Abstract
OBJECTIVES
The safe use of medications in pediatric patients requires practitioners to consider the unique pharmacokinetics and pharmacodynamics of drugs prescribed in this age group. In an effort to create a standard of care for the safe use of medications in this population, a list of drugs that are potentially inappropriate for use in pediatric patients has been developed and titled the “KIDs List.”
METHODS
A panel of 7 pediatric pharmacists from the Pediatric Pharmacy Association were recruited to evaluate primary, secondary, and tertiary literature; FDA Pediatric Safety Communications; the Lexicomp electronic database; and product information for drugs that should be considered potentially inappropriate for use in pediatric patients. Information was rated using predefined criteria. A PubMed search was conducted using the following terms: adverse drug events OR adverse drug reactions. The search was limited to humans; age <18 years; case reports, observational studies, or clinical trials; and English language. No date range was used. Results were used to create an evidence-based list of candidate drugs that was then peer-reviewed and subjected to a 30-day public comment period prior to being finalized.
RESULTS
A PubMed search yielded 4049 unique titles, of which 210 were deemed relevant for full review. Practitioner recommendations highlighted an additional 77 drugs. FDA Pediatric Safety Communications and the Lexicomp database yielded 22 and 619 drugs, respectively. After critical analysis, peer review, and public review the final KIDs List contains 67 drugs and/or drug classes and 10 excipients.
CONCLUSIONS
This extensive effort led to compilation of the first list of drugs that are potentially inappropriate for prescribing in all or in a select subgroup of pediatric patients. If avoidance is not clinically possible, the drug should be used with caution and accompanied by appropriate monitoring.
Keywords: adverse drug reaction, drugs, excipient, medications, pediatrics, potentially inappropriate medications, medication safety
Introduction
According to the World Health Organization (WHO), adverse drug reactions (ADRs) are defined as “any noxious and unintended response to a drug that occurs in man at doses normally used for prophylaxis, treatment of diagnosis of disease, or for the modification of physiological function.”1 The vast majority of ADRs are benign, but some can be associated with significant morbidity and mortality. Although some ADRs are iatrogenic and unpredictable, others are unintended, but expected based on our knowledge of the pharmacology of the drug. Regardless of etiology, these are probably or definitely preventable. In addition to harm, preventable ADRs add unnecessary burden to the patient and parents and cost to the health care system.
Almost 30 years ago a list of inappropriate drugs for use in patients 65 years and older residing in nursing homes was created.2 Since that time the American Geriatric Society has updated and published what has become known as the “Beers Criteria.”3 The Beers Criteria represents a standard of care that has improved safe prescribing and use of drugs in older adults. A comparable evidence-based list of drugs that are associated with unintended and preventable ADRs would enhance medication safety in the pediatric population. With this in mind, the Pediatric Pharmacy Association (PPA) commissioned a group of pediatric pharmacists to evaluate the medical literature and compile a list of drugs that should be “avoided” or “used with caution” in all or a subset of the pediatric population.
The KIDs List is an essential first step to improving medication safety by serving as a reference tool to identify medications associated with a high risk for ADRs, thereby decreasing serious ADRs and creating a tool that could be used to evaluate and enhance the quality of care, decrease costs, and identify areas for needed research in the pediatric population. It is our hope that this resource will also serve as a catalyst for an increased dialogue among interprofessional practitioners and respective pediatric institutions and that it will enhance public awareness of the problem. With these goals in mind, we publish the Key Potentially Inappropriate Drugs in Pediatrics, or the “KIDs” List.
Background
Incidence of ADRs. The minimum rate of ADRs in all patients worldwide is estimated to be 5% per course of drug therapy.4 Serious ADRs occur in 6.7% of hospitalized adult patients, with a fatality rate of 0.32%.5 It has been estimated that ADRs cause 100,000 to 197,000 deaths annually in the United States and Europe, respectively.5,6 In fact, it has been noted that ADRs may be the fourth to sixth leading cause of death in adults.5
The frequency of ADRs in children have been investigated in a number of systemic reviews across more than 2 decades.7–11 These studies have explored ADR rates that caused hospitalization, occurred during hospital stay, or happened in the community setting. In a review of 80 studies reporting ADRs in children, Smyth et al10 found that the incidence of an ADR causing hospital admission ranged from 0.4% to 10.3%. Another study reported that ADRs were responsible for 4% of admissions to a large British children's hospital, with the ADR directly leading to the admission in 71% of cases.12 The authors concluded that 33% of the reactions were possibly avoidable.12 Smyth et al10 reviewed 21 prospective studies of hospitalized pediatric patients and found that ADRs occurred in up to 16.8% of patients. Thiesen et al9 reported that 17.7% of all children who spend more than 48 hours in a hospital experienced at least 1 ADR. Neonates occupy a unique subset of pediatric patients who have a high risk for ADRs and an even higher risk for serious ADRs. Kaguelidou et al11 used information between 1986 and 2012 housed in the French pharmacovigilance database to look specifically at the occurrence of ADRs in neonates <1 month of life. Of the 1688 neonates experiencing an ADR, 59% were considered serious.11 Regardless of environment, the incidence and prevalence of ADRs appear higher in the pediatric population than that noted in adults.
Estimates for ADRs in the community setting are even harder to determine and are often complicated by unintentional overdoses. In a review of 33 studies, Aagaard et al8 noted an ADR rate of 1.46% in outpatients. They also reported differences in ADR rates in the pediatric population, with about 25%, 50%, and 25% of ADRs occurring in children ages <1 year, 1 to 10 years, and >10 years, respectively.8
Multiple underlying reasons for the higher rates of ADRs in the pediatric population exist, including lack of FDA labeling in various pediatric populations and age-related differences in drug disposition and effect. Data on prescription medication use were available for 38,277 children and adolescents from 1999 to 2014, and Hales et al13 found that the overall use of any prescription medication in the past 30 days was 21.9%. During 2013–2014, Qato et al14 found that 19.8% of children and adolescents were prescribed at least 1 medication, and 7.5% used multiple medications. Rieder15 reported on a population of 1 million Canadian children and noted that about 20% of all prescriptions were written for 70% of patients, which suggested that patients with complex or chronic diseases frequently receive polytherapy.
Off-Label Use. Currently more than 1400 medications are available in the United States, with about 20 to 30 new medications being FDA approved each year.15 The approval and subsequent release of new medications onto the market often occurs without the benefit of even limited experience in pediatric patients. This lack of information often requires practitioners to prescribe drugs in an “off-label” manner, employing poorly defined dose strategies, which increases the risk of ADRs. The Best Pharmaceuticals for Children Act and the Pediatric Research Equity Act in the United States and 2 European reports (from the European Medicines Agency and European Union Commission) were designed to encourage more studies of medications used in the pediatric population.16 Although these legislative decisions provide incentives and requirements for pediatric studies of new drugs and their labeling, medications on the market prior to these acts often do not benefit from legislative incentives. Despite these initiatives, off-label use of medicines in children is still widespread. In fact, 50% of medications in the United States are still not labeled for use in children.17 Off-label use among European countries ranges from 13% to 69% and 2% to 100% of prescriptions prescribed off-label in the hospital and primary care settings, respectively.18 Off-label use of drugs presents an even larger and more complex issue in preterm and full-term neonates, in infants and children ages <2 years, in children with rare or chronic diseases, and in those who are critically ill. In fact, Nir-Neuman et al19 reported that among the 1064 prescriptions for 49 medications in critically ill neonates, 64.8% involved off-label use. Likewise, the number of critically ill pediatric patients receiving at least 1 off-label medication was 88.7%. The risk of ADRs in the pediatric population is increased because pediatric practitioners must rely on case reports, anecdotal observational experience, and historical dogma in lieu of evidence-based studies.
Altered Pharmacokinetics. Another important contributing factor to an increased rate of ADRs in the pediatric population is the relationship of ontogeny of systems and the resultant impact of developmental pharmacology on drug therapy. Growth and development from birth to adolescence is a dynamic process that increases a patient's risk for ADRs as he or she undergoes significant maturational changes in body composition and organ function.20–22 Because the pharmacologic response to a drug is dependent on these changes, an approach to medication use in the pediatric arena requires an understanding of physiologic characteristics at various ages combined with a comprehensive knowledge of the pharmacokinetics of a specific drug. Without question, age is correlated with drug pharmacokinetics resulting from changes in absorption, distribution, metabolism, and excretion. Developmental changes in absorptive surfaces (e.g., gastrointestinal tract, skin, pulmonary tract), intragastric pH, and changes in gastric emptying times and intestinal motility rates affect drug absorption. Maturational changes occur in gut drug transports and drug-metabolizing enzymes. Neonates have a thinner stratum corneum, which enhances percutaneous absorption of drugs. During a decade, body composition changes as total body water decreases and body fat increases. Phase l and phase 2 hepatic metabolizing enzyme systems mature over time. These processes are responsible for the biotransformation of drugs. The ontogeny of these reactions is significantly under-developed in premature and full-term neonates. The kidney is responsible for the clearance of many drugs from the body. The development of renal function (i.e., glomerular filtration, tubular secretion) approaches that of an adult by the first year of life.
Methods
Panel Selection and Composition. The PPA Board of Directors commissioned this work on March 23, 2017. Seven pediatric pharmacists were recruited from the PPA membership, in part based on experience in various subpopulations of pediatric practice. These practice domains included, but were not limited to, neonatal and pediatric critical care, hematology/oncology, and general pediatrics. Each panel member completed a conflict of interest disclosure form at the beginning of the process and again at each meeting of the panel. No panel member had a conflict of interest that precluded participation.
Process and Operational Definitions. The process began with discussion regarding the process that would be used to identify, review, and assess information related to ADRs in the pediatric population. The focus of the early meetings of the panel related to definition of terms and methodologies used to identify and assess ADRs. Once abstracts were identified, the full text of a subset of articles that met inclusion criteria were pulled and reviewed.
