Abstract
Rift Valley fever virus (RVFV), a member of the Phlebovirus genus in the Bunyaviridae family, is transmitted by mosquitoes and infects both humans and domestic animals, particularly cattle and sheep. Since primary RVFV strains must be handled in BSL-3+ or BSL-4 facilities, a RVFV cell–cell fusion assay will facilitate the investigation of RVFV glycoprotein function under BSL-2 conditions. As for other members of the Bunyaviridae family, RVFV glycoproteins are targeted to the Golgi, where the virus buds, and are not efficiently delivered to the cell surface. However, overexpression of RVFV glycoproteins using an alphavirus replicon vector resulted in the expression of the glycoproteins on the surface of multiple cell types. Brief treatment of RVFV glycoprotein expressing cells with mildly acidic media (pH 6.2 and below) resulted in rapid and efficient syncytia formation, which we quantified by β-galactosidase α-complementation. Fusion was observed with several cell types, suggesting that the receptor(s) for RVFV is widely expressed or that this acid-dependent virus does not require a specific receptor to mediate cell–cell fusion. Fusion occurred over a broad temperature range, as expected for a virus with both mosquito and mammalian hosts. In contrast to cell fusion mediated by the VSV-G glycoprotein, RVFV glycoprotein-dependent cell fusion could be prevented by treating target cells with trypsin, indicating that one or more proteins (or protein-associated carbohydrate) on the host cell surface are needed to support membrane fusion. The cell–cell fusion assay reported here will make it possible to study the membrane fusion activity of RVFV glycoproteins in a high-throughput format and to screen small molecule inhibitors for the ability to block virus-specific membrane fusion.
Keywords: Fusion, Rift Valley fever virus, Glycoproteins, Entry, Bunyaviridae, Phlebovirus, Alphavirus vector
Introduction
Rift Valley fever virus (RVFV) infects both humans and many domesticated animals, causing acute fevers and, sometimes, retinal or hepatic complications with hemorrhagic symptoms (Flick and Bouloy, 2005). Approximately 1–3% of humans that become infected with RVFV die of the disease, with case fatality proportions significantly higher for infected animals. RVFV, which is spread by infected mosquitoes, was first described in Kenya in 1931 and has since been documented throughout much of Africa. In 2000, RVFV spread to the Arabian peninsula, where it caused the first recorded outbreak outside of the African continent (CDC, 2000a, CDC, 2000b).
RVFV is a member of the genus Phlebovirus in the family Bunyaviridae. Members of the Bunyaviridae family have a single-stranded, tripartite RNA genome of negative polarity. The medium RNA segment (M segment) encodes the viral glycoproteins, GN and GC, and two non-structural proteins, which are translated as a polyprotein precursor (Schmaljohn, 2001). The glycoproteins GN and GC are sufficient for RVFV entry, which is predicted to employ a class II fusion mechanism that is activated by low pH following endocytosis of the virion (Garry and Garry, 2004, Ronka et al., 1995). The receptor(s) or attachment factors for RVFV are unknown, although the virus infects a wide range of cell types.
Study of the RVFV lifecycle is difficult due to the fact that primary virus strains must be handled in BSL-3+/4 containment facilities. The inherent difficulty of studying aspects of RVFV under these conditions can be avoided if assays are developed that allow for investigation of the viral proteins in a BSL-2 setting. For example, a cell–cell fusion assay using only the glycoproteins GN and GC would make it possible to study the structure and function of these proteins under BSL-2 conditions. While fusion assays for members of the Bunyaviridae family have been described, including La Crosse virus in the genus Orthobunyavirus and Hantaan virus in the genus Hantavirus, no fusion assay has been described for viruses in the genus Phlebovirus (Arikawa et al., 1986, Jacoby et al., 1993, Ogino et al., 2004, Plassmeyer et al., 2005, Pobjecky et al., 1986). One of the difficulties in the development of a cell–cell fusion assay for RVFV is that its glycoproteins are targeted to and retained in the Golgi, where the virus buds. When expressed individually, GN is targeted to the Golgi while GC is retained in the endoplasmic reticulum (ER) (Gerrard and Nichol, 2002, Wasmoen et al., 1988). Thus, GN is necessary for the proper Golgi localization of GC during viral assembly.
To study the fusion activity of the RVFV glycoproteins, we overexpressed GN and GC in hopes of saturating the Golgi retention mechanisms that normally prevent efficient transport to the cell surface. While plasmid vectors did not allow for sufficiently high levels of expression to achieve this goal, expression of the glycoproteins from an alphavirus replicon vector led to readily detectable cell surface expression. We found that brief low pH incubation of multiple cell types expressing the RVFV glycoproteins on their surface resulted in cell–cell fusion. Expression of the omega and alpha subunits of β-galactosidase in the effector and target cells, respectively, made it possible to quantify fusion by measuring enzymatic activity of theα-complemented β-galactosidase (Holland et al., 2004). Cell–cell fusion was induced when cells were incubated at pH 6.2 or below, occurred over a broad range of temperatures, and was dependent upon one or more trypsin-sensitive proteins (or protein-associated carbohydrate) on the surface of target cells. The development of a high-throughput cell–cell fusion assay for RVFV will make it possible to study the structure–function relationships of the viral glycoproteins and to identify host cell factors needed to support RVFV entry.
Results
Expression of RVFV glycoproteins on the cell surface
To study the membrane fusion activity of RVFV glycoproteins in the context of a cell–cell fusion assay, they must first be transported from the Golgi to the cell surface. To achieve this, we overexpressed the GN/GC polyprotein from the ZH501 strain of RVFV in HeLa cells either from the eukaryotic expression vector pWRG7077-R4 (Spik et al., 2006) or from VEE or Sindbis-like virus-based replicon vectors (Heise et al., 2003, Thompson et al., 2006) and examined their localization by indirect immunofluorescence microscopy. When the RVFV glycoproteins were expressed from the plasmid vector, they were targeted to the Golgi and were not expressed on the cell surface at levels that could be detected, consistent with other studies (Gerrard and Nichol, 2002, Wasmoen et al., 1988) (Figs. 1A and B ). Since proteins that are retained in the Golgi can sometimes be targeted to the cell surface upon overexpression (Bos et al., 1993, Linstedt et al., 1997), we next examined the localization of the RVFV glycoproteins when expressed from the alphavirus vectors. When compared to expression via pWRG7077, we found that both the VEE and Sindbis virus vectors produced high levels of the RVFV glycoproteins as judged by immunoblot analysis (Fig. 1E and data not shown), though GN and GC were too close in size (55 kDa and 57 kDa, respectively) to clearly resolve. In addition, both GN and GC were detected on the surface of non-permeabilized cells when expressed via the VEE vector (Figs. 1C and D). Similar results were obtained with the Sindbis-like virus replicon, but because the VEE replicon particles (VRP) could be produced to higher titers, these were used in subsequent experiments.
Fig. 1.
