Abstract
Low back pain in adolescent athletes is quite common, and an isthmic spondylolysis is the most common identifiable cause. Spondylolysis, a bone stress injury of the pars interarticularis, typically presents as focal low back pain which worsens with activity, particularly with back extension movements. Research on spondylolysis has focused on diagnosis, radiographic healing, the effects of bracing, and rest from activity. Although physical therapy is frequently recommended for adolescent athletes with spondylolysis, there have been no randomized controlled trials investigating rehabilitation. Additionally, there are no detailed descriptions of physical therapy care for adolescent athletes with spondylolysis. The purpose of this clinical commentary is to provide a brief background regarding the pathology of isthmic spondylolysis and provide a detailed description of a proposed plan for physical therapy management of spondylolysis in adolescent athletes.
Level of Evidence:
5
Keywords: Adolescent, Low Back Pain, Stress Fracture, Movement System
INTRODUCTION
Half of all adolescents report experiencing low back pain (LBP) and those who are active in sports report an even higher rate.1,2 The growing spine of the adolescent introduces variables into the assessment and management of lumbar injuries which do not exist in the developed spine of the adult.3 The most common identifiable cause of LBP in the adolescent athlete is an isthmic spondylolysis, a stress injury in the pars interarticularis.4-6 Research on spondylolysis has focused on diagnosis, radiographic healing, the effects of bracing, and rest from activity. Although spondylolysis is a common injury among adolescent athletes, no detailed description of physical therapy care for this population exists. The purpose of this clinical commentary is to provide a brief background regarding the pathology of isthmic spondylolysis and provide a detailed description of a proposed plan for physical therapy management of spondylolysis in adolescent athletes.
PREVALENCE
The prevalence of spondylolysis in adolescent athletes is reported to be 7-21%.7-9 The prevalence of spondylolysis in symptomatic adolescent athletes is reported to be two to five times higher than nonathletes, with a prevalence of 14-30% among adolescent athletes reporting LBP.6,10,11 Spondylolysis is 1.6-4.5 times more prevalent in adolescent males than females reporting LBP.6,11 Spondylolysis occurs in other populations but at a much lower rate; the prevalence reported in children is 2.5-4.5%, increasing to 6% in the general adolescent and adult populations.4,5,12,13 Spondylolysis may be present in asymptomatic individuals as well,12 and an incidental identification of a spondylolysis in an asymptomatic individual should not warrant treatment.
ANATOMY AND MECHANISM OF INJURY
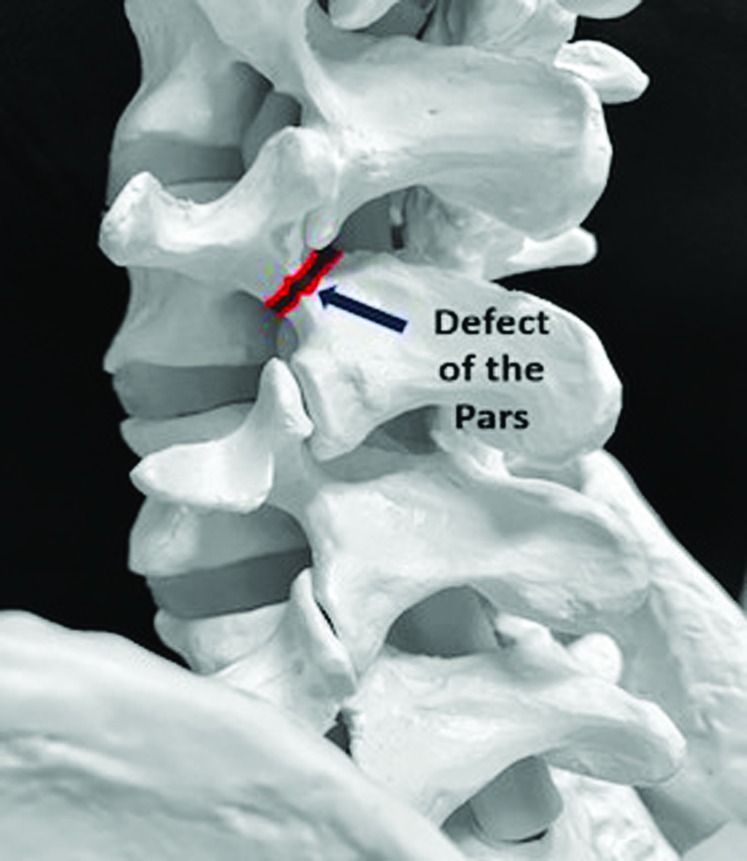
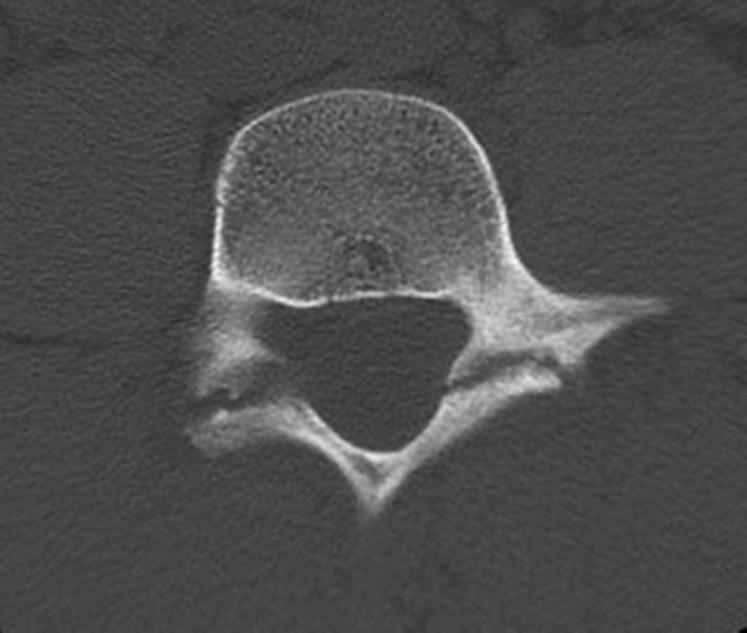
Isthmic spondylolysis is the most common type of spondylolysis and is the focus of this clinical commentary.14,15 Isthmic spondylolysis refers to an overuse stress injury in the pars interarticularis (Figure 1 and Figure 2). A spondylolysis may be unilateral or bilateral and most commonly occurs at the L5 vertebra with L4 being the next most commonly affected level.14 An association has been noted with spondylolysis and spina bifida occulta.4,16-18 Additionally, some evidence shows that individuals with a spondylolysis have a pars with a smaller cross-sectional area than other adolescents.19 Among adolescent spondylolytic injuries, there are different subgroups: acute or active, progressive, and terminal. These subgroups are determined by the appearance of the lesion on imaging, rather than the chronicity of the injury.20,21
Figure 1.
