Abstract
Introduction:
Many scoring systems have been developed to assist in diagnosis of acute appendicitis (AA). This study aimed to compare the screening performance characteristics of Alvarado, Eskelinen, Ohmann, Raja Isteri Pengiran Anak Saleha (RIPASA), and Tzanakis scores in predicting the need for appendectomy in AA patients.
Methods:
Our study prospectively evaluated AA patients that were treated in a tertiary hospital’s emergency department. The obtained data were used to calculate Alvarado, Tzanakis, RIPASA, Eskelinen and Ohmann scores. Patients were categorized into two groups according to their histopathological results: positive (PA) and negative appendectomy (NA). The accuracy of different scoring systems in diagnosing AA was investigated.
Results:
74 patients suspected to AA with the mean age of 36.68 ± 11.97 years were studied (56.8% male). The diagnosis was histopathologically confirmed in 65 cases (87.8%). Median Alvarado, Tzanakis, RIPASA, Eskelinen and Ohmann scores were significantly higher in patients with positive appendectomy. The area under the curve (AUC), sensitivity, and specificity of Tzanakis score in the cut-off value of 8 were 0.965, 84.4%, and 100%, respectively. For Ohmann and Alvarado scores, these measures were 0.941; 71.9%, 89.9% and 0.938, 60.9%, 89.9%, respectively. Tzanakis scoring system had the best screening performance in detection of cases with AA.
Conclusion:
Tzanakis score is more sensitive and specific than Alvarado, RIPASA, Eskelinen and Ohmann scores in identifying AA patients needing appendectomy.
Key Words: Appendicitis, Emergency Medicine, Diagnosis, Sensitivity and Specificity, Alvarado, Eskelinen, Ohmann, Raja Isteri Pengiran Anak Saleha Appendicitis, Tzanakis
Introduction
Acute appendicitis (AA) is the most common reason for surgical intervention among patients admitted to the emergency department (ED) with abdominal pain (1). Approximately one-third of AA cases present with atypical clinical symptoms (2). Perforation and negative appendectomy (NA) rates were as high as 12-21% and 13-36%, respectively, for patients that were diagnosed solely through physical examinations (3, 4).
In recent years, many scoring systems have been developed based on anamnesis scores, clinical symptoms and findings, and inflammatory parameters, to assist in diagnosis of AA (5-8). The Alvarado score is the first of these systems. It is based on symptoms, and clinical and laboratory results (9). Then Raja Isteri Pengiran Anak Saleha (RIPASA) system was developed for patients in Asia. In recent years Eskelinen, Ohmann and Tzanakis scores, which added radiological methods such as ultrasound to the scoring systems; clinical and laboratory findings were also followed. These scoring systems aim to reduce NA and mortality/morbidity rates by preventing complications (5-10).
Despite being inexpensive, reproducible and easy-to-use with high success rates, these systems still have not become a part of routine practice. This study aimed to compare the screening performance characteristics of Alvarado, Eskelinen, Ohmann, RIPASA and Tzanakis scores in predicting the need for appendectomy in AA patients.
Methods
Study design and setting
In this prospective cross-sectional study, patients who were admitted to the emergency department of a tertiary hospital (Health Science University Antalya Training and Research Hospital, Antalya, Turkey) with abdominal pain suspected to AA between May 2, 2019 and December 1, 2019 were evaluated. This study was approved by the ethics committee of the hospital (Ethics code: 2019-129). All subjects consented to participate in the study, and the data were recorded by ED physicians.
Participants
All cases with abdominal pain suspected to AA, who were referred to ED during the study period, were included using non-probability sampling method. The exclusion criteria were as follows: (a) being under 18 years of age, (b) elective appendectomy, (c) incarcerated or inguinal hernia, (d) non-operable patients, (e) not accepting hospitalization, and (f) incomplete data.
