Abstract
Interventional orthobiologics is changing the landscape of orthopedic medicine. Various methods exist for treatment of many different musculoskeletal pathologies. Candidacy for such injections remains a debated topic, and current research is underway for stratifying the patients that would be most successful for certain techniques. Described in this commentary are the various methods of interventional orthobiologic techniques available such as: prolotherapy, platelet rich plasma (PRP), mesenchymal stromal cells (MSCs), culture-expanded MSCs and amniotic-based products. Here we review the healing cascade and how this relates to the application of the various injectates and rehabilitation protocols. In conclusion, there exists orthobiologic techniques for the healing of a multitude of musculoskeletal ailments, from ligamentous instabilities/tears, tendon derangements and osteoarthritis, however candidacy grades continue to be an area for discussion as to which type of treatment is the most beneficial, and which rehabilitation protocols are required. More randomized controlled trials and comparative analyses are needed for direct correlative conclusions for which interventional orthobiologic treatment and rehabilitation protocol is best after each respective treatment.
Level of Evidence:
5
Keywords: mesenchymal stromal cells (MSCs), orthobiologics, orthopedic medicine, Platelet Rich Plasma (PRP), regenerative medicine, regenerative rehabilitation, Stem Cells
INTRODUCTION TO REGENERATIVE REHABILITATION
Regenerative rehabilitation is defined by the American Physical Therapy Association as the integration of interventional orthobiologic techniques coupled with appropriate rehabilitation protocols that harness the bodies innate healing mechanisms through movement to augment the orthobiologic injections.1 From regenerative rehabilitation stems a separate but interconnected field known as mechanotherapy. Mechanotherapy refers to the therapeutic modalities used to propagate the physiologic mechanism by which body movements provide mechanical stimuli to remodel cells. This field examines mechanobiology, transduction and adaptation to effectively direct tissue modeling and remodeling.2 In 2016, mechanotherapy was defined as exercise-based activity that promoted the adequate force through a specific bodily structure that contributed to the restructuring, stabilization and eventual contribution to healing.3
Physical therapy is a pivotal part of the regenerative/orthobiologic landscape. The aim of all regenerative therapy is to facilitate healing through targeted specific mechano-adaptations (through appropriate exercise and mobilization of joints) in order to foster healthy balance of forces to prevent future injuries and maximize well-being.4 Understanding interventional orthobiologics procedures and how cellular responses respond to mechano-transduction will help guide the development of appropriate rehabilitation programs for each type of regenerative therapy.5 The purpose of this commentary is to provide a history of orthobiologics and describe the role of rehabilitation after these interventional procedures. This will allow the reader to better understand the physiology of disease states requiring orthobiologic interventions and to describe how interventional orthobiologics should be coupled with rehabilitation for optimal healing and return to function.
The Healing Cascade, as it relates to the musculoskeletal system
The healing cascade encompasses three major phases: 1) inflammation, 2) proliferation, and 3) maturation.6 Inflammation is the start of the healing cascade from injury to approximately days 4 to 6, and the beginning is characterized by initial bleeding from injury which causes the body to need to stop the bleeding with vasoconstriction which activates the coagulation cascade which leads to formation of a clot from platelets composed of collagen, thrombin and fibronectin.5 This clot works as the scaffold for other healing cells such as cytokines and growth factors to invade and start the inflammatory cascade.
Growth factors modulate healing and the inflammatory phase which then results in vasodilatation with increased vascular permeability and migration of cells.6 The inflammatory phase also summons neutrophils through various cell signaling, which help with managing cellular debris while uninjured tissues are protected by protease inhibitors.7 Subsequently, the body switches to other cells known as monocytes that signal macrophages to move in to clear out the neutrophils to then release fibroblasts and begin the proliferative phase of healing.5
Proliferation is characterized by angiogenesis and fibroplasia, modulated by the fibroblasts and epithelial cells during approximately days four to 14. Angiogenesis occurs as a mechanism of the body to enhance blood flow to the injured area. Next, fibroplasia commences when fibroblasts come in and begin to lay down collagen.
Maturation and remodeling is the phase between approximately day 8 and one year composed of strengthening of the extracellular matrix (ECM) and production of collagen in an organized network.5 The organization continues to form along lines of stress, however it never returns back to its original state.6
The estimation regarding the amount of time each phase takes is dependent on patient age, comorbidities, and level of injury. There is not a distinct stepwise approach but more of a progression with overlap of the various phases of healing. This is more of an estimate to help in coordinating appropriate rehab protocols after injury. The largest difference between regenerative rehabilitation and post-orthopedic surgery rehabilitation is not only to get the patient back to activity that was being done prior to the intervention, but also to change the biomechanical factors that contributed to the injury in the first place.
MUSCULOSKELETAL TISSUES: STRUCTURE AND FUNCTION RELATED TO HEALING
The musculoskeletal system is composed of different types of connective tissue, including muscles, tendons, ligaments, cartilage and bone.7 Each of these tissues is unique with regard to function and composition, and has healing potential, to some degree,
Muscles
The main function of muscle is to generate contractions that transmit load across a joint to facilitate motion and provide stability.7 In skeletal muscle injury the healing cascade is activated when the muscle tissue is injured, due to myofiber rupture along with damage to local capillaries. This triggers an influx of calcium and clot formation begins.9 Inflammatory cells migrate to the injured site, activates fibroblasts and satellite cells (SC's) which are myogenic stem cells.7-10 During the proliferative phase of muscle healing, SC's differentiate into myoblasts, and in the remodeling phase the new myofibers differentiate into muscle fibers.7,10
The ability of skeletal muscle to respond to trauma such as associated with exercise, immobilization, trauma, or chemical insult relies on the regenerative capacity that exists due to the presence of myogenic SC's.11 Teixeira et al. proposed that skeletal muscle loading may increase the number of SC's, their proliferation, and their differentiation capacities which collectively enhances skeletal muscle regeneration. Skeletal muscle loading increases both vascularization and collagen turnover.11 The data collected by Teixeira et al suggests that active skeletal muscles (muscle that has been in movement such as after exercise) might be better prepared to respond effectively to a muscle injury. Therefore, the authors implied that even electric stimulation should be considered in limbs that have impaired movement to preserve the SC pool in order to improve skeletal muscle rehabilitation.11
Tendons
Tendons primarily function to interlink the muscle and bone and have been demonstrated to have specific structural characteristics. The location of a tendon in vivo affects the mechanics and the amount of shear, compression, tension or torque placed on a tendon, which makes in vitro modeling of tendons difficult to extrapolate.12
Tendinopathies encompass over 30% of all musculoskeletal consultations.13 The process of tendon remodeling involves both synthesis and degradation of collagen with a net degradation that begins immediately after exercise then shifts to a net synthesis.14 Matrix metalloproteinases (MMP) have been shown to play a part in tendinopathy, however, it is unclear whether overloading inhibits the MMP activity leading to the transformation from adaptation to degeneration.15
Mechano-biologically, tendons have been shown to improve with loading which activate protein kinases and increase turnover of Type 1 collagen to promote anabolism.16,17 The underlying mechanisms associated with pathogenesis of tendinopathies is largely unknown.18 However, many orthobiologic treatments have been targeted to manage various upper and lower extremity tendinopathies.
Ligaments
Ligaments function to link bones with other bones, in order to stabilize a joint. Ligaments function in a similar model to tendon, however with decreased tensile loads. They function to provide passive joint stability throughout normal range of motion of a joint and to provide joint proprioception.7,19 Traumatic ligamentous injury can result in either a partial or complete tear and can proceed through the typical three phases of healing that includes inflammation, proliferation and remodeling.7 During the first phase, retraction of the disrupted segments of ligament forms a gap and within that gap a clot forms reigning in cytokines and the inflammatory phase.7,20,21 In the fibroblast/ proliferation phase the disorganized fragments are mostly composed of less organized collagen, and in the remodeling phase the fragments start to organize and improve to withstand tensile loads and for force transmission.7 Ligamentous tissue that has been damaged and then heals, is not as elastic as the original healthy ligament.7,22
Cartilage
The articular cartilage present in joints can withstand an impressive amount of forces (compression, shear, etc.) and allows for smooth gliding motion without friction.7 The absence of blood supply is what limits the healing capabilities of articular cartilage. A defect that penetrates cartilage into the subchondral plate has a greater capacity to heal because it may facilitate clot formation and cell migration7,23. Once cartilage heals it is histologically more like fibrocartilage than hyaline cartilage and will be stiffer than original cartilage.7,24,25
Bone
Bone also proceeds through the same healing cascade of inflammation, proliferation and remodeling. With a fracture, the inflammation phase begins with bleeding and then the clot forms. The release of cytokines and growth factors which are responsible for proliferation of chrondroblasts and osteoblasts fills the fracture site with granulation tissue.7,26,27 Chrondrocytes initially form a soft callus then osteoblasts gradually replace soft callus with immature woven bone and eventually to hard callus.7,28 If bony fragments from a fracture are well approximated the healing is more reliable than a torn ligament or tendon due to the inherent blood supply of the bone that is absent in other tissues.
Review Of Interventional Orthobiologic Techniques
Because each tissue type in the body has differences and similarities in healing, orthobiologic techniques have been developed that are specific to each connective tissue type. Vora et al. described regenerative therapy (a.k.a interventional orthobiologics) as “the injection of a small volume of solution into multiple sites of painful ligament and tendon insertions and adjacent joint spaces, with the goal of reducing pain and ostensibly promoting tissue repair and growth”.29 p. S104
The first type of regenerative therapy to be discussed is the use of a hypertonic solution known as prolotherapy that has aided in paving the field for other types of orthobiologic therapeutics.
Prolotherapy
Prolotherapy is the use of a composition of hypertonic dextrose solution for promoting local healing of chronically injured extra-articular and intra-articular tissue through stimulating both inflammatory and noninflammatory pathways. In the 1950s, Dr. George Hackett, a general surgeon in the United States, formalized the injection protocols for prolotherapy as an orthobiologic injection technique.30 Liu et al injected the medial collateral ligaments of rabbits with sodium morrhuate (irritant), and found that after repeated injections there was a significant increase in collagen fibrils and this increased stabilization.31 Hypertonic dextrose is the most commonly used prolotherapy solution with favorable outcomes shown in multiple clinical trials dating back to the 2000s for treatment of OA.32 Dextrose prolotherapy is proposed to function by creating a hyperosmolar environment to induce the healing cascade via releasing growth factors and scarring down/forming collagen that eventually strengthens with improved tensile strength.32 This in-turn promotes the tightening or strengthening of a tissue from a big picture standpoint. The magnitude of benefit of prolotherapy is varied by treatment protocols, evaluation intervals, and therapeutic measurement tools.33
Clinical Research
Two studies of dextrose prolotherapy in the treatment of hand osteoarthritis exist, one study compared it to steroid injection and the other compared prolotherapy to lidocaine. In the steroid comparison study hand movement and function improved more in the prolotherapy group at six months than the group receiving steroid injection.34 In the study comparing with lidocaine, the prolotherapy improved more in pain during movement and range of motion at six months as compared to those treated with lidocaine.35 Centeno et al. published a case series in 2005 in which the cervical posterior elements were injected under fluoroscopic-guidance, and demonstrated a statistically significant improvement in pain scores and improved stability in flexion translation.36
The use of dextrose prolotherapy for knee osteoarthritis is supported by Level 1 evidence in the form of a systematic review and meta-analysis published in 2016.37 Sit et al. compared four randomized controlled studies noted that intraarticular and periarticular hypertonic dextrose knee injections over three to five sessions had a statistically significant and clinically relevant effect in the improvement of function and pain when compared to formal home therapy exercise alone and the benefits were sustained for one year.35,38-40
Low back pain and Sacroilitis
A Cochrane review was performed in 2009 to determine if injection therapy with prolotherapy is more effective than placebo or other treatments for patients with subacute or chronic low back pain in which 18 trials were selected for review.41 The injection sites varied from epidural sites and facet joints (intra-articular, peri-articular and nerve blocks) to local sites (tender and trigger points) along with a variety of drugs that were compared including corticosteroids, local anesthetics, and a variety of other drugs which prevents head to head comparison.41 Only 10 of the 18 randomized controlled trials pooled were rated as a high-quality methodology; however, insufficient evidence was noted to support for or against the use of any injection therapy in the subacute and chronic low back pain.41
Kim et al published a randomized controlled trial noting that sacroiliac joint prolotherapy injections were found to be superior to steroid injections.42 And again, a retrospective cohort study by Hoffman et al noted that prolotherapy may be a satisfactory option for SI joint instability.43
A recent prospective study by Solmaz et al concluded that prolotherapy injections performed posterior and laterally may be a viable option prior to considering reoperation in failed back surgery syndrome (FBSS).44 All injections were done using ultrasound and posterior injections performed were directed to the posterior sacroiliac ligament insertions bilaterally, iliolumbar ligament insertions bilaterally, while lateral injections targeted the transverse ligament insertions and lumbar facet joints bilaterally. Laterally, the ultrasound was also used to direct injections into the pubofemoral ligamentous insertion, piriformis muscle origin and insertion, iliofemoral ligament insertion and ischiofemoral ligament insertion.44
Tendinopathy
Rabago et al and Scarpone et al published two randomized-controlled trials that have demonstrated effectiveness of prolotherapy in lateral epicondylosis where prolotherapy participants showed improved isometric strength and grip strength compared to baseline status and to controls.45,46 Osgood Schlatter disease is a tendinopathy of the patellar tendon at the tibial tubercle of children age 9-17 who are engaged in kicking sports.45 Prolotherapy was compared to lidocaine only, and at one year 84% of the prolotherapy treated knees were pain free with comparison to the 46% of lidocaine-treated knees.45 Treatment of rotator cuff tendinopathy was tested in a three-arm masked randomized controlled trial with comparison between prolotherapy and a control solution placed at the enthesis of the rotator cuff tendons and another a third group with a superficial saline injection.45,47 Pain was the primary outcome in the rotator cuff study, and 59% of the prolotherapy participants reported a 2.8-point change on the VAS (visual analog scale) pain score with comparison to 37% who received saline at the enthesis and 27% who received the superficial saline injections.45,47
The next orthobiologic is known as platelet rich plasma which is the use of concentrated autologous blood that has been separated into its most enriching growth factor components as further described below.
