Abstract
A mysterious disease was reported on May 24, 2003, when the Wisconsin Division of Public Health (DPH) received notice of a 3-year-old girl who had been hospitalized in central Wisconsin with cellulites and fever after being bitten by a prairie dog on May 13. The laboratory isolated a gram-negative bacillus, raising concerns that it might be tularemia or plague; ultimately, it was identified as an acinetobacter species and was considered to be a contaminant. Because no other such cases were reported at the time, the case was thought to be merely an isolated event. However, within two weeks, on June 2, 2003, evidence of a much wider scenario began to emerge. On that date, the Wisconsin DPH received notice from the Marshfield Laboratory that the mother of the first patient had become ill on May 26 and that electron-microscopic evidence of a poxvirus was found in a skin lesion. On that same day, another report, this time from the Milwaukee Health Department, of a strange illness was received at the DPH and described the case of a meat inspector who resided in southeastern Wisconsin and also was a distributor of exotic animals. By July 30, 2003, 72 confirmed or suspected cases of monkeypox had been reported in Wisconsin, Illinois, and Indiana and represented a large outbreak. The peak in the onset of illness occurred between May 29 and June 9, 2003, and no further cases of illness have been reported in humans since June 22, 2003. Traceback investigations from the child and other patients followed the route of introduction of monkeypox into Wisconsin to a distributor in Illinois, who had received a shipment of exotic animals imported into the United States through Texas from Ghana, West Africa.
On Wednesday, June 11, 2003, The Secretary of the United States Department of Health and Human Services, Tommy G. Thompson, announced an immediate embargo on the importation of all rodents from Africa. He also announced a ban on the distribution, sale, and transport of prairie dogs and six specific African rodent species.1 The next day, the state of Wisconsin Department of Health and Family Services issued an emergency order regarding the prohibition of importation, sale, and/or release of prairie dogs or any mammal known to have had contact with prairies dogs since April 1, 2003 (Table 1). 2
Table 1.
Emergency Prohibition Order Issued by Wisconsin Department of Health and Family Services2
| In response to the reports of monkeypox, the Wisconsin State Epidemiologist, Jeffrey P. Davis, M.D., per Chapter 254.51, issued the following prohibitions: |
| Importation of a prairie dog or of any mammal known to have had contact with prairie dogs since April 1, 2003 into Wisconsin |
| Sale of any prairie dog or any mammal known to have had contact with prairie dogs since April 1, 2003 |
| Allowing any prairie dog or any mammal known to have had contact with prairie dogs to have contact with any member of the public |
| Releasing any prairie dogs or any mammal known to have had contact with prairie dogs to the wild |
| Intrastate sale or offering for sale or any other type of commercial or public distribution, including release into the environment of rodents from Africa, to include tree squirrels, rope squirrels, dormices, Gambian giant-pouched rats, brush-tailed porcupines, and striped mice |
These actions came on the heels of a report issued on June 9, 2003, from the Centers for Disease Control and Prevention (CDC) that an extensive multidisciplinary investigation into recent cases of febrile rash illness in Wisconsin, Illinois, and Indiana showed that the patients had had direct or close contact with recently purchased ill prairie dogs.3 The CDC report also noted that scientists at the Marshfield Clinic in Marshfield, Wisconsin, had recovered viral isolates from a patient and a prairie dog that were demonstrated by electron microscopy to be a virus morphologically consistent with a poxvirus.4 Preliminary results of serologic testing, polymerase chain reaction (PCR), and gene sequencing performed at the CDC indicated that the causative agent was monkeypox virus, and additional evaluations by the CDC using electron microscopy and immunohistochemical studies were consistent with the finding of an orthopoxvirus. The findings represented the first reported evidence of community acquired monkeypox-like infection in the United States—and the emergence of yet another infectious disease in the Western hemisphere. The incident came shortly after the emergence of a previously unknown infectious disease, severe acute respiratory syndrome (SARS), which had started in China and been transmitted worldwide in a short period of time (see Seminars in Pediatric Infectious Diseases, July, 2003).5
