Abstract
Background: Older adults frequently report a preference to “trial” intubation and mechanical ventilation (MV) if faced with life-threatening respiratory failure. Understanding the anticipated outcome of unplanned MV is key to structuring a time-limited trial of treatment.
Objective: To characterize the time-to-death (TTD) among adults 65 years of age and older, who undergo emergency intubation and MV.
Design: Retrospective cohort study.
Setting/Subjects: All patients 65 years of age and older, who underwent emergency department (ED) intubation from 2008 to 2015, from 417 hospitals were included.
Measurements: The primary outcome was TTD after emergency intubation.
Results: We identified 41,463 ED encounters. The median TTD was three days (interquartile range, IQR, 1–8). There was a statistically significant change in the median TTD by age decile, with the shortest TTD, two days, in the oldest age group (p < 0.001). TTD was shortest among those with myocardial infarction (one day, IQR 4) and sepsis (two days, IQR 5). Bivariate analysis comparing TTD by Charleston Comorbidity Index (CCI) revealed a trend of increasing TTD with increasing CCI score among decedents. Patients with a CCI of 0 had a median TTD of one day (IQR 4), whereas the median TTD among those with a CCI >4 was four days (IQR 9).
Conclusions: In a large, nationally representative cohort of older adults undergoing ED intubation, the median time from intubation to death was short; however, the length of time between intubation and death varied considerably by principal diagnosis. This information will help guide providers' prognostication after emergency intubation and enhance serious illness conversations by informing expectations.
Tweet: Thirty-five percent of older adults die after ED intubation—most only survive two or three days after intubation.
Keywords: critical care, decision making, geriatrics, mechanical ventilation, prognosis, time-limited trial
Introduction
Nearly 70% of older adults report that they prioritize quality of life over longevity,1 yet the use of high-intensity medical interventions toward the end of life has been increasing.2 Between 2001 and 2011, the proportion of critically ill older adults treated with intubation and mechanical ventilation (MV) rose by 30% and the rate is predicted to double by 2020.3 Unfortunately, outcomes for these patients are poor: 35%–40% die in the hospital, and among hospital survivors, 60% face significant reductions in functional status and less than a third return home.4 While understanding patient preferences for treatment is key to avoiding undesirable, aggressive treatments,5 transforming a given patient's preference for “quality” over “quantity” into a specific treatment decision is challenging, particularly in the context of acute respiratory failure. In fact, many older adults would elect for a “trial” of intubation and MV if faced with acute respiratory failure.6,7
Understanding the anticipated prognosis is key to providing expectations to families after emergency intubation of older adults. Specifically, having an estimate of the length of time in which a patient is at higher risk of death after emergency intubation and death can help providers guide family expectations. However, data regarding the outcomes after emergency intubation among older adults are limited to studies focused on specific clinical conditions such as dementia3,8 or cancer,9 and utilize data that are now 10–20 years old.3,8 No study has focused on the time-to-death (TTD) among the estimated 30% of older adults undergoing emergency intubation, who do not survive hospitalization.
The objective of this study is to further characterize TTD among adults older than 65, who undergo emergency intubation and MV. This information will help guide providers' prognostication after emergency intubation and enhance serious illness conversations by informing expectations.
Methods
Data for this investigation came from the Vizient Clinical Data Base/Resource Manager™ (CDB/RM™), an individual-level administrative database from a consortium of 117 academic medical centers and over 300 affiliated hospitals across the United States.10 Using data from 2008 to 2015, we identified all emergency department (ED) encounters of patients 65 years of age and older, who required ED intubation, determined by procedure codes for intubation (CPT 31500). Patients were included in the analysis whether they died in the ED or were admitted to the hospital. Encounters with principal hospital diagnosis code(s) for trauma and cardiac arrest were excluded, given that the natural history of these disease processes is often determined by powerful confounders, such as the use of targeted temperature management, which we would not be able to measure in this administrative database.11,12 Patients receiving out-of-hospital intubation were also excluded.