Platelet Rich Plasma
Platelet rich plasma (PRP) is a substance that is composed from whole blood which consists of higher concentration of platelets from whole blood that is spun down into separate components and concentrated to be more potent than is physiologically possible. The goal of the use of PRP is to have supra-therapeutic platelet concentration in a small volume of plasma in order to induce healing potential in tissue that has otherwise poor inherent healing capacity including joints, cartilage, tendons, and ligaments.48 PRP therapy initially gained popularity in dentistry and cardiac surgery in the 80's and 90's.48 The mechanism behind PRP is to enhance the healing cascade in a controlled fashion due to a higher concentration of platelets and growth factors being injected than are normally physiologically present. The platelets play a central role in the anabolic mechanism of healing by releasing growth factors stored in the alpha granules.48 The key growth factors stored in alpha granules are: Platelet-derived growth factor, transforming growth factor-beta, vascular endothelial growth factor, epidermal growth factor, basic fibroblast growth factor, and Insulin-like growth factor 1. A common misconception is that PRP is a stem cell treatment. PRP is not a stem cell procedure as the blood contains little if any circulating mesenchymal stromal cells (MSCs, aka stem cells) in comparison with bone marrow.
The presence or absence of leukocytes in PRP is important. Leukocytes are essential mediators of the inflammatory response, that assist the host defense in protection against infectious agents, and contribute to wound healing.49 Although leukocytes aid in the protection against infectious agents, they can also oppose the intended healing effects of the platelets. Boswell et al. proposed that reducing leukocyte concentrations in PRP is more important than maximizing the PRP.49 It is important to note that red blood cells are eliminated from the PRP preparation as the iron contained in heme can release cytotoxic oxygen free radicals which can be a toxic/destructive process in human synoviocytes.48 Of note, application of PRP in individuals on NSAIDs is not recommended as NSAIDs inhibit platelet degranulation and therefore inhibit platelet function and may have a diminished therapeutic effect.48,50
Types of PRP and why does it matter?
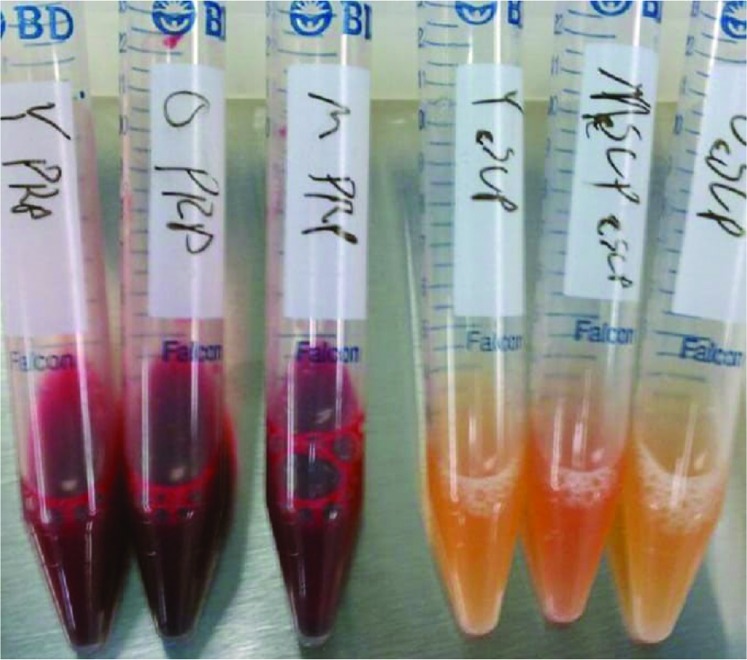
There are two types of PRP that are used for injections: 1) Leukocyte rich (LR-PRP) which is red in color and is rich in red (RBC) and white blood cells (WBC); 2) Leukocyte poor (LP-PRP) which is white blood cell (leukocyte) and red blood cell poor51 as shown in Figure 1.
Figure 1.
Vials on the left of picture are red LR-PRP which has high concentration of platelets and also contains RBCs and WBCs. The amber colored vials on the right of the picture are LP-PRP without the RBCs or WBCs which contains the concentrated platelets as well. Used with permission from Centeno-Schultz Clinic.
The composition of the preparations continues to be a widely debated topic for standardization proceedings and what types are better for which structures of the musculoskeletal system. Based on the literature for knee OA, the red LR-PRP can be toxic to synoviocytes,52 and on the other hand the amber has been shown to stimulate cartilage better than the red53 and was found to have more functionality and pain relieving benefits as compared to the red.52 The concern with removing the RBCs and WBCs is that healing cells are being eliminated, however it has been shown that taking out the RBCs and WBCs did not impact the PRPs ability to heal.54 The debate with maintaining leukocytes is that that type of PRP also maintains neutrophils which can be harmful to healing tissues and increase the inflammatory response. However, that leukocytes generally maintained are monocytes and lymphocytes which have been shown to be present with stem cells and thus a higher percentage theoretically increases stem cells.55 Leukocyte rich PRP (amber with white blood cells) was shown to decrease cytokine production and promote tissue regeneration56 in tenocytes. More studies need to be conducted on the specific types of PRP in order to better stratify a standardized treatment protocol.
Does concentration matter?
Berger et al. demonstrated that concentration matters with reference to healing potential.57 Age plays a role in how much blood is needed to concentrate in order to obtain the desired effect; therefore, older cells tend to require higher PRP concentrations to kick start the healing cascade. Berger et al. concluded that higher concentrations of platelet lysate can induce tenocytes to heal tendinopathies in older populations.57
Clinical Evidence
Tendinopathy
Based on the previously described heterogeneity in processing, PRP has had variable reports of efficacy in the literature. PRP for common extensor tendinopathy has demonstrated efficacy in treating chronic common extensor tendinopathy when compared to steroids at one- and two-year follow-ups.48,58,59 Examination of the results of treatment of Achilles and patellar tendinopathy in case series60-69 and retrospective studies70-72 has demonstrated that PRP injections improved function and pain with good functional outcomes for about four years post-injection. Many studies of rotator cuff tendinopathy have been performed with platelet rich fibrin injections done intraoperatively, however, platelet rich fibrin differs in concentration as compared to that which is used in PRP for tendinosis, not in an operating room setting. Gumina et al published on intraoperative PRP fibrin which improved repair integrity for large tears without an associated greater improvement in function73 and had lower re-tear rates for small to large tears at one year.48,73-76 Mautner et al. studied the optimization of ingredients for tendinopathy concluded that higher platelet counts with leukocytes and a slightly acidic pH injected under ultrasound guidance may be ideal to facilitate the healing of tendinopathies that have failed other conservative management.55
PRP in Osteoarthritis
Osteoarthritis (OA) is related to intraarticular cartilage loss from a joint space, due to injury or joint instability, and is related to the inadequate healing cascade of articular cartilage, leading to subsequent additional degeneration. Laver et al. performed a systematic review which encompassed the treatment of hip and knee OA.77 Twenty-six of the included studies examined knee OA and three studies examined hip OA, and the results demonstrated variability in PRP processing, all injections were directed intraarticularly without other periarticular structures however the authors concluded that PRP can be beneficial for both knee and hip OA in terms of pain and functionality.77 Another systematic review conducted by Shen et al. demonstrated that intraarticular PRP injections are more efficacious in treatment of knee OA in terms of pain relief and functional improvement at 3, 6, and 12 months follow-up compared with other injectates (saline placebo, hyaluronic acid [HA], ozone, and corticosteroids).78
Most studies that have been performed are only performed via an intraarticular approach not taking into consideration the entire joint and treating the instabilities (such as laxity of ligaments) that may have led to the osteoarthritis to begin with. However, a pilot study on knee osteoarthritis published by Sit et al, described a PRP injection protocol that involved a single intraarticular injection and extraarticular injections in the medial coronary and medial collateral ligaments.79 This is the start of exploring whether concomitant intra-articular and extra-articular PRP injections are feasible in producing a favorable outcome.79 In order to have decreased pain in osteoarthritis, off-loading the region of cartilage that is subjected to the highest force is important to prevent further degeneration, and part of rehabilitation protocols post knee procedures would be to recommend an unloader brace. It is important to note that treatments offered to date cannot regrow cartilage, however injecting the structures surrounding a lax or unstable joint can help to stabilize and improve the healing environment to improve pain and function.
Lumbar Radiculopathy
Low back pain with radiculopathy is treated most commonly with an epidural steroid injection which is the most commonly performed pain management procedure in the United States.80-82 The side effects of steroids have led to the trial of orthobiologics in the spine. Clinical evidence for PRP in the literature are mostly limited to treatment of facet and intradiscal pathology.80,83-85 Bhatia performed a small pilot study of PRP for the treatment of radiculopathy and reported gradual improvement in Visual Analog Scale, straight leg raise test and Oswestry Disability Index sustained over three months.86
Platelet lysate (PL) may be preferable to PRP for the treatment of radicular pain as PRP carries a potential for platelet adhesion and aggregation which increases the risk of vascular occlusion.87 PL is created by lysing platelets and removing cell debris, resulting in GF-rich (Growth Factor-rich) injectate, devoid of other platelet material.88 PL also has been shown to promote the proliferation of various cell types including mesenchymal stromal cells (MSCs) aka stem cells.89 PL has also been shown to be beneficial in peripheral nerve regeneration in patients with peripheral neuropathy and peripheral nerve regeneration after injury.90-95 Centeno et al. published a retrospective review of 470 patients treated with platelet lysate for lumbar radicular pain, and tracked them for 24 months.80 Over 72% of these patients reported significantly less pain after treatment which was sustained for 24 months.80 Patients also reported increased function over time which may suggest continued effect of PL over time.80
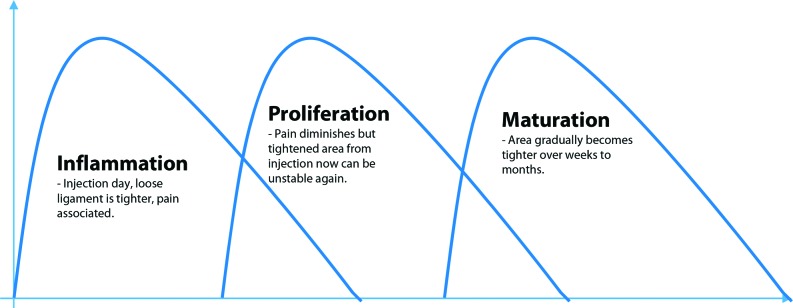
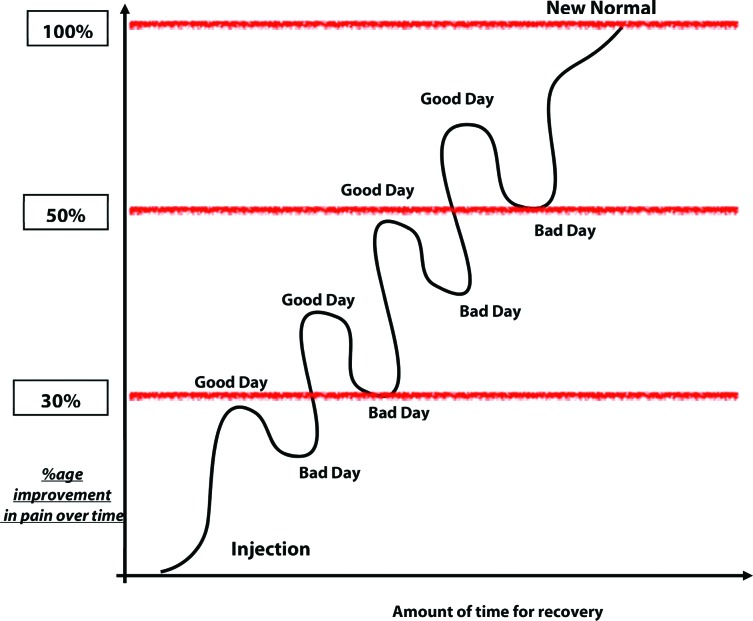
PRP and PL therapies tend to have a prolonged recovery time, which are directly correlated with the healing cascade and the phases of healing as portrayed in Figure 2:
Figure 2.
