Abstract
Background/Purpose:
Hamstring strain (HS), a common condition found among the injured physically active population, is often treated with rest, stretching, and modalities. Primal Reflex Release Technique™ (PRRT™) is a manual therapy technique used to treat pain caused by over-stimulation of the body's primal reflexes. The purpose of this case series was to explore the immediate effects of PRRT™ for treating hamstring strains.
Description of Cases:
A multi-site case series approach was used to report on the treatment of six patients with HS using PRRT™. The Numeric Pain Rating Scale (NPRS), Patient Specific Functional Scale (PSFS) and range of motion (ROM) measurements were collected, as well as evaluation of symmetry of the sacroiliac joints, reported as sacroiliac dysfunction(SJD).
Outcomes:
Primal Reflex Release Technique™ (PRRT™) was an effective treatment for subjects with HS. Subjects reported a significant decrease in pain on the NPRS, averaging five points over the course of the treatment (95% CI of 3.374, 6.626). Functional measures on the PSFS were significantly improved following treatment (post-treatment mean = 7.8 ± 1.84, pre-treatment mean = 4.8 ± .97, p < .001; CI: -2.1, -3.9). The mean change on the Passive Knee Extension Test (PKE) (mean = 8.20 ° ± 3.96 °) and ASLR (mean = 10.333 ° ± 8.98 °) indicated statistically significant improvements of post-treatment ROM (mean change = 8.20 ° ± 3.96 °, p = .01). The presence of SJD was observed in all subjects prior to treatment and resolved in all subjects when reassessed after treatment.
Discussion:
In this case series, the use of PRRT™ resulted in decreased pain, increased function, and increased range of motion, as well as resolved SJD. The Primal Reflex Release Technique™ may be useful in decreasing symptoms of HS acutely, but long-term effects are unknown at this time. Clinicians should consider using a treatment which targets the autonomic nervous system when addressing pain associated with HS.
Level of Evidence:
Level 4 - case series
Keywords: Autonomic nervous system, primal reflex, sacroiliac joint dysfunction, up-regulation
Introduction
The incidence and re-injury rates of hamstring strain (HS) in the physically active have not improved over the past thirty years.1 The hamstrings continue to be the most commonly strained multi-joint muscle group in the active population.2-5 For example, Serner et al. reported that 8-18% of all soccer injuries are HS related.6 Although researchers currently debate the primary cause of HS, possible contributing factors include decreased hamstring length, previous HS injury, and/or muscle imbalances between the hamstring and quadriceps muscles.7 Diagnosis of HS severity is traditionally based on clinical signs and symptoms collected from the history and physical examination.8,9 The physical examination includes palpation for tenderness, swelling, and/or deformity, manual muscle testing, and bilateral range of motion assessment.8 Generally, clinicians utilize the grading scale to classify a first, second or third-degree strain based on signs and symptoms found during the clinical exam (Table 1).9
Table 1.
Muscle grading.9
| Grading Scale | Definition |
|---|---|
| Mild (First Degree) | Tear of a few muscle fibers with minor swelling or discomfort. No associated loss of strength, limited range of motion, or deformity. |
| Moderate (Second degree) | Greater damage to muscle with clear loss of strength. May have limited range of motion, visible muscle damage including bruising/swelling, and includes pain. |
| Severe (Third Degree) | Total lack of muscle function. Loss of strength, loss of range of motion, muscle damage. |
The presence of pelvic abnormalities in soccer players has been linked to hamstring dysfunction and muscle strain.10-14 Previously, Cibulka, Rose, Delitto, and Sinacore15 reported participants diagnosed with HS also commonly present with sacroiliac joint dysfunction (SJD), which was defined as asymmetrical innominates. Treatment incorporating manipulation of the sacroiliac (SI) joint with a high velocity manipulation (HVLA) resulted in increased ability to create force in the hamstrings (as indicated by increased peak hamstring torque) and also resolved SJD.15 Asymmetrical iliac bones or malalignment of the innominates (i.e., SJD) may add tension to muscles that are attached to the pelvic girdle,16 which may predispose a patient to mechanical injury at the hamstrings.17 After injury, the autonomic nervous system (ANS) may remain in a heightened state of sensitivity in order to protect from further injury. This state may be referred to as “up-regulated” and can be associated with pain, muscle spasm, muscle guarding, and altered motor behavior.18 An intervention aimed at down regulation of the nerves innervating the hamstring muscles may be helpful in addressing the symptoms of up-regulation and HS compared to traditional treatments that address tissue healing through lengthening or strengthening the hamstring muscle.
