Abstract
Objectives:
In the United States, an estimated 553,000 people are homeless on any given night. Few data provide large-scale, contemporary insight with regard to recent patterns of acute illness in this vulnerable population. We evaluated patterns, causes, and outcomes of acute hospitalization among homeless persons compared with a demographics-standardized and risk-standardized nonhomeless cohort.
Methods:
Retrospective study comparing 185,292 hospitalizations for homeless individuals and 32,322,569 hospitalizations for demographics-standardized nonhomeless individuals between 2007 and 2013 in Massachusetts, Florida, and California. Annual hospitalization rates for homeless persons were calculated and causes of hospitalization were compared with a demographics-standardized nonhomeless cohort. Logistic and linear regression models were used to estimate risk-standardized outcomes.
Results:
From 2007 to 2013, hospitalizations for the homeless increased in Massachusetts (294 to 420 hospitalizations per 1000 homeless residents), Florida (161 to 240/1000), and California (133 to 164/1000). Homeless patients were on average 46 years of age, often male (76.1%), white (62%), and either uninsured (41.9%) or insured by Medicaid (31.7%). Hospitalizations for homeless persons, compared with demographics-standardized nonhomeless, were more frequently for mental illness and substance use disorder (52% vs. 18%, P < 0.001). Homeless compared with risk-standardized nonhomeless individuals had lower in-hospital mortality rates (0.9% vs. 1.2%, P < 0.001), longer mean length of stay (6.5 vs. 5.9 d, P < 0.001), and lower mean costs per day ($1 535 vs. $1 834, P < 0.001).
Conclusions:
Hospitalizations among homeless persons are rising. Despite greater policy and public health focus over the last few decades, mental illness and substance use remain primary drivers of acute hospitalization among homeless adults. Policy efforts should address barriers to the use of ambulatory care services, and behavioral health services in particular, to help reduce acute care use and improve the long-term health of homeless individuals.
Keywords: Homeless persons, homelessness, vulnerable populations, health disparities, health outcomes, public health, affordable care act
In the United States, an estimated 553,000 people are homeless on any given night, although the number of individuals that experience homelessness annually is significantly higher.1,2 The homeless population face competing demands, such as food, shelter, and safety, and as a result, are less likely to have a reliable source of health care.3 Homeless persons also have a high burden of mental illness and substance use disorder, for which access to treatment services are often limited.4 These factors contribute to greater use of acute care services, low life expectancy and high mortality rates among people experiencing homelessness.5,6
In recent years, efforts to address the health of the homeless population have intensified in the United States, through increased funding under the Affordable Care Act (ACA) for health centers that care for homeless persons, the expansion of federally funded Health Care for the Homeless clinical services, and enthusiasm for a “housing first” approach for chronic homelessness.7,8 Despite these efforts, surprisingly little contemporary data exist with regard to recent patterns and causes of acute hospitalization and associated outcomes among homeless people. Most US-based studies on hospitalizations among homeless adults are outdated or predominately focus on a single center or city. One prior study of New York City in the 1990s, for example, found that over half of hospitalizations of homeless individuals were for mental illness or substance use disorder and that these hospitalizations were associated with excess costs relative to nonhomeless adults.9 It is unclear, however, whether these patterns have changed in light of significant policy efforts in the United States to improve the health of homeless people. A large-scale, contemporary understanding of acute illness in this vulnerable population is important for policymakers and public health experts, to inform initiatives that aim to improve the health of this population.
In this study, we aimed to fill this gap by examining hospitalizations of homeless people in 3 states representing a diversity of geographies and demographics—Massachusetts, Florida, and California—across a 7-year period (2007–2013). We addressed 3 main research questions: First, how have trends in hospitalizations of homeless people changed over time? Second, how do reasons for hospital admission and clinical comorbidities at time of hospitalization compare between homeless and demographically similar nonhomeless individuals? And finally, how do in-hospital mortality, length of stay, and costs of care differ between homeless and nonhomeless hospitalized patients, after accounting for differences in demographics, admission diagnosis, and clinical comorbidities?
