Abstract
We developed a novel concept that allows to considerably improve the performance of conventionally used filtering-facepiece respirators against fine and ultrafine aerosols including airborne viral and bacterial agents. The concept is based on the continuous emission of unipolar ions. The effect was evaluated through the real-time monitoring of the concentration and size distribution of fine and ultrafine aerosol particles. The measurements were conducted inside and outside of a respiratory mask that was face sealed on a breathing manikin. A commonly used Type N95 respirator and surgical mask were utilized for the tests. The manikin was placed in a 24.3-m3 indoor test chamber and exposed to polydisperse surrogate aerosols simulating viral and bacterial particles with respect to the aerodynamic size. The particle penetration through the mask was found to decrease by one-to-two orders of magnitude as a result of continuous unipolar ion emission in the chamber. The flux of air ions migrated to the breathing zone and imparted electrical charges of the same polarity to the aerosol particles and the respirator filter surface. This created an electrostatic shield along the external surface of the filter, thus enhancing the protection characteristics provided by the respirator. The above performance enhancement effect is crucial for minimizing the infectious risk in the cases when the conventional filtering-facepiece respirators are not able to provide an adequate protection against airborne viruses and bacteria.
Keywords: Filter, Respiratory protection, Mask, Particle charge, Ion emission
1. Introduction
The outbreaks of emerging diseases (e.g., SARS) and the threat of bioterrorism have triggered an urgent demand for adequate respiratory protection against bioaerosol agents, including airborne viruses and bacteria. Particular interest has been directed towards increasing the efficiency of existing respiratory protection devices.
The filtering-facepiece masks, including Type N95 respirators, are frequently used in indoor air environments to prevent or considerably reduce inhalation of droplet nuclei that can potentially carry viable microorganisms. Millions of workers, including health-care personnel, routinely use respirators in their workplaces (United States Department of Labor, 1995). In case of bioterrorist attack in a major urban area, there may be a need in millions readily available respiratory protection devices. The existing respirators have been extensively evaluated against fine particles (e.g., Brosseau, Evans, Ellenbecker, & Feldstein, 1989; Chen, Ruuskanen, Pilacinski, & Willeke, 1990; Chen & Willeke, 1992; Huang, Willeke, Qian, Grinshpun, & Ulevicius, 1998; Johnston, Myers, Colton, Birkner, & Campbell, 2001; Qian, Willeke, Grinshpun, Donnelly, & Coffey, 1998; Halvorsen, 1998) and microorganisms (Centers for Disease Control and Prevention, 1994; Lee, Slavcev, & Nicas, 2004a; Qian, Willeke, Grinshpun, & Donnelly, 1997; Qian et al., 1998; Reponen, Wang, Willeke, & Grinshpun, 1999; Willeke, Qian, Donnelly, Grinshpun, & Ulevicius, 1996). At the same time, the protection efficiency of existing facepiece respirators have not been well characterized with respect to ultrafine particles, i.e. those below 0.1 μm (Hinds, 1999).
The respirators differ from one another by their filtration efficiency, which is dependent on the filter properties and the particle size. For example, a Type N95 respirator may allow up to 5% penetration in “a worst case scenario,” when most-penetrating sodium chloride particles of 0.3 μm mass median aerodynamic diameter are drawn through the filter at a flow rate of 85 l min−1 (Federal Register, 1995). The penetration efficiency of larger Mycobacterium tuberculosis bacteria (Mtb, 0.8 μm) through a face-sealed N95 respirator at strenuous workload is as low as about 0.5% (Qian et al., 1998). The face-sealed filter of a conventional health-care mask, which ensures relatively low pressure drop and consequently good comfort level, allows approximately 15% of airborne Mtb surrogate bacteria to penetrate, thus providing 85% protection against these bacteria (Willeke et al., 1996).
