Abstract
Annually, 10% of cirrhotic patients with ascites develop refractory ascites for which large-volume paracentesis (LVP) is a frequently used therapeutic procedure. LVP, although a safe method, is associated with circulatory dysfunction in a significant percentage of patients, which is termed paracentesis-induced circulatory dysfunction (PICD). PICD results in faster reaccumulation of ascites, hyponatremia, renal impairment, and shorter survival. PICD is diagnosed through laboratory results, with increases of >50% of baseline plasma renin activity to a value ≥4 ng/mL/h on the fifth to sixth day after paracentesis. In this review, we discuss the pathophysiology and prevention of PICD.
Keywords: Refractory ascites, Plasma renin activity, Large-volume paracentesis, Cirrhosis, Portal hypertension
Introduction
Ascites is a major complication of liver cirrhosis, with an annual incidence of 5–10% in compensated cirrhosis.1 Dietary sodium restriction and oral diuretics are the first treatment choices for uncomplicated ascites.2,3 Annually, 10% of cirrhotic patients with ascites develop refractory ascites, which is associated with a poor prognosis that reduces transplant-free survival to 50% per year.4 In refractory ascites, transjugular intrahepatic portosystemic shunt (TIPS), increased doses of diuretics, or large-volume paracentesis (LVP) are the few effective measures apart from liver transplant in routine practice. Of these, LVP is the preferred treatment of choice as it is faster, more effective, and associated with fewer side effects.5 TIPS,4 although effective in a selected group of patients, may be associated with ascites recurrence and hepatic encephalopathy. In addition, its high cost and lack of availability at some places make it a less desirable option. Therapeutic paracentesis in patients with cirrhosis and tense ascites leads to circulatory dysfunction, which is termed paracentesis-induced circulatory dysfunction or post paracentesis circulatory dysfunction.6,7 PICD usually occurs following LVP (>5–6 L) and results in faster reaccumulation of ascites, hyponatremia, renal impairment, and shorter survival.7
Epidemiology
The incidence of PICD is estimated to be 80% among patients not receiving any plasma volume expander, 33% to 38% in patients receiving polygeline/saline solution/dextran 70, and 11% to 20% among patients receiving albumin.8,9
The definition of PICD
Gines et al.8 first defined PICD as an increase in plasma renin activity (PRA) on the sixth day after paracentesis of more than 50% of the pretreatment value to a level > 4 ng/ml/h. The value of 4 ng/mL/h was determined based on 36 healthy volunteers who were on a 50 mmol/day sodium diet for 7 days. The mean value in healthy volunteers was 1.35 ± 0.94 ng/mL/h (range, 0.1–4.0). Whether this value of 4 ng/mL/h holds for patients with cirrhosis and refractory ascites who have a hyperactive renin-angiotensin-aldosterone system is still unclear. In the same study, 280 cirrhotic patients with ascites had documented PRA value at baseline. The baseline value in those who developed PICD (n = 85) was 8.0 ± 7.3 ng/ml/h, which was similar to those who did not (n = 195), i.e., 9.3 ± 11.5 ng/ml/h. The landmark study by Wilkinson et al.10 showed that cirrhosis with refractory ascites would invariably have high PRA due to reduced renal blood flow with the highest value being 21.77 nmol/L/h and mean value of 9.5 nmol/L/h, while those with ascites would have a value double that of the healthy controls (3.99 nmol/L/h and 1.82 nmol/L/h, respectively). This indicates that the PRA needs to rise by >50% on day 6 in patients with cirrhosis and refractory ascites to be called PICD. The diagnosis of PICD is primarily based on the laboratory value of PRA and can be diagnosed only after 5 to 6 days of paracentesis. Although it is a valid objective measure, the difficulties of measuring PRA due to the technical requirements (blood sample should be taken after overnight fasting and at least 1 h of bed rest), cost, and questionable benefit in patients with refractory ascites who undergo repeated paracentesis, makes it a less favored option for clinicians. The PRA is dependent on age11,12 (PRA and plasma aldosterone levels are highest in newborns and lowest in the elderly population), gender (more in men),12 race (more in whites),12 sodium intake (increased sodium intake suppresses renin activity),13 diurnal variation (sleep inhibits renin activity),14 posture (upright posture for 120 m increases renin activity),15 drugs such as diuretics (chronic treatment with diuretics increases the PRA),16,17 and beta-blockers (beta-blockers profoundly suppress renin activity).17 Measuring aldosterone concentration has no significant role in diagnosing PICD.