METHODS
Data Source
We used data from the State Inpatient Databases (SIDs) of the Healthcare Cost and Utilization Project, created by the Agency for Healthcare Research and Quality. Each SID includes all inpatient discharges from short-term, acute care, nonfederal, general, and other specialty hospitals in participating states. We used 2007–2013 hospital discharge data from Massachusetts and Florida, and 2007–2011 hospital data from California (data for California in 2012 and 2013 were not available). We selected these 3 states because they are populous, diverse, geographically dispersed, and include information on whether patients are homeless at the time of hospitalization. Discharge records from these databases contain information collected from billing records, including patient demographics, clinical comorbidities, diagnoses, expected payer. Costs for each hospitalization were determined by applying American Hospital Association cost to charge ratios to the total hospital charges provided in the SID, as has been carried out in prior studies.10,11
Patient Population
We identified all hospitalizations of homeless people across the study period using a unique “homeless” variable provided by the SIDs for each state, as has been previously used by the Agency for Healthcare Research and Quality.12,13 We calculated the annual rate of hospitalizations for homeless people for each state, using year-specific state homeless populations obtained from the US Department of Housing and Urban Development as a denominator.14 As an additional analysis, we also examined the annual rate of hospitalizations for homeless people using total state populations for each year as a denominator, as reported by the US Census Bureau.15
Our main analytic cohort was restricted to hospitalizations among homeless and nonhomeless patients 18 years or older of age for whom discharge diagnoses and mortality data were available. We then stratified all homeless hospitalizations and nonhomeless hospitalizations based on data elements available in the SID, including patient characteristics (age, sex, race) and insurance payer, and by state and year of hospitalization. This resulted in 6236 unique strata defined by the demographic elements above, in which each stratum was a unique combination of age (in 5-year age intervals; ie, 25–29, 30–34), sex, race, insurance payer, state, and year. Strata where there were no homeless subjects or nonhomeless subjects were removed. We used the relative size of each stratum for the homeless cohort (eg, proportion of all homeless subjects that fall within each stratum) to reweight each corresponding nonhomeless stratum. The reweighted nonhomeless cohort is referred to as the demographics-standardized nonhomeless cohort as demographics have been standardized relative to the homeless cohort.
Statistical Analyses
Continuous variables were summarized by means and standard deviations; categorical variables were summarized by percentages.
We compared the primary reason for hospitalization between the homeless and demographics-standardized nonhomeless cohort using primary discharge diagnosis clinical classification of diseases (CCS) categories.16 Discharge diagnoses were recoded using the CCS software into broad categories, available as separate variables within the SID data set. For the homeless cohort, rates for each respective cause of hospitalization were estimated by simple proportions. For the demographics-standardized nonhomeless cohort, rates were estimated accounting for weights. We also used CCS-coded diagnoses to estimate comorbidity rates for homeless and demographics-standardized nonhomeless cohorts using the approach described above. Differences in the rates of comorbidities between homeless and demographics-standardized nonhomeless cohorts were tested by paired t tests (eg, homeless and nonhomeless subjects in a stratum were considered a pair).
To compare outcomes, including in-hospital mortality, length of stay, and costs between homeless and nonhomeless populations, we first fit a logistic regression model (for mortality) or linear regression model (for length of stay and cost) to the nonhomeless cohort using demographics (age, sex, race, insurance payer, state of hospitalization, and year of hospitalization), primary discharge diagnosis, and 22 clinical comorbidities as covariates. The estimated models were then applied to the homeless cohort demographics, primary discharge diagnosis and 22 clinical comorbidities to predict outcomes. These predicted outcomes represent the nonhomeless risk-standardized outcomes in that the risk profiles have been standardized relative to the homeless cohort. The differences between homeless observed outcomes and nonhomeless risk-standardized outcomes, as well as associated 95% confidence intervals, were calculated using the t statistic. As a sensitivity analysis, we excluded the state of Massachusetts because 7 comorbidities were not available for this state, and reran our multivariate model adjusted for demographics, primary discharge diagnosis, and all 29 clinical comorbidities.
The Institutional Review Board evaluated this study and deemed it non-human subjects research. Analyses were performed using SAS version 9.4 64-bit (SAS Institute Inc., Cary, NC).
RESULTS
Study Population and Hospitalization Rates
We initially identified 202,439 total hospitalizations for homeless people across the study period. The absolute number of hospitalizations increased over time across all states and is shown in eTable 1 (Supplemental Digital Content 1, http://links.lww.com/MLR/B638) along with homeless populations by year and state. Hospitalization rates of homeless people in Massachusetts increased from 294 per 1000 homeless residents in 2007 to 420 per 1000 homeless residents in 2013 (Fig. 1A). In Florida, there were 161 hospitalizations per 1000 homeless residents in 2007, followed by a steady increase to 240 hospitalizations per 1000 homeless residents by 2013 (Fig. 1B). California also experienced an increase from 133 to 164 hospitalizations per 1000 homeless residents from 2007 to 2011 (Fig. 1C). We observed a similar rise in hospitalization rates over time when we used state total populations rather than state homeless populations as a denominator (eFig. 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B638).