Data gathering
The following data were recorded for all subjects: complaints at the time of admission, and examination and laboratory findings. Significant ultrasonography (US) and abdominal computed tomography (CT) scan findings were also recorded. The following US findings indicated acute appendicitis: (a) non-compressible, (b) >6 mm outer diameter, (c) appendicolith, (d) target appearance in axial section, and (e) periappendiceal inflammation with fat stranding. The following CT findings indicated acute appendicitis: (a) dilated lumen (≥7mm), (b) appendicolith, (c) periappendiceal fluid collection, and (d) inflamed mesoappendix. The obtained data were used to calculate Alvarado, Tzanakis, RIPASA, Eskelinen and Ohmann scores. All patients underwent appendectomy and were categorized into two groups according to histopathologic diagnosis: positive appendectomy (PA) and negative appendectomy (NA).
Evaluated Scores
Alvarado
The Alvarado system evaluates 8 parameters, which include symptoms, clinical findings and leukocyte count. The highest possible score is 10, and appendectomy is recommended for scores >7 (11).
Ohmann and Eskelinen
The Ohmann score is also composed of 8 parameters (Tenderness in right lower quadrant, rebound tenderness, presence of urinary system complaint, character of pain, relocalization of pain to the right lower quadrant, age, leukocyte count, abdominal rigidity), a score ≥12 indicates AA (12). In addition to these parameters, the Eskelinen scoring system also considers the duration of pain and laboratory results. A score >57 indicates AA (13).
RIPASA and Tzanakis
Tzanakis et al. developed a scoring system consisting of 4 simplified variables and 15 points based on the combination of clinical evaluation, ultrasonography and laboratory parameters. RIPASA is a scoring system developed for the Asian and middle-eastern population with 15 objective parameters obtained during routine history taking, physical examination, and haematological assessment and urinalysis. A RIPASA score >12 and a Tzanakis score >8 indicate AA (8, 14).
Statistical Analysis
The data were analysed using SPSS version 18.0. Descriptive statistics for categorical data are expressed as numbers and percentages, while mean ± standard deviation and median (minimum-maximum) were used to express continuous data based on normal distribution. Student's t-test was used for variables with normal distribution, and Mann-Whitney U-test was used for variables without normal distribution. The screening performance characteristics of the scoring systems were measured. A greater area under the receiver operating characteristic (ROC) curve (AUC) indicates better diagnostic value. p<0.05 was considered statistically significant.
Results
Baseline characteristics of studied cases
The study included a total of 74 patients with a preliminary AA diagnosis: 42 males (56.8%) and 32 females (43.2%). Table 1 shows the baseline characteristics of studied cases. The median age was 33 (range: 18-63) years. The diagnosis was histopathologically confirmed in 65 cases (87.8%). Among these, 7 patients (9.4%) had perforated AA and 3 (4.0%) had lymphoid hyperplasia. 9 (12.2%) patients had negative appendectomy, 1 of these (1.4%) being ovarian cyst rupture. The mean white blood cell (WBC) count was 14.12 ± 4.71 ×103/mm3. The median scores of different systems were as follows: Alvarado score 7 (2-10); Ohmann score 13 (4-16); RIPASA score 10 (4.5-13.5); Tzanakis score 13 (3-15); Eskelinen score 51.1 (29.8-67.6).
Table 1.