ADR. The panel adopted the WHO description of an ADR: “Any noxious and unintended response to a drug that occurs in man at doses normally used for prophylaxis, treatment of diagnosis of disease, or for the modification of physiological function.”1
Potentially Inappropriate Use. Potentially inappropriate medications are defined by the Beers Criteria as “medications or medication classes that should generally be avoided in persons 65 years or older because they are either ineffective or they pose unnecessarily high risk for older persons and a safer alternative is available.”23 For the KIDs List, potentially inappropriate medications are thus defined as “medications or medication classes that should generally be avoided in persons younger than 18 years because they pose an unnecessarily high risk for children and a safer alternative is available.” Drug ineffectiveness was not a criteria for the KIDs List. This list is meant to serve as a clinical tool and is not meant to replace clinical judgment or be used in a punitive manner. Needs of an individual patient, management of a disease(s), or unique situations may surpass the recommendations of this list. The choice of appropriate medications for pediatric patients should involve an interprofessional health care team that takes into consideration the values and preferences of the child and legal guardians.
Avoid Versus Caution. Two recommendations were used in the KIDs List: avoid and caution. Avoid was used when either the strength of the recommendation was strong or the potential adverse effect was of a life-threatening or life-altering nature. Caution was used to describe drugs in which the quality of evidence was low or very low or the strength of the recommendation was weak, or if there was a clear therapeutic need for the drug despite the evidence still demonstrating a higher risk in children than in adults.
Ages. Because maturation of physiologic systems affects the likelihood of ADRs given the pharmacology of the drug or excipient, the panel felt it was necessary to use subsets of ages in considering the different levels of risk for an ADR. Hence, patients were further stratified as: 1) very low birth weight, defined as <1500 g; 2) neonates <1 month; 3) infants <24 months; and 4) children <18 years. The definition of age for “children” (i.e., birth to 18 years) used in the KIDs List encompasses neonates, infants, young children, older children, and adolescents, rather than the traditional age definitions.24,25 The panel did not find evidence that children and adolescents were different with regard to evidence in the literature supporting a different drug restriction strategy.
Strength of Recommendation. This assessment reflected a classification by the panel describing the seriousness of an ADR, the extent to which the clinician can be confident in concluding that the desirable effects of an intervention outweigh the undesirable effects. A “strong” recommendation is predicated on the belief that most informed clinicians would choose the recommended course of action. The implication of a strong recommendation is that when the clinician is presented with information about a specific ADR he or she would choose to avoid or use the drug cautiously in lieu of assuming the risk of the ADR. A strong recommendation allows clinicians to have confidence in their interactions with patients and to structure discussions accordingly. Conversely, a weak recommendation is consistent with significant variability in the decisions that a clinician would make when presented with information about a specific ADR. Because these decisions may vary according to the parents' and patients' values and preferences, the clinician must ensure that drug treatment is in keeping with their values and preferences.
Quality of Evidence. The quality of evidence is a reflection of the aggregate of published information. When the quality of evidence is high, the strength of a recommendation is greater than if the quality is low. The quality of evidence definitions used for the KIDs List were based on those from the GRADE recommendations26 and used by the Beers Criteria.27 Although the Beers group eliminated the “very low” classification, the KIDs List panel elected to keep it given the paucity of high-quality data on adverse drug events in children. An assessment of “high quality” indicates that further published information or research is very unlikely to alter our confidence in the recommendation or estimate of ADR effect. “Moderate” quality suggests that further research may have an important impact on our confidence because it may influence or change the evidence regarding a recommendation. A “low” estimate of quality implies that further published information or research is likely to affect our confidence in the estimate of effect and is likely to change the conclusion. A “very low” implies that any estimate of effect is very uncertain.
Literature Search and Review. Electronic databases, published communications, information from package inserts, practice guidelines, member expertise, and external reviewers were used to ensure that the maximum number of drugs and excipients were identified for initial consideration. The process is described in Figure 1. Articles and sources were collected, screened, and assessed for eligibility using the PRISMA strategy.28
Figure 1.
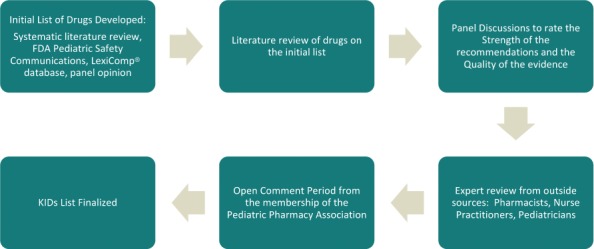
Methods for development of the KIDs List.
Electronic Databases. An initial PubMed search was conducted on October 24, 2017. The search strategy included “adverse drug events” and “ADR” as keywords and/or mesh-terms, which were combined with “< 18-years-old” as a filter. Other filters included “human studies,” “case reports,” “observational studies,” and “clinical trials.” Date ranges were not used, but the search was restricted to items published in the English language.
Lexi-Drugs Online and Pediatric and Neonatal Lexi-Drugs Online databases were searched by a Lexicomp staff member on November 20, 2017. The fields “ALERT: US Boxed Warnings,” “Special Alerts,” and “Warnings & Precautions (contains Contraindications and Warnings/Precautions)” were searched using the following terms: “children” OR “pediatric” OR “neonate” OR “infant” OR “child” OR “adolescent.” A panel member narrowed the list based on predefined inclusion and exclusion criteria. The list of potential candidate monographs was categorized for distribution according to the specialty expertise of the panel members.
FDA Communications. FDA Pediatric Safety Communications29 were searched by 1 panel member. The site was searched for reports through January 2019. PubMed searches were performed on identified drugs using the methods previously described.
Panel Members. Individuals on the panel suggested drugs and excipients that were thought to be potentially harmful in pediatric patients. These suggestions were based on past experience, pharmacy education, or residency training, or anecdotal evidence among the community of pediatric pharmacists. A PubMed search on each drug was conducted using the methods previously described. Full texts of all pertinent manuscripts were brought forward to the panel for review and discussions regarding inclusion.
Inclusion Criteria. Drugs and excipients were considered for inclusion if: 1) the drug was commercially available in the United States (did not require pediatric labeling); 2) the ADR was documented in medical literature and was clearly attributed to the drug or excipient; 3) a safer therapeutic alternative was available; 4) the ADR occurred in patients between 0 and 18 years of age; and 5) the incidence, frequency, and severity of the ADR were greater in the pediatric population than in adults.
Exclusion Criteria. Drugs and excipients were excluded if: 1) the agent was a vaccine, drug device, herbal product, parenteral nutrition component, inhaled anesthetic, contrast agent, or illicit drug; or 2) the ADR was due to teratogenicity, drug exposure based on breastfeeding, an overdose, or an allergic reaction. Therapeutic effectiveness of drugs and FDA labeling were not considered when comparing drugs.
Extraction of Data. Once abstracts, articles, monographs, or communications were available they were reviewed by 2 panel members for inclusion and exclusion based on predefined criteria. If one of those individuals concluded that the drug or excipient warranted further consideration it was discussed by the full panel.
Analysis. Between October 2017 and January 2019, the panel held weekly or monthly meetings via conference calls. During these meetings the panel reviewed and discussed candidate drugs and excipients. Panel members were assigned to conduct follow-up PubMed research on drugs and excipients identified during the process. Panel members conducted the research between the meetings and returned with references and a recommendation action (i.e., avoid, caution) and determination of strength of recommendation and quality of evidence to the whole panel for discussion. The panel decided by consensus the merits of the research available, whether it met inclusion or exclusion criteria, and its bearing on whether the drug should be included in the KIDs List.
Internal and External Review. The manuscript was reviewed by 2 pediatric pharmacists from PPA as well as an interprofessional group of individuals (see Acknowledgments) who are recognized experts in pediatric drug therapy. The document was also reviewed by 1 nurse practitioner representing the Academy of Neonatal Nursing, and 1 nurse practitioner representing the National Association of Nurse Practitioners. Comments generated by these reviewers were researched and discussed by the panel, and a revised manuscript was developed. This manuscript was submitted to the more than 1500 members of PPA for review via an electronic communication. Comments were accepted during a 30-day period. The panel discussed and researched all comments and generated the final KIDs List manuscript. The List will be updated at least every 5 years or earlier if data become available prompting action.
Results
A summary of the systemic review and identification of included drugs and excipients is outlined in Figure 2. The initial PubMed search yielded 4049 unique titles. A total of 973 abstracts were reviewed by 2 panel members who identified 210 articles for full-text review. A search of all 3600 monographs included in the two Lexicomp databases yielded 1038 drugs, of which 619 were included for consideration by the full panel. The drugs fell into the following categories: neonatal (n = 30), neurology/psychology (n = 79), infectious disease/pulmonary (n = 106), hematology/oncology (n = 85), general pediatrics (n = 116), critical care (n = 100), and endocrinology/nephrology (n = 103). Expert opinion led to the identification of an additional 77 drugs, which were evaluated via literature searches. The review of FDA Pediatric Safety Communications yielded 31 relevant announcements. Of those, 22 were forwarded to the full panel for consideration.
Figure 2.
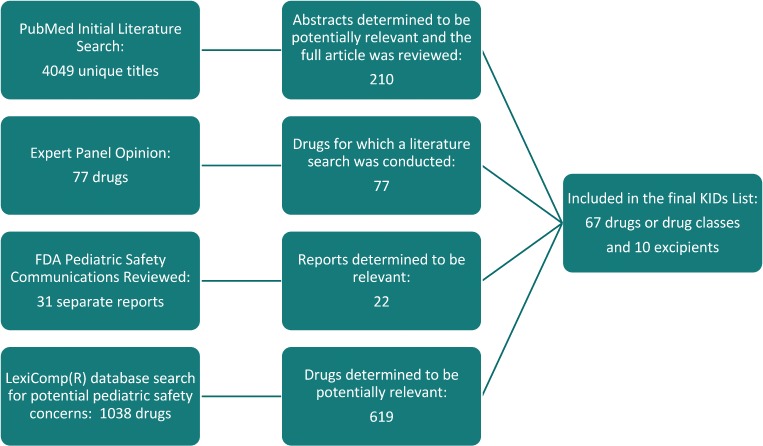
Results of literature search, expert opinions, FDA Pediatric Safety Communications, and Lexicomp® database search.
Ultimately, 126 items were cited in the report, with 110 and 16 associated with drugs and excipients, respectively. These included peer-reviewed publications, such as research articles, case reports, or series; systemic reviews; and national guidelines. The citations also included important committee/panel reports from national organizations. Communications from the FDA, CDC and opinion items, as well as prescribing information from package inserts, were also included.
