Abstract
Background
Poor adherence to antihypertensives is associated with negative outcome of the disease as well as loss of health-care resources. Addressing the epidemic of poor adherence requires identifying factors associated with this behaviour. The aim of this study is to describe adherence to antihypertensive medication among Lebanese hypertensive patients and to evaluate the association between socio-economic, patient- and conditions-related factors and non-adherence.
Methods
A cross-sectional study was carried out on adherence to antihypertensive medications covering all governorates of Lebanon. This study was conducted between February 2018 and January 2019 on a random sample of 1497 hypertensive patients. A face-to-face questionnaire was used to assess adherence to antihypertensive medication and its determinants according to the five World Health Organization (WHO) main categories. Logistic regression analysis was performed to test the adjusted association between the multiple exposure factors, and drug adherence data were collected by trained interviewers.
Results
Adherence to antihypertensive medications was reported by 1253 (83.7%) of the patients. After multivariate analysis, patients who tried to control their stress level (OR = 0.77, 95% CI [0.38–0.95]), those who had normal BP readings (OR =0.49, 95% CI [0.18–0.97]), and those who believed in the effectiveness of their treatment (OR = 0.31, 95% CI [0.14–0.76]) had a significantly lower chance to exhibit non-adherence to their treatment. However, older patients (OR= 1.87, 95% CI [1.23–2.21]), divorced/separated patients (OR= 2.14, 95% CI [1.31–5.48]), married (OR=1.96, 95% CI [1.27–3.90]), widowed (OR=2.11, 95% CI [1.62–6.50]), obese patients (OR = 1.76, 95% CI [1.21–1.94]), and patients who smoked hookah and cigarettes (OR = 2.62, 95% CI [1.17–6.76]) were more likely to exhibit non-adherence.
Conclusion
Our study highlights the influence of factors such as old age, marital status, BMI and high level of emotional stress on non-adherence to medication in hypertensive patients. These determinants should be incorporated into adherence improving strategies.
Keywords: non-adherence, antihypertensive medications, patient-related factors, condition-related factor, Lebanon
Introduction
The prevalence of hypertension (HT) is growing rapidly worldwide and is reaching epidemic proportions.1 In Lebanon, a population-based study conducted in 2015 revealed that the prevalence rate of HT was 36.9%.2 Antihypertensive medications are effective in lowering blood pressure (BP), preventing target organ damage, averting cardiovascular disease, and reducing mortality.3 Despite the efficacy of antihypertensive agents, non-adherence to these medications limits optimal clinical outcomes.3
Understanding adherence and developing interventions to improve adherence levels are difficult as several factors are associated with adherence levels. The World Health Organization (WHO) proposed to categorize these factors into five main categories: patient’s socio-economic-, therapy-, health-care system-, conditions-, and patient’s related factors.4 In regard to conditions-related factors, stress has been reported to adversely affect the adherence to antihypertensive medication and causes poor BP control.5–7 On the contrary, patients who are aware of the negative impact of stress show better adherence to treatment.8 Other patient-related factors such as tobacco use and high body mass index (BMI) may negatively affect adherence to antihypertensive medication as well.9,10 As for socioeconomic factors, a low social support may be a common risk factor for non-adherence in older patients.11
The 2014 Cochrane review of interventions aimed to promote medication adherence suggesting that it is possible that such interventions have been ineffective because the adherence problem is not sufficiently understood.12 Despite the evidence supporting the efficacy of a range of promising interventions, gaps in knowledge persist.9,10,13,14 Many factors that may affect antihypertensive adherence such as social support, stress, smoking, self-monitoring of BP, attitude toward treatment and weight disorder have never been evaluated in Lebanon. However they have been evaluated in other parts of the world such as the USA, the China, Greece, Italy, Ethiopia, UAE, Gambia and Seychelles who have different health-care systems, reimbursement rules or cultural attitudes to marriage or beliefs in medicine. Therefore, the objective of this study is to describe the antihypertensive medication adherence among Lebanese hypertensive adults’ patients, and to evaluate the association between some socio-economic-, patient- and conditions-related factors and the non-adherence pattern to antihypertensives.
Methods
Source Population
This cross-sectional study was conducted from February 1, 2018 to January 31, 2019. Participants were randomly selected from outpatient clinics in Rafic-Hariri University hospital in Beirut, community pharmacies and cardiology clinics dispersed all over Lebanon.
Eligible participants were Lebanese, 18 years old or older, diagnosed with essential hypertension by a cardiovascular physician, and taking at least one antihypertensive medication such as diuretics, beta-blockers, ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers, alpha blockers and alpha-2 receptor agonists.
Excluded from the study were patients who were not Lebanese, pregnant, under drugs that could increase blood pressure or had secondary HT. If no informed consent was given, participants were also excluded.
Data Collection
Permission letters were sent to 30 pharmacies across Lebanon in order to facilitate cooperation with field interviewers. The cardiologists were contacted by a telephone call in order to gain entry to their clinics and to meet hypertensive patients.