Baseline characteristics of studied patients
| Variables | Values (n=74) |
|---|---|
| Age (years) | |
| Median (min-max) | 33 (18-63) |
| Mean ± standard deviation | 36.68 ± 11.97 |
| Gender, n (%) | |
| Male | 42 (56.8) |
| Female | 32 (43.2) |
| Appendectomy findings for AA | |
| Positive | 65 (87.8) |
| Negative | 9 (12.2) |
| Histopathological findings, n (%) | |
| Acute appendicitis | 53 (71.6) |
| Perforated appendicitis | 7 (9.4) |
| Lymphoid hyperplasia | 3 (4.0) |
| Unusual histopathological findings | 2 (2.8) |
| Appendix vermiformis | 8 (10.8) |
| Others | 1 (1.4) |
| Clinical findings, n (%) | |
| Sensitivity on lower right quadrant | 64 (86.5) |
| Defense-rigidity | 49 (66.2) |
| Rebound | 44 (59.5) |
| Fever (>37.3°) | 27 (36.5) |
| Nausea-Vomiting | 26 (35.1) |
| Laboratory findings | |
| WBC count (×103/mm3) | 14.12±4.71 |
| Neutrophils (×103/mm3) | 11.10±4.57 |
| Lymphocytes (×103/mm3) | 1.95±0.82 |
| C-reactive protein (mg/dL) | 24 (0-331) |
| Scores, median (min-max) | |
| Alvarado | 7 (2-10) |
| Ohmann | 13 (4-16) |
| RIPASA | 10 (4.5-13.5) |
| Tzanakis | 13 (3-15) |
| Eskelinen | 51.1 (29.8-67.6) |
AA: acute appendicitis; WBC: white blood cell; RIPASA: Raja Isteri Pengiran Anak Saleha Appendicitis.
Comparing the scores
Table 2 compares the baseline characteristics as well as scores between cases with negative and positive appendectomy. Median age was significantly higher in patients with positive appendectomy (p=0.006). There was no significant difference between patients with positive and negative appendectomy regarding gender (p=0.163). Ultrasonography results were not sufficient for diagnosing AA (p = 0.501); however, computed tomography (CT) scans were able to significantly determine AA (p <0.001). Median Alvarado, Tzanakis, RIPASA, Eskelinen and Ohmann scores were significantly higher in patients with positive appendectomy.
Table 2.
Comparing the baseline characteristics as well as acute appendicitis scores between cases with positive and negative appendectomy findings
| Variables |
Appendectomy findings
|
P value | |
|---|---|---|---|
| Negative (n=9) | Positive (n=65) | ||
| Age (years) | |||
| Median (min-max) | 27 (19-46) | 36 (18-63) | 0.006 |
| Gender, n (%) | |||
| Male | 3 (33.3) | 39 (60) | 0.163 |
| Female | 6 (66.7) | 26 (40) | |
| Ultrasonography findings, n (%) | |||
| Negative | 5 (55.6) | 28 (43.1) | 0.501 |
| Positive | 4 (44.4) | 37 (56.9) | |
| Computed tomography scan findings, n (%) | |||
| Negative | 5 (71.4) | 2 (3.6) | <0.001 |
| Positive | 2 (28.6) | 55 (96.4) | |
| Laboratory findings | |||
| WBC count (×103/mm3) | 10.38±3.00 | 14.64±4.69 | 0.01 |
| Neutrophils (×103/mm3) | 7.10±2.91 | 11.66±4.51 | 0.004 |
| Lymphocytes (×103/mm3) | 2.60±0.85 | 1.86±0.78 | 0.022 |
| C-reactive protein (mg/dL) | 9 (0-321) | 33 (0-331) | <0.001 |
| Clinical findings, n (%) | |||
| Sensitivity on lower right quadrant | 3 (33.3) | 61 (93.8) | <0.001 |
| Defense guarding | 3 (33.3) | 46 (70.8) | 0.026 |
| Rebound | 3 (33.3) | 41 (63.1) | 0.146 |
| Fever (>37.3°) | 4 (44.4) | 23 (35.4) | 0.716 |
| Nausea-Vomiting | 2 (22.2) | 24 (36.9) | 0.480 |
| Scores, median (min-max) | |||
| Alvarado | 4 (2-5) | 7 (3-10) | <0.001 |
| Ohmann | 8 (4-13) | 13.5 (8-16) | <0.001 |
| RIPASA | 6 (4.5-8) | 10 (4.5-13.5) | <0.001 |
| Tzanakis | 4 (3-7) | 13 (3-15) | <0.001 |
| Eskelinen | 35.1 (33.8-49.2) | 53.9 (29.8-67.6) | <0.001 |
WBC: White blood cell; RIPASA: Raja Isteri Pengiran Anak Saleha Appendicitis; min: minimum; max: maximum.
