Abstract
Objective: This article describes the findings of a study examining the ability of persons with strokes to use home virtual rehabilitation system (HoVRS), a home-based rehabilitation system, and the impact of motivational enhancement techniques on subjects' motivation, adherence, and motor function improvements subsequent to a 3-month training program.
Materials and Methods: HoVRS integrates a Leap Motion controller, a passive arm support, and a suite of custom-designed hand rehabilitation simulations. For this study, we developed a library of three simulations, which include activities such as flexing and extending fingers to move a car, flying a plane with wrist movement, and controlling an avatar running in a maze using reaching movements. Two groups of subjects, the enhanced motivation (EM) group and the unenhanced control (UC) group, used the system for 12 weeks in their homes. The EM group trained using three simulations that provided 8–12 levels of difficulty and complexity. Graphics and scoring opportunities increased at each new level. The UC group performed the same simulations, but difficulty was increased utilizing an algorithm that increased difficulty incrementally, making adjustments imperceptible.
Results: Adherence to both the EM and UC protocols exceeded adherence to home exercise programs described in the stroke rehabilitation literature. Both groups demonstrated improvements in upper extremity function. Intrinsic motivation levels were better for the EM group and motivation levels were maintained for the 12-week protocol.
Conclusion: A 12-week home-based training program using HoVRS was feasible. Motivational enhancement may have a positive impact on motivation, adherence, and motor outcome.
Keywords: Stroke, Rehabilitation, Hand, Virtual reality, Telerehabilitation, Motivation
Introduction
Persistent, hand-related disability has a substantial effect on the productivity of the growing cohort of younger persons with milder strokes1 and increases the cost of care for older and more impaired persons with strokes.2 Current service delivery models emphasizing short, independence-focused inpatient rehabilitation stays3 and intermittent, low-volume outpatient rehabilitation encounters4 restrict the amount of rehabilitation a patient receives. Over a decade of research has produced some insight into total volume5 of rehabilitation necessary to elicit changes in hand function. Facility-based rehabilitation rarely meets the volume described in these studies.4 This points to the need for rehabilitation that can be performed independently, in the home.
Unfortunately, adherence to unsupervised home exercise regimens is poor in persons with strokes.6,7 Low motivation levels are cited as an important barrier.8,9 Several small sample studies have cited higher levels of motivation associated with videogame-based rehabilitation than real-world exercise or simple virtual rehabilitation.9,10 Studies of patients with stroke describe patients participating in videogame-like training activities, performing five to six times more repetitions than patients performing traditional activities.4,11,12 Few studies have directly examined the adherence of persons with stroke to self-directed rehabilitation activity performance in the home. A single study of traditional, self-directed home exercise reported a 66% retention rate with weekly exercise time <60 minutes.13 Three small studies examining game-based virtual rehabilitation cited study retention rates over 90% and mean self-directed exercise performance times that ranged between 75 and 135 minutes per week over interventions that lasted between 6 and 8 weeks.14–16 This increase is substantial, but these training times still fall short of the training volumes associated with upper extremity (UE) motor improvements.
Standing in stark contrast, commercial videogame usage in the United States is performed by a large cohort of persons in the age group in which strokes occur most often. In a 2016 study published by AARP, 40% of a group of 2516 persons older than 50 years reported regular videogame usage. This group averaged over 5 hours of videogame play per week (250% more than the highest levels of virtual reality (VR)-based home rehabilitation participation cited above).15 One of the reasons underpinning the amount of time these games are played is the structure of the games themselves. A game's rules, progression of play, difficulty, and system of rewards for successful performance, all contribute to the enjoyment associated with these games, and therefore the amount of time people spent playing them.17 Best practices in the field of game mechanics have evolved steadily18 and the use of game mechanics to influence human behavior has spread into a variety of fields.19–21
Adaptive difficulty algorithms have been utilized in virtual rehabilitation studies for over a decade. They are associated with accelerated motor control improvements and increased time on task in laboratory-based virtual rehabilitation.22–25 In our proposed study, we expand on this approach by utilizing a method of game mechanics called scaffolding; when a participant masters each new motor skill, we will introduce another new feature of the game, show the player how to perform the new skill, offer a safe scenario in which the player can practice it, and require the player to master it before moving onto the next skill.26 This approach is associated with dramatic increases in autonomous time on task in non-rehabilitation simulations.27–29 Scaffolding will be coupled with in-game rewards, such as newer more exciting graphics and more ornate avatars to further entice the player to face and overcome the next challenge.28 This article will describe the findings of a feasibility/pilot study designed to establish the ability of persons with strokes to use home virtual rehabilitation system (HoVRS) at home with minimal support. We will also examine the impact of scaffolding and in-game rewards on the intrinsic motivation (as measured using the Intrinsic Motivation Inventory [IMI]), adherence to the program (measured in total rehabilitation minutes), and its effectiveness (measured with the Fugl–Meyer assessment).