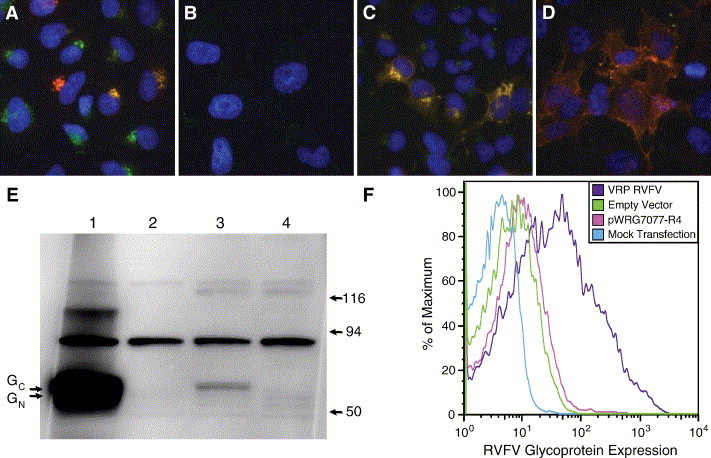
Expression of RVFV glycoproteins from strain ZH501. (A–D) Detection of RVFV GN and GC by indirect immunofluorescence in HeLa cells, stained with anti-RVFV polyclonal HMAF (red), anti-TGN46 (trans-Golgi network marker; green), and the nuclei stained with DAPI (blue). From left to right, pWRG7077-R4 transfected cells: permeabilized (A) and non-permeabilized (B); VRP (VEE Replicon Particle) RVFV infected cells: permeabilized (C) and non-permeabilized (D). (E) Detection of RVFV GN and GC by immunoblot analysis using anti-RVFV polyclonal antibodies. Lane 1 shows RVFV VRP cell lysate, lane 2 shows VRP empty vector lysate, lane 3 shows pWRG7077-R4 transfected cell lysate, and lane 4 shows mock transfected cell lysate. Lysates were from infected or transfected 293T/17 cells. Molecular markers are shown in kDa, arrows indicate position of GN and GC. (F) Surface expression of RVFV GN and GC measured by FACS. 293T/17 cells were transfected with pWRG7077-R4 or infected with VEE RVFV at MOI 5.0 or a control vector as indicated. Cells were stained with anti-RVFV HMAF at 1:100 for 1 h on ice and analyzed on a FACScan 24 h post-infection/transfection. The channel with the highest number of cells for each sample is set to 100; the data are expressed as a percentage of the maximum number of cells.
To quantify the extent to which the RVFV glycoproteins were delivered to the cell surface, 293T/17 cells were transfected with pWRG7077-R4 or infected with VRPs, both expressing strain ZH501 M segment. The next day, the cells were stained with hyperimmune mouse ascitic fluid prepared against RVFV and analyzed by flow cytometry. We found that expression of the RVFV glycoproteins from the pWRG7077-R4 plasmid resulted in low levels of surface expression, while expression via the VRP resulted in much higher levels of surface expression (Fig. 1F). Thus, overexpression of the RVFV glycoproteins by an alphavirus vector results in readily detectable surface expression, perhaps as a result of saturating normal Golgi retention or retrieval mechanisms.
RVFV cell–cell fusion using replicon vectors
Since alphavirus replicon vectors expressed RVFV glycoproteins on the surface of infected cells, they were utilized to develop a cell–cell fusion assay. Members of the Bunyaviridae family, including Phleboviruses, are pH-dependent (Gonzalez-Scarano, 1985, Gonzalez-Scarano et al., 1984, Hacker and Hardy, 1997, Jacoby et al., 1993, Ronka et al., 1995). Therefore, 24 h after infection with VRPs, we briefly incubated cells in a low pH buffer to induce conformational changes in the glycoproteins that might normally occur after endocytosis of the virus. If the glycoproteins undergo the proper conformational changes, the membranes of two adjacent cells may fuse, forming a syncytium. We found that several cell types formed syncytia following expression of the RVFV glycoproteins and brief treatment at pH 5.2, including 293T/17 cells, HeLa cells, FLK cells, Huh-7 and HepG2 liver cells, CHO cells, and Vero cells (Fig. 2 and data not shown). Syncytia formation was not observed when cells were maintained at neutral pH nor was fusion observed when cells infected with a control VRP expressing no glycoproteins (vector 3014) were incubated at either low or neutral pH (Fig. 2). Thus, cell–cell fusion was dependent upon the presence of RVFV glycoproteins at the cell surface as well as upon incubation at mildly acidic pH.
Fig. 2.
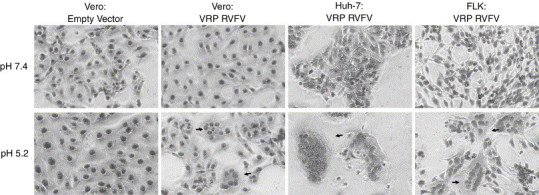
Low pH-triggered syncytia formation of VEE replicon particle infected cells. Vero, Huh-7 (human hepatoma), or FLK (fetal lamb kidney) cells were infected with either an empty VRP (vector 3014; expresses no glycoproteins) or a VRP expressing the RVFV glycoproteins as indicated in the figure. Results with the negative control empty vector are shown only for the Vero cells. After 24 h infection, the cells were treated with buffer at pH 7.4 or pH 5.2 for 1 min then incubated with DMEM 10% FBS for 2 h. The cells were then fixed with methanol, stained with Giemsa, and photographs taken. Arrows indicate syncytia.
β-galactosidase α-complementation quantification of cell–cell fusion
To more rigorously characterize the conditions under which RVFV glycoprotein-mediated fusion occurred, we sought to develop a quantitative cell–cell fusion assay based upon the use of the VEE replicon system and activation of a reporter gene after syncytia formation. However, due to the ability of alphavirus replicons to inhibit host protein synthesis after infection (Kaariainen and Ranki, 1984), multiple approaches that relied upon the expression of a reporter gene subsequent to cell–cell fusion failed. Therefore, we explored the use of the β-galactosidase α-complementation-based fusion assay. In this assay, the alpha subunit of β-galactosidase is expressed in one cell population, while the omega subunit is expressed in another. If fusion between the cell populations occurs after they are mixed, the alpha and omega subunits (produced prior to cell–cell fusion) assemble and functional β-galactosidase is formed, the activity of which can be readily quantified following cell lysis and addition of a chemiluminescent substrate (Holland et al., 2004). By expressing the relatively stable omega subunit in 293T/17 cells 24 h prior to infection with an alphavirus replicon vector, we reasoned that sufficient protein would remain following alphavirus-induced host–cell protein synthesis shut-off such that fusion could still be assayed.
The β-galactosidase α-complementation assay was used to quantify fusion induced by several viral glycoproteins, including those from RVFV, vesicular stomatitis virus (VSV, a pH-dependent virus) (White et al., 1981), and Nipah virus (NiV, a pH-independent virus) (Bossart et al., 2002, Tamin et al., 2002). Target 293T/17 cells were transfected with pCMVα (Holland et al., 2004) expressing the alpha subunit of β-galactosidase, while 293T/17 effector cells were transfected with pCMVω, expressing the omega subunit of β-galactosidase. In addition, effector cells were cotransfected with plasmids expressing either the VSV or NiV glycoproteins. Alternatively, effector cells were infected with VRPs expressing the RVFV glycoproteins or a vector that did not express any glycoprotein 24 h after transfection of the cells with the pCMVω plasmid. The effector and target cells were mixed 48 h after transfection, allowed to interact for 45–60 min, and then incubated for 10 min at the indicated pH (Fig. 3 ). Two and one-half hours later, the cells were lysed and β-galactosidase activity measured.