Data were collected through a structured questionnaire composed of different sections which were developed and organized by the researchers following extensive literature review and discussions with hypertensive patients and their treating physicians. The questionnaire was administered by trained interviewers via face-to-face interviews that lasted up to 45 mins. Arabic, the country’s official language was used during interviews in order to enhance the patients’ comprehension. The questionnaire was pilot tested on 45 patients not involved in the study in order to assess its legibility.
Study Measures
Medication Adherence
Non-adherence to antihypertensive medications was self-reported. After clearly describing the WHO definition of medication adherence to participants, they were asked to indicate whether they took their antihypertensive medications as prescribed by their health-care providers or not.
BP measurement
BP measurements were done based on the recommendations of the American Heart Association (AHA) guidelines for measuring BP.15 BP was read with an automated BP machine (Omron HEM-RML 31) after participants rested for 10 mins in a seated position with the right arm placed at the level of the heart. Controlled HT was defined as a BP reading <140 systolic or <90 diastolic mmHg at the time of data collection. BP readings >140 systolic and/or >90 diastolic mmHg were defined as uncontrolled HT. Standardized and identical automated BP machines were used by all trained interviewers.
Patient-related factors
Age and sex were obtained through self-report. Height was measured by trained interviewers to the nearest 0.1 cm with a non-stretchable measuring tape. Participants’ weight was measured to the nearest 0.1 kg with a digital scale (Omron HBF-500). Height and weight were measured with clothes on but no shoes. BMI was calculated for each participant by dividing weight in kilogram by height in meters squared.
Smoking and alcohol status were acquired via self-reported questions and smokers were defined as those currently smoking at the time of data collection. Ex-smokers were defined as those who had smoked greater than 100 cigarettes in their lifetime but had not smoked in the last 28 days.16 Patients’ belief in the effectiveness of the treatment was assessed via direct self-reported question: “Do you believe that your treatment is helpful?” and patients’ awareness about medication adherence was assessed via the following question: “Do you think that non-adherence to medication will affect your health status?”
Socio-economic Factors
Marital status, living status, educational level, occupation, monthly income, and the presence of health insurance were obtained through self-report.
Condition-related factors
Stress was assessed via the following direct question: “Is reducing stress one of your primary goals to control BP?”
Ethical Statement
In order to complete the Institutional Review Boards (IRB) requirements, the interviewers passed an exam offered by the National Institute of Health (NIH) office for extramural research: “Protecting Human Research Participants”. The study protocol was reviewed and approved by the IRB of the Lebanese University and the IRB of Rafic-Hariri University hospital. In accordance with the privacy rule of the Health Insurance Portability and Accountability Act and the declaration of Helsinki, all patients who participated in the study gave written informed consent.
Statistical Analyses
The data on 1497 questionnaires was entered and analyzed by Statistical Package for the Social Sciences (SPSS) program version 20. As part of quality control, data entered into the computer was double-checked for its accuracy by random assessment of the survey responses and the data entered. Qualitative data were represented in frequency and percentage, while quantitative data, such as BP, weight and height, were represented by mean and standard deviation (SD).
Logistic regression analysis was performed to test the adjusted association between the multiple exposure factors and drug adherence. Odds ratios (OR) and their respective 95% confidence interval (CI) were reported, and p <0.05 was used to determine statistical significance. Based on clinical judgment and known confounders, adjustment included age, gender, educational level, marital status, monthly income and health insurance.
Results
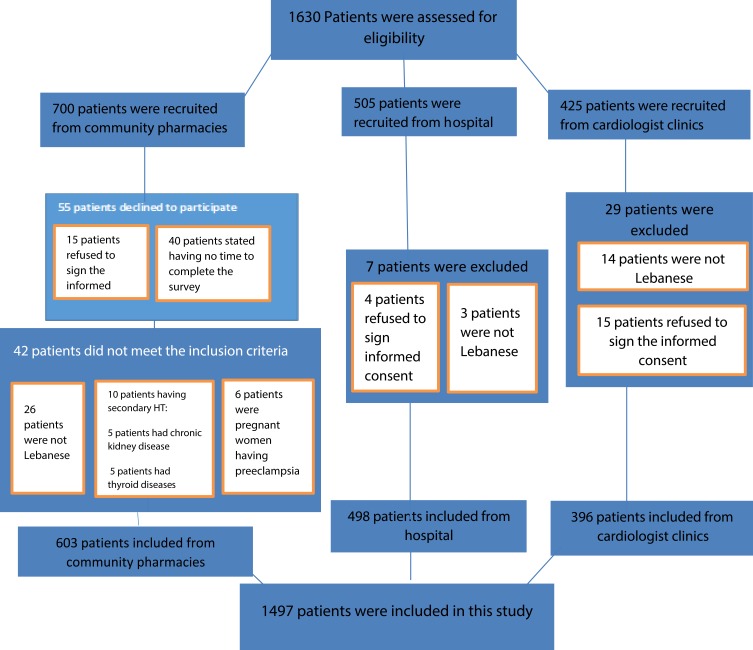
A total of 1497 participants was included in this study (Figure 1). As shown in Table 1, 603 (40.2%) participants were recruited from community pharmacies, 498 (33.3%) from Rafic-Hariri University hospital and 396 (26.5%) from private cardiology clinics.
