole resistant. Despite the addition of amphotericin B the patient died 8 weeks later. C. glabrata was isolated from the bone marrow at autopsy.
Methods: The series of patient isolates, from time of transplant to death, had susceptibilities performed as per NCCLS document M27-A. The isolates were typed using Cg6 probe and MLST.
Results: he susceptibilities demonstrated caspofungin resistance in the blood isolate (> 8 μg/ml) and azole resistance in all but a few of the initial stool isolates. All the isolates were shown to be identical by Cg6 and were determined to be MLST group 1, which has previously been shown to be the most prevalent clade of C. glabrata worldwide.
Discussion: This describes the first caspofungin resistant clinical isolate of C. glabrata. It has been recently reported in C. albicans. This data details an isolate that has developed resistance in the presence of therapy. Resistance to caspofungin is not common and is thought to be due to mutations in the beta-1–3-glucan synthase (FKS) gene. There are 3 FKS genes in C. glabrata. Preliminary sequencing data of one of these genes has so far revealed no non-conservative mutations. The 2 remaining genes are yet to be sequenced and the presence of other mechanisms cannot be ruled out.
P1159: Deoxycholate amphotericin B and its lipid formulations enhance antifungal activity of human neutrophils against hyphae of Apergillus fumigatus and Fusarium solani
J. Dotis, M. Simitsopoulou, M. Dalakiouridou, T. Konstantinou, T.J. Walsh, E. Roilides (Thessaloniki, GR; Bethesda, USA)
Objective: Innate immune response is critical in the antifungal host defense against invasive aspergillosis and fusariosis, and neutrophils (PMNs) constitute an important component of it. We studied the effects of deoxycholate amphotericin B (DAMB) and its lipid formulations liposomal amphotericin B (LAMB), lipid-complex (ABLC) and colloidal-dispersion (ABCD) on antifungal activity of human PMNs against hyphae of Aspergillus fumigatus and Fusarium solani.
Methods: PMNs were isolated from healthy donors by dextran sedimentation/Ficoll centrifugation. They were incubated with no drugs, 1 or 5 mg/L DAMB and 5 or 25 mg/L LAMB, ABLC and ABCD at 37°C/5% CO2 for 2h. Hyphae of A. fumigatus and F. solani germinated after incubation of conidial suspensions in YNB for 17 h at 32°C and 25°C respectively, were added at an effector:target (E:T) ratio 5:1 or 10:1. After 2 h, PMN-induced hyphal damage was assessed using the XTT colorimetric assay at 450 nm. Statistical analysis was performed using ANOVA with Dunnett test for multiple comparisons.
| % damage of A. fumigatus hyphae (n = 6) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| (mg/L) DAMB |
LAMB |
ABLC |
ABCD |
||||||
| E:T ratio | PMNs only | 1 | 5 | 5 | 25 | 5 | 25 | 5 | 25 |
| 5:1 | 19.04 ± 2.33 | 58.31 ± 10.06** | 86.84 ± 2.44** | 43.99 ± 4.76** | 68.88 ± 3.7** | 65.43 ± 2.98** | 77.69 ± 3.33** | 62.11 ± 3.88** | 75.53 ± 2.83** |
| 10:1 | 23.75 ± 2.52 | 66.37 ± 5.79** | 90.35 ± 1.18** | 58.54 ± 1.69** | 78.23 ± 3.48** | 73.07 ± 2.89** | 79.22 ± 2.33** | 70.36 ± 2.9** | 77.14 ± 2.05** |
| %damage of F. solani hyphae (n = 8) | |||||||||
| 5:1 | 12.18 ± 2.51 | 47.68 ± 5.91** | 90.69 ± 2.12** | 34.85 ± 4.88** | 66.41 ± 3.94** | 41.77 ± 5.92** | 43.73 ± 5.33** | 32.79 ± 5.26 | 47.75 ± 2.82** |
| 10:1 | 22.26 ± 4.09 | 51.60 ± 3.38** | 96.05 ± 1.96** | 42.99 ± 3.37* | 84.24 ± 2.72** | 58.71 ± 3.52**** | 60.34 ± 4.83** | 43.36 ± 6.96* | 59.73 ± 5.91** |
Results: They are summarized in the table (*p < 0.05, **p < 0.01). No decrease of PMN viability was induced by the drugs at the concentrations used. All amphotericin B formulations at both concentrations resulted in significant increases of PMN-induced damage of A. fumigatus hyphae at 5:1 and 10:1 E:T ratios as compared to untreated PMNs (p < 0.01). Similar increases were induced by all amphotericin B formulations when pre-treated PMNs were incubated with F. solani hyphae (p < 0.05), except for ABCD-pretreated PMNs at 5 mg/L and 5:1 ratio where a tendency of increase was shown. DAMB 5 mg/L exerted the highest increase in PMN-induced hyphal damage against both fungi (p < 0.01).
Conclusion: Both deoxycholate and lipid amphotericin B formulations enhance the damage induced by human PMNs on hyphae of A. fumigatus and F. solani. DAMB appears to show the highest enhancement among them. These immunomodulatory effects of amphotericin B formulations on PMN antifungal activities against the two filamentous fungi may be important in the antifungal therapy of invasive aspergillosis and fusariosis in immunocompromised patients.
P1160: Species distribution and antifungal susceptibility in yeast isolated from peritoneal fluid over a period of 17 years
J. Martínez-Alarcón, M.J. Goyanes, T. Peláez, L. Alcalá, J.V. Guinea, M.A. Fernández-Chico, E. Bouza (Madrid, E)
Background: Yeast pathogens are uncommon isolates in the setting of peritonitis. Most cases of fungal peritonitis due to yeasts are caused by Candida species, although other yeasts have occasionally been reported.
Objectives: To study the evolution of peritonitis due to yeasts, its distribution by species and its antifungal susceptibility in our hospital over the last 17 years.
Methods: Retrospective study for the period January 1988 to October 2004 of all the episodes of yeast peritonitis diagnosed in our microbiology lab. The in vitro activities of amphotericin B (AB), fluconazole (FZ), itraconazole (IZ), ketoconazole (KZ), voriconazole (VZ), and flucytosine (FC) were determined by the broth microdilution method following NCCLS criteria.
Results: A total of 510 peritoneal fluids, from 349 patients, showed positive yeast growth (560 isolates). The peritonitis rates per 100.000 patient admissions during the two periods of study were respectively: 32.8 (1988–1995) and 50.6 (1996–2004) (p < 0.005). Globally,
Candida albicans was the most frequently isolated yeast (313. 55.9%) followed by C. glabrata (78; 13.9%), C. parapsilosis (63; 11.3%), C. tropicalis (44. 7.9%), C. krusei (19. 3.4%) and others (43. 7.7%). The species distribution in both the adult and paediatric population was respectively as follows: C. albicans (59.2%/39.1%), C. glabrata (16.5%/1.1%), C. tropicalis (7.1%/12%), C. parapsilosis (5.1%/42.4%), C. krusei (4.1%/0%) and others (8.1%/5.4%). C. parapsilosis was the specie most frequently isolated from paediatric patients (42.4%), whereas C. albicans was the most isolated in adult patients (59.2%). Number of isolates tested, and MIC90 of AB, FZ, IZ, KZ, VZ and FC (mcg/mL) were as follows: 102 C. albicans (0.06, 0.25, 0.06, 0.016, 0.008, 0.125), 29 C. glabrata (0.125, 16, 1, 1, 0.5, 0.06), 30 C. parapsilosis (0.125, 1, 0.125, 0.125, 0.016, 0.125), 19 C. tropicalis (0.125,1,0.25,0.25,0.06,0.25) and 6 C. krusei (0.125,64,0.5,1,0.25,8).
Conclusions: In our hospital, peritonitis due to yeasts increased significantly during the study period. The species distribution was different between the adult and paediatric population. In adult patients, C. albicans was the most isolated species, with C. parapsilosis as the most important in children.
P1161: Biofilm production and antifungal susceptibility patterns of Candida species isolated from hospitalised patients
M. Demirbilek, F. Timurkaynak, F. Can, O. Kurt Azap, H. Arslan (Ankara, TR)
Objectives: The aim of this study was to investigate the production of slime factor among Candida species which were isolated from hospitalized patients. Another aim of this study was to see in vitro activities of antifungal agents and to compare these results with slime production.
Methods: Total 116 Candida spp (79 C. albicans and 37 nonalbicans Candida spp) isolated from various specimens were included to the study. Fluconazole, itraconazole, amphotericin B and caspofungin susceptibilities of these strains were determined by broth microdilution method according to NCCLS M27-A2 standards. Biofilm production of Candida spp. was determined by microplate method on polystyrene microtiter plates using Brain Heart Infusion broth supplemented with 0.25% Glucose as a growth medium.
Results: Caspofungin and amphotericin B was the most active agents which MIC90 values 1mg/ml and 0.5 mg/ml respectively. Fluconazole resistance (MICs > 64) was obtained from 24 of the isolates (21%). Biofilm formation was detected in 33 of the total strains (28%). Statistically important difference (p < 0.05) was determined between the biofilm production of C. albicans (21.5%) and nonalbicans species (%48.4). Significant correlation between biofilm production and amphotericin B MIC values was established (p < 0.05)
Conclusion: Candida species are one of the most important etiologic agents of catheter related infections especially biolfilm producing strains. This study showed us biofilm production rates are too high particularly in non-albicans strains. This will explain the rising incidences of non albicans strains especially C. parapsilosis in serious infections. Our study also implicated that the MIC values amphotericin B which was one of the most active agent against Candida infections had a significant correlation with slime production. This will be a problem in treatment of slime producing Candida infections with this drug.
P1162: Update on susceptibility profile of clinical isolates of Scedosporium species, Spain 2004
M. Cuenca-Estrella, A. Gomez-Lopez, E. Mellado, A. Monzon, J. Rodriguez-Tudela (Majadahonda, E)
Objectives: Scedosporium spp. are quite common as agents of invasive mycoses at Spain. Mycology Reference Laboratory has conducted retrospective surveillance for Scedosporium infections during last five years. We have analysed the antifungal drug susceptibility profiles of these species and proportion of resistance among the isolates.
Methods: A collection of 135 clinical isolates was tested. All strains were recovered during a period of five years (2000–2004) from 38 Spanish hospitals. Each clinical isolate represented an unique isolate from a patient. Clinical isolates were identified by routine procedures. A broth microdilution test was performed by following the NCCLS reference method, document M-38A. Antifungal drug tested were amphotericin B (AMB), itraconazole (ITC), voriconazole(VRC), posaconazole(POS) and terbinafine(TBF). Aspergillus flavus ATCC 204304 and Aspergillus fumigatus ATCC 204305 were used as reference strains for susceptibility testing.
Results: Table displays MIC ranges, MIC geometric means (GM), and MICs including 50% (MIC50) and 90% (MIC90) of isolates in mg/L, classified per species:
| Species (No of isolates) | AMB | ITC | VRC | POS | TBF | |
|---|---|---|---|---|---|---|
| S. apiospermum (N = 69) | Range | 1.0–32.0 | 0.5–16.0 | 0.12–16.0 | 0.25–16.0 | 8.0–32.0 |
| GM | 4.7 | 3.7 | 0.9 | 1.3 | 17.1 | |
| MIC50 | 4.0 | 8.0 | 1.0 | 1.0 | 8.0 | |
| MIC90 | 16.0 | 16 0 | 8.0 | 8.0 | 32.0 | |
| S. prolificans (N = 66) | Range | 2,0–32.0 | 8.0–16.0 | 8.0–16.0 | 8.0–16.0 | 8.0–32.0 |
| GM | 12.8 | 9.6 | 9.4 | 10.5 | 19.2 | |
| MIC50 | 16.0 | 8.0 | 8.0 | 16.0 | 16.0 | |
| MIC90 | 32.0 | 16.0 | 16.0 | 16.0 | 32.0 |
Conclusions: (i) Scedosporium spp. carry on with high MICs of antifungal agents, even for new antifungal agent as POS. (ii) S. prolificans is a multi-resistant organism. (iii) S. apiospermum is resistant to ITC and TBF, but 15% of strains are susceptible in vitro to AMB (MIC < 2 mg/L), 75% to VRC (MIC < 2 mg/L), and 60% to POS (MIC < 2 mg/L). (iv) These findings reinforced the need of continued surveillance programmes that analyze antifungal susceptibility profiles of medically important fungal isolates.
P1163: Assessing susceptibility of fungi isolated from hospital environment to disinfectants
M. Staniszewska, B. Tadeusiak, W. Kurztkowski, B. Jakimiak, E. Rohm-Rodowald (Warsaw, PL)
Objectives: The hospital infection control including prevention and killing of environmental pathogenic microorganisms with the application of properly designed disinfecting procedures and adequate chemical disinfectants, belongs to basic duties of hospital management. In this study the sensitivity of yeasts and dermatophytes to disinfectants was determined. Two agents were assayed through out the study as following: I (99% sodium dichloroisocyanurate: 1.5 g active chlorine in tablet); II (9.5 % glutaraldehyde, 7.5% glyoxal, 9.6 % didecylodimethylammonium chloride). Seventeen clinical strains of Candida albicans and Epidermophyton floccosum, Microsporum canis, Trichophyton rubrum, Trichophyton mentagrophytes, Scopulariopsis spp. were used.
Methods: Phase I – qualitative suspension test method (National Institute of Hygiene, Poland) was used. Antifungal activity on C. albicans and dermatophytes was evaluated by determination of the MIC. Observation of the inhibition or destruction of invasive form development and spores were studied with the use of phase – contrast microscopic techniques. Phase II – carrier test methods: qualitative (NIH) and quantitative European Standard EN 13697 were applied.
Results: MIC values assessed in this study were independent of places where the disinfectants were applied. Noticeable inhibition of the growth of dermatophytes was observed with MIC values ranging (mg/l): I–100 to 120; II – 0.012 to 0.02. In case of C. albicans MIC values ranging (mg/l): I–140 to 160; II–0.0005 to 0.012 were obtained. The comparison of fungal suspension treated with chemical agents and control suspension at direct microscopic count showed significant reduction of the amount of cells. The investigation of the second phase showed the activity of disinfectants: I (1000 mg/l, 15 min) and II (1% and 2%, 15 min) to fungal pathogens. Disinfectants in used parameters showed activity to fungi in the place of application.
Conclusion: Those studies revealed that investigated strains showed different susceptibility to disinfectants. Strains of Candida albicans demonstrated significantly higher resistance to chlorine compounds than dermatophytes but more sensitivity to aldehydes. Using proper disinfectant in clinical environment is an essential tool in eradication of fungal infection.
Skin and soft tissue infections
P1164: Bacteriologic efficacy of meropenem versus imipenem-cilastatin for the treatment of patients with complicated skin and skin structure infections
J. Iaconis, N. Soto, P.J. Turner (Waltham, Wilmington, USA; Macclesfield, UK)
Objectives: In a recent multicentre, double-blind study, the broad-spectrum carbapenem, meropenem (MEM), had comparable efficacy to imipenem-cilastatin (IPM) in patients with complicated skin and skin structure infections (cSSSI). This study presents the clinical and bacterial response rates for MEM and IPM in the subgroup of microbiologically documented infections.
Methods: This multicentre, randomized, double-blind study compared MEM with IPM (both 500 mg IV every 8 hours) in patients hospitalized with cSSSI. The primary efficacy endpoints were clinical and bacteriological responses at follow-up in the fully evaluable (FE) patient population (all patients meeting eligibility criteria and who had an identified pathogen prior to treatment). Subgroup analysis was conducted in patients with polymicrobial infections.
Results: Of the 1037 patients enrolled and treated in the trial, 440 comprised the FE population. Of all the pretreatment pathogens isolated, the majority were aerobic Gram-positive organisms (827/1444; 57%) followed by aerobic Gram-negative organisms (378/1444; 26%) and anaerobic organisms (239/1444; 17%). Polymicrobial infections were seen in 38% of all documented infection. Gram-positive pathogens included 402 Staphylococcus aureus isolates, (284 methicillin-susceptible [S; 100% to MEM and IPM], 118 methicillin-resistant [excluded from FE analyses]), Streptococcus pyogenes (n = 89, 100% S to MEM and IPM), S. agalactiae (n = 59; 100% S to MEM and IPM), and E. faecalis (n = 52; 82% S to MEM and 100% S to IPM). Aerobic Gram-negative and anaerobic organisms included Escherichia coli (n = 64, 100% S to MEM and IPM), Proteus spp. (n = 52; 100% S to MEM and IPM), Pseudomonas aeruginosa (n = 53; 94% S to MEM and 92% S to IPM), Bacteroides spp. (n = 74; 97% S to MEM and 100% S to IPM), and Peptostreptococcus spp. (n = 63; 100% S to MEM and IPM). Satisfactory clinical (cure or improvement) response rates were 88.5% (MEM) and 83.1% (IPM) in the FE group, and 87.3% (MEM) and 81.2% (IPM) in patients with polymicrobial infections; bacteriological (documented or presumed eradication, colonization) response rates were 79.4% (MEM) and 79.2% (IPM) in the FE group, and 78.5% (MEM) and 72.9% (IPM) in the polymicrobial infection group.
Conclusion: In patients with cSSSI and documented infection (including polymicrobial infections), MEM (500 mg IV every 8 hours) had comparable clinical and bacteriological efficacy to IPM (500 mg IV every 8 hours).
P1165: Molecular typing of Hungarian Streptococcus pyogenes isolates
B. Krucsó, K. Csiszár, M. Gacs, J. Pászti (Budapest, Salgótarján, HUN)
Objectives: The aim of the authors was the examination of the genetic relatedness of the Hungarian Streptococcus pyogenesclinical isolates by emm amplicon characterisation and PFGE analysis, as well as the determination of the prevalent emm types among the strains originated from different infections.
Methods: From 2003 to 2004 40 S. pyogenes strains were isolated from two Hungarian counties. Out of the isolates, 15 originated from respiratory, 17 from superficial pyogen, and 8 from invasive infections, like Streptococcal shock syndrome (STSS), meningitis and sepsis. emm gene detection and restriction analysis of the emm amplicon (with HincII and HaeIII; DdeI enzymes) was performed in all strains. The sequence of the emm amplicon from all invasive isolates and from one strain of all RFLP groups was determined, and macrorestriction chromosomal analysis by PFGE (Pulsed Field Gel Electrophoresis) method for these isolates was also performed.
Results: As a result of the restriction analysis of the emm amplicons 17 restriction patterns were differentiated. Most emm types were standard types: emm 1.0, emm12.0, emm 28.0, emm59.0, emm66.0, emm75.0, emm76.0, emm77.0, emm 80.0, emm 81.1, emm84.0, emm110.1, emm118.0, plus one new allelic variant (emm 110.2) was identified. Moreover, two GAS strains had a type (stg6 and stg485) previously found in group G streptococci. The emm types varied among the isolates originated from different sources. The next emm types were identified among the invasive isolates: emm 1.0, emm 28.0, emm 66.0, emm 80.0, emm 81.1, emm84.0, stg6. Some emm type could be further differentiated into several PFGE genotypes, and within a PFGE genotype different emm types could be observed.
Conclusions: This report provides epidemiological information from a geographic area has not been examined by emm characterisation. PFGE and emm type analysis showed high genetic diversity among the 40 GAS strains. The most frequent emm types were emm1.0, emm28.0, emm 81.1 and emm84.0 in the two counties.
P1166: Molecular characterisation of group A streptococci from invasive disease episodes in Poland
K. Szczypa, E. Sadowy, R. Izdebski, L. Strakova, W. Hryniewicz (Warsaw, PL; Prague, CZ)
Objectives: The past decade has witnessed a worldwide increase in serve invasive GAS infections. These rapidly progressive infections are associated with high mortality rates despite prompt antimicrobial therapy. The aim of this study was to characterize GAS isolates causing severe invasive disease in different regions of Poland by emm-typing, multilocus sequence typing (MLST), PFGE, virulence genes distribution and their susceptibility to antimicrobial agents.
Methods: A total of 42 GAS isolates from blood (54.7%), pus (33.3%), sputum (7.1%), peritoneum fluid (4.7%) and other sources were examined. Susceptibility to penicillin, erythromycin, clindamycin, telithromycin, tetracycline, levofloxacin, chloramphenicol, quinupristin/dalfopristin and linezolid was determined by the microdilution method according to the NCCLS guidelines. Clonality of all isolates was studied by emm typing, PFGE of Sma I-restricted bacterial DNA as well as MLST. The strains were also tested for the presence of speA, speB, speC, speF and ssa genes by PCR.
Results: Resistance to erythromycin was found in four isolates (9.5%), two of them exhibited the iMLSB and two the cMLSB phenotype. Twenty-one (50%) and five (11.9%) were resistant to tetracycline and chloramphenicol, respectively. All tested isolates were fully susceptible to penicillin, levofloxacin, quinupristin/ dalfopristin and linezolid. Twenty different emm types were detected, of which emm1 (23.8%) and emm12 (21.4%) were most common, followed by emm85, emm60 and emm81. All emm1 types and emm12 types corresponded to the ST28 and ST36, respectively. Altogether, 24 different PFGE patterns, designated A–Y were discerned among the isolates, with two predominant profiles A (n = 10) and B (n = 9). Our study showed that all isolates possessed speB and speF genes, while the frequencies of speC and speA were 59.5% and 26%, respectively.
Conclusion: Two clones predominated among GAS strains causing severe invasive disease in Poland; these clones were of emm type 1 and 12.
P1167: Characterisation of methicillin-resistant Staphylococci in Ulaanbaatar, Mongolia
D. Orth, K. Grif, L. Erdenichemeg, B. Strommenger, C. Cuny, G. Walder, C. Lass-Flörl, M.P. Dierich, W. Witte (Innsbruck, A; Ulaanbaatar, MNG; Wernigerode, D)
Objectives: Methicillin-resistant Staphylococcus aureus (MRSA) has become one of the most prevalent nosocomial pathogen throughout the world, capable of causing a wide range of hospital infections. This study was aimed to characterize the Mongolian MRSA by antibiotic susceptibility patterns and molecular genotyping.
