Abstract
Treatment for mandibular fractures is commonly performed via open reduction fixation with mini titanium or resorbable plates and screws. The investigators hypothesized differences in maximum mechanical stress forces and deflection with each plating material; however, it was proposed that the experimental forces withstood by the resorbable system would be enough to withstand normal forces produced during mastication.
The sample was composed of fresh cadaver mandibles that were harvested, fractured, and fixated with plates and screws. The predictor variable was fracture fixation and included a titanium plating or resorbable poly-L-lactide plating system. The primary outcome measure was maximum load withstood before plating failure measured in Newtons (N). Descriptive and bivariate statistics were computed, P value was set at .05.
The sample was composed of six mandibles with and grouped by type of fixation modality, Titanium (T) (n = 3) and Resorbable (n = 3). There was a statistically significant correlation between the T group and increased maximum load (N) before failure as compared to the R group, (P = 0.023).
The results suggest that fracture fixation with titanium plates and screws can withstand greater maximum forces before failure; however, the resorbable plating system withstood forces similar to/or greater than the maximum forces produced during normal mastication.
Keywords: Biomedical engineering, Dentistry, Materials science, Surgey, Resorbable plates, Titanium plates, Fracture, Fixation, Poly-l-lactic acid, Mandible
Biomedical engineering; Dentistry; Materials science; Surgey; Resorbable plates; Titanium plates; Fracture; Fixation; Poly-l-lactic acid; Mandible.
1. Introduction
When compared to other maxillofacial fractures, mandible fractures are the most common after nasal fractures with an incidence of approximately 38% [1]. Common ways that the mandible can become fractured is through either assault (most common), motor vehicle accidents, falls, and sports [1]. Treatment for mandibular fractures is commonly performed via open reduction fixation with mini titanium or resorbable plates and screws.1 Historically, the first documented use of metal plating for a facial fracture surgical procedure was in 1945 [2]. Shortly thereafter, the metal known as titanium began making its way into the operating rooms of physicians and dentist with high rates of success [3].
The operational benefits of titanium have made it an excellent material for surgical processes. Titanium is very easy to handle, does not have bulky dimensional change, causes less scatter during computed tomography (CT) scanning, has no displacement during magnetic resonance imaging (MRI), and has incredible tensile strength and rigidity [4, 5, 6]. Nonetheless, there are a few disadvantages when using titanium for things like mandibular fixations such as the need for a second surgery to remove the plate, increase risk for bisphosphonate-related osteonecrosis, impact of facial growth, titanium particles found in scar tissue, sensitivity to temperatures, and possible stress-shielding [4, 7].
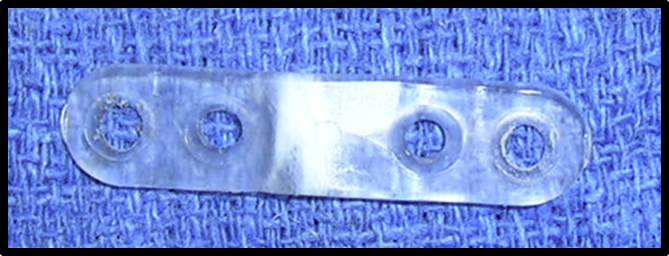
To combat some of the adverse effects of titanium, a biological resorbable material made from polylactic acid was created. The first study that looked at the potential of this resorbable material was in 1966 when Kulkarni et al. implanted guinea pigs and rats with poly L (+) lactic acid (Figure 1) [8]. The polylactic acid was discovered to be nontoxic, non-tissue reactive, did not accumulate in vital organs, and had a slow degradation process, making it an ideal candidate for surgical implants [8]. It was not until 1971 when the first reported surgical facial fracture procedure utilized resorbable materials [9]. Since then, polylactic acid and the several generations of modified polymeric plates and screws have been used more and more in surgical practices due to their positive benefits.
Figure 1.
Typical resorbable poly-L-lactide plate used during this study.
The effectiveness of resorbable plates and screws for surgical fixation of bone fractures is attributed to its unique abilities such as promoting osteoconductivity, radiolucency, no metal accumulation, non-corrosive, decreases in pain, decreases in stress-shielding, possible decreases in post-surgical infection rates, and reduction in the need for a second surgery to remove the plates and screws [4, 6, 7, 10]. However, resorbable materials are not without their limitations. Compared to titanium plates and screws, polylactic acid is less stable, has decreased mechanical strength, takes months to years to fully biodegrade, has increased refracture rates, and presents with possible inflammatory tissue responses similar to that of a bacterial infection [4, 10].