The Primal Reflex Release Technique™ (PRRT™) is a treatment paradigm theorized to decrease pain and muscle spasm by targeting, resetting reflexes, and using reciprocal inhibition to “down regulate” the autonomic nervous system (ANS).18 Reflexes can produce protective muscle contraction during the fight or flight response after injury.19 The ANS enacts a release of messenger chemicals including acetylcholine20 and serotonin19 which reinforces the protective spasm or trigger points while the patient's pain continues. The overactive neurons create a cutaneous or nociceptive stimulus affecting the muscle spindles that in turn affect the length and tension of a muscle.21 When mechanical tension is present, as a result of up-regulated areas of facilitated muscle(s), stimulation of reflexes may be beneficial as a treatment because as the “the agonist muscle receives a nerve impulse to contract, its antagonist simultaneously receives an impulse to relax.”22 Targeting reflexes to stimulate a contraction of the antagonist muscle can be used to produce a signal from the ANS to relax the protective mechanisms in the agonist muscle.23 The Primal Reflex Release Technique™ utilizes the relationship between agonist and antagonist muscles to increase the afferent activity gained from the mechanoreceptors, resulting in a neurological downregulation of the muscles.23
The Primal Reflex Release Technique™ may be suited for patients diagnosed with HS because PRRT™ utilizes reflexive stimulation to downregulate the protective response of the ANS to treat both pain in the musculoskeletal system and address possible upregulation or protective muscle contractions.18 A cluster protocol of five PRRT™ techniques has been introduced as a recommended treatment for the hamstring muscles, addressing the reflexes along the sciatic nerve pathway.24 The purpose of this case series was to explore the immediate effects of PRRT™ for treating hamstring strains.
METHODS
Description of Cases: Subject History and Systems Review
Ethical approval was obtained from the Institutional Review Board prior to beginning data collection; signed informed consent was collected from each participant prior to study inclusion. The study was conducted using six patients who presented to the athletic training clinics at two locations (Clinic A had three patients, Clinic B had three patients) with hamstring pain. Patient histories are presented in Table 2.
Table 2.
Narrative summary of initial findings
| Patient | Age | Sex | Sport | Patient History Physical Exam |
Hamstring Diagnosis |
|---|---|---|---|---|---|
| 1 | 20 | M | Track | Presented after a sprint in which he felt a pull on the lateral side of the right hamstring. Reported a current pain (on the NPRS) of 7 while resting and 9 while attempting to run. Rated pain on resisted knee flexion and hip extension as 8. Rated pain on PROM PKET as 8. SIJ dysfunction noted on the forward bend, with the right SIJ rotated anteriorly on return-to-standing, compared bilaterally. Goniometric measurement of PKET was 41 degrees. ASLR was 50 degrees. |
Grade 1 |
| 2 | 23 | M | Track | Presented after a sprint in which he felt a pull on the medial side of the left hamstring. Reported a current pain of 5 while resting and 8 while attempting to run. Left innominate appeared to be rotated anteriorly when palpated and compared to the right side. Goniometric measurement of PKET was 46 degrees. ASLR was 95 degrees. |
Grade 1 |
| 3 | 46 | M | Competitive stair climbing | Presented after a stair climbing competition with pain in the right lateral hamstring. Rated a pain 6 while resting and 8 while doing stairs. SIJ dysfunction noted on the forward bend, with right SIJ rotated anteriorly on return to standing compared bilaterally. Goniometric measurement of PKET was 31 degrees. ASLR was 87 degrees. |
Grade 1 |
| 4 | 17 | M | Football | Presented after football practice including place-kicking practice in the right. Rated pain 5 at rest and 6 while running. SI dysfunction noted during standing and hip flexion test as well as prone leg length test. Goniometric measurement of PKET was 67 degrees. ASLR was 70 degrees. |
Grade 1 |
| 5 | 17 | M | Football | Presented after football practice with pain in right proximal hamstring. Left innominate anteriorly rotated and positive hip flexion test and leg length test. ASLR was measured as 67 degrees. PKET not collected due to time constraints. |
Grade 1 |
| 6 | 15 | F | Basketball | Presented after basketball practice and noted pain in left hamstring after a sudden stop. SIJ dysfunction noted during palpation in supine and standing and decreased motion in left SIJ during forward flexion. Goniometric measurement of PKET was 48 degrees. ASLR was 55 degrees. |
Grade 1 |
NPRS = Numeric Pain Rating Scale; PROM = Passive Range of Motion; PKET = Passive Knee Extension Test; SIJ = Sacroiliac Joint; ASLR = Active Straight Leg Raise
Subjects were excluded if any overt neurologic signs/conditions, such as sensory paresthesia or motor paresis, present during the initial evaluation or if the patient had a medical history of recent fracture, previously diagnosed neurological condition, or previous spinal surgery.
Clinical Impression #1
Subjects were included in the study if they had the presence of signs and/or symptoms of HS, all subjects presented with grade one HS (Table 1).9 The signs and symptoms of a HS matched those used in the previous study assessing SJD and hamstring strains and were defined as pain and/or ecchymosis localized to involved muscle, pain on resistive isometric position (knee flexion with hip extension), and/or pain on passive range of motion (PROM) of the involved muscle (hip flexion with the knee flexed and extended).15
Examination and Reliability
The initial examination included an extensive history relating to pain location, intensity, and mechanism of injury. All subjects (N = 6) presented to the athletic training clinic within 72 hours after feeling pain in their hamstring during activity (pain was not reported prior to the activity).