Depiction of an Isthmic Spondylolysis.
Figure 2.
Radiographic image of bilateral spondylolysis at L4 vertebra.
The mechanism of injury for spondylolysis is thought to be excessive and repetitive extension movements, particularly when combined with rotation.11 Risk of spondylolytic injury exists for all athletes, but athletes who perform repetitive extension and rotation motions, have an even higher risk.3,5,6,8,20,22,23 Sports such as baseball, throwing events in track and field, cricket, diving, gymnastics, soccer, wrestling, and weightlifting have a higher risk of spondylolysis.6,8,11,24
CLINICAL PRESENTATION
The adolescent athlete will typically present with complaints of atraumatic, insidious-onset, focal LBP which worsens with activity, especially lumbar extension movements. Adolescent athletes with symptomatic spondylolysis typically present with axial LBP without radiation into the legs.22 Adolescents with a spondylolysis demonstrated increased lumbar lordosis and tightness of the hamstring muscles when compared to adolescents without a spondylolysis.19,25 Currently, patient history and clinical special tests have little diagnostic value.26,27 The most well-known clinical test to screen for spondylolysis is the single-leg hyperextension test, however this test has been found to be neither sensitive nor specific for detecting spondylolysis.28,29 Therefore, imaging is necessary when a clinician wishes to confidently determine if a spondylolytic lesion is present in an adolescent athlete with LBP.26
IMAGING
The most appropriate imaging to diagnose a spondylolysis has not been clearly established. Two-view radiographs include anterior-posterior (AP) and lateral views while four-view radiographs additionally include oblique views of the spine. Four-view radiographs have fallen out of favor due to exposing the patient to higher levels of radiation with little, if any, increased sensitivity.30 Radiographs have low sensitivity making it difficult to rule out a spondylolysis without advanced imaging.31 Computed tomography (CT) or single photon emission computed tomography (SPECT) have historically been considered the gold standard for diagnosing spondylolysis. SPECT/CT is quite sensitive for detecting lesions, but exposes the patient to significant amounts of radiation.32,33 Magnetic resonance imaging (MRI) has become more popular in the diagnosis of spondylolysis.34,35 The diagnostic accuracy of MRI for detecting spondylolysis has improved in recent years approaching that of SPECT/CT,31 and has the advantage of no ionizing radiation.33 There remain, however, challenges to MRI's use, with issues of cost, insurance coverage, access, and variable quality of imaging in different centers. Tofte et al.36 recommends using two-view radiographs as the best initial study, subsequently followed by MRI in early diagnosis or CT with more persistent LBP.
OUTCOME MEASURES
Traditional adult patient reported outcome measures for LBP, such as the Oswestry Disability Index and the Roland-Morris Disability Questionnaire, have significant limitations for adolescent athletes with spondylolysis. The Oswestry Disability Index becomes notably less reliable for high functioning individuals, such as adolescent athletes, because of a significant floor effect.37 The Roland-Morris Disability Questionnaire is similarly not designed for higher functioning populations.38,39 Adolescents with a spondylolysis typically struggle with higher level activities such as running, jumping and sport specific motions, but are relatively quickly able to perform ADL's without much difficulty. The Micheli Functional Scale (MFS) is a relatively new patient-reported outcome measure specifically designed for adolescent athletes with LBP.40 The MFS demonstrates high internal consistency (α = 0.90), and the concurrent validity has been established using the Oswestry Disability Index.40,41 The minimal clinically important difference has yet to be established for the MFS. Although more research is needed on the psychometric properties of the MFS, the authors believe this outcome measure is the most appropriate to use in this population.
Non-Surgical and Surgical Care
Non-surgical care should be the initial treatment for adolescent athletes with spondylolysis.14,42 The vast majority of patients with spondylolysis can successfully be managed with non-surgical care;14 and surgery, involving direct repair or indirect reduction and compression,43,44 may only be indicated after failure to improve with at least six months of comprehensive treatment.45
Rest from Activity
Cessation of sport activity is recommended for at least three months in this population.46 Resting from sport for three months has been closely associated with a favorable clinical outcome.47,48 Varying recommendations on the optimal time to begin physical therapy have been made with some recommending starting early, when symptoms have resolved,3,49,50 and others recommending no rehabilitation until after three months of rest.42,51 In a retrospective review,52 patients whose physical therapy was initiated earlier were able to return to sport sooner than the patients who physical therapy was not initiated until after three months. Recommendations for activity modification including sport and initiating physical therapy are based on low-level evidence.46,52 The authors believe that supervised therapeutic exercise can be completed safely and should be initiated early within the first few weeks after diagnosis to help reduce muscle atrophy, deconditioning, and potentially reduce time out of sport.
Bracing
Although lumbar bracing may be prescribed in an attempt to stabilize the spine and promote healing, controversy exists about the efficacy of bracing for spondylolysis. Several investigators have advocated for the routine use of lumbar bracing using several different types of lumbosacral orthoses to limit extension and rotation of the spine.53-59 However, in a meta-analysis of patients with spondylolysis, bracing was not found to influence clinical outcomes.14 Additionally, bracing prescription was not found to be predictive of the long-term ability to participate in sport, symptom recurrence, or the patient's perceived outcome.60 A randomized controlled trial is necessary to determine the true effectiveness of bracing, but based on the current evidence, the authors recommend forgoing routine use of bracing and instead reserve its use for patients whose symptoms fail to improve.