Figure 1.
Flow chart of cohort creation.
Table 1.
Baseline Characteristic and Patient-Related Factors
| Variables | Adherent Participants; N= 1253 (%) |
Non-Adherent Participants; N=244 (%) |
Total Participants, N=1497 (%) |
|||
|---|---|---|---|---|---|---|
| Location | ||||||
| Community Pharmacies | 504 | (83.6) | 99 | (16.4) | 603 | (40.2) |
| Rafic-Hariri University hospital | 372 | (74.7) | 126 | (25.3) | 498 | (33.3) |
| Clinics | 376 | (94.9) | 20 | (5.1) | 396 | (26.5) |
| Patient-Related Factors | ||||||
| Age | ||||||
| 18–44 | 180 | (90.0) | 20 | (10.0) | 200 | (13.4) |
| 45–64 | 297 | (75.8) | 95 | (24.2) | 392 | (26.2) |
| ≥65 | 776 | (85.7) | 129 | (14.3) | 905 | (60.4) |
| Gender | ||||||
| Male | 598 | (82.6) | 126 | (17.4) | 724 | (48.3) |
| Female | 655 | (84.7) | 118 | (15.3) | 773 | (51.7) |
| BMI (kg/m2) | ||||||
| <18.5 | 6 | (66.7) | 3 | (33.3) | 9 | (0.6) |
| 18.5–24.9 | 262 | (82.4) | 56 | (17.6) | 318 | (21.4) |
| 25–29.9 | 602 | (89.2) | 73 | (10.8) | 675 | (45.0) |
| ≥30 | 383 | (77.4) | 112 | (22.6) | 495 | (33.0) |
| Lifestyle | ||||||
| Smoking Status | ||||||
| Smoking Cigarettes | 355 | (80.7) | 85 | (19.3) | 440 | (29.4) |
| Smoking Hookah | 82 | (59.4) | 56 | (40.6) | 138 | (9.2) |
| Smoking hookah and cigarette | 73 | (50.0) | 73 | (50.0) | 146 | (9.8) |
| Never smoked | 479 | (95.2) | 24 | (4.8) | 503 | (33.6) |
| Ex-smoker | 264 | (97.8) | 6 | (2.2) | 270 | (18.0) |
| Do you think that non-adherence to medication will affect your health status? | ||||||
| Yes | 1157 | (93.7) | 78 | (6.3) | 1235 | (82.5) |
| No | 96 | (36.6) | 166 | (63.4) | 262 | (17.5) |
| Do you believe that your treatment is helpful? | ||||||
| Yes | 1151 | (93.9) | 75 | (6.1) | 1226 | (81.9) |
| No | 102 | (37.6) | 169 | (62.4) | 271 | (18.1) |
Patient-Related Factors
Baseline characteristics are shown in Table 1. Participants did not differ significantly in relation to gender. A larger number of women (n=773, 51.7%) than men (n=724, 48.3%) was part of this study. By age group, 200 (13.4%) were between 18 and 44, 392 (26.2%) were between 45 and 64, and 905 (60.4%) were above 65 years of age. Obesity (BMI ≥ 30 kg/m2) was found in 33.0% of patients. Active smoking was reported by 724 (48.4%) participants. The study also showed that 1235 (82.5%) of the participants were aware that non-adherence may affect their health status, and 1226 (81.9%) believed that their treatment regimens were helpful.
Socio-Economic and Condition-Related Factors
As shown in Table 2, low monthly family income of less than USD 1000 was reported by 549 (36.7%). Low education level (less than high school) was reported by 744 (49.7%) and 1116 (74.6%) reported to be married. Living alone was reported by 206 (13.8%) of the participants and 1157 (77.3%) of participants were accompanied by a family member or friend when visiting their physicians. In addition, 838 (56.0%) aimed at reducing their stress level and 1171 (78.2%) participants were covered by health insurance.
Table 2.