Methods: Strains of S. aureus were collected from various sites of patients from four different medium-sized university hospitals of Ulaanbaatar city (Mongolia), in 2000–2002. The study included two hundred seven strains of S. aureus. Susceptibility testing was performed by disk diffusion according to National Committee for Clinical Laboratory Standards guidelines. All strains were screened by polymerase chain reaction for the presence of the mecA gene. Molecular genotyping was performed using automated ribotyping with EcoRI as restriction enzyme and PFGE with SmaI as restriction enzyme.
Results: Among the 207 S. aureus 6 isolates (2.9%) were positive for the mecA gene by PCR. All of the 6 MRSA strains were resistant to oxacillin, susceptible to amikacin, vancomycin, teicoplanin, fucidic acid and rifampicin. Only one isolate was intermediate-resistant to gentamicin, tobramycin and trimethoprim-sulfamethoxazole. Three of the 6 MRSA strains were intermediate resistant to ciprofloxacin. Five of the 6 isolates were resistant to erythromycin and all were resistant to tetracycline and chloramphenicol. Three of the 6 MRSA isolates were of MLST St 154, possessed a SCC-mec element of type IV c and the determinant for Panton-Valentine Leukocidin (lukS-lukF). The remaining 3 MRSA isolates exhibited MLST ST 239, contained a SCC-mec element of type III and were lukS-lukF negative. Automated ribotyping as well as PFGE divided the 6 MRSA strains into 4 different types, three strains showed unique patterns using both typing methods.
Conclusion: The limited use of antibiotics in Mongolia is assumed to be the reason for the low rate of MRSA found in Mongolian hospitals and for their susceptibility against most antibiotics. Molecular typing indicates that on one hand ‘old’ MRSA (ST 239) are still prevailing in Mongolia and that a cMRSA until now described for Sweden had been spread to Mongolia (ST 154).
P1168: First report of Staphylococcus aureus with reduced susceptibility to vancomycin (VISA) in Denmark
A. Sandberg, A. Bolmström, R. Skov (Copenhagen, DK; Solna, S)
Objective: Are VISA/hVISA isolates present among MRSA isolates in Denmark?
Methods: All MRSA isolates in Denmark are referred to the Staphylococcus reference laboratory at Statens Serum Institute. From January 1st 2003 to October 31st 2004 a total of 576 isolates were screened by the Etest macromethod for VISA/hVISA. i.e. each isolate was plated on Brain Heart Infusion agar (BHI, Difco) using a McFarland 2.0 inoculum, vancomycin (VA) and teicoplanin (TP), Etest was applied and the isolates were incubated for 48 h in ambient air (Walsh et al, JCM, 2001). VA and TP MIC > 6 mg/L or TP MIC > 8 mg/L was used as the screen interpretive criteria for hVISA/VISA phenotype. Screen positive isolates were verified by population analysis profiles (PAP) using BHI with 0, 0.5, 1, 2, 2.5, 4, 8 and 16 mg/L VA. These isolates were also MIC tested by the standard Etest method, and NCCLS broth microdilution (BMD). Agar screen with 4 and 6 mg/L VA and betalactam+VA antagonism for ampicillin, cefoxitin, cefaclor, cefo-taxime, ceftazidime and imipenem using Etest on BHI plate ± VA 2 mg/L was also done. Presence of the vanA and vanB gene was investigated by PCR.
Results: 15 potential hVISA/VISA isolates were found by the Etest macro-method. Four isolates had hVISA and one had VISA phenotype by PAP and none of them were positive for the vanA and vanB gene. The betalactam+VA antagonism test was positive for all four isolates. Agar screen, BMD and standard Etest did not reliably detect the hVISA isolates. Four patients acquired the isolates outside Denmark and it appears that cross infection occurred in Denmark in the fifth case.
Conclusion: This is the first report of VISA and hVISA isolates in Scandinavia. Standard MIC methods including the NCCLS reference do not reliably detect these isolates and specialised VISA/hVISA phenotypic tests are necessary. Etest macromethod was easy to perform and efficiently detected the VISA/ hVISA strains. In one hVISA case, there is evidence for cross infection in Denmark.
P1169: Actinomyces spp.: a disregarded pathogen?
S. Palombarani, M. Almuzara, K. Bombicino, H. Rodriguez, E. Bertona, A. Famiglietti, C. Vay (Buenos Aires, RA)
We present 45 Actinomyces spp isolations, their identification to a species level and their clinical sources. In addition, we perform susceptibility testing of 23 of those strains to 13 drugs. The identification of Actinomyces spp was done taking into account their cultural features, growth's atmosphere and biochemical and enzimatical tests, according to schemes proposed by Sarkonen N., Funke G., Moncla B., Hillier S., and Bernard K. We studied too, the clinical sources of Actinomyces spp, if they were isolated lonely or in association with mucosa's normal flora. The susceptibility testing was performed by the agar dilution method, with Mueller Hinton agar supplemented with 5% sheep blood. The reading of minimum inhibitory concentration (MICs) were done after 48 hours incubation at 37°C in at atmosphere enriched with CO2. All strains were grown at 37°C on sheep blood agar plates with CO2 added. A. radingae, A. europaeus, and A. odontolyticus were the most frequent isolated species (7 each one) followed by A. israelii, A. graevenitzii, A. turicensis and A. viscosus. In 27 isolations, Actinomyces spp were recovered as sole microorganism, and in the 18 remainder, in association with mucosa's normal flora. There were not relations between Actinomyces species and the clinical sources of the samples. MICs for penicilin, ampicilin and cefotaxime were from <0.016 to 0.25 μg/ml. There was a bimodal behaviour with macrolides: erythromycin, azithromycin and clarithromycin (MICs from 0.032 to 128 μg/ml) and the same was observed with quinolones: levofloxacin, ciprofloxacin and moxifloxacin (MICs from 0.032 to 8 μg/ml). All isolations presented MICs for vancomycin <0.125 μg/ml. The identification of the Actinomyces genus presents diagnostic difficulties due to its growth requirements. Some species are not so infrequent, and the sources from which they are recovered suggest that they may be of clinical relevance, for they are often isolated as sole pathogen.
P1170: Isotretinoin versus tetracycline: a comparative study with regard to efficiency in the treatment of acne vulgaris
C. Oprica, L. Emtestam, C.E. Nord (Stockholm, S)
Tetracyclines are most commonly used for treatment of moderate and severe inflammatory acne, and systemically administered isotretinoin has proved to be the most efficient treatment, used in patients with moderate or severe acne that fails to respond to other therapies.
Objectives: A randomized clinical trial was conducted to compare the clinical efficacy and the antimicrobial susceptibility of Propionibacterium acnes strains isolated before, during and after treatment with either tetracycline or isotretinoin in patients with acne vulgaris.
Methods: 52 male and female patients, 15–35 years of age, with moderate or severe acne, were randomized into two groups of 26 patients each. They received oral tetracycline hydrochloride 1 gram/day together with topical retinoid (differine gel 0.1%) or isotretinoin (Roaccutane) 1 mg/kg/day. The therapy was given for a 6-month period. Clinical evaluation (Leeds acne grading system and lesions counting) and bacterial samples were taken before the treatment started, during the treatment and 2 months after the treatment had stopped. Dermatology Life Quality Index questionnaire was completed by patients before and after treatment, in order to determine impairment of life quality.
Results: Acne severity was significantly reduced by both regimens during therapy, and patients in the isotretinoin group continuously improved the acne scores after the treatment had stopped. After 6 months of treatment, isotretinoin produced greater lesion reductions than tetracycline. The mean per cent reduction in the different lesion counts was as follows: 83% versus 45% for non-inflammatory lesions (p < 0.01) and 80% versus 56% for inflammatory lesions (p < 0.01) in isotretinoin or tetracycline group, respectively. In the drug-free period, the group of patients treated with isotretinoin presented significantly less inflammatory lesions compared to the group treated with tetracycline (p < 0.001). Both treatments had improved the life quality (p < 0.01), independent of acne severity. Resistant P. acnes strains were isolated after treatment in both the tetracycline group (53%) and isotretinoin group (25%).
Conclusions: Both treatments were effective during treatment period. More resistant strains were recovered from the tetracycline group.
P1171: Psoas abscesses. Differences between pyogenic and tuberculous abscess
F.J. Fernández-Fernández, J. de la Fuente-Aguado, S. Pérez-Fernández, L. Vázquez-Tuñas, B. Sopeña-Pérez Argüielles, C. Martínez-Vázquez (Vigo, E)
Objectives: To compare the demographic characteristics, clinical features, laboratory, microbiologic and imaging data, therapeutic options and outcome of pyogenic and tuberculous psoas abscesses.
Patients and methods: Retrospective descriptive study of the medical records of the patients diagnosed of psoas abscess in our institution, in the period between January/1994 and october/2004.
Results: In this period 14 patients were diagnosed of psoas abscess, all of them secondary to a adjacent source of infection. Nine patients had pyogenic abscess, and M. tuberculosis was the causal microorganism in 5 patients. In 3 patients there were bilateral involvement, and all three were tuberculous abscess. An underlying disease was present in 67% patients of pyogenic abscess, and only in 20% of tuberculous abscess. These one were malignancy, intravenous drug use, cirrhosis, use of steroids, and 3 with inflammatory bowel disease. Patients with tuberculous abscess were younger (37 vs 49 years), and they presented with a longer duration of symptoms from presentation to diagnosis (145 vs 15 days) than patients with pyogenic abscess. Abdominal pain was the most frequent symptom at diagnosis in pyogenic abscess (78%), whereas lumbar pain (80%) was in tuberculous abscess. Other clinical manifestations were similar in both groups. The source of infection in pyogenic abscess was gastrointestinal in 7 patients (4 polymicrobial), and in 1 patient infection of an aortobifemoral bypass and sacroilitis (both caused by S. aureus). All tuberculous abscess were secondary to spondilitis. There were no differences between both groups in analysis or imaging alterations. Culture of the abscess was positive in all cases practised. Drainage was performed in 12 patients (7 percutaneous), without differences in both groups. Clinical improvement was more delayed in patients with tuberculous abscess than in patients with pyogenic abscess (18 vs 10 days). There were no deaths in any group.
Conclusions: Tuberculous psoas abscesses presents in younger patients with lesser underlying diseases and a more prolonged clinical presentation than pyogenic abscesses. These tuberculous abscesses are secondary to spondilitis, usually with bilateral involvement.
P1172: Prevalence of Micro-organisms isolated from wounds of inpatients versus outpatients in a Spanish teaching hospital
E. García-Peñuela, A. Pérez de Ayala, D. Domingo, E. Aznar, T. Alarcón, M. López-Brea (Madrid, E)
Objective: To study the prevalence of microorganisms isolated from wounds of in-patients and out-patients (emergency, consultation and primary care) in a Spanish University Hospital of 500 beds.
Methods: Descriptive retrospective study performed from informatics data obtained in the Microbiology Department of Hospital de la Princesa during January 2000 to December 2003. Culture, isolation, identification and susceptibility were performed following standard recommendations.
Results: The total number of wounds during this period was 3753. From these, 1981 were obtained from in-patients, being positives 1510 (76.22%) resulting a total of 2154 microorganisms. Polimicrobian infection was detected in 543 samples. The specimens of outpatients were 1772, being positives 1328 (74.9%) resulting a total of 1762 microorganisms. In 470 samples more than one microorganisms were detected. Frequency of isolation from in-patient and outpatient were as follows: Staphylococcus aureus (18.1% and 27%), Escherichia coli (13.13% and 7.71%) and Pseudomonas sp. (8.45% and 10%) respectively (p < 0.05). Less frequent microorganisms isolated were Enterococcus faecalis (7.28% and 2.78%), Streptococcus sp. (3.94% and 7.38%), fungi (2.36% and 1.3%) and anaerobes (1.3% and 0.79%) from inpatients and out-patients, respectively.
Conclusions: Positive rates of wounds cultures were similar in both groups.
- Staphylococcus aureus was the most prevalent microorganism, being most frequent in outpatients.
- Among enterobacteria Escherichia coli was the most frequent, followed by Proteus mirabilis.
P1173: Vitamin E as an adjuvant for the therapy of patients with hidradenitis suppurativa
A. Antonopoulou, M. Mouktaroudi, M. Kyriakopoulou, M. Raftogiannis, F. Baziaka, D. Plachouras, H. Giamarellou, E.J. Giamarellos-Bourboulis (Athens, GR)
Objectives: Hidradenitis suppurativa (HD) is a chronic disorder characterized from dilatation of sweat glands and recurrent bacterial infections. Vitamin E was administered in several patients as an antioxidant in an attempt to relieve tissue function probably altered by the locally increased oxidant status.
Methods: Twenty nine patients with HD, 15 male and 19 female, were enrolled over a period of twelve months. All have presented with more than three episodes of bacterial exacerbations for at least two years. A detailed medical history was taken upon first evaluation and patients were examined for areas affected by the disease. They were asked to self-evaluate the severity of their condition on a scale of 1 to 10 (1 representing intact skin and 10 maximum severity). Patients were divided into three groups of treatment: A (n = 6), controls; B (N = 8), vitamin E orally 200 mg bid; and C (N = 15), vitamin E 200 mg tid orally. Patients were withhold from any antimicrobial regime. Patients were followed-up at three-month intervals; they were asked to re-evaluate their condition, and to provide details regarding frequency of relapses before and after the initiation of treatment.
Results: Mean ± SE duration of the disease was 11.7 ± 1.9) years and of involved areas 3.84 ± 035, with axillas and groin being involved in the majority of cases. Mean interval between exacerbations before initiation of therapy with vitamin E was 33.98 ± 9.43 days and after initiation of therapy 91.35 ± 21.64 days (p: 0.042). For group B, mean ± SE time interval between exacerbations before initiation of treatment was 45.00 ± 27.39 days and after initiation of treatment 69.00 ± 38.42 days. For group C, respective values were 36.30 ± 9.42 days and 132 ± 12 days. Mean ± SE of self-evaluation scores before therapy with vitamin E was 9.00 ± 0.71 and 4.33 ± 1.76 for patients of groups B and C respectively. They were 4.75 ± 1.31 and 2.75 ± 1.55 respectively after twelve months of follow-up. The latter changes constituted a significant improvement (p: 0.027).
Conclusion: Vitamin E seems to improve the overall clinical condition of patients with HD substantially. Further placebo-controlled studies are necessary to confirm these results.
P1174: Clonal diversity and toxin genes of Staphylococcus aureus causing infections in a clinical ward over a 12-year period (1992–2003)
S. Pollini, G. Zanelli, A. Sansoni, S. Cresti, C. Cellesi, G.M. Rossolini (Siena, I)
Objectives: S. aureus remains one of the leading bacterial pathogens worldwide, representing a major challenge for antimicrobial chemotherapy. The aim of this study was to evaluate the molecular epidemiology of S. aureus infections observed in an Infectious Disease ward during the past 12 years.
Methods: 38 nonreplicate S. aureus isolates were collected from patients with staphylococcal infections (including food-borne infections, osteomyelitis, skin and soft tissue infections [SSTI], pneumonia, meningitis and bacteraemia/endocarditis; mostly community-acquired) at the Infectious Diseases Clinic, University of Siena, during the period 1st Feb 1992–31st March 2003. All isolates were analysed for antimicrobial resistance, clonal diversity and toxin genes (sea-e, eta-d, tst, lukS-PV and lukF-PV). Susceptibility testing was performed according to the NCCLS guidelines. Clonal diversity was determined by PFGE and by analysis of the coagulase (coa) and protein A (spa) genes polymorphism. Toxin genes were analysed by PCR and restriction mapping.
Results: Most isolates (35, 92%) were methicillin-susceptible (MSSA), while 2 were methicillin-resistant (MRSA, mecA-positive) and 1 borderline. Genotyping revealed a single MRSA clone and remarkable clonal diversity among the MSSA isolates (at least 20 distinct clonal lineages). Several clones (including 6 MSSA and the MRSA clone) were detected over prolonged times (2–8 years). The most prevalent clone was detected over a 8-year period and was exclusively associated with SSTI (mostly bullous impetigo). Toxin genes were overall detected in 87% of isolates, the most frequent being sea (45%), tst (32%) and eta and/or etb genes (29%). Six isolates (all MSSA) harboured the lukS-PV and lukF-PV genes.
Conclusions: MRSA were rare and appeared only since 1997. Significant clonal diversity was observed within MSSA. A significant relationship was observed between toxin production and some infections (e.g. SSTI).
P1175: Severe group A streptococcal infections in Romania. A surveillance within the Strep-EURO project
B. Luca, M. Straut, V. Ungureanu, C. Schalen, A. Jasir On behalf of the Strep-EURO study group
Objectives: In the last 20 years, severe invasive streptococcal infections, often afflicting otherwise healthy subjects and yielding high mortality rates, have been increasingly recorded in Europe and other areas. Our main objective was to investigate the situation in Romania lacking earlier data in the field.
Methods: The strains used in this study were clinical isolates from nine regions in Romania. The strains were mainly blood isolates, but some were from other sterile sites. The in vitro susceptibility to antibiotics was tested by disk diffusion on PDM agar following the standard instruction. T-typing was performed by slide agglutination using sera from Sevapharma, Prague. Spe gene detection and emm sequence typing was performed according to provious publications.
Results: During eighteen months 33 cases were reported. Most prevalent T-type was 3,13 followed by types 12 and 1. More than fifteen different emm types were recognised, most of them unusual types; only four were type 1. Half of the reported cases were from children below 12 years. Out of all strains, 50% harboured speC gene, and 25 harboured speA. Erythromycin resistance was uncommon (one isolate), whereas an overall high rate of tetracycline resistance was found (54%).
Conclusion: This is the first report on severe invasive streptococcal infections since no surveillance has been previously done in Romania. The population covered was from eight out of 42 provinces. The emm type distribution might be of concern since many unusual types, not previously associated with severe disease, were found. This may be partly related to the dissemination of new types in populations immune to classical types.
Since tetracycline is not used in the treatment of streptococcal infections the level of tetracycline resistance among clinical isolates, appeared comparatively high. In contrast to several European countries, macrolide resistance seems not to be common among invasive group A streptococci in Romania.
Acknowledgment: The Strep-EURO project is funded by the European Commission.
P1176: Severe soft tissue infection and secondary bacteraemia due to community-acquired MRSA in a traveller returning from the Congo
R. Padmanabhan, R. Shrestha, G. Hall, S. Gordon, L. Saravolatz (Cleveland, Detroit, USA)
Objectives: Community acquired MRSA is increasingly becoming a global problem. These isolates possess the Staphylococcal cassette chromosome (SCC) mec type IV in their genome and a different pattern of antibiotic susceptibilities than hospital acquired strains. They are frequently virulent and cause predominantly skin and soft tissue infections by virtue of a Panton Valentine Leukocidin (PVL) toxin gene. A returning traveler, who had spent the preceding four weeks in Congo, presented with a staphylococcal bacteraemia and a large cutaneous ulcer of the right lower extremity that progressed to extensive soft tissue necrosis. He first experienced symptoms in Kinshasa International Airport, while awaiting his return flight to the United States, approximately 48 hours prior to presentation at our facility.
Methods: MRSA that was isolated from blood was susceptible to vancomycin, clindamycin, erythromycin, tetracycline, trimethoprim-sulfamethoxazole and gentamicin. Pulse Field Gel Electrophoresis (PFGE) analysis was performed using Sma1 on the patient's isolate along with another strain from our hospital and compared to other strains isolated from the Midwestern United States. PCR amplification of the genes encoding Panton–Valentin Leukocidin (PVL) was performed using primers described elsewhere.
Results: PFGE demonstrated that the Congo strain was different from any of the other Midwestern United States strains. SCC mec typing of this isolate revealed that this strain was type IV. PCR analysis did not detect sequences specific for the PVL gene.
Conclusions: The differential diagnosis of an ulcer in a returning traveler is large and includes bacterial, fungal, helminthic, protozoal, viral and arthropod borne causes. MRSA should be added to this list. The widespread occurrence of CA-MRSA in many parts of the world would support the finding of this organism on the African continent. To our knowledge, this represents the first CA-MRSA with the SCC type IV mec gene reported from Congo.
P1177: Ten-year of community-acquired methicillin-resistant Staphylococcus aureus ST80-IV clone in Denmark
A.R. Larsen, R.V. Goering, L.V. Pallesen, R. Skov (Copenhagen, DK; Omaha, USA)
Objectives: To determine the epidemiology in Denmark of the pandemic European CA-MRSA clone ST80-IV with respect to subtypes, dissemination, acquisition and types of infection.
Methods: All methicillin resistant Staphylococcus aureus (MRSA) isolated in Denmark between 1999–2003 were referred to and stored at the Staphylococcus Laboratory, Statens Serum Institut (N = 617). The isolates were characterized by macro-restriction (SmaI) analysis using PFGE, SCCmec typing, dru sequence typing, antibiotic susceptibility testing and PCR amplification of the Panton Valentine Leukocidin gene (pvl). Clinical and epidemiological information from all patients were obtained from discharge summaries and registered.
Results: Between 1999 and 2003, the MRSA ST80-IV clone accounted for 28% (172/617) of the total number of MRSA in Denmark and 30% (146/490) of Infections due to ST80-IV had primarily community onset (122/146) and thereby ST80-IV accounted for 67% of all community onset MRSA in the period. More than 80% of the ST80-IV infections were skin and soft tissue infections. By comparing the antibiogram of ST80-IV (streptomycin-, kanamycin-, tetracycline- and fusidic acid -resistant and gentamicin sensitive) with the isolates stored in our S. aureus bacteraemia collection, we traced the ST80-IV clone back to 1993. Before 1999 one to five ST80-IV isolates were encountered pr. year, which increased to 25, 26, 50, 26 and 45 isolates in the years after. By PFGE, the ST80-IV isolates exhibited nine different patterns (A1–9), of which 60% were type A1. Nine Type A1 isolates, isolated 1993–2003 were subjected to dru typing, which has earlier enabled separation of PFGE clones into subtypes. This was however not possible for the ST80-IV isolates.