The examination also included an assessment of SJD defined as an examination of innominate alignment.15,25 Both investigators utilized the same protocol for assessing the level of the anterior superior iliac spine (ASIS).25 The subjects were assessed in supine and standing positions and the SI joint at the posterior superior iliac spine (PSIS) with movement during weight bearing forward flexion of the hips, standing hip and knee flexion (marching) alternating legs, and supine leg-length assessments.25 Sacroiliac joint dysfunction was noted with positive or negative results on these three special tests pre and post-intervention, a negative result was only recorded if all three tests were negative.25 If one, two, or three of the tests were positive, the result recorded was positive.25 Assessment of SJD was categorized as asymmetrical (positive) or symmetrical (negative).15,25
Each investigator collected passive knee extension test (PKET) and active straight leg raise (ASLR) measurements at their respective clinics, and intra-rater reliability was established for each rater prior to data collection (Table 3). Reliability in assessing SJD is reported to range between excellent reliability (Kappa coefficient of .88)26 and poor reliability (kappa range of .11 to .23).27 Importantly, reliability increases with cluster testing of pain provocation tests (five positive tests resulted in a specificity of .88).28 In cases where pain may originate away from the site of dysfunction (known as regional interdependence),29 identifying the presence of SJD even when pain is not present may be helpful. The first investigator had seven years of athletic training experience. The second investigator had 11 years of athletic training experience. Both investigators completed the PRRT™ home-study course24 and a level-one PRRT™ course prior to completing the study.30
Table 3.
Intra-rater reliability for range of motion.
| Variable | Rater 1 | SEM | MDC | Rater 2 | SEM | MDC |
|---|---|---|---|---|---|---|
| PKET (average of 3 reps) | 0.966° | 3.106° | 8.608° | .843° | 2.380° | 6.596° |
| ASLR L (average of 3 reps) | 0.981° | 2.119° | 5.872° | .984° | 1.897° | 5.2582° |
PKET = Passive Knee Extension Test; ASLR = Active Straight Leg Raise L = Left-side
In this case series, the researchers used PRRT™, and collected outcomes for pain, function, range of motion and SJD. Patient outcomes were collected using the Numeric Pain Rating Scale (NPRS) and the Patient Specific Functional Scale (PSFS). Clinician-rated outcomes were collected in the form of range-of-motion (ROM) measurements for PKET and ASLR along with SJD.
Clinical Impression #2
The subjects all were within normal limits for manual muscle testing (knee flexion, knee extension, hip flexion). Two of the six subjects had decreased ASLR results compared to normal ranges prior to treatment while PKET measurements were all limited compared to reported norms (Table 2). All six subjects were categorized as asymmetrical SJD (positive tests) prior to treatment.
INTERVENTION
Outcome Measures
The NPRS and PSFS were collected at initial evaluation and following the first treatment. Patients were asked to rate their pain on a scale of 0-10 (0 = no pain; 10 = worst pain imaginable).31 An improved change in score of 2 points (or more) on the NPRS indicate a minimally clinically important difference (MCID).32 The clinicians used the PSFS score to determine the functional status of the patient.33 The patient self-selected two to three functional measures (tasks) and rated their ability to complete each task (0 = unable to perform an activity; 10 = able to perform an activity at the same level as before the injury).33 The minimal detectable change (MDC) is three points for an average of the three functions and is two points for a single function.34 The clinician-rated outcomes obtained were PKE and ASLR range-of-motion measurements at initial evaluation and following the first treatment. The clinician recorded the outcome of SJD on all tests (standing flexion test, sitting forward flexion test, and prone knee flexion test).
Treatment Procedure
Each subject, after consenting and meeting inclusion criteria, was treated using similar methods as Cibulka, et al,15 however, in the current study, the use of PRRT™ treatment replaced the HVLA manipulation. Prior to treatment, each patient used a moist heat pack for 10 minutes on the involved hamstring in order to replicate the Cibulka study.15 The following techniques of PRRT™ were then completed: plantar reflex (primal), SI/Lumbar and L1 release, hamstring release, gastrocnemius release and eversion release as recommended in the PRRT guidelines.30 This cluster protocol of five PRRT™ techniques were chosen to focus on downregulating musculature of the posterior chain and targeting the specific release of the sciatic nerve.30 Each technique was applied for 12 seconds exept for the planar reflex which was held for one minute. All patients were treated following the same protocol.
The plantar reflex is used to treat lower quarter pain conditions from the lumbar area down to the foot.18 The patient, was positioned supine with the foot over the edge of the plinth (Figure 1), and was asked to hold a pencil between his toes while maintaining full plantar flexion and the motion of inversion to eversion for one minute.