Pathophysiology of PICD
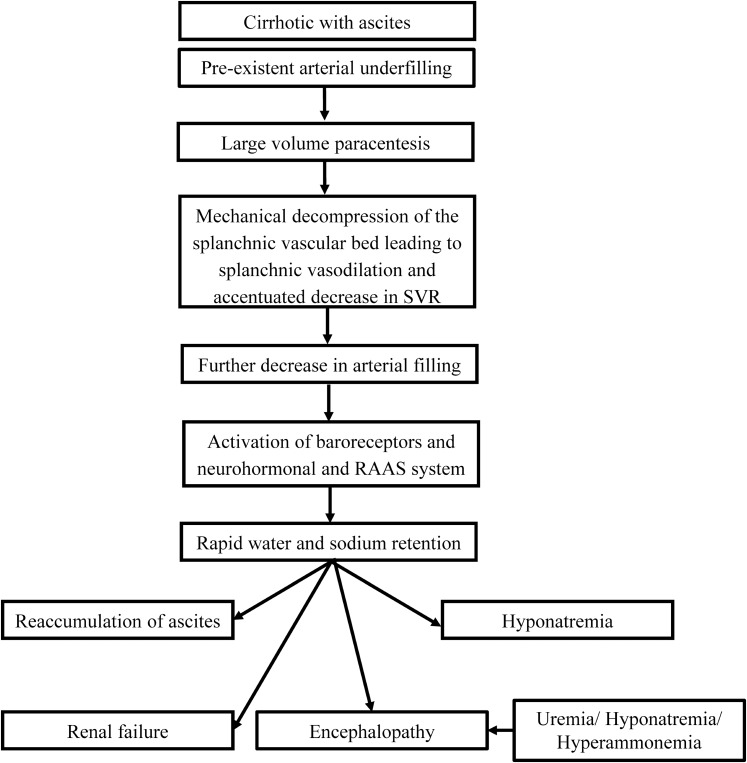
LVP causes mechanical decompression of the splanchnic vascular bed leading to splanchnic vasodilation, a further decrease in the arterial filling, and activation of neurohormonal systems. This results in free water and sodium retention. As a consequence, patients develop rapid reaccumulation of ascites, hyponatremia, renal injury, and encephalopathy (Fig. 1). Maintaining the intraabdominal pressure by pneumatic girdle prevents the circulatory disturbance occurring after paracentesis.18 This was the argument of peritoneovenous shunt proponents that ascites will have unidirectional flow from the abdomen into the systemic circulation leading to the expansion of effective arterial blood volume, increase in cardiac output, renal blood flow, right atrial pressure, and atrial natriuretic peptide concentration and decrease in renin and aldosterone concentrations.19,20 This procedure has not been widely accepted due to several complications, including sepsis, coagulopathies, and pulmonary edema, and is currently extinct.21
Fig. 1. Mechanism of PICD and complications.
The degree of activation of the renin-angiotensin-aldosterone system and sympathetic nervous system 6 days after paracentesis correlates inversely with changes in systemic vascular resistance (SVR).22 Within 60 m of paracentesis (<5 L), a significant increase in cardiac output, together with a reduction in mean arterial pressure (MAP), and consequently, calculated SVR experiences a significant decrease.23 The flow rate of ascites has no relationship to the development of PICD.24 There is increased cardiac output and PRA and decreased central venous and wedge pressure 24 h after LVP.25 Whether edematous or not, all patients undergoing LVP have reduced creatinine clearance from 77 to 60 mL/m after 48 h.16
Prevention of PICD
Albumin8,26–28 Albumin is an essential plasma protein produced by hepatocytes. It accounts for 75% of the plasma colloid oncotic pressure and has a half-life of 15–21 days. With a molecular weight of 67 kDa and 607 amino acids, albumin is an asset for physicians. The free cysteine (Cys-34) residue accounts for the single free redox-active thiol (-SH) moiety, which accounts for ∼80% of extracellular antioxidant properties through nitrosylation, oxidation, and thiolation. Patients with ascites usually have hypoalbuminemia. The causes of hypoalbuminemia are i) reduced hepatic synthesis and secretion, ii) dilution by increased intravascular and interstitial volume, and iii) loss in the ascitic fluid. The combination of hypoalbuminemia and impaired albumin function leads to marked disturbance in the transport, metabolism, and excretion of many endogenous and exogenous substances. Infusion of exogenous albumin in ascites patients may serve the dual purpose of replenishing the levels of circulating albumin and the functional activity of the albumin pool. These are effects specific to albumin not shared by other plasma volume expanders and may contribute to superior effectiveness. Albumin is available in preparations of 5%, 20%, and 25% solutions, with a sodium content equivalent to that of serum. The studies on PICD have involved only 20% albumin in either 8 g/L of ascitic fluid tapped or 4 g/L of ascitic fluid removed.
The first study was conducted by Pere Gines,29 who evaluated 105 patients with daily paracentesis of 4–6 L until the disappearance of ascites. Fifty-two patients received albumin (40 g with each tap), and the other group received no volume expander. The number of complications (acute kidney injury [AKI] and hyponatremia) was significantly higher in patients who had no albumin infusion. However, the authors reported no mortality benefit with albumin infusion. This landmark study paved the path for further studies on albumin.
In 1996, Gines et al. compared albumin with dextran 70 and polygeline for the prevention of PICD.8 A total of 289 patients undergoing paracentesis were enrolled, and it was reported that albumin decreased the incidence of PICD to 18.5% compared to 34.4% in the dextran 70 group and 37.8% in the polygeline group. The mean PRA was 9.2 ± 10.3 ng/ml/h in the albumin arm, 9.5 ± 11.7 in dextran 70, and 8.6 ± 9.8 in the polygeline group, indicating that the upper limit (i.e., two standard deviations) was about 30 ng/ml/h in some patients. PICD was associated with a shorter time to readmission and shorter survival. This was the first randomized study to demonstrate the superiority of albumin.
