Abstract
Digital health technologies such as smartphones present the potential for increased access to care and on-demand services. However, many patients with serious mental illnesses (eg, schizophrenia) have not been offered the digital health training necessary to fully utilize these innovative approaches. To bridge this digital divide in knowledge and skills, we created a hands-on and interactive training program grounded in self-determination theory, technology use cases, and the therapeutic alliance. This article introduces the need and theoretical foundation for and the experience of running the resulting Digital Opportunities for Outcomes in Recovery Services (DOORS) group in the setting of 2 programs: a first episode psychosis program and a clubhouse for individuals with serious mental illness. The experience of running these 2 DOORS groups resulted in 2 publicly available, free training manuals to empower others to run such groups and adapt them for local needs. Future work on DOORS will expand the curriculum to best support digital health needs and increase equity of access to and knowledge and skills related to technology use in serious mental illness.
Keywords: psychosis, applications (apps), technology, digital health, smartphones, equity, Digital Opportunities for Outcomes in Recovery Services (DOORS)
Increasing access to high quality and evidence-based mental health services remains both a challenge and a priority for health care. Whether measured in terms of personal suffering, lost productivity, premature mortality, or increased healthcare spending, it is clear that there is a need for innovative solutions to meet the expanding demand for mental health services. Given the rapid expansion of mobile technology, especially smartphones, it is logical that these digital tools may offer one potential solution. Data have repeatedly shown that those with mental health conditions, including serious mental illnesses such as bipolar disorder or schizophrenia, have high rates of access to smartphones and interest in digital mental health offerings.1,2 The digital divide of access to smartphones and other digital tools that once existed between people with serious mental illness and those without has rapidly narrowed, thus creating opportunities for novel clinical interventions and portals of care. The myriad of apps available today promise to help those with mental health conditions to monitor symptoms, connect with care, self-manage symptoms, and even predict relapse. The potential of on-demand mental health services only a fingertip away has fueled unprecedented interest, as indicated by the over 10,000 related apps available today for immediate download,3 but the closing of this first digital divide has revealed a second.4
Increasing access to smartphones and the availability of digital mental health apps have not yet transformed the field or patient trajectories. Rather, the initial excitement about a potential panacea has transformed into an understanding that realizing the potential of digital mental health requires not only developing new apps, but also developing new skills for people using these technologies.4 This second digital divide is not focused on material access to digital tools like smartphones or apps but rather on the core competencies, autonomy, and skills required to effectively utilize these novel tools to improve mental health. Although this second digital divide is less immediately tangible than the first one involving access, even brief actual experience with technology ranging from fitness trackers to smartphone apps to virtual reality to smart home devices immediately reveals the extent of this new digital divide.5
To address this divide, patients and clinicians have advocated for digital literacy skills programs that can equip individuals with mental illness with the core competencies, autonomy, and skills to fully engage with the plethora of digital health interventions that currently exist.6 While there are many paths toward equity and bridging this second digital divide, in this article we introduce one approach with hands-on training and functional education that offers people the skills to meaningfully engage with technology toward their recovery. The Digital Opportunities for Outcomes in Recovery Services (DOORS) program represents an evidence-based effort to formally bridge this new digital divide and deliver on the potential of digital mental health.
The DOORS digital health curriculum and the technology journey of participants in the group are supported by key elements of self-determination theory (SDT), which are defined by Ryan and Deci as the “three ‘psychological needs’ [of] autonomy (motivated behavior towards agency and self-expression), competence (motivated behavior towards knowledge, skill or learning), and relatedness (interpersonal connection).”7 Elements of competence include mastery of using and navigating digital devices toward health outcomes. Elements of autonomy include learning skills to independently approach, evaluate, and master use of these tools to advance personal values and goals. Finally, elements of relatedness include using technology to foster meaningful relationships to advance recovery, both with peers and with clinicians. As part of their technology journey, participants learn to (a) recognize the benefits and availability of digital health technology, (b) make informed decisions when downloading apps, and (c) use digital tools toward their recovery with a unique focus on trust around any technology use being ultimately aligned toward both increasing the therapeutic alliance (Fig. 1) and supporting strategies for self-managing chronic conditions. Through this process, participants can strengthen their competence and autonomy in using digital technology to support their health and to foster relatedness with their care providers and with others who have shared the lived experience of mental illness.