Depicts the healing cascade as it relates to healing after a PRP injection.
The general timeline depicted in Figure 4 can be extrapolated to represent the phases of healing involved and how long it takes with PRP injections. However, there is a range among patients as this depends on the structure being treated. For example, in mild knee osteoarthritis the initial inflammatory flare can last from a few days to a week and then the patient will start to feel better over the course of a few weeks, and in this scenario the LR-PRP vs LP-PRP does not seem to make a difference in flare response. The flare response and timing after an injection varies. Figure 5 demonstrates the level of pain and how it can be gradual with “ups” and “downs” prior to completely healing. Joints tend to be “faster responders” than tendons and ligaments. Typically, tendons and ligaments can take up to two to three months to feel improvement. One study on patients with lateral epicondylosis noted that significantly more patients noted improvement at six months than the three month mark post procedure.89 Also, in reference to pain, the patient may experience waxing and waning pain symptoms, and may take a “one-step forward, two-steps backward” approach with a trend being towards the positive as portrayed in Figure 3.
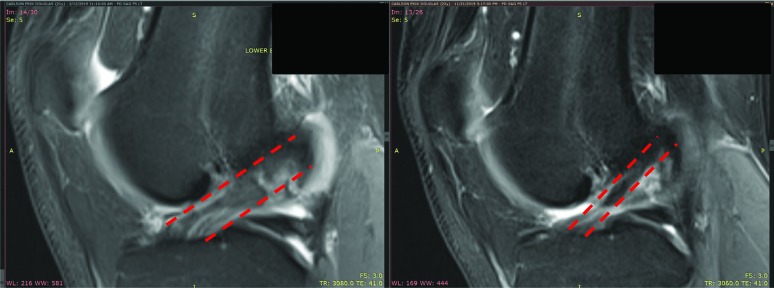
Figure 4.
Pre and post MRI 9 months apart from Bone marrow stem cell injection into ACL and surrounding knee structures. Copyright release of photograph obtained during patient evaluation.
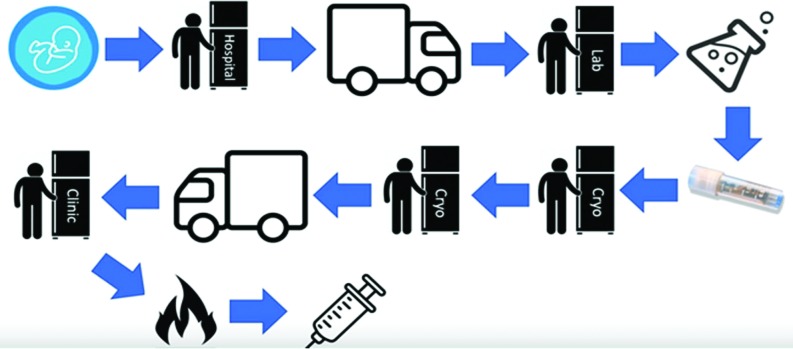
Figure 5.
The process that amniotic products go through prior to injection.
Figure 3.
Describes the ebb and flow of recovery after a PRP or Stem cell injection. There will be “Good” days and “Bad” days but the natural course will slowly progress to a decrease in pain, and tightening of the ligament and tendon. PRP has a shorter time course than stem cell treatments, however every patient varies on recovery rate.
Is PRP treatment permanent?
If the disease process is in degenerative nature, the relief from PRP can last from one to two years in mild arthritis, however in more severe arthritis pain relief may only last a few to six months. In cases of arthritis, PRP works to attempt to improve the environment to help with pain but does not alter (regrow or regenerate cartilage) a degenerated joint. There are current trials being conducted on how the knee microenvironment and content within the synovial fluid can play a role in pain control.
It is important to note that when using orthobiologics to treat tendons or ligaments the theory is that this intervention is more of a semi-permanent solution as it is assisting in repairing the tendon. With that said, many tendons can be stubborn and ligaments may require multiple treatments prior to deeming them as “healed”.
The next orthobiologic is stem cells which can be harvested from bone marrow and fat, which contains nucleated cells and growth factors that serve to start the healing cascade.
Stem Cells
Stem cells have become a much-debated topic in the media, with the biggest difference being between embryonic and adult stem cells. From a treatment standpoint there is also a debate on how the adult cells are harvested and what the yield of cells is and how they are being processed which is what impacts treatment efficacy.
Orthopedic surgeons have been using bone marrow aspirate in the use of non-union fractures and avascular necrosis for many years. A recommended treatment was first described in 1939 for non-union fracture that improved implantation of cancellous bone chips from the proximal tibia to stabilize the fixation.96 Hernigou et al. have been performing bone marrow stem cell injections into avascular necrosis lesions of the hip and knees which has been demonstrated to be a successful alternative to replacement in some patients.96-98
What cells sources for Stem Cells are used in orthopedics?
The most common cell types include: bone marrow nucleated cells, adipose stromal vascular fraction (SVF), adipose fat grafts, and amniotic fluid stem cells, listed in order in which they will be discussed. There are two types of groups in the stem cell world and that is allogeneic (comes from another person) or autologous (comes from the person themself). Allogeneic stem cells are most commonly from the amniotic cord blood, followed by amniotic and embryonic tissues. Autologous stem cells are most commonly from bone marrow aspiration or adipose-derived. The process of autologous-derived stem cells that is extracted from bone marrow or fat results in a heterogenous mixture of cells that can be centrifuged and lysed to create a more concentrated stem cell product. The process of taking cells out and concentrating them for use in orthopedic procedures under US FDA regulations is classified as “minimal manipulation”94,99 and legally acceptable. After the process of centrifugation, the resultant solution must be reinserted back into the patient within 24 hours in order to also meet the regulation standard of “minimal manipulation”. Any cell that is removed and cultured in vitro to increase the cell concentration over a number of weeks is not considered “minimal manipulation”99,100 and is currently illegal in the United States.
Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) was a term coined in the 90's to represent a class of cells that has in vitro capacity to form bone, cartilage, fat and other tissues via the mesogenic process.101,102 Because of their multi-potent capabilities, MSC lineages have been used successfully in animal models to regenerate articular cartilage.103-117 In 2006, The International Society for Cellular Therapy recommended that cells should fulfill the following criteria to be considered as MSCs: 1) the cells must adhere to plastic in culture conditions; 2) must express CD markers, which are cluster for differentiation (CD) cell surface glycoprotein antigens such as 73, 90 and 105, and cannot express CD 34, 45, 14, 11b and 19, and cannot express HLA-DR; and 3) they should be able to differentiate into osteoblasts, chrondroblasts, and adipocytes in vitro.118
The perceived risk of these types of orthobiologic cell therapies has been the risk of cancer or tumor formation, however, Hernigou et al. published a 12.5 year follow-up of 1873 patients receiving autologous bone marrow-derived stromal progenitors and found no increased cancer/tumor risk at site of placement or in any other distant site.119 Centeno et al in 2016, reported on a total of 3012 procedures along with 2373 patients followed for up to 2.2 years demonstrated seven cases of reported neoplasms (lower than general population) and concluded that there is no increased risk of neoplasm with MSC treatment.120
What are the sources of MSCs?
Bone marrow aspiration is a technique used to harvest bone marrow concentrate (BMC) which is derived from bone marrow stroma. The safest way to harvest this is with ultrasound or fluoroscopic guidance at the posterior iliac crest, as this has been shown to have the highest concentration of bone marrow MSCs.121 Multi-site draws of small volumes have been shown to yield the highest number of total nucleated cells.122 Hernigou et al. published positive outcomes on patients being treated with higher concentration of colony forming units (CFU) of BMC123,124 than lower concentrations that are found in raw bone marrow aspiration without concentrating it. Regarding dose, a higher concentration of total nucleated cells (TNCs) within bone marrow concentrate demonstrated more improvement and pain and function than lower concentrations,125,126 and Centeno et al. found TNC concentrations of >4x 108 to be the most effective.125
Adipose tissue is another source for harvesting MSCs via lipoaspiration of subcutaneous fat from areas such as the abdomen, flank, perigluteal region and thighs. However, studies have shown that bone marrow MSCs have greater intrinsic osteogenic and chondrogenic differentiation potential when compared with adipose MSC's.127,128
Synovial MSCs came into favor with the hypothesis that MSCs closest to the target tissue would better differentiate into that target tissue. Koga et al. noted that synovial MSCs have the greatest chrondrogenic potential and lowest osteogenic potential, while bone marrow has the greater osteogenic potential than does adipose.129 The utility of synovial MSC harvest is limited as it is low volume and the concentration cannot be improved without culture expansion, therefore this may be a consideration to be used in culture expansion techniques in the future.
Bone Marrow Concentrate (BMC) Clinical Research
Knee osteoarthritis is a common joint pain that afflicts approximately 50 million adults with a large healthcare expenditure.129-132 And the common regimen for people with severe osteoarthritis is non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, steroid injections or knee arthroplasty (TKA). Steroid injections have been shown to hasten the progression of cartilage loss.132,133 Complications of the above treatment options to date have many side effects and can be riddled with complications such as deep vein thrombosis and neuropathy with persistent pain after a TKA occurring in approximately 34% of patients.132,134,135 Cell based therapies have been researched previously and have some encouraging results although few controlled trials exist.132,136,137 Centeno et al. published a randomized controlled trial of a specific protocol of image-guided percutaneous injection of a combination of bone marrow concentrate (BMC) and platelet products versus an exercise therapy regimen. Comparing the exercise therapy group to the BMC group it was noted that there was significant improvement in activity levels, pain, ROM and stability at three months in the BMC group over those who followed a home exercise program alone.132 All of the exercise therapy group crossed over to the BMC group, and it was noted that at a two year follow-up there was still noted to be significant improvement in pain and function that was sustained after the BMC procedure.132
Centeno et al also conducted a prospective case series injecting autologous bone marrow concentrate as an investigational approach to treatment of anterior cruciate ligament (ACL) tears.138 Patients included in the study had sustained Grades 1-3 ligament injury, with 1cm or less of retraction.138 Grade 1 was defined as partial tear with less than half of the ligament disrupted, Grade 2 was defined as partial tear with greater than half of the ligament disrupted and Grade 3 was defined as a completely torn ligament.139 Seven of ten patients completed all pre- and post-procedural outcome measures including pre- and post- intervention imaging and demonstrated improvement in at least four of the five measures which were the Numeric Pain Scale (NPS), the Lower Extremity Functional Scale (LEFS), the International Knee Documentation Committee (IKDC) form, a modified version of the Single Assessment Numeric Evaluation (SANE), and grey scale measurements of the MRI to determine healing. Four of the five measures were statistically significantly different including the LEFS, SANE, IKDC and MRI grey scale measurements. ImageJ software was used to measure MRI pixel intensity and a trend towards darker ACLs (indicates more normal appearing) was demonstrated in five subjects, three of those subjects the change in pixel quality was statistically significantly different, however not completely normal appearing.
Figure 4 demonstrates an MRI of a torn ACL at left and post procedure on the right, and this is an example of an MRI that was examined using ImageJ software, however the improvement is apparent to the naked eye. Post procedural rehabilitation was given with the goal of advancing activity as tolerated and allow the patient to load the ligament dependent on pain since past studies had demonstrated loading as being essential to ligament healing.138,140 Bracing was not part of the protocol and therapy regimens were not standardized. The authors concluded that although it was a small case series, the precise injection of autologous bone marrow-derived nucleated cells into the ACL maybe a viable treatment method for Grades 1,2 and non-retracted Grade 3 tears.138
Centeno et al studied a total of 115 shoulders in 102 patients who were treated with autologous BMC injections for symptomatic osteoarthritis at the glenohumeral joints and/or rotator cuff tears.141 Shoulders treated with BMC noted a statistically significant different in NPS of 44% reduction in pain when the minimum important difference is defined as 30%, with functional improvement and pain reduction that started at one month post treatment and was noted to be sustained for up to two years.141 No serious adverse events were reported after the procedures.141
PRP vs Stem cells for treatment
The public often struggles with which type of intervention to consider. The options are vast and poorly understood by most, thus, the best way to describe the difference is with a construction site analogy. Stem cells are known as the general contractor coordinating the repair job, and if needed can turn into “brick and mortar” cells as well. PRP provides the supplies needed to do the job. The general consensus is that PRP is better for mild arthritis and partial ligament tears and stem cells is better for treating more severe arthritis and bigger tendon tears.132,142 Controversy remains regarding exact recommendations and research providing direct comparison between prolotherapy, PRP and stem cells, however preliminary studies are leaning towards the consensus above, and further randomized controlled, multi-site studies are needed to better stratify pathology to specific treatment required.