If the bacterial concentration in the air is 1000 m−3, an unprotected individual breathing at 30 l min−1 inhales 1800 microorganisms per hour, whereas the one wearing a perfectly fit N95 respirator inhales up to 90 microorganisms per hour. If the infectious dose of a bioaerosol agent of interest is less than 90, the N95 respirator may not provide an adequate respiratory protection once the exposure time exceeds one hour. The use of an improperly fit-tested tight-fitting respirator may further decrease the respiratory protection level because of the additional particle penetration that occurs through the face-seal leaks (Chen et al., 1990; Chen & Willeke, 1992; Oestenstad, Dillion, & Perkins, 1990a; Oestenstad, Perkins, & Rose, 1990b). Based on the above considerations, it seems very useful if the filtration efficiency of existing respirators can be increased while the comfort level provided by these devices would remain the same.
With respect to the respiratory exposure and protection, the particle aerodynamic diameter range of d a∼0.04–2 μm is of special public interest because of its health relevance. Many bioaerosol agents, including viruses and bacteria that cause emerging diseases as well as those that can be used for biological warfare or in the event of bioterrorism, belong to this size range. For example, according to the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov), the dimension of the coronavirus virion (the etiological agent of the SARS) are (60–120)×(160–200) nm, which corresponds to da∼0.1 μm. For Bacillus anthracis (bacteria causing anthrax), da∼1 μm. As the above range is broad and includes both the fine and ultrafine particle fractions (Baron & Willeke, 2001; Hinds, 1999), the particle penetration efficiency through the filter media can be affected by several mechanisms and is generally characterized by the particle aerodynamic size. This allows testing the performance of respirator filters against pathogenic agents using non-pathogenic aerosol surrogates that simulate the aerodynamic characteristics of the particles of interest.
In this study, we developed and evaluated a novel concept that drastically enhances the performance of conventional filtering-facepiece respirators against fine and ultrafine aerosol particles. The concept is based on the continuous emission of unipolar ions into the air in the vicinity of the respirator. The aerosol particles are unipolarly charged by air ions primarily due to the diffusion charging mechanism (Adachi, Kousaka, & Okuyama, 1985; Frank, Cederfelt, & Martinsson, 2004; Hernandez-Sierra, Alguacil, & Alonso, 2003; Wiedensohler et al., 1994). The ion-filter interaction and the deposition of unipolarly charged particles on the external surface of the filter impose significant unipolar charge on the filter. This creates a shield for the incoming particles (as they carry charges of the same polarity), which decreases the penetration efficiency through the filter.
2. Experimental measurements
The new concept was experimentally evaluated in a non-occupied, unventilated indoor test chamber (L×W×H=3.78 m×2.44 m×2.64 m=24.3 m3). This facility, developed in the Center for Health-Related Aerosol Studies at the University of Cincinnati, has been used in our previous studies (Choe et al., 2000; Grinshpun, Choe, Trunov, Willeke, Menrath, & Friedman 2002, Grinshpun, Adhikari, Lee, Trunov, Mainelis, Yermakov, & Reponen 2004).
The experimental setup is schematically shown in Fig. 1. A breathing manikin with a face-sealed respiratory mask was exposed to the airborne polydisperse surrogate aerosols that simulated viral and bacterial particles with respect to their aerodynamic size. The leakage tests were conducted between the mask and the face of the manikin with a bubble-producing liquid (Trubble Bubble, New Jersey Meter Co., Paterson, NJ, USA). The manikin operated at a breathing flow rate, 30 l min−1, representing human breathing during light workloads (Mineral Resources, 1994; Johnson, Weiss, & Grove, 1992).
Fig. 1.
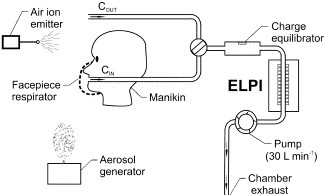
Schematics of the experimental setup.
The electrical low pressure impactor (ELPI, TSI Inc./Dekati Ltd., St. Paul, MN, USA) was used to determine the concentration and aerodynamic particle size distribution in real-time. This instrument utilizes the cascade impaction principle and—in addition—has a direct-reading capability. The aerosol particles are charged by the corona charger downstream of the ELPI inlet and subsequently detected by the electrometers inside the cascade impactor.