Conclusions: ST80-IV isolates cause a large proportion of the MRSA infections in Denmark and in particular among the infections with a community onset. The success of ST80-IV as an infective clone outside the hospital environment may in part be due to its small SCCmec type IV and its ability to cause skin and soft tissue infections probably associated with the expression of PVL. The dru sequence typing could not subdivide the major type of ST80-IV found in Denmark pointing out the strict clonality of this clone, which may indicate that it is a very well adapted pathogen.
P1178: Epidemiology and management of pressure ulcers in an acute care hospital
F. Barbut, B. Parzybut, R. Farid, D. Neyme, M. Kosmann, L. Luquel (Paris, F)
Objectives: The aims of the study were to determine pressure ulcer prevalence in an acute care hospital, to identify risk factors, to evaluate the medical and non medical management of pressure ulcers and to study the microbiological contamination of pressure ulcers.
Methods: For each patient, a standardized questionnaire was completed. The questionnaire included demographic data (age, sex, previous hospitalizations…) and the risk factors of the Braden scale. Detection of pressure ulcer was performed by skin examination of patients by two experts in skin care. Management of ulcer pressure was evaluated by reviewing the clinical charts of each patient with pressure ulcer. Each pressure ulcer was swabbed and inoculated on selective media. All the data were entered and analysed with EpiInfo 6.04d (CDC, Atlanta, Ga).
Results: A total of 549 patients (59 ± 19 years old) were included : 75 ulcer pressures were observed in 37 patients (prevalence = 6.9%). Heel anckle was the most frequent localization (40%), followed by sacrum (20%), elbow (11%), spinous processes (7%) and ischial tuberosities (7%). Pressure ulcers were stage I (24%), stage II (29%), stage III (31%) and stage IV (16%). Eighty percents of pressure ulcers were acquired within the hospital. Using univariate analysis, risk factors significantly associated with pressure ulcer were : Braden cutoff < 15 (OR = 6.56, p < 0.0001), neurological disorders (OR = 2.30, p = 0.009), previous ulcer pressures (OR = 6.36, p < 0.0001), and hospitalization in an intensive care unit (p = 0.0003). Among the criteria used for Braden scale, humidity, activity, motility, nutrition friction and shear were significantly associated with ulcer pressures (p < 0.05). Among the 75 pressure ulcers, 9.3% were diagnosed only by the experts in skin care and 83.8% were treated. Treatment was considered inappropriate in 31.5% (mostly in stage I and III) according to the French guidelines. Microbiological results showed that 24.5 % of ulcer pressures, mostly from stage III and IV were colonized with multiple resistant bacteria (i.e. methicillin resistant Staphylococcus aureus, extended spectrum beta-lactamase Enterobacteriaceae).
Conclusion: This prospective prevalence study led to a better awareness of patients at risk for pressure ulcer. This surveillance also contributed to a better knowledge of the mobile unit of geriatrics recently created within the hospital.
P1179: Suction drainage culture in the management of musculoskeletal infection
L. Legout, R. Stern, M. Assal, P. Rohner, P. Hoffmeyer, L. Bernard Osteomyelitis Study Group
Background: Following surgery for a musculoskeletal infection (MI), a positive suction drainage culture (SDC) is consistent with persistent sepsis and an unfavorable evolution in the majority of cases. The objective of this study was to determine the effect of a negative SDC obtained in a subsequent operation or repeated operations on the outcome of MI.
Methods: One hundred patients treated surgically for MI utilizing suction drainage for 24–48 hours postoperative and appropriate antimicrobial therapy were enrolled in this prospective study. Surgical treatment consisted of the routine practice developed for the treatment of MI, consisting of drainage of purulent material, débridement, and prosthetic exchange or implant removal. The accumulated drainage fluid in the reservoir was cultured. SDC was considered negative if all bottles resulted in negative cultures. Patients were placed into one of three possible MI treatment groups according to the SDC results identified after the first surgical procedure, as follows: (I) Patients with a negative SDC and no new operation was performed; (II) Patients with a positive SDC and a new operation(s) was performed until the SDC was negative; and (III) Patients with a positive SDC and there was no new operation. The duration of antibiotic therapy for those with osteomyelitis ranged from 6 to 12 weeks, while others with MI (soft tissue infection) were treated for 10–21 days.
Results: The 3 groups were similar with regards to gender, age, underlying conditions, MI, bacterial organism, surgery, and antibiotic therapy. The majority of patients (84%) had osteomyelitis in the presence of an implant. At final review, a cure was obtained in 90% of patients (45 of 50) in group I, 87% of patients (20 of 23) in group 2, and 44% of patients (4 of 9) in group 3.
Conclusion: A negative SDC following MI surgery is a strong indication as to the eventual outcome of the infectious process.
P1180: Microbial aetiology of osteomyelitis of the foot in diabetic patients
L. Legout, M. Assal, R. Stern, P. Rohner, P. Hoffmeyer, L. Bernard (Geneva, CH)
Foot infections in diabetic patients (pts) are often accompagnied by osteomyelitis and they are the leading cause of diabetes-related hospitalization and lower-extremity amputation. Acute infections in pts who have not recently received antibiotic therapy are predominantly caused by aerobic gram-positive cocci, often as a monomicrobial infection. Although chronic wounds tend to develop polymicrobial flora.
Objective: To know the microbial etiology of osteomyelitis of the foot in diabetic pts, to determine the best choice empirical antibiotics combination.
Methods: Diabetic pts with osteomyelitis of the foot admitted in our unit between 2002 and 2004 were included. The infection was documented with intraoperative samples and osteomyelitis was histolopathologically prouved. Clinical and biological data were collected.
Results: 87 diabetics pts (64 males, 23 females) with a median age 65 years(23–94) were included. The co-morbidities were chronic renal failure (n = 35), arteriopathy (n = 34), obesity (n = 13), alcoholism (n = 10), immunodepression (n = 10). The clinical data were fever (40%), shock (2%), local signs as erythema (90%), fistula (86%), necrosis (43%) and foul odor (54%). The median rates of neutrophils polynuclear, C-reactive protein and erythrocyte sedimentation were respectively 9.7 G/L, 131 mg/l, 82 mm. 59 pts (68%) had a polymicrobial infection. The intra-operative samples (n = 87) yieled a majority of gram positive cocci [MSSA:n = 30;MRSA:n = 15; CNS:n = 15; Streptococcus sp:n = 34; Enterococcus sp: n = 15], following with gram negative bacteria [Pseudomonas sp: n = 12; Proteus sp: n = 11; Morganella sp: n = 11; E. coli: n = 8; Klebsiella sp: n = 6; E. cloacae: n = 6; Citrobacter sp: n = 4; Serratia sp: n = 3, others: n = 3] and anaerobes (n = 17). 10 pts had positive blood samples. S. aureus is the most frequent pathogen isolated especially in monomicrobial infections and infections with positive blood samples. Pseudomonas spp. seems to be correlated with chronic renal failure and immunodepression. No clinical data was significantly associated with a special bacteria, except necrosis and foul odor with gram negative bacteria or anaerobes.
Conclusion: Our results are according with clinical studies in the literature. The major difficulty to treat osteomyelitis of diabetics foot is to well documented the infection. Selecting an appropriate antibiotic to treat is particularly important because of the prolonged duration of therapy required and potential resistance of pathogens.
P1181: The duration of hospitalisation (length of stay) in patients hospitalised with complicated skin and skin structure infections: identifying clinical and microbiologic risk factors in a comparison of tigecycline with vancomycin/aztreonam
R. Mallick, S. Solomon (Collegeville, USA)
Objectives: Despite therapeutic advances in the treatment of complicated skin and skin structure infections (cSSSI), prolonged hospital stays are a major cost driver and highlight the need for expanded broad-spectrum therapies that enable faster cure and discharge.
Methods: We pooled data from 2 double-blind, randomized, multinational clinical studies in patients with cSSSI. Patients were randomly assigned to receive tigecycline (100-mg dose, then 50 mg twice daily [BID]) or vancomycin with aztreonam (1 g vancomycin + 2 g aztreonam BID) administered intravenously for 5 to 14 days. Formal test of cure was assessed at least 12 days after antibiotic termination (which was based on clinical assessments). Length of stay (LOS) reflects comorbidities and disease severity as well as therapy duration. We used a Cox proportional hazard (CPH) model adjusting for potential clinical and microbiologic risk factors, to evaluate LOS.
Results: Among the 1116 modified intent-to-treat patients, the most common infection diagnoses at baseline were cellulitis (58.9%) and major abscess (27.9%). The most common underlying etiologies were spontaneous infection (52.3%) and trauma (27.6%). About 20.2% of patients had diabetes; 6.9% had peripheral vascular disease. Staphylococcus aureus was the most common causative pathogen (about 50% of patients) among 540 patients with confirmed microbiology and complete hospitalization data. However, about 18% of patients had a gramnegative causative pathogen, primarily Escherichia coli. About half the patients were polymicrobial. Overall, there were no differences between the treatment groups in LOS (p = 0.794). The estimated CPH model identified diabetes, trauma, a gramnegative causative pathogen, absence of cure, use of concomitant medications, infected ulcer, ICU and non-US hospital setting for treatment initiation as risk factors for significantly higher LOS. Adjusting for all of these factors, treatment with tigecycline was associated with faster discharge (hazard ratio = 1.22; p = 0.019 [∼1 day shorter LOS]). This difference was almost entirely attributable to the subgroup of patients in which the causative pathogen was gram-negative.
Conclusions: Diabetes, gram-negative pathogen, and infected ulcers are risk factors for prolonged LOS. Tigecycline, the first glycylcycline antibiotic, was associated with shorter LOS in those patients with a primary gram-negative pathogen, consistent with its expanded broad-spectrum activity.
P1182: Global variations in infection diagnoses, aetiologies, co-morbidities, and causative microbiology in hospitalised patients with complicated skin and skin structure infections: evidence from a pooled clinical database
R. Mallick, S. Solomon (Collegeville, USA)
Objectives: Given heterogeneous clinical presentation of complicated skin and skin structure infections (cSSSI), we used a large multinational, pooled clinical database to examine global differences in etiologies, comorbidities, infection subtypes, and causative pathogen distributions.
Methods: Data were pooled from 2 double-blind, randomized, multinational clinical trials for patients with cSSSI treated with tigecycline (100-mg dose, then 50 mg twice a day [BID]) or vancomycin with aztreonam (1 g vancomycin + 2 g aztreonam, BID) administered intravenously for 5 to 14 days. We compared key baseline clinical and microbiological characteristics across regions: United States (US), Canada, Europe, Latin America, Asia, South Africa and Australia using the chi-square test of proportions.
Results: Among 1,116 modified intent-to-treat patients with cSSSI, regions varied by subdiagnoses, etiologies and co-morbidities (p < 0.0001). Although deep/extensive cellulitis was the most common sub-diagnosis overall (∼59%), it was most common in South Africa (91%); major abscess was the most common cSSSI subdiagnosis in the US (46%). Spontaneous infections were the most common etiology overall (52%), reported most commonly in Asia (69%); trauma (28%) was the 2nd most common, reported most commonly in South Africa (40%). About 20% of all patients presenting with cSSSI had diabetes; this proportion was highest in Asia and Canada (∼34% each) and in the US (∼30%). Among 540 patients with confirmed microbiology, Staphylococcus aureus was the most common causative pathogen but varied significantly in prevalence across regions (about 50% of patients overall, 82% in the US, 67 to 68% in Europe and Asia, and 39% in South Africa). About 42% of patients had polymicrobial infections. About 18% had a gram-negative causative pathogen, mostly Escherichia coli. Gram-negative causative pathogen prevalence was greatest in Asia (39%).
Conclusions: This analysis showed significant global variations in cSSSI subdiagnoses, etiologies, comorbidities and causative pathogens. Consistent with findings of the SENTRY Antimicrobial Surveillance Program, S. aureus was identified as the predominant pathogen in cSSSI, especially in the US. Gramnegative pathogens were also identified as causative in a substantial proportion of complicated skin infections. These findings may offer guidance in selecting effective empiric therapy, especially regarding newer agents with expanded broad-spectrum activity.
P1183: A novel approach for evaluating the microbiological efficacy of tigecycline in patients with complicated skin and skin-structure infections
A. Meagher, P. Ambrose, J. Passarell, B. Cirincione, T. Babinchak, E.J. Ellis-Grosse (Buffalo, Albany, Collegeville, USA)
Objectives: Tigecycline (T) is a glycylcycline in development for the treatment of patients (pts) with serious infections, including complicated skin and skin-structure infections (cSSSI). While cSSSI can be caused by a mixture of Grampositive and -negative bacteria, Staphylococcus aureus and streptococci are the predominant pathogens. Previous analyses combining all pathogens have failed to identify an exposure-response (ER) relationship. A method was developed to create more homogenous pt populations for the microbiological (M) ER analysis of T in the treatment of cSSSI.
Methods: Pts from 3 cSSSI clinical trials (one Phase 2 & two Phase 3) with T pharmacokinetic data and classified as both clinically and M evaluable, were pooled for analysis. Pts received 100 mg loading dose (LD)/50 mg q12h (100/50) or 50 mg LD/25 mg q12h (50/25). At the test of cure visit, M (eradication or persistence) response was evaluated. Indeterminate responses were excluded. Non pathogenic baseline isolates were excluded. Five homogeneous pt cohorts (C) were created based on baseline pathogens: S. aureus only (C1); S. aureus or streptococci (C2); 2 Gram-positive pathogens (C3); polymicrobial (C4); other monomicrobial infections (C5). Prospective step-wise procedures for combining C to increase sample size were used. Logistic regression was used to evaluate steady-state 24 hr area under the concentration-time curve (AUC) to MIC ratio (AUC/MIC) to predict response.
Results: The dataset included 58 pts with 88 observations. C1 (n = 20) and C2 (n = 9) could not be evaluated due to small sample size. Analysis began with pooled C2 + C3. Continuous AUC/MIC ratio was marginally significant (p = 0.1130); a pt was 5.1% more likely to have successful response for every one-unit increase in AUC/MIC. Adding C4, including pathogens with MIC values up to 16 mcg/mL, decreased AUC/MIC, added cures to the lower end of the distribution, and added significant noise to the analysis. Adding C5 increased sample size and further decreased the ability to detect a relationship.
| Cohorts (Patients/Pathogens) | Pathogen-Level Microbiological Response |
Odds Ratio | Area under the ROCa Curve | |
|---|---|---|---|---|
| Eradication n (%) | Eradication n (%) | |||
| 2 + 3 (36/41) | 35 (85%) | 6 (15%) | 1.051 | 0.767 |
| 2+3+4 (50/BO) | 66 (83%) | 14 (17%) | 1.025 | 0.611 |
| 2+3+4+5 (58/83) | 74 (84%) | 14 (16%) | 1 023 | 0.604 |
Receiver Operator Characteristic
Conclusion: Analysis of all pathogens combined could not identify an ER relationship. Polymicrobial infections with Gramnegative and anaerobic pathogens, associated with high MIC values, added noise to the analysis and decreased the predictive capability of the model. The approach of creating homogenous populations based on two key pathogens in cSSSI, S. aureus and streptococci, was critical for identifying significant ER relationships.
P1184: Exposure-response analysis of the efficacy of tigecycline in patients with complicated skin and skin-structure infections
A. Meagher, J. Passarell, B. Cirincione, S. Van Wart, K. Liolios, T. Babinchak, E.J. Ellis-Grosse, P. Ambrose (Buffalo, Collegeville, Albany, USA)
Objectives: Tigecycline (T), the first glycylcycline to reach clinical trials, is in development for the treatment of patients (pts) with serious infections, including complicated skin and skin-structure infections (cSSSI). Pharmacokinetic-pharmacodynamic (PK-PD) relationships, including pt covariates, for microbiological (M) & clinical (C) efficacy of T were evaluated in pts with cSSSI.
Methods: Pts from 3 cSSSI clinical trials (one Phase 2 & two Phase 3), with PK data and classified as both C & M evaluable, were pooled for analysis. Only those pts with infections due to Staphylococcus aureus and/or streptococci, the predominant pathogens in cSSSI, were prospectively evaluated. Pts received 100 mg loading dose (LD)/50 mg q12h (100/50) or 50 mg LD/25 mg q12h (50/25). At the test of cure visit, M (eradication or persistence) & C (cure or failure) outcomes were assessed. Indeterminate responses were excluded. Steady-state 24 hr area under the concentration-time curve (AUC) and AUC/MIC ratio were evaluated as predictors of response. Pt covariates included: age, weight, country, baseline Pseudomonas aeruginosa or anaerobes, & comorbidities (diabetes, peripheral vascular disease). Classification and regression tree (CART) analyses determined AUC/MIC breakpoints (BP). Logistic regression (one observation/pt) was performed to determine predictors of efficacy.

Results: The dataset included 35 pts with 40 S. aureus and/or streptococcal baseline pathogens. MIC values ranged from 0.06 to 0.5 mcg/mL. Clinical cure was achieved in 30 (85.7%) pts and 35 (87.5%) pathogens were successfully eradicated. The median AUC/MIC ratio was 13.5 and 29 for the 25 and 50 mg dose groups, respectively. Covariates were not significant predictors of efficacy. CART identified a significant AUC/MIC BP of 12.5 (p = 0.0177 for M and 0.0341 for C). The continuous AUC/MIC ratio was marginally significant based on sample size (p = 0.0563 for M & 0.1960 for C) and was deemed the most informative model. For each unit increase in AUC/MIC, within the observed range, pts were 3.7% more likely to have a successful C response and 17.1% more likely to have a successful M response.
Conclusion: Pts with AUC/MIC ratios ≥12.5 were 13.5 times more likely to have successful M response. At the median AUC/MIC ratio of 13.5 & 29 for the 50/25 & 100/50 dose groups, the model-predicted probability of C success was 0.66 & 0.96, respectively. T is likely to be an important treatment option for cSSSI.
P1185: Streptococcus pneumoniae spinal infection
L. Cuadra, E. Calbo, R. Pallarés, J.M. Aguado, E. Pérez-Trallero, M. Xercavins, J. Garau (Terrassa, Barcelona, Madrid, San Sebastian, E)
Introduction: Vertebral osteomyelitis and/or sacroiliitis due to Streptococcus pneumoniae are extremely rare. Although it is one of the most common pathogen isolated in blood cultures, there are only about 30 cases reported in the literature. In the main series of vertebral osteomyelitis (VO) SPSI represents less than 1% of cases (1/587).
Material and methods: We report 6 cases of spinal infection due to S. pneumoniae (5 VO and 1 SI with psoas abscess) seen between 1999 and 2004 at 4 different acute care hospitals.
Results: The 6 cases reported were part of a total of 1227 episodes of pneumococcal bacteraemia (0.48%). Mean age of the patients was 57.1 years (range 37–82); there were 4 men. Alcohol abuse 2/6, immunosupression 2/6 and smoking 4/6 were the most common comorbilities. Blood cultures were positive in all cases, epidural pus and vertebral biopsy were also positive in 3/ 6. All strains were susceptible to penicillin. Diagnoses were made by MRI in 4 and CT scanning 2. All patients recived betalactam agents during a mean of seven weeks (3.8–10.7) in monotherapy (cefotaxime 4/6, ampicillin 1/6) or in combination (with vancomicin+gentamicin in 1 case). One case needed surgery, because of progression of a psoas abscess. Other foci were found in three cases (psoas and paravertebral abscesses and acromio-clavicular arthritis).
Conclusions: SPSI is a rare presentation of invasive pneumococcal disease. Underlying disease is comnmon and other territories are frequently involved. Infective endocarditis must be ruled out. Its course appears to be benign. Beta-lactam antibiotics are a good option, and surgery is occasionally indicated for progressive disease despite appropriate antimicrobial therapy.
P1186: Lumbar spine spondylitis due to Staphylococcus schleiferi following coronary angioplasty: isolation of the pathogen in peripheral blood cultures
A. Karakolios, C. Karagiannidou, T. Kallinikidis, F. Markou, V. Kontos, G. Tsinopoulos (Serres, GR)
A 70-year old man presented with acute, severe lower back pain 3 weeks after having been subjected to coronary angioplasty for ischaemic heart disease. He was treated with NSAIDs but not antibiotics without any improvement. CT scan of the lumbar spine showed changes in L5-S1 vertebrae that were consistent with spondylitis. MRI imaging, as well as confirming spondylitis at L5-S1, it also revealed the presence of a left paravertebral abscess. On admission to hospital, low grade fever was documented. Clinical examination of the lower limbs was normal. Staphylococcus schleiferi, sensitive to several antibiotics, was isolated from 3 sets of blood cultures taken from both arms. Initially, Ciprofloxacin 200 mg bd IV was administered for 4 weeks. Despite continuous clinical improvement, MRI imaging 8 weeks after the commencement of antibiotic treatment showed no improvement of the radiological findings. Thus, Levofloxacin 500 mg bd p.o. Rifampicin 300 mg bd p.o. were given for further 16 weeks. At the end of the treatment, the patient was symptom-free, resumed full activity and MRI imaging showed considerable improvement. Multiple blood cultures taken from both arms at different time points can help isolate pathogens causing spondylitis averting thus the need for difficult, interventional sampling of the focus of infection.
P1187: Diabetes and use of topical ocular antibiotics: a population-based case-control study
A.K. Hansen, R.W. Thomsen, H.H. Hundborg, L.L. Knudsen, H.C. Schønheyder (Aalborg, Aarhus, DK)
Objectives: We conducted this population-based case-control study to examine whether patients with diabetes mellitus have an increased relative risk of being treated with topical ocular antibiotics, as compared with population controls.
Methods: Incident cases were defined as 24,559 individuals who redeemed a prescription for a topical ocular antibiotic in 1999 in North Jutland County, Denmark. Ten gender- and age-matched population controls per case were selected, using a unique personal identifier. Diabetes prior to the topical ocular antibiotic prescription was determined by record-linkage with the County Prescription Database and Hospital Discharge Registry. We did conditional logistic regression to estimate odds ratios (ORs) for ocular antibiotic use among diabetic individuals and population controls, with adjustment for a range of comorbid diseases.