Figure 1.

Schematic of the theory and technology journey underlying the DOORS program
DOORS indicates Digital Opportunities for Outcomes in Recovery Services
APPLYING THEORY TO PRACTICE
The complexity of bridging the digital divide can thus be understood as an interplay between self-determination theory and the therapeutic alliance. Because there will be no uniform solution or single path forward, we explored utilizing DOORS in 2 distinct settings: a first-episode psychosis (FEP) clubhouse and a chronic phase schizophrenia clubhouse. Clubhouses are organizations that support people with mental illness through offering supportive environments, recovery services, and opportunities to access employment and training programs among numerous other roles. To address these different needs, we created 2 versions of DOORS with the FEP version designed to focus more on autonomy and the chronic phase version focused more on competency. Both groups focused equally on evaluating apps and sought to help learners develop their own sense of how much trust they want to put into these technologies. We ran 2 exploratory groups and collected qualitative feedback to guide future efforts and to enable others to develop their own initiatives. In this article, we report on the process of running these groups, qualitive feedback from each, and lessons learned. Two manuals for facilitators are provided in supplemental digital content included with this article. These manuals provide detailed session outlines, handouts, and references to help support clinicians in leading digital skill groups. The intermediate skill level manual was generated for the FEP group and the introductory manual was generated for the schizophrenia chronic phase group. These manuals, which are in the public domain and available for use at no cost, are also available online at: https://www.digitalpsych.org/digital-skills-training.html. Future updates and new materials and content will continue to be made available at this website.
The process of creating the DOORS curriculum and manuals was divided into 5 stages: 1) creation of the framework and curriculum, 2) running the FEP group, 3) revision of content and creation of new content for the chronic phase schizophrenia group, 4) running the chronic phase group, and 5) creation of group facilitator manuals for public sharing and comment. The content areas were formulated through a review of the literature, clinical experience, and patient input concerning challenges in using apps toward recovery. The learning goals for patients of identifying digital resources for wellness, better understanding their lived experience, making informed decisions about apps, and using apps and data for behavior change were directly linked to the stages of the curriculum.
THE FEP GROUP
The first 2 sessions focused largely on recognizing the variety of apps available that can aid in improving one’s health and understanding how to choose apps. The purpose of the first session was to build autonomy by communicating how skills the group members already had could be utilized for digital mental health. Group members were introduced to the concept of digital health, and they explored both how they use their phones and their experience with digital health technology. When the group members were surveyed about what they wanted in apps, they responded that they would like help with “identifying mental health triggers,” “relaxing when I’m having paranoid thoughts,” and “improving sleep.” The FEP group noted that, when considering an app, they utilized a number of different criteria when considering an app (Fig. 2). It was notable that the FEP group was heavily engaged with apps but overall they were not aware of the use of apps as tools toward recovery. Of the 15 participants surveyed, only a handful of individuals had experience using apps for wellness-related reasons (Fig. 3). However, many members of the group were interested in trying apps related to fitness, nutrition, and relaxation. While they were in the group, participants used a mindfulness app to check in on their physical and emotional states and found it useful to reflect on how they were feeling in the moment.
Figure 2.
