Abstract
Objectives
Management of missed Monteggia lesions presents a challenging clinical scenario for pediatric orthopaedic surgeons as the patient may be exposed to possible morbidities and increased complications. There are several evidenced surgical strategies described. We aimed to present 18 patients diagnosed within 4 months of injury who were treated using 4 of the identified many surgical strategies.
Methods
Eighteen consecutive cases of missed Monteggia lesions were treated in our institution between 2011 and 2014. The mean delay from injury to surgery was 8.3 weeks (range 4–16). Bilateral preoperative and postoperative radiographs, Oxford Elbow Score, the direction of radial head dislocation, Bado classification, ulnar pathology (plastic deformation or fracture), carrying angle, head–neck ratio, any abnormal bony architecture, and any related condition.
Results
There were no major complications to surgery. All patients had regained painless range of motion of the forearm and elbow, and reduced radiocapitellar joint. Ligament reconstruction or transcapitellar k-wire fixation did not influence the radiographic or clinical outcome.
Conclusions
Because conservative treatment of this injury may cause high morbidity, surgical management should be preferred in the foreground. The ulnar deformity is a key point in the reduction of the radiocapitellar joint. The preferred treatment strategy has no significant effect on the results as long as it provides radial head reduction.
Keywords: Missed monteggia lesion, Children, Ulnar osteotomy, Radial head dislocation
1. Introduction
One of the many complications of acute Monteggia lesion and its equivalent is delayed diagnosis, especially in children. Management of missed Monteggia lesions presents a challenging clinical scenario for pediatric orthopaedic surgeons as the patient may be exposed to possible morbidities and increased complications thereby making management more difficult for the surgeon.
A variety of surgical techniques have been described and validated in literature. These procedures include open or closed reduction of the radial head, repair or reconstruction of the annular ligament, temporary fixation of the radial head with a transcapitellar k-wire, and ulnar and/or radial osteotomies.1, 2, 3, 4, 5, 6, 7 There are even several ulnar fixation methods such as Ilizarov external fixator, plate, cross k-wire, intramedullary k-wire or a combination of these techniques.5,6,8,9
The clinical outcome of the surgical management of delayed or chronic radial head dislocation is still unpredictable. This is because this pathology is infrequent and several different presentations are referred to by the same name. There are many known morbidity complications including joint stiffness, restricted elbow range of motion, radial head or elbow instability, non-union or malunion of the osteotomies, narrowing or growth disturbance of the radial neck, avascular necrosis of the radial head, nerve injury, infection and secondary degenerative arthritis.3,10, 11, 12, 13, 14 For these complicated injuries, most authors recommend aiming for direct reduction of the radial head,1,3,10 while others recommend a different approach of indirect reduction of the radial head with correction or over-correction of the ulnar deformity.5,15,16 If there is radiocapitellar joint dislocation, this can eventually cause a hypertrophic and distorted radial head.17
If this condition is followed up conservatively without treatment, poor long-term outcomes can be expected with pain, instability, deformity, loss of strength, and decreased range of motion.18,19 The objective of this retrospective study was to evaluate the clinical and radiological outcome of patients who were treated for missed Monteggia lesions.
2. Methods
This retrospective evaluation of clinical records and radiographic images was approved by our hospital Institutional Review Board. The study included a total of 18 children (12 male, 6 female) who were treated for dislocation of the radial head (≥3 weeks post-injury) and malunion or plastic deformation of the ulna between November 2011 and December 2014. All patients were treated initially at other hospitals and were referred to our department for treatment. None of the patients had a history of forearm, arm or elbow pathology or surgery. Initially 26 patients were identified from the hospital records. After the exclusion of patients with incomplete follow-up data, congenital dislocation, multiple exostoses, or syndromic disorders, evaluation was made of a total of 18 patients who had regular follow-up clinical data and radiographic examinations.