Fig. 3.
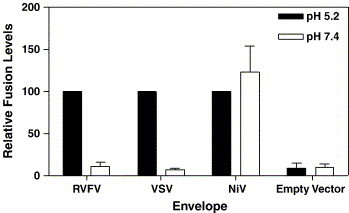
β-galactosidase α-complementation quantification of cell–cell fusion. 293T/17 target cells transfected with pCMVα were mixed with 293T/17 effector cells transfected with pCMVω and either transfected with VSV-G or NiV glycoprotein constructs or infected with VRPs expressing the RVFV glycoproteins or no glycoproteins (empty vector). The cells were treated with buffer at pH 5.2 or 7.4 for 10 min. Cells were then incubated 2.5 h with media at 37 °C, after which the cells were lysed and β-galactosidase activity measured. Each experiment was completed in triplicate; each envelope was normalized to 100% at pH 5.2, with VRP empty vector normalized to RVFV fusion at pH 5.2. Bars indicate standard error of the mean.
We found that cells expressing the RVFV glycoproteins fused at pH 5.2, with relative light units (RLU) of 60–100 typically being measured. In contrast, only background levels (typically < 10 light units) of β-galactosidase activity were measured at pH 7.4. As expected, cells expressing the VSV-G glycoprotein fused efficiently at acid pH (typically 100–150 RLU), while cells expressing the NiV glycoproteins fused at both pH 7.4 and pH 5.2 (typically 350–500 RLU). Significant levels of β-galactosidase activity were not obtained when cells infected with a VRP that did not express a viral glycoprotein were used. We optimized the conditions needed for RVFV glycoprotein-mediated membrane fusion by varying the length of low-pH treatment and the length of time allowed for syncytia formation/α-complementation. We determined that RVFV fusion was optimal with low pH treatment incubation for 6–10 min and that syncytia formation was easily quantifiable 2.5 h after acid treatment (data not shown).
pH and temperature dependence of RVFV glycoprotein-mediated membrane fusion
To determine the pH threshold at which the RVFV glycoproteins mediate membrane fusion, we used the β-galactosidase complementation assay, incubating cells at pH values ranging from pH 5.0 to pH 7.4 for 10 min, prior to a 2.5-hour incubation at neutral pH. The RVFV glycoproteins began to induce cell–cell fusion at pH 6.2, with near maximal fusion being attained at pH 5.0 (Fig. 4A). Fusion activity often decreased below pH 5.0 (data not shown), perhaps due to cytotoxic effects. An empty VRP did not induce fusion at any pH value (Fig. 4A). Each experiment was completed in triplicate, and all of the values were normalized to RVFV induced fusion at pH 5.0. VSV-G was used as a positive control and induced fusion at pH values of less than 6.4, consistent with published results (White et al., 1981) (data not shown).
Fig. 4.
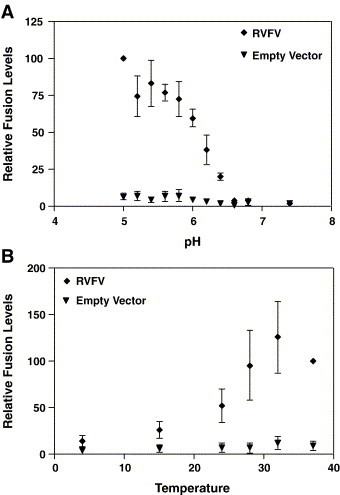
pH and temperature dependence of RVFV glycoprotein induced cell–cell fusion. 293T/17 target cells transfected with pCMVα were mixed with 293T/17 effector cells transfected with pCMVω and infected with either an empty VRP vector or the VRP vector expressing the RVFV glycoproteins. In panel A, the cells were treated with buffer at the specified pH for 10 min. The cells were then incubated 2.5 h with media at 37 °C at pH 7.4, after which β-galactosidase activity was measured. In panel B, the temperature dependence of cell–cell fusion was determined by mixing the effector and target cells for 1 h at 37 °C, then incubating them at the indicated temperature for an additional 10 min. The cells were incubated at pH 5.2 for 10 min at the indicated temperature then returned to pH 7.4 for 10 min, again at the indicated temperature. Cells were then incubated at 37 °C for 2.5 h after which β-galactosidase activity was measured. Each experiment was completed in triplicate; the fusion level was normalized to RVFV fusion at pH 5.0. Bars indicate standard error of the mean.
Since RVFV infects both mammals and mosquitoes, the glycoproteins should induce cell–cell fusion over a range of temperatures. To examine this, the β-galactosidase α-complementation fusion assay was used to quantify fusion at different temperatures, from 4 °C to 37 °C (Fig. 4B). Cells were mixed together at 37 °C for 1 h, and then incubated at the indicated temperature for 10 min. The pH was then adjusted to pH 5.2 at the specified temperature for 10 min, the media was neutralized, and the cells returned to 37 °C 10 min later to ensure that the efficiency of α-complementation at different temperatures was not a consideration for interpretation of the fusion results. We found that RVFV glycoproteins induced cell–cell fusion from room temperature (24 °C) up to 37 °C, with increased fusion at 28 °C, 32 °C and 37 °C. When the experiment was performed at 42 °C, no quantifiable cell–cell fusion was observed (data not shown). The data indicate that RVFV fused at lower temperatures, although the glycoproteins functioned optimally at temperatures from 28 to 37 °C.
RVFV receptor characterization: trypsin inhibition
Although the receptor and/or attachment factors are not known for RVFV, the cell–cell fusion assay can be used to begin to understand the interactions between the glycoproteins and the cellular receptor(s) for RVFV. To this end, target cells were treated with trypsin, at 7 μg/μl or 15 μg/μl, to cleave proteins from the target cell surface. RVFV glycoprotein-induced cell–cell fusion was inhibited by trypsin treatment of the target cells, indicating that the receptor(s) for RVFV is typsin-sensitive (Fig. 5 ). NiV was used as a positive control since ephrin-B2, the receptor for NiV (Bonaparte et al., 2005, Negrete et al., 2005), is a trypsin-sensitive protein (Bossart et al., 2001, Eaton et al., 2004). As seen in Fig. 5, NiV glycoprotein-induced cell–cell fusion was inhibited at both pH 5.2 and pH 7.4 by trypsin treatment of the target cells. This effect was not the product of nonspecific toxicity of the trypsin treatment because VSV-G-induced cell–cell fusion was not affected, which agrees with previously published reports that the VSV cellular receptor is not protease sensitive (Schlegel et al., 1983) (Fig. 5). Thus, one or more proteins (or protein-associated carbohydrate) on the surface of target cells are needed for RVFV glycoprotein-mediated membrane fusion to occur.
Fig. 5.