A randomized study comparing saline versus albumin in 2003 also showed significant benefits with albumin.30 Seventy-two patients were enrolled (35 in the saline group and 37 in the albumin group). The baseline heart rate and MAP in the saline group were 83.1 ± 8.6/m and 81.5 ± 12.2 mmHg and 82.4 ± 10.6/m and 83.1 ± 11.7 mmHg in the albumin group, respectively. The serum albumin was also comparable with 2.67 ± 0.48 g/dL in the saline group and 2.56 ± 0.65 g/dL in the albumin group. The baseline PRA value in the saline group was 5.4 ± 5.4, and in the albumin group was 5.2 ± 4.5 ng/mL/h. The volume of ascites removed was comparable in both groups (>6 L) over a mean duration of ∼90 min. The amount of albumin given was 260 ± 115.1 mL (20% albumin at 8 g/L ascites), and saline was 1075 ± 365 mL (170 mL of 3.5% saline solution per L ascites removed at 999 mL/h). There were 10 patients with complications in the saline group compared to only 6 in the albumin group. The incidence of PICD (based on PRA rise) was 33.3% in the saline group and only 11.4% in the albumin group (p = 0.03). When <6 L was tapped, the incidence of PICD was similar in both groups (6.7% in saline vs. 5.6% in the albumin group; p = 0.9). MAP, hemoglobin, and potassium levels at baseline were predictors of PICD. The type of plasma expander was found to have a significant preventive effect on PICD by both univariate and multivariate analysis. Albumin was a better alternative when >6 L was tapped.
A pilot study by Richard Moreau et al.,31 conducted in 2000 (published in 2006) comparing synthetic colloid (3.5% polygeline) with albumin, concluded that albumin was more effective in preventing liver-related complications. The study was prematurely discontinued because of safety concerns about bovine-derived products. A total of 68 patients were enrolled: 30 in the albumin group and 38 in the polygeline group. One unit of the study colloid (blinded) provided either 20 g albumin or 17.5 g polygeline. The amount transfused was fixed as 1 U if below 4 L, 2U if between 4 L and below 6 L, 3U if between 6 L and below 8 L, and 4 U if 8 L or more. The patients were followed up for 6 months, and the number of taps and complications due to liver disease was assessed. The polygeline group had a 1.6-fold higher risk of developing liver-related complications than the albumin group.
An open-label randomized study comparing half the dose of albumin (4 g/L of ascites tapped) with the conventional dose (8 g/L ascites) concluded that half the dose was effective and economical for preventing the complications (PICD) of LVP.32
Terlipressin33 Terlipressin (N-α-triglycyl-8-L-lysine-vasopressin) (formula: C52H74N16O15S2) is a vasopressin 1 (V1) receptor agonist with a molecular weight of 1227.4. It is a cyclic dodecapeptide that exists as a white freeze-dried fluffy powder, with a distribution half-life of ∼8 m. Terlipressin plasma concentrations decline exponentially following intravenous IV administration, with an elimination half-life of approximately 1 h and plasma clearance of approximately 9 ml/kg/min. Terlipressin, a prodrug, is cleaved by endopeptidases, resulting in slow release of lysine vasopressin, the active metabolite. Measurable concentrations of vasopressin appear in the plasma from about 20–30 m post-dose, peaking at 1–2 h post-dose. Although terlipressin is used in PICD, its short half-life requires it to be given for prolonged periods to achieve a sustained MAP rise. Terlipressin increases systemic vascular resistance, reduces the portal pressure, and has been used for variceal bleed,34 hepatorenal syndrome (HRS),35 septic shock,36,37 and prevention of PICD.38
A pilot study comparing the efficacy of terlipressin versus albumin showed that terlipressin is as effective as albumin in maintaining the arterial volume post paracentesis.38 The authors randomly allotted 11 patients to terlipressin and 13 to the albumin arm. A total of 3 mg terlipressin was given, 1 mg at the onset of paracentesis, and then 1 mg at 8 h and 16 h. Albumin was given at a dose of 8 g/L ascites removed. Fifty percent within 2 h and 50% after 6 h of paracentesis. After completion, only 10 in each arm were included for analysis. The volume of ascites removed was similar in both groups. They measured the plasma renin concentrations (not the PRA). The number of patients (three in each arm) who had decreased arterial blood volume (based on >50% decrease in plasma renin concentrations on day 6) did not differ between the two groups. Only one patient in each group developed hyponatremia. There were no adverse events noted in either group. The authors concluded that terlipressin is as efficacious in maintaining the arterial blood volume post paracentesis by splanchnic vasoconstriction.
Another pilot study of 40 patients comparing terlipressin with albumin showed that terlipressin is as efficacious as albumin in the prevention of PICD.39 The baseline PRA was similar in both the treatment group with 19.15 ± 12.17 ng/mL/h in the albumin group vs. 20.11 ± 10.60 ng/mL/h in the terlipressin group. There were no side effects reported in the study; neither there was any difference in the occurrence of PICD. There was an insignificant decline in sodium levels 6 days after paracentesis, which was also similar in both groups. The authors concluded that terlipressin is equivalent to albumin.