Results: Among individuals treated with topical ocular antibiotics, 2.5% had diabetes as compared with 2.0% among control subjects. The overall adjusted OR for use of ocular antibiotics in diabetic individuals was 1.24 (95% confidence interval [CI]: 1.13–1.35). Stratified analyses showed that children between 3 and 15 years with diabetes had a 60% increased relative risk for ocular antibiotic use, whereas the effect of diabetes as a risk factor was low in individuals over 65 years and in those with presence of other diseases.
Conclusions: These results suggest that diabetes is a risk factor for the use of topical ocular antibiotics, especially in younger individuals.
P1188: Bacterial pathogens and their antibiotic susceptibility in infectious conjunctivitis in general practice
R.P. Rietveld, J.H. Sloos, P.J.E. Bindels, H.C.P.M. van Weert (Amsterdam, Alkmaar, NL)
Objectives: Determination of bacterial species and their susceptibility to antibiotics in infectious conjunctivitis in general practice.
Methods: 179 patients suspected of having infectious conjunctivitis were included from 25 general care centres in the Netherlands. From both eyes a swab was taken and pathogens found in the bacterial cultures were tested for their susceptibility using the Etest for chloramphenicol, fusidic acid, trimethoprim, ciprofloxacin, and gentamicin (MICs according to Dutch national criteria).
Results: 80/220 affected eyes were culture positive. Streptococcus pneumoniae (n = 55) was the most predominant pathogen, followed by Haemophilus influenzae (n = 19), and Staphylococcus aureus (n = 18). Only for chloramphenicol and ciprofloxacin the MIC90s were in the susceptible or intermediate susceptible range for all three pathogens, whereas this was not the case for the other antibiotics tested, of which at least one MIC90 was in the resistant range.
Conclusion: In only one thirdth of the patients suspected of infectious conjunctivis in general practice a bacterial pathogen was found. Although the prescription of antibiotics can be debated on the basis of our results, chloramphenicol and ciprofloxacin seems to be superior above fusidic acid, trimethoprim, and gentamicin.
P1189: Investigation of the aetiology of a trachoma-like condition in a rural population in Guangxi province, PRC
P. Cho, M.V. Boost, W. Ng (Hong Kong, HK)
Objectives: To determine the presence of trachoma in primary school children of the Zhuang and Yiao ethnic minority groups in Dujan county in Guangxi, China.
Method: Primary school children were examined using a slit lamp and several were noted to display follicular/papillary conjunctivitis suggestive of trachoma. To confirm the etiology of the condition, children were examined on a follow-up visit. For each subject, after examination with the slit lamp, the upper lid was everted after the application of a topical anesthetic (Novesin), and a dacron swab was passed along the upper tarsal lengthwise four times. Strict aseptic precautions were employed to prevent cross-contamination during sample collection. Swabs were placed in DNA-free tubes, transported to Hong Kong, and tested using the Roche Amplicor kits for detection of Chlamydia trachomatis following the manufacturer's instructions. Twenty children displayed significant conjunctival signs and photographs of the everted upper lids were taken to determine if these visual signs correlated with presence of trachoma as confirmed by PCR.
Results: Sixty-five of 120 primary school students were willing to be tested, and 29% of these were positive for trachoma by PCR. Comparison of photographs and PCR result indicated that not all children who showed signs of conjunctivitis were positive for trachoma. In addition, some children whose eyelids displayed milder form for conjunctivitis were positive by PCR. No obvious corneal involvement was observed for these children.
Conclusions: It was confirmed that hyper-epidemic levels of trachoma can be found among ethnic minority children in Dujan county. This may be related to the poor hygiene standards and the scarcity of water in this limestone region. PCR was not positive for all children showing signs of follicular/papillary conjunctivitis, which may indicate that some cases were in a dormant stage. It is also possible that failure to detect the organism was due to sampling error or delay in PCR analysis. Nevertheless, the high level of infection is a cause for concern as trachoma remains one of the leading causes of blindness, and further investigation and treatment are warranted.
P1190: Clinical and epidemiological considerations about anthrax in Constanta county, Romania
S. Rugina, I.M. Dumitru, C.N. Rugina, E. Dumea, E. Basca (Constanta, RO)
Introduction: Anthrax is by primarily a disease of herbivores but humans can become infected as they come into contact with infected animals or their products.
Objective: To study the cases of human anthrax diagnosed in the last twelve years and their characteristics: epidemiology, clinical forms and evolution.
Material and method: It is a retrospective study on a period of twelve years performed in Infectious Diseases Clinical Hospital. The diagnosis was based by smear, and culture of vesicular fluid or CSF.
Results: During this period fifteen cases of anthrax in humans were identified. The repartition of cases according to sex groups revealed a high predominance of male cases (13 cases). The disease was most prevalent in 35–44 age group and after 55–years old (6 cases), although anthrax can be observed between 15 years and 65 years. In all cases anthrax was occupational disease and the provenience of patients was rural area. The annual incidence of anthrax was characterized by a low value and irregular frequency of the disease. The most cases were in 1994 (6 cases) and 2004 (5 cases). According to the seasonal repartition, anthrax was most prevalent in the summer months (11 cases). The most frequent clinical form of anthrax was the cutaneous anthrax (14 cases), and only one patient achieved anthrax meningitis. Under specific treatment with penicillin G, all the patients with cutaneous anthrax recovery complete, only the patient with anthrax meningitis died.
Conclusions: In Constantza County, anthrax remained sporadic in the last years. After a free period (2001–2003) 5 cases of coutaneous anthrax were registered in 2004. A good cooperation between veterinary and physicians and individual awareness of the materials is the key to prevention of anthrax.
P1191: Microbiological characteristics of anthrax strains
L. Lukhnova, G. Temiraliyeva, T. Meka-Mechenko, Y. Pazylov, S. Zakaryan, J. Denissov (Almaty, KAZ)
Objectives: The Kazakh Science Center for Quarantine and Zoonotic Diseases (KSCQZD) has a collection of pathogens of especially dangerous infections that have been isolated in Kazakhstan. By Kazakh government resolution, the KSCQZD's collection is the official collection of pathogenic bacteria for Kazakhstan. KSCQZD has 71 strains of B. anthracis that were isolated in various years (1952–2004).
Methods: We studied the biological properties of 30 anthrax strains from our collection: 16 from humans, 4 from soil, 5 from sheepskins, 2 from sheep organs, and 3 from the external environment. We tested the anthrax strains using standard identification tests.
Results: The growth of the Bacillus anthracis strains on the Hottinger's agar was typical (R – form), and no distinctions based on the origin of the strains were noted. All of the strains form spores and are immobile. When stained with specific antibody directed toward anthrax antigens, all strains stained positive. Three of the B. anthracis strains did not have capsules when originally studied, but after 7 cultures on the Hottinger's agar, the strains’ ability to form capsules in a CO2 atmosphere was restored. The anthrax strains are sensitive to anthrax bacteriophage and penicillin. The strains have lipolytic and hemolytic activity. All of the 30 strains tested have hemopeptic activity, which is indirect evidence of their virulence. The strains have no phosphatase enzymes or lecithinase. The strains we studied ferment glucose, sucrose, glycerin, and rhamnose, and they form acid without gas. The strains all grew in synthetic “A” medium, although growth was weak. When L-tyrosine, L-tryptophan, L-threonine, and L-methionine were added to the synthetic “A” medium, the pathogen grows in the typical manner. Two anthrax strains are moderately resistant to rifampicin (MIC 1.5–16), and three are not sensitive. The anthrax strains are highly sensitive to tetracycline, benzylpenicillin, gentamycin, and oxacillin.
Conclusions: Regardless of their source of isolation and time of storage, the anthrax strains isolated during outbreaks are virulent, spore-forming, and capsule-forming cultures. This study confirms that virulent forms of B. anthracis are still circulating in Kazakhstan. The research described in this abstract was made possible in part by support provided by the U.S. Defense Threat Reduction Agency under the project «KB0-1950-AL-03» and administered by U.S. CRDF.
P1192: The importance of laboratory methods in diagnosing anthrax in humans
L. Lukhnova, A. Aikimbayev, T. Meka-Mechenko, G. Temiraliyeva, S. Zakaryan, M. Sagatova (Almaty, KAZ)
Objectives: Isolation of anthrax bacillus using bacteriological methods is slow and frequently misleading. The literature suggests anthrax bacillus is isolated in 13% to 48% of patients infected with Bacillus anthracis. The pathogen quickly perishes or transforms into atypical forms. The number of bacilli in a clinical specimen is often low or below the sensitivity of culture. This suggests other methods would be useful in establishing the diagnosis of anthrax, specifically; serological methods would be beneficial in diagnosing infection with Bacillus anthracis.
Methods: We conducted studies to assess various methods for diagnosis of Bacillus anthracis infection in patients. We reviewed archival data and our own results on pathological material from patients infected with Bacillus anthracis in the Southern and Eastern Kazakhstan oblasts.
Results: The most informative test for detection of anthrax in patients was the delayed type hypersensitivity (DTH) or dermatoallergic test with anthraxin. Eighty one per cent of patients with signs and symptoms of anthrax gave a positive reaction with anthraxin. The Ascoli reaction complete with scab was positive in 72.1% of patients, and the indirect hemeagglutination (IHA) test was positive in 65.6% of patients. The clinico-epidemiological diagnosis of anthrax was confirmed with culture in 44% of cases. Serum samples from patients diagnosed with anthrax in the Eastern Kazakhstan oblast were evaluated using IHA in 2001-2004. High titres of specific antibodies (1:6401:5120) were detected in patients with dermatologic anthrax lesions from which anthrax was isolated.
Conclusion: Our data suggest the anthraxin DTH test and IHA are good methods for establishing a diagnosis of anthrax. Cultures for anthrax bacillus were the least efficient method for establishing the diagnosis. When results of laboratory tests are negative or inconclusive, one still has to rely on the clinicoepidemiological diagnosis. The research described in this abstract was made possible in part by support provided by the U.S. Defense Threat Reduction Agency (DTRA) under the project «KB0-1950-AL-03» and administered by U.S. Civilian Research and Development Foundation (CRDF).
Fluroquinolones, in vitro studies
P1193: Comparative bactericidal activity of moxifloxacin and levofloxacin against viridans streptococci at simulated salivary concentrations
R. Davidson, C. Howley, S. Campbell (Halifax, CAN)
Objectives: The fluoroquinolones are bactericidal agents frequently used in the treatment of respiratory tract infections. The viridans Streptococci (VGS), although associated with disease, generally exist as part of the normal human oral flora. As such, they may exposed to antibiotics with greater frequency than oppurtunistic pathogens. Preliminary data suggest that the VGS may act as a reservoir for fluoroquinolone resistance in S.pneumoniae through horizontal transfer. Here, we compared the killing kinetics of moxifloxacin (MXF) and levofloxacin (LEV), against VGS at simulated saliva concentrations.
Methods: Eight strains of VGS, 4 S. mitis (2 with parC mutation) and 4 S.oralis, (2 with parC mutation) were challenged with MXF and LEV in a pharmacodynamic model utilizing Mueller–Hinton broth supplemented with 5% lysed horse blood. Cultures were inoculated at a density of 1 × 108 cfu/ml, incubated at 35ordm;C, and examined for viable growth at 0, 1, 2, 4, 6, 12, and 24 hrs after exposure to the antibiotics at concentrations simulating salivary levels. Salivary concentrations of MXF (400 mg), and LEV (500 mg) were 3.19 and 3.71 μg/ml respectively. Protein binding of MFX and LEV were taken to be 50% and 30%. Adjusted salivary levels were 1.6 (MXF) and 2.6 (LEV) ug/ml. PCR was used to amplify parC and gyrA, and mutations detected by DNA sequencing.
Results: Both MXF and LEV were highly bactericidal against susceptible strains of VGS at salivary concentrations. MFX typically eradicated the VGS by 6 hours and LEV by 12–24 hours. For parC mutants, both MXF and LEV were consistently bactericidal resulting in eradication after12 hours for MXF and 24 hours for LEV. Regrowth was observed in both strains of S.mitis (parC) exposed to LEV (2 of 10 experiments). The MIC of these strains to LEV increased 4 fold and DNA sequencing revealed the selection of a gyrA mutation in each strain. No regrowth was detected in the S. oralis strains.
Conclusions: Both MXF and LEV are extremely active against susceptible VGS at concentrations of drug found in saliva, however, superior killing kinetics were consistently observed with MXF. MXF consistently eradicated strains with a parC mutation, however, regrowth was observed on 2 occasions with LEV suggesting that MXF may be less likely to drive resistance among VGS. Again, this may have implications due to the ability of VGS to exchange its genetic determinants with S. pneumoniae.
P1194 Moxifloxacin and ciprofloxacin uptake by human neutrophils and their influence on viability, phagocytosis, oxidative burst, and chemotaxis
A.M. Berg, J. Altrichter, B. Drewelow, R.G. Mundkowski (Rostock, D)
Objectives: The influence of antibiotics on the immune defence is of increasing interest. The purpose of this study was to set up a cellular model for correlating the intracellular concentrations of the fluorochinolones Moxifloxacin and Ciprofloxacin with selected cell functions of early immune response. A human promyelotic cell line which is used for sepsis treatment by the Extracorporeal Immune Support System (EISS®, Teraklin GmbH) was chosen to establish the model. The second stage involved native human polymorphonuclear neutrophiles (PMNs) as target cells.
Methods: The promyelotic model cell line was differentiated towards neutrophils with all-trans retinoic acid, human PMNs were isolated using dextran sulfate sedimentation and density gradient centrifugation. The cells were incubated with antibiotic concentrations within the therapeutic range and above (0.5-2 Cmax) for time periods up to 8 hours. The extra- and intracellular concentrations were determined by HPLC-UV. The viability of the cells was controlled using the Trypanblue-exclusion assay. Phagocytosis and oxidative burst were assessed by a combined flow cytometric assay after stimulation of the cells with serum-opsonised fluorescein-isothiocyanate-conjugated E. coli in the presence of dihydroethidium as an indicator of superoxid production. A two-compartement chamber system was used to study the influence of either fluorochinolone on the chemotaxis.
Results: With either cell type, Moxifloxacin accumulated rapidly with peak concentrations within 15 min whereas intracellular maximum concentrations of Ciprofloxacin were achieved after 2 h. The accumulation rate of both antibiotics inside the native PMNs was more than twice as high as in differentiated EISS® cells. Neither Moxifloxacin nor Ciprofloxacin showed a significant influence on viability and the immune response parameters phagocytosis and oxidative burst of native PMNs; chemotaxis ability was reduced to a minor degree. Viability and phagocytosis of the diffentiated EISS®-cells remain unaffected whereas the oxidative burst appeared decreased. Chemotactic acticity of EISS®-cells could not be stimulated.
Conclusions: A significant accumulation of Moxifloxacin and Ciprofloxacin was determined in both cell types. However, no relevant influence on viability, phagocytosis, oxidative burst, and chemotaxis was observed. Hence no hints were found suggesting a restricted use of Moxifloxacin and Ciprofloxacin for immunocompromised patients.
P1195: Prospective, multicentre in vitro study to determine resistance rates and comparative activity of moxifloxacin vs. clinical bacterial isolates from patients with respiratory tract infections (MOXIAKTIV study)
A. Dalhoff, G. Korfmann, E. Jacobs (Kiel, Leverkusen, Dresden, D)
Objective: To determine the prevalence of resistance in current clinical isolates of S. pneumoniae, H. influenzae, M. catarrhalis, S. aureus and K. pneumoniae as well as the in vitro susceptibility to moxifloxacin and other iv antibiotics in Germany.
Methods: Up to 20 isolates of each of the above-mentioned species were cultured on standard media and tested for in vitro susceptibility using E-test® in each of the 29 study centres in Germany. For validation, an ATCC control strain was included for each species. Drugs tested were moxifloxacin, levofloxacin, amoxicillin/clavulanate, cefuroxime, clarithromycin and penicillin G. The latter two were not tested for Klebsiellae. S. aureus was additionally tested for oxacillin resistance and K. pneumoniae was tested for production of extended spectrum beta-lactamases (ESBL). DIN breakpoints were used where applicable.
Results: Overall, 1859 pathogens of 1,811 hospitalised patients with respiratory tract infections were analysed. Results for moxifloxacin are summarized in table 1. Of S. pneumoniae isolates 93.3% were susceptible to penicillin G and 85.7% to clarithromycin. With an MIC90 of 1 mg/l, the in vitro activity of levofloxacin was markedly lower than that of moxifloxacin. H. influenzae showed almost 100% susceptibility to fluoroquinolones, but only 4.5% to clarithromycin (MIC90 32 mg/l). As beta-lactamase production is common among H. influenzae isolates in Germany, amoxicillin/clavulanate showed far higher susceptibility rates than penicillin G (87.9% vs. 1.0%). Due to a high rate of beta-lactamase production only 9.8% of Moraxella isolates were susceptible to penicillin G, compared with 99.1% to amoxicillin/clavulanate. Moraxella isolates were fully susceptible to the fluoroquinolones. Overall, 13.0% of Klebsiella isolates produced an ESBL. Interestingly, ESBL prevalence was 38.8% in Eastern Germany, but below 10% in Western Germany. ESBL producers of Klebsiella were less susceptible to antibiotics other than cefotaxime or ceftazidime than non-ESBL producers.
Table 1.
MIC90 and susceptibility to moxifloxaczin (n = number of isolates)
| Moxifloxacin | S. pneumoniae (n = 426) | H. influencae (n = 398) | M. catarrhalis (n = 112) |
S. aureus |
K. pneumoniae (n = 438) | |
|---|---|---|---|---|---|---|
| MSSA (n = 406) | MRSA (n = 75) | |||||
| MIC90 (mg/L) | 0.19 | 0.125 | 0.125 | 1 | 8 | 0.75 |
| susceptible (%) | 99.3 | 99.7 | 100 | 91.4 | 9.3 | 94.1 |
Conclusion: For all species tested, the fluoroquinolones achieved the highest overall susceptibility rate (92.8%) compared to the other antibiotics (penicillin G: 36.9%, clarithromycin: 60.5%, ampicillin/clavulanate: 85.7%, cefuroxime: 89.6%). Moxifloxacin showed a high activity against current respiratory pathogens in Germany and was the most active fluoroquinolone, in particular against Gram-positive pathogens.
P1196: Double and triple combinations of ciprofloxacin with other antipseudomonal drugs against multidrug resistant isolates of Pseudomonas aeruginosa in vitro
B. Henkle, M. El-Azizi, A. Entabi, F. Malal, N. Khardori (Springfield, USA)
Objectives: Drug combinations have become the best choice in treatment of serious infections with resistant microorganisms including P. aeruginosa (PA). We tested Ciprofloxacin (CIP) in double and triple combinations with ceftazidime (CAZ), imipenem (IMP), piperacillin (PIP), and amikacin (AMK) against 20 MDR clinical isolates of PA.
Methods: The MIC for each drug alone was determined by broth microdilution technique described by NCCLS. Double and triple combinations of CIP with other drugs were tested by using 96-well plates and by time–kill assay. Rows A to G were assigned for the drugs as follows: row A for CIP alone, B for second drug, C for third drug, D for CIP + second drug, E for CIP + third drug, F for second drug + third drug and G for the three drugs together. Row H was left for drug-free control. Briefly, all wells were filled with 50 μl of cation adjusted Muller Hinton broth. The drugs at 2X of the highest tested concentrations in 50 μl of the medium (alone, in double or in triple combinations) were delivered to wells A1–G1. Two-fold serial dilutions were made by using multichannels pipettes. Bacterial suspensions (5 μl) were added to bring the initial inoculum size to 5 × 105 cfu/ml and the plates were incubated at 37°C for 24 h. Synergy was considered only in triple combinations if the growth-free wells with lowest concentration of the most potent drug were at least 2-fold less than the growth-free wells containing the most potent drug alone or in double combinations with the two other drugs.
Results: The best synergistic effects were observed in combination of AMK with CAZ (80%) or PIP (80%) and in combination of CAZ with PIP (60%) or CIP (60%). Antagonism was observed in combination of IMP with CAZ (60%) or PIP (50%). In triple combinations of AMK-CAZ-CIP, synergy was observed in all isolates (100%). Good results were also observed in combination of AMK-PIP-CIP (70%) and CAZ-PIP-CIP (70%). No antagonism was observed in any of the triple combinations tested.
Conclusion: Our data show that triple combination of antipseudomonal drugs is better than using one or two drugs in treating PS infections
P1197: Determination of the mutant prevention concentration and minimal inhibitory concentration of gemifloxacin against penicillin susceptible and resistant clinical isolates of Streptococcus pneumoniae
J. Blondeau, S. Borsos, C. Hesje, L. Blondeau (Saskatoon, CAN)
Objective: While MIC measurements determine the in vitro drug concentrations required to inhibit the growth of 100,000 organisms/ml, it may not detect resistant subpopulations that are detected at higher inoculums (≥1 billion organisms) as used in the MPC assay. As quinolones are widely used for treating SP infections and quinolone resistance is a concern, we tested GM–a newly approved compound–by MIC and MPC against PS and PRSP.
Methods: MIC testing was by microbroth dilution in accordance with NCCLS guidelines. For MPC testing, 10 billion organisms were applied to agar plates containing drug and read at 24 and 48 hours following incubation. The lowest concentration preventing any growth was the MPC. Organisms with high MPC values (≥2 μg/ml) were screened for amino acid substitution in the quinolone resistance determining region.
Results: A total of 402 clinical SP isolates were tested: 320 PS, 69 penicillin intermediate (PI) and 13 PR. The following represents the MIC50/90 (μg/ml) and range (μg/ml) respectively against PR, PI, PS strains: 0.031/0.063, ≤0.002-2; 0.031/0.063, ≤0.002-0.5; 0.031/0.063, 0.016–0.125. MPC50/90 and range values respectively were: 0.125/0.25, 0.031–8; 0.125/0.5, 0.031–2; 0.25/0.5, 0.063–0.5. By MIC < 1% of isolates had values ≥1 μg/ml as compared to 4.5% by MPC. The modal MIC was 0.031 μg/ml and 0.125 μg/ml for the MPC. Eight isolates had MPCs ≥2 μg/ ml and had amino acid substitution in either of gyrA, parC or both. For 74 isolates with MPCs to levofloxacin ≥ 4 μg/ml, all had MPCs to GM of ≤0.25 μg/ml and for 58% ≤ 0.125 μg/ml.
