To the Editor:
The experience in management of the endoscopy unit during the COVID-19 pandemic shared by Thompson et al,1 Repici et al,2 and Soetikno et al3 deserves recognition. Identifying the risk of fecal–oral transmission4 and subsequently preventing potential nosocomial infections caused by digestive endoscopy are urgent issues.
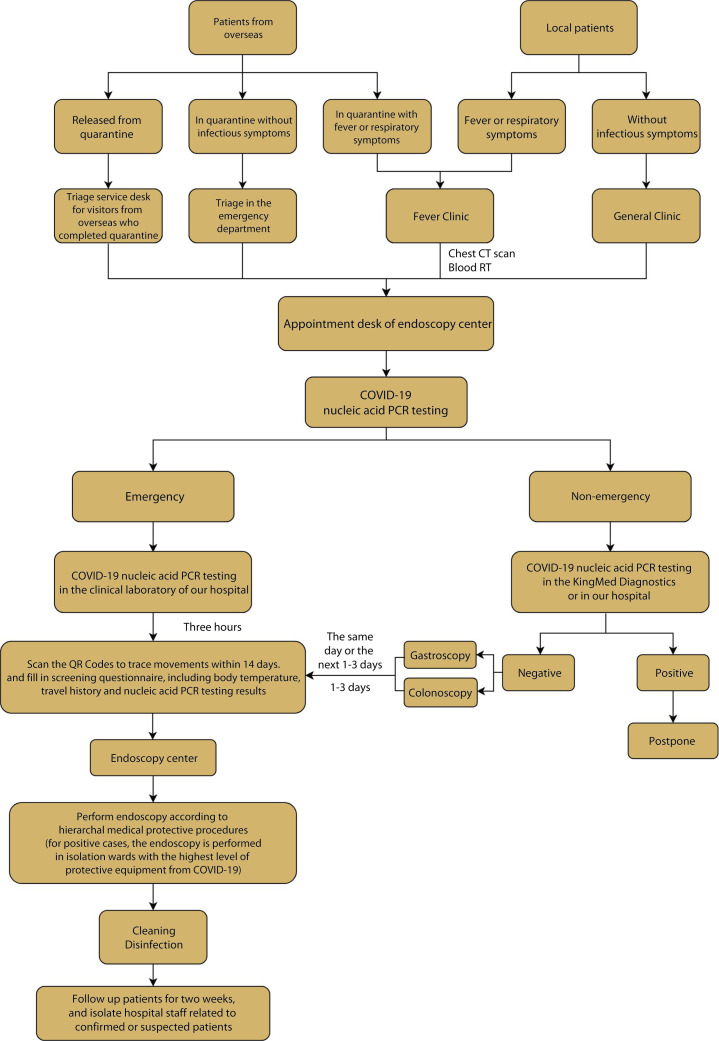
Faced with the situation of the reduced number of new domestic cases for the past month and the mounting number of imported cases in South China, our center has restored nonemergency service and executed a strict protocol (Fig. 1 ) since March 2, 2020. Patients who seek endoscopy examinations or treatment must undergo triage and make appointments beforehand. For those with fever or respiratory symptoms, chest CT scans and routine blood tests are further required. Patients from overseas who are still in 14-day quarantine but have no infectious symptoms also undergo triage in the emergency department. For those released from quarantine, an official releasing document issued by the health authority is required, and they must register before making endoscopy appointments. After appointments are made, throat swabs must be collected and used for COVID-19 nucleic acid polymerase chain reaction testing. Emergency patients undergo 3-hour rapid testing on the day of endoscopy, whereas nonemergency patients can choose either the 3-hour self-paying test or the 24-hour free test, within 3 days before endoscopy. After getting the COVID-19 test result, patients scan the quick responce code provided by the Chinese government to report possible history of exposure for the previous 14 days. They are also asked to complete screening questionnaires, which include questions regarding body temperature, travel history, and nucleic acid polymerase chain reaction testing results within 3 days. Only after complete evaluation are patients admitted to the endoscopy center. During the endoscopy examination, medical workers are required to wear hierarchal personal protective equipment including surgical masks, face shields or goggles, disposable hats and shoe covers, gowns, and gloves.
Figure 1.
Flow chart for diagnosis and treatment in endoscopy center during resuming period. Based on our clinical experience, the flow chart describes the medical procedure in our endoscopy center, including initial screening, endoscopic operation, medical precautions for medical workers, cleaning and disinfection after examination, and patient follow-up. For discharged COVID-19 patients, we perform endoscopy if necessary and issue relevant certification materials. Blood RT, Blood routine test; PCR, polymerase chain reaction; QR Code, quick responce code.
For the past 19 work days at this writing, the number of endoscopic cases in our center has increased gradually and reached 70 cases per day, which is 35% of our full capacity, with a total case number of 1361 since March 2, 2020. More importantly, no endoscopy-related COVID-19 nosocomial infections have been reported because of the strict execution of screening protocols in our center. Our experience demonstrates that strict screening procedures may prevent the spread of COVID-19 during digestive endoscopy during the resuming period.
Disclosure
All authors disclosed no financial relationships.
References
- 1.Thompson C.C., Shen L., Lee L.S. COVID-19 in endoscopy: Time to do more? Gastrointest Endosc. 2020;92:435–439. doi: 10.1016/j.gie.2020.03.3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Repici A, Maselli R, Colombo M, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. Epub 2020 Mar 13. [DOI] [PMC free article] [PubMed]
- 3.Soetikno R, Teoh AY, Kaltenbach T, et al. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. Epub 2020 Mar 27. [DOI] [PMC free article] [PubMed]
- 4.Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. Epub 2020 Feb 26. [DOI] [PMC free article] [PubMed]