Midodrine40 Midodrine is an α1-agonist whose active metabolite is desglymidodrine. It acts on the alpha-adrenergic receptors of the arteriolar and venous vasculature, producing an increase in vascular tone and elevation of blood pressure. It is rapidly absorbed orally. The bioavailability of midodrine is similar, whether given intravenously or orally. Plasma levels of the prodrug peak after about 0.5 h and decline with a half-life of approximately 25 m. Blood concentrations of desglymidodrine peak at 1 to 2 h after a dose of midodrine and has a half-life of about 3 to 4 h. The absolute oral bioavailability is 93% and is unaffected by food. Neither midodrine nor desglymidodrine is bound significantly to plasma proteins, and 80% of the drug is eliminated via the renal route by active secretion. An increase in PRA after short-term noradrenaline infusion (also an alpha-adrenergic agonist) has been demonstrated in patients with hepatorenal syndrome, suggesting a vasoconstrictive effect on the renal artery.41 It is unknown whether midodrine also exerts similar effects. Midodrine has been used for refractory ascites,42 HRS,35 and prevention of PICD.43
Two small pilot studies done on midodrine had conflicting results. One pilot study with 40 patients concluded that midodrine is as effective as albumin.43 Midodrine was administered at a dose of 5–10 mg (mean 8.62 ± 1.51mg) three times per day to maintain a MAP at 10mmhg higher than baseline. Albumin was given at a dose of 8 g/L ascitic fluid removed (mean 48.4 ± 12.1 g). PRA at baseline and 6 days post paracentesis did not differ among the two groups. Alcohol was the most common etiology of liver disease in both groups. Other causes of liver disease were hepatitis B virus, hepatitis C virus, autoimmune, and idiopathic. Most interestingly, even with such a high Child’s score (∼10), patients had preserved serum albumin levels of 3.2 ± 0.54 g/dL in the albumin group and 3.17 ± 0.49 g/dL in the midodrine group. Two patients had an increase in PRA by >50% from baseline in the albumin group, but none in the midodrine group had significant PRA elevation. None developed AKI or hyponatremia, although there was a significant decrease in serum sodium levels on day 6 in both groups. A significant increase in 24-h urine volume and urine sodium excretion was observed in the midodrine group. One patient in the albumin group developed a febrile reaction, and one patient in the midodrine group developed headaches and pruritis. Only three patients (two in the albumin group and one in the midodrine group) required repeat paracentesis within 3 months of the treatment. This was a randomized trial with a follow-up of 3 months and also reported adverse events.
A pilot study by Appenrodt et al.44 evaluating the role of midodrine in prevention PICD after LVP42 concluded that midodrine in a fixed short-term dose is ineffective compared to albumin. A total of 24 patients with 13 in the albumin arm and 11 in the midodrine arm were included. Midodrine was given at a dose of 12.5 mg three times a day for 2 days post paracentesis and albumin at a dose of 8 g per L ascites removed. The causes of liver cirrhosis in the study were alcohol, hepatitis (the cause of hepatitis was not mentioned in the article), and idiopathic. The median volume of ascites removed was 6.3 L. A total of 4 patients (2 in each arm) recruited were in Child’s class B, and 20 were Child C cirrhotic (11 in the albumin and 9 in the midodrine groups). PICD developed in six patients in the midodrine group (60%) and four patients (31%) in the albumin group. None of the patients in the albumin group developed AKI compared to two in the midodrine arm. Hyponatremia was noted in seven patients in the albumin group compared to four in the midodrine group. Plasma renin concentration increased from 677.5 to 1337.5 µU/mL in the midodrine arm, whereas in the albumin arm, it increased from 385 to 402 µU/mL on day 6. There were no side effects, even with 37.5 mg midodrine/day.
Noradrenaline45 Noradrenaline is the principal neurotransmitter of the sympathetic nervous system produced by the adrenal medulla. Noradrenaline is preferred over adrenaline in shock as it causes global vasoconstriction, while adrenaline leads to venoconstriction and promotes venous return to the heart. Noradrenaline is a potent alpha agonist. Although noradrenaline is an economical choice, its benefits in the prevention of PICD are not well known. As the duration of action is only 1–2 m, it needs to be given by slow infusion. Noradrenaline infusion can cause severe peripheral and visceral vasoconstriction leading to a decrease in renal blood flow by 20% and cerebral blood flow by 10% without affecting the skeletal muscle and liver blood flow.46 Post paracentesis, cirrhotics develop hypovolemia, and the systemic effects can be worsened by noradrenaline infusion. Moreover, cirrhotics with ascites have higher levels of norepinephrine, but the receptors are desensitized; hence, norepinephrine infusion is less effective in cirrhotics.47 Norepinephrine has been used in shock,37 HRS,48 and PICD.49
A small pilot study comparing noradrenaline with albumin reported that noradrenaline is an economical and efficacious choice over albumin.49 Noradrenaline was started in a continuous infusion at an initial dose of 0.5 mg/h with a maximum dose given up to 3 mg/h. The infusion rate was titrated in steps of 0.125 mg/h to maintain the MAP at 10 mmHg above the baseline. The MAP was maintained at that level for the next 72 h with close monitoring. Effective arterial blood volume, as indicated by PRA before and 6 days after paracentesis, did not differ in the two groups (mean ∼20 ng/mL/h). All patients underwent LVP. Two patients in the noradrenaline group and one in the albumin group had a rise in PRA by >50% on the sixth day. None of the patients developed renal impairment or hyponatremia. Only one patient receiving noradrenaline complained of restlessness. Further, one patient in each arm developed spontaneous bacterial peritonitis (SBP) on follow-up.
Contraindications to LVP: LVP leads to an accentuation of the arteriolar vasodilation, which is already present in cirrhotic patients with ascites. Therefore, LVP should be deferred in patients with spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, and variceal bleed.
Combination therapies
A large trial of 150 patients (presented as an abstract at a major conference) on combination therapy of vasoconstrictor and albumin showed a significant decrease in the number of complications in patients receiving midodrine with albumin.50 The benefit was lacking when terlipressin was used with albumin. However, terlipressin was given for only 1 day, whereas midodrine was given for 3 days. Complications such as pain abdomen, headache, and bradycardia were common in the terlipressin arm and whereas patients receiving midodrine experienced urinary retention, headache, hypertension, and anxiety. The combination therapy should be further explored for the prevention and treatment of PICD.