Materials and Methods
Study procedures were approved by the Institutional Review Board of Rutgers, The State University of New Jersey.
Subjects
Inclusion criteria were (1) 40–80 years of age, (2) unilateral right- or left-sided stroke, (3) score of 22 or greater on the Montreal Cognitive Assessment,30,31 (4) no hemispatial neglect or proprioceptive loss, (5) Fugl-Meyl Upper Extremity Fugl-Meyer Assessment (UEFMA) of 36-58/6631, and (6) no receptive aphasia. Exclusion criteria were (1) UE orthopedic pathology and (2) other central nervous system pathology. Subjects described in this study were a convenience sample recruited at stroke support groups. The first three utilized unenhanced simulations, while the enhanced simulations were completed. The second group of three used enhanced simulations. Subsequent subjects have been assigned to groups using a random number generator.
Description of system
We have developed the HoVRS to facilitate intensive, hand-focused rehabilitation in the home.32 The system integrates a Leap Motion controller, a passive arm support, and a suite of hand rehabilitation simulations. The Leap Motion provides camera-based measurement of finger joint positions,33 allowing for integrated virtual arm and finger activities without a wearable apparatus. If the patient's arm is severely impaired, a spring compensation system (such as the Armon™ Edero or Saebo™ Mobile Arm Support) was provided to the subject. This system consists of a forearm orthosis that counter balances gravity to provide graded support to the arm during activity. Support is adjusted (and eventually removed) as patients' strength improves.
Using the Unity Game Engine, we have developed a library of interactive games focused on specific hand movement34; 3D assets were created using 3DS Max and the interactions were programmed using C#. A comprehensive calibration procedure is used to measure each subject's active range of motion within the Leap Motion controller visual area and scaled to fit into the videogame virtual environment.
Treatment protocol
Two groups, the enhanced motivation (EM) group and the unenhanced control (UC) group, used the New Jersey Institute of Technology-HoVRS system to train movement of their shoulder, elbow, wrist, and fingers. The study team set up the apparatus in their home at the initial visit and trained them to use it. Subjects practiced in their homes independently with online or in-person support as needed. Both groups were instructed to practice as much as possible, but at least 20 minutes, daily for 12 weeks.
The EM group trained using three simulations. These simulations provided the user with 8–12 levels of gradually increasing difficulty and complexity. A screen announced each level change and the graphics for each new level changed substantially. Scoring opportunities increased at each new level as well. The UC group performed the same three simulations. Difficulty was increased, utilizing an adaptive control algorithm that increased difficulty based on performance. Difficulty changes were extremely incremental, making them imperceptible for most subjects. Graphics and scoring did not change as difficulty level changed.
Description of simulations
For this study, we developed a library of three task-based simulations that train hand manipulation and arm transport. One simulation, Speed Bump, trains hand opening integrated with pronation and supination. Lowest levels of speed bump require progressive increases in the amount of hand opening. As the levels progress, the car speeds up, requiring faster hand opening and closing. The highest levels require pronation and supination integrated with hand opening to negotiate a more complicated course. The second simulation, Urban Aviator, trains wrist movement, by presenting targets that subjects navigate a plane over and around buildings to collect. Lowest levels of this simulation require progressively larger wrist flexion and extension movements that control the pitch of the plane. Increases in difficulty are achieved by larger vertical distances between targets and faster game flow. The third simulation, Maze Runner, trains shoulder and elbow disassociation in a horizontal plane integrated with hand opening. Lower levels of the game require progressively larger amplitude movements to elicit avatar direction changes. Subsequent levels add faster and more frequent direction changes, narrower paths, and obstacles that subjects jump over or off using hand opening and closing.