FIGURE 1.
Annual trends in homeless hospitalizations per 1000 homeless residents in Massachusetts (A), Florida (B), and California (C).
Baseline Characteristics
After excluding patients below 18 years of age and hospitalizations with missing discharge diagnosis codes and/or mortality information, our main analytic cohort included 185,292 hospitalizations for homeless individuals and 32,322,569 hospitalizations for nonhomeless individuals. Compared with admissions for the nonhomeless, among those for homeless persons, mean age (46 y of age) and other demographics (62% white; 42% uninsured; 32% insured by Medicaid) were identical following standardization (Table 1).
TABLE 1.
Baseline Characteristics of Homeless Versus Demographics-standardized Nonhomeless Cohorts
| Homeless (N = 185,292) (%) | Demographics-standardized* Nonhomeless (N = 32,322,569) (%) | P | |
|---|---|---|---|
| Age (SD) (y) | 46.1 (12.8) | 46.1 (12.8) | 1.0 |
| Male | 76.1 | 76.1 | 1.0 |
| Female | 23.9 | 23.9 | 1.0 |
| Race | |||
| White | 62.0 | 62.0 | 1.0 |
| Black | 20.0 | 20.0 | 1.0 |
| Hispanic | 15.2 | 15.2 | 1.0 |
| Other | 2.8 | 2.8 | 1.0 |
| Insurance | |||
| Medicare | 20.8 | 20.8 | 1.0 |
| Medicaid | 31.7 | 31.7 | 1.0 |
| Private | 5.6 | 5.6 | 1.0 |
| Uninsured/self-pay | 41.9 | 41.9 | 1.0 |
| Clinical comorbidities | |||
| Alcohol abuse | 31.0 | 14.1 | < 0.001 |
| Drug abuse | 29.4 | 14.0 | < 0.001 |
| Hypertension | 28.9 | 38.1 | < 0.001 |
| Chronic pulmonary disease | 17.4 | 15.0 | < 0.001 |
| Fluid and electrolyte disorders | 16.0 | 18.9 | < 0.001 |
| Anemias | 12.4 | 13.8 | < 0.001 |
| Psychoses | 10.6 | 7.0 | < 0.001 |
| Neurological disorders | 9.7 | 6.9 | < 0.001 |
| Liver disease | 9.6 | 6.0 | < 0.001 |
| Diabetes w/o complications | 9.5 | 14.8 | < 0.001 |
| Depression | 6.5 | 8.0 | < 0.001 |
| Obesity | 5.2 | 10.7 | < 0.001 |
| Coagulation disorder | 5.1 | 4.7 | < 0.001 |
| Weight loss | 3.1 | 3.2 | < 0.001 |
| Renal failure | 2.9 | 7.4 | < 0.001 |
| Hypothyroidism | 2.9 | 4.4 | < 0.001 |
| Congestive heart failure | 2.4 | 4.1 | < 0.001 |
| Diabetes w/o complications | 1.8 | 4.1 | < 0.001 |
| Peripheral vascular disease | 1.5 | 3.0 | < 0.001 |
| AIDS/HIV | 1.3 | 0.9 | < 0.001 |
| Metastatic cancer | 0.3 | 1.3 | < 0.001 |
| Solid tumor w/o metastases | 0.6 | 1.1 | < 0.001 |
Standardized by age, sex, race, insurance payer, state of hospitalization, and year of hospitalization.
AIDS/HIV indicates acquired immunodeficiency syndrome/human immunodeficiency virus.
Clinical Comorbidities and Reasons for Hospital Admission
Homeless patients differed significantly from nonhomeless patients in terms of comorbidities and reasons for admission. Homeless individuals were more likely to have a history of alcohol abuse (31% vs. 14%, P< 0.001), drug abuse (29% vs. 14%, P <0.001), liver disease (10% vs. 6%, P < 0.001), and psychoses (11% vs. 7%, P <0.001) (Table 1).