Socio-Economic and Condition-Related Factors
| Variables | Adherent Participants; N= 1253 (%) |
Non-Adherent Participants, N=244 (%) |
Total Participants, N=1497 (%) |
|||
|---|---|---|---|---|---|---|
| Socio-economic factors | ||||||
| Marital status | ||||||
| Single | 64 | (41.8) | 89 | (58.2) | 153 | (10.2) |
| Married | 1084 | (97.1) | 32 | (2.9) | 1116 | (74.6) |
| Divorced | 20 | (29.0) | 49 | (71.0) | 69 | (4.6) |
| Widowed | 85 | (53.4) | 74 | (46.6) | 159 | (10.6) |
| Living alone | ||||||
| Yes | 10 | (4.8) | 196 | (95.2) | 206 | (13.8) |
| No | 1243 | (96.3) | 48 | (3.7) | 1291 | (86.2) |
| Education level | ||||||
| No formal education | 198 | (78.0) | 56 | (22.0) | 254 | (17.0) |
| Primary education | 448 | (91.4) | 42 | (8.6) | 490 | (32.7) |
| Secondary education | 374 | (85.4) | 64 | (14.6) | 438 | (29.3) |
| University studies | 233 | (74.0) | 82 | (26.0) | 315 | (21.0) |
| Does someone accompany you when visiting your physician | ||||||
| Yes | 995 | (86.0) | 162 | (14.0) | 1157 | (77.3) |
| No | 258 | (75.9) | 82 | (24.1) | 340 | (22.7) |
| Monthly income | ||||||
| Less than 1000$ | 500 | (91.0) | 49 | (9.0) | 549 | (36.7) |
| 1000 to 2000$ | 358 | (86.5) | 56 | (13.5) | 414 | (27.7) |
| More than 2000$ | 81 | (91.0) | 8 | (9.0) | 89 | (5.9) |
| No answer | 314 | (70.6) | 131 | (29.4) | 445 | (29.7) |
| Do you have a health insurance? | ||||||
| Yes | 1064 | (90.9) | 107 | (9.1) | 1171 | (78.2) |
| No | 189 | (58.0) | 137 | (42.0) | 326 | (21.8) |
| Condition-related factor | ||||||
| Is reducing stress one of your primary goals to control BP?” | ||||||
| Yes | 786 | (93.8) | 52 | (6.2) | 838 | (56.0) |
| No | 467 | (70.9) | 192 | (29.1) | 659 | (44.0) |
Adherence Pattern and Blood Pressure Characteristic
With regards to non-adherence, 244 (16.3%) of the participants declared not taking their antihypertensive medications as prescribed by their doctors. Among these non-adherent participants, 153 (62.7%) related this behaviour to mere forgetfulness. As shown in Table 3, 1031 (68.9%) checked their BP at home.
Table 3.
Adherence Pattern and Blood Pressure Characteristics
| Variables | Number of Participants; N=1497 | Percentage (%) |
|---|---|---|
| Adherent | 1253 | 83.7 |
| Non-adherent | 244 | 16.3 |
| Main reason of non-adherence in non-adherent patients | ||
| Side effects | 22 | 9.0 |
| High medication cost | 22 | 9.0 |
| Interaction with other medications | 2 | 0.8 |
| Simple forgetfulness | 153 | 62.7 |
| Do not need/Do not think about it | 40 | 16.4 |
| Others | 5 | 2.1 |
| Do you check your blood pressure at home? | ||
| Yes | 1031 | 68.9 |
| No | 466 | 31.1 |
Factors Associated with Antihypertensive Medication Non-Adherence in Lebanese Adults
In Table 4, logistic regression analysis was used to evaluate predictors of non-adherence to antihypertensive medications. The variables included age, gender, marital status, living arrangements, BMI, smoking status, stress, education level, health insurance regular check-up of BP, normal BP reading, patients ‘awareness about non-adherence and belief in the effectiveness of the treatment.
Table 4.
Factors Associated with Antihypertensive Medication Non-Adherence in Lebanese Adults
| Factor | Number of Non-Adherent Patients (N=244), (%) | Crude OR (95% CI) | Age-Sex Adjusted OR (95% CI) | Fully Adjusted(a) OR (95% CI) | |
|---|---|---|---|---|---|
| Patient-related | |||||
| Age (years) | |||||
| 18–44 | 20 | 10.0 | 1 | 1 | 1 |
| 45–64 | 95 | 24.2 | 1.43 (1.11–1.72) | 1.52 (1.16–1.76) | 1.39 (1.13–1.67) |
| ≥65 | 129 | 14.3 | 1. 67 (1.13–1.96) | 1.95 (1.16–2.29) | 1.87 (1.23–2.21) |
| Sex | |||||
| Male | 126 | 17.4 | 1 | 1 | 1 |
| Female | 118 | 15.3 | 1.76 (0.42–2.41)* | 1.74(0.51–2.40)* | 1.49 (0.39–1.64)* |
| Lifestyle | |||||
| BMI (kg/m2) | |||||
| <18.5 | 3 | 33.3 | 1.68(1.27–3.42) | 1.43(1.14–1.87) | 1.11 (1.02–1.27) |
| 18.5–24.9 | 56 | 17.6 | 1 | 1 | 1 |
| 25–29.9 | 73 | 10.8 | 1.46(1.22–1.80) | 1.23 (1.07–2.04) | 1.54 (1.23–1.89) |
| ≥30 | 112 | 22.6 | 1.71(1.41–1.94) | 1.74 (1.34–1.95) | 1.76 (1.21–1.94) |
| Smoking Status | |||||
| Smoking Cigarettes | 85 | 19.3 | 1.45 (1.14–2.71) | 1.77 (1.13–2.79) | 1.87 (1.34–2.98) |
| Smoking Hookah | 56 | 40.6 | 1.54 (1.26–1.97) | 2.08 (1.12–3.87) | 2.32 (1.35–4.97) |