Outcomes
The impact of game mechanics on motivation was measured utilizing a 12-item version of the IMI.35 We utilized three questions each from the interest/enjoyment, perceived competence, value/usefulness, and effort/importance subscales (Supplementary Data). The primary outcome measure considering adherence was the total number of training minutes performed by the subject over the course of the study. We chose to utilize a time on task measure as opposed to counting repetitions, due to the continuous action of our simulations. The secondary measures will include the average number of sessions per week and average minutes per session. We utilized average sessions per week to evaluate subjects' willingness to choose to play the games over other activities. We chose the average minutes per session metric to evaluate a subject's willingness to play the games for an extended time. The main clinical outcome was the UEFMA. We used the percent of recovery model36 to interpret Fugl–Meyer scores because it acts to control the impact of level of impairment on treatment outcome. We measured activity level improvement using the Box and Blocks Test (BBT).37
Statistical analyses
Descriptive statistics are utilized due to the preliminary nature of this work. Student's t-tests were done on all 11 subjects for the 2 clinical outcome measures as a preliminary evaluation of the effectiveness of training activities to elicit changes in motor abilities.
Results
The entire 11-subject group performed >400 sessions in their homes without the supervision or assistance of study personnel. There were no adverse events. Subjects encountered six unique issues that required technical support. Four were resolved remotely and two required on-site/in-person assistance. Subjects performing the enhanced program (n = 5) were slightly younger and slightly more impaired (mean age 58 ± 9 years, mean UEFMA 44 ± 14) than the subjects who performed the unenhanced training program (n = 6) (mean age 65 ± 15 years, mean UEFMA 51 ± 8).
Higher IMI scores in EM group subjects
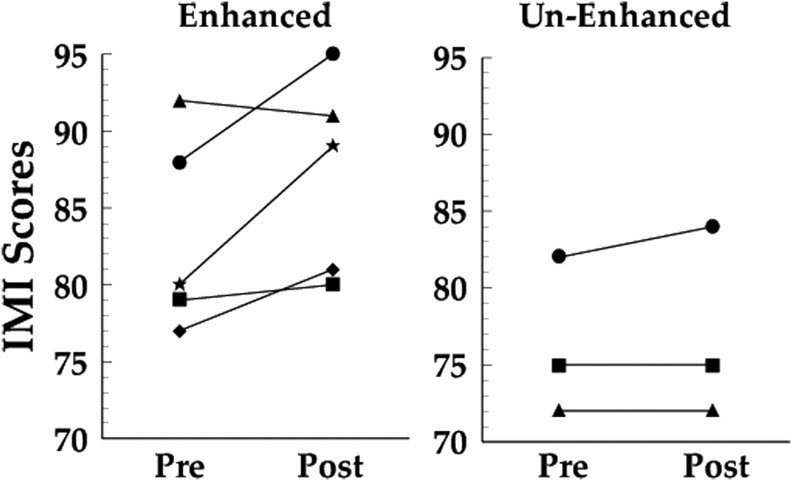
The last 8 subjects completed a 12-item IMI compiled for this trial. Each subject utilized the scale twice, once a week after orientation day and once postintervention. Initial IMI scores for the five subjects performing enhanced simulations ranged between 75 and 93. All, but one of these subjects demonstrated increased scores at postintervention. The three subjects performing unenhanced simulations started with IMI scores between 70 and 82. Two demonstrated stable post-test scores and one improved (Fig. 1).
FIG. 1.
Total IMI scores collected after 1 week of training (pretest) and after completion of protocol (post-test). Note: The first three unenhanced group subjects completed the protocol before the IMI was implemented. IMI, intrinsic motivation inventory.
IMI subscale scores
Mean subscale scores for the two groups reveal several trends. Individual item responses remained relatively stable between pretest and post-test. The one exception was effort/intensity question number 2, which decreased from pretest to post-test by 2 full points for the UC group. The largest difference between EM and UC groups was for the three interest/enjoyment subscale questions. This difference remained stable across both measurements (Table 1).
Table 1.