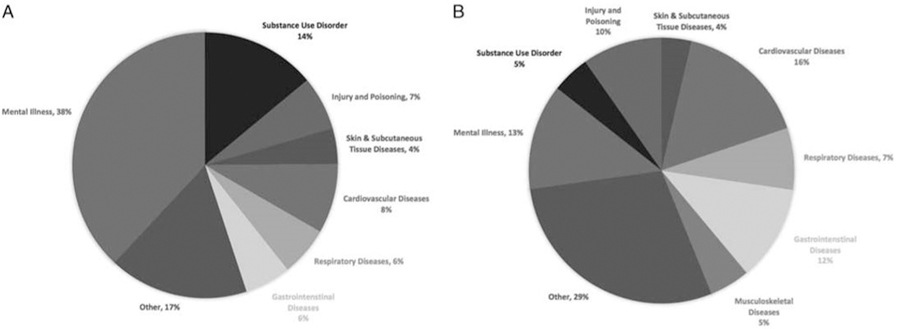
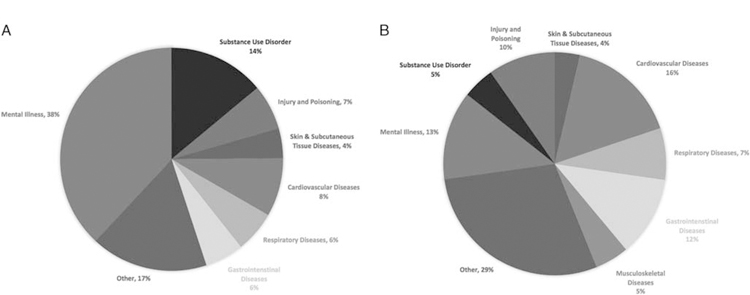
Hospitalizations for homeless individuals, when compared with demographics-standardized nonhomeless persons, were markedly more likely to be for mental illness (38% vs. 13%, P < 0.001) and substance use disorder (14% vs. 5%, P < 0.001), but less likely to be for cardiovascular diseases (8% vs. 16%, P< 0.001), gastrointestinal illness (6% vs. 12%, P <0.001), or injury or poisoning (7% vs. 10%, P < 0.001). Figures 2A and 2B demonstrate other common reasons for hospitalization in the 2 groups.
FIGURE 2.
Most common reasons for hospitalizations from 2007 to 2013. A, Causes of hospitalization in the homeless cohort. B, Causes of hospitalization in the demographics-standardized nonhomeless cohort.
Clinical Outcomes
Overall, in-hospital mortality rates were low among both homeless and risk-standardized nonhomeless adults (0.9% vs. 1.2%, P < 0.001) (Table 2). In-hospital mortality rates for homeless adults varied among states, and were lowest in Massachusetts (0.77%) compared with Florida (0.84%) and California (1.0%) (eTable 2, Supplemental Digital Content 1, http://links.lww.com/MLR/B638). Mean length of stay was higher among homeless compared with risk-standardized nonhomeless individuals (6.5 vs. 5.9 d, P < 0.001). Hospitalizations for the homeless had lower mean costs per day ($1,535 vs. $1,834, P <0.001) and for the entire hospitalization ($10,391 vs. $11,027, P <0.001). In our sensitivity analysis that excluded the state of Massachusetts, patterns of in-hospital outcomes were similar (eTable 3, Supplemental Digital Content 1, http://links.lww.com/MLR/B638).
TABLE 2.
In-hospital Outcomes of Homeless Versus Risk-standardized Nonhomeless Cohorts
| Homeless | Nonhomeless (Risk-standardized*) | Homeless-Nonhomeless (Risk-standardized) |
||
|---|---|---|---|---|
| Difference (95% CI) | P | |||
| Mortality (%) | 0.91 (0.87–0.95) | 1.18 (1.17–1.20) | −0.28 (−0.32 to −0.24) | < 0.0001 |
| Mean length of stay (d) | 6.54 (6.49–6.59) | 5.89 (5.88–5.90) | 0.65 (0.59–0.70) | < 0.0001 |
| Average cost per day | $1535 ($1527–$1543) | $1833 ($1828–$1838) | −$298 (−$307 to −$289) | < 0.0001 |
| Cost per hospitalization | $10,391 ($10,296–$10,486) | $11,027 ($10,992–$11,062) | −$636 (−$737 to −$535) | < 0.0001 |
Standardized by demographics (age, sex, race, insurance payer, state of hospitalization, and year of hospitalization), primary discharge diagnosis, and 22 clinical comorbidities.