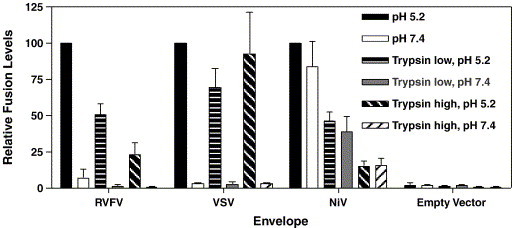
RVFV dependent cell–cell fusion is sensitive to trypsin treatment of the target cells. 293T/17 target cells transfected with pCMVα were treated with trypsin for 15 min at 7 μg/μl (low) or 15 μg/μl (high) to cleave surface proteins. After inhibiting the trypsin with soybean trypsin inhibitor, the target cells were mixed with 293T/17 effector cells transfected with pCMVω and either transfected with VSV-G or NiV glycoprotein constructs or infected with VRP vectors expressing the RVFV glycoproteins or no glycoproteins (empty vector). The cells were treated with buffer at pH 5.2 or 7.4 for 10 min. Cells were then incubated 2.5 h with media at 37 °C pH 7.4, after which β-galactosidase activity was measured. Each experiment was completed in triplicate; each envelope was normalized to 100% at pH 5.2, with VRP empty vector normalized to RVFV fusion at pH 5.2. Bars indicate standard error of the mean.
Discussion
Relatively little is known about the structure and function of RVFV glycoproteins. While it is evident that GN and GC must attach the virus to the cell surface and mediate membrane fusion, little is known about their oligomeric structures, the roles that GN and GC play in virus entry, or the mechanisms by which antibodies neutralize RVFV. Likewise, the host cell factors needed for RVFV entry are largely uncharacterized, though the broad species and cell tropism of RVFV suggests that it either interacts with a highly conserved receptor or can bind to a variety of receptors or attachment factors.
The greatest stumbling block in developing a cell–cell fusion assay for RVFV is that its glycoproteins, like those of other Bunyaviridae members, are targeted to and retained in the Golgi apparatus, where the virus buds (Gerrard and Nichol, 2002, Kuismanen, 1984, Kuismanen et al., 1984, Schmaljohn, 2001, Shi et al., 2004, Wasmoen et al., 1988). For a cell–cell fusion assay to be developed, either the viral glycoproteins need to be expressed on the cell surface or large amounts of virus need to be added to the outside of cells to induce fusion-from-without. Since we sought to develop an assay that would enable us to manipulate the viral glycoproteins to test structural and functional hypotheses, we investigated approaches that would result in delivery of RVFV GN and GC to the cell surface. Gerrard and Nichol have shown that, when coexpressed, both GN and GC are delivered to the Golgi by virtue of a targeting signal present within the transmembrane and cytoplasmic domains of GN. Interestingly, some GN reached the cell surface under their conditions, raising the possibility that the RVFV glycoproteins are localized to the Golgi at least in part by a retrieval mechanism from the cell surface (Gerrard and Nichol, 2002). If so, then overexpression of the glycoproteins could alter the steady state distribution of GN and GC such that sufficient levels are attained on the plasma membrane for the induction of cell–cell fusion. Indeed, the distribution of several cellular proteins that reside in the Golgi can be altered upon overexpression, resulting in enhanced delivery to the cell surface (Bos et al., 1993, Linstedt et al., 1997).
Expression of the RVFV GN and GC polyprotein from an alphavirus vector resulted in readily detectable surface expression of these molecules. The alphavirus replicon technology can be used to express a variety of proteins, including other viral glycoproteins that are not naturally targeted to the cell surface and are therefore difficult to manipulate in cell–cell fusion or pseudovirion assays (Heise et al., 2003, Thompson et al., 2006). Cells expressing the RVFV glycoproteins on the cell surface formed syncytia when incubated at mildly acidic pH, suggesting that this virus utilizes one or more endocytic pathways for cellular infection, with endosomal pH playing a critical role in inducing the fusion reaction. Other members of the Bunyaviridae family for which acid pH dependence has been shown include La Crosse, Hantaan, and California encephalitis viruses (Gonzalez-Scarano, 1985, Gonzalez-Scarano et al., 1984, Hacker and Hardy, 1997, Jacoby et al., 1993, Ronka et al., 1995). Thus, the fact that RVFV glycoproteins induced cell–cell fusion at low pH is not surprising. However, it remains to be determined if RVFV needs other cellular factors in addition to low pH for membrane fusion to occur. For example, the SARS coronavirus (Simmons et al., 2005) and Ebola virus (Chandran et al., 2005) envelope proteins require a low-pH dependent endoproteolytic cleavage event in order for fusion to be elicited, while the ASLV envelope protein must first bind to its specific receptor, which triggers conformational changes in the envelope protein that render it competent to elicit membrane fusion upon subsequent exposure to low pH (Mothes et al., 2000). Since cell surface RVFV glycoproteins were capable of eliciting efficient cell–cell fusion, it is less likely that proteolytic activation of either GN or GC is a required triggering event, though this possibility cannot be ruled out. Whether binding to a specific receptor might be needed prior to acid treatment is also not known and cannot be addressed at present since the receptor(s) for RVFV is unknown.
RVFV glycoprotein-induced fusion occurred over a broad temperature range, as might be expected for a virus that replicates in both mammalian and insect hosts. This correlates with data from fusion-from-without assays using La Crosse virus, which induces syncytia formation at temperatures above 25 °C (Pobjecky et al., 1986). Furthermore, the growth of many members of the Bunyaviridae family, including Tahyna virus (Danielova, 1975), is decreased at incubation at lower temperatures in cell culture. Experiments examining the susceptibility of Culex pipiens and Aedes fowleri mosquitoes to RVFV determined that adult mosquitoes held at lower temperatures (13–19 °C) were less susceptible to RVFV infections, which correlates with our data indicating less RVFV-induced fusion at lower temperatures (Brubaker and Turell, 1998, Turell, 1989, Turell et al., 1985); however, there is no evidence that fusion efficiency is the only factor in mosquito susceptibility to RVFV infection.
Inhibition of RVFV induced cell–cell fusion was attempted using neutralizing anti-RVFV sera; however, the antibodies were unable to block cell–cell fusion. Several reports have shown that some neutralizing anti-RVFV antibodies do not block virus binding to the cell (Besselaar and Blackburn, 1992, Besselaar and Blackburn, 1994), a phenomenon also seen with Dugbe virus, a member of the Nairovirus genus (Green et al., 1992). In the context of a cell–cell fusion assay, the presence of antibodies may not completely block the proximity of the overexpressed RVFV glycoproteins to the target cell membrane. Therefore, when the pH is lowered, conformational changes triggered in the glycoproteins may still induce cell–cell fusion even when antibodies are present. Furthermore, a large amount of antibody was necessary for inhibition of the Hantaan virus cell–cell fusion assay (Ogino et al., 2004), indicating inefficient inhibition of cell–cell fusion. This phenomenon has also been seen for other virus families; for example, higher concentrations of entry inhibitors are necessary to block HIV cell–cell fusion when compared to inhibition of infection (Reeves et al., 2005).
Because RVFV infects many cell types, with no known cell refractory to RVFV infection, it is likely that the receptor for RVFV is widespread or that there is no single receptor needed for virus infection. As noted previously, some acid-dependent viruses require specific receptors, whereas others can elicit fusion with artificial membranes at low pH, thus demonstrating that the presence of host cell proteins is not required (Corver et al., 2000, White and Helenius, 1980). To further explore the target cell requirements for RVFV glycoprotein-mediated fusion, we treated target cells with trypsin and found that this largely abolished RVFV-dependent membrane fusion, though it did not affect fusion elicited by VSV-G. This indicates that a host cell surface protein or protein-associated carbohydrate is necessary for RVFV cell–cell fusion, and perhaps for virus infection as well. Currently, we are in the process of analyzing a more extensive panel of proteases for their effects on RVFV fusion.