Mean Individual Intrinsic Motivation Inventory Question Scores Grouped by Subscale
| Interest/enjoyment | Effort/importance | Perceived competence | Value/usefulness | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Enhanced | |||||||||||||
| Pretest | 6 (0.6) | 6 (0.9) | 6.2 (0.7) | 6.4 (0.5) | 6.2 (0.4) | 6.8 (0.4) | 5.4 (0.5) | 4.6 (1.7) | 5.4 (0.8) | 6.6 (0.5) | 6.6 (0.8) | 6.6 (0.5) | 66.2 (5.0) |
| Post-test | 6.2 (0.7) | 6 (0.6) | 6.2 (1.2) | 6.8 (0.4) | 6 (0.9) | 7 (0) | 5.8 (0.4) | 5.4 (1.4) | 5.6 (1.2) | 7 (0) | 7 (0) | 6.8 (0.5) | 69 (3.0) |
| Unenhanced | |||||||||||||
| Pretest | 3.7 (0.5) | 4 (0.8) | 5 (0.8) | 6.3 (0.9) | 5.7 (0.5) | 6.3 (0.9) | 4.7 (0.5) | 4.3 (0.5) | 5.7 (1.9) | 5.7 (0.9) | 5.7 (1.2) | 5.7 (0.9) | 57 (7.1) |
| Post-test | 4.3 (1.2) | 4.3 (0.5) | 5.3 (1.2) | 6.7 (0.5) | 3.7 (1.9) | 6 (1.4) | 4.7 (0.5) | 5.3 (0.5) | 6 (1.4) | 5 (1.6) | 6 (0.8) | 5.7 (0.9) | 57.3 (7.4) |
Increased adherence
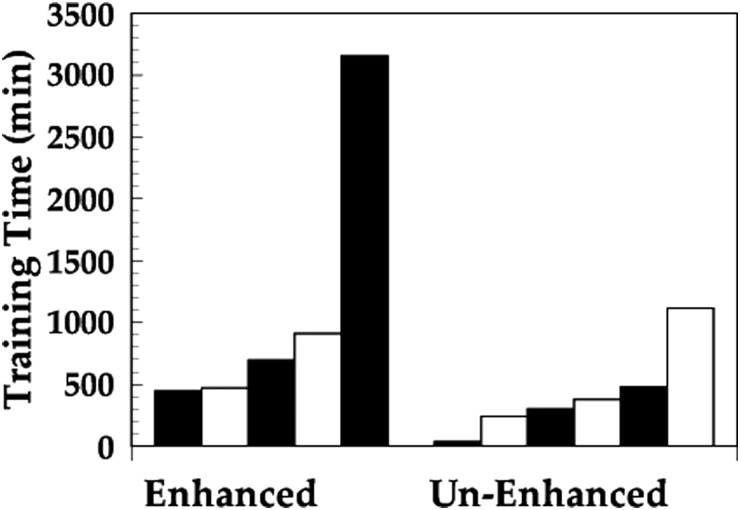
The five subjects utilizing enhanced versions of the simulations averaged 95 ± 95 minutes of training per week, range was between 40 and 276 minutes. The six subjects performing unenhanced simulations averaged 35 ± 31 minutes of training per week, range was between 3 and 93 minutes (Fig. 2).
FIG. 2.
Total training time as collected by the training system for the entire 12-week protocol.
The larger training times demonstrated by the EM group seem to be accomplished by maintaining the length of training sessions over the duration of the training protocol. Average training time per session over the first 2 weeks for the two groups did not differ substantially (18 ± 4 minutes/session for UC group and 14 ± 9 for the EM group). UC group subjects decreased training time per session by the end of the protocol, while the EM group's average training time remained essentially the same (10 ± 5 minutes/session UC group, 15 ± 8 for EM group). Similar to training duration per session, the average number of training sessions over the first 2 weeks for the two groups did not differ significantly (4.4 ± 1.5 sessions for UC group subjects and 3.6 ± 1.4 for the EM group; P = 0.47). The UC group's average number of training sessions per week decreased by the end of the trial to 3.8 ± 1.5, while the EM group's increased to an average of 4.2 ± 2.3.