The final KIDs List contains 67 drugs (Table 1). The most frequently cited groups included anti-infectives, antipsychotics, dopamine antagonists and gastrointestinal agents. Most of the drugs (85%) required a prescription. Most of the drugs were available in various and multiple dosage formulations, including oral, parenteral, and external.
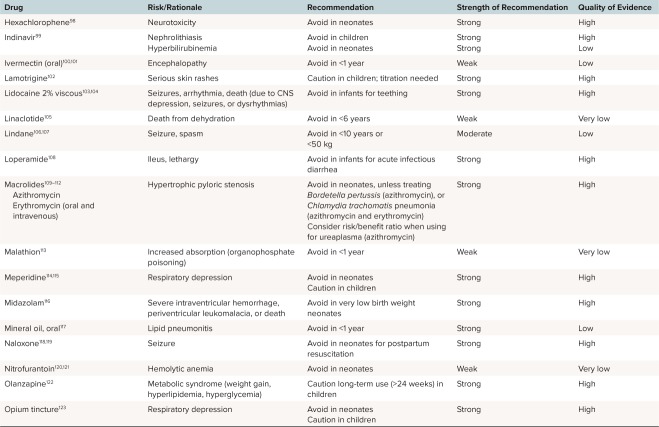
Table 1.
The KIDs List
| Drug | Risk/Rationale | Recommendation | Strength of Recommendation | Quality of Evidence | ||||
|---|---|---|---|---|---|---|---|---|
| Atazanavir51 | Kernicterus | Caution in neonates unless pharmacogenetic testing is used | Weak | Very low | ||||
| Benzocaine52–57 | Methemoglobinemia | Avoid in infants for teething or pharyngitis | Strong | High | ||||
| Camphor58–60 | Seizures | Caution in children | Weak | Low | ||||
| Carbinoxamine61 | Death | Avoid in <1 year | Strong | Low | ||||
| Ceftriaxone62,63 | Kernicterus | Caution in neonates | Weak | Very low | ||||
| Chloramphenicol64 | Gray baby syndrome | Avoid in neonates unless serum concentration monitoring is used | Strong | High | ||||
| Chlorhexidine65 | Chemical burn | Caution in very low birth weight neonates | Strong | Low | ||||
| Codeine66–69 | Respiratory depression, death | Avoid in children unless pharmacogenetic testing is used | Strong | High | ||||
| Darunavir70 | Seizures, death | Avoid in <3 years or <10 kg | Strong | Very low | ||||
| Daptomycin71 | Neuromuscular and skeletal adverse events | Caution in <1 year | Weak | Very low | ||||
| Dicloxacillin72 | Kernicterus | Caution in neonates | Weak | Very low | ||||
| Dicyclomine73 | Apnea | Avoid in <6 months | Strong | Low | ||||
| Difluprednate74,75 | Increased intraocular pressure | Caution in children | Weak | Low | ||||
| Diphenoxylate and atropine76 | Respiratory depression, death | Avoid in <6 years | Strong | Moderate | ||||
| Dopamine antagonists | Acute dystonia (dyskinesia); increased risk of respiratory depression, extravasation, and death with intravenous use | Avoid in infants Caution in children | Strong:
|
Moderate | ||||
| Gentamicin ophthalmic ointment95–97 | Severe ocular reactions | Avoid in neonates | Strong | High | ||||
| Hexachlorophene98 | Neurotoxicity | Avoid in neonates | Strong | High | ||||
| Indinavir99 | Nephrolithiasis | Avoid in children | Strong | High | ||||
| Hyperbilirubinemia | Avoid in neonates | Strong | Low | |||||
| Ivermectin (oral)100,101 | Encephalopathy | Avoid in <1 year | Weak | Low | ||||
| Lamotrigine102 | Serious skin rashes | Caution in children; titration needed | Strong | High | ||||
| Lidocaine 2% viscous103,104 | Seizures, arrhythmia, death (due to CNS depression, seizures, or dysrhythmias) | Avoid in infants for teething | Strong | High | ||||
| Linaclotide105 | Death from dehydration | Avoid in <6 years | Weak | Very low | ||||
| Lindane106,107 | Seizure, spasm | Avoid in <10 years or <50 kg | Moderate | Low | ||||
| Loperamide108 | Ileus, lethargy | Avoid in infants for acute infectious diarrhea | Strong | High | ||||
Macrolides109–112
|
Hypertrophic pyloric stenosis | Avoid in neonates, unless treating Bordetella pertussis (azithromycin), or Chlamydia trachomatis pneumonia (azithromycin and erythromycin) Consider risk/benefit ratio when using for ureaplasma (azithromycin) | Strong | High | ||||
| Malathion113 | Increased absorption (organophosphate poisoning) | Avoid in <1 year | Weak | Very low | ||||
| Meperidine114,115 | Respiratory depression | Avoid in neonates Caution in children | Strong | High | ||||
| Midazolam116 | Severe intraventricular hemorrhage, periventricular leukomalacia, or death | Avoid in very low birth weight neonates | Strong | High | ||||
| Mineral oil, oral117 | Lipid pneumonitis | Avoid in <1 year | Strong | Low | ||||
| Naloxone118,119 | Seizure | Avoid in neonates for postpartum resuscitation | Strong | High | ||||
| Nitrofurantoin120,121 | Hemolytic anemia | Avoid in neonates | Weak | Very low | ||||
| Olanzapine122 | Metabolic syndrome (weight gain, hyperlipidemia, hyperglycemia) | Caution long-term use (>24 weeks) in children | Strong | High | ||||
| Opium tincture123 | Respiratory depression | Avoid in neonates Caution in children | Strong | High | ||||
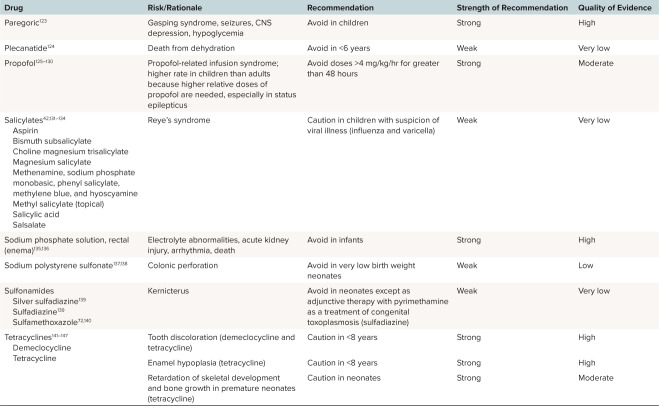
| Paregoric123 | Gasping syndrome, seizures, CNS depression, hypoglycemia | Avoid in children | Strong | High | ||||
| Plecanatide124 | Death from dehydration | Avoid in <6 years | Weak | Very low | ||||
| Propofol125–130 | Propofol-related infusion syndrome; higher rate in children than adults because higher relative doses of propofol are needed, especially in status epilepticus | Avoid doses >4 mg/kg/hr for greater than 48 hours | Strong | Moderate | ||||
Salicylates42,131–134
|
Reye's syndrome | Caution in children with suspicion of viral illness (influenza and varicella) | Weak | Very low | ||||
| Sodium phosphate solution, rectal (enema)135,136 | Electrolyte abnormalities, acute kidney injury, arrhythmia, death | Avoid in infants | Strong | High | ||||
| Sodium polystyrene sulfonate137,138 | Colonic perforation | Avoid in very low birth weight neonates | Weak | Low | ||||
| Sulfonamides | Kernicterus | Avoid in neonates except as adjunctive therapy with pyrimethamine as a treatment of congenital toxoplasmosis (sulfadiazine) | Weak | Very low | ||||
Tetracyclines141–147
|
Tooth discoloration (demeclocycline and tetracycline) Enamel hypoplasia (tetracycline) Retardation of skeletal development and bone growth in premature neonates (tetracycline) | Caution in <8 years Caution in <8 years Caution in neonates | Strong Strong Strong | High High Moderate | ||||
| Topical corticosteroids (medium, high and very high potency)148,149 | Adrenal suppression; higher rate of systemic absorption in children than adults | Avoid in <1 year for diaper dermatitis | Strong | Low | ||||
| Tramadol66,150 | Respiratory depression | Caution in children unless pharmacogenomic testing is used | Weak | Low | ||||
Tricyclic antidepressants151–153
|
Sudden cardiac death | Avoid in children (desipramine) Caution in children (imipramine) | Strong | High (desipramine) Moderate (imipramine) | ||||
| Valproic acid and derivatives154–156 | Pancreatitis, fatal hepatotoxicity | Avoid in infants Caution in <6 years | Strong | High | ||||
| Verapamil157–159 | Asystole | Avoid in <1 year | Weak | Low | ||||
Table 1.
The KIDs List
Table 1.
The KIDs List
Table 1.
The KIDs List
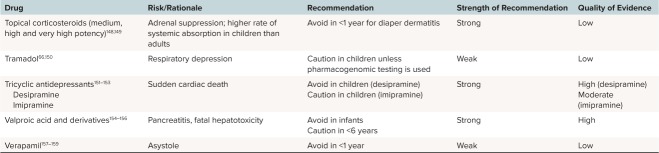
There was sufficient evidence to classify 39 drugs/excipients as “avoid” and 23 as “use with caution.” As expected, most of the drugs classified as “avoid” had a combination of strength of recommendation plus quality of evidence as either “strong” and “high” or “strong” and “moderate” (65%). Far fewer drugs classified as “use with caution” had a combination of strength of recommendation plus quality of evidence as either “strong” and “high” or “strong” and “moderate” (29%). Ten excipients were identified (Table 2). Six of these pharmaceutical vehicles were noted as “avoid” and 4 were determined to be “use with caution.” Five excipients noted as “avoid” were specific for neonates.
Table 2.