DISCUSSION
In this study of homeless people in 3 states, we found that hospitalizations among homeless individuals are rising and that these hospitalizations tend to be for a very different set of conditions than the nonhomeless, even after accounting for differences in demographics. Over one-half of hospitalizations for homeless people during our study period were for mental illness and substance use disorder. Despite greater policy and public health focus over the last few decades, these conditions still remain the primary drivers of acute hospitalizations among homeless adults, similar to patterns observed in analyses of US cities from the 1990s.9,17 In addition, we found that in-hospital mortality rates were low for both homeless and risk-standardized nonhomeless individuals, and although homeless adults experienced longer lengths of stay, their mean costs of care per hospitalization were lower.
The reasons for the increase in hospitalizations among homeless individuals that we observed are unknown, but may have been driven, at least in part, by aging of the homeless population with an associated increase in health needs and potentially, the rise of the opioid epidemic, which disproportionately impacted the homeless population years ahead of the general population.5,18 Notably, homeless hospitalization rates in Massachusetts were over double that of any other state during the study period, an estimate that is similar to one prior claims-based study of homeless individuals covered by Medicaid in Massachusetts.6 This high hospital utilization rate may reflect the fact that Massachusetts was an early expander of Medicaid coverage (in the 1990s and then in 2006) which resulted in an estimated 80% of homeless individuals being insured and enhanced homeless persons’ access to acute care services, as well as the presence of the large and comprehensive Boston Health Care for the Homeless Program (BHCHP).6,19,20 Homeless individuals have complex medical and social needs, and often face barriers to and lack longitudinal, reliable access to health care services.21 Access to such services through insurance likely increases utilization by meeting previously unmet health care needs, and may also explain the lower in-hospital mortality rates that we observed in Massachusetts relative to other states.
We found that across all states, over one-half of acute hospitalizations for homeless individuals were for mental illness and substance use disorder, in contrast to just 18% of hospitalizations for nonhomeless individuals. Persons with behavioral health disorders, whether homeless or not, have a greater burden of medical comorbidities, receive worse care quality, and are less likely to be adherent to treatment.6,22–24 Furthermore, mortality among individuals with mental illness is 2-fold to 4-fold higher than the general population.25,26 Access to and coordination of behavioral health services, especially for homeless individuals, may be fragmented and inefficient. These challenges likely explain the strikingly high observed rate of acute hospital use, among the homeless cohort, for mental illness and substance use disorder. The ACA, which expanded mental health and substance use disorder services, and required them to be covered at parity with medical and surgical benefits may help facilitate access to these outpatient services for homeless persons, and diminish the need for acute hospital use. In addition, the ACA also provided incentives to implement Patient-Centered Medical Homes, which emphasize the delivery of collaborative, patient-centered, comprehensive care and support the integration of mental health and primary care, the latter of which has been shown to improve mental health outcomes.27–29 The emergence of integrated health care delivery models may also help address some of these challenges, and could have lessons for how the health care system might approach improving outcomes for chronically underserved populations such as the homeless. Future investigations should examine whether these emerging health delivery models improve the provision of behavioral health services to the homeless.
Of course, despite heightened recognition of the need for better outpatient behavioral health services for vulnerable populations, competing unmet needs or barriers—such as lack of insurance—may impede homeless persons’ access to reliable, longitudinal health care. Nearly half of all hospitalized homeless individuals in our study were uninsured at the time of admission. Insurance mediates access to a wide range of outpatient health services, such as ambulatory care visits, preventative care, and mental health services, all of which may be beneficial to homeless individuals who often have multiple coexisting medical and behavioral conditions. Early evidence suggests that the expansion of Medicaid eligibility under the ACA, which began in 2014, has led to significant increases in coverage, improved access to care, and broader benefits for homeless individuals, and providers who treat these populations report having access to more treatment options as a result of Medicaid coverage.30 Furthe evaluation of the impact of Medicaid expansion on the homeless will provide important insight with regard to whether insurance should be one part of a multifaceted strategy to reduce acute care use and improve the health of this population.21
We also found that homeless persons had longer lengths of stay compared with a nonhomeless cohort, although per hospitalization (and daily) expenditures were lower. One potential explanation for these spending patterns is that homeless persons receive less intensive care during a hospitalization, because behavioral health disorders and social circumstances preclude complete diagnostic workups and/or therapeutic interventions, or because care teams’ implicit biases lead to differences in care delivered.31,32 The longer lengths of stay we observed among nonhomeless patients are consistent with prior studies,33 and could be due to unmeasured illness severity, but more likely reflects a reticence to discharge homeless persons without an established destination (eg, a shelter).