The following orthobiologic procedure to be discussed is culture-expanded stem cells which are currently not legal in the United states, however it is an important technique to discuss as it is the next step of treatment for potential enhancement of more significant healing than existing treatments. As it has been shown that higher concentration of MSCs can lead to greater reduction in pain and promote proliferation of cartilage for tissue healing.143,144
Culture Expanded MSCs Clinical Research
Culture-expanded MSCs are MSCs that are plated on plastic and grown for weeks at a time to multiply the number of stem cells yielded and increase the TNC for better healing potential and pain relief, as stated above. This design is currently illegal in the United States due to the regulation of section 351 of the Public Service Act (42 U.S.C. 262) as it is considered “more-than-manipulated” cellular therapy.142
Centeno et al. studied six patients who received injections of adult autologous culture expanded MSCs in their thumb CMC joints. Preoperative radiographic reading demonstrated two patients with Grade 2 OA (obvious arthrosis), and four patients with Grade 3 OA (destroyed joint) of the first CMC.145,146 The authors concluded that the injection of culture-expanded MSCs with platelet-derived growth factors into first CMC joint of the hand was associated with positive outcomes similar-to those reported with arthroscopic hemitrapeziectomy with tendon interposition.147 However, this was only a case series and further studies with larger sample sizes and randomization is necessary for direct inference on whether culture-expanded stem cells can replace surgical options.
Centeno et al published on the treatment of lumbar degenerative disc disease of culture-expanded mesenchymal stem cells into the discs of the lumbar spine as a prospective pilot study of 33 patients for up to six years. The study demonstrated that patients had improvement in pain from three months to six years, along with SANE improvement of 60% and 20 of 33 patients underwent post-treatment MRI and 85% had a reduction of disc bulge of 23%, without any significant adverse events.148 Prior to this study in 2010, Centeno et al tested the safety and feasibility of culture-expanded MSCs in the spine and demonstrated no tumorgenicity and no significant adverse events.149
Allogeneic (Amniotic) Products
The drive behind the production of allogeneic products is to create a substance that can be “shelf-stable” and can provide benefit without subjecting the patient to the harvesting process of autologous stem cells.
However, these allogenic products do contain growth factors, interleukins, and hyaluronic acid,150,151 which is an important point as there could be some utility in these products to help stimulate healing via other growth factors that are present in amniotic products and not in PRP. Therefore, using allogenic products as an adjunct therapy to autologous therapy is a much more promising option than amniotic products in isolation.
What do amniotic or cord blood product viability numbers really mean?
Viability testing is performed on products as a snapshot to discern how many cells are “alive” but does not factor in the health or vitality of the live or viable cells. Therefore, no matter if the cells are barely alive similar-to a sick patient on life support, versus a cell that is alive similar to an individual who is active and running or working out. In short, viability testing does not measure whether the cell functions. Accordingly, percentage of viability can be a misleading number, and due to the manufacturing process of amniotic products as demonstrated in Figure 5, it is speculated that the cells are essentially nonfunctional and not living by the time an injection occurs into the patient.
The process of making an amniotic product is not as pure as taking it straight from the umbilical cord then transporting it to the lab for processing and then injecting it into the patient. The process that actually occurs is demonstrated in Figure 5, and when the baby is born the cord blood is taken into freezer storage and later gets transported into the lab for processing and packaging which is then cryopreserved, until it is sold to the clinic. When ready to be used, the product is flash warmed to room temperature very quickly and gets injected into the patient. The cells that were viable at the lab processing phase have gone through such a drastic change during the distinct process of flash warming additional cells may lose viability (especially those that were barely hanging on to begin with). Therefore, by the time the patient receives the injectate the cord blood that was taken originally is likely no longer viable living tissue.
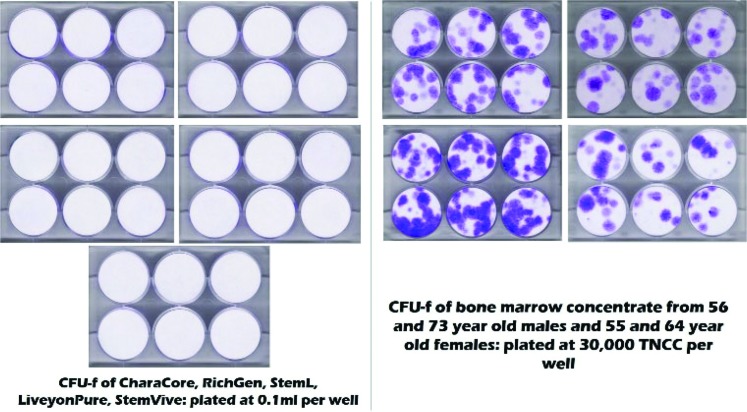
Unpublished data courtesy of Centeno-Schultz Clinic demonstrate the lack of living stem cells via direct comparison of amniotic products versus older adult bone marrow stem cells in Figure 6 below.
Figure 6.
Assessment of colony forming units (CFU-F, aka, MSC colonies) which are the purple dots on the right, and absent on the left. The left side demonstrates the absence of nucleated cells. TNCC = total nucleated cell count. Used with permission from Centeno-Schultz Clinic.
Also, a veterinary research scientist from Cornell University conducted independent research and concluded that out of 11 amnion products currently on the market that were tested, no living cells and low growth factor levels were noted in all products. She concluded in her talk at the AMSSM Sports Medcast and BMJ talk medicine Episode #360 with, “The amnion field is the wild west right now”.152
Other studies have demonstrated similar results. Secco et al. examined 10 matched umbilical cord and amniotic cord samples, and the authors were only able to culture out MSCs from one (10% recovery) noted from umbilical cord blood.153 Sibov et al. plated 118 umbilical cord blood units with only 11 containing MSCs (∼10% recovery)154 and finally, Divya et al. plated 45 umbilical cord blood samples, nine of which generated MSCs (20% recovery), however the timing for growth in culture was approximately 2-3 weeks.155
Are these products approved by the FDA? Comparisons between donor tissue products and PRP
There are two pathways for FDA approval of donor tissues that are designated sections through the Public Health Service Act (PHSA) are: 1) 361 registration that is largely unregulated and 2) 351 cellular drug approval142 and uses these two sections for interventional orthobiologic products for regulating biologics. Current amniotic products on the market have only a 361 registration which requires no clinical trials or data. The 361-registration process involves only a check box form that is performed online. However, when companies claim to have living cells this makes the products a drug and many of these companies are riding the line between an online registration which is 361 versus a 351 which includes obtaining grants and funding for research and Stage 1, 2, and 3 clinical trials that can take up to 5-10 years for approval. Many of the companies are likely selling dead umbilical cord stem cells but discuss the research on their websites from a completely different perspective, claiming live culture-expanded umbilical cord stem cells, which is what is known as the classic “bait and switch”.
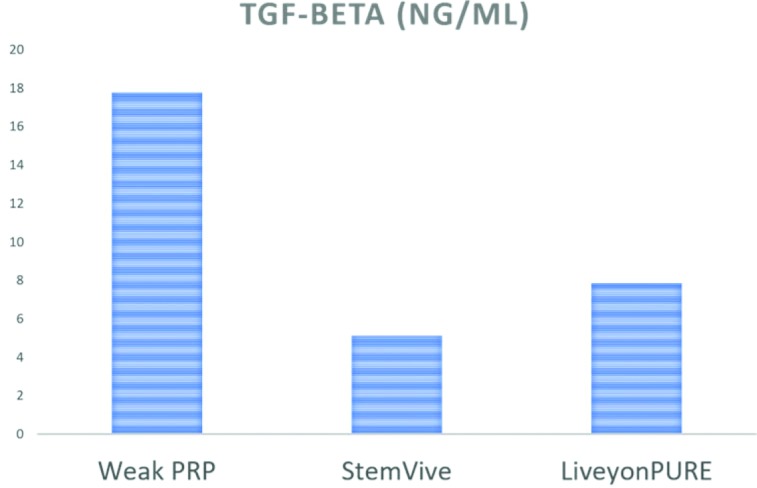
Based on an internal research assessment from the Centeno-Schultz clinic, what the amniotic products do have is a variety of growth factors, however when the growth factors in LiveyonPure and StemVive were analyzed in comparison to a weak PRP of approximately two times more concentrated than platelet content in whole blood, and the results are displayed in Figures 7-11. Transforming Growth Factor (TGF-beta) is a good growth factor that should be present for positive results with biologic therapy. As shown in Figure 7, 2x PRP demonstrated superior density over both amniotic products.
Figure 7.
Transforming Growth Factor (TGF-beta) demonstrated higher amounts in a weak PRP formulation than in two amniotic products: StemVive and Liveyon Pure. Used with permission from the Centeno-Schultz Clinic.
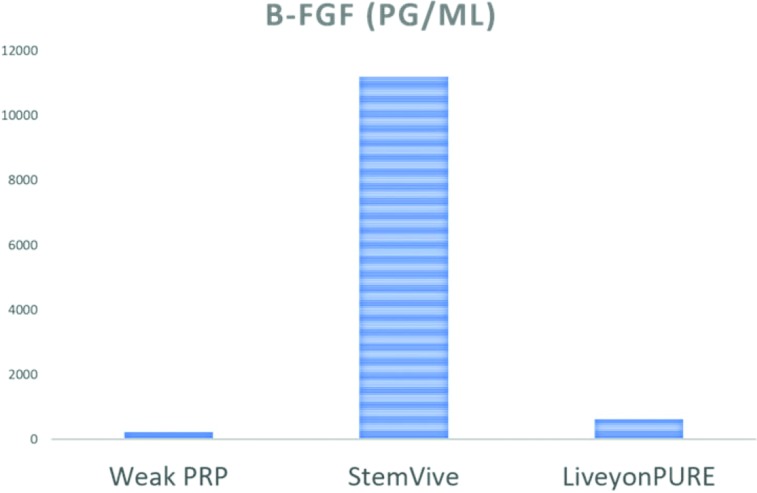
Figure 11.
bFGF, a positive growth factor for tendon healing, StemVive had the greatest content with Weak PRP and Liveyon Pure demonstrating minimal content. Used with permission from the Centeno-Schultz Clinic.
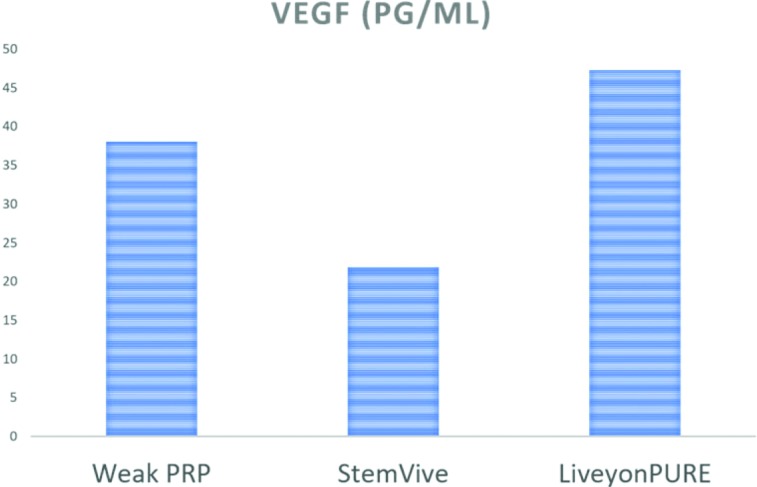
Vascular endothelial growth factory (VEGF) is important for helping develop new blood vessels. As shown in Figure 8, internal data from the Centeno-Schultz clinic demonstrated that weak PRP (2x concentration) has a lower concentration of VEGF as compared to LiveyonPURE, however this low of a concentration would not be used therapeutically. However, using a traditional 7x-14x concentration (moderate strength PRP) could demonstrate greater concentration of VEGF.
Figure 8.
Vascular Endothelial Growth Factor (VEGF) higher contents in Liveyon Pure > PRP 2x > StemVive. Used with permission from the Centeno-Schultz Clinic.
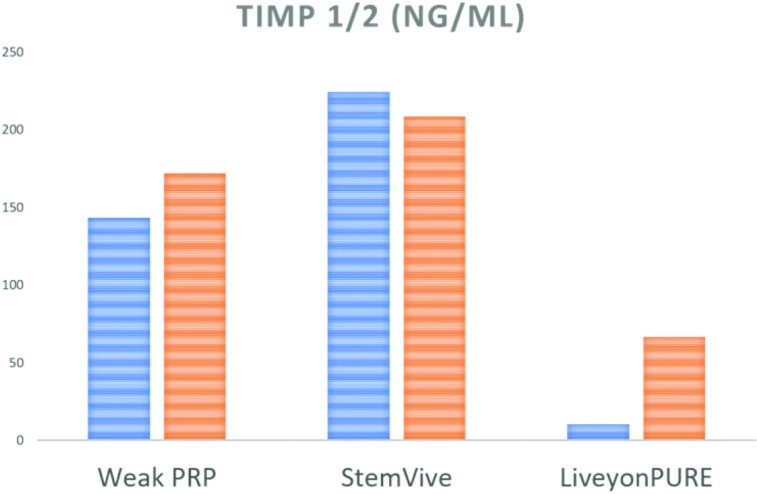
Tissue Inhibitor of MetalloProteinases (TIMP) is an anti-breakdown cytokine that may help protect joints against OA. The internal data demonstrated that StemVive had higher concentrations than weak PRP or LiveyonPURE. However, as noted above in a traditional 7x-14x PRP the levels could be higher than in the weak PRP solution as displayed from internal data from the Centeno-Schultz clinic in Figure 9.