The particles were collected by the ELPI inside and outside the respirator using identical sampling lines. For these measurements, a 10-mCi Kr85 charge equilibrator (3M Company, St. Paul, MN, USA) was installed upstream of the ELPI inlet to neutralize the particles to Boltzmann charge equilibrium. This allowed us to avoid the influence of high electric charges, imparted by the particles as a result of their interaction with air ions, on the ELPI performance. The time resolution of the instrument was adjusted to 10 s. The data were recorded in 12 ELPI channels (each channel=impaction stage), from 0.04 to 8.4 μm. The latter sizes represent the midpoint diameters of the first and the 12th impaction stages (the midpoint=the geometric mean of the stage's boundaries).
The natural aerosol concentration in the indoor test chamber was not sufficient, particularly for the measurement inside the mask, because the filter removed considerable number of ambient airborne particles. To increase the initial background aerosol concentration, we used a smoke generator. The smoke particles covered primarily the submicrometer aerodynamic size range (Cheng, Bechtold, Yu, & Hung, 1995) with a sharp decrease in the particle number at d a>1.5–2 μm. Thus, the data recorded in the first 8 measurement channels of the ELPI (da=0.04–1.3 μm) were used for the analysis.
The measured aerosol concentrations inside (C IN) and outside (C OUT) the mask were incorporated into the equation for the respirator penetration efficiency, E p:
| Ep=CINCOUT, | (1) |
which was determined as a function of the particle aerodynamic diameter. E P is actually the inversed protection factor that is frequently used as a respirator performance index.
Initially, the background tests were conducted by measuring the penetration efficiency of the mask with no ion emission. Then, a unipolar ion emitter was turned on at a distance of 20 cm from the mask, and E p(d a) was determined in 3-min time intervals during 12 min. The continuous air ion emission in the chamber decreased C OUT as the particles, charged by ions to the same polarity, repelled and subsequently migrated toward the chamber's walls and deposited on these walls (Grinshpun et al., 2004). The change in the C OUT-value that occurred during each 3-min time interval due to ionic air purification in the chamber was taken into account through the linear interpolation of C OUT(t).
In this study, we used a negative ion emitter (VI-2500, Wein, Inc., Los Angeles, CA, USA) producing an air ion concentration of N i∼1.3×106 elementary charges per cm3 as determined at a distance of 1 m from the source. The ion concentration was measured by the Air Ion Counter (AlphaLab Inc., Salt Lake city, UT, USA) that operates within the range of 10 – 2×106 ions per cm3.
Two types of filtering-facepiece respiratory masks commercially available from a major manufacturer were tested in this study. One was the NIOSH (US National Institute for Occupational Safety and Health) certified N95 respirator and the other one was a conventional disposable surgical mask. The N95 respirator consists of inner and outer cover webs made of rayon. Its filter made of polyester and polypropylene with the electrostatically charged microfibers providing relatively high filtering efficiency. In the surgical mask, the polypropylene filter is sandwiched between inner and outer webs made of rayon. The filter of a surgical mask has lower filtration efficiency as compared to the one of an N95 respirator. Thus, the effect of ion emission on the respirator filter efficiency was tested for the masks having two distinctly different original performance characteristics.
The average values and the standard deviations of the penetration efficiency were calculated for each set of conditions as a result of at least three replicates. The data were statistically analyzed using the Microsoft Excel software package (Microsoft Co., Redmond, WA, USA).
3. Results
Fig. 2 shows the normalized initial aerosol concentration measured outside the respirator mask. Each data point represents an average of six replicates. It is seen that the aerosol particles were primarily within a range of d a≈0.04–0.5 μm (the concentration ΔN/Δ log da was between >104 and >105 cm−3), while fewer micron-size particles were detected (ΔN/Δ log da∼103 cm−3). For each measured particle size, the initial aerosol concentration was reproducible with the variability (the coefficient of variation) not exceeding about 50% for six replicates.
Fig. 2.