The purpose of this pilot study was to compare mechanical stress forces and deflection on the traditional titanium plating and screw system versus resorbable poly-L-lactide plates and screws when used in mandibular fracture fixation. We hypothesize differences in maximum mechanical stress forces and deflection with each plating material; however, we propose that the experimental forces withstood by the resorbable system will be enough to withstand normal forces produced by muscles used in mastication. In this report, we identify differences between the maximum forces between the titanium and resorbable groups. Affirmation of the differential maximum force responses within the plated fractures has the potential to serve as a foundation for paving the way for resorbable poly-L-lactide plates and screws as being a more viable standard of treatment for mandibular fracture fixation.
2. Materials and methods
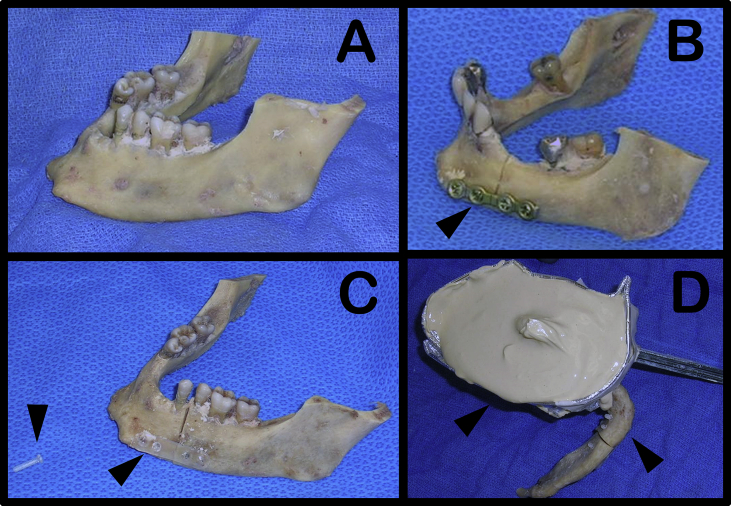
This pilot study was exempt from the Vanderbilt University Institutional Review Board. A sample size of six fresh (1-2-weeks-old) cadaver mandible specimens (Figure 2A) were harvested from the Anatomical Donation Program at Vanderbilt University Medical Center fulfilling all procedural requirements. An approximate 90° osteotomy was performed through the alveolus and body of each mandible and then fixated with either titanium midface plates (1.5mm thickness, Stryker CMF, Freiburg, Germany) or resorbable poly-L-lactide plates and screws (Stryker) (Figure 2B,C). Each mandible, regardless of the material used, had at a minimum two screws placed into the distal and proximal segments of the fracture on the mandibular body.
Figure 2.
(A) Freshly harvested mandible prior to 90° osteotomy. (B) Osteosynthesis, after 90° osteotomy, utilizing a titanium plate and screws. (C) Osteosynthesis utilizing poly-L-lactic resorbable plate and screws (shown by black arrows). (D) Mandible sample being cast into plaster mixture to keep the sample stationary once it was attached to the MTS Bionix 858 multipurpose servohydraulix machine.
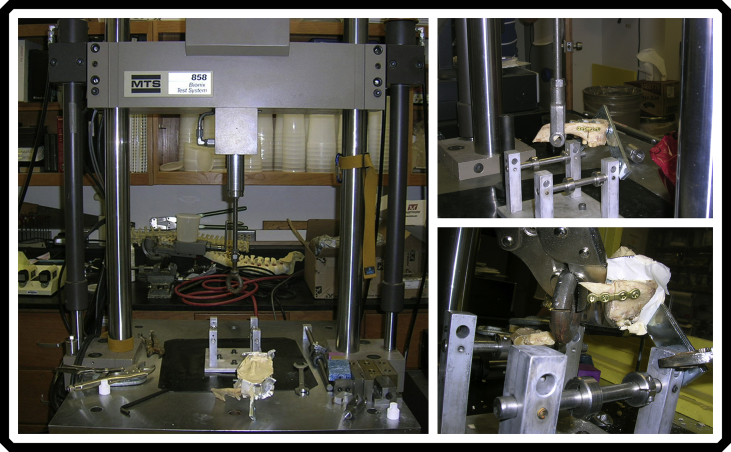
Once the mandibles were plated with their respective material, the non-plated side of the mandible was cast into a plaster mixture so that the plated side was still exposed (Figure 2D) and the entire sample was stationary. The plated and casted mandible samples were then attached to a MTS Bionix 858 multipurpose servohydraulix machine (Figure 3) which allowed the osteotomy sites to be cyclically loaded to assess their deflection and were stressed to failure. All mandibles were loaded in similar anatomic sites; however, distances and angles where the MTS Bionix machine applied maximum force to each mandible varied to some extent due to the slight differences in mandible sizes. The MTS Bionix was programmed to steadily move the mandibular samples until the forces measured 10 Newtons (N) and a deflection measurement in millimeters (mm) was recorded. The same process was used only one other time to evaluate the force (N) at deflection failure (mm), the maximum load (N), and where exactly the failure site took place on each sample.