Conclusion: GM is a new fluoroquinolone with low MIC and MPC values against SP and 95% of strains–regardless of penicillin susceptibility-had MPCs ≤ 0.5 μg/ml and 91% ≤ 0.25 μg/ml. This data suggests that GM is highly efficacious in vitro against SP and with low MPC values is less likely to select for quinolone resistant SP following drug exposure. No differences were seen in MIC or MPC values between PS, PI, PR strains suggesting no co-resistance with GM. GM retained low MPC values against some organisms with high MPC values to other quinolones.
P1198: In vitro activities of moxifloxacin and ciprofloxacin against Staphylococcus aureus isolates
A. Azap, S. Özkan, H. Aygüin, S. Gül, D. Yagci, O.K. Memikoglu, E. Tekeli (Ankara, TR)
Objective: To determine the in-vitro activities of moxifloxacin and ciprofloxacin against methicillin-susceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA) strains.
Methods: The study was conducted in a University Hospital in Turkey. A total of 440 non-repeat isolates (196 MSSA and 244 MRSA) from various clinical specimens were included in the study. All isolates were identified as S. aureus by phenotypic characteristics, Gram staining, catalase and tube coagulase tests. MICs of the drugs were determined by an agar dilution method, according to the NCCLS criteria. The drugs were obtained from their manufacturer (Bayer Inc). S. aureus ATCC 29213 was used as quality control strain.
Results: Twenty-seven (14%) of 196 MSSA strains and 239 (98%) of 244 MRSA strains were resistant to ciprofloxacin. MIC50 and MIC90 values of 27 ciprofloxacin-resistant MSSA strains for moxifloxacin were 0.25 mg/L and 4 mg/L, respectively. MIC50 and MIC90 values of ciprofloxacin-susceptible MSSA strains for moxifloxacin were ≤0.125 mg/L and 0.250 mg/L, respectively. Moxifloxacin was 4-fold more active than ciprofloxacin against MSSA strains. There was not any difference between these two quinolones against MRSA strains (MIC90s: ≥16 mg/L).
Conclusion: MRSA strains are major causes of nosocomial infections. Despite advances in antibacterial therapy, treatment of infections caused by MRSA is still troublesome. New quinolone-derived compounds such as moxifloxacin are reported to have improved activities against S. aureus including MRSA. In this first study on in-vitro activity of moxifloxacin against S. aureus from Turkey, the moxifloxacin MICs were higher than those reported from different countries. This may be due to excessive quinolone use in our country. According to our findings we conclude that moxifloxacin should not be used in MRSA infections in our setting, but it can be a good alternative to ciprofloxacin in treatment of infections caused by MSSA.
P1199: BIVEMOX III: results of the Belgian in vitro evaluation of moxifloxacin (winter 2003–2004)
J. Verhaegen, M.J. Struelens, H. Goossens, Y. Glupczynski, S. Lauwers, G. Verschraegen, P. De Mol, D. Govaerts, G. Mascart, J. Frans, A. Bousse, S. Vingerhoedt (Leuven, Brussels, Antwerp, Mont-Godinne, Ghent, Montigny-Le-Tilleul, Bonheiden, B)
Objectives: A multicentric study during the winter period of 2003–2004 was performed in Belgium to assess the in-vitro activity of moxifloxacin on S. pneumoniae (Sp), H. influenzae (Hi) and M. catarrhalis (Mc) clinical isolates collected from the respiratory tract by determination of the MIC's using the Etest and to compare these results against 9 other antimicrobial agents. These results were also compared for Sp versus those of the previous study (winter periods 2000–2002) for interpretive criteria S – I – R (according the NCCLS – breakpoints).
Methods: 10 Belgian university and non-university medical microbiology laboratories participated during the past winter period in this multicentre in-vitro evaluation of moxifloxacin. Each laboratory included 40 strains of Sp and 20 strains of Hi and Mc. The total number of evaluable strains (with the exclusion of duplicate isolates) was 758. Testing conditions: Method and antibiotics: susceptibility testing was performed in the participating centres by using the E-test. The antibiotics tested were penicillin, ampicillin, amoxi/clav., doxycycline, clarithromycin, cefuroxime, ceftriaxone, ciprofloxacin, levofloxacin and moxifloxacin. Medium : Sp and Mc : Mueller–Hinton agar with 5% blood; Hi : HTM agar. Inoculum : direct suspension and 0.5 Mc Farland standard. Incubation : 35°C for 24 hours in 5% CO2. Quality control was performed using ATCC reference strains (S. pneumoniae ATCC 49619; H. influenzae ATCC 49766).
Results: See graphs 1 and 2.
| Sp |
Sp |
Mc |
Mc |
Hi |
Hi |
|
|---|---|---|---|---|---|---|
| Antibiotic mg/L | MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 |
| penicillin G | 0.03 | 0.5 | 64 | 64 | 1 | 64 |
| ampicillin | 0.015 | 0.25 | 1 | 4 | 0.5 | 128 |
| amoxi/clav | 0.008 | 0.25 | 0.12 | 0.25 | 1 | 2 |
| cefuroxime | 0.03 | 1 | 1 | 4 | 1 | 4 |
| ceftriaxone | 0.03 | 0.25 | 0.5 | 1 | 0.008 | 0.03 |
| doxycycline | 0.12 | 8 | 0.12 | 0.25 | 1 | 1 |
| clarithromycin | 0.25 | 256 | 0.25 | 0.25 | 32 | 32 |
| ciprofloxacin | 1 | 2 | 0.06 | 0.06 | 0.03 | 0.03 |
| levofloxacin | 1 | 1 | 0.03 | 0.06 | 0.03 | 0.03 |
| moxifloxacin | 0.12 | 0.25 | 0.06 | 0.12 | 0.06 | 0.06 |
| Sp |
|||
|---|---|---|---|
| Antibiotic mg/L | R (%) | I (%) | S (%) |
| penicillin G | 0.7 | 18.1 | 81.2 |
| ampicillin | |||
| amoxi/clav | 0.5 | 1.1 | 98.4 |
| cefuroxime | 7.8 | 2.7 | 89.5 |
| ceftriaxone | 0 | 4.4 | 95.6 |
| doxycycline | 19 | 10.2 | 70.8 |
| clarithromycin | 37.3 | 0.3 | 62.4 |
| ciprofloxacin | |||
| levofloxacin | 0.8 | 0.3 | 98.8 |
| moxifloxacin | 0.5 | 0 | 99.5 |
Conclusions: This follow-up Belgian multicentre study confirms the excellent in-vitro potency of moxifloxacin against clinical isolates of Sp, Hi and Mc and it demonstrates that it is the most potent fluoroquinolone available in Belgium for the treatment of lower respiratory tract infections. According the NCCLS – breakpoints, there are no major S – I – R differences for Sp between these results (2003–2004) and the results of the previous study (2000–2002). This means that the use of new fluoroquinolones like moxifloxacin and levofloxacin has not led, to date, to an increase of resistance in Sp. However, repeated follow-up surveys will continue to be needed in order to assess the activity of fluoroquinolones and to monitor the ecological impact of the recently increased fluoroquinolone usage for respiratory tract infections in Belgium in the forthcoming years.
P1200: Moxifloxacin as an alternative antibiotic in treatment of Porphyromonas gingivalis associated periodontitis – conclusions from in vitro studies
W. Pfister, E. Straube, K.-H. Schmidt, A. Schmitt, T. Seltmann, S. Eick (Jena, D)
Objectives: The objective of several experiments was to evaluate the in vitro activity of moxifloxacin against Porphyromonas gingivalis (P.g.).
Methods: MICs of moxifloxacin against 16 strains of P.g. were determined by E-test (AB Biodisk, Solna, Sweden). Furthermore the spontaneous mutation rate and the induction of resistant strains by the 0.25-fold MIC of the antibiotic were determined. To find the target of resistance fragments of gyrA and gyrB were sequenced. Finally the efficacy of moxifloxacin against P. gingivalis ATCC 33277 considering special conditions such as effects on the strain in a biofilm or within epithelial cells (KB cells) was evaluated.
Results: Moxifloxacin had very low MIC values (ranging from 0.006–0.032 μg/ml), but subinhibitory concentrations of the fluoroquinolone induced very fast mutations. The spontaneous mutation rate was up to 5 ×10−8 after the two-fold MIC and 1.2 × 10−8 after the eight-fold MIC. Often the mutants exhibited a high resistance MICs >32 mg/L. All these mutants bore Ser-83–>Phe substitution in gyrA. The 5-fold MIC eliminated P.g. ATCC 33277 within biofilms after 24 h, and the 100-fold MIC was able to kill all intracellular P. gingivalis within KB cells.
Conclusions: Moxifloxacin showed a very good activity against planctonic P. gingivalis and P.g. within a biofilm. This antibiotic in a higher concentration was also efficient to intracellular bacteria. But a rapid development of resistance was observed in laboratory. Moxifloxacin might be an alternative in the antibiotic treatment of P. gingivalis associated periodontitis, nevertheless clinical studies should focus not only on improvement of clinical parameters but also on occurrence of resistant strains.
P1201: Levofloxacin activity on respiratory isolates of Streptococcus pneumoniae with decreased susceptibility to ciprofloxacin in Spain
J. García-de-Lomas, J.L. Juan-Bañón, C. García-Rey, R. Dal-Ré On behalf of the Spanish Surveillance Group for Respiratory Pathogens
Objectives: To test the activity of levofloxacin against recent respiratory isolates of S. pneumoniae with reduced susceptibility to ciprofloxacin (MIC ≥ 2 mg/L; n = 607) belonging to the national surveillance SAUCE-3 (n = 2721; Nov01–Oct02) and to identify chromosomal mutations in isolates with a levofloxacin MIC ≥ 4 mg/L.
Methods: The activity of levofloxacin was tested by broth microdilution following NCCLS recommendations. Genotypic sequenciation of the QRDR (gyrA, gyrB, parC and pare) was done on all the strains with a levofloxacin MIC ≥ 4 mg/L.
Results: Levofloxacin MIC distribution, MIC50 and MIC90 (in bold) are given in the Table for the whole sample and broken into ciprofloxacin MIC categories. Mutations in gyrA (E85K) were found in 8 (18.6%) strains. No gyrB mutations were found. Mutation in parC occurred in 100% these strains (26 S79F; 12 S79Y; 2 S79I; 1 S79R; 1 D831; 1 D83N). Finally, mutation of pareE was found in 17 (39.5%) strains and all of them had the change I460V. One single parC mutation occurred in 24 (55.8%) strains, two mutations in 15 (34.8%) (3 parC+gyrA and 13 parC+parE), and 3 mutations in parC+parE+gyrA in 5 (11.6%) strains.
| Levofloxacin MIC |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cipro MIC | ≤0.125 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | 32 | %R |
| >2 (n = 607) | 5 (0.8) 37 (6.9) | 344 (63.6) | 164 (90.6) | 12 (92.6) | 13 (94.5) | 23 (98.5) | 8 (99.8) | 1 (100) | (5.3) |
| >4 (n = 127) | 3 (2.4) | 22 (19.7) | 46 (55.9) | 11 (64.6) | 13 (74.8) | 23 (92.9) | 8 (99.2) | 1 (100) | (25.2) |
| 2 (n = 480) | 5 (1.0) 34 (8.1) | 322 (75.2) | 118 (99.8) | 1 (100) | (0.0) | ||||
| 4 (n = 55) | 1 (1.8) | 17 (30.9) | 32 (90.9) | 1 (92.7) | 4 (100) | (0.0) | |||
| >8 (n = 72) | 2 (2.8) | 5 (9.7) | 14 (29.2) | 10 (43.1) | 9 (55.6) | 23 (87.5) | 8 (98.6) | 1 (100) | (44.4) |
Conclusions: 1) Levofloxacin MIC50 and MIC90 for pneumococcal strains with decreased susceptibility to ciprofloxacin were 0.5 and 1 mg/L, respectively. Resistance to levofloxacin (MIC ≥ 8) occurred in 32 isolates (1.2% of the SAUCE-3 collection). 2) Activity of levofloxacin was negatively affected only among pneumococcal isolates with a very high MIC of ciprofloxacin (≥8 mg/L). In this case, levofloxacin MIC50 and MIC90 were 4 and 8, respectively, and 44.4% of these strains were resistant to levofloxacin. 3) All sequenced strains with a levofloxacin MIC ≥ 4 mg/L had a mutation in the parC gene (single in 56% strains), but none of them in the gyrB. The most common mutations identified were parC/S79F, parE/I460V, parC/S79Y and gyrA/E85K. 4) One single parC mutation was found in 62% and 22% strains with a levofloxacin MIC ≤8 and ≥16 mg/L, respectively.
P1202: Application of PK/PD modelling and simulation (M+S) to define pharmaco-dynamic breakpoints for fluoroquinolones
H. Stass, A. Bauernfeind, I. Schneider, A. Dalhoff (Wuppertal, Munich, D)
Background: We studied the application of PK/PD modeling techniques as an alternative method to define pharmacodynamic breakpoints complementary to conventional microbiological breakpoints for fluoroquinolones (FQs).
Methods: 8 Staphylococcus aureus strains with MICs ranging from 0.03–8 mg/L were exposed to fluctuating concentrations of Levo- (LFX) Gati- (GFX) and Moxifloxacin (MFX) mimicking their total serum concentration profiles following oral doses of 400 mg MFX, 400 mg GFX, 500 and 750 mg LFX over 24 h using the sedimentation model. Strains were cultivated in Brain Heart infusion broth at 37°C. Viable counts were quantitated at 14 sampling points. As PD-measure the AUBKCnorm (i.e. Area Under the Bacterial Kill Curve normalized to the initial inoculum [h]; AUBKCnorm <24 indicates a bactericidal activity, >24 bacterial growth) was determined for the time kill experiment and plotted as a function of MIC for each treatment.
Results: The AUBKCnorm vs MIC function was similar for all treatments following a bimodal profile. While the slope of all FQs studied was shallow for MICs below 1 mg/L with AUBKCnorm <5 h, AUBKCnorm started increasing steeply beyond this point. It intercepted the 24 cut off line at concentrations of 1.5 mg/L for LFX 500 mg, 2 mg/L for GFX, 2.4 mg/L for MFX and 3.1 mg/L for LFX 750 mg. This indicates that S. aureus with susceptibilites beyond these MICs would no longer be eradicated by the corresponding treatments. Thus, according to our investigations a breakpoint for FQs integrating both microbiological and clinical pharmacokinetic relation-ships results in a value of 1 mg/L for LFX 500 mg, and 2 mg/L for MFX, GFX, and LFX 750 mg.
Conclusion: Pharmacodynamic breakpoints determined by PK/PD M+S which are taking into respect the fluctuating concentration time profiles encountered in patients are suitable surrogates complementing the data obtained in microbiological experiments.
P1203: A multicentre agar and broth dilution susceptibility testing study of fluoroquinolones against the Bacteroides fragilis group
K.E. Aldridge, D. Snydman, D. Hecht, C. Edlund, J. Herrington (New Orleans, Boston, Chicago, USA; Stockholm, S; West Haven, USA)
Objectives: The development of fluoroquinolones (FQ) antimicrobials has resulted in effective therapy for a variety of infections due to aerobic and facultatively anaerobic gram-positive and -negative pathogens. FQ activity against anaerobes has not been as promising with only trovafloxacin receiving FDA approval for anaerobic infections. Moreover, more recent reports of increased resistance to FQ among the B. fragilis group has prompted interested to determine if these increases are due to susceptibility testing methodology problems. This study was designed to compare the susceptibility results from five laboratories that tested the same 70 isolates against FQ using agar dilution(AD) and broth microdilution (BMD) testing.
Methods: Seventy clinical isolates of the B. fragilis group identified by only a sequential number were distributed to each of the five participating laboratories. Four of the laboratories performed AD and one laboratory performed BMD susceptibility testing using NCCLS recommendations including breakpoints where appropriate. Serial two-fold dilutions of moxifloxacin (MOX), gatifloxacin (GATE), trovafloxacin (TROV), and metronidzaole (METRO) were prepared in the test medium within a range of 0.03 to 64 mg/L. Plates were inoculated with 1 × 105 CFU per spot or well, incubated anaerobically for 48 hours and the MIC read. QC was performed using NCCLS-recommended ATCC strains.
Results: MIC values for each antimicrobial were collated as MIC90 and per cent (%) of isolates inhibited at ≤2 and ≤4 mg/L:
| MOX |
TROV |
GATE |
METRO |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC90 | 2 | 4 | MIC90 | 2 | 4 | MIC90 | 2 | 4 | MIC90 | 2 | 4 | |
| Lab 1 | 16 | 56 | 64 | 8 | 66 | 87 | 16 | 43 | 60 | 1 | 100 | 100 |
| Lab 2 | 16 | 57 | 67 | 4 | 63 | 91 | 32 | 49 | 56 | 2 | 96 | 100 |
| Lab 3 | 16 | 50 | 67 | 8 | 43 | 77 | 32 | 39 | 59 | 1 | 100 | 100 |
| Lab 4 | 16 | 50 | 64 | 8 | 49 | 64 | 16 | 43 | 59 | 1 | 100 | 100 |
| Lab 5 | 8 | 64 | 74 | 4 | 60 | 34 | 16 | 54 | 63 | 2 | 100 | 100 |
Conclusions: These data indicate that inter-laboratory testing of the same test isolates gave very similar results for each antimicrobial. BMDgave slightly lower MIC results than AD but was not significantly different. We conclude that susceptibility methodology is not responsible for unusually high resistance rates.
P1204: Global evaluation of gemifloxacin activity tested against community-acquired respiratory tract pathogens, Haemophilus influenzae and Moraxella catarrhalis (1999–2004)
J. Ross, D. Biedenbach, T. Fritsche, H. Sader, R. Jones (North Liberty, USA)
Objectives: Chronic lower respiratory tract disease and pneumonia are among the top ten leading causes of death in the United States. As resistance (R) to commonly used drug classes continues to increase, the newer generation fluoroquinolones (FQs) have provided an excellent therapeutic alternative for community-acquired respiratory tract infections (CARTI). The potency of gemifloxacin(GEMI) against H. influenzae and M. catarrhalis isolates was determined over a period of six years.
Methods: A total of 12,152 isolates of H. influenzae (9,411), M. catarrhalis (2,741) and other Haemophilus spp. (66; not presented) were collected during 1999–2004 from North America, Latin America and Europe. Reference NCCLS test methods were utilized and MIC results were interpreted by current breakpoint criteria M100-S15 (2005). Comparison agents included: ciprofloxacin (CIPRO), levofloxacin (LEVO), gatifloxacin (GATI), and moxifloxacin (MOXI).
Results: H. influenzae and M. catarrhalis susceptibilities (S) to GEM I have not changed over the last six years. GEMI had equal or greater potency when compared to other FQs. H. influenzae isolates tested showed >99.9% S to GEMI (MIC90 from on-scale values, 0.004 mg/L). In 2003 and 2004, CIPRO, GATI, LEVO, and MOXI showed complete S among H. influenzae isolates, but some had higher MIC values indicating single-step QRDR mutations (MIC ≥ 0.12 mg/L). One H. influenzae isolate was R to all FQs tested (MIC values: GEMI 2, CIPRO >4, LEVO >4, GATI >4, MOXI >4 mg/L) and had multiple QRDR mutations. The number of beta-lactamase (BL)-negative/ampicillin-R isolates recovered in this study was only 7 or 0.1% overall. GEMI shows similarly high potency against M. catarrhalis with the highest observed MIC at 2 mg/L (1999–2002); >99.9% were at ≤0.12 mg/L
| MIC 50/10» in mg/L (%S) |
|||||
|---|---|---|---|---|---|
| Organism/year (no. tested) | GEMI | CIPRO | LEVO | GATI | MOXI |
| H. influenzae | |||||
| 1999-2002 (6213) | ≤.008/2 (>99) | ≤.03/4 (>99) | ≤.03/>4 (>99) | ≤.03/>4 (>99) | ≤.03/>4 (>99) |
| 2003 (1854) | ≤.002/.12 (100) | ≤12/.5 (100) | ≤.03/.12 (100) | ≤.03/.12 (100) | ≤.03/.12 (100) |
| 2004 (1344) | ≤.016/.03 (100) | ≤.03/.25 (100) | ≤.03/.25 (100) | ≤.03/.12 (100) | ≤.03/.25 (100) |
| BL-Negative | |||||
| 1999-2002 (4841) | ≤.008/2 (>99) | ≤.03/4 (>99) | ≤.03/>4 (>99) | ≤.03/>4 (>99) | ≤.03/>4 (>99) |
| 2003 (1423) | ≤.002/.12 (100) | ≤12/.5 (100) | ≤.03/.12 (100) | ≤.03/.12 (100) | ≤.03/.12 (100) |
| 2004 (1037) | ≤.016/.03 (100) | ≤.03/.25 (100) | ≤.03/.25 (100) | ≤.03/.12 (100) | ≤.03/.25 (100) |
| BL-Positive | |||||
| 1999-2002 (1286) | ≤.008/25 (>99) | ≤.03/.25 (100) | ≤.03/.25 (100) | ≤.03/.12 (100) | ≤.03/.25 (100) |
| 2003 (402) | ≤.002/.03 (100) | ≤12/≤.12 (100) | ≤.03/.06 (100) | ≤.03/≤.03 (100) | ≤.03/.06 (100) |
| 2004 (307) | ≤.016/.03 (100) | ≤.03/.06 (100) | ≤.03/.06 (100) | ≤.03/≤.03 (100) | ≤.03/.25 (100) |
| M. catarrhalis | |||||
| 1999-2002 (2473) | .008/2 (NA) | ≤.03/.5 (NA) | ≤.03/1 (NA) | ≤.03/.25 (NA) | .06/.12 (NA) |
| 2003 (268) | ≤.12/≤.12 (NA) | ≤.03/≤.12 (NA) | ≤.03/.06 (NA) | ≤.03/.06 (NA) | .06/.12 (NA) |
Conclusions: GEMI continues to be a highly potent FQ when tested against the two most commonly isolated Gram-negative CARTI pathogens; H. influenzae and M. catarrhalis. This potency and spectrum was consistent across six years and three continents.