Monkeypox in the western hemisphere
A mysterious disease was reported on May 24, 2003, when the Wisconsin Division of Public Health (DPH) received notice of a 3-year-old girl who had been hospitalized in central Wisconsin with cellulites and fever after being bitten by a prairie dog on May 13. The prairie dog had been purchased two days earlier at a “swap meet,” where animals were traded or bought. It had become ill on the same day that it bit the child, and at the time was noted to have ocular discharge, lymphadenopathy, and papular skin lesions. It died on May 20, 2003. An enlarged submandibular lymph node noted on the prairie dog was submitted to Marshfield Laboratories (Marshfield, Wisconsin) for bacterial culture. The laboratory isolated a gram-negative bacillus, raising concerns that it might be tularemia or plague; ultimately, it was identified as an acinetobacter species and was considered to be a contaminant. Because no other such cases were reported at the time, the case was thought to be merely an isolated event.4
However, within two weeks, on June 2, 2003, evidence of a much wider scenario began to emerge. On that date, the Wisconsin DPH received notice from the Marshfield Laboratory that the mother of the first patient had become ill on May 26 and that electron-microscopic evidence of a poxvirus was found in a skin lesion. On June 4, the DPH was informed that an orthopoxvirus had been visualized by negative-stain electron microscopy of cell-culture supernatants from the patient (the mother) and the prairie dog.
On that same day (June 2), another report, this time from the Milwaukee Health Department, of a strange illness was received at the DPH and described the case of a meat inspector who resided in southeastern Wisconsin and also was a distributor of exotic animals. He had sustained a bite and a scratch from a prairie dog on May 18, and a nodular lesion had developed at the scratch site on March 23, accompanied by fever, chills, sweats, and lymphadenopathy that began on May 26. He had been examined at a local emergency department and released, but by May 31, his condition had worsened and he was hospitalized. Again, tularemia and plague were considered in the differential diagnosis. By June 3, he was linked to the index case: he had sold two prairie dogs to the patient’s family at the swap meet. With the epidemiologic link established between the cases in different regions of Wisconsin, public health case-finding and animal “trace-back” and “trace-forward” activities were initiatied.4
Test results performed on different patients revealed an alarming situation. On June 6, PCR testing performed by the CDC on three other patients (patient 4, the meat inspector; patient 7, an individual who had purchased two prairie dogs from a pet store in southeastern Wisconsin; and patient 8, an employee of the pet store) revealed monekypox-virus DNA signatures. The next day, the complete sequence of the hemagglutinin gene taken from the virus of the meat inspector/distributor proved to be identical to hemagglutinin gene sequences derived from one of two reference monkeypox-virus clades. That same day, 11 patients with confirmed or suspected monkeypox were identified in Wisconsin and were linked by direct contact with prairie dogs sold by the meat inspector/distributor. Three patients, the child, her mother, and another family member were in northeastern Wisconsin; the other 8 patients were in southeastern Wisconsin. The latter group was composed of the distributor and his wife, two employees of two different pet stores that had received prairie dogs from the distributor, two veterinarians in different clinics who had treated prairie dogs sold by the distributor, and a person who had purchased a prairie dog from one of the pet stores and her houseguest (Figure 1).Two days later (June 9), PCR analyses of tissue- and virus-culture supernatants from the second patient (mother of the 3-year-old girl) and the prairie dog were positive for monkeypox-virus DNA signatures.4
Figure 1.