Data included patient demographic information, procedure codes, diagnosis codes, length of stay (LOS), and in-hospital mortality. Our primary outcome was TTD after ED intubation measured in median number of days and interquartile ranges (IQR). Encounters with missing data for the outcome (death) were excluded from the analysis. A priori predictor variables for the primary outcome included the following: age, principal hospital diagnosis, and Charlson Comorbidity Index (CCI) score. Bivariate associations between each variable and the primary outcome were analyzed using chi-square analysis. The Strobe Guidelines for reporting cohort studies were followed.13 This study was approved by the hospital's institutional review board.
Results
We identified 41,463 ED encounters of patients 65 years of age or older, who underwent nontraumatic ED intubation. There were no missing data on the primary outcome (in-hospital death). There were 6427 patients with missing data for the principal diagnosis, leaving a total of 35,036 patients for that analysis. Just over half of the patients were female (54%). The majority were >75 years of age (54%) and white (64%). Nearly half of patients were 65–74 years of age and only 7% were >90 years of age. Overall hospital mortality was 35%; however, for those older than 90, mortality was 50% (Table 1).
Table 1.
Baseline Characteristics
| All, N = 41,463, N (%) | Decedents, n (%) | Survivors, n (%) | p* | |
|---|---|---|---|---|
| 14,512 (35) | 25,951 (65) | |||
| Age | <0.001 | |||
| 65–74 | 18,901 (45.6) | 5399 (28.6) | 13,502 (71.4) | |
| 75–79 | 7708 (18.6) | 2624 (34.0) | 5084 (66.0) | |
| 80–84 | 6877 (16.6) | 2760 (40.1) | 4117 (59.9) | |
| 85–89 | 5167 (12.5) | 2220 (43.0) | 2947 (57.0) | |
| ≥90 | 2810 (6.8) | 1390 (49.5) | 1420 (50.5) | |
| Sex | 0.53 | |||
| Male | 21,245 (51.2) | 7397 (34.8) | 13,848 (65.2) | |
| Female | 20,208 (48.7) | 6991 (34.6) | 13,217 (65.4) | |
| Race | <0.001 | |||
| White | 26,471 (63.8) | 9537 (36.0) | 16,934 (64.0) | |
| Black | 9718 (23.4) | 2936 (30.2) | 6782 (69.8) | |
| Other | 5284 (12.7) | 1920 (36.4) | 3354 (63.6) | |
| Principal diagnosis (N = 35,036) | <0.001 | |||
| Sepsis | 11,952 (33.2) | 5136 (42.9) | 6836 (57.1) | |
| Respiratory failure | 9297 (26.5) | 2069 (22.3) | 7228 (77.8) | |
| Cerebrovascular disease | 5460 (15.6) | 3016 (55.2) | 2444 (44.8) | |
| Myocardial infarction | 1801 (5.1) | 774 (43.0) | 1027 (57.0) | |
| Epilepsy and convulsions | 1219 (3.5) | 77 (6.3) | 1142 (93.7) | |
| Pneumonia | 848 (2.4) | 265 (31.3) | 583 (68.8) | |
| Congestive heart failure | 799 (2.3) | 195 (24.4) | 604 (75.6) | |
| Aspiration pneumonitis | 755 (2.2) | 219 (29.0) | 536 (71.0) | |
| COPD | 598 (1.7) | 82 (13.7) | 516 (86.3) | |
| Cardiac dysrhythmias | 485 (1.4) | 162 (33.4) | 323 (66.6) | |
| Charlson Comorbidity Index | <0.001 | |||
| 0 | 4032 (9.7) | 1264 (31.4) | 2768 (68.7) | |
| 1–2 | 16,277 (39.3) | 5699 (35.0) | 10,578 (65.0) | |
| 3–4 | 12,730 (30.7) | 4283 (33.6) | 8447 (66.4) | |
| >4 | 8424 (20.3) | 3147 (37.4) | 5277 (62.6) |
p-Value based on Kruskal-Wallis testing.