Figure 3.
Different views of the MTS Bionix 858 multipurpose servohydraulix machine with a titanium group mandible sample being mechanically stressed to failure.
2.1. Statistical analysis
Assuming unequal variances, a Welch's t-test was used to determine statistical significance of initial deflection under a 10 Newtons (N) load, the deflection failure (mm), and maximum load (N) between the titanium (T) and resorbable (R) groups.
3. Results
Six mandible test subjects, each with one of two types of fixation modality (titanium or resorbable) were biomechanically stressed and evaluated. The initial deflection under a 10 Newtons (N) load, the deflection failure, failure site, and max load were measured and are presented in Table 1. The overall mean and median age of the mandibular samples was 84.5 years with the youngest being 65 years and the oldest being 96 years. The mean age of the T and R groups was 87+/-6 years and 82+/-12 years, respectively. Other demographics of this sample include 4 of the mandibles being male, and 2 were female; along with 4 having dentition present and 2 without dentition.
Table 1.
Population demographics with maximum values obtained for each sample.
| Patient Number | Plate Material | Age (yr) | Sex | Dentition | Deflection 10 N Load (mm) |
Deflection Fail (mm) |
Fail Site | Maximum Load (N) |
|---|---|---|---|---|---|---|---|---|
| 1 | Titanium | 83 | M | Present | 0.034 | 7.777 | Bone | 389.7 |
| 2 | Titanium | 83 | M | Absent | 0.780 | 10.710 | Bone | 331.7 |
| 3 | Titanium | 96 | F | Present | 0.062 | 9.590 | Bone | 272.4 |
| 4 | Resorbable | 65 | M | Present | 0.161 | 7.410 | Screw | 260.5 |
| 5 | Resorbable | 94 | M | Absent | 0.016 | 8.350 | Screw | 135.0 |
| 6 | Resorbable | 86 | F | Present | 0.196 | 2.620 | Screw | 140.5 |
When placed under a starting load of 10 N, the amount of deflection in millimeters (mm) varied among each of the subjects, with the T group having the most initial deflection at 0.780 mm and the R group having the least initial deflection at 0.016 mm. The mean for this initial 10 N load in the T and R groups were 0.292+/-0.345 mm and 0.124+/-0.078 mm, respectively (Table 2). No statistical significance in initial deflection was found during the initial 10 N starting load (P = 0.286) (Table 2).
Table 2.
Group statistical evaluation of values obtained.
| Group | n | Mean | SD | Maximum | Minimum | Welch's T Test P |
|
|---|---|---|---|---|---|---|---|
| Maximum Load (N) | T | 3 | 331.3 | 47.9 | 389.7 | 272.4 | 0.023 |
| R | 3 | 178.7 | 57.9 | 260.5 | 135.0 | ||
| Deflection Fail (mm) | T | 3 | 9.359 | 1.480 | 10.710 | 7.777 | 0.100 |
| R | 3 | 6.127 | 3.073 | 8.350 | 2.620 | ||
| Deflection 10 N Load (mm) | T | 3 | 0.292 | 0.345 | 0.780 | 0.034 | 0.286 |
| R | 3 | 0.124 | 0.078 | 0.780 | 0.016 | ||
| Age | T | 3 | 87 | 6 | 96 | 83 | |
| R | 3 | 82 | 12 | 94 | 63 |
SD = Standard Deviation.