The average interval between the initial injury and the surgery was 8.3 weeks (range 4–16 weeks), and the average age of the patients at the time of surgery was 6.9 years (range, 2.6–12.2 years). All patients had complaints of pain and limited range of motion of the elbow and forearm. None of the children presented with sensory or motor nerve palsy. AP and lateral radiographs of the elbow were taken, Monteggia lesion was confirmed in all patients and the direction of radial head dislocation and type of ulna fracture were noted (Table 1). For each patient a record was made of measurements on the preoperative and postoperative radiographs, the direction of radial head dislocation, Bado classification, ulnar pathology (plastic deformation or fracture), carrying angle, head–neck ratio, any abnormal bony architecture, and any related condition. In 1967, Bado classified Monteggia lesion into four types, depending on the direction of the dislocation of the radial head and the angulation of the ulnar fracture.20 The directions of dislocation are anterior, posterior and lateral in types I, II and III respectively. Type IV is defined as a both-bone forearm fracture with dislocation of the radial head. According to the Bado Classification, in the current series the injuries were 7 type-I, 5 type-II, 1 type-III, and 5 type-1 equivalent (with concomitant radial head fracture).
Table 1.
The detailed information about demographical, and clinical properties.
| Case | Gender | Side | Age at operation (year:month) | Delay between injury and operation (weeks) | Carrying angle at follow-up (degrees) |
Bado type | Type of ulna fracture | Strategy | Surgical procedure | ROM |
Follow-up (months) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Injured arm |
Normal Arm |
||||||||||||||||
| Before surgery |
After surgery |
PS | FE | ||||||||||||||
| Injured arm | Normal arm | PS | FE | PS | FE | ||||||||||||
| 1 | M | L | 3:2 | 12 | 8 | 7 | 2 | Complete, transverse | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 90-0-80 | 140-0-5 | 80-0-80 | 130-0-0 | 90-0-80 | 140-0-5 | 48 |
| 2 | M | L | 10 | 4 | 11 | 10 | 1e | Plastic deformation | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 90-0-90 | 120-5-0 | 80-0-80 | 130-0-0 | 90-0-80 | 135-0-0 | 50 |
| 3 | F | L | 10 | 9 | 8 | 8 | 2 | Plastic deformation | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 70-0-80 | 120-0-0 | 45-0-70 | 150-0-5 | 90-0-100 | 145-0-5 | 56 |
| 4 | M | L | 12 | 14 | 10 | 10 | 1 | Complete, transverse | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 70-0-70 | 130-0-10 | 70-0-70 | 130-0-0 | 80-0-110 | 140-0-5 | 79 |
| 5 | M | R | 12:2 | 13 | 10 | 8 | 2 | Plastic deformation | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 70-0-80 | 120-5-0 | 90-5-0 | 120-5-0 | 95-0-100 | 135-0-0 | 84 |
| 6 | F | R | 6 | 7 | 16 | 12 | 1 | Complete, transverse | 1 | Open reduction, ulnar osteotomy (plate), transcapitellar k-wire, anular lig. reconst | 70-0-70 | 100-10-0 | 90-0-70 | 120-0-0 | 90-0-90 | 130-0-5 | 85 |
| 7 | M | R | 9:4 | 4 | 7 | 5 | 1 | Plastic deformation | 2 | Closed reduction, ulnar osteotomy (cross k-wire), transcapitellar k-wire | 90-0-90 | 130-0-5 | 90-0-90 | 130-0-0 | 90-0-90 | 130-0-0 | 51 |