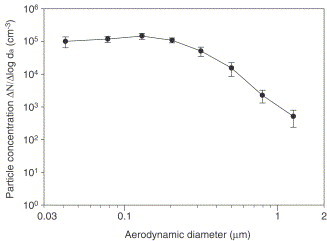
Initial particle size distribution measured outside the mask. The error bars represent the standard deviations of 6 tests.
Fig. 3 presents the data obtained with two types of face-sealed respirators: N95 respirator and a surgical mask. When no air ion emission was introduced, the E p-value, averaged over the test range of d a, was about 1.8% for the N95 respirator. The particle size did not considerably affect the penetration through the N95 respirator filter, although some decrease of E p with increasing d a was observed for d a≈0.04–0.5 μm. Once the negative ion emission began, the penetration decreased to 0.27% during the first 3 min. At t=12 min, it further decreased to about 0.11%, enhancing the N95 respirator filter performance approximately by a factor of 17 (Fig. 3a). For the surgical mask, the initial penetration efficiency ranged from 18.7% (da=0.04 μm) to 11.1% (da=1.3 μm). Resulting from the emission of negative ions, the average penetration efficiency through the surgical mask dropped from 15.4% (t=0) to 0.19% (t=12 min), demonstrating a 80-fold enhancement (Fig. 3b). The data in Fig. 3 show that the most pronounced effect occurred within the first 3-min interval.
Fig. 3.
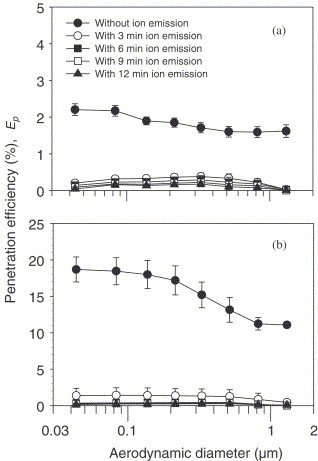
Effect of air ion emission on the penetration efficiency of two respiratory masks: N95 respirator (a) and surgical mask (b). The penetration efficiency measured with no ion emission (circles) is compared to that obtained with the negative ion emission (Ni∼1.3×106 e− cm−3) during t=3 min (void circles); t=6 min (squares); t=9 min (void squares); and t=12 min (triangles).
4. Discussion
4.1. Baseline test
It was surprising to observe that the initial penetration efficiency (t=0) of ultrafine particles through both masks slightly increased with decreasing particle size. In contrast, the available filtration models predict that the peak penetration is reached at d a between 0.1 and 0.3 μm, and the particles below 0.1 μm should be collected more efficiently as their size decreases (diffusion regime) (Halvorsen, 1998; Hinds, 1999; Lee & Mukund, 2001). The following considerations explain the results of our baseline test for the ultrafine particles. These models (and the laboratory-generated experimental data that support them) characterize the particle penetration through a homogeneous perfectly sealed fibrous filter material but not through a respirator mask. The design of a filtering-facepiece respirator does not assure a perfect peripheral connection of the assembly, so micro-leaks may be present between the core filter material and the elastic peripheral support. These leaks can contribute to the penetration of the ultrafine particles. In addition, although the mask was “glued” on the manikin, some very small, micrometer- or submicrometer-size leaks may still remain. Most of soap-bubble-based air leak detection methods are capable to identify micro-leaks greater than 1 μm. If d a is much lower than the characteristic size of the micro-leaks (⪡1 μm), the particles may penetrate through these remaining submicrometer micro-leaks, thus affecting the overall aerosol penetration efficiency through the filtering mask. One more possible factor is associated with the spatial variations in fiber diameter, orientation, packing density, as well as initial fiber electrostatic charge level (for those masks utilizing electret filter media). These variations have been shown to significantly affect the respirator performance increasing the penetration efficiency of particles of ∼0.1 μm (Huang et al., 1998).