Figure 1.
Plantar Release PRRT™: Patient plantar-flexes ankle and holds pen with toes for 1 minute.
The SI/Lumbar and L1 release was used to address an upregulation of the ANS specific to the coccyx, SI, Lumbar, or L1 areas.18 The patient was positioned supine on the plinth (Figure 2). The patient was asked to bend their affected-side knee to 90 degrees and move the knee over the unaffected-side leg. The clinician stood on the unaffected side and provided static resistance as the patient contracted hip abductors. The patient was then asked to hold isometric abduction and external rotation against the clinician with the affected side while hiking the opposite hip upward.18 The patient slowly exhaled while performing the technique for 12 seconds for one application.18
Figure 2.
S1/Lumbar Release PRRT™: Patient adducts leg with hip flexion. The clinician resists against abduction of the hip.
The hamstring release was used to address an upregulation of the ANS for the hamstring area.18 The patient was positioned in supine, and the involved hip was flexed to 45 degrees (Figure 3). The knee was flexed to 20 degrees. The Simultap technique was then applied for 12 seconds: The clinician tapped (i.e., stimulate deep tendon reflex) on two separate areas at the same time. In this case, the Simultap was used for the mid-belly of the hamstring (involved) and the patellar tendon.
Figure 3.
Hamstring Release PRRT™: Patient hip flexes to 90 degrees, knee flexed Simultaps hamstring tendons and patellar tendon.
The gastrocnemius release was applied as a fourth PRRT™ component to treat lower quarter pain (Figure 4).18 The patient was positioned in supine, and the hip and knee were flexed (45 degrees and 90 degrees respectively) with the ankles in 90 degrees of dorsiflexion. A Simultap was used on the ankle dorsiflexors and the patellar tendon.18
Figure 4.
Patient hip-flexes and knee-flexes; clinician to 90 degrees; clinician simultaps on patellar tendon and on dorsiflexors of ankle.
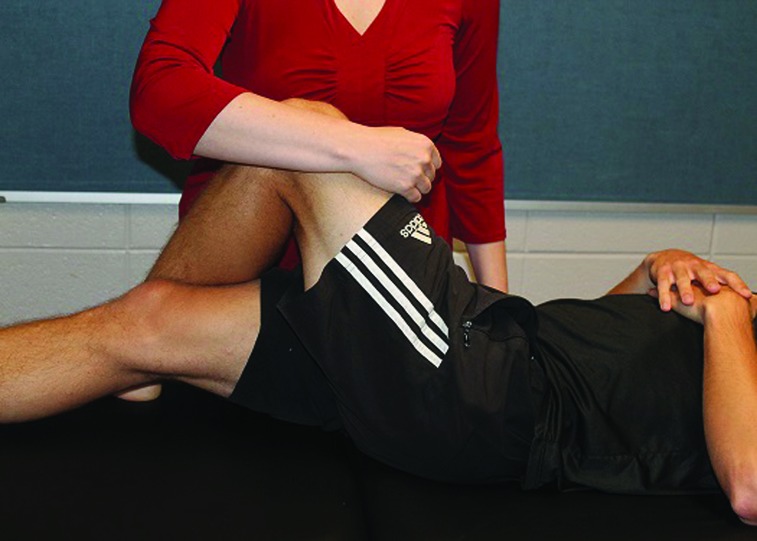
For consistency with the Cilbulka et al. case report, following the PRRT™ treatment the clinician began passive stretching of the patient's hamstring (Figure 5). The clinician completed three repetitions of 30-second holds at the patient's point of comfort.
Figure 5.
Stretching Passive Hamstring Technique: Clinician moves leg to hip flexion and knee extension and holds at end; patient stretches for 30 seconds.
Results and Outcomes
Both clinician and patient rated outcomes were assessed prior to and following treatment to the six patients treated with PRRT™. Outcomes of NPRS, PSFS and range of motion were both clinically and statistically significant different compared to pre-treatment measurements with an a priori alpha level set at .05 and 95% confidence intervals (Table 4). Paired t-tests of pre-treatment and post-treatment measurements were performed on range of motion (both PKET and ASLR). Cohen's d effect sizes were calculated using the formula d = (M2 - M1) / SDpooled where M equals the mean and SD is the pooled standard deviation (Table 4).35
Table 4.