Figure 9.
Tissue Inhibitor of MetalloProteinases (TIMP) 1 in blue and 2 in orange are noted to be highest in StemVive > PRP2x > Liveyon Pure. Used with permission from the Centeno-Schultz Clinic.
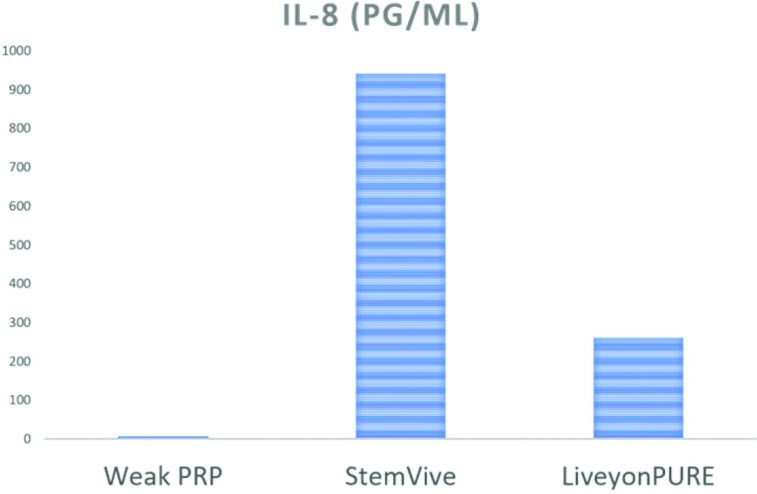
Interleukin-8 (IL-8) on the other hand is a cytokine that is potentially negative to healing, as it can attract white blood cells and increase inflammation in an area. To give a clinical example, the serum blood levels of IL-8 in a knee arthritis patient are generally lower than 10pg/mL, however in this study the composition of IL8 in the internal data demonstrated that LiveyonPure was almost 300 and in Stemvive was more than 900 as displayed in Figure 10 (internal data from the Centeno-Schultz clinic). This concentration could indicate increased inflammation without promoting the healing cascade. There is an epigenetic study by Takahashi et al. that correlated increased IL-8 to the progression of OA due to inflammation and reports IL-8 as a possible target for decreasing inflammation by modulating expression.156
Figure 10.
Interleukin-8 (IL-8), an inflammatory cytokine, ideally would need to be low to nonexistent, and StemVive had the most followed by LiveyonPure, then Weak PRP. Used with permission from the Centeno-Schultz Clinic.
Basic Fibroblast Growth Factor (bFGF) is a good growth factor that promotes the growth of tendon cells, the internal data from the Centeno-Schultz clinic demonstrated that the higher concentrations in some solutions could explain why some providers are noting positive results with tendon type injuries such as rotator cuff tears. As noted in Figure 11, bFGF was highest in StemVive and much lower in the weak PRP and LiveyonPure samples.
Other internal Centeno-Schultz clinic data has tested two additional birth tissue products and found that StemVive produced more bFGF than the other two products, which is impressive however clinical translation of these findings is unknown to date, and only speculative benefit may be seen in tendinopathies.
Allogeneic products in summary
Growth factors are present in widely variant levels in various preparations used in orthobiologic interventions, as demonstrated in the figures above. Which of those could prove beneficial in treatment of stubborn tendons due to bFGF levels being higher is yet unknown due to the lack of research comparing amniotic products to weak PRP in the treatment of tendons. The mislabeling of amniotic stem cells is what brings about much debate, however the proposition of calling them amniotic growth factors may be a new discussion. To date, the indications for amniotic products are not clear, and the risk for possible donor/recipient mismatch and cell dose are amplified with multiple transfusion exposures (aka, multiple injections) that might sensitize the recipient to donor alloantigens and cause the recipient to have an immune response against the product.157 This graft versus host reaction could prove much more harmful than the benefit of improving tendinopathy, however more studies are needed.
CURRENT REHABILITATION CONSIDERATIONS IN REGENERATIVE ORTHOPEDIC MEDICINE
Research on rehabilitation protocols for regenerative procedures is lacking. To date, there are no standard protocols for rehabilitation after interventional orthobiologic procedures in humans. However, animal studies exist that corroborate the mechano-transduction model for promotion of healing. In the equine population undergoing PRP injections, it has been shown that controlled gradual return to activity is the best course of action, with restricted exercise in the acute and subacute phases of tendon and ligament healing being paramount.158
McKay et al. recently published proposed regenerative rehabilitation guidelines and proposed protocols for the treatment of knee osteoarthritis.159 They suggest that moderate physical exercise decreases the progression to severe knee osteoarthritis by inducing a protective effect against cartilage degradation.15,159 A common issue in patients with knee osteoarthritis is weakness of the quadriceps which has also been correlated with ligamentous instability and therefore inactivity as a result.159,160 There are patients that have weak muscles and have ligamentous laxity and those with strong muscles but continue to have ligamentous laxity.159 In those patients that have weak muscles, muscle strengthening is beneficial, and in those with strong muscles, knee stabilizing exercises are necessary.160 A combination of interventions targeting restoration of mobility, strength, stability, proprioception and neuromuscular control is recommended in post orthbiologic rehabilitation due to the role rehabilitation plays in chondrocyte stimulation and role in improving function of patients with knee OA159 after orthobiologics.
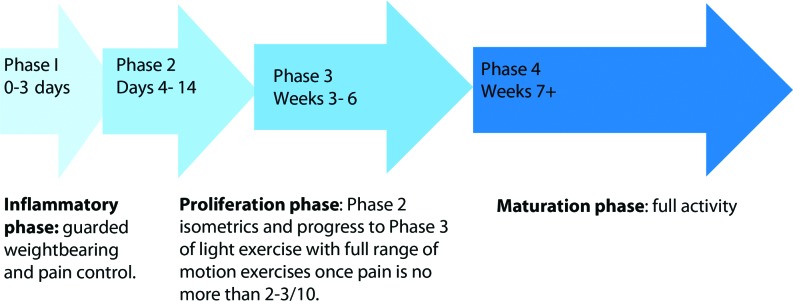
General rehabilitation guidelines exist for PRP and stem cell therapy which involve four phases of therapy. The following example applies the four phase approach to the rehabilitation of a patient with various joint pathologies after PRP48 which can be extrapolated to stem cell therapies however typically with a longer time course of action to allow for healing. See descriptions in Table 1 and a graphic display in Figure 12.48
Table 1.
Descriptions of the four phases of rehabilitation, in general after a orthobiologic procedure.
| Phase 1: Begins during post-injection day 0 to 3, and the goal is protection of the injected region and pain control. | Immobilization and/or complete unloading (non-weigh bearing status) of affected joint can be avoided in the lower extremity, however, a sling may be considered for shoulder and unloading brace for knee OA. Partial weight bearing with crutches for AVN of hip and use of a walking boot for ankle/foot pathologies should be utilized. Gentle range of motion out of the immobilizing device should be performed passively and actively (to tolerance) for short durations (2-3 minutes), multiple times per day (3 times). |
| Phase 2: enconroasses days 4 to 14 with the goal of increasing tissue tolerance to loading and discontinue immobilization/unloading devices and slowly progress to weight bearing and avoid shear stress. | Continue active and passive range motion activities for 3-5 minutes/session, 3-5 times a day. Begin sub maximal isometric exercises for affected tendons/joints, begin progressive loading for lower extremity pathologies, unloaded cycling, and core stability exercises. Proceed to next level if pain score is at or under a 2 out of 10 on a visual analog scale. |
| Phase 3: encompasses weeks 3-6 with the goal of full range of motion to affected joint, increase tissue tolerance to loading and improve strength/endurance. | For knee and Hip OA can walk as much as tolerated and start jogging. Biking with hills, and experience no more than 2/10 mild pain. For shoulder OA can start upper body light exercises along with modified yoga and biking |
| Phase 4: encompasses weeks 7+ with the goal of return to full activities that were being performed prior to procedure. | No strict restrictions are advised, gradual return to full functional activity is recommended. The target for 100% of desired activities is at 8-12 weeks. |
Figure 12.
General phases of healing summarizing the regenerative rehabilitation process.
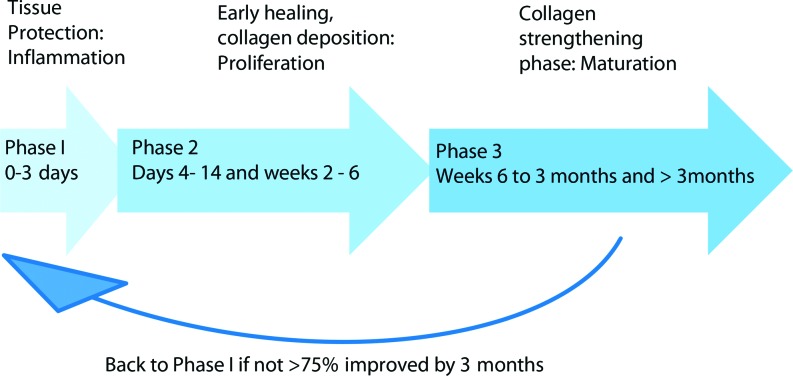
A suggested rehabilitation protocol following platelet-rich plasma for treatment of tendons is slightly different to the OA model above, this protocol encompasses three phases versus four phases as noted above in the protocol for treatment of joints.55 See descriptions of the phases in Table 2, along with a summary of the phases in Figure 13.55
Table 2.
Descriptions of the three phases of rehabilitation, in tendinopathy after an orthobiologic procedure.
| Phase 1: Begins days 0-3 after intervention and focuses on tissue protection due to the likelihood of tissue inflammation. | For tendons of the LE, the patient should be non-weightbearing or utilize protected weightbearing. Gentle AROM may be performed 2-3x a day for 10-15minutes, using caution to avoid excessive loading or stress on the involved/treated tendon. |
|---|---|
| Phase 2: Related to early tissue healing and facilitation of collagen deposition. This typically begins days 4-14 after intervention and lasts until week 6. | Begin to progress to full weightbearing without protective device. Start light activities and aerobic exercise that avoids loading. May begin gentle prolonged stretching and glut/core muscle strengthening. Weeks 2-6 also fall under this phase; during which time eccentric exercises should be avoided, and start low weight, high repetitive isometrics and more dynamic stretching. |
| Phase 3: Is the collagen strengthening phase, occurring weeks 6-12 post intervention. | Begin eccentric exercises (starting eccentric exercises too soon can halt the healing cascade due to halting angiogenesis due to too much load) Would recommend keeping pain scale to 2-3/10 and starting with two repetitions of 15. Progress to weight bearing functional activities in the lower quarter. Begin functional retraining of the upper quarter in patient relevant methods (weight bearing, plyometrics, etc) At months 3 + reassess improvement and if not >75% improved from original injury, consider repeat injection and return to Phase 1. |
Figure 13.
Three proposed phases of rehabilitation after PRP injection for tendinopathy healing.
Currently, there is no consensus on rehabilitation after PRP injections but as described above, the notion of gradually increasing the load and activity as tolerated may augment the tissue healing cascade,55 along with gauging the intensity of workouts based on pain level to keep it at a minimum of 2/10 to avoid further soft tissue injury.
Therapeutic modalities that can help augment recovery after regenerative injections: Blood Flow Restriction
Blood flow restriction (BFR) is a rapidly growing therapeutic modality for helping apply load through the muscles in areas that are unable to tolerate the addition of enough load to achieve a strengthening stimulus either due to muscular inhibition or pain. It is currently being used in several post-operative conditions such as after ACL reconstructions. BFR utilizes an applied tourniquet to the extremity of the injured patient, which partially restricts the blood flow to the limb, as the patient undergoes mobilization or exercise.159,161 Takarada et al. demonstrated that with BFR, only the muscles whose bloodflow was restricted (due to the BFR) demonstrated a significant increase in muscle cross sectional area and thigh strength.162 The exact mechanism of this phenomenon is not readily understood, however the proposed mechanisms include increased selective fiber type recruitment, alterations in metabolic accumulation, activation of muscle protein synthesis, and the induction of cell swelling.163 There is also a proposed metabolite theory in which the increase in metabolic byproducts from anaerobic metabolism such as lactate and hydrogen. In BFR, the “burn” (release of byproducts of hydrogen and lactate) in the muscle that is felt during treatment releases growth factors and helps in hypertrophy and healing of the muscle.163 Which was shown in discussion about the healing cascade, that stimulating muscles improves the satellite cell population contributing to healing. In the early stages of healing the goal is to mitigate atrophy and promote healing, therefore with BFR this can be achieved with isometric-type exercises without ranging an already inflamed and otherwise painful joint. More studies are still needed to provide any direct correlation with BFR in patients that have undergone orthobiologic procedures. At this time, the theoretical perspective of BFR is compelling however will need to have more studies with patients that have undergone orthobiologic type procedures.