| Smoking hookah and cigarette | 73 | 50.0 | 2.36 (1.43–1.96) | 2.43 (1.26–4.49) | 2. 62 (1.17–6.76) |
| Never smoked | 24 | 4.8 | 1 | 1 | 1 |
| Ex-smoker | 6 | 2.2 | 0.84 (0.45–2.61)* | 1.16 (0.48–1.97)* | 0.86 (0.43–1.05)* |
| Patients’ Awareness About Importance of Medication Adherence | |||||
| Yes | 78 | 6.3 | 0.24 (0.12–0.56) | 0.20 (0.15–0.61) | 0.22 (0.13–0.54) |
| No | 166 | 63.4 | 1 | 1 | 1 |
| Patients’ belief in treatment | |||||
| Yes | 75 | 6.1 | 0.29 (0.11–0.67) | 0.33 (0.19–0.69) | 0.31 (0.14–0.76) |
| No | 169 | 62.4 | 1 | 1 | 1 |
| Self-Measurement of BP | |||||
| Yes | 60 | 24.6 | 0.51 (0.24–0.92) | 0.63 (0.31–0.95) | 0.67 (0.32–0.91) |
| no | 184 | 75.4 | 1 | 1 | 1 |
| Normal BP Reading | |||||
| Yes | 43 | 17.6 | 0.58(0.21–0.96) | 0.51 (0.14–0.93) | 0.49 (0.18–0.97) |
| No | 201 | 82.4 | 1 | 1 | 1 |
| Social/Economic-Related | |||||
| Marital status | |||||
| Single | 89 | 58.2 | 1 | 1 | 1 |
| Married | 32 | 2.9 | 1.84 (1.12–3.41) | 1.91 (1.38–3.94) | 1.96 (1.27–3.90) |
| Divorced/Separated | 49 | 71.0 | 2.28 (1.30–4.40) | 2.31 (1.21–4.81) | 2.14 (1.31–5.48) |
| Widowed | 74 | 46.6 | 2.51 (1.75–7.81) | 2.63 (1.52–8.43) | 2.11 (1.62–6.50) |
| Living Arrangements | |||||
| alone | 196 | 95.2 | 1 | 1 | 1 |
| With others | 48 | 3.7 | 1.48 (1.26–2.14) | 1.51 (1.24–2.54) | 1.95 (1.19–2.68) |
| Education Level | |||||
| No formal education | 56 | 22.0 | 2.44 (0.81–3.96)* | 2.53(0.45–4.10)* | 2.23 (0.72–3.74)* |
| Primary education | 42 | 8.6 | 1.46 (1.07–2.30)* | 1.76 (0.27–3.06)* | 1.31 (0.41–4.17)* |
| Secondary education | 64 | 14.6 | 1.29 (0.45–1.32)* | 1.67 (0.52–1.81)* | 1.59 (0.54–1.89)* |
| University studies | 82 | 26.0 | 1 | 1 | 1 |
| Having a Health Insurance? | |||||
| Yes | 107 | 9.1 | 1.07 (0.08–2.24)* | 1.29 (1.10–1.85) | 1.29 (1.11–1.74) |
| No | 137 | 42.0 | 1 | 1 | 1 |
| Condition-related factor | |||||
| Controlling stress | |||||
| Yes | 52 | 6.2 | 0.62 (0.37–0.91) | 0.53(0.23–0.94) | 0.77 (0.38–0.95) |
| No | 192 | 29.1 | 1 | 1 | 1 |
Notes: aAdjusted for the following covariates: age, gender, educational level, marital status, monthly income and health insurance. *Variables those were not significant during logistic regression analysis at P value < 0.05.
As shown in Table 4, when fully adjusted for the selected covariates such as age, gender, education level, marital status, monthly income and health insurance, the logistic regression showed that patients who tried to control their stress level (OR = 0.77, 95% CI [0.38–0.95]) were less likely to be non-adherent to their antihypertensive treatment. In addition to that, those who had normal BP readings (OR =0.49, 95% CI [0.18–0.97]), those who believed in the effectiveness of their treatment (OR = 0.31, 95% CI [0.14–0.76]) and those who self-measured their BP (OR = 0.67, 95% CI [0.32–0.91]) had a significantly lower chance of being non-adherent to their antihypertensive therapies.
On the other hand, older patients (OR= 1.87, 95% CI [1.23–2.21]), divorced/separated patients (OR= 2.14, 95% CI [1.31–5.48]), married (OR=1.96, 95% CI [1.27–3.90]), widowed (OR=2.11, 95% CI [1.62–6.50]), obese patients (OR = 1.76, 95% CI [1.21–1.94]), and patients who smoked hookah and cigarettes (OR = 2.62, 95% CI [1.17–6.76]) were more likely to exhibit non-adherence.
Discussion
The present study aimed to describe the antihypertensive medication adherence among Lebanese hypertensive adults’ patients and to investigate the association between some socio-economic-, patient- and conditions-related factors and non-adherence pattern. In our study, 244 (16.3%) of the participants did not adhere to their antihypertensives, which was lower than the results found in the majority of other countries.17–24 The result could be explained by the absence of one of the most common barriers to medication adherence which is the cost factor, as 78.2% of the study group had a health insurance. The results were also supported by the increased awareness among the study participants as 81.9% of them were aware about the importance of adherence to treatment. In addition, variations in adherence rates could be explained by cultural factors, such as cultural health perception of HT, social support and self-care behaviours among different populations.