Larger hand function improvements
When examined as a single, 11-subject cohort, raw score changes for UEFMA and BBT were statistically significant. Using a Student's t-test for each of these two measures, the pretest to post-test score change were significant for the BBT, for the entire group (P = 0.0485) and for the entire group with the subject whose improvement exceeded 2 standard deviations (SDs) from the mean (P = 0.0331). There were no outliers when considering raw score for UEFMA for all 11 subjects. Student's t-test was statistically significant (P < 0.001). Two EM group subjects demonstrated a four-point improvement in UEFMA, while eight subjects (five unenhanced and three enhanced) demonstrated an increase of five or more points. Page et al.38 cite an Minimum Clinically Important Difference of 4.25 points for the UEFMA in chronic stroke subjects. Two EM group subjects made changes in score on the BBT, which were beyond measurement error. One of these subjects demonstrated a clinically important difference.39
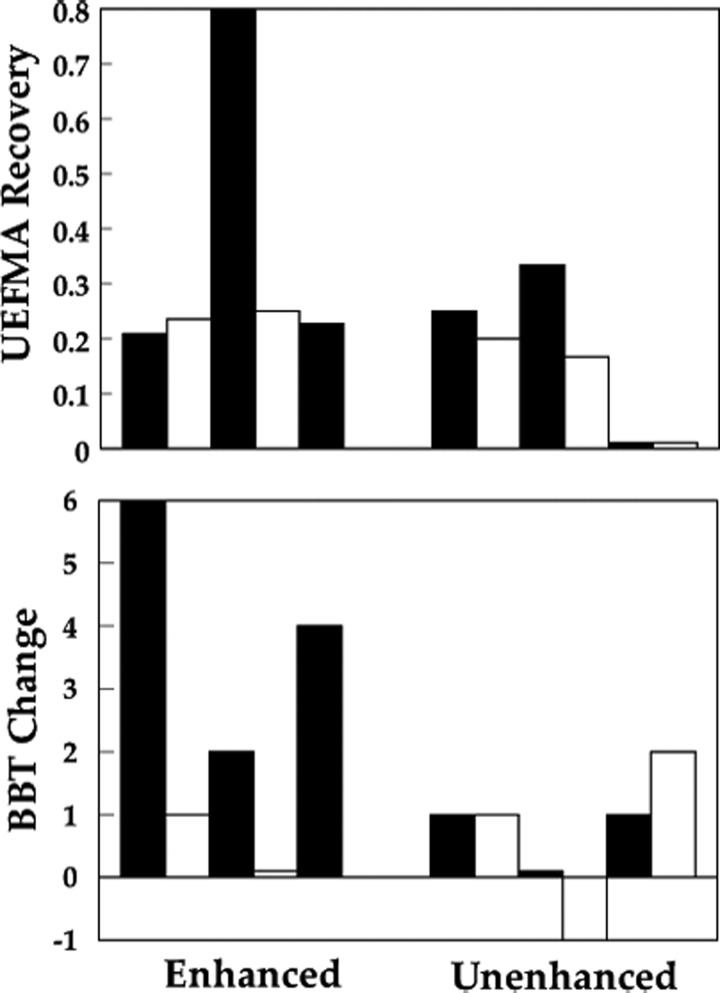
In the EM group, UEFMA recovery ranged from 0.2 to 0.8. In the UC group, recovery ranged from 0 to 0.4 (Fig. 3). BBT score changes ranged between −1 and 4 for UC group subjects and between 1 and 6 for EM group subjects (Fig. 3). These preliminary data suggest that motivational enhancements might have an impact on motor outcomes associated with unsupervised training in persons with stroke.
FIG. 3.
Top panel: UEFMA recovery, calculated as (post-UEFMA—pre-UEFMA)/(66—pre-UEFMA). Bottom panel: change in BBT score, calculated as (No. Blocks pretest)—(No. Blocks post-test). BBT, Box and Blocks Test; UEFMA, Upper Extremity Fugl-Meyer Assessment.
Power analyses
All calculations are based on a one-tailed t-test with α = 0.05 and 1–ß = 0.8.
Motivation testing
Using an effect size of 0.84 detected in our pilot subjects, we will need to collect data from 18 subjects per group.
Adherence testing
Using an effect size of 0.83 detected in our pilot subjects, we will need to collect data from 19 subjects per group.