Finally, in-hospital mortality rates were low among homeless and nonhomeless patients, even after accounting for differences in demographics, comorbidity profiles, and admission diagnosis. More globally, however, homeless individuals are known to have premature mortality and high mortality rates.34 For example, a recent analysis of the homeless population in Boston showed that the mean age of death was 51 years, and that homeless mortality rates had not improved compared with the early 1990s, predominately due to a rise in drug overdose deaths.5,35 These findings add a contemporary, national perspective to a growing body of literature with regard to health outcomes among this vulnerable population.
This study has several limitations. We focused on homeless hospitalizations in just 3 states, and so our findings may not be generalizable more broadly. Our identification of homeless individuals relied on data from the SIDs, and between-state or between-provider differences in identifying homelessness could impact our estimates. However, to our knowledge, this is the largest study to date of homeless hospitalizations, and includes 3 states that differ in demography and health care markets. We were also unable to delineate whether hospitalized patients were chronically, transiently, or formerly homeless. In addition, we did not have information with regard to Veteran status, which might influence access to health care services. To calculate homeless hospitalization rates per 1000 homeless residents, we used annual homeless populations provided by the US Department of Housing and Urban Development for each state, for which definitions of homelessness may have varied. However, we observed similar patterns in hospitalization rates over time when we used total state populations, rather than annual homeless populations, as a denominator.
Public Health Implications
In summary, our findings provide a large-scale, contemporary evaluation of patterns of homeless hospitalizations in 3 states across a several-year period. The rate of homeless hospitalizations has increased since 2007, and mental illness and substance use disorder account for over one-half of hospital admissions among homeless persons, differing starkly from demographics-standardized nonhomeless hospitalized patients. In addition, although hospital lengths of stay were longer for homeless persons, total and daily expenditures were lower than nonhomeless persons, which may reflect differences in intensity of care, and requires further study.
Despite greater policy and public health focus over the last few decades, mental illness and substance use disorder still remain the primary drivers of acute hospitalizations among homeless adults. These data reinforce that there is an urgent need to reduce financial and nonfinancial barriers to the use of ambulatory care, for behavioral health services in particular, to improve long-term management of physical and mental illness for homeless individuals. As policy initiatives under the ACA continue to evolve, such as higher funding for community health centers, expansion of Medicaid eligibility, and the implementation of integrated health care delivery models, future investigations should seek to understand their impact on the health of this highly vulnerable population.
Supplementary Material
Acknowledgments
R.K.W. is supported by National Institutes of Health Training Grant T32HL007604–32, Brigham and Women’s Hospital, Division of Cardiovascular Medicine. K.E.J.M. receives research support from the National Heart, Lung, and Blood Institute (K23HL109177–03). R.W.Y. receives research support from the National Heart, Lung and Blood Institute (R01HL136708) and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology.
Footnotes
R.K.W. previously served as a consultant for Sanofi and Regeneron. K.E.J.M. does contract work for the US Department of Health and Human Services, where she continues former employee of the US Department work on a limited basis as a contractor. The remaining authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.The US Department of Housing and Urban Development. The 2017 Annual Homeless Assessment Report (AHAR) to Congress, The US Department of Housing and Urban Development; 2017.
- 2.Koh HK, O’Connell JJ. Improving health care for homeless people. JAMA. 2016;316:2586–2587. [DOI] [PubMed] [Google Scholar]
- 3.Gelberg L, Gallagher TC, Andersen RM, et al. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87:217–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mental Health in America-Access to Care Data. Mental Health America. Available at: http://www.mentalhealthamerica.net/issues/mental-health-america-access-care-data. Accessed February 17, 2018.
- 5.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173:189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin WC, Bharel M, Zhang J, et al. Frequent emergency department visits and hospitalizations among homeless people with medicaid: implications for medicaid expansion. Am J Public Health. 2015;105(suppl 5): S716–S722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Housing First. National Alliance to End Homelessness. 2016. Available at: https://endhomelessness.org/resource/housing-first/. Accessed February 3, 2018.