P1205: Norfloxacin as a marker of decreased susceptibility to fluoroquinolones in enterobacteria using the Vitek 2 system
L. López, J. Alcala, F. Torres, E.J. Perea, A. Pascual (Seville, E)
Objective: The detection of Nalidixic acid resistance acquires importance in enterobacteria since already resistant strains develop more frequently resistance to fluorquinolones than susceptible strains. Many clinical laboratories have incorporated the VITEK 2 system because their benefit in routine, but Nalidixic testing is not included for enterobacteria cards. The aim of this study was the use of Norfloxacin VITEK MICs value as alternative marker to detect Nalidixic acid resistant enterobacteria strains.
Material and methods: A total of 1013 isolates of Enterobacteriaceae were analyzed and routinely inoculated into the VITEK 2 ID-GNB and AST-N020 cards (bioMérieux) and then loaded into the VITEK 2 system, as recommended by the manufacturer. Ninety-six strains with a higher Norfloxacin VITEK MIC value (1–4 mg/L), but still within the susceptibility range established by the NCCLS breakpoints, and 100 strains with a Norfloxacin VITEK MIC ≤0.5 mg/L were selected. They were further tested with a 30 microg-Nalidixic acid-disk (Nal) (Oxoid) according to NCCLS reference.
Results: The Norfloxacin 1–4 mg/L and susceptible to ciprofloxacin phenotype represented the 9% of total isolates loaded in the VITEK system during the study, similar to the prevalence observed in previous analysis in Spain. Both selected groups, one with the highest and the other with the lowest Norfloxacin VITEK MIC value, included 60% and 58% E. coli isolates, 8% and 20% S. enterica isolates, respectively. Among the Norfloxacin VITEK MIC 1–4 mg/L strains 93 isolates (98%) were Nal resistant, and 76 (79%) were ciprofloxacin susceptible. The agreement between Norfloxacin VITEK MIC ≤0.5 mg/L and Nal susceptibility was foun in 97 (97%) strains. Two isolates (one E. cloacae and one K. pneumoniae) with Norfloxacin VITEK MIC 1–4 mg/L were Nal-S and 3 isolates (two E. coli and one P. mirabilis) with Norfloxacin VITEK MIC ≤0.5 mg/L were Nal-R.
Conclusion: When using VITEK 2 system for enterobacteria, the consideration of MIC of norfloxacin >0.5 mg/L could be an alternative marker of nalidixic acid resistance (and decreased susceptibility to fluoroquinolones).
Antibacterial susceptibility studies – I
P1206: Ceftazidime, glycopeptides and azithromycin in combination against P. aeruginosa
B. Repetto, S. Roveta, E.A. Debbia, D.L. Rocca, A. Marchese (Genoa, I)
Objectives: P. aeruginosa is an important nosocomial pathogen, which causes serious and often lethal infections in immunocompromised hosts. This pathogen is intrinsically resistant to many antibiotics and can easily develop resistance towards many currently available agents. Natural resistance can be attributed to the low permeability of the P.aeruginosa outer membrane to a variety of antibiotics including glycopeptides (GLYs). Since GLYs are powerful antibiotics against gram-positive bacteria and resistance is very rarely develop, it seemed interesting to evaluate the effect of combining these antimicrobial agents with antibiotics that might disorganize the structure of the outer membrane allowing the entrance of glicopeptides into the gram-negative cells. In order to verify this hypothesis, ceftazidime (CAZ) has been tested in association with vancomycin (VAN) or teicoplanin (TEI). The same experiments have been carried out also in the presence of azithromycin (AZI), which is normally a non anti-pseudomonal agents but has been shown to interfere with some virulence factors.
Methods: A bacterial suspension of about 109 CFU/ml was seeded on plates containing a fixed concentration of GLYs (500 mg/l) and increasing doses (2x,4x,8x,16x) of CAZ. Survivors were counted after 48 hr at 37°C. Results were interpreted as synergism (99%), additivity (90%), and indifference (10%) of the CFU/ml reduction found in the drugs combination in comparison to the drug alone. The same experiments have been repeated adding AZI (16 mg/l) and using GLYs at concentrations ranging from 500 to 300 mg/l.
Results: CAZ in combination with GLYs reacted synergically in 20 out of 59 cases, additivity was found in 31/59 interactions and indifference was noted in 8/59 tests. Preliminary results (12 tests performed) indicated that the addition of AZI increased the incidence of synergisms and additivities even when using GLYs concentration of 300 mg/l.
Conclusions: CAZ combined with GLYs gave additive or synergistic results in the great majority of experiments, while the simultaneous combination of AZI, CAZ and a GLY always produce an additive or synergistic effect against P. aeruginosa. These data, given the high concentration of GLYs employed, could be of particular interest in clinical situations where the drugs could be topically administered.
P1207: A multicentre correlation study of VITEK 2 with reference methods for telithromycin, mupirocin, and daptomycin against Staphylococcus spp.
K.E. Aldridge, A. Dizney, K. Thomson, G. Procop (New Orleans, Omaha, Cleveland, USA)
Objective: Clinical studies have shown that appropriate antimicrobial therapy based on in vitro susceptibility data correlates with better patient outcome. VITEK 2 is a fully automated susceptibility testing methodology providing rapid(6–8 h) results for a variety of aerobic and facultatively anaerobic Gram-positive and -negative pathogens which have been shown to correlate to established reference methods. The objective of this study was to correlate the susceptibility results of Vitek 2 testing of telithromycin, mupirocin, and daptomycin against Staphylococcus spp. with those from reference methodology.
Methods: Three geographically distinct clinical microbiology laboratories participated in the testing with each site testing 100 consecutive clinical islates and 84 blinded challenge isolates of staphylococci sent to each site. VITEK 2 testing was performed according to the manufacturer's recommendations. The challenge isolates were also tested using a manual preparation of the inoculum. NCCLS recommended reference agar and broth microdilution methods were used to test telithromycin, mupirocin, and daptomycin. MIC results were collated to determine the per cent (%) of isolates susceptible(S), intermediate(I), and resistant(R) based on CA-SFM, BSAC, and NCCLS recommended breakpoints. Essential(EA) and categorical(CA) agreements were then determined.
Results: For telithromycin the MIC values indicated S, I,&R %s of 79.5,0.6, and 20.9 for clinical isolates and 76.2, 1.2, and 22.6 for the challenge isolates.EA and CA with reference methods were 100% for clinical isolates and 97.6% and 98.8% for challenge isolates. Overall for telithromycin the EA and CA were 99.5% and 99.7%. For mupirocin the MIC values indicated S and R %s of 88.5 and 11.5 for clinical isolates and 98.8 and 1.2 for the challenge isolates. EA and CA were 99.7% and 99% for clinical isolates and 100% for the challenge isolates. Overall the EA and CA for mupirocin were 99.7% and 99.2% respectively. 100% of isolates were S to daptomycin. EA was 98% for clinical isolates; 99.1% for challenge isolates; and overall was 98.2% for daptomycin.
Conclusion: Using both clinical and challenge isolates of Staphylococcus spp. VITEK 2 results showed a high correlation with reference method results for each agent. EA and CA significantly exceeded regulatory requirements for equivalence between VITEK 2 and reference methodologies.
P1208: In vitro efficacy of tigecycline tested against community-acquired respiratory tract infection and nosocomial pneumonia pathogens
R. Jones, M. Stilwell, H. Sader, T. Fritsche (North Liberty, USA)
Objective: To compare and contrast the pathogens involved in CARTI and NP cases when tested against tigecycline, a novel glycylcycline (formerly GAR936). All MIC tests were performed by reference broth microdilution methods to determine susceptibility (S) and resistance (R).
Methods: The organisms numbered 9,347, a total of 2,004 from NP and 7,343 from CARTI. The most frequent CARTI pathogens were: S. pneumoniae (SPN; 2,865), H. influenzae (HI; 4,011) and M. catarrhalis (MCAT; 607). The rank order of NP isolates was: S. aureus (SA; 56.9%), P. aeruginosa (PSA; 13.9%), SPN (5.8%), Klebsiella spp. (KSP; 3.4%), Enterobacter spp. (ENT; 3.1%), Acinetobacter spp. (AC; 2.6%), E. coli (EC; 2.4%), S. maltophilia (SM; 1.6%), beta-streptococci (BST; 1.5%) and Serratia spp. (SER; 1.2%). All tests were NCCLS (M7-A7) interpreted using M100-S14.
Results: The characteristics of the organism collection were (CARTI/NP isolates): SPN PEN-R (34/41%); HI AMP-R (22/19%) and clarithromycin-R (13%/ND); and MCAT beta-lactamase-positive (96%/ND). Tigecycline MIC results are found in the table: PSA was less tigecycline-S (MIC90, 16 mg/L), but all ESBL-producing KSP and EC had tigecycline MICs at ≤2 mg/L and tetracycline-R strains were also tigecycline-S.
| MIC50/90 (mg/L) |
|||
|---|---|---|---|
| Organism (CARTI/NP) | CARTI | NP | %≤2/≤4 mg/L |
| SPN (2.748/117) | ≤0.12/≤0.12 | ≤0.12/≤0.12 | 100/100 |
| HI (3.995/16) | 0.5/1 | 0.5/1 | 100/100 |
| MCAT (600/7) | ≤0.12/0.25 | 0.25/- | 100/100 |
| SA (−/1.140) | – | 0.25/0.5 | 100/100 |
| KSP (−/69) | – | 0.5/1 | 96/100 |
| ENT (−/63) | – | 0.5/2 | 98/100 |
| AC (−/53) | – | 1/4 | 85/100 |
| EC (−/49) | – | 0.25/0.5 | 100/100 |
| SM (−/32) | – | 1/2 | 88/100 |
| β St (−/30) | – | ≤0.12/≤0.12 | 100/100 |
| SER (−/24) | – | 1/4 | 75/92 |
Conclusions: Tigecycline in vitro activity against CARTI and NP pathogens was high, showing potency against R phenotypes of SP, HI, Enterobacteriaceae and some difficult to treat non-fermentative Gramnegative bacilli. Empiric parenteral application of tigecycline for serious pneumonia cases appears prudent for patients less likely to have PSA as the causative pathogen or as directed therapy of S organisms.
P1209: Activity of tigecycline tested against an international collection (1999-2003) of resistant bacterial pathogens
T. Fritsche, H. Sader, R. Jones (North Liberty, USA)
Objective: To evaluate the activity and potency of tigecycline (TIG) when tested against a large international collection of common bacterial pathogens displaying increasing and worrisome resistance (R) profiles. TIG is a novel glycylcycline derivative of minocycline that has demonstrated activity against a variety of Grampositive and -negative pathogens, making it an attractive candidate for treatment of community-acquired pneumonia, mixed aerobic/anaerobic infections and SSTI.
Methods: Non-duplicate clinically-significant bacterial isolates (10,275 strains) were collected from 2000 to 2004 in >70 medical centres participating in the global TIG surveillance program. Isolates originated from North America (39%); Europe (41%); Latin America (18%); and the Asia-Australia (2%). All isolates were tested using NCCLS broth microdilution methods against TIG and representative comparator agents including ciprofloxacin (CIP) and tetracycline (TET).
Results: TIG results for the R organism subsets are in the Table: TIG was highly active (MIC50 and 90, ≤0.25 and ≤0.5 mg/L, respectively) against all resistant SA, CoNS, ESP, SPN and VGS with >99% of strains inhibited by ≤2 mg/L. While potency of TIG against R subsets of ENT was less (MIC50 and 90, ≤0.5 and ≤4 mg/L, respectively), the vast majority of TET-R isolates remained S to TIG (>98% of isolates were inhibited by ≤4 mg/L). No geographic differences in TIG potency among ESBL-producing, CIP-R or TET-R ENT strains were noted.
| MIC (mg/L) |
% inhibited at MIC (mg/L) |
||||
|---|---|---|---|---|---|
| Organism (# tested) | 50% | 90% | ≤ 1 | ≤ 2 | ≤ 4 |
| S. aureus (SA) | |||||
| Oxacillin-R (3,867) | 0.25 | 0.5 | >99 | 100 | – |
| TET-R (1,138) | 0.25 | 0.5 | >99 | 100 | – |
| Coag neg staphylococci (CoNS) | |||||
| Oxacillin-R (3,887) | ≤ 0.12 | 0.5 | >99 | 100 | – |
| TET-R (1,138) | ≤ 0.12 | 0.5 | >99 | 100 | – |
| Enterococcus spp. (ESP) | |||||
| Van A (520) | ≤ 0.12 | 0.25 | 100 | – | – |
| Van B (95) | ≤ 0.12 | 0.25 | 100 | – | – |
| S pneumoniae (SPN) | |||||
| Penicillin-R (570) | ≤ 0.12 | 0.12 | >99 | 100 | – |
| CIP-R (171) | ≤ 0.12 | ≤ 0.12 | 99 | 100 | – |
| TET R (733) | ≤ 0.12 | ≤ 0.12 | >99 | >99 | >99 |
| Viridans group streptococci (VGS) | |||||
| Penicillin-R (28) | ≤0.12 | 0.12 | 100 | – | – |
| Enterobacteriaceae (ENT) | |||||
| TET-R (2,829) | 0.5 | 4 | 77 | 88 | 98 |
| CIP-R (1,055) | 0.25 | 2 | 82 | 91 | 98 |
| E. coli ESBL (279) | 0.25 | 0.5 | >99 | >99 | 100 |
| Kiebsiella spp. ESBL (317) | 0.5 | 2 | 86 | 95 | 100 |
| Total % Inhibited | – | – | 94 | 97 | >99 |
Conclusions: Among R subsets of commonly occurring pathogens, 97% were inhibited by ≤2 mg/L of TIG and >99% were inhibited by ≤4 mg/L (the current NCCLS breakpoint for TET). TIG is highly stable to most TET-R determinants, including protected ribosomes and efflux mechanisms, and may represent a superior choice among parenteral agents for broad-spectrum coverage, including the most commonly occurring- and problematic-R phenotypes.
P1210: Determination of the minimum inhibitory and mutant prevention concentration of telithromycin against clinical isolates of Streptococcus pneumoniae
S. Borsos, C. Hesje, L. Blondeau, J. Blondeau Saskatoon, CAN
Objective: Telithromycin (TL) is a novel ketolide antimicrobial agent that has recently been approved for use in North America for respiratory tract infections of which SP is a principal pathogen. The global escalation of penicillin (P) and macrolide (M) resistant SP has compromised the use of beta-lactam and macrolide compounds. TL was reported to be active against P and M resistant SP. The MPC defines the antimicrobial drug concentration required to prevent the outgrowth of resistant subpopulations from high density bacterial cultures. We tested TL by both MIC and MPC against clinical isolates of SP -- including P and M resistant strains.
Methods: MIC testing was by microbroth dilution (utilizing 100,000 cfu/ml) with Todd-Hewitt broth in accordance with NCCLS guidelines. For MPC testing ≥1 billion organisms were applied to agar plates containing 2 fold concentration increments of TL and incubated at 35–37°C and 5% CO2 and screened for growth at 24 and 48 hours. The lowest drug concentration preventing growth was recorded as either the MIC or MPC depending on the assay.
Results: To date, 372 clinical SP isolates were tested by MIC and 245 by MPC. By MIC testing the MIC50/90 and range values were 0.008/0.063 μg/ml and 0.002–1 μg/ml respectively. The modal MIC value was 0.08 μg/ml and 88% of strains were inhibited by ≤0.016 μg/ml. For MPC testing, MPC50/90 and range values were 0.031/0.25 μg/mland ≤0.008- >0.5 μg/ml respectively. The modal MPC value was 0.031 μg/ml and 84% of strains were inhibited by ≤0.125 μg/ml and 97% by ≤0.5 μg/ml. Both MIC and MPC values were elevated against strains that were macrolide resistant–MIC50/90 0.063/0.25 μg/ml; 0.25–0.5/≥ 0.5 μg/ml. Achievable TL drug concentration in serum, epithelial lining fluid, white blood cells, alveolar macrophages and bronchial mucosa would exceed the MPC90 values by 9x, 5x, 56x, 164x, 3x respectively and MIC90 values by 36x, 18x, 223x, 651x, 12x respectively.
Conclusion: TL is highly active against SP -- including strains that are macrolide resistant. By MPC testing, TL was highly active with 90% of strains having MPCs ≤0.25 μg/ml. This data suggests that TL is useful for treating SP infections and has a lower propensity to select for resistant subpopulations and achieves drug concentrations in various compartments that exceed the MPC90 values by 3 to 164x.
P1211: Determination of the minimum inhibitory concentration and mutant prevention concentration of garenoxacin against over 500 clinical isolates of Streptococcus pneumoniae
J. Blondeau, S. Borsos, P. Hedlin, G. Hansen, M. Brandt (Saskatoon, CAN)
Objectives: Garenoxacin (GRN) is an investigational des-F(6)-quinolone with enhanced in vitro activity against gram-positive cocci. The global escalation in antimicrobial resistance amongst respiratory tract pathogens –particularly SP-has highlighted the importance of quinolone compounds for treating SP infections. The mutant prevention concentration (MPC) is a novel in vitro measurement that defines the drug concentration threshold that would require an organism to simultaneously acquire two or more resistance mutations for growth in the presence of the drug. We measured the MICs and MPCs for GRN against clinical isolates of SP, including multidrug resistant strains and those with elevated MPCs to levofloxacinGRN.
Methods: Microbroth dilution in accordance with NCCLS guidelines was followed for MIC testing using Todd-Hewitt broth and two-fold concentration drug increments. For MPC testing, ≥1 billion organisms were applied to agar plates containing GRN, incubated at 35–37°C and 5% CO2 and screened for colony growth at 24 and 48 hours. The MPC was the lowest drug concentration that completely prevented growth. Select organisms with GRN MPC values >2 μg/ml were screened for amino acid substitution in the quinolone resistance determining region.
Results: For 524 strains the MIC50/90 and range values, respectively were 0.063/0.125 μg/ml and ≤0.008-2 μg/ml and not different against penicillin or macrolide resistance strains. For 99% of strains, MICs were ≤0.25 μg/ml. For the 516 strains tested by MPC, the MIC50/90 and range values respectively were 0.125/0.5 μg/ml and ≤0.031– ≥2 μg/ml. For 97% of strains, MPC values were ≤0.5 μg/ml. MIC and MPC values were not impacted by SP resistance to beta-lactams, macrolides, tetracycline or trimethoprim/sulfamethoxazole. For 98 isolates that had MPC values to levofloxacin ≥4 μg/ml, 92 (94%) had GRN MPCs GRN of ≤0.5 μg/ml and of these, 73 (75%) were ≤0.25 μg/ml. Based on achievable and sustainable serum drug concentration, GRN drug concentrations in serum would be expected to remain above the MPC90 value for >24 hours.
Conclusion: GRN exhibits potent activity against SP, as measured by both MIC and MPC, and is active against strains with high MIC/MPC values for other quinolones. GRN is less likely to select for quinolone resistant SP isolates and may be useful for therapy in patients infected with an organism resistant to other quinolones.
P1212: Killing of Streptococcus pneumoniae by azithromycin, clarithromycin, telithromycin and gemifloxacin using the minimum inhibitory and mutant prevention drug concentrations
J. Blondeau, S. Borsos (Saskatoon, CAN)
Objective: SP continues to be a significant respiratory pathogen & increasing antimicrobial resistance has compromised the use of beta-lactam & macrolide compounds. Bacterial eradication impacts on clinical outcome & as bacterial load at the site of infection exceeds the inoculum used in standardized susceptibility testing, elimination of higher organism numbers is necessary for successful therapy. We determined the killing of macrolide & quinolone susceptible SP by Az, CL, TL & GM against a range of bacterial inoculums using the MIC & MPC drug concentrations.
Method: The MICs were determined by microbroth dilution in accordance with NCCLS guidelines. For MPC testing, ≥1 billion organisms were inoculated to agar plates containing drug & incubated & read at 24 & 48 hours. The MIC & MPC were recorded as the lowest concentration showing no growth. For kill experiments, 1 million–1 billion colony forming units (cfu/ ml) were exposed to drug & sampled at 0, 30 min, 1, 2, 3, 4, 6, 12 & 24 hours following drug exposure & log10 reduction & % reduction in viable cells recorded.
Results: The MIC/MPC (μg/ml) values for Az, CL, TL & GM were 0.063/0.5, 0.031/0.5, 0.008/0.016 & 0.031/0.25 respectively. Exposure of 1 million–1 billion cfu/ml to the MIC drug concentration resulted in +0.38 to) 0.65 log10 reduction by 6 hours with Az as compared to +0.12 to −1.11 for CL, +0.43 to) 0.74 for TL & +0.07 to) 4.64 for GM (biggest decrease over 6 hours). Significant log10 reductions occurred by 12 & 24 hours for all drugs. Following exposure of 1 million–1 billion cfu/ml to MPC drug concentration resulted in the following log10 reduction by 6 hours of drug exposure: Az −0.10 to −3.72; CL −0.02 to −3.77; TL +0.36 to −0.89; GM −0.30 to -5.03 (biggest decrease over 6 hours). A ≥3 log10 reduction in viable cells was seen for all drugs following 12–24 hours of drug exposure.
Conclusion: Bacterial load at the site of infection may range from 1 million–1 billion organisms & kill experiments utilizing higher bacterial inoculums provided a more accurate measure of antibiotic performance in high biomass situations. It has been previously established that a 3 log10 reduction in viable cells is indicative of bactericidal activity. All agents tested achieved ≥3 log reduction by 12–24 hours & kill was greater & fastest with MPC versus MIC drug concentrations. This data suggests that dosing to achieve MPC drug concentration results is more rapid & thorough killing.