Effectiveness testing
Using an effect size of 0.88 detected in our pilot subjects for this comparison, we will need to collect data from 17 subjects per group. Based on power calculations, we will need 38 subjects. Assuming a 20% dropout rate, we will recruit 45 subjects.
Discussion
We are confident that feasibility was demonstrated. Adherence to the EM and UC protocols exceeded traditionally presented home exercise programs described in the stroke rehabilitation literature. This training elicited measurable improvements in UE function in both groups. Safety of the system and intervention approach was confirmed. Our power analyses identified a manageable sample size to attain adequately powered comparisons.
While the differences between the two groups were modest, several trends that emerged were encouraging. The EM group did not demonstrate a decrease in training time per session, or the number of sessions that they performed each week. The UC group demonstrated nonsignificant trends toward decrease in both of these metrics. Going forward, we plan to extend the length of the protocol in an attempt to determine if the adherence patterns for the two protocols continue to diverge.
There was a nonsignificant trend toward higher overall scores for the EM group on the IMI at both time points. A study with a larger sample will be necessary to make generalizable statements based on this comparison. Analysis of the individual IMI items identifies some interesting trends and areas for future investigation. EM group subjects demonstrated trends toward higher scores on the 3 interest/enjoyment subscale questions and a trend toward longer exercise times. Subjects in Popović et al.40 demonstrated a similar difference in interest enjoyment scores between subjects utilizing VR-based games compared to a control that performed real-world versions of the same training tasks. The VR group in the Popović study demonstrated better interest/enjoyment scores, better adherence to the training program, and better motor outcomes. Interest/enjoyment scale scores remained stable between pretest and post-test. We consider this a positive outcome, based on the fact that subjects had performed these activities for 12 weeks. This is a novel finding based on the fact that none of the studies of technology-supported rehabilitation in persons with stroke have reported follow-up IMI data.
The total training volume fell short of the amount associated with meaningful UE improvements41 and the volume demonstrated by healthy adults playing commercial computer games.15 Important new studies establish that the relationship between volume of training performed by a person poststroke and the improvement in motor performance they experience subsequent to training is not linear.42,43 Our initial findings have been consistent with the findings of these larger studies. The subjects performing the most training in our study did not make the largest gains in UE function. This said, these studies were performed on directly supervised subjects with training appointments. The training schedule utilized, resulting in even the lowest doses in these studies, far exceeds the training times typically performed by unsupervised stroke subjects in their homes. This said, our pilot data suggest that attending to motivation might have an impact on the time that autonomously operating persons with strokes perform these interventions.
This study utilized modest motivational enhancements. In an attempt to bolster training time per session, we will add the elements of competition and narrative into our simulations. These two elements are associated with increased time on task. In a parallel effort to increase the number of training sessions, we will use e-mail and text reminders, calling attention to weekly quests that will allow participation in a modified version of one of the games for bonus points. This approach incorporates novelty, urgency and external reminders, all elements associated with more frequent game-play,
This article describes a preliminary study that has weaknesses. The sample size is small, which limits its generalizability and makes the power analyses reported susceptible to high or low performers. There is a high performer in two of the three power analyses in the EM group, with scores between 2 and 3 SDs above the mean for the entire sample. We chose to utilize these outcomes because these high performers did not exceed 3 SDs from the mean and their performance was not outside typically observed values for persons with stroke. Our IMI data are incomplete, due to the fact that we finalized and adopted this measure after we collected data on three subjects.
Conclusion
This pilot study presents preliminary data that suggest that the study of motivation enhancement in persons with UE hemiparesis due to chronic stroke is feasible and that modest motivational enhancements may have an impact on adherence to a 3-month rehabilitation program.
