Dear Editor,
Recently, there have been some studies of COVID-19 reported in this journal.1 , 2 The 2019 coronavirus outbreak has affected more than 60 countries. As of 6 March 2020, 100,326 patients have been reported, including 80,718 cases in China and 19,608 in other countries. The cause, a novel contagious respiratory virus named as severe acute respiratory syndrome coronavirus 2(SARS-CoV-2), also known as COVID-19, is a serious threat to global public health, like severe acute respiratory syndrome coronavirus (SARS-CoV) in 2003 and middle east respiratory syndrome coronavirus (MERS-CoV) in 2015. Though less lethal, COVID-19 seems to be more infectious than SARS; it can spread through respiratory, aerosol, and fecal-oral transmission.3 The basic reproductive number of the virus, R 0, was estimated to be 2.2 to 2.7.4 , 5 Without effective controls, COVID-19 may soon evolve into a global pandemic.
China has successfully curbed the rapid spread of COVID-19 by adopting containment strategies such as building shelter hospitals and blockading cities. The number of newly diagnosed cases has continued to decline since 16 February 2020. One important key to the prevention and control of COVID-19 is to find suspected cases through patients’ close contacts as soon as possible. Here we show how to adopt close contacts tracking management in a cluster investigation. It provides references for other regions to formulate and implement effective measures.
On 26 January 2020, a patient from fever clinics was tested nucleic acid positive for SARS-CoV-2 and become the first diagnosed case in Jiaxing. The local health administration initiated public health emergency response immediately. The patient received isolation treatment in a hospital, and the case was reported to the National Infectious Disease Information System. A response team consisted of Jiaxing center for disease control and prevention (CDC) officers, clinicians, and community workers moved fast by using close contacts tracking management. This method included three parts—epidemiological survey of cases, tracking of close contacts, and management of quarantine. It was based on Prevention and Control Protocol for Novel Coronavirus Pneumonia (version 2).6
Firstly, investigators from Jiaxing CDC conducted a face-to-face interview with a case. Demographic and clinical characteristics were summarized using descriptive statistics in 24 h. The focus of investigation were exposure history and close contacts of the case. People who had unprotected close contact with a case were defined as close contacts, such as those living, studying, or working together, or those travelling on the same vehicle during onset. Close contacts would be found in the shortest time by using epidemiological surveys and big data analysis. Then, all of them were required to stay at home or be isolated for 14 days. During the quarantine, they were under medical observation including checking of body temperature and clinical symptoms. Community workers provided them with life support, including food, medicine, and other daily necessities. Close contacts would be transferred to the hospital for treatment and nucleic acid test when they showed symptoms such as fever, cough, or diarrhea. When the last contact was released from medical observation, the cluster epidemic was over.
Respiratory samples including nasopharyngeal and throat swabs, and sputum or bronchoalveolar lavage fluid were put into viral transport mediums. Samples of the patients were tested for influenza A and B viruses using the Xpert Xpress Flu/RSV assay (GeneXpert System, Cepheid, Sunnyvale, CA, USA) according to the manufacturer's instructions. The nucleic acid test for SARS-CoV-2 was run by real-time RT-PCR. Test kit was from Zhuo Cheng Hui Sheng Biotechnology Co., Ltd and Berger Medical Technology Co., Ltd.
From January 26 to 28, the team had investigated 547 close contacts, including family members, colleagues, hospital visitors, co-diners, contacts at farmers' markets, and bus passengers. The close contact time ranged from January 18 to 26. All of them received centralized isolation and medical observation.
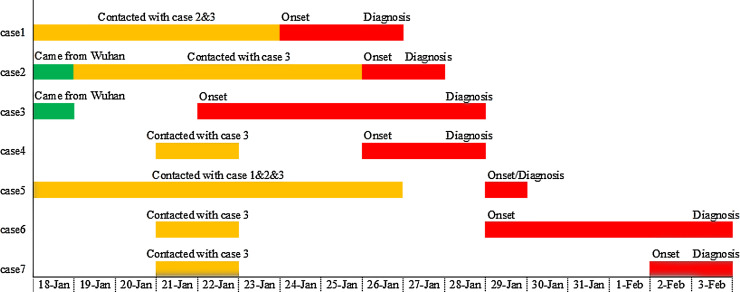
There were 7 cases in the cluster of COVID-19, including 4 from one family. Five of them were common cases, one was a severe case, and one was a mild case. No death occurred. We numbered the cases according to the chronology of diagnosis. The characteristics of the cluster cases are summarized in Table 1 . The chronology of cluster cases is presented in Fig. 1 .
Table 1.