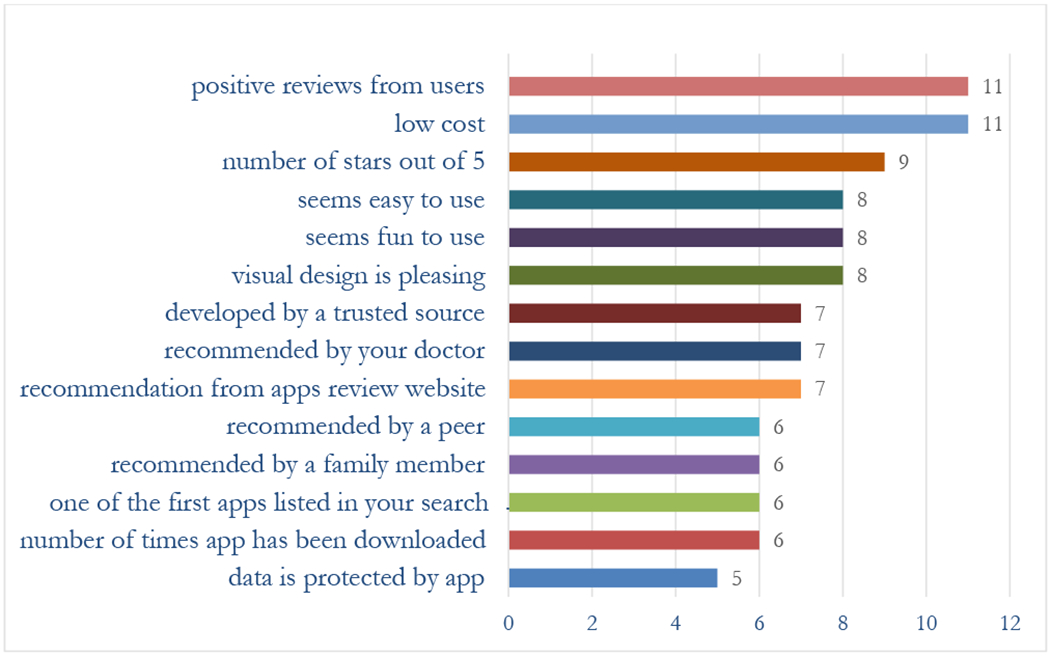
Number of participants in the first-episode psychosis group using different criteria to evaluate health-related apps
Figure 3.
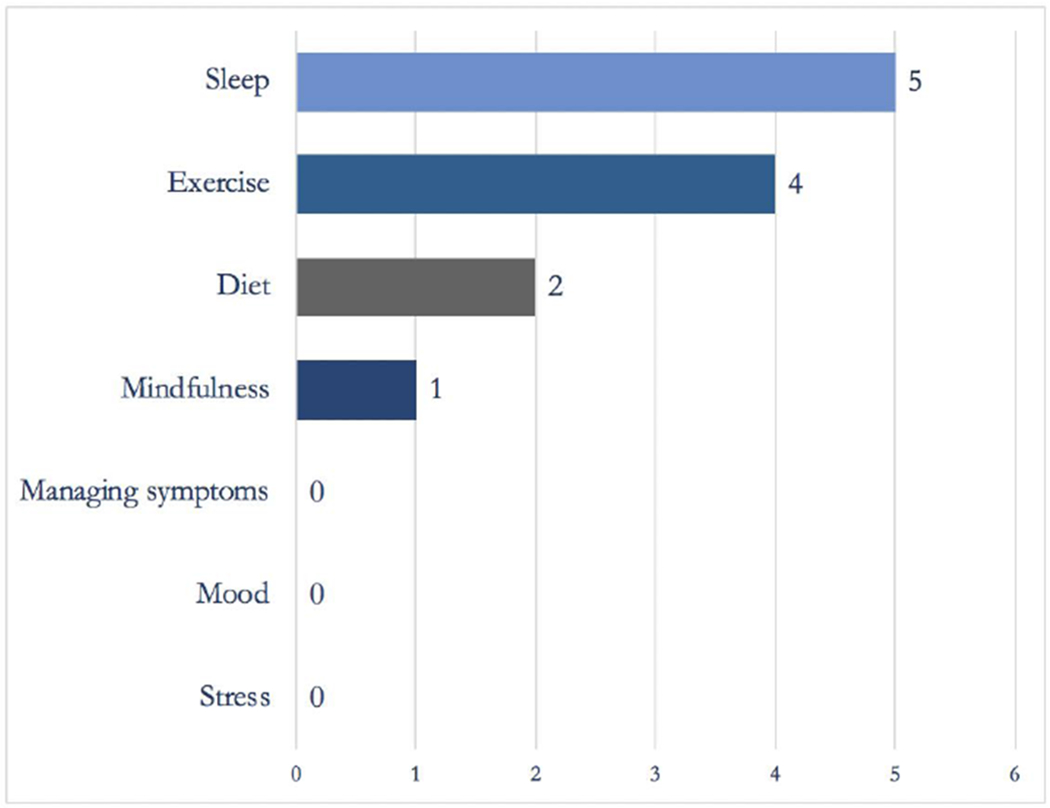
Number of participants in the first-episode psychosis group that had used a smartphone app to help with sleep, exercise, diet, mindfulness, managing symptoms, mood, or stress
In the second session, we focused on improving group members’ competencies in evaluating apps by exploring descriptions of two meditation apps listed in the app store. Although on the surface the first app appeared to be of interest, closer inspection revealed that it suffered from numerous flaws, including no privacy policy or data protections, not being updated in several years, and having been developed by an unknown developer. Initially, 80% of participants said “yes” they would download the app. However, after they were offered education about additional app evaluation criteria, 80% changed their answer to “no” the second time they evaluated the app. This activity revealed that teaching basic skills in app evaluation can have an immediate impact on decision-making and can equip participants with the skills and competencies to carefully select digital tools on their own.