| 8 | M | L | 6 | 7 | 17 | 7 | 2 | Complete, transverse (olecranon) | 2 | Closed reduction, ulnar osteotomy (cross k-wire), transcapitellar k-wire | 90-0-80 | 120-0-5 | 70-0-80 | 130-0-5 | 90-0-80 | 135-0-5 | 51 |
| 9 | M | R | 3:4 | 5 | 12 | 10 | 3 | Plastic deformation | 2 | Closed reduction, ulnar osteotomy (cross k-wire), transcapitellar k-wire | 90-0-80 | 130-0-10 | 70-0-80 | 140-0-0 | 90-0-90 | 140-0-0 | 52 |
| 10 | F | L | 3:6 | 6 | 11 | 10 | 1 | Complete, transverse | 2 | Closed reduction, ulnar osteotomy (cross k-wire), transcapitellar k-wire | 90-0-80 | 130-0-5 | 90-0-80 | 120-0-0 | 90-0-90 | 130-0-5 | 55 |
| 11 | M | R | 4 | 6 | 11 | 9 | 1 | Complete, transverse | 2 | Closed reduction, ulnar osteotomy (cross k-wire), transcapitellar k-wire | 80-0-70 | 140-0-90 | 80-0-80 | 155-0-10 | 80-0-100 | 140-0-5 | 58 |
| 12 | F | L | 10 | 4 | 10 | 8 | 1e | Complete, transverse | 3 | Open reduction, ulnar osteotomy (intramedullary k-wire), transcapitellar k-wire, radial head fixation with k-wire | 90-0-80 | 130-0-5 | 90-0-80 | 120-0-0 | 90-0-90 | 135-0-0 | 52 |
| 13 | F | R | 6 | 10 | 14 | 8 | 1e | Complete, transverse | 3 | Open reduction, ulnar osteotomy (intramedullary k-wire), transcapitellar k-wire, radial head fixation with k-wire | 80-0-80 | 140-0-5 | 80-0-90 | 130-0-0 | 80-0-90 | 135-0-5 | 75 |
| 14 | M | R | 9:2 | 9 | 8 | 6 | 1 | Complete, transverse | 4 | Closed reduction, ulnar osteotomy (plate) | 80-0-90 | 140-0-5 | 70-0-70 | 140-0-0 | 80-0-90 | 140-0-5 | 52 |
| 15 | F | L | 5.8 | 4 | 9 | 7 | 1e | Complete, transverse | 4 | Closed reduction, ulnar osteotomy (plate) | 30-0-40 | 100-0-0 | 60-0-70 | 120-30-0 | 70-0-90 | 130-0-5 | 57 |
| 16 | M | R | 5 | 9 | 9 | 5 | 1e | Plastic deformation | 4 | Closed reduction, ulnar osteotomy (plate) | 70-0-30 | 120-0-0 | 80-0-45 | 130-0-0 | 80-0-90 | 135-0-0 | 60 |
| 17 | M | R | 7:1 | 16 | 10 | 8 | 2 | Complete, transverse | 4 | Closed reduction, ulnar osteotomy (plate) | 90-0-45 | 120-0-0 | 80-0-80 | 130-0-5 | 80-0-90 | 130-0-0 | 68 |
| 18 | M | L | 2:6 | 10 | 12 | 10 | 1 | Complete, transverse | 4 | Closed reduction, ulnar osteotomy (plate) | 40-0-40 | 120-0-0 | 80-0-80 | 130-10-0 | 80-0-100 | 140-0-0 | 82 |
There were 4 different combinations of treatment strategies performed by 3 different surgeons for the missed Monteggia lesions of the children in this study. The treatment strategies included open or closed reduction of radiocapitellar joint with or without transcapitellar k-wire fixation and/or annular ligament reconstruction, and ulnar osteotomy fixed with cross k wires, intramedullary k-wire or plate. All these treatment strategies have been previously described in literature.2,4, 5, 6, 7,13 The strategies that we used are given in Table 1. If there was a plastic deformation or bony union of the ulna with acceptable angulation, the ulnar osteotomy was performed at the junction of distal 2/3 and proximal 1/3 of the ulna. If bony union of the ulna was not been completely achieved, the ulnar osteotomy was performed at the level of callus.