Change in overall patient and clinician outcomes from initial evaluation to post-treatment.
| Outcome Measure | N | Mean Pre-treatment Score | Mean Post-treatment Score | Mean Change in Score | p-value | Confidence Interval | Cohen's d | Power |
|---|---|---|---|---|---|---|---|---|
| NPRS | 6 | 5.7 | .67 | 5.0 | .001* | 3.4, 6.6 | 6.1 | 1.00 |
| PSFS | 6 | 4.8 | 7.8 | 3.0 | .000* | −2.1, −3.9 | 1.9 | 1.00 |
| PKET | 5 | 58.4° | 66.6° | 8.2° | .010* | 3.3, 13.11 | .81 | .853 |
| ASLR | 6 | 69.8° | 80.2° | 10.3° | .037* | .9, 19.8 | .67 | 1.00 |
N = Number of patients; NPRS = Numeric Pain Rating PKET = Passive Knee Extension Test; ASLR = Active Straight Leg Raise
Note for PSFS that a negative number represents a positive change for the patient outcome.
Statistically significant difference at p < 0.05.
Pain: Numeric Pain Rating Scale
Pain scores on the NPRS (N=6) averaged 5.7 pre-treatment and .67 immediately following the PRRT™ treatment. A statistically significant difference from the pre- (5.67 ± .33) to post-test measurement (.67 ± .33) was found (t(6) = 7.91 p = .001, two-tailed). The Cohen's d value of 6.1 suggests a large effect size from the NPRS rating pre-treatment to post-treatment.35 The mean decrease in pain was 5.0, which exceeds the MCID of 2.0 and is clinically significant.32
Function: Patient Specific Functional Scale and Range of Motion
The mean functional score of 7.8 was calculated for the six subjects indicating a high level of function was present after the PRRT™ treatment compared to a mean score of less than five (4.8) for the scores prior to treatment. A statistically significant difference from the pre- (4.8 ± .94) to post-test measurement (7.8 ± 1.86) was found (t(6) = 3.526, p = .000, two-tailed). Analysis of the change in mean PSFS scores from pretreatment to post treatment scores 35,36 resulted in a Cohen's d of 1.9, suggesting a large effect size from the treatment.35 Five of the six patients exceeded a large change MCID of 2.7 in total PSFS mean score.34 All PSFS results, including specific tasks for each subject, can be seen in Table 5.
Table 5.
Patient specific functional scale: pre and post-treatment information
| ID | Activity 1 | Pre | Post | Activity 2 | Pre | Post | Activity 3 | Pre | Post |
|---|---|---|---|---|---|---|---|---|---|
| 1 | running | 6 | 8 | squats | 5 | 7 | stairs down | 6 | 9* |
| 2 | running | 4 | 4 | squat | 5 | 6 | lunge | 5 | 7 |
| 3 | running | 4 | 5 | squat | 4 | 5 | stairs down | 5 | 8* |
| 4 | running | 5 | 9* | cutting | 4 | 10* | stance | 5 | 8* |
| 5 | running | 6 | 9* | squats | 5 | 8* | drop step | 2 | 7* |
| 6 | running | 5 | 10* | stairs down | 5 | 10* | N/A | N/A | |
| N | Mean Pre-Treatment Score | Mean Post Treatment Score | Mean Change in Score | ||||||
| 6 | 4.8 | 7.8 | 3.0* | ||||||
satisfies minimal detectable change identified for total PSFS score of 330
Passive Knee Extension Test
An immediate increase in the mean range of motion measurement of PKET was found from pre to post-treatment (mean of 8.20 degrees). A statistically significant difference between the pre-PKET (mean = 58.40 ° ± 8.82 °) and the post-PKET (mean = 66.60 ° ± 11.26 °) was found (p = .01; Table 4). The mean change (mean = 8.20 ° ± 3.96 °) suggests that the treatment was nearly effective enough to produce a clinically significant difference (MDC of 8.60 °) and the Cohen's d value of .81 suggests a large effect size from the treatment.35
Active Straight Leg Raise
An increase in ASLR range of motion was found when comparing pre-treatment to post-treatment measurements (10.3 degrees). A statistically significant difference between the pre-ASLR (mean = 69.83 ° ± 16.27 °) and the post-ASLR (mean = 80.17 ° ± 14.39 °) was found (p = .037; 95% CI: .908, 19.759; Table 4). The mean change (mean = 10.33 ° ± 8.98 °) suggests that the treatment was clinically significant, surpassing the MCID (5.9 °) after one visit and the Cohen's d value of .67 suggests a medium effect size from the treatment.35
Sacroiliac Joint Dysfunction
A resolution of SJD occurred after one treatment for 100% of the patients (N = 6). Resolution of previously assessed SJD was observed in all six patients.
DISCUSSION
The purpose of this case series was to examine the immediate effects of a PRRT treatment on subject's symptoms following a HS including pain, function, and presence of SJD. The results provide preliminary evidence that the use of the PRRT protocol can produce immediate changes that are clinically and statistically significant following a first-degree HS (N=6). The single PRRT treatment produced substantial improvement in measures of pain (NRS) and function (PSFS and ROM). The results of this case series are unique as the treatment used which focuses on the proposed mechanism of downregulating the neuromuscular system is not commonly used. The results of this case series provide initial support that this type of treatment may be effective for reducing pain and dysfunction following a first degree HS.