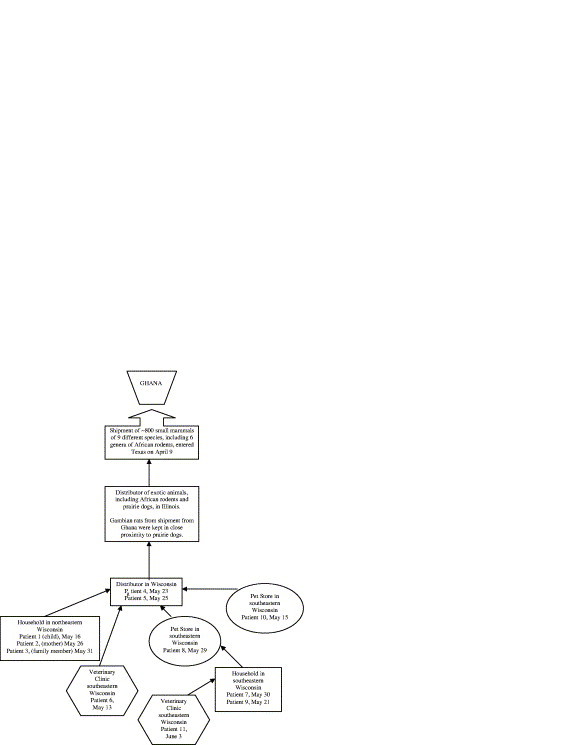
Diagram Showing Links Between Meat Inspector/Distributor and Laboratory-confirmed and Suspected Cases of Monkey-pox. Dates indicate onset of illness; patient numbers determined by means of clinical and laboratory date obtained on or after June 7, 2003. (Adapted from Reed KD, Melski JW, Graham MB and coworkers4)
By July 30, 2003, 72 confirmed or suspected cases of monkeypox had been reported in Wisconsin, Illinois, and Indiana and represented a large outbreak. The peak in the onset of illness occurred between May 29 and June 9, 2003, and no further cases of illness have been reported in humans since June 22, 2003.4
Source of monkeypox in the United States
Traceback investigations from the child and other patients followed the route of introduction of monkeypox into Wisconsin to a distributor in Illinois, who had received a shipment of exotic animals imported into the United States through Texas from Ghana, West Africa (Figure 1). This probable source of introduction involved a shipment of animals that entered Texas on April 9 and included approximately 800 small mammals. Among nine different species in the shipment were six genera of African rodents: rope squirrels (Funiscuirus spp.), tree squirrels (Heliosciurus spp.), Gambian giant rats (Cricetomys spp.), brush-tailed porcupines (Atherurus spp.), dormice (Graphiurus spp.), and striped mice (Hybomys spp.). CDC laboratory testing with PCR and virus isolation of some of the animals revealed that one Gambian giant rat, three dormice, and two rope squirrels were infected with monkeypox virus. Evidence of infection also was found in some of the animals that had been separated from the remainder of the shipment on its arrival into the United States. When the Gambian rats arrived in Illinois, they were kept in close proximity to the prairie dogs implicated in the outbreak in Wisconsin and other states.6, 7
History of the disease
Monkeypox is a rare viral disease caused by Monkeypox virus, a member of the orthopoxvirus group of viruses. It is endemic to the rain forest countries of central and west Africa. It was discovered first in 1958 in laboratory monkeys, and later testing of blood of animals from Africa revealed evidence of monkeypox infection in numerous African rodents. The first report of monkeypox in humans was made in 1970, when the virus was detected in persons living in remote African locations. Between 1981 and 1986, 37 documented cases of monkeypox were reported in the Democratic Republic of Congo (formerly Zaire).8, 9
The largest outbreak of monkeypox was reported from the same area between February 1996 and February 1997, raising concerns about whether samples of the smallpox virus should be retained for comparative research with related viruses like monkeypox. From February to August of 1996, 71 clinical cases of monkeypox, including six deaths, were reported in 13 villages in Zaire.8 The number of secondary cases was highest in August, at the peak of the outbreak.9 Of the 11 specimens collected, all were positive for monkeypox and showed only minor genetic variation compared with other strains collected during 1970 to 1979. As the outbreak continued, with the World Health Organization (WHO) reporting that local health workers put the number of new cases at 170 between March and May of 1997 (58 in March, 52 in April, and 60 in May),10 David Heymann, then chief of the WHO’s new branch devoted to emerging diseases, expressed concern but also cautioned that some of the cases might be chicken pox.8
The cases all were in the same Katako-Kombe region visited earlier by a WHO-organized team. The team, which had gone to the region in February of 1997, was headed by Ali Khan of the CDC and was sponsored by the Zairian Ministry of Health as well as WHO, spent 5 days in the 12 villages that were located at the center of the outbreak.8 Although the trip was cut short because of civil unrest and attacks on villages, Khan and his colleagues were able to provide a detailed report on April 11, in which they suggested that 73 percent of the 89 people studied were infected by other people. That figure represented a large jump from the 30 percent “secondary contact” rate that had been reported by Zdenek Jezek in the studies of the 1981 to 1986 epidemic.11 The 1997 report also included one patient who appeared to have been the source of eight other infections, twice the highest chain of transmission previously noted.8 Other differences also were noted (Table 2). Although some concern had been expressed that the monkeypox was changing and becoming more virulent or more transmissible, such possibilities were eliminated when researchers analyzed part of one isolate from a person infected in 1996 and found no difference between it and strains collected in Zaire between 1970 and 1979.8
Table 2.