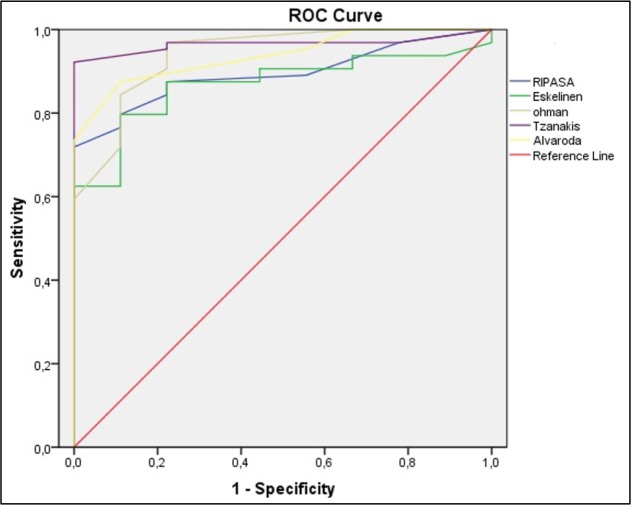
Screening performance characteristics of the studied systems in determining cases with AA are presented in table 3 and figure 1. Tzanakis score was able to determine AA better than the other scoring systems, followed by Ohmann and Alvarado scores, respectively (based on AUC). AUC, sensitivity, and specificity of Tzanakis score in the cut-off value of 8 were 0.965, 84.4%, and 100%, respectively. For Ohmann and Alvarado scores, these measures were 0.941; 71.9%, 89.9% and 0.938, 60.9%, 89.9%, respectively. Tzanakis scoring system had the best screening performance in detection of cases with AA.
Table 3.
Screening performance characteristics of different scoring systems in prediction of acute appendicitis in emergency department
| Alvarado | Ohmann | RIPASA | Tzanakis | Eskelinen | |
|---|---|---|---|---|---|
| TP | 40 | 47 | 55 | 56 | 42 |
| TN | 8 | 8 | 8 | 8 | 7 |
| FP | 1 | 1 | 1 | 1 | 2 |
| FN | 25 | 18 | 10 | 9 | 23 |
| Sensitivity | 60.9 (48.64-73.35) |
71.9 (59.81-82.69) |
75 (64.81-86.47) |
84.4 (75.34-93.47) |
64.1 (51.77-76.08) |
| Specificity | 89.9 (51.75-99.72) |
89.9 (51.75-99.72) |
99.72 (51.75-100) |
99.88 (51.75-99.72) |
78 (39.99-99.19) |
| PPV | 97.56 (86.19-99.61) |
97.92 (88.04-99.67) |
98.04 (88.69-99.69) |
98.25 (89.80-99.72) |
95.45 (85.93-98.63) |
| NPV | 24.24 (17.89-31.98) |
30.77 (21.98-41.21) |
34.78 (24.44-46.80) |
47.06 (31.72-62.97) |
23.33 (15.86-32.96) |
| PLR | 5.54 (0.86-35.56) |
6.51 (1.02-41.55) |
6.92 (1.09-44.15) |
7.75 (1.22-49.24) |
2.91 (0.85-10.00) |
| NLR | 0.43 (0.29-0.64) |
0.21 (0.20-0.49) |
0.26 (0.16-0.43) |
0.16 (0.08-0.30) |
0.45 (0.28-0.73) |
| AUC | 0.93 (0.87-0.99) |
0.94 (0.88-1.00) |
0.89 (0.81-0.97) |
0.96 (0.90-1.00) |
0.86 (0.77-0.97) |
Data are presented with 95% confidence interval (CI). Measures are calculated in cut-offs: ≥8 for Alvarado score; ≥12 for Ohmann score; ≥12 for RIPASA score; ≥8 for Tzanakis score; ≥57 for Eskelinen score.