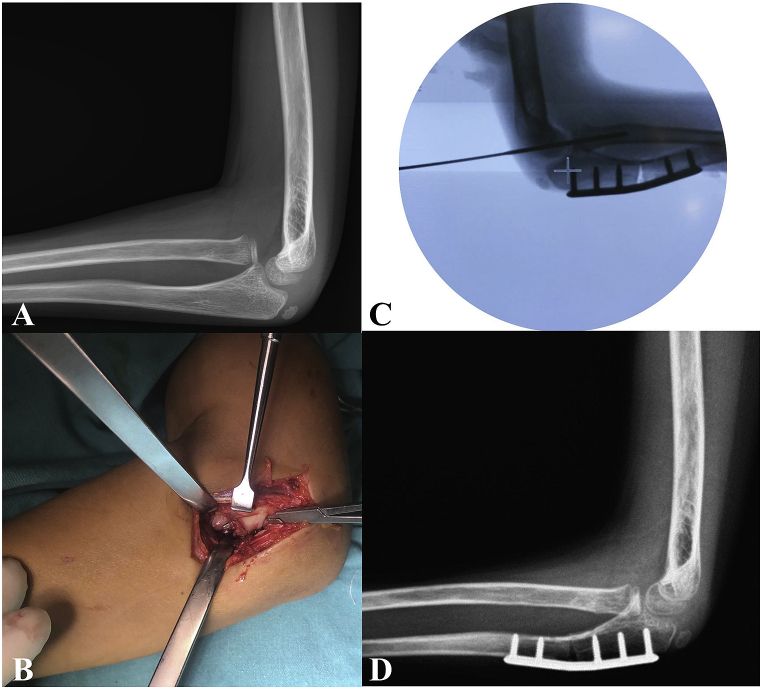
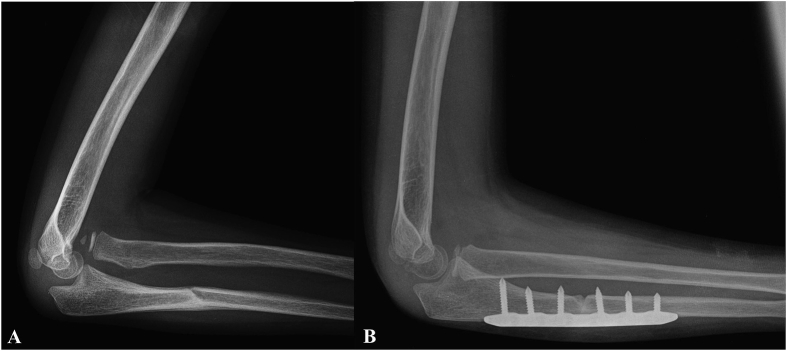
There were 3 different ulnar fixation methods of plate, cross k-wire and intramedullary k-wires that were preferred by the 3 different surgeons (Fig. 1). There was no requirement for bone grafting at the osteotomy site in any patient. The osteotomy site was angulated to overcorrect the ulnar deformity until easily closed reduction of the radial head (strategy 2 or 4) (Fig. 2), which was evaluated with fluoroscopy in all combinations of full flexion, extension, protonation and supination in both lateral and anteroposterior (AP) views. If the closed reduction was not achieved, open reduction of the radial head was performed (strategy 1 or 3). There was requirement for radial osteotomy, or neurolysis in any of the patients.
Fig. 1.
Case number 2. A, lateral radiograph of the left elbow was showing a Bado type 1 Monteggia injury. B, intraoperative image showed annular ligament as obstacle of radial head reduction. C, intraoperative fluoroscopy was confirmed good reduction of the radial head and overcorrection of ulnar osteotomy. The osteotomy site was angulated, and then rigidly fixed with a plate bent to the desired shape. D, postoperative boney union has been acquired at third month.
Fig. 2.
Case number 14. A, lateral radiograph of the right elbow was showing a Bado type 1 Monteggia injury. B, postoperative lateral radiograph of the right elbow at six month.
Patients, who had transcapitellar k-wire, were splinted with a long-arm plaster cast for 6 weeks, at which point the k-wire was removed and active range of motion was permitted. Physiotherapy was not recommended. At the final follow-up examination, clinical notes were taken about pain, stability, disturbance of daily and sporting activities, elbow and forearm range of motion. The functional status of the patients was evaluated with the Oxford Elbow Score (OES)21,22 at the time of the final follow-up examination. This questionnaire consists of 12 items with 5 response options. The items consist of assessment of elbow function, pain, and social-psychological status. Each assessment ranges from 0 to 100, where 100 is the best possible outcome. AP and lateral radiographs were taken to determine the congruence of the radiocapitellar joint, carrying angle and the presence of any deformity.
3. Results
The average follow-up period was 62 months (range, 48–85 months). The overall pre- and post-operative clinical and radiological data are shown in Table 1. All patients had a history of elbow or forearm trauma. Of the 18 referred injuries, 4 had misdiagnosis of isolated ulna fracture, and 14 had a missed Monteggia lesion without pre-diagnosis. Of the 18 injuries, 7 were classified as Bado type I, 5 as Bado type I equivalent (associated with radial head fracture), 5 as Bado type II, and 1 as Bado type III on the basis of radiographs made at the time of the injury.20 No patient had radial head deformity or osteoarthritic changes of the elbow at the time of surgery. There was no sign of distal radio-ulnar joint pathology.