The fusion mechanism for members of the Bunyaviridae family is not known, though modeling studies suggest that these viruses employ a class II fusion mechanism, similar to members of the Alphaviridae and Flaviviridae families (Garry and Garry, 2004, Tischler et al., 2005). While there is no specific experimental evidence for this, the pH dependence of the virus and the necessity for both GN and GC for fusion are consistent with a class II fusion mechanism. The fusion assay described here will allow further investigation of the structural elements of GC necessary to induce cell–cell fusion. The development of this quantitative cell–cell fusion assay will make it possible to more fully explore the conditions needed for RVFV-induced membrane fusion, to study the structure–function relationships of the viral glycoproteins, and to screen for small molecules that block RVFV entry or fusion that could be used as antiviral drugs.
Materials and methods
Cell lines
Vero E6 (African green monkey kidney fibroblast (CV-1)), HeLa (human, cervix carcinoma), U87 (human, glioblastoma–astrocytoma), FLK (fetal lamb kidney), CHO (Chinese hamster ovary), MDBK (Madin-Darby bovine kidney), PK13 (porcine fibroblasts), BHK (baby hamster kidney), and 293T/17 (human embryonic kidney) cells were maintained in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) (Invitrogen, Carlsbad, CA).
Plasmids and replicons
Venezuelan equine encephalitis (VEE) replicon particles (VRP) with 3014 coat proteins and Girdwood (Sindbis-like) replicon particle stocks expressing RVFV M segment, strain ZH501, or empty VRP (3014 coat) were produced as previously described (Heise et al., 2003, Thompson et al., 2006). Briefly, full-length transcripts were derived from linearized plasmids containing viral cDNA templates by using SP6- or T7-specific mMessage Machine in vitro transcription kits (Ambion, Austin, TX). Transcripts were electroporated into BHK-21 cells grown in minimal essential medium (MEM; 10% fetal calf serum [Gibco, Carlsbad, CA], 10% tryptose phosphate broth [Sigma, Saint Louis, MO], and 0.29 mg of l-glutamine per ml [Invitrogen, Carlsbad, CA]). Supernatants were harvested at 24–27 h post-electroporation, and 10% of the supernatant was screened for the presence of replication competent virus using a previously described cytopathic effect (CPE) assay (Heise et al., 2003, Thompson et al., 2006). Supernatants that passed CPE testing were considered safe for use under BSL-2 conditions and were concentrated by pelleting through a 20% sucrose cushion, resuspended in PBS, pH 7.4, frozen in 0.1-ml aliquots, and replicon particles titrated on BHK-21 cells as previously described (Heise et al., 2003, Thompson et al., 2006).
The RVFV plasmid pWRG7077-R4, a kind gift from Dr. Connie Schmaljohn at United States Army Medical Research Institute for Infectious Diseases (USAMRIID), expresses the RVFV M segment from strain ZH501 beginning at the fourth in-frame start codon. Therefore, it expresses GN and GC but does not encode the entire non-structural M segment proteins (Spik et al., 2006). The codon-optimized NiV-F (pcNiV-Fopt, accession no. AY816748) and NiV-G (pcNiV-Gopt, accession no. AY816746), a kind gift from Dr. Benhur Lee at the University of California, Los Angeles, were synthesized chemically and subcloned into the pcDNA3.1 mammalian expression vector (Levroney et al., 2005).
Expression of RVFV glycoproteins
To analyze the expression of RVFV glycoproteins in cells infected with the alphavirus replicons, we performed immunoblots as previously described (Bertolotti-Ciarlet et al., 2005). Briefly, 293T/17 cells were infected with VEE replicons expressing the RVFV glycoproteins at a multiplicity of infection (MOI) of 5 or transfected with pWRG7077-R4 using Lipofectamine 2000 following manufacturer's instructions (Invitrogen Corporation, Carlsbad, CA). At 24 h post-infection or transfection, cell extracts were prepared in 50 mM Tris–HCl, pH 7.4, 5 mM EDTA, 1% Triton X-100, and Complete protease inhibitor cocktail (Roche Applied Sciences, Indianapolis, IN). Cell lysates were incubated at 4 °C for 10 min and then centrifuged at 10,000×g for 10 min. The supernatant was mixed with sample buffer (0.08 M Tris–HCl, pH 6.8, 2% SDS, 10% glycerol, 5% β-mercaptoethanol, 0.005% bromophenol blue) and incubated at 95 °C for 3 min before electrophoresis in Criterion 4–15% Tris–HCl sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) (Bio-Rad, Hercules, CA). Immunoblot analysis was performed using rabbit polyclonal antibodies raised against RVFV peptides in both GN at residue 374 (CFEHKGQYKGTMDSGQTKRE) and GC at residue 976 (CFERGSLPQTRNDKTFAASK) (ProSci, Poway, CA), and goat anti-rabbit horseradish peroxidase-conjugated secondary antibody (Amersham Pharmacia, Buckinghamshire, UK) followed by visualization with SuperSignal West Femto Maximum Sensitivity Substrate (Pierce Biotechnology, Inc., Rockford, IL).
Localization and surface expression of RVFV glycoproteins
To visualize RVFV proteins on cells transfected with the RVFV M segment, HeLa cells grown on 12 mm glass coverslips (Fisher Scientific, Pittsburgh, PA) in 24 well plates were transfected using Lipofectamine 2000 (Invitrogen Corporation, Carlsbad, CA) following the manufacturer's instructions. Twenty-four hours post-transfection, the cells were fixed using 2% formaldehyde for 10 min at room temperature. Cells were permeabilized with 0.5% TX-100 for 10 min. To prevent nonspecific antibody binding, cells were then incubated with phosphate buffered saline (PBS) containing 4% FBS for 30 min. The cells were incubated with hyperimmune mouse ascitic fluid (HMAF) against RVFV (generous gift from Dr. Mike Parker at USAMRIID) and sheep anti-TGN46 (Serotec Inc., Raleigh, NC) Golgi antibody diluted 1:250 in PBS 4% FBS for 1 h. A 1:500 dilution of an anti-mouse Alexa-594 secondary antibody (Invitrogen Corporation, Carlsbad, CA) was used to detect the RVFV antibody, goat anti-sheep Alexa-488 secondary antibody (Invitrogen Corporation, Carlsbad, CA) was used to detect the Golgi, and the nuclei were stained with DAPI (4′,6-Diamidino-2-phenylindole) at a 1:1000 dilution. The coverslips were mounted onto slides using Fluoromount-G (SouthernBiotech, Birmingham, AL).
To analyze cellular expression of RVFV glycoproteins expressed from alphavirus replicons by indirect immunofluorescence, HeLa cells grown on 12 mm coverslips in a 24 well plate were infected with a VEE replicon particle (VRP) expressing RVFV glycoproteins (Collett et al., 1985) or an empty VRP. The replicons were diluted to an MOI of 5 in 200 μl PBS 1% FBS. After 1 h, 250 μl DMEM 10% FBS was added to each well, and the cells were incubated for 24 h at 37 °C. Cells were fixed and stained as described for transfected cells. Immunofluorescent images were taken on a Nikon E600 microscope at 60× magnification utilizing UV illumination.