TP: true positive; TN: true negative; FP: false positive; FN: false negative; PPV: positive predictive value; NPV: negative predictive value; PLR: positive likelihood ratio; Negative likelihood ratio; AUC; area under the receiver operating characteristic (ROC) curve.
Figure 1.
The area under the Receiver operating characteristic (ROC) curve of studied scoring systems in detecting acute appendicitis cases with positive appendectomy in emergency department. (p <0.001 for all scoring systems)
Discussion
Based on the findings of the present study, Tzanakis score has higher sensitivity and specificity in the diagnosis of AA compared to Alvarado, RIPASA, Eskelinen and Ohmann scores.
The differential diagnosis of AA only requires simple physical and laboratory analyses; however, it is commonly misdiagnosed due to atypical findings. Perforation and NA rates are still significantly high. The importance of timely and precise diagnosis has led researchers to develop different scoring systems (15). Alvarado is the first and most widely used among them (10). It is simple, easy-to-use and can successfully predict AA (16). Subraman et al. reported the sensitivity and specificity of Alvarado score to be 68% and 86.96%, respectively (17). Whereas, Elhosseiny et al. found these values to be 65.2% and 100%, respectively (18). We have found the sensitivity and specificity of Alvarado scores to be 60.9% and 89.9%, respectively. Khan et al. reported NA and perforated appendectomy rates to be 15.6% and 7.8%, respectively (19). Researchers have been trying to develop better diagnostic methods to decrease these numbers.
Studies suggest that the RIPASA score is more accurate than the Alvarado score, especially in Eastern societies (18). Frountzas et al. studied 2161 cases of AA and found that while the RIPASA system was more sensitive, it had a lower specificity than the Alvarado system (20). Chong et al. studied the RIPASA scoring system, and found that it had 97.5% sensitivity, 81.8% specificity and 91.8% diagnostic accuracy (21). We have found that the AUC for the RIPASA score was slightly lower than the Alvarado score (0.893 vs. 0938).
The Ohmann score is a simple test that can help diagnose patients with suspected AA (22). Similarly, the Eskelinen score is considerably successful in ruling out the diagnosis of AA (23). Erdem et al. found that the sensitivity and specificity of the Ohmann and Eskelinen scores 96% and 42%, and 100% and 44%, respectively (24). We found that Ohmann and Eskelinen scores failed to diagnose AA, but they were sufficiently specific. The Eskelinen score is at a disadvantage due to its decimal calculations that make it less practical. It also may require additional diagnostic methods, such as laboratory testing or ultrasonography, for differential diagnosis.
The Tzanakis score was suggested as a combined clinical evaluation of US results and inflammatory markers, the highest possible score is 15, and ≥8 indicates AA. The sensitivity and specificity were 95.4% and 97.4%, respectively (25). Sigdel et al. reported that the Tzanakis score was as effective as the Alvarado score, with a lower false-negative rate (26). Studies show sensitivity levels to be between 85-96%, but Sigdel et al. attribute these low rates to differences in the experience levels of radiologists that perform US (26, 27).
Limitation
The limitations of our study are as follows: (a) the relatively small sample size despite the prospective nature of the study, and (b) different physicians deciding for appendectomy for different cases. Further prospective studies with larger sample sizes are required to support our findings.
Conclusion
Tzanakis score has higher sensitivity and specificity in diagnosis of AA compared to Alvarado, RIPASA, Eskelinen and Ohmann scores.
Acknowledgements
The author would like to thank MD. Aysegul Korkut for helping in preparation of this paper.
Author contribution
All the authors made a substantial contribution in study design, data interpretation and writing and reviewing the manuscript.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Ethics committee approval was received for this study.
Funding and support
No funding and support was received for this study.