In two additional case series assessing the use of PRRT™, both Hansberger36 and Honeycutt37 reported immediate changes in pain and function using PRRT™, although their studies were focused on patients complaining of plantar fasciitis36 and breathing pattern dysfunctions.37 Pain was assessed using the NPRS and in each study a decrease in pain was reported (mean change score 5.0 points,36 and 3 points37). Hansen-Honeycutt et al.,37 reported that the decrease in pain may have been attributed to either restoring normal movement patterns or diminishing associated tender areas. When using PRRT™ to treat HS similar assumptions could apply; improvements to function (measured by the PSFS and range of motion) could be attributed to decreasing pain in the area or decreasing protective muscle spasm to improve motor control and recruitment of the hamstring muscle group.
In this case series, high functional levels were reported after PRRT™ treatment. In the case study performed by Cilbulka et al.15 immediate changes in function were assessed using HS torque values. Positive changes in function was reported in both the current case series as well as the Cilbulka et al.15 study (mean PSFS change of 3 points and mean torque change of 8.1 foot pounds). Addressing neuromuscular dysfunction (i.e., downregulating muscles of the posterior chain) in patients diagnosed with a Grade 1 HS may allow for quick resolution of symptoms as compared to the time it takes in the standard tissue healing model. The standard tissue healing model includes three overlapping phases: inflammatory response, fibroplastic repair, and maturation-remodeling phase.37 Symptoms caused by damage to the soft tissue can take up to three years to resolve during the maturation-remodeling phase.37 However, it should be noted that this case series did not follow subjects for the timeframe associated with the standard tissue healing model.
Perhaps a treatment focused on restoring motor control and muscle recruitment is a possible addition or alternative to traditional treatments for hamstring strains to induce meaningful outcomes. Up to 70% of MRI clinically diagnosed hamstring injuries include no evidence of fibrous tissue damage after examination. 38 Therefore, it may benefit clinicians to evaluate and treat grade one HS from a perspective where tissue damage is not the only cause of pathology. Theoretically, the symptoms reported in the grade one HS population may indicate dysfunction within the neuromuscular system. Primal Reflex Release Technique™ has been successful in resolving these symptoms immediately by targeting the downregulation of the posterior chain, which is in line with the idea that the dysfunction is occurring at the neurological level.38,40 By downregulating the muscles of the posterior chain, decreased hamstrings muscle tension may be attributed to the presence of a neurological dysfunction rather than a disruption of hamstring tissue. Faster symptom resolution in patients would be seen with treatments affecting the neurological system if the healing process is not needed to repair damaged tissue.
To track patient recovery, both patient-rated and clinician-rated outcomes can be measured with a focus on down regulating the nervous system resulting to influence the musculature. Two out of the six subject's measurements of active straight leg raise were less than the reported normal range of motion pre-treatment,41 while six out of six subjects were within normal range (65 degrees or more) post-treatment. All five subjects (one subject was not tested due to time constraints) with pre-treatment PKET measurements, demonstrated measures less than the reported normal range of motion (70-80 degrees).42 Following the single treatment of PRRT™, three of five subjects met normal ranges of motion on the PKET (Table 4).
Although the change in PKET after PRRT™ was statistically significant (mean change = 10 degrees), the comparison group in Cibulka's study utilizing heat and stretching alone was reported to have a PKET change of 12 degrees. Range of motion measurements (ROM) alone appear to indicate comparable changes to isolated treatments of heat and stretching, but the control groups ROM mean prior to treatment was less than normal (42 degrees) and remained less than normal ranges after treatment (54 degrees) indicating that, while change occurred, resolution of the deficient ROM was not seen in the control group. In the current study, three of the five subjects treated with PRRT™ had measurements within normal range after treatment. Furthermore, when combined with the significant changes in pain and function ratings a treatment including PRRT™ appears to have a positive effect on the patient's symptoms as well as possible increases in range of motion. Further research comparing signs and symptoms of HS to the treatment of heat and stretch alone would allow for clearer comparisons of how PRRT™ effects HS.
Treatment utilizing PRRT™ may also have positive effects on SJD. Faulty movement patterns may predispose active individuals to HS and SJD. Cluster testing can be used to determine whether a patient has SJD.26 The PRRT™ treatment was designed to downregulate the neuromuscular system at the posterior chain which likely positively affected the SI joint. Further consideration and research is warranted on the treatment of SJD with PRRT™.
LIMITATIONS
Several limitations occurred due to the choice of following the design of the case report by Cibulka et al.,15 including application of a heat pack before treatment and clinician-applied static stretching after treatment, which add to the variables to consider when assessing the results. Either of these two interventions could also have affected the results of the study. This case series lacked a control group, which did not allow for comparison to another intervention or to no intervention. The researchers accepted these limitations with the intent to compare to the outcomes of function and range of motion to the previously collected data in the Cibulka study.15
While intra-rater reliability of range of motion was established prior to data collection, however, no inter-rater reliability was established. A lack of inter-rater reliability data may result in measurement error if the study is duplicated as it cannot be verified that the clinicians were producing the same measurements. Additionally, both the researchers and patients were not blinded in this case series, which may have led to biasing the outcomes. The researchers also utilized a convenience sample of patients which may limit the applicability of study results to other patient populations.