OES was evaluated postoperatively at the final follow-up examination. The average functional score was 90, the average social-psychological score was 85, and the average pain score was 86. Parents assisted the children in completing the OES questionnaire evaluation. There was no statistical significance between the OES and time interval from injury to surgery, treatment strategy, or age at surgery.
The most common clinical finding was a substantial decrease in supination and extension compared to the normal arm. The postoperative average elbow flexion was 130.8° (range, 120°-155°), extension was −0.84° (range, −30°-10°), protonation was 77.5° (range, 45°-90°), and supination was 72° (range, 0°-90°). There was loss of postoperative elbow range of motion (ROM) in all directions compa to the normal elbow, the average loss was 7.8° in protonation, 19.7° in supination, 5.5° in flexion, and 1.7° in extension. Theredre was no statistically significant relationship between surgical strategy, postoperative elbow ROM, delayed time from injury to surgery, Bado classification, and carrying angle. There was an average increase of 2.5° in the carrying angle.
A detailed comparison of the treatment strategies applied to patients is given in Table 2. The highest ROM loss in supination and protonation compared to the normal extremity was seen in strategy 1, strategy 3 in flexion and strategy 4 in extension. The most loss of ROM in all the strategies was seen in supination. The most increase in carrying angle was found in strategy 2.
Table 2.
Comparison of the results of the treatment strategies.
| Number of patients | Average age (year:month) | Average increase in carrying angle (degree) | Average lost degree in ROM (injured arm compared to normal arm) (degree) |
Average follow up period (month) | ||||
|---|---|---|---|---|---|---|---|---|
| Pronation | Supination | Flexion | Extension | |||||
| Strategy 1 | 6 | 8:9 | 1.3 | 13.3 | 32.5 | 7.5 | 1.7 | 67 |
| Strategy 2 | 5 | 5:2 | 3.4 | 8 | 8 | 0 | 0 | 53.4 |
| Strategy 3 | 2 | 8 | 4 | 0 | 5 | 10 | 2.5 | 63.5 |
| Strategy 4 | 5 | 5:9 | 2.4 | 4 | 23 | 5 | 9 | 63.8 |
The average ROM loss in the injured arm compared to the normal arm was evaluated in all the strategies (Table 2). The maximum loss of average protonation was in strategy 1 with 13.3°, supination was also in strategy 1 with 32.5°, flexion was in strategy 3 with 10°, and extension was in strategy 4 with 9°.
The radiocapitellar joint was maintained in a completely reduced position and was stable in all patients at the final follow-up examination. In 5 patients with radial head fracture, union was obtained without any deformity and 2 of these patients had radial head hypertrophy. Reduction loss of the radiocapitellar joint was not observed in any patient, but mild osteoarthritic changes of the radiocapitellar joint were observed in 1 patient. With the exception of 2 patients, all the other patients had an increase in carrying angle compared with the contralateral elbow (Table 1).
All patients had union at the ulnar osteotomy site. There was no non-union or malunion in the ulnar osteotomy site, infection, k-wire migration or breakage, neurovascular or any other complication after surgery.
4. Discussion
Radial head resection has been used historically in missed Monteggia lesions in children.16,23 In late presenting cases, radial head resection can be performed after skeletal maturity as a salvage procedure.16,23 Most authors have stated that ulnar deformity is a key point in the reduction of the radiocapitellar joint.24,25 The reduction of the radiocapitellar joint is one of the most important goals in cases of missed Monteggia lesion. In the absence of reduction of the radiocapitellar joint, it will progressively undergo dysplastic changes leading to well-known long-term outcomes that may result in disability of the extremity.1,7,19 An increased time interval between the Monteggia lesion and reconstructive surgery may worsen the outcome. However, these injuries occur mostly in children who have a significant amount of growth remaining and high potential for remodeling.