Summary of characteristics for the cluster cases with COVID-19.
| Characteristics | Case 1 | Case 2 | Case 3* | Case 4 | Case 5 | Case 6 | Case 7 |
|---|---|---|---|---|---|---|---|
| Relationship | Son-in-law of Cases 2 and 3 | Mother-in-law of Case 1 | Father-in-law of Case 1 | Co-diner of Case 3 | Daughter of Case 1 | Co-diner of Case 3 | Co-diner of Case 3 |
| Sex | Male | Female | Male | Male | Female | Male | Female |
| Age | 29 years | 51 years | 54 years | 41 years | 4 months | 57 years | 41 years |
| Occupation | Office worker | Cloth merchant | Cloth merchant | Company manager | NA | Government employee | Office worker |
| Medical history | N | Gastric cancer surgery | N | N | N | N | N |
| Wuhan residence history | N | Y | Y | N | N | N | N |
| Clinical symptoms | Cough; fever; expectoration | Dry and itchy throat; fever; cough; blurred vision | Fever; cough | Fever; chills; fatigue; leg pain; cough | Fever; diarrhea | Fever; cough; expectoration | Fever; chills |
| Body temperature (°C) | 38.1 | 38.5 | 37.8 | 38.0 | 37.5 | 37.8 | 38.0 |
| Leukocyte count (109/L) (normal range 3.9–9.9) | 7.8 | 1.3 (↓) | 2.9(↓) | 5.4 | 7.5 | 5.4 | 8.9 |
| Lymphocyte count (109/L) (normal range 1.1–3.6) | 0.8(↓) | 0.6 (↓) | 0.7 (↓) | 7.6 (↑) | 3.0 | 1.0 (↓) | 0.7 (↓) |
| Radiological changes of lung | N | N | N | Y | N | Y | Y |
| Date of symptom onset | 2020/1/24 | 2020/1/25 | 2020/1/22 | 2020/1/26 | 2020/1/29 | 2020/1/29 | 2020/2/2 |
| Test samples | Throat swab | Throat swab | Throat swab | Throat swab | Throat swab | Sputum | Throat swab |
| Date of nucleic acid test positive | 2020/1/26 | 2020/1/27 | 2020/1/28 | 2020/1/28 | 2020/1/29 | 2020/2/3 | 2020/2/3 |
| Severity of pneumonia | Severe | Common | Common | Common | Mild | Common | Common |
| Outcome | Cure | Cure | Cure | Cure | Cure | Cure | Cure |
Fig 1.
Chronology of cluster cases with COVID-19.
Case 1
Case 1 has been living in Jiaxing. He had neither visited Wuhan before the onset, nor had contact with a diagnosed COVID-19 patient or wild animals. Considering the outbreak epidemic of Wuhan, the people that Case 1 had contact with who had recently sojourned in Wuhan should be the investigation target. In the morning of January 18, Case 1 drove to the train station to pick up his father-in-law (Case 3) and mother-in-law (Case 2) who had returned from Wuhan. They lived together for the next few days.
Case 1 showed symptoms of cough and expectoration on January 24. He went to the fever clinic around 12:00 AM on January 25. Nucleic acid test of SARS-CoV-2 at 9:00 AM on January 26 was positive.
Cases 2 and 3
Through the inquiry of Case 1, it was known that his father-in-law and mother-in-law had recently returned from Wuhan. Investigators had taken quarantine measures and retrospective investigations on them. Cases 2 and 3 had lived in Wuhan for several years. They came to Jiaxing for Chinese New Year on January 18. They had never been to the South China Seafood Market (where the animal origin of the virus was found) or eaten wild animals in Wuhan. They had not been to hospitals in Wuhan in the past months. They were living with their daughter, son-in-law (Case 1), grandson, and granddaughter (Case 5) during their visit in Jiaxing. During their visit time, they had ignored the official warning of the epidemic and did not reduce social activities.
In the morning of January 25, Case 2 had a dry and itchy throat. The throat swab sample was tested positive for nucleic acid at 4:00 AM on January 27.
Case 3 had a fever of 37.8 °C in the evening on January 22, and a dry cough the next day. He did not seek treatment as his symptoms were mild. After his son-in-law (Case 1) was diagnosed, Case 3 was taken to the hospital as a symptomatic close contact. The first nucleic acid test was negative on January 27, and the second was positive on January 28.
According to the time of onset and epidemiological history, investigators conducted an in-depth investigation on the activities and contacts of Cases 1–3.
Case 4
Cases 4 and 3 had attended a wedding banquet during January 21 to 22. He was a co-diner of Case 3. The symptoms of fever, chills, fatigue, leg pain, and cough began to appear in Case 4 from 7:00 PM on January 26. He was confirmed positive at 7:40 PM on January 28.
Case 5
Case 5 is the daughter of Case 1. She was taken care of by Case 2 since January 18. During the quarantine, Case 5 showed low fever and diarrhea at around 4:00 AM on January 29. She was confirmed positive at 9:30 PM on January 29. Her mother and brother tested negative.
Case 6
Cases 6 and 3 spoke face to face for 15 min in the evening of January 21. They had dinner at the same table the next day. On January 29, he developed symptoms of low fever, cough, and expectoration. The first nucleic acid test of throat swabs was negative on February 1, and the second test of sputum was positive on February 3.