PROGNOSIS
Excellent short-term clinical outcomes should be expected for adolescents with spondylolysis,14 however these positive short-term clinical outcomes are not maintained by all.60,61 A recent systematic review suggests that with non-surgical treatment, consisting of activity restriction, rest, and physical therapy with or without adjunctive bracing, 92% of individuals are able to return to sport with little to no pain within six months.62 The short-term clinical outcomes for athletes with a spondylolysis appear to be more promising than adolescents with non-specific LBP, as only 33-35% of the adolescents with non-specific LBP were without pain and dysfunction following individualized physical therapy exercise and manual therapy.63,64 Long-term efficacy (1.5-8 years) of non-surgical treatment for spondylolysis suggests that LBP interfering with activity returns in 45%-51% of individuals, and 18-40% decreased or stopped their sport participation due to pain.60,61
Non-surgical treatment of spondylolytic injuries has attempted to promote bony healing of the lesion.56,59,65 In a meta-analysis of 10 radiographic studies,14 only 28% of spondylolytic lesions healed. Unilateral injuries were significantly more likely to heal (71%) compared to bilateral injuries (18%).14 Additionally, acute lesions had a 68% chance of healing, while terminal or chronic lesions did not heal with non-surgical treatment.14 Despite a goal to promote bony healing, radiographic healing is not associated with quality of life or ability to return to sport.14,49,66 Repeat imaging to assess for radiographic healing is no longer recommended in a patient who is responding well to treatment, due to unnecessary exposure to radiation as well as the associated cost.33 In the authors opinion, clinicians should base treatment progression on functional ability and not bony healing, since it is not associated with clinical outcomes.
PSYCHOSOCIAL IMPACT OF SPONDYLOLYSIS INJURY
Spondylolysis is typically viewed through the biomedical model due to the existence of a discrete identifiable injury to the vertebra. In contrast, the authors recommend clinicians address this condition using the biopsychosocial approach. Spondylolytic injuries not only affect athletes physically but also psychologically and socially with athletes experiencing feelings of loss, decreased self-esteem, anxiety, frustration, isolation, and depression.67-69 These psychosocial factors are important for clinicians to consider and address throughout rehabilitation, as these adolescent athletes are often unable to participate in their desired sport for months.67,69,70 Effective patient-clinician communication and positive relationships can provide social support and are also associated with improved health outcomes.68,71 Moreover, athletes may perceive their low back as “broken” resulting from the explanation they have received regarding the spondylolytic injury. This exaggerated perception can easily increase fear of activity and fear of re-injury. Clinicians should reassure adolescent athletes that, although they have a bone stress injury, their back is not “broken”. Furthermore, the positive outcomes seen in this patient population and the high likelihood of a making full return to sport should be emphasized.14,60
RATIONALE OF PHYSICAL THERAPY CARE
Though physical therapy treatment for adolescent athletes with spondylolysis has not been specifically described in the literature, there is value in leveraging evidence from other relevant populations. The presence of a spondylolysis has been found to result in lumbar instability, with increased translation and rotation motion occurring segmentally.72-75 Establishing good performance of specific muscles, including the transversus abdominis and multifidus, has been theorized to promote segmental lumbar stability for this population.76,77 In a randomized controlled trial of adults with spondylolysis, targeting the deep abdominals and lumbar multifidus muscles was found to be superior to general exercise.76 The clinical practice guidelines on low back pain recommend motor control exercises, transversus abdominis training, lumbar multifidus training, and dynamic lumbar stabilization exercises for individuals with spinal instability including spondylolysis.78 Additional recommendations applicable to athletes with spondylolysis as they progress back to sport include trunk coordination and motor control training, functional strengthening, and endurance exercises.78
FRAMEWORK FOR TREATMENT
The authors propose a framework for the physical therapy treatment of adolescent athletes with acute spondylolysis. In many ways physical therapy for the adolescent athlete with spondylolysis is similar to those with non-specific LBP, but there are certain factors that are important for this population. First and foremost is that the athlete has a healing bone stress injury. Phase I of the program is performed in a relatively static and neutral lumbar position allowing for muscle activation and strengthening while avoiding undue stress on the injured pars interarticularis. During this phase, the authors recommend addressing the deep abdominals and lumbar multifidus, as targeting these muscles was found to be superior to general exercise among adults with spondylolysis or spondylolisthesis.76
Second, as the patient's symptoms improve, extension and rotation motions should be promoted, not avoided. Recommendations have been made to avoid exercises that cause extension or rotation motions in adolescent athletes with spondylolysis.79 Although repetitive forceful extension and rotation is thought to be the mechanism of injury and end-range extension stresses the pars interarticularis,80 these motions are functional and necessary in most sports.81,82 It is important for athletes to progressively work into these motions to be successful when they return to sport.
Finally, clinicians should remember that although there is a bone stress injury in the lumbar spine, athletes use their entire body when participating in sport. Impairments in other regions can increase stress throughout the lumbar spine and should be addressed.83,84
REHABILITATION
This rehabilitation program (Table 1) is designed with three phases to progress patients through their rehabilitation. The first, “isolated” phase uses exercises that target specific muscle groups. The “integrated” phase emphasizes coordinated performance of the muscles throughout the body during functional exercises. The final “return to sport” phase highlights advanced exercises and sport reintegration. Progression is based on achieving specific criteria, as opposed to following a rigid, time-based protocol. This approach allows athletes to progress at their own pace, yet still ensures safe and comprehensive care.
Table 1.
Physical Therapy for Youth Athletes with Spondylolysis.
| Phase | I. Isolated Training | II. Integrated Training | III. Return to Sport Training |
|---|---|---|---|
| Objectives |
|
|
|
| Muscle Performance Considerations |
|
|
|
| Mobility Considerations |
|
|
|
| Test/Assess |
|
|
|
| Criteria to begin next Phase |
|
|
Discharge Criteria:
|
Abbreviations: ROM, Range of motion; UE, upper extremity; LE, lower extremity; TA, transverse abdominis; MT; multifidus.