P1213: Effect of the efflux pump inhibitors on the MIC of quinolones for MDR strains of non-fermentative Gram-negative rods
A.E. Laudy, I. Wojtal, E. Witkowska, B.J. Starosciak (Warsaw, PL)
Fluoroquinolones are a therapeutic option in treatment of infections caused by non-fermentative Gram-negative bacteria. However, resistance to these antibiotics rapidly increase in clinical isolates. The efflux mechanism is the most common cause of multidrug resistance of strains P. aeruginosa, A. baumanii and S. maltophilia. These MDR pumps belonging to the RND family are inhibited by Phe-Arg-beta-naphthylamide [MC207,110]. However, different results of reserpine effect on the activity of RND pumps was established. In our study, we searched for effect of the efflux pump inhibitors (MC207,110, reserpine and rescinnamine) on the MIC of quinolones for MDR clinical isolates of P. aeruginosa, A. baumanii and S. maltophilia. We looked for a interdependence between structure of quinolones and ability of tested inhibitors to inhibit efflux of these antibiotics.
Results: The MDR strains were resistant to all tested quinolones (nalidixic acid-NAL, pipemidic acid-KP, norfloxacin-NOR, ciprofloxacin-CIP and ofloxacin-OF). Among studied inhibitors only MC207,110 affected the susceptibility of all tested strains to quinolones, first of all to NAL. Effect of MC207,110 on the MIC depended on its concentration, but did not depend on the temperature. For majority of P. aeruginosa and A. baumanii strains the MIC of all quinolones decreased in the presence of MC207,110. The highest decrease of the MIC of quinolones was obtained for P. aeruginosa (4–512-fold). For A. baumanii strains the MIC of KP, NOR, CIP and OF decreased only from 2- to 4-fold but the MIC of NAL decreased to 16-fold. Moreover, the presence of this inhibitor increased the sensitivity of 80% of S. maltophilia only to NAL (4- to 16-fold). Reserpine and rescinnamine did not effect on the MIC of quinolones for all studied MDR strains. However, reserpine alkaloides showed inhibitors activity against control strains of S. aureus (decrease MIC of NOR).
Conclusions: Our data confirm that MC207,110 inhibited efflux pumps not only in P. aeruginosa but also in A. baumanii and S. maltophilia strains. Additionally, obtained results suggested possibility that for quinolones, depending on their structure, are different binding sites in efflux pumps. Furthermore, probably also MC207,110 binds to specific site of pumps depending on the efflux systems. So, the effect of this inhibitor on MIC of quinolones depends on genus of bacteria, kind of pumps and structure of agents.
P1214: In vitro activity of fucidic acid against Staphylococcus aureus strains
A. Azap, H. Aygun, S. Özkan, G.Y. Bozkurt, H. Sahintürk, A. Genc, O.K. Memikoglu, E. Tekeli (Ankara, TR)
Objective: This study was undertaken to investigate the in vitro susceptibility of Staphylococcus aureus strains to fusidic acid.
Methods: A total of 440 S. aureus [244 methicillin-susceptible S. aureus (MSSA) and 196 methicillin-resistant S. aureus (MRSA)] strains isolated from various clinical specimens were included in the study. All isolates were identified as S. aureus by phenotypic characteristics, Gram staining, catalase and tube coagulase tests. Minimal inhibitory concentrations (MICs) were determined by agar dilution method, according to the NCCLS criteria. The drug was obtained from the manufacturer. S. aureus ATCC 29213 was used as quality control strain. Strains with MIC value of ≥2 mg/ L were interpreted as resistant to fusidic acid according to the British and French guidelines.
Results: None of the MSSA strains were found to be resistant while 2 (0.8%) of 244 MRSA strains were resistant and 4 (1.6%) were intermediate to fusidic acid. MIC50 and MIC90 values were ≤0.125 mg/L for both MSSA and MRSA.
Conclusions: Staphylococci cause both community acquired and nosocomial infections. Methicillin resistance makes this organism difficult-to-treat. Community acquired MRSA is a great concern nowadays because the therapeutical alternatives are limited. Fusidic acid inhibits protein synthesis. It has only a few side effects and is usually well-tolerated by patients as an oral drug. Fusidic acid can be considered as an alternative drug for the treatment of infections due to both methicillin susceptible and resistant S. aureus strains.
P1215: Evaluation of synergy between glycopeptides, levofloxacin and beta-lactams against methicillin-resistant Staphylococcus aureus
L. Drago, E. De Vecchi, L. Nicola, L. Tocalli, M.R. Gismondo (Milan, I)
Objectives: Aim of the study was in vitro evaluation of different combinations of antibiotics used in the treatment of hospital acquired pneumonia caused by methicillin resistant Staphylococcus aureus (MRSA).
Methods: Double drugs combinations [levofloxacin (LVX) and cefotaxime (CTX) with VA/TP and triple combinations (LVX + amikacin (AMK) + VA/TP, LVX + ceftazidime (CAZ) + VA/TP, LVX + cefepime (CPM) + VA/TP, LVX + imipenem (IMI) + VA/TP, LVX + piperacillin/tazobactam (PTZ) + VA/TP] were considered. Synergy was evaluated by means of checkerboard assay against 50 (double combinations) and 25 (triple combination) MRSA strains isolated from respiratory tract infections and by means of time kill curves (5 strains). In checkerboard assay synergy was defined as fractional inhibitory concentration index (FICi) of <0.5, additivity as FICi >0.5 and >1, indifference as FICi >1 and antagonism as FICi >2, while in time kill studies synergy was defined as a >2 log decrease in bacterial count of combinations in respect to the most active single drug. Moreover, mutational rates of single and combined drugs at antimicrobial concentrations equal to the resistance breakpoints were calculated in 10 strains
Results: Synergy and additivity were the prevalent effects, while no antagonism was observed in checkerboard assay. In particular, LVX + VA/TP and CTX + TP/VA gave synergy in 16/50, 9/50, 43/50 and 23/50 strains, respectively. Combinations of LVX + VA + CAZ/CPM/PTZ and of LVX + TP + CAZ/CPM/PTZ yielded synergy or additivity in all the tested strains, with combinations of LVX + TP + CAZ/PTZ giving synergy in 20/25 strains. Time kill curves evidenced synergy for LVX/CTX + VA/TP after 12 and 24 h of incubation. Synergistic triple combinations occurred more frequently with LVX + TP than with LVX + VA after 12 and 24 h. For single antibiotics, mutational frequencies ranged between 10–5 and <10–9 for LVX, CTX, AMK and IMI, and <10–9 for VA and TP. When tested in double and triple combinations, mutational frequencies fell below 10–9 for all the combinations.
Conclusion: The study provide in vitro evidence of synergy between glycopeptides with fluoroquinolones, cephalosporins and beta-lactams and of limitations of occurrence of mutations in MRSA strains responsible of respiratory infections, thus underlining a potential role in therapy of such infections.
P1216: Comparative activity (MIC and MBC) of daptomycin, quinupristin/dalfopristin, linezolid, vancomycin and teicoplanin against a large worldwide collection of VISA/hVISA
A. Bolmström, A. Engelhardt, Å. Karlsson, E. Edling, P. Ho (Solna, S)
Objective: The worldwide emergence and possible dissemination of vancomycin (VA) resistance in staphylococci involving vanA (VRS), VISA and hetero-VISA phenotypes comprise formidable clinical threats. Comparisons of the in vitro activity of newer Gram positive agents using larger worldwide collections of VISA strains become increasingly important both for individual therapy guidance and for epidemiologic purposes.
Method: A 10 country collection of 243 staphylococci (217 MRSA, 26 MSSA), of which 150 were VISA (E-test macromethod and PAP-AUC, Walsh et al, JCM 2001) was assessed. MIC of DP, QD, LZ, VA and TP were determined using the NCCLS broth microdilution (BMD) and E-test. MBC for all agents for a subset of 46 VISA and non-VISA strains were determined using an Etest MBC procedure and BMD.
Results: Inter-method agreement (n = 2430) for all antibiotics were ±95% ±1 dilution for MIC and ±80% for MBC results. The continuous gradient format in E-test allowed detection of subtle upward shifts in MIC and MBC distributions of VISA, as well as the detection of persister colonies in MBC assays seen with the less bactericidal compounds.
| MIC & MBC range |
MIC50&MBC50 |
MIC90&MBC90 |
||||
|---|---|---|---|---|---|---|
| Non-VISA | VISA | Non-VISA | VISA | Non-VISA | VISA | |
| Daptomycin MIC | 0.25-4 |
0.125-4 |
0.5 |
0.75 |
1 |
1.5 |
| MBC | 0.38 - 6 | 0.38-8 | 2 | 2 | 4 | 6 |
| Quinupristin/Dalfopristin | 0.19-32 |
0.19-32 |
0.38 |
0.5 |
0.75 |
24 |
| 0.125-6 | 0.25 - 32 | 0.75 | 0.75 | 2 | 32 | |
| Linezolid | 0.25 - 3 |
0.38-2 |
1 |
1 |
1.5 |
1.5 |
| 0.5-256 | 1-256 | 3 | 3 | 12 | 256 | |
| Vancomycin | 0.5-3 |
1 - 12 |
1.5 |
2 |
2 |
4 |
| 1-256 | 2-256 | 4 | 4 | 12 | 12 | |
| Teicoplanin | 0.125-4 |
0.75 - 32 |
1 |
2 |
4 |
16 |
| 0.125 - 256 | 4-256 | 4 | 12 | 8 | 256 | |
Conclusion: MIC distributions showed that daptomycin and linezolid maintained potency against the large collection of VISA while quinupristin/dalfopristin and glycopeptides showed a shift towards reduced activity. MBC results showed daptomycin to be superior to linezolid (bacteriostatic) and the other agents. The potential usefulness of newer agents for VISA should be continually assessed with respect to both their static and cidal activities in order to detect subtle shifts in susceptibility as early as possible.
P1217: Performance of a unique E-test Daptomycin gradient + calcium gradient on Isosensitest compared to NCCLS broth microdilution in Mueller Hinton
A. Bolmström, A. Engelhardt, Å. Karlsson, P. Ho, A. Wanger, R.A. Howe (Solna, S; Houston, USA; Bristol, UK)
Objective: Daptomycin (DP) requires physiologic levels of free calcium ions (Ca2+) for expression of adequate activity. Susceptibility testing methods can be significantly influenced by Ca2+ variations in agar and broth. NCCLS broth microdilution (BMD) uses a final physiologic level of 50 μg/mL calcium for DP testing. E-test DP is a unique gradient which incorporates a constant level of calcium. E-test DP has been shown to be equivalent to BMD when tested with commercially available Mueller Hinton (MH) agar. Since Isosensitest (ISO) is used in some parts of Europe, and has an inherently low level of calcium (approximately 5–10 μg/mL), it is important to evaluate the performance of E-test DP on ISO in comparison to BMD.
Method: A 3 lab study compared E-test DP on ISO to NCCLS BMD. A total of 760 clinical and stock strains comprising E. faecalis (180), S. aureus MR (172), S. aureus MS (69), S. pyogenes (190), S. agalactiae (119) and S. dysagalactiae (30) were used. Interlaboratory reproducibility was evaluated using 25 bias/precision strains tested at all sites and 3 NCCLS QC strains were used to compare E-test DP on ISO values to NCCLS MH values. The various methods were used according to standard recommendations. NCCLS susceptible breakpoints ≥1 μg/mL for staphylococci and streptococci and >4 μg/mL for enterococci were used as is and as adjusted upwards by 1 dilution.
Results: Percentage essential agreement (EA), Category agreement (CA) and Inter-Laboratory Reproducibility (REP):
| Organism | Etest ISO vs BMD MH |
REP |
||
|---|---|---|---|---|
| EA ± 1 dil | CA (NCCLS BP) | CA (ISO* BP) | EA ± 1 dil | |
| All strains tested | 87.7 | 88.2 | 98.5 | 98.7 |
| Staphylococci | 82.9 | 66.2 | 96.1 | 95.6 |
| Enterococci | 87.4 | 96.3 | 99.5 | 100 |
| Streptococci | 91.1 | 98.5 | 100 | 100 |
ISO adjusted breakpoints (BP)
Conclusions: E-test DP on ISO were 1–2 dilutions higher for staphylococci and enterococci due to the lower CA level. Clustering of elevated ISO MICs around the NCCLS breakpoints gave lower CAT and this improved to 99% with adjusted breakpoints. Results for streptococci on ISO agreed with BMD. To achieve equivalence to NCCLS, E-test DP values for Gram + aerobes on ISO should be adjusted upwards by 1 dilution to ≥2 μg/mL for staphylococci and streptococci and ≥8 μg/mL for enterococci.
P1218: Four years experience of using E-tests for antibiotic combination testing of isolates from cystic fibrosis
I.M. Gould, K.E. Milne, F.M. Mackenzie (Aberdeen, UK)
Objectives: Between April 1999 and March 2003 cystic fibrosis (CF) centres from around Scotland submitted multi-resistant Gramnegative isolates from CF patients to our laboratory for assessment of MICs and Fractional Inhibitory Concentration Indices (FICI). We present the results of the combination testing.
Methods: E test strips were used to establish the FICI of the antibiotic combination pairs. Combination testing was carried out on 125 strains of Pseudomonas aeruginosa (PA), 69 strains of Burkholderia cepacia (BC) and 29 strains of Stenotrophomonas maltophilia (SM) from 96 CF patients. 19, 13 and 6 combination pairs were tested between 10 and 69 times against PA, BC and SM respectively. The FICI results were categorised as synergistic (FICI ≤ 0.5), additive (FICI = 0.5 to ≤1.0), indifferent (FICI = 1.0 to ≤2.0) and antagonistic (FICI > 2.0).
Results: 1107 combinations were tested. Synergy was found in 3.1% of PA, 9.7% of BC and 8.6% of SM. 31.6%, 32.6% and 25.8% of PA, BC and SM respectively demonstrated an additive effect. 64.2% of PA, 54.5% of BC and 62.4% of SM demonstrated an indifferent effect. Antagonism was found in 1.1%, 3.2% and 3.2% of PA, BC and SM respectively. The top synergistic combinations for PA, BC and SM were amikacin∼ceftazidime (AK∼TZ), tobramycin(TM)∼TZ and levofloxacin∼ticarcillin/clavulanate (LE∼TLC) respectively. The top additive combinations for PA and BC were TM∼TLC, ciprofloxacin∼meropenem (CI∼MP) respectively. LE∼piperacillin/tazobactam (PTC) and LE∼TLC were joint top additive combinations for SM. 7, 11 and 3 combinations demonstrated antagonism against PA, BC and SM respectively. The overall rate of synergy was 5.6%, the additive rate was 31.4%, the indifferent rate was 61.1% and antagonism was 1.9%
Conclusions: Overall very little antagonism was demonstrated (1.9%). The level of demonstrable synergy was 5.6%. Some combinations clearly give lower FICIs than others but this is species specific.
P1219: Study of comparative activities of quinupristin–dalfopristin and linezolid against macrolide-resistant viridans group streptococci by using time-kill methodology
C. Rodriguez-Avial, I. Rodriguez-Avial, J.J. Picazo (Madrid, E)
Objectives: Viridans group streptococci (VGS) resistant to penicillin, macrolides and other antimicrobial are increasingly found. Linezolid and quinupristin-dalfopristin exert their mechanism of action by protein synthesis inhibition and are agents with activity against multidrug resistant gram-positive cocci. This study was aimed to determine, by time-kill curves, the activity of linezolid and quinupristin–dalfopristin against five VGS expressing various degrees of resistance to erythromycin and harbouring different erythromycin resistance determinants
Methods: The species, erythromycin MICs (mg/l) and the erythromycin resistance genes present for each of the five isolates tested were: S. anginosus/0.06/none, S. sanguis/4/mef(A), S. sanguis/64/erm(B), S. mitis/256/erm(B) +mef(A), S. anginosus/256/erm(B) +mef(A). Quinupristin–dalfopristin and linezolid MICs for all strains were 1 and 0.5 mg/l respectively. Strains were incubated in cation-adjusted Mueller–Hinton broth supplemented with 5% lysed horse blood. Each of the five isolates were exposed to linezolid and quinupristin–dalfopristin for 24 hours in a shacking water bath in presence of 2 × MIC. Colony counts were performed at 0, 4, 8 and 24 hours.
Results: Time-kill studies showed that for linezolid, the antibiotic concentration of 2 × MIC was bacteriostatic for each strain irrespectively of the resistance to erythromycin and the genes harboured, showing a 90% of killing at 24 h. The in vitro activity of quinupristin–dalfopristin was predominantly bactericidal with a 99.9% of killing at 3 h. The exception were the 2 strains with erm(B) + mef(A) determinants, in one of them, a S. milleri, the bactericidal activity was delayed to 24 h, and in the other strain, a S. mitis, the activity was bactericidal at 3 h but with regrowth at 24 h.
Conclusions: When VGS are implicated in infections in neutropenic patients and in cases of endocarditis where bactericidal activity is usually considered mandatory, we have to considered that: linezolid was bacteriostatic, at the concentration tested, against all strains and the rapid killing of quinupristin–dalfopristin against VGS was lost when the strain presented the erm(B) and mef(A) genes together.
P1220: Comparative antimicrobial susceptibility patterns in different groups of species of viridans group streptococci and Streptococcus bovis isolated fom blood cultures
I. Rodriguez-Avial, C. Rodriguez-Avial, J.J Picazo (Madrid, E)
Objectives: Viridans group Streptococci (VGS) and S. bovis are part of the normal human microbiota and are implicated as a cause of endocarditis and sepsis in neutropenic patients. Because of their resident nature are frequently exposed to the antimicrobial agents. This study was performed to study the resistance phenotypes to penicillin (P), erythromycin (E), clindamycin (Cc), ciprofloxacin (C) and tetracycline (T) and also to determine whether there are any differences in the antimicrobial susceptibility patters among the difference species of the VGS and S. bovis.
Methods: The 145 VGS and 10 S. bovis were isolated from blood and identified at species level by ID 32-Strep system (68 S. mitis, 44 S. anginosus, 25 S. sanguis, 7 S. salivarius and 1 S. mutans). MICs were determined by the agar dilution method and the percentages of resistance determined according to NCCLS criteria for streptococci other than S. pneumoniae.
Results: Overall, 64.5% of the streptococci were resistant at least to one of the antibiotic tested and of these, 32% was resistant to 3 or more. The most susceptible species were S. anginosus and S. salivarius (57% susceptibility to all antibiotics tested). The only S. mutans strain was susceptible to all the antibiotics tested. The resistance phenotypes for the different species are shown in the table.
| No. of strains |
||||||
|---|---|---|---|---|---|---|
| Phenotype | No. of strains | S. mitis | S. anginosus | S. sanguis | S. salivarius | S. bovis |
| Susceptible | 54 | 18 | 25 | 6 | 4 | 1 |
| P | 10 | 6 | 1 | 1 | 2 | – |
| E | 3 | 1 | 1 | 1 | – | – |
| T | 2 | 2 | – | – | – | – |
| C | 1 | 1 | – | – | – | – |
| ECc | 1 | – | 1 | – | – | – |
| EP | 15 | 10 | – | 4 | 1 | – |
| ET | 2 | – | 1 | 1 | – | – |
| EC | 4 | 3 | 1 | – | – | – |
| ECcP | 2 | 1 | 1 | – | – | – |
| ECcT | 24 | 4 | 12 | 1 | – | 7 |
| ECcPT | 19 | 12 | 1 | 5 | – | 1 |
| ECcTC | 3 | 1 | – | 1 | – | 1 |
| ECcPTC | 1 | 1 | – | 4 | – | – |
| EPT | 6 | 2 | – | – | – | – |
| EPTC | 1 | 1 | – | – | – | – |
| PT | 1 | 1 | – | – | – | – |
| PC | 3 | 2 | – | 1 | – | – |
| TC | 2 | 2 | – | – | – | – |
| Total | 154 | 68 | 44 | 25 | 7 | 10 |
Conclusions: As expected Cc resistance was always associated with E resistance. Overall, the phenotype most frequently founded was ECcT in 24 strains (15.5%) and it was present in the 70% of S. bovis and 27% of S. anginosus. The pattern ECcPT was the second more common phenotype (12.3%) and the most frequent in S. sanguis and S. mitis with 20% and 17.6% respectively. S. mitis was the specie that showed more number of phenotypes (17). Heterogeneity in the susceptibility patterns in the species of VGS indicates the need for accurate identification.
P1221: In vitro antibacterial activity of temocillin against extended spectrum beta-lactamases Enterobacteriaceae producing clinical isolates
H. Rodriguez-Villalobos, A. Cardentey-Reyes, S. Cuvelier, J. Frankard, V. Malaviolle, C. Nonhoff, R. De Mendonça, M.J. Struelens (Brussels, B)
Objectives: Temocillin is a methoxy-derivative of ticarcillin, active on Enterobacteriaceae and stable against b-lactamases, including AmpC and extended spectrum b-lactamases (ESBL). However data concerning its activity on ESBL producing strains are limited. The aim of this study was describe the range of minimal inhibitory concentration (MIC) of temocillin in different species of ESBL producing Enterobacteriaceae from a single tertiary care centre in Belgium .
Methods: ESBL producing Enterobacteriaceae (172 E. aerogenes, 164 E. coli, 104 E. cloacae,58 K. pneumoniae and 35 other) strains from patients hospitalised in our institution during the period of 1 January 2000 to 31 December 2003. ESBL production was screened by double-disk test and confirmed by Oxoid combined disk method. Characterisation of enzymes was performed by multiplex PCR for bla TEM, bla SHV and bla CTX-M gene families detection and by DNA sequencing and/or Iso-electric focusing. MICs (mg/L) were determined by agar dilution method according to NCCLS guidelines. Susceptibility was determined according to breakpoints provided by Fuchs et al: Susceptible MIC ≤ 16 mg/L. (Eur J Clin Microbiol 1985)
Results: Isolates originated from screening rectal swabs (28%), urinary tract (25%), respiratory tract (19%), wound (10%), blood (6%), gastrointestinal tract (4%), or other sites (8%) from 135 male and 233 female patients with a mean age of 61 (range, 0–94) years. The antimicrobial activity of temocillin against ESBL producing Enterobacteriaceae is summarised in the table.