The third and fourth sessions shifted back to the topic of autonomy and focused on individual goals and using apps to meet those goals. In the third session, group members were introduced to an app called “mindLAMP” (Learn, Assess, Manage, and Prevent),8 and they learned how apps can be used to track mental health both through surveys and sensors. Exploring participants’ concerns, we found that, while they are comfortable sharing sensitive mental health information via app surveys and sensitive personal information such as geolocation via GPS on their phones, some expressed a preference to do this within the context of a therapeutic relationship in which such data would be used to augment their personal care. Group participants presented a spectrum of thoughts on trust of smartphone apps, with some feeling at ease and others guarded.
In the final session, participants reviewed their LAMP data, including results from the weekly surveys as well as step count data. During the group discussion, participants considered whether their perception of their physical activity aligned with the information provided by their smartphones and were surprised by the discrepancies. They also reflected on what it was like using digital technology to develop more insight into their lived experience and how they might consider using these tools to further their health-related goals.
ADAPTING DOORS
On the basis of our experience with the initial group, we recognized several opportunities for improvement. Although many FEP participants did possess high levels of technology competency, some did need help with basic competencies and were not able to partake as fully in the group content. We realized there is a need to offer smaller group breakout sessions that can meet participants where they are in terms of their current level of digital literacy and prioritize skill development in the areas that are most important to group members. Realizing the chronic phase group would likely benefit from more help with smartphone competencies, we created new modules to facilitate learning and skills. The manual that is shared with this paper includes all content from this group but also expanded introductory content offered over 2 additional sections which offer the group facilitator flexibility in offering 6 sessions, skipping the new introductory content, or combining sessions to still offer 4 sessions. We also added pre-post measurements to begin to quantify the response to DOORs using the eHealth Literacy Scale (eHEALS),9 modified to ask about smartphones instead of the Internet.
CHRONIC PHASE GROUP
During the first session with the chronic phase schizophrenia group, the participants shared their knowledge and experience using smartphone technology and began generating ideas for how these digital tools could be used to advance their health goals. Participants shared ideas for content tailored to their personal needs and named specific skills they were hoping to acquire through participation in this digital skills group. Group participants also discussed the challenges they’ve faced using smartphone technology, including lack of technical skills and expensive data plans.10,11 Although some participants had experience using their smartphones to increase their physical activity or to self-manage anxiety, most had not explored the ways in which digital technology could support their health. Given higher levels of familiarity with smartphone technology in this group, we did not offer the 2 new introductory modules but rather began with the section noted above, highlighting the flexible nature of DOORS.
In the second group session, group participants learned about basic smartphone competencies such as how to access WiFi. After the large group discussion, participants broke into small groups based on their stated interests in uses/responses from the previous week’s discussions (Fig. 4). These 4 small groups focused on a) competencies of setting up and navigating smartphones, b) competencies accessing voicemail and sending text messages, c) downloading and using music apps, and d) downloading and using nutrition and exercise apps. Participants were eager and motivated to learn, but they encountered challenges related to using the touchscreen and navigating to specific features. Group participants who were interested in wellness apps sometimes struggled to identify the correct app to download, navigate through the setup process, and accurately enter information once the app had been downloaded. Receiving guidance from staff members or “digital navigators” proved crucial in enabling participants to effectively access and utilize the digital tools that were of interest to them.12 With mastery of these skills, many participants became excited about using apps to increase their autonomy, with one popular example being the public transit app and another the hospital portal to check clinical appointments.
Figure 4.

Smartphone skills and examples of apps in which the participants in the chronic phase schizophrenia group expressed interest
In the third session, participants discussed ways in which aspects of their lived experience, such as mood, behavior, and symptoms, might be connected, and how digital technology could help them gain more insight into these connections. Participants downloaded mindLAMP, practiced taking a survey within the app assessing their daily mood, and made a prediction regarding their mood/step count for the following week. Group participants also shared their experience using their newly acquired digital skills and tools to enhance their health, which included exercising more and using music for self-soothing.