To guide treatment initially, it is essential to understand the following conceptualization of the trunk muscles. This conceptualization draws a distinction between two muscular systems based on their functional role: a local muscle system and a global muscle system. The local system provides precise, tonic segmental stabilization, while the global system is responsible for movement generation.85 This two-category grouping of trunk muscles is listed in Table 2.
Table 2.
Local and Global Muscle Systems of the Core. (Adapted from Hoogenboom and Kiesel31)
| Local Muscle System | Global Muscle System |
|---|---|
| Multifidi | Rectus Abdominis |
| Transversus Abdominis | External oblique |
| Quadratus lumborum (medial portion) | Internal Oblique (anterior fibers) |
| Diaphragm | Longissimus and Iliocostalis (thoracic portion) |
| Internal Oblique (posterior fibers) | Quadratus lumborum (lateral portion) |
| Intertransversarii and Interspinales | Latissimus dorsi |
| Iliocostalis and longissimus (lumbar portions) | Iliacus |
| Psoas Major (posterior portion) | Psoas Major (anterior portion) |
| Hip rotators* | Hip extensors and adductors |
| Hip abductors* | Hamstring and Quadriceps |
| Hip rotators* | |
| Hip abductors* |
Disagreement exists about whether these are local or global.
Phase I – Isolated Training
Objectives of Phase I
At the outset of Phase I, clinicians have a critically important role in promoting positive beliefs about LBP. Even with the presence of a spondylolytic injury, patients should be encouraged to stay active and view movement as beneficial to their recovery. Initially, patients will benefit from avoiding pain-eliciting activities. However, this guidance should be offered within the overarching theme of remaining active.
Exercise interventions in this phase target isolated muscle groups and any movement restrictions. It should be noted that scapular stabilizers, hip muscles and other muscles of the local system likely need attention as well. Adolescent athletes with acute spondylolysis may need interventions for pain control, such as therapeutic modalities or manual therapy. Like other populations with LBP, these interventions should be used sparingly. Thrust (manipulation) manual therapy is not recommended in the lumbar spine. When pain-control interventions are used, the goal should be to promote activity and exercise.
Muscle Performance Considerations
The patient is encouraged to begin targeted exercises to improve activation and performance of the local muscle system. Exercises should occur in a pain-minimized neutral position, and not in end-range. Exercises can be progressed by adding extremity movements while maintaining a neutral spinal position. Detailed descriptions of local stabilization have previously been described.85 Younger patients may have difficulty performing or engaging in the focused local exercises in Phase I. The authors find that use of external feedback such as attempting to keep a half foam roll or towel roll steady on their back or abdominal muscles may help with performance. For these athletes who find these “low level” exercises too easy or boring, adding an unstable surface, can increase difficulty and improve patient engagement.
Mobility Considerations
In this first phase, athletes should achieve lumbar motion required for activities of daily living. For most adolescent athletes, specific motion exercises will not be necessary as their motion will return once the pain subsides. Patients with spondylolysis may present with decreased flexibility of the hip flexor and hamstring muscles.19,25,86 Excessive tightness of the hip flexor muscles results in increased lumbar lordosis, which can increase the stress on the posterior elements of the lumbar spine.87 If the clinician determines that stretching of these muscles is appropriate, care should be taken to maintain a neutral spine position while stretching.
Clinicians should identify and address impairments in other areas of the body integral to the athlete's sport. A good understanding of each patient's sport and sport-specific movements can help identify a relationship between the individual's LBP and a seemingly unrelated impairment. For example, a baseball pitcher who has limited trunk rotation and shoulder external rotation may perform excessive lumbar extension and rotation to be able to pitch effectively.88 This excessive lumbar motion results in increased lumbar stress which is compounded by the repetitive nature of pitching and may be a potential cause of spondylolysis.81
Phase I Tests and Criteria to Progress to Phase II
Tests of the local muscles guide exercise selection and verify progress in the first phase. Qualitative assessment via palpation is an acceptable method, but the pressure biofeedback unit test of the transversus abdominis and the multifidus lift test attempt to bring more objectivity and standardization.89,90 The transversus abdominis should be judged as “good,” defined by a 4 mmHG drop for at least 10 seconds using a pressure biofeedback device in prone (Figure 3), and an obvious (palpable) contraction of the multifidus should be noted (Figure 4).72 Although the multifidus is difficult to assess clinically, the multifidus lift test has shown acceptable reliability (Kappa 0.75-0.81) and a moderate correlation with real-time ultrasound imaging.90
Figure 3.
Pressure Biofeedback Unit Test of the Transverse Abdominis.
The patient is prone over a pressure biofeedback device, which is inflated to 70 mmHg. The therapist provides the cue “Draw in abdominal wall for 10 seconds without moving your back and while breathing normally.” The therapist records the length of time the patient can hold a ≥4mmHg drop, while monitoring for improper compensations. Performance is considered “good” with a duration of 10 seconds or greater.
Figure 4.
Multifidus Lift Test.
Patient lies prone, with shoulders at approximately 120˚ of abduction and elbows at 90˚ of flexion. The therapist palpates immediately lateral and adjacent to the interspinous space of L4/L5 and L5/S1. The patient is instructed to lift their contralateral arm towards the ceiling approximately 5 cm. The therapist qualitatively assesses multifidus as contralateral arm is lifted. A normal contraction is described as a robust and obvious muscle contraction, while little or no palpable contraction is considered abnormal.
At the end of Phase I, the clinician should assess the quality and quantity of lumbar motion. Lumbar motion can be assessed using an inclinometer,91 and the athlete should be able to demonstrate lumbar motion within normal limits. Clinicians must recognize that functional motion for athletes will likely exceed normal ranges in some sports. Repeated forward and backward bending of the lumbar spine should be pain-free and without aberrant movement.92
PHASE II – INTEGRATED TRAINING
Objectives
The goal of Phase II is to integrate the local muscle system with the global muscle system during dynamic functional exercises. In this phase, exercises should incorporate greater resistance and be performed throughout increasing ranges of spinal motion. Additionally, the endurance of the local muscle system should be progressed to prepare for the demands of the athlete's sport. During this phase, the athlete should achieve sufficient strength and flexibility in other to ensure controlled spinal movement during functional activities including extension.