Excipients With Known or Potential Harms When Used in Pediatric Patients
| Excipient | Rationale | Recommendation | Strength of Recommendation | Quality of Evidence |
|---|---|---|---|---|
| Benzyl alcohol, sodium benzoate, benzoic acid33,34,160–163 | Gasping syndrome | Avoid exposure of >99 mg/kg/day in neonates (with the exception of sodium phenylacetate/sodium benzoate used for the treatment of urea cycle disorders) | Strong | High |
| Ethanol/ethyl alcohol34,164 (this excludes ethanol lock) | CNS depression, hypoglycemia | Caution in <6 years; maximum of 5% vol/vol ethanol with clinician supervision | Strong | Moderate |
| Isopropyl alcohol165,166 | Chemical burn | Caution in very low birth weight neonates | Strong | Low |
| Methylparaben, propylparaben167 | Kernicterus | Caution in <2 months | Strong | Very low |
| Phenylalanine168 | Cognitive and behavioral problems | Avoid in children with an unknown phenylketonuria test | Strong | High |
| Polysorbate 80169–171 | E-Ferol syndrome | Avoid in <1 year (any amount) | Strong | High |
| Propylene glycol33,34,172,173 | Lactic acidosis, CNS depression, hypoglycemia, hemolysis, seizure | Avoid doses >3 g/day in neonates; caution doses >34 mg/kg/day in neonates | Strong | Moderate |
Discussion
Pediatric patients have a unique vulnerability to ADRs. Some drugs may require more caution in children because of underdeveloped metabolic pathways or organ or tissue systems, whereas others may be less harmful, such as with those drugs that have enhanced renal clearance in young healthy kidneys. Through a lengthy process, we identified 67 drugs and drug classes and 10 excipients that are potentially inappropriate for use in all or a subgroup of pediatric patients. The number of strong recommendations in the KIDs List was lower (68%) than that seen in the Beers Criteria3 (95%). This highlights the need for more evidence to further define and clarify these adverse reactions in the pediatric population.
Intent. The KIDs List is meant to serve as an evidence-based guide to improve the safety of medication use in pediatric patients. The primary target audience of this publication is health care professionals caring for patients younger than 18 years in the acute and chronic institutional setting, as well as ambulatory and community settings. The KIDs List is intended to be a guide, and the recommendations do not suggest absolute contraindication of any drug in any pediatric patient. As in all medical cases, the entire clinical picture of the patient must be assessed and evaluated by the health care professionals directly involved in the patient's care, and treatment with drugs on this list may be warranted, depending on the clinical situation. The KIDs List is not a substitute for clinical judgment. There may be specific populations or diseases for which treatment with any of these drugs is warranted. The intent of the KIDs List is to improve the safety of medication use in children, educate clinicians and patients, and serve as a quality control tool.
It should be noted that some drugs included on this list are also on the WHO Model List of Essential Medicines for Children.30 Acceptable therapeutic alternatives readily available in the United States (for the same indication) played a role in the expert panel's determination of recommendation in the KIDs List. The KIDs List is not intended to nullify the WHO Model List of Essential Medicines for Children. Use of these drugs in other countries for certain clinical conditions may be warranted.
Application. This list should serve as a useful resource for clinicians and institutions caring for children and provide a basis for allocation of resources and additional research to improve drug safety in the pediatric population. During the review, only those drugs approved for use in the United States, regardless of US FDA-labeled age, were considered; hence, application of this list for pediatric patients in countries other than the United States may not be appropriate.
Limitations. Generation of the KIDs List resulted in several unexpected challenges. The panel sought to identify whether adverse events from individual drugs were associated with a chemical or therapeutic class effect. Evaluation of individual drugs within a class of drugs with concerning in vitro data was impossible in some cases. For example, numerous drugs displace bilirubin from albumin in vitro, raising the concern for increased risk of kernicterus in neonates. However, some drugs (e.g., ibuprofen) have corresponding clinical data demonstrating safety in neonates.31,32 These drugs were excluded from the list. Several other drugs with similar in vitro concerns are included in the list with a weak recommendation based on a very low quality of data. This is not because corresponding data corroborate in vitro data with clinical evidence of ADRs in pediatric patients, but because in vivo data are lacking. In these cases, we hope health care professionals will carefully evaluate the real-world impact of these agents before widespread clinical use occurs. The KIDs List highlights areas of research needed in the pediatric population.
Excipients posed a challenge for the panel because no complete list of drugs with benzyl alcohol, ethanol, propylene glycol, and other excipients exists. Each drug may be noted to contain excipients, but not always the amount within the product. Although it is known that certain excipients have led to significant adverse effects and death in pediatric patients, there are not documented acceptable limits for all excipients in neonates and children.33,34 Therefore, we considered excipients individually and included available information. Clinicians must remain diligent about the presence and concentration of these excipients in drugs prescribed to pediatric patients.
Considered but Not Included. Many drugs were proposed for inclusion in the KIDs List based on historical or personal beliefs, but were not included because evidence was not sufficient to include them based on the methodology used by the panel. Some of the drugs and drug classes that were commonly recommended, but not included are considered here.
Over-the-counter pediatric cough and cold preparations have come under scrutiny because there is limited literature to demonstrate clinical effectiveness, and the risks of toxicity are well documented.35,36 These medications were not included in the KIDs List because safety issues were closely linked with overdoses, and the panel could not find a clear toxicity risk when labeled dosing regimens are used in recommended doses.37 This should not be taken as an endorsement of these products for clinical use; there simply was not enough evidence to confer a clear safety risk when using therapeutic doses of these agents in children.
Supporting evidence for the historical recommendation to avoid fluoroquinolones in children was not found to be sufficiently robust.38 After discussion of the potential for clinical benefit, particularly in certain populations, such as patients with complicated urinary tract infections,39 cystic fibrosis,40 and certain community-acquired pneumonia cases,41 a decision was made to not include this class of drugs.
Aspirin also has a long history of being avoided in children because of the proposed association with Reye syndrome. Recent literature42 contesting this association, along with its frequent use and proven benefit in certain populations, such as those with Kawasaki disease,43 postischemic stroke,44 and cardiac surgery patients,44,45 led to the panel's decision to give a weak recommendation to use with caution in children with suspicion of viral illness (influenza and varicella).
Although pediatric labeling can be an endorsement of safety for the indication, the panel reviewed primary literature and compared the safety of drugs within therapeutic classes. From this perspective, the risks of some FDA-approved drugs were deemed significant enough to warrant inclusion of those drugs on the KIDs List. Likewise, although FDA Pediatric Safety Communications were used to identify drugs with a higher likelihood of harm in pediatric patients, their existence was not, in and of itself, considered evidence of a higher likelihood of harm. Although it is acknowledged that the FDA may have internal data not found in the primary literature, the panel nevertheless sought to understand the reasoning behind FDA warnings and, when based on the primary literature, the panel applied the GRADE approach to determine whether to place a drug on the KIDs List. Sildenafil is an example of a drug excluded from the KIDs List that has an FDA warning that recommends against pediatric use. Upon review of the STARTS-146 and STARTS-247 trials, the panel decided that sildenafil did not carry an age-specific toxicity concern. Rather, it could be safely used in pediatric patients if dosed correctly in the proper subpopulations of patients with pulmonary arterial hypertension.
Antidepressants presented a similar challenge. In 2004, the FDA issued a US Boxed Warning on the entire class of antidepressants, indicating they were associated with an increased risk of suicidality and suicidal ideation in children.48 When considering a class effect with these drugs, the panel felt antidepressants are clinically beneficial to many pediatric patients and including this entire class of drugs would not provide clinicians with a useful decision support tool. The panel made an effort to determine if any particular drug in the class posed a greater risk than others49,50 and found that at this time there is insufficient evidence to suggest that any of these drugs have a higher risk of suicidality or suicidal ideation, and thus the class was left off the list. This is another example where additional research may influence this decision for the next version of the KIDs List.
Future Directions. The panel expects significant feedback on this document. Our intent is to collect comments and consider the recommendations in light of new literature. An updated KIDs List will be published when a critical mass of new data warrants an update. This list is the first step in the ongoing work of clinicians and researchers to continuously improve the safety of pediatric pharmacotherapy, used in combination with a thorough process that incorporates drug-drug interaction checking, pharmacogenomics results, and patient-specific and clinical factors.
Conclusions
An extensive literature review and panel discussion facilitated compilation of the first iteration of a list of drugs and excipients that should generally be avoided or used with caution in all or select subgroups of pediatric patients. The KIDs List serves as a tool to improve drug safety for children. It provides a starting point in clinical decision-making, functioning as an evidence-based reference of the risks associated with relatively contraindicated drugs in the pediatric population. This list also serves as a reference to combat historical dogma, accurately reflecting the rationale and level of evidence supporting contraindications and highlighting knowledge gaps in the published literature. Recommendations found in this list will evolve over time with additional research and clinical experience. Although knowledge of pediatric pharmacology has increased dramatically, ongoing efforts to promote investigation of pediatric pharmacotherapy will improve the depth and quality of future iterations of this list.
Acknowledgments
The panel wishes to acknowledge the organizational support of the Pediatric Pharmacy Association in the creation of this manuscript. We appreciate Wolters-Kluwer Clinical Drug Information Inc for its generous assistance with use and a query of their Lexi-Drugs and Pediatric and Neonatal Lexi-Drugs databases. We also recognize the work of Stephanie J. Phelps, BScPharm, PharmD; Jeff Cies, PharmD, MPH; Shannon Manzi, PharmD; Collin Hovinga, PharmD, MS; Jared Cash, BS, PharmD, MBA; Edress Darcy, PharmD; Kelly Wade, MD, PhD, MSCE; Gregory Kearns, PharmD, PhD; Debra Fraser, MN, RNC-NIC; Michael Cohen, BScPharm, MS, ScD (hon), DPS (hon); and Teri Woo, PhD, ARNP, CPNP-PC, for their critical review and constructive comments concerning this manuscript.
ABBREVIATIONS
- ADR
adverse drug reaction
- CNS
central nervous system
- FDA
Food and Drug Administration
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- PPA
Pediatric Pharmacy Association
- WHO
World Health Organization
Footnotes
Disclosure The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria. The authors had full access to all the data and take responsibility for the integrity and accuracy of the data analysis. Dr Thackray is funded by National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748.
Ethical Approval and Informed Consent Given the nature of this study, institution review board/ethics committee approval was not required.
Endorsements This manuscript was endorsed by the Pediatric Pharmacy Association, Academy of Neonatal Nursing, Institute for Safe Medication Practices, and National Association of Pediatric Nurse Practitioners.
REFERENCES
- 1.World Health Organization Safety of medicines – a guide to detecting and reporting adverse drug reactions – why health professionals need to take action. 2002 http://apps.who.int/medicinedocs/en/d/Jh2992e/2.html Accessed January 19, 2020.