Whole Body Vibration
Whole body vibration (WBV) is an intervention that involves the use of a vibrating platform that changes amplitudes while the patient is either positioned statically (supine, sitting, kneeling, or standing) or performing a dynamic movement.159,164 The purpose of the vibratory stimulus is to induce reflex motor contractions which may assist in improving muscle recruitment and proprioception. In the elderly with knee OA the induction of isometric, concentric, and eccentric contractions of the hip, knee extensor muscle groups and the plantar flexors assists in improving the control and execution of functional movements such as those required for static and dynamic balance and gait performance.159,164 This modality has been shown to possibly slow the progression of cartilage loss due to the modulation of skeletal tissue, increasing oscillation of chondrocytes, and potentially augmenting thickness of the chondrocyte layer,159,165 therefore it has been suggested to be used in combination with the regenerative rehabilitation program for patients with knee OA who have been treated with orthobiologics. The theory behind whole body vibration as above is interesting, however no distinct research has been done to prove this in vivo.
CONCLUSIONS
Prolotherapy may work well in “tilling the soil” for other interventional orthobiologic techniques in order to kick start the inflammatory cascade to promote healing. Prolotherapy is used as either a first line treatment for mild instability of ligaments and/or tendons, however it will produce more collagen that is not as strong as the original collagen. PRP is a treatment adjunct for mild to moderate tendinopathy and ligamentous laxity cases. PRP seems to work best for mild arthritis by providing growth factors that help conjugation of collagen back to Type I collagen, providing collagen that is stronger and more robust than the injured structure. Finally, MSCs are used in more severe or refractory cases of tendon and ligamentous injury as well as in treatment of moderate to severe osteoarthritis that can be coupled with bone augmentation treatments in disease states that are more advanced such as avascular necrosis, bone marrow edema, or cystic changes. Although more aggressive surgeries may be warranted in refractory or severe cases where orthobiologics did not help; having an orthobiologic option coupled with targeted rehabilitation protocols would be optimal prior to moving onto surgery.
Interventional orthobiologics as a field, is in its infancy and has a long way to go to develop consensus regarding the types of procedures to utilize for various patients as well as the recommendations for physical therapy management after procedures. Such recommendations need to be formulated based on patient specifics and correlated with the mechanobiology of the body segment or tissue being treated. Being familiar with the stages of healing as they relate to orthobiologics is crucial to understanding the limitations of the patient at certain timepoints in healing and wisely choosing physical therapy interventions. The 30,000-foot view is that rehabilitation post-orthopedic surgical procedures directs more emphasis on returning a patient back to the level prior to the surgery, with the hope of gaining additional function. The goal of regenerative rehabilitation is not only to restore a patient back to the level of function prior to the injection (which is not as debilitating as surgery), but also to restore the biomechanical influences that contributed to the injury by focusing on the joint or injured area as a part of a whole. The goal of interventional orthobiologics is not only to heal damaged to tissue but to rectify the kinetics of the surrounding structure in order to optimize the body's function as a whole.
Adjunctive modalities for regenerative rehabilitation such as blood flow restriction and whole-body vibration with the goal of strengthening an injured peripheral segment rapidly in order to maintain or improve muscle mass and enhance proprioception are currently being explored. These two adjunctive interventions could facilitate the continued direction towards movement as the best rehabilitation alternative and the avoidance of immobilization and bedrest. To move orthopedics and sports medicine away from the current emphasis on pain management, the use of NSAIDs, steroid injections and rest, towards progressive movement, combined with strengthening is desired. A combined rehabilitative approach to improving biomechanics along with utilizing regenerative injections of prolotherapy, PRP and/or MSCs to induce healing and promote stability may assist in keeping joints, ligaments, tendons and muscles healthy and stronger as we age or prevent future injury in the younger population.
References
- 1.Regenerative Rehabilitation. Secondary Regenerative Rehabilitation 11/7/2017 2017. http://www.apta.org/RegenerativeRehab/.
- 2.Ng JL Kersh ME Kilbreath S Knothe Tate M. Establishing the basis for mechanobiology-based physical therapy protocols to potentiate cellular healing and tissue regeneration. Front Physiol. 2017;8:303 10.3389/fphys.2017.00303[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson WR Scott A Loghmani MT Ward SR Warden SJ. Understanding mechanobiology: Physical therapists as a force in mechanotherapy and musculoskeletal regenerative rehabilitation. Phys Ther. 2016;96(4):560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y McNamara LM Schaffler MB Weinbaum S. A model for the role of integrins in flow induced mechanotransduction in osteocytes. Proc Natl Acad Sci. 2007;104(40):15941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Head PL. Rehabilitation considerations in regenerative medicine. Phys Med Rehabil Clin N Am. 2016;27(4):1043-54. [DOI] [PubMed] [Google Scholar]
- 6.Liu SH Yang RS al-Shaikh R Lane JM. Collagen in tendon, ligament, and bone healing. A current review. Clin Orthop Relat Res. 1995;318:265-78. [PubMed] [Google Scholar]
- 7.Rand E Gellhorn AC. The healing cascade: Facilitating and optimizing the system. Phys Med Rehabil Clin N Am. 2016;27(4):765-81. [DOI] [PubMed] [Google Scholar]
- 8.Baoge L Van Den Steen E Rimbaut S et al. Treatment of skeletal muscle injury: a review. ISRN Orthop. 2012;2012:689012 10.5402/2012/689012[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jarvinen TA Jarvinen TL Kaariainen M Kalimo H Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745-64. [DOI] [PubMed] [Google Scholar]
- 10.Tidball JG. Mechanisms of muscle injury, repair, and regeneration. Compr Physiol. 2011;1(4):2029-62. [DOI] [PubMed] [Google Scholar]
- 11.Teixeira E Duarte JA. Skeletal muscle loading changes its regenerative capacity. Sports Med. 2016;46(6):783-92. [DOI] [PubMed] [Google Scholar]
- 12.Fang F Lake SP. Experimental evaluation of multiscale tendon mechanics. J Orthop Res. 2017;35(7):1353-65. [DOI] [PubMed] [Google Scholar]
- 13.McCormick A Charlton J Fleming D. Assessing health needs in primary care. Morbidity study from general practice provides another source of information. Br Med J. 1995;310(6993):1534-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magnusson SP Langberg H Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol. 2010;6(5):262-8. [DOI] [PubMed] [Google Scholar]
- 15.Sun HB Andarawis-Puri N Li Y et al. Cycle-dependent matrix remodeling gene expression response in fatigue-loaded rat patellar tendons. J Orthop Res. 2010;28(10):1380-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnoczky SP Tian T Lavagnino M Gardner K Schuler P Morse P. Activation of stress-activated protein kinases (SAPK) in tendon cells following cyclic strain: the effects of strain frequency, strain magnitude, and cytosolic calcium. J Orthop Res. 2002;20(5):947-52. [DOI] [PubMed] [Google Scholar]
- 17.Langberg H Rosendal L Kjaer M. Training-induced changes in peritendinous type I collagen turnover determined by microdialysis in humans. J Physiol. 2001;534:297-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andarawis-Puri N Flatow EL Soslowsky LJ. Tendon basic science: Development, repair, regeneration, and healing. J Orthop Res. 2015;33(6):780-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact. 2004;4(2):199-201. [PubMed] [Google Scholar]
- 20.Brommer EJ Dooijewaard G Dijkmans BA Breedveld FC. Depression of tissue-type plasminogen activator and enhancement of urokinase-type plasminogen activator as an expression of local inflammation. Thromb Haemost. 1992;68(2):180-4. [PubMed] [Google Scholar]
- 21.Rosc D Powierza W Zastawna E Drewniak W Michalski A Kotschy M. Post-traumatic plasminogenesis in intraarticular exudate in the knee joint. Med Sci Monit. 2002;8(5):371-8. [PubMed] [Google Scholar]
- 22.Thornton GM Leask GP Shrive NG Frank CB. Early medial collateral ligament scars have inferior creep behaviour. J Orthop Res. 2000;18(2):238-46. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg VM Caplan AI. Biologic restoration of articular surfaces. Instr Course Lect. 1999;48:623-7. [PubMed] [Google Scholar]
- 24.Mobasheri A Kalamegam G Musumeci G Batt ME. Chondrocyte and mesenchymal stem cell-based therapies for cartilage repair in osteoarthritis and related orthopaedic conditions. Maturitas. 2014;78(3):188-98. [DOI] [PubMed] [Google Scholar]
- 25.Nehrer S Spector M Minas T. Histologic analysis of tissue after failed cartilage repair procedures. Clin Orthop Relat Res. 1999(365):149-62. [DOI] [PubMed] [Google Scholar]
- 26.Oryan A Monazzah S Bigham-Sadegh A. Bone injury and fracture healing biology. Biomed Environ. Sci 2015;28(1):57-71. [DOI] [PubMed] [Google Scholar]
- 27.Schindeler A McDonald MM Bokko P Little DG. Bone remodeling during fracture repair: The cellular picture. Semin Cell Dev Biol. 2008;19(5):459-66. [DOI] [PubMed] [Google Scholar]
- 28.Goldhahn J Feron JM Kanis J et al. Implications for fracture healing of current and new osteoporosis treatments: an ESCEO consensus paper. Calcif Tissue Int. 2012;90(5):343-53. [DOI] [PubMed] [Google Scholar]
- 29.Vora A Borg-Stein J Nguyen RT. Regenerative injection therapy for osteoarthritis: fundamental concepts and evidence-based review. Phys Med Rehabil. 2012;4(5 Suppl):S104-9. [DOI] [PubMed] [Google Scholar]
- 30.Reeves KD Sit RW Rabago DP. Dextrose Prolotherapy: A Narrative review of basic science, clinical research, and best treatment recommendations. Phys Med Rehabil Clin N Am. 2016;27(4):783-823. [DOI] [PubMed] [Google Scholar]
- 31.Liu YK Tipton CM Matthes RD Bedford TG Maynard JA Walmer HC. An in situ study of the influence of a sclerosing solution in rabbit medial collateral ligaments and its junction strength. Connect Tissue Res. 1983;11(2-3):95-102. [DOI] [PubMed] [Google Scholar]
- 32.Rabago D Best TM Zgierska AE Zeisig E Ryan M Crane D. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43(7):471-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hung CY Hsiao MY Chang KV Han DS Wang TG. Comparative effectiveness of dextrose prolotherapy versus control injections and exercise in the management of osteoarthritis pain: a systematic review and meta-analysis. J Pain Res. 2016;9:847-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jahangiri A Moghaddam FR Najafi S. Hypertonic dextrose versus corticosteroid local injection for the treatment of osteoarthritis in the first carpometacarpal joint: a double-blind randomized clinical trial. J Orthop Sci. 2014;19(5):737-43. [DOI] [PubMed] [Google Scholar]
- 35.Reeves KD Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Altern Ther Health Med. 2000;6(2):68-74, 77-80. [PubMed] [Google Scholar]
- 36.Centeno CJ Elliott J Elkins WL Freeman M. Fluoroscopically guided cervical prolotherapy for instability with blinded pre and post radiographic reading. Pain Physician. 2005;8(1):67-72. [PubMed] [Google Scholar]
- 37.Sit RW Chung V Reeves KD et al. Hypertonic dextrose injections (prolotherapy) in the treatment of symptomatic knee osteoarthritis: A systematic review and meta-analysis. Sci Rep. 2016;6:25247 10.1038/srep25247[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dumais R Benoit C Dumais A et al. Effect of regenerative injection therapy on function and pain in patients with knee osteoarthritis: a randomized crossover study. Pain Med. 2012;13(8):990-9. [DOI] [PubMed] [Google Scholar]
- 39.Rabago D Kijowski R Woods M et al. Association between disease-specific quality of life and magnetic resonance imaging outcomes in a clinical trial of prolotherapy for knee osteoarthritis. Arch Phys Med Rehabil. 2013;94(11):2075-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rabago D Patterson JJ Mundt M et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11(3):229-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Staal JB de Bie RA de Vet HC Hildebrandt J Nelemans P. Injection therapy for subacute and chronic low back pain: an updated Cochrane review. Spine. 2009;34(1):49-59. [DOI] [PubMed] [Google Scholar]