Table 1.
Percentage of susceptibility, MIC 50, MIC 90 and principal enzyme type by species
| Species | Temocillin% susceptibility | MIC50 (mg/L) | MIC90 (mg/L) | ESPL type enzymes |
|---|---|---|---|---|
| Enterobacter aerogenes | 93 | 4 | 16 | 82%TEM |
| Enterobacter cloacae | 99 | 2 | 8 | 90% SHV12+TOHO2 |
| Escherichia coli | 92 | 8 | 16 | 43%TEM 37%TEM+CTX-M |
| Klebsiella pneumoniae | 95 | 2 | 16 | 47%THM+SHV+CTX-M |
| All species | 94 | 4 | 16 |
Conclusions: This study confirmed the good in vitro activity of temocillin against multiresistant ESBL-producing clinical isolates of Enterobacteriaceae. Its activity included Enterobacter AmpC depressed mutant strains that co-produced multiple ESBL. These data suggest that temocillin could be a valuable drug to be considered in the treatment of infections by some ESBL-producing Enterobacteriaceae.
P1222: In vitro activity of ertapenem against cefpodoxime-resistant Gram-negative bacilli from urine
F. M'Zali, M. Wilcox, C. Oliviera, S. Wallis, M. Wallis, M. Denton (Leeds, UK)
Introduction: Resistance to commonly used antibiotics for urinary tract infection (UTI) is of growing concern. This is due to the emergence of extended-spectrum beta-lactamase (ESBL) producing bacteria in the community with reports from different parts of the world. The appearance and dissemination of these resistant bacteria cause serious concerns for the treatment of urinary tract infections (UTIs).
Objectives: Ertapenem is the latest member of the carbapenem class of antimicrobials. The aim of this study was to assess the activity of ertapenem against a collection of cefpodoxime-resistant Gram-negative bacilli isolated from urine samples of community and hospital-based patients.
Materials and methods: Between June and October 2004, our laboratory received 10,234 urine samples. Of these 2246 gave a positive culture, of which 446 from hospitalised patients and 1800 from the community. Of these 258 were gram negative bacilli resistant to cefpodoxime 1 mg/l. The identity of the isolates was confirmed using API 20E or API 20NE (Biomerieux, France). ESBL production was sought using the MASTDD and the identity of the resistant determinant(s) was carried out using a combination of PCR and nucleotide sequence analysis technology. The minimum inhibitory concentration (MIC) to ertapenem was determined using E-test strips (AB Biodisk, Sweden).
Results: Of the 258 isolates resistant to cefpodoxime, 83 were positive for ESBL production and the enzymes produced were:
TEM-1, SHV-5, SHV-12, CTX-M-15, CTX-M3 and CTX-M9 singly or in combination. Ertapenem proved active against all Enterobacteriaceae regardless of production of ESBLs (MIC range 0.003–0.125 mg/l). For Acinetobacter sp. Pseudomonas sp. and Stenotrophomonas sp the MIC were higher (range between 038 and 4 mg/l).
Conclusion: This study confirmed the in vitro activity of ertapenem against cefpodoxime resistant Gram-negative bacilli regardless of the presence or absence of ESBL production or the type of ESBL produced. Ertapenem was less active against non-Enterobacteriaceae. Identification of Gram-negative organisms to species level is an important predictor of likely susceptibility to ertapenem.
P1223: In vitro activity of telithromycin against erythromycin-susceptible and resistant pneumococci
G. Poulakou, I. Katsarolis, I. Matthaiopoulou, P. Panagopoulos, A. Avlamis, C. Antachopoulos, D. Sofianou, C. Skevaki, M. Kazantzi, L. Ftika, V. Papatolis, E. Kastrisiou, A. Pangalis, K. Konstantopoulos, C. Koubaniou, H. Giamarellou on behalf of the Hellenic Study Group for the susceptibility of streptococcus pneumoniae 2004 HSSSP-2004
Objectives: To assess the in vitro activity of telithromycin (TEL) against erythromycin-sensitive (Ery S) and resistant (Ery R) isolates of Streptococcus pneumoniae isolated from the nasopharynx of healthy children in Greece 2004.
Methods: The strains studied were isolated by nasopharyngeal sampling in healthy children, aged 2–6 y, attending day-care centres and were collected during a nation-wide surveillance study for the susceptibility of pneumococci. Ery MICs were determined by E-test according to NCCLS methodology. TEL MICs were determined by agar dilution. NCCLS breakpoints (Jan 2004) were applied for Ery and TEL: for susceptibility (0.5 and 1 mg/L, respectively; ≥1 and 4 mg/L for resistance. For macrolide resistance phenotype, the double disk diffusion test was used and 3 phenotypes identified: M, constitutive and inducible MLSB (cMLSB and iMLSB, respectively).
Results: Of the 275 strains studied, 76 were Ery S and 159 were Ery R. All strains but two (MIC 4 and 8 mg/L) were susceptible to TEL. In particular, results for telithromycin for the Ery S strains, showed an MIC range for TEL between 0.008–0.5, with MIC50 of 0.015 and MIC90 of 0.06. For Ery R in total, MIC50 and MIC90 were 0.125 and 0.5 (range 0.008–8). With respect to macrolide resistance phenotype, the distribution per type was: M 54.5% (Ery MIC range 1–32), and cMLSB and iMLSB (Ery MIC range 4 to (256) 39% and 6.5% respectively. The two strains resistant to TEL displayed the cMLSB phenotype (Ery MIC (256). For each different macrolide resistance phenotype, MIC50/MIC90 of TEL had the following values: M phenotype 0.25/0.5 – cMLSB 0.06/1 – iMLSB 0.03/0.06.
Conclusions: TEL is active against both Ery S and R strains, irrespective of macrolide resistance mechanisms, although MICs for resistant strains are higher. This finding along with the very low-level of pneumococci resistance to TEL (<1%), in accordance to other European and global surveillance data, render TEL an alternative potent agent for the treatment of respiratory tract infections caused by pneumococci, especially in the setting of macrolide resistance.
Mechanisms of resistance to macrolides
P1224: Mechanisms of macrolide resistance in Streptococcus pneumoniae nasopharyngeal isolates in Athens, Greece in 2003
K. Volonakis, M. Souli, I. Galani, E. Koratzanis, H. Giamarellou (Chaidari, GR)
Background: The constant increase in macrolide consumption has been known to raise macrolide resistance of S. pneumoniae strains. Annual surveillance of resistance rates of S. pneumoniae, which is the most common cause of upper and lower respiratory tract infections in the community is warranted.
Methods: A total of 485 S. pneumoniae isolates were collected from 1396 healthy children, with ages 1–6 years, attending day care centres during the winter months of 2003 in Athens (nasopharyngeal carriage 34.7%). Four-hundred-and-forty-seven of these were evaluated for antimicrobial susceptibilities using the E-test (AB Biodisk, Sweden) and agar dilution methods. Macrolide-non-susceptible isolates reached the number of 135 (30.2%), whereas all were telithromycin susceptible. A hundred-thirty-seven isolates were available for further testing for phenotypic and genotypic resistance patterns. Phenotypic resistance was studied by disk diffusion using 2 μg clindamycin, 15 μg erythromycin and 7.5 μg quinopristin disks. Genotypes were studied by PCR for the presence of ermAM and mefE genes known to prevail in this area.
Results: Fifty-one isolates (38.3%) were assigned to the constitutive macrolide-lincosamine-streptogrammin B resistance phenotype (cMLSB). No isolates demonstrated an inducible MLSB phenotype by this method. Forty-nine of these carried the ermAM gene (34.3%) and three carried both ermAM and mefE genes (2.18%). Eighty-seven isolates (63.5%) had the M phenotype (macrolide resistance) and all of these contained the mefE gene.
Conclusions: Our findings are in contrast to European studies and to previous Greek studies, where the erm gene prevailed or at least equaled the prevalence of mef gene. This is the first report of isolates carrying both ermAM and mef genes in Greece. Knowledge of the resistant mechanisms to macrolides is crucial for the empiric antibiotic treatment of community acquired infections.
P1225: Antibiotic susceptibility, mechanisms of macrolide resistance and clonal relationship in group B streptococci
J.J. González, A. Andreu, P. Alomar, M.A. Blanco, A. Bordes, J. Bosch, J. Cacho, A. Cid, A. Coira, M. de Cueto, E. Dopico, J.M. García-Arenzana, A. Gil-Setas, C. Gimeno, C. Guardia, S. Illescas, T. Juncosa, J. Lite, R. Martínez, B. Orden, M. Peréz-Pascual, M. Rebollo, M. de la Rosa, M. Rodriguez-Mayo, I. Sanfeliu, F. Sanz, P. Villanueva, L. Viñas Spanish Group of Perinatal Infection. Spanish Society for Clinical Microbiology and Infectious Diseases
Objectives: (1) To study the antimicrobial susceptibility among group B streptococci (GBS) strains of vertical transmission to different antibiotics in order to evaluate alternatives for intrapartum chemoprophylaxis to women allergic to penicillin and colonized by a GBS strain resistant to macrolides and/or lincosamides; (2) characterize the mechanisms of resistance to macrolides and lincosamide; (3) evaluate the clonal relationship between these strains.
Methods: A total of 610 strains collected in a multicentre study: 131 isolated between 1997 and 2002 from newborns diagnosed of early-onset GBS disease and 479 strains collected in 2002 from vagina or rectum of pregnant women. Microdilution method was used to study the antimicrobial susceptibility and disk diffusion to define the macrolide-lincosamide resistance phenotype. PCR was performed to determine the presence of ermB, ermTR and mefA resistance genes. To evaluate the clonal relationship, PFGE of total DNA was done using SmaI.
Results: All the strains were susceptible to penicillin, ampicillin, vancomycin, quinupristin/dalfopristin, levofloxacin and teicoplanin. The 12.45% were resistant to erythromycin and azithromycin, 11.80% to josamycin, 11.31% to clindamycin, 1.80% to telithromycin and 0.32% to fosfomycin. Among the macrolide resistant strains, the 90.8% presented a constitutive MLSb phenotype (cMLSB), 5.26% an inducible MLSb phenotype (iMLSB) and the remaining 3.94% a M phenotype. Three strains were susceptible to macrolides and resistant to clindamycin. The ermB, ermTR and mefA genes were presented in 63.2%, 30.3% and 3.9% of the macrolide resistant strains. Two strains did not amplified none of the studied genes. The 100% of the strains harbouring the ermB gene showed a constitutive phenotype. All the strains showing an inducible phenotype harboured the ermTR gene. The 11 telithromycin resistant strains presented a cMLSB phenotype; of them 10 posses the ermB gene and one the ermTR.
Conclusion: In Spain, there is a high rate of resistance to macrolides and lincosamides that makes mandatory to perform susceptibility testing to GBS strains isolated from pregnant women allergic to penicillin. In our region ErmB methilase is the main cause of macrolide resistance, followed by the ErmTR and the macrolide eflux pump in a low proportion. There is a wide clonal diversity among resistant strains to macrolides, lincosamides and telithromycin.
P1226: Detection of the ermX determinant of macrolide resistance in clinical strains of Corynebacterium urealyticum
A. Ortiz, J.I. García-Cía, R. Fernández-Roblas, J. Esteban (Madrid, E)
Objectives: To detect the presence of the ermX macrolide resistance gene in clinical isolates of C. urealyticum.
Methods: 57 C. urealyticum strains were isolated from clinical samples in the Fundación Jiménez Díaz hospital. The strains were maintained frozen until the studies to evaluate macrolide resistance were performed. Antibiotic susceptibility testing was performed by agar dilution assay in 14 cases and by disc diffusion assay in 43 cases. Detection of ermX gene was performed by using primers Cerm-1 and Cerm-2 according to the protocol described by Rosato et al. DNA was extracted by boiling a suspension of bacteria in distilled water. Amplification products were analysed by agarose gel electrophoresis and molecular weight of the amplicons were calculated by using the PhotoCapt software (BioGene, USA).
Results: 46 strains were resistant to erythromycin and clindamycin, and 11 were susceptible to both antimicrobials. We detected the gen ermX in 34 cases (all of them resistant). 12 macrolide-resistant strains gave negative results for ermX detection. The susceptible strains did not show any amplification product.
Conclusions: The ermX gene is detected in 73.9 % of macrolide-resistant Corynebacterium urealyticum strains. However, there were 26.1 % macrolide-resistant strains in which ermX gene was not detected. Other resistance determinants must be involved in macrolide resistance among Corynebacterium urealyticum.
P1227: Characterisation of phenotype and genotype of macrolide-resistant Streptococcus pyogenes
C.K. Lee, S.Y. Bae, S.W. Ryu, J.A. Kwon, Y.J. Cho, Y.K. Kim, K.N. Lee (Seoul, KOR)
Objectives: The resistance of Streptococcus pyogenes to macrolide is a world wide problem. The aim of present study was to determine the prevalence of antibiotic resistance rate of erythromycin (EM) resistant isolates from Korea, and evaluate their genetic mechanism, phenotype distribution and clonal relationship.
Methods: Total 51 EM resistant S. pyogenes from clinical specimens from 1996 to 2003 were studied; agar dilution method to determine minimal inhibitory concentrations (MICs) to 9 antimicrobial agents was performed. Resistance phenotypes were determined by triple-disc test and resistance induction experiment with sub-inhibitory concentration of erythromycin (0.05 μg/ml). Their genetic mechanisms of resistance were determined by PCR. The genetic relatedness of them was also investigated by means of emm genotyping and random amplified polymorphic DNA (RAPD) analysis.
Results: An average EM resistance rate was 23% and their cross-resistance rate to clarithromycin, azithromycin, and spiramycin were 100%, 98%, and 67%, respectively. The most common resistance phenotype was inducible MLS (iMLS; 51%), followed by constitutive MLS (cMLS;31%), and M type (18%). 18 of 26 iMLS isolates (69%) showed novel iMLSd phenotype, which had small (9–12 mm) inhibition zones around all three discs on triple-disc test and high level resistance to clinamycin and spiramycin after erythromycin induction. All isolates of the cMLSa and iMLSd harboured ermB gene, while iMLSc and M isolates harboured ermA and mefA gene, respectively. All iMLSd isolates were emm12 except one while all multidrug resistance cMLSa isolates were emm28 genotype. iMLSd isolates made a tight cluster on phylogenetic tree and 78% of them showed a common pattern by RAPD analysis.
Conclusion: iMLSd was most common macrolide resistance phenotype in Korea and emm gene and RAPD analysis was suggestive of its clonal relationship.
P1228: Detection of inducible clindamycin resistance in cutaneous staphylococci clinical isolates by phenotypic and genotypic method
L. Merino, M.J. Torres, A. Cantos, M. Ruiz, J. Aznar (Seville, E)
Objectives: To study the inducible clindamycin resistance in Staphylococcus aureus and Coagulase-Negative Staphylococci by phenotypic and genotypc methods.
Material and methods: A group of 117 erythromycin-resistant clinical isolates [(57 S. aureus and 60 coagulase-negative staphylococci (CNS)] from cutaneous samples were selected from recent (December 2003 to June 2004) 536 clinical isolates of Staphylococcus spp. (401 S. aureus and 135 CNS). Identification and susceptibility testing of the isolates were performed with the MicroScan instrument. The standard NCCLS disk diffusion test was performed on each isolate using unsupplemented Mueller–Hinton agar (Becton Dickinson Microbiology Systems, Cockeysville, Md.) and standard 15-μg erythromycin disks and 2-μg clindamycin disks (Becton Dickinson). On the same agar plates, two additional pairs of disks were placed by hand to provide distances of 15 and 20 mm between the respective erythromycin-clindamycin disk pairs to detect inducible clindamycin resistance. Real-time PCR was performed with oligonucleotide primers specific for the ermA, ermB, ermC and mrsA genes as described by Martineau et al (AAC.2000), using Faststart DNA MasterPlus SYBR Green I.
Results: Twenty-nine (24.8%) S. aureus and 31 (26.5%) CNS of the 117 erythromycin-resistant clinical isolates were susceptible to clindamycin, and the remaining 57 (48.7%) isolates were clindamycin resistant, 40 (34.2%) with inducible resistance (21 S. aureus and 19 CNS), and 17 (14.5%) isolates with constitutive clindamycin resistance (7 S. aureus and 10 coagulase-negative staphylococci). The mrsA gene was present in all the clindamycin susceptible isolates except for 1 CNS. Among the 40 isolates with clindamycin inducible resistance, 37 isolates possess either ermA or ermC while 1 CNS isolate possess both ermC and mrsA. One CNS and 1 S. aureus isolates were negative for all the genes tested. All 17 isolates with constitutive clindamycin resistance amplified to any of the genes tested. Among the S. aureus isolates, 2 have the ermA gene, 4 the ermC and 1 both ermC and mrsA genes. All the CNS isolates possess the ermC but 3 of them possess also the mrsA gene (Table 1).
Table 1.
Resistance genotype of 117 erythromycin resistant cutaneous isolates of S. aureus and CNS
| No. of isolates with genotype |
|||||||
|---|---|---|---|---|---|---|---|
| Organims and phenotype | no. of isolates | ermA | ermB | ermC | mrsA | ermC/mrsA | others |
| S. aureus | 57 | 4 | 0 | 22 | 29 | 1 | 1 |
| CS | 29 | 0 | 0 | 0 | 29 | 0 | 0 |
| CRind | 21 | 2 | 0 | 18 | 0 | 0 | 1 |
| CRconst | 7 | 2 | 0 | 4 | 0 | 1 | 0 |
| CNS | 60 | 0 | 0 | 24 | 30 | 4 | 2 |
| CS | 31 | 0 | 0 | 0 | 30 | 0 | 1 |
| CRind | 19 | 0 | 0 | 17 | 0 | 1 | 1 |
| CRconst | 10 | 0 | 0 | 7 | 0 | 3 | 0 |
Conclusions: The disk-diffusion test detected all the clindamycin resistant strains, and none of the clindamycin inducible resistant strains was detected by the Microscan. The ermC gen was the most prevalent among the clindamycin resistant, in both CNS and S. aureus isolates.
P1229: Ribosomal protein L22 mutations in Bacillus anthracis associated with cross-resistance between macrolide, lincosamide, streptogramin and ketolide antibiotics
D.J. Farrell, A. Athamna, M. Athamna, D.J. Bast,
E. Rubinstein (London, UK; Kfar-Qaraa, IL; Toronto, CAN; Tel Hashomer, IL)
Objectives: In vitro selection of resistance and cross-resistance between macrolide, lincosamide, streptogramin and ketolide (MLSK) antibiotics in the Sterne and ST-1 strains of B. anthracis have recently been demonstrated (Athamna A et al., J Antimicrob Chemother 2004; 54: 424). The aim of this study was to determine ribosomal mutations associated with this resistance.
Methods: Primers were designed and used to amplify and sequence the L4, L22 riboprotein genes and the 11 copies of the 23S rRNA gene using B. anthracis str. Ames complete genome (GenBank Accession No. NC_003997).
Results: (MICs in mg/L) Two significant mutations associated with resistance were found. A 4 amino acid (AA) insertion (a tandem duplication of 90MGRA93) into the L22 gene at position 94 was found in the ST-1 strain with a quinupristin/dalfopristin (Q/D) MIC of 128 selected after 18 passages in Q/D. This strain was cross-resistant to telithromycin, erythromycin, clarithromycin and clindamycin with MICs of 16, 64, 16 and 8 respectively. An 8 amino acid insertion (MGRAMGRA) into the L22 gene (also at position 94) was found in the Sterne strain with a clarithromycin MIC of 64 after 18 passages in clarithromycin. This strain was cross-resistant to telithromycin, Q/D, erythromycin and clindamycin with MICs of 16, 8, 32 and 1 respectively.
Conclusions: Tandem duplications of L22 90MGRA93 were found to be important in MLSK resistance in 2 separate strains of B. anthracis demonstrating that this locus is important for resistance development under selective pressure of Q/D and clarithromycin. Importantly, these mutations were also associated with cross-resistance to other MLSK antibiotics.
P1230: Horizontal transfer of the MLSB resistance gene erm(B) between the human pathogen Clostridium difficile and the ruminal anaerobe Butyrivibrio fibrisolvens
P. Mastrantonio, F. Barbanti, P. Spigaglia (Rome, I)
Objectives: The aim of this study was to investigate the possibility of in vitro transfer of the MLSB resistance gene, erm(B) between the human pathogen Clostridium difficile and the ruminal commensal Butyrivibrio fibrisolvens.
Methods: The erm(B)-positive C. difficile strain CD51 was used in filter matings as donor, whereasthe B. fibrisolvens strain 1.230, tetracycline resistant, and the B. fibrisolvens strain 2221R, rifampicin resistant, were used as recipients. The strains were cultured in M2GSC broth, with 30% of sterile rumen, in anaerobic conditions and the filter matings were performed on sheep blood agar plates, supplemented with hemin (0.1%) and vitamin K (0.1%). The same medium, supplemented with erythromycin (20 mcg/ml) and tetracycline (10 mcg/ml), were used to select the transconjugants. MIC values were assessed by E-tests. The erm(B) transfer was confirmed by PCR and by hybridisation assays, using an erm(B) probe on transconjugant genomes digested with PvuII and with SmaI (PFGE).
Results: The transfer average frequency was 5 × 10−7. MIC values for erythromycin were >256 mg/l both in donor and transconjugants. An internal fragment of the erm(B) gene (730 bp) was amplified in all the transconjugants and a specific band was visualised in hybridisation assays on transconjugant genomes digested with both PvuII and SmaI. The re-transfer of the erm(B) gene from B. fibrisolvens transconjugants to C. difficile 1977, an erythromycin susceptible strain, was also obtained.
Conclusion: The in vitro transfer of the MLSB resistance gene erm(B) from C. difficile to B. fibrisolvens and vice-versa, is an important result supporting the possibility that horizontal transfer of resistant genes between human pathogenic bacteria and animal commensal microorganisms could occur, under natural conditions, more easily than expected.