Differences in the 1996–1997 Outbreak of Monkeypox in Zaire Compared with Earlier Outbreaks9
| It represented the largest cluster of monkeypox cases ever reported. |
| The proportion of cases in patients aged 15 years and older (27.2%) was substantially higher than previously reported (7.5%). |
| The proportion of secondary cases (73.0%) was substantially higher than previously reported (29.6%). |
| The clustering of cases by households and the chains of transmission, previously not described, suggested that person-to-person transmission accounted for most of the cases. |
| The case-fatality proportion (3.3%) was lower than that previously reported (9.8%). |
Clinical picture and transmission
The signs and symptoms of monkeypox are similar to those of smallpox, but usually much milder. Patients present with fever, headache, muscle aches, backache, swollen lymph nodes, a general feeling of discomfort, and exhaustion. Within 1 to 3 days after onset of fever, a vesicular and pustular rash similar to that of smallpox develops, often beginning on the face but occasionally on other parts of the body. The initially papular rash (Figure 2) progresses to vesiculation, pustulation (Figure 3), and crusting (Figure 4), found in different stages simultaneously on the face, head, trunk, and extremities. The incubation period is 12 days, with a range of 7 to 17 days.12, 13, 14 Illness typically lasts 2 to 4 weeks.
Figure 2.

Initial papular stage of monkeypox rash. (Used with permission of Dr. Kurt Reed and courtesy of Marshfield Clinic, Marshfield, Wisconsin).
Figure 3.

Vesiculation and pustulation of progessive stages of monkeypox rash. (Used with permission of Dr. Kurt Reed and courtesy of Marshfield Clinic, Marshfield, Wisconsin).
Figure 4.

Crusting stage of monkeypox rash. (Used with permission of Dr. Kurt Reed and courtesy of Marshfield Clinic, Marshfield, Wisconsin).
Transmission occurs by an animal bite or direct contact with the animal’s lesions or body fluids. Immunohistochemical assays for orthopoxviruses in the prairie dogs demonstrated abundant amounts of viral antigens in surface epithelial cells of lesions in conjunctiva and tongue, and less amounts in adjacent macrophages, fibroblasts, and connective tissues. Viral antigens were abundant in bronchial epithelial cells, macrophages, and fibroblasts; virus isolation and electron microscopy demonstrated active viral replication in lungs and tongue. These findings suggest that both respiratory and direct mucocutaneous exposures may be important routes of transmission of monkeypox virus between rodents and to humans.12
Monkeypox also has been spread by person-to-person transmission, most likely by respiratory droplets during direct and prolonged face-to-face contact. It also can be spread by direct contact with body fluids of an infected person or with virus-contaminated objects, such as linens, bedding, or clothing.6
Physicians should be alert to the symptoms and consider monkeypox in persons with fever, cough, headache, myalgias, rash, or lymph node enlargement that presents 3 weeks after contact with prairie dogs or Gambia giant rats. Cases of these illnesses in humans and animals should be reported to the state or local health departments as soon as they are suspected.15
Treatment and prevention
To date, no proven, safe cure exists for monkeypox.6 The CDC recommends that persons who present to the emergency room or to an outpatient clinical with fever and vesiculopostular be placed in a private examination room, or a negative pressure room if available, as quickly as possible and examined, keeping in mind a differential diagnosis of chickenpox, vaccinia in a person recently vaccinated against smallpox, and even the unlikely possibility of smallpox. The CDC also has set forth certain general precautionary methods that should be implemented (Table 3). 16
Table 3.