References
- 1.Karaman K, Ercan M, Demir H, Yalkın Ö, Uzunoğlu Y, Gündoğdu K, et al. The Karaman score: A new diagnostic score for acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2018;24(6):545–51. doi: 10.5505/tjtes.2018.62436. [DOI] [PubMed] [Google Scholar]
- 2.Dal F, Çiçek Y, Pekmezci S, Kocazeybek B, Tokman HB, Konukoğlu D, et al. Role of Alvarado score and biological indicators of C-reactive protein, procalicitonin and neopterin in diagnosis of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2019;25(3):229–37. doi: 10.5505/tjtes.2018.57362. [DOI] [PubMed] [Google Scholar]
- 3.Çalışkan YK. Original Alvarado scoring system in the diagnosis of acute appendicitis: A cohort study. Journal of Surgery and Medicine. 2017;1(2):28–31. [Google Scholar]
- 4.Bakula B, Biljak VR, Bakula M, Rašić F, Šimundić A-M. Retrospective Evaluation of the Diagnostic Accuracy of the Modified Alvarado Scoring System (MASS) in a Croatian Hospital. Acta medica academica. 2019;48(2) doi: 10.5644/ama2006-124.256. [DOI] [PubMed] [Google Scholar]
- 5.Karimi E, Aminianfar M, Zarafshani K, Safaie A. The accuracy of emergency physicians in ultrasonographic screening of acute appendicitis; a cross sectional study. Emergency. 2017;5:1. [PMC free article] [PubMed] [Google Scholar]
- 6.Jain S, Gehlot A, Songra M. Modified alvarado score in diagnosis of acute appendicitis: a clinicopathological study. International Surgery Journal. 2018;5(3):878–82. [Google Scholar]
- 7.Pasumarthi V, Madhu C. A comparative study of RIPASA score and ALVARADO score in diagnosis of acute appendicitis. International Surgery Journal. 2018;5(3):796–801. [Google Scholar]
- 8.Lakshminarasimhaiah AKS, Nagaraja A, Srinivasaiah M. Evaluation of Tzanakis scoring system in acute appendicitis: a prospective study. International Surgery Journal. 2017;4(10):3338–43. [Google Scholar]
- 9.Benabbas R, Hanna M, Shah J, Sinert R. Diagnostic Accuracy of History, Physical Examination, Laboratory Tests, and Point‐of‐care Ultrasound for Pediatric Acute Appendicitis in the Emergency Department: A Systematic Review and Meta‐analysis. Academic Emergency Medicine. 2017;24(5):523–51. doi: 10.1111/acem.13181. [DOI] [PubMed] [Google Scholar]
- 10.Ferlengez E, Ferlengez AG, Akbulut H, Kadioglu H. Evaluation of four different scoring systems in the management of acute appendicitis; a prospective clinical study/Akut Apandisit Degerlendirilmesinde Dort Farkli Skorlama Sisteminin Degerlendirilmesi; ileri Donuk Klinik Calisma. The Medical Bulletin of Haseki. 2013;51(1):15–8. [Google Scholar]
- 11.Yılmaz EM, Kapçı M, Çelik S, Manoğlu B, Avcil M, Karacan E. Should Alvarado and Ohmann scores be real indicators for diagnosis of appendicitis and severity of inflammation? Turkish Journal of Trauma and Emergency Surgery. 2017;23(1):29–33. doi: 10.5505/tjtes.2016.89894. [DOI] [PubMed] [Google Scholar]
- 12.Lintula H, Pesonen E, Kokki H, Vanamo K, Eskelinen M. A diagnostic score for children with suspected appendicitis. Langenbeck's archives of surgery. 2005;390(2):164–70. doi: 10.1007/s00423-005-0545-8. [DOI] [PubMed] [Google Scholar]
- 13.Kiyak G, Korukluoğlu B, Ozgün Y, Devay AO, Kuşdemir A. Evaluation of Ohmann and Eskelinen scores, leukocyte count and ultrasonography findings for diagnosis of appendicitis. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES. 2009;15(1):77–81. [PubMed] [Google Scholar]