Meta-analysis
A meta-analysis by Bernardi et al. in 2012, which compared albumin with other therapies such as colloids or vasoconstrictors, showed that albumin remains the best choice for patients undergoing LVP.9 Seventeen randomized controlled trials, reported from 1988 to 2010 with a total of 1,225 patients, met all selection criteria and were included (Table 1). The mean age of the study population ranged from 46.9 to 61.4 years. Seventy-four percent were males (range, 60.0-90.0%) with mean baseline serum albumin ranging from 26 to 29 g/L, and the mean Child-Pugh score ranged from 8.8 to 11.0. The mean volume of ascitic fluid removed ranged from 5.5 to 15.9 L. The dose of albumin varied from 5–10 g/L of fluid tapped. The vasoconstrictors were terlipressin, midodrine, and noradrenaline. Compared to no treatment, albumin reduced the odds of PICD by 93%, 61% when compared to another volume expander, and 30% when compared to a vasoconstrictor. Compared to untreated control patients in whom 16.5% developed hyponatremia, only ∼4% developed hyponatremia in the albumin group. In total, albumin reduced the odds of developing PICD by 66%, hyponatremia by 42%, and death by 36%.
Table 1. Meta-analysis on the role of albumin in patients undergoing paracentesis.
| Author | No. of trials included | Characteristics of trials included | Conclusions |
| Bernardi et al.9, 2012 | 17 (n = 225 participants) | Nine trials comparing albumin with other volume expanders formed the leading category, i.e. 74% (903 of 1,225) of all patients in the meta-analysis, compared with 13% each for trials with no treatment or vasoconstrictor as the control regimen. | Albumin remains superior to other treatment modalities, and further added that the combination of vasoconstrictor with albumin would further decrease the incidence of PICD, which has not been investigated to date. |
| Kwok et al.51, 2013 | 16 (n = 1518 participants) | Four studies with no active comparator, and eight studies comparing plasma expander to albumin, and four other studies of cirrhotic patients with infection compared the use of antibiotics with and without albumin | Albumin use significantly reduced risk of paracentesis-induced circulatory dysfunction, but there was a nonsignificant difference in complications and mortality. |
| Simonetti et al.52, 2019 | 27 (n = 1592 participants) | Five of the trials assessed plasma expanders (albumin in four trials and ascitic fluid in one trial) versus no plasma expander. The remaining 22 trials assessed one type of plasma expander, i.e. dextran, hydroxyethyl starch, polygeline, intravenous infusion of ascitic fluid, crystalloids, or mannitol versus another type of plasma expander, i.e. albumin in 20 of these trials and polygeline in one trial. | There was neither any benefit nor any adverse effect in using any plasma expanders including albumin, polygeline, dextrans, hydroxyethyl starch, intravenous infusion of ascitic fluid, and crystalloids in patients undergoing paracentesis. |
Another meta-analysis51 that included 16 trials on albumin concluded that albumin use significantly reduced the risk of paracentesis-induced circulatory dysfunction, but there was a nonsignificant difference in complications and mortality. The authors also noted that there was a significant reduction in mortality and renal impairment when albumin was used in cirrhosis with infection.
A recent Cochrane review,52 which included 27 randomized trials, concluded that there was neither any benefit nor any adverse effect in using any plasma expander, including albumin, polygeline, dextrans, hydroxyethyl starch, intravenous infusion of ascitic fluid, and crystalloids in patients undergoing paracentesis. The data on albumin/volume expanders originated from a few, small, short-term trials that were at high risk of systemic errors, selection bias, and random errors. They also suggested that more extensive trials with adherence to CONSORT and SPIRIT guidelines are required to assess the role of plasma expanders, including albumin, in paracentesis. The review did not consider trials comparing vasoconstrictors with volume expanders. The advantages and disadvantages of the drugs that have been used for PICD prevention are shown in Table 2.
Table 2. Drugs used in the prevention of PICD.
| Drug | Advantages | Disadvantages |
| Albumin | Evidence from a higher number of trials | Cost Need for IV infusion |
| Terlipressin | Efficacy similar to albumin | Evidence from small pilot studies |
| Noradrenaline | Efficacy similar to albumin Economical | Adverse events are common Need for IV infusion/admission |
| Midodrine | Good oral bioavailability Maintains MAP effectively Can be given in daycare/outpatient |
Small pilot studies Less studied Efficacy still controversial |
Abbreviations: IV, intravenous; MAP, mean arterial pressure.
Differential diagnosis
The complications of PICD are usually attributed to cirrhosis of the liver and are thought to be a complication of the disease (cirrhosis). The usual differentials, which are considered in practice while missing the history of LVP, are shown in Table 3.
Table 3. Differential diagnosis of PICD complication.
| Complication of PICD | Common differentials in practice |
| Hyponatremia | Diuretic induced/dilutional |
| Encephalopathy | Type B/C encephalopathy Dyselectrolytemia Uremia |
| Acute kidney injury | Diuretic-induced |
Treatment of PICD
Volume expansion with albumin infusion is the mainstay of treatment. The use of vasoconstrictors can also help in treatment but needs to be evaluated. However, avoiding paracentesis and withholding diuretics/beta-blockers during PICD prevents the worsening of hemodynamics and encephalopathy.