The treatment strategies proposed here have been previously described in various papers.2,4, 5, 6, 7,13,26 Most of the strategies are aimed at correcting or overcorrecting ulnar malunion, which prevents reduction of the radial head. The surgical techniques consist of an ulnar osteotomy and different fixation methods, ulnar correction-overcorrection, and open or closed radial head reduction. The correction or overcorrection maintains the radial head in place. In some cases reduction of the radial head cannot be achieved by closed means, so in those cases, open reduction can be recommended to easily remove the obstruction, which is a remnant of the annular ligament interposed within the radiocapitellar joint. In this study, the results showed that the reconstruction of the annular ligament (in strategy 1) did not provide positive results to the extent expected, as in a previously published study.24 The reduction of the radiocapitellar joint was stable without such reconstruction (in strategy 2,3, and 4). As previously reported, this due to the need for more dissection for annular ligament reconstruction, which may cause elbow stiffness, heterotopic ossification, radio-ulnar synostosis, or avascular necrosis of the radial head.10,12,27 It is likely that elbow stiffness was the reason why strategy 1 did not produce better results than the other strategies. Radial head avascular necrosis, heterotopic ossification or radioulnar synostosis was not observed in any patient. Rodgers et al. stated that a short graft may result in tight constriction and thinning of the radial neck, and functional restriction after the Bell Tawse procedure.28 Lådermann et al. reported that if re-dislocation occurs, it may not be related to the absence of annular ligament reconstruction, but rather to a lack of angulation of the ulnar osteotomy.7
For stabilization of the radiocapitellar joint, transcapitellar k-wire may be used as an alternative to annular ligament repair, although complications such as breakage or migration of k-wires may occur in this technique. In the current series, no k-wire related complications were seen in strategies 1, 2 and 3.
Dysplastic changes were not seen any of the patients. This could be attributed to the time interval between injury and surgery of the patients in this study being relatively shorter than in previous studies.7,18,19
A variety of ulnar fixation methods have been described in literature, including Ilizarov, external fixator, plate, cross k-wire, intramedullary k-wire or a combination of these recommended techniques.5,6,8,9,13 All osteotomies in this study were internally fixed with plates, cross k-wires or intramedullary k-wire to minimize the risk of displacement. The external fixator might not have been well tolerated as this group of patients was mostly composed of children. As it is possible to obtain correction or over-correction in a single stage, progressive correction with external fixator may not be necessary.13,29 No bone grafting was used in this series. Grafting of the osteotomy line, which has been supported in previous studies,7,30,31 can be considered unnecessary in this population of children with very high union and remodeling potential. Bone union was obtained in all patients in this study. The prediction of remodeling of the ulna is difficult after osteotomy and fixation. Therefore, it is difficult to determine the center of rotation of angulation. For ulnar correction/overcorrection, some authors have recommended proximal ulnar osteotomy25,32 while others have recommended osteotomy at the ulna deformity site.6,11 In this study, if there was a plastic deformation or bony union of ulna, the ulnar osteotomy was performed at the junction of distal 2/3 and proximal 1/3 of the ulna, and if there was an ulna fracture with incomplete bony union, the ulnar osteotomy was performed at the level of callus.
Previous studies have used the Mayo Elbow Performance Index30,33 and Oxford Elbow Score24 in the postoperative clinical evaluation of missed Monteggia lesions. In the current study, the OES was used. There was no significant difference between the results of this study and the results of the Rahbek et al. study on the basis of OES.24 There was no statistically significant difference between the OES and time from injury to surgery, fixation techniques of ulnar osteotomy or age at surgery.
There were some limitations to this study, primarily that it was retrospective in design and there was no control group. Due to the rarity of the condition, there was a small group of patients in this study with no possibility of statistical study and the results include only mid-term functional outcomes. Moreover, there were different Bado types of injury in these patients.
According to our experience, the most important point is the reduction of the radial head rather than the type of surgery chosen for the management of missed Monteggia lesions. According to the results of this study, the preferred treatment strategy has no significant effect on the results as long as it provides radial head reduction. It can be considered that the best way to improve outcomes is that the surgeon should select the treatment strategy with which he is most familiar and has the most experience. Surgical correction of the deformity seems to result in excellent pain-free range of motion of the elbow, forearm, and wrist, with no pain or instability at the distal radioulnar joint in the mid-term follow-up. The long-term outcomes of such injuries require further observation.
Funding
None.
Ethical approval
The study was approved by the institutional review board at the Kartal Dr. Lütfi Kırdar Training and Research Hospital.