Muscle Performance Considerations
In contrast to the initial phase when the spine remains in static, supported positions, patients now perform unsupported, dynamic exercises. Exercises advance to functional upright positions and progress from single plane to multiple planes including end-range spinal movements while assuring proper movement patterns. Clinicians should include exercises that build eccentric strength and force development. Additionally, clinicians must not forget about the strength of other muscles in the sport specific kinetic chain, including the hips, scapulothoracic, and shoulder musculature.
Mobility Considerations
Exercise progressions should promote controlled, normalized lumbopelvic rhythm and be monitored to avoid uncontrolled lumbar motion.82 The functional motion an athlete needs for sport, not only in the lumbar spine but also in other areas such as the hips and shoulders, often exceeds normal motion. Therefore, clinicians should focus on achieving sufficient motion for the demands of sport.
Phase II Tests and Criteria to Progress to Phase III
The athlete's ability to integrate the local and global muscle systems during dynamic functional movement will be assessed using clinical tests recommended in the LBP clinical practice guidelines to assess trunk muscle power and endurance.78 The prone double leg raise can be useful to judge the pain-free performance and endurance of the athlete's extensor muscles (Figure 5).93 The supine double leg lowering test can assess global trunk flexion performance (Figure 6). Lateral core strength and endurance can be assessed using a timed lateral plank. The patient should demonstrate full, pain-free lumbar movement all directions. The MFS can provide insight into the patient's beliefs about their functional level and scores should approach 0% on the ADL (part B) and pain (part C) subsections. It is important to consider the requirements of the athlete's sport as certain sports require greater strength, power, endurance and mobility to be successful and the patient should demonstrate sufficient motion and strength in their sport/position specific kinetic chain.
Figure 5.
Prone Double Leg Raise Test.
The patient is positioned in prone with hands underneath their forehead. The therapist instructs the patient to raise both legs until their knees are off the table and hold the position. The test is timed until the patient can no longer maintain knee clearance or reports pain.
Figure 6.
Supine Double Leg Lowering Test.
The patient is positioned in supine; the therapist elevates both of the patient's fully extended legs to the point at which the sacrum begins to rise off the table. The patient is instructed to maintain contact of the low back with the table while slowly lowering extended legs to the table without assistance. The examiner observes and measures when the lower back loses contact with the tabletop due to anterior pelvic tilt.
PHASE III – RETURN TO SPORT
Objectives of Phase III
The primary objective of this phase is to reintegrate the athlete back into sport. The second objective is to ensure that the athlete is able to translate dynamic core exercises to sport specific activity. The third objective is to maximize aerobic capacity, endurance, and sport specific strength. As the athlete has been at a reduced level of activity, their aerobic capacity, endurance, and sport specific muscle strength may have suffered. Clinicians must not forget that athletes can practice for hours most days of the week and one to two hours of physical therapy a week is not adequate preparation. Finally, the clinician should work with the athlete and family to establish a proper training regimen and ongoing independent management program following discharge.
Phase III Considerations
Successful reintegration of the athlete into sport cannot be completed solely within the confines of the clinic. The athlete should perform a monitored, graded return to practice and competition. The clinician should communicate with the family, coach and the athletic trainer to determine an appropriate initial tolerable level of sport participation. Input from all of these sources will help the clinician know when to progress the athlete until they are participating fully in all aspects of sport. Injured athletes should progressively perform higher levels of sport activity until they can fully resume sport safely as an effective athlete. The return-to-sport progression may be relatively short or take many weeks depending on how long the athlete was out of sport as well as the intensity and level of the sport to which they are returning. An overview of how to progress each athlete back to their desired sport is outside of the scope of this commentary, but many return-to-sport progressions exist which can guide clinicians who may be unfamiliar with this process.94-98
Sport specific exercises should mimic the wide array of activities the athlete will need to perform. Balls and unstable surfaces can be incorporated to stress the athlete's ability to respond in the unpredictable environment of their sport.
Patient assessment and criteria for discharge Phase III
At this stage of rehabilitation, athletes are returning to sport and preparing for discharge. The athlete's sport-specific mechanics should be assessed for impaired movement or compensations throughout the kinetic chain. Attaining perfect form is unlikely and not expected in these adolescent athletes, however even minor improvements may help reduce the stress on the pars interarticularis as the athlete resumes sport.81,82 The clinician should also monitor the athlete's symptoms as they reintegrate back into sport. Athletes should be able to resume similar competitive levels with little to no pain even during high level sport activity.60 There are no significant change scores reported for the MFS, but in our experience most athletes score at or near zero at discharge.
CONCLUSIONS
Evidence in non-surgical care of isthmic spondylolysis in adolescents is growing and physical therapy is frequently recommended, thus, this commentary provides much needed guidance regarding the phased implementation of physical therapy care. Although the physical therapy recommendations in this commentary are largely based on expert opinion and research generalized from similar populations, they are helpful in establishing a safe and effective approach for treating adolescent athletes with a spondylolysis. Additionally, the rehabilitation program in this commentary may serve as a framework for developing additional studies designed to assess physical therapy care for this population.