- 2.Beers MH, Ouslander JG, Rollingher I et al. Explicit criteria for determining inappropriate medication use in nursing home residents: UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151(9):1825–1832. [PubMed] [Google Scholar]
- 3.The American Geriatrics Society Beers Criteria Update Expert Panel American Geriatrics Society 2019 Updated AGS Beers Criteria(R) for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–694. doi: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 4.Elzagallaai AA, Greff M, Rieder MJ. Adverse drug reactions in children: the double-edged sword of therapeutics. Clin Pharmacol Ther. 2017;101(6):725–735. doi: 10.1002/cpt.677. [DOI] [PubMed] [Google Scholar]
- 5.Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200–1205. doi: 10.1001/jama.279.15.1200. [DOI] [PubMed] [Google Scholar]
- 6.European Commission Proposal for a regulation amending, as regards pharmacovigilance of medicinal products for human use. Regulation (EC) No 726/2004. Impact assessment. 2008 Available at: http://ec.europa.eu/health/files/pharmacos/pharmpack_12_2008/pharma-covigilance-ia-vol1_en.pdf Accessed February 2, 2020.
- 7.Clavenna A, Bonati M. Adverse drug reactions in childhood: a review of prospective studies and safety alerts. Arch Dis Child. 2009;94(9):724–728. doi: 10.1136/adc.2008.154377. [DOI] [PubMed] [Google Scholar]
- 8.Aagaard L, Christensen A, Hansen EH. Information about adverse drug reactions reported in children: a qualitative review of empirical studies. Br J Clin Pharmacol. 2010;70(4):481–491. doi: 10.1111/j.1365-2125.2010.03682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thiesen S, Conroy EJ, Bellis JR et al. Incidence, characteristics and risk factors of adverse drug reactions in hospitalized children – a prospective observational cohort study of 6,601 admissions. BMC Med. 2013;11:237. doi: 10.1186/1741-7015-11-237. doi: 10.1186/1741-7015-11-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smyth RM, Gargon E, Kirkham J et al. Adverse drug reactions in children—a systematic review. PLoS One. 2012;7(3) doi: 10.1371/journal.pone.0024061. e24061. doi: 10.1371/journal.pone.0024061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaguelidou F, Beau-Salinas F, Jonville-Bera AP, Jacqz-Aigrain E. Neonatal adverse drug reactions: an analysis of reports to the French pharmacovigilance database. Br J Clin Pharmacol. 2016;82(4):1058–1068. doi: 10.1111/bcp.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallagher RM, Bird KA, Mason JR et al. Adverse drug reactions causing admission to a paediatric hospital: a pilot study. J Clin Pharm Ther. 2011;36(2):194–199. doi: 10.1111/j.1365-2710.2010.01194.x. [DOI] [PubMed] [Google Scholar]
- 13.Hales CM, Kit BK, Gu Q, Ogden CL. Trends in prescription medication use among children and adolescents—United States, 1999–2014. JAMA. 2018;319(19):2009–2020. doi: 10.1001/jama.2018.5690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qato DM, Alexander GC, Guadamuz JS, Lindau ST. Prescription medication use among children and adolescents in the United States. Pediatrics. 2018;142(3) doi: 10.1542/peds.2018-1042. pii: e20181042. [DOI] [PubMed] [Google Scholar]
- 15.Kinch MS, Haynesworth A, Kinch SL, Hoyer D. An overview of FDA-approved new molecular entities: 1827–2013. Drug Discov Today. 2014;19(8):1033–1039. doi: 10.1016/j.drudis.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 16.Rose K. The challenges of pediatric drug development. Curr Ther Res Clin Exp. 2019;90:128–134. doi: 10.1016/j.curtheres.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sachs AN, Avant D, Lee CS et al. Pediatric information in drug product labeling. JAMA. 2012;307(18):1914–1915. doi: 10.1001/jama.2012.3435. [DOI] [PubMed] [Google Scholar]
- 18.Schrier L, Hadjipanayis A, Stiris T et al. Off-label use of medicines in neonates, infants, children, and adolescents: a joint policy statement by the European Academy of Paediatrics and the European society for Developmental Perinatal and Pediatric Pharmacology [published online ahead of print January 3, 2020] Eur J Pediatr. doi: 10.1007/s00431-019-03556-9. [DOI] [PubMed] [Google Scholar]
- 19.Nir-Neuman H, Abu-Kishk I, Toledano M et al. Unlicensed and off-label medication use in pediatric and neonatal intensive care units: no change over a decade. Adv Ther. 2018;35(7):1122–1132. doi: 10.1007/s12325-018-0732-y. [DOI] [PubMed] [Google Scholar]
- 20.Kearns GL, Abdel-Rahman SM, Alander SW et al. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349(12):1157–1167. doi: 10.1056/NEJMra035092. [DOI] [PubMed] [Google Scholar]
- 21.van den Anker J, Reed MD, Allegaert K, Kearns GL. Developmental changes in pharmacokinetics and pharmaco-dynamics. J Clin Pharmacol. 2018;58(suppl 10):S10–S25. doi: 10.1002/jcph.1284. [DOI] [PubMed] [Google Scholar]
- 22.Lu H, Rosenbaum S. Developmental pharmacokinetics in pediatric populations. J Pediatr Pharmacol Ther. 2014;19(4):262–276. doi: 10.5863/1551-6776-19.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fick DM, Cooper JW, Wade WE et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 24.Hardin AP, Hackell JM. Committee on Practice and Ambulatory Medicine. Age limit of pediatrics. Pediatrics. 2017;140(3) doi: 10.1542/peds.2017-2151. pii: e20172151. doi: 10.1542/peds.2017-2151. [DOI] [PubMed] [Google Scholar]
- 25.US Dept of Health and Human Services; Food and Drug Administration Guidance for industry and FDA staff: pediatric expertise for advisory panels. 2003 https://www.fda.gov/media/72451/download Accessed December 6, 2019.
- 26.Guyatt GH, Oxman AD, Kunz R et al. Going from evidence to recommendations. BMJ. 2008;336(7652):1049–1051. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The American Geriatrics Society Beers Criteria Update Expert Panel American Geriatrics Society 2015 Updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–2246. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. W64. [DOI] [PubMed] [Google Scholar]
- 29.US Food and Drug Administration FDA Pediatric Safety Communications. https://www.fda.gov/science-research/pediatrics/fda-pediatric-safety-communications Accessed January 7, 2019.
- 30.World Health Organization Model list of essential medicines for children, 7th list. 2019 https://apps.who.int/iris/bitstream/handle/10665/325772/WHO-MVP-EMP-IAU-2019.07-eng.pdf?ua=1 Accessed August 9, 2019.
- 31.Ahlfors CE. Effect of ibuprofen on bilirubin-albumin binding. J Pediatr. 2004;144(3):386–388. doi: 10.1016/j.jpeds.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 32.Desfrere L, Thibaut C, Kibleur Y et al. Unbound biliru-bin does not increase during ibuprofen treatment of patent ductus arteriosus in preterm infants. J Pediatr. 2012;160(2):258–264.e1. doi: 10.1016/j.jpeds.2011.07.014. doi: 10.1016/j.jpeds.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics Committee on Drugs “Inactive” ingredients in pharmaceutical products: update (subject review) Pediatrics. 1997;99(2):268–278. doi: 10.1542/peds.99.2.268. [DOI] [PubMed] [Google Scholar]
- 34.Nahata MC. Safety of “inert” additives or excipients in paediatric medicines. Arch Dis Child Fetal Neonatal Ed. 2009;94(6):F392–F393. doi: 10.1136/adc.2009.160192. [DOI] [PubMed] [Google Scholar]
- 35.Sharfstein JM, North M, Serwint JR. Over the counter but no longer under the radar—pediatric cough and cold medications. N Engl J Med. 2007;357(23):2321–2324. doi: 10.1056/NEJMp0707400. [DOI] [PubMed] [Google Scholar]
- 36.Kuehn BM. Debate continues over the safety of cold and cough medicines for children. JAMA. 2008;300(20):2354–2356. doi: 10.1001/jama.2008.647. [DOI] [PubMed] [Google Scholar]
- 37.Green JL, Wang GS, Reynolds KM et al. Safety profile of cough and cold medication use in pediatrics. Pediatrics. 2017;139(6) doi: 10.1542/peds.2016-3070. pii: e20163070. [DOI] [PubMed] [Google Scholar]
- 38.Jackson MA, Schutze GE, Committee on Infectious Diseases The use of systemic and topical fluoroquinolones. Pediatrics. 2016;138(5) doi: 10.1542/peds.2016-2706. pii: e20162706. [DOI] [PubMed] [Google Scholar]
- 39.Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc; 2016. Cipro (ciprofloxacin hydrochloride) [package insert] [Google Scholar]
- 40.Mogayzel PJ, Jr, Naureckas ET, Robinson KA et al. Cystic Fibrosis Foundation pulmonary guideline. pharmacologic approaches to prevention and eradication of initial Pseudomonas aeruginosa infection. Ann Am Thorac Soc. 2014;11(10):1640–1650. doi: 10.1513/AnnalsATS.201404-166OC. [DOI] [PubMed] [Google Scholar]
- 41.Bradley JS, Byington CL, Shah SS et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76. doi: 10.1093/cid/cir531. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schror K. Aspirin and Reye syndrome: a review of the evidence. Paediatr Drugs. 2007;9(3):195–204. doi: 10.2165/00148581-200709030-00008. [DOI] [PubMed] [Google Scholar]
- 43.McCrindle BW, Rowley AH, Newburger JW et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi: 10.1161/CIR.0000000000000484. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 44.Monagle P, Chan AKC, Goldenberg NA et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e737S–e801S. doi: 10.1378/chest.11-2308. doi: 10.1378/chest.11-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Monagle P, Cochrane A, Roberts R et al. A multicenter, randomized trial comparing heparin/warfarin and acetyl-salicylic acid as primary thromboprophylaxis for 2 years after the Fontan procedure in children. J Am Coll Cardiol. 2011;58(6):645–651. doi: 10.1016/j.jacc.2011.01.061. [DOI] [PubMed] [Google Scholar]
- 46.Barst RJ, Ivy DD, Gaitan G et al. A randomized, double-blind, placebo-controlled, dose-ranging study of oral sildenafil citrate in treatment-naive children with pulmonary arterial hypertension. Circulation. 2012;125(2):324–334. doi: 10.1161/CIRCULATIONAHA.110.016667. [DOI] [PubMed] [Google Scholar]
- 47.Barst RJ, Beghetti M, Pulido T et al. STARTS-2: long-term survival with oral sildenafil monotherapy in treatment-naive pediatric pulmonary arterial hypertension. Circulation. 2014;129(19):1914–1923. doi: 10.1161/CIRCULATIONAHA.113.005698. [DOI] [PubMed] [Google Scholar]
- 48.US Food and Drug Administration Suicidality in children and adolescents being treated with antidepressant medications. 2004 https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-possible-harm-exceeding-recommended-dose-over-counter-sodium Accessed December 2, 2019.