Level of evidence
IV.
Informed consent
Informed consent was obtained from all individual participants' parents included in the study.
Declaration of competing interest
The authors declare that they have no conflicts of interest concerning this article.
References
- 1.Bell Tawse A. The treatment of malunited anterior Monteggia fractures in children. J. Bone Joint Surg. Br. Vol. 1965;47(4):718–723. [PubMed] [Google Scholar]
- 2.Degreef I., De Smet L. Missed radial head dislocations in children associated with ulnar deformation: treatment by open reduction and ulnar osteotomy. J Orthop Trauma. 2004;18(6):375–378. doi: 10.1097/00005131-200407000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Devnani A. Missed Monteggia fracture dislocation in children. Injury. 1997;28(2):131–133. doi: 10.1016/s0020-1383(96)00160-x. [DOI] [PubMed] [Google Scholar]
- 4.Hui J.H., Sulaiman A.R., Lee H.-C., Lam K.-S., Lee E.-H. Open reduction and annular ligament reconstruction with fascia of the forearm in chronic Monteggia lesions in children. J Pediatr Orthop. 2005;25(4):501–506. doi: 10.1097/01.bpo.0000158812.37225.b3. [DOI] [PubMed] [Google Scholar]
- 5.Mehta S. Flexion osteotomy of ulna for untreated Monteggia fracture in children. Indian J Surg. 1985;47:15–19. [Google Scholar]
- 6.Wang Q., Du Mm, Pei Xj. External fixator‐assisted ulnar osteotomy: a novel technique to treat missed monteggia fracture in children. Orthop Surg. 2019 Feb;11(1):102–108. doi: 10.1111/os.12426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lädermann A., Ceroni D., Lefevre Y., De Rosa V., De Coulon G., Kaelin A. Surgical treatment of missed Monteggia lesions in children. J. Children's Orthopaedics. 2007;1(4):237–242. doi: 10.1007/s11832-007-0039-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ring D., Waters P.M. Operative fixation of Monteggia fractures in children. J. Bone Joint Surg. Br. Vol. 1996;78(5):734–739. [PubMed] [Google Scholar]
- 9.Bor N., Rubin G., Rozen N., Herzenberg J.E. Chronic anterior monteggia lesions in children: report of 4 cases treated with closed reduction by ulnar osteotomy and external fixation. J Pediatr Orthop. 2015;35(1):7–10. doi: 10.1097/BPO.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 10.Oner F., Diepstraten A. Treatment of chronic post-traumatic dislocation of the radial head in children. J. Bone Joint Surg. Br. Vol. 1993;75(4):577–581. doi: 10.1302/0301-620X.75B4.8331112. [DOI] [PubMed] [Google Scholar]
- 11.Kim H.T., Park B.G., Suh J.T., Yoo C.I. Chronic radial head dislocation in children, Part 2: results of open treatment and factors affecting final outcome. J Pediatr Orthop. 2002;22(5):591–597. [PubMed] [Google Scholar]
- 12.De H.B. Radial neck osteolysis after annular ligament reconstruction. A case report. Clin Orthop Relat Res. 1997;(342):94–98. [PubMed] [Google Scholar]
- 13.Hasler C., Von Laer L., Hell A. Open reduction, ulnar osteotomy and external fixation for chronic anterior dislocation of the head of the radius. J. Bone Joint Surg. Br. Vol. 2005;87(1):88–94. [PubMed] [Google Scholar]
- 14.Verneret C., Langlais J., Pouliquen J., Rigault P. Old post-traumatic dislocation of the radial head in children. Revue de chirurgie orthopedique et reparatrice de l'appareil moteur. 1989;75(2):77–89. [PubMed] [Google Scholar]
- 15.Belangero W., Livani B., Zogaib R. Treatment of chronic radial head dislocations in children. Int Orthop. 2007;31(2):151–154. doi: 10.1007/s00264-006-0153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tajima T., Yoshizu T. Treatment of long-standing dislocation of the radial head in neglected Monteggia fractures. J Hand Surg. 1995;20(3):S91–S94. doi: 10.1016/s0363-5023(95)80177-4. [DOI] [PubMed] [Google Scholar]