REFERENCES
- 1.Burton AK Clarke RD McClune TD et al. The natural history of low back pain in adolescents. Spine (Phila Pa 1976). 1996;21(20):2323-2328. [DOI] [PubMed] [Google Scholar]
- 2.Calvo-Munoz I Gomez-Conesa A Sanchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr. 2013;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Luigi AJ. Low back pain in the adolescent athlete. Phys Med Rehabil Clin N Am. 2014;25(4):763-788. [DOI] [PubMed] [Google Scholar]
- 4.Fredrickson BE Baker D McHolick WJ et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66(5):699-707. [PubMed] [Google Scholar]
- 5.Micheli LJ Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149(1):15-18. [DOI] [PubMed] [Google Scholar]
- 6.Selhorst M Fischer A MacDonald J. Prevalence of spondylolysis in symptomatic adolescent athletes: an assessment of sport risk in nonelite athletes. Clin J Sport Med. 2019;29(5):421-425. [DOI] [PubMed] [Google Scholar]
- 7.Crawford CH 3rd Ledonio CG Bess RS et al. Current evidence regarding the etiology, prevalence, natural history, and prognosis of pediatric lumbar spondylolysis: a report from the scoliosis research society evidence-based medicine committee. Spine Deform. 2015;3(1):12-29. [DOI] [PubMed] [Google Scholar]
- 8.Soler T Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000;28(1):57-62. [DOI] [PubMed] [Google Scholar]
- 9.Hoshina H. Spondylolysis in athletes. Phys Sportsmed. 1980;8(9):75-79. [DOI] [PubMed] [Google Scholar]
- 10.Schroeder GD LaBella CR Mendoza M et al. The role of intense athletic activity on structural lumbar abnormalities in adolescent patients with symptomatic low back pain. Eur Spine J. 2016;25(9):2842-2848. [DOI] [PubMed] [Google Scholar]
- 11.Rossi F Dragoni S. The prevalence of spondylolysis and spondylolisthesis in symptomatic elite athletes: radiographic findings. Radiography. 2001;7(1):37-42. [Google Scholar]
- 12.Ramadorai U Hire J DeVine JG et al. Incidental findings on magnetic resonance imaging of the spine in the asymptomatic pediatric population: a systematic review. Evid Based Spine Care J. 2014;5(2):95-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Urrutia J Cuellar J Zamora T. Spondylolysis and spina bifida occulta in pediatric patients: prevalence study using computed tomography as a screening method. Eur Spine J. 2016;25(2):590-595. [DOI] [PubMed] [Google Scholar]
- 14.Klein G Mehlman CT McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009;29(2):146-156. [DOI] [PubMed] [Google Scholar]
- 15.DiFiori JP Benjamin HJ Brenner J et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24(1):3-20. [DOI] [PubMed] [Google Scholar]
- 16.Roche MB Rowe GG. The incidence of separate neural arch and coincident bone variations; a survey of 4,200 skeletons. Anat Rec. 1951;109(2):233-252. [DOI] [PubMed] [Google Scholar]
- 17.Turner RH Bianco AJ Jr. Spondylolysis and spondylolisthesis in children and teen-agers. J Bone Joint Surg Am. 1971;53(7):1298-1306. [PubMed] [Google Scholar]
- 18.Jackson DW Wiltse LL Cirincoine RJ. Spondylolysis in the female gymnast. Clin Orthop Relat Res. 1976(117):68-73. [PubMed] [Google Scholar]
- 19.Wren TAL Ponrartana S Aggabao PC et al. Increased lumbar lordosis and smaller vertebral cross-sectional area are associated with spondylolysis. Spine. 2018;43(12):833-838. [DOI] [PubMed] [Google Scholar]
- 20.Syrmou E Tsitsopoulos PP Marinopoulos D et al. Spondylolysis: a review and reappraisal. Hippokratia. 2010;14(1):17-21. [PMC free article] [PubMed] [Google Scholar]
- 21.Tsirikos AI Garrido EG. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Br. 2010;92(6):751-759. [DOI] [PubMed] [Google Scholar]
- 22.Standaert CJ. Low back pain in the adolescent athlete. Phys Med Rehabil Clin N Am. 2008;19(2):287-304, ix. [DOI] [PubMed] [Google Scholar]
- 23.Cavalier R Herman MJ Cheung EV et al. Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006;14(7):417-424. [DOI] [PubMed] [Google Scholar]
- 24.Gregory PL Batt ME Kerslake RW. Comparing spondylolysis in cricketers and soccer players. Br J Sports Med. 2004;38(6):737-742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young JA Cuff SC Yang J et al. Comparison of spinal and pelvic posture and muscle flexibility in those with spondylolytic and non-spondylolytic low back pain. J Musculoskel Res. 2016;19(03):1650011. [Google Scholar]
- 26.Alqarni AM Schneiders AG Cook CE et al. Clinical tests to diagnose lumbar spondylolysis and spondylolisthesis: A systematic review. Phys Ther Sport. 2015;16(3):268-275. [DOI] [PubMed] [Google Scholar]
- 27.Grodahl LH Fawcett L Nazareth M et al. Diagnostic utility of patient history and physical examination data to detect spondylolysis and spondylolisthesis in athletes with low back pain: A systematic review. Man Ther. 2016;24:7-17. [DOI] [PubMed] [Google Scholar]
- 28.Masci L Pike J Malara F et al. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40(11):940-946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gregg CD Dean S Schneiders AG. Variables associated with active spondylolysis. Phys Ther Sport. 2009;10(4):121-124. [DOI] [PubMed] [Google Scholar]
- 30.Beck NA Miller R Baldwin K et al. Do oblique views add value in the diagnosis of spondylolysis in adolescents? J Bone Joint Surg Am. 2013;95(10):e65. [DOI] [PubMed] [Google Scholar]
- 31.Kobayashi A Kobayashi T Kato K et al. Diagnosis of radiographically occult lumbar spondylolysis in young athletes by magnetic resonance imaging. Am J Sports Med. 2013;41(1):169-176. [DOI] [PubMed] [Google Scholar]
- 32.Miglioretti DL Johnson E Williams A et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller R Beck NA Sampson NR et al. Imaging modalities for low back pain in children: a review of spondyloysis and undiagnosed mechanical back pain. J Pediatr Orthop. 2013;33(3):282-288. [DOI] [PubMed] [Google Scholar]