Conclusions
PICD is a dreaded complication of paracentesis and is associated with a high incidence of morbidity and mortality. It is often overlooked and is a commonly missed diagnosis. The differentials in any patient presenting with worsening of complications of cirrhosis should include PICD. The diagnosis is clinical, and the measurement of PRA may or may not aid in diagnosis. PICD should be redefined as any complication (kidney injury, hyponatremia, encephalopathy, variceal bleed) developing after paracentesis with or without a concurrent rise in PRA.
Way forward
More extensive randomized trials involving a larger sample size on the prevention of PICD with vasoconstrictors (with or without volume expanders) with clinical endpoints other than laboratory-based are suggested.
Abbreviations
- LVP
large-volume paracentesis
- MAP
mean arterial pressure
- PICD
paracentesis-induced circulatory dysfunction
- PRA
plasma renin activity
- TIPS
transjugular intrahepatic portosystemic shunt
References
- 1.Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122–128. doi: 10.1002/hep.1840070124. [DOI] [PubMed] [Google Scholar]
- 2.Bernardi M, Laffi G, Salvagnini M, Azzena G, Bonato S, Marra F, et al. Efficacy and safety of the stepped care medical treatment of ascites in liver cirrhosis: a randomized controlled clinical trial comparing two diets with different sodium content. Liver. 1993;13:156–162. doi: 10.1111/j.1600-0676.1993.tb00624.x. [DOI] [PubMed] [Google Scholar]
- 3.Angeli P, Dalla Pria M, De Bei E, Albino G, Caregaro L, Merkel C, et al. Randomized clinical study of the efficacy of amiloride and potassium canrenoate in nonazotemic cirrhotic patients with ascites. Hepatology. 1994;19:72–79. doi: 10.1002/hep.1840190113. [DOI] [PubMed] [Google Scholar]
- 4.Bureau C, Thabut D, Oberti F, Dharancy S, Carbonell N, Bouvier A, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology. 2017;152:157–163. doi: 10.1053/j.gastro.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Ginés P, Arroyo V, Quintero E, Planas R, Bory F, Cabrera J, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234–241. doi: 10.1016/0016-5085(87)91007-9. [DOI] [PubMed] [Google Scholar]
- 6.Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651–1653. doi: 10.1002/hep.26359. [DOI] [PubMed] [Google Scholar]
- 7.EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis J. Hepatol. 2010;53:397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Ginès A, Fernández-Esparrach G, Monescillo A, Vila C, Domènech E, Abecasis R, et al. Randomized trial comparing albumin, dextran 70, and polygeline in cirrhotic patients with ascites treated by paracentesis. Gastroenterology. 1996;111:1002–1010. doi: 10.1016/s0016-5085(96)70068-9. [DOI] [PubMed] [Google Scholar]
- 9.Bernardi M, Caraceni P, Navickis RJ, Wilkes MM. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172–1181. doi: 10.1002/hep.24786. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson SP, Smith IK, Williams R. Changes in plasma renin activity in cirrhosis: a reappraisal based on studies in 67 patients and “low-renin” cirrhosis. Hypertension. 1979;1:125–129. doi: 10.1161/01.hyp.1.2.125. [DOI] [PubMed] [Google Scholar]
- 11.Bauer JH. Age-related changes in the renin-aldosterone system. Physiological effects and clinical implications. Drugs Aging. 1993;3:238–245. doi: 10.2165/00002512-199303030-00005. [DOI] [PubMed] [Google Scholar]
- 12.James GD, Sealey JE, Müller F, Alderman M, Madhavan S, Laragh JH. Renin relationship to sex, race and age in a normotensive population. J Hypertens Suppl. 1986;4:S387–S389. [PubMed] [Google Scholar]
- 13.Sharma AM, Schorr U, Oelkers W, Distler A. Effects of sodium salts on plasma renin activity and norepinephrine response to orthostasis in salt-sensitive normotensive subjects. Am J Hypertens. 1993;6:780–785. doi: 10.1093/ajh/6.9.780. [DOI] [PubMed] [Google Scholar]
- 14.Stern N, Sowers JR, McGinty D, Beahm E, Littner M, Catania R, et al. Circadian rhythm of plasma renin activity in older normal and essential hypertensive men: relation with inactive renin, aldosterone, cortisol and REM sleep. J Hypertens. 1986;4:543–550. doi: 10.1097/00004872-198610000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Cohen EL, Conn JW, Rovner DR. Postural augmentation of plasma renin activity and aldosterone excretion in normal people. J Clin Invest. 1967;46:418–428. doi: 10.1172/JCI105543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lijnen P, Fagard R, Staessen J, Amery A. Effect of chronic diuretic treatment on the plasma renin-angiotensin-aldosterone system in essential hypertension. Br J Clin Pharmacol. 1981;12:387–392. doi: 10.1111/j.1365-2125.1981.tb01231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seifarth C, Trenkel S, Schobel H, Hahn EG, Hensen J. Influence of antihypertensive medication on aldosterone and renin concentration in the differential diagnosis of essential hypertension and primary aldosteronism. Clin Endocrinol (Oxf) 2002;57:457–465. doi: 10.1046/j.1365-2265.2002.01613.x. [DOI] [PubMed] [Google Scholar]