Finally, an a priori sample size calculation was not conducted, as is typical in case series research. A small sample size can affect power, but the post hoc analysis suggests adequate power (.85-1.0) was achieved given the effect sizes ranged from moderate (.61, .67) to high levels, (1.9, .81) and within pair correlations were high for most variables.36,42,43 The assessment of clinical significance was explored by comparing to the MDC or MCID which is important when analyzing a limited sample size.43,44
CONCLUSIONS
The results of this case series suggest that PRRT™ is useful in decreasing pain and increasing function in patients presenting with symptoms of HS in the short term. Primal Reflex Release Technique™ is used for downregulating dysfunction of the protective response of the ANS by manual reflex stimulation. In this case series the novel treatment used resulted in immediate changes in pain, function, and normalization of SJD. Further research on the effects of PRRT™ on muscle strains and the effects of PRRT™ on pain and function over longer periods of time are warranted.
REFERENCES
- 1.Mendiguchia J Alentorn-Geli E Brughelli M. Hamstring strain injuries: are we heading in the right direction? Br J Sports Med. 2012;46(2):81-85. [DOI] [PubMed] [Google Scholar]
- 2.Davis DS Ashby PE McCale KL Mcquain JA Wine JM. The effectiveness of three stretching techniques on hamstring flexibility using consistent stretching parameters. J Strength Cond Res. 2005;19(1):27-32. [DOI] [PubMed] [Google Scholar]
- 3.DeWeiger VC Gorniak GC Shamus E. The effect of static stretch and warm-up exercise on hamstring length over the course of 24 hours. J Orthop Sports Phys Ther. 2003;33(12):727-732. [DOI] [PubMed] [Google Scholar]
- 4.Kage V Ratnam R. Immediate effect of Active Release Technique versus Mulligan bent leg raise in subjects with hamstring tightness: a randomized clinical trial. Int J Physiother Res. 2014;2(1):301-304. [Google Scholar]
- 5.Kuilart K Woollam M Barling E Lucas N. The active knee extension test and Slump test in subjects with perceived hamstring tightness. Int J Osteopath Med. 2005;8:89-97. [Google Scholar]
- 6.Serner A Tol JT Jomaah H et al. Diagnosis of acute groin injuries: a prospective study of 110 athletes. Am J Sports Med. 2015;43(8):1857-1864. [DOI] [PubMed] [Google Scholar]
- 7.Beijsterveldt AMC Port IGL Vereijken A Backx FJG. Risk factors for hamstring injuries in male soccer players: a systematic review of prospective studies. Scand J Med Sci Sports. 2013;23(3):253-262. [DOI] [PubMed] [Google Scholar]
- 8.Sherry MA & Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3),116-125. [DOI] [PubMed] [Google Scholar]
- 9.Craig TT. Comments in Sports Medicine. Chicago, IL: American Medical Association; 1973.
- 10.Gerhardt MB Romero AA Silvers HJ Harris DJ Watanabe D Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40(3):584–588. [DOI] [PubMed] [Google Scholar]
- 11.Hölmich P Hölmich L Bjerg A. Clinical examination of athletes with groin pain: an intraobserver and interobserver reliability study. Br J Sports Med. 2004;38(4): 46-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nilstad A Andersen TE Bahr R Holme I Steffen K. Risk factors for lower extremity injuries in elite female soccer players. Am J Sports Med. 2014; 42, 940-948. [DOI] [PubMed] [Google Scholar]
- 13.Thorborg K Branci S Nielsen MP Tang L Nielsen MB Hölmich P. Eccentric and isometric hip adduction strength in male soccer players with and without adductor-related groin pain: an assessor-blinded comparison. Orthop J Sports Med. 2014;2(2):2325967114521778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilmore J. Groin pain in the soccer athlete: fact, fiction, and treatment. Clin J Sports Med. 1998;17:787–793. [DOI] [PubMed] [Google Scholar]
- 15.Cibulka MT Rose SJ Delitto A Sinacore DR. Hamstring muscle strain treated by mobilizing the sacroiliac joint. Phys Ther. 1986;66(8):1220-1223. [DOI] [PubMed] [Google Scholar]
- 16.Vleeming A Schuenke M Masi A Careiro J Danneels L Willard F. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liebenson C. Hip dysfunction and back pain. J Bodyw Mov Ther. 2007;11(2):111-115. [Google Scholar]
- 18.Iams J. When reflexes rule: a new paradigm in understanding why some patients don't get well. Adv Phys Ther Rehab Med. 2005;16(3):41. [Google Scholar]
- 19.Kasprowicz DE. Understanding the autonomic nervous system–a missing piece in the treatment of chronic pain. ND. Retrieved from http://www.boernepti.com/media/file/340330/Understanding%20the%20ANS.pdf. Accessed December 7, 2015.