- 8.Katz MH. Homelessness-challenges and progress. JAMA. 2017;318: 2293–2294. [DOI] [PubMed] [Google Scholar]
- 9.Salit SA, Kuhn EM, Hartz AJ, et al. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338:1734–1740. [DOI] [PubMed] [Google Scholar]
- 10.Levit KR, Friedman B, Wong HS. Estimating inpatient hospital prices from state administrative data and hospital financial reports. Health Serv Res. 2013;48:1779–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabbatini AK, Kocher KE, Basu A, et al. In-hospital outcomes and costs among patients hospitalized during a return visit to the emergency department. JAMA. 2016;315:663–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun R, Karaca Z, Wong HS. Characteristics of homeless individuals using emergency department services in 2014 In: Statistical Brief #229: Healthcare Cost and Utilization Project; 2017. [PubMed] [Google Scholar]
- 13.Karaca Z, Wong HS, Mutter RL. Characteristics of homeless and nonhomeless individuals using inpatient and emergency department services, 2008 In: Statistical Brief #152: Healthcare Cost and Utilization Project; 2013. [PubMed] [Google Scholar]
- 14.US Department of Housing and Urban DevelopmentUdoHau. CoC homeless populations and subpopulations reports Development. US Department of Housing and Urban Development; 2018. [Google Scholar]
- 15.Population and Housing Unit Estimates. United States Census Bureau. 2018. Available at: https://www.census.gov/programs-surveys/popest.html. Accessed May 15, 2018.
- 16.Clinical Classifications Software (CCS) for ICD-9-CM Fact Sheet. Healthcare Cost and Utilization Project. 2018. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp. Accessed January 4, 2018.
- 17.Martell JV, Seitz RS, Harada JK, et al. Hospitalization in an urban homeless population: the Honolulu Urban Homeless Project. Ann Intern Med. 1992;116:299–303. [DOI] [PubMed] [Google Scholar]
- 18.Hahn JA, Kushel MB, Bangsberg DR, et al. Brief report: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006;21:775–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connell JJ, Oppenheimer SC, Judge CM, et al. The Boston Health Care for the Homeless Program: a public health framework. Am J Public Health. 2010;100:1400–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bharel M, Lin WC, Zhang J, et al. Health care utilization patterns of homeless individuals in Boston: preparing for Medicaid expansion under the Affordable Care Act. Am J Public Health. 2013;103(suppl 2):S311–S317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. [DOI] [PubMed] [Google Scholar]
- 22.Lin WC, Zhang J, Leung GY, et al. Chronic physical conditions in older adults with mental illness and/or substance use disorders. J Am Geriatr Soc. 2011;59:1913–1921. [DOI] [PubMed] [Google Scholar]
- 23.Gilmer TP, Dolder CR, Lacro JP, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161:692–699. [DOI] [PubMed] [Google Scholar]
- 24.Druss BG, Rosenheck RA, Desai MM, et al. Quality of preventive medical care for patients with mental disorders. Med Care. 2002;40:129–136. [DOI] [PubMed] [Google Scholar]
- 25.Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72: 1172–1181. [DOI] [PubMed] [Google Scholar]
- 26.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Croghan T, Brown J, eds. Quality AfHRa. Integrating mental health treatment into the patient centered medical home Agency for Healthcare Research and Quality. 2010. Available at: https://www.pcmh.ahrq.gov/page/integrating-mental-health-treatment-patient-centered-medical-home. Accessed January 18, 2018. [Google Scholar]
- 28.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. [DOI] [PubMed] [Google Scholar]
- 29.Bruce ML, Ten Have TR, Reynolds CF III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. [DOI] [PubMed] [Google Scholar]
- 30.DiPietro B, Artiga S, Gates A. Early Impacts of the Medicaid Expansion for the Homeless Population. The Kaiser Family Foundation. 2014. Available at: https://www.kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/. Accessed February 2, 2018.
- 31.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46: 678–685. [DOI] [PubMed] [Google Scholar]
- 32.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102: 979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hwang SW, Weaver J, Aubry T, et al. Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Med Care. 2011;49:350–354. [DOI] [PubMed] [Google Scholar]
- 34.Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol. 2009; 38:877–883. [DOI] [PubMed] [Google Scholar]
- 35.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331:304–309. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.