- 42.Kim WM Lee HG Jeong CW Kim CM Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16(12):1285-90. [DOI] [PubMed] [Google Scholar]
- 43.Hoffman MD Agnish V. Functional outcome from sacroiliac joint prolotherapy in patients with sacroiliac joint instability. Complement Ther Med. 2018;37:64-68. [DOI] [PubMed] [Google Scholar]
- 44.Solmaz I Akpancar S Orscelik A Yener-Karasimav O Gul D. Dextrose injections for failed back surgery syndrome: a consecutive case series. Eur Spine J. 2019;28(7):1610-17.31115685 [Google Scholar]
- 45.Rabago D Nourani B. Prolotherapy for osteoarthritis and tendinopathy: a descriptive review. Curr Rheum Rep. 2017;19(6):34; 10.1007/s11926-017-0659-3[published Online First Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 46.Scarpone M Rabago DP Zgierska A Arbogast G Snell E. The efficacy of prolotherapy for lateral epicondylosis: a pilot study. Clin J Sport Med. 2008;18(3):248-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bertrand H Reeves KD Bennett CJ Bicknell S Cheng AL. Dextrose prolotherapy versus control injections in painful rotator cuff tendinopathy. Arch Phys Med Rehabil. 2016;97(1):17-25. [DOI] [PubMed] [Google Scholar]
- 48.Wu PI Diaz R Borg-Stein J. Platelet-rich plasma. Phys Med Rehabil Clin N Am. 2016;27(4):825-53. [DOI] [PubMed] [Google Scholar]
- 49.Boswell SG Cole BJ Sundman EA Karas V Fortier LA. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy. 2012;28(3):429-39. [DOI] [PubMed] [Google Scholar]
- 50.Schippinger G Pruller F Divjak M et al. Autologous platelet-rich plasma preparations: Influence of nonsteroidal anti-inflammatory drugs on platelet function. Orthop J Sports Med. 2015;3(6):2325967115588896, 10.1177/2325967115588896[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mautner K Malanga GA Smith J et al. A call for a standard classification system for future biologic research: the rationale for new PRP nomenclature. Phys Med Rehabil. 2015;7(4 Suppl):S53-S59. [DOI] [PubMed] [Google Scholar]
- 52.Riboh JC Saltzman BM Yanke AB Fortier L Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med. 2016;44(3):792-800. [DOI] [PubMed] [Google Scholar]
- 53.Cavallo C Filardo G Mariani E et al. Comparison of platelet-rich plasma formulations for cartilage healing: an in vitro study. J Bone Joint Surg Am. 2014;96(5):423-9. [DOI] [PubMed] [Google Scholar]
- 54.Giusti I Di Francesco M D'Ascenzo S et al. Leukocyte depletion does not affect the in vitro healing ability of platelet rich plasma. Exp Ther Med. 2018;15(4):4029-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mautner K Malanga G Colberg R. Optimization of ingredients, procedures and rehabilitation for platelet-rich plasma injections for chronic tendinopathy. Pain Manag. 2011;1(6):523-32. [DOI] [PubMed] [Google Scholar]
- 56.El-Sharkawy H Kantarci A Deady J et al. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. J Periodontol. 2007;78(4):661-9. [DOI] [PubMed] [Google Scholar]
- 57.Berger DR Centeno CJ Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019;8(1):32-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gosens T Peerbooms JC van Laar W den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1200-8. [DOI] [PubMed] [Google Scholar]
- 59.Peerbooms JC Sluimer J Bruijn DJ Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255-62. [DOI] [PubMed] [Google Scholar]
- 60.Charousset C Zaoui A Bellaiche L Bouyer B. Are multiple platelet-rich plasma injections useful for treatment of chronic patellar tendinopathy in athletesϿ. a prospective study. Am J Sports Med. 2014;42(4):906-11. [DOI] [PubMed] [Google Scholar]
- 61.Deans VM Miller A Ramos J. A prospective series of patients with chronic Achilles tendinopathy treated with autologous-conditioned plasma injections combined with exercise and therapeutic ultrasonography. J Foot Ankle Surg. 2012;51(6):706-10. [DOI] [PubMed] [Google Scholar]
- 62.Ferrero G Fabbro E Orlandi D et al. Ultrasound-guided injection of platelet-rich plasma in chronic Achilles and patellar tendinopathy. J Ultrasound. 2012;15(4):260-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Finnoff JT Fowler SP Lai JK et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. Phys Med Rehabil. 2011;3(10):900-11. [DOI] [PubMed] [Google Scholar]
- 64.Gaweda K Tarczynska M Krzyzanowski W. Treatment of Achilles tendinopathy with platelet-rich plasma. Int J Sports Med. 2010;31(8):577-83. [DOI] [PubMed] [Google Scholar]
- 65.Gosens T Den Oudsten BL Fievez E van ‘t Spijker P Fievez A. Pain and activity levels before and after platelet-rich plasma injection treatment of patellar tendinopathy: a prospective cohort study and the influence of previous treatments. Int Orthop. 2012;36(9):1941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kon E Filardo G Delcogliano M et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper's knee. Injury. 2009;40(6):598-603. [DOI] [PubMed] [Google Scholar]
- 67.Monto RR. Platelet rich plasma treatment for chronic Achilles tendinosis. Foot Ankle Int. 2012;33(5):379-85. [DOI] [PubMed] [Google Scholar]
- 68.Oloff L Elmi E Nelson J Crain J. Retrospective analysis of the effectiveness of platelet-rich plasma in the treatment of Achilles tendinopathy: Pretreatment and posttreatment correlation of magnetic resonance imaging and clinical assessment. Foot Ankle Spec. 2015;8(6):490-7. [DOI] [PubMed] [Google Scholar]
- 69.Volpi P Quaglia A Schoenhuber H et al. Growth factors in the management of sport-induced tendinopathies: results after 24 months from treatment. A pilot study. J Sports Med Phys Fitness. 2010;50(4):494-500. [PubMed] [Google Scholar]
- 70.Mautner K Colberg RE Malanga G et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. Phys Med Rehabil. 2013;5(3):169-75. [DOI] [PubMed] [Google Scholar]
- 71.Murawski CD Smyth NA Newman H Kennedy JG. A single platelet-rich plasma injection for chronic midsubstance achilles tendinopathy: a retrospective preliminary analysis. Foot Ankle Spec. 2014;7(5):372-6. [DOI] [PubMed] [Google Scholar]
- 72.Owens RFJG J Conti SF et al. Clinical and magnetic resonance imaging outcomes following platelet rich plasma injection for chronic midsubstance Achilles tendinopathy. Foot Ankle Int. 2011;11(32):1032-39. [DOI] [PubMed] [Google Scholar]
- 73.Gumina S Campagna V Ferrazza G et al. Use of platelet-leukocyte membrane in arthroscopic repair of large rotator cuff tears: a prospective randomized study. J Bone Joint Surg Am. 2012;94(15):1345-52. [DOI] [PubMed] [Google Scholar]
- 74.Castricini R Longo UG De Benedetto M et al. Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. Am J Sports Med. 2011;39(2):258-65. [DOI] [PubMed] [Google Scholar]
- 75.Chahal J Mall N MacDonald PB et al. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. 2012;28(5):720-7. [DOI] [PubMed] [Google Scholar]
- 76.Randelli P Arrigoni P Ragone V Aliprandi A Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg. 2011;20(4):518-28. [DOI] [PubMed] [Google Scholar]
- 77.Laver L Marom N Dnyanesh L Mei-Dan O Espregueira-Mendes J Gobbi A. PRP for degenerative cartilage disease: A systematic review of clinical studies. Cartilage. 2017;8(4):341-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shen L Yuan T Chen S Xie X Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12(1):16, 10.1186/s13018-017-0521-3 [published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sit RWS Wu RWK Law SW et al. Intra-articular and extra-articular platelet-rich plasma injections for knee osteoarthritis: A 26-week, single-arm, pilot feasibility study. The Knee, 10.1016/j.knee. 2019.06.018[published Online First Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 80.Centeno C Markle J Dodson E et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38, 10.1186/s40634-017-0113-5[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cohen SP. Epidural steroid injections for low back pain. Br Med J. 2011;343:d5310 10.1136/bmj.d5310[published Online First Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 82.Manchikanti L. The growth of interventional pain management in the new millennium: a critical analysis of utilization in the medicare population. Pain Physician. 2004;7(4):465-82. [PubMed] [Google Scholar]
- 83.Akeda K Ohishi K Masuda K et al. Intradiscal injection of autologous platelet-rich plasma releasate to treat discogenic low back pain: A preliminary clinical trial. Asian Spine J. 2017;11(3):380-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kirchner F Anitua E. Intradiscal and intra-articular facet infiltrations with plasma rich in growth factors reduce pain in patients with chronic low back pain. J Craniovertebr Junction Spine. 2016;7(4):250-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tuakli-Wosornu YA Terry A Boachie-Adjei K et al. Lumbar intradiskal platelet-rich plasma (PRP) Injections: A prospective, double-blind, randomized controlled study. Phys Med Rehabil. 2016;8(1):1-10. [DOI] [PubMed] [Google Scholar]
- 86.Bhatia R Chopra G. Efficacy of platelet rich plasma via lumbar epidural route in chronic prolapsed intervertebral disc patients-A pilot study. J Clin Diagn Res. 2016;10(9):UC05-UC07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wybier M. Transforaminal epidural corticosteroid injections and spinal cord infarction. Joint Bone Spine. 2008;75(5):523-5. [DOI] [PubMed] [Google Scholar]
- 88.Doucet C Ernou I Zhang Y et al. Platelet lysates promote mesenchymal stem cell expansion: a safety substitute for animal serum in cell-based therapy applications. J Cell Physiol. 2005;205(2):228-36. [DOI] [PubMed] [Google Scholar]
- 89.Burnouf T Strunk D Koh MB Schallmoser K. Human platelet lysate: Replacing fetal bovine serum as a gold standard for human cell propagation? Biomaterials. 2016;76:371-87. [DOI] [PubMed] [Google Scholar]
- 90.Abbasipour-Dalivand S Mohammadi R Mohammadi V. Effects of local administration of platelet rich plasma on functional recovery after bridging sciatic nerve defect using silicone rubber chamber; An experimental study. Bull Emerg Trauma. 2015;3(1):1-7. [PMC free article] [PubMed] [Google Scholar]
- 91.Anjayani S Wirohadidjojo YW Adam AM Suwandi D Seweng A Amiruddin MD. Sensory improvement of leprosy peripheral neuropathy in patients treated with perineural injection of platelet-rich plasma. Int J Dermatol. 2014;53(1):109-13. [DOI] [PubMed] [Google Scholar]
- 92.Elgazzar RF Mutabagani MA Abdelaal SE Sadakah AA. Platelet rich plasma may enhance peripheral nerve regeneration after cyanoacrylate reanastomosis: a controlled blind study on rats. Int J Oral Maxillofac Surg. 2008;37(8):748-55. [DOI] [PubMed] [Google Scholar]
- 93.Hibner M Castellanos ME Drachman D Balducci J. Repeat operation for treatment of persistent pudendal nerve entrapment after pudendal neurolysis. J Minim Invasive Gynecol. 2012;19(3):325-30. [DOI] [PubMed] [Google Scholar]
- 94.Kuffler DP Reyes O Sosa IJ Santiago-Figueroa J. Neurological recovery across a 12-cm-long ulnar nerve gap repaired 3.25 years post trauma: case report. Neurosurgery. 2011;69(6):E1321-6. [DOI] [PubMed] [Google Scholar]
- 95.Malahias MA Johnson EO Babis GC Nikolaou VS. Single injection of platelet-rich plasma as a novel treatment of carpal tunnel syndrome. Neural Regen Res. 2015;10(11):1856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Campbell WC. Delayed union and nonunion of fractures. St. Louis, MO: C.V Mosby Company; 1939:648-725. [Google Scholar]
- 97.Hernigou P Daltro G Filippini P Mukasa MM Manicom O. Percutaneous implantation of autologous bone marrow osteoprogenitor cells as treatment of bone avascular necrosis related to sickle cell disease. Open Orthop J. 2008;2:62-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hernigou P Daltro G Hernigou J. Hip osteonecrosis: stem cells for life or behead and arthroplasty? Int Orthop. 2018;42(7):1425-28. [DOI] [PubMed] [Google Scholar]
- 99.Hasty KA Cho H. Stem cell considerations for the clinician. Phys Med Rehabil Clin N Am. 2016;27(4):855-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.US Food and Drug Administration. Guidance for industry and FDA staff: Minimal manipulation of structural tissue (jurisdictional update). Secondary US Food and Drug Administration. Guidance for industry and FDA staff: Minimal manipulation of structural tissue (jurisdictional update) 2016. http://www.fda.gov/regulatoryinformation/guidances/ucm126197.htm.