To analyze surface expression of RVFV glycoproteins by flow cytometry, 293T/17 cells were transfected with pWRG7077-R4 RVFV M segment ZH501 using Lipofectamine 2000 or infected with the VRP expressing RVFV M segment ZH501 at a MOI of 5 for 24 h. Cells were then surface stained with anti-RVFV mouse HMAF for 1 h on ice then stained with anti-mouse secondary antibody conjugated to phycoerythrin (PE) for 30 min on ice. The cells were analyzed on a FACScan (Becton Dickinson, Franklin Lakes, NJ) and evaluated using FlowJo software (TreeStar, Inc., Ashland, OR).
RVFV syncytia formation fusion assay
Cells infected with Girdwood (Sindbis-like) or VEE alphavirus replicon particles encoding RVFV M segment strain ZH501, as described above, were treated with 100 μl Earle's salt solution 20 mM HEPES (4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid) and 20 mM MES (2-Morpholinoethanesulfonic acid) at the specified pH for 1 to 10 min at 37 °C 24 h post-infection. 500 μl DMEM 10% FBS was then added, and the cells were incubated for 1–2 h at 37 °C. Cells were then fixed with methanol on ice for 5–7 min and allowed to dry before treatment for 15 min with Giemsa stain (Sigma, Saint Louis, MO) diluted 1:10 in water at room temperature. Images were captured using a Nikon Eclipse TE300 microscope at 40× magnification.
RVFV β-galactosidase α-complementation quantification
To quantify the fusion activity of RVFV glycoproteins, we used the β-galactosidase fusion assay as described by Holland et al. using 293T/17 cells. β-galactosidase α-complementation is based on the fact that the β-galactosidase enzyme is a dimer; the dimerization domain (the alpha subunit) can be separated from the rest of the protein (the omega subunit). Target cells were transfected with pCMVα (Holland et al., 2004) expressing the alpha subunit of β-galactosidase, while the effector cells were transfected with pCMVω, expressing the omega subunit of β-galactosidase. As a positive control for pH-dependent fusion, vesicular stomatitis virus glycoprotein (VSV-G) expressing cells were used; 7 μg pBlueScript-VSV-G was cotransfected with 7 μg pCMVω into effector cells. As a positive control for pH-independent fusion, Nipah virus (NiV) codon optimized F and G protein expressing cells were used; 3.5 μg pcDNA3.1 NiV F, 3.5 μg pcDNA3.1 NiV G, and 7 μg pCMVω were cotransfected into effector cells. For RVFV glycoprotein expressing cells, 293T/17 cells were transfected with 7 μg pCMVω using Lipofectamine 2000. Twenty-four hours post-transfection, the pCMVω transfected cells were infected with VRPs expressing RVFV glycoproteins from the ZH501 M segment or with empty 3014 VRP, as described above. Twenty-four hours post-transfection, all cells were treated with 500 mM sodium butyrate to boost expression of proteins from the pCMV vectors.
Forty-eight hours post-transfection, the cells were resuspended in DMEM, and 2.5 × 105 cells of targets and effectors were combined (Holland et al., 2004). The mixed cells were incubated for 30 to 60 min to allow for effector and target cell binding. Then, cells were gently spun down at 800–900 rpm for 2 min, the supernatant removed and the cells treated with 100 μl of Earle's salt solution with 20 mM HEPES and 20 mM MES from pH 5.0 to 7.4 for 5–10 min at 37 °C to induce pH-dependent conformational changes in glycoproteins and allow for cell–cell fusion. The pH was neutralized by adding 500 μl DMEM 10% FBS with 10 mM HEPES, and the cells then incubated at 37 °C for 2.5 to 4 h to allow for syncytia formation and α-complementation. To monitor the extent of fusion, the cells were spun down, lysed using Galacto-Star lysis buffer, and read following the Galacto-Star directions (Applied Biosystems, Foster City, CA). Each experiment was completed in triplicate. At least three individual experiments were normalized to 100% at low pH, and then the normalized values were averaged together.
Temperature dependence of RVFV-mediated membrane fusion
To analyze the effect of different temperatures on the fusion activity of RVFV glycoproteins, the fusion assay described above was utilized with several modifications. The pCMVα transfected target cells and RVFV glycoprotein expressing effector cells were combined at 37 °C and incubated for 1 h to allow for cell–cell binding. The cells were pelleted at 800–900 rpm for 2 min, and the supernatant aspirated. Then, 100 μl of buffer at the desired pH and specified temperature, from 4 °C to 37 °C, was added for 10 min. As described above, DMEM 10% FBS with 10 mM HEPES was added to normalize the pH and the cells were incubated at the specified temperatures for an additional 10 min. The cells were then incubated at 37 °C for 2.5 h to enable β-galactosidase complementation to occur under identical conditions regardless of the temperature at which the cells were incubated at acid pH.
Fusion inhibition by trypsin
To analyze the effect of trypsin treatment on RVFV glycoprotein fusion activity, pCMVα transfected target cells were suspended in DMEM then treated with 7 or 15 μg/μl of trypsin (l-1-tosylamido-2-phenylethyl chloromethyl ketone) (Sigma, St. Louis, MO) for 15 min at 37 °C. Soybean trypsin inhibitor (50 μg/μl; Sigma, St. Louis, MO) was then added and incubated for 30 min at 37 °C to inactivate the trypsin, preventing cleavage of proteins on the effector cells. The targets and effectors were then combined for 45 min, and the fusion assay completed and results analyzed as described above.
Acknowledgments
We would like to thank Benhur Lee (UCLA) for supplying the codon optimized NiV plasmids, Connie Schmaljohn (USAMRIID) for supplying the RVFV M segment plasmids, Mike Parker (USAMRIID) for the anti-RVFV HMAF, Martha Collier, Nancy Davis, and Robert Johnston (UNC-CH) for packaging the VEE replicon particles, Kenya Madric (UNC-CH) for packaging the Sindbis-like replicon particles, and Nathaniel Landau (The Salk Institute for Biological Studies) for the β-galactosidase α-complementation plasmids.
This work was supported by NIH grants from the Middle Atlantic Regional Center for Excellence in Biodefense and Emerging Infectious Diseases (U54 AI 057168), T32 AI 055400, and by a Developmental Award from the Southeastern Regional Center for Excellence in Biodefense and Emerging infectious diseases (SERCEB; U54 AI057157) to MTH.
Contributor Information
Robert W. Doms, Email: doms@mail.med.upenn.edu.
Andrea Bertolotti-Ciarlet, Email: aciarlet@mail.med.upenn.edu.