- 34.Rush JK Astur N Scott S et al. Use of magnetic resonance imaging in the evaluation of spondylolysis. J Pediatr Orthop. 2015;35(3):271-275. [DOI] [PubMed] [Google Scholar]
- 35.Ledonio CG Burton DC Crawford CH 3rd et al. Current evidence regarding diagnostic imaging methods for pediatric lumbar spondylolysis: a report from the scoliosis research society evidence-based medicine committee. Spine Deform. 2017;5(2):97-101. [DOI] [PubMed] [Google Scholar]
- 36.Tofte JN CarlLee TL Holte AJ et al. Imaging pediatric spondylolysis: a systematic review. Spine. 2017;42(10):777-782. [DOI] [PubMed] [Google Scholar]
- 37.Brodke DS Goz V Lawrence BD et al. Oswestry disability index: a psychometric analysis with 1,610 patients. Spine J. 2017;17(3):321-327. [DOI] [PubMed] [Google Scholar]
- 38.Kent P Grotle M Dunn KM et al. Rasch analysis of the 23-item version of the Roland Morris Disability Questionnaire. J Rehabil Med. 2015;47(4):356-364. [DOI] [PubMed] [Google Scholar]
- 39.Hall AM Maher CG Latimer J et al. The patient-specific functional scale is more responsive than the Roland Morris disability questionnaire when activity limitation is low. Eur Spine J. 2011;20(1):79-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.d’Hemecourt PA Zurakowski D d’Hemecourt CA et al. Validation of a new instrument for evaluating low back pain in the young athlete. Clin J Sport Med. 2012;22(3):244-248. [DOI] [PubMed] [Google Scholar]
- 41.MacDonald JP d'Hemecourt PA Micheli LJ. The reliability and validity of a pediatric back outcome measure. Clin J Sport Med. 2016;26(6):490-496. [DOI] [PubMed] [Google Scholar]
- 42.Kurd MF Patel D Norton R et al. Nonoperative treatment of symptomatic spondylolysis. J Spinal Disord Tech. 2007;20(8):560-564. [DOI] [PubMed] [Google Scholar]
- 43.Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52(3):432-437. [PubMed] [Google Scholar]
- 44.Nicol RO Scott JH. Lytic spondylolysis. Repair by wiring. Spine. 1986;11(10):1027-1030. [DOI] [PubMed] [Google Scholar]
- 45.Radcliff KE Kalantar SB Reitman CA. Surgical management of spondylolysis and spondylolisthesis in athletes: indications and return to play. Curr Sports Med Rep. 2009;8(1):35-40. [DOI] [PubMed] [Google Scholar]
- 46.Bouras T Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. Eur J Orthop Surg Traumatol. 2015;25 Suppl 1:S167-175. [DOI] [PubMed] [Google Scholar]
- 47.El Rassi G Takemitsu M Woratanarat P et al. Lumbar spondylolysis in pediatric and adolescent soccer players. Am J Sports Med. 2005;33(11):1688-1693. [DOI] [PubMed] [Google Scholar]
- 48.El Rassi G Takemitsu M Glutting J et al. Effect of sports modification on clinical outcome in children and adolescent athletes with symptomatic lumbar spondylolysis. Am J Phys Med Rehabil. 2013;92(12):1070-1074. [DOI] [PubMed] [Google Scholar]
- 49.Sys J Michielsen J Bracke P et al. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Eur Spine J. 2001;10(6):498-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iwamoto J Takeda T Wakano K. Returning athletes with severe low back pain and spondylolysis to original sporting activities with conservative treatment. Scand J Med Sci Sports. 2004;14(6):346-351. [DOI] [PubMed] [Google Scholar]
- 51.Standaert CJ. Spondylolysis in the adolescent athlete. Clin J Sport Med. 2002;12(2):119-122. [DOI] [PubMed] [Google Scholar]
- 52.Selhorst M Fischer A Graft K et al. Timing of physical therapy referral in adolescent athletes with acute spondylolysis: a retrospective chart review. Clin J Sport Med. 2017;27(3):296-301. [DOI] [PubMed] [Google Scholar]
- 53.d'Hemecourt PA Zurakowski D Kriemler S et al. Spondylolysis: returning the athlete to sports participation with brace treatment. Orthopedics. 2002;25(6):653-657. [DOI] [PubMed] [Google Scholar]
- 54.Kraft DE. Low back pain in the adolescent athlete. Pediatr Clin North Am. 2002;49(3):643-653. [DOI] [PubMed] [Google Scholar]
- 55.McTimoney CA Micheli LJ. Current evaluation and management of spondylolysis and spondylolisthesis. Curr Sports Med Rep. 2003;2(1):41-46. [DOI] [PubMed] [Google Scholar]
- 56.Steiner ME Micheli LJ. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine. 1985;10(10):937-943. [DOI] [PubMed] [Google Scholar]
- 57.King HA. Back Pain in Children. Orthop Clin North Am. 1999;30(3):467-474. [DOI] [PubMed] [Google Scholar]
- 58.Kessous E Borsinger T Rahman A et al. Contralateral spondylolysis and fracture of the lumbar pedicle in a young athlete. Spine. 2017;42(18):E1087-e1091. [DOI] [PubMed] [Google Scholar]
- 59.Hu SS Tribus CB Diab M et al. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671. [PubMed] [Google Scholar]
- 60.Selhorst M Fischer A Graft K et al. Long-rerm clinical outcomes and factors that predict poor prognosis in athletes after a diagnosis of acute spondylolysis: a retrospective review with telephone follow-up. J Orthop Sports Phys Ther. 2016;46(12):1029-1036. [DOI] [PubMed] [Google Scholar]
- 61.Sousa T Skaggs DL Chan P et al. Benign natural history of spondylolysis in adolescence with midterm follow-up. Spine Deform. 2017;5(2):134-138. [DOI] [PubMed] [Google Scholar]
- 62.Overley SC McAnany SJ Andelman S et al. Return to play in adolescent athletes with symptomatic spondylolysis without listhesis: a meta-analysis. Global Spine J. 2018;8(2):190-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ahlqwist A Hagman M Kjellby-Wendt G et al. Physical therapy treatment of back complaints on children and adolescents. Spine. 2008;33(20):E721-727. [DOI] [PubMed] [Google Scholar]
- 64.Selhorst M Selhorst B. Lumbar manipulation and exercise for the treatment of acute low back pain in adolescents: a randomized controlled trial. J Man Manip Ther. 2015; 23:226-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86-a(2):382-396. [DOI] [PubMed] [Google Scholar]