- 17.Kim H.T., Conjares J.N.V., Suh J.T., Yoo C.I. Chronic radial head dislocation in children, part 1: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop. 2002;22(5):583–590. [PubMed] [Google Scholar]
- 18.Chen W.-S. Late neuropathy in chronic dislocation of the radial head: report of two cases. Acta Orthop Scand. 1992;63(3):343–344. doi: 10.3109/17453679209154798. [DOI] [PubMed] [Google Scholar]
- 19.Jacobsen K., Holm O. Chronic Monteggia injury in a child. Ugeskr Laeger. 1998;160(28):4222–4223. [PubMed] [Google Scholar]
- 20.Bado J.L. 7 the monteggia lesion. Clin Orthop Relat Res. 1967;50:71–86. [PubMed] [Google Scholar]
- 21.Dawson J., Doll H., Boller I. The development and validation of a patient-reported questionnaire to assess outcomes of elbow surgery. J. Bone Joint Surg. Br. Vol. 2008;90(4):466–473. doi: 10.1302/0301-620X.90B4.20290. [DOI] [PubMed] [Google Scholar]
- 22.Dawson J., Doll H., Boller I. Comparative responsiveness and minimal change for the Oxford Elbow Score following surgery. Qual Life Res. 2008;17(10):1257–1267. doi: 10.1007/s11136-008-9409-3. [DOI] [PubMed] [Google Scholar]
- 23.Stoll T.M., Willis R.B., Paterson D. Treatment of the missed Monteggia fracture in the child. J. Bone Joint Surg. Br. Vol. 1992;74(3):436–440. doi: 10.1302/0301-620X.74B3.1587897. [DOI] [PubMed] [Google Scholar]
- 24.Rahbek O., Deutch S.R., Kold S., Søjbjerg J.O., Møller-Madsen B. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J. Children's Orthopaedics. 2011;5(6):449–457. doi: 10.1007/s11832-011-0372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bouyala J., Chrestian P., Ramaherison P. High osteotomy of the ulna in the treatment of residual anterior dislocation following Monteggia fracture (author's transl) Chir Pediatr. 1978;19(3):201–203. [PubMed] [Google Scholar]
- 26.Liao S., Pan J., Lin H. A new approach for surgical treatment of chronic Monteggia fracture in children. Injury. 2019 Jun;50(6):1237–1241. doi: 10.1016/j.injury.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Gyr B.M., Stevens P.M., Smith J.T. Chronic Monteggia fractures in children: outcome after treatment with the Bell–Tawse procedure. J Pediatr Orthop B. 2004;13(6):402–406. doi: 10.1097/01202412-200411000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Rodgers W., Waters P.M., Hall J.E. Chronic monteggia lesions in children.: complications and results of reconstruction. JBJS. 1996;78(9):1322–1329. doi: 10.2106/00004623-199609000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Exner G. Missed chronic anterior Monteggia lesion: closed reduction by gradual lengthening and angulation of the ulna. J. Bone Joint Surg. Br. Vol. 2001;83(4):547–550. doi: 10.1302/0301-620x.83b4.11103. [DOI] [PubMed] [Google Scholar]
- 30.Goyal T., Arora S.S., Banerjee S., Kandwal P. Neglected Monteggia fracture dislocations in children: a systematic review. J Pediatr Orthop B. 2015;24(3):191–199. doi: 10.1097/BPB.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 31.Hubbard J., Chauhan A., Fitzgerald R., Abrams R., Mubarak S., Sangimino M. Missed pediatric monteggia fractures. JBJS reviews. 2018;6(6) doi: 10.2106/JBJS.RVW.17.00116. e2-e2. [DOI] [PubMed] [Google Scholar]
- 32.Bouyala J., Bollini G., Jacquemier M. The treatment of old dislocations of the radial head in children by osteotomy of the upper end of the ulna. Apropos of 15 cases. Revue de chirurgie orthopedique et reparatrice de l'appareil moteur. 1988;74(2):173–182. [PubMed] [Google Scholar]
- 33.Nakamura K., Hirachi K., Uchiyama S. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. JBJS. 2009;91(6):1394–1404. doi: 10.2106/JBJS.H.00644. [DOI] [PubMed] [Google Scholar]