Supplementary Material
Acknowledgments
This work was supported, in part, by NIDILRR 90RE5021-01-00 (Foulds). The authors state that they have no conflicts of interest to report.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Data
Questionnaire available online
References
- 1. Faria-Fortini I, Michaelsen SM, Cassiano JG, Teixeira-Salmela LF. Upper extremity function in stroke subjects: Relationships between the international classification of functioning, disability, and health domains. J Hand Ther 2011; 24:257–265 [DOI] [PubMed] [Google Scholar]
- 2. Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil 2014; 95:986..e1–995.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fluet G, Patel J, Qiu Q, et al. . Early versus delayed VR-based hand training in persons with acute stroke. Paper presented at: (ICVR), 2017 International Conference on Virtual Rehabilitation. Philadelphia PA [Google Scholar]
- 4. Lang CE, MacDonald JR, Reisman DS, et al. . Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil 2009; 90:1692–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lohse KR, Lang CE, Boyd LA. Is more better? Using metadata to explore dose–response relationships in stroke rehabilitation. Stroke 2014; 45:2053–2058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jurkiewicz MT, Marzolini S, Oh P. Adherence to a home-based exercise program for individuals after stroke. Top Stroke Rehabil 2011; 18:277–284 [DOI] [PubMed] [Google Scholar]
- 7. Miller KK, Porter RE, DeBaun-Sprague E, et al. . Exercise after stroke: Patient adherence and beliefs after discharge from rehabilitation. Top Stroke Rehabil 2017; 24:142–148 [DOI] [PubMed] [Google Scholar]
- 8. Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. JRRD 2008; 45:315–322 [DOI] [PubMed] [Google Scholar]
- 9. Mihelj M, Novak D, Milavec M, et al. . Virtual rehabilitation environment using principles of intrinsic motivation and game design. Presence: Teleoperators and Virtual Environments 2012; 21:1–15 [Google Scholar]
- 10. Fitzgerald D, Trakarnratanakul N, Smyth B, Caulfield B. Effects of a wobble board-based therapeutic exergaming system for balance training on dynamic postural stability and intrinsic motivation levels. JOSPT 2010; 40:11–19 [DOI] [PubMed] [Google Scholar]
- 11. Rand D, Givon N, Weingarden H, et al. . Eliciting upper extremity purposeful movements using video games A comparison with traditional therapy for stroke rehabilitation. Neurorehabil Neural Repair 2014; 28:733–739 [DOI] [PubMed] [Google Scholar]
- 12. Peters DM, McPherson AK, Fletcher B, et al. . Counting repetitions: An observational study of video game play in people with chronic poststroke hemiparesis. JNPT 2013; 37:105–111 [DOI] [PubMed] [Google Scholar]
- 13. Miller KJ, Adair BS, Pearce AJ, et al. . Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: A systematic review. Age Ageing 2014; 43:188–195 [DOI] [PubMed] [Google Scholar]
- 14. Standen PJ, Threapleton K, Connell L, et al. . Patients' use of a home-based virtual reality system to provide rehabilitation of the upper limb following stroke. Phys Ther 2015; 95:350. [DOI] [PubMed] [Google Scholar]
- 15. Anderson GO. Video Games: Attitudes and Habits of Adults Age 50-Plus. Washington DC: AARP Research, June 2016 [Google Scholar]
- 16. Wittmann F, Held JP, Lambercy O, et al. . Self-directed arm therapy at home after stroke with a sensor-based virtual reality training system. J NeuroEngineering Rehabil 2016; 13:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ryan RM, Rigby CS, Przybylski A. The motivational pull of video games: A self-determination theory approach. Motiv Emot 2006; 30:344–360 [Google Scholar]
- 18. Rouse R., III Game Design: Theory and Practice. Boca Raton FL: Jones & Bartlett Learning; 2010 [Google Scholar]
- 19. Hamari J, Lehdonvirta V. Game design as marketing: How game mechanics create demand for virtual goods. Int J Business Sci Appl Manag 2010; 5:14–29 [Google Scholar]
- 20. Kapp KM. The Gamification of Learning and Instruction: Game-Based Methods and Strategies for Training and Education. San Francisco CA: John Wiley & Sons; 2012 [Google Scholar]
- 21. Orji R, Vassileva J, Mandryk RL. Modeling the efficacy of persuasive strategies for different gamer types in serious games for health. User Model User Adapt Interact 2014; 24:453–498 [Google Scholar]