The median TTD was three days (IQR 1–8). The median TTD was three days among those 65–74 years of age (IQR 1–8), 75–79 years of age (IQR 1–8), and 85–89 years of age (IQR 1–7). The median TTD was two days among those 80–84 years of age (IQR 1–7) and those >90 years of age (IQR 1–6). These differences were statistically significant, showing a trend of shortest TTD in the oldest age group (p < 0.001) (Table 2).
Table 2.
Length of Stay Among Decedents and Survivors
| LOS in days, median (IQR) |
||||
|---|---|---|---|---|
| All, n = 41,463 | Decedentsa | Survivorsb | p* | |
| 3 (1–8) | 9 (5–15) | |||
| Age | <0.001 | |||
| 65–74 | 8 (4–14) | 3 (1–8) | 9 (5–15) | |
| 75–79 | 7 (3–13) | 3 (1–8) | 9 (6–15) | |
| 80–84 | 7 (3–12) | 2 (1–7) | 9 (6–15) | |
| 85–89 | 7 (2–12) | 3 (1–7) | 9 (6–14) | |
| ≥90 | 5 (2–0) | 2 (1–6) | 8 (5–12) | |
| Principal diagnosis | <0.001 | |||
| Sepsis | 8 (3–15) | 3 (1–9) | 11 (7–18) | |
| Respiratory failure | 7 (4–12) | 4 (1–8) | 8 (5–12) | |
| Cerebrovascular disease | 5 (1–12) | 2 (1–5) | 11 (5–19) | |
| Myocardial infarction | 5 (1–11) | 1 (1–4) | 9 (5–15) | |
| Epilepsy and convulsions | 6 (4–10) | 9 (5–13) | 6 (4–10) | |
| Pneumonia | 9 (5–14) | 6 (2–12) | 10 (6–14) | |
| Congestive heart failure | 8 (4–13) | 4 (1–12) | 8 (5–13) | |
| Aspiration pneumonitis | 8 (5–14) | 5 (1–10) | 9 (6–14) | |
| COPD | 7 (5–11) | 6 (2–11) | 8 (5–12) | |
| Cardiac dysrhythmias | 6 (2–11) | 2 (1–4) | 9 (5–13) | |
| Charlson Comorbidity Index | <0.001 | |||
| 0 | 6 (2–11) | 1 (1–5) | 8 (4–14) | |
| 1–2 | 7 (3–12) | 2 (1–7) | 8 (5–14) | |
| 3–4 | 8 (4–14) | 3 (1–8) | 10 (6–16) | |
| >4 | 8 (4–14) | 4 (1–10) | 10 (6–16) | |
p-Value based on Kruskal-Wallis testing.
LOS for decedents is time-to-death.
LOS for survivors is time-to-discharge.
IQR, interquartile range; LOS, length of stay.
When evaluating TTD by primary hospital diagnosis, TTD was shortest among those with myocardial infarction (one day, IQR 1–4), cerebrovascular accident (two days, IQR 1–5), and cardiac dysrhythmia (two days, IQR 1–4). The two most common diagnoses, sepsis (43%) and respiratory failure (22%), had a TTD of three and four days, respectively (Table 2). Patients with principal diagnosis of seizure had the longest median TTD (nine days, IQR 5–13). Among survivors of ED intubation, hospital stays were over a week long (nine days, IQR 5–15).