4.2. Enhancement due to the unipolar air ion emission
The enhancement of the respirator performance, observed almost immediately after the ion emitter started operating, can be attributed to the electrostatic effect. The emitted negative ions as well as the particles charged by these ions in the air, impose significant negative charge on the respirator filter. This forms the “electrostatic shield” against the particles moving toward the mask. The repelling forces decrease the number of particles that can approach the filter. The above-described effect works outside of the respirator, as opposite to the aerosol filtration by diffusion, impaction, interception, and electrostatic deposition (Lee & Mukund, 2001) that takes place inside the filter. Therefore, the ion-induced decrease in the particle penetration efficiency does not cause the pressure drop increase through the filter providing the enhanced performance with the same comfort level.
To quantitatively characterize the effect, we calculated the velocity of particle migration induced by the electrostatic interaction in the vicinity of the filter. It was then compared to the velocity of the air flow through the filter caused by inhalation. In this calculation, we used information about the airborne particle electric charges and the air ion density, obtained by the ELPI and the Air Ion Counter, respectively. The particle size of da=0.1 μm was chosen, as it represents the dominant size range used in our experiments. Furthermore, this value is at the boarder line between the fine and ultrafine particle size ranges. In addition, many viral particles have an aerodynamic diameter of ∼0.1 μm. Two main assumptions were made. First, the aerosol particles and air ions that interacted with the respirator were assumed to give all their electric charges to the respirator filter. Second, the charged filter was assumed to act as a point-charge located at the center of the respirator's surface. At the ion emission level produced in our experiment, a 0.1 μm particle carries, on average, 10 elementary charges (Lee, Yermakov, & Grinshpun, 2004b). The calculation showed that the total electric charge acquired by the respirator filter, as a result of a 3-min continued emission from the VI-2500 ion source, is about 1.5×1013 elementary charges, if the breathing flow rate is 30 l min−1. The ion concentration at the center of the respirator was determined to be approximately 1.6×108 cm−3 (this point located 20 cm from the ion emission source). Thus, the particle migration velocity was found to exceed the air flow velocity, created by the inhalation in the breathing zone, approximately by a factor of 75. This suggests that the effect of the repelling force between the unipolarly charged particles and filter surface is much stronger than the aerodynamic force. Therefore, although our assumptions may not be sufficiently conservative, the above assessment demonstrates that the enhancement of the respirator performance by the unipolar ion emission is governed by the electrostatic “shield” mechanism.
The drastic decrease of the particle penetration through the respirator filter due to continuous unipolar ion emission may be critical in providing additional respiratory protection by existing masks against viral and bacterial particles. For example, an individual exposed to the influenza virus concentration of 10,000 m−3 inhales approximately 4500×0.18=810 viruses during 15 min when breathing through a conventional surgical mask at 30 l min−1 in the absence of ion emission (E p≈18% for 0.1 μm particles). The continuous emission of negative air ions (Ni∼106 e− cm−3) in a 25-m3 room would reduce the indoor viral concentration by a factor of 9 during that 15-min interval (Lee 2004a, Lee, Yermakov, & Grinshpun 2004b). In addition, it would enhance the surgical mask protection reducing E p from 18% to at least 0.19%. Thus, only about (4500/9)×0.0019=0.95≈1 virus would be inhaled in 15 min. Given that the infectious dose of influenza A2 is 790 viruses (Lawrence Berkeley National Laboratory), the ion emission effect would make an important difference with respect to the health risk.
While this study is limited to the negative ion emission, we anticipate that the respirator performance enhancement effect can be achieved also by generating positive air ions, as long as the ion concentration in the vicinity of the mask (breathing zone) is sufficiently high. Future studies will address the effects of polarity and the ion emission rate on the particle penetration efficiency through respirator filters.
Generally, the mask protection factor depends not only on its filter penetration efficiency but also on its face fit (in practice, the facepiece mask is not sealed to the human face allowing the particles to penetrate through the leak). This pathway may become especially apparent when the filter material is highly efficient. Therefore, future tests involving human subjects, different fit factors, and other experimental conditions (flow rates and different masks) are needed to better characterize the enhancement effect, discovered in this study, and link it to the exposure.
Acknowledgements
The experimental evaluation part of this investigation was supported by the Wein Products Inc., Los Angeles, CA, USA. The participation of Dr. Lee in this study was partly due to the Post-doctoral Fellowship Program and the Advanced Environmental Monitoring Research Center (ADEMRC) Program of the Korea Science & Engineering Foundation (KOSEF). The authors are thankful for this support.