References
- Arikawa J., Takashima I., Hashimoto N., Takahashi K., Yagi K., Hattori K. Epidemiological studies of hemorrhagic fever with renal syndrome (HFRS) related virus infection among urban rats in Hokkaido, Japan. Arch. Virol. 1986;88(3–4):231–240. doi: 10.1007/BF01310877. [DOI] [PubMed] [Google Scholar]
- Bertolotti-Ciarlet A., Smith J., Strecker K., Paragas J., Altamura L.A., McFalls J.M., Frias-Staheli N., Garcia-Sastre A., Schmaljohn C.S., Doms R.W. Cellular localization and antigenic characterization of crimean-congo hemorrhagic fever virus glycoproteins. J. Virol. 2005;79(10):6152–6161. doi: 10.1128/JVI.79.10.6152-6161.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besselaar T.G., Blackburn N.K. The synergistic neutralization of Rift Valley fever virus by monoclonal antibodies to the envelope glycoproteins. Arch. Virol. 1992;125(1–4):239–250. doi: 10.1007/BF01309641. [DOI] [PubMed] [Google Scholar]
- Besselaar T.G., Blackburn N.K. The effect of neutralizing monoclonal antibodies on early events in Rift Valley fever virus infectivity. Res. Virol. 1994;145(1):13–19. doi: 10.1016/s0923-2516(07)80002-1. [DOI] [PubMed] [Google Scholar]
- Bonaparte M.I., Dimitrov A.S., Bossart K.N., Crameri G., Mungall B.A., Bishop K.A., Choudhry V., Dimitrov D.S., Wang L.F., Eaton B.T., Broder C.C. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc. Natl. Acad. Sci. U.S.A. 2005;102(30):10652–10657. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos K., Wraight C., Stanley K.K. TGN38 is maintained in the trans-Golgi network by a tyrosine-containing motif in the cytoplasmic domain. EMBO J. 1993;12(5):2219–2228. doi: 10.1002/j.1460-2075.1993.tb05870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossart K.N., Wang L.F., Eaton B.T., Broder C.C. Functional expression and membrane fusion tropism of the envelope glycoproteins of Hendra virus. Virology. 2001;290(1):121–135. doi: 10.1006/viro.2001.1158. [DOI] [PubMed] [Google Scholar]
- Bossart K.N., Wang L.F., Flora M.N., Chua K.B., Lam S.K., Eaton B.T., Broder C.C. Membrane fusion tropism and heterotypic functional activities of the Nipah virus and Hendra virus envelope glycoproteins. J. Virol. 2002;76(22):11186–11198. doi: 10.1128/JVI.76.22.11186-11198.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker J.F., Turell M.J. Effect of environmental temperature on the susceptibility of Culex pipiens (Diptera: Culicidae) to Rift Valley fever virus. J. Med. Entomol. 1998;35(6):918–921. doi: 10.1093/jmedent/35.6.918. [DOI] [PubMed] [Google Scholar]
- CDC Outbreak of Rift Valley Fever—Saudi Arabia, August–November 2000. Morb. Mort. Wkly. Rep. 2000;49:905–908. [PubMed] [Google Scholar]
- CDC Outbreak of Rift Valley Fever—Yemen, August–October 2000. Morb. Mort. Wkly Rep. 2000;49:1065–1066. [PubMed] [Google Scholar]
- Chandran K., Sullivan N.J., Felbor U., Whelan S.P., Cunningham J.M. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308(5728):1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collett M.S., Purchio A.F., Keegan K., Frazier S., Hays W., Anderson D.K., Parker M.D., Schmaljohn C., Schmidt J., Dalrymple J.M. Complete nucleotide sequence of the M RNA segment of Rift Valley fever virus. Virology. 1985;144(1):228–245. doi: 10.1016/0042-6822(85)90320-4. [DOI] [PubMed] [Google Scholar]
- Corver J., Ortiz A., Allison S.L., Schalich J., Heinz F.X., Wilschut J. Membrane fusion activity of tick-borne encephalitis virus and recombinant subviral particles in a liposomal model system. Virology. 2000;269(1):37–46. doi: 10.1006/viro.1999.0172. [DOI] [PubMed] [Google Scholar]
- Danielova V. Growth of Tahyna virus at low temperatures. Acta Virol. 1975;19(4):327–332. [PubMed] [Google Scholar]
- Eaton B.T., Wright P.J., Wang L.F., Sergeyev O., Michalski W.P., Bossart K.N., Broder C.C. Henipaviruses: recent observations on regulation of transcription and the nature of the cell receptor. Arch. Virol., Suppl. 2004;(18):122–131. [PubMed] [Google Scholar]
- Flick R., Bouloy M. Rift Valley fever virus. Curr. Mol. Med. 2005;5(8):827–834. doi: 10.2174/156652405774962263. [DOI] [PubMed] [Google Scholar]
- Garry C.E., Garry R.F. Proteomics computational analyses suggest that the carboxyl terminal glycoproteins of Bunyaviruses are class II viral fusion protein (beta-penetrenes) Theor. Biol. Med. Model. 2004;1(1):10. doi: 10.1186/1742-4682-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrard S.R., Nichol S.T. Characterization of the Golgi retention motif of Rift Valley fever virus G(N) glycoprotein. J. Virol. 2002;76(23):12200–12210. doi: 10.1128/JVI.76.23.12200-12210.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Scarano F. La Crosse virus G1 glycoprotein undergoes a conformational change at the pH of fusion. Virology. 1985;140(2):209–216. doi: 10.1016/0042-6822(85)90359-9. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Scarano F., Pobjecky N., Nathanson N. La Crosse bunyavirus can mediate pH-dependent fusion from without. Virology. 1984;132(1):222–225. doi: 10.1016/0042-6822(84)90107-7. [DOI] [PubMed] [Google Scholar]
- Green E.M., Armstrong S.J., Dimmock N.J. Mechanisms of neutralization of a nairovirus (Dugbe virus) by polyclonal IgG and IgM. J. Gen. Virol. 1992;73(Pt 8):1995–2001. doi: 10.1099/0022-1317-73-8-1995. [DOI] [PubMed] [Google Scholar]
- Hacker J.K., Hardy J.L. Adsorptive endocytosis of California encephalitis virus into mosquito and mammalian cells: a role for G1. Virology. 1997;235(1):40–47. doi: 10.1006/viro.1997.8675. [DOI] [PubMed] [Google Scholar]
- Heise M.T., White L.J., Simpson D.A., Leonard C., Bernard K.A., Meeker R.B., Johnston R.E. An attenuating mutation in nsP1 of the Sindbis-group virus S.A.AR86 accelerates nonstructural protein processing and up-regulates viral 26S RNA synthesis. J. Virol. 2003;77(2):1149–1156. doi: 10.1128/JVI.77.2.1149-1156.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland A.U., Munk C., Lucero G.R., Nguyen L.D., Landau N.R. Alpha-complementation assay for HIV envelope glycoprotein-mediated fusion. Virology. 2004;319(2):343–352. doi: 10.1016/j.virol.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Jacoby D.R., Cooke C., Prabakaran I., Boland J., Nathanson N., Gonzalez-Scarano F. Expression of the La Crosse M segment proteins in a recombinant vaccinia expression system mediates pH-dependent cellular fusion. Virology. 1993;193(2):993–996. doi: 10.1006/viro.1993.1213. [DOI] [PubMed] [Google Scholar]