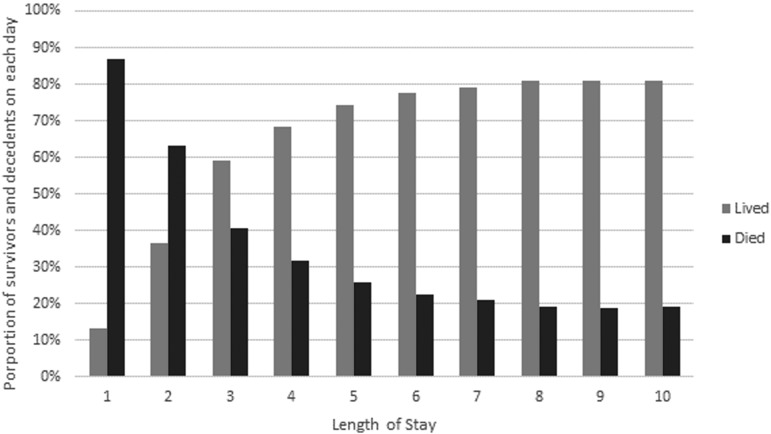
Overall, the probability of dying diminishes with each day of survival (Fig. 1). For instance, nearly 90% of those with an LOS of only one day are decedents, whereas among those with an LOS of eight days, only 18% are decedents. Paradoxically, bivariate analysis comparing TTD by Charleston Comorbidity Index (CCI), revealed a trend of increasing TTD with increasing CCI score. Patients with a CCI of 0 had a median TTD of one day (IQR 1–5), whereas the median TTD among those with a CCI of 1–2 was two days (IQR 1–7), versus three days (IQR 1–8) among those with CCI of 3–4 and four days (IQR 1–10) among those with CCI of >4. A similar trend was seen among hospital survivors: those with higher CCI scores had longer median hospital LOS (Table 2).
FIG. 1.
Survival outcomes each day after hospital presentation.
Discussion
In a large, nationally representative cohort of older adults undergoing emergent intubation and invasive MV, the median time from intubation to death was short; however, the length of time between intubation and death varied considerably depending on the principal diagnosis. Death after ED intubation is most likely to occur within the first several days, particularly among those with primary cardiopulmonary diagnosis, CVA, or sepsis, after which point, the probability of death is significantly lower. This information can help to shape family expectations after ED intubation.
We found that, among hospital decedents, age had little impact on median TTD. This finding is in keeping with previous studies, which have shown that, while age is a factor in intensive care unit (ICU) survival, it is not the primary determinant of mortality.14 Interestingly, the extent of comorbid illness had a paradoxical relationship with TTD, whereby hospital decedents with higher CCI actually survived longer. Given the limitations of this administrative dataset, it remains unclear what is driving this phenomenon. It is unlikely that higher CCI actually confers a survival benefit.15 It is possible that the paradoxical relationship between TTD and CCI is reflective of an unmeasured confounder of survival time among decedents, rather than an actual survival benefit conferred by increased CCI.16 “Reversals” of association between risk factors and mortality have been well documented in other index-event cohort studies, and found to be attributable to collider bias and conditioning.17,18 This hypothesis is supported by the fact that overall increased CCI was associated with higher mortality. Another possible confounder may be a stronger preference for aggressive care among a small subset of patients with extensive comorbid disease burden. Further studies are required to evaluate this relationship.
There are several limitations to this study. First, use of a retrospective database limits our ability to understand the relationship between death and the decision to withdraw life-sustaining treatment (LST) and death. However, we know from previous studies that the majority of deaths in the ICU occur after the decision to withhold or withdraw LST, rather than a failure of LST itself.19–21 Thus, it is important for clinicians to understand this limitation when making inferences about prognosis. The natural history of respiratory failure treated with intubation and MV is necessarily different among hospital survivors and decedents. Future studies must explore these relationships further. Finally, this study is based on administrative data. As with all claims database research, our findings are vulnerable to misclassification bias due to coding inaccuracies and omissions.17,18,22
Conclusion
For older adults with serious illness, the decision to initiate MV is often fraught with uncertainty. The median time from intubation to death was short (three days); however, the length of time between intubation and death varied considerably depending on the principal diagnosis. Improved understanding of prognosis in the initial days after emergency intubation may help clinicians to mobilize additional support such as palliative care and provide families with more accurate anticipatory guidance.
Author Disclosure Statement
No conflicts have been disclosed.
Poster Presentation at American College of Emergency Physicians, National Assembly, 2018.