- 49.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi: 10.1001/archpsyc.63.3.332. [DOI] [PubMed] [Google Scholar]
- 50.Dopheide JA. Recognizing and treating depression in children and adolescents. Am J Health Syst Pharm. 2006;63(3):233–243. doi: 10.2146/ajhp050264. [DOI] [PubMed] [Google Scholar]
- 51.Zhang D, Chando TJ, Everett DW et al. In vitro inhibition of UDP glucuronosyltransferases by atazanavir and other HIV protease inhibitors and the relationship of this property to in vivo bilirubin glucuronidation. Drug Metab Dispos. 2005;33(11):1729–1739. doi: 10.1124/dmd.105.005447. [DOI] [PubMed] [Google Scholar]
- 52.Cooper HA. Methemoglobinemia caused by benzocaine topical spray. South Med J. 1997;90(9):946–948. doi: 10.1097/00007611-199709000-00018. [DOI] [PubMed] [Google Scholar]
- 53.Darracq MA, Daubert GP. A cyanotic toddler. Pediatr Emerg Care. 2007;23(3):195–199. doi: 10.1097/PEC.0b013e3180330a2c. [DOI] [PubMed] [Google Scholar]
- 54.Moore TJ, Walsh CS, Cohen MR. Reported adverse event cases of methemoglobinemia associated with benzo-caine products. Arch Intern Med. 2004;164(11):1192–1196. doi: 10.1001/archinte.164.11.1192. [DOI] [PubMed] [Google Scholar]
- 55.Rodriguez LF, Smolik LM, Zbehlik AJ. Benzocaine-induced methemoglobinemia: report of a severe reaction and review of the literature. Ann Pharmacother. 1994;28(5):643–649. doi: 10.1177/106002809402800515. [DOI] [PubMed] [Google Scholar]
- 56.US Food and Drug Administration Risk of serious and potentially fatal blood disorder prompts FDA action on oral over-the-counter benzocaine products used for teething and mouth pain and prescription local anesthetics. https://www.fda.gov/drugs/drug-safety-and-availability/risk-serious-and-potentially-fatal-blood-disorder-prompts-fda-action-oral-over-counter-benzocaine Accessed December 4, 2019.
- 57.US Food and Drug Administration Reports of a rare, but serious and potentially fatal adverse effect with the use of over-the-counter (OTC) benzocaine gels and liquids applied to the gums or mouth. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-reports-rare-serious-and-potentially-fatal-adverse-effect-use-over Accessed December 4, 2019.
- 58.American Academy of Pediatrics: Committee on Drugs: camphor: who needs it? Pediatrics. 1978;62(3):404–406. [PubMed] [Google Scholar]
- 59.Camphor revisited: focus on toxicity: Committee on Drugs: American Academy of Pediatrics. Pediatrics. 1994;94(1):127–128. [PubMed] [Google Scholar]
- 60.Love JN, Sammon M, Smereck J. Are one or two dangerous?: camphor exposure in toddlers. J Emerg Med. 2004;27(1):49–54. doi: 10.1016/j.jemermed.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 61.US Food and Drug Administration Carbinoxamine products: enforcement action dates. 2006 Jun 9; https://www.federalregister.gov/documents/2006/06/09/E6-9033/carbinoxamine-products-enforcement-action-dates Accessed April 29, 2019.
- 62.Donnelly PC, Sutich RM, Easton R et al. Ceftriaxone-associated biliary and cardiopulmonary adverse events in neonates: a systematic review of the literature. Paediatr Drugs. 2017;19(1):21–34. doi: 10.1007/s40272-016-0197-x. [DOI] [PubMed] [Google Scholar]
- 63.Martin E, Fanconi S, Kalin P et al. Ceftriaxone-bilirubin-albumin interactions in the neonate: an in vivo study. Eur J Pediatr. 1993;152(6):530–534. doi: 10.1007/BF01955067. [DOI] [PubMed] [Google Scholar]
- 64.Evans LS, Kleiman MB. Acidosis as a presenting feature of chloramphenicol toxicity. J Pediatr. 1986;108(3):475–477. doi: 10.1016/s0022-3476(86)80905-2. [DOI] [PubMed] [Google Scholar]
- 65.Neri I, Ravaioli GM, Faldella G et al. Chlorhexidine-induced chemical burns in very low birth weight infants. J Pediatr. 2017;191:262–265.e2. doi: 10.1016/j.jpeds.2017.08.002. doi: 10.1016/j.jpeds.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 66.US Food and Drug Administration FDA Drug Safety Communication: FDA restricts use of prescription codeine pain and cough medicines and tramadol pain medicines in children; recommends against use in breastfeeding women. 2017 Apr 20; https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-restricts-use-prescription-codeine-pain-and-cough-medicines-and Accessed April 29, 2019.
- 67.Tobias JD, Green TP, Cote CJ. Section on Anesthesiology and Pain Medicine; Committee On Drugs. Codeine: time to say “no”. Pediatrics. 2016;138(4) doi: 10.1542/peds.2016-2396. doi:10.1542/peds.2016–2396. [DOI] [PubMed] [Google Scholar]
- 68.Voronov P, Przybylo HJ, Jagannathan N. Apnea in a child after oral codeine: a genetic variant – an ultra-rapid metabolizer. Paediatr Anaesth. 2007;17(7):684–687. doi: 10.1111/j.1460-9592.2006.02182.x. [DOI] [PubMed] [Google Scholar]
- 69.US Food and Drug Administration FDA Drug Safety Communication: FDA requires labeling changes for prescription opioid cough and cold medicines to limit their use to adults 18 years and older. 2018 Jan 11; https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-requires-labeling-changes-prescription-opioid-cough-and-cold Accessed October 14, 2019.
- 70.US Department of Health and Human Services Guidelines for the use of antiretroviral agents in pediatric HIV infection, darunavir. https://aidsinfo.nih.gov/guidelines/html/2/pediatric-arv/129/darunavir Accessed April 29, 2019.
- 71.Cubicin (daptomycin) [package insert] Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2018. [Google Scholar]
- 72.Wadsworth SJ, Suh B. In vitro displacement of bilirubin by antibiotics and 2-hydroxybenzoylglycine in newborns. Antimicrob Agents Chemother. 1988;32(10):1571–1575. doi: 10.1128/aac.32.10.1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Williams J, Watkins-Jones R. Dicyclomine: worrying symptoms associated with its use in some small babies. Br Med J (Clin Res Ed) 1984;288(6421):901. doi: 10.1136/bmj.288.6421.901. doi:10.1136/bmj.288.6421.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Birnbaum AD, Jiang Y, Tessler HH, Goldstein DA. Elevation of intraocular pressure in patients with uveitis treated with topical difluprednate. Arch Ophthalmol. 2011;129(5):667–668. doi: 10.1001/archophthalmol.2011.82. [DOI] [PubMed] [Google Scholar]
- 75.Slabaugh MA, Herlihy E, Ongchin S, van Gelder RN. Efficacy and potential complications of difluprednate use for pediatric uveitis. Am J Ophthalmol. 2012;153(5):932–938. doi: 10.1016/j.ajo.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 76.Freese B, Medawar C, Herxheimer A. No more lomotil for infants. Lancet. 1981;2(8250):816–817. doi: 10.1016/s0140-6736(81)90238-5. [DOI] [PubMed] [Google Scholar]
- 77.Ayd FJ., Jr. A survey of drug-induced extrapyramidal reactions. JAMA. 1961;175:1054–1060. doi: 10.1001/jama.1961.03040120016004. [DOI] [PubMed] [Google Scholar]
- 78.Merchan-Naranjo J, Tapia C, Bailon C et al. Secondary effects of antipsychotic treatment in naive or quasi-naive children and adolescents: design of a follow-up protocol and baseline results. Rev Psiquiatr Salud Ment. 2012;5(4):217–228. doi: 10.1016/j.rpsm.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 79.Bateman DN, Rawlins MD, Simpson JM. Extrapyramidal reactions to prochlorperazine and haloperidol in the United Kingdom. Q J Med. 1986;59(230):549–556. [PubMed] [Google Scholar]
- 80.Aguilar EJ, Keshavan MS, Martinez-Quiles MD et al. Predictors of acute dystonia in first-episode psychotic patients. Am J Psychiatry. 1994;151(12):1819–1821. doi: 10.1176/ajp.151.12.1819. [DOI] [PubMed] [Google Scholar]
- 81.Casteels-Van Daele M, Jaeken J, Van der Schueren P, Van den Bon P. Dystonic reactions in children caused by metoclopramide. Arch Dis Child. 1970;45(239):130–133. doi: 10.1136/adc.45.239.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bateman DN, Craft AW, Nicholson E, Pearson AD. Dystonic reactions and the pharmacokinetics of metoclopramide in children. Br J Clin Pharmacol. 1983;15(5):557–559. doi: 10.1111/j.1365-2125.1983.tb02090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bateman DN, Darling WM, Boys R, Rawlins MD. Extrapyra-midal reactions to metoclopramide and prochlorperazine. Q J Med. 1989;71(264):307–311. [PubMed] [Google Scholar]
- 84.Yis U, Ozdemir D, Duman M, Unal N. Metoclopramide induced dystonia in children: two case reports. Eur J Emerg Med. 2005;12(3):117–119. doi: 10.1097/00063110-200506000-00004. [DOI] [PubMed] [Google Scholar]
- 85.Karimi Khaledi M, Suda KJ, Shelton CM. Tardive dyskine-sia after short-term treatment with oral metoclopramide in an adolescent. Int J Clin Pharm. 2012;34(6):822–824. doi: 10.1007/s11096-012-9685-4. [DOI] [PubMed] [Google Scholar]
- 86.Eras Z, Oguz SS, Dilmen U. Is metoclopramide safe for the premature infant? Eur Rev Med Pharmacol Sci. 2013;17(12):1655–1657. [PubMed] [Google Scholar]
- 87.Ernst M, Gonzalez NM, Campbell M. Acute dystonic reaction with low-dose pimozide. J Am Acad Child Adolesc Psychiatry. 1993;32(3):640–642. doi: 10.1097/00004583-199305000-00022. [DOI] [PubMed] [Google Scholar]
- 88.Research Triangle Park, NC: GlaxoSmithKline; 2004. Compazine (prochlorperazine maleate) [package insert] [Google Scholar]
- 89.Lau Moon Lin M, Robinson PD et al. The safety of prochlorperazine in children: a systematic review and meta-analysis. Drug Saf. 2016;39(6):509–516. doi: 10.1007/s40264-016-0398-9. [DOI] [PubMed] [Google Scholar]
- 90.Muniz AE. Prochlorperazine-induced extrapyramidal effects mimicking meningitis in a child. South Med J. 2000;93(6):629–630. [PubMed] [Google Scholar]
- 91.Phenergan (promethazine HCl) [package insert] Philadelphia, PA: Wyeth; 2004. [Google Scholar]