- 66.Miller SF Congeni J Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med. 2004;32(4):928-933. [DOI] [PubMed] [Google Scholar]
- 67.Covassin T Beidler E Ostrowski J et al. Psychosocial aspects of rehabilitation in sports. Clin Sports Med. 2015;34(2):199-212. [DOI] [PubMed] [Google Scholar]
- 68.Tracey J. The emotional response to the injury and rehabilitation process. Journal of Applied Sport Psychology. 2003;15(4):279-293. [Google Scholar]
- 69.Mainwaring LM. Restoration of self: A model for the psychological response of athletes to severe knee injuries. Canadian Journal of Rehabilitation. 1999;12:143-154. [Google Scholar]
- 70.O'Sullivan P Smith A Beales D et al. Understanding adolescent low back pain from a multidimensional perspective: Implications for management. J Orthop Sports Phys Ther. 2017;47(10):741-751. [DOI] [PubMed] [Google Scholar]
- 71.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423-1433. [PMC free article] [PubMed] [Google Scholar]
- 72.Sakamaki T Katoh S Sairyo K. Normal and spondylolytic pediatric spine movements with reference to instantaneous axis of rotation. Spine. 2002;27(2):141-145. [DOI] [PubMed] [Google Scholar]
- 73.Mimura M. [Rotational instability of the lumbar spine--a three-dimensional motion study using bi-plane X-ray analysis system]. Nihon Seikeigeka Gakkai Zasshi. 1990;64(7):546-559. [PubMed] [Google Scholar]
- 74.Niggemann P Kuchta J Beyer HK et al. Spondylolysis and spondylolisthesis: prevalence of different forms of instability and clinical implications. Spine. 2011;36(22):E1463-1468. [DOI] [PubMed] [Google Scholar]
- 75.Wang JP Zhong ZC Cheng CK et al. Finite element analysis of the spondylolysis in lumbar spine. Biomed Mater Eng. 2006;16(5):301-308. [PubMed] [Google Scholar]
- 76.O'Sullivan PB Phyty GD Twomey LT et al. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959-2967. [DOI] [PubMed] [Google Scholar]
- 77.Ward SR Kim CW Eng CM et al. Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J Bone Joint Surg Am. 2009;91(1):176-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Delitto A George SZ Van Dillen LR et al. Low back pain. J Orthop Sports Phys Ther. 2012;42(4):A1-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lawrence KJ Elser T Stromberg R. Lumbar spondylolysis in the adolescent athlete. Phys Ther Sport. 2016;20:56-60. [DOI] [PubMed] [Google Scholar]
- 80.Berger RG Doyle SM. Spondylolysis 2019 update. Curr Opin Pediatr. 2019;31(1):61-68. [DOI] [PubMed] [Google Scholar]
- 81.Singh H Lee M Solomito MJ et al. Lumbar hyperextension in baseball pitching: A potential cause of spondylolysis. J Appl Biomech. 2018:1-6. [DOI] [PubMed] [Google Scholar]
- 82.Smith J. Moving beyond the neutral spine: stabilizing the dancer with lumbar extension dysfunction. J Dance Med Sci. 2009;13(3):73-82. [PubMed] [Google Scholar]
- 83.Sueki DG Cleland JA Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013;21(2):90-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shimamura KK Cheatham S Chung W et al. Regional interdependence of the hip and lumbo-pelvic region in divison ii collegiate level baseball pitchers: a preliminary study. Int J Sports Phys Ther. 2015;10(1):1-12. [PMC free article] [PubMed] [Google Scholar]
- 85.Hoogenboom BJ Kiesel K. 74 - Core stabilization training. In: Giangarra CE, Manske RC editors. Clinical Orthopaedic Rehabilitation: a Team Approach (Fourth Edition). Philadelphia: 2018. p. 498-513.e491. [Google Scholar]
- 86.Purcell L Micheli L. Low back pain in young athletes. Sports Health. 2009;1(3):212-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bugg WG Lewis M Juette A et al. Lumbar lordosis and pars interarticularis fractures: a case-control study. Skeletal Radiol. 2012;41(7):817-822. [DOI] [PubMed] [Google Scholar]
- 88.Wasser JG Zaremski JL Herman DC et al. Prevalence and proposed mechanisms of chronic low back pain in baseball: part i. Res Sports Med. 2017;25(2):219-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Storheim K Bo K Pederstad O et al. Intra-tester reproducibility of pressure biofeedback in measurement of transversus abdominis function. Physiother Res Int. 2002;7(4):239-249. [DOI] [PubMed] [Google Scholar]
- 90.Hebert JJ Koppenhaver SL Teyhen DS et al. The evaluation of lumbar multifidus muscle function via palpation: reliability and validity of a new clinical test. Spine J. 2015;15(6):1196-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Saur PM Ensink FB Frese K et al. Lumbar range of motion: reliability and validity of the inclinometer technique in the clinical measurement of trunk flexibility. Spine. 1996;21(11):1332-1338. [DOI] [PubMed] [Google Scholar]
- 92.Hicks GE Fritz JM Delitto A et al. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84(12):1858-1864. [DOI] [PubMed] [Google Scholar]
- 93.Arab AM Salavati M Ebrahimi I et al. Sensitivity, specificity and predictive value of the clinical trunk muscle endurance tests in low back pain. Clin Rehabil. 2007;21(7):640-647. [DOI] [PubMed] [Google Scholar]
- 94.Hurd W Hunter-Giordano A Axe M et al. Data-based interval hitting program for female college volleyball players. Sports Health. 2009;1(6):522-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Spigelman T Sciascia A Uhl T. Return to swimming protocol for competitive swimmers: a post-operative case study and fundamentals. Int J Sports Phys Ther. 2014;9(5):712-725. [PMC free article] [PubMed] [Google Scholar]
- 96.Jayanthi N Esser S. Racket sports. Curr Sports Med Rep. 2013;12(5):329-336. [DOI] [PubMed] [Google Scholar]
- 97.Chang ES Bishop ME Baker D et al. Interval throwing and hitting programs in baseball: Biomechanics and rehabilitation. Am J Orthop. 2016;45(3):157-162. [PubMed] [Google Scholar]
- 98.Sweeney EA Howell DR James DA et al. Returning to sport after gymnastics injuries. Curr Sports Med Rep. 2018;17(11):376-390. [DOI] [PubMed] [Google Scholar]