- 22. Adamovich SV, Fluet GG, Mathai A, et al. . Design of a complex virtual reality simulation to train finger motion for persons with hemiparesis: A proof of concept study. J NeuroEngineering Rehabil 2009; 6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. da Silva Cameirão M, Bermúdez i Badia S, Duarte E, Verschure PF. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: A randomized controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor Neurol Neurosci 2011; 29:287–298 [DOI] [PubMed] [Google Scholar]
- 24. Merians AS, Poizner H, Boian R, et al. . Sensorimotor training in a virtual reality environment: Does it improve functional recovery poststroke? Neurorehabil Neural Repair 2006; 20:252–267 [DOI] [PubMed] [Google Scholar]
- 25. Adamovich SV, Merians AS, Boian R, et al. . A virtual reality-based exercise system for hand rehabilitation post-stroke. Stud Health Technol Inform 2002; 85:64–70 [PubMed] [Google Scholar]
- 26. Ram A, Leake D. Learning, goals, and learning goals. Goal-driven learning. Art Intel Rev 1995; 9387–422 [Google Scholar]
- 27. Bostan B. Player motivations: A psychological perspective. CIE 2009; 7:22 [Google Scholar]
- 28. Pea RD. The social and technological dimensions of scaffolding and related theoretical concepts for learning, education, and human activity. J Learn Sci 2004; 13:423–451 [Google Scholar]
- 29. Landers RN, Bauer KN, Callan RC, Armstrong MB. Psychological theory and the gamification of learning. In: Reiners T, Wood LC. (eds) Gamification in Education and Business. Switzerland: Springer; 2015, pp. 165–186 [Google Scholar]
- 30. Nasreddine ZS, Phillips NA, Bédirian V, et al. . The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. JAGS 2005; 53:695–699 [DOI] [PubMed] [Google Scholar]
- 31. Deakin A, Hill H, Pomeroy VM. Rough guide to the Fugl–Meyer Assessment: Upper limb section. Physiotherapy 2003; 89:751–763 [Google Scholar]
- 32. Qiu Q, Cronce A, Fluet GG, Patel J, Merians AS, Adamovich SA. Upper extremity functional recovery from home based virtual rehabilitation in persons with stroke. IEEE Engineering in Medicine and Biology Conference, Orlando FL, 2016 [Google Scholar]
- 33. Guna J, Jakus G, Pogačnik M, et al. . An analysis of the precision and reliability of the leap motion sensor and its suitability for static and dynamic tracking. Sensors 2014; 14:3702–3720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Qiu Q, Cronce A, Fluet GG, et al. . Home Based Virtual Rehabilitation for upper extremity functionality recovery post stroke. International Conference on Disability, Virtual Reality and Assistive Technologies, Los Angeles CA, 2016 [Google Scholar]
- 35. McAuley E, Duncan T, Tammen VV. Psychometric properties of the Intrinsic Motivation Inventory in a competitive sport setting: A confirmatory factor analysis. Res Q Exerc Sport 1989; 60:48–58 [DOI] [PubMed] [Google Scholar]
- 36. Krakauer JW, Marshall RS. The proportional recovery rule for stroke revisited. Ann Neurol 2015; 78:845–847 [DOI] [PubMed] [Google Scholar]
- 37. Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther 1985; 39:386–391 [DOI] [PubMed] [Google Scholar]
- 38. Page SJ, Fulk GD, Boyne P. Clinically important differences for the upper-extremity Fugl–Meyer Scale in people with minimal to moderate impairment due to chronic stroke. Phys Ther 2012; 92:791–798 [DOI] [PubMed] [Google Scholar]
- 39. Chen H-M, Chen CC, Hsueh I-P, et al. . Test-retest reproducibility and smallest real difference of 5 hand function tests in patients with stroke. Neurorehabil Neural Repair 2009; 23:435–440 [DOI] [PubMed] [Google Scholar]
- 40. Popović MD, Kostić MD, Rodić SZ, et al. . Feedback-mediated upper extremities exercise: Increasing patient motivation in poststroke rehabilitation. BioMed Res Int 2014; 2014:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kwakkel G. Impact of intensity of practice after stroke: Issues for consideration. Disabil Rehabil 2006; 28:823–830 [DOI] [PubMed] [Google Scholar]
- 42. Lang CE, Strube MJ, Bland MD, et al. . Dose response of task-specific upper limb training in people at least 6 months poststroke: A phase II, single-blind, randomized, controlled trial. Ann Neurol 2016; 80:342–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Winstein CJ, Wolf SL, Dromerick AW, et al. . Effect of a task-oriented rehabilitation program on upper extremity recovery following motor stroke: The ICARE randomized clinical trial. JAMA 2016; 315:571–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.