In the final session, participants reviewed their LAMP data and compared their step count data to what they had predicted their results would be for the week. The contrast between their actual step count and their predicted step count sparked a group discussion of strategies for increasing exercise. To conclude the group, participants reflected on what they had learned over the past 4 weeks and set SMART goals to continue using digital technology to work toward their health goals. The acronym SMART stands for specific, measurable, achievable, relevant, and timely (see Appendix D in the intermediate/advanced skill level manual).
Participants completed pre and post eHEALS assessments, with scores improving across all domains related to using smartphones for accessing health information. Most notably, group participants indicated that it was important for them to know how to access health resources on their smartphone and that they felt more confident in their ability to find helpful health resources by the end of the 4-week group (Fig. 5). Participants provided additional feedback about their group experience indicating that they had made lifestyle changes based on the knowledge they acquired during the DOORS group, and they expressed a strong desire for more sessions to continue learning about digital health tools.
Figure 5:
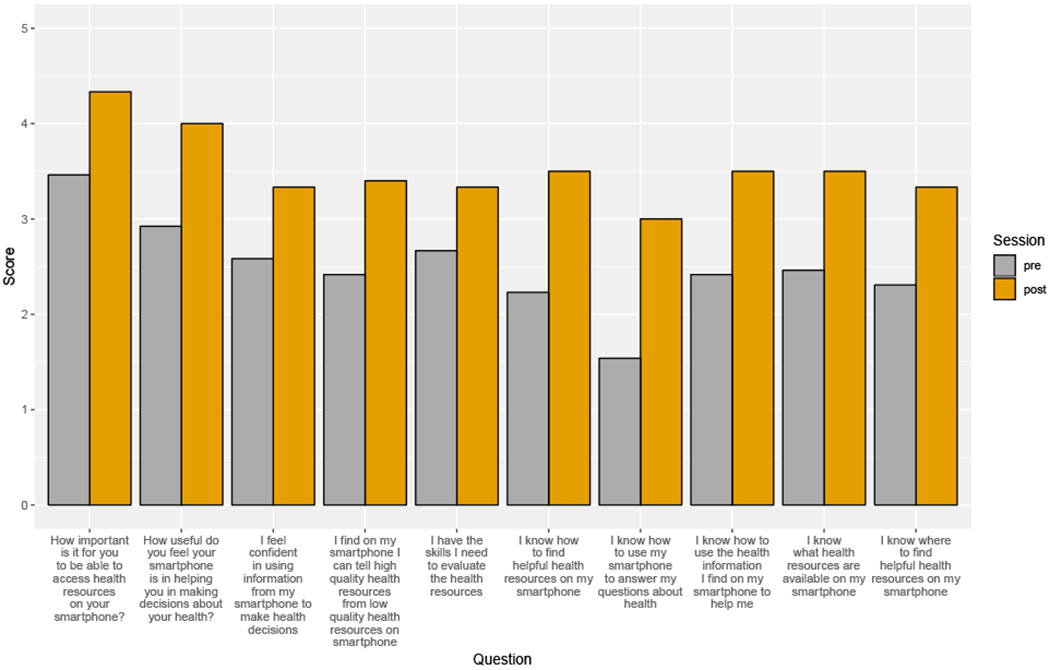
Pre and post scores on the eHEALS in the chronic phase schizophrenia group eHEALS indicates the e Health Literacy Scale
DISCUSSION
DOORS represents an effort to bridge the second digital divide between people with serious mental illness and those without, by helping those with serious mental illnesses develop competency, autonomy, and relatedness around using digital tools such as smartphone apps toward their recovery. Focusing on recognition of the need to use these tools, knowledge to evaluate apps, and skills to use them, the program seeks to support patients at all stages of their technology journey. While patient feedback in the initiatives described here was positive, continued improvement is needed. We hope that, by sharing our facilitator manuals in the public domain, others will develop, expand, and customize DOORS to suit the needs of their patients. As more health services move toward digitally based portals, treatments, and therapy offerings (eg, some insurers now offer apps in partnership with technology companies and pharmacies),13 it is critical that efforts such as DOORS are available to ensure equitable and equal access to care.