- 92.Starke PR, Weaver J, Chowdhury BA. Boxed warning added to promethazine labeling for pediatric use. N Engl J Med. 2005;352(25):2653. doi: 10.1056/NEJM200506233522522. doi: 10.1056/NEJM200506233522522. [DOI] [PubMed] [Google Scholar]
- 93.Kahn A, Blum D. Phenothiazines and sudden infant death syndrome. Pediatrics. 1982;70(1):75–78. [PubMed] [Google Scholar]
- 94.Tigan (trimethobenzamide hydrochloride) [package insert] New York, NY: Pfizer Inc; 2017. [Google Scholar]
- 95.Binenbaum G, Bruno CJ, Forbes BJ et al. Periocular ulcerative dermatitis associated with gentamicin ointment prophylaxis in newborns. J Pediatr. 2010;156(2):320–321. doi: 10.1016/j.jpeds.2009.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Merlob P, Metzker A. Neonatal orbital irritant contact dermatitis caused by gentamicin ointment. Cutis. 1996;57(6):429–430. [PubMed] [Google Scholar]
- 97.Nathawad R, Mendez H, Ahmad A et al. Severe ocular reactions after neonatal ocular prophylaxis with gentamicin ophthalmic ointment. Pediatr Infect Dis J. 2011;30(2):175–176. doi: 10.1097/INF.0b013e3181f6c2e5. [DOI] [PubMed] [Google Scholar]
- 98.Robertson AF. Reflections on errors in neonatology, II: the “heroic” years, 1950 to 1970. J Perinatol. 2003;23(2):154–161. doi: 10.1038/sj.jp.7210843. [DOI] [PubMed] [Google Scholar]
- 99.US Dept of Health and Human Services Guidelines for the use of antiretroviral agents in pediatric HIV infection, archived drugs, indinavir. 2018 https://aidsinfo.nih.gov/guidelines/html/2/pediatric-arv/131/indinavir Accessed February 3, 2020.
- 100.Brooks PA, Grace RF. Ivermectin is better than benzyl benzoate for childhood scabies in developing countries. J Paediatr Child Health. 2002;38(4):401–404. doi: 10.1046/j.1440-1754.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- 101.American Academy of Pediatrics . Cutaneous larva migrans. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red Book: 2018 Report of the Committee on Infectious Diseases. 31st ed. Vol. 2018. Elk Grove Village, IL: American Academy of Pediatrics; pp. 307–308. [Google Scholar]
- 102.Lamictal (lamotrigine) [package insert] Research Triangle Park, NC: GlaxoSmithKline; 2018. [Google Scholar]
- 103.US Food and Drug Administration FDA Drug Safety Communication: FDA recommends not using lidocaine to treat teething pain and requires new Boxed Warning. 2014 Jun 26; https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-recommends-not-using-lidocaine-treat-teething-pain-and-requires Accessed April 29, 2019.
- 104.Curtis LA, Dolan TS, Seibert HE. Are one or two dangerous?: lidocaine and topical anesthetic exposures in children. J Emerg Med. 2009;37(1):32–39. doi: 10.1016/j.jemermed.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 105.Linzess (linaclotide) [package insert] Irvine, CA: Allergan USA Inc; 2017. [Google Scholar]
- 106.Friedman SJ. Lindane neurotoxic reaction in nonbullous congenital ichthyosiform erythroderma. Arch Dermatol. 1987;123(8):1056–1058. [PubMed] [Google Scholar]
- 107.Frankowski BL, Bocchini JA., Jr Council on School Health and Committee on Infectious Diseases. Head lice. Pediatrics. 2010;126(2):392–403. doi: 10.1542/peds.2010-1308. [DOI] [PubMed] [Google Scholar]
- 108.Li ST, Grossman DC, Cummings P. Loperamide therapy for acute diarrhea in children: systematic review and meta-analysis. PLoS Med. 2007;4(3):e98. doi: 10.1371/journal.pmed.0040098. doi:10.1371/journal.pmed.0040098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Eberly MD, Eide MB, Thompson JL, Nylund CM. Azithromycin in early infancy and pyloric stenosis. Pediatrics. 2015;135(3):483–488. doi: 10.1542/peds.2014-2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nair V, Loganathan P, Soraisham AS. Azithromycin and other macrolides for prevention of bronchopulmonary dysplasia: a systematic review and meta-analysis. Neonatology. 2014;106(4):337–347. doi: 10.1159/000363493. [DOI] [PubMed] [Google Scholar]
- 111.American Academy of Pediatrics . Pertussis (whooping cough) In: Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red Book: 2018 Report of the Committee on Infectious Diseases. 31st ed. Elk Grove Village, IL: American Academy of Pediatrics; 2018. pp. 620–634. [Google Scholar]
- 112.Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Chlamydia trachomatis. Red Book: 2018 Report of the Committee on Infectious Diseases. 31st ed. Elk Grove Village, IL: American Academy of Pediatrics; 2018. pp. 276–283. [Google Scholar]
- 113.Ovide 0.5% (malathion) [package insert] Hawthorne, NY: TaroPharma; 2011. [Google Scholar]
- 114.Kumar P, Denson SE, Mancuso TJ, Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125(3):608–615. doi: 10.1542/peds.2009-2863. [DOI] [PubMed] [Google Scholar]
- 115.Committee on Practice Bulletins-Obstetrics. Practice bulletin no. 177: obstetric analgesia and anesthesia. Obstet Gynecol. 2017;129(4):e73–e89. doi: 10.1097/AOG.0000000000002018. doi: 10.1097/AOG.0000000000002018. [DOI] [PubMed] [Google Scholar]
- 116.Anand KJ, Barton BA, McIntosh N et al. Analgesia and sedation in preterm neonates who require ventilatory support: results from the NOPAIN trial: Neonatal Outcome and Prolonged Analgesia in Neonates. Arch Pediatr Adolesc Med. 1999;153(4):331–338. doi: 10.1001/archpedi.153.4.331. [DOI] [PubMed] [Google Scholar]
- 117.Ikeda K. Oil aspiration pneumonia (lipoid pneumonia): clinical, pathologic and experimental consideration. Am J Dis Child. 1935;49(4):985–1006. [Google Scholar]
- 118.Gibbs J, Newson T, Williams J, Davidson DC. Nal-oxone hazard in infant of opioid abuser. Lancet. 1989;2(8655):159–160. doi: 10.1016/s0140-6736(89)90214-6. [DOI] [PubMed] [Google Scholar]
- 119.Perlman JM, Wyllie J, Kattwinkel J et al. Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics. 2010;126(5):e1319–e1344. doi: 10.1542/peds.2010-2972B. doi: 10.1542/peds.2010-2972B. [DOI] [PubMed] [Google Scholar]
- 120.Zao J, Koren G, Bozzo P. Using nitrofurantoin while breast-feeding a newborn. Can Fam Physician. 2014;60(6):539–540. [PMC free article] [PubMed] [Google Scholar]
- 121.Nordeng H, Lupattelli A, Romoren M, Koren G. Neonatal outcomes after gestational exposure to nitrofurantoin. Obstet Gynecol. 2013;121(2, pt 1):306–313. doi: 10.1097/AOG.0b013e31827c5f88. [DOI] [PubMed] [Google Scholar]
- 122.Correll CU, Manu P, Olshanskiy V et al. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA. 2009;302(16):1765–1773. doi: 10.1001/jama.2009.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hudak ML, Tan RC, Commitee on Drugs; Committee on Fetus and Newborn; American Academy of Pediatrics Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540–e560. doi: 10.1542/peds.2011-3212. doi: 10.1542/peds.2011-3212. [DOI] [PubMed] [Google Scholar]
- 124.Trulance (plecanatide) [package insert] New York, NY: Synergy Pharmaceuticals Inc; 2018. [Google Scholar]
- 125.Kam PC, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007;62(7):690–701. doi: 10.1111/j.1365-2044.2007.05055.x. [DOI] [PubMed] [Google Scholar]
- 126.Krajcova A, Waldauf P, Andel M, Duska F. Propofol infusion syndrome: a structured review of experimental studies and 153 published case reports. Crit Care. 2015;19:398. doi: 10.1186/s13054-015-1112-5. doi:10/1186/s13054-015-1112–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Walli A, Poulsen TD, Dam M, Borglum J. Propofol infusion syndrome in refractory status epilepticus: a case report and topical review. Case Rep Emerg Med. 2016;2016 doi: 10.1155/2016/3265929. 3265929. doi: 10.1155/2016/3265929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kaye AD, Fox CJ, Padnos IW et al. Pharmacologic considerations of anesthetic agents in pediatric patients: a comprehensive review. Anesthesiol Clin. 2017;35(2):e73–e94. doi: 10.1016/j.anclin.2017.01.012. doi: 10.1016/j.anclin.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 129.Vasile B, Rasulo F, Candiani A, Latronico N. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med. 2003;29(9):1417–1425. doi: 10.1007/s00134-003-1905-x. [DOI] [PubMed] [Google Scholar]
- 130.Brophy GM, Bell R, Claassen J et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- 131.Davis DL, Buffler P. Reduction of deaths after drug labelling for risk of Reye's syndrome. Lancet. 1992;340(8826):1042. doi: 10.1016/0140-6736(92)93058-u. doi:10.1016/0140–6736(92)93058–u. [DOI] [PubMed] [Google Scholar]
- 132.Belay ED, Bresee JS, Holman RC et al. Reye's syndrome in the United States from 1981 through 1997. N Engl J Med. 1999;340(18):1377–1382. doi: 10.1056/NEJM199905063401801. [DOI] [PubMed] [Google Scholar]
- 133.Centers for Disease Control and Prevention Surgeon general's advisory on the use of salicylates and Reye syndrome. MMWR Morb Mortal Wkly Rep. 1982;31(22):289–290. [PubMed] [Google Scholar]
- 134.Centers for Disease Control and Prevention National surveillance for Reye syndrome, 1981: update, Reye syndrome and salicylate usage. MMWR Morb Mortal Wkly Rep. 1982;31(5):53–56. 61. [PubMed] [Google Scholar]
- 135.Martin RR, Lisehora GR, Braxton M, Jr, Barcia PJ. Fatal poisoning from sodium phosphate enema: case report and experimental study. JAMA. 1987;257(16):2190–2192. [PubMed] [Google Scholar]
- 136.US Food and Drug Administration FDA Drug Safety Communication: FDA warns of possible harm from exceeding recommended dose of over-the-counter sodium phosphate products to treat constipation. 2014 Jan 8; https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-possible-harm-exceeding-recommended-dose-over-counter-sodium Accessed April 29, 2019.