- 14.Butt MQ, Chatha SS, Ghumman AQ, Farooq M. RIPASA score: a new diagnostic score for diagnosis of acute appendicitis. J Coll Physicians Surg Pak. 2014;24(12):894–7. [PubMed] [Google Scholar]
- 15.Kollár D, McCartan D, Bourke M, Cross K, Dowdall J. Predicting acute appendicitis? A comparison of the Alvarado score, the Appendicitis Inflammatory Response Score and clinical assessment. World journal of surgery. 2015;39(1):104–9. doi: 10.1007/s00268-014-2794-6. [DOI] [PubMed] [Google Scholar]
- 16.Jalil A, Shah SA, Saaiq M, Zubair M, Riaz U, Habib Y. Alvarado scoring system in prediction of acute appendicitis. J Coll Physicians Surg Pak. 2011;21(12):753–55. [PubMed] [Google Scholar]
- 17.Subramani B, Kalaichelvan L, Selvam G, Madhavan L. Comparison between RIPASA and alvarado scoring in diagnosing acute appendicitis. J Evid Based Med Health. 2017;4(11):624–7. [Google Scholar]
- 18.Elhosseiny MM, Eltokhy E, Elekiabi OA, Elaidy MM, Tamer Mohamed El shahidy, et al. Comparative Study between Alvarado Score& Ripasa Score in Diagnosis of Acute Appendicitis. J Surgery. 2018;6(2) [Google Scholar]
- 19.Khan I, ur Rehman A. Application of Alvarado scoring system in diagnosis of acute appendicitis. Journal of Ayub Medical College Abbottabad. 2005;17:3. [PubMed] [Google Scholar]
- 20.Frountzas M, Stergios K, Kopsini D, Schizas D, Kontzoglou K, Toutouzas K. Alvarado or RIPASA score for diagnosis of acute appendicitis? A meta-analysis of randomized trials. International Journal of Surgery. 2018;56:307–14. doi: 10.1016/j.ijsu.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Chong CF, Thien A, Mackie AJA, Tin AS, Tripathi S, Ahmad M, et al. Evaluation of the RIPASA Score: a new scoring system for the diagnosis of acute appendicitis. Brueni Int Med J. 2010;6:17–26. [Google Scholar]
- 22.Ahn S, Lee H, Choi W, Ahn R, Hong J-S, Sohn CH, et al. Clinical importance of the heel drop test and a new clinical score for adult appendicitis. PloS one. 2016;11(10) doi: 10.1371/journal.pone.0164574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zielke A, Sitter H, Rampp T, Bohrer T, Rothmund M. Clinical decision-making, ultrasonography, and scores for evaluation of suspected acute appendicitis. World journal of surgery. 2001;25(5):578–84. doi: 10.1007/s002680020078. [DOI] [PubMed] [Google Scholar]
- 24.Erdem H, Çetinkünar S, Daş K, Reyhan E, Değer C, Aziret M, et al. Alvarado, Eskelinen, Ohhmann and Raja Isteri Pengiran Anak Saleha appendicitis scores for diagnosis of acute appendicitis. World Journal of Gastroenterology: WJG. 2013;19(47):9057. doi: 10.3748/wjg.v19.i47.9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malla B, Batajoo H. Comparison of Tzanakis score vs alvarado score in the effective diagnosis of acute appendicitis. Kathmandu University medical journal. 2014;12(1):48–50. doi: 10.3126/kumj.v12i1.13638. [DOI] [PubMed] [Google Scholar]
- 26.Sigdel G, Lakhey P, Misra P. Tzanakis Score vs Alvarado in Acute Appendicitis. Journal of Nepal Medical Association. 2010;49:178. [PubMed] [Google Scholar]
- 27.Umar MM, Abubakar IU, Agbo SP. Comparative study of alvarado score and its modifications in the preoperative diagnosis of acute appendicitis at a tertiary center in Sokoto, Nigeria. Nigerian Journal of Surgery. 2020;26(1):16. doi: 10.4103/njs.NJS_46_19. [DOI] [PMC free article] [PubMed] [Google Scholar]