Our research on adherence to antihypertensive treatments has shown that patient’s non-adherence to medication was mainly related to the following factors: Marital status, age, BMI, smoking pattern, controlling stress, having normal BP readings, self-measurement of BP and believing in the effectiveness of the therapy regimen, all with different effects on adherence level.
This study showed that married (OR=1.96, 95% CI [1.27–3.90]), widowed (OR=2.11, 95% CI [1.62–6.50]), divorced or separated patients (OR= 2.14, 95% CI [1.31–5.48]) were more likely to exhibit non-adherence as compared to single patients. To our knowledge, this is the first study in Lebanon that evaluates the impact of marital status on adherence to antihypertensives among Lebanese patients. Hu et al in their study in the Chinese community, found a positive association between family social support and adherence to medication. A 10-unit increase in family social support increased the odds ratio of taking medication by 1.39 (95% CI, 1.03–1.87).12 A study by Osamor25 in Nigeria showed that patients who had support from friends displayed better compliance to treatment than those who did not. Another study by Sayers et al demonstrated a positive effect of family support on adherence to treatment.26 Maguire and colleagues also found that high level of social support were associated with high level of adherence.27 Although marital status is considered a measure of social network, this factor alone could not always reflect the lack of family support since widowed, divorced or separated people may be well supported by their families. Nevertheless, this factor may affect the emotional well-being of patients and it showed a significant impact on adherence to treatment.28
Age is a factor reported as affecting adherence, but inconsistently. This study has shown that adherence to treatment was negatively correlated with age, contrary to the findings of other studies which stated that young age leads to lower adherence.17,29,30 However, the results of some reports were consistent with our findings.31–33 A study showed that patients under 65 years of age achieved better adherence than elderly subjects (P=0.0005).33 The lowest adherence was observed among old age pensioners (>65 years old).34 These findings may be linked to the main cause of non-adherence determined by our study, especially the aspect of mere forgetfulness. Memory impairment and limited ability to absorb new information are usually observed in elder patients since people tend to forget more as they grow older.35
In this study, almost half of our participants reported to be active smokers. This population had a two-fold risk of being non-adherent to their antihypertensives compared to never smokers. To our knowledge, there are very few publications that show a link between the smoking pattern and adherence to antihypertensive treatments. Our findings support the results of the study conducted in the Midwestern United States which concludes that adherence to medications used for chronic conditions was significantly lower among smokers.36 In support of this finding, another study showed the negative association between smoking water pipe and adherence to treatment.36 Smoking less than three water pipes per week compared to no water pipe smoking was significantly associated with a decrease in the adherence score.37 In other studies, no significant association between medication adherence and smoking was found.34,38
Other factors that could affect treatment adherence, include normal BP readings, self-monitoring of BP, and the belief in the effectiveness of the therapy regimen. In our study, those who had normal BP had a significantly lower chance of being non-adherent to their antihypertensive therapies. Studies conducted in Ethiopia and in Greece showed that controlling BP was associated with high adherence.17,18 Also, the result of a study by Marquez-Contreras et al showed an improved adherence rate in patients who carried out self-monitoring in comparison with usual care.39 In addition to that, in a randomized clinical trial by van Onzenoort et al, self-monitoring as an adjunct to office BP measurement resulted in higher adherence to treatment.40 As mentioned previously, the belief in the effectiveness of treatment was reported by 1226 (81.9%) of the participants. Witnessing a positive outcome of the treatment makes patients feel more secure, satisfied and confident about the given treatment and this encourages them to continue their treatment.18,39
In this study, the logistic regression analysis showed that patients who tried to control their stress level were less likely to be non-adherent to their antihypertensive treatment (OR = 0.77, 95% CI [0.38–0.95]). This is consistent with findings from a Greek study.17 Also, Kretchy et al (2014) stated that stress among patients increased their chances to be less adherent to antihypertensive medications.41 The relationship between stress and non-adherence suggests the importance of recognizing stress as a risk factor for poor adherence to antihypertensives.
Most studies examined patients’ weight following the advice of their physicians, but no study showed adherence to HT medications among obese and underweight patients.42,43 In this study, both obese and underweight patients showed a higher chance of being non-adherent to HT medications. The low adherence of these patients could be related to the underlying causes behind the weight disorder such as mental disorders which contribute to this behaviour.41 More research is recommended on the association between BMI and adherence to HT medications.
The large sample of the population and the wide geographical coverage of this study are considered points of strength. This ensured the inclusion of participants of different socio-demographic characteristics. Moreover, several limitations of our study should be addressed. First, the data were collected using an interviewer-administered method. Although this method is less expensive and easily applicable, the study is prone to social desirability and recall bias. In this regard, participants were adequately informed about the relevance of this study and the importance of telling the truth. Secondly, single BP readings were used to classify BP as controlled or uncontrolled, which may increase classification bias. In addition to the above, we did not account for “white-coat” adherence, which is defined as improving medication-taking behaviour shortly before and after an appointment with a health-care provider.
Conclusion
In summary, the present study confirmed that factors such as marital status, age, BMI, smoking habits, controlling stress level, having good BP readings, self-measurement of BP and believing in physician’s treatment, were significantly associated with adherence to antihypertensive treatment. Future research should examine our findings and test whether managing these factors may contribute to better treatment adherence and improved BP control.