Disclaimer
Reference to any companies or specific commercial products does not constitute or imply their endorsement, recommendation, or favouring by the University of Cincinnati or the authors.
References
- Adachi M., Kousaka Y., Okuyama K. Unipolar and bipolar diffusion charging of ultrafine aerosol particles. Journal of Aerosol Science. 1985;16:109–123. [Google Scholar]
- Baron P.A., Willeke K. Aerosol measurement: Principles, techniques, and applications. Wiley; New York: 2001. [Google Scholar]
- Brosseau L.M., Evans J.S., Ellenbecker M.J., Feldstein M.L. Collection efficiency of respirator filters challenged with monodisperse latex aerosols. American Industrial Hygiene Association Journal. 1989;50:544–549. doi: 10.1080/15298668991375137. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (1994). Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities. Morbidity and Mortality Weekly Report 43, 1–132. [PubMed]
- Chen C.C., Ruuskanen J., Pilacinski W., Willeke K. Filter and leak penetration characteristics of a dust and mist filtering facepiece. American Industrial Hygiene Association Journal. 1990;51:632–639. doi: 10.1080/15298669091370275. [DOI] [PubMed] [Google Scholar]
- Chen C.C., Willeke K. Characteristics of face seal leakage in filtering facepieces. American Industrial Hygiene Association Journal. 1992;53:533–539. doi: 10.1080/15298669291360120. [DOI] [PubMed] [Google Scholar]
- Cheng Y.S., Bechtold W.E., Yu C.C., Hung I.F. Incense smoke: Characterization and dynamics in indoor environments. Aerosol Science and Technology. 1995;23:271–281. [Google Scholar]
- Choe K.T., Trunov M., Grinshpun S.A., Willeke K., Harney J., Trakumas S., Mainelis G., Bornschein R., Clark S., Friedman W. Particle settling after lead-based paint abatement work and clearance waiting period. American Industrial Hygiene Association Journal. 2000;61:798–807. doi: 10.1080/15298660008984589. [DOI] [PubMed] [Google Scholar]
- Federal Register. (1995). Respiratory protective devices: Final rules and notice, US Government, Vol. 60:110 (PP. 30336–30398).
- Frank G.P., Cederfelt S.I., Martinsson B.G. Characterisation of a unipolar charger for droplet aerosols of 0.1–20 μm in diameter. Journal of Aerosol Science. 2004;35:117–134. [Google Scholar]
- Grinshpun, S. A., Adhikari, A., Lee, B. U., Trunov, M., Mainelis, G., Yermakov, M., & Reponen, T. (2004). Indoor air pollution control through ionization. In C. A. Brebbia (Ed.), Air pollution XII. Wessex Institute of Technology Press, Southampton, UK, in print.
- Grinshpun S.A., Choe K.T., Trunov M., Willeke K., Menrath W., Friedman W. Efficiency of final cleaning for lead-based paint abatement in indoor environments. Applied Occupational and Environmental Hygiene. 2002;17:222–234. doi: 10.1080/104732202753438306. [DOI] [PubMed] [Google Scholar]
- Halvorsen, T. (1998). Respirator Fit Testing Application Notes. TSI Incorporated. Website; http://www.tsi.com/fittest/app_note/iti_062.htm.