- 20.Bertoti DB. Functional Neurorehabilitation Through the Life Span. Philadelphia, PA: F.A. Davis; 2004. [Google Scholar]
- 21.Hall JE. Guyton and Hall Medical Physiology. Elsevier Health Sciences; 2015. [Google Scholar]
- 22.Arey LB Burrows W Greenhill JP Hewitt RM. Dorland's illustrated medical dictionary. Am J Med Sci. 1957;234(6):733. [Google Scholar]
- 23.Hartman LS. Handbook of osteopathic technique. Springer: 2013. [Google Scholar]
- 24.Iams J. Primal Reflex Release Technique Home Study Course. October 2015.
- 25.Nasypany A. SI & Pelvic Girdle #1 Initial Assessment. https://www.youtube.com/watch?v=H26DmIrAuiQ. Published Oct. 15, 2014. Retrieved Aug 15, 2016.
- 26.Cibulka MT Delitto A Koldehoff RM. Changes in innominate tilt after manipulation of the sacroiliac joint in patients with low back pain. Phys Ther. 1988; 68(9), 1359-1363. [DOI] [PubMed] [Google Scholar]
- 27.Riddle DL Freburger JK. Evaluation of the presence of sacroiliac joint region dysfunction using a combination of tests: a multicenter intertester reliability study. Phys Ther. 2002;82(8):772-781. [PubMed] [Google Scholar]
- 28.Laslett M Aprill CN McDonald B Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207-218. [DOI] [PubMed] [Google Scholar]
- 29.Wainner RS Whitman JM Cleland JA Flynn TW. (2007). Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37(11): 658-660. [DOI] [PubMed] [Google Scholar]
- 30.Nasypany A. Primal Reflex Release Technique: Level 1 Seminar. Presented at University of Idaho; July 2-3, 2016; Moscow ID.
- 31.Farrar JT Pritchett YL Robinson M Prakash A Chappell A. The clinical importance of changes in the 0 to 10 numeric rating scale for worst, least, and average pain intensity: analyses of data from clinical trials of duloxetine in pain disorders. J Pain. 2010;11(2):109–118. [DOI] [PubMed] [Google Scholar]
- 32.Williamson A Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. [DOI] [PubMed] [Google Scholar]
- 33.Sterling M Brentnall D. Patient specific functional scale. Aust J Physiother. 2007;53(1): 65. [DOI] [PubMed] [Google Scholar]
- 34.Stratford P Gill C Westaway M Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiother Can. 1995;47(4): 258-264. [Google Scholar]
- 35.Hurley WL Denegar CR Hertel J. Research Methods: A Framework for Evidence-Based Clinical Practice. Baltimore, MD: Lippincott, Williams, & Wilkins; 2011. [Google Scholar]
- 36.Hansberger BL Baker RT May J Nasypany A. A novel approach to treating plantar fasciitis - effects of primal reflex release technique - a case series. Int J Sports Phys Ther. 2015;10(5):690-699. [PMC free article] [PubMed] [Google Scholar]
- 37.Prentice, William E. Arnheim's Principles of Athletic Training : a Competency-Based Approach. New York, NY: McGraw-Hill, 2003.
- 38.Ekstrand J Healy JC Walden M Lee JC English B Hagglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112-117. [DOI] [PubMed] [Google Scholar]
- 39.Hansen-Honeycutt J Chapman EB Nasypany A Baker RT & May J. A clinical guide to the assessment and treatment of breathing pattern disorders in the physically active: part 2, a case series. Int J Sports Phys Ther. 2016;11(6): 971–979. [PMC free article] [PubMed] [Google Scholar]
- 40.Orchard JW. Lumbar spine region pathology and hamstring and calf injuries in athletes: is there a connection? Br J Sports Med. 2004;38(4):502-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carregaro R. Silva L. & GilCoury HJ. Comparison between two clinical tests for the evaluation of posterior thigh muscles flexibility. Revista Brasileira de Fisioterapia, 11(2):139-145. [Google Scholar]
- 42.Davis DS Quinn RO Whiteman CT Williams JD Young CR. Concurrent validity of four clinical tests used to measure hamstring flexibility. J Strength Cond Res. 2008; 22(2):583-8. [DOI] [PubMed] [Google Scholar]
- 43.de Winter JC. Using the Student's t-test with extremely small sample sizes. Pract Assess Res Eval. 2013;18(10):1-12. [Google Scholar]
- 44.Lachin JM. Introduction to sample size determination and power analysis for clinical trials. Contr Clin Trials. 1981;2(2):93-113. [DOI] [PubMed] [Google Scholar]