Acknowledgment
This project has been funded with support from Lebanese University.
Disclosure
FV is supervises two PhD students who are employed with F. Hoffmann-La Roche Ltd (Basel, Switzerland [RH] and Welwyn Garden City, UK); the topics of their PhD are not related to the current study and he has not received any funding or reimbursements for this. The authors report no other conflicts of interest in this work.
References
- 1.Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matar D, Frangieh AH, Abouassi S, et al. Prevalence, awareness, treatment, and control of hypertension in Lebanon. J Clin Hypertens (Greenwich). 2015;17(5):381–388. doi: 10.1111/jch.12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoon S, Fryar C, Carroll M Hypertension Prevalence and Control among Adults: united States, 2011–2014. NCHS Data Brief, No 220. Hyattsville, MD: National Center for Health Statistics; 2015. Available from: www.cdc.gov/nchs/data/databriefs/db220.htm. Accessed December18, 2016. [PubMed] [Google Scholar]
- 4.WHO.int [homepage on the Internet]. Global status report on non-communicable diseases 2014; 2014:298 Available from: www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed November10, 2017.
- 5.Krousel-Wood M, Islam T, Muntner P, et al. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40(3):248–257. doi: 10.1007/s12160-010-9217-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darviri AK, Artemiadis A, Protogerou A, et al. A health promotion and STRESS management program (HEAL-STRESS study) for pre-hypertensive and hypertensive patients: a quasi-experimental study in Greece. J. Hum. Hypertens. 2016;30(6):397–403. doi: 10.1038/jhh.2015.99 [DOI] [PubMed] [Google Scholar]
- 7.Flack JM, Sica DA, Bakris G, et al. Management of high blood pressure in Blacks: an update of the International Society on hypertension in blacks consensus statement. Hypertension. 2010;56(5):780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892 [DOI] [PubMed] [Google Scholar]
- 8.Hayrettin K, Yokuşoğlu M, Uzun S, et al. The effect of the content of the knowledge on adherence to medication in hypertensive patients. Anadolu Kardiyol Derg. 2009;9(3):183–188. [PubMed] [Google Scholar]
- 9.Aggarwal B, Mosca L. Lifestyle and psychosocial risk factors predict non-adherence to medication. Ann Behav Med. 2010;40(2):228–233. doi: 10.1007/s12160-010-9212-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Natarajan N, Putnam W, van Aarsen K, et al. Adherence to antihypertensive medications among family practice patients with diabetes mellitus and hypertension. Can Fam Physician. 2013;59(2):e93–e100. [PMC free article] [PubMed] [Google Scholar]
- 11.Costa Rdos S, Nogueira LT. Family support in the control of hypertension. Rev Lat Am Enfermagem. 2008;16(5):871–876. doi: 10.1590/S0104-11692008000500012 [DOI] [PubMed] [Google Scholar]
- 12.Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;20(11):CD000011. doi: 10.1002/14651858.CD000011.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu H, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviors in Chinese local community. J Hum Hypertens. 2015;29(3):198–203. doi: 10.1038/jhh.2014.58 [DOI] [PubMed] [Google Scholar]
- 14.Van der Laan DM, Elders PJM, Boons CCLM, Beckeringh JJ, Nijpels G and Hugtenburg JG. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens. 2017;31(11):687–694. doi: 10.1038/jhh.2017.48 [DOI] [PubMed] [Google Scholar]
- 15.Paul KW, Robert MC, Wilbert SA, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;(71):e127– 248. doi: 10.1161/HYP.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Health - Manatū Hauora. Definitions of Smoking Status. New Zealand: Ministry of Health; 2015. June 04 Available from: https://www.health.govt.nz/ourwork/preventative-health-wellness/tobacco-control/tobacco-control-information-practitioners/definitions-smoking-status Accessed December12, 2018. [Google Scholar]
- 17.Tsiantou V, Pantzou P, Pavi E, et al. Factors affecting adherence to antihypertensive medication in Greece: results from a qualitative study. Patient Prefer Adherence. 2010;7(4):335–343. doi: 10.2147/PPA.S12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ambaw A, Alemie G, Yohannes S, et al. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;10(4):12–282. doi: 10.1186/1471-2458-12-282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bader RJK, Koprulu F, Hassan NAGM, et al. Predictors of adherence to antihypertensive medication in northern United Arab Emirates. Eastern Mediter Health J. 2015;21(5):309–318. doi: 10.26719/2015.21.5.309 [DOI] [PubMed] [Google Scholar]
- 20.Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120(16):1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299 [DOI] [PubMed] [Google Scholar]
- 21.Hotle E, Muntner P, Joyce C, et al. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39(4):481–487. doi: 10.1093/ageing/afq040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo H, He H, Jiang J. Study on the compliance of antihypertensive drugs in patients with hypertension. Chin J Epidemiol. 2001;22(6):418–420. [PubMed] [Google Scholar]