While biomechanical stress was further applied to the T and R groups, the mean deflection failure between the two groups was observed. The overall mean for the deflection failure was 7.743+/-2.548mm. The T group mean was measured to be 9.359+/-1.208 mm and R was 6.127+/-2.509 mm (Table 2). The minimum deflection recorded upon failure was seen in the R group at 2.620 mm while the maximum deflection was witnessed to be 10.710 mm found in the T group; with no significant association between the T and R groups when measuring deflection failure (P = 0.100) (Table 2).
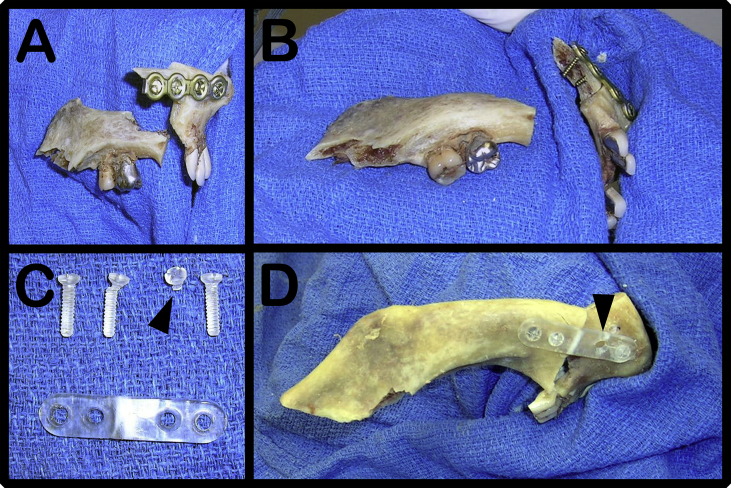
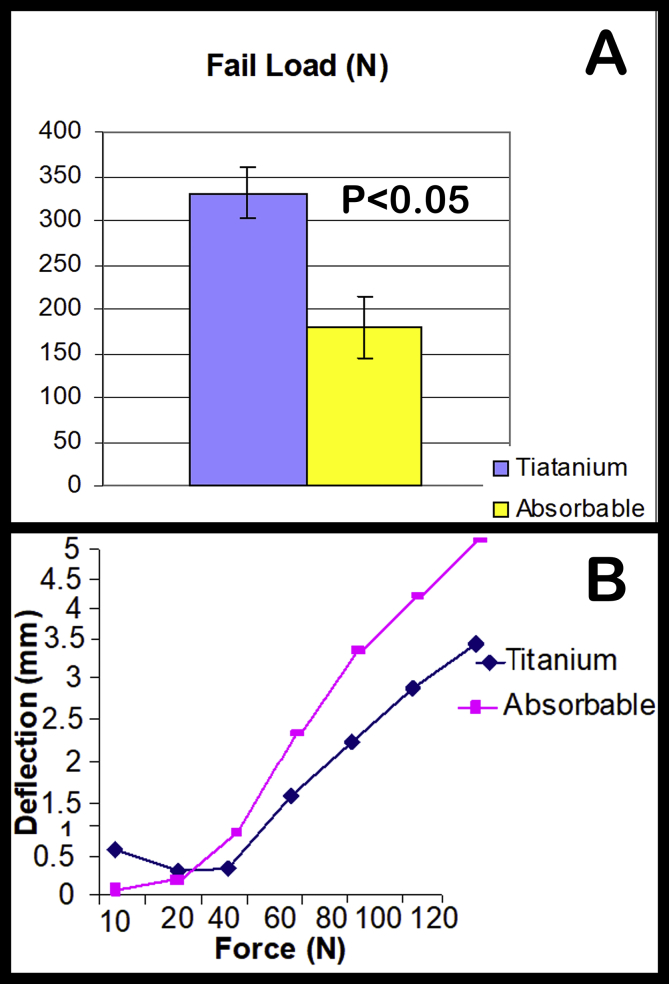
At the point when the groups were stressed under a maximum load (N), there were two different points of failure within the fixation system. The failure sites were either found at the location of the bone itself (Figure 4A,B) or the actual screws that fixated the plate to the bone (Figure 4C,D). The T group all had a bone failure site compared to the R group that all had screw failure sites. The overall mean maximum loads the two groups were able to withstand was 255.0+/-93.0 N with the lowest being 135.0 N and the greatest being 389.7 N. The mean max load of the T and R groups was 331.3+/-47.9 N and 178.7+/-57.9 N, respectively. The peak load the T group was able to withstand before bone failure was 389.7 N, which led to a 7.777 mm deflection before failure (Figure 5A,B). The highest max load the R group was able to withstand before screw failure was 260.5 N, which led to a 7.41 mm deflection before failure (Figure 5A,B). There was a significant association between the maximum load on the plated mandibles and the type of plate used (P = 0.023).