Although the 2 DOORS groups served different populations, both were similar with regard to a focus on evaluating apps. This approach is consistent with a recent national survey suggesting that evaluating mental health apps is a priority for patients, families, and clinicians.14 Participants in both groups noted that they were not sure how to make an informed decision about apps and often relied on star ratings in the app store (Fig. 2) and picking from apps that have positive user reviews. While app evaluation can be a nuanced process, we found that, even with simple guidelines concerning what to look for in an app, participants were able to screen out more risky apps with ease. The fact that data protection was rated as the least important factor when participants in the FEP group were initially asked about selecting apps highlights the potential for education about digital privacy that will be of benefit to all participants. While evaluating apps is an important skill for all patients as more health services move toward digital offerings, our approach also highlights that new knowledge must be matched with new skills. Many participants in both groups had issues downloading or installing apps and were unsure how to best utilize them to work toward recovery or share information with their clinical team.
Although the FEP group was already comfortable using apps, in general they showed limited awareness of or interest in using apps to work toward recovery. While these participants were able to use the LAMP app without difficulty, they displayed less interest in their personal data than the chronic phase group. This finding may reflect that each group had a different perspective and level of interest in recovery. It also makes sense in terms of self-determination theory—the FEP group may have needed more assistance with developing autonomy toward managing their illnesses and a focus on using apps to work toward their personal goals. We found that many participants were not sure how to use apps toward relatedness but that they expressed interest in using apps to better connect with and share their lived experience with their clinical teams. Lal et al15 previously reported similar results, noting that, based on a survey study, young people diagnosed with FEP, being tech-savvy, expressed interest in using the Internet, social media, and mobile technologies to receive mental health-related services. Numerous studies have found that individuals with schizophrenia desire to use tech not just for self-care16 but also to better connect with their support network and care teams.17–20 DOORS offers one approach for bridging the clinical and digital worlds in a manner that is acceptable and relevant to younger individuals with lived experience of mental illness.
The chronic phase group was more interested in building digital competencies and learning how to use apps to work toward their health goals.21 Many participants were able to take the digital skills and tools learned during the group and independently use them to make progress with their goals. For instance, all 4 group members who expressed an interest in increasing their step count had done so by the end of the 4 weeks and had plans for continuing to improve their fitness levels after the conclusion of the group. These results are also supported by reports in the literature that older patients are equally interested in digital mental health22 and can benefit from these interventions,20 despite a limited background in digital technology.
In both groups, we noticed that there was a spectrum of trust related to using digital health technologies. It was not that the younger participants in the FEP group, as digital natives, had greater trust—if anything, we found the opposite. The practical implication is that it is challenging to make assumptions about what level of digital care patients may find both acceptable and beneficial. In part, the potential of tools like smartphone apps for improving mental health is their scalability and ability to reach millions at almost no cost, facilitate prevention with real time monitoring, and offer a plethora of on-demand and triggered resources and interventions.23 But realizing the potential of digital mental health technology24 requires that patients be willing to trust these new tools to monitor, alert, and intervene on their behalf and understand how these tools can advance their personal recovery. On the basis of both the theory behind DOORS and our experiences with the 2 groups described in this article, we propose that the path toward such trust in digital health tools will involve ensuring competency, autonomy, and relatedness toward creating a therapeutic alliance (be it with the app itself, peers supporting it, or clinicians). While using technology to boost the therapeutic alliance between a patient and clinician is often an important goal, DOORS focuses on helping people develop the competence, autonomy, and relatedness to become ready for this new model of care while also promoting self-management and personal recovery through the use of digital health technology.
Like any new program, DOORS has much room for improvement. In future iterations, we will measure potential improvements in the three elements of self-determination theory and the therapeutic alliance. A peer support component of DOORS would better introduce and teach relatedness around digital health, and we hope to adapt mindLAMP to offer such features and serve as a didactic tool in the near future. We will also collect further qualitative and quantitative data to better assess the impact of the program. Finally, while our initial 2 groups focused on patient groups with first episode psychosis and schizophrenia, DOORS can be applied across the diagnostic spectrum and we plan to assess its potential in those with anxiety, depression, posttraumatic stress disorder, and bipolar disorder in the future.