- 137.Bennett LN, Myers TF, Lambert GH. Cecal perforation associated with sodium polystyrene sulfonate-sorbitol enemas in a 650 gram infant with hyperkalemia. Am J Perinatol. 1996;13(3):167–170. doi: 10.1055/s-2007-994318. [DOI] [PubMed] [Google Scholar]
- 138.Rugolotto S, Gruber M, Solano PD et al. Necrotizing enterocolitis in a 850 gram infant receiving sorbitol-free sodium polystyrene sulfonate (Kayexalate): clinical and histopathologic findings. J Perinatol. 2007;27(4):247–249. doi: 10.1038/sj.jp.7211677. [DOI] [PubMed] [Google Scholar]
- 139.Silvadene cream 1% (silver sulfadiazene) [package insert] New York, NY: Pfizer Inc; 2016. [Google Scholar]
- 140.Bactrim (sulfamethoxazole and trimethoprim) [package insert] Philadelphia, PA: Mutual Pharmaceutical Company Inc; 2013. [Google Scholar]
- 141.Cohlan S, Bevelander G, Tiamsic T. Growth inhibition of prematures receiving tetracycline: a clinical and laboratory investigation of tetracycline-induced bone fluorescence. Am J Dis Child. 1963;105(5):453–461. [Google Scholar]
- 142.Hamp SE. The tetracyclines and their effect on teeth: a clinical study. Odontol Tidskr. 1967;75(1):33–49. [PubMed] [Google Scholar]
- 143.Demers P, Fraser D, Goldbloom RB et al. Effects of tetracyclines on skeletal growth and dentition: a report by the Nutrition Committee of the Canadian Paediatric Society. Can Med Assoc J. 1968;99(17):849–854. [PMC free article] [PubMed] [Google Scholar]
- 144.Conchie JM, Munroe JD, Anderson DO. The incidence of staining of permanent teeth by the tetracyclines. Can Med Assoc J. 1970;103(4):351–356. [PMC free article] [PubMed] [Google Scholar]
- 145.American Academy of Pediatrics Committee on drugs: requiem for tetracyclines. Pediatrics. 1975;55(1):142–143. [PubMed] [Google Scholar]
- 146.Cohlan SQ. Tetracycline staining of teeth. Teratology. 1977;15(1):127–129. doi: 10.1002/tera.1420150117. [DOI] [PubMed] [Google Scholar]
- 147.Grossman ER, Walchek A, Freedman H. Tetracyclines and permanent teeth: the relation between dose and tooth color. Pediatrics. 1971;47(3):567–570. [PubMed] [Google Scholar]
- 148.Tempark T, Phatarakijnirund V, Chatproedprai S et al. Exogenous Cushing's syndrome due to topical cortico-steroid application: case report and review literature. Endocrine. 2010;38(3):328–334. doi: 10.1007/s12020-010-9393-6. [DOI] [PubMed] [Google Scholar]
- 149.Bulus AD, Andiran N, Kocak M. Cushing's syndrome: hidden risk in usage of topical corticosteroids. J Pediatr Endocrinol Metab. 2014;27(9–10):977–981. doi: 10.1515/jpem-2013-0262. [DOI] [PubMed] [Google Scholar]
- 150.US Food and Drug Administration FDA Drug Safety Communication: FDA evaluating the risks of using the pain medicine tramadol in children aged 17 and younger. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-evaluating-risks-using-pain-medicine-tramadol-children-aged-17-and Accessed December 4, 2019.
- 151.Varley CK. Sudden death related to selected tricyclic an-tidepressants in children: epidemiology, mechanisms and clinical implications. Paediatr Drugs. 2001;3(8):613–627. doi: 10.2165/00128072-200103080-00006. [DOI] [PubMed] [Google Scholar]
- 152.Amitai Y, Frischer H. Excess fatality from desipramine in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2006;45(1):54–60. doi: 10.1097/01.chi.0000184931.26176.4a. [DOI] [PubMed] [Google Scholar]
- 153.Vetter VL, Elia J, Erickson C et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactiv-ity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117(18):2407–2423. doi: 10.1161/CIRCULATIONAHA.107.189473. [DOI] [PubMed] [Google Scholar]
- 154.Willmore LJ, Wilder BJ, Bruni J, Villarreal HJ. Effect of valproic acid on hepatic function. Neurology. 1978;28(9, pt 1):961–964. doi: 10.1212/wnl.28.9.961. [DOI] [PubMed] [Google Scholar]
- 155.Star K, Edwards IR, Choonara I. Valproic acid and fatalities in children: a review of individual case safety reports in VigiBase. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0108970. e108970. doi:10.1371/journal.pone.0108970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Melexopoulou C, Marinaki S, Darema M et al. Valproate-induced hyperammonemic encephalopathy in a renal transplanted patient. Ren Fail. 2014;36(6):955–956. doi: 10.3109/0886022X.2014.900423. [DOI] [PubMed] [Google Scholar]
- 157.Abinader E, Borochowitz Z, Berger A. A hemodynamic complication of verapamil therapy in a neonate. Helv Paediatr Acta. 1981;36(5):451–455. [PubMed] [Google Scholar]
- 158.Epstein ML, Kiel EA, Victorica BE. Cardiac decompensation following verapamil therapy in infants with supra-ventricular tachycardia. Pediatrics. 1985;75(4):737–740. [PubMed] [Google Scholar]
- 159.Lapage MJ, Bradley DJ, Dick M., 2nd. Verapamil in infants: an exaggerated fear? Pediatr Cardiol. 2013;34(7):1532–1534. doi: 10.1007/s00246-013-0739-8. [DOI] [PubMed] [Google Scholar]
- 160.Benzyl alcohol: toxic agent in neonatal units. Pediatrics. 1983;72(3):356–358. [PubMed] [Google Scholar]
- 161.Gershanik J, Boecler B, Ensley H et al. The gasping syndrome and benzyl alcohol poisoning. N Engl J Med. 1982;307(22):1384–1388. doi: 10.1056/NEJM198211253072206. [DOI] [PubMed] [Google Scholar]
- 162.Brown WJ, Buist NR, Gipson HT et al. Fatal benzyl alcohol poisoning in a neonatal intensive care unit. Lancet. 1982;1(8283):1250. doi: 10.1016/s0140-6736(82)92377-7. doi: 10.1016/s0140-6736(82)92377-7. [DOI] [PubMed] [Google Scholar]
- 163.Hiller JL, Benda GI, Rahatzad M et al. Benzyl alcohol toxicity: impact on mortality and intraventricular hemorrhage among very low birth weight infants. Pediatrics. 1986;77(4):500–506. [PubMed] [Google Scholar]
- 164.Committee on Drugs Ethanol in liquid preparations intended for children. Pediatrics. 1984;73(3):405–407. [PubMed] [Google Scholar]
- 165.Weintraub Z, Iancu TC. Isopropyl alcohol burns. Pediatrics. 1982;69(4):506. [PubMed] [Google Scholar]
- 166.Schick JB, Milstein JM. Burn hazard of isopropyl alcohol in the neonate. Pediatrics. 1981;68(4):587–588. [PubMed] [Google Scholar]
- 167.Rasmussen LF, Ahlfors CE, Wennberg RP. The effect of paraben preservatives on albumin binding of bilirubin. J Pediatr. 1976;89(3):475–478. doi: 10.1016/s0022-3476(76)80557-4. [DOI] [PubMed] [Google Scholar]
- 168.Cederbaum S. Phenylketonuria: an update. Curr Opin Pediatr. 2002;14(6):702–706. doi: 10.1097/00008480-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 169.Bove KE, Kosmetatos N, Wedig KE et al. Vasculopathic hepatotoxicity associated with E-Ferol syndrome in low-birth-weight infants. JAMA. 1985;254(17):2422–2430. [PubMed] [Google Scholar]
- 170.Balistreri WF, Farrell MK, Bove KE. Lessons from the E-Ferol tragedy. Pediatrics. 1986;78(3):503–506. [PubMed] [Google Scholar]
- 171.Centers for Disease Control and Prevention Unusual syndrome with fatalities among premature infants: association with a new intravenous vitamin E product. MMWR Morb Mortal Wkly Rep. 1984;33(14):198–199. [PubMed] [Google Scholar]
- 172.MacDonald MG, Getson PR, Glasgow AM et al. Propylene glycol: increased incidence of seizures in low birth weight infants. Pediatrics. 1987;79(4):622–625. [PubMed] [Google Scholar]
- 173.Allegaert K, Vanhaesebrouck S, Kulo A et al. Prospective assessment of short-term propylene glycol tolerance in neonates. Arch Dis Child. 2010;95(12):1054–1058. doi: 10.1136/adc.2010.190330. [DOI] [PubMed] [Google Scholar]