General Precautions for Infection Control of Monkeypox
| Use of hand hygiene after every contact with an infected patient and/or the environment of care |
| Use of gown and gloves for contact with infected patients |
| Protection from virus spread by droplets or aerosols: NIOSH-certified N95 (or comparable) filtering disposable respirator for the healthcare workers or, if not available, surgical masks worn to protect against transmission through contact or large droplets. The respirator or mask should be applied prior to entering the patient’s room. |
| Use of eye protection (e.g., face shield or goggles) if splash or spray of body fluids is likely to occur, as recommended by Standard Precautions |
| Containment and disposal of contaminated waste (e.g., dressings) in accordance with facility-specific guidelines for infectious waste or local regulations pertaining to household waste |
| Proper care exerted in handling soiled linens (e.g., bedding, towels, clothing) to avoid contact with lesion exudates |
| Careful handling of patient-care equipment to prevent contamination of skin and clothing and care taken to ensure that used equipment is cleaned and reprocessed appropriately |
| Implementation of proper procedures for cleaning and disinfecting environmental surfaces in the patient care environment; any EPA-registered hospital detergent-disinfectant currently used by healthcare facilities may be used. |
Adapted from CDC Interim Infection Control and Exposure Management Guidelines.7
The sporadic outbreaks of human monkeypox in Africa and the recent outbreak in the United States have demonstrated that naturally occurring zoonotic orthopoxvirus diseases are a public health concern, which could be eliminated or greatly reduced with a viable vaccine. Currently, the CDC recommends smallpox vaccine for protection against monkeypox for a limited number of individuals who may be exposed to the virus (Table 4) but cautions against such precaution, even after exposure to monkeypox, if the individual has a weakened immune system (eg, from cancer treatment, organ transplant, human immunodeficiency virus [HIV] infection, primary immune deficiency disorders, severe autoimmune disorders, and medications used to treat autoimmune disorders) or a life-threatening allergy to latex or to smallpox vaccine or any of its ingredients.17 Because the smallpox vaccine is a live orthopoxvirus vaccine administered to the skin, the vaccine itself can pose a serious health risk. Hence, research is underway to develop a vaccine against monkeypox.
Table 4.