- 101.Caplan AI. Biomaterials and bone repair. Biomaterials. 1988(87):15-24. [Google Scholar]
- 102.Caplan AI. Mesenchymal Stem Cells: Time to change the name! Stem Cells Transl Med. 2017;6(6):1445-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Barry FP. Mesenchymal stem cell therapy in joint disease. Novartis Found Symp. 2003;249:86-96; discussion 96-102, 70-4, 239-41. [PubMed] [Google Scholar]
- 104.Buckwalter JA Mankin HJ. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487-504. [PubMed] [Google Scholar]
- 105.Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9(5):641-50. [DOI] [PubMed] [Google Scholar]
- 106.Carter DR Beaupre GS Giori NJ Helms JA. Mechanobiology of skeletal regeneration. Clin Orthop Relat Res. 1998(355 Suppl):S41-55. [DOI] [PubMed] [Google Scholar]
- 107.Centeno CJ Busse D Kisiday J Keohan C Freeman M Karli D. Regeneration of meniscus cartilage in a knee treated with percutaneously implanted autologous mesenchymal stem cells. Med Hypotheses. 2008;71(6):900-8. [DOI] [PubMed] [Google Scholar]
- 108.Johnstone B Yoo JU. Autologous mesenchymal progenitor cells in articular cartilage repair. Clin Orthop Relat Res. 1999(367 Suppl):S156-62. [DOI] [PubMed] [Google Scholar]
- 109.Luyten FP. Mesenchymal stem cells in osteoarthritis. Curr Opin Rheumatol. 2004;16(5):599-603. [DOI] [PubMed] [Google Scholar]
- 110.Magne D Vinatier C Julien M Weiss P Guicheux J. Mesenchymal stem cell therapy to rebuild cartilage. Trends Mol Med. 2005;11(11):519-26. [DOI] [PubMed] [Google Scholar]
- 111.Murphy JM Fink DJ Hunziker EB Barry FP. Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum. 2003;48(12):3464-74. [DOI] [PubMed] [Google Scholar]
- 112.Nevo Z Robinson D Horowitz S Hasharoni A Yayon A. The manipulated mesenchymal stem cells in regenerated skeletal tissues. Cell Transplant. 1998;7(1):63-70. [DOI] [PubMed] [Google Scholar]
- 113.Noel D DF Jorgense C. Regenerative medicine through mesenchymal stem cells for bone and cartilage repair. Curr Opin Invest Drugs. 2002;7(3):1000-4. [PubMed] [Google Scholar]
- 114.Redman SN Oldfield SF Archer CW. Current strategies for articular cartilage repair. Eur Cell Mater. 2005;9:23-32. [DOI] [PubMed] [Google Scholar]
- 115.Tallheden T Dennis JE Lennon DP Sjogren-Jansson E Caplan AI Lindahl A. Phenotypic plasticity of human articular chondrocytes. J Bone Joint Surg Am. 2003;85-A Suppl 2:93-100. [DOI] [PubMed] [Google Scholar]
- 116.Wakitani S Goto T Pineda SJ et al. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1994;76(4):579-92. [DOI] [PubMed] [Google Scholar]
- 117.Walsh CJ Goodman D Caplan AI Goldberg VM. Meniscus regeneration in a rabbit partial meniscectomy model. Tissue Eng. 1999;5(4):327-37. [DOI] [PubMed] [Google Scholar]
- 118.Dominici M Le Blanc K Mueller I et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-7. [DOI] [PubMed] [Google Scholar]
- 119.Hernigou P Homma Y Flouzat-Lachaniette CH Poignard A Chevallier N Rouard H. Cancer risk is not increased in patients treated for orthopaedic diseases with autologous bone marrow cell concentrate. J Bone Joint Surg Am. 2013;95(24):2215-21. [DOI] [PubMed] [Google Scholar]
- 120.Centeno CJ Al-Sayegh H Freeman MD Smith J Murrell WD Bubnov R. A multi-center analysis of adverse events among two thousand, three hundred and seventy two adult patients undergoing adult autologous stem cell therapy for orthopaedic conditions. Int Orthop. 2016;40(8):1755-65. [DOI] [PubMed] [Google Scholar]
- 121.McDaniel JS Antebi B Pilia M et al. Quantitative assessment of optimal bone marrow site for the isolation of porcine mesenchymal stem cells. Stem Cells Int. 2017;2017:1836960 10.1155/2017/1836960[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hernigou P Homma Y Flouzat Lachaniette CH et al. Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells. Int Orthop. 2013;37(11):2279-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hernigou P Poignard A Beaujean F Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005;87(7):1430-7. [DOI] [PubMed] [Google Scholar]
- 124.Hernigou P Poignard A Zilber S Rouard H. Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop. 2009;43(1):40-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Centeno CJ Al-Sayegh H Bashir J Goodyear S Freeman MD. A dose response analysis of a specific bone marrow concentrate treatment protocol for knee osteoarthritis. BMC Musculoskelet Disord. 2015;16:258 10.1186/s12891-015-0714-z[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jo CH Chai JW Jeong EC et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: A 2-year follow-up study. Am J Sports Med. 2017;45(12):2774-83. [DOI] [PubMed] [Google Scholar]
- 127.Li CY Wu XY Tong JB et al. Comparative analysis of human mesenchymal stem cells from bone marrow and adipose tissue under xeno-free conditions for cell therapy. Stem Cell Res Ther. 2015;6:55 10.1186/s13287-015-0066-5[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mohamed-Ahmed S Fristad I Lie SA et al. Adipose-derived and bone marrow mesenchymal stem cells: a donor-matched comparison. Stem Cell Res Ther. 2018;9(1):168 10.1186/s13287-018-0914-1[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Koga H Muneta T Nagase T et al. Comparison of mesenchymal tissues-derived stem cells for in vivo chondrogenesis: suitable conditions for cell therapy of cartilage defects in rabbit. Cell Tissue Res. 2008;333(2):207-15. [DOI] [PubMed] [Google Scholar]
- 130.CDC. National and state medical expenditures and lost earnings attributable to arthritis and other rheumatic conditions - United States. MMWR Morb Mortal Wkly Rep. 2003(56):4-7. [PubMed] [Google Scholar]
- 131.CDC. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation - United States, 2010-2012. MMWR Morb Mortal Wkly Rep. 2013;44(62):869-73. [PMC free article] [PubMed] [Google Scholar]
- 132.Centeno C Sheinkop M Dodson E et al. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018;16(1):355 10.1186/s12967-018-1736-8[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vaishya R Pariyo GB Agarwal AK Vijay V. Non-operative management of osteoarthritis of the knee joint. J Clin Orthop Trauma. 2016;7(3):170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Belmont PJ Jr. Goodman GP Waterman BR Bader JO Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20-6. [DOI] [PubMed] [Google Scholar]
- 135.Grosu I Lavand’homme P Thienpont E. Pain after knee arthroplasty: an unresolved issue. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1744-58. [DOI] [PubMed] [Google Scholar]
- 136.Rodriguez-Fontan F Piuzzi NS Kraeutler MJ Pascual-Garrido C. Early clinical outcomes of intra-articular injections of bone marrow aspirate concentrate for the treatment of early osteoarthritis of the hip and knee: A cohort study. Phys Med Rehabil. 2018;10(12):1353-59. [DOI] [PubMed] [Google Scholar]
- 137.Shapiro SA Kazmerchak SE Heckman MG Zubair AC O'Connor MI. A prospective, single-blind, placebo-controlled trial of bone marrow aspirate concentrate for knee osteoarthritis. Am J Sports Med. 2017;45(1):82-90. [DOI] [PubMed] [Google Scholar]
- 138.Centeno CJ Pitts J Al-Sayegh H Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res 2015;8:437-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hong SH Choi JY Lee GK Choi JA Chung HW Kang HS. Grading of anterior cruciate ligament injury. Diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomogr. 2003;27(5):814-9. [DOI] [PubMed] [Google Scholar]
- 140.Hsu WH Peng KT Lai LJ Hung CH Chang PJ. Cellular senescence occurring in the rabbit medial collateral ligament during healing. J Orthop Res. 2013;31(1):81-90. [DOI] [PubMed] [Google Scholar]
- 141.Centeno CJ Al-Sayegh H Bashir J Goodyear S Freeman MD. A prospective multi-site registry study of a specific protocol of autologous bone marrow concentrate for the treatment of shoulder rotator cuff tears and osteoarthritis. J Pain Res. 2015;8:269-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Administration UDoHaHSFaD. Regulatory considerations for human cells, tissues, and cellular and tissue-based products: Minimal manipulation and homologous use: Guidance of industry and food and drug administration staff, 2017. https://www.fda.gov/media/109176/download.
- 143.Pettine KA Suzuki RK Sand TT Murphy MB. Autologous bone marrow concentrate intradiscal injection for the treatment of degenerative disc disease with three-year follow-up. Int Orthop. 2017;41(10):2097-103. [DOI] [PubMed] [Google Scholar]
- 144.Pittenger MF Mackay AM Beck SC et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143-7. [DOI] [PubMed] [Google Scholar]
- 145.Centeno CJ Freeman MD. Percutaneous injection of autologous, culture-expanded mesenchymal stem cells into carpometacarpal hand joints: a case series with an untreated comparison group. Wien Med Wochenschr. 2014;164(5-6):83-7. [DOI] [PubMed] [Google Scholar]
- 146.Sodha S Ring D Zurakowski D Jupiter JB. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. 2005;87(12):2614-8. [DOI] [PubMed] [Google Scholar]
- 147.Buterbaugh GA Brown TR Horn PC. Ulnar-sided wrist pain in athletes. Clin Sports Med 1998;17(3):567-83. [DOI] [PubMed] [Google Scholar]
- 148.Centeno C Markle J Dodson E et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017;15(1):197 10.1186/s12967-017-1300-y[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Centeno CJ Schultz JR Cheever M Robinson B Freeman M Marasco W. Safety and complications reporting on the re-implantation of culture-expanded mesenchymal stem cells using autologous platelet lysate technique. Curr Stem Cell Res Ther. 2010;5(1):81-93. [DOI] [PubMed] [Google Scholar]
- 150.Ellis I Banyard J Schor SL. Differential response of fetal and adult fibroblasts to cytokines: cell migration and hyaluronan synthesis. Development. 1997;124(8):1593-600. [DOI] [PubMed] [Google Scholar]
- 151.Willett NJ Thote T Lin AS et al. Intra-articular injection of micronized dehydrated human amnion/chorion membrane attenuates osteoarthritis development. Arthritis Res Ther. 2014;16(1):R47 10.1186/ar4476[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fortier L. AMSSM Sports Medcast and BMJ Talk Medicine. In: McFadden D, ed. Episode #360: Regenerative Medicine: Game Changing Innovation of Next Big Flop? 360 ed, 2019.
- 153.Secco M Zucconi E Vieira NM et al. Multipotent stem cells from umbilical cord: cord is richer than blood! Stem Cells. 2008;26(1):146-50. [DOI] [PubMed] [Google Scholar]
- 154.Sibov TT Severino P Marti LC et al. Mesenchymal stem cells from umbilical cord blood: parameters for isolation, characterization and adipogenic differentiation. Cytotechnology. 2012;64(5):511-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Divya MS Roshin GE Divya TS et al. Umbilical cord blood-derived mesenchymal stem cells consist of a unique population of progenitors co-expressing mesenchymal stem cell and neuronal markers capable of instantaneous neuronal differentiation. Stem Cell Res Ther. 2012;3(6):57 doi: 10.1186/scrt148[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Takahashi A de Andres MC Hashimoto K Itoi E Oreffo RO. Epigenetic regulation of interleukin-8, an inflammatory chemokine, in osteoarthritis. Osteoarthritis Cartilage. 2015;23(11):1946-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Stavropoulos-Giokas C Dinou A Papassavas A. The role of HLA in cord blood transplantation. Bone Marrow Res. 2012;2012:485160 10.1155/2012/485160[published Online First Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ortved KF. Regenerative medicine and rehabilitation for tendinous and ligamentous injuries in sport horses. Vet Clin North Am Equine Pract. 2018;34(2):359-73. [DOI] [PubMed] [Google Scholar]
- 159.McKay J Frantzen K Vercruyssen N et al. Rehabilitation following regenerative medicine treatment for knee osteoarthritis-current concept review. J Clin Orthop Trauma. 2019;10(1):59-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Knoop J Steultjens MP Roorda LD et al. Improvement in upper leg muscle strength underlies beneficial effects of exercise therapy in knee osteoarthritis: secondary analysis from a randomised controlled trial. Physiotherapy. 2015;101(2):171-7. [DOI] [PubMed] [Google Scholar]
- 161.Loenneke JP Wilson JM Wilson GJ Pujol TJ Bemben MG. Potential safety issues with blood flow restriction training. Scand J Med Sci Sports. 2011;21(4):510-8. [DOI] [PubMed] [Google Scholar]
- 162.Takarada Y Tsuruta T Ishii N. Cooperative effects of exercise and occlusive stimuli on muscular function in low-intensity resistance exercise with moderate vascular occlusion. Jpn J Physiol. 2004;54(6):585-92. [DOI] [PubMed] [Google Scholar]
- 163.Hylden C Burns T Stinner D Owens J. Blood flow restriction rehabilitation for extremity weakness: a case series. J Spec Oper Med. 2015;15(1):50-6. [PubMed] [Google Scholar]
- 164.Simao AP Avelar NC Tossige-Gomes R et al. Functional performance and inflammatory cytokines after squat exercises and whole-body vibration in elderly individuals with knee osteoarthritis. Arch Phys Med Rehabil. 2012;93(10):1692-700. [DOI] [PubMed] [Google Scholar]
- 165.Wang P Yang L Liu C et al. Effects of Whole Body Vibration Exercise associated with Quadriceps Resistance Exercise on functioning and quality of life in patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil 2016;30(11):1074-87. [DOI] [PubMed] [Google Scholar]