- 18.Cabrera J, Falcón L, Gorriz E, Pardo MD, Granados R, Quinones A, et al. Abdominal decompression plays a major role in early postparacentesis haemodynamic changes in cirrhotic patients with tense ascites. Gut. 2001;48:384–389. doi: 10.1136/gut.48.3.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campbell PJ, Skorecki KL, Logan AG, Wong PY, Leung WM, Greig P, et al. Acute effects of peritoneovenous shunting on plasma atrial natriuretic peptide in cirrhotic patients with massive refractory ascites. Am J Med. 1988;84:112–119. doi: 10.1016/0002-9343(88)90017-4. [DOI] [PubMed] [Google Scholar]
- 20.Shaw-Stiffel T, Campbell PJ, Sole MJ, Greig P, Wong PY, Blendis LM. Renal prostaglandin E2 and other vasoactive modulators in refractory hepatic ascites: response to peritoneovenous shunting. Gastroenterology. 1988;95:1332–1338. doi: 10.1016/0016-5085(88)90369-1. [DOI] [PubMed] [Google Scholar]
- 21.Greig PD, Langer B, Blendis LM, Taylor BR, Glynn MF. Complications after peritoneovenous shunting for ascites. Am J Surg. 1980;139:125–131. doi: 10.1016/0002-9610(80)90241-x. [DOI] [PubMed] [Google Scholar]
- 22.Peltekian KM, Wong F, Liu PP, Logan AG, Sherman M, Blendis LM. Cardiovascular, renal, and neurohumoral responses to single large-volume paracentesis in patients with cirrhosis and diuretic-resistant ascites. Am J Gastroenterol. 1997;92:394–399. [PubMed] [Google Scholar]
- 23.Ruiz-del-Arbol L, Monescillo A, Jimenéz W, Garcia-Plaza A, Arroyo V, Rodés J. Paracentesis-induced circulatory dysfunction: mechanism and effect on hepatic hemodynamics in cirrhosis. Gastroenterology. 1997;113:579–586. doi: 10.1053/gast.1997.v113.pm9247479. [DOI] [PubMed] [Google Scholar]
- 24.Elsabaawy MM, Abdelhamid SR, Alsebaey A, Abdelsamee E, Obada MA, Salman TA, et al. The impact of paracentesis flow rate in patients with liver cirrhosis on the development of paracentesis induced circulatory dysfunction. Clin Mol Hepatol. 2015;21:365–371. doi: 10.3350/cmh.2015.21.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simon DM, McCain JR, Bonkovsky HL, Wells JO, Hartle DK, Galambos JT. Effects of therapeutic paracentesis on systemic and hepatic hemodynamics and on renal and hormonal function. Hepatology. 1987;7:423–429. doi: 10.1002/hep.1840070302. [DOI] [PubMed] [Google Scholar]
- 26.Caironi P, Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7:259–267. doi: 10.2450/2009.0002-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caraceni P, Tufoni M, Bonavita ME. Clinical use of albumin. Blood Transfus. 2013;11(Suppl 4):s18–25. doi: 10.2450/2013.005s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia-Martinez R, Caraceni P, Bernardi M, Gines P, Arroyo V, Jalan R. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology. 2013;58:1836–1846. doi: 10.1002/hep.26338. [DOI] [PubMed] [Google Scholar]
- 29.Ginès P, Titó L, Arroyo V, Planas R, Panés J, Viver J, et al. Randomized comparative study of therapeutic paracentesis with and without intravenous albumin in cirrhosis. Gastroenterology. 1988;94:1493–1502. doi: 10.1016/0016-5085(88)90691-9. [DOI] [PubMed] [Google Scholar]
- 30.Sola-Vera J, Miñana J, Ricart E, Planella M, González B, Torras X, et al. Randomized trial comparing albumin and saline in the prevention of paracentesis-induced circulatory dysfunction in cirrhotic patients with ascites. Hepatology. 2003;37:1147–1153. doi: 10.1053/jhep.2003.50169. [DOI] [PubMed] [Google Scholar]
- 31.Moreau R, Valla DC, Durand-Zaleski I, Bronowicki JP, Durand F, Chaput JC, et al. Comparison of outcome in patients with cirrhosis and ascites following treatment with albumin or a synthetic colloid: a randomised controlled pilot trail. Liver Int. 2006;26:46–54. doi: 10.1111/j.1478-3231.2005.01188.x. [DOI] [PubMed] [Google Scholar]
- 32.Alessandria C, Elia C, Mezzabotta L, Risso A, Andrealli A, Spandre M, et al. Prevention of paracentesis-induced circulatory dysfunction in cirrhosis: standard vs half albumin doses. A prospective, randomized, unblinded pilot study. Dig Liver Dis. 2011;43:881–886. doi: 10.1016/j.dld.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Pesaturo AB, Jennings HR, Voils SA. Terlipressin: vasopressin analog and novel drug for septic shock. Ann Pharmacother. 2006;40:2170–2177. doi: 10.1345/aph.1H373. [DOI] [PubMed] [Google Scholar]
- 34.Seo YS, Park SY, Kim MY, Kim JH, Park JY, Yim HJ, et al. Lack of difference among terlipressin, somatostatin, and octreotide in the control of acute gastroesophageal variceal hemorrhage. Hepatology. 2014;60:954–963. doi: 10.1002/hep.27006. [DOI] [PubMed] [Google Scholar]
- 35.Cavallin M, Kamath PS, Merli M, Fasolato S, Toniutto P, Salerno F, et al. Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: A randomized trial. Hepatology. 2015;62:567–574. doi: 10.1002/hep.27709. [DOI] [PubMed] [Google Scholar]