Individuals for Whom CDC Recommends Smallpox Vaccine to Prevent Monkeypox
| Anyone investigating animal or human monkeypox cases (e.g., public health workers and animal control workers) |
| Healthcare providers who are caring for patients with monkeypox, may be required to care for such patients, or have been in close contact with such patients in the previous 4 days, with vaccination considered up to 14 days after exposure |
| Anyone who has been in contact within the previous 4 days with anyone with monkeypox, with vaccination considered up to 14 days after exposure |
| Anyone, including veterinarians and veterinary technicians, who has had direct physical contact within the previous 4 days with an affected animal acquired since April 15, 2003, with vaccination considered up to 14 days after exposure |
| Anyone else, including children younger than 1 year old, pregnant women, and individuals with skin conditions, who has been exposed to monkeypox in the previous 14 days |
Adapted from Centers for Disease Control and Prevention. Smallpox vaccine and monkeypox. http://www.cdc.gov/ncidod/monkeypox/smallpoxvaccine_mpox.htm (accessed 5/19/04)
In March, 2004, the National Institutes of Health (NIH) reported that researchers at the National Institute of Allergy and Infectious Diseases (NIAID) had found that a mild, experimental smallpox vaccine, the modified vaccinia Ankara (MVA), is nearly as effective as is the standard smallpox vaccine in protecting monkeys against monkeypox. One importance of the finding, noted by Anthony S. Fauci, director of NIAID, relates to the search for a replacement vaccine for people with health conditions that preclude their being able to use the current smallpox vaccine. He also noted that an initial MVA injection might help lessen the side effects experienced from Dryvax, the only commercially available smallpox vaccine in the United States, and might serve as an important prevaccine for large-scale vaccination efforts in the event of a bioterror threat involving smallpox.18
Moss and colleagues reported in March 2004 a study comparing MVA with Dryvax, in which they divided 24 cynomologus monkeys into four groups of six monkeys each: (a) group 1 received two injections of MVA, one at the start of the study and a second 2 months later; (b) group 2 received the MVA vaccine at the start of the study and the Dryvax vaccine 2 months later; (c) group 3 received no injection at the start and the Dryvax vaccine 2 months later; and (d) group 4 received no vaccines. The researchers monitored the immune responses throughout the immunization period and later, after the monkeys were exposed to monkeypox. Two months after being given the second vaccination, all 24 monkeys were exposed to monkeypox. All the immunized monkeys remained healthy with no signs of disease except for a small number of lesions on those in the MVA-only group; the unvaccinated monkeys had more than 500 lesions each and became gravely ill or died.19 Studies are ongoing to determine the duration of protection offered by MVA versus Dryvax and the effect of dosage, as well as to evaluate the immune response to MVA in humans.
Hooper and colleagues also reported in March 2004 that rhesus macaques vaccinated with a DNA vaccine consisting of four vaccinia virus genes (L1R, A27L, A33R, and B5R) were protected from severe disease after receiving a lethal challenge with monkeypox virus. Animals vaccinated with a single gene that encodes a target of neutralizing antibodies developed severe disease but survived. Their results are the first demonstration that a subunit vaccine approach to smallpox-monkeypox immunization is feasible.20
Recently, Tesh and colleagues described a possible new model for studying infections caused by monkeypox virus.21 Their discovery that it produces a similar disease in ground squirrels and that these rodents can be used instead of monkeys in experiments should make work on a vaccine substantially easier.
The future
The developments of vaccines, ongoing research, and prohibitions on importation of exotic animals promise to provide means to thwart another attack of monkeypox such as occurred in the United States in 2003. The suggestions that occasionally have been voiced concerning the use of monkeypox as a weapon of bioterrorism do not seem to be of much concern. Nonetheless, such instances as the outbreak in 2003 are reminders that all healthcare providers, in addition to infectious disease specialists, must stay alert to the possibility of a new or re-emerging disease when patients present with unusual manifestations.