Figure 4.
(A–B) Demonstrates mandibular fracture fixation with titanium plating system and the failure point being at the mandible bones itself during mechanical stress testing. (C–D) Demonstrates mandibular fracture fixation with poly-L-lactic resorbable plating system and the failure point being at the screw during mechanical stress testing.
Figure 5.
(A) Mean maximum force values obtained for each group with a statistical significance of P < 0.05. (B) Force values obtained for specific displacement values.
4. Discussion
Titanium plating systems have been the gold standard for mandibular fracture fixation for almost 75-years; yet, there are still many disadvantages to this procedure. Alternatively, literature and surgical practices have shown that the resorbable poly-L-lactic plating systems have the capacity to compensate for the deficiencies of titanium while still withstanding normal to high mandibular forces during mastication and speech. One of the greatest disadvantages the titanium plating system has been shown to produce is the potential need for a secondary surgery to remove the device.
Unfortunately, postoperative complications after removal of the titanium plates include increased risk for re-fracture, malunion, nonunion, facial asymmetry, occlusal derangement, and impaired mouth opening [11]. On the other hand, the biodegradable properties of the resorbable plating system mitigates the need for a secondary surgery due to their capability of being resorbed over a period ranging from 2 to 5 years [4]. Furthermore, resorbable plates are radiolucent; thus, full visibility of the fracture site is available to the clinician. When used to stabilize bone fixation reconstruction of larger defects, the radiolucent property may enable the surgeon to see the progress of the bone graft more easily compared to titanium plating devices which do not allow the full visualization of the fracture site on postoperative radiographs [12]. Additionally, resorbable plates demonstrated a decreased incidence of infection and tissue inflammation, as illustrated in Lopez et al., which detailed that only 4 of 443 resorbable plating fixation surgeries became infected compared to a study by Taylan et al., which established that 2 of 19 titanium plating fixation surgeries were infected while none of the resorbable plating systems became infected [13, 14]. However, resorbable plates are not without their own complications. According a study by Sukegawa et al., of the 87 people who had maxillofacial surgery done with poly-L-lactic acid plate system, 10 (11.5%) showed increased incidences of postoperative plate exposure while not increasing risk for nonunion, infection, swelling, or malunion [15].
Our study directly compared the differences in maximum mechanical stress forces and deflection with each plating material and we proposed that the experimental forces withstood by the resorbable system would be enough to withstand normal forces produced by muscles used in mastication. The limitations of this study are the sample sizes for each group and the mechanical stress forces were applied in an ex vivo environment where the biodegradation process of the resorbable plating system was not accounted for within force and displacement measurements. The results of our study did affirm that titanium plates and screws can withstand greater maximum forces before failure; additionally, the poly-L-lactic plating system was able to withstand forces similar to forces produced in males and females during normal mastication. This potential mastication force dilemma could be effectively resolved if we were to adapt the resorbable plating system to include voluntary maxillomandibular fixation or other temporary limitations on chewing. It is also worth noting that the failure point in the resorbable plating system was the poly-L-lactic screws and not the plate itself. New technology is becoming available for new methods of adhering resorbable plates to bone such as the Rapidsorb Injectable Polymer System which eliminates the need for screws and injects the resorbable material into the bone to tack down the resorbable plate.
Further investigations into the maximum mechanical strength of different resorbable plate adherence methods along with greater sample sizes would help further potential of resorbable poly-L-lactide plating systems becoming a more viable standard of treatment for mandibular fracture fixation.
5. Conclusion
In conclusion, differences in maximum mechanical stress forces and deflection with each plating material found that the experimental forces withstood by the resorbable system was similar to normal forces produced by muscles used in mastication. Preliminary titanium plating systems findings did present with a significant association between the maximum load (N) withstood compared to the resorbable plating systems. However, there was not a significant association when comparing the deflection 10 N load and deflection failure in millimeters (mm). Although the maximum load that the resorbable plating system was able to withstand was not equal to the forces that were measured with titanium, the benefits of resorbable plating systems does offer a solid foundation to providing a potentially better prognostic surgical approach with mandibular fracture fixation. Increased sample numbers will be required to confirm this notion.