- 36.Morelli A, Ertmer C, Rehberg S, Lange M, Orecchioni A, Cecchini V, et al. Continuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot study. Crit Care. 2009;13:R130. doi: 10.1186/cc7990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choudhury A, Kedarisetty CK, Vashishtha C, Saini D, Kumar S, Maiwall R, et al. A randomized trial comparing terlipressin and noradrenaline in patients with cirrhosis and septic shock. Liver Int. 2017;37:552–561. doi: 10.1111/liv.13252. [DOI] [PubMed] [Google Scholar]
- 38.Singh V, Kumar R, Nain CK, Singh B, Sharma AK. Terlipressin versus albumin in paracentesis-induced circulatory dysfunction in cirrhosis: a randomized study. J Gastroenterol Hepatol. 2006;21:303–307. doi: 10.1111/j.1440-1746.2006.04182.x. [DOI] [PubMed] [Google Scholar]
- 39.Moreau R, Asselah T, Condat B, de Kerguenec C, Pessione F, Bernard B, et al. Comparison of the effect of terlipressin and albumin on arterial blood volume in patients with cirrhosis and tense ascites treated by paracentesis: a randomised pilot study. Gut. 2002;50:90–94. doi: 10.1136/gut.50.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McTavish D, Goa KL. Midodrine. A review of its pharmacological properties and therapeutic use in orthostatic hypotension and secondary hypotensive disorders. Drugs. 1989;38:757–777. doi: 10.2165/00003495-198938050-00004. [DOI] [PubMed] [Google Scholar]
- 41.Saló J, Ginès A, Quer JC, Fernández-Esparrach G, Guevara M, Ginès P, et al. Renal and neurohormonal changes following simultaneous administration of systemic vasoconstrictors and dopamine or prostacyclin in cirrhotic patients with hepatorenal syndrome. J Hepatol. 1996;25:916–923. doi: 10.1016/s0168-8278(96)80297-2. [DOI] [PubMed] [Google Scholar]
- 42.Singh V, Singh A, Singh B, Vijayvergiya R, Sharma N, Ghai A, et al. Midodrine and clonidine in patients with cirrhosis and refractory or recurrent ascites: a randomized pilot study. Am J Gastroenterol. 2013;108:560–567. doi: 10.1038/ajg.2013.9. [DOI] [PubMed] [Google Scholar]
- 43.Singh V, Dheerendra PC, Singh B, Nain CK, Chawla D, Sharma N, et al. Midodrine versus albumin in the prevention of paracentesis-induced circulatory dysfunction in cirrhotics: a randomized pilot study. Am J Gastroenterol. 2008;103:1399–1405. doi: 10.1111/j.1572-0241.2008.01787.x. [DOI] [PubMed] [Google Scholar]
- 44.Appenrodt B, Wolf A, Grünhage F, Trebicka J, Schepke M, Rabe C, Lammert F, et al. Prevention of paracentesis-induced circulatory dysfunction: midodrine vs albumin. A randomized pilot study. Liver Int. 2008;28:1019–1025. doi: 10.1111/j.1478-3231.2008.01734.x. [DOI] [PubMed] [Google Scholar]
- 45.Hardman JG, Limbird LE, Gilman AG. 11th edition. New York, NY: McGraw-Hill; 2006. Goodman and Gilman’s The Pharmacological Basis of Therapeutics; p. 248. [Google Scholar]
- 46.Swan HJ. Noradrenaline, adrenaline, and the human circulation. Br Med J. 1952;1:1003–1006. doi: 10.1136/bmj.1.4766.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nicholls KM, Shapiro MD, Van Putten VJ, Kluge R, Chung HM, Bichet DG, et al. Elevated plasma norepinephrine concentrations in decompensated cirrhosis. Association with increased secretion rates, normal clearance rates, and suppressibility by central blood volume expansion. Circ Res. 1985;56:457–461. doi: 10.1161/01.res.56.3.457. [DOI] [PubMed] [Google Scholar]
- 48.Saif RU, Dar HA, Sofi SM, Andrabi MS, Javid G, Zargar SA. Noradrenaline versus terlipressin in the management of type 1 hepatorenal syndrome: A randomized controlled study. Indian J Gastroenterol. 2018;37:424–429. doi: 10.1007/s12664-018-0876-3. [DOI] [PubMed] [Google Scholar]
- 49.Singh V, Kumar B, Nain CK, Singh B, Sharma N, Bhalla A, et al. Noradrenaline and albumin in paracentesis-induced circulatory dysfunction in cirrhosis: a randomized pilot study. J Intern Med. 2006;260:62–68. doi: 10.1111/j.1365-2796.2006.01654.x. [DOI] [PubMed] [Google Scholar]
- 50.Kulkarni AV, Sukriti S, Maiwall R, Jindal A, Ali R, Thomas S. Midodrine with albumin is safe and effective in preventing complications post-large volume paracentesis-an open labelled randomised controlled trial (NCT-03144713) Hepatology. 2018;68:72A–73A. [Google Scholar]
- 51.Kwok CS, Krupa L, Mahtani A, Kaye D, Rushbrook SM, Phillips MG, et al. Albumin reduces paracentesis-induced circulatory dysfunction and reduces death and renal impairment among patients with cirrhosis and infection: a systematic review and meta-analysis. Biomed Res Int. 2013;2013:295153. doi: 10.1155/2013/295153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simonetti RG, Perricone G, Nikolova D, Bjelakovic G, Gluud C. Plasma expanders for people with cirrhosis and large ascites treated with abdominal paracentesis. Cochrane Database Syst Rev. 2019;6:CD004039. doi: 10.1002/14651858.CD004039.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]