- Kaariainen L., Ranki M. Inhibition of cell functions by RNA–virus infections. Annu. Rev. Microbiol. 1984;38:91–109. doi: 10.1146/annurev.mi.38.100184.000515. [DOI] [PubMed] [Google Scholar]
- Kuismanen E. Posttranslational processing of Uukuniemi virus glycoproteins G1 and G2. J. Virol. 1984;51(3):806–812. doi: 10.1128/jvi.51.3.806-812.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuismanen E., Bang B., Hurme M., Pettersson R.F. Uukuniemi virus maturation: immunofluorescence microscopy with monoclonal glycoprotein-specific antibodies. J. Virol. 1984;51(1):137–146. doi: 10.1128/jvi.51.1.137-146.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levroney E.L., Aguilar H.C., Fulcher J.A., Kohatsu L., Pace K.E., Pang M., Gurney K.B., Baum L.G., Lee B. Novel innate immune functions for galectin-1: galectin-1 inhibits cell fusion by Nipah virus envelope glycoproteins and augments dendritic cell secretion of proinflammatory cytokines. J. Immunol. 2005;175(1):413–420. doi: 10.4049/jimmunol.175.1.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linstedt A.D., Mehta A., Suhan J., Reggio H., Hauri H.P. Sequence and overexpression of GPP130/GIMPc: evidence for saturable pH-sensitive targeting of a type II early Golgi membrane protein. Mol. Biol. Cell. 1997;8(6):1073–1087. doi: 10.1091/mbc.8.6.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mothes W., Boerger A.L., Narayan S., Cunningham J.M., Young J.A. Retroviral entry mediated by receptor priming and low pH triggering of an envelope glycoprotein. Cell. 2000;103(4):679–689. doi: 10.1016/s0092-8674(00)00170-7. [DOI] [PubMed] [Google Scholar]
- Negrete O.A., Levroney E.L., Aguilar H.C., Bertolotti-Ciarlet A., Nazarian R., Tajyar S., Lee B. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature. 2005;436(7049):401–405. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- Ogino M., Yoshimatsu K., Ebihara H., Araki K., Lee B.H., Okumura M., Arikawa J. Cell fusion activities of Hantaan virus envelope glycoproteins. J. Virol. 2004;78(19):10776–10782. doi: 10.1128/JVI.78.19.10776-10782.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plassmeyer M.L., Soldan S.S., Stachelek K.M., Martin-Garcia J., Gonzalez-Scarano F. California serogroup Gc (G1) glycoprotein is the principal determinant of pH-dependent cell fusion and entry. Virology. 2005;338(1):121–132. doi: 10.1016/j.virol.2005.04.026. [DOI] [PubMed] [Google Scholar]
- Pobjecky N., Smith J., Gonzalez-Scarano F. Biological studies of the fusion function of California serogroup Bunyaviruses. Microb. Pathog. 1986;1(5):491–501. doi: 10.1016/0882-4010(86)90011-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves J.D., Lee F.H., Miamidian J.L., Jabara C.B., Juntilla M.M., Doms R.W. Enfuvirtide resistance mutations: impact on human immunodeficiency virus envelope function, entry inhibitor sensitivity, and virus neutralization. J. Virol. 2005;79(8):4991–4999. doi: 10.1128/JVI.79.8.4991-4999.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronka H., Hilden P., Von Bonsdorff C.H., Kuismanen E. Homodimeric association of the spike glycoproteins G1 and G2 of Uukuniemi virus. Virology. 1995;211(1):241–250. doi: 10.1006/viro.1995.1397. [DOI] [PubMed] [Google Scholar]
- Schlegel R., Tralka T.S., Willingham M.C., Pastan I. Inhibition of VSV binding and infectivity by phosphatidylserine: is phosphatidylserine a VSV-binding site? Cell. 1983;32(2):639–646. doi: 10.1016/0092-8674(83)90483-x. [DOI] [PubMed] [Google Scholar]
- Schmaljohn C.a.J.W.H. Bunyaviridae: the viruses and their replication. In: Knipe P.M.H.D.M., Griffin D.E., Martin M.A., Lamb R.A., Roizman B., Straus S.E., editors. Fields Virology. 4th ed. Lippincott, Williams and Wilkins; Philadelphia, PA: 2001. [Google Scholar]
- Shi X., Lappin D.F., Elliott R.M. Mapping the Golgi targeting and retention signal of Bunyamwera virus glycoproteins. J. Virol. 2004;78(19):10793–10802. doi: 10.1128/JVI.78.19.10793-10802.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons G., Gosalia D.N., Rennekamp A.J., Reeves J.D., Diamond S.L., Bates P. Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proc. Natl. Acad. Sci. U.S.A. 2005;102(33):11876–11881. doi: 10.1073/pnas.0505577102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spik K., Shurtleff A., McElroy A.K., Guttieri M.C., Hooper J.W., Schmaljohn C. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine. 2006;24(21):4657–4666. doi: 10.1016/j.vaccine.2005.08.034. [DOI] [PubMed] [Google Scholar]
- Tamin A., Harcourt B.H., Ksiazek T.G., Rollin P.E., Bellini W.J., Rota P.A. Functional properties of the fusion and attachment glycoproteins of Nipah virus. Virology. 2002;296(1):190–200. doi: 10.1006/viro.2002.1418. [DOI] [PubMed] [Google Scholar]
- Thompson J.M., Whitmore A.C., Konopka J.L., Collier M.L., Richmond E.M., Davis N.L., Staats H.F., Johnston R.E. Mucosal and systemic adjuvant activity of alphavirus replicon particles. Proc. Natl. Acad. Sci. U.S.A. 2006;103(10):3722–3727. doi: 10.1073/pnas.0600287103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tischler N.D., Gonzalez A., Perez-Acle T., Rosemblatt M., Valenzuela P.D. Hantavirus Gc glycoprotein: evidence for a class II fusion protein. J. Gen. Virol. 2005;86(Pt 11):2937–2947. doi: 10.1099/vir.0.81083-0. [DOI] [PubMed] [Google Scholar]
- Turell M.J. Effect of environmental temperature on the vector competence of Aedes fowleri for Rift Valley fever virus. Res. Virol. 1989;140(2):147–154. doi: 10.1016/s0923-2516(89)80092-5. [DOI] [PubMed] [Google Scholar]
- Turell M.J., Rossi C.A., Bailey C.L. Effect of extrinsic incubation temperature on the ability of Aedes taeniorhynchus and Culex pipiens to transmit Rift Valley fever virus. Am. J. Trop. Med. Hyg. 1985;34(6):1211–1218. doi: 10.4269/ajtmh.1985.34.1211. [DOI] [PubMed] [Google Scholar]
- Wasmoen T.L., Kakach L.T., Collett M.S. Rift Valley fever virus M segment: cellular localization of M segment-encoded proteins. Virology. 1988;166(1):275–280. doi: 10.1016/0042-6822(88)90174-2. [DOI] [PubMed] [Google Scholar]
- White J., Helenius A. pH-dependent fusion between the Semliki Forest virus membrane and liposomes. Proc. Natl. Acad. Sci. U.S.A. 1980;77(6):3273–3277. doi: 10.1073/pnas.77.6.3273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J., Matlin K., Helenius A. Cell fusion by Semliki Forest, influenza, and vesicular stomatitis viruses. J. Cell Biol. 1981;89(3):674–679. doi: 10.1083/jcb.89.3.674. [DOI] [PMC free article] [PubMed] [Google Scholar]