CONCLUSION
Bridging the second digital divide between people with serious mental illness and those without by offering new skills and resources to help people to take full advantage of digital health tools is becoming a global health priority. DOORS represents one approach toward addressing this gap between the impressive potential of these new tools and the elements of self-determination theory (autonomy, competence, and relatedness) to recognize, evaluate, and use these tools in the journey toward recovery. By openly sharing the manuals and tools we developed in running our initial groups, we hope others will improve and expand on them and accelerate progress in this field.
Supplementary Material
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Torous J, Wisniewski H, Liu G, et al. Mental health mobile phone app usage, concerns, and benefits among psychiatric outpatients: comparative survey study. JMIR Ment Health. 2018;5:e11715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torous J, Chan SR, Yee-Marie Tan S, et al. Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: a survey in four geographically distinct psychiatric clinics. JMIR Ment Health. 2014;1:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74:437–438. [DOI] [PubMed] [Google Scholar]
- 4.Torous J, Rodriguez J, Powell A. The new digital divide for digital biomarkers. Digit Biomark. 2017;1:87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffman L, Benedetto E, Huang H, et al. Augmenting mental health in primary care: a 1-year study of deploying smartphone apps in a multi-site primary care/behavioral health integration program. Front Psychiatry. 2019;10:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naslund JA, Aschbrenner KA, Bartels SJ. Wearable devices and smartphones for activity tracking among people with serious mental illness. Ment Health Phys Act. 2016;10:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. [DOI] [PubMed] [Google Scholar]
- 8.Torous J, Wisniewski H, Bird B, et al. Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach. J Technol Behav Sci. 2019;4:73–85. doi: 10.1007/s41347-019-00095-w [DOI] [Google Scholar]
- 9.Norman CD, Skinner HA. eHEALS: the eHealth Literacy Scale. J Med Internet Res. 2006;8:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berry N, Lobban F, Bucci S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry. 2019;19:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry N, Bucci S, Lobban F. Use of the Internet and mobile phones for self-management of severe mental health problems: qualitative study of staff views. JMIR Ment Health. 2017;4:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noel VA, Carpenter-Song E, Acquilano SC, et al. The technology specialist: a 21st century support role in clinical care. NPJ Digit Med. 2019;2:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farr C. Apple and Aetna are teaming up on a new app to help track and reward healthy behavior. CNBC: Health Tech Matters; January 29, 2019. Available at: https://www.cnbc.com/2019/01/28/apple-aetna-team-up-on-attain-health-tracking-app.html. Accessed June 11, 2019.
- 14.Hollis C, Sampson S, Simons L, et al. Identifying research priorities for digital technology in mental health care: results of the James Lind Alliance Priority Setting Partnership. Lancet Psychiatry. 2018;5:845–854. [DOI] [PubMed] [Google Scholar]
- 15.Lal S, Dell’Elce J, Tucci N, et al. Preferences of young adults with first-episode psychosis for receiving specialized mental health services using technology: a survey study. JMIR Ment Health. 2015;2:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torous J, Staples P, Slaters L, et al. Characterizing smartphone engagement for schizophrenia: results of a naturalist mobile health study. Clin Schizophr Relat Psychoses. 2017. August 4. doi: 10.3371/CSRP.JTPS.071317. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 17.Firth J, Torous J. Smartphone Apps for schizophrenia: a systematic review. JMIR Mhealth Uhealth. 2015;3:e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gay K, Torous J, Joseph A, et al. Digital technology use among individuals with schizophrenia: results of an online survey. JMIR Ment Health. 2016;3:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schrank B, Sibitz I, Unger A, et al. How patients with schizophrenia use the Internet: qualitative study. J Med Internet Res. 2010;12:e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schlosser DA, Campellone TR, Truong B, et al. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophr Bull. 2018;44:1010–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiauzzi E, Newell A. Editorial: patient perspective mental health apps in psychiatric treatment: a patient perspective on real world technology usage. JMIR Ment Health, 2019;6:12292 10.2196/12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wykes T, Brown M. Over promised, over-sold and underperforming? – e-health in mental health. J Ment Health. 2016;25:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biagianti B, Hidalgo-Mazzei D, Meyer N. Developing digital interventions for people living with serious mental illness: perspectives from three mHealth studies. Evid Based Ment Health. 2017;20:98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhugra D, Tasman A, Pathare S, et al. The WPA-Lancet Psychiatry Commission on the Future of Psychiatry. Lancet Psychiatry. 2017;4:775–818. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