Declarations
Author contribution statement
Brady Burns, Joseph-Michael Fields, Angel Farinas, Alonda Pollins, Galen Perdikis: Analyzed and interpreted the data; Wrote the paper.
Wesley Thayer: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
Special thanks to Dr. Lillian Nanney.
References
- 1.Oruç M., Işik V.M., Kankaya Y., Gürsoy K., Sungur N., Aslan G. Analysis of fractured mandible over two decades. J. Craniofac. Surg. 2016;27:1457–1461. doi: 10.1097/SCS.0000000000002737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts W.R. The case for mandibular plating. Br. J. Oral Surg. 1964;1:200–204. doi: 10.1016/s0007-117x(63)80072-4. [DOI] [PubMed] [Google Scholar]
- 3.Jorge J.R.P., Barão V.A., Delben J.A., Faverani L.P., Queiroz T.P., Assunção W.G. Titanium in Dentistry: historical development, state of the art and future perspectives. J. Indian Prosthodont. Soc. 2013;13:71–77. doi: 10.1007/s13191-012-0190-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanno T., Sukegawa S., Furuki Y., Nariai Y., Sekine J. Overview of innovative advances in bioresorbable plate systems for oral and maxillofacial surgery. Jpn. Dent. Sci. Rev. 2018;54:127–138. doi: 10.1016/j.jdsr.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim Y.H., Choi M., Kim J.W. Are titanium implants actually safe for magnetic resonance imaging examinations? Arch. Plast. Surg. 2019;46:96–97. doi: 10.5999/aps.2018.01466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim H.-Y., Jung C.-H., Kim S.-Y., Cho J.-Y., Ryu J.-Y., Kim H.-M. Comparison of resorbable plates and titanium plates for fixation stability of combined mandibular symphysis and angle fractures. J. Korean Assoc. Oral Maxillofac. Surg. 2014;40:285–290. doi: 10.5125/jkaoms.2014.40.6.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park Y.-W. Bioabsorbable osteofixation for orthognathic surgery. Maxillofac. Plast. Reconstr. Surg. 2015;37:6. doi: 10.1186/s40902-015-0003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kulkarni R.K., Pani K.C., Neuman C., Leonard F. Polylactic acid for surgical implants. Arch. Surg. 1966;93:839–843. doi: 10.1001/archsurg.1966.01330050143023. [DOI] [PubMed] [Google Scholar]
- 9.Cutright D.E., Hunsuck E.E., Beasley J.D. Fracture reduction using a biodegradable material, polylactic acid. J. Oral Surg. 1971;29:393–397. [PubMed] [Google Scholar]
- 10.Sukegawa S., Kanno T., Katase N., Shibata A., Takahashi Y., Furuki Y. Clinical evaluation of an unsintered hydroxyapatite/poly-l-lactide osteoconductive composite device for the internal fixation of maxillofacial fractures. J. Craniofac. Surg. 2016;27:1391–1397. doi: 10.1097/SCS.0000000000002828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anyanechi C.E., Saheeb B.D. Complications of mandibular fracture: study of the treatment methods in Calabar, Nigeria. W. Indian Med. J. 2014;63:349–353. doi: 10.7727/wimj.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laughlin R.M., Block M.S., Wilk R., Malloy R.B., Kent J.N. Resorbable plates for the fixation of mandibular fractures: a prospective study. J. Oral Maxillofac. Surg. 2007;65:89–96. doi: 10.1016/j.joms.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 13.Lopez J., Siegel N., Reategui A., Faateh M., Manson P.N., Redett R.J. Absorbable fixation devices for pediatric craniomaxillofacial trauma: a systematic Review of the literature. Plast. Reconstr. Surg. 2019;144:685–692. doi: 10.1097/PRS.0000000000005932. [DOI] [PubMed] [Google Scholar]
- 14.Taylan Filinte G. The dilemma of pediatric mandible fractures: resorbable or metallic plates? Turkish J. Trauma Emerg. Surg. 2015;21:509–513. doi: 10.5505/tjtes.2015.23922. [DOI] [PubMed] [Google Scholar]
- 15.Sukegawa S., Kanno T., Matsumoto K., Sukegawa-Takahashi Y., Masui M., Furuki Y. Complications of a poly-l-lactic acid and polyglycolic acid osteosynthesis device for internal fixation in maxillofacial surgery. Odontology. 2018;106:360–368. doi: 10.1007/s10266-018-0345-6. [DOI] [PubMed] [Google Scholar]