Case 7
As a co-diner of Case 3, Case 7 also showed symptoms during the quarantine. Local CDC tested Case 7 as positive for the coronavirus on February 3.
It is a public health emergency caused by imported cases from Wuhan. Two cases in the family were closely related to Cases 2 and 3, but it was impossible to accurately determine who was Patient Zero. The other three cases were caused by direct contact with Case 3. According to the time of onset and number of pathogenic persons, it was considered that Case 3 was a ‘superspreader’ in the transmission. Jiaxing CDC and community workers reacted swiftly since the first case was confirmed. In 72 h, 547 people had been contacted and isolated, 6 cases found. Fourteen days after the first case, the transmission chain was cut.
COVID-19 is a new infectious respiratory disease. It has spread extremely rapidly from a single city to the world in only about 60 days. The novel coronavirus is highly contagious as assessed by the characterization and exploratory analysis of 72,314 cases. Children seemed to be as susceptible as adults.7 , 8 The youngest infected person in our study was only four months old. Fortunately, COVID-19 is mild for 81% of patients, and the overall mortality rate is only 2.3%.9
In order to avoid panic, it is necessary to announce the epidemic situation to the public in time. These policies can help citizens understand the virus and cooperate with the prevention. In our city, we have been promoting the prevention of seasonal respiratory infectious diseases since the beginning of January. After the outbreak of COVID-19, we published the epidemic data and risk assessment every day. It was helpful to find those close contacts of confirmed cases. This study provides important insights on how to design effective prevention and control strategies.
Some studies have found that patients showing asymptomatic infections during the incubation period also have transmission.10 Therefore, the time range of close contact was from two days before the onset to isolation in our investigation. Our results show that the incubation period falls within 14 days (range of 5–12 days). This was consistent with other studies.11 , 12 All the cases in the survey had symptoms such as fever, etc., suggesting that symptom screening is still important. In particular, temperature monitoring in the fever clinics may help to find suspected cases.
The disease is more complicated than we expected, and the mechanism is still unknown. COVID-19 can show the clinical characteristics of normal or reduced leukocyte count, decreased lymphocyte count, and lung lesions,13 , 14 which are helpful in the differential diagnosis. For the differences of viral load and physical fitness, the progression and infection time of COVID-19 is not consistent. Early detection and treatment could help to halt the deterioration and reduce the investment of follow-up medical resources. All the cases in the study were treated in time after symptoms onset. After a period of supportive treatment, they recovered without using ventilators or extracorporeal membrane oxygenation (ECMO).
At present, COVID-19 patients are recognized as the only source of human-to-human transmission. Managing patients and close contacts is an effective way to control the situation. After the first case was confirmed, we found all close contacts and isolated them for medical observation. Finally, five close contacts were diagnosed. As a result of the adoption of close contact tracking management technology, the epidemic did not spread widely.
Indeed, the key point of COVID-19 prevention and control is to find suspected cases from close contacts as soon as possible. It will not only reduce risks of community infection, but also help save medical resources. We would like to inform public health colleagues who are preparing or may have experienced COVID-19 in their countries to detect the outbreak early and respond quickly using China's experience.
Declaration of Competing Interest
The authors declare no conflicts of interest.
Acknowledgments
Acknowledgments
We thank Jiaxing First Hospital for the assistance and guidance, it provided clinical data for this study.
Sources of funding
This work was supported by Medical Science and Technology Project of Zhejiang (Grant 2019327380 to Dr. Ge)
References
- 1.He Y., Wang Z.L., Li F. Public health might be endangered by possible prolonged discharge of SARS-CoV-2 in stool. J Infect. 2020 doi: 10.1016/j.jinf.2020.02.031. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang W., Tambyah P.A., Hui S.C. Emergence of a novel coronavirus causing respiratory illness from Wuhan, China. J Infect. 2020 doi: 10.1016/j.jinf.2020.01.014. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/S2468-1253(20)30048-0. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. NEMJ. 2020 doi: 10.1056/NEJMoa2001316. published online Jan 29https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30260-9. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.General Office of National Health Commission of the People's Republic of China. Prevention and control protocol for novel coronavirus pneumonia (version 2) [EB/OL]. http://www.gov.cn/zhengce/zhengceku/2020-02/07/content_5475813.htm
- 7.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- 8.Wei M., Yuan J., Liu Y. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 doi: 10.1001/jama.2020.2131. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Wkly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 10.Pan X., Chen D., Xia Y. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30114-6. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lauer S.A., Grantz K.H., Bi Q. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020 doi: 10.7326/M20-0504. published online Mar 10. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linton N.M., Kobayashi T., Yang Y. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020 doi: 10.3390/jcm9020538. published online Feb 17https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu X.W., Wu X.X., Jiang X.G. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020 doi: 10.1136/bmj.m606. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]