References
- 1. Steinhauser KE, Christakis NA, Clipp EC, et al. : Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284:2476–2482 [DOI] [PubMed] [Google Scholar]
- 2. Barnato A, McClellan M, Kagay C, et al. : Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res 2004;39:363–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lagu T, Zilberberg MD, Tjia J, et al. : Use of mechanical ventilation by patients with and without dementia, 2001 through 2011. JAMA Intern Med 2014;174:999–1001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ouchi K, Hohmann S, Goto T, et al. : Index to predict in-hospital mortality in older adults after non-traumatic emergency department intubations. West J Emerg Med 2017;18:690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bernacki RE, Block SD: Communication about serious illness care goals: A review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003 [DOI] [PubMed] [Google Scholar]
- 6. Pearlman RA, Cain KC, Patrick DL, et al. : Preferences for life-sustaining treatments in advance care planning and surrogate decision making. J Palliat Med 2000;3:37–48 [DOI] [PubMed] [Google Scholar]
- 7. Patrick DL, Pearlman RA, Uhlmann RF, et al. : Validation of preferences for life-sustaining treatment: Implications for advance care planning. Ann Intern Med 1997;127:509–517 [DOI] [PubMed] [Google Scholar]
- 8. Lagu T, Zilberberg MD, Tjia J, et al. : Dementia and outcomes of mechanical ventilation. J Am Geriatr Soc 2016;64:e63–e66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gupta A, Das A, Tariq R, et al. : Trends in outcomes of patients with metastatic cancer undergoing intubation and mechanical ventilation: Results of the National Hospital Discharge Survey. J Natl Compr Canc Netw 2018;16:286–292 [DOI] [PubMed] [Google Scholar]
- 10. Vizient: www.vizientinc.com/Who-we-are (Last accessed December9, 2016)
- 11. Bougouin W, Lascarrou JB, Dumas F, et al. : Targeted temperature management after cardiac arrest: The longer, the better? J Thorac Dis 2018;10:49–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Laver S, Farrow C, Turner D, et al. : Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med 2004;30:2126. [DOI] [PubMed] [Google Scholar]
- 13. Vandenbroucke JP, von Elm E, Altman DG, et al. : STROBE initiative. PLoS Med 2007;4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reyes JCL, Alonso JV, Fonseca J, et al. : Characteristics and mortality of elderly patients admitted to the Intensive Care Unit of a district hospital. Indian J Crit Care Med 2016;20:391–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mnatzaganian G, Ryan P, Norman PE, et al. : Accuracy of hospital morbidity data and the performance of comorbidity scores as predictors of mortality. J Clin Epidemiol 2012;65:107–115 [DOI] [PubMed] [Google Scholar]
- 16. Quan H, Li B, Couris CM, et al. : Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–682 [DOI] [PubMed] [Google Scholar]
- 17. Cole SR, Platt RW, Schisterman EF, et al. : Illustrating bias due to conditioning on a collider. Int J Epidemiol 2010;39:417–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Flanders D, Eldridge R, McClellan W: A nearly unavoidable mechanism for collider bias with index-event studies. Epidemiology 2014;25:762–764 [DOI] [PubMed] [Google Scholar]
- 19. Prendergast TJ, Luce JM: Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med 1997;155:15–20 [DOI] [PubMed] [Google Scholar]
- 20. McLean RF, Tarshis J, Mazer CD, et al. : Death in two Canadian intensive care units: Institutional difference and changes over time. Crit Care Med 2000;28:100–103 [DOI] [PubMed] [Google Scholar]
- 21. Holzapfel L, Demingeon G, Piralla B, et al. : A four-step protocol for limitation of treatment in terminal care. An observational study in 475 intensive care unit patients. Intensive Care Med 2002;28:1309–1315 [DOI] [PubMed] [Google Scholar]
- 22. Shahian DM, Iezzoni LI, Meyer GS, et al. : Hospital-wide mortality as a quality metric: Conceptual and methodological challenges. Am J Med Qual 2012;27:112–123 [DOI] [PubMed] [Google Scholar]