- 23.Van der Sande MA, Milligan PJ, Nyan OA, et al. Blood pressure patterns and cardiovascular risk factors in rural and urban Gambian communities. J Hum Hypertens. 2000;14(8):489–496. doi: 10.1038/sj.jhh.1001050 [DOI] [PubMed] [Google Scholar]
- 24.Bovet P, Burnier M, Madeleine G, et al. Monitoring one-year compliance to antihypertension medication in the Seychelles. Bull World Health Organ. 2002;80(1):33–39. [PMC free article] [PubMed] [Google Scholar]
- 25.Osamor PE. Social support and management of hypertension in south-west Nigeria. Cardiovasc J Afr. 2015;26(1):29–33. doi: 10.5830/CVJA-2014-066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sayers SL, Riegel B, Pawlowski S, et al. Social support and self-care of patients with heart failure. Ann Behav Med. 2008;35(1):70–79. doi: 10.1007/s12160-007-9003-x [DOI] [PubMed] [Google Scholar]
- 27.Maguire LK, Hughes CM, McElnay JC. Exploring the impact of depressive symptoms and medication beliefs on medication adherence in hypertension – a primary care study. Patient Educ Couns. 2008;73(2):371–376. doi: 10.1016/j.pec.2008.06.016 [DOI] [PubMed] [Google Scholar]
- 28.Ranak BT, Brian A, David E, et al. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med. 2008;31(6):489–497. doi: 10.1007/s10865-008-9173-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siba J, Hicham J, Aline H, et al. Quality of life and its association with treatment satisfaction, adherence to medication, and trust in physician among patients with hypertension: a cross-sectional designed study adherence. J Cardiovasc Pharmacol Ther. 2018;23(6):532–542. doi: 10.1177/1074248418784292 [DOI] [PubMed] [Google Scholar]
- 30.Hadi N, Rostami GN. Determinant factors of medication compliance in hypertensive patients of Shiraz, Iran. Arch Iran Med. 2004;7(4):292–296. [Google Scholar]
- 31.Simpson RJ. Challenges for improving medication adherence. JAMA. 2006;296(21):2614–2616. doi: 10.1001/jama.296.21.jed60074 [DOI] [PubMed] [Google Scholar]
- 32.Sattler ELP, Lee JS, Perri MIII. Medication (re)fill adherence measures derived from pharmacy claims data in older Americans. A review of the literature. Drugs Aging. 2013;30(6):383–399. doi: 10.1007/s40266-013-0074-z [DOI] [PubMed] [Google Scholar]
- 33.Cotter G, Shemesh E, Zehavi M, et al. Lack of aspirin effect: aspirin resistance or resistance to taking aspirin? Am Heart J. 2004;147(2):293–300. doi: 10.1016/j.ahj.2003.07.011 [DOI] [PubMed] [Google Scholar]
- 34.Bruce WS, Wendy DL. The association of smoking with medical treatment adherence in the workforce of a large employer. Patient Prefer Adherence. 2014;8:477–486. doi: 10.2147/PPA.S60927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Preventive Services Task Force. Cognitive impairment in older adults: screening. 2014. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cognitive-impairment-in-older-adults-screening. Accessed March23, 2020.
- 36.Lucine H, Mary BS, Souheil H, et al. Adherence to insulin, emotional distress, and trust in physician among patients with diabetes: a cross-sectional study. Diabetes Ther. 2018;9(2):713–726. doi: 10.1007/s13300-018-0389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang PS, Bohn RL, Knight E, et al. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504–511. doi: 10.1046/j.1525-1497.2002.00406.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yianna E, Papadopulos JS, Cokkinos DV, et al. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12(3):243–249. doi: 10.1097/00149831-200506000-00010 [DOI] [PubMed] [Google Scholar]
- 39.Márquez-Contreras E, Martell-Claros N, Gil-Guillén V, et al. Efficacy of a home blood pressure monitoring program on therapeutic compliance in hypertension: the EAPACUM-HTA study. J Hypertens. 2006;24(1):169–175. [DOI] [PubMed] [Google Scholar]
- 40.Van Onzenoort HA, Verberk WJ, Kroon AA, et al. Effect of self-measurement of blood pressure on adherence to treatment in patients with mild-to-moderate hypertension. J Hypertens. 2010;28(3):622–627. doi: 10.1097/HJH.0b013e328334f36b [DOI] [PubMed] [Google Scholar]
- 41.Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Ment Health Syst. 2014;(21):8–25. doi: 10.1186/1752-4458-8-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. West J Nurs Res. 2006;28(2):190–209. doi: 10.1177/0193945905283367 [DOI] [PubMed] [Google Scholar]
- 43.Whelton SP, Hyre AD, Pedersen B, et al. Effect of dietary fiber intake on blood pressure: a meta-analysis of randomized, controlled clinical trials. J Hypertens. 2005;23(3):475–481. doi: 10.1097/01.hjh.0000160199.51158.cf [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- WHO.int [homepage on the Internet]. Global status report on non-communicable diseases 2014; 2014:298 Available from: www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed November10, 2017.
- U.S. Preventive Services Task Force. Cognitive impairment in older adults: screening. 2014. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cognitive-impairment-in-older-adults-screening. Accessed March23, 2020.