References
- 1.U.S. Health and Human Services. HHS bans rodent imports from Africa; prohibits domestic commerce in rodents and prairie dogs. Actions intended to prevent spread of monkeypox virus http://www.hhs.gov/news/press/2003pres/20030611a.html (accessed 9/12/04)
- 2.Wisconsin Department of Health and Family Services. Monkeypox Emergency order_issued June 12, 2003. http://www.dhfs.state.wi.us/dph_bcd/monkeypox/Order.htm (accessed 8/10/04)
- 3.Centers for Disease Control and Prevention. Preliminary report: Mul-tistate outbreak of monkeypox in persons exposed to pet prairie dogs. http://www.cdc.gov/ncidod/monkeypox/report060903.htm (accessed 9/12/04)
- 4.Reed K.D., Melski J.W., Graham M.B. The detection of monkeypox in humans in the Western Hemisphere. N Engl J Med. 2004;350:342–350. doi: 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- 5.Demmler G.G., Ligon B.L. Severe acute respiratory syndrome (SARS): a review of the history, epidemiology, prevention, and concerns for the future. Sem Pediatr Infect Dis. 2003;14:240–244. doi: 10.1016/S1045-1870(03)00056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Monkeypox home. Questions and answers about monkeypox. 2003 November 3, http://www.cdc.gov/ncidod/monkeypox/qa.htm (accessed 8/5/04) [Google Scholar]
- 7.U.S. Food and Drug Administration Interim rule to prevent transmission of monkeypox. FDA News. 2003 November 3, http://www.fda.gov/bbs/topics/NEWS/2003/NEW00970.html (accessed 8/10/04) [Google Scholar]
- 8.Cohen J. Exotic Diseases: Is an old virus up to new tricks? Science. 1997;277:312–313. doi: 10.1126/science.277.5324.312. [DOI] [PubMed] [Google Scholar]
- 9.Mwamba P.T., Tshioko K.F., Moudi A. Human monkeypox in Kasai Oriental, Zaire (1996–1997) Eurosurveillance Monthly. 1997;2:33–35. doi: 10.2807/esm.02.05.00161-en. Published jointly in Morbidity and Mortality Weekly Report 1997 (Vol. 46, No 14 of 11 April) and Weekly Epidemiological Report (vol. 72, No. 15 of 11 April) [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Monkeypox in the Democratic Republic of the Congo (former Zaire). Disease outbreaks reported 31 July 1997.
- 11.Jezek Z., Marennikova S.S., Mutumbo M., Nakano J.H., Paluku K.M., Szczeniowski M. Human monkeypox: A study of 2,510 contacts of 214 patients. J Infect Dis. 1986;154:551–555. doi: 10.1093/infdis/154.4.551. [DOI] [PubMed] [Google Scholar]
- 12.Guarner J., Johnson B.J., Paddock C.D. Monkeypox transmission and pathogenesis in prairie dogs. Emerg Infect Dis. 2004;10:426–431. doi: 10.3201/eid1003.030878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerberding JL, McClellan MB. Joint order of the Centers for Disease is feasible. Control and Prevention and the Food and Drug Administration, Department of Health and Human Services. http://www.fda.gov/oc/opacom/hottopics/monkeypox/monkeypox.html
- 14.Spano A.J., Lipsman J. Alert: Monkeypox in humans from prairie dogs & rabbits. 2003 11 June. [Google Scholar]
- 15.American Medical Association. Monkeypox outbreak-First in Western hemisphere: Animal-to-human transmission results in outbreak. http://www.ama-assn.org/ama/pub/article/1949–7749.html
- 16.Centers for Disease Control and Prevention Updated interim infection control and exposure management guidance in the health-case and community setting for patients with possible monkeypox virus infection. 2003 July 18, http://www.cdc.gov/ncidod/monkeypox/infectioncontrol.htm (accessed 8/6/04) [Google Scholar]
- 17.Centers for Disease Control and Prevention. Smallpox vaccine and monkeypox. http://www.cdc.gov/ncidod/monkeypox/smallpoxvaccine_mpox.htm(accessed 5/19/04)
- 18.Wenger J. Effectiveness of safer smallpox vaccine demonstrated against monkeypox. 2004 NIH News, Wednesday, March 10, http://www.nih.gov/news/pr/mar2004/niaid-10.htm (accessed 9/1/04) [Google Scholar]
- 19.Earl P.L., Americo J.L., Wyatt L.S. Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature. 2004;428:182–185. doi: 10.1038/nature02331. [DOI] [PubMed] [Google Scholar]
- 20.Hooper J.W., Thompson E., Wilhelmsen C. Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. J Virol. 2004;78:4433–4443. doi: 10.1128/JVI.78.9.4433-4443.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tesh RB, Watts DM, Sbrana E, Siirin M, Popov VL, Xiao S-Y. Experimental infection of ground squirrels (spemophilus tridecemlineatus) with monkeypox virus. Emerging Infec Dis 10:2004 http:www.cdc.gov/ncidod/EID/vol10no9/04-0310.htm [DOI] [PMC free article] [PubMed]