- Hernandez-Sierra A., Alguacil F.J., Alonso M. Unipolar charging of nanometer aerosol particles in a corona ionizer. Journal of Aerosol Science. 2003;34:733–745. [Google Scholar]
- Hinds W.C. Aerosol technology: Properties, Behavior, and Measurement of Airborne Particles. 2nd ed. Wiley-Interscience; New York: 1999. [Google Scholar]
- Huang C., Willeke K., Qian Y., Grinshpun S.A., Ulevicius V. Method for measuring the spatial variability of aerosol penetration through respirator filters. American Industrial Hygiene Association Journal. 1998;59:461–465. doi: 10.1080/15428119891010208. [DOI] [PubMed] [Google Scholar]
- Johnston A.R., Myers W.R., Colton C.E., Birkner J.S., Campbell C.E. Review of respirator performance testing in the workplace: Issues and concerns. American Industrial Hygiene Association Journal. 2001;53:705–712. doi: 10.1080/15298669291360409. [DOI] [PubMed] [Google Scholar]
- Johnson A.T., Weiss R.A., Grove C. Respirator performance rating table for mask design. American Industrial Hygiene Association Journal. 1992;53:193–202. doi: 10.1080/15298669291359500. [DOI] [PubMed] [Google Scholar]
- Lawrence Berkeley National Laboratory, Environment, Health & Safety Division; http://www-nsd.lbl.gov/ehs/biosafety/html/infectious_dose.htm.
- Lee K.W., Mukund R. Filter collection. In: Baron P.A., Willeke K., editors. Aerosol measurement: Principles, techniques, and applications. Wiley; New York: 2001. pp. 197–228. [Google Scholar]
- Lee K., Slavcev A., Nicas M. Respiratory protection against Mycobacterium tuberculosis: Quantitative fit test outcomes for five type N95 filtering-facepiece respirators. Journal of Occupational and Environmental Hygiene. 2004;1:22–28. doi: 10.1080/15459620490250026. [DOI] [PubMed] [Google Scholar]
- Lee, B. U., Yermakov, M., & Grinshpun, S. A. (2004b). Removal of fine and ultrafine particles from indoor air environments by the unipolar ion emission. Atmospheric Environment, in press. [DOI] [PMC free article] [PubMed]
- Mineral Resources. (1994). Code of Federal Regulations, Title 30, Pt. 11, pp. 91–96.
- National Center for Biotechnology Information, The universal virus database of the international committee on taxonomy of viruses; http://www.ncbi.nlm.nih.gov/ICTVdb/ICTVdB/19010000.htm.
- Oestenstad R.K., Dillion H.K., Perkins L.L. Distribution of faceseal leak sites on a half-mask respirator and their association with facial dimensions. American Industrial Hygiene Association Journal. 1990;51:285–290. doi: 10.1080/15298669091369664. [DOI] [PubMed] [Google Scholar]
- Oestenstad R.K., Perkins J.L., Rose V.E. Identification of faceseal leak sites on a half-mask respirator. American Industrial Hygiene Association Journal. 1990;51:280–284. doi: 10.1080/15298669091369655. [DOI] [PubMed] [Google Scholar]
- Qian Y., Willeke K., Grinshpun S.A., Donnelly J. Performance of N95 respirators: Reaerosolization of bacteria and solid particles. American Industrial Hygiene Association Journal. 1997;58:876–880. doi: 10.1080/15428119791012216. [DOI] [PubMed] [Google Scholar]
- Qian Y., Willeke K., Grinshpun S.A., Donnelly J., Coffey C.C. Performance of N95 respirators: Filtration efficiency for airborne microbial and inert particles. American Industrial Hygiene Association Journal. 1998;59:128–132. doi: 10.1080/15428119891010389. [DOI] [PubMed] [Google Scholar]
- Reponen T.A., Wang Z., Willeke K., Grinshpun S.A. Survival of Mycobacteria on N95 personal respirators. Infection Control and Hospital Epidemiology. 1999;20:237–241. doi: 10.1086/501618. [DOI] [PubMed] [Google Scholar]
- United States Department of Labor. (1995). Respirator Use and Practice, USDL 02-141.
- Wiedensohler A., Buscher P., Hansson H.C., Martinsson B.G., Stratmann F., Ferron G., Busch B. A novel unipolar charger for ultrafine aerosol particles with minimal particle losses. Journal of Aerosol Science. 1994;25:639–649. [Google Scholar]
- Willeke K., Qian Y., Donnelly J., Grinshpun S., Ulevicius V. Penetration of airborne microorganisms through a surgical mask and a dust/mist respirator. American Industrial Hygiene Association Journal. 1996;57:348–355. doi: 10.1080/15428119691014882. [DOI] [